Abstract
Ensuring healthcare access is critical to maintain health and prevent illness. Prior studies demonstrate gender disparities in healthcare access. Less is known about how these vary with age, race/ethnicity, and ASCVD status. We utilized cross-sectional data from 2016 to 2019 CDC Behavioral Risk Factor Surveillance System (BRFSS), a nationally representative U.S. telephone-based survey of adults (≥18 years). Measures of difficulty accessing healthcare included absence of healthcare coverage, delay in healthcare access, absence of primary care physician, >1-year duration since last routine checkup, inability to see doctor due to cost, and cost-related medication non-adherence (CRMNA). We studied association between gender and these variables using multivariable-adjusted logistic regression models, stratifying by age, race/ethnicity, and ASCVD status. Our population consisted of 1,737,397 individuals; 54% were older (≥45 years), 51% women, 63% non-Hispanic White, 12% non-Hispanic Black,17% Hispanic, 9% reported ASCVD. In multivariable-adjusted models, women were more likely to report delay in healthcare access: odds ratio (OR) and (95% confidence interval): 1.26 (1.11,1.43), inability to see doctor due to cost: 1.29 (1.22,1.36), and CRMNA: 1.24 (1.01,1.50). They were less likely to report lack of healthcare coverage: 0.71 (0.66,0.75) and PCP: 0.50 (0.48,0.52). Disparities were pronounced in younger (<45 years) women, Black women, and women with ASCVD. Despite being less likely to report lack of healthcare coverage, women are more likely to report barriers to healthcare access. Identifying and addressing these barriers, particularly among younger women and Black women, is crucial to ensure equitable healthcare access to all.
Keywords: women, gender disparities, age disparities, race disparities, access to healthcare, cost-related medication non-adherence, atherosclerotic cardiovascular disease
Introduction
Women’s health is becoming increasingly recognized as a global public health issue, with many guidelines and societies recognizing the underdiagnosis and undertreatment of women. 1 It is therefore vital to ensure the continued delivery of healthcare to effectively diagnose health conditions and institute preventive measures in this population. This is especially important in the outpatient setting, where a majority of preventive care is provided to patients. 2 Several factors can compromise healthcare access, including patient-level factors related to purchasing a healthcare plan and system-related factors that can affect patients’ ability to access the healthcare system despite having health insurance. It is important to identify and overcome these barriers, particularly among women to ensure appropriate longitudinal medical care, including age-appropriate screening, control of risk factors, and medication prescription and titration. 2
Atherosclerotic cardiovascular disease (ASCVD) remains the leading cause of morbidity and mortality in the United States (U.S.) and among women in particular. 3 Several studies have demonstrated that women with ASCVD often experience delays in accessing timely healthcare, undergo fewer diagnostic procedures, and have poorer outcomes than men. 4–6 The American Heart Association guidelines on prevention of cardiovascular disease among women highlight the importance of access to primary care services as an essential determinant for the delivery of preventive care among women. 7,8
This study evaluates the prevalence of difficulty accessing medical care and cost-related medication non-adherence (CRMNA) among women and specifically among those with ASCVD. We also examine the interrelationship of gender with age, race/ethnicity, and ASCVD status to identify subgroups of women who may be particularly susceptible to these barriers in accessing medical care.
Methods
Study Design
The Behavioral Risk Factor Surveillance System (BRFSS) survey is a nationwide telephone-based survey established by the Centers for Disease Control and Prevention. 9 BRFSS is administered to a random sample representative of adult residents above 18 years in all 50 states in the U.S., the District of Columbia, and the 3 U.S. territories ─ making it the largest telephone-based survey in the world. The survey evaluates the use of preventive services, chronic health conditions, and health-related risk behaviors among U.S adults. We utilized data from the 2016 to 2019 BRFSS surveys. Gender was self-reported, and for this analysis was considered binary (women and men). All other variables were self-reported as well and have been validated against other national survey data. 10,11 The study was exempt from Institutional Review Board approval since it utilized de-identified data from a publicly available dataset.
