Abstract
Environmental experiences early in life have strong and enduring consequences for cognitive, emotional, and neurobiological development and related physical and mental health trajectories. The powerful influence of early caregiver nurturance and stimulation on promoting positive neurodevelopmental outcomes has been demonstrated across species. These findings elucidate the environmental conditions known to facilitate healthy neurodevelopment and underscore the potential for modifiable psychosocial factors in the environment to be harnessed to inform early preventive interventions to promote health and adaptive development. A framework for early preventive interventions to enhance nurturing and responsive caregiving for implementation during early sensitive periods of brain development delivered within existing health or educational infrastructures is proposed. Emotional development during sensitive periods is an important, under-recognized, and abundantly modifiable predictor of mental and physical health outcomes that warrants investment of resources and integration of interventions into public health infrastructure for children worldwide. Future studies are needed to further clarify whether and when sensitive periods are present for key developmental domains to inform the optimal timing and targets of these interventions. Numerous available empirically supported early interventions may be modified and applied in briefer and more feasible modalities of delivery to broader populations of developing children. As well established in growth and development across species, essential environmental inputs that are particularly important at specified developmental periods facilitate optimal growth trajectories. Such principles hold great potential in application to early child neurodevelopment to facilitate a thriving and resilient human population.
Keywords: Developmental enhancement, Neurodevelopment, Prevention, Sensitive periods
Environmental experiences early in life exert a profound influence on health and development across the life course (1). The pervasive and enduring consequences of environmental adversity for physical and mental health problems and related alterations in cognitive, emotional, and neurobiological development have been empirically demonstrated in both animals and humans (2,3). Conversely, the influence of early caregiver nurturance and stimulation on promoting positive neurodevelopmental outcomes has been demonstrated across species (4). This work has helped to shed light on the environmental conditions known to facilitate healthy development, enhance resilience, and prevent the emergence of psychopathology and physical health problems. Importantly, this body of work underscores the potential for modifiable psychosocial factors in the environment to be harnessed to inform early preventive interventions to promote health and adaptive development.
Evidence linking key dimensions of the early environment to neurocognitive development has been leveraged to inform the design of early childhood development programs. In particular, these findings have been increasingly translated and applied in early childhood education, where the importance of cognitive stimulation in the first years of life has gained broad acceptance, shaping the curriculum of numerous early child educational programs (5,6). While there has been increased attention to environmental influences on emotional development with the advent of trauma-informed approaches in some settings, the critical role of emotional support and security has not achieved widespread prominence or priority in early childhood education frameworks or in public health interventions and policies (7).
In addition to the increasingly well-recognized need for cognitive stimulation in early life, sensitive and responsive caregiving is also critical to support adaptive behavioral, emotional, and cognitive outcomes. Although early interventions have been consistently shown to be effective at increasing sensitive caregiving and, in turn, improving child outcomes such as attachment security (8), such programs have yet to be taken up broadly as a public health priority. In this paper, we propose a framework for early preventive interventions that focuses on enhancing sensitive and responsive caregiving and the quality of the caregiver-child relationship for implementation during early sensitive periods of brain development to achieve maximal effect. We also propose that these interventions be delivered within existing health or educational infrastructures to provide maximal access and remove barriers to care. We review existing empirically supported interventions for young children that target this domain, as well as a novel, brief internet-based intervention. We briefly review the proposed mechanism of action and cost-effectiveness of empirically proven interventions.
The Foundational Importance of Supportive Caregiving in Early Childhood
Decades of basic developmental research have established the importance of a sensitive, emotionally available, nurturing, and consistent caregiver in the first 5 years of life. Substantial evidence demonstrates that caregiving characterized by sensitive and contingent responses to the child, particularly to child distress, is necessary for the formation of a secure attachment relationship between the child and caregiver (9, 10, 11, 12) and promotes adaptive emotional and cognitive development (13, 14, 15). Children who do not receive this type of caregiving are more likely to experience maladaptive developmental outcomes and are at elevated risk for psychopathology across the life course (16, 17, 18, 19, 20). Of central importance is the consistent availability of at least one primary caregiver. A primary caregiver is defined as an adult who is committed to the care and well-being of the child and available to meet their physical and emotional needs during the first years of life and ideally beyond. Infants and toddlers who are shifted from one household to another, as is frequently the case in foster care, are at high risk for the development of attachment disturbances, psychopathology, and developmental delays (21). Simply put, a supportive and consistent primary caregiving relationship is the foundation of healthy development. Support may manifest in many different ways, but a requirement is that an adult caregiver is present, emotionally available, and responsive to the child more often than not. The presence of this supportive caregiver is necessary not only to meet the basic needs of the child but also to buffer the negative effects of inevitable environmental challenges, stressors, and adversities.
Validation of children’s self-worth by caregivers is another fundamental component of sensitive and responsive caregiving that has increasingly been linked to adaptive developmental and academic outcomes (22). Validation does not mean providing blind praise or reinforcement for whatever the child is doing. Instead, the expression of interest in the child and his/her daily activities, characteristics, and self-generated preferences is a primary way in which validation of self-worth is communicated and fostered. Beyond this, varying kinds of expressions of approval, affection, and warmth in daily interactions also provide the developing child with a sense of security and self-esteem (23). While there are multiple ways in which this might be expressed, this type of validation most often occurs naturally and spontaneously in daily parent-child interactions. However, in cases where a caregiver is experiencing high levels of stress, a child is very difficult to soothe or manage, or a caregiver has very low self-worth, this may not arise naturally. Acknowledgment, tolerance, and validation of the child’s expression of emotions—both positive and negative—is also critical for fostering adaptive emotional development (24,25). Even fleeting recognition and acceptance of negative emotional expression may be important for children. Caregiver acceptance and acknowledgment of the child’s expression of a wide array of emotions—including negative emotions—affords the child the opportunity to begin to understand and manage the broad range of feelings that are an inevitable part of the human experience (15,26). Therefore, caregiver validation of the child’s appropriate expression of emotions is an important component of sensitive and responsive caregiving and a key target in prevention of negative developmental outcomes later in life. Indeed, several empirically proven early interventions, described below, explicitly target these aspects of sensitive and responsive caregiving.
