Abstract
Methemoglobinemia is a rare disorder associated with oxidization of divalent ferro‐iron of hemoglobin (Hb) to ferri‐iron of methemoglobin (MetHb). Methemoglobinemia can result from either inherited or acquired processes. Acquired forms are the most common, mainly due to the exposure to substances that cause oxidation of the Hb both directly or indirectly. Inherited forms are due either to autosomal recessive variants in the CYB5R3 gene or to autosomal dominant variants in the globin genes, collectively known as HbM disease. Our recommendations are based on a systematic literature search. A series of questions regarding the key signs and symptoms, the methods for diagnosis, the clinical management in neonatal/childhood/adulthood period, and the therapeutic approach of methemoglobinemia were formulated and the relative recommendations were produced. An agreement was obtained using a Delphi‐like approach and the experts panel reached a final consensus >75% of agreement for all the questions.
1. INTRODUCTION
1.1. Pathophysiology and clinical findings
Methemoglobinemia is a rare disorder associated with oxidization of divalent ferro‐iron of hemoglobin (Hb) to ferri‐iron of methemoglobin (MetHb). 1 The presence of iron in the ferric [Fe3+] state results in allosteric changes that permit the binding of oxygen irreversibly. The corresponding ferro‐globins in the tetramer shifts the oxygen‐dissociation curve of Hb to the left. This shift leads to increased affinity of the ferrous iron for oxygen and thus impaired oxygen release to the tissue, 2 resulting in hypoxia with the so called “functional anemia” without Hb decrease. 3 Methemoglobinemia can result from either inherited or acquired processes. Acquired forms are the most common, mainly due to the exposure to substances that cause oxidation of the Hb both directly or indirectly. Inherited forms are due either to autosomal recessive variants in the CYB5R3 gene or to autosomal dominant variants in the globin genes, collectively known as HbM disease. 1 , 4 , 5 The diagnosis of methemoglobinemia should be suspected in case of unexplained cyanosis and hypoxemia. The clinical presentation is variable from mildly symptomatic to severe cases. 2 The main findings are cyanosis, pallor, fatigue, weakness, headache, central nervous system depression, metabolic acidosis, seizures, dysrhythmias, coma, and death. 6 The severity of the presentation depends on the percentage of MetHb (Table 1), the rate of increase in MetHb levels, the intrinsic ability of the patient to clear it, and the patient's underlying functional status. MetHb can be expressed either by concentration or percentage (calculated by dividing the concentration of MetHb by the concentration of total Hb). 2 The percentage is the correct way to evaluate the methemoglobinemia. Of note, the cyanosis is determined by the total amount of MetHb, i.e. more than 1.5 g/dL of MetHb. Several comorbidities such as anemia, heart failure, chronic obstructive pulmonary disease, and any pathologies that could impair the capacity of Hb to deliver oxygen may worsen the symptoms of methemoglobinemia. 6 It is also important to consider the duration and amount of exposure to an oxidizing agent. 3
TABLE 1.
Signs, symptoms, and causes of methemoglobinemia
| MetHb level | Signs | Symptoms | Causes |
|---|---|---|---|
| <10% | Low pulse oximeter readings, alteration of the skin color (pale, gray, blue) | Asymptomatic | Acquired |
| 10%‐30% |
Cyanosis Dark brown blood |
Asymptomatic/confusion | Enzymopenic methemoglobinemia, HbM, acquired |
| 30%‐50% | Dyspnea, dizziness, syncope | Confusion, chest pain, palpitations, headache, fatigue | Acquired ± hereditary |
| 50%‐70% | Tachypnea, metabolic acidosis, dysrhythmias, seizure, delirium, coma | Confusion, chest pain, palpitations, headache, fatigue | Acquired ± hereditary |
| >70% | Severe hypoxemia, death | ‐ | Acquired ± hereditary |
Abbreviations: HbM, M group variants of Hb; MetHb, methemoglobin.
1.2. Hereditary methemoglobinemia
1.2.1. Enzyme deficiency
Hereditary methemoglobinemia is a rare genetic condition caused by NADH cytochrome b5 reductase deficiency (also known as NADH diaphorase deficiency) due to biallelic mutations in the CYB5R3 gene that codes the cytochrome b5 reductase enzyme (CYB5R) (Table 2). 7 To date, more than 80 different disease‐causing variants in the CYB5R3 gene have been reported (HGMD Professional 2020.4), 7 , 8 , 9 and genotype–phenotype correlation has been described in this disease. 10 , 11 Patients with biallelic causative variants in CYB5R3 gene often exhibit erythrocytosis. Based on the severity of the enzyme deficiency, this condition can be classified into two different subtypes: (i) type I, mainly due to missense variants that cause a production of an unstable enzyme purely in the red blood cells, associated with MetHb levels above 25%, cyanosis, headache, fatigue, and dyspnea; of note, in these cases, cyanosis may be the only sign since most of type I patients are asymptomatic, and (ii) type II, caused by variants that lead to either low expression or low activity of the enzyme in all the tissues and associated with alterations in the lipid metabolism and neurological involvement. In the latter condition, 8%‐40% of the Hb is in the form of MetHb. 7 Type II is associated with high morbidity and mortality because of severe neurologic manifestations. The difference between methemoglobin types I and II is due to differential expression of CYB5R isoforms in red blood cells compared to other cell types. 7
TABLE 2.
Acquired and hereditary forms of methemoglobinemia
| Disease | Transmission | Cyanosis | Anemia | Other symptoms | Gene(s) | MetHb level % | CYB5R activity | Hb electrophoresis/HPLC |
|---|---|---|---|---|---|---|---|---|
| Drug exposure | Acquired | Yes | No | ‐ | ‐ | Variable | Normal | Normal |
| Methemoglobinemia, type I | Autosomal recessive |
Yes since birth |
No | ‐ | CYB5R3 | 20–30 | Decreased | Normal |
| Methemoglobinemia, type II | Autosomal recessive |
Yes since birth |
No | Neurological involvement | CYB5R3 | 8–40 | Decreased | Normal |
| Methemoglobinemia, type IV | Autosomal recessive | Yes | No |
46,XY DSD Ambiguous genitalia |
CYB5A | 12–19 | Normal | Normal |
| HbM disease | Autosomal dominant |
Yes since birth or after HbF/A switching |
Yes | ‐ | HBA1, HBA2, HBB, HBG1, HBG2 | 12–25 | Normal | Abnormal |
| Unstable Hb | Autosomal dominant | Yes | Yes | ‐ | HBA1, HBA2, HBB, HBG1, HBG2 | Variable (Stressor induced) | Normal |
N or Abnormal |
Abbreviation: DSD, disorder of sexual differentiation.
