Abstract
Objectives
The therapeutic effect of acupuncture treatments (AT) on functional gastrointestinal disorders (FGIDs) is contentious. A meta‐analysis was conducted to assess the efficacy and safety of acupuncture for FGIDs.
Methods
The Cochrane Library, EMBASE, PUBMED, Web of Science, Wanfang Database, China National Knowledge Infrastructure, and VIP Database were searched through December 31, 2019 with no language restrictions. Risk ratio (RR) with 95% confidence interval (CI) was calculated to determine the improvement in symptom severity after treatment.
Results
A total of 61 randomized controlled trials (RCTs) on FGIDs were included. The pooled results illustrated the following: compared to pharmacotherapy (RR 1.13, 95% CI 1.09–1.17), placebo acupuncture (RR 1.69, 95% CI 1.37–2.08), no specific treatment (RR 1.86, 95% CI 1.31–2.62), and AT as an adjuvant intervention to other active treatments (RR 1.25, 95% CI 1.21–1.30), AT had more favorable improvements in symptom severity; sub‐group analysis results classified according to functional dyspepsia, irritable bowel syndrome, and functional constipation also supported this finding; and the incidence of adverse events was lower in AT than in other treatments (RR 0.75, 95% CI 0.56–0.99).
Conclusions
This meta‐analysis found that AT was significantly associated with relief of FGIDs symptoms; however, the evidence level was moderate or low. Further data from rigorously designed and well powered RCTs are needed to verify the effectiveness and safety of AT as a FGIDs treatment.
PROSPERO PROTOCOL NUMBER: CRD42020169508.
Keywords: Acupuncture, Functional constipation, Functional dyspepsia, Functional gastrointestinal disorders, Irritable bowel syndrome
Introduction
Functional gastrointestinal disorders (FGIDs) are now defined as disorders caused by a combination of genetics, psychological factors, social factors, disturbance in the gut‐brain axis, and environmental stressors. 1 Irritable bowel syndrome (IBS), functional dyspepsia (FD), and functional constipation (FC) are the most common FGIDs. They are a challenge to public health because they are ubiquitous, affect the quality of life, and cause social and economic burdens.
The efficacy of pharmacological treatments, such as prokinetic agents, proton pump inhibitors, anticholinergic spasms, tricyclics, antidiarmodials, 5‐HT3 antagonists, and antidepressants, remains unsatisfactory because of the associated adverse effects. For instance, 5‐HT3 antagonists and 5‐HT4 agonists, pose a potential risk of ischaemic colitis and cardiovascular events, respectively. 2 In addition, single agents of pharmacotherapy target only one symptom at a time and thus are unlikely to be effective in patients with symptoms in the upper and lower digestive tracts, and the combined use of drugs to treat upper and lower abdominal symptoms raises the possibility of side effects.
Whilst available treatment options for FGIDs have limited efficacy, complementary and alternative medicine (CAM) provides a new treatment option for gastroenterology specialists and patients with gastrointestinal diseases. 3 Acupuncture treatment (AT) has become increasingly recognized as a CAM. 3 Acupuncture involves application of needles, heat, pressure, and other treatments to various skin locations called acupuncture points (or acupoints) to improve the body's ability to self‐regulate and control symptoms.
In the East, acupuncture has been practised for thousands of years and is considered an active treatment for FGIDs for a long time. However, currently, no strong evidence to show the effectiveness and safety of AT for FGIDs exists. Systematic reviews on acupuncture for individual FGIDs are scarce. Nevertheless, relevant multi‐centre RCTs have been conducted recently. Hence, this study aimed to summarize the evidence in the RCTs and conduct a meta‐analysis to evaluate the effectiveness and safety of AT in FGIDs.
Methods
Literature search
According to the PRISMA guidelines, 4 EMBASE, Cochrane Library, PUBMED, Web of Science, WanFang Database, China National Knowledge Infrastructure, and VIP Database were searched through December 31, 2019 with no language restrictions. The following terms were used: functional gastrointestinal disease, acupuncture, electro‐acupuncture, meridians, acupoints, dyspepsia, irritable bowel syndrome, constipation, and randomized controlled trials (RCTs) (Fig. 1). The full literature search strategy is provided as an additional file (Table S4). Moreover, we also considered all RCTs included in the systematic reviews related to FD, IBS, and FC. PROSPERO registration: CRD42020169508.
FIGURE 1.
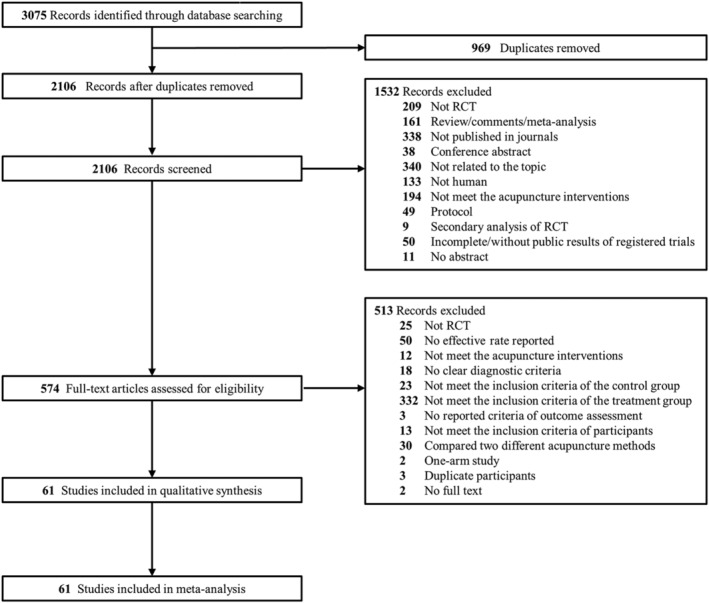
A flowchart of literature search and selection process.
