ABSTRACT
Frequencies of combined abnormalities of femoral version (FV) and acetabular version (AV) and of abnormalities of the McKibbin index are unknown. To investigate the prevalence of combined abnormalities of FV and AV and of abnormalities of the McKibbin index in symptomatic patients with femoroacetabular impingement (FAI), a retrospective, Institutional Review Board (IRB)-approved study of 333 symptomatic patients (384 hips) that were presented with hip pain and FAI was performed. The computed tomography/magnetic resonance imaging based measurement of central AV, cranial AV and FV was compared among five subgroups with distinguished FAI subgroups and patients that underwent a hip preservation surgery. The allocation to each subgroup was based on AP radiographs. Normal AV and FV were 10–25°. The McKibbin index is the sum of central AV and FV. Of patients that underwent a hip preservation surgery, 73% had a normal McKibbin index (20–50°) but 27% had an abnormal McKibbin index. Of all patients, 72% had a normal McKibbin index, but 28% had abnormal McKibbin index. The prevalence of combined abnormalities of FV and AV varied among subgroups: a higher prevalence of decreased central AV combined with decreased FV of patients with acetabular-retroversion group (12%) and overcoverage (11%) was found compared with mixed-type FAI (5%). Normal AV combined with normal FV was present in 41% of patients with cam-type FAI and in 34% of patients with overcoverage. Patients that underwent a hip preservation surgery had normal mean FV (17 ± 11°), central AV (19 ± 7°), cranial AV (16 ± 10°) and McKibbin index (36 ± 14°). Frequency of combined abnormalities of AV and FV differs between subgroups of FAI patients. Aggravated and compensated McKibbin index was prevalent in FAI patients. This has implications for open hip preservation surgery (surgical hip dislocation or femoral derotation osteotomy) or hip arthroscopy or non-operative treatment.
INTRODUCTION
Combined acetabular version (AV) and femoral version (FV) are becoming increasingly recognized as important factors in patients with femoroacetabular impingement (FAI). Both have a profound influence on hip range of motion [1, 2], especially internal and external rotations [1, 3]. Combined abnormalities of AV and FV were associated with hip pain and hip degeneration before the description of FAI [4]. Although this has been well investigated in the arthroplasty literature [5, 6], their prevalence and their influence on the hip joint in patients with FAI are discussed controversially. The prevalence of increased and decreased FV varies in the literature and depends on the measurement method. Previous reports are characterized by different definitions for the normal values of FV and a large heterogeneity of measurement techniques and imaging modalities. The reported prevalence of patients with abnormal FV in FAI ranged from 13% [7] to 24% [8] for <5° and from 15% [8] to 34% [1] for >20°. A prevalence of increased FV > 25° of 22% was found for patients with hip dysplasia [4]. The effect of= both increased and decreased FV was investigated for patients that underwent hip arthroscopy [9]. Recently, decreased FV has been identified as a factor associated with a revision surgery after hip arthroscopy at 2-year follow-up [10]. Variations in FV and McKibbin index were recognized as contributing factors to hip pain and FAI [11]. However, a recent systematic review investigating the influence of FV for the outcome of hip arthroscopy summarized five studies [12] and they reported that hips with normal FV and hips with femoral retroversion (FV < 5°) exhibited mostly similar outcome scores and similar failure rates [12]. It has been previously described that abnormal AV, mainly acetabular retroversion can be associated with hip pain [13], hip impingement [16] and the development of osteoarthritis of the hip [4, 15].
Variations in rotational morphology of both the acetabulum and proximal femur play a large role in the biomechanics of the hip joint. Severe femoral and acetabular retroversion was associated with anterior extra-articular subspine hip impingement [2, 16]. While increased FV was associated with in-toeing gait [17] and posterior extra-articular ischiofemoral hip impingement [14] that could potentially lead to hip instability. A recent study has shown that abnormalities of FV can outweigh the effect of cam impingement on hip internal rotation [18]. But these rotational deformities and abnormalities of the McKibbin index remain poorly understood and different measurement methods and definitions of abnormal FV add confusion.
The clinical significance of combined abnormalities of FV and AV in FAI patients undergoing a hip preservation surgery is controversial [1, 3, 19–21]. Especially two combined abnormalities of FV and AV could be a concern for patients undergoing a hip preservation surgery because they could aggravate each other. Increased FV combined with increased AV results in a high McKibbin index and increases hip internal rotation [1, 3] and could be contributing factors to anterior hip instability [14]. On the other hand, decreased FV combined with decreased AV results in a low McKibbin index and decreased hip internal rotation [1] and could aggravate anterior hip impingement conflict [2]. The aim of this study was to investigate the prevalence of these unfortunate combinations. Furthermore, it is unclear if specific subtypes of FAI are associated with abnormalities of the McKibbin index.
Thus, the purpose of this study is to investigate the prevalence of combined abnormalities of FV and AV and of abnormalities of the McKibbin index in symptomatic FAI patients.
PATIENTS AND METHODS
This is an IRB-approved retrospective study of 333 patients (384 hips) seeking to compare abnormalities of FV and AV among different distinguished subgroups of FAI. All symptomatic patients that had been referred to the university hospital of Bern in a 5-year period were evaluated for a hip preservation surgery (January 2011–December 2015). All patients presented with pain at the time of image acquisition. Inclusion criteria included the presence of hip pain, radiographic signs of skeletal maturity, no previous surgery of hip joint altering AV and/or FV, no post-traumatic condition, no avascular necrosis of the femoral head, availability of standard plain radiographs and the availability of either computed tomography (CT) [22] or magnetic resonance imaging (MRI) of the pelvis/hip including the distal femur condyles [23] to allow for measurement of FV according to the method described by Murphy et al. [24]. Out of a total of 462 patients (538 hips) of a previous study [11], 154 hips were excluded for the following reasons: hip dysplasia [78 patients (90 hips)], patients with Legg-Calvé-Perthes disease [25 patients (30 hips)], patients with no obvious pathology [19 patients (23 hips)] patients with osteoarthritis that underwent THA and avascular necrosis of the femoral head [5 patients (5 hips), Fig. 1]. This resulted in a total of 384 hips in 333 patients for inclusion in this study (Table I).