Difficulty Accessing Healthcare and Cost-Related Medication Non-Adherence
The absence of healthcare coverage was identified if participants answered “No” to the question: “Do you have any kind of healthcare coverage, including health insurance, prepaid plans such as HMOs [Health Maintenance Organizations], or government plans such as Medicare, or Indian Health Service?” Difficulty accessing medical care was defined if participants answered “Yes” to one of the following questions: “Have you delayed getting needed medical care for any of the following reasons in the past 12 months?” (The participants were asked to select the most important reasons, and possible responses included: “You couldn’t get through on the telephone”; “You couldn’t get an appointment soon enough”; “Once you got there, you had to wait too long to see the doctor”; “The (clinic/doctor’s) office wasn’t open when you got there”; “You didn’t have transportation”; or “Other”). The absence of primary care physician was defined if participants answered “No” to the question: “Do you have one person you think of as your personal doctor or healthcare provider?” Time since last routine checkup was based on how participants responded to the question: “About how long has it been since you last visited a doctor for a routine checkup?” A routine checkup in BRFSS was defined as a “general physical exam, not an exam for a specific injury, illness, or condition.” We defined a duration greater than one year since the last routine checkup as being inadequate. Inability to see a doctor due to cost was defined if participants answered “Yes” to the question: “Was there a time in the past 12 months when you needed to see a doctor but could not because of cost?” CRMNA was identified if participants answered “Yes” to the question: “Not including over the counter (OTC) medications, was there a time in the past 12 months when you did not take your medications as prescribed because of cost?”
Assessment of Covariates
Cardiovascular comorbidities included the following: Hypertension was defined if participants reported having been told they have high blood pressure by a doctor, nurse, or other health professional. Hyperlipidemia was defined if participants reported having had their cholesterol checked and been told by a doctor, nurse, or other health professionals that it was high. Diabetes mellitus was defined if participants were ever told they had diabetes. Cigarette status was characterized as “Ever” or “Never” depending on how participants answered the question, “Have you smoked at least 100 cigarettes in your entire life?”. “Ever” smokers were then classified as current smokers if they reported smoking cigarettes daily or on some days. Chronic kidney disease was defined if participants reported ever being told that they have kidney disease, excluding kidney stones, bladder infection, and incontinence. ASCVD was identified if participants reported a prior history of coronary heart disease or stroke.
Non-cardiovascular comorbidities included the following: Chronic obstructive pulmonary disease was identified if participants reported ever being told they have chronic obstructive pulmonary disease (COPD), emphysema, or chronic bronchitis. Asthma was defined if participants reported ever being told they have asthma. Arthritis was defined if participants reported ever having a doctor diagnose them as having some form of arthritis. Cancer was identified if participants reported ever being told they have skin cancer or any other type of cancer.
Statistical Analysis
Prevalence of demographic variables, comorbidities, difficulty with healthcare access, and CRMNA was analyzed using survey weights as the BRFSS utilized design weighting and iterative proportional fitting to ensure representativeness of the data in the U.S. population. 12 Baseline characteristics were summarized using counts (weighted percentages) and stratified by gender.
We then used multivariable logistic regression models to evaluate the association of gender (women vs. men) and difficulty in healthcare access and CRMNA in the overall study population and among those with ASCVD. Furthermore, we evaluated the interrelationship of gender with age using the following categories: men <45 years, women <45 years, men ≥45 years, and women ≥45 years; we used men <45 years as the reference. We defined the “younger” age group as those <45 years, and “older” as those ≥45 years. Similarly, we evaluated interrelationship of gender and ethnicity/race using the following categories: Non-Hispanic White men, Non-Hispanic White women, Non-Hispanic Black men, and Non-Hispanic Black women; we used Non-Hispanic White men as the reference. Analyses were adjusted for age, race/ethnicity, education, household income, employment status, and comorbidity burden (hypertension, hyperlipidemia, diabetes mellitus, current cigarette smoking, chronic kidney disease, COPD, asthma, arthritis, and cancer). Odds Ratios (95% Confidence Interval) were calculated, and graphically displayed using bar charts.
Analyses were conducted using Stata version 16.1 (StataCorp, College Station, Texas). Bar charts were generated using Excel version 16.41. A two-sided p-value <0.05 was considered statistically significant.
Results
Our study population consisted of 1,737,397 individuals, representing 255,200,373 in the U.S. age >18 years, of whom 54% were ≥45 years, 51% women, 63% White, 12% Black, 17% Hispanic, and 9% with ASCVD. Twelve percent of the population reported absence of healthcare coverage, 21% reported having a delay in healthcare access, and 10% reported CRMNA. In the overall study population, 23% of individuals reported not having a primary care physician (PCP), 26% not having a routine checkup in over 1 year, and 13% having not been able to see a doctor due to cost.
Compared to men, women were less likely to have an income ≥$75,000 and more likely to be unemployed. Cardiovascular comorbidities were generally more prevalent among men than women, while non-cardiovascular comorbidities were generally more common among women (Table 1).
Table 1.
