Abstract
Aims and objectives
Overall, this study aimed to describe nursing care for patients with dementia in acute hospitals, with the objectives of describing the provided nursing care (a), nurses’ attitudes and perceptions in caring for patients with dementia (b), and exploring how nurses deal with challenging behaviour (c). Additionally, we determined background variables associated with caring for people with dementia.
Background
Due to comorbidities, people with dementia are frequently admitted to acute care hospitals. Here, they are at high risk of complications. Nurses strive for good care but regularly experience insufficient knowledge and skills regarding caring for people with dementia.
Design
A cross‐sectional survey study design.
Methods
Data were collected in seven Dutch acute hospitals and through social media. In total, 229 hospital nurses completed the questionnaire. We used the Geriatric In‐Hospital Nursing Care Questionnaire and two subscales of Hynninen on managing challenging behaviour. This report followed the STROBE checklist.
Results
Nurses express that they often apply general preventive interventions not explicitly related to dementia care. In general, nurses have mixed feelings about the nursing care provided in their department. For challenging behaviour, a variety of approaches, including restrictive measures and medication, is applied. The nurses’ attitudes and perceptions are influenced by the type of hospital where the nurses work, the level of education, the number of hours nurses work, and if the nurses completed a course on dementia in the last year.
Conclusions
Despite a positive attitude, nurses do not have the specific knowledge and skills needed to provide proper care. Nurses who recently completed a course on dementia had more positive attitudes and perceptions towards caring for patients with dementia.
Relevance to clinical practice
The results of this research can be used to improve the quality of nursing care for patients with dementia in acute hospitals.
Keywords: acute care, attitude, challenging behaviour, dementia, experiences, hospitals, nursing care
What does the paper contribute to the global clinical community?
This quantitative study confirms results from earlier qualitative studies, namely, nurses strive to provide proper care but have insufficient knowledge about caring for patients with dementia. The attitudes towards and perceptions of caring for patients with dementia in acute hospitals can be improved.
A quantitative approach to a relevant topic makes international comparisons possible.
The attitudes and perceptions of nurses are influenced by the type of hospital where nurses work, the level of education, the number of hours nurses work in the ward and if they completed a course on dementia in the last year.
1. INTRODUCTION
Worldwide, approximately 50 million, mostly older people, have dementia. Annually, this number increases by 10 million (World Health Organization, 2019). In the Netherlands, over 280,000 people are currently living with dementia (Alzheimer Nederland, 2019). People with dementia are regularly hospitalised, not for their dementia but because of, for example, fractures, chronic diseases or infections, such as respiratory, urinary or gastrointestinal infections (Toot, Devine, Akporobaro, & Orrell, 2013). On average, people with dementia have three or more physical illnesses (Mukaetova‐Ladinska, Teodorczuk, & Cerejeira, 2009). The national average percentage of people with dementia admitted to the hospital in 2017 is 25.3%, compared to 17% in a comparable group without dementia (Vektis, 2019). The exact percentage of patients with dementia in hospitals is unknown. An estimate is that people with dementia occupy approximately one‐quarter of hospital beds (Brooker, Milosevic, Evans, Bruce, & Thompson, 2014; Feast, White, Candy, Kupeli, & Sampson, 2020). People with dementia have an increased risk of complications during their hospital stay, caused by infections, a decline in functional and nutritional status, and incontinence, and the result is an unwanted longer hospital stay (Fogg, Griffiths, Meredith, & Bridges, 2018; Möllers, Stocker, Wei, Perna, & Brenner, 2019). In addition to the variety of comorbidities of people with dementia, nurses often have to manage patients’ challenging behaviour, such as aggression, agitation, resistance to care or wandering (Dewing & Dijk, 2016; Evripidou, Charalambous, Middleton, & Papastavrou, 2019).
2. BACKGROUND
The focus in acute hospitals is primarily on physical care and meeting medical targets, whereby nurses experience time pressures and staff shortages (Reilly & Houghton, 2019). The individual care needs of people with dementia are not always recognised and understood by nurses (Dewing & Dijk, 2016).
Earlier studies show that nurses tend to avoid caring for patients with dementia, especially when they exhibit challenging behaviour (Clissett, Porock, Harwood, & Gladman, 2014; Hynninen, Saarnio, & Isola, 2016). Also, nurses experience difficulties in dealing with and caring for the family of these patients (Ernst, Petry, Luethi, & Naef, 2019). Especially for patients with dementia, care must be adapted to their specific needs (Feast et al., 2020). The nurses’ attitude towards dementia affects their provision of care and the amount and type of physical restraints and restrictive medical measures they apply (Dewing & Dijk, 2016). Nursing care is related to patient safety and quality of care, and an assumption is that there is also a strong relationship between the provided care, nurses’ attitudes on and perceptions of dementia and nursing outcomes (Persoon, Bakker, van der Wal‐Huisman, & Olde Rikkert, 2015).
Nurses experience deficits in their knowledge, skills and attitudes regarding the specific care needs of patients with dementia, and managing challenging behaviour is an issue (Turner, Eccles, Elvish, Simpson, & Keady, 2017). Most studies on care for patients with dementia in an acute hospital setting have used a qualitative perspective as shown in recent reviews (Digby, Lee, & Williams, 2016; Evripidou et al., 2019), or focus on a specific part of the nursing care, like orthopaedic care (Jensen, Pedersen, Wilson, Bang Olsen, & Hounsgaard, 2019). In addition, it is unknown if acute hospital type, the experience of nurses, their level of education, courses and the number of hours that nurses work on the ward influence the quality of care for patients with dementia, the nurses’ attitudes towards caring for patients with dementia and their perceptions of this care. This knowledge gap also accounts for the Dutch acute hospitals setting.
Therefore, in this paper we aim to describe the results of a quantitative study about nursing care for patients with dementia in acute hospital settings, nurses’ attitudes towards caring for patients with dementia and their perceptions of this care; additionally, we gain insights into how nurses manage challenging behaviour of hospitalised patients with dementia. Finally, a number of variables influencing caring for patients with dementia are measured.
3. METHODS
3.1. Design
A cross‐sectional survey study design was applied. During June 2018 and July 2019, data collection took place in seven acute care hospitals in the northern region of the Netherlands: one university hospital, three nonuniversity teaching hospitals and three general hospitals. The hospitals' sizes varied from 263 beds–542 beds, and the university hospital had 1,300 beds. An online questionnaire, including all relevant information, was distributed through contact persons who sent this questionnaire to department managers. The survey was also nationally distributed through Facebook because of its widespread use among nurses. We did a call on a national private nursing group for questionnaires of a professional nursing magazine and on an open group for nurses in general. After 3 weeks, a reminder was sent. On Facebook, a request was performed and repeated once after 1 week. Because the hospitals participated at different times, nurses had the opportunity to participate throughout the entire investigation period. The hospital sampling was based on convenience, and social media sampling was based on self‐selection.
We included all nurses directly caring for patients with dementia in a hospital, with at least 3 months of experience as a nurse, and a willingness to participate. All types of wards were included, except for paediatrics and obstetrics. QualtricsXM (version 2018) was used as an online survey tool for distribution. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement has been applied for the current article (von Elm et al., 2008).
3.2. Data sources
To assess the provided nursing care, nurses’ attitudes towards and perceptions of nursing care for patients with dementia in acute hospitals, we combined two validated questionnaires. The questionnaire was based on the Dutch Geriatric In‐Hospital Nursing Care Questionnaire (GerINCQ; Persoon et al., 2015). This instrument measures the performed nursing care of older patients, nurses’ attitudes towards this care and the perception of caring for older patients in an acute hospital setting from the perspective of nurses. The internal consistency was α = 0.86. The GerINCQ had five subscales with 67 items and two additional open questions. The five subscales were performed intervention, α = 0.72 (13 items); ageing‐sensitive care, α = 0.88 (13 items); professional responsibility, α = 0.89 (12 items); attitudes towards caring for older patients, α = 0.64 (14 items); and perceptions of caring for older patients, α = 0.67 (18 items; Persoon et al., 2015). The content validity of the instrument is high (Persoon et al., 2015). The original questionnaire addressed nursing care for older patients in acute hospitals. Because we focused on older patients with dementia, the original term “older patients” was altered to “patients with dementia” in consultation with the authors. Following the recommendation of the authors, the original 5‐point Likert scale was changed into a 4‐point Likert scale (Persoon et al., 2015). Based on the literature, one question was added on “disruptive behaviour to other patients” to the subscale perception (Featherstone, Northcott, Harden, et al., 2019; Hunter et al., 2013).
To gain more insight into how nurses manage challenging behaviour, we simultaneously took two validated subscales of the questionnaire of Hynninen et al. (2016). These were developed to describe care practices of older patients with dementia: managing challenging behaviour (11 items) and u se of alternative approaches instead of physical restraints (nine items; Hynninen et al., 2016). These subscales provided a satisfactory impression of the possible reactions of nurses in managing challenging behaviour. The reliability of these subscales was respectively 0.63 and 0.77 (Hynninen et al., 2016). In order to compare the results of both questionnaires, it was decided to adjust these scales to a 4‐point Likert scale as well.