Methemoglobinemia resulting from CYB5R deficiency is endemic among certain populations in the US and Russia. 12 A selection advantage of the African‐specific polymorphism CYB5R3‐Thr117Ser, detected in 46% of African Americans, has been hypothesized to offer protection against malaria infection. Although not known to have any functional significance, this variant appears to ameliorate the severity of anemia in SCD patients with malaria, in the absence of glucose‐6‐phosphate dehydrogenase (G6PD) deficiency. 13
In very rare cases, inherited methemoglobinemia is caused by deficiency of the electron acceptor cytochrome b5. 14 This causes methemoglobinemia associated with ambiguous genitalia due to a homozygous variant in the CYB5A gene, encoding the microsomal cytochrome b5 (Table 2). 15 This condition is due to isolated 17,20‐lyase deficiency since the cofactor cytochrome b5 is required for optimal 17,20‐lyase activity. 16
1.2.2. M‐hemoglobins
In addition to the autosomal recessive methemoglobinemia subtypes, a rare MetHb group, called M group variants of Hb, results from autosomal dominant variants in the genes encoding alpha‐globin (HBA1, HBA2), beta‐globin (HBB), or gamma‐globin (HBG1, HBG2). Patients with HbM disease are cyanotic but usually otherwise asymptomatic (Table 2). In HbM disease, structural abnormalities in the globin portion of the molecule cause heme iron to auto‐oxidize. To understand the mechanism of M variants we must dissect the mechanism by which Hb binds oxygen and releases it. Heme is localized in a hydrophobic pocket between the E and F α‐helices of each of the four globin chains. The iron atom in the heme forms four bonds with the pyrrole nitrogen atoms of the porphyrin ring and a fifth covalent bond with the imidazole nitrogen of a histidine residue in the nearby F α‐helix. 17 This histidine, residue 87 in the α chain and 92 in the β chain, is designated as the proximal histidine. On the opposite side of the porphyrin ring the iron atom lies adjacent to another histidine residue to which, however, it is not covalently bonded. This distal histidine is in position 58 in the α chain and in position 63 in the β chain. Oxygen is discharged from the heme pocket as a superoxide anion, removing an electron from the iron and leaving it in the ferric state. The enzymatic machinery of the erythrocytes reduces the iron to the divalent form, converting the MetHb to Hb. In most forms of the HbM, tyrosine is substituted for either the proximal or the distal histidine. Tyrosine can form an iron‐phenolate complex that resists reduction to the divalent state by the metabolic systems of the RBC. At least 13 different HbM variants have been reported. 4 , 5 , 18 Four HbMs are a consequence of substitution of tyrosine for histidine in the proximal and distal sites of the α and β chains. These four HbMs have been designated by the geographic names of their discovery, i.e. Boston, Saskatoon, Iwate, and Hyde Park. Analogous His→Tyr substitutions in the γ chain of fetal Hb (HbF) have also been documented and have been designated Hb F‐M‐Osaka 19 and Hb FMFort Ripley. 20
Patients with HbM develop cyanosis. For the α‐globin variants, the dusky color is evident at birth, while the clinical manifestations of β‐globin variants become evident only after β chains have replaced the fetal γ chains at 6 to 9 months of age. Hemolytic anemia with jaundice can be present, as observed in HbM Saskatoon and HbM Hyde Park. 21 Additionally, some patients with unstable Hb also have elevated MetHb levels associated with hemolytic anemia. 22 , 23 This is the case of HbChile (β28 Leu → Met), an unstable Hb characterized by chronic methemoglobinemia. 24
Other unstable hemoglobin variants develop MetHb only after stressor events. 25
1.3. Acquired methemoglobinemia
Acquired methemoglobinemia is the consequence of drug ingestion or toxic exposure that cause acceleration of Hb oxidization from the ferrous to the ferric state (Table 2). The drugs that cause methemoglobinemia are numerous, including sulfonamides, lidocaine and other aniline derivatives, and nitrites (Table 3). The most common drugs are benzocaine and lidocaine. 26 , 27 , 28 Nitrates and the nitrites contaminating water supplies or used as preservatives in foods can also be trigger agents. 29 The symptoms are those of anemia, as MetHb does not transport oxygen and may comprise shortness of breath, palpitations, and vascular collapse. Drugs that induce methemoglobinemia often also cause hemolysis. Newborn infants are particularly susceptible to the development of methemoglobinemia because the activity of CYB5R is lower compared to adult period. 30 Thus, methemoglobinemia is observed in infants because of toxic materials, such as aniline dyes used on diapers 31 and the ingestion of nitrate‐contaminated water 32 , 33 and even of beets. 34 Inhaled nitric oxide is approved for treatment of infants with pulmonary hypertension because of its vasodilatory effect on pulmonary vessels. During the binding and release of nitric oxide from Hb, MetHb is formed at a higher rate. In a study of 163 treated infants, MetHb was above 5% in one and between 2.5% and 5% in 16 infants. 35
TABLE 3.
Some drugs that cause methemoglobinemia
| Phenazopyridine (Pyridium) |
| Sulfamethoxazole |
| Dapsone |
| Aniline |
| Paraquat/monolinuron |
| Nitrate |
| Nitroglycerin |
| Amyl nitrite |
| Isobutyl nitrite |
| Sodium nitrite |
| Benzocaine |
| Prilocaine |
| Methylene blue |
| Chloramine |
Some recreational drugs are also associated with acquired methemoglobinemia, including amyl nitrate (poppers), nitrous oxide (laughing gas) and adulterants used in cocaine (local anesthetics, phenacetin). These can be associated with very high levels of methemoglobinemia (>90%) and fatalities are well described. 36 The clinical history should include details of recreational drug use where appropriate.
1.4. Diagnostic approaches and differential diagnosis
Given the different pathogenic basis of this group of diseases, an accurate clinical and family history, evaluation of consanguinity (more common in CYB5R3 deficiency), as well as review of environmental and drug exposure, is fundamental in making the diagnosis, and differentiating hereditary from acquired forms. In acquired forms, evidence of cyanosis is usually of recent origin and history of drug or toxin exposure should be promptly investigated; a long‐life history of cyanosis or report of dusky skin or blue sclera in the family would be suggestive of congenital forms. Of note, cyanosis may also result from cardiac and pulmonary disease, particularly when right‐to‐left shunting is present.
The key diagnostic tests in the differential diagnosis are MetHb evaluation, measurement of CYB5R activity and genotyping. MetHb levels are best measured using the change of absorbance of MetHb at 630 nm that occurs when cyanide is added, converting the MetHb to cyan‐MetHb, as initially described in the spectrophotometric method by Evelyn‐Malloy. 37 , 38 Human blood contains less than 1% MetHb. There is a direct correlation between MetHb levels and symptoms. CYB5R activity is best measured using ferricyanide as a receptor, measuring the rate of oxidation of NADH. 39 In congenital CYB5R3 deficiency, the residual enzyme activity is usually less than 20% of normal. DNA sequencing of CYB5R3 gene allows characterization of the defect and confirmation of the diagnosis.
Electrophoresis at pH 7.1, can be used to identify HbM variants caused by mutations affecting α‐, β‐, or rarely, γ‐ globin genes. More than 13 different pathogenic variants have been reported to be associated with HbM disease in the HbVar database (https://globin.bx.psu.edu/hbvar/). However, when suspecting a HbM‐variant, targeted sequencing of the α‐ and the ß‐globin genes is commonly selected as the technically simpler, more widely available and more specific diagnostic procedure. Direct sequencing of the globin genes is also appropriate, and can be useful in the presence of transfused blood or to exclude electrophoretically silent variants.
Finally, the advent of next generation sequencing (NGS) technologies allows the determination of significant variants for individual patients suffering from rare red cell disorders including methemoglobinemia, increasing the number of new diagnoses and facilitating differential diagnosis. 40 , 41
1.5. Methods
Our recommendations are based on a systematic literature search. All articles on methemoglobinemia were identified by a PubMed, Online Mendelian Inheritance in Man, and Textbook search, including all the additional relevant references cited in the articles found. The key search terms were “methemoglobin”, “methemoglobinemia”, “inherited methemoglobinemia”, “acquired methemoglobinemia”. The literature search was performed from June 2020 to January 2021. We obtained 92 studies which cover the period from 1933 to 2021. The steering committee and expert panel included 22 members who have been selected for their recognized expertise in research and clinical practice in methemoglobin, with a wide geographical representation in order to provide an international perspective. EHA and EuroBloodNet verified the absence of relevant competing conflict of interests of the authors and supervised the project in regard to compliance to, and consistency with, the methodology adopted by its Committee on Guidelines. EHA provided the organizational and logistic assistance and funding for the necessary face‐to‐face meetings or teleconferences. With this background, a series of questions regarding methemoglobinemia as were formulated and the relative recommendations were produced. An agreement was obtained using a Delphi‐like approach as previously performed. 42 Multiple rounds of questionnaires were generated by a steering committee and a final questionnaire has been sent to a panel of experts. The responses by this expert panel was aggregated and shared with the group after each round. The experts adjusted their answers in subsequent rounds; thus, the final response has been reached through consensus >75% (Figure 1).
FIGURE 1.
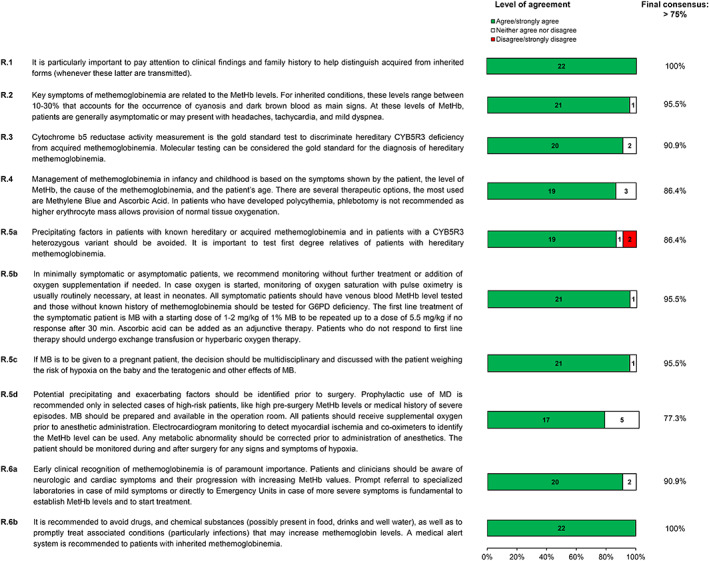
Delphi survey. Level of agreement was assessed by 5‐point Likert scale, 1/2 strongly agree/agree (green bar of histogram), three neither agree or disagree (blank bar of histogram), 4/5 disagree/strongly disagree (red bar of histogram). For each recommendation indicated with R1, R2, R3, R4, R5a, R5b, R5c, R5d, R6a, and R6b, it is indicated the level of agreement with the colored histogram and the final percentage of agreement reached. Final consensus was reached with > 75% of agreement [Color figure can be viewed at wileyonlinelibrary.com]
QUESTIONS
Q1. When should congenital methemoglobinemia be considered as a possible diagnosis?