Fig. 1.
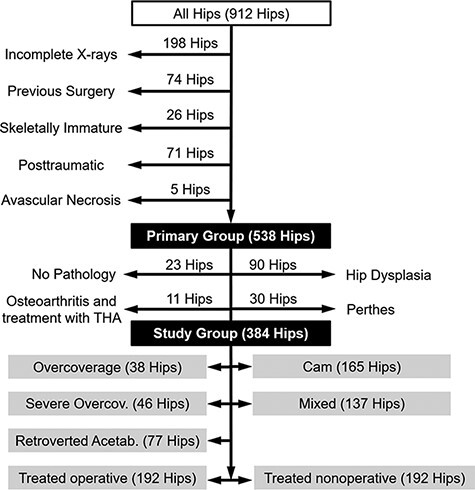
Exclusion criteria and subgroups for the patients are shown.
Table I.
(A) Definition of study groups. The allocation to a specific group was performed based on the morphological analysis of the conventional anteroposterior pelvic radiograph and the cross-table lateral radiographs of the hip. (B) Excluded patients are listed below with the definitions. See also Fig. 1
| (A) Group | Definition | Number of hips (patients) |
|---|---|---|
| Total | 384 (333) | |
| Subgroups | Five subgroups were analysed. | |
| Cam-type FAI | Alpha angle > 50° [29] with neck-shaft angle of 125–140° and with normal acetabulum (LCE angle 23–33°) [30], not all retroversion signs positive | 165 (142) |
| Mixed FAI* | Alpha angle > 50° [29] and LCE angle 34–39°, not all retroversion signs positive | 137 (118) |
| Overcoverage | LCE angle 34–39° [30] with alpha angle < 50°, not all retroversion signs positive | 38 (33) |
| Severe overcoverage | LCE angle > 39° [4], and/or protrusio acetabuli (defined as femoral head touching or crossing the ilioischial line) | 46 (41) |
| Acetabular Retroversion | Positive cross-over sign [13], positive ischial spine sign [53], positive posterior wall sign [13], retroversion index > 30% [35] and independent from alpha angle | 77 (65) |
| (B) Excluded | ||
| Hip Dysplasia | LCE angle < 22° [30] | 90 (78) |
| Perthes | Documented avascular necrosis of femoral head in childhood | 30 (25) |
| No obvious pathology | No obvious acetabular and femoral pathology, normal LCE angle (22–34°) and normal alpha angle (< 50°) | 23 (19) |
| THA | Patients treated with total hip arthroplasty (THA) | 11 (11) |
FAI = femoroacetabular impingement; LCE = lateral centre edge angle.
The hips in the mixed group can overlap with the other subgroups.
As part of the routine workup, all patients were clinically evaluated by one of the attending hip surgeons (KAS and MT) with more than 10 years of experience in the hip preservation surgery. This included a thorough acquisition of the patient history, a goniometric measurement of the hip range of motion, the evaluation of the anterior and posterior impingement tests [25], the assessment of hip instability [26] (using the posterior impingement test or the FABER tests), the assessment of abductor strength [27] and general joint laxity [28]. The posterior impingement test was used as a potential indicator for anterior hip instability [25].
Routine radiographic evaluation generally consisted of a supine anteroposterior (AP) pelvic radiograph taken with a standardized technique [25] and a cross-table lateral radiograph of the hip. Additional projections or functional views were acquired if needed for diagnosis or surgical planning. The AP pelvic radiograph was then assessed with previously described and validated computer software (Hip2Norm) to correct for pelvic tilt and obliquity if needed. This software allows accurate and reliable measurement of eight radiographic parameters of the hip. The alpha angle was measured as a measure of femoral asphericity on the axial cross table radiograph. All radiographic measurements were performed by two independent observers (TDL and IAST) with experience in musculoskeletal radiology. Good interobserver reliability was described in a previous publication [11].
Based on the analysis of the conventional supine radiographs, the patient cohort was subdivided into five different subgroups (Table I): (i) cam-type FAI (alpha angle >50°), (ii) Pincer-type FAI due to overcoverage [lateral centre edge (LCE) angle 35–39°], (iii) Pincer-type FAI due to severe overcoverage (LCE angle > 39°), (iv) Pincer FAI due to acetabular retroversion and (v) mixed-type FAI. The allocation to each group was based on previously published reference values for acetabular and femoral morphology (Table I) [4, 29, 30]. Half of the 384 hips (333 patients) with FAI underwent surgical treatment (192 hips, 50%), and the mean age of all patients was 33 years (Table II). An equal number of hips were treated operatively and non-operatively (192 and 192 hips, Table II) with 170 (51%) patients in the operative group and 163 (49%) patients in the non-operative group. Overall, hip arthroscopy and open surgical hip dislocation were most often performed for treatment of these patients (Table II). Hip arthroscopy was most often performed for patients with cam-type FAI while open surgical hip dislocation was most often performed for patients with severe overcoverage (Table II). A minority of patients with mixed-type FAI can be in more than one subgroup. The sum of the hips in subgroups can be higher than 384 hips.
Table II.
