Abstract
Objective
The purpose of this study was to assess the wear experience of silicone hydrogel daily disposable contact lenses with water surface technology over a long day of lens wear.
Methods
Thirty-five soft contact lens wearers were refit with the daily disposable study lenses and participants scored their initial impressions of comfort, vision and satisfaction using a visual analog scale (VAS). Participants used their smart phones to complete surveys of comfort and vision on a scale of 1–10 at 10, 12, 14, and 16 hours of lens wear on 5 weeknights. A participant score for each time point was calculated by averaging the evening responses. End of study VAS surveys of symptoms were also completed.
Results
Median (Interquartile Range) VAS initial impression scores were 99.00 (12.00) for quality of vision, 98.00 (16.00) for comfort, and 100.00 (13.00) for satisfaction. The end of study surveys found end of day median VAS scores of 87.00 (19.00) for end of day quality of vision and 75.00 (24.50) for end of day comfort. The median score for overall quality of vision was 93.00 (14.00) and for overall comfort was 93.00 (16.50). The median score for end of day dryness was 37.00 (55.00) and overall dryness was 13.00 (34.00).
Conclusion
The daily disposable lenses with water surface treatment used in this study maintained high median scores for comfort and quality of vision for up to 16 hours of wear.
Keywords: daily disposable contact lenses, water surface contact lenses, comfort, end of day comfort, long wear time
Background
Soft contact lenses are used by an estimated 40.9 million adults in the United States.1 While contact lenses are medical devices, soft lenses which are worn for daily wear and no extended wear, are considered a moderate risk device, with risks to wearers are minimized by proper lens care and hygiene. Because daily disposable contact lenses are replaced each day, less tear protein and debris collects upon the lens surface than occurs than with reusable lenses. As a result, wearing these lenses decreases the risk of triggering giant papillary conjunctivitis (GPC) and/or ocular allergic responses in patients.2 Additionally, daily disposable contact lenses do not require the use of disinfecting solution and overnight storage of lenses, which are associated with a greater risk of corneal infiltrative events.3 The ease of use and convenience of not needing to clean lenses may have an effect on contact lens hygiene compliance. In a 2019 study examining compliance of soft contact lens wearers, Rueff et al found that individuals wearing daily disposable lenses were more likely to be compliant with their lens replacement schedule compared to individuals wearing two-week or monthly replacement lenses.4 A large multicenter study found that wearing daily disposable contact lenses was protective against corneal infiltrative events (CIEs) and proposed that poor hygiene with lens care products and lens storage cases with planned replacement lens wearers was a key difference when comparing adverse events with the two types of soft lenses.5 Additional benefits are reflected in a study which found less superficial punctate staining and symptoms of dryness when comparing daily disposable contact lens wear with planned replacement lens wear.6
Previous studies have found that satisfaction with soft contact lens wear is influenced by both vision and comfort.7 Comfort is known to decrease over the course of a day for many soft contact lens wearers, and this end-of-day discomfort is usually associated with symptoms of dryness.8 Since discomfort has been found to play a large role in discontinuation of soft contact lens wear,9,10 finding innovative ways to improve lens comfort is important. Symptoms of dryness are commonly associated with contact lens discomfort.8 A large review of soft contact lens properties found that factors such as frequency of lens replacement, lens edge profile, osmolarity, and lens movement can play a role in comfort.11 Additionally, bulk properties of lens materials and surface modifications can be made to soft lenses in order to lower the coefficient of friction or increase the surface lubricity.12 Because soft lenses have different designs and material properties, it is difficult to differentiate which properties affect comfort independently. As a result, it is necessary to investigate individual soft contact lens designs to assess the impact of replacement schedule, edge and fit properties, and lens and surface treatments to determine their impact on vision and comfort collectively. Previous lenses with water surface treatment have shown high levels of comfort with lens wear.13,14 The lenses investigated in this study utilize a water surface technology that provides greater than 80% water content at the lens surface, which increases lubricity and wettability of the lens at the surface, while a silicone hydrogel core provides high oxygen transmissibility.15 The purpose of this study was to fit existing soft contact lens wearers with a daily disposable water surface lens and assess their wear experience over 16 hours of lens wear. Key endpoints for the study were subjective assessment of comfort and vision at 10, 12, 14 and 16 hours of contact lens wear and subjective responses to a Visual Analog Scale (VAS) survey of lens wear symptoms (comfort, dryness, vision) at the end of the study.