Congenital methemoglobinemia should be considered in the following clinical situations:
Known family history of methemoglobinemia.
Typically methemoglobinemia due to NADH‐cytochrome b5 reductase deficiency is inherited in an autosomal recessive fashion and so there may be no family history unless the patient is from a small community or their parents are fairly closely related. 43 Alpha, beta and gamma globin mutations causing HbM typically exhibit an autosomal dominant inheritance. Nevertheless, many of these cases are due to de novo mutational events, thus showing a non‐dominant inheritance pattern.
Cyanosis in a newborn baby, infant, child, or adult not associated with hypoxemia, cold exposure or other known explanation
MetHb levels should be measured. Levels are typically >10% if blue discoloration is present. Typically, congenital cases will present at birth in this way, although milder cases may present later in childhood or even adulthood associated with an acute increase in MetHb levels, possibly associated with illness or environmental exposure. Typically, the child is otherwise well (methemoglobinemia, type I) (Table 2) and the cyanosis does not improve with oxygen therapy.
Incidental finding of increased MetHb level.
This occurs most commonly when venous or arterial blood gases are analyzed for some reason, and a high MetHb level is noticed. Usually, the levels are between 3% and 10%, with higher levels likely to cause noticeable cyanosis.
Pulse oximetry showing unexpected or discordant results compared to clinical assessment or other measures of oxygenation
Pulse oximetry screening at birth or before newborns are discharged may reveal subclinical hypoxemia. 44 Methemoglobinemia interferes with the accuracy of pulse oximetry. 45 This is related to MetHb having a modified light absorption pattern, which interferes with the algorithm used to calculate oxygen saturation. For this reason, most pulse oximeters give a fixed reading of about 85% when significant amounts of MetHb are present, which does not change much with varying levels of methemoglobinemia or hypoxia.
Detection of methemoglobinemia by co‐axial pulse oximetry
Some co‐axial pulse oximeters are able to detect MetHb levels, and these may occasionally detect increased MetHb levels incidentally, although these are not used in routine practice. 46
Severe neurodevelopmental disorder, typically presenting in the first year of life
Typically these children have clinically apparent methemoglobinemia, combined with severe neurological deficits, including profound cognitive impairment, growth retardation, microcephaly and dystonia (methemoglobinemia, type II) (Table 2). 47
(Recommendations) It is particularly important to pay attention to clinical findings and family history to help distinguish acquired from inherited forms (whenever these latter are transmitted).
The experts panel reached 100% (22/22) of consensus on this recommendation (Figure 1).
Q2. What are the key symptoms of methemoglobinemia?
Methemoglobinemia, type I
MetHb levels are typically 20%‐30%. This is a generally rare disorder with frequencies of up to 1:1000 in some isolated populations with founder mutations. The most striking feature is the blue discoloration, which typically may be very intense and give a lavender or slate‐gray appearance. The blue discoloration is apparent all over the body, particularly the lips, nose, cheeks, and buccal mucosa and does not improve with supplemental oxygen. This is present from birth and is persistent without much variation unless it has been treated. Most often, there are no other clinical features and no impairment of cardiorespiratory function. There are some reports of patients with headaches, tachycardia and mild dyspnea, attributed to reduced blood oxygenation, and possibly associated mild polycythemia. 48 Anecdotally, it is reported that fatigue and breathlessness may become more common with increasing age, possibly related to exacerbation of deteriorating cardiovascular function.
Methemoglobinemia, type II
As for type I, MetHb levels are typically 20%‐30%. This is a very rare disorder, but case reports and small case series suggest that the neurological features are fairly homogeneous. Neurological examination is typically normal for the first few months of life, but marked abnormalities emerge by 9 months. Microcephaly is nearly always present. Typical neurological features include axial hypotonia, variable dystonia, choreo‐athetoid movements and opisthotonos. Typically, psychomotor skills do not progress beyond those expected of a one‐year‐old, and patients do not learn to speak or walk. Growth retardation is common, compounded by difficulties feeding and swallowing. Strabismus occurs in more than 80% of patients, with significant numbers also having seizures. Neurological problems are not typically progressive, but life expectancy is reduced, predominantly due to swallowing difficulties and respiratory complications. Death typically occurs in the first decade of life, although some patients survive into adulthood. 49
M‐hemoglobins
Patients have no signs and symptoms other than the discoloration of their skin and mucous membranes. The cyanosis is similar to that in enzymopenic methemoglobinemia, with lavender blue appearance of skin. The main distinguishing feature is that there can be a family history suggesting autosomal dominant inheritance, as illustrated by the recognition of an autosomal dominant condition called “Kochikuro” (black mouth) in Japan since the 1800s, which was subsequently shown to be caused by Hb M‐Iwate. 50 MetHb levels are reported to vary from 12.5%‐25%, with levels possibly higher in β‐globin variants, such as Hb M‐Saskatoon, than α‐globin variants, such as Hb M‐Iwate, although there is considerable overlap.(Recommendations) Key symptoms of methemoglobinemia are related to the MetHb levels. For inherited conditions, these levels range between 10% and 30% that accounts for the occurrence of cyanosis and dark brown blood as main signs. At these levels of MetHb, patients are generally asymptomatic or may present with headaches, tachycardia, and mild dyspnea (see Table 1 ).
The experts panel reached 95.5% (21/22) of consensus on this recommendation (Figure 1).
Q3. What is the diagnostic approach and differential diagnosis of congenital and acquired forms of methemoglobinemia? What are the functional and molecular tests to be performed in cases of new variants where diagnosis is reached through NGS?
Although it is of importance to establish a hereditary cause for methemoglobinemia, the distinction between acquired and inherited causes is not required for treatment of the acute patient and, hence, treatment should be initiated while the cause is being investigated.
The key tests in the differential diagnosis of methemoglobinemia are the measurement of MetHb levels using blood gas measurement by co‐oximetry, the measurement of cytochrome b5 reductase enzymatic activity, and DNA analysis. CYB5R enzymatic activity, previously called methemoglobin reductase or methemoglobin diaphorase, is generally measured using ferricyanide as a substrate and oxidation of NADH at 340 nm according to the following reaction 39 :
Elevated MetHb may also occur in patients with unstable hemoglobins and other hemolytic anemias, such as G6PD deficiency. In these patients, hemolysis is the main sign and symptom and methemoglobinemia may appear after exposure to oxidant drugs. Heinz body formation may be observed at peripheral blood examination. Isopropanol or heat stability testing is usually altered in these cases and may be useful in the differential diagnosis. When suspecting a Hb‐variant, the most efficient approach to the diagnosis is targeted sequencing of the globin genes.
With the advent of NGS technologies the causative genes of hereditary methemoglobinemia are usually included in targeted NGS panels and the identification of pathogenic variants enables either the confirmation or exclusion of inherited and acquired forms or methemoglobinemia. In case new variants are identified in CYB5R3, the enzyme activity assay described above can be used to assess their pathogenicity.
(Recommendations) Cytochrome b5 reductase activity measurement is the gold standard test to discriminate hereditary CYB5R3 deficiency from acquired methemoglobinemia. Molecular testing can be considered the gold standard for the diagnosis of hereditary methemoglobinemia.
The experts panel reached 90.9% (20/22) of consensus on this recommendation (Figure 1).
Q4. What is the clinical management of methemoglobinemia in neonatal/childhood period and the therapeutic approach?
Clinical management of methemoglobinemia in neonatal/childhood period
Management of methemoglobinemia in infancy and childhood is based on several factors including whether the patient is symptomatic, the total amount of methemoglobin, the cause of the methemoglobinemia, and the patient's age. Of note, the cyanosis is determined not by percentage of methemoglobin but the total amount of methemoglobin. MetHb levels > 70% are considered potentially lethal. In acquired methemoglobinemia, treatment is indicated at levels of 20% in symptomatic patients and 30% in asymptomatic patients. Patients who are symptomatic or those with additional factors compromising oxygen delivery such as congenital heart disease, lung disease, significant anemia, or carbon monoxide poisoning should be treated at levels between 10% and 30%. In hereditary methemoglobinemia, higher levels of MetHb are better tolerated, with some patients asymptomatic even up to levels of 30%‐40%.
