Abstract
Background
Postoperative ileus (POI) is an important complication of gastrointestinal (GI) surgery. Acupuncture has been increasingly used in treating POI. This study aimed to assess the effectiveness and safety of acupuncture for POI following GI surgery.
Methods
Seven databases (PubMed, Embase, the Cochrane Library, China National Knowledge Infrastructure, Wan fang Data, VIP Database for Chinese Technical Periodicals, and Chinese Biomedical Literature Database) and related resources were searched from inception to May 30, 2021. Randomized controlled trials (RCTs) reporting the acupuncture for POI in GI were included. The quality of RCTs was assessed by the Cochrane Collaboration Risk of Bias tool, and the certainty of the evidence was evaluated by the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) approach. A meta-analysis was performed by using RevMan 5.4 software.
Results
Eighteen RCTs involving 1413 participants were included. The meta-analysis showed that acupuncture could reduce the time to first flatus (TFF) (standardized mean difference [SMD] = −1.14, 95% confidence interval [CI]: −1.54 to −0.73, P < 0.00001), time to first defecation (TFD) (SMD = −1.31, 95% CI: −1.88 to −0.74, P < 0.00001), time to bowel sounds recovery (TBSR) (SMD = −1.57, 95% CI: −2.14 to −1.01, P < 0.00001), and length of hospital stay (LOS) (mean difference [MD] = −1.68, 95% CI: −2.55 to −0.80, P = 0.0002) compared with usual care. A subgroup analysis found that acupuncture at distal acupoints once daily after surgery had superior effects on reducing TFF and TFD. A sensitivity analysis supported the validity of the finding. Acupuncture also manifested an effect of reducing TFF, TFD and TBSR compared with sham acupuncture but the result was not stable. Relatively few trials have reported whether adverse events have occurred.
Conclusions
Acupuncture showed a certain effect in reducing POI following GI surgery with very low-to-moderate quality of evidence. The overall safety of acupuncture should be further validated. More high-quality, large-scale, and multicenter original trials are needed in the future.
Introduction
Postoperative ileus (POI) is one of the most frequently occurring complications of gastrointestinal (GI) surgery that continues to prove challenging [1]. Approximately 24% of patients undergoing colectomy will develop this complication [2]. POI is a pathologic GI tract dysmotility characterized by abdominal distension, pain, delayed passage of flatus and stool, nausea, vomiting, and inability to tolerate an oral diet [3, 4]. POI is also a critical risk factor for severe morbidity, such as dehydration, electrolyte imbalance, or sepsis [5]. These conditions not only decrease the patient’s quality of life but also lead to prolonged hospitalization, increased hospital costs, and 30-day readmission rates [6–8]. Consequently, POI imposes a substantial financial and medical resource burden on the healthcare system. The annual costs of POI management in the US have been USD 1.5 billion [9].
The indistinct mechanism and etiology of POI, which involves opioid analgesia, intestinal operation, postoperative stress or anxiolytic medications, increase the difficulty of its prevention and treatment [5, 10]. Effective strategies for POI management to accelerate postoperative GI function recovery is exigent. The usual care patient receives after GI surgery mainly includes routine nasogastric tubes, intravenous fluids, parenteral nutrition, and early mobilization [11]. The POI management adopting multidisciplinary approaches is also recommended, including minimizing surgical manipulation of the intestine, epidural analgesia, and stimulating bowel motility treatments, such as alvimopam, coffee, and chewing gum [12–14]. However, the definite clinical efficacy of those therapies is controversial [15, 16]. There has been a need to seek complementary and alternative medicine approaches for POI management [17].
Acupuncture is a form of conventional medical practice that has been used in East Asia for thousands of years [18]. It stimulates specific acupoints to correct the imbalance of energy within the body. Owing to its nonpharmacological and minimally invasive advantages, acupuncture is commonly applied to various GI diseases including irritable bowel syndrome [19, 20], gastroparesis [21, 22], and constipation [23]. Several clinical trials have shown the potential effectiveness of acupuncture on GI function recovery, such as the bidirectional regulation effect on gastric myoelectrical activity and reduction of abdominal distension [24, 25].
Some previous meta-analyses evaluating the effectiveness of acupuncture in POI have been reported. A previous study [26], which included abdominal surgery patients, found that electroacupuncture (EA) or transcutaneous electric acupoint stimulation (TEAS) is effective for POI. Another two previous meta-analyses examined the effectiveness of acupuncture in cancer patients and showed that acupuncture and related therapies could improve the recovery of GI function [27, 28]. However, the evidence of acupuncture for POI is still inconclusive in GI surgery patients. GI surgery is one of the most common types of major abdominal surgery and has a direct impact on the GI tract. Aiming to provide more targeted evidence for clinicians, we focused on POI patients undergoing GI surgery in this systematic review and meta-analysis to critically evaluate the effectiveness and safety of acupuncture.
Materials and methods
The registered study protocol of this systematic review and meta-analysis is available in the PROSPERO International prospective register of systematic reviews database (https://www.crd.york.ac.uk/prospero/, identification number: CRD42020183593). We performed this study according to the Cochrane Handbook for Systematic Reviews of Interventions [29] and followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Statement (PRISMA) guidelines [30].
Database and search strategy
The following databases were searched up to May 30, 2021: PubMed, Embase, the Cochrane Library, China National Knowledge Infrastructure (CNKI), Wan fang Data, Chongqing VIP Database (CQVIP), and Chinese Biomedical Literature Database (CBM). The ClinicalTrials.gov was also searched to avoid omitting ongoing or unpublished studies. The reference lists of other systematic reviews and all included studies were used to obtain relevant studies. The following keywords were searched: “acupuncture”, “acupuncture therapy”, “electroacupuncture”, “transcutaneous electrical acupoint stimulation”, “postoperative ileus”, “postoperative bowel disfunction”, and “gastrointestinal surgery”. The detailed search strategy is available in S1 Appendix. The literature regions and publication types were not restricted.
Study selection
Inclusion criteria
(I) Participants: participants should be > 18 years old following GI surgery. (II) Interventions: acupuncture therapies, including manual acupuncture (MA), EA, TEAS, abdominal acupuncture and so on; (III) Comparisons: usual care or sham acupuncture. (IV) Outcomes: primary outcomes were time to first flatus (TFF) and time to first defecation (TFD), and secondary outcomes were time to bowel sounds recovery (TBSR) and length of hospital stay (LOS). (V) Study design: randomized controlled trial (RCT).
Exclusion criteria
(I) Non-GI surgery patients. (II) The acupuncture regimen was acupuncture combined with oral herbal medicine, embedding, acupoint injection, or other non-acupuncture-related therapy. (III) The comparison represented other techniques of traditional Chinese medicine, herbal medications, or other acupuncture styles. (IV) The primary outcome was insufficient.
Data extraction
The data extraction process was independently performed by two reviewers (ZY and ZQ X). The two reviewers independently selected articles following the inclusion and exclusion criteria and assessed the full texts of the selected trials. The relevant information was extracted as follows: first author, year of publication, country, baseline characteristics of patients, number of patients, surgical procedures, intervention details, control types and main outcomes. All information was included in a standardized data extraction form. Divergence would be conquered by the adjudication of the supervisor (KW).
Risk of bias assessment
The methodological qualities were assessed by two investigators (LK and YL) according to the Cochrane risk of bias (ROB) tool [29]. ROB was classified into three grades: low risk, high risk, or unclear risk. It included seven domains: (I) random sequence generation; (II) allocation concealment; (III) blinding of participants and personnel; (IV) blinding of outcome assessment; (V) selective reporting; (VI) incomplete outcome data; (VII) other bias. Disagreements were discussed between the two reviewers, and if these were unresolved, a third reviewer (JL) was added to the discussion until a consensus was reached.
Evidence quality assessment
We used the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach to rate the overall quality of evidence [31]. The GRADE guideline has five domains, including the risk of bias, inconsistency, indirectness, imprecision, and potential publication bias. GRADE provides four levels of quality (high, moderate, low, and very low) for evidence grading. Two researchers (ZY and XQ W) performed the assessment process independently, and a third researcher (KW) then reviewed the evalution. Any disagreement was resolved by discussion with professional specialist advice.
Data analysis
We used Review Manager (RevMan) version 5.4.1 software (The Nordic Cochrane Center, The Cochrane Collaboration, Copenhagen, Denmark [32]) to perform the meta-analysis. The continuous variables were assessed by mean difference (MD) with a 95% confidence interval (CI) when the unit was the same. Otherwise, the standardized mean difference (SMD) was used. A P value of < 0.05 was considered statistically significant. The magnitude of the effect size of SMD was rated as follows: ≤ 0.2 indicated a small effect, 0.5 indicated a moderate effect, and ≥ 0.8 indicated a large effect. As for the testing of heterogeneity, we used χ2 test. If I2 was < 50% in the results, we selected a fixed-effects model to pool the data. Otherwise, a random-effects model was adopted.
To explore the source of heterogeneity, subgroup analysis was conducted to analyze the primary outcomes. Sensitivity analysis was performed by excluding each RCT sequentially and comparing the model characteristics to test the robustness of the result. A funnel plot was used to detect publication bias when at least 10 trials were included. Additionally, we used Stata 12.0 software (StataCorp, Texas, USA) to put Egger’s test aiming to assess the funnel plot. The significant publication bias was defined as a P-value of < 0.1.