Methods
This prospective, open-label study was approved by the Institutional Review Board at The Ohio State University and is registered on ClinicalTrials.gov (#NCT04535310). This study complied with the Declaration of Helsinki and all participants completed electronic written informed consent prior to screening.
Subjective data was collected from participants throughout the study using REDCap (Research Electronic Data Capture), a secure, web-based software platform hosted by The Ohio State University which was designed to support data capture for research studies.16,17 Participants completed all surveys and assessments utilizing their personal smart device to access the REDCap surveys.
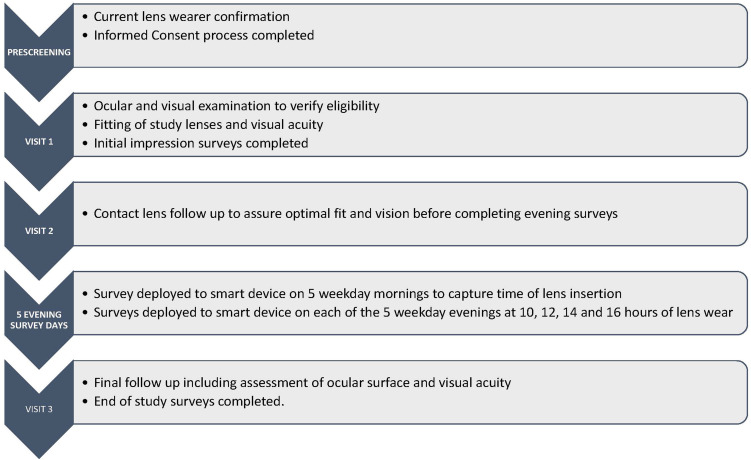
A diagram of the study design can be found in Figure 1. Participants responded to recruitment material and answered prescreening questions to confirm that they were soft spherical contact lens wearers. After completing the informed consent process, participants completed a demographic survey, responded to questions about current lens wear habits, and were examined by slit lamp biomicroscope. To be eligible to enroll in the study, participants were required to be 18–40 years old, current wearers of spherical soft contact lenses with 20/25 or better vision in their habitual lenses, and no self-reported changes in ocular or systemic health in the past 30 days. Additionally, participants could have no active ocular infections or inflammation, and had to be able to wear soft contact lenses for long hours with easy access to a smart phone. At Visit 1, after confirming eligibility to participate, participants were fit with the study lenses the study lens (PRECISION1® One-Day Contact Lenses, Alcon Inc, Fort Worth, TX, USA) and vision and fitting characteristics were examined. Once the fitting was complete, participants completed a VAS survey of initial lens impressions on their own smart phone. Each VAS survey was completed by moving a slider along a line to correspond with their impression of each quality on a scale from 0 to 100. The initial quality of vision VAS was anchored with “POOR Quality” at 0 and “EXCELLENT Quality” at 100. The initial comfort VAS was anchored with “POOR Comfort” at 0 and “EXCELLENT Comfort” at 100. The initial satisfaction VAS was anchored with “NOT Satisfied” at 0 and “EXTREMELY Satisfied” at 100. After completing the survey, additional study lenses were dispensed to be worn until a follow-up visit approximately 1 week (±3 days) later.
Figure 1.
Study design.
At Visit 2, visual acuity, slit lamp assessments of ocular health and contact lens fit, and an over-refraction were completed to ensure that the lens fit and prescription were optimized. Subjects were dispensed additional lenses to wear until Visit 3, approximately 1 week (±3 days) later, and were instructed to look for surveys on their smart phone each of the next 5 business days.
On survey completion days, participants were sent a survey via REDCap each morning to record the time of contact lens insertion for the day. Each evening a survey was later automatically deployed at 10, 12, 14 and 16 hours of lens wear. The surveys were deployed on 5 weekdays between Visit 2 and Visit 3 to maintain consistency. Evening surveys included a 1–10 grading scale for ease of use, assessing comfort with 1 anchored as “Poor comfort” and 10 anchored as “Excellent comfort” and assessing vision with 1 anchored as “Poor vision” and 10 anchored as “Excellent vision”. Scores for the evening time points were averaged for each participant for each time point to result in one overall evening score at 10, 12, 14, and 16 hours of wear for each subject. These mean scores per participant were used to calculate median and interquartile range of the scores for all participants.