Early Experiences Scaffold Brain and Behavioral Development
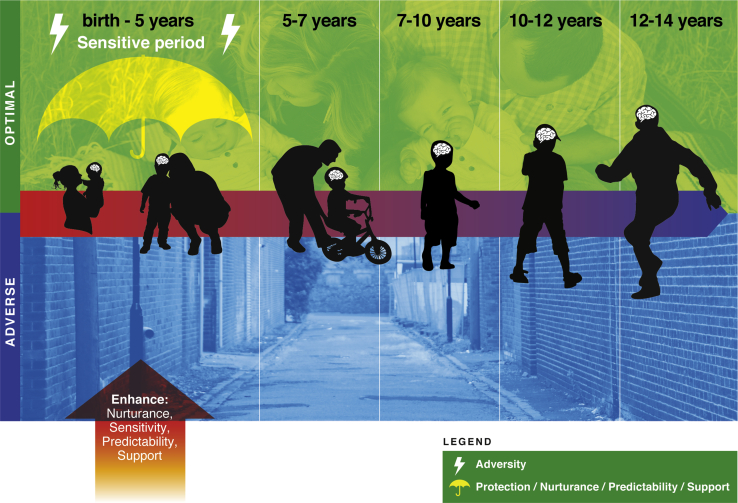
These principles provide a framework for the necessary environmental conditions for children to thrive. Unfortunately, a substantial proportion of children worldwide are raised in environments that do not provide these necessary supports or are characterized by meaningful adversity. Experiences of adversity involve stressors that are either severe or chronic, are likely to require meaningful adaptation by a child, and reflect either the presence of harmful input or the absence of environmental inputs that are necessary to support adaptive brain development (27). Common forms of adversity include experiences involving threat of harm to the child—including physical and sexual abuse, exposure to domestic violence, and other forms of trauma—and experiences involving deprivation, or the absence of expected inputs from the environment in terms of cognitive and social stimulation and emotional support—including physical and emotional neglect, institutional rearing, and material deprivation (28). Population-based studies suggest that approximately half of all children in the United States will encounter at least one such form of adversity by the time they reach adulthood (29, 30, 31). From a public health perspective, this raises alarm, as children who experience high levels of adversity are at an elevated risk of developing virtually all commonly occurring forms of psychopathology as well as a wide range of physical health problems across the life course relative to those who have not encountered adversity (29,30,32, 33, 34). A focus on harnessing the caregiver-child relationship during early sensitive periods to prevent these negative outcomes is proposed below (see Figure 1).
Figure 1.
Early prevention to enhance neurodevelopment.
Early Experiences and Brain Plasticity
Experiences of adversity may have a disproportionate impact when they occur early in life as a result of the heightened brain plasticity that characterizes childhood (35). Plasticity refers to the capacity of the brain to be changed by environmental experiences. This plasticity occurs as a result of specific neural mechanisms that promote learning and structural and functional brain changes in response to experience (36,37). Some of these mechanisms are experience expectant and reflect neural preparation to biologically encode particular types of expected environmental experiences that occur during specific windows of development referred to as sensitive periods (38). These sensitive periods are characterized by dramatic increases in plasticity that allow expected environmental experiences to produce rapid and substantial changes in neural circuits and behavior (39). Because plasticity declines dramatically once the sensitive window closes, the experience-expectant learning that occurs during these periods produces relatively enduring changes in both the brain and behavior. Expected environmental experiences encompass sensory inputs, exposure to language, experiences of caregiving, and many others (40,41). When these inputs are absent or diminished in frequency or intensity, substantial changes in brain and behavioral development occur. In contrast, other forms of plasticity are experience dependent, which are learning mechanisms that are available throughout life (38). These mechanisms also produce changes in learning and neural circuits in response to experience but in a less dramatic fashion than experience-expectant learning. Although experience-dependent learning is not constrained to a specific period of development, this type of plasticity is highest during childhood and adolescence (42).
Heightened brain plasticity in early life confers many advantages, allowing children to rapidly learn from experience and adapt to the environment. For example, language development involves a series of cascading sensitive periods in childhood (41). The plasticity that accompanies these sensitive periods allows children to rapidly learn the sounds and structures of their native language, a task that is more difficult and requires greater effort when undertaken later in life after these sensitive windows have closed (43). Germane to our focus on preventive interventions targeting social and emotional domains, the formation of a secure attachment to a primary caregiver occurs in response to nurturing and responsive caregiving that occurs during a sensitive period in the first 2 years of life (44). However, this elevated plasticity in early life can come at a cost when the early environment is characterized by stress and adversity; specifically, these experiences may be more likely to contribute to meaningful negative changes in brain and behavioral health outcomes when they occur during these windows of heightened plasticity. Below, we briefly summarize a rapidly growing literature linking experiences of early-life adversity to alterations in brain and behavioral development.
Why Prevention Is Necessary: Neurodevelopmental Consequences of Early-Life Adversity
Adverse experiences characterized by deprivation—or an absence of expected social and cognitive inputs from the environment—have been linked to widespread changes in the structure of the cortex, as well as specific changes in networks that subserve higher-order cognitive functions, including executive functions and language (45). Reduced cortical thickness and gray matter volume have been observed in numerous studies of children exposed to early-life deprivation, with the most pronounced changes occurring in the prefrontal cortex (46, 47, 48, 49). Studies that measure cognitive stimulation and linguistic input directly have demonstrated that reductions in these social and cognitive inputs early in life are associated with altered structure and function of the frontoparietal network that support executive functions (50,51) and the frontotemporal language network (52,53). These findings parallel extensive evidence demonstrating difficulties with executive functions and language skills in children raised in environments characterized by early deprivation (54, 55, 56, 57, 58, 59). Critically, reductions in social cognitive stimulation and the associated changes in neural structure and function play a meaningful role in explaining socioeconomic disparities in cognitive development and academic outcomes in children (52,59).
In contrast, early-life adversity experiences characterized by threat are associated most consistently with alterations in neural circuits that underlie emotion processing and emotion regulation (45). Heightened response in the amygdala and other regions of the salience network—such as the anterior insula—to negative emotional stimuli that could signal the presence of a threat in the environment has been observed in children exposed to trauma (60, 61, 62, 63, 64). In addition to these functional patterns, children exposed to trauma also exhibit reductions in the volume of the hippocampus and medial prefrontal cortex (47,65, 66, 67, 68, 69), regions that play a key role in modulating amygdala responses to threat as well as many forms of learning and memory (70,71). These changes in neural circuits involved in emotion processing parallel an extensive literature documenting elevated perceptual sensitivity and attention biases to threat-related stimuli, heightened emotional reactivity, and difficulties in emotion regulation among children who have experienced trauma (72, 73, 74, 75, 76, 77, 78). Alterations in frontoamygdala and hippocampal networks likely explain these patterns of emotion processing, reactivity, and regulation and have recently been shown to mediate the link between early-life trauma and multiple forms of psychopathology (62,79).
Caregiving Buffering and Developmental Outcomes After Adversity
Sensitive and responsive caregiving has been linked to adaptive social, emotional, and cognitive development, as described earlier, and more recently has been linked with patterns of structural neurodevelopment in regions involved in emotion processing (80, 81, 82). In addition, supportive caregiving has also been shown to promote resilience and buffer against the emergence of negative developmental outcomes in children who have experienced adversity. Children who receive sensitive and responsive caregiving are less likely to develop psychopathology and physical health problems, to experience difficulties in school, and to exhibit changes in social, emotional, and cognitive development after experiences of adversity (83, 84, 85, 86, 87). Furthermore, changes in brain function have been observed in several early interventions as a result of improvements in the caregiver-child relationship, suggesting that these neural alterations may be modifiable when targeted early in development (88,89).
Informing Early Preventive Interventions
As reviewed above, early experiences have a powerful impact on brain and behavioral development with implications for lifelong health and well-being. The experience of a nurturing caregiver is foundational to healthy brain development and appears to be particularly powerful during early childhood, given the numerous sensitive periods that occur during this window of development (see Figure 1). Although sensitive periods for attachment formation in the first 2 years of life are established, more work is needed to determine whether and when sensitive periods exist for other aspects of emotional development. Interventions designed to increase supportive caregiving may not only prevent children from being exposed to certain forms of adversity (e.g., maltreatment) but may also prevent the emergence of psychopathology and other developmental problems in children who have experienced adversity. Based on this, we emphasize interventions designed to enhance caregiver sensitivity, responsiveness, and nurturance in early childhood (90) in the context of brief dyadic interventions delivered as part of primary care or school-based programs to promote greater access. Future work is needed to inform whether and when there might be optimal timing of these interventions within specific sensitive periods during early childhood.