Infants are at greater risk of developing methemoglobinemia, attributed to lower levels of erythrocyte CYB5R activity estimated to be around 50%‐60% of adult values. In addition, infants have higher levels of HbF which is more readily oxidized to MetHb than adult hemoglobin.
In critically ill hospitalized infants, inhaled nitric oxide therapy for pulmonary hypertension may lead to methemoglobinemia, 51 necessitating regular monitoring. Methemoglobinemia may occur in the first few months of life in infants with marked metabolic acidosis, typically associated with sepsis or diarrhea and dehydration. It is speculated that infants' higher intestinal pH promotes growth of Gram‐negative organisms such as Escherichia coli or Campylobacter jejuni that convert dietary nitrates to nitrites, which in turn induce methemoglobinemia. Infants who ingest well water contaminated with nitrates are also susceptible to methemoglobinemia. 52 So too are infants and young children exposed to local anesthetics such as lidocaine for circumcision, 53 or to benzocaine, an analogue of aniline, in teething gels.
Therapeutic approach
1.6. Treatment of toxic methemoglobinemia
Halt Exposure
The agent precipitating methemoglobinemia should be stopped or removed.
Supportive Therapy
Intravenous hydration and oxygen supplementation should be instituted. If necessary, cardiopulmonary support with mechanical ventilation and pressor support are indicated. 2 For endogenous reducing enzymes to be effective, adequate glucose must be available. Glucose is also needed to form NADPH via the hexose monophosphate shunt, which is necessary for methylene blue (see below) to be effective.
Infants with methemoglobinemia resulting from diarrhea and acidosis may improve with aggressive hydration and bicarbonate to correct the acidosis alone as long as the methemoglobin level is < 20%.
Methylene Blue (Methylthioninium chloride)
Methylene Blue (MB) is the primary treatment for decreasing MetHb levels. It acts by accepting an electron from NADPH, and, in its new form, leukomethylene blue acts to reduce the 3+ ferric state back to the 2+ ferrous state in erythrocytes. The usual starting dose is 1–2 mg/kg (0.2 mL/kg of a 1% solution) infused intravenously over 3 to 5 minu. The dose may be repeated at 1 mg/kg if methemoglobinemia does not significantly decrease within 30–60 min. Methylene blue should reduce MetHb levels significantly in less than an hour. 54 Risk of worsening of methemoglobinemia increases with repeated doses, with toxic levels of MB reached at a total dose > 7 mg/kg. A rebound phenomenon of increased MetHb levels after completion of therapy is attributed to the reversal of the reduction reaction. In cases of worsening methemoglobinemia after MB treatment, urgent exchange transfusion should be performed.
Patients with continued production of MetHb from a long‐acting oxidant stress such as after dapsone ingestion may require repeat dosing every 6–8 h for up to 2–3 days or MB may be given as a continuous IV infusion of 0.10–0.25 mg/kg/hr.
Caution administering MB
Several patient populations are at risk for complications after MB administration. Patients with G6PD deficiency significant hemolytic anemia. Heinz body hemolytic anemia after MB administration. 55 Paradoxically, while MB is an oxidant, its metabolic product leukomethylene blue is a reducing agent. Large doses (4 mg/kg) may result in proportionately higher levels of the oxidizing agent, MB, rather than the reducing agent, leukomethylene blue. 55 Thus, MB may induce hemolysis, and paradoxically, worsen methemoglobinemia in patients with G6PD deficiency. In addition, because G6PD is the first enzyme in the hexose monophosphate shunt, the only source of NADPH in the erythrocyte, patients with G6PD deficiency may not produce sufficient NADPH to reduce MB to leukomethylene blue. Thus MB therapy may be ineffective in the G6PD patient with methemoglobinemia, 55 , 56 and alternate treatments such as ascorbic acid, or in severe cases, exchange transfusion, should be considered. 2 MB should be avoided in patients with G6PD deficiency, and ideally, all patients should be tested for G6PD deficiency before MB. In an emergency, a family history of G6PD deficiency should be sought before MB therapy is instituted.
Methylene blue administration may precipitate serotonin syndrome in individuals receiving selective serotonin reuptake inhibitors and other serotonergic antidepressants. 57 This is attributed to the MB acting as a potent monoamine oxidase inhibitor.
Methylene blue should be used with caution in pregnant women because of concerns about teratogenicity, and possible intestinal atresia. Diagnostic studies utilizing MB in utero via intraamniotic injection and postnatally in doses of 2–4 mg/kg in premature infants has led to hemolysis and methemoglobinemia in non‐G6PD‐deficient infants. 58 , 59
Methylene blue should be used cautiously in patients with renal failure and in anesthetized patients where it may inhibit guanylate cyclase, decreasing nitric oxide‐mediated vasodilatation leading to systemic and pulmonary hypertension.
Ascorbic Acid
Ascorbic acid or Vitamin C is a natural water‐soluble vitamin which reduces excessive oxidative stress. Ascorbic acid can directly reduce MetHb, but the reaction rate is too slow for it to be effective when used alone as it generally requires multiple doses and may take 24 h or longer to lower MetHb levels. 7 , 60 Ascorbic acid is the treatment of choice when MB is not available 61 and in cases of methemoglobinemia and G6PD deficiency. 62 Dosing is not standardized. Doses in adults have ranged from 0.5 g every 12 hr × 16 doses, 1 g every 12 hr × 14 doses, 1.5‐2 g iv × 3–4 infusions, 5 g every 6 hr × 6 doses, or even 10 g × one dose, 63 while doses in children have ranged from 0.5 g every 12 hr × 16 doses and 1 g every 4 hr × 8 doses. 63
N‐acetylcysteine
The role of N‐acetylcysteine in the treatment of methemoglobinemia is unclear. In vitro studies show N‐acetylcysteine can act as a cofactor to enhance reduction and increase intracellular glutathione. It has been suggested for use in patients with methemoglobinemia and G6PD deficiency and acetaminophen induced methemoglobinemia. 62
Other
Case reports have described treatment of refractory methemoglobinemia with blood transfusions, exchange transfusion, 64 , 65 hemodialysis, and hyperbaric oxygen.
1.7. Treatment of inherited methemoglobinemia
In hereditary methemoglobinemia due to CYB5R deficiency, treatment of cyanosis is primarily for cosmetic reasons. However, many patients or parents strongly desire treatment for themselves or their children, respectively. Treatment options, benefits and risks should be discussed accordingly.
Methylene Blue
Methylene blue with or without ascorbic acid is prescribed in more severe cases of congenital methemoglobinemia. 2 , 7 , 66 In some countries, oral MB 100–300 mg per day is administered with dose adjustment according to MetHb levels. Of note, HbMs are not typically responsive to MB. Some unstable Hbs, such Hb Cheverly, Hb Evans, may allow water to enter the homophobic heme pocket during stressor events, thus methemoglobinemia is only intermittent. If significantly elevated, these subgroup of unstable Hbs could respond to MB. 25
Ascorbic Acid
Many patients are adequately treated with ascorbic acid alone, given in varying dosing regimens, from 0.2–1.0 g/day orally in divided doses. 67 Methylene blue and ascorbic acid both effectively facilitate the reduction of MetHb and no trials for comparison are available. The choice of medication and dosing regimen should be tailored to the patient. Chronic administration may lead to formation of sodium oxalate nephrolithiasis. 68
Riboflavin (Vitamin B2)
Riboflavin can accelerate reduction of MetHb levels via the nicotinamide adenine dinucleotide‐flavin reductase system. There are limited data available on the use of riboflavin in hereditary methemoglobinemia. Described cases administer riboflavin at a dose of 20–30 mg/day 69 or 20 mg three times a day. 70
Other considerations
In methemoglobinemia associated with hemoglobin disorders, both HbM and unstable Hb, MB and ascorbic acid treatment are ineffective and should be avoided. 25 , 71 The reducing ability of erythrocytes is normal and iron oxidation is stabilized by globin chains. In patients who have developed polycythemia, phlebotomy is not recommended as higher erythrocyte mass allows provision of normal tissue oxygenation. 72
(Recommendations) Management of methemoglobinemia in infancy and childhood is based on the symptoms shown by the patient, the level of MetHb, the cause of the methemoglobinemia, and the patient's age. There are several therapeutic options, the most used are Methylene Blue and Ascorbic Acid. In patients who have developed polycythemia, phlebotomy is not recommended as higher erythrocyte mass allows provision of normal tissue oxygenation.
The experts panel reached 86.4% (19/22) of consensus on this recommendation (Figure 1).
Q5. What is the clinical management of methemoglobinemia in adulthood and therapeutic approach (daily life, during emergency e.g., surgery, pregnancy)?