For the translation of the subscales of Hynninen, we performed the forward–backward translation of the English version by two independent translators from a certified translation agency. The translations were independently assessed by two researchers (AK and EF) to determine the optimal translation of the question formulations and the answer options (Maneesriwongul & Dixon, 2004). There were no differences of opinion on a linguistic or cultural basis. The final selection of all items was made unanimously.
Finally, we added relevant background variables such as the level of education, experiences, skills, working hours per week and completed courses on dementia in the last year. A small pilot (n = 10) was done. Based on the pilot, the duration of filling in the questionnaire was estimated, and the introduction was clarified.
To prevent bias, we emphasised that there were no right or wrong answers. In addition, we used different orders per questionnaire to increase the chance of fully completed surveys and to prevent the last part from being filled in the least accurately.
3.3. Measurement
3.3.1. Analyses
To measure nursing care, we used the subscales performed interventions and dementia‐sensitive care (Persoon et al., 2015). These subscales measure on a team level to what extent nurses use physical and geriatric care‐related interventions in the care for older patients with dementia and how satisfied nurses are with dementia‐sensitive, psychosocial‐related, geriatric care delivery in their department.
Attitude and perception were measured by the use of the subscales professional responsibility, attitudes towards caring for older patients and perceptions of caring for older patients. Regarding their attitude, nurses were asked about how responsible nurses feel for diverse aspects of nursing care, such as the development of complications and miscommunication. They were also questioned on their daily experience of dementia care‐related items, for example, involvement and admission. Finally, to evaluate the perception of nurses, different items were used on the experience of dementia‐related care for patients with dementia and the experience of disruptive behaviour. In the open questions nurses were able to indicate what they find demanding in the care of patients with dementia and what training their department needs (Persoon et al., 2015).
Additionally, the subscales reactions to challenging behaviour and the use of alternative approaches instead of physical restraints were applied (Hynninen et al., 2016). Nurses were asked how often they use different types of responses when a patient displays challenging behaviour and which alternative approaches they use instead of physical restraints.
Data were analysed using the IBM SPSS statistics (version 25). Only the data of complete questionnaires were included in the study. We started with descriptive analyses of the background characteristics of the nurses. Item performance was applied by item means, Cronbach's alpha if item deleted, and percentage per answer (Appendix 1). There were no indications that would lead to adjustments to the scale. We continued with performing Cronbach's alpha of the total scale and the subscales to evaluate the internal consistency and calculating means with confidence intervals. In order to compare the outcomes of the subscales, we rescaled the outcomes of each subscale total by dividing the number of variables, which led to new outcomes on a scale from one to five. Spearman's rho was used to analyse if there were significant (p < .01) correlations between the subscales and background variables, and the items and background variables. Finally, the two open questions were briefly analysed by thematic analysis by atlas.ti computer software (version 7.5; Atlas.ti Scientific Software Development GmbH) to get more insight into the data. Inductively, the answers were coded, clustered in themes and iteratively refined by two researchers.
3.4. Ethical considerations
The study was performed following the Helsinki declaration, and all the participants provided digitally informed consent before filling out the questionnaire. The regional Medical Ethical Committee considered approval unnecessary (decision M17.221048) because the questionnaire was intended for staff. Permission to access staff was given in participating hospitals. The response was utterly anonymous. No one could be identified based on the results.
4. RESULTS
4.1. Participants and descriptive data
We received 429 questionnaires from hospital nurses and 113 from nurses through social media (total n = 542). Of this, 229 nurses (=42%) completed the questionnaire. The average time to complete the questionnaires was 15 min. The response rate based over five hospitals is 29%, for the two other hospitals, it was not clear how many nurses received the survey. The length of the questionnaire and the lack of affinity with the target group were the main reasons for not completing it. The distribution of nurses between the university hospital, nonuniversity teaching hospitals and general hospitals was evenly spread. Some ward managers sent it to all the nurses, and some decided to send it to a few nurses in their ward. The participating number of wards per hospital varied from one to four.
An overview of the characteristics of the nurses is presented in Table 1. A small percentage of nurses work in other hospitals types, for example private hospitals. In practice, most nurses work on combined wards such as medical‐geriatric, medical‐surgical or intensive care. For this reason, this ward variable was an unsuitable background variable in the analyses. Almost half of the nurses were educated at a secondary vocational level, and a similar portion had a bachelor's degree. However, in the Netherlands, nurses are educated on two different levels, vocational level and on bachelor level. In practice, they perform the same tasks. Although we report the highest completed education, the respondents were able to fill in all completed education in the questionnaire. This shows that some nurses worked with older people as a care assistant before they became a nurse. The experience of nurses was evenly spread between the groups. In all, 61.1% of the nurses worked more than 24 hr per week, of which only 9% of the nurses worked more than 33 hr per week. The group of nurses who participated via social media is comparable to the group from the northern hospitals. The nurses graded their skills in caring for patients with dementia at on average 7.2 on a scale from 1 to 10, with a range of 3 to 10. In all, 62.5% of the participating nurses completed a course on caring for patients with dementia the past year.
Table 1.
Characteristics of the nurses (n = 229)
| Characteristics of the nurses | n | % |
|---|---|---|
| Hospitalsa | ||
| University | 50 | 21.8 |
| Nonuniversity teaching hospital (top‐clinical) | 60 | 26.2 |
| General | 99 | 43.2 |
| Other | 23 | 8.7 |
| Ward type | ||
| Medical | 38 | 16.8 |
| Surgical | 66 | 29.2 |
| Geriatric | 20 | 8.8 |
| Other | 102 | 45.1 |
| Level of education (n = 218)a | ||
| Nursing student | 4 | 1.8 |
| Secondary vocational level 4 | 109 | 48.9 |
| Bachelor level | 105 | 47.1 |
| Master level | 5 | 2.2 |
| Experience nurse (n = 223)a | ||
| ≤5 years | 115 | 51.6 |
| 6–10 years | 36 | 16.1 |
| 11–20 years | 14 | 6.3 |
| 21–30 years | 33 | 14.8 |
| 31 years or more | 25 | 11.2 |
| Experience current hospital (n = 223) | ||
| ≤5 | 167 | 73.9 |
| 6–10 | 26 | 11.5 |
| 11–20 | 13 | 5.8 |
| 21–30 | 13 | 5.8 |
| ≥31 | 7 | 3.1 |
| Experience current ward (n = 226) | ||
| ≤5 years | 183 | 81.0 |
| 6–10 years | 16 | 7.1 |
| 11–20 years | 19 | 8.4 |
| 21–30 years | 7 | 3.1 |
| ≥31 years | 1 | 0.4 |
| Experience working with older people (n = 226) | ||
| ≤5 | 57 | 25.2 |
| 6–10 | 43 | 19.0 |
| 11–20 | 48 | 21.2 |
| 21–30 | 46 | 20.4 |
| ≥31 | 32 | 14.2 |
| Hours per weeka | ||
| Flexible | 2 | 0.9 |
| ≤16 | 9 | 4.0 |
| 17–24 | 79 | 35 |
| 25–32 | 116 | 51.3 |
| ≥33 | 20 | 8.8 |
| Grade skills (n = 221) | Mean (range) 7.2 (3–10) | |
| Course on dementia in the last year (n = 226)a | ||
| Yes | 144 | 63.7 |
| No | 82 | 36.3 |
n = Number of participants, if different.
Variables used for correlation with subscales.
4.2. Reliability
The internal reliability of the GerINCQ (0.83) was good, as measured by Cronbach's alpha (Field, 2013). The reliability of the subscales varied between 0.62 and 0.86, as shown in Table 2. The Cronbach's alphas of the GerINCQ and the subscales we found are comparable, although the Cronbach's alphas of the subscales attitude and perception are lower than the desired 0.7. The Cronbach's alphas of the subscales of Hynninen were lower than in the original study. The reliability of the scale about reactions on challenging behaviour was already low, but the scale about the use of alternative approaches was 0.17 lower and changed from good to poor (Nunnally, 1978).
Table 2.
Overview psychometric properties of the GerINCQ and Hynninen per subscale
| Subscale | Questionnaire | Item mean | 95% Confidence interval | Cronbach's alpha | 95% Confidence interval | ||
|---|---|---|---|---|---|---|---|
| Lower | Upper | Lower | Upper | ||||
| Performed interventions | GerINCQ | 3.46 | 2.81 | 2.89 | 0.69 | 0.62 | 0.74 |
| Dementia‐sensitive care delivery | GerINCQ | 3.29 | 2.82 | 2.90 | 0.84 | 0.81 | 0.87 |
| Professional responsibility | GerINCQ | 3.11 | 3.06 | 3.17 | 0.89 | 0.86 | 0.91 |
| Attitude towards caring for patients with dementia | GerINCQ | 3.12 | 3.08 | 3.15 | 0.71 | 0.66 | 0.77 |
| Perceptions of caring for patients with dementia | GerINCQ | 2.64 | 2.61 | 2.67 | 0.62 | 0.55 | 0.69 |
| Reaction when a patient with dementia displays challenging behaviour | Hynninen | 2.71 | 2.68 | 2.74 | 0.51 | 0.41 | 0.60 |
| Use of alternative approaches instead of physical restraints | Hynninen | 3.10 | 3.07 | 3.14 | 0.60 | 0.51 | 0.67 |
4.3. Nursing care, attitudes, perceptions and managing challenging behaviour
As shown in Table 2, the item means vary from 2.64 to 3.46, and the weighted means from 2.71 to 3.11. The data are summarised in a box‐and‐whisker plot, as presented in Figure 1. Concerning the overall median, five of the seven measured subscales have a median above the mean. The subscale responsibility has the most extensive spread and the subscale reactions the smallest. The results of the single item analysis are shown in Appendix 1.