The final study visit consisted of final assessment of ocular health and vision, completion of the Contact Lens Questionnaire-8 (CLDEQ-8),18 and completion of end of study surveys. End of study surveys included VAS assessments of (0–100 scale): overall quality of vision, end of day quality of vision, overall comfort, end of day comfort, overall dryness, and end of day dryness. Overall and end of day quality of vision VAS surveys were anchored with 0 as “POOR Quality” and 100 as “EXCELLENT Quality”. Overall comfort and end of day comfort were each anchored with “POOR Comfort” at 0 and “EXCELLENT Comfort” at 100. Overall dryness and end of day dryness were anchored with “No Dryness” at 0 and “MAXIMUM Dryness” at 100. Participants were also surveyed on their satisfaction with the study lens and their preference and ease of use with daily disposable lenses. The scales for convenience, ease of use, and preference for daily disposable contact lenses were 0 to 10, in which a score of 0 was not convenient, easy, or preferred, respectively; five was marked as neutral; and 10 was labelled as very convenient, easy, or preferred, respectively.
Statistical Analysis
This was not a comparative study, and therefore descriptive statistics were used to evaluate survey responses. Normality of the data was assessed with Anderson-Darling test. Because the majority of the data were not normal, non-parametric assessments were completed, and median and interquartile range (IQR) values were calculated to determine overall results. To obtain a single evening survey score for each time point per participant, a mean participant score was calculated by averaging the evening survey scores, resulting in a single mean participant score for 10 hours, 12 hours, 14 hours and 16 hours of wear. Overall, median and interquartile range scores of all participants were calculated for each time point. Vision and comfort scores at each time point were compared with Mann–Whitney analysis to determine if any changes were statistically significant. Initial impression VAS scores from the day of the study lens fitting and overall VAS scores obtained at the end of the study were compared with Mann–Whitney. Overall VAS scores and end of day VAS scores obtained at the end of the study were also compared by Mann–Whitney analysis.
Results
Twenty-seven female and 8 male participants consented and completed the study. The mean (± standard deviation) age of the participants was 25.6 (4.8) years. Demographics of the participants can be found in Table 1. When enrolling in the study, 21 of the participants wore planned replacement lenses habitually and fourteen participants wore daily disposable lenses habitually.
Table 1.
Demographics
| n=35 | |
|---|---|
| Age | Mean (standard deviation): 25.6 (4.8). Range: 18–38. |
| Gender | Female 27 (77%); Male 8 (23%) |
| Ethnicity | Hispanic or Latino 1 (3%); Not Hispanic or Latino 34 (97%) |
| Race | White/Caucasian 26 (74%); Asian 7 (20%); More than one race 2 (6%) |
Visual Acuity
LogMAR visual acuity was measured at every visit while participants were wearing the study lenses. Mean monocular and binocular visual acuity was better than the equivalent of 20/20 Snellen. Visual acuity with the study lenses is reported in Table 2. The mean LogMAR binocular acuity is equivalent to 20/12.5 Snellen visual acuity.
Table 2.
Visual Acuity Data While Participants Wore Daily Disposable Study Contact Lenses
| n=35 | OD | OS | OU |
|---|---|---|---|
| Mean LogMAR acuity | −0.13 | −0.15 | −0.20 |
| Standard deviation | 0.08 | 0.08 | 0.06 |
| Mean Snellen equivalent | 20/16 | 20/16+2 | 20/12.5 |
Initial Impressions Assessment
Median (IQR) values for the VAS Initial Impression Survey were extremely high, with a score of 99.0 (12.0) for quality of vision, a score of 98.0 (16.0) for comfort, and a median score of 100 (13.00) for satisfaction.
Subjective Assessment of Comfort and Vision at Evening Time Points
All 35 subjects were deployed surveys at 10, 12, 14 and 16 hours of wear each night for 5 nights between Visit 2 and Visit 3 for a total of 700 surveys. Of the surveys deployed, 8 survey replies were missed by 5 subjects (1 subject missed 4 surveys, although they were not for the same time points). Since the participant scores at each time point were computed by averaging the scores over the five evenings, the score for participants with a missing survey were calculated by averaging the existing scores.
All evening survey scores (at all time points) for all participants had median values in the high portion of the 0–10 scales (≥7). At 10 hours of wear, the median score (IQR) for comfort was 9.0 (1.2), 8.6 (1.4) at 12 hours; 8.0 (1.4) at 14 hours; and 7.4 (1.7) at 16 hours of wear. Median quality of vision scores were 9.8 (1.0) at 10 hours; 9.6 (1.6) at 12 hours; 9.2 (1.8) at 14 hours and 8.4 (1.7) at 16 hours of wear. Analysis with Mann–Whitney compared the comfort score at each time point and found no difference between the 10 and 12 hours scores, and found a significant difference (P < 0.05) in scores when comparing the 10 and 16 hour time points. There were also significant differences when comparing the 12 and 14 hour time points (P = 0.03) and the 14 and 16 hour time points (P = 0.02). Comparison of the quality of vision scores found a significant difference between the 10 and 16 hour time points (P = 0.001), but no significant differences when comparing any of the 2 hour time increments.
