In 1972, two landmark papers in this journal described the partograph, 1 , 2 a chart designed to provide finite referral criteria for midwives working in peripheral clinics who needed to refer women in labour to Harare Hospital, Zimbabwe (then Rhodesia). This innovation coincided with influential reports from the National Maternity Hospital in Dublin of the ‘active management of labour’ (early amniotomy, proactive use of oxytocin and one‐to‐one nursing care) with the objective of achieving birth within a limited time frame. 3 The partograph was globally adopted, and has been used as part of the assessment of labour progress for nearly half a century. It was recommended by the World Health Organization (WHO) in the early 1990s as a routine tool for displaying the progress of labour. Despite its global acceptance, utilisation and correct completion rates as low as 31 and 3%, respectively, have been reported. 4
Following the update of its global recommendations on intrapartum care in 2018, 5 the WHO initiated a process to revise the partograph in light of recent evidence, including a new understanding of the individual variability of the progress of labours resulting in good perinatal outcomes, and the fact that many women do not experience a labour that conforms to the average rate on which the partograph design was based. 6 , 7 A large study and corresponding systematic reviews published in this journal 8 , 9 , 10 and subsequent analysis 11 failed to find evidence to support the use of a cervical dilatation rate of 1 cm/hour as a screening tool to predict adverse labour outcomes. The new WHO recommendations based on the emerging evidence on normal labour progression, as well as recommendations informed by the global shift towards improving experience of childbirth, 5 necessitated the design of a new labour monitoring tool called the WHO Labour Care Guide (Figure 1). WHO has also published a corresponding user's manual to support healthcare providers on how to successfully use the new tool. 12 The Labour Care Guide is distinct from previous partograph designs in its approach to labour duration, triggers for clinical interventions and its emphasis on respectful maternity care.
Figure 1.
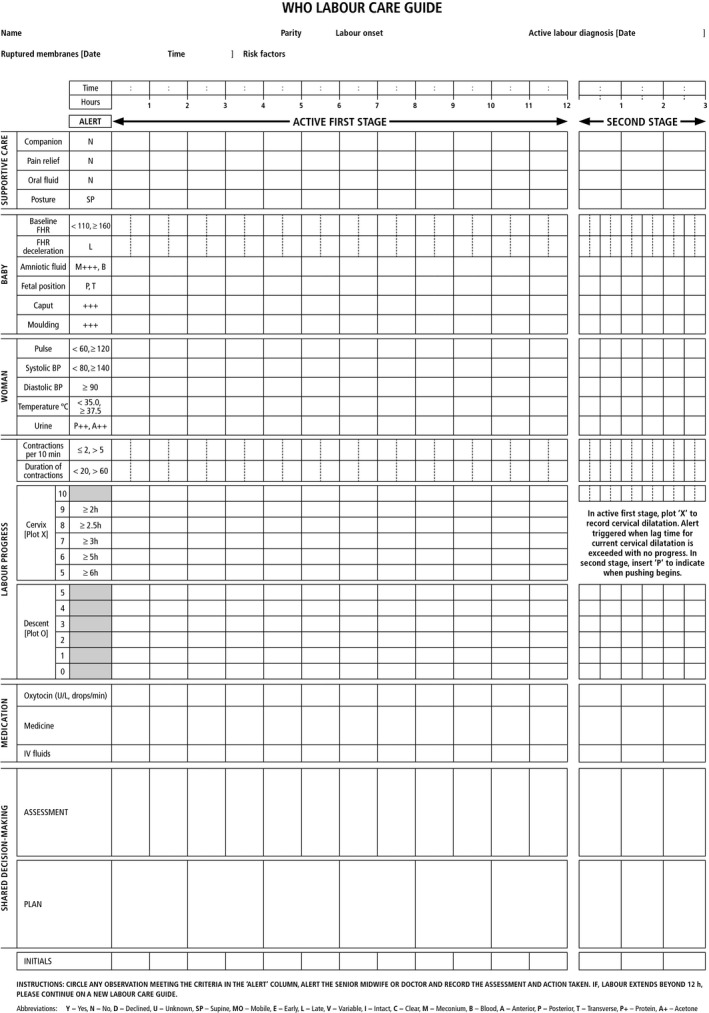
WHO Labour Care Guide.
It is anticipated that a departure from the familiar partograph format may provoke anxiety and even antipathy among healthcare professionals. Change is not easy and should not take place simply for the sake of change. This commentary explores the key concepts that motivated the WHO decision to review and revise the partograph format.
What has not changed?