Avoiding precipitating factors
Many substances have been reported to precipitate methemoglobinemia, usually precipitating the transformation of Hb to MetHb. The substances to be avoided are listed below including toxins such as nitrates, copper, sulfate, chlorite, chloramines, and chlorates, pesticide, medications like dapsone, 73 , 74 , 75 , 76 local anesthetics: benzocaine 77 prilocaine, lidocaine, tetracaine, cocaine mixed with aniline, 78 sulfonamides, and nitroglycerine.
(Recommendations) Precipitating factors in patients with known hereditary or acquired methemoglobinemia and in patients with a CYB5R3 heterozygous variant should be avoided. It is important to test first degree relatives of patients with hereditary methemoglobinemia.
The experts panel reached 86.4% (19/22) of consensus on this recommendation (Figure 1). The disagreement is related to the inclusion of patients with heterozygous CYB5R3 variants. As a general rule for recessive disorders, we have to consider that genetic testing can fail to identify biallelic variants. Thus, in presence of a clear clinical diagnosis, most of the experts agree to consider monoalleic patients as biallelic ones.
Management of methemoglobinemia in the acute setting
The direct management of methemoglobinemia during an acute episode requires the stratification of the patients according to the symptoms and MetHb level. A good history should be taken to identify the precipitating factor. In case of suspicion of continuous exposure, such as to a pesticide, the medical personnel should wear adequate protective equipment and the patient should be decontaminated. Additionally, it is essential to search for a history of G6PD deficiency. 79 Indeed, methylene blue cannot be used in patients with G6PD as it is ineffective in such patients and it can worsen G6PD deficiency hemolysis. However, there are no sufficient evidence to recommend routine functional assay for G6PD activity. 62
The main morbidity in methemoglobinemia is due to the hypoxic state. Thus, if the patient is asymptomatic, they can be monitored without additional treatment. Oxygen supplementation should be added as needed. If the patient is symptomatic with a high MetHb level, treatment should be initiated. High MetHb level is defined as a level more than 10%‐30%, with >20% as most reported level in the literature. 77 The first‐line treatment of MetHb is intravenous (IV) methylene blue (MB) which acts as a cofactor to reduce the MetHb to oxyhemoglobin in the erythrocytes. 80 The first dose of MB varies from 0.3 mg/kg up to 5.5 mg/kg 2 infused over 3 to 5 min, 81 commonly between 1 and 2 mg/kg. 2 , 82 The dose can be repeated 81 if symptoms do not resolve within 30 min. The expected time by which the MetHb level should normalize is 1 h after the administration of iv MB. 2 Many reports suggest the addition of ascorbic acid to MB. Ascorbic acid can be given orally, intramuscularly or IV. 83 If there is no improvement with the use of repeated dose of MB, therapeutic whole blood exchange (TWBE) or hyperbaric oxygen therapy should be considered. 84 , 85 , 86 , 87 , 88 In a systematic review, TWBE lead to a survival rate of 81.6% in patients refractory to MB. 89 , 90
(Recommendations) In minimally symptomatic or asymptomatic patients, we recommend monitoring without further treatment or addition of oxygen supplementation if needed. In case oxygen is started, monitoring of oxygen saturation with pulse oximetry is usually routinely necessary, at least in neonates. All symptomatic patients should have venous blood MetHb level tested and those without known history of methemoglobinemia should be tested for G6PD deficiency. The first line treatment of the symptomatic patient is MB with a starting dose of 1–2 mg/kg of 1% MB to be repeated up to a dose of 5.5 mg/kg if no response after 30 min. Ascorbic acid can be added as an adjunctive therapy. Patients who do not respond to first line therapy should undergo exchange transfusion or hyperbaric oxygen therapy.
The experts panel reached 95.5% (21/22) of consensus on this recommendation (Figure 1).
Management of methemoglobinemia in special situations
1.8. Pregnancy
Methemoglobinemia attack during pregnancy can lead to significant morbidity to the fetus due to hypoxia. Pregnancy is a physiologic state during which there is increased oxygen demand that increases as the pregnancy advances. 91 In fact, this physiologic state might be the insulting event and might precipitate symptomatic methemoglobinemia in pregnant women. 92 It is well known that MB is teratogenic. 93 Among teratogenic effects jejunal/ileal atresia is the most reported. Additionally, it has been reported to lead to fetal demise. Other adverse effects on the newborn are hyperbilirubinemia, hemolytic anemia, Heinz‐body formation, birthmarks, methemoglobinemia, respiratory distress, skin photo‐sensitization desquamation. Moreover, oxygen is essential to the fetus during organogenesis. Hypoxia exacerbated by methemoglobinemia may cause intrauterine growth restriction, prematurity, morphological and functional cardiac changes through cardiac tissue damage. 94
MB should only be used in pregnancy when the risks are felt to outweigh the benefits. Exchange red cell transfusion may be an effective alternative, if there is time for this to be arranged and appropriate matched blood is available.
(Recommendations) If MB is to be given to a pregnant patient, the decision should be multidisciplinary and discussed with the patient weighing the risk of hypoxia on the baby and the teratogenic and other effects of MB.
The experts panel reached 95.5% (21/22) of consensus on this recommendation (Figure 1).
1.9. Surgery
Surgery carries a particular risk for patients with known methemoglobinemia particularly because of the well‐established risk of precipitation of the disease after exposure to anesthetics. Preoperative evaluation of patients with known methemoglobinemia is essential to allow identification of previous acute episodes, and other comorbidities that may exacerbate hypoxia like cardiac, pulmonary and vessel diseases. 95 Blood and fresh frozen plasma should be prepared (in centers where such products are not readily available) in case TWBE is needed. The use of prophylactic MB prior to surgery is controversial. Some studies report the successful use of prophylactic MB. 95 However, there is not enough data to support its prophylactic use. Additionally, MB is not a drug without toxicity. It can cause among others local tissue necrosis, anemia which further exacerbate hypoxia, and excessive doses can lead to hemolysis which is more common in the pediatric population. 96 , 97 Furthermore, several reported cases show successful treatment of patients who develop methemoglobinemia during surgery through proper identification of patients and monitoring. 95 , 98 In major surgery, where there is likely to be prolonged anesthesia or inevitable exposure to drugs likely to worsen methemoglobinemia, preoperative exchange transfusion may be appropriate to reduce the operative risks.
(Recommendations) Potential precipitating and exacerbating factors should be identified prior to surgery. Prophylactic use of MD is recommended only in selected cases of high‐risk patients, like high pre‐surgery MetHb levels or medical history of severe episodes.
MB should be prepared and available in the operation room. All patients should receive supplemental oxygen prior to anesthetic administration. Electrocardiogram monitoring to detect myocardial ischemia and co‐oximeters to identify the MetHb level can be used. Any metabolic abnormality should be corrected prior to administration of anesthetics. The patient should be monitored during and after surgery for any signs and symptoms of hypoxia.
The experts panel reached 77.3% (17/22) of consensus on this recommendation (Figure 1).
Q6. What useful information should be given to patients affected by hereditary methemoglobinemia (main information about their condition, skin color, lifestyle, drug/food to be avoided) and their health care providers?
Signs and symptoms of methemoglobinemia are generally proportional to the MetHb level in peripheral blood, and quite different in congenital versus acquired/acute methemoglobinemia: in the former patients are often asymptomatic despite the presence of a gray cyanosis, while in the latter the neurologic and cardiac symptoms often have an abrupt onset, frequently associated with a history of exposure to methemoglobinemia‐inducing substances.
(Recommendation) Early clinical recognition of methemoglobinemia is of paramount importance. Patients and clinicians should be aware of neurologic and cardiac symptoms and their progression with increasing MetHb values. Prompt referral to specialized laboratories in case of mild symptoms or directly to Emergency Units in case of more severe symptoms is fundamental to establish MetHb levels and to start treatment.
The experts panel reached 90.9% (20/22) of consensus on this recommendation (Figure 1).
Several drugs, foods and drinks, and various clinical conditions (particularly infections) may increase the levels of MetHb. Among drugs, it is worth remembering phenacetin, phenazopyridine, dapsone, chloroquine, primaquine, trimethoprim, sulfonamides, rasburicase, cyclophosphamide, flutamide, and metoclopramide may increase MetHb. Benzocaine, lidocaine, prilocaine, and articaine have been reported as possible causes of increased MetHb. In addition, nitrate derivatives such nitroglycerin, nitroprusside, amyl nitrite, nitric oxide, and nitrates salt have been associated with methemoglobinemia. Several industrial products (aniline dyes, naphthalene, aminophenols, chlorates, bromates, herbicides, and pesticides) may also cause methemoglobinemia. Patients, particularly infants and pregnant women should avoid consumption of well water or food from areas grown where ground water is contaminated by excessive nitrates from fertilizers or inappropriate manure utilization.