End of Study Assessments of Lens Wear Symptoms
Results of the overall impression VAS survey can be found in Table 3. Overall median (IQR) results for quality of vision [93.0 (14.0)] and comfort [93.0 (16.5)] were over 90 on the 100 point scale. Dryness was scored low, with a median score of 13.0 (34.0). End of day median scores were 87.0 (19.0) for quality of vision and 75.0 (24.5) for comfort. The median end of day dryness score was 37.0 (55.0). All values calculated for end of day surveys are reported in Table 3. Statistical comparisons of initial impression scores and overall scores for comfort and quality of vision found no statistical differences (P > 0.05). Comparisons of overall scores and end of day scores found statistical differences for comfort (P = 0.001) dryness (P = 0.02) and for quality of vision (P = 0.02).
Table 3.
Visual Analog Scale Assessments of Overall Quality of Vision, Comfort, and Dryness and End-of-Day Vision, Comfort, and Dryness
| n=35 | Overall Quality of Vision | Overall Comfort | Overall Dryness | End of Day Quality of Vision | End of Day Comfort | End of Day Dryness |
|---|---|---|---|---|---|---|
| Median | 93.0 | 93.0 | 13.0 | 87.0 | 75.0 | 37.0 |
| Interquartile range | 14.0 | 16.5 | 34.0 | 19.0 | 24.5 | 55.0 |
The CLDEQ-8 validated dry eye questionnaire was administered to subjects after wearing the study contact lenses for two weeks. The CLDEQ-8 specifically asks patients to answer the questions based upon their experiences over the past two weeks of lens wear. The median (IQR) CLDEQ-8 score was 11.0 (7.5). This value is lower than the cutoff point associated with frequent symptoms of dry eye.19
Lens Wear Experience
The final survey included questions regarding the participants’ experiences with daily disposable lenses and with the study contact lenses. The median (IQR) score for the participant ranking of convenience with daily disposable lens wear was 10.0 (0.5). The median rank for the question, “How easy to use are daily disposable lenses?” was 10.0 (1.0). The median score for the prompt “Please rate your preference for daily disposable lenses to reusable contact lenses” was 9.0 (3.5). The median score for the question, “Overall, how satisfied are you with the study lenses?” was 8.0 (2.0).
Discussion
Eye care practitioners recognize the health benefits of daily disposable silicone hydrogel contact lenses, with recent international surveys finding that 82% of practitioners felt that silicone daily disposable lenses should be the standard of care for fitting 1-day contact lens patients.20 While the health benefits of the high oxygen permeability of silicone hydrogel materials and daily replacement lenses are well documented,21 these properties alone do not guarantee successful contact lens wear. Discomfort of lenses is the most common reason for contact lens wear discontinuation.22,23 As a result, various modifications of lens materials and surface treatments have been made in an attempt to develop lenses which sustain comfort throughout the day. The lens used in this study utilizes water surface technology in which a silicone hydrogel core with 51% water content is surrounded by a hydrogel surface with water content >80%.15 While previous studies have shown that comfort and vision were rated high for this lens design, no studies have collected subjective assessments of lenses while wearing the lenses for 16 hours. A previous study using the same lenses found a median (IQR) overall comfort score of 92.0 (18.00) and end of day comfort was 82.50 (51.25),14 which was similar to the findings in this study, although wear time was not reported in that study.
Ocular comfort is known to decrease over the course of a day both with and without contact lens wear, although comfort has been shown to decline more when wearing lenses.24,25 Studies of end of day comfort can be difficult to quantify, since many patients define their “end of day” differently. This study was designed to collect end of day findings over long wear periods in order to determine if this lens would remain comfortable in various patient scenarios. As expected with soft lens wear, the median comfort score declined from 10 to 16 hours, however, the score of 7.4 at 16 hours of wear is still quite high. Of note, the end of day VAS score of 75 mirrors this 16 hour score closely, in this study population, which likely indicates that 16 hours of wear was the end of the day for participants.