Results
Search results
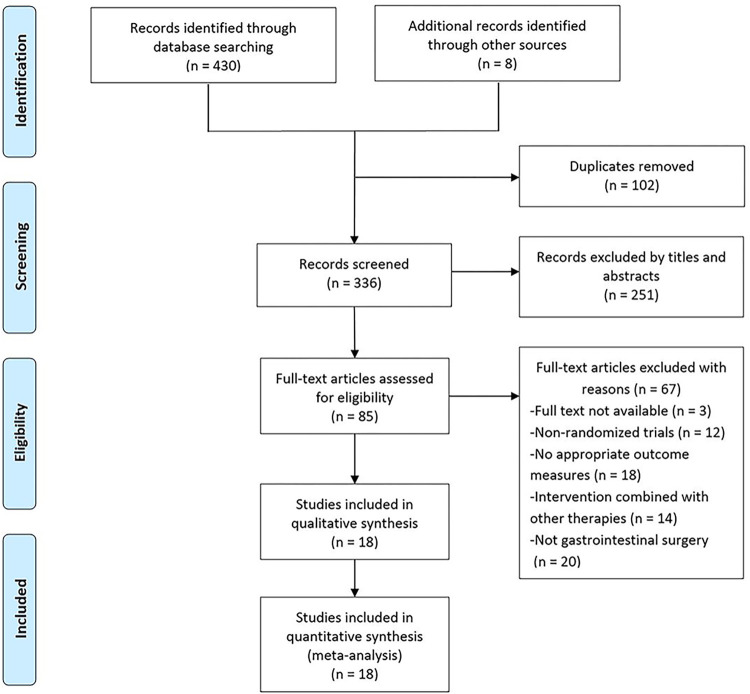
We initially identified 430 studies through database searching and eight studies through other sources. After removing 102 duplicates, 336 articles were screened, and 251 articles were removed by titles and abstract. Furthermore, 67 studies were excluded after reviewing full texts based on eligibility criteria. Finally, 18 studies [33–50] were included in this study (Fig 1).
Fig 1. The flow diagram of study selection.
Study characteristics
Included RCTs were published from 2008 to 2020. Sixteen trials [33–39, 41–48, 50] were from China, one trial [40] was from Korea, and one trial [49] was from America. The study size ranged from 30 to 165. The main characteristics of the studies are summarized in Table 1.
Table 1. Characteristics of included studies in the systematic review and meta-analysis.
| Study | Country | Sample size (M/F) | Ages (I/C) | Surgical approach | Control a | Intervention | Course of treatment | Outcomes |
|---|---|---|---|---|---|---|---|---|
| Xu 2020 [33] | China | I: 16/14 C: 15/15 |
I: 28.55 ± 9.75 C: 29.64 ± 9.34 |
Open | UC | EA | NA | TFF, TBSR, LOS |
| Gu 2019 [35] | China | I: 31/27 C: 29/30 |
I: 57.59 ± 7.32 C: 56.67 ± 6.23 |
Laparoscopic | SA | TEAS | From 30 min before anesthetic induction to 2 days after operation | TFF, TFD, TBSR, VAS, AC, Incidence of PONV, Patient satisfaction |
| Pu 2019 [34] | China | I: 20/11 C: 16/15 |
I: 55.07 ± 10.17 C: 56.13 ± 11.08 |
Open | UC | EA | 5 consecutive postoperative days | TFF, TFD, TBSR, LOS, PSA |
| Chen 2018 [36] | China | I: 22/11 C: 24/6 |
I: 63.0 ± 9.70 C: 59.0 ± 8.30 |
Open, laparoscopic | UC | TEAS | Starting on postoperative day 1, for 5 consecutive days or until passing flatus | TFF, TFD, LOS, TNTR, TLSD, PSA |
| Kang 2017 [39] | China | I: 39/29 C: 41/27 |
I: 41.28 ± 10.36 C: 40.75 ± 10.19 |
Unclear | UC | EA | NA | TFF, TFD, TBSR, LOS, ADL |
| Jung 2017 [40] | Korea | I: 16/2 C: 16/2 |
I: 60.94 ± 9.43 C: 60.06 ± 13.18 |
Open, laparoscopic | UC | EA | 5 consecutive postoperative days | TFF, TFD, LOS, SWI, SSD, the number of remnant sitz markers in the small intestine on abdominal radiograph |
| Yuan 2017 [37] | China | I: 12/18 C: 16/14 |
I: 53.9 ± 9.8 C: 54.6 ± 10.4 |
Laparoscopic | SA | TEAS | Half an hour before operation, then 3 consecutive postoperative days | TFF, TBSR, LOS, Incidence of PONV, AC |
| Qian 2017 [38] | China | I: 20/10 C: 17/13 |
I: 59 ±10 C: 60 ± 11 |
Unclear | UC | MA | 7 consecutive postoperative days | TBSR, TFF, LOS, TGTR, IPAR, QOL, Hospitalization expenses |
| Zhang 2014 [41] | China | I: 11/8 C: 11/9 |
I: 63 ± 9 C: 60 ± 10 |
Open | SA | EA | 30 min after operation, then 4 consecutive postoperative days | TFF, TFD, TBSR, |
| Xiao 2014 [42] | China | I: 18/12 C1: 19/11 C2: 14/16 |
I: 55.87 ± 10.49 C1: 55.33 ± 10.83 C2: 54.63 ± 10.25 |
Open | UC | I1: EA I2: MA |
5 consecutive postoperative days | TFF, TFD, TBSR, PSA |
| Tong 2014 [43] | China | I: 24/18 C: 26/16 |
I: 58.6 ± 15.1 C: 59.2 ± 14.7 |
Open | UC | MA | 2 consecutive postoperative days | TFF, TFD, TBSR, TLFI, TNTR, PSA |
| Wang 2013 [44] | China | I: 41/23 C: 43/21 |
I: 40.5 ± 9.7 C: 42.3 ± 9.1 |
Unclear | UC | MA | 10 consecutive postoperative days | TFF, TFD, TBSR |
| Ng 2013 [45] | China | I: 35/20 C1: 33/22 C2: 31/24 |
I: 67.4 ± 9.7 C1: 67.4 ± 10.7 C2: 68.5 ± 10.6 |
Laparoscopic | C1: UC C2: SA |
EA | Starting on postoperative day 1, for 4 consecutive days or until the first defecation | TFF, TFD, LOS, TTSD, TWI, VAS, AC |
| Shi 2012 [46] | China | I: 15/15 C: 17/13 |
I: 53.17 ± 13.491 C: 53.77 ± 13.320 |
Unclear | UC | EA | 3 consecutive postoperative days | TFF, TFD, TBSR, PSA |
| Yang 2011 [47] | China | I: 21/10 C: 18/11 |
I: 60.9 ± 6.63 C: 62 ± 6.98 |
Unclear | UC | EA | Starting on postoperative day 1 until 3 days after first defecation | TFF, TFD, TBSR |
| Wang 2011 [48] | China | I: 11/4 C: 9/6 |
I: 58.0 ± 10.24 C: 60.4 ± 11.01 |
Open | UC | MA | 5 consecutive postoperative days | TFF, TFD, TBSR, PSA |
| Meng 2010 [50] | China | M: 47 F: 38 |
I: 54.3 (mean) C: 53.1(mean) |
Unclear | UC | EA | Starting on postoperative day 1, for 6 consecutive days or until the first bowel movement | TFF, TFD, EGEG, QOL |
| Garcia 2008 [49] | America | I: 25/13 C: 26/14 |
35–45: 14 46–55: 24 56–65: 26 66–75: 12 75: 1 |
Unclear | UC | EA | Starting on postoperative day 1, for 4 consecutive days or until the first defecation | TFF, TFD, LOS, AC, QOL |
a Usual care included: routine nasogastric tubes, intravenous fluids, parenteral nutrition and early mobilization.
Abbreviations: I/C, Intervention group/Control group; M/F, Male/Female; MA, manual acupuncture; EA, electroacupuncture; TEAS, transcutaneous electrical acupoint stimulation; UC, usual care; SA, sham acupuncture; ERAS, enhanced recovery after surgery; NA, not available; TFF, time to first flatus; TBSR, time to bowel sounds recovery; LOS, length of hospital stay; TFD, time to first defecation; VAS, visual analogue scale; AC, analgesic consumption; PONV, postoperative nausea and vomiting; PSA, postoperative symptom assessment; TNTR, time to nasogastric tube removal; TLSD, time to liquid and semi-liquid diet; ADL, activities of daily living; SWI, start of water intake; SSD, start of soft diet; TGTR, time to gastric tube removal; IPAR, incidence of postoperative adverse reactions; QOL, quality of life status, including pain, nausea, insomnia, abdominal distention and general sense of well-being; TLFI, time to liquid food intake; TTSD, time to tolerated a solid diet; TWI, time to walk independently; EGEG, electro-gastroenterography.
Eighteen studies included 1413 participants, of whom 666 were in the intervention group, and 747 were in the control group. There were 845 males and 568 females among these participants. The age of participants ranged from 28.55 years to 68.5 years.