Increasing Financial and Material Supports for Caregivers
One approach to fortifying supportive caregiving has focused on tax and other public policies designed to provide greater financial support to caregivers of young children. Caregivers experiencing the financial strain that accompanies poverty are often burdened by long and unpredictable work hours and experience numerous stressors that can—through no fault of their own—make them less physically and emotionally available to their children. Reducing financial strain as a means of improving supportive caregiving has resulted in tangible positive impacts on child outcomes, including better nutrition, growth and development, and decreased morbidity (91). This approach is currently being empirically tested in a large-scale randomized controlled trial in the United States entitled Baby’s First Steps, which is providing income in the form of monthly cash transfers to new parents (92). This randomized controlled trial will test whether cash payments (provided without restriction on spending) designed to reduce financial strain on parents will impact developmental outcomes, including brain development, and the role that changes in supportive parenting play in explaining these effects. Similar approaches have been applied in other contexts but have not been readily available in the United States. Through the recently implemented 2021 American Rescue Plan that expanded child tax credits in the United States, eligible families will receive $300 per child younger than 6 years, as well as $250 per child ages 6 and older each month (93). The administration estimated that almost 90% of children in the United States would receive funding, with the potential to lift millions of children out of poverty if the program continues (94). If this policy change becomes permanent, the impact on children could be enormous by reducing material deprivation and financial strain for caregivers, which would, in turn, allow for enhanced supportive and responsive parenting that is associated with improved developmental outcomes for children.
Beyond direct financial assistance, social policies that provide support to caregivers such as paid parental leave of sufficient length, flexible work schedules, and access to affordable and conveniently located childcare have also proven to be effective strategies to reduce caregiver stress (66). Programs that focus on enhancing caregiver mental health—with a particular focus on depression—to enhance supportive and responsive parenting have also proven useful in mitigating poor developmental outcomes for children (95). These types of structural interventions have the potential to reduce parental stress, enhance responsive caregiving, and positive influence numerous aspects of emotional and cognitive development in children, making them a particularly promising approach.
Caregiver Support and Education/Training
Beyond policies and approaches that provide material support to caregivers, another common approach in prevention studies is to target parenting behavior and practices directly through education, training, or coaching. Parenting is among the most difficult tasks that adults undertake. Despite a large evidence base that validates best practices, little instruction or coaching in these techniques is routinely provided to new parents as a part of standard care (96). This is a substantial missed opportunity to enhance developmental outcomes, particularly for children experiencing adversity, given the potential for parenting interventions to reduce exposure to adversity and mitigate the impact of adversity on children’s development and mental health. In the following sections, we describe empirically supported approaches to improving supportive and responsive parenting among parents of children who have experienced adversity or are at high risk for such exposures (e.g., as a result of poverty or parental substance abuse).
Personalized and Tiered Prevention Approaches
For families experiencing adversity, prevention programs that require individual therapeutic sessions may be needed. Numerous parenting interventions designed to increase caregiver sensitivity and responsiveness to the child’s developmental needs have demonstrated positive impacts on child emotional and behavioral outcomes as well as mental health. Here, we briefly review existing evidence-based approaches. Several very brief home-based interventions have demonstrated positive effects on positive parenting and child emotional and behavioral outcomes, including the Nurse Family Partnership, which provides in-person support and education to new mothers (69), and the Family Check-Up, a three-session well-validated early intervention that targets parenting in early childhood (97).
Many evidence-based programs use a teach-and-coach approach that provides caregivers with feedback during interactions with their children. A relatively brief dyadic approach that targets sensitive parenting and attachment security entitled Attachment and Bio-behavioral Catch-Up has been applied in foster care and high-risk birth family settings. This 10-session in-home intervention has proven effective at improving attachment security and numerous aspects of child emotional development and is feasible (98). Perhaps the most widely used coaching intervention for young children is Parent Child Interaction Therapy (PCIT), which focuses on enhancing the caregiver-child relationship and establishing consistent and predictable discipline strategies. Standard PCIT is lengthy, taking 18–20 sessions, focuses mostly on establishing effective discipline, and is effective at reducing disruptive behavior and preventing child maltreatment, with large effect sizes (99, 100, 101). Numerous adaptations of PCIT have been developed, including one that targets emotion development (PCIT-ED) (102), and several have been implemented through school or primary care settings (103). A recent PCIT-ED adaptation was developed as a preventive intervention rather than treatment for children experiencing adversity (THRIVE). This six-session intervention targets the caregiver-child relationship through internet-based coaching to enhance sensitive and responsive care and promote adaptive emotional development. It has been evaluated in children ages 3–7 at high risk for experiencing adversity and demonstrated promising effects on behavioral outcomes, impairment, and parenting stress (104). THRIVE requires minimal therapist training and can be implemented by school counselors, nurses, or social workers, which makes it feasible and cost-effective for delivery in schools and primary care settings. Other effective interventions also use video coaching during caregiver-child interactions to promote positive parenting and allow the caregiver to gain perspective on their own parenting behaviors (105, 106, 107).
A more intensive empirically validated dyadic treatment entitled Child Parent Psychotherapy designed for caregivers with a history of trauma builds caregiving skills and parenting to facilitate secure attachment within this context. Child Parent Psychotherapy focuses on enhancing attachment and nurturance and has proven highly effective but is also more time-intensive and requires more advanced training than most other early interventions (105,108,109). Other empirically proven interventions targeting the parent-child dyad have been done in group formats such as Circle of Security (110,111).
Cost Efficacy of Early Intervention
Numerous longitudinal studies have demonstrated the cost-effectiveness of early interventions that target caregiving. Perhaps the most well-known is the economic analysis of Heckman et al. (112) on long-term outcomes of children who participated in early preschool–based preventive interventions. Despite the high intensity of this early intervention in a high-risk sample, adaptive outcomes including employment and varying metrics of financial security demonstrated the cost-effectiveness of the early intervention, which was quantified at 6% gain for every dollar invested (112). Similar evidence has now emerged from long-term outcomes of several early intervention programs in Turkey, Jamaica, and Pakistan (113, 114, 115). These studies show that early interventions resulted in significantly better adult outcomes from an earning and adaptation perspective (114). This growing body of data clearly shows that even from a purely financial perspective, early intervention has a great societal payoff.
Sensitive Period–Informed Preventive Interventions: A Future Goal
As knowledge of sensitive periods in human development increases, this information can be leveraged to determine whether parenting interventions are maximally effective when delivered during sensitive periods of development (e.g., for attachment formation). Recent evidence suggests that the neurodevelopmental consequences of early adversity differs as a function of both the type and timing of the experience (45,80). Although the promise of identifying developmental windows of heightened plasticity for intervention has frequently been articulated (4,116), empirical evidence remains limited outside of studies of previously institutionalized children (117). Experimental studies that administer these types of early interventions across multiple developmental stages are needed to determine whether optimal windows of opportunity for intervention exist. Data of this kind are needed to evaluate intervention timing and target (e.g., skill/domain) and determine whether increasing efficacy by capitalizing on sensitive period plasticity is possible.