Radiographic parameters and surgical treatment of all patients and of the subgroups are shown
| Parameter | Overall study group | Patients treated surgically | Patients treated non-surgically | Overcoverage | Severe over-coverage | Retroverted acetabulum | Cam-type FAI | Mixed-type FAI |
|---|---|---|---|---|---|---|---|---|
| Number of hips (patients) | 384 (333) | 192 (170) | 192 (163) | 38 (33) | 46 (41) | 77 (65) | 165 (142) | 137 (118) |
| Age at imaging (years) | 33 ± 12 (14–71) |
31 ± 11 (14–60) |
33 ± 12 (16–71) |
30 ± 12 (15–71)* |
39 ± 11 (17–60) |
27 ± 9 (14–59) |
34 ± 12 (16–65) |
31 ± 11 (14–67) |
| LCE angle (°) | 33 ± 7 (23–63) |
33 ± 7 (23–63) |
33 ± 7 (23–52) |
35 ± 2 (32–40) |
45 ± 5 (36–63) |
35 ± 7 (23–54) |
28 ± 3 (23–35) |
37 ± 6 (23–63) |
| Acetabular index (%) | 1 ± 6 (−14–21) |
0 ± 6 (−14–17) |
2 ± 5 (−14–21) |
−1 ± 5 (−13–9) |
−6 ± 5 (−14–2) |
0 ± 5 (−14–15) |
5 ± 5 (−9–21) |
−1 ± 5 (−12–17) |
| Extrusion index (%) | 18 ± 7 (−3–36) |
18 ± 7 (−3–36) |
17 ± 7 (−1–36) |
15 ± 4 (10–26) |
7 ± 5 (−3–22) |
16 ± 7 (1–29) |
22 ± 5 (10–36) |
15 ± 5 (−1–29) |
| Retroversion index (%) | 15 ± 18 (0–100) |
15 ± 16 (0–63) |
15 ± 19 (0–100) |
11 ± 10 (0–29) |
6 ± 9 (0–28) |
43 ± 16 (30–100) |
8 ± 9 (0–45) |
22 ± 21 (0–100) |
| Neck-shaft angle (°) | 131 ± 6 (107–161) |
132 ± 7 (110–161) |
130 ± 7 (107–148) |
133 ± 8 (117–161) |
130 ± 7 (118–153) |
131 ± 7 (110–146) |
130 ± 6 (107–148) |
130 ± 7 (110–150) |
| Alpha angle (°) | 61 ± 11 (33–95) |
61 ± 11 (35–95) |
59 ± 11 (33–88) |
46 ± 7 (33–65) |
55 ± 13 (38–85) |
58 ± 12 (37–87) |
65 ± 9 (51–95) |
64 ± 9 (50–91) |
| Cross-over sign pos. (%) | 81% | 82% | 79% | 84% | 59% | 100% | 78% | 85% |
| Posterior wall sign pos. (%) | 60% | 59% | 61% | 50% | 41% | 100% | 53% | 68% |
| Ischial spine sign pos. (%) | 62% | 65% | 59% | 66% | 57% | 100% | 41% | 82% |
| COS, PWS, ISS and RI > 30% | 36% | 39% | 33% | 0% | 0% | 100% | 0% | 38% |
| Surgical treatment | 50% | 100% | 0% | |||||
| SHD | 33% | 65% | 0% | 32% | 48% | 30% | 22% | 40% |
| HAS | 15% | 29% | 0% | 5% | 7% | 8% | 24% | 9% |
| PAO | 3% | 6% | 0% | 0% | 0% | 16% | 0% | 6% |
Continuous values are expressed as mean ± SD with range in parentheses, LCE = lateral centre edge angle, FAI = femoroacetabular impingement; COS = Cross-over sign; ISS = ischial spine sign; PWS = posterior wall sign; RI = retroversion index; SHD = surgical hip dislocation including femoral osteotomies, PAO = periacetabular osteotomy; HAS = hip arthroscopy.
In order to calculate FV and AV, all symptomatic patients either underwent standardized protocol-specific magnetic resonance imaging (68% of the patients) and/or CT of the hip. The use of each of these imaging modalities for this purpose has been validated by previous studies that compared the measurement of FV [31] and AV [32] on MRI and on CT, which showed comparable results and good correlation [33]. MR arthrography [34, 35] was obtained according to a standardized technique. In brief, the scans were performed using a Siemens TRIO 3.0T high field scanner (Erlangen, Germany). The patients were positioned supine, and the feet were fixed using tape in a neutral position to prevent motion during scanning. A radial proton density sequence was acquired for evaluation of chondrolabral lesions. Sagittal and coronal proton density-weighted and axial T1-weighted were acquired of which the axial slices were used for measurements of FV and AV. A second axial T1-weighted sequence of the femoral condyles was used for measurements of FV [11, 36]. These sequences were taken immediately after the original axial T1-weighted sequences and the patient was instructed not to move the leg to ensure the accurate measurement. If needed for surgical planning, CT was acquired in a minority of patients according to a previously validated protocol [2] in supine position. A slice thickness of 2 mm and an interval of reconstruction of 1.7 mm were chosen. Radiation dose of the pelvic CT scan had a range between 119 and 539 mGycm (dose length product).
FV was measured according to Murphy et al. [24] by two different independent observers (TDL and FS) using three reference points on transverse slices at different femoral locations: the femoral head centre, the centre of the base of the femoral neck and the condylar axis. The method described by Murphy et al. is performed by superimposing the centre of the femoral head on the CT section through the base of the femoral neck [24] and showed better reproducibility (variance of 0.4° and a standard deviation of 0.6°) compared with one single transverse CT section through the femoral neck [37]. This method showed a good reproducibility [36] and the similarity to method of a summation image described by Tönnis et al. [4]. Normal FV was 10–25° according to Tönnis et al. [4]. Decreased FV was defined as FV < 10°. Other reported normal values [38–42] for FV ranged from 8° to 18° using various measurement methods. Definitions and categories for FV vary in the orthopaedic literature. Reported thresholds for categorizing FV were >25° [43], <10° [4, 33], <5° [7, 44] and <0° [40] and for increased FV reported thresholds were >15° [44], >22° [33] and >25° [4, 7, 43].
Central AV was measured by two different observers according to Hetsroni [45] (3 o’clock version) was defined as the angle between a sagittal line and a line connecting the anterior and posterior acetabular rim on the level of the femoral head centre. Pelvic positioning was neutralized connecting the bilateral centre of the femoral head on axial images as described previously [11]. Normal central AV and FV were defined from 10° to 25° (Fig. 2) [4]. Decreased AV was defined as <10°. Increased AV and FV were characterized as >25°. Abnormal AV and FV were defined as <10° or >25° (Fig. 3). Cranial AV was measured similarly to the central AV on an axial slice 5 mm distal to the acetabular roof according to Jamali et al. [46]. The McKibbin index [9, 47] is defined as the sum of FV and AV (also called Combined femoral torsion and acetabular version index [1]). An increased McKibbin index was defined as >50° and a decreased McKibbin index was defined as <20°.