In terms of intervention, three types of acupuncture techniques were involved: MA, EA, and TEAS. Among all studies, a total of 23 acupoints were used. The commonly used acupoints were ST36, ST37, and SP6, which were located in the stomach meridian and spleen meridian. All trials [33–50] reported the treatment timing. Two trials [35, 37] performed acupuncture before and after the operation, respectively. Other trials [33, 34, 36, 38–50] all performed acupuncture after the operation. Eleven studies [33–35, 38, 41–43, 45, 47–49] reported deqi sensation. The acupuncture retention time varied from 20 to 60 minutes. The frequency of treatment comprised once per day (1/d), twice per day (2/d), or three times per day (3/d). The main details of the interventions are summarized in Table 2.
Table 2. Details of intervention.
| Trials | Intervention | Acupoints selection | Starting intervention | Frequency | Response sought | Retention time | Stimulus parameter |
|---|---|---|---|---|---|---|---|
| Xu 2020 [33] | EA | ST36, SP6, PC6, CV12 | Postoperative 6h | 2/d | DS | 20 min | Dilatational wave, 2Hz |
| Gu 2019 [35] | TEAS | ST36 and PC6 | 1.30 min before anesthetic induction 2. Postoperative day 1 |
3/d | DS | 1.60 min 2.30 min |
5−30 mA |
| Pu 2019 [34] | EA | PC6, SP4, ST37, ST36 | Postoperative day 1 | 1/d | DS | 30 min | Discontinuous wave, 2 Hz, 1−10 mA |
| Chen 2018 [36] | TEAS | ST36 and PC6 | Postoperative day 1 | 2/d | NA | 60 min | ST36: 2 s on, 3 s off, 25 Hz, 0.5 ms, 2−6 mA; PC6: 0.1 s on, 0.4 s off, 100 Hz, 0.25ms, 2−6 mA. |
| Kang 2017 [39] | EA | ST36 | Postoperative day 1 | 1/d | NA | 30 min | Continuous wave |
| Jung 2017 [40] | EA | ST36, SP6, LI4, SJ6, LV3, LI11 GV20†, EX-HN3†, GV26†, CV24† |
Postoperative day 1 | 1/d | NA | 25−30 min | ST36, SP6, LI4, TE6:100 Hz |
| Yuan 2017 [37] | TEAS | PC6, LI4, ST36 | 1. Preoperative 30 min 2. Postoperation |
1/d | NA | 30min | NA |
| Qian 2017 [38] | MA | ST36, ST37, ST39 | Postoperative day 1 | 1/d | DS | 20 min | NA |
| Zhang 2014 [41] | EA | ST36 | Postoperative 30 min | 1/d | DS | 30 min | 2 Hz, 0.16 ms |
| Xiao 2014 [42] | EA | ST36, ST37 | Postoperative day 1 | 1/d | DS | 20 min | Dilatational wave |
| Tong 2014 [43] | MA | ST36, SP6, ST37, SP4 | Postoperative 2 h | 1/d | DS | 30min | NA |
| Wang 2013 [44] | MA | CV12†, CV10†, CV6†, CV4†; ST25, SP15, ST26, Xiafengshidian |
Postoperation | 1/d | NA | 30 min | NA |
| Ng 2013 [45] | EA | ST36, SP6, LI4, SJ6 | Postoperative day 1 | 1/d | DS | 20 min | 100 Hz |
| Shi 2012 [46] | EA | ST36, ST37, ST39 | Postoperative 6 h | 2/d | NA | 30 min | Dilatational wave 4 Hz/20 Hz |
| Yang 2011 [47] | EA | ST36, ST37, ST39 | Postoperative day 1 | 1/d | DS | 30 min | Continuous wave |
| Wang 2011 [48] | MA | PC6, SP4, ST37, ST36 | Postoperative 24h | 1/d | DS | 30 min | NA |
| Meng 2010 [50] | EA | SJ6, GB34, ST36, ST37 | Postoperative day 1 | 1/d | NA | 20 min | SJ6, GB34: Continuous wave, 2 Hz |
| Garcia 2008 [49] | EA | LI4, SP6, ST36, ST25, CV6†, CV12† | Postoperative day 1 | 2/d | DS | 20 min | LI 4 (positive) to ST 36 (negative), 50 Hz, 16 mA |
†unilaterally
Abbreviations: MA, manual acupuncture; EA, electroacupuncture; TEAS, transcutaneous electroacupuncture stimulation; ST36, zusanli acupoint; SP6, sanyinjiao acupoint; PC6, neiguan acupoint; CV12, zhongwan acupoint; SP4, gongsun acupoint; ST37, shangjuxu acupoint; LI4, hegu acupoint; SJ6, zhigou acupoint; LV3, taichong acupoint; LI11, quchi acupoint; GV20, baihui acupoint; EX-HN3, yintang acupoint; GV26, shuigou acupoint; CV24, chengjiang acupoint; ST39, xiajuxu acupoint; CV10, xiawan acupoint; CV6, qihai acupoint; CV4, guanyuan acupoint; ST25, tianshu acupoint; SP15, daheng acupoint; ST26, wailing acupoint; GB34, yanglingquan acupoint; DS, de qi sensation, the achievement of a radiating sensation with paresthesia was indicative of effective needling; NA, not available.
In terms of control, 14 studies [33, 34, 36, 38–40, 42–44, 46–50] used usual care, and three studies [35, 37, 41] applied sham acupuncture plus usual care. Additionally, there was one study [45] that set up two control groups including usual care and sham acupuncture.
The main outcomes of most trials were TFF, TFD, TBSR, and LOS. Additionally, there were trials reporting the analgesic consumption, postoperative nausea and vomiting, and time to nasogastric tube removal.
Risk of bias assessment
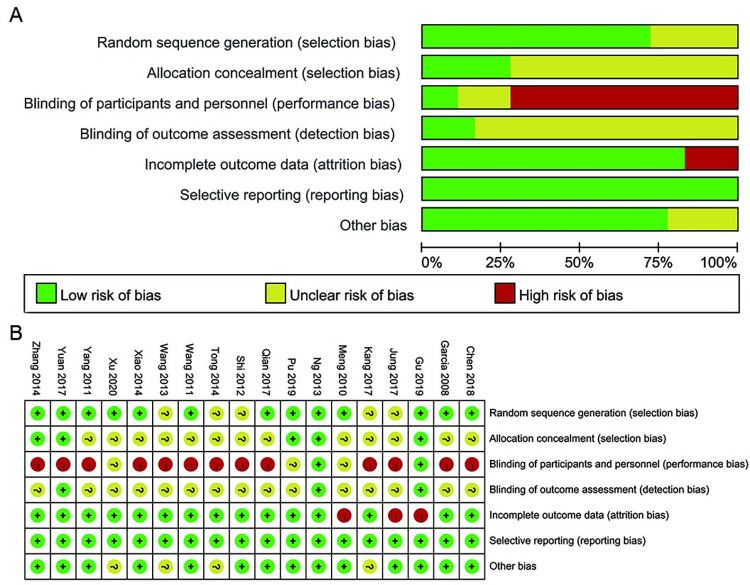
The risk of bias of each included trial is listed in Fig 2. All studies were described as “randomized” but five [39, 40, 43, 44, 46] did not describe details of sequence generation; hence, these were judged as “unclear risk”. Five studies [34, 35, 37, 41, 45] described the method of allocation concealment; therefore, these were judged as “low risk”. Thirteen trials [33, 36, 38–40, 42–44, 46–50] did not offer the details of the allocation concealment; hence, we judged them as “unclear risk”. It was not possible for practitioners to be blinded in the acupuncture treatment. Therefore, we judged two trials [35, 45] as “low risk” of performance bias since the outcome investigator was blind to group allocation, meaning the acupuncture performer did not participate in the data collection. Thirteen trials [36–44, 46–49] did not use the blind method; thus, we judged these trials as “high risk”. Furthermore, three trials [33, 34, 50] did not mention the details of the blinding method; therefore, we judged them as “unclear risk”. Three trials [35, 37, 45] described the blinding of the outcome assessor; hence, these were judged as “low risk”. Fifteen trials [33, 34, 36, 38–44, 46–50] did not adequately describe whether the outcome assessor was blinded to the treatment allocation; therefore, these were judged as “unclear risk”. Three trials [35, 40, 50] had a high risk of attrition bias due to participants’ withdrawal from the studies. All the trials reported the predetermined outcome measures; hence, the reporting bias were judged as “low risk”. Four trials [33, 39, 43, 44] were judged at unclear risk of other potential bias due to insufficient registration information.
Fig 2. Risk of bias summary.