Early Preventive Interventions as Routine Care
There is no shortage of empirically supported early interventions for children experiencing adversity. However, a significant problem facing most communities is the lack of access and availability of these services. For this reason, creating new service delivery models that identify children in need of intervention and deliver interventions in health and educational settings where families are already receiving services is critical to make these essential and cost-effective preventions more readily available. Models in which mental health services are either embedded in pediatric primary care or consultation with child mental health clinicians is made available to assist primary care physicians with the management of emotional and behavioral problems have become more common. However, these systems were not generally designed to provide readily accessible preventive care for children facing adversity. Federal legislation has been passed to support early intervention programs, but most communities have yet to implement this programming, many programs target children with clear developmental delays rather than those facing adversity, and significant gaps in access and delivery have been noted (118). Many of the effective interventions reviewed above have been delivered in the context of mental health care or through unique privately or community-funded programs. However, these programs are not widespread and remain unavailable to most families who could benefit from services. Indeed, the vast majority of children who have experienced adversity have never received mental health care, even those with clinically meaningful psychopathology (119). Based on this, interventions that are designed for delivery in primary care or in schools and are supported by sustainable funding streams represent an important pathway forward.
Conclusions
Translating findings from developmental, cognitive, and affective neuroscience, we propose future implementation of sustainable and accessible early childhood prevention programs that target enhancing caregiver support and nurturance within existing systems of care. Such programs would harness key experiential factors to promote healthy brain and behavioral development delivered during sensitive periods of neurodevelopment. Emotional development during the first years of life is an important, under-recognized, and abundantly modifiable target for interventions aimed at improving mental and physical health outcomes for children who have experienced adversity. Optimizing emotional development during sensitive periods warrants further investigation, investment of resources, and integration of interventions into public health infrastructure and routine educational and health care programs for children (120). Extensive evidence underscores the power of a sensitive, responsive, and nurturing caregiver on brain and behavioral development, and emerging evidence suggests that these targets may also be foundational to physical health (81). Future studies are needed to clarify and specify whether and when sensitive periods are present for emotional development domains to inform the optimal timing of these interventions during early childhood. Numerous empirically supported early interventions may be modified and applied in briefer and more feasible modalities of delivery to broader populations of developing children. As applied to many areas of growth and development across flora and fauna, there are essential environmental inputs that are particularly important at specified developmental periods to facilitate optimal growth trajectories. Such principles hold great potential in application to early child neurodevelopment to facilitate a thriving and resilient human population.
Acknowledgments and Disclosures
This study is supported by grants from the National Institute of Mental Health (Grant Nos. R01-MH103291, R01-MH106482, and R37-MH119194 [to KAM] and Grant No. R01-MH113883 [to JLL]) and the National Institute on Drug Abuse (Grant Nos. R01 MH113570, R01 DA046224, and R34 DA050272-01 [to CR]).
JLL would also like to acknowledge Abigail Kirchmeier for her technical assistance with Figure 1.
The authors report no biomedical financial interests or potential conflicts of interest.
References
- 1.Black M.M., Walker S.P., Fernald L.C.H., Andersen C.T., DiGirolamo A.M., Lu C., et al. Early childhood development coming of age: Science through the life course. Lancet. 2017;389:77–90. doi: 10.1016/S0140-6736(16)31389-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nelson C.A., 3rd, Zeanah C.H., Fox N.A. How early experience shapes human development: The case of psychosocial deprivation. Neural Plast. 2019;2019:1676285. doi: 10.1155/2019/1676285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Birnie M.T., Kooiker C.L., Short A.K., Bolton J.L., Chen Y., Baram T.Z. Plasticity of the reward circuitry after early-life adversity: Mechanisms and significance. Biol Psychiatry. 2020;87:875–884. doi: 10.1016/j.biopsych.2019.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Luby J.L., Baram T.Z., Rogers C.E., Barch D.M. Neurodevelopmental optimization after early-life adversity: Cross-species studies to elucidate sensitive periods and brain mechanisms to inform early intervention. Trends Neurosci. 2020;43:744–751. doi: 10.1016/j.tins.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barnett W.S. Long-term effects of early childhood programs on cognitive and school outcomes. Future Child. 1995;5:25–50. [PubMed] [Google Scholar]
- 6.Zigler E., Abelson W.D., Trickett P.K., Seitz V. Is an intervention program necessary in order to improve economically disadvantaged children’s IQ scores? Child Dev. 1982;53:340–348. [PubMed] [Google Scholar]
- 7.Richter L.M., Daelmans B., Lombardi J., Heymann J., Boo F.L., Behrman J.R., et al. Investing in the foundation of sustainable development: Pathways to scale up for early childhood development. Lancet. 2017;389:103–118. doi: 10.1016/S0140-6736(16)31698-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bakermans-Kranenburg M.J., Van Ijzendoorn M.H., Juffer F. Less is more: Meta-analyses of sensitivity and attachment interventions in early childhood. Psychol Bull. 2003;129:195–215. doi: 10.1037/0033-2909.129.2.195. [DOI] [PubMed] [Google Scholar]
- 9.Ainsworth M.D., Blehar M., Waters E., Wall S. Erlbaum; Hillsdale, New Jersey: 1978. Patterns of Attachment. [Google Scholar]
- 10.Dunst C.J., Kassow D.Z. Caregiver sensitivity, contingent social responsiveness, and secure infant attachment. J Early Intensive Behav Interv. 2008;5:40–56. [Google Scholar]
- 11.McElwain N.L., Booth-LaForce C. Maternal sensitivity to infant distress and nondistress as predictors of infant-mother attachment security. J Fam Psychol. 2006;20:247–255. doi: 10.1037/0893-3200.20.2.247. [DOI] [PubMed] [Google Scholar]
- 12.Pederson D.R., Moran G., Sitko C., Campbell K., Ghesquire K., Acton H. Maternal sensitivity and the security of infant-mother attachment: AQ-sort study. Child Dev. 1990;61:1974–1983. doi: 10.1111/j.1467-8624.1990.tb03579.x. [DOI] [PubMed] [Google Scholar]