Selection criteria
Inclusion criteria included the following: (i) RCTs published in journals; (ii) adult subjects (18–75 years old) diagnosed with FD, IBS, or FC; diagnostic criteria including but not limited to the Rome criteria; 1 , 5 , 6 , 7 (iii) AT interventions, including manual acupuncture, electro‐acupuncture, and manual acupuncture combined with moxibustion; (iv) control group composed of those with sham acupuncture, medication treatment, no (specific) treatment, or AT as an adjuvant intervention to another treatment; and (v) studies reporting the rate of symptom improvement after treatment.
Exclusion criteria were as follows: (i) studies that did not meet the aforementioned inclusion criteria; (ii) duplication (i.e. the same data of subjects in different studies by the same authors); (iii) full text was unavailable; and (iv) the format of the result report could not be used for the meta‐analysis of the risk ratio (RR).
Data collection
Two reviewers screened all records identified by independent search and reviewed full texts for eligibility. For studies that met the inclusion criteria, data were independently extracted by two authors and reviewed by the corresponding author. Data on author names, publication year, country, subjects (mean age, sample sizes), interventions (treatment and control groups), effective rate, adverse events, and outcome assessment criteria were obtained.
Any differences were settled through discussion. Authors of studies whose reported data were incomplete or ambiguous were contacted.
Assessment of risk of bias
Using Cochrane Collaboration risk of bias tool, 8 two authors independently evaluated the methodological quality of all included RCTs based on seven items, and the RCTs were classified as ‘high risk’, ‘low risk’, and ‘uncertain’.
Data synthesis and analysis
Outcome measures: Review Manager (version 5.3) was used to express a dichotomous result (e.g. efficiency) as risk ratio (RR), with 95% confidence interval (CI). In the presence of large amounts of heterogeneity (I2 > 50% or P < 0.05), a random‐effects model was employed to calculate the combined RR; otherwise, a fixed‐effects model was used. We tackled the missing data and analyzed the results based on intention‐to‐treat (ITT) principle. 8 Moreover, in some RCTs, patients treated with acupuncture were divided into different groups according to the acupuncture points and methods used. As the acupuncture points and methods used in each group are common acupuncture prescriptions for FGIDs, we combined the results of the different acupuncture groups to obtain information that is closer to the true clinical curative effect.
Missing data and adverse events: Based on the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions (chapter 16), 8 studies whose number of adverse events in the study groups was zero were excluded from the meta‐analysis.
Assessment of heterogeneity: When heterogeneity was observed (I2 > 50% or P < 0.05), we attempted to identify the potential factors by exploring the individual characteristics of the study and subgroup analysis.
Publication bias: STATA (version 16.0) was employed to perform funnel chart and Egger's test to assess for potential publication bias when at least 10 studies were included.
Sensitivity analysis: We performed sensitivity analysis using either fixed‐effects or random‐effects model to assess whether the results were robust.
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) system was applied to confirm the level of evidence and the strength of the recommendation.
Results
Literature search
Literature search identified 3,075 publications. A total of 969 duplicates were eliminated, and 574 were excluded after title and abstract screening based on the exclusion criteria. After reviewing full‐text publications, 61 RCTs were selected according to the inclusion criteria, involving 9,447 participants, of which 4,942 participants received ATs (Fig. 1).
Characteristics of included RCTs
A total of 61 RCTs 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 associated with AT for FGIDs that met the inclusion criteria were selected. Experimental details of clinical research are summarized in (Table S1). The 9,447 participants in 61 RCTs were divided as follows: 2875 with FD in 21 studies, 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 3,220 with IBS in 24 studies, 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 and 3,352 with FC in 16 studies. 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 There were 12 multi‐centre and 49 single‐centre RCTs with sample sizes ranging from 48 to 1,075, the age range of participants was 33–75 years, and the duration of therapy lasted 2–12 weeks. Except for one RCT 29 using the Chicago NUD International Conference Standard, the other 60 RCTs used the Rome criteria. For the acupuncture methods, 20 studies used electro‐acupuncture and 41 studies applied manual acupuncture; since traditional Chinese medicine (TCM) acupuncture is often accompanied by moxibustion, five RCTs 18 , 24 , 27 , 30 , 45 used acupuncture accompanied by moxibustion. For acupoints, the six most commonly used acupoints in the included RCTs were ST36, CV12, PC6, ST25, ST37, and BL25. Regarding the background of acupuncture therapists, all acupuncturists in the included RCTs were fully trained in TCM acupuncture. In this meta‐analysis, the primary outcome was post‐treatment efficacy rate, and the post‐treatment efficacy rates reported in all included studies were based on symptom improvement.
Methodological quality
Based on the Cochrane Collaboration risk of bias assessment tool, 8 all 61 RCTs reported appropriate methods of random sequence generation. Sixteen studies mentioned allocation concealment, 21 studies addressed performance bias, 11 studies reported blinding of outcome assessors, and 60 studies addressed attrition bias (Fig. S1). The methodological quality summary is presented in the supporting documents (Fig. S2).
Acupuncture versus pharmacotherapy
In total, 40 RCTs compared AT with pharmacotherapy, and all RCTs were performed in China. The pharmacological drugs used in the control group included prokinetic agents (itopride, domperidone), 5‐HT4 agonists (mosapride), antispasmodic calcium antagonist (pinaverium bromide), antidiarmodials (loperamide hydrochloride), Bifidobacterium, and antidepressants (flupentixol, melitracen). The number of RCTs concerned with FD, IBS, and FC were 13, 19, and 8, respectively.
The pooled results indicated that AT is significantly better at improving symptoms than pharmacotherapy (RR 1.13, 95% CI 1.09–1.17, I2 = 24%, Figure 2). Nevertheless, the GRADE analysis showed that the overall quality of the evidence for such finding was moderate because of the high risk of bias, which could be attributed to uncertain blinding in most studies (Table 1). Moreover, the subgroup analysis (Fig. 2) showed that AT is superior to pharmacotherapy therapy in relieving the symptoms of FD (RR 1.08, 95% CI 1.03–1.14), IBS (RR 1.16, 95% CI 1.11–1.22), and FC (RR 1.16, 95% CI 1.06–1.28).