Baseline characteristics of the study population comparing women versus men
| Men (n= 776,666; 48.7%) |
Women (n= 969,333; 51.2%) |
|
|---|---|---|
| Demographics | ||
| Age (years) | ||
| 18−34 | 31.3% | 28.5% |
| 35−44 | 16.7% | 15.9% |
| 45−54 | 16.7% | 16.3% |
| 55−64 | 16.5% | 16.8% |
| ≥65 | 18.9% | 22.5% |
| Race/Ethnicity | ||
| White | 62.7% | 62.6% |
| Black | 11.2% | 12.5% |
| Hispanic | 17.5% | 16.7% |
| Other | 8.6% | 8.2% |
| Education | ||
| Less than High School | 14.0% | 12.8% |
| High School – Some College | 59.0% | 60.0% |
| Greater than college | 27.0% | 28.3% |
| Annual Income | ||
| <$50,000 | 46.6% | 54.2% |
| $50,000−$75,000 | 15.5% | 14.3% |
| ≥$75,000 | 38.0% | 31.4% |
| Employment Status | ||
| Employed | 65.0% | 50.0% |
| Unemployed | 11.9% | 24.5% |
| Student | 5.4% | 5.9% |
| Retired | 17.7% | 19.4% |
| Cardiovascular Comorbidities | ||
| Hypertension | 34.7% | 30.6% |
| Hyperlipidemia | 35.2% | 30.6% |
| Diabetes Mellitus | 11.6% | 11.6% |
| Chronic Kidney Disease | 2.9% | 3.3% |
| Current Cigarette Smoking | 17.0% | 13.2% |
| Atherosclerotic Cardiovascular Disease | 9.8% | 7.5% |
| Non-Cardiovascular Comorbidities | ||
| Chronic Obstructive Pulmonary Disease | 5.8% | 7.3% |
| Asthma | 12.0% | 16.3% |
| Arthritis | 21.1% | 29.2% |
| Cancer | 10.5% | 12.8% |
| Presence and Access to Healthcare and Medication Non-Adherence | ||
| Absence of Healthcare Coverage | 13.8% | 10.7% |
| Delay in Access to Healthcare | 19.0% | 23.1% |
| Absence of Primary Care Physician | 29.1% | 17.4% |
| Greater than 1 Year Since Last Routine Checkup | 30.6% | 22.0% |
| Inability to See Doctor Due to Cost | 11.9% | 14.5% |
| Cost-related Medication Non-adherence | 8.3% | 11.7% |
P<0.001 for all comparisons
In multivariable-adjusted models, women were more likely to report a delay in healthcare access: Odds Ratio (95% Confidence Interval) 1.26 (1.11,1.43), inability to see a doctor due to cost: 1.29 (1.22,1.36), and CRMNA: 1.24 (1.01,1.50). On the other hand, women were less likely to report the absence of healthcare coverage: 0.71 (0.66,0.75), absence of a PCP: 0.50 (0.48,0.52), and not having a routine checkup in over 1 year: 0.72 (0.69,0.75) (Table 2).
Table 2.
Odds ratios (95% confidence interval) for the association of gender (women vs. men) and difficulty in healthcare access and cost-related medication non-adherence in the overall study population and among those with atherosclerotic cardiovascular disease
| Overalla | Atherosclerotic Cardiovascular Diseasea | |||
|---|---|---|---|---|
| Unadjusted | Adjustedb | Unadjusted | Adjustedb | |
| Absence of Healthcare coverage | 0.74 (0.73,0.76) | 0.71 (0.66,0.75) | 0.85 (0.77,0.93) | 0.82 (0.66,1.02) |
| Absence of Primary Care Physician | 0.54 (0.53,0.55) | 0.50 (0.48,0.52) | 0.69 (0.64,0.75) | 0.62 (0.50,0.77) |
| Greater than 1 year Since Last Routine Checkup | 0.64 (0.63,0.65) | 0.72 (0.69,0.75) | 0.86 (0.81,0.92) | 1.00 (0.86,1.15) |
| Delay in Access to Healthcare | 1.28 (1.21,1.34) | 1.26 (1.11,1.43) | 1.29 (1.12,1.47) | 1.17 (0.82,1.68) |
| Inability to See Doctor Due to Cost | 1.25 (1.23,1.28) | 1.29 (1.22,1.36) | 1.31 (1.24,1.39) | 1.25 (1.07,1.45) |
| Cost-related Medication Non-adherence | 1.45 (1.35,1.56) | 1.24 (1.01,1.50) | 1.57 (1.32,1.85) | 1.15 (0.74,1.78) |
Referent category = men
Model is adjusted for age, race/ethnicity, income, education, comorbidities (hypertension, hyperlipidemia, diabetes mellitus, current cigarette smoking, chronic obstructive pulmonary disease, asthma, arthritis, and cancer)
Compared to younger men, younger women were more likely to report a delay in healthcare access: 1.47 (1.21,1.80), inability to see a doctor due to cost: 1.39 (1.29,1.50), and CRMNA: 1.51 (1.05,2.15). Older men and women were less likely to report difficulty accessing healthcare and CRMNA than younger men (Figure 1). White women, Black men, and Black women were more likely to report delay in healthcare access: [1.30 (1.13, 1.50), 1.01 (0;.76, 1.35), 1.40 (1.09–1.79), respectively], inability to see a doctor due to cost [1.36 (1.28,1.44), 1.27 (1.13,1.43), 1.46 (1.32,1.62), respectively], while only White women were significantly less likely to report inability to take medication due to cost [1.29 (1.04,1.59)], compared to White men (Figure 2).