Figure 1.
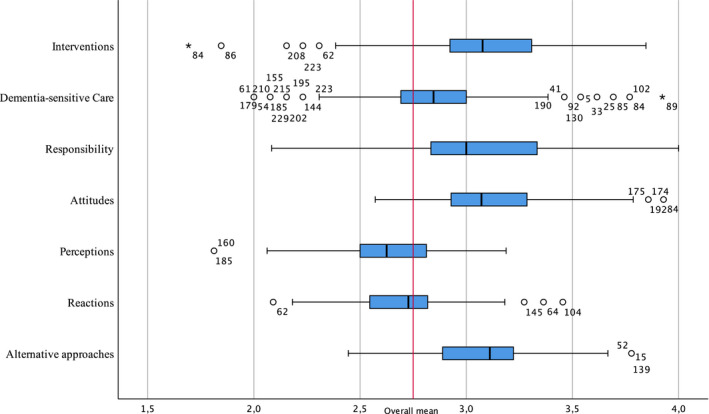
Box‐and‐whiskers plots [Colour figure can be viewed at wileyonlinelibrary.com]
4.4. Nursing care
As shown in Table 2, the mean score of the subscale Performed interventions is 3.46. A comparison of this score is difficult because the original study used a 5‐point Likert scale (Persoon et al., 2015). There, the average score varied between 3.2 and 3.4. Most nurses (n = 192) perceive that in the last 12 months, less than half of the percentage of the patients they care for were patients with dementia. In addition, two‐thirds of the nurses (n = 148) assert that the proportion of their shift that they devote to care for patients with dementia is less than half.
To gain insight into the meaning of the result of the subscale, outcomes at a single item level are relevant. The most performed interventions are the following: interventions to prevent pressure ulcers (n = 219), prevent a delirium (n = 217) and prevent a fall (n = 220). The lowest score of enteral nutrition as an intervention to prevent malnutrition, with a mean of 1.94, stands out here. This means that nurses mention rarely or never perform enteral nutrition as an intervention to prevent malnutrition (n = 200). Another rarely used intervention is the use of physical movement‐restrictive measures (n = 160).
Because the focus of our study is dementia care, we are specifically interested in dementia‐related interventions. More than half of the nurses (n = 142) imply that they never or rarely organise activities for patients with dementia, as an intervention to prevent delirium. Additionally, nearly half of the nurses (n = 113) indicate that they often use urinary catheters. Concerning the use of restrictive measurements, nearly two‐thirds of the nurses state that they often or always use restrictive medical measures (n = 161) and sleep medication (n = 135). Almost one‐third (n = 69) of the nurses point out that they almost or often use physical movement restrictions, despite the risks of these interventions.
In general, the participating nurses are satisfied with the dementia‐sensitiveness of care provided in their department. The average score on this subscale is 3.29 (Table 2). The original study reported a score varying between 3.1 and 3.6 on a 5‐point Likert scale (Persoon et al., 2015). Nurses state that they are most satisfied with how often patients with dementia are treated with respect (n = 222). The points with which nurses are less satisfied concern the adjustment of the care activities to the pace to patients with dementia in their department (n = 119) and more than half of the nurses (n = 116) are discontented with how the presence of patients with dementia is considered in the planning of the shifts, for example, when determining the number of nurses needed for a shift or when dividing the care among the nursing staff.
4.5. Attitude and perception
As presented in Table 2, the mean score of Professional Responsibility is 3.11. The interpretation on single item level shows that the score differs from 2.61 to 3.33. Nurses feel most responsible for the development of pressure ulcers (n = 218) and arranging the discharge (n = 218) of patients with dementia. Nurses feel least responsible for behavioural problems (n = 100), urinary tract infections (n = 64) and development of delirium (n = 68) in patients with dementia.
The mean score of the subscale attitudes (Table 2) is 3.12. The means of the single item scores vary between 2.63 and 3.52. Nurses often or always create optimum communication conditions (n = 228) and keep a close eye on confused patients with dementia (n = 228). The lowest scores show that around a quarter of the participating nurses indicate they rarely or never allow more time for starting discharge planning at admission (n = 94), allow more time for preparing the discharge (n = 89) and allowing extra time for the admission (n = 85).
The mean score of the item perception is 2.64. The items with the highest mean concern the perception of negative behaviour like the experience that patients are restless at night (n = 212) and demand much attention (n = 195). Also, nurses indicate feeling sufficiently or very proficient (n = 201) in providing care for patients with dementia. The lowest scores are related to the experience of the proportion of patientswith dementia. Most nurses (n = 192) experience that the proportion of patients with dementia in the past year was less than half. Furthermore, most nurses (n = 158) experience that they spend less than half of their time caring for people with dementia. The mean of the item about how nurses experience training is also low. More than half of the nurses (n = 115) feel that they have had insufficient training to provide adequate nursing care to patients with dementia.
4.6. What makes the care for patients with dementia demanding (qualitative)
As described, more than half of the nurses frequently experience caring for patients with dementia as demanding. Nurses were asked to explain what they find demanding in the care for patients with dementia. Nurses express a broad range of situations concerning the organisation of care, professional aspects and aspects of the disease.
Insufficient time is mentioned as an essential factor in what makes the care for patients with dementia demanding. This insufficient time is related to the perceived high workload but also to the perceived complexity of care because of dementia, the combination of care for other patients, the presence and absence of informal carers and the availability of volunteers.
It takes time and patience from a nurse to provide the care they deserve to a confused patient or patient with dementia. This means that time is often too short for the other duties of the nurse.
Nurses indicate that they are dissatisfied with the lack of opportunities for proper care, to pay attention to patients, for adequate monitoring of patients. Additionally, a small number of nurses say that they do not have an affinity with the target group, are not interested in patients with dementia or, even stronger, believe that patients with dementia should not be admitted to their ward.
Our department is not suitable for patients with dementia.
Finally, the responding nurses indicate that the unpredictable behaviour of patients with dementia is stressful, as are restless behaviour, aggression, wandering and disorientation. The nurses are concerned about possible complications such as falls, malnutrition because the patient does not want to eat, and delirium and safety, for example, when wandering.
Care must be taken that they do not fall (…) and do not wander around and bother other patients, start shouting about the ward because they do not know how the bell works and, as a result, make other patients restless.
4.7. Needs regarding training (qualitative)
Nurses were asked to describe their needs regarding training. These needs are partly disease‐focused, and partly nursing care focused. Nurses express that they want knowledge of dementia, delirium and depression, gerontology, geriatrics, medication in general and specifically about problem behaviour.
Repetition of which medication to give the best, and practical tips that patients also take this.
In addition, nurses mention that they want to learn how to manage dementia, particularly with problem behaviour such as wandering and aggression. They state they require more knowledge of restrictive measures and interventions aimed at safety.
Managing different types of dementia, freedom restrictive measures (which exist and how to use them). There are several restrictive measures, but these are not always used in a timely and effective matter.
4.8. Managing challenging behaviour
The mean score on this subscale is 2.71 (Table 2). The means per factor scores (subscales) are presented in Table 3. The means vary from 1.41 on the subscale react by ignoring to 3.30 on react with care. Nurses use various ways to respond to challenging behaviour.
Table 3.
Means per subscale of responses managing challenging behaviour (n = 229)
| Reaction when a patient with dementia displays challenging behaviour | Use of alternative approaches instead of physical restraints | ||||||
|---|---|---|---|---|---|---|---|
| F1 react with care | F2 react by ignoring | F3 reaction with power | F4 react casually | F1 use of professional knowledge | F2 use of medication | F3 use of problem‐solving | |
| Mean | 3.30 | 1.41 | 2.63 | 2.98 | 3.25 | 2.65 | 3.19 |
| Std. error of mean | 0.02 | 0.03 | 0.03 | 0.03 | 0.02 | 0.03 | 0.03 |
| Median | 3.25 | 1.50 | 2.67 | 3.00 | 3.20 | 2.50 | 3.00 |
| Std. deviation | 0.35 | 0.44 | 0.40 | 0.40 | 0.33 | 0.45 | 0.38 |
| Minimum | 2.50 | 1.00 | 1.67 | 2.00 | 2.20 | 1.00 | 2.50 |
| maximum | 4.00 | 3.00 | 3.67 | 4.00 | 4.00 | 4.00 | 4.00 |
The mean of the factor react with care is the highest, at 3.30. Nurses react, for example, by being present, asking what is wrong and organise activities. Nurse state that they rarely react by ignoring this factor has the lowest mean score of 1.41. The factor possible reactions with power has a mean of 2.63. This factor describes how often nurses state that they use physical force to calm the situation or take the patient to his or her room and give orders to the patient. The factor react casually to challenging behaviour, has a mean of 2.98, this is applied when nurses use humour or tolerate the challenging behaviour because the patient has the right to be angry.