Overall effectiveness of acupuncture
Acupuncture versus usual care
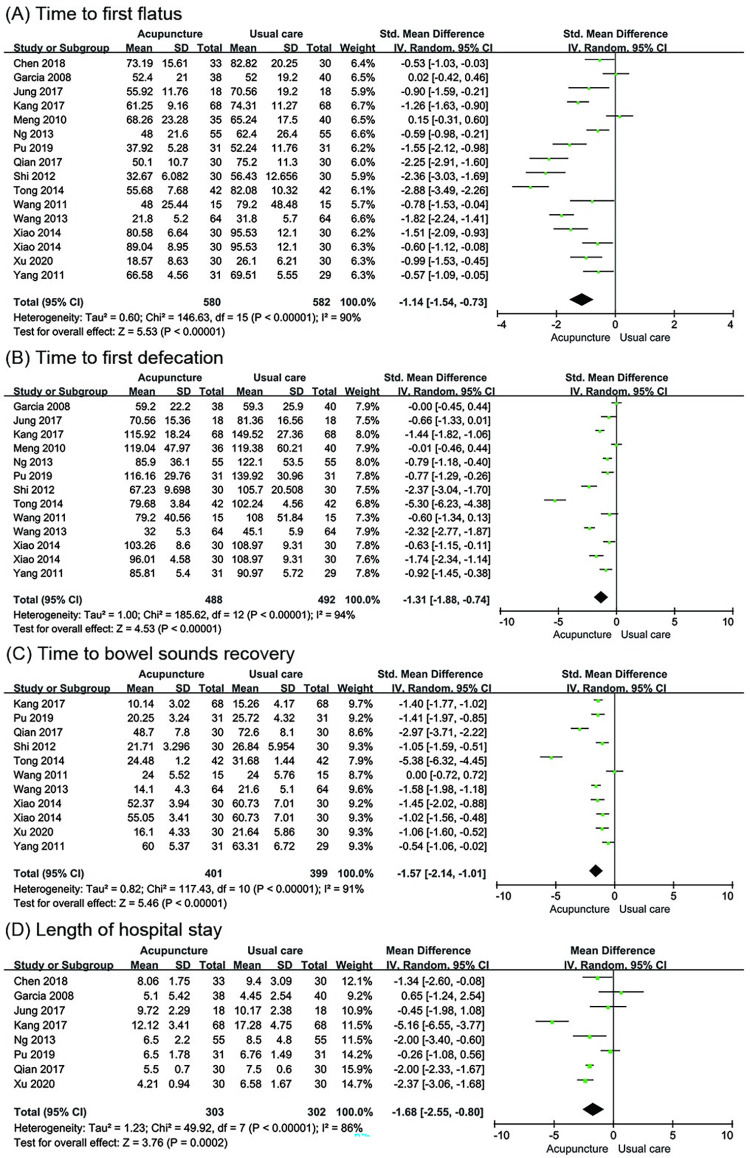
Time to first flatus. Fifteen trials [33, 34, 36, 38–40, 42–50] involving 1162 participants evaluated the change in TFF (hour). Pooled results indicated that acupuncture had a better effect in shortening the TFF compared to usual care (SMD = -1.14; 95% CI: -1.54 to -0.73; P < 0.00001; I2 = 90%; Fig 3A).
Fig 3.
Meta-analysis of acupuncture versus usual care for (A) Time to first flatus, (B) Time to first defecation, (C) Time to bowel sounds recovery and (D) Length of hospital stay.
Time to first defecation. Twelve trials [34, 39, 40, 42–50] with 980 participants examined the change in TFD (hour). The analysis data showed that acupuncture resulted in a reduction in TFD compared to usual care (SMD = -1.31; 95% CI: -1.88 to -0.74; P < 0.00001; I2 = 94%; Fig 3B).
Time to bowel sounds recovery. Ten trials [33, 34, 38, 39, 42–44, 46–48] involving 800 participants reported this outcome and showed significant shortening of TBSR (hour) in the acupuncture group compared to the usual care group (SMD = -1.57; 95% CI: -2.14 to -1.01; P < 0.00001; I2 = 91%; Fig 3C).
Length of hospital stay. Eight trials [33, 34, 36, 38–40, 45, 49] involving 605 participants reported the LOS (day). The LOS was shorter in the acupuncture group compared to the usual care group (MD = -1.68d; 95% CI: -2.55 to -0.80; P = 0.0002; I2 = 86%; Fig 3D).
Acupuncture versus sham acupuncture
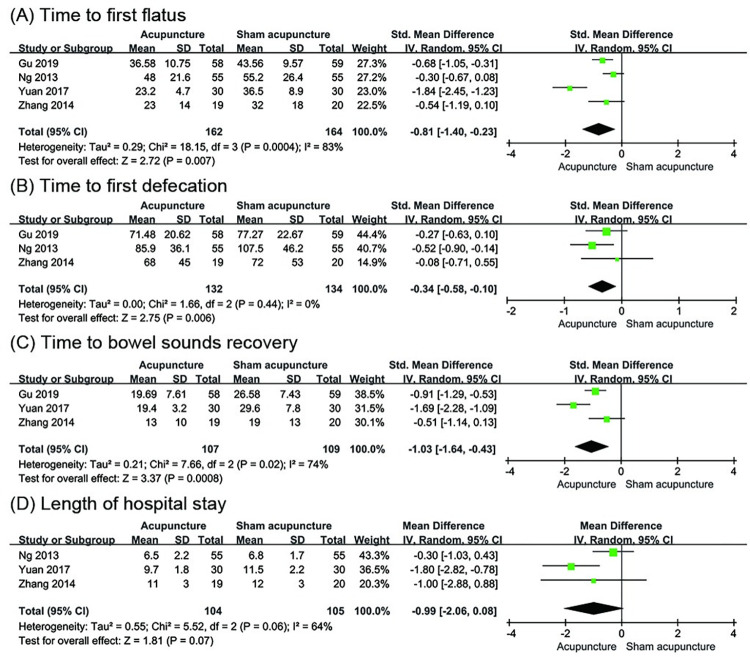
Time to first flatus. Four trials [35, 37, 41, 45] involving 326 participants evaluated the change in TFF. The results showed a difference between the acupuncture group and the sham acupuncture group (SMD = -0.81; 95% CI: -1.40 to -0.23; P = 0.007; I2 = 83%; Fig 4A).
Fig 4.
Meta-analysis of acupuncture versus sham acupuncture for (A) Time to first flatus, (B) Time to first defecation, (C) Time to bowel sounds recovery and (D) Length of hospital stay.
Time to first defecation. Three trials [35, 41, 45] with 266 participants evaluated the change in TFD. The analysis data showed that acupuncture had a better effect in reducing TFD compared to sham acupuncture (SMD = -0.34; 95% CI: -0.58 to -0.10; P = 0.006; I2 = 0%; Fig 4B).
Time to bowel sounds recovery. Three trials [35, 37, 41] involving 216 participants reported TBSR and showed more reduction in the acupuncture group compared to the sham acupuncture group (SMD = -1.03; 95% CI: -1.64 to -0.43; P = 0.0008; I2 = 74%; Fig 4C).
Length of hospital stay. Three trials [37, 41, 45] involving 209 participants reported the LOS. The result showed that there was no statistical difference between the acupuncture group and the sham acupuncture group (MD = -0.99 d; 95% CI: -2.06 to -0.08; P = 0.07; I2 = 64%; Fig 4D).
Subgroup analysis
Due to the limited number of studies, we only analyzed the primary outcomes TFF and TFD in the comparison between acupuncture and usual care. The subgroups were based on the following characteristics: (I) acupuncture technique: MA, EA, or TEAS; (II) acupoints combination: distal acupoints combination or distal–proximal acupoints combination; (III) frequency of treatment sessions: 1 session per day (1/d) or 2 sessions per day (2/d). The results are listed in the Table 3.
Table 3. Subgroup analysis.
| Outcome | Subgroup | Studies | Patients | Effect Sizes SMD | 95%CI | Heterogeneity I2 (%) | P value |
|---|---|---|---|---|---|---|---|
| Time to first flatus | Acupuncture technique | ||||||
| MA | 5 | 362 | -1.67 | [-2.47, -0.86] | 90 | < 0.0001 | |
| EA | 10 | 737 | -0.94 | [-1.38, -0.49] | 87 | < 0.0001 | |
| TEAS | 1 | 63 | -0.53 | [-1.03, -0.03] | - | = 0.04 | |
| Acupoints combination | |||||||
| Distal acupoints combination | 12 | 896 | -1.19 | [-1.64, -0.74] | 89 | < 0.00001 | |
| Distal–proximal acupoints combination | 3 | 266 | -0.93 | [-2.05, 0.19] | 94 | = 0.1 | |
| Frequency of treatment session | |||||||
| 1/d | 11 | 901 | -1.2 | [-1.66, -0.75] | 89 | < 0.00001 | |
| 2/d | 4 | 261 | -0.94 | [-1.85, -0.03] | 92 | = 0.04 | |
| Time to first defecation | Acupuncture technique | ||||||
| MA | 4 | 302 | -2.18 | [-3.87, -0.50] | 97 | = 0.01 | |
| EA | 9 | 678 | -0.93 | [-1.40, -0.46] | 88 | = 0.0001 | |
| Acupoints combination | |||||||
| Distal acupoints combination | 10 | 774 | -1.32 | [-1.92, -0.73] | 93 | <0.0001 | |
| Distal–proximal acupoints combination | 2 | 206 | -1.16 | [-3.43, 1.11] | 98 | = 0.32 | |
| Frequency of treatment session | |||||||
| 1/d | 10 | 842 | -1.32 | [-1.93, -0.72] | 93 | <0.0001 | |
| 2/d | 2 | 138 | -1.17 | [-3.49, 1.14] | 97 | = 0.32 | |
Abbreviations: MA, manual acupuncture; EA, electroacupuncture; TEAS, transcutaneous electrical acupoint stimulation; SMD, standardized mean difference; 95%CI, 95% Confidence interval.