In addition to discomfort, poor vision while wearing soft contact lenses has also been identified as a cause of contact lens dissatisfaction.22,23 The mean LogMAR binocular visual acuity in the study lenses was −0.20 (equivalent to 20/12.5 Snellen visual acuity) and the median score of 87 (19) at 16 hours of lens wear was high with the study lens. While there was a small decline in the quality of vision scores over the course of the late evening, it is interesting that there was not a significant difference when comparing the changes at two hours increments. Overall, the median comfort and vision scores throughout evening wear revealed in this study suggest that these lenses can be worn successfully by many patients over long hours of wear.
Limitations of this study include the fact that this was an unmasked, non-comparison study. Since the habitual lenses worn by the participants prior to the study could be any soft lens material and could be either daily disposable or re-wearable lenses, previous comfort experiences with lenses may have varied in the past and could have influenced results. It is known that soft contact lenses, even those with similarly labelled parameters, may fit differently from one another,26 and consequently may perform differently from patient to patient. In this study, all 35 participants were successfully fit with the study lenses. Similar studies with other soft lenses and lens materials would help to create a broader understanding of the known decrease in soft lens comfort over the course of a day with varied lens materials.
Conclusion
Fitting patients in silicone hydrogel daily disposable contact lenses is beneficial as a result of both the high frequency of replacement and the increased oxygen permeability of the lenses. The results of this study show that in addition to these health benefits, the study lens is also looked upon favorably by lens wearers with high median rankings for comfort and vision throughout a long day of lens wear, which is of great benefit to lens wearers and to the practitioners who fit lenses.
Acknowledgments
Funding for this investigator initiated trial was provided by Alcon, Inc., Fort Worth, TX, USA. The project described was supported in part by Award Number Grant UL1TR002733 from the National Center for Advancing Translational Sciences. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Advancing Translational Sciences or the National Institutes of Health.
Data Sharing Statement
Data reported in this manuscript are available within the article. Study-level data including the study protocol are available. To request access to the data, the researcher must sign a data use agreement. All proposals should be directed to Fogt.78@osu.edu for up to 36 months following article publication.
Disclosure
Dr Jennifer Swingle Fogt reports grants from Alcon, Inc, during the conduct of the study; grants and/or personal fees from Alcon, Eyenovia, Nevakar, Unicon, Contamac, Innovega, and Bausch + Lomb, outside the submitted work. The authors report no other conflicts of interest in this work.
References
- 1.Arita R, Mori N, Shirakawa R, et al. Meibum color and free fatty acid composition in patients with meibomian gland dysfunction. Invest Ophthalmol Vis Sci. 2015;56(8):4403–4412. doi: 10.1167/iovs.14-16254 [DOI] [PubMed] [Google Scholar]
- 2.Hickson-Curran S, Spyridon M, Hunt C, Young G. The use of daily disposable lenses in problematic reusable contact lens wearers. Cont Lens Anterior Eye. 2014;37(4):285–291. doi: 10.1016/j.clae.2014.03.002 [DOI] [PubMed] [Google Scholar]
- 3.Steele KR, Szczotka-Flynn L. Epidemiology of contact lens-induced infiltrates: an updated review. Clin Exp Optom. 2017;100(5):473–481. doi: 10.1111/cxo.12598 [DOI] [PubMed] [Google Scholar]
- 4.Rueff EM, Wolfe J, Bailey MD. A study of contact lens compliance in a non-clinical setting. Cont Lens Anterior Eye. 2019;42(5):557–561. doi: 10.1016/j.clae.2019.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chalmers RL, Keay L, McNally J, Kern J. Multicenter case-control study of the role of lens materials and care products on the development of corneal infiltrates. Optom Vis Sci. 2012;89(3):316–325. doi: 10.1097/OPX.0b013e318240c7ff [DOI] [PubMed] [Google Scholar]