(Recommendation) It is recommended to avoid drugs, and chemical substances (possibly present in food, drinks and well water), as well as to promptly treat associated conditions (particularly infections) that may increase methemoglobin levels. A medical alert system is recommended to patients with inherited methemoglobinemia.
The experts panel reached 100% (22/22) of consensus on this recommendation (Figure 1).
Patients with hereditary/congenital methemoglobinemia often ask for “what should be done” for their children and partners. Maybe we can advise for testing them for MetHb and perform molecular analysis in case of elevated levels (> 10%). If there is a molecular diagnosis in the family, molecular testing should be offered to first line family members where possible.
CONFLICT OF INTEREST
The authors have declared that no conflict of interest exists.
AUTHOR CONTRIBUTIONS
Collected the literature data and wrote the paper: Achille Iolascon, Paola Bianchi, Immacolata Andolfo, Roberta Russo, Wilma Barcellini, Elisa Fermo, Gergely Toldi, Stefano Ghirardello, Davis Rees, Richard Van Wijk, Antonis Kattamis, Patrick G. Gallagher, Noemi Roy, Ali Taher and Razan Mohty. Critically reviewed the manuscript: Andreas Kulozik, Lucia De Franceschi, Antonella Gambale, Mariane De Montalembert, Gian Luca Forni, Cornelis L. Harteveld and Josef Prchal.
ACKNOWLEDGMENTS
This work was generated within the scientific working group (SWG) of red cell and iron of European Hematology Association (EHA) and of the European Reference Network on Rare Hematological Diseases (ERN‐EuroBloodNet) FPA 739541. Open Access Funding provided by Universita degli Studi di Napoli Federico II within the CRUI‐CARE Agreement.
Iolascon A, Bianchi P, Andolfo I, et al. Recommendations for diagnosis and treatment of methemoglobinemia. Am J Hematol. 2021;96(12):1666‐1678. doi: 10.1002/ajh.26340
Funding information Funding Statement: Open Access Funding provided by Universita degli Studi di Napoli Federico II within the CRUI‐CARE Agreement. WOA Institution: Universita degli Studi di Napoli Federico II Blended DEAL: CARE; Funding for Open Access was approved for this article. If included below, please make sure the Funding Statement is added to the content:; Funding Statement: Open Access Funding provided by Universita degli Studi di Napoli Federico II within the CRUI‐CARE Agreement.; WOA Institution: Universita degli Studi di Napoli Federico II Blended DEAL: CARE
DATA AVAILABILITY STATEMENT
Data sharing not applicable ‐ no new data generated.
REFERENCES
- 1. Prchal J. Chapter 51: Methemoglobinemia and Other Dyshemoglobinemias. 10th ed. McGraw Hill; 2021. [Google Scholar]
- 2. Wright RO, Lewander WJ, Woolf AD. Methemoglobinemia: etiology, pharmacology, and clinical management. Ann Emerg Med. 1999;34(5):646‐656. [DOI] [PubMed] [Google Scholar]
- 3. Ludlow JT, Wilkerson RG, Nappe TM. Methemoglobinemia. StatPearls Publishing; 2021. [PubMed] [Google Scholar]
- 4. Curry S. Methemoglobinemia. Ann Emerg Med. 1982;11(4):214‐221. [DOI] [PubMed] [Google Scholar]
- 5. van Zwieten R, Verhoeven AJ, Roos D. Inborn defects in the antioxidant systems of human red blood cells. Free Radic Biol Med. 2014;67:377‐386. [DOI] [PubMed] [Google Scholar]
- 6. Skold A, Cosco DL, Klein R. Methemoglobinemia: pathogenesis, diagnosis, and management. South Med J. 2011;104(11):757‐761. [DOI] [PubMed] [Google Scholar]
- 7. Percy MJ, Lappin TR. Recessive congenital methaemoglobinaemia: cytochrome b(5) reductase deficiency. Br J Haematol. 2008;141(3):298‐308. [DOI] [PubMed] [Google Scholar]
- 8. Dekker J, Eppink MH, van Zwieten R, et al. Seven new mutations in the nicotinamide adenine dinucleotide reduced‐cytochrome b(5) reductase gene leading to methemoglobinemia type I. Blood. 2001;97(4):1106‐1114. [DOI] [PubMed] [Google Scholar]
- 9. Nicolas‐Jilwan M. Recessive congenital methemoglobinemia type II: hypoplastic basal ganglia in two siblings with a novel mutation of the cytochrome b5 reductase gene. Neuroradiol J. 2019;32(2):143‐147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fermo E, Bianchi P, Vercellati C, et al. Recessive hereditary methemoglobinemia: two novel mutations in the NADH‐cytochrome b5 reductase gene. Blood Cells Mol Dis. 2008;41(1):50‐55. [DOI] [PubMed] [Google Scholar]
- 11. Gupta V, Kulkarni A, Warang P, Devendra R, Chiddarwar A, Kedar P. Mutation update: variants of the CYB5R3 gene in recessive congenital methemoglobinemia. Hum Mutat. 2020;41(4):737‐748. [DOI] [PubMed] [Google Scholar]
- 12. Balsamo P, Hardy WR, Scott EM. Hereditary methemoglobinemia due to diaphorase deficiency in navajo Indians. J Pediatr. 1964;65:928‐931. [DOI] [PubMed] [Google Scholar]
- 13. Gordeuk VR, Shah BN, Zhang X, et al. The CYB5R3(c) (.350C>G) and G6PD a alleles modify severity of anemia in malaria and sickle cell disease. Am J Hematol. 2020;95(11):1269‐1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hegesh E, Hegesh J, Kaftory A. Congenital methemoglobinemia with a deficiency of cytochrome b5. N Engl J Med. 1986;314(12):757‐761. [DOI] [PubMed] [Google Scholar]
- 15. Kok RC, Timmerman MA, Wolffenbuttel KP, Drop SL, de Jong FH. Isolated 17,20‐lyase deficiency due to the cytochrome b5 mutation W27X. J Clin Endocrinol Metab. 2010;95(3):994‐999. [DOI] [PubMed] [Google Scholar]
- 16. Idkowiak J, Randell T, Dhir V, et al. A missense mutation in the human cytochrome b5 gene causes 46,XY disorder of sex development due to true isolated 17,20 lyase deficiency. J Clin Endocrinol Metab. 2012;97(3):E465‐E475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lehmann H. Man's Haemoglobins: Including the Haemoglobinopathies and their Investigation. Lippincott; 1975. [Google Scholar]
- 18. Kulozik AE. Hemoglobin variants and the rarer hemoglobin disorders. Pediatric Hematology; Wiley; 2006:231‐254. [Google Scholar]
- 19. Hayashi A, Fujita T, Fujimura M, Titani K. A new abnormal fetal hemoglobin, Hb FM‐Osaka (alpha 2 gamma 2 63His replaced by Tyr). Hemoglobin. 1980;4(3–4):447‐448. [DOI] [PubMed] [Google Scholar]
- 20. Priest JR, Watterson J, Jones RT, Faassen AE, Hedlund BE. Mutant fetal hemoglobin causing cyanosis in a newborn. Pediatrics. 1989;83(5):734‐736. [PubMed] [Google Scholar]
- 21. Wild B, Bain BJ. Investigation of abnormal haemoglobins and thalassaemia. Dacie and Lewis Practical Haematology. 10th ed. Churchill Livingstone; 2006:271‐310. [Google Scholar]
- 22. Agarwal AM, Prchal JT. Methemoglobinemia and other dyshemoglobinemias. In: Kaushansky K, Lichtman MA, Prchal JT, et al., eds. Williams Hematology, 9e; McGraw‐Hill; 2015. [Google Scholar]
- 23. Stamatoyannopoulos G, Nute PE, Giblett E, Detter J, Chard R. Haemoglobin M Hyde Park occurring as a fresh mutation: diagnostic, structural, and genetic considerations. J Med Genet. 1976;13(2):142‐147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hojas‐Bernal R, McNab‐Martin P, Fairbanks VF, et al. Hb Chile [beta28(B10)Leu‐>met]: an unstable hemoglobin associated with chronic methemoglobinemia and sulfonamide or methylene blue‐induced hemolytic anemia. Hemoglobin. 1999;23(2):125‐134. [DOI] [PubMed] [Google Scholar]
- 25. Rangan A, Savedra ME, Dergam‐Larson C, et al. Interpreting sulfhemoglobin and methemoglobin in patients with cyanosis: an overview of patients with M‐hemoglobin variants. Int J Lab Hematol. 2021;43:837‐844. [DOI] [PubMed] [Google Scholar]