- 13.Fay-Stammbach T., Hawes D.J., Meredith P. Parenting influences on executive function in early childhood: A review. Child Dev Perspect. 2014;8:258–264. [Google Scholar]
- 14.Groh A.M., Fearon R.M.P., van IJzendoorn M.H., Bakermans-Kranenburg M.J., Roisman G.I. Attachment in the early life course: Meta-analytic evidence for its role in socioemotional development. Child Dev Perspect. 2017;11:70–76. [Google Scholar]
- 15.Morris A.S., Criss M.M., Silk J.S., Houltberg B.J. The impact of parenting on emotion regulation during childhood and adolescence. Child Dev Perspect. 2017;11:233–238. [Google Scholar]
- 16.Groh A.M., Roisman G.I., van IJzendoorn M.H., Bakermans-Kranenburg M.J., Fearon R.P. The significance of insecure and disorganized attachment for children’s internalizing symptoms: A meta-analytic study. Child Dev. 2012;83:591–610. doi: 10.1111/j.1467-8624.2011.01711.x. [DOI] [PubMed] [Google Scholar]
- 17.Humphreys K.L., Gleason M.M., Drury S.S., Miron D., Nelson C.A., 3rd, Fox N.A., Zeanah C.H. Effects of institutional rearing and foster care on psychopathology at age 12 years in Romania: Follow-up of an open, randomised controlled trial. Lancet Psychiatry. 2015;2:625–634. doi: 10.1016/S2215-0366(15)00095-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McLaughlin K.A., Zeanah C.H., Fox N.A., Nelson C.A. Attachment security as a mechanism linking foster care placement to improved mental health outcomes in previously institutionalized children. J Child Psychol Psychiatry. 2012;53:46–55. doi: 10.1111/j.1469-7610.2011.02437.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Smyke A.T., Zeanah C.H., Jr., Fox N.A., Nelson C.A., 3rd A new model of foster care for young children: The Bucharest early intervention project. Child Adolesc Psychiatr Clin N Am. 2009;18:721–734. doi: 10.1016/j.chc.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 20.Stormshak E.A., Bierman K.L., McMahon R.J., Lengua L.J. Parenting practices and child disruptive behavior problems in early elementary school. Conduct Problems Prevention Research Group. J Clin Child Psychol. 2000;29:17–29. doi: 10.1207/S15374424jccp2901_3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stovall K.C., Dozier M. Infants in foster care: An attachment theory perspective. Adoption Q. 1998;2:55–88. [Google Scholar]
- 22.van IJzendoorn M.H., Dijkstra J., Bus A.G. Attachment, intelligence, and language: A meta-analysis+ Soc Dev. 1995;4:115–128. [Google Scholar]
- 23.Harter S. In: Self-Esteem Issues and Answers: A Sourcebook of Current Perspectives. Kernis M., editor. Psychology Press; New York: 2006. The development of self-esteem; pp. 144–150. [Google Scholar]
- 24.Chaplin T.M., Cole P.M., Zahn-Waxler C. Parental socialization of emotion expression: Gender differences and relations to child adjustment. Emotion. 2005;5:80–88. doi: 10.1037/1528-3542.5.1.80. [DOI] [PubMed] [Google Scholar]
- 25.Eisenberg N., Valiente C., Morris A.S., Fabes R.A., Cumberland A., Reiser M., et al. Longitudinal relations among parental emotional expressivity, children’s regulation, and quality of socioemotional functioning. Dev Psychol. 2003;39:3–19. doi: 10.1037//0012-1649.39.1.3. [DOI] [PubMed] [Google Scholar]
- 26.Lunkenheimer E., Hamby C.M., Lobo F.M., Cole P.M., Olson S.L. The role of dynamic, dyadic parent–child processes in parental socialization of emotion. Dev Psychol. 2020;56:566–577. doi: 10.1037/dev0000808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McLaughlin K.A. Future directions in childhood adversity and youth psychopathology. J Clin Child Adolesc Psychol. 2016;45:361–382. doi: 10.1080/15374416.2015.1110823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McLaughlin K.A., Sheridan M.A., Lambert H.K. Childhood adversity and neural development: Deprivation and threat as distinct dimensions of early experience. Neurosci Biobehav Rev. 2014;47:578–591. doi: 10.1016/j.neubiorev.2014.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McLaughlin K.A., Green J.G., Gruber M.J., Sampson N.A., Zaslavsky A.M., Kessler R.C. Childhood adversities and first onset of psychiatric disorders in a national sample of adolescents. Arch Gen Psychiatry. 2012;69:1151–1160. doi: 10.1001/archgenpsychiatry.2011.2277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Green J.G., McLaughlin K.A., Berglund P., Gruber M.J., Sampson N.A., Zaslavsky A.M., et al. Childhood adversities and adult psychopathology in the National Comorbidity Survey Replication (NCS-R) I: Associations with first onset of DSM-IV disorders. Arch Gen Psychiatry. 2010;62:113–123. doi: 10.1001/archgenpsychiatry.2009.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Finkelhor D., Ormrod R., Turner H., Hamby S.L. The victimization of children and youth: A comprehensive, national survey. Child Maltreat. 2005;10:5–25. doi: 10.1177/1077559504271287. [DOI] [PubMed] [Google Scholar]
- 32.Felitti V.J., Anda R.F., Nordenberg D., Williamson D.F., Spitz A.M., Edwards V., et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 33.Widom C.S., Czaja S.J., Bentley T., Johnson M.S. A prospective investigation of physical health outcomes in abused and neglected children: New findings from a 30-year follow-up. Am J Public Health. 2012;102:1135–1144. doi: 10.2105/AJPH.2011.300636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wegman H.L., Stetler C. A meta-analytic review of the effects of childhood abuse on medical outcomes in adulthood. Psychosom Med. 2009;71:805–812. doi: 10.1097/PSY.0b013e3181bb2b46. [DOI] [PubMed] [Google Scholar]
- 35.Kolb B., Gibb R. Searching for the principles of brain plasticity and behavior. Cortex. 2014;58:251–260. doi: 10.1016/j.cortex.2013.11.012. [DOI] [PubMed] [Google Scholar]
- 36.Nelson C.A., Gabard-Durnam L.J. Early adversity and critical periods: Neurodevelopmental consequences of violating the expectable environment. Trends Neurosci. 2020;43:133–143. doi: 10.1016/j.tins.2020.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McLaughlin KA, Gabard-Durnam L (in press): Experience-driven plasticity and the emergence of psychopathology: A mechanistic framework integrating development and the environment into the Research Domain Criteria (RDoC) model. J Abnorm Psychol. [DOI] [PMC free article] [PubMed]
- 38.Greenough W.T., Black J.E., Wallace C.S. Experience and brain development. Child Dev. 1987;58:539–559. [PubMed] [Google Scholar]
- 39.Takesian A.E., Hensch T.K. Balancing plasticity/stability across brain development. Prog Brain Res. 2013;207:3–34. doi: 10.1016/B978-0-444-63327-9.00001-1. [DOI] [PubMed] [Google Scholar]
- 40.Gabard-Durnam L., McLaughlin K.A. Sensitive periods in human development: Charting a course for the future. Curr Opin Behav Sci. 2020;36:120–128. [Google Scholar]
- 41.Werker J.F., Hensch T.K. Critical periods in speech perception: New directions. Annu Rev Psychol. 2015;66:173–196. doi: 10.1146/annurev-psych-010814-015104. [DOI] [PubMed] [Google Scholar]