FIGURE 2.
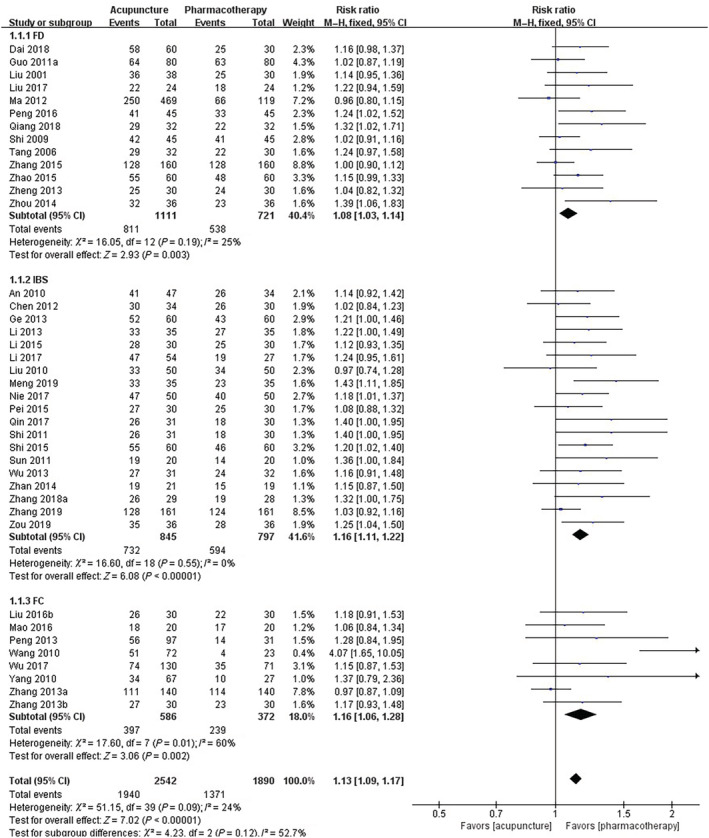
Forest plot of comparison of efficacy: Acupuncture versus pharmacotherapy for functional gastrointestinal disorders. IBS, irritable bowel syndrome; FD, functional dyspepsia; FC, functional constipation.
TABLE 1.
Summary of Findings
| Bibliography: Acupuncture for functional gastrointestinal disorders. | |||||
|---|---|---|---|---|---|
| Outcomes | No of Participants (studies) | Quality of the evidence(GRADE) | Relative effect (95% CI) | Anticipated absolute effects | |
| Risk with Control | Risk difference with Acupuncture versus pharmacotherapy (95% CI) | ||||
|
Acupuncture vs. pharmacotherapy Effective rate |
4,432(40 studies) |
due to risk of bias |
RR 1.13 (1.09 to 1.17) | Study population | |
| 725 per 1,000 | 94 more per 1,000(from 65 more to 123 more) | ||||
| Moderate | |||||
| 757 per 1,000 | 98 more per 1,000(from 68 more to 129 more) | ||||
|
Acupuncture vs. placebo acupuncture Effective rate |
2,800(12 studies) |
due to risk of bias, inconsistency |
RR 1.69 (1.37 to 2.08) | Study population | |
| 289 per 1,000 | 199 more per 1,000(from 107 more to 312 more) | ||||
| Moderate | |||||
| 357 per 1,000 | 246 more per 1,000(from 132 more to 386 more) | ||||
|
Acupuncture plus other active treatments vs. other active treatments Effective rate |
2,128(13 studies) |
⊕ ⊕ ⊕⊝MODERATE † due to nconsistency |
RR 1.25 (1.21 to 1.3) | Study population | |
| 740 per 1,000 | 185 more per 1,000(from 155 more to 222 more) | ||||
| Moderate | |||||
| 778 per 1,000 | 195 more per 1,000(from 163 more to 232 more) | ||||
|
Acupuncture vs. no specific treatment Effective rate |
564(4 studies) |
due to risk of bias, inconsistency |
RR 1.86 (1.31 to 2.62) | Study population | |
| 314 per 1,000 | 270 more per 1,000(from 97 more to 509 more) | ||||
| Moderate | |||||
| 329 per 1,000 | 283 more per 1,000(from 102 more to 533 more) | ||||
|
Adverse events Adverse events rate |
3,951(18 studies †† ) |
due to risk of bias |
RR 0.75 (0.56 to 0.99) | Study population | |
| 49 per 1,000 | 12 fewer per 1,000(from 0 fewer to 22 fewer) | ||||
| Moderate | |||||
| 42 per 1,000 | 309 more per 1,000(from 0 fewer to 18 fewer) | ||||
*The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI).CI: Confidence interval; RR: Risk ratio;
GRADE Working Group grades of evidence.
High quality: Further research is very unlikely to change our confidence in the estimate of effect.
Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate.
Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Very low quality: We are very uncertain about the estimate.
High risk of performance and detection bias owing to nonblinding.
The funnel plot (Fig. S3) was symmetrically distributed after trim‐and‐fill analysis, demonstrating that the conclusion will not be affected by publication bias
Heterogeneity: I2 = 79%.
Heterogeneity: I2 = 63%.