The mean score on the scale of the use of alternative approaches is 3.10 (Table 2). Nurses use different approaches as an alternative approach to physical restraints. As shown in Table 3, the factor with the highest score is the use of professional knowledge, with a mean of 3.25. Nurses indicate that they regularly negotiate with colleagues or family about the best way to respond. Regarding the use of medication, the mean score is 2.65. This factor describes how often nurses point out that they provide painkillers or sedative medication as a reaction to challenging behaviour. Finally, the mean of the factor use problem‐solving is 3.19. This factor describes techniques such as distracting the patient's attention and attempt to organise an expert consultation, for example, a clinically geriatric.
4.9. Associations between background variables and items
The correlations between the background variables and the subscales and between the background variables and the items were computed. Statistically significant relationships are reported (Table 4). We expected that experience would correlate with the items. However, we found no statistically significant relations. We only found correlations with items about attitudes and perceptions.
Table 4.
Significant (p < .01) correlations between subscales and background variables, and items and background variables (n = 229)
| Subscale/item | Hospital | Education | Hours | Course | |
|---|---|---|---|---|---|
| Subscale attitudes | Rho | −0.230 | |||
| p value | 0.001 | ||||
| Items | |||||
| Behavioural problems in a patient with dementia? | Rho | −0.205 | −0.204 | 0.184 | |
| p value | 0.002 | 0.002 | 0.005 | ||
| Development of delirium in patients with dementia? | Rho | 0.171 | |||
| p value | 0.010 | ||||
| I create optimum communication conditions for patients with dementia by making use, for example, of the patient's glasses or hearing aid | Rho | 0.171 | |||
| p value | 0.010 | ||||
| I allow more time for preparing the discharge of patients with dementia than I do for the discharge of an older patient without dementia | Rho | 0.187 | |||
| p value | 0.005 | ||||
| Subscale perception | Rho | −0.185 | |||
| p value | 0.005 | ||||
| Items | |||||
| In the past 12 months, which proportion of the patients you cared for were patients with dementia? | Rho | −0.229 | 0.178 | ||
| p value | 0.000 | 0.007 | |||
| Roughly what proportion of your shift do you devote to the care of patients with dementia in your department? | Rho | −0.208 | |||
| p value | 0.002 | ||||
| How proficient do you think you are in providing care for patients with dementia? | Rho | −0.201 | −0.187 | 0.223 | |
| p value | 0.002 | 0.005 | 0.001 | ||
| To what extent do you feel recognised by your colleagues for your care of patients with dementia? | Rho | −0.222 | 0.174 | ||
| p value | 0.001 | 0.009 | |||
| How do you experience the training of nurses in the provision of care to patients with dementia in your department? | Rho | −0.233 | 0.176 | ||
| p value | 0.000 | 0.008 | |||
Hospital Type: 1 = university, 2 = nonuniversity teaching hospital, 3 = general hospital.
Education: Level of education 1 = nursing student, 2 = secondary vocational level 4, 3 = bachelor level, 4 = master level.
Hours: Hours per week.
Course on dementia: 1 = no, 2 = yes.
At scale level, we found a positive correlation between the subscale attitudes towards caring for people with dementia if nurses followed a course of dementia last year. Taking a course on dementia could lead to a better attitude in the care of patients with dementia. We found a negative correlation between the subscale perceptions of caring for patients with dementia and the hospital type. In order to understand these outcomes, the outcomes at item level are relevant.
We found negative correlations between some items and the type of hospital, the level of education and the number of hours nurses work in the ward. The participating nurses working in university hospitals spend a lower proportion of their shift on patients with dementia, and they feel less competent. These nurses consider the training for dementia‐related care in their department to be inadequate. Nurses with a bachelor or master level feel less responsible for the behavioural problems of patients with dementia; they feel less competent and less recognised by colleagues for their care for patients with dementia. The fewer hours nurses worked on the ward, the less responsible they felt for behavioural problems.
Positive correlations were found between the items, and if nurses followed a course on dementia last year. Nurses that completed a course on dementia in the last year devoted a more substantial part of their shift to caring for patients with dementia, they felt more responsible for behavioural problems and for the development of delirium. Additionally, they created optimum communication conditions for patients with dementia by making use, for example, of the patient's glasses or hearing aid. Eventually, nurses that followed a course felt more recognised by their colleagues for the care they provided to patients with dementia.
5. DISCUSSION
This study focused on the nursing care for patients with dementia in Dutch acute hospital settings and the nurses’ attitudes towards and perceptions of this care, to gain additional insights into how nurses manage challenging behaviour, and finally, which variables influence the nursing care of patients with dementia.
Although it is not precisely known how many patients with dementia are on average in a ward, the perceptions seem to be in line with estimates of 25%–40% (Brooker et al., 2014; Feast et al., 2020).
The findings of nursing care show that participating nurses often perform general preventive interventions. However, they perform fewer interventions related to dementia care, such as organising activities, to prevent delirium. Previous research has shown that when preventive interventions are carried out from person‐centred care, this can prevent complications (Feast et al., 2020). The literature has demonstrated that day structure, and activities are essential for patients with dementia and play a role in preventing delirium (Handley, Bunn, & Goodman, 2017; Prato, Lindley, Boyles, Robinson, & Abley, 2018). Additionally, the use of urinary catheters, of which half of the nurses in our study state to use often or always, is a possible cause of agitation and increases the risk of infections and delirium as a result (Palmer et al., 2014). In addition, the literature has demonstrated that the use of urinary catheters influences the length of hospital stay of older patients because their recovery is delayed by their limited ability to mobilise (Surkan & Gibson, 2018). A possible explanation for this is that nurses have a basic knowledge of care, but no specific knowledge of interventions related to the care for patients with dementia. The low score concerning the use of tube feeding seems appropriate, regarding international guidelines, where the use of tube feeding in a temporary crisis is described as a possibility (Volkert et al., 2015). The participating nurses indicate that they often use medical and physical restrictive measures. The use of medical restraints leads to a higher risk of complications. Therefore, patients’ mobility, the situation before admission and the perspective from the view of the person with dementia must be considered (Featherstone, Northcott, Harden, et al., 2019). The choice of medical restraints is often used by nurses as a last resort for managing challenging behaviour, because of insufficient time, to increase safety or insufficient knowledge of alternatives to restraint, but this choice is also influenced by a negative attitude and nurses’ insufficient knowledge (Hynninen, Saarnio, & Isola, 2015; Moyle, Borbasi, Wallis, Olorenshaw, & Gracia, 2011). However, our findings show that participating nurses say that they mostly “react with care” as a reaction to challenging behaviour and that they use “professional knowledge” as an alternative approach. These desirable reactions seem to contradict the frequent use of freedom‐restricting measures. Follow‐up research is needed to gain more insight into the situations that lead to the use of these restrictive measures. In addition, more research is necessary to investigate the possible preventive role of activities during admission in relation to challenging behaviour.
The nurses report various aspects related to the dementia‐sensitiveness of care in their department that could be improved. The care activities could be more adapted to the needs and pace of patients with dementia. Internationally, personal care is described as the gold standard for the care of people with dementia (The American Geriatrics Society Expert Panel on Person‐Centered Care, 2016). The basic principles of person‐centred care are based on approaching the person as an individual from the perspective of the person with dementia (Brooker, 2004). Person‐centred care is not only about the level of care providers but is also essential at other organisational levels. This means that people with dementia are also taken into account in the planning of shifts, whereby the complexity of care at the psychosocial level is higher. However, in acute hospitals, the complexity of care is determined mainly by physical aspects related to the cause of admission and are therefore not considered in the planning of shifts (Dewing & Dijk, 2016; Handley et al., 2017). Ward managers also relate planning problems to the insufficient number of nursing staff on duty (Timmons et al., 2016). For the provision of care, the high complexity of care for patients with dementia must be taken into account in the planning of care.
Related to the results of attitudes and perception, our findings show that the participating nurses often feel responsible for the consequences of treatment but seem unaware of how to prevent behavioural problems and delirium. This finding corresponds to other studies where the cause of behavioural issues is placed on the patient and not on the environment (Featherstone, Northcott, & Bridges, 2019; Kitwood, 1993). Another possibility is that nurses do not recognise delirium in patients with dementia. Studies have demonstrated that 30% of patients with dementia are screened for delirium (Möllers et al., 2019; Timmons et al., 2016). Delirium is a severe complication for patients with dementia and associated with increased morbidity and mortality (Jackson et al., 2017). The most effective treatment of delirium is prevention (Parrish, 2019). In order to be able to recognise changes in behaviour, nurses must be aware of how the patient behaved prior to admission in coordination with the close relatives, who know the patient well and therefore see changes in behaviour faster. Based on the score of the scale, we conclude that the nurses in our study have a positive attitude towards caring for patients with dementia, and this is demonstrated, for example, by keeping a close eye on confused patients with dementia. Not all nurses allow extra time for admission and discharge. This extra time is essential because when additional time is spent on admission to learn more about the patient with dementia, this can positively influence the quality of care. Ineffective communication can lead to misunderstanding and negative feelings or anxiety and helps nurses understand the behaviour of patients with dementia (Allwood et al., 2017; Handley, Bunn, & Goodman, 2018; Prato et al., 2018). It is unclear whether these results describe how the participating nurses intend to provide their care or how they actually provide this care. For example, nurses indicate that they often involve the person with dementia in decisions concerning their care and treatment. However, they also indicate that reasoning with a patient with dementia is not possible. Additionally, the results of the open questions provide another impression of the attitude of nurses. To gain more clarity on this topic, it is essential to compare these results with the experiences of patients with dementia and their informal carers or observations in hospitals. Although the nurses say they feel proficient, they find it challenging to combine the care for patients with dementia with their responsibilities for other patients. The nurses indicated that caring for patients with dementia is demanding because of the insufficient for this more complex care, a high workload and a shortage of nursing staff. This finding corroborates results in the literature (Gladman et al., 2012; Machiels, Metzelthin, Hamers, & Zwakhalen, 2017; Tropea, Logiudice, Liew, Roberts, & Brand, 2017). Reinforcement of organisational support is a condition for improving the quality of care (Evripidou et al., 2019).