- 42.Fu M., Zuo Y. Experience-dependent structural plasticity in the cortex. Trends Neurosci. 2011;34:177–187. doi: 10.1016/j.tins.2011.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kuhl P.K. Brain mechanisms in early language acquisition. Neuron. 2010;67:713–727. doi: 10.1016/j.neuron.2010.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Smyke A.T., Zeanah C.H., Fox N.A., Nelson C.A., Guthrie D. Placement in foster care enhances quality of attachment among young institutionalized children. Child Dev. 2010;81:212–223. doi: 10.1111/j.1467-8624.2009.01390.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McLaughlin K.A., Weissman D., Bitrán D. Childhood adversity and neural development: A systematic review. Annu Rev Dev Psychol. 2019;1:277–312. doi: 10.1146/annurev-devpsych-121318-084950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McLaughlin K.A., Sheridan M.A., Winter W., Fox N.A., Zeanah C.H., Nelson C.A. Widespread reductions in cortical thickness following severe early-life deprivation: A neurodevelopmental pathway to attention-deficit/hyperactivity disorder. Biol Psychiatry. 2014;76:629–638. doi: 10.1016/j.biopsych.2013.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Edmiston E.E., Wang F., Mazure C.M., Guiney J., Sinha R., Mayes L.C., Blumberg H.P. Corticostriatal-limbic gray matter morphology in adolescents with self-reported exposure to childhood maltreatment. Arch Pediatr Adolesc Med. 2011;165:1069–1077. doi: 10.1001/archpediatrics.2011.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hodel A.S., Hunt R.H., Cowell R.A., Van Den Heuvel S.E., Gunnar M.R., Thomas K.M. Duration of early adversity and structural brain development in post-institutionalized adolescents. NeuroImage. 2015;105:112–119. doi: 10.1016/j.neuroimage.2014.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Herzberg M.P., Hodel A.S., Cowell R.A., Hunt R.H., Gunnar M.R., Thomas K.M. Risk taking, decision-making, and brain volume in youth adopted internationally from institutional care. Neuropsychologia. 2018;119:262–270. doi: 10.1016/j.neuropsychologia.2018.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mueller S.C., Maheu F.S., Dozier M., Peloso E., Mandell D., Leibenluft E., et al. Early-life stress is associated with impairment in cognitive control in adolescence: An fMRI study. Neuropsychologia. 2010;48:3037–3044. doi: 10.1016/j.neuropsychologia.2010.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rosen M.L., Sheridan M.A., Sambrook K.A., Meltzoff A.N., McLaughlin K.A. Socioeconomic disparities in academic achievement: A multimodal investigation of neural mechanisms in children and adolescents. Neuroimage. 2018;173:298–310. doi: 10.1016/j.neuroimage.2018.02.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Romeo R.R., Leonard J.A., Robinson S.T., West M.R., Mackey A.P., Rowe M.L., Gabrieli J.D.E. Beyond the 30-million-word gap: Children’s conversational exposure is associated with language-related brain function. Psychol Sci. 2018;29:700–710. doi: 10.1177/0956797617742725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Romeo R.R., Segaran J., Leonard J.A., Robinson S.T., West M.R., Mackey A.P., et al. Language exposure relates to structural neural connectivity in childhood. J Neurosci. 2018;38:7870–7877. doi: 10.1523/JNEUROSCI.0484-18.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Miller A.B., Sheridan M.A., Hanson J.L., McLaughlin K.A., Bates J.E., Lansford J.E., et al. Dimensions of deprivation and threat, psychopathology, and potential mediators: A multi-year longitudinal analysis. J Abnorm Psychol. 2018;127:160–170. doi: 10.1037/abn0000331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Spratt E.G., Friedenberg S.L., Swenson C.C., Larosa A., De Bellis M.D., Macias M.M., et al. The effects of early neglect on cognitive, language, and behavioral functioning in childhood. Psychology (Irvine) 2012;3:175–182. doi: 10.4236/psych.2012.32026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Windsor J., Benigno J.P., Wing C.A., Carroll P.J., Koga S.F., Nelson C.A., et al. Effect of foster care on young children’s language learning. Child Dev. 2011;82:1040–1046. doi: 10.1111/j.1467-8624.2011.01604.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pollak S.D., Nelson C.A., Schlaak M.F., Roeber B.J., Wewerka S.S., Wiik K.L., et al. Neurodevelopmental effects of early deprivation in postinstitutionalized children. Child Dev. 2010;81:224–236. doi: 10.1111/j.1467-8624.2009.01391.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bos K.J., Fox N.A., Zeanah C.H., Nelson C.A. Effects of early psychosocial deprivation on the development of memory and executive function. Front Behav Neurosci. 2009;3:16. doi: 10.3389/neuro.08.016.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rosen M.L., Hagen M.P., Lurie L.A., Miles Z.E., Sheridan M.A., Meltzoff A.N., McLaughlin K.A. Cognitive stimulation as a mechanism linking socioeconomic status with executive function: A longitudinal investigation. Child Dev. 2020;91:e762–e779. doi: 10.1111/cdev.13315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.McLaughlin K.A., Peverill M., Gold A.L., Alves S., Sheridan M.A. Child maltreatment and neural systems underlying emotion regulation. J Am Acad Child Adolesc Psychiatry. 2015;54:753–762. doi: 10.1016/j.jaac.2015.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.McCrory E.J., De Brito S.A., Sebastian C.L., Mechelli A., Bird G., Kelly P.A., Viding E. Heightened neural reactivity to threat in child victims of family violence. Curr Biol. 2011;21:R947–R948. doi: 10.1016/j.cub.2011.10.015. [DOI] [PubMed] [Google Scholar]
- 62.Jenness J.L., Peverill M., Miller A.B., Heleniak C., Robertson M.M., Sambrook K.A., et al. Alterations in neural circuits underlying emotion regulation following child maltreatment: A mechanism underlying trauma-related psychopathology. Psychol Med. 2021;51:1880–1889. doi: 10.1017/S0033291720000641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ganzel B.L., Kim P., Gilmore H., Tottenham N., Temple E. Stress and the healthy adolescent brain: Evidence for the neural embedding of life events. Dev Psychopathol. 2013;25:879–889. doi: 10.1017/S0954579413000242. [DOI] [PubMed] [Google Scholar]