Thirty studies reported adverse events (Table S1), of which 18 studies compared acupuncture with other treatments and the data is available for pooled analysis.
inconclusive allocation concealment and blinding
Acupuncture versus placebo acupuncture
In 12 acupuncture placebo‐controlled RCTs, nine were conducted in China; the remaining three, in the USA, UK, and Canada. In seven RCTs of manual acupuncture, three 10 , 53 , 54 used shallow acupuncture (i.e. the skin was gently pierced 2–3 mm) on non‐acupoints, one study 52 used Streitberger needles, one study 37 used non‐penetrating acupuncture (blunt needle tapped against the skin) on the same acupoints as those in the acupuncture group, and one study 61 performed acupuncture on non‐acupoints. For electro‐acupuncture, two studies 12 , 23 used electro‐acupuncture on non‐acupoints, two studies 59 , 62 used shallow acupuncture (2–5 mm) on non‐acupoints with no electric current, and one study 25 used shallow electro‐acupuncture (5–10 mm) on non‐acupoints (Table S2). Acupuncture has a significantly better effect on symptom improvement than sham acupuncture (RR 1.69, 95% CI 1.37–2.08, I2 = 79%) (Fig. 3). The overall quality of the evidence for this outcome was low because of the high risk of bias (uncertain blinding) and substantial heterogeneity based on GRADE analysis (Table 1).
FIGURE 3.
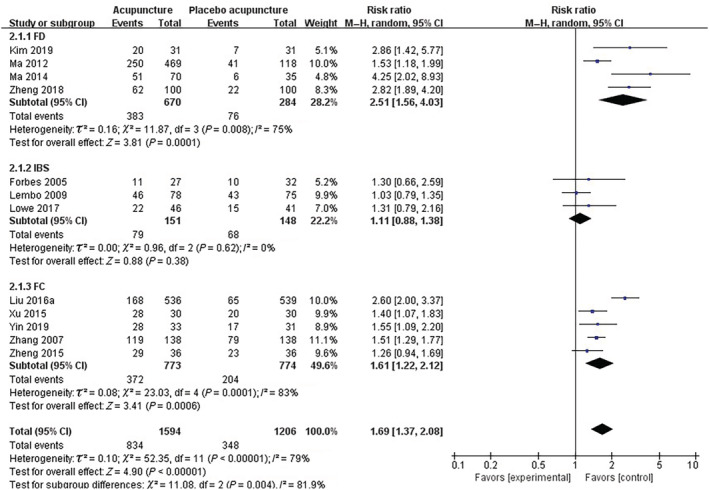
Forest plot of comparison of efficacy: Acupuncture versus placebo acupuncture for functional gastrointestinal disorders. IBS, irritable bowel syndrome; FD, functional dyspepsia; FC, functional constipation.
In the subgroup analysis, the pooled results illustrated that AT was better than sham acupuncture in alleviating symptoms for FD (RR 2.51, 95% CI 1.56–4.03) and FC (RR 1.61, 95% CI 1.22–2.12), but not for IBS (RR 1.11, 95% CI 0.88–1.38); the finding for the IBS subgroup was consistent with that of a previous meta‐analysis. 70 In addition, all three studies in the IBS subgroup showed ‘low risk’ based on the assessment of risk of bias, and they explicitly reported blinding of patients and evaluators, although the acupuncturists were not blinded. Due to the particularity of acupuncture, the absence of blinding amongst acupuncturists had a substantial effect on the experimental outcome. Moreover, the three studies in the IBS subgroup were completed in the USA, UK, and Canada, whilst the studies in the other two subgroups were conducted in China; we could not rule out the effect of national differences on the results. For the FD subgroup, there was no heterogeneity (I2 = 0%) after removing the RCT 25 (Ma 2012), and the difference was still statistically significant (RR 3.04, 95% CI 2.22–4.17). For the FC subgroup, there was also no heterogeneity (I2 = 0%) after removing the RCT 59 (Liu 2016a), and the pooled result remained statistically significant (RR 1.45, 95% CI 1.29–1.63), which could be attributed to the large sample size of these two RCTs. 25 , 59
Acupuncture as an adjuvant intervention to other active treatments
A total of 13 RCTs compared AT plus active therapeutics with other active therapeutics. For the active therapeutics, eight trials 21 , 26 , 33 , 34 , 50 , 55 , 57 , 63 , 66 used Chinese herbal medicine and four studies 9 , 11 , 13 , 17 used pharmacotherapy. The pooled results (Fig. 4) indicated that AT as an adjuvant intervention to other active therapeutics is beneficial to improve clinical efficacy (RR 1.25, 95% CI 1.21–1.30, I2 = 42%), and the quality of evidence was moderate based on GRADE analysis (Table 1). Moreover, results of the three subgroup analyses of FD (RR 1.30, 95% CI 1.22–1.38), IBS (RR 1.25, 95% CI 1.16–1.35), and FC (RR 1.20, 95% CI 1.13–1.28) also supported this finding. For the FD subgroup, there was no heterogeneity (I2 = 0%) after removing the RCT 11 (Chuang 2019), and the difference was still statistically significant (RR 1.21, 95% CI 1.14–1.28). The possible reason for the heterogeneity was the extremely high methodological quality of this RCT (low risk in seven items), which is far from the quality of research methods in other studies.
FIGURE 4.
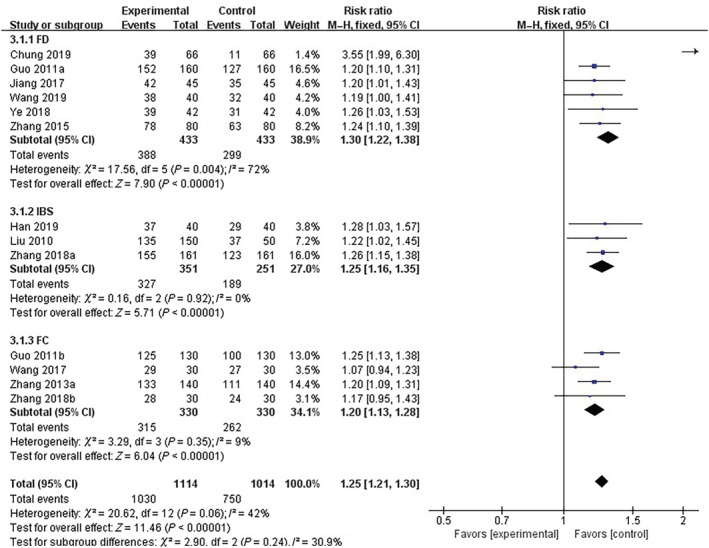
Forest plot of comparison of efficacy: Acupuncture as an adjuvant to other active treatments for functional gastrointestinal disorders. IBS, irritable bowel syndrome; FD, functional dyspepsia; FC, functional constipation.