Figure 1.
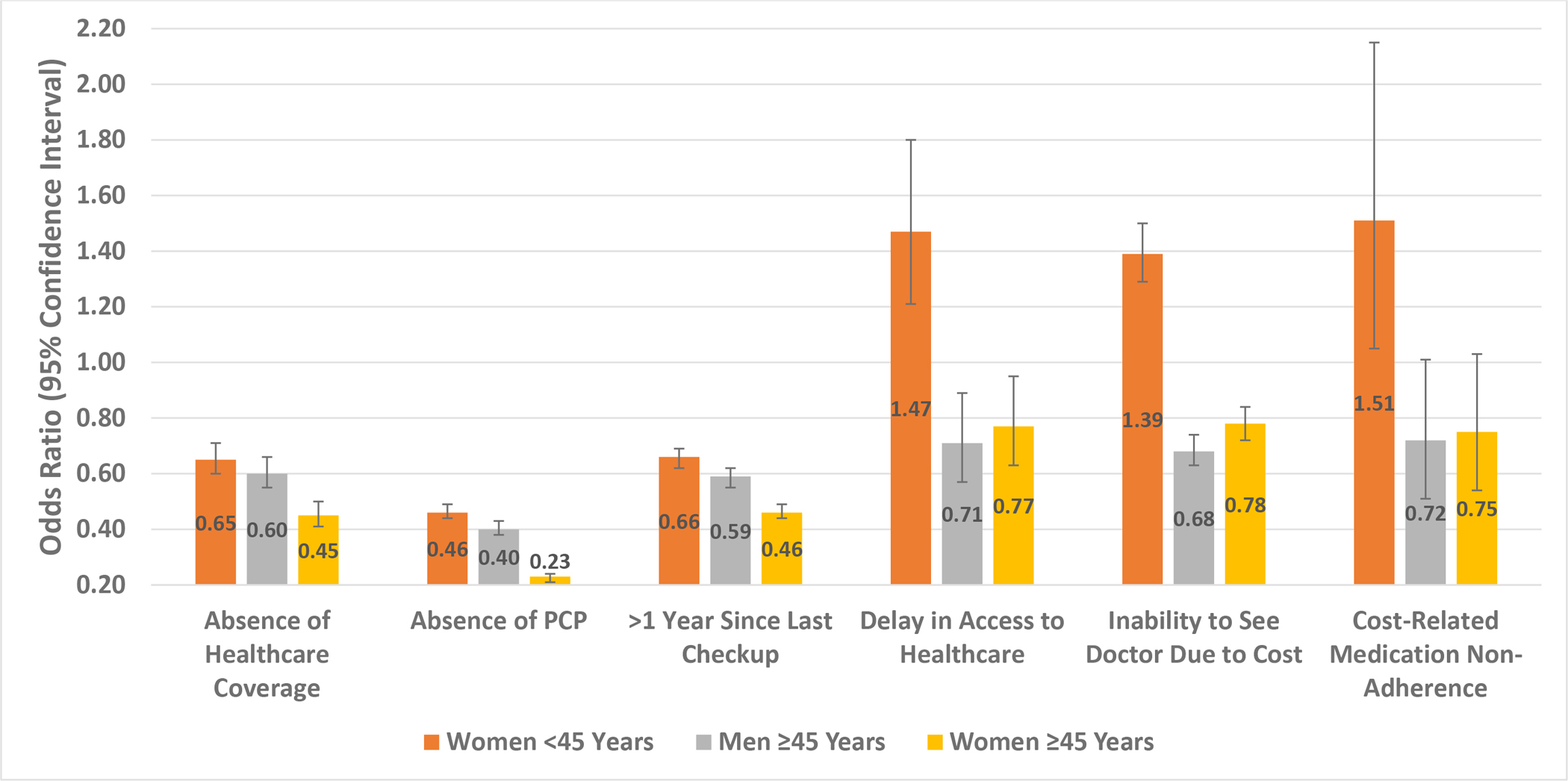
Odds ratios (95% confidence interval) for the association of gender and age groups and difficulty in healthcare access and cost-related medication non-adherence (reference group is men <45 years)
*Model is adjusted for race/ethnicity, income, education, comorbidities (hypertension, hyperlipidemia, diabetes mellitus, current cigarette smoking, chronic obstructive pulmonary disease, asthma, arthritis, and cancer)
Figure 2.