- 64.Suzuki H., Luby J.L., Botteron K.N., Dietrich R., McAvoy M.P., Barch D.M. Early life stress and trauma and enhanced limbic activation to emotionally valenced faces in depressed and healthy children. J Am Acad Child Adolesc Psychiatry. 2014;53:800–813.e10. doi: 10.1016/j.jaac.2014.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Weissman D.G., Lambert H.K., Rodman A.M., Peverill M.A., Sheridan M.A., McLaughlin K.A. Reduced hippocampal and amygdala volume as a mechanism underlying stress sensitization to depression following childhood trauma. Depress Anxiety. 2020;37:916–925. doi: 10.1002/da.23062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gold A.L., Sheridan M.A., Peverill M., Busso D.S., Lambert H.K., Alves S., et al. Childhood abuse and reduced cortical thickness in brain regions involved in emotional processing. J Child Psychol Psychiatry. 2016;57:1154–1164. doi: 10.1111/jcpp.12630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hanson J.L., Chung M.K., Avants B.B., Shirtcliff E.A., Gee J.C., Davidson R.J., Pollak S.D. Early stress is associated with alterations in the orbitofrontal cortex: A tensor-based morphometry investigation of brain structure and behavioral risk. J Neurosci. 2010;30:7466–7472. doi: 10.1523/JNEUROSCI.0859-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hanson J.L., Nacewicz B.M., Sutterer M.J., Cayo A.A., Schaefer S.M., Rudolph K.D., et al. Behavioral problems after early life stress: Contributions of the hippocampus and amygdala. Biol Psychiatry. 2015;77:314–323. doi: 10.1016/j.biopsych.2014.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Saxbe D., Khoddam H., Del Piero L.D., Stoycos S.A., Gimbel S.I., Margolin G., Kaplan J.T. Community violence exposure in early adolescence: Longitudinal associations with hippocampal and amygdala volume and resting state connectivity. Dev Sci. 2018;21 doi: 10.1111/desc.12686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Dixon M.L., Thiruchselvam R., Todd R., Christoff K. Emotion and the prefrontal cortex: An integrative review. Psychol Bull. 2017;143:1033–1081. doi: 10.1037/bul0000096. [DOI] [PubMed] [Google Scholar]
- 71.Phelps E.A. Human emotion and memory: Interactions of the amygdala and hippocampal complex. Curr Opin Neurobiol. 2004;14:198–202. doi: 10.1016/j.conb.2004.03.015. [DOI] [PubMed] [Google Scholar]
- 72.Heleniak C., Jenness J.L., Van der Stoep A.V., McCauley E., McLaughlin K.A. Childhood maltreatment exposure and disruptions in emotion regulation: A transdiagnostic pathway to adolescent internalizing and externalizing psychopathology. Cognit Ther Res. 2016;40:394–415. doi: 10.1007/s10608-015-9735-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.McLaughlin K.A., Lambert H.K. Child trauma exposure and psychopathology: Mechanisms of risk and resilience. Curr Opin Psychol. 2017;14:29–34. doi: 10.1016/j.copsyc.2016.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Pollak S.D., Tolley-Schell S.A. Selective attention to facial emotion in physically abused children. J Abnorm Psychol. 2003;112:323–338. doi: 10.1037/0021-843x.112.3.323. [DOI] [PubMed] [Google Scholar]
- 75.Pollak S.D., Kistler D.J. Early experience is associated with the development of categorical representations for facial expressions of emotion. Proc Natl Acad Sci U S A. 2002;99:9072–9076. doi: 10.1073/pnas.142165999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Pollak S.D., Sinha P. Effects of early experience on children’s recognition of facial displays of emotion. Dev Psychol. 2002;38:784–791. doi: 10.1037//0012-1649.38.5.784. [DOI] [PubMed] [Google Scholar]
- 77.Shackman J.E., Shackman A.J., Pollak S.D. Physical abuse amplifies attention to threat and increases anxiety in children. Emotion. 2007;7:838–852. doi: 10.1037/1528-3542.7.4.838. [DOI] [PubMed] [Google Scholar]
- 78.Weissman D.G., Bitran D., Miller A.B., Schaefer J.D., Sheridan M.A., McLaughlin K.A. Difficulties with emotion regulation as a transdiagnostic mechanism linking child maltreatment with the emergence of psychopathology. Dev Psychopathol. 2019;31:899–915. doi: 10.1017/S0954579419000348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Weissman D.G., Jenness J.L., Colich N.L., Miller A.B., Sambrook K.A., Sheridan M.A., McLaughlin K.A. Altered neural processing of threat-related information in children and adolescents exposed to violence: A transdiagnostic mechanism contributing to the emergence of psychopathology. J Am Acad Child Adolesc Psychiatry. 2020;59:1274–1284. doi: 10.1016/j.jaac.2019.08.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Luby J.L., Tillman R., Barch D.M. Association of timing of adverse childhood experiences and caregiver support with regionally specific brain development in adolescents. JAMA Network Open. 2019;2 doi: 10.1001/jamanetworkopen.2019.11426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kok R., Thijssen S., Bakermans-Kranenburg M.J., Jaddoe V.W., Verhulst F.C., White T., et al. Normal variation in early parental sensitivity predicts child structural brain development. J Am Acad Child Adolesc Psychiatry. 2015;54:824–831.e1. doi: 10.1016/j.jaac.2015.07.009. [DOI] [PubMed] [Google Scholar]
- 82.Whittle S., Vijayakumar N., Dennison M., Schwartz O., Simmons J.G., Sheeber L., Allen N.B. Observed measures of negative parenting predict brain development during adolescence. PLoS One. 2016;11 doi: 10.1371/journal.pone.0147774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Miller G.E., Chen E. The biological residue of childhood poverty. Child Dev Perspect. 2013;7:67–73. doi: 10.1111/cdep.12021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hostinar C.E., Sullivan R.M., Gunnar M.R. Psychobiological mechanisms underlying the social buffering of the hypothalamic–pituitary–adrenocortical axis: A review of animal models and human studies across development. Psychol Bull. 2014;140:256–282. doi: 10.1037/a0032671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Luthar S.S. In: Developmental Psychopathology: Risk, Disorder, and Adaptation. Cicchetti D., Cohen D.J., editors. John Wiley & Sons, Inc.; 2006. Resilience in development: A synthesis of research across five decades; pp. 739–795. [Google Scholar]
- 86.Masten A.S. Ordinary magic. Resilience processes in development. Am Psychol. 2001;56:227–238. doi: 10.1037//0003-066x.56.3.227. [DOI] [PubMed] [Google Scholar]
- 87.Obradović J., Long J.D., Cutuli J.J., Chan C.K., Hinz E., Heistad D., Masten A.S. Academic achievement of homeless and highly mobile children in an urban school district: Longitudinal evidence on risk, growth, and resilience. Dev Psychopathol. 2009;21:493–518. doi: 10.1017/S0954579409000273. [DOI] [PubMed] [Google Scholar]
- 88.Barch D.M., Whalen D., Gilbert K., Kelly D., Kappenman E.S., Hajcak G., Luby J.L. Neural indicators of anhedonia: Predictors and mechanisms of treatment change in a randomized clinical trial in early childhood depression. Biol Psychiatry. 2020;88:879–887. doi: 10.1016/j.biopsych.2020.06.032. [DOI] [PubMed] [Google Scholar]
- 89.Bick J., Palmwood E.N., Zajac L., Simons R., Dozier M. Early parenting intervention and adverse family environments affect neural function in middle childhood. Biol Psychiatry. 2019;85:326–335. doi: 10.1016/j.biopsych.2018.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Biglan A., Flay B.R., Embry D.D., Sandler I.N. The critical role of nurturing environments for promoting human well-being. Am Psychol. 2012;67:257–271. doi: 10.1037/a0026796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Britto P.R., Lye S.J., Proulx K., Yousafzai A.K., Matthews S.G., Vaivada T., et al. Nurturing care: Promoting early childhood development. Lancet. 2017;389:91–102. doi: 10.1016/S0140-6736(16)31390-3. [DOI] [PubMed] [Google Scholar]
- 92.Noble K.G., Magnuson K.A., Gennetian L.A., Duncan G.J., Yoshikawa H., Fox N.A., Halpern-Meekin S. 2021. Baby’s first years: Design of a randomized controlled trial of poverty reduction in the United States 148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Stein J. The Washington Post; 2021. IRS begins sending monthly checks to millions of American parents in crucial test for Biden. [Google Scholar]