Acupuncture versus no specific treatment
Four RCTs that compared acupuncture with no specific treatment were conducted in Korea, 19 USA, 52 UK, 46 and China. 36 Two studies 19 , 52 compared acupuncture with waiting, and two studies 36 , 46 compared acupuncture with usual care. The pooled result (Fig. 5) showed that AT was superior to no specific treatment in symptom improvement (RR 1.86, 95% CI 1.31–2.62, I2 = 63%), and the quality of evidence was low based on GRADE analysis (Table 1). Heterogeneity was reduced in the subgroup analysis, and the results of the subgroup analysis (Fig. 5) showed that such superiority is present not only in the FD subgroup (RR 23.19, 95% CI 3.29–163.46) but also in the IBS subgroup (RR 1.73, 95% CI 1.44–2.08).
FIGURE 5.
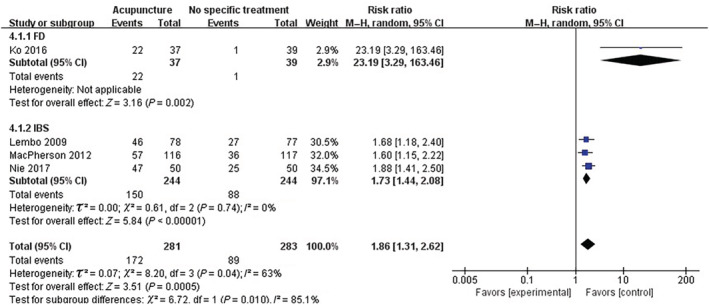
Forest plot of comparison of efficacy: Acupuncture vs no specific treatment for functional gastrointestinal disorders. IBS, irritable bowel syndrome; FD, functional dyspepsia; FC, functional constipation.
Adverse events
Amongst the included RCTs, 30 studies reported on adverse events (Table S1), of which ten studies showed that the number of adverse events in the study groups was zero. No serious adverse events occurred in 30 studies. Moreover, four studies 10 , 25 , 46 , 59 described the details of the assessment of acupuncture‐related adverse events, including broken needles, nausea/syncope during acupuncture, persistent severe pain/haematoma around the acupuncture site, bleeding/numbness/infection around the acupuncture site, and insomnia/dizziness/other discomfort after acupuncture.
In addition, we used numbers of ‘as‐treated’ to analyze the occurrence of adverse events. The pooled result (Fig. 6) indicated that the incidence of adverse events of AT was relatively lower than that of other treatments (RR 0.75, 95% CI 0.56–0.99, I2 = 9%), although the level of evidence was low because of inconclusive allocation concealment and blinding (Table 1).
FIGURE 6.
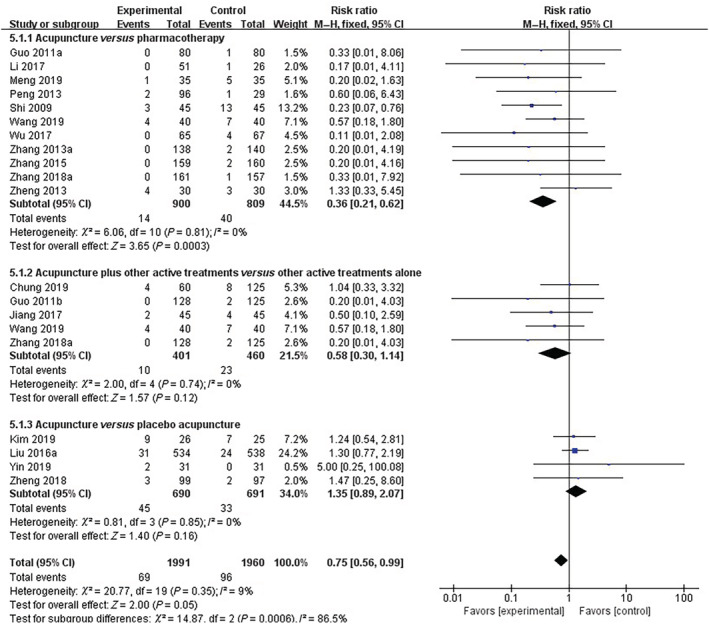
Forest plot of comparison of adverse events.
Subgroup analysis (Fig. 6) found that the number of adverse events of AT was lower than that of pharmacotherapy (RR 0.36, 95% CI 0.21–0.62), and AT used as an adjunct therapy to other active treatments did not increase the number of adverse events (RR 0.58, 95% CI 0.30–1.14). The incidence of adverse events was not statistically different between AT and sham acupuncture (RR 1.35, 95% CI 0.89–2.07).
Sensitivity analyses
For all of the aforementioned comparisons, the statistical significance of the meta‐analysis results has not changed, regardless of whether the analysis adopted a random‐effects or fixed‐effects model.
Publication bias
For 40 RCTs on acupuncture versus pharmacotherapy, funnel plot (Fig. S3 ‐A1) and Egger's test (P = 0.0000) suggested possible publication bias. After supplementing 15 studies based on trim‐and‐fill analysis, the funnel plot (Fig. S3 ‐A2) was symmetrically distributed. In addition, the log risk‐ratio (95% CI) was statistically significant both before and after trim‐and‐fill analysis (Table S3), thereby demonstrating that the conclusion would not be affected by publication bias.
Moreover, the funnel plot (Fig. S3 ‐B) of acupuncture versus placebo acupuncture was symmetrical, indicating absence of publication bias, which is supported by the results of Egger's test (P = 0.1173). In addition, the funnel plot of acupuncture as an adjuvant therapy (Fig. S3‐C) and Egger's test (P = 0.0683) both showed no potential publication bias. The funnel plot of adverse events (Fig. S3‐E) and Egger's test (P = 0.8309) also showed no potential publication bias. As there were only four studies on the comparison between acupuncture and moxibustion without specific treatment, there was no need to test for publication bias.