The subgroup analysis showed that studies with all types of acupuncture techniques had a significant effect on reducing TFF and TFD substantially. Regarding the type of acupoints combination, studies that applied distal acupoints combination showed significant improvement in reducing TFF (SMD = -1.19; 95% CI: -1.64 to -0.74; P < 0.00001; I2 = 89%) and TFD (SMD = -1.32; 95% CI: -1.92 to -0.73; P < 0.0001; I2 = 93%). In the analysis based on the frequency of treatment sessions, both two frequencies showed a significant effect in reducing TFF. However, only acupuncture treatment with 1 session per day showed significant improvement in reducing TFD (SMD = -1.32; 95% CI: -1.93 to -0.72; P < 0.0001; I2 = 93%). No factors could account for the heterogeneity.
Sensitivity analysis
In comparison with usual care, there were no changes in the significant outputs from the meta-analysis by omitting a single study. These heterogeneities did not influence the stability of the result. In comparison with sham acupuncture, there were changes in the outputs after excluding each study. After removing the study conducted by Gu et al. [35], the results of TFF (P = 0.06), TFD (P = 0.07), and TBSR (P = 0.06) showed no significance. After excluding the study conducted by Ng et al. [45], the result of TFD (P = 0.17) showed no significance, and the result direction of LOS (P = 0.0004) was reversed. After removing the study of Yuan et al. [37], the heterogeneity was significantly reduced, and the result was not altered (see S2 Appendix).
Adverse events
There were four studies [34, 36, 49, 50] that reported the information on adverse events. Only one study [36] reported mild bruising of the wrist due to TEAS. Three studies [34, 49, 50] stated that there were no adverse events for acupuncture.
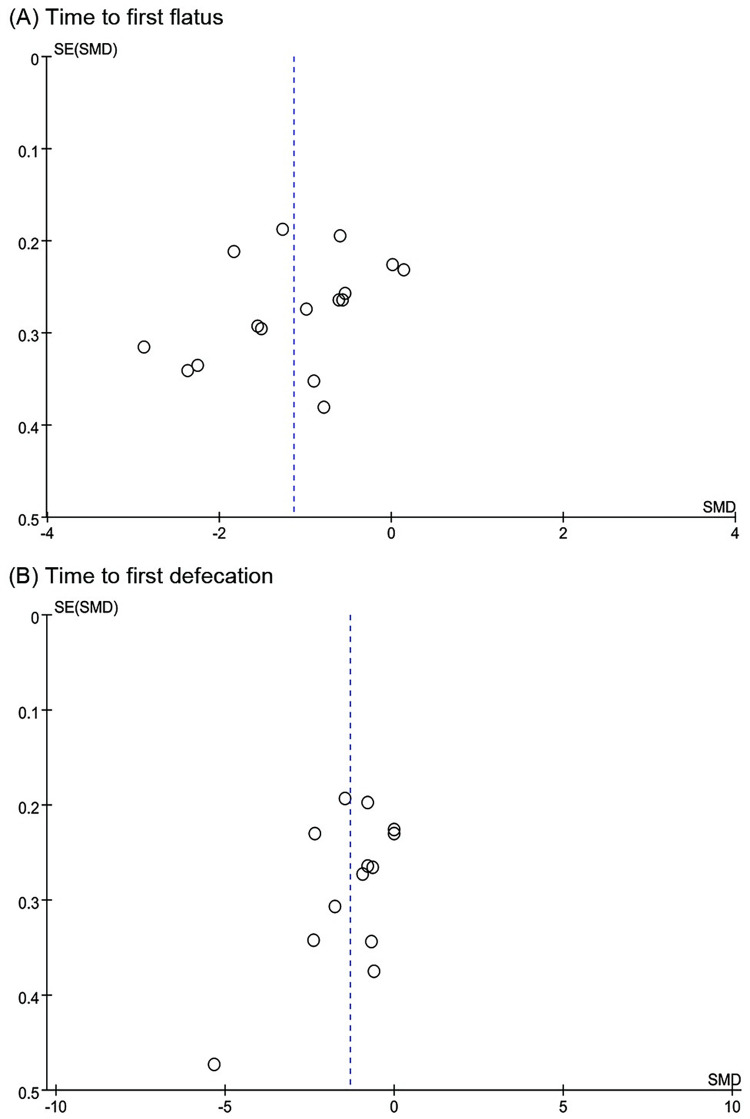
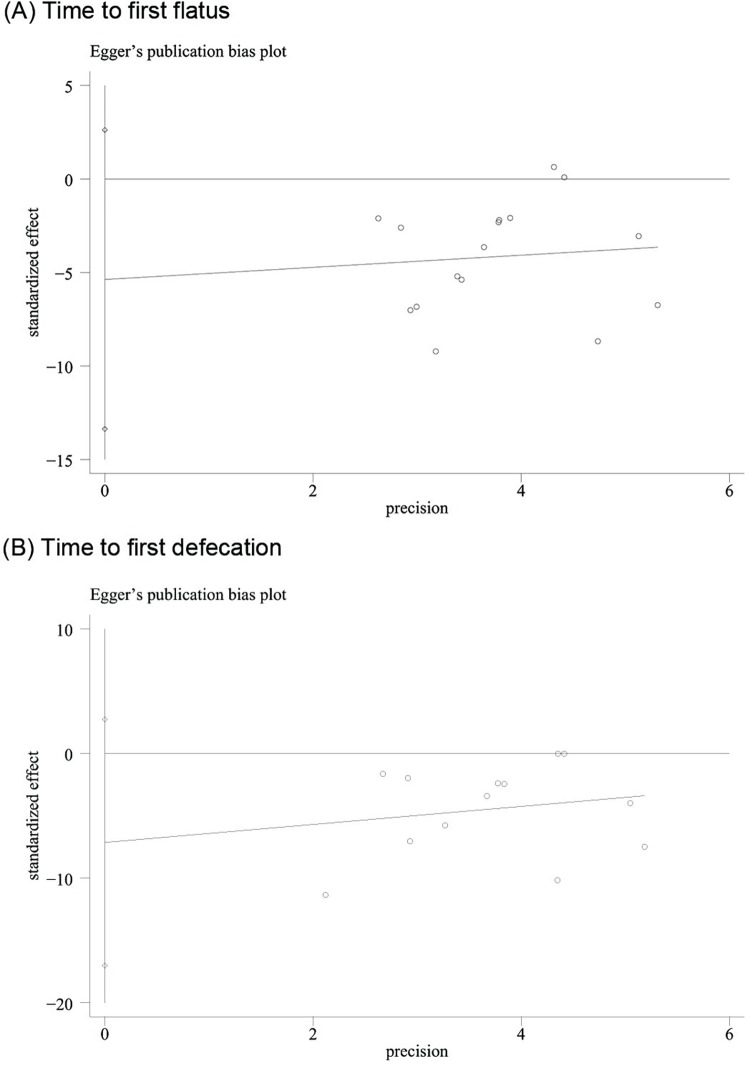
Publication bias
The funnel plot of 15 trials included in the meta-analysis for TFF (Fig 5A) showed that these were approximately symmetric. Additionally, the funnel plot of 12 trials reported for TFD (Fig 5B) showed a similar tendency. Egger’s test demonstrated that there was no obvious publication bias (TFF: P = 0.171; TFD: P = 0.14) (Fig 6).
Fig 5.
Funnel plot of acupuncture versus usual care for (A) Time to first flatus and (B) Time to first defecation.
Fig 6.
Egger’s test of acupuncture versus usual care for (A) Time to first flatus and (B) Time to first defecation.
Level of overall evidence
Table 4 displays a summary of the overall certainty in evidence for the effectiveness of acupuncture on the relevant outcomes. In the comparison of acupuncture with usual care, the evidence indicated with a low level of certainty that acupuncture was associated with reducing TFF, TFD, and TBSR. A moderate level of certainty suggested that acupuncture was associated with reducing LOS as compared with usual care. Certainty in the evidence for the comparison of acupuncture with sham acupuncture was variable in TFF (very low), TFD (low), TBSR (very low), and LOS (low).
Table 4. The overall evidence quality for outcome measure.
| Group | N | Participants | Absolute effect [95%CI] | Certainty assessment | Certainty | Importance | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| I | C | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | |||||
| Acupuncture vs. Usual care | Time to First Flatus | ||||||||||
| 15 | 580 | 582 | SMD-1.14 [-1.54, -0.73] | Seriousa | Seriousa | No | No | No | Low | Critical | |
| Time to First Defecation | |||||||||||
| 12 | 488 | 492 | SMD-1.31 [-1.88, -0.74] | Seriousa | Seriousa | No | No | No | Low | Critical | |
| Time to Bowel Sounds Recovery | |||||||||||
| 10 | 401 | 399 | SMD-1.57 [-2.14, -1.01] | Seriousa | Seriousa | No | No | No | Low | Critical | |
| Length of hospital stay | |||||||||||
| 8 | 303 | 302 | MD-1.68 [-2.55, -0.80] | No | Seriousa | No | No | No | Moderate | Importance | |
| Acupuncture vs. Sham acupuncture | Time to First Flatus | ||||||||||
| 4 | 162 | 164 | SMD-0.81 [-1.40, -0.23] | Seriousa | Seriousa | No | Seriousc | No | Very Low | Critical | |
| Time to First Defecation | |||||||||||
| 3 | 132 | 134 | SMD-0.34 [-0.58, -0.10] | Seriousa | No | No | Seriousc | No | Low | Critical | |
| Time to Bowel Sounds Recovery | |||||||||||
| 3 | 107 | 109 | SMD-1.03 [-1.14, -0.43] | Seriousa | Seriousa | No | Seriousc | No | Very Low | Critical | |
| Length of hospital stay | |||||||||||
| 3 | 104 | 105 | MD-0.99 [-0.26, 0.08] | No | Seriousa | No | Seriousc | No | Low | Importance | |
Abbreviations: N, No. of studies; I, intervention; C, control; CI, confidence interval; MD, mean difference; SMD, standard mean difference.
a. Downgraded due to serious risk of bias: high risk of performance bias and unclear risk of selection bias and detection bias.
b. Downgraded due to substantial heterogeneity.
c. Downgraded due to small sample size.