Fig. 2.

The nine possible combinations of FV and AV are shown. Two combinations (top left, A and right below, I) had an aggravated McKibbin index (red). Normal values for both AV and FV were between 10° and 25° according to Tönnis et al. [4]. The two combinations on below left (C) and on top right (G) had a compensated McKibbin index.
Fig. 3.

(A and B) Prevalences of possible combinations of FV and AV are shown for all patients (A) and for patients treated surgically (B).
Two different observers (TDL and FS) measured FV and AV independently at two different time points on a random sample of 50 hips taken from the patient cohort. A good agreement (defined as intraclass correlation coefficient [ICC] >0.8 [48]) was found for both reproducibility and reliability of FV (Intraobserver ICC of observer 1 of 0.93, ranging from 0.87 to 0.96 and Intraobserver ICC of observer 2 of 0.97, ranging from 0.95 to 0.98). A substantial agreement (defined as ICC >0.6 [48]) was found for reproducibility and reliability of central AV (ICC of observer 1 of 0.8, ranging from 0.65 to 0.89 and ICC of observer 2 of 0.78, ranging from 0.61 to 0.87). Interobserver agreement for FV was 0.96 (0.94–0.97) and for AV was 0.75 (0.62–0.83).
A power analysis and sample size calculation was performed for FV in a fixed effect, one-way analysis of variance (ANOVA) design with a level of significance of 1%, beta error of 5%, given previously reported mean values of FV of 21° in 27 normal hips [14], 10° in 33 cam-type hips [49], 18° in 10 pincer hips [49] and 58° in 13 valgus hips [14] and a published standard deviation of 17° [14]. With five groups, this resulted in a total number of 140 hips (28 hips per group). A post-hoc power analysis using the results of FV of the group with cam-type FAI and alpha of 1% (0.01) showed a power of 97% (clincalc.com, accessed on 15 September 2021).
A normal distribution was present for all continuous parameters, which were confirmed using the Kolmogorov–Smirnov test. Continuous variables among the study groups were compared using the univariate ANOVA. Adjustment for multiple comparisons was done with the Bonferroni correction for five groups (0.05/5 = 0.01). A P-value below 0.01 was considered significant. Continuous values for each study group were compared using the unpaired Student’s t-test. Categorical variables were compared among the study groups using the Chi-squared test.
RESULTS
Of patients that underwent a hip preservation surgery, 73% had a normal McKibbin index (20–50°) but 27% had an abnormal McKibbin index. Of all patients, 72% had a normal McKibbin index but 28% had an abnormal McKibbin index (Table III).
Table III.
Results of mean FV and AV and prevalence analysis for FV and McKibbin index are shown
| Parameter | Overall study group | Patients treated surgically | Patients treated non-surgically | Overcoverage | Severe over-coverage | Retroverted acetabulum | Cam-type FAI | Mixed-type FAI |
|---|---|---|---|---|---|---|---|---|
| Number of hips (patients) | 384 (333) | 192 (170) | 192 (163) | 38 (33) | 46 (41) | 77 (65) | 165 (142) | 137 (118) |
| Femoral version (°) [24] | 16 ± 11 (−16–58) |
17 ± 11 (−15–58) |
16 ± 11 (−16–55) |
17 ± 14 (−16–58) |
20 ± 11 (−12–47) |
16 ± 11 (−4–48) |
15 ± 10 (−15–55) |
17 ± 11 (−13–46) |
| Central Acetabular version (°) | 18 ± 7 (−1–38) |
19 ± 7 (1–35) |
17 ± 7 (−1–35) |
20 ± 5 (5–29) |
19 ± 7 (6–35) |
13 ± 6 (−1–26) |
19 ± 6 (2–33) |
16 ± 7 (−1–33) |
| Cranial Acetabular version (°) | 16 ± 7 (−21–40) |
16 ± 10 (−21–40) |
16 ± 9 (−14–39) |
18 ± 8 (−9–33) |
20 ± 10 (−5–40) |
9 ± 10 (−21–28)* |
19 ± 8 (−8–35) |
14 ± 10 (−21–34) |
| McKibbin index (°) [47] | 34 ± 14 (−5–83) |
36 ± 14 (−5–80) |
33 ± 14 (−5–83) |
37 ± 17 (2–80) |
39 ± 14 (4–71) |
28 ± 13 (−1–72)* |
35 ± 13 (−5–83) |
32 ± 13 (−5–77) |
| Prevalence analysis | ||||||||
| McKibbin index 20–50° | 72% | 73% | 70% | 66% | 70% | 66% | 76% | 72% |
| McKibbin index <20 or >50° | 28% | 27% | 30% | 34% | 30% | 34% | 24% | 28% |
| Decreased FV <10° | 25% | 21% | 30% | 29%* | 11% | 31%* | 28%* | 23% |
| Increased FV >25° | 20% | 21% | 19% | 29% | 24% | 14% | 15% | 20% |
| Abnormal FV (<10° or >25°) | 45% | 42% | 49% | 58%* | 35% | 45% | 43% | 44% |
| Normal FV (10–25°) | 55% | 56% | 51% | 42%* | 65% | 55% | 57% | 56% |
Continuous values are expressed as mean ± SD with range in parentheses, level of significance was adjusted with a Bonferroni correction for five groups (0.05/5 = 0.01), FAI = femoroacetabular impingement.
Significant difference compared with severe overcoverage.
The prevalence of abnormalities of FV and AV varied between the subgroups: Decreased AV combined with decreased FV was prevalent in acetabular-retroversion group (12%) and overcoverage (11%). None of the patients with severe overcoverage had decreased AV combined with decreased FV (Table IV).
Table IV.