Discussion
This meta‐analysis included 61 RCTs. We compared AT with pharmacotherapy, no specific treatment, placebo acupuncture and AT as adjuvant therapy. Our pooled results show that AT is relatively effective at relieving symptoms in patients with FGIDs. Only a few adverse events attributable to acupuncture were found amongst the 18 RCTs. However, heterogeneity and high risk of bias lowered our level of certainty surrounding this evidence.
Acupuncture is part of traditional Chinese medicine (TCM), acupuncture theory believes that the human body is connected through meridians. Physical stimuli (needle, heat, pressure, etc.) are used to activate the acupuncture points on meridians to improve the body's self‐regulation ability and potentially hasten recovery. Most forms of acupuncture use disposable stainless steel needles, each of which is slightly thicker than human hair. These needles are inserted into “acupuncture points” on the skin. The inserted needle may rotate, move up and down at different speeds and depths, be heated, or be charged with a weak current. The mechanism of AT of FGIDs remains unclear. Past experiments 14 , 21 , 71 have attempted to reveal the underlying mechanisms of acupuncture on cerebral activity, the brain‐intestine axis, gastrointestinal hormones, and other sub‐systems. Amongst the 61 RCTs on FGIDs, more than 126 acupuncture points were used according to TCM syndromes and personalized diagnosis. In the included studies, the most commonly adopted acupoints were ST36, CV12, and PC6 for the treatment of FD; ST36, SP6, and ST25 for IBS; and ST37 and BL25 for FC. Clinically, special combinations of acupuncture points are often used, such as Shu‐Mu acupoint coordination. For example, in TCM, BL2 and CV12 are the Shu‐point and Mu‐point of the stomach, respectively; thus, they are a common acupuncture prescription for FD. Moreover, BL25 and ST25 are compatible and are generally used for the treatment of FC. The efficacy of acupuncture is affected by several factors, such as the combination of different acupuncture points, special acupoint selection, and the depth of acupuncture. Future follow‐up trials and network meta‐analysis on acupoint formulae and the most promising acupuncture methods are warranted. No medical treatment method could exclude the subjective impressions of patients. Thus, to affirm the objectivity of the efficacy of acupuncture, placebo acupuncture is necessary. Placebo acupuncture is also called ‘sham acupuncture’, which is the same as the placebo in drug research. We summarized the operation of sham acupuncture of included RCTs, including non‐acupoints, non‐therapeutic acupoints, shallow acupuncture, non‐penetrating acupuncture, electro‐acupuncture without current/with little current (Table S2). Of the 61 studies, 12 studies used sham acupuncture, and the pooled results showed that AT is better than sham acupuncture in alleviating symptoms of FD (RR 2.51, 95% CI 1.56–4.03) and FC (RR 1.96, 95% CI 1.07–3.62). However, in the IBS subgroup, the results did not show statistical differences (RR 1.11, 95% CI 0.88–1.38). The efficacy of sham acupuncture is controversial, as no perfect placebo needle method exists, a reasonable design is used to minimize the therapeutic effect of placebo acupuncture, which in turn allows for better verification of the therapeutic effect of acupuncture.
In contrast to previous meta‐analyses on acupuncture for FGIDs, 70 , 72 , 73 this study assessed the efficacy of acupuncture for FD, IBS, FC using a subgroup analyses of the different diseases. In addition, we have added new RCTs that were not included in previous meta‐analyses and made a variety of comparisons, including AT versus drug treatment, acupuncture versus waiting in a queue, acupuncture versus placebo acupuncture, and acupuncture as an adjuvant therapy for other treatments. These comparisons demonstrated the efficacy of acupuncture for FD, IBS, and FC. However, most of the RCTs included in this study had limitations, including a lack of a rigorous study design, detailed description of the methodology, and standardized evaluation of the efficacy. The most common methodological flaw was deficient reporting of allocation concealment and blinding. The incomplete report of blinding is one of the main reasons for downgrading the assessment of the GRADE evidence in this study. Furthermore, another limitation of this study is that only RCTs with dichotomous results were selected and evaluated, in order to reduce heterogeneity. Therefore, to avoid loss bias and improve the robustness of the data, all the original data in this meta‐analysis were re‐analyzed based on the ITT priniciple. 8
Well‐implemented blinding or masking methods could reduce measurement bias and placebo effects. Amongst the included studies, 11 studies were double‐blind RCTs, 10 studies reported patient blinding, and 11 of these 21 studies reported blinding of the efficacy assessors. Double‐blinding is difficult to achieve given the role of communication between the therapist and the patient during acupuncture. To conduct double‐blind experiments with acupuncture, Takakura et al. 74 designed a double‐blind, non‐penetrating placebo needle that could be easily pressed into the skin with matching penetrating power. The needle is encased in an opaque catheter, and the look and feel of this needle is indistinguishable from the actual needle (i.e. neither the therapist nor the patient knows if the needle penetrates the skin). Several studies have used double‐blind placebo needles. However, there is a persistent gap between double‐blind placebo needles trials and flexible application in AT clinical practice. In recent years, nonblinded pragmatic trials have been used to achieve clinically relevant results. Such trials emphasize practical applicability and extrapolation in real‐world situations. This design is particularly appropriate for researching complex and flexible interventions, 75 such as acupuncture. To avoid the introduction of bias, efficacy assessors and statisticians should be blinded throughout nonblinded pragmatic trials.