Discussion
Main findings
This systematic review and meta-analysis aimed to assess the effectiveness and safety of acupuncture for POI among patients undergoing GI surgery. Low to moderate quality of evidence showed that acupuncture could reduce the TFF, TFD, TBSR, and LOS compared with usual care. The subgroup analysis indicated that acupuncture treatment with distal acupoints combination and frequency of 1 session per day had effectiveness in reducing TFF and TFD. The sensitivity analysis and the publication bias supported the stability of the overall effect size. Very low to low-quality evidence suggested that acupuncture had an effect on reducing TFF, TFD, and TBSR compared with sham acupuncture. However, this result should be interpreted with caution since the sensitivity analysis indicated that the result was not stable. Relatively few trials reported information on adverse events from acupuncture; hence, the overall safety should be further validated.
Quality of the evidence
The overall quality of evidence for related outcomes was very low to moderate. In this meta-analysis, the serious risk of bias was the main problem in the included trials. It was mostly related to the deficient report of blinding and uncertainties about the allocation concealment, which have a potential impact on exaggerating the true effect size of acupuncture. Actually, it is challenging to have a low risk of bias in blinding in acupuncture clinical trials. First, it is infeasible to make the acupuncturist blinded to patients due to the nature of acupuncture intervention [51]. Second, participants who have experience with acupuncture are difficult to be blinded due to their general recognition of acupuncture. Therefore, future RCTs should pay more attention to how to make participants not being able to distinguish the real acupuncture from a sham control [52]. Moreover, the allocation concealment should be adequately reported.
Acupoints combination
Based on the theory of traditional Chinese acupuncture, the acupoints combination is the key to ensuring the comprehensive curative effects of acupuncture. Distal–proximal acupoints combination and distal acupoints combination are the two basic methods for combining acupoints. Compared with previous studies, we assessed the effectiveness of acupuncture for POI using the subgroup analysis of the different acupoints combination for the first time in this review. The distal acupoints refer to acupoints distant from the abdomen of the GI district, and proximal acupoints are defined as acupoints on the abdomen closer to the GI district. There were three studies [33, 44, 49] that applied distal–proximal acupoints combination and fifteen studies [34–43, 45–48, 50] that applied distal acupoints combination. In both two types of acupoints combination, ST36 was the main acupoint which located below the knee and on the tibialis anterior muscle. ST36 showed tropism for all GI disorders and had great efficacy in clinical practice, making it one of the master acupoints in Traditional Chinese Medicine [53]. Additionally, most studies on the distal acupoints combination chose lower limb acupoints. There was also one study [40] that combined scalp acupoints with limb acupoints. In the distal–proximal acupoints combination, the proximal acupoints included CV12, CV10, CV6, and CV4, which all were located on the midline of the abdomen.
Surprisingly, we found that acupuncture treatment with distal acupoints combination showed effectiveness in reducing TFF and TFD compared with usual care. However, the distal–proximal acupoints combination showed no statistical difference. Given the potential injuries to the abdomen from GI surgery, one possible reason is that applying acupuncture on proximal acupoints located on the abdomen may cause discomfort to the patient. Furthermore, it may have the risk of infection on the incision site when applying acupuncture on proximal acupoints. Due to the limited number of studies, the effectiveness and safety of the distal–proximal acupoints combination remain to be confirmed. Additionally, which form of acupoints combination is better is also worth studying in the future.
Mechanism of acupuncture
Intestinal manipulation in GI surgery causes autonomic dysfunction, inflammatory activation, agonism at intestinal opioid receptors, modulation of GI hormone activity, and electrolyte derangements [3]. These events lead to significant delays in GI transit and finally result in POI. Acupuncture can directly induce motility acceleration to restore GI transit through the parasympathetic efferent pathway [54, 55]. The main factor responsible for the prolonged dysmotility of the GI tract associated with POI is intestinal inflammation [56]. The recent studies by Yang et al. [57, 58] showed that EA can alleviate intestinal inflammation via activation of the α7nAChR-mediated Janus kinase 2/signal transducer and activator of transcription 3 (JAK2/STAT3) signaling pathway in POI. In addition, several molecules involved in the inflammation, such as nitric oxide (NO), have a direct effect on intestinal contractility. After intestinal manipulation, NO disrupts the generation and propagation of pacemaker potentials by interstitial cells of Cajal (ICC). Deng et al. [59, 60] found that acupuncture can improve postoperative GI motility by facilitating ICC recovery. The potential mechanism may illustrate our findings that acupuncture promotes postoperative intestinal function recovery and reduces POI.
Limitations
There were some unavoidable limitations in this review. First, the population that underwent GI surgery in the included trials was mostly Asians. Therefore, our evidence should be used prudently in other regions and other surgeries. Second, significant heterogeneity was observed when investigating the effect of acupuncture. However, the subgroup analysis did not address the heterogeneity. Considering that GI surgery is highly complex, multiple factors—such as the type of surgical approaches, usual care mode, and anesthesia method—may account for heterogeneity. Third, the safety of acupuncture was not fully evaluated due to the limited number of trials. Last, based on the fact that the purpose of the present study was to assess the effectiveness and safety of acupuncture for POI following GI surgery, we considered only RCTs for inclusion in this review.
RCTs are considered the gold standard of evidence-based medicine for health interventions because they are designed to minimize the risk of bias. A non-randomized controlled trial (NRCT) could not satisfactorily eliminate possible biases due to other factors (apart from treatment), which may affected the results by other confounding factors and may severely compromise the validity of their results [61]. However, the applicability of RCT results is limited due to restrictive selection criteria. In contrast, NRCTs are generally more likely to reflect real-life clinical practice because they have a wider range of participants and longer follow-up. Incorporating data from NRCTs to complement RCTs can generate more comprehensive evidence to guide healthcare decisions [62, 63]. In our future research, we will include data from NRCTs to assess acupuncture from a more pragmatical perspective.
Implications for research
There is a need for large, high-quality, multicenter RCTs to further determine the effectiveness and safety of acupuncture in populations beyond the Asian area. Larger studies may also help identify the clinical difference in GI surgery details.
Given the discrepant results for acupoint combination and frequency of treatment sessions in the subgroup analysis, future studies could focus specifically on the acupuncture therapeutic parameters of acupoints combination, frequency, stimulation and duration to formulate optimal acupuncture treatment scheme for POI following GI surgery. In addition, to better evaluate the safety of acupuncture, the description of acupuncture operation details and adverse events should be clearly reported in future research according to the Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA) guideline [64].
Increased health care costs are associated with prolonged hospital stay in POI patients [9]. Previous study has shown that 1-day earlier hospital time to discharge contributed to potentially beneficial for overall healthcare costs [65]. In this meta-analysis, acupuncture had an advantage in reducing LOS compared with usual care by an average of 1.68 days. It is worth to address whether acupuncture may bring potential economic benefits by reducing LOS in future studies.
Conclusions
In conclusion, the evidence of this systematic review showed that acupuncture has certain effect in reducing TFF, TFD, TBSR and LOS compared to usual care. Acupuncture may be considered as a promising intervention in the management of POI following GI surgery. Taking into consideration of the very low to moderate quality of the overall body of evidence, the findings from this systematic review should be interpreted with caution. High-quality, large-sample, multi-center original studies are needed in the future.