Prevalence of nine combinations of FV and AV are displayed. Visualization of the nine combinations are shown in Fig. 3A for all patients, in Fig. 4 for patients with cam-type FAI, in Fig. 5 for patients with mixed-type FAI and in Fig. 3B for patients treated surgically
| Group | Group name | Overall Prevalence | Combination | Cam-type FAI | Mixed-type FAI | Overcoverage | Severe overcoverage | Acetabular Retroversion | |
|---|---|---|---|---|---|---|---|---|---|
| A | Increased AV with increased FV | 3% | Aggravated | 4% | 2% | 5% | 2% | 1% | Fig. 3A |
| B | Normal AV with increased FV | 15% | Moderate | 11% | 15% | 24% | 20% | 8% | Fig. 3B |
| C | Decreased AV with increased FV | 2% | Compensated | 1% | 4% | 0% | 2% | 5% | Fig. 3C |
| D | Increased AV with normal FV | 10% | Moderate | 11% | 7% | 8% | 17% | 0% | Fig. 3D |
| E | Normal AV with normal FV | 38% | Normal | 41% | 37% | 34% | 37% | 34% | Fig. 3E |
| F | Decreased AV with normal FV | 7% | Moderate | 4% | 11% | 0% | 11% | 21% | Fig. 3F |
| G | Increased AV with decreased FV | 2% | Compensated | 4% | 1% | 2% | 2% | 0% | Fig. 3G |
| H | Normal AV with decreased FV | 18% | Moderate | 21% | 17% | 16% | 9% | 19% | Fig. 3H |
| I | Decreased AV with decreased FV | 5% | Aggravated | 3% | 6% | 11% | 0% | 12% | Fig. 3I |
Aggravated combination (red) was present in groups A and I. FV = femoral version; AV = acetabular version.
aggravated = red moderate = yellow compensated = green Normal = green.
The prevalence of combined normal AV and normal FV varied between the subgroups (Figs 3 and 4): The prevalence of normal FV combined with normal AV was lower of the patients with overcoverage (34%) and acetabular retroversion (34%, Table IV) compared with severe overcoverage (37%) and mixed-type FAI (37%, Fig. 5). Normal AV combined with normal FV was present in 41% of patients with cam-type FAI.
Fig. 4.

Prevalences of possible combinations of FV and AV are shown for patients with cam-type FAI. Two combinations (top left, and right below) had an aggravated McKibbin index (red). Normal values for both AV and FV were between 10° and 25° according to Tönnis et al. [4]. The two combinations on below left and on top right had a compensated McKibbin index.
Fig. 5.

Prevalences of possible combinations of FV and AV are shown for patients with mixed-type FAI. Two combinations (top left, and right below) had an aggravated McKibbin index (red). Normal values for both AV and FV were between 10° and 25° according to Tönnis et al. [4]. The two combinations on below left and on top right had a compensated McKibbin index.
The prevalence of the abnormal McKibbin index varied among subgroups. Patients with overcoverage had higher prevalence (34%) of the abnormal McKibbin index (<20° or >50°) compared with patients with cam-type FAI (24%, Table III). Of all patients, decreased AV combined with decreased FV was present in 5% (Table IV) while increased AV (>25°) combined with increased FV (>25°) was present in 3% (Table IV).
The prevalence of decreased FV (FV < 10°) combined with normal AV was higher in patients with cam-type FAI (21%, Fig. 4) compared with mixed-type FAI (17%, Table IV) and compared with patients that underwent a hip preservation surgery (14%). Mean FV of patients treated with a hip preservation surgery (16 ± 10°) and of all subgroups was in the normal range (Table III).
DISCUSSION
Variations of AV and FV have been increasingly recognized as important factors in FAI patients undergoing a hip preservation surgery [3]. The vast majority of the literature on FAI predates the recent advances in understanding of FAI and combinations of FV and AV and its impact on the hip [4, 24, 50]. The aim of this study was to detect the prevalence of combined abnormalities of AV and FV and the prevalence of abnormalities of the McKibbin index in FAI patients.
Most importantly, 28% of all patients presented with a decreased or increased McKibbin index (Table III). The prevalence of a decreased and increased McKibbin index varied among subgroups. Decreased AV combined with decreased FV was prevalent in acetabular-retroversion group (12%) and overcoverage (11%). Theoretically, FAI patients with an increased or decreased McKibbin index (aggravated McKibbin index) could be at risk for anterior or posterior (Fig. 2) extra-articular hip impingement [2]. Interestingly, the mean of AV and FV of all patients was in the normal range (10–25°, Table III). The mean values of FV and AV could be neutralized by subgroups with increased and decreased FV/AV.
Comparing the results for the prevalence of combined abnormalities of AV and FV (Table III) with the results found in the literature, a previous study found a slightly higher prevalence. Tönnis and Heinecke [4] reported a prevalence of 16% of combined abnormalities of AV and FV using the same thresholds for abnormal AV and FV. They found that 10% of their patients had decreased AV combined with decreased FV while 6% had increased AV (>25°) combined with increased FV (>25°) [4]. Another study defined a normal McKibbin index (Combined femoral torsion and acetabular version index) between 20° and 45° and found that 19% of 442 hips had increased AV (>20°) combined with increased FV (>20°) while 7% had decreased AV (<15°) combined with decreased FV (<10°) [1]. Interestingly, 21% of the patients with cam-type FAI (without pincer deformity) had normal AV combined with decreased FV. This is important because decreased FV was associated with anterior extra-articular subspine hip impingement [2].
There are different definitions for normal values of AV and FV and for prevalence of abnormal FV and AV [1, 7, 51]. In a previous study by Tibor et al. [51] and in contrast to the results of the current study, normal AV was defined between 15° and 20° (Supplementary Table I). They reported a prevalence of normal [51] AV of 40% while others reported a prevalence of normal AV of 27% using the same definition [1]. The reason for a discrepancy compared with other studies could be different definitions of normal AV used in other studies [1, 51].
Using the normal range of 10–25°, only 38% of patients presented with normal FV combined with normal AV (Table IV). A previous large cohort study [1] reported a prevalence of normal FV combined with normal AV of 7% (Supplementary Table II) using different definitions for normal values (10–20° for FV and 15–20° for AV).