To improve the quality of acupuncture research, TCM symptoms of patients and personalized AT deserve attention. Moreover, randomization of clinical study cases ensures comparability between observation and control groups. However, most researchers ignore the extraction and analysis of TCM dialectical data when checking the balance of basic data in each group. From the perspective of TCM, it is difficult to determine the comparability between groups without dialectical data because of the basis of AT originates from the dialectical treatment of TCM. Moreover, in a clinical control study, establishing a blank control group is helpful to objectively evaluate the efficacy of acupuncture. AT is a traditional medicine that continues to face obstacles, such as the lack of evidence of clinical effectiveness and safety. Thus, high quality double‐blind RCTs that provide reliable clinical evidence on the safety of AT, which could enable patients to be provided with improved treatment options, are needed.
Conclusions
This meta‐analysis found that AT was significantly associated with relief of FGIDs symptoms; however, the evidence level was moderate or low. Our study is limited by the quality of methodology—and its corresponding high risk of bias—heterogenous diagnostic and evaluation criteria, the small sample size, and the diversity of acupuncture interventions. Future, rigorously designed RCTs are needed to provide reliable evidence to verify the effectiveness and safety of AT as a treatment for FGIDs.
Funding Support
This research was supported by National Natural Science Foundation of China (No.81973936).
Supporting information
Figure S1. Risk of bias graph: review authors' judgments about each risk of bias item presented as percentages across all included studies.
Figure S2. Risk of bias summary: review authors' judgments about each risk of bias items for each included study.
Figure S3. Funnel plot of comparison, IBS, irritable bowel syndrome; FD, functional dyspepsia; FC, functional constipation.
Table S1. Characteristics of the included studies.
Table S2. Types of sham acupuncture.
Table S3. Trim and fill analysis.
Table S4. Search strategies.
Wang, X. , Wang, H. , Guan, Y. , Cai, R. , and Shen, G. (2021) Acupuncture for functional gastrointestinal disorders: A systematic review and meta‐analysis. Journal of Gastroenterology and Hepatology, 36: 3015–3026. 10.1111/jgh.15645.
Author contribution: GMS and XYW designed the study; YYG and RLC extracted data; XYW and HW analyzed and interpreted the data, XYW wrote the manuscript; GMS approved the manuscript.
Declaration of conflict of interest: The authors declare no conflict of interest.
References
- 1. Drossman DA, Hasler WL. Rome IV‐functional gi disorders: disorders of gut‐brain interaction. Gastroenterology 2016; 150: 1257–1261. [DOI] [PubMed] [Google Scholar]
- 2. Brandt LJ, Chey WD, Foxx‐Orenstein AE et al. An evidence‐based position statement on the management of irritable bowel syndrome. Am. J. Gastroenterol. 2009; 104: S1–S35. [DOI] [PubMed] [Google Scholar]
- 3. Ouyang H, Chen J. Therapeutic roles of acupuncture in functional gastrointestinal disorders. Aliment. Pharmacol. Ther. 2004; 20: 831–841. [DOI] [PubMed] [Google Scholar]
- 4. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group . Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. Int. J. Surg. 2010; 8: 336–341. [DOI] [PubMed] [Google Scholar]
- 5. Drossman DA. The functional gastrointestinal disorders and the Rome II process. Gut 1999; 45: II1–II5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Drossman DA. The functional gastrointestinal disorders and the Rome III process. Gastroenterology 2006; 130: 1377–1390. [DOI] [PubMed] [Google Scholar]
- 7. Drossman DA. The Functional Gastrointestinal Disorders: Diagnosis, Pathophysiology, and Treatment: A Multinational Consenus. Little Brown & Company, 1994. [Google Scholar]
- 8. Higgins J, Wells G. Cochrane Handbook for Systematic Reviews of Interventions. 2011. [Google Scholar]
- 9. Wang W. Clinical value of compound digestive enzyme capsule combined with acupuncture in the treatment of functional dyspepsia. Chin. J. Convalescent. Med. 2019; 28: 585–586. [Google Scholar]
- 10. Kim MR, Li HW, Yang JW et al. Observation on therapeutic effect of acupuncture at "experienced ten acupoints" for postprandial distress syndrome. Zhongguo Zhen Jiu 2019; 39: 1165–1168. [DOI] [PubMed] [Google Scholar]
- 11. Chung VCH, Wong CHL, Wu IXY et al. Electroacupuncture plus on‐demand gastrocaine for refractory functional dyspepsia: Pragmatic randomized trial. J. Gastroenterol. Hepatol. 2019; 34: 2077–2085. [DOI] [PubMed] [Google Scholar]
- 12. Zheng H, Xu J, Sun X et al. Electroacupuncture for patients with refractory functional dyspepsia: a randomized controlled trial. Neurogastroenterol. Motil. 2018; 30: e13316. [DOI] [PubMed] [Google Scholar]
- 13. Ye Y, Zhu LB, Tan YG. Therapeutic observation of three‐segment point selection plus mosapride for functional dyspepsia. Shanghai J. Acu‐Mox. 2018; 37: 1136–1139. [Google Scholar]
- 14. Qiang L, Jiang Y. Electroacupuncture for functional dyspepsia and the influence on serum Ghrelin, CGRP and GLP‐1 levels. World J. Acupunct. Moxibustion. 2018; 28: 86–90. [Google Scholar]
- 15. Dai M, Fang XY, Wu YW et al. Clinical study of needling the three abdominal acupoints for functional dyspepsia. Shanghai J. Acu‐Mox. 2018; 37: 599–604. [Google Scholar]