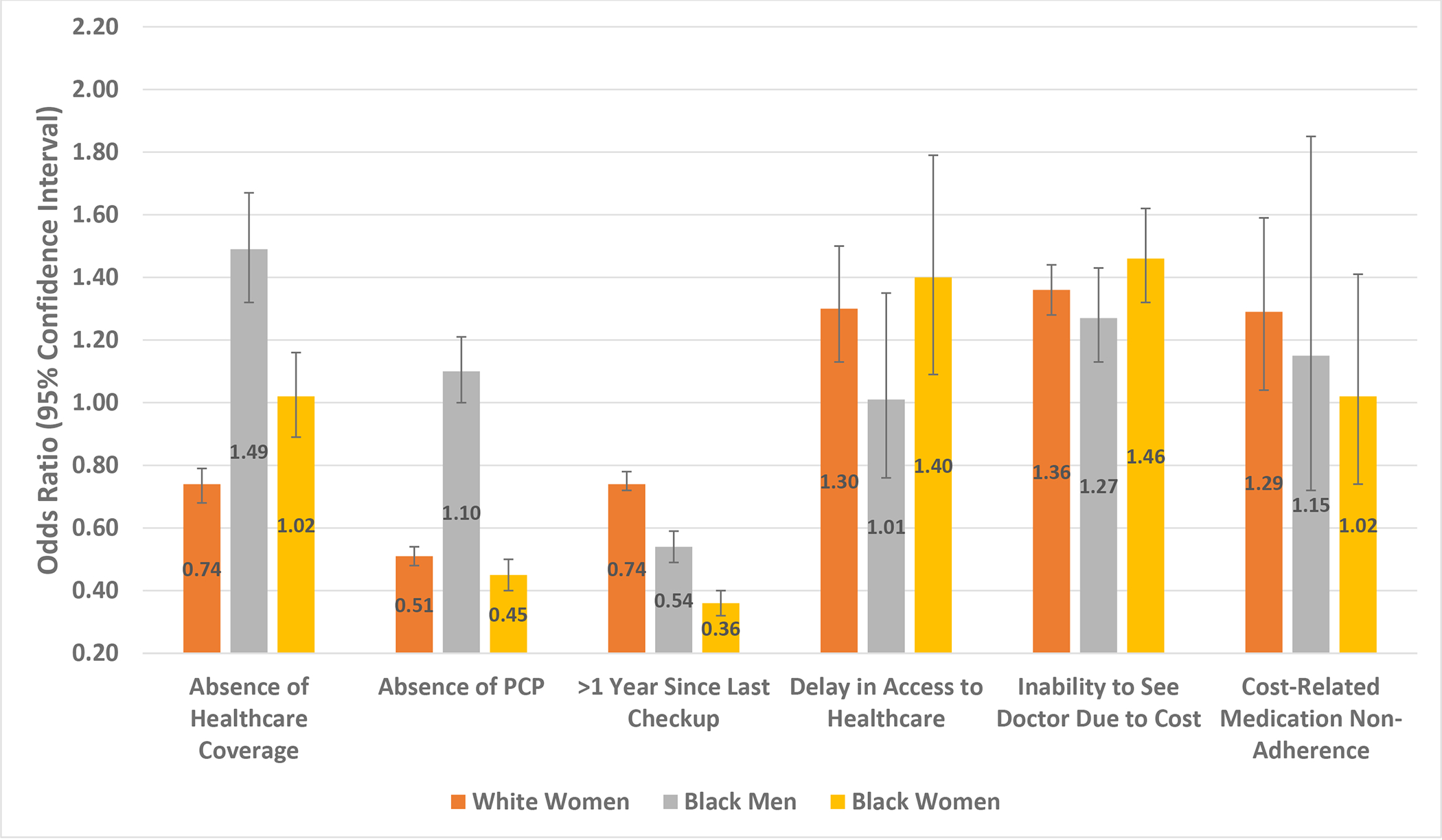
Odds ratios (95% confidence interval) for the association of gender and race groups and difficulty in access to health care and cost-related medication non-adherence (reference group is White men)
*Model is adjusted for age, income, education, comorbidities (hypertension, hyperlipidemia, diabetes mellitus, current cigarette smoking, chronic obstructive pulmonary disease, asthma, arthritis, and cancer
Among those with ASCVD, women vs. men remained less likely to report lack of healthcare coverage (6.7% vs. 7.8%) or absence of a PCP (7.6% vs. 10.6%), but more likely to have a delay in healthcare access (28.6% vs. 23.7%), be unable to see a doctor due to cost (17.7% vs. 14.0%), and report CRMNA (20.7% vs. 14.3%) (all p <0.001). These trends persisted in multivariable-adjusted models but were only significant for the absence of PCP: 0.62 (0.50,0.77) and inability to see a doctor due to cost: 1.25 (1.07,1.45) (Table 2).