- 6.Ichijima H, Karino S, Sakata H, Cavanagh HD. Improvement of subjective symptoms and eye complications when changing from 2-week frequent replacement to daily disposable contact lenses in a subscriber membership system. Eye Contact Lens. 2016;42(3):190–195. doi: 10.1097/ICL.0000000000000167 [DOI] [PubMed] [Google Scholar]
- 7.Diec J, Naduvilath T, Tilia D, Bakaraju RC. The relationship between vision and comfort in contact lens wear. Eye Contact Lens. 2020;47:271–276. [DOI] [PubMed] [Google Scholar]
- 8.Chalmers RL, Begley CG. Dryness symptoms among an unselected clinical population with and without contact lens wear. Cont Lens Anterior Eye. 2006;29(1):25–30. doi: 10.1016/j.clae.2005.12.004 [DOI] [PubMed] [Google Scholar]
- 9.Dumbleton K, Woods CA, Jones LW, Fonn D. The impact of contemporary contact lenses on contact lens discontinuation. Eye Contact Lens. 2013;39(1):93–99. doi: 10.1097/ICL.0b013e318271caf4 [DOI] [PubMed] [Google Scholar]
- 10.Nichols JJ, Willcox MD, Bron AJ, et al. The TFOS international workshop on contact lens discomfort: executive summary. Invest Ophthalmol Vis Sci. 2013;54(11):TFOS7–TFOS13. doi: 10.1167/iovs.13-13212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stapleton F, Tan J. Impact of contact lens material, design, and fitting on discomfort. Eye Contact Lens. 2017;43(1):32–39. doi: 10.1097/ICL.0000000000000318 [DOI] [PubMed] [Google Scholar]
- 12.Jones L, Brennan NA, Gonzalez-Meijome J, et al. The TFOS international workshop on contact lens discomfort: report of the contact lens materials, design, and care subcommittee. Invest Ophthalmol Vis Sci. 2013;54(11):TFOS37–70. doi: 10.1167/iovs.13-13215 [DOI] [PubMed] [Google Scholar]
- 13.Michaud L, Forcier P. Comparing two different daily disposable lenses for improving discomfort related to contact lens wear. Cont Lens Anterior Eye. 2016;39(3):203–209. doi: 10.1016/j.clae.2015.11.002 [DOI] [PubMed] [Google Scholar]
- 14.Rutschilling R, Fogt JS. Wear experience of a water surface daily disposable contact lens in existing silicone hydrogel planned replacement lens wearers. Clin Optom. 2022;14:27–34. doi: 10.2147/OPTO.S353666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cummings S, Giedd B, Pearson C. Clinical performance of a novel daily disposable soft contact lens. J Cont Lens Res Sci. 2020;4(1):e23–e30. doi: 10.22374/jclrs.v4i1.39 [DOI] [Google Scholar]
- 16.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Koh S, Chalmers R, Kabata D, Shintani A, Nishida K. Translation and validation of the 8-item Contact Lens Dry Eye Questionnaire (CLDEQ-8) among Japanese soft contact lens wearers: the J-CLDEQ-8. Invest Ophth Vis Sci. 2019;60(9):533–539. [DOI] [PubMed] [Google Scholar]
- 19.Chalmers RL, Keay L, Hickson-Curran SB, Gleason WJ. Cutoff score and responsiveness of the 8-item Contact Lens Dry Eye Questionnaire (CLDEQ-8) in a large daily disposable contact lens registry. Contact Lens Anterio. 2016;39(5):342–352. doi: 10.1016/j.clae.2016.04.005 [DOI] [PubMed] [Google Scholar]
- 20.Orsborn G, Dumbleton K. Eye care professionals’ perceptions of the benefits of daily disposable silicone hydrogel contact lenses. Cont Lens Anterior Eye. 2019;42(4):373–379. doi: 10.1016/j.clae.2019.02.012 [DOI] [PubMed] [Google Scholar]
- 21.Sulley A, Dumbleton K. Silicone hydrogel daily disposable benefits: the evidence. Cont Lens Anterior Eye. 2020;43(3):298–307. doi: 10.1016/j.clae.2020.02.001 [DOI] [PubMed] [Google Scholar]
- 22.Richdale K, Sinnott LT, Skadahl E, Nichols JJ. Frequency of and factors associated with contact lens dissatisfaction and discontinuation. Cornea. 2007;26(2):168–174. doi: 10.1097/01.ico.0000248382.32143.86 [DOI] [PubMed] [Google Scholar]
- 23.Pucker AD, Tichenor AA. A review of contact lens dropout. Clin Optom. 2020;12:85–94. doi: 10.2147/OPTO.S198637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Willcox MD, Zhao Z, Naduvilath T. Cytokine changes in tears and relationship to contact lens discomfort. Mol Vis. 2015;21:293–305. [PMC free article] [PubMed] [Google Scholar]
- 25.McMonnies CW. An amplifying cascade of contact lens-related end-of-day hyperaemia and dryness symptoms. Curr Eye Res. 2018;43(7):839–847. doi: 10.1080/02713683.2018.1457163 [DOI] [PubMed] [Google Scholar]
- 26.Barr JT. “Generic” soft contact lenses: scientific, clinical, and regulatory matters. Contact Lens Spectrum. 2021;2021:37–40. [Google Scholar]