- 26. McGuigan MA. Benzocaine‐induced methemoglobinemia. Can Med Assoc J. 1981;125(8):816. [PMC free article] [PubMed] [Google Scholar]
- 27. O'Donohue WJ Jr, Moss LM, Angelillo VA. Acute methemoglobinemia induced by topical benzocaine and lidocaine. Arch Intern Med. 1980;140(11):1508‐1509. [PubMed] [Google Scholar]
- 28. Kane GC, Hoehn SM, Behrenbeck TR, Mulvagh SL. Benzocaine‐induced methemoglobinemia based on the Mayo Clinic experience from 28 478 transesophageal echocardiograms: incidence, outcomes, and predisposing factors. Arch Intern Med. 2007;167(18):1977‐1982. [DOI] [PubMed] [Google Scholar]
- 29. Johnson CJ, Kross BC. Continuing importance of nitrate contamination of groundwater and wells in rural areas. Am J Ind Med. 1990;18(4):449‐456. [DOI] [PubMed] [Google Scholar]
- 30. Lo SC, Agar NS. NADH‐methemoglobin reductase activity in the erythrocytes of newborn and adult mammals. Experientia. 1986;42(11–12):1264‐1265. [DOI] [PubMed] [Google Scholar]
- 31. Graubarth J, Bloom CJ, Coleman FC, Solomon HN. Dye poisoning in the nursery: a review of seventeen cases. JAMA. 1945;128(16):1155‐1157. [Google Scholar]
- 32. Knobeloch L, Proctor M. Eight blue babies. WMJ. 2001;100(8):43‐47. [PubMed] [Google Scholar]
- 33. Lukens JN. Landmark perspective: the legacy of well‐water methemoglobinemia. Jama. 1987;257(20):2793‐2795. [PubMed] [Google Scholar]
- 34. Sanchez‐Echaniz J, Benito‐Fernandez J, Mintegui‐Raso S. Methemoglobinemia and consumption of vegetables in infants. Pediatrics. 2001;107(5):1024‐1028. [DOI] [PubMed] [Google Scholar]
- 35. Hamon I, Gauthier‐Moulinier H, Grelet‐Dessioux E, Storme L, Fresson J, Hascoet JM. Methaemoglobinaemia risk factors with inhaled nitric oxide therapy in newborn infants. Acta Paediatr. 2010;99(10):1467‐1473. [DOI] [PubMed] [Google Scholar]
- 36. Hunter L, Gordge L, Dargan PI, Wood DM. Methaemoglobinaemia associated with the use of cocaine and volatile nitrites as recreational drugs: a review. Br J Clin Pharmacol. 2011;72(1):18‐26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Evelyn KE, Malloy HT. Microdetermination of oxyhemoglobin, methemoglobin, and sulfhemoglobin in a single sample of blood. J Biol Chem. 1938;126(2):655‐662. [Google Scholar]
- 38. Beutler E. Carboxyhemoglobin, methemoglobin, and sulfhemoglobin determinations. In: Beutler E, Lichtman MA, Coller BS, Kipps TJ, eds. Williams Hematology. McGraw‐Hill; 1995. [Google Scholar]
- 39. Beutler E. Red Cell Metabolism: A Manual of Biochemical Methods. Grune & Stratton; 1984. [Google Scholar]
- 40. Bianchi P, Vercellati C, Fermo E. How will next generation sequencing (NGS) improve the diagnosis of congenital hemolytic anemia? Ann Transl Med. 2020;8(6):268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Russo R, Marra R, Rosato BE, Iolascon A, Andolfo I. Genetics and genomics approaches for diagnosis and research into hereditary anemias. Front Physiol. 2020;11:613559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Matar CF, Bou‐Fakhredin R, Russo R, Andolfo I, Iolascon A, Taher AT. Recommendations for pregnancy in Fanconi anemia. Expert Opin Biol Ther. 2021. 10.1080/14712598.2021.1913119. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 43. Cawein M, Behlen CH 2nd, Lappat EJ, Cohn JE. Hereditary diaphorase deficiency and methemoglobinemia. Arch Intern Med. 1964;113:578‐585. [DOI] [PubMed] [Google Scholar]
- 44. Ward J, Motwani J, Baker N, Nash M, Ewer AK, Toldi G. Congenital Methemoglobinemia identified by pulse oximetry screening. Pediatrics. 2019;143(3):e20182814. [DOI] [PubMed] [Google Scholar]
- 45. Barker SJ, Tremper KK, Hyatt J. Effects of methemoglobinemia on pulse oximetry and mixed venous oximetry. Anesthesiology. 1989;70(1):112‐117. [DOI] [PubMed] [Google Scholar]
- 46. Feiner JR, Bickler PE, Mannheimer PD. Accuracy of methemoglobin detection by pulse CO‐oximetry during hypoxia. Anesth Analg. 2010;111(1):143‐148. [DOI] [PubMed] [Google Scholar]
- 47. Worster‐Drought C, White JC, Sargent F. Familial idiopathic methaemoglobinaemia, associated with mental deficiency and neurological abnormalities. Br Med J. 1953;2(4828):114‐118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Jaffe ER. Hereditary methemoglobinemias associated with abnormalities in the metabolism of erythrocytes. Am J Med. 1966;41(5):786‐798. [DOI] [PubMed] [Google Scholar]
- 49. Ewenczyk C, Leroux A, Roubergue A, et al. Recessive hereditary methaemoglobinaemia, type II: delineation of the clinical spectrum. Brain. 2008;131(Pt 3):760‐761. [DOI] [PubMed] [Google Scholar]
- 50. Shibata S, Miyaji T, Iuchi I, Tamura A. Substitution of tyrosine for histidine (87 in the alpha‐chain of hemoglobin M‐Iwate). Nihon Ketsueki Gakkai Zasshi. 1964;27:13‐18. [PubMed] [Google Scholar]
- 51. Centorrino R, Shankar‐Aguilera S, Foligno S, De Luca D. Life‐threatening extreme Methemoglobinemia during standard dose nitric oxide therapy. Neonatology. 2019;116(3):295‐298. [DOI] [PubMed] [Google Scholar]
- 52. Greer FR, Shannon M, American Academy of Pediatrics Committee on Nutrition; American Academy of Pediatrics Committee on Environmental Health . Infant methemoglobinemia: the role of dietary nitrate in food and water. Pediatrics. 2005;116(3):784‐786. [DOI] [PubMed] [Google Scholar]
- 53. Boran P, Tokuc G, Yegin Z. Methemoglobinemia due to application of prilocaine during circumcision and the effect of ascorbic acid. J Pediatr Urol. 2008;4(6):475‐476. [DOI] [PubMed] [Google Scholar]
- 54. Finch CA. Treatment of intracellular methemoglobinemia. Bull New Engl Med Cent. 1947;9(6):241‐245. [PubMed] [Google Scholar]
- 55. Harvey JW, Keitt AS. Studies of the efficacy and potential hazards of methylene blue therapy in aniline‐induced methaemoglobinaemia. Br J Haematol. 1983;54(1):29‐41. [DOI] [PubMed] [Google Scholar]
- 56. Rosen PJ, Johnson C, McGehee WG, Beutler E. Failure of methylene blue treatment in toxic methemoglobinemia. Association with glucose‐6‐phosphate dehydrogenase deficiency. Ann Intern Med. 1971;75(1):83‐86. [DOI] [PubMed] [Google Scholar]
- 57. Zuschlag ZD, Warren MW, Schultz SK. Serotonin toxicity and urinary analgesics: a case report and systematic literature review of methylene blue‐induced serotonin syndrome. Psychosomatics. 2018;59(6):539‐546. [DOI] [PubMed] [Google Scholar]
- 58. McEnerney JK, McEnerney LN. Unfavorable neonatal outcome after intraamniotic injection of methylene blue. Obstet Gynecol. 1983;61(3 Suppl):35S‐37S. [PubMed] [Google Scholar]
- 59. Allegaert K, Miserez M, Lerut T, Naulaers G, Vanhole C, Devlieger H. Methemoglobinemia and hemolysis after enteral administration of methylene blue in a preterm infant: relevance for pediatric surgeons. J Pediatr Surg. 2004;39(1):E35‐E37. [DOI] [PubMed] [Google Scholar]
- 60. Breakey VK, Gibson QH. Familial idiopathic methaemoglobinaemia. Lancet. 1951;1(6661):935‐938. [DOI] [PubMed] [Google Scholar]
- 61. Rino PB, Scolnik D, Fustinana A, Mitelpunkt A, Glatstein M. Ascorbic acid for the treatment of methemoglobinemia: the experience of a large tertiary care pediatric hospital. Am J Ther. 2014;21(4):240‐243. [DOI] [PubMed] [Google Scholar]