Table 1 summarises the similarities and changes between the modified WHO partograph and the Labour Care Guide. The fundamental and innovative characteristic of the original ‘Philpott chart’ was the graphical representation of the progress of labour in terms of women's cervical dilatation and descent of the fetal presenting part, against time. 1 , 2 This concept has not changed other than in appearance, and retains its key position in the Labour Care Guide. In addition, formal regular recording of important clinical parameters describing duration and frequency of uterine activity and the wellbeing of the woman and baby, remain. The Labour Care Guide remains a record of clinical rather than ultrasound‐based parameters. 13
Table 1.
Similarities and differences between the partograph and the Labour Care Guide
| Modified WHO partograph | WHO Labour Care Guide |
|---|---|
| Similarities | |
| Graphical representation of the progress of labour in terms of women's cervical dilatation and descent of the fetal presenting part, against time | |
| Formal regular recording of important clinical parameters describing the wellbeing of the woman and baby | |
| Differences | |
| Active phase defined as starting from 4 cm of cervical dilatation | Active phase defined as starting from 5 cm of cervical dilatation |
| Fixed 1 cm/hour ‘alert’ line and ‘action’ lines | Evidence‐based time limits at each centimetre of cervical dilatation |
| No second‐stage section | Intensified monitoring in second stage |
| No recording of supportive care interventions | Explicit recording of labour companionship, pain relief, oral fluid intake and posture |
| Records strength, duration and frequency of uterine contractions | Records duration and frequency of uterine contractions |
| No explicit requirement to respond to deviations from expected observations of any labour parameter, other than cervical dilatation alert and action lines | Requires deviations to be highlighted and the corresponding response to be recorded by the provider |
What has changed and why?
Briefly, when compared with the previous partograph designs, the Labour Care Guide includes the following changes: the 1 cm/hour ‘alert’ line and its corresponding ‘action’ line have been replaced with evidence‐based time limits at each centimetre of cervical dilatation during active first stage of labour; the starting point of active first stage of labour is a cervical dilatation of 5 cm (instead of 4 cm or less); it includes a section for monitoring the second stage of labour; it includes a section to assess and promote the use of supportive interventions to improve overall childbirth experience; it no longer records strength of uterine contractions, which is difficult to clinically quantify and standardise; and it requires deviation from expected observations of any labour parameter to be highlighted and the corresponding response to be recorded by the provider.
Graphical display of the limits of ‘normal’ labour progression
The original partograph uses a line drawn at 1 cm/hour from the first cervical assessment thought to be indicative of active first stage of labour (3 or 4 cm), as the ‘alert’ or expected normal progress line, and a parallel line 2 hours (or more usually 4 hours) later as the ‘action’ line to identify prolonged labour. This format was based on the seminal work of Friedman and Kroll, which showed that the average rate of cervical dilatation in primiparous women was biphasic, being slower before 3 cm dilatation and approximately 1 cm/hour after 3 cm. 14 The fundamental flaw of translating this statistical summary of a large number of labours to a template for individual women is that it does not account for the variability in the rates of progression between women. In addition, the fact that the ‘action line’ threshold for prolonged labour is predetermined for the whole labour does not account for the non‐linear progress of individual women's labours. For example, if labour has progressed rapidly and is then arrested, it would take more than 4 hours to then reach the action line. On the other hand, if labour has been slow as the result of inadequate uterine activity and crossed the action line, it may subsequently progress normally but evoke anxiety because of being on the ‘wrong’ side of the action line, which becomes unhelpful in terms of guiding progress for the rest of the labour.
The revised chart for evaluating labour progress in the Labour Care Guide differs fundamentally in that the guiding parameters for labour progress are dynamic as opposed to being static. Rather than having a fixed‐rate limit over the entire active first stage of labour, consideration for intervention is guided by an evidence‐based time limit for each centimetre of cervical dilatation, derived from the 95th centiles of labour duration at different centimetre levels in women with normal perinatal outcomes. 6 As a result, even if the time to, for example, 9 cm dilatation is unusually fast, the expected limit for progressing from 9 to 10 cm remains the same. As for other parameters in the ‘alert’ column, if the time to progress from 9 to 10 cm, for example, exceeded 2 hours, then the relevant cervical assessment (‘x’) would be circled and the steps taken to respond would be documented in the ‘plan’ section.
The absence of the diagonal labour progress limit lines is the most striking difference between the Labour Care Guide and the partograph. Although the lines have been removed, the parameters remain, in a more current evidence‐based format, and there is an explicit requirement for a documented response when these parameters are exceeded.