- 94.Stein J. The Washington Post; 2021. Child cash benefit will begin hitting millions of parents’ bank accounts. [Google Scholar]
- 95.Letourneau N.L., Dennis C.L., Cosic N., Linder J. The effect of perinatal depression treatment for mothers on parenting and child development: A systematic review. Depress Anxiety. 2017;34:928–966. doi: 10.1002/da.22687. [DOI] [PubMed] [Google Scholar]
- 96.Clauss-Ehlers C.S. In search of an evidence-based approach to understand and promote effective parenting practices. Couple Fam Psychol Res Pract. 2017;6:135–153. [Google Scholar]
- 97.Dishion T.J., Shaw D., Connell A., Gardner F., Weaver C., Wilson M. The family check-up with high-risk indigent families: Preventing problem behavior by increasing parents’ positive behavior support in early childhood. Child Dev. 2008;79:1395–1414. doi: 10.1111/j.1467-8624.2008.01195.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Dozier M., Bernard K. Attachment and biobehavioral catch-up: Addressing the needs of infants and toddlers exposed to inadequate or problematic caregiving. Curr Opin Psychol. 2017;15:111–117. doi: 10.1016/j.copsyc.2017.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ward M.A., Theule J., Cheung K. Parent–child interaction therapy for child disruptive behaviour disorders: A meta-analysis. Child Youth Care Forum. 2016;45:675–690. [Google Scholar]
- 100.Chaffin M., Silovsky J.F., Funderburk B., Valle L.A., Brestan E.V., Balachova T., et al. Parent-child interaction therapy with physically abusive parents: Efficacy for reducing future abuse reports. J Consult Clin Psychol. 2004;72:500–510. doi: 10.1037/0022-006X.72.3.500. [DOI] [PubMed] [Google Scholar]
- 101.Timmer S.G., Urquiza A.J., Zebell N.M., McGrath J.M. Parent-child interaction therapy: Application to maltreating parent-child dyads. Child Abuse Negl. 2005;29:825–842. doi: 10.1016/j.chiabu.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 102.Luby J.L., Barch D.M., Whalen D., Tillman R., Freedland K.E. A randomized controlled trial of parent-child psychotherapy targeting emotion development for early childhood depression. Am J Psychiatry. 2018;175:1102–1110. doi: 10.1176/appi.ajp.2018.18030321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Elkins R.M., Mian N., Comer J., Pincus D.B. The Guilford Press; New York: 2016. Parent–Child Interaction Therapy and Its Adaptations; p. 271. [Google Scholar]
- 104.McLaughlin K.A., Pautsch J., Luby J.L. 2021. THRIVE Manual. Unpublished manual. Washington University School of Medicine and Harvard University. [Google Scholar]
- 105.Fisher P.A., Frenkel T.I., Noll L.K., Berry M., Yockelson M. Promoting healthy child development via a two-generation translational neuroscience framework: The Filming Interactions to Nurture Development video coaching program. Child Dev Perspect. 2016;10:251–256. doi: 10.1111/cdep.12195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Olds D.L. The nurse–family partnership: An evidence-based preventive intervention. Infant Ment Health J. 2006;27:5–25. doi: 10.1002/imhj.20077. [DOI] [PubMed] [Google Scholar]
- 107.Juffer F., Bakermans-Kranenburg M.J., van IJzendoorn M.H. Pairing attachment theory and social learning theory in video-feedback intervention to promote positive parenting. Curr Opin Psychol. 2017;15:189–194. doi: 10.1016/j.copsyc.2017.03.012. [DOI] [PubMed] [Google Scholar]
- 108.Lieberman A.F. The treatment of attachment disorder in infancy and early childhood: Reflections from clinical intervention with later-adopted foster care children. Attach Hum Dev. 2003;5:279–282. doi: 10.1080/14616730310001596133. [DOI] [PubMed] [Google Scholar]
- 109.Bernard K., Meade E.B., Dozier M. Parental synchrony and nurturance as targets in an attachment based intervention: Building upon Mary Ainsworth’s insights about mother–infant interaction. Attach Hum Dev. 2013;15:507–523. doi: 10.1080/14616734.2013.820920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Webster-Stratton C., Reid M.J. In: Evidence-based Psychotherapies for Children and Adolescents. 3rd ed. Kazdin A.E., Weisz J.R., editors. Guildford Publications; New York: 2017. The Incredible Years Parents, Teachers, and Children Training Series: A multifaceted treatment approach for young children with conduct problems. [Google Scholar]
- 111.Huber A., McMahon C., Sweller N. Improved child behavioural and emotional functioning after Circle of Security 20-week intervention. Attach Hum Dev. 2015;17:547–569. doi: 10.1080/14616734.2015.1086395. [DOI] [PubMed] [Google Scholar]
- 112.Heckman J.J. Skill formation and the economics of investing in disadvantaged children. Science. 2006;312:1900–1902. doi: 10.1126/science.1128898. [DOI] [PubMed] [Google Scholar]
- 113.Kagitcibasi C., Sunar D., Bekman S., Baydar N., Cemalcilar Z. Continuing effects of early enrichment in adult life: The Turkish Early Enrichment Project 22 years later. J Appl Dev Psychol. 2009;30:764–779. [Google Scholar]
- 114.Gertler P., Heckman J., Pinto R., Zanolini A., Vermeersch C., Walker S., et al. Labor market returns to an early childhood stimulation intervention in Jamaica. Science. 2014;344:998–1001. doi: 10.1126/science.1251178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Yousafzai A.K., Rasheed M.A., Rizvi A., Armstrong R., Bhutta Z.A. Effect of integrated responsive stimulation and nutrition interventions in the Lady Health Worker programme in Pakistan on child development, growth, and health outcomes: A cluster-randomised factorial effectiveness trial. Lancet. 2014;384:1282–1293. doi: 10.1016/S0140-6736(14)60455-4. [DOI] [PubMed] [Google Scholar]
- 116.McLaughlin K.A., Gabard-Durnam L. Experience-driven plasticity and the emergence of psychopathology: A mechanistic framework integrating development and the environment into the Research Domain Criteria (RDoC) model. J Abnorm Psychol. 2020 doi: 10.1037/abn0000598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Nelson C.A., 3rd, Zeanah C.H., Fox N.A., Marshall P.J., Smyke A.T., Guthrie D. Cognitive recovery in socially deprived young children: The Bucharest Early Intervention Project. Science. 2007;318:1937–1940. doi: 10.1126/science.1143921. [DOI] [PubMed] [Google Scholar]
- 118.McManus B.M., Richardson Z., Schenkman M., Murphy N.J., Everhart R.M., Hambidge S., Morrato E. Child characteristics and early intervention referral and receipt of services: A retrospective cohort study. BMC Pediatr. 2020;20:84. doi: 10.1186/s12887-020-1965-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Finkelhor D., Turner H., LaSelva D. Receipt of behavioral health services among us children and youth with adverse childhood experiences or mental health symptoms. JAMA Network Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.1435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Chang S.M., Grantham-McGregor S.M., Powell C.A., Vera-Hernández M., Lopez-Boo F., Baker-Henningham H., Walker S.P. Integrating a parenting intervention with routine primary health care: A cluster randomized trial. Pediatrics. 2015;136:272–280. doi: 10.1542/peds.2015-0119. [DOI] [PubMed] [Google Scholar]