- 62. Rehman A, Shehadeh M, Khirfan D, Jones A. Severe acute haemolytic anaemia associated with severe methaemoglobinaemia in a G6PD‐deficient man. BMJ Case Rep. 2018;2018:223369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Sahu KK, Dhibar DP, Gautam A, Kumar Y, Varma SC. Role of ascorbic acid in the treatment of methemoglobinemia. Turk J Emerg Med. 2016;16(3):119‐120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Patnaik S, Natarajan MM, James EJ, Ebenezer K. Methylene blue unresponsive methemoglobinemia. Indian J Crit Care Med. 2014;18(4):253‐255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Golden PJ, Weinstein R. Treatment of high‐risk, refractory acquired methemoglobinemia with automated red blood cell exchange. J Clin Apher. 1998;13(1):28‐31. [DOI] [PubMed] [Google Scholar]
- 66. Zorc JJ, Kanic Z. A cyanotic infant: true blue or otherwise? Pediatr Ann. 2001;30(10):597‐601. [DOI] [PubMed] [Google Scholar]
- 67. Deeny J, Murdock ET, Rogan JJ. Familial idiopathic methaemoglobinaemia: treatment with ascorbic acid. Br Med J. 1943;1(4301):721‐723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Crivelli JJ, Mitchell T, Knight J, et al. Contribution of dietary oxalate and oxalate precursors to urinary oxalate excretion. Nutrients. 2020;13(1). 10.3390/nu13010062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Kaplan JC, Chirouze M. Therapy of recessive congenital methaemoglobinaemia by oral riboflavine. Lancet. 1978;2(8098):1043‐1044. [DOI] [PubMed] [Google Scholar]
- 70. Hirano M, Matsuki T, Tanishima K, et al. Congenital methaemoglobinaemia due to NADH methaemoglobin reductase deficiency: successful treatment with oral riboflavin. Br J Haematol. 1981;47(3):353‐359. [DOI] [PubMed] [Google Scholar]
- 71. Vichinsky EP, Lubin BH. Unstable hemoglobins, hemoglobins with altered oxygen affinity, and m‐hemoglobins. Pediatr Clin North Am. 1980;27(2):421‐428. [DOI] [PubMed] [Google Scholar]
- 72. Cohen RJ, Sachs JR, Wicker DJ, Conrad ME. Methemoglobinemia provoked by malarial chemoprophylaxis in Vietnam. N Engl J Med. 1968;279(21):1127‐1131. [DOI] [PubMed] [Google Scholar]
- 73. Salamat A, Watson HG. Drug‐induced methaemoglobinaemia presenting with angina following the use of dapsone. Clin Lab Haematol. 2003;25(5):327‐328. [DOI] [PubMed] [Google Scholar]
- 74. Walker JG, Kadia T, Brown L, Juneja HS, de Groot JF. Dapsone induced methemoglobinemia in a patient with glioblastoma. J Neurooncol. 2009;94(1):149‐152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Ward KE, McCarthy MW. Dapsone‐induced methemoglobinemia. Ann Pharmacother. 1998;32(5):549‐553. [DOI] [PubMed] [Google Scholar]
- 76. Williams S, MacDonald P, Hoyer JD, Barr RD, Athale UH. Methemoglobinemia in children with acute lymphoblastic leukemia (ALL) receiving dapsone for pneumocystis carinii pneumonia (PCP) prophylaxis: a correlation with cytochrome b5 reductase (Cb5R) enzyme levels. Pediatr Blood Cancer. 2005;44(1):55‐62. [DOI] [PubMed] [Google Scholar]
- 77. Cortazzo JA, Lichtman AD. Methemoglobinemia: a review and recommendations for management. J Cardiothorac Vasc Anesth. 2014;28(4):1043‐1047. [DOI] [PubMed] [Google Scholar]
- 78. Guay J. Methemoglobinemia related to local anesthetics: a summary of 242 episodes. Anesth Analg. 2009;108(3):837‐845. [DOI] [PubMed] [Google Scholar]
- 79. Pomoni A, Aggeli I, Loutsi E, Hatzimichael E, Chaliasos N, Makis A. Cyanosis due to Methemoglobinemia as the presenting sign of Glucose‐6‐phosphate dehydrogenase deficiency in a child: diagnostic and clinical implications. J Pediatr Hematol Oncol. 2020. 10.1097/MPH.0000000000001967. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 80. Steele CW, Spink WW. Methylene blue in the treatment of poisonings associated with methemoglobinemia. N Engl J Med. 1933;208:1152‐1153. [Google Scholar]
- 81. Goluboff N. Methemoglobinemia due to benzocaine. Pediatrics. 1958;21(2):340‐341. [Google Scholar]
- 82. Ginimuge PR, Jyothi SD. Methylene blue: revisited. J Anaesthesiol Clin Pharmacol. 2010;26(4):517‐520. [PMC free article] [PubMed] [Google Scholar]
- 83. de Geus KF, Anas AA, Franssen R, Duijkers FAM, Bikker H, Linthorst GE. Congenital methaemoglobinaemia in a 61‐year‐old patient with normal haemoglobin levels. Neth J Med. 2018;76(4):194‐197. [PubMed] [Google Scholar]
- 84. Altintop I, Sanri E, Tatli M, Akcin ME, Denizbasi A. Methemoglobinemia treated with hyperbaric oxygen therapy: a case report. Turk J Emerg Med. 2018;18(4):176‐178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Cho Y, Park SW, Han SK, Kim HB, Yeom SR. A case of methemoglobinemia successfully treated with hyperbaric oxygenation monotherapy. J Emerg Med. 2017;53(5):685‐687. [DOI] [PubMed] [Google Scholar]
- 86. Lindenmann J, Fink‐Neuboeck N, Schilcher G, Smolle‐Juettner FM. Severe methaemoglobinaemia treated with adjunctive hyperbaric oxygenation. Diving Hyperb Med. 2015;45(2):132‐134. [PubMed] [Google Scholar]
- 87. Lindenmann J, Matzi V, Kaufmann P, et al. Hyperbaric oxygenation in the treatment of life‐threatening isobutyl nitrite‐induced methemoglobinemia‐a case report. Inhal Toxicol. 2006;18(13):1047‐1049. [DOI] [PubMed] [Google Scholar]
- 88. Goldstein GM, Doull J. Treatment of nitrite‐induced methemoglobinemia with hyperbaric oxygen. Proc Soc Exp Biol Med. 1971;138(1):137‐139. [DOI] [PubMed] [Google Scholar]
- 89. Singh P, Rakesh K, Agarwal R, et al. Therapeutic whole blood exchange in the management of methaemoglobinemia: case series and systematic review of literature. Transfus Med. 2020;30(3):231‐239. [DOI] [PubMed] [Google Scholar]
- 90. Bhasker B, Ramakrishna AA. Therapeutic whole blood exchange using plasma exchange kit on a cell separator in a patient with refractory methemoglobinemia. Transfus Apher Sci. 2020;59(6):102910. [DOI] [PubMed] [Google Scholar]
- 91. LoMauro A, Aliverti A. Respiratory physiology of pregnancy: physiology masterclass. Breathe (Sheff). 2015;11(4):297‐301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Grauman Neander N, Loner CA, Rotoli JM. The acute treatment of Methemoglobinemia in pregnancy. J Emerg Med. 2018;54(5):685‐689. [DOI] [PubMed] [Google Scholar]
- 93. Cragan JD. Teratogen update: methylene blue. Teratology. 1999;60(1):42‐48. [DOI] [PubMed] [Google Scholar]
- 94. Hutter D, Kingdom J, Jaeggi E. Causes and mechanisms of intrauterine hypoxia and its impact on the fetal cardiovascular system: a review. Int J Pediatr. 2010;2010:401323‐401329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Kus A, Berk D, Hosten T, Gurkan Y, Solak M, Toker K. The role of preoperative evaluation for congenital methemoglobinemia. Turk J Anaesthesiol Reanim. 2014;42(4):223‐226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Garza F, Kearney TE. Chapter 205. Methylene blue. In: Olson KR, ed. Poisoning and Drug Overdose, 6e. The McGraw‐Hill Companies; 2012. [Google Scholar]
- 97. Umbreit J. Methemoglobin‐it's not just blue: a concise review. Am J Hematol. 2007;82(2):134‐144. [DOI] [PubMed] [Google Scholar]
- 98. Konig MW, Dolinski SY. A 74‐year‐old woman with desaturation following surgery. Co‐oximetry is the first step in making the diagnosis of dyshemoglobinemia. Chest. 2003;123(2):613‐616. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable ‐ no new data generated.