When analysing the prevalence of abnormalities of the McKibbin index for the subgroups, considerable differences between the subgroups were detected. Hips with abnormalities of the McKibbin index (Fig. 3A) are potentially at risk for extra-articular hip impingement (aggravated McKibbin index) and for decreased or increased hip internal rotation [3]. On the other hand, decreased AV combined with increased FV could potentially compensate (Figs 2 and 3A) each other and this subgroup had a mean McKibbin index in the normal range. The same effect could play a role for hips with increased AV combined with decreased FV and this combination could be called compensated combination (Fig. 2, Table IV) and also had a mean McKibbin index in the normal range.
This study has implications. We recommend to analyse both FV and AV in every patient evaluated for the hip preservation surgery, especially for patients with mixed-type FAI (Fig. 5). Therefore, we changed clinical practice and assess the AV and FV in all patients evaluated for the hip preservation surgery to search for combined abnormalities. This study supports patient-specific evaluation of young FAI patients [35] because of the variability of FV and AV. This could help to decide for operative or non-operative treatment, for example, in case of a compensated combination (e.g. increased AV combined with decreased FV), non-operative treatment could theoretically be a successful option before operative treatment.
There are several limitations for this study. First, despite the large number of patients, this study group does not represent a cross-sectional analysis. Although collected consecutively, it rather should be considered as a selective patient group from a university hospital, which may contain a higher percentage of abnormal values compared with the general population. There is a potential selection bias of patients seen in a university centre. This study is a prevalence analysis and we cannot comment on surgical outcome or on implications for femoral osteotomies. Second, measurements of FV depend on the used measurement method and should be interpreted with caution. The results of FV are based on the Murphy method while other measurements methods showed variation in FV [36]. In addition, we did not standardize the values for AV to the anterior pelvic plane and had no three-dimensional information [52]. Given a mean pelvic tilt of 4° in a supine position, we could generally have underestimated AV [53]. However, by using the same method of previous studies [45], this allows for a direct comparison to the reported values from previous studies. Third, the age of the patients ranged from 14 to 71 years. This might be problematic because AV and FV could be age-dependent, and associations with age were previously described [1]. However, the change of AV and FV occurs mostly in childhood and adolescence before closure of the growth plates [54]. To the best of the author’s knowledge and in accordance to previous reports, there is no evidence of relevant age-dependent changes of AV or FV once skeletal maturity is reached, except the changes associated with the development of osteoarthritis [4]. Since all hips from the study group had closed physes and the mean age of the study group was 32 years, this should not have influenced the results. In addition, some patients were analysed in more than one subgroup, because patients with mixed-type FAI can be in more than one subgroup. This could have influenced the results, but only few patients were included in more than one subgroup.
This study differs from the previous reports for variable reasons. Some authors did not distinguish among subgroups of impingement [45, 55], such as acetabular retroversion. Acetabular retroversion is a known cause for pincer-type FAI [16, 53]. In contrast, this analysis contains a large number of symptomatic FAI patients, linking combined abnormalities of FV and AV with subtypes of FAI.
CONCLUSION
In summary, an abnormal McKibbin index was prevalent in 27% of FAI patients that underwent open hip preservation surgery or hip arthroscopy. The frequency of combined abnormalities of AV and FV differs between subgroups of FAI patients. The aggravated and compensated McKibbin index was prevalent in FAI patients. Based on the results of this study, evaluation of AV and FV for young and active patients with hip pain can be recommended. This could help to detect patients with abnormalities of the McKibbin index in order to guide surgical decision-making and optimize patient outcomes of patients undergoing hip arthroscopy or open hip preservation surgery. This could also help for decision-making for operative or non-operative treatment.
Supplementary Material
ACKNOWLEDGEMENTS
We thank Dr Inga Todorski for her support for this study.
Contributor Information
Till D Lerch, Department of Diagnostic, Interventional and Paediatric Radiology, University of Bern, Inselspital, Bern University Hospital, Bern, Switzerland.
Tiziano Antioco, Department of Diagnostic, Interventional and Paediatric Radiology, University of Bern, Inselspital, Bern University Hospital, Bern, Switzerland.
Malin K Meier, Department of Orthopaedic Surgery, University of Bern, Inselspital, Bern University Hospital, Bern, Switzerland.
Adam Boschung, Department of Orthopaedic Surgery, University of Bern, Inselspital, Bern University Hospital, Bern, Switzerland; Department of Orthopaedic Surgery and Traumatology, Fribourg Cantonal Hospital, University of Fribourg, Fribourg, Switzerland.
Markus S Hanke, Department of Orthopaedic Surgery, University of Bern, Inselspital, Bern University Hospital, Bern, Switzerland.
Moritz Tannast, Department of Orthopaedic Surgery, University of Bern, Inselspital, Bern University Hospital, Bern, Switzerland; Department of Orthopaedic Surgery and Traumatology, Fribourg Cantonal Hospital, University of Fribourg, Fribourg, Switzerland.
Klaus A Siebenrock, Department of Orthopaedic Surgery, University of Bern, Inselspital, Bern University Hospital, Bern, Switzerland.
Florian Schmaranzer, Department of Diagnostic, Interventional and Paediatric Radiology, University of Bern, Inselspital, Bern University Hospital, Bern, Switzerland.
Simon D Steppacher, Department of Orthopaedic Surgery, University of Bern, Inselspital, Bern University Hospital, Bern, Switzerland.
SUPPLEMENTARY DATA
Supplementary Data are available at Journal of Hip Preservation Surgery online.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
Swiss National Science Foundation (P2BEP3_195241) to Till Lerch. Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research and that informed consent for participation in the study was obtained.