Discussion
In a nationally representative U.S. sample, a substantial proportion of women reported difficulty accessing medical care and having CRMNA. In general, women were more likely to report a delay in healthcare access, inability to see a doctor due to cost, and CRMNA, despite being more likely to have healthcare coverage, a PCP, and a routine checkup in the last year. These results were similar among younger women, White women and Black women, and women with ASCVD.
Women continue to have unmet healthcare needs 13,14 and much of this has been attributed to the high cost of care. We found that women had lower income and were more likely to be unemployed compared to men. However, the disparities in healthcare access and cost-related restrictions among women persisted even after adjusting for income and education, indicating that socioeconomic factors other than income and education could further explain this disparity. Prior studies have suggested reasons for the higher healthcare costs associated with women, including longer life expectancy and reproductive healthcare costs, with unique factors related to pregnancy and menopause. 3,15,16 Providers for these services frequently operate on an independent and fee-for-service basis, providing one possible explanation for the higher costs experienced by women. 17
The Kaiser Family Foundation (KFF) has conducted surveys on women’s healthcare to evaluate factors that can uniquely compromise women’s health. 18 Although the proportion of women with health coverage had increased since the Affordable Care Act (ACA) implementation, a substantial number of women report paying out of pocket for screening tests including pap smears and mammograms, despite provisions made by the ACA that these services be rendered without cost-sharing. 18 These high out-of-pocket costs may be particularly troublesome among lower-income women. About 30% of women in the KFF survey reported having unpaid medical bills and about 40% had to make tradeoffs in paying for other basic necessities such as food or bills in order to afford healthcare services. 18
Importantly, we found similar disparities in access to healthcare among women with ASCVD. The annual prevalence and mortality rates of ASCVD are similar among men and women. Yet, several studies have shown that this subset of women are underrecognized and undermanaged, including having lower referral rates for secondary prevention such as cardiac rehabilitation 19 and the underuse of goal-directed medical therapy in women with acute coronary syndrome. 20 Furthermore, the KFF survey showed a steady increase in the proportion of women taking 6 or more medicines, 18 which may further contribute to the higher prevalence of CRMNA among women, as seen in our study. Women with a high pill burden are more likely to experience poorer health, which may further exacerbate the difficulty accessing medical care and CRMNA.
Younger women were also more likely to report a delay in healthcare access, inability to see a doctor due to cost, and CRMNA. Younger women may be particularly susceptible to healthcare access barriers that are related to their informal roles as caregivers. The KFF survey found that women often cited transportation and childcare as barriers to healthcare access, with lower-income women more likely to be affected. 8 In addition to these barriers, there is also the aforementioned additional cost and burden of reproductive healthcare that uniquely affects this population.