Our research shows that that the fewer hours nurses work per week, the less responsible they feel for behavioural problems. Almost all the participants in this study work part‐time. Although the Netherlands has the highest number of part‐time employees in Europe, it is not known how the number of part‐time nurses relates to other countries (Eurostat, 2020). The number of part‐timers might negatively influence the continuity of care, which is important, particularly for patients with dementia because it helps them feel safe (Nilsson, Edvardsson, & Rushton, 2018). Compared with nurses working in a university hospital, nurses working in a general hospital had more experience, more often completed a course on dementia in the last year and have a lower level of education. Additionally, these nurses may have had more positive experiences in caring for patients with dementia. Some of these nurses worked as a care assistant before they became a nurse. Therefore, these nurses have a higher affinity with dementia care and are more motivated to complete a course on dementia. Higher educated nurses experience more difficulties in caring for patients with dementia and have taken a course less often. The literature has demonstrated that the gerontological and geriatric content of nursing courses in the Netherlands is insufficient (Bleijenberg, 2012) and that training can be effective (Scerri & Scerri, 2013; Surr et al., 2017, 2018). Based on the increasing number of patients with dementia and shortages of nursing staff, new approaches to caring for patients with dementia are vital (Evripidou et al., 2019). Nurses are aware of their insufficient knowledge and skills in caring for patients with dementia and want to learn more about the disease and how to manage problem behaviour. Our study shows that nurses who have taken a course feel more responsible for the development of delirium and behavioural problems, create optimum communication conditions and allow more time to prepare for discharge, even though the content of the courses is unknown. Nurses with an affinity for patients with dementia may also choose more quickly to complete a course on this subject.
We could not confirm the correlations between background the variables and subscales about managing challenging behaviour (Hynninen et al., 2016). However, our study showed that medical restraints as an alternative approach to physical restrictions are regularly used. Nurses believe that potentially challenging behaviour is under control, but restraints often cause complications and negative experiences for patients with dementia and their informal carers (Boltz, Chippendale, Resnick, & Galvin, 2015; Digby et al., 2016; Featherstone, Northcott, Harden, et al., 2019; Fukuda, Shimizu, & Seto, 2015). The focus of this article is on outcomes on scale level. Both instruments are relatively new. With regard to the GerINCQ, concerning measuring the care for patients with dementia, the researchers believe that several concepts can be measured per subscale. Further research could focus on research into these factors within the subscales. Both scales seem to contain items that might be better encoded reversed so that the results per subscale can be better interpreted. A follow‐up study may provide more clarity about this.
5.1. Limitations
This study has several limitations. First, selection bias may have influenced the results of this study. More than 60% of the participating nurses completed a course on dementia in the last year. In addition, we expected that the nurses recruited through social media would have an affinity for the topic; this probably affected the generalisability of our findings. Plausibly, in reality, the outcomes are less favourable.
By using self‐report, we measure the care from the perspective of nurses. We do not know how patients with dementia experience nursing care in the Netherlands. Despite the anonymity of the questionnaire, some of the answers seemed socially desirable. For example, nurses score high on the attitude scale and low on the perception scale. The picture that emerges from the open questions is also more negative than that based on the quantitative part. We posit that nurses strive to provide satisfactory care, but in reality, they cannot always realise this objective.
More generally, questionnaires tend to have low response rates and, therefore, risk bias (Polit & Beck, 2017). In order to increase the chance of response, we have paid much attention to the invitations. The contact persons have also tried to motivate departments to participate in the survey.
We altered the original instrument by changing the term elderly to patients with dementia and transforming the five‐point Likert to a four‐point Likert scale. The reliability of the total scale is comparable to the original version, and this also applies to the reliability of the subscales. However, in the two used subscales of Hynninen, on managing challenging behaviour, we found a difference in Cronbach's alpha, especially in the scale about reactions to challenging behaviour; the change to a 4‐point Likert scale or selection bias could explain this part. However, we have not been able to find a suitable explanation for the low score of the scale reactions on challenging behaviour. This requires more research in similar groups. In general, more psychometric evaluation, for example, factor analysis to reduce the number of items and improve the interpretation by coding some items reversed, could improve the usability of the total scale. The GerINCQ does not measure positive behaviour related to patients with dementia. Adding items on positive behaviour provides an improved picture of the perception of nurses towards patients with dementia.
Finally, the generalisability could have been influenced by cultural differences, differences in the general health system, and differences in ward levels such as the culture of care, staffing levels, types of leadership and type of ward.
6. CONCLUSION
The nurses participating in our study are insufficiently aware of specific dementia‐related care aspects, such as the prevention of delirium and challenging behaviour and regular use of urinary catheters. Medical and physical restrictive measures are frequently applied as an intervention in the care for patients with dementia. This seems inconsistent with how nurses indicate that they react to challenging behaviour.
Nurses express a positive attitude towards caring for patients with dementia and strive to provide adequate care. Although nurses have a strong sense of responsibility in preventing delirium, it is not clear whether they have sufficient knowledge about delirium in patients with dementia to succeed in this. In addition, nurses do not always experience the care for patients with dementia as satisfying but regularly as demanding. This phenomenon is due mostly to dementia‐related aspects and particularly challenging behaviour such as restless behaviour, aggression, wandering and disorientation.
The participating nurses feel proficient and use different approaches in managing challenging behaviour. However, they still use medical and physical restraints, despite the professional standards focusing on alternative psychosocial interventions. The nurses indicate that the training of nurses could be improved, even though this study shows a positive relation between completed a course on dementia in the last year and attitudes and perceptions. Among the research population, the given care is influenced by the hospital type, level of education and the number of hours that nurses work in the ward. Research on dementia care on the level of ward managers and directors could provide additional insights into the awareness of the importance of dementia‐friendly nursing care. Finally, more research is necessary on sufficient forms of education and training, during formal education and on the job, because nurses indicate that they want to provide proper care but are insufficiently equipped to do so.
6.1. Relevance to clinical practice
In order to improve care for patients with dementia in the hospital, nurses must become aware of their ability to influence the behaviour of patients with dementia through the use of dementia‐related preventive interventions. Awareness can be stimulated by deploying dementia nurses in each department, who act as role models and for teaching on the job. This requires a positive learning climate and a policy aimed at quality improvement and person‐centred care. In addition, patients’ stories can be used. In future training and education, more emphasis should be put on nurses’ awareness of their skills and abilities.
7. ETHICAL CONSIDERATIONS
The study was performed following the Helsinki declaration, and all the participants provided informed consent before filling out the questionnaire. The Medical Ethical Committee of the University Medical Centre Groningen considered approval unnecessary (decision M17.221048) because the questionnaire was intended for staff. The response was utterly anonymous. No one could be identified based on the results. Appendix A1, A2
CONFLICT OF INTEREST
None.
Supporting information
Supplementary Material
ACKNOWLEDGMENTS
The authors would like to thank all participating nurses for filling in the questionnaires and all contact persons in the hospitals for their help with distributing the questionnaires.
Appendix 1. GerINCQ and Hynninen overview mean, Cronbach's alpha if item deleted, percentages per category
Table A1.