Definition of active phase of first stage of labour
The original partograph defined the onset of the active phase of first stage of labour as 3 cm dilatation of the cervix, based on the point of inflection on the Friedman curve. Modification of the partograph led to shifting of this point to 4 cm by the WHO. 15 While the 3 or 4 cm thresholds were often described as reflecting Friedman's original work, it is interesting that Friedman recently noted that this was a misunderstanding of his work, and acknowledged that the point of inflection indeed varies from one woman to another. 16 The Labour Care Guide uses 5 cm, a point where the median dilatation rate in low‐risk women with no adverse perinatal outcomes was found to exceed 1 cm/hour (i.e. transition to a more rapid cervical dilatation progression). 10 This reduces premature designation of the active phase of labour, which has been a major iatrogenic cause of apparent poor labour progress and unnecessary interventions. 17 , 18
The Labour Care Guide acknowledges that the latent phase of the first stage of labour is problematic to define because it can be identified with certainty only in retrospect. The time of onset is often unclear, and its duration is very variable between women. Premature plotting of suspected latent phase is a potential source of unnecessary intervention inherent in the original design of the partograph, which designated 8 hours for the latent phase. This is avoided in the modified partograph designs and in the Labour Care Guide by only initiating documentation of labour progress once the active phase has been diagnosed.
The second stage of labour
An important limitation of the original partograph design and its modifications is that they do not include the second stage of labour. There is no explicit requirement to continue monitoring the condition of the woman and baby, or progression during the second stage of labour. Increased uterine activity compounded by maternal expulsive efforts make the second stage of labour a particularly critical time, and reduced vigilance at this time may lead to poor outcomes. This deficit has been addressed in the Labour Care Guide with closer attention to progress and the wellbeing of both woman and baby being required during the second stage.
Supportive intrapartum care
The Labour Care Guide is designed to emphasise the importance of the experiential dimension of childbirth by requiring explicit recording of evidence‐based practices that matter not only for women's positive birth experience but also for improving clinical outcomes for women and their newborns. The Labour Care Guide includes assessment of labour companionship, oral hydration, maternal position and mobility, and pain management, with the aim of promoting the use of these evidence‐based yet often neglected practices.
Labour monitoring‐to‐action
As indicated by its name, the Labour Care Guide is much more than a technical tool to monitor labour progress and a woman and her baby's wellbeing. The tool also prompts the comprehensive recordings of maternal vital signs, fetal wellbeing and labour progression, and contains reference values for maternal and fetal observations. To reinforce the care purpose of the tool, there is an explicit requirement to identify any observation that is inconsistent with good care, wellbeing or labour progress by circling it and documenting the clinical or supportive care response in consultation with the woman, prompting early recognition and action to improve the quality of care that the woman and her baby receive. In the ‘Assessment’ section the caregiver records the overall assessment and any additional findings not previously documented but important for labour monitoring, and in the ‘Plan’ section the care plan formulated in discussion with the woman is documented. This establishes the Labour Care Guide as a contemporaneous monitoring and response tool, rather than just a labour record that might be completed in retrospect.
Conclusion
Considerable research, knowledge synthesis, consultation, field testing and refinement have gone into the development of the Labour Care Guide. 19 , 20 Much future research on its implementation and impact on labour care and outcomes, including women's experiences of care, is needed. We hope that this commentary on the fundamental concepts underpinning its development will reassure healthcare providers that use of the new tool will not detract from, but rather will augment, the purposes of the original partograph. Much has changed in how we provide evidence‐based, respectful intrapartum care in the last 50 years, and we hope that the Labour Care Guide has responded to these advances and will encourage best practices that include the promotion of good quality, respectful and compassionate care for all women, newborns and their families.
Disclosure of interests
None declared. Completed disclosure of interests form available to view online as supporting information.
Contribution to authorship
The idea of this commentary was conceived by OTO. GJH prepared the first draft of the article with substantial input by OTO. All authors (GJH, OTO, SB, MBonet, MBucagu, BD, SD, HG, CSEH, VH, TL, BL, DL, PL, FEMcC, RP, ZQ, JPS, MES, PHB, VV, JPV) contributed to the content and development of the article. All authors reviewed and agreed to the final version of this manuscript.
Details of ethics approval
No ethics approval required.
Funding
This commentary was written without external funding. Open Access publication was supported by the UNDP/UNFPA/UNICEF/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), a cosponsored programme executed by the WHO.
Acknowledgements
We acknowledge the contributions that other members of the WHO Technical Working Group on Labour Care Guide made to the development of the Labour Care Guide: Richard Adanu, Jeffery Smith and Jeffery S.A. Stringer. The contents of this publication are the responsibility of the authors and do not reflect the views of the UNDP/UNFPA/UNICEF/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), World Health Organization, United States Agency for International Development (USAID) or the United States Government.
Supporting information
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Hofmeyr GJ, Bernitz S, Bonet M, Bucagu M, Dao B, Downe S, Galadanci H, Homer CSE, Hundley V, Lavender T, Levy B, Lissauer D, Lumbiganon P, McConville FE, Pattinson R, Qureshi Z, Souza JP, Stanton ME, ten Hoope‐Bender P, Vannevel V, Vogel JP, Oladapo OT. WHO next‐generation partograph: revolutionary steps towards individualised labour care. BJOG 2021; 10.1111/1471-0528.16694.128:1658–1662.