Supporting information
(DOCX)
(DOCX)
(DOCX)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by the 2019 Project of Building Evidence Based Practice Capacity for TCM [2019XZZX-ZJ0011]; the Shanghai Clinical Research Center for Acupuncture and Moxibustion Accelerating [20MC1920500]; the Development of Chinese Medicine Three-Year Action Plan of Shanghai [ZY (2018-2020)-CCCX-2004-04]; the Scientific Research Project of Shanghai Municipal Health Commission [201840011]; the Clinical Key Specialty Construction Foundation of Shanghai [shslczdzk04701]; and the Shanghai Health System Talent Training Program [2018BR24]. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Guyton K, Alverdy JC. The gut microbiota and gastrointestinal surgery. Nat Rev Gastroenterol Hepatol. 2017;14(1):43–54. Epub 2016/11/04. doi: 10.1038/nrgastro.2016.139 . [DOI] [PubMed] [Google Scholar]
- 2.Asgeirsson T, El-Badawi KI, Mahmood A, Barletta J, Luchtefeld M, Senagore AJ. Postoperative ileus: it costs more than you expect. J Am Coll Surg. 2010;210(2):228–231. doi: 10.1016/j.jamcollsurg.2009.09.028 . [DOI] [PubMed] [Google Scholar]
- 3.Vather R, OGrady G, Bissett IP, Dinning PG. Postoperative ileus: mechanisms and future directions for research. Clin Exp Pharmacol Physiol. 2014;41(5):358–370. doi: 10.1111/1440-1681.12220 . [DOI] [PubMed] [Google Scholar]
- 4.Kehlet H. Postoperative ileus. Gut. 2000;47 Suppl 4((Suppl IV)47): iv85–iv6. doi: 10.1136/gut.47.suppl_4.iv85 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Venara A, Neunlist M, Slim K, Barbieux J, Colas PA, Hamy A, et al. Postoperative ileus: Pathophysiology, incidence, and prevention. J Visc Surg. 2016;153(6):439–446. doi: 10.1016/j.jviscsurg.2016.08.010 . [DOI] [PubMed] [Google Scholar]
- 6.Augestad KM, Delaney CP. Postoperative ileus: impact of pharmacological treatment, laparoscopic surgery and enhanced recovery pathways. World J Gastroenterol. 2010;16(17):2067–2074. doi: 10.3748/wjg.v16.i17.2067 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bragg D, El-Sharkawy AM, Psaltis E, Maxwell-Armstrong CA, Lobo DN. Postoperative ileus: Recent developments in pathophysiology and management. Clin Nutr. 2015;34(3):367–376. doi: 10.1016/j.clnu.2015.01.016 . [DOI] [PubMed] [Google Scholar]
- 8.Peters EG, Pattamatta M, Smeets BJJ, Brinkman DJ, Evers S, de Jonge WJ, et al. The clinical and economical impact of postoperative ileus in patients undergoing colorectal surgery. Neurogastroenterol Motil. 2020;32(8): e13862. doi: 10.1111/nmo.13862 . [DOI] [PubMed] [Google Scholar]
- 9.Iyer S, Saunders WB, Stemkowski S. Economic burden of postoperative ileus associated with colectomy in the United States. J Manag Care Pharm. 2009;15(6):485–494. doi: 10.18553/jmcp.2009.15.6.485 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Drake TM, Ward AE. Pharmacological management to prevent ileus in major abdominal surgery: a systematic review and meta-analysis. J Gastrointest Surg. 2016;20(6):1253–1264. doi: 10.1007/s11605-016-3140-0 . [DOI] [PubMed] [Google Scholar]
- 11.Wattchow D, Heitmann P, Smolilo D, Spencer NJ, Parker D, Hibberd T, et al. Postoperative ileus-An ongoing conundrum. Neurogastroenterol Motil. 2021;33(5): e14046. doi: 10.1111/nmo.14046 . [DOI] [PubMed] [Google Scholar]
- 12.Sanfilippo F, Spoletini G. Perspectives on the importance of postoperative ileus. Curr Med Res Opin. 2015;31(4):675–676. doi: 10.1185/03007995.2015.1027184 . [DOI] [PubMed] [Google Scholar]
- 13.Scott MJ, Baldini G, Fearon KC, Feldheiser A, Feldman LS, Gan TJ, et al. Enhanced Recovery After Surgery (ERAS) for gastrointestinal surgery, part 1: pathophysiological considerations. Acta Anaesthesiol Scand. 2015;59(10):1212–1231. doi: 10.1111/aas.12601 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Traut U, Brügger L, Kunz R, Pauli-Magnus C, Haug K, Bucher HC, et al. Systemic prokinetic pharmacologic treatment for postoperative adynamic ileus following abdominal surgery in adults. Cochrane Database Syst Rev. 2008;(1): CD004930. doi: 10.1002/14651858.CD004930.pub3 . [DOI] [PubMed] [Google Scholar]
- 15.Harnsberger CR, Maykel JA, Alavi K. Postoperative Ileus. Clin Colon Rectal Surg. 2019;32(3):166–170. doi: 10.1055/s-0038-1677003 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van Bree SH, Nemethova A, Cailotto C, Gomez-Pinilla PJ, Matteoli G, Boeckxstaens GE. New therapeutic strategies for postoperative ileus. Nat Rev Gastroenterol Hepatol. 2012;9(11):675–683. doi: 10.1038/nrgastro.2012.134 . [DOI] [PubMed] [Google Scholar]
- 17.Chapman SJ, Pericleous A, Downey C, Jayne DG. Postoperative ileus following major colorectal surgery. Br J Surg. 2018;105(7):797–810. doi: 10.1002/bjs.10781 . [DOI] [PubMed] [Google Scholar]
- 18.Kaptchuk TJ. Acupuncture: theory, efficacy, and practice. Ann Intern Med. 2002;136(5):374–383. doi: 10.7326/0003-4819-136-5-200203050-00010 . [DOI] [PubMed] [Google Scholar]
- 19.Ma XP, Hong J, An CP, Zhang D, Huang Y, Wu HG, et al. Acupuncture-moxibustion in treating irritable bowel syndrome: how does it work? World J Gastroenterol. 2014;20(20):6044–6054. doi: 10.3748/wjg.v20.i20.6044 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pei LX, Geng H, Guo J, Yang GH, Wang L, Shen RR, et al. Effect of Acupuncture in Patients With Irritable Bowel Syndrome: A Randomized Controlled Trial. Mayo Clin Proc. 2020;95(8):1671–1683. doi: 10.1016/j.mayocp.2020.01.042 . [DOI] [PubMed] [Google Scholar]
- 21.Wu XF, Li P, Liu L, Chen XL, Yue ZH. A Clinical Randomized Controlled Trial of Acupuncture Treatment of Gastroparesis Using Different Acupoints. Pain Res Manag. 2020;2020:8751958. doi: 10.1155/2020/8751958 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang CP, Kao CH, Chen WK, Lo WY, Hsieh CL. A single-blinded, randomized pilot study evaluating effects of electroacupuncture in diabetic patients with symptoms suggestive of gastroparesis. J Altern Complement Med. 2008;14(7):833–839. doi: 10.1089/acm.2008.0107 . [DOI] [PubMed] [Google Scholar]
- 23.Liu ZS, Yan SY, Wu JN, He LY, Li N, Dong GR, et al. Acupuncture for Chronic Severe Functional Constipation: A Randomized Trial. Ann Intern Med. 2016;165(11):761–769. doi: 10.7326/M15-3118 . [DOI] [PubMed] [Google Scholar]
- 24.Shiotani A, Tatewaki M, Hoshino E, Takahashi T. Effects of electroacupuncture on gastric myoelectrical activity in healthy humans. Neurogastroenterol Motil. 2004;16(3):293–298. doi: 10.1111/j.1365-2982.2004.00504.x . [DOI] [PubMed] [Google Scholar]
- 25.Shin KM, Park JE, Lee S, Choi SM, Ahn YC, Lee JW, et al. Effect of siguan acupuncture on gastrointestinal motility: a randomized, sham-controlled, crossover trial. Evid Based Complement Alternat Med. 2013;2013:918392. doi: 10.1155/2013/918392 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen KB, Huang Y, Jin XL, Chen GF. Electroacupuncture or transcutaneous electroacupuncture for postoperative ileus after abdominal surgery: A systematic review and meta-analysis. Int J Surg. 2019;70:93–101. doi: 10.1016/j.ijsu.2019.08.034 . [DOI] [PubMed] [Google Scholar]
- 27.Liu YH, May BH, Zhang AL, Guo XF, Lu CJ, Xue CC, et al. Acupuncture and Related Therapies for Treatment of Postoperative Ileus in Colorectal Cancer: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Evid Based Complement Alternat Med. 2018;2018:3178472. doi: 10.1155/2018/3178472 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu YH, Dong GT, Ye Y, Zheng JB, Zhang Y, Lin HS, et al. Effectiveness of Acupuncture for Early Recovery of Bowel Function in Cancer: A Systematic Review and Meta-Analysis. Evid Based Complement Alternat Med. 2017;2017:2504021. doi: 10.1155/2017/2504021 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane Handbook for Systematic Reviews of Interventions, version 5.2.0 (updated June 2017). Cochrane. 2017. Available from: http://training.cochrane.org/handbook. [Google Scholar]
- 30.Tugwell P and Tovey D. PRISMA 2020. J Clin Epidemiol. 2021;134: A5–A6. doi: 10.1016/j.jclinepi.2021.04.008 . [DOI] [PubMed] [Google Scholar]
- 31.Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–394. doi: 10.1016/j.jclinepi.2010.04.026 . [DOI] [PubMed] [Google Scholar]
- 32.The Cochrane Collaboration. RevMan 5.4.1. 2020.