We also demonstrated race-related disparities with both White women and Black women reporting delay in healthcare access care and cost-related barriers more often compared with White men. Despite the ACA, the rates of uninsured individuals among Black and Hispanic groups remain significantly higher than among Whites. 21 Lower education and health literacy may further broaden these disparities. 22 However, our results showed that even after adjusting for income and education level, these disparities still existed among Black women. Other contributory factors that have been examined in the Black community and may impede access to healthcare include the quality of housing, food quality and ease of access, violence, and incarceration. 23–25
It is important to identify solutions that simultaneously address several barriers to healthcare access among women. 26 Providing transportation for these patients (such as Lyft or Uber) can help circumvent some logistical barriers. 27 Another potential solution for young women with children is the concept of “pair-clinics”, in which the mother and child are seen together in clinic, a concept that has been evaluated in patients affected by HIV. The ACA has improved healthcare coverage, although full implementation of its provisions is required to lower cost-sharing so that women can pay medical bills, undergo screening tests, and afford medications. This issue is especially important in recent times, given the legal challenges that the ACA is facing. Lastly, racial disparities in medical care should be viewed within the broader context of systemic racism and unconscious biases based on negative stereotypes. Improving racial sensitivity and awareness among healthcare providers and increasing recruitment of providers from minority backgrounds may help increase racial sensitivity and decrease racial disparities in healthcare. 28
This study has certain limitations. All our variables were self-reported, which can generate recall bias. We were not able to confirm whether there was an objectively longer delay in accessing health care between women vs men; it may be that women in general have greater expectations for their healthcare experience, a concept that has been documented in the literature. 29 Only binary gender (women vs men) was included, and further studies addressing healthcare access issues in non-binary gender would be of significant value to this field. Our definition of ASCVD did not include transient ischemic attacks or peripheral arterial disease, and therefore we may have underestimated the true prevalence of ASCVD. We may not have comprehensively evaluated all factors related to difficulty accessing medical care. Lastly, cross-sectional analysis limits our ability to establish causality or the direction of association.
In conclusion, women in general and specifically younger women and Black women report more difficulty accessing medical care and more CRMNA despite being more likely to report having healthcare coverage than men. Such disparities should be addressed beyond healthcare coverage provision to provide equitable access to healthcare for all individuals.
Disclosures/Funding
Salim S. Virani
Research support: Department of Veterans Affairs, World Heart Federation, Tahir and Jooma Family
Honorarium: American College of Cardiology (Associate Editor for Innovations, acc.org)
Fatima Rodriguez
Funding Sources: Dr. Rodriguez was funded by a career development award from the National Heart, Lung, and Blood Institute (K01 HL 144607) and the American Heart Association/Robert Wood Johnson Harold Amos Medical Faculty Development Program.
Disclosures: Outside the submitted work, Dr. Rodriguez reports equity from Carta and consulting fees from Novartis and NovoNordisk.
Footnotes
All authors had access to the data and were involved in writing the manuscript
References
- 1.Ribeiro PS, Jacobsen KH, Mathers CD, Garcia-Moreno C. Priorities for women’s health from the Global Burden of Disease study. Int J Gynaecol Obstet Off organ Int Fed Gynaecol Obstet 2008; 102: 82–90. [DOI] [PubMed] [Google Scholar]
- 2.Khera A, Baum SJ, Gluckman TJ, et al. Continuity of Care and Outpatient Management for Patients with and at High Risk for Cardiovascular Disease during the COVID-19 Pandemic: A Scientific Statement from the American Society for Preventive Cardiology. Am J Prev Cardiol 2020; : 100009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leslie C, Melinda D, Islam E, et al. Summary of Updated Recommendations for Primary Prevention of Cardiovascular Disease in Women. J Am Coll Cardiol 2020; 75: 2602–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mehran R, Vogel B, Ortega R, Cooney R, Horton R. The Lancet Commission on women and cardiovascular disease: time for a shift in women’s health. Lancet 2019; 393: 967–8. [DOI] [PubMed] [Google Scholar]
- 5.Pagidipati NJ, Peterson ED. Acute coronary syndromes in women and men. Nat Rev Cardiol 2016; 13: 471–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peters SAE, Woodward M, Jha V, Kennedy S, Norton R. Women’s health: a new global agenda. BMJ Glob Heal 2016; 1: e000080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mosca L, Banka CL, Benjamin EJ, et al. Evidence-Based Guidelines for Cardiovascular Disease Prevention in Women: 2007 Update. Circulation 2007; 115: 1481–501. [DOI] [PubMed] [Google Scholar]
- 8.Lori M, J. BE, Kathy B, et al. Effectiveness-Based Guidelines for the Prevention of Cardiovascular Disease in Women—2011 Update. Circulation 2011; 123: 1243–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Behavioral Risk Factor Surveillance System. https://www.cdc.gov/brfss/index.html.