GerINCQ overview mean, Cronbach's alpha if item deleted, percentages per category
| Subscales and items | Mean | Cronbach's alpha if item deleted | Percent | |||
|---|---|---|---|---|---|---|
| Performed interventions (Please state to what extent the following interventions are used with the patients with dementia you care for) | Never | Rarely | Often | Always | ||
| Nursing interventions to prevent pressure ulcers | 3.46 | 0.65 | 1 | 3 | 45 | 51 |
| Nursing interventions to prevent a delirium | 3.40 | 0.65 | 0 | 5 | 50 | 45 |
| Nursing interventions to prevent a fall | 3.40 | 0.67 | 0 | 4 | 52 | 44 |
| Nursing interventions to prevent malnutrition | 3.39 | 0.65 | 0 | 6 | 48 | 45 |
| Offering activities | 2.30 | 0.69 | 17 | 45 | 28 | 10 |
| Use of incontinence material | 3.08 | 0.68 | 0 | 7 | 78 | 15 |
| Active mobilisation policy | 3.17 | 0.66 | 1 | 10 | 59 | 30 |
| Enteral nutrition | 1.94 | 0.68 | 19 | 68 | 11 | 1 |
| Urinary catheters | 2.50 | 0.67 | 2 | 48 | 47 | 3 |
| Pain medication | 2.92 | 0.68 | 1 | 20 | 66 | 14 |
| Sleep medication | 2.56 | 0.68 | 4 | 37 | 57 | 2 |
| Medical restrictive measures | 2.70 | 0.67 | 5 | 24 | 66 | 5 |
| Physical movement‐restrictive measures | 2.21 | 0.67 | 11 | 59 | 28 | 2 |
| Dementia‐sensitive care delivery (At the department where you work how satisfied are you about the extent to which) | Mean | Cronbach's alpha if item deleted | Highly unsatisfied | Unsatisfied | Satisfied | Very satisfied |
|---|---|---|---|---|---|---|
| Patients with dementia treated with respect | 3.29 | 0.83 | 0 | 3 | 64 | 33 |
| Pace adjusted to people with dementia | 2.49 | 0.82 | 4 | 48 | 42 | 6 |
| Independence of people with dementia is encouraged | 2.85 | 0.83 | 0 | 21 | 71 | 8 |
| Patients with dementia can make decisions about their care and treatment | 2.69 | 0.83 | 0 | 32 | 65 | 3 |
| Informal carers of patients with dementia receive information | 3.05 | 0.83 | 0 | 13 | 69 | 18 |
| Communication takes place with informal carers about decisions concerning the care and treatment of patients with dementia | 3.17 | 0.83 | 0 | 8 | 67 | 23 |
| There is monitoring of and attention to the burden on informal carers of patients with dementia | 2.90 | 0.83 | 2 | 18 | 66 | 13 |
| Nurses adapt the care to the needs of patients with dementia | 2.90 | 0.82 | 0 | 17 | 74 | 9 |
| Nurses are aware that there can be a difference in the effect of medical/nursing interventions on patients with dementia compared with younger patients | 2.90 | 0.83 | 0 | 19 | 70 | 10 |
| Nurses request information about the patient's situation prior to admission | 2.70 | 0.83 | 5 | 29 | 56 | 10 |
| Patients with dementia are considered in the planning of each shift | 2.48 | 0.83 | 7 | 44 | 43 | 7 |
| Continuity of care between hospital departments is adequate | 2.49 | 0.82 | 1 | 21 | 73 | 5 |
| Continuity of care after discharge is adequate | 2.85 | 0.83 | 0 | 17 | 73 | 10 |
| Professional responsibility (How responsible do you feel for) | Mean | Cronbach's alpha if item deleted | Never responsible | Rarely responsible | Frequently responsible | Always responsible |
|---|---|---|---|---|---|---|
| Fall incidents among people with dementia | 3.26 | 0.87 | 0 | 8 | 58 | 34 |
| Development of pressure ulcers among patients with dementia | 3.33 | 0.87 | 0 | 5 | 58 | 38 |
| Deterioration in the nutritional status of patients with dementia | 3.08 | 0.87 | 0 | 14 | 64 | 22 |
| Urinary tract infections among patients with dementia as a consequence of urinary catheters | 2.86 | 0.87 | 3 | 24 | 55 | 17 |
| Retention of mobility among patients with dementia? | 3.21 | 0.88 | 0 | 7 | 67 | 27 |
| Behavioural problems in a patient with dementia? | 2.61 | 0.88 | 5 | 39 | 47 | 9 |
| Patients with dementia who are anxious and/or dejected? | 3.00 | 0.87 | 1 | 16 | 65 | 18 |
| The development of delirium in patients with dementia? | 2.90 | 0.88 | 3 | 26 | 48 | 23 |
| Wounds as a consequence of using sedative medication in patients with dementia? | 3.18 | 0.87 | 0 | 11 | 59 | 30 |
| Wounds as a consequence of using restrictive measures in patients with dementia? | 3.38 | 0.88 | 0 | 6 | 51 | 43 |
| Miscommunication with patients with dementia and informal carers? | 3.20 | 0.88 | 1 | 6 | 66 | 27 |
| Arranging the discharge of patients with dementia? | 3.32 | 0.89 | 0 | 4 | 58 | 37 |
| Attitude towards caring for patients with dementia (How would you describe your everyday experience for each of the following items?) | Mean | Cronbach's alpha if item deleted | Never | Rarely | Often | Always |
|---|---|---|---|---|---|---|
| I observe patients with dementia more carefully than younger patients | 3.14 | 0.69 | 1 | 11 | 59 | 29 |
| I keep a close eye on confused patients with dementia | 3.48 | 0.69 | 0 | 0 | 51 | 48 |
| I talk in simple language to patients with dementia | 3.31 | 0.70 | 0 | 3 | 62 | 35 |
| I talk more loudly and clearly when I speak with patients with dementia | 2.97 | 0.73 | 3 | 21 | 52 | 24 |
| I create optimum communication conditions for patients with dementia by making use of, for example, the patient's glasses or hearing aid | 3.52 | 0.69 | 0 | 0 | 47 | 53 |
| I allow extra time for the admission of patients with dementia | 2.70 | 0.69 | 3 | 34 | 52 | 11 |
| I use the case history details of patients with dementia to plan the care | 3.14 | 0.69 | 1 | 10 | 62 | 27 |
| I involve patients with dementia in decisions concerning their health | 2.98 | 0.70 | 0 | 13 | 76 | 11 |
| For the patients with dementia, I start the discharge planning when they are admitted | 2.63 | 0.71 | 9 | 32 | 46 | 13 |
| I allow more time for preparing the discharge of patients with dementia than I do for the discharge of an older patient without dementia | 2.69 | 0.70 | 6 | 33 | 47 | 14 |
| I take the patient's health history from the informal carer's point of view | 3.21 | 0.71 | 1 | 11 | 54 | 34 |
| I involve informal carers of patients with dementia in the care of that patient | 3.37 | 0.70 | 0 | 3 | 56 | 41 |
| I am aware that patients with dementia can be less assertive | 3.17 | 0.69 | 0 | 7 | 68 | 25 |
| I encourage patients with dementia to retain their independence during a hospital admission | 3.31 | 0.70 | 0 | 8 | 53 | 39 |
| Perceptions of caring for patients with dementia | Mean | Cronbach's alpha if item deleted | Almost none | Less than half | More than half | Nearly all |
|---|---|---|---|---|---|---|
| In the past 12 months, which proportion of the patients you cared for were patients with dementia? | 2.00 | 0.59 | 18 | 66 | 14 | 2 |
| Roughly what proportion of your shift do you devote to the care of patients with dementia in your department? | 2.17 | 0.59 | 18 | 51 | 27 | 4 |
| Never satisfying | Rarely satisfying | Frequently satisfying | Always satisfying | |||
| How satisfying is your work with patients with dementia? | 2.68 | 0.65 | 4 | 30 | 59 | 7 |
| Never demanding | Rarely demanding | Frequently demanding | Always demanding | |||
| How demanding do you find the work with patients with dementia? | 2.57 | 0.63 | 4 | 38 | 56 | 2 |
| Never difficult | Rarely difficult | Frequently difficult | Always difficult | |||
| How difficult do you find it to care for restless patients with dementia? | 2.78 | 0.64 | 2 | 29 | 58 | 10 |
| Not proficient | Insufficient proficient | Sufficient proficient | Very proficient | |||
| How proficient do you think you are in providing care for patients with dementia? | 2.98 | 0.63 | 0 | 12 | 78 | 10 |
| Never | Rarely | Often | Always | |||
| To what extent do you feel recognised by your colleagues for your care of patients with dementia? | 2.85 | 0.59 | 2 | 20 | 70 | 8 |
| To what extent do you feel supported by your superiors in the provision of care for patients with dementia? | 2.57 | 0.61 | 7 | 37 | 49 | 7 |
| Poor | Good | Excellent | ||||
| How do you experience the training of nurses in the provision of care to patients with dementia in your department? | 2.48 | 0.61 | 4 | 46 | 47 | 3 |
| Some patients can exhibit behaviour that others experience as disruptive, and that applies to older patients as well. During your provision of care, how often do you experience that older patients: Note: Of course, older patients can be lovely, funny, touching, modest, etc., but these aspects will not be enquired about here | Never | Rarely | Often | Always | ||
| Cannot be reasoned with | 2.38 | 0.59 | 3 | 56 | 41 | 0 |
| Are not cooperative | 2.62 | 0.60 | 0 | 39 | 60 | 1 |
| Demand a lot of attention | 2.92 | 0.61 | 1 | 14 | 78 | 7 |
| Are confused | 2.93 | 0.60 | 0 | 9 | 88 | 3 |
| Are restless at night | 2.99 | 0.62 | 1 | 7 | 86 | 7 |
| Are slow | 2.92 | 0.61 | 1 | 13 | 79 | 7 |
| Display disruptive behaviour towards other patients | 2.45 | 0.60 | 2 | 52 | 45 | 0 |
Table A2.
Hynninen overview mean, Cronbach's alpha if item deleted, percentages per category
| Subscales and items | Mean | Cronbach's alpha if item deleted | Never | Percent | ||
|---|---|---|---|---|---|---|
| Reaction when a patient with dementia displays challenging behaviour | Rarely | Often | Always | |||
| F1 React with care | ||||||
| I ask her/him what is wrong | 3.41 | 0.48 | 0 | 3 | 53 | 44 |
| I check the patient record for patient's background and possible instructions | 3.42 | 0.46 | 1 | 4 | 48 | 47 |
| I organise activities for the patient, for example, switching on the TV in the patient room | 3.08 | 0.46 | 1 | 8 | 72 | 18 |
| I am present for the patient; I touch, speak and listen | 3.29 | 0.46 | 0 | 3 | 66 | 31 |
| F2 React by ignoring | ||||||
| I do nothing | 1.33 | 0.55 | 67 | 32 | 0 | 0 |
| I pretend not to hear, see or notice anything | 1.49 | 0.54 | 56 | 40 | 4 | 0 |
| F3 react with power | ||||||
| I take her/him to her/his room | 3.17 | 0.47 | 2 | 6 | 64 | 28 |
| I use physical force to calm the situation | 1.52 | 0.54 | 56 | 36 | 7 | 0 |
| I give orders to the patient | 3.18 | 0.45 | 1 | 7 | 63 | 29 |
| F4 react casually | ||||||
| I manage humour | 3.23 | 0.47 | 0 | 4 | 69 | 27 |
| I tolerate the behaviour because the patient has the right to become angry | 2.73 | 0.50 | 1 | 29 | 65 | 5 |
| Use of alternative approaches instead of physical restraints | Mean | Cronbach's alpha if item deleted | Never | Rarely | Often | Always |
|---|---|---|---|---|---|---|
| F1 use of professional knowledge | ||||||
| I try to make the physical care environment safer | 3.44 | 0.53 | 0 | 2 | 52 | 45 |
| I am present for the patient; I touch, speak and listen | 3.28 | 0.54 | 0 | 2 | 69 | 29 |
| I can manage the patient's challenging behaviour | 2.98 | 0.58 | 0 | 10 | 82 | 8 |
| I negotiate with my colleagues about the correct approach | 3.21 | 0.53 | 0 | 4 | 69 | 26 |
| I negotiate with the patient's family about the correct approach | 3.34 | 0.53 | 0 | 3 | 60 | 37 |
| F2 use of medication | ||||||
| I give sedative medication to the patient | 2.64 | 0.62 | 0 | 37 | 61 | 2 |
| I give painkillers to the patient | 2.66 | 0.60 | 3 | 32 | 61 | 4 |
| F3 use of problem‐solving | ||||||
| I try to draw the patient's attention elsewhere | 3.13 | 0.57 | 0 | 4 | 79 | 17 |
| I try to organise expert consultation for the patient | 3.24 | 0.58 | 0 | 9 | 56 | 34 |
Keuning‐Plantinga A, Roodbol PF, Krijnen WP, Finnema EJ. Nurses’ perceptions in caring for people with dementia in Dutch acute hospitals. J Clin Nurs. 2022;31:1800–1816. 10.1111/jocn.15458
REFERENCES
- Allwood, R. , Pilnick, A. , O’Brien, R. , Goldberg, S. , Harwood, R. H. , & Beeke, S. (2017). Should I stay or should I go? How healthcare professionals close encounters with people with dementia in the acute hospital setting. Social Science and Medicine, 191, 212–225. 10.1016/j.socscimed.2017.09.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alzheimer Nederland . (2019). Factsheet cijfers en feiten over dementie | Alzheimer Nederland. Alzheimer Nederland, 2019. Retrieved from https://www.alzheimer‐nederland.nl/factsheet‐cijfers‐en‐feiten‐over‐dementie [Google Scholar]
- Bleijenberg, N. (2012). Dutch nursing students’ knowledge and attitudes towards older people—A longitudinal cohort study. Journal of Nursing Education and Practice, 2(2), 1–8. 10.5430/jnep.v2n2p1 [DOI] [Google Scholar]
- Boltz, M. , Chippendale, T. , Resnick, B. , & Galvin, J. E. (2015). Testing family‐centered, function‐focused care in hospitalised persons with dementia. Neurodegenerative Disease Management, 5(3), 203–215. 10.2217/nmt.15.10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooker, D. (2004). What is person‐centred care in dementia? Reviews in Clinical Gerontology, 13(3), 215–222. 10.1017/S095925980400108X [DOI] [Google Scholar]
- Brooker, D. , Milosevic, S. , Evans, S. , Bruce, M. , & Thompson, R. (2014). RCN Development Programme: Transforming dementia care in hospitals evaluation report. Worcester. Retrieved from http://www.worcester.ac.uk/documents/FULL_RCN_report_Transforming_dementia_care_in_hospital.pdf [Google Scholar]
- Clissett, P. , Porock, D. , Harwood, R. H. , & Gladman, J. R. F. (2014). The responses of healthcare professionals to the admission of people with cognitive impairment to acute hospital settings: An observational and interview study. Journal of Clinical Nursing, 23(13–14), 1820–1829. 10.1111/jocn.12342 [DOI] [PubMed] [Google Scholar]
- Dewing, J. , & Dijk, S. (2016). What is the current state of care for older people with dementia in general hospitals? A literature review. Dementia, 15(1), 106–124. 10.1177/1471301213520172 [DOI] [PubMed] [Google Scholar]
- Digby, R. , Lee, S. , & Williams, A. (2016). The experience of people with dementia and nurses in hospital: An integrative review. Journal of Clinical Nursing, 26(9–10), 1152–1171. 10.1111/jocn.13429 [DOI] [PubMed] [Google Scholar]
- Ernst, J. , Petry, H. , Luethi, N. , & Naef, R. (2019). Acute care delivery to persons with cognitive impairment: A mixed method study of health professionals’ care provision and associated challenges. Aging & Mental Health, 1–10. 10.1080/13607863.2019.1616162 [DOI] [PubMed] [Google Scholar]
- Eurostat . (2020). Part‐time employment rate 2019. Retrieved June 26, 2020, from https://ec.europa.eu/eurostat/databrowser/view/tesem100/default/bar?lang=en [Google Scholar]
- Evripidou, M. , Charalambous, A. , Middleton, N. , & Papastavrou, E. (2019). Nurses’ knowledge and attitudes about dementia care: Systematic literature review. Perspectives in Psychiatric Care, 55(1), 48–60. 10.1111/ppc.12291 [DOI] [PubMed] [Google Scholar]
- Feast, A. R. , White, N. , Candy, B. , Kupeli, N. , & Sampson, E. L. (2020). The effectiveness of interventions to improve the care and management of people with dementia in general hospitals: A systematic review. International Journal of Geriatric Psychiatry, 35, 463–488. 10.1002/gps.5280 [DOI] [PubMed] [Google Scholar]
- Featherstone, K. , Northcott, A. , & Bridges, J. (2019). Routines of resistance: An ethnography of the care of people living with dementia in acute hospital wards and its consequences. International Journal of Nursing Studies, 96, 53–60. 10.1016/j.ijnurstu.2018.12.009 [DOI] [PubMed] [Google Scholar]
- Featherstone, K. , Northcott, A. , Harden, J. , Harrison Denning, K. , Tope, R. , Bale, S. , & Bridges, J. (2019). Refusal and resistance to care by people living with dementia being cared for within acute hospital wards: An ethnographic study. Health Services and Delivery Research, 7(11), 1–92. 10.3310/hsdr07110 [DOI] [PubMed] [Google Scholar]
- Field, A. (2013). Discovering statistics using IBM SPSS. Discovering Statistics Using SPSS (4TH edn, pp.1–916). London, UK: SAGE Publications Ttd. 10.1234/12345678 [DOI] [Google Scholar]
- Fogg, C. , Griffiths, P. , Meredith, P. , & Bridges, J. (2018). Hospital outcomes of older people with cognitive impairment: An integrative review. International Journal of Geriatric Psychiatry, 33, 1177–1197. 10.1002/gps.4919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fukuda, R. , Shimizu, Y. , & Seto, N. (2015). Issues experienced while administering care to patients with dementia in acute care hospitals: A study based on focus group interviews. International Journal of Qualitative Studies on Health and Well‐Being, 10, 25828. 10.3402/qhw.v10.25828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gladman, J. , Porock, D. , Griffiths, A. , Clissett, P. , Harwood, R. H. , Knight, A. , … Kearny, F. (2012). Better Mental Health: Care for Older People with Cognitive Impairment in General Hospitals. Final report NIHR Service Delivery and Organisation programme. Southampton: Queen’s Printer and Controller of HMSO. http://www.netscc.ac.uk/netscc/hsdr/files/project/SDO_FR_08‐1809‐227_V01.pdf [Google Scholar]
- Handley, M. , Bunn, F. , & Goodman, C. (2017). Dementia‐friendly interventions to improve the care of people living with dementia admitted to hospitals: A realist review. British Medical Journal Open, 7(7), 1–13. 10.1136/bmjopen-2016-015257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Handley, M. , Bunn, F. , & Goodman, C. (2018). Supporting general hospital staff to provide dementia sensitive care: A realist evaluation. International Journal of Nursing Studies, 96, 61–71. 10.1016/j.ijnurstu.2018.10.004 [DOI] [PubMed] [Google Scholar]
- Hunter, P. V. , Hadjistavropoulos, T. , Smythe, W. E. , Malloy, D. C. , Kaasalainen, S. , & Williams, J. (2013). The Personhood in Dementia Questionnaire (PDQ): Establishing an association between beliefs about personhood and health providers’ approaches to person‐centred care. Journal of Aging Studies, 27(3), 276–287. 10.1016/j.jaging.2013.05.003 [DOI] [PubMed] [Google Scholar]
- Hynninen, N. , Saarnio, R. , & Isola, A. (2015). Treatment of older people with dementia in surgical wards from the viewpoints of the patients and close relatives. Journal of Clinical Nursing, 24, 3691–3699. 10.1111/jocn.13004 [DOI] [PubMed] [Google Scholar]
- Hynninen, N. , Saarnio, R. , & Isola, A. (2016). Care practices of older people with dementia in the surgical ward—A questionnaire survey. Journal of Clinical Nursing, 4, 1–9. 10.1177/2050312116676033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson, T. A. , Gladman, J. R. F. , Harwood, R. H. , MacLullich, A. M. J. , Sampson, E. L. , Sheehan, B. , & Davis, D. H. J. (2017). Challenges and opportunities in understanding dementia and delirium in the acute hospital. PLoS Medicine, 14(3), 1–9. 10.1371/journal.pmed.1002247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen, A. M. , Pedersen, B. D. , Wilson, R. L. , Bang Olsen, R. , & Hounsgaard, L. (2019). Nurses’ experiences of delivering acute orthopaedic care to patients with dementia. International Journal of Older People Nursing, 14(4), 1–16. 10.1111/opn.12271 [DOI] [PubMed] [Google Scholar]
- Kitwood, T. (1993). Towards a theory of dementia care: The interpersonal process. Ageing and Society, 13(1), 51–67. 10.1017/S0144686X00000647 [DOI] [PubMed] [Google Scholar]
- Machiels, M. , Metzelthin, S. F. , Hamers, J. P. H. , & Zwakhalen, S. M. G. (2017). Interventions to improve communication between people with dementia and nursing staff during daily nursing care: A systematic review. International Journal of Nursing Studies, 66, 37–46. 10.1016/j.ijnurstu.2016.11.017 [DOI] [PubMed] [Google Scholar]
- Maneesriwongul, W. , & Dixon, J. K. (2004). Instrument translation process: A methods review. Journal of Advanced Nursing, 48(2), 175–186. 10.1111/j.1365-2648.2004.03185.x [DOI] [PubMed] [Google Scholar]
- Möllers, T. , Stocker, H. , Wei, W. , Perna, L. , & Brenner, H. (2019). Length of hospital stay and dementia: A systematic review of observational studies. International Journal of Geriatric Psychiatry, 34(1), 8–21. 10.1002/gps.4993 [DOI] [PubMed] [Google Scholar]
- Moyle, W. , Borbasi, S. , Wallis, M. , Olorenshaw, R. , & Gracia, N. (2011). Acute care management of older people with dementia: A qualitative perspective. Journal of Clinical Nursing, 20(3–4), 420–428. 10.1111/j.1365-2702.2010.03521.x [DOI] [PubMed] [Google Scholar]
- Mukaetova‐Ladinska, E. B. , Teodorczuk, A. , & Cerejeira, J. M. (2009). Dementia in the acute hospital. British Journal of Psychiatry, 195(5), 461–462. 10.1192/bjp.195.5.461 [DOI] [PubMed] [Google Scholar]
- Nilsson, A. , Edvardsson, D. , & Rushton, C. (2018). Nurses' descriptions of person‐centred care for older people in an acute medical ward—on the individual, team and organisational levels'. Journal of Clinical Nursing. 10.1111/jocn.14738 [DOI] [PubMed] [Google Scholar]
- Nunnally, J. C. (1978). Psychometric theory. New York, NY: McGraw‐Hill. [Google Scholar]
- Palmer, J. L. , Lach, H. W. , McGillick, J. , Murphy‐White, M. , Carroll, M. B. , & Armstrong, J. L. (2014). The dementia friendly hospital initiative education program for acute care nurses and StaffNIH public access. Journal of Continuing Education in Nursing, 45(9), 416–424. 10.1109/TMI.2012.2196707.Separate [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parrish, E. (2019). Delirium superimposed on dementia: Challenges and opportunities. Nursing Clinics of North America, 54(4), 541–550. 10.1016/j.cnur.2019.07.004 [DOI] [PubMed] [Google Scholar]
- Persoon, A. , Bakker, F. C. , van der Wal‐Huisman, H. , & Olde Rikkert, M. G. M. (2015). Development and validation of the geriatric in‐hospital nursing care questionnaire. Journal of the American Geriatrics Society, 63(2), 327–334. 10.1111/jgs.13243 [DOI] [PubMed] [Google Scholar]
- Polit, D. F. , & Beck, C. T. (2017). Nursing research generating and assessing evidence for nursing practice. In Burns C. (Ed.), Nurse education in practice , 10th ed. Philadelphia, PA: Wolters Kluwer Health. [Google Scholar]
- Prato, L. , Lindley, L. , Boyles, M. , Robinson, L. , & Abley, C. (2018). Empowerment, environment and person‐centred care: A qualitative study exploring the hospital experience for adults with cognitive impairment. Dementia, 18, 2710–2730. 10.1177/1471301218755878 [DOI] [PubMed] [Google Scholar]
- Reilly, J. C. , & Houghton, C. (2019). The experiences and perceptions of care in acute settings for patients living with dementia: A qualitative evidence synthesis. International Journal of Nursing Studies, 96, 82–90. 10.1016/j.ijnurstu.2019.04.018 [DOI] [PubMed] [Google Scholar]
- Scerri, A. , & Scerri, C. (2013). Nursing students’ knowledge and attitudes towards dementia—A questionnaire survey. Nurse Education Today, 33(9), 962–968. 10.1016/j.nedt.2012.11.001 [DOI] [PubMed] [Google Scholar]
- Surkan, M. J. , & Gibson, W. (2018). Interventions to mobilise elderly patients and reduce length of hospital stay. Canadian Journal of Cardiology, 34(7), 881–888. 10.1016/j.cjca.2018.04.033 [DOI] [PubMed] [Google Scholar]
- Surr, C. A. , Gates, C. , Irving, D. , Oyebode, J. , Smith, S. J. , Parveen, S. , … Dennison, A. (2017). Effective dementia education and training for the health and social care workforce: A systematic review of the literature. Review of Educational Research, 87(5), 966–1002. 10.3102/0034654317723305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surr, C. A. , Sass, C. , Burnley, N. , Drury, M. , Smith, S. J. , Parveen, S. , … Oyebode, J. (2018). Components of impactful dementia training for general hospital staff: A collective case study. Aging and Mental Health, 24, 511–521. 10.1080/13607863.2018.1531382 [DOI] [PubMed] [Google Scholar]
- The American Geriatrics Society Expert Panel on Person‐Centered Care . (2016). Person‐centered care: A definition and essential elements. The American Geriatrics Society, 20(1), 15–18. 10.1111/jgs.13866 [DOI] [PubMed] [Google Scholar]
- Timmons, S. , O’Shea, E. , O’Neill, D. , Gallagher, P. , de Siún, A. , McArdle, D. , … Kennelly, S. (2016). Acute hospital dementia care: Results from a national audit. BMC Geriatrics, 16, 113. 10.1186/s12877-016-0293-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toot, S. , Devine, M. , Akporobaro, A. , & Orrell, M. (2013). Causes of hospital admission for people with dementia: A systematic review and meta‐analysis. Journal of the American Medical Directors Association, 14, 463–470. 10.1016/j.jamda.2013.01.011 [DOI] [PubMed] [Google Scholar]
- Tropea, J. , Logiudice, D. , Liew, D. , Roberts, C. , & Brand, C. (2017). Caring for people with dementia in hospital: Findings from a survey to identify barriers and facilitators to implementing best practice dementia care. International Psychogeriatrics, 29(3), 467–474. 10.1017/S104161021600185X [DOI] [PubMed] [Google Scholar]
- Turner, A. , Eccles, F. J. , Elvish, R. , Simpson, J. , & Keady, J. (2017). The experience of caring for patients with dementia within a general hospital setting: A meta‐synthesis of the qualitative literature. Aging & Mental Health, 21(1), 66–76. 10.1080/13607863.2015.1109057 [DOI] [PubMed] [Google Scholar]
- Vektis (2019). Zorggebruik van mensen met dementie in beeld Colofon, Zeist: Vektis. https://www.vektis.nl/uploads/NieuwsDocs/Definitieverapportageindicatorendementienetwerken2018.pdf [Google Scholar]
- Volkert, D. , Chourdakis, M. , Faxen‐Irving, G. , Frühwald, T. , Landi, F. , Suominen, M. H. , … Schneider, S. M. (2015). ESPEN guidelines on nutrition in dementia. Clinical Nutrition, 34(6), 1052–1073. 10.1016/j.clnu.2015.09.004 [DOI] [PubMed] [Google Scholar]
- von Elm, E. , Altman, D. G. , Egger, M. , Pocock, S. J. , Gøtzsche, P. C. , & Vandenbroucke, J. P. (2008). The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Journal of Clinical Epidemiology, 61(4), 344–349. 10.1016/j.jclinepi.2007.11.008 [DOI] [PubMed] [Google Scholar]
- World Health Organization . (2019). Fact sheet Dementia. Retrieved September 24, 2019, from https://www.who.int/news‐room/fact‐sheets/detail/dementia [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