- 33.Xu SG, Lu Y, Liu JL, Wu l. Observation on the effect of electroacupuncture on the recovery of gastrointestinal function after appendectomy. Zhong Hua Yi Xue. 2020;12(18):101–102. doi: 10.3969/j.issn.1674-7860.2020.18.040 [DOI] [Google Scholar]
- 34.Pu L, Yin YQ, Wen Y. Effect of electroacupuncture on the gastrointestinal function recovery after abdominal operation: a randomized controlled study. Beng Bu Yi Xue Yuan Xue Bao. 2019;44(5):687–689. doi: 10.13898/j.cnki.issn.1000-2200.2019.05.036 [DOI] [Google Scholar]
- 35.Gu SH, Lang HB, Gan JH, Zheng ZW, Zhao F, Tu Q. Effect of transcutaneous electrical acupoint stimulation on gastrointestinal function recovery after laparoscopic radical gastrectomy–A randomized controlled trial. European Journal of Integrative Medicine. 2019;26:11–17. doi: 10.1016/j.eujim.2019.01.001 [DOI] [Google Scholar]
- 36.Chen KB, Lu YQ, Chen JD, Shi DK, Huang ZH, Zheng YX, et al. Transcutaneous electroacupuncture alleviates postoperative ileus after gastrectomy: A randomized clinical trial. World J Gastrointest Surg. 2018;10(2):13–20. doi: 10.4240/wjgs.v10.i2.13 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yuan L, Guo J, Tang W, Wang J, Fu GQ, Guo F. Effect of transcutaneous electrical acupoint stimulation on gastrointestinal function in perioerative period of laparoscopic intestinal surgery. Lin Chuang Ma Zui Xue Za Zhi. 2017;33(6):567–569. doi: 10.3969/j.issn.1004-5805.2017.06.012 [DOI] [Google Scholar]
- 38.Qian CL, Liu H, Zhang J, Zhang BG, Qiu WJ, Shen ZY, et al. Clinical study on acupuncture at lower he-sea point for promoting functional recovery after stomach cancer surgery. Shang Hai Zhen Jiu Za Zhi. 2017;36(9):1044–1048. doi: 10.13460/j.issn.1005-0957.2017.09.1044 [DOI] [Google Scholar]
- 39.Kang H, Ma X, Sun YH, Sun QQ. Study on electroacupuncture at Zusanli to promote the recovery of Gastrointestinal function after Gastrointestinal Operation in Rapid Rehabilitation surgery. Dang Dai Yi Xue. 2017;23(30):137–139. [Google Scholar]
- 40.Jung SY, Chae HD, Kang UR, Kwak MA, Kim IH. Effect of Acupuncture on Postoperative Ileus after Distal Gastrectomy for Gastric Cancer. J Gastric Cancer. 2017;17(1):11–20. doi: 10.5230/jgc.2017.17.e2 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhang ZD, Wang CS, Li QY, Zhang MY, Zhao HF, Dong LL, et al. Electroacupuncture at ST36 accelerates the recovery of gastrointestinal motility after colorectal surgery: a randomised controlled trial. Acupunct Med. 2014;32(3):223–226. doi: 10.1136/acupmed-2013-010490 . [DOI] [PubMed] [Google Scholar]
- 42.Xiao C. Clinical study on acupuncture promoting the recovery of gastrointestinal function after surgery for colorectal cancer. M.Sc. Thesis, The Hunan University Of Chinese Medicine; 2014.
- 43.Tong WY, A IGL, X L. Effects of acupuncture on gastrointestinal function in postoperative rectal cancer patients. Zhong Yi Yao Dao Bao. 2014;20(12):39–41. doi: 10.13862/j.cnki.cn43-1446/r.2014.12.014 [DOI] [Google Scholar]
- 44.Wang YK. Clinical observation of abdominal acupuncture promoting the recovery of intestinal function in patients with incomplete intestinal obstruction after appendicitis operation. Anhui Zhong Yi Xue Yuan Xue Bao. 2013;32(3). doi: 10.3969/j.issn.1000-2219.2013.03.019 [DOI] [Google Scholar]
- 45.Ng SSM, Leung WW, Mak TWC, Hon SSF, Li JCM, Wong CYN, et al. Electroacupuncture reduces duration of postoperative ileus after laparoscopic surgery for colorectal cancer. Gastroenterology. 2013;144(2):307–313.e1. doi: 10.1053/j.gastro.2012.10.050 [DOI] [PubMed] [Google Scholar]
- 46.Shi JE. The clinical study on the effect of using electro-acupuncture on Zusanli Shangjuxu Xiajuxu postoperative gastrointestinal motility. M.Sc. Thesis, The Guangzhou University of Chinese Medicine. 2012.
- 47.Yang JJ. Researching in the effect of gastrointestinal function in patients with colon cancer resection by electrical acupuncture lower confluent point. M.Sc. Thesis, The Guangzhou University of Chinese Medicine. 2011.
- 48.Wang HM. the effect of acupuncture in promoting postoperative recovery of gastrointestinal function after colorectal carcinoma resection in Fast-Track programme. M.Sc. Thesis, The Nanjing University of Chinese Medicine. 2011.
- 49.Garcia MK, Skibber JM, Rodriguez-Bigas MA, Chang DZ, Feig BW, Bisanz AK, et al. Acupuncture to prevent prolonged postoperative ileus: A randomized controlled trial. Med Acupunct. 2008;20(2):83–88. doi: 10.1089/acu.2008.0607 [DOI] [Google Scholar]
- 50.Meng ZQ, Garcia MK, Chiang JS, Peng HT, Shi YQ, Fu J, et al. Electro-acupuncture to prevent prolonged postoperative ileus: a randomized clinical trial. World J Gastroenterol. 2010;16(1):104–111. doi: 10.3748/wjg.v16.i1.104 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chen H, Yang M, Ning Z, Lam WL, Zhao YK, Yeung WF, et al. A Guideline for Randomized Controlled Trials of Acupuncture. Am J Chin Med. 2019;47(1):1–18. doi: 10.1142/S0192415X19500010 . [DOI] [PubMed] [Google Scholar]
- 52.Hopton AK, Macpherson H. Assessing blinding in randomised controlled trials of acupuncture: challenges and recommendations. Chin J Integr Med. 2011;17(3):173–176. doi: 10.1007/s11655-011-0663-9 . [DOI] [PubMed] [Google Scholar]
- 53.Iwa M, Matsushima M, Nakade Y, Pappas TN, Fujimiya M, Takahashi T. Electroacupuncture at ST-36 accelerates colonic motility and transit in freely moving conscious rats. Am J Physiol Gastrointest Liver Physiol. 2006;290(2): G285–G292. doi: 10.1152/ajpgi.00068.2005 . [DOI] [PubMed] [Google Scholar]
- 54.Okada M, Itoh K, Kitakoji H, Imai K. Mechanism of Electroacupuncture on Postoperative Ileus Induced by Surgical Stress in Rats. Med Acupunct. 2019;31(2):109–115. doi: 10.1089/acu.2018.1322 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fang JF, Fang JQ, Shao XM, Du JY, Liang Y, Wang W, et al. Electroacupuncture treatment partly promotes the recovery time of postoperative ileus by activating the vagus nerve but not regulating local inflammation. Sci Rep. 2017;7:39801. doi: 10.1038/srep39801 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Muller PA, Koscsó B, Rajani GM, Stevanovic K, Berres ML, Hashimoto D, et al. Crosstalk between muscularis macrophages and enteric neurons regulates gastrointestinal motility. Cell. 2014;158(2):300–313. doi: 10.1016/j.cell.2014.04.050 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yang NN, Yang JW, Ye Y, Huang J, Wang L, Wang Y, et al. Electroacupuncture ameliorates intestinal inflammation by activating α7nAChR-mediated JAK2/STAT3 signaling pathway in postoperative ileus. Theranostics. 2021;11(9):4078–4089. doi: 10.7150/thno.52574 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Yang NN, Ye Y, Tian ZX, Ma SM, Zheng Y, Huang J, et al. Effects of electroacupuncture on the intestinal motility and local inflammation are modulated by acupoint selection and stimulation frequency in postoperative ileus mice. Neurogastroenterol Motil. 2020;32(5): e13808. doi: 10.1111/nmo.13808 . [DOI] [PubMed] [Google Scholar]
- 59.Deng JJ, Yang S, Yuan Q, Chen YZ, Li DD, Sun HM, et al. Acupuncture Ameliorates Postoperative Ileus via IL-6-miR-19a-KIT Axis to Protect Interstitial Cells of Cajal. Am J Chin Med. 2017;45(4):737–755. doi: 10.1142/S0192415X17500392 . [DOI] [PubMed] [Google Scholar]
- 60.Deng JJ, Lai MY, Tan XH, Yuan Q. Acupuncture protects the interstitial cells of Cajal by regulating miR-222 in a rat model of post-operative ileus. Acupunct Med. 2019;37(2):125–132. doi: 10.1177/0964528419829755 . [DOI] [PubMed] [Google Scholar]
- 61.Altman DG, Bland JM. Statistics notes. Treatment allocation in controlled trials: why randomise? BMJ. 1999; 318(7192):1209. doi: 10.1136/bmj.318.7192.1209 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Faber T, Ravaud P, Riveros C, Perrodeau E, Dechartres A. Meta-analyses including non-randomized studies of therapeutic interventions: a methodological review. BMC Med Res Methodol. 2016;16:35. doi: 10.1186/s12874-016-0136-0 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sarri G, Patorno E, Yuan HB, Guo JJ, Bennett D, Wen XR, et al. Framework for the synthesis of non-randomised studies and randomised controlled trials: a guidance on conducting a systematic review and meta-analysis for healthcare decision making. BMJ Evid Based Med. 2022;27(2):109–119. doi: 10.1136/bmjebm-2020-111493 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.MacPherson H, Altman DG, Hammerschlag R, Youping L, Taixiang W, White A, et al. Revised STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): extending the CONSORT statement. PLoS Med. 2010;7(6): e1000261. doi: 10.1371/journal.pmed.1000261 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wolff BG, Michelassi F, Gerkin TM, Techner L, Gabriel K, Du W, et al. Alvimopan, a novel, peripherally acting mu opioid antagonist: results of a multicenter, randomized, double-blind, placebo-controlled, phase III trial of major abdominal surgery and postoperative ileus. Ann Surg. 2004;240(4):728–734; discussion 34–5. doi: 10.1097/01.sla.0000141158.27977.66 . [DOI] [PMC free article] [PubMed] [Google Scholar]