- 10.Pierannunzi C, Hu SS, Balluz L. A systematic review of publications assessing reliability and validity of the Behavioral Risk Factor Surveillance System (BRFSS), 2004–2011. BMC Med Res Methodol 2013; 13: 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li C, Balluz LS, Ford ES, Okoro CA, Zhao G, Pierannunzi C. A comparison of prevalence estimates for selected health indicators and chronic diseases or conditions from the Behavioral Risk Factor Surveillance System, the National Health Interview Survey, and the National Health and Nutrition Examination Survey, 20. Prev Med (Baltim) 2012; 54: 381–7. [DOI] [PubMed] [Google Scholar]
- 12.CDC. Weighting the BRFSS Data. https://www.cdc.gov/brfss/annual_data/2017/pdf/weighting-2017-508.pdf. (accessed April 17, 2019).
- 13.Socías ME, Koehoorn M, Shoveller J. Gender Inequalities in Access to Health Care among Adults Living in British Columbia, Canada. Women’s Heal issues Off Publ Jacobs Inst Women’s Heal 2016; 26: 74–9. [DOI] [PubMed] [Google Scholar]
- 14.Bryant T, Leaver C, Dunn J. Unmet healthcare need, gender, and health inequalities in Canada. Health Policy 2009; 91: 24–32. [DOI] [PubMed] [Google Scholar]
- 15.Ward BW, Schiller JS. Prevalence of multiple chronic conditions among US adults: estimates from the National Health Interview Survey, 2010. Prev Chronic Dis 2013; 10: E65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Johnson PJ, Jou J, Upchurch DM. Health Care Disparities Among U.S. Women of Reproductive Age by Level of Psychological Distress. J Womens Health (Larchmt) 2019; 28: 1286–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.American Academy of Family Physicians (AAFP). ACOs flourishing in 2014, study reports. AAFP News, 2014. http://www.aafp.org/news/practice-professional-issues/20140722acosgrow.html. Accessed January 14, 2021 [Google Scholar]
- 18.Women’s Coverage, Access, and Affordability: Key Findings from the 2017 Kaiser Women’s Health Survey. Kaiser Fam. Found. https://www.kff.org/womens-health-policy/issue-brief/womens-coverage-access-and-affordability-key-findings-from-the-2017-kaiser-womens-health-survey/. [Google Scholar]
- 19.Aragam KG, Moscucci M, Smith DE, et al. Trends and disparities in referral to cardiac rehabilitation after percutaneous coronary intervention. Am Heart J 2011; 161: 544–551.e2. [DOI] [PubMed] [Google Scholar]
- 20.Tran HV, Waring ME, McManus DD, et al. Underuse of Effective Cardiac Medications Among Women, Middle-Aged Adults, and Racial/Ethnic Minorities With Coronary Artery Disease (from the National Health and Nutrition Examination Survey 2005 to 2014). Am J Cardiol 2017; 120: 1223–9. [DOI] [PubMed] [Google Scholar]
- 21.Buchmueller TC, Levinson ZM, Levy HG, Wolfe BL. Effect of the Affordable Care Act on Racial and Ethnic Disparities in Health Insurance Coverage. Am J Public Health 2016; 106: 1416–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Statistics USB of L. THE EMPLOYMENT SITUATION.
- 23.Kershaw KN, Osypuk TL, Do DP, De Chavez PJ, Diez Roux A V. Neighborhood-level racial/ethnic residential segregation and incident cardiovascular disease: the multi-ethnic study of atherosclerosis. Circulation 2015; 131: 141–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Golembeski C, Fullilove R. Criminal (in)justice in the city and its associated health consequences. Am J Public Health 2005; 95: 1701–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gaskin DJ, Thorpe RJJ, McGinty EE, et al. Disparities in diabetes: the nexus of race, poverty, and place. Am J Public Health 2014; 104: 2147–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jacobs B, Ir P, Bigdeli M, Annear PL, Van Damme W. Addressing access barriers to health services: an analytical framework for selecting appropriate interventions in low-income Asian countries. Health Policy Plan 2012; 27: 288–300. [DOI] [PubMed] [Google Scholar]
- 27.Powers BW, Rinefort S, Jain SH. Nonemergency Medical Transportation: Delivering Care in the Era of Lyft and Uber. JAMA 2016; 316: 921–2. [DOI] [PubMed] [Google Scholar]
- 28.Williams DR, Rucker TD. Understanding and addressing racial disparities in health care. Health Care Financ Rev 2000; 21: 75–90. [PMC free article] [PubMed] [Google Scholar]
- 29.Okunrintemi V, Valero-Elizondo J, Patrick B, et al. Gender Differences in Patient-Reported Outcomes Among Adults With Atherosclerotic Cardiovascular Disease. J Am Heart Assoc 2018; 7: e010498. [DOI] [PMC free article] [PubMed] [Google Scholar]