Data availability
Data sharing is not applicable to this article as no new data were created or analysed in this study.
References
- 1. Philpott RH, Castle WM. Cervicographs in the management of labour in primigravidae. I. The alert line for detecting abnormal labour. J Obstet Gynaecol Br Commonw 1972;79:592–8. [DOI] [PubMed] [Google Scholar]
- 2. Philpott RH, Castle WM. Cervicographs in the management of labour in primigravidae. II. The action line and treatment of abnormal labour. J Obstet Gynaecol Br Commonw 1972;79:599–602. [DOI] [PubMed] [Google Scholar]
- 3. O'Driscoll K, Jackson RJ, Gallagher JT. Prevention of prolonged labour. Br Med J 1969;2:477–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bedada KE, Huluka TK, Bulto GA, Roga EY. Low utilization of partograph and its associated factors among obstetric care providers in governmental health facilities at West Shoa Zone, Central Ethiopia. Int J Reprod Med 2020;2020:3738673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. WHO Recommendations: Intrapartum Care for a Positive Childbirth Experience. Geneva: World Health Organization; 2018. [PubMed] [Google Scholar]
- 6. Oladapo OT, Souza JP, Fawole B, Mugerwa K, Perdoná G, Alves D, et al. Progression of the first stage of spontaneous labour: a prospective cohort study in two sub‐Saharan African countries. PLoS Med 2018;15:e1002492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Abalos E, Oladapo OT, Chamillard M, Díaz V, Pasquale J, Bonet M, et al. Duration of spontaneous labour in ‘low‐risk’ women with ‘normal’ perinatal outcomes: a systematic review. Eur J Obstet Gynecol Reprod Biol 2018;223:123–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Souza JP, Oladapo OT, Fawole B, Mugerwa K, Reis R, Barbosa‐Junior F, et al. Cervical dilatation over time is a poor predictor of severe adverse birth outcomes: a diagnostic accuracy study. BJOG 2018;125:991–1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bonet M, Oladapo OT, Souza JP, Gulmezoglu AM. Diagnostic accuracy of the partograph alert and action lines to predict adverse birth outcomes: a systematic review. BJOG 2019;126:1524–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Oladapo OT, Diaz V, Bonet M, Abalos E, Thwin SS, Souza H, et al. Cervical dilatation patterns of 'low‐risk' women with spontaneous labour and normal perinatal outcomes: a systematic review. BJOG 2018;125:944–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Abalos E, Chamillard M, Diaz V, Pasquale J, Souza JP. Progression of the first stage of spontaneous labour. Best Pract Res Clin Obstet Gynaecol 2020;67:19–32. [DOI] [PubMed] [Google Scholar]
- 12. WHO Labour Care Guide: User's Manual. Geneva: World Health Organization; 2020. [Google Scholar]
- 13. Haberman S, Atallah F, Nizard J, Buhule O, Albert P, Gonen R, et al. A novel partogram for stages 1 and 2 of labor based on fetal head station measured by ultrasound: a prospective multicenter cohort study. Am J Perinatol 2020. 10.1055/s-0040-1702989 [DOI] [PubMed] [Google Scholar]
- 14. Friedman EA, Kroll BH. Computer analysis of labour progression. J Obstet Gynaecol Br Commonw 1969;76:1075–9. [DOI] [PubMed] [Google Scholar]
- 15. Managing Complications in Pregnancy and Childbirth: A Guide for Midwives and Doctors, 2nd edn. Geneva: World Health Organization; 2017. [Google Scholar]
- 16. Cohen WR, Friedman EA. Perils of the new labor management guidelines. Am J Obstet Gynecol 2015;212:420–7. [DOI] [PubMed] [Google Scholar]
- 17. Bailit JL, Dierker L, Blanchard MH, Mercer BM. Outcomes of women presenting in active versus latent phase of spontaneous labor. Obstet Gynecol 2005;105:77–9. [DOI] [PubMed] [Google Scholar]
- 18. Chuma C, Kihunrwa A, Matovelo D, Mahendeka M. Labour management and obstetric outcomes among pregnant women admitted in latent phase compared to active phase of labour at Bugando Medical Centre in Tanzania. BMC Pregnancy Childbirth 2014;14:68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Vogel JP, Comrie‐Thomson L, Pingray V, Gadama L, Galadanci H, Goudar S, et al. Usability, acceptability, and feasibility of the World Health Organization Labour Care Guide: a mixed‐methods, multicountry evaluation. Birth 2020;1–10. 10.1111/birt.12511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Laisser R, Danna VA, Bonet M, Oladapo OT, Lavender T. An exploration of health professional’s views of the new WHO Labour Care Guide: a qualitative evaluation. Afr J Midwifery Womens Health (in press). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analysed in this study.