LIST OF ABBREVIATIONS
FV = femoral version; AV = acetabular version; FAI = femoroacetabular impingement; CT = computed tomography; MRI = magnetic resonance imaging; IRB = Institutional Review Board
REFERENCES
- 1. Chadayammuri V, Garabekyan T, Bedi A et al. Passive hip range of motion predicts femoral torsion and acetabular version. J Bone Joint Surg Am 2016; 98: 127–34. [DOI] [PubMed] [Google Scholar]
- 2. Lerch TD, Boschung A, Todorski IAS et al. Femoroacetabular impingement patients with decreased femoral version have different impingement locations and intra- and extraarticular anterior subspine FAI on 3D-CT-based impingement simulation: implications for hip arthroscopy. Am J Sports Med 2019; 47: 3120–32. doi: 10.1177/0363546519873666 [DOI] [PubMed] [Google Scholar]
- 3. Shin J, Adeyemi TF, Hobson T et al. The bipolar hip: how acetabular and femoral pathomorphology affects hip motion in femoral acetabular impingement syndrome. Arthroscopy 2020; 36: 1864–71.doi: 10.1016/j.arthro.2020.02.044. [DOI] [PubMed] [Google Scholar]
- 4. Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am 1999; 81: 1747–70. [DOI] [PubMed] [Google Scholar]
- 5. Bunn A, Colwell CW, D’Lima DD. Bony impingement limits design-related increases in hip range of motion. Clin Orthop Relat Res 2012; 470: 418–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Shoji T, Yasunaga Y, Yamasaki T et al. Low femoral antetorsion and total hip arthroplasty: a risk factor. Int Orthop 2015; 39: 7–12. [DOI] [PubMed] [Google Scholar]
- 7. Dolan MM, Heyworth BE, Bedi A et al. CT reveals a high incidence of osseous abnormalities in hips with labral tears. Clin Orthop Relat Res 2011; 469: 831–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kelly BT, Bedi A, Robertson CM et al. Alterations in internal rotation and alpha angles are associated with arthroscopic cam decompression in the hip. Am J Sports Med 2012; 40: 1107–12. [DOI] [PubMed] [Google Scholar]
- 9. Fabricant PD, Fields KG, Taylor SA et al. The effect of femoral and acetabular version on clinical outcomes after arthroscopic femoroacetabular impingement surgery. J Bone Joint Surg Am 2015; 97: 537–43. [DOI] [PubMed] [Google Scholar]
- 10. Redmond JM, Gupta A, Dunne K et al. What factors predict conversion to THA after arthroscopy? Clin Orthop Relat Res 2017; 475: 2538–45.doi: 10.1007/s11999-017-5437-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lerch TD, Todorski IAS, Steppacher SD et al. Prevalence of femoral and acetabular version abnormalities in patients with symptomatic hip disease: a controlled study of 538 hips. Am J Sports Med 2018; 46: 122–34. [DOI] [PubMed] [Google Scholar]
- 12. Wang C, Sun Y, Ding Z et al. Influence of femoral version on the outcomes of hip arthroscopic surgery for femoroacetabular impingement or labral tears: a systematic review and meta-analysis. Orthop J Sports Med 2021; 9: 23259671211009190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br 1999; 81-B: 281–8. [DOI] [PubMed] [Google Scholar]
- 14. Siebenrock KA, Steppacher SD, Haefeli PC et al. Valgus hip with high antetorsion causes pain through posterior extraarticular FAI. Clin Orthop Relat Res 2013; 471: 3774–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Giori NJ, Trousdale RT. Acetabular retroversion is associated with osteoarthritis of the hip. Clin Orthop Relat Res 2003: 263–9. doi: 10.1097/01.blo.0000093014.90435.64. [DOI] [PubMed] [Google Scholar]
- 16. Lerch TD, Siegfried M, Schmaranzer F et al. Location of intra- and extra-articular hip impingement is different in patients with pincer-type and mixed-type femoroacetabular impingement due to acetabular retroversion or protrusio acetabuli on 3D CT-based impingement simulation. Am J Sports Med 2020; 48: 661–72. [DOI] [PubMed] [Google Scholar]
- 17. Lerch TD, Eichelberger P, Baur H et al. Prevalence and diagnostic accuracy of in-toeing and out-toeing of the foot for patients with abnormal femoral torsion and femoroacetabular impingement: implications for hip arthroscopy and femoral derotation osteotomy. Bone Joint J 2019; 101-B: 1218–29. [DOI] [PubMed] [Google Scholar]
- 18. Kraeutler MJ, Chadayammuri V, Garabekyan T et al. Femoral version abnormalities significantly outweigh effect of cam impingement on hip internal rotation. J Bone Joint Surg Am 2018; 100: 205–10. [DOI] [PubMed] [Google Scholar]
- 19. Audenaert EA, Peeters I, Vigneron L et al. Hip morphological characteristics and range of internal rotation in femoroacetabular impingement. Am J Sports Med 2012; 40: 1329–36. [DOI] [PubMed] [Google Scholar]
- 20. Bouma HW, Hogervorst T, Audenaert E et al. Can combining femoral and acetabular morphology parameters improve the characterization of femoroacetabular impingement? Clin Orthop Relat Res 2015; 473: 1396–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ejnisman L, Philippon MJ, Lertwanich P et al. Relationship between femoral anteversion and findings in hips with femoroacetabular impingement. Orthopedics 2013; 36: e293–300. [DOI] [PubMed] [Google Scholar]
- 22. Tannast M, Kubiak-Langer M, Langlotz F et al. Noninvasive three-dimensional assessment of femoroacetabular impingement. J Orthop Res 2007; 25: 122–31. [DOI] [PubMed] [Google Scholar]
- 23. Sutter R, Dietrich TJ, Zingg PO et al. Assessment of femoral antetorsion with MRI: comparison of oblique measurements to standard transverse measurements. AJR Am J Roentgenol 2015; 205: 130–5. [DOI] [PubMed] [Google Scholar]
- 24. Murphy SB, Simon SR, Kijewski PK et al. Femoral anteversion. J Bone Joint Surg Am 1987; 69: 1169–76. [PubMed] [Google Scholar]
- 25. Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis—what the radiologist should know. AJR Am J Roentgenol 2007; 188: 1540–52. [DOI] [PubMed] [Google Scholar]
- 26. Martin HD, Palmer IJ. History and physical examination of the hip: the basics. Curr Rev Musculoskelet Med 2013; 6: 219–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Medical Research Council . Aids to the Investigation of Peripheral Nerve Injuries. War Memorandum No 7, revised 2nd edn. London: HM Stationery Office, 1943. [Google Scholar]