- 16. Liu X, Li XL, Li YX et al. Clinical observation on the Yuan‐Luo acupuncture treatment of functional dyspepsia. JCAM 2017; 33: 56–58. [Google Scholar]
- 17. Jiang GD. Clinical curative effect and EGG changes of functional dyspepsia treated by acupuncture combined with medicine. JCAM 2017; 33: 20–23. [Google Scholar]
- 18. Peng KM, Luo P. Clinical observation of acupuncture and moxibustion for functional dyspepsia with emotional disorder. JCAM 2016; 32: 1–4. [PubMed] [Google Scholar]
- 19. Ko SJ, Kuo B, Kim SK et al. Individualized acupuncture for symptom relief in functional dyspepsia: a randomized controlled trial. J. Altern. Complement. Med. 2016; 22: 997–1006. [DOI] [PubMed] [Google Scholar]
- 20. Zhao J, Yan HL, Liu N, Shi ZM. Ziwuliuzhu acupuncture combined with dialectical acupoints in the treatment of 60 cases with functional dyspepsia. JETCM 2015; 24: 1636–1638. [Google Scholar]
- 21. Zhang CX, Guo LK. Dalitong granule combined with electroacupuncture in the treatment of functional dyspepsia: a randomized controlled trial. Chin. J. Integr. Med. 2015; 21: 743–750. [DOI] [PubMed] [Google Scholar]
- 22. Zhou L, Hu Y, Sun GJ. Clinical observation of acupuncture based on syndrome differentiation in improving the quality of life in patients with functional dyspepsia. Shanghai J. Acu‐Mox. 2014: 718–721. [Google Scholar]
- 23. Ma CY, Huang Q, Wan WJ et al. Effects of syndrome‐differentiation acupuncture on life quality in patients with functional dyspepsia. Zhongguo Zhen Jiu 2014; 34: 125–129. [PubMed] [Google Scholar]
- 24. Zheng XY, Song X, Jiang XY, Zhang GZ, Chen JQ. Clinical observation of acupuncture for treatment of Pi Wei Qi deficiency functional dyspepsia. J. Trop. Med. 2013; 13: 232–234. [Google Scholar]
- 25. Ma TT, Yu SY, Li Y et al. Randomised clinical trial: an assessment of acupuncture on specific meridian or specific acupoint vs. sham acupuncture for treating functional dyspepsia. Aliment. Pharmacol. Ther. 2012; 35: 552–561. [DOI] [PubMed] [Google Scholar]
- 26. Guo LK, Zhang CX, Guo XF. Long‐term efficacy and safety research on functional dyspepsia treated with electroacupuncture and Zhizhu Kuanzhong capsule. Zhongguo Zhen Jiu 2011; 31: 1071–1077. [PubMed] [Google Scholar]
- 27. Shi HJ, Zhang JQ, Guo H. Clinical observation of acupuncture and moxibustion in treating 90 cases of functional dyspepsia. Beijing J. Tradit. Chin. Med. 2009; 28: 732–733. [Google Scholar]
- 28. Tang SX, Xu ZH, Tang P, Liang LX. Clinical control study on acupuncture treatment of functional dyspepsia. J. Sichuan Tradit. Chin. Med. 2006; 24: 101–102. [Google Scholar]
- 29. Liu W, Wang J, Hao Z. Clinical study on effect of acupuncture on gastrointestinal motility in the patient of functional dyspepsia. Zhongguo Zhen Jiu 2001; 21: 267–269. [Google Scholar]
- 30. Zou W, Mao JY, Liu M, Yu T. Clinical study on warm acupuncture treatment of diarrhea irritable bowel syndrome with spleen‐stomach deficiency syndrome. Shaanxi J. Tradit. Chin. Med. 2019; 40: 1786–1788. [Google Scholar]
- 31. Zhang X, Ding M, Feng H. Acupuncture with Du's heat‐reinforcing method for diarrhea‐predominant irritable bowel syndrome: a randomized controlled trial. J. Acupunct. Tuina Sci. 2019; 17: 124–130. [Google Scholar]
- 32. Meng GJ. Acupuncture treatment for depressive symptom in diarrhea‐predominant irritable bowel syndrome: a randomized controlled study. J. Acupunct. Tuina Sci. 2019; 17: 422–426. [Google Scholar]
- 33. Han ZC, Ren LL, Lu F, Ruan CC, Tang BB. Analysis of the acupuncture combined with traditional Chinese medicine in the treatment of diarrhea‐predominant pattern irritable bowel syndrome patients. Chin. J. Gen. Pract. 2019; 17: 1911–1913. [Google Scholar]
- 34. Zhang C, Guo L, Wang Y, Zhang L, Chang T. Electroacupuncture combined with qibei mixture for diarrhea‐predominant irritable bowel syndrome: a randomized controlled trial. WJAM 2018; 28: 19–24. [Google Scholar]
- 35. Qin Y, Yi W, Lin S, Yang C, Zhuang Z. Clinical effect of abdominal acupuncture for diarrhea irritable bowel syndrome. Zhongguo Zhen Jiu 2017; 37: 1265–1268. [DOI] [PubMed] [Google Scholar]
- 36. Nie XN. A randomized controlled study of head and body acupuncture needling method in treatment of diarrhea type irritable bowel syndrome. J. Chengdu Univ. Tradit. Chin. Med. 2017; 40. [Google Scholar]
- 37. Lowe C, Aiken A, Day AG, Depew W, Vanner SJ. Sham acupuncture is as efficacious as true acupuncture for the treatment of IBS: a randomized placebo controlled trial. Neurogastroenterol. Motil. 2017; 29: e13040. [DOI] [PubMed] [Google Scholar]
- 38. Li J, Lu J, Sun J et al. Acupuncture with regulating mind and spleen for diarrhea irritable bowel syndrome and sleep quality: a randomized controlled trial. Zhongguo Zhen Jiu 2017; 37: 9–13. [DOI] [PubMed] [Google Scholar]
- 39. Shi ZM, Li XQ, Liu LN, Liu JP, Guo YJ, Zhou H. Ziwu Liuzhu acupuncture treatment of irritable bowel syndrome. JCAM 2015; 31: 37–39. [Google Scholar]
- 40. Pei L, Zhu L, Sun J, Wu X, Chen L. Constipation predominant irritable bowel syndrome treated with acupuncture for regulating the mind and strengthening the spleen: a randomized controlled trial. Zhongguo Zhen Jiu 2015; 35: 1095–1098. [PubMed] [Google Scholar]
- 41. Li XQ, Mu SY, Lu Q, Lu X. Therapeutic observation of diarrhea‐predominant irritable bowel syndrome majorly treated