- 28. Naal FD, Hatzung G, Müller A et al. Validation of a self-reported Beighton score to assess hypermobility in patients with femoroacetabular impingement. Int Orthop 2014; 38: 2245–50. [DOI] [PubMed] [Google Scholar]
- 29. Nötzli HP, Wyss TF, Stoecklin CH et al. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br 2002; 84-B: 556–60. [DOI] [PubMed] [Google Scholar]
- 30. Tannast M, Hanke MS, Zheng G et al. What are the radiographic reference values for acetabular under- and overcoverage?. Clin Orthop Relat Res 2015; 473: 1234–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hesham K, Carry PM, Freese K et al. Measurement of femoral version by MRI is as reliable and reproducible as CT in children and adolescents with hip disorders. J Pediatr Orthop 2017; 37: 557–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Goronzy J, Blum S, Hartmann A et al. Is MRI an adequate replacement for CT scans in the three-dimensional assessment of acetabular morphology? Acta Radiol 2019; 60: 726–34. [DOI] [PubMed] [Google Scholar]
- 33. Botser IB, Ozoude GC, Martin DE et al. Femoral anteversion in the hip: comparison of measurement by computed tomography, magnetic resonance imaging, and physical examination. Arthroscopy 2012; 28: 619–27. [DOI] [PubMed] [Google Scholar]
- 34. Schmaranzer F, Todorski IAS, Lerch TD et al. Intra-articular lesions: imaging and surgical correlation. Semin Musculoskelet Radiol 2017; 21: 487–506. [DOI] [PubMed] [Google Scholar]
- 35. Steppacher SD, Lerch TD, Gharanizadeh K et al. Size and shape of the lunate surface in different types of pincer impingement: theoretical implications for surgical therapy. Osteoarthritis Cartilage 2014; 22: 951–8. [DOI] [PubMed] [Google Scholar]
- 36. Schmaranzer F, Lerch TD, Siebenrock KA et al. Differences in femoral torsion among various measurement methods increase in hips with excessive femoral torsion. Clin Orthop Relat Res 2019; 477: 1073–83.doi: 10.1097/CORR.0000000000000610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Weiner DS, Cook AJ, Hoyt WA et al. Computed tomography in the measurement of femoral anteversion. Orthopedics 1978; 1: 299–306. [PubMed] [Google Scholar]
- 38. Bråten M, Terjesen T, Rossvoll I. Femoral anteversion in normal adults. Ultrasound measurements in 50 men and 50 women. Acta Orthop Scand 1992; 63: 29–32. [DOI] [PubMed] [Google Scholar]
- 39. Kingsley PC, Olmsted KL. A study to determine the angle of anteversion of the neck of the femur. J Bone Joint Surg Am 1948; 30: 745–51. [PubMed] [Google Scholar]
- 40. Koerner JD, Patel NM, Yoon RS et al. Femoral version of the general population: does “normal” vary by gender or ethnicity? J Orthop Trauma 2013; 27: 308–11. [DOI] [PubMed] [Google Scholar]
- 41. Strecker W, Keppler P, Gebhard F et al. Length and torsion of the lower limb. J Bone Joint Surg Br 1997; 79-B: 1019–23. [DOI] [PubMed] [Google Scholar]
- 42. Toogood PA, Skalak A, Cooperman DR. Proximal femoral anatomy in the normal human population. Clin Orthop Relat Res 2009; 467: 876–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Fabricant PD, Bedi A, De La Torre K et al. Clinical outcomes after arthroscopic psoas lengthening: the effect of femoral version. Arthroscopy 2012; 28: 965–71. [DOI] [PubMed] [Google Scholar]
- 44. Ferro FP, Ho CP, Briggs KK et al. Patient-centered outcomes after hip arthroscopy for femoroacetabular impingement and labral tears are not different in patients with normal, high, or low femoral version. Arthroscopy 2015; 31: 454–9. [DOI] [PubMed] [Google Scholar]
- 45. Hetsroni I, Dela Torre K, Duke G et al. Sex differences of hip morphology in young adults with hip pain and labral tears. Arthroscopy 2013; 29: 54–63. [DOI] [PubMed] [Google Scholar]
- 46. Jamali AA, Mladenov K, Meyer DC et al. Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the “cross-over-sign”. J Orthop Res 2007; 25: 758–65. [DOI] [PubMed] [Google Scholar]
- 47. McKibbin B. Anatomical factors in the stability of the hip joint in the newborn. J Bone Joint Surg Br 1970; 52-B: 148–59. [PubMed] [Google Scholar]
- 48. Montgomery AA, Graham A, Evans PH et al. Inter-rater agreement in the scoring of abstracts submitted to a primary care research conference. BMC Health Serv Res 2002; 2: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Sutter R, Dietrich TJ, Zingg PO et al. Femoral antetorsion: comparing asymptomatic volunteers and patients with femoroacetabular impingement. Radiology 2012; 263: 475–83. [DOI] [PubMed] [Google Scholar]
- 50. Tönnis D, Heinecke A. Diminished femoral antetorsion syndrome: a cause of pain and osteoarthritis. J Pediatr Orthop 1991; 11: 419–31. [DOI] [PubMed] [Google Scholar]
- 51. Tibor LM, Liebert G, Sutter R et al. Two or more impingement and/or instability deformities are often present in patients with hip pain. Clin Orthop Relat Res 2013; 471: 3762–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Zeng G, Schmaranzer F, Degonda C et al. MRI-based 3D models of the hip joint enables radiation-free computer-assisted planning of periacetabular osteotomy for treatment of hip dysplasia using deep learning for automatic segmentation. Eur J Radiol Open 2021; 8: 100303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Lerch TD, Boschung A, Schmaranzer F et al. Lower pelvic tilt, lower pelvic incidence, and increased external rotation of the iliac wing in patients with femoroacetabular impingement due to acetabular retroversion compared to hip dysplasia. Bone Jt Open 2021; 2: 813–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Albers CE, Schwarz A, Hanke MS et al. Acetabular version increases after closure of the triradiate cartilage complex. Clin Orthop Relat Res 2017; 475: 983–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Klingenstein GG, Zbeda RM, Bedi A et al. Prevalence and preoperative demographic and radiographic predictors of bilateral femoroacetabular impingement. Am J Sports Med 2013; 41: 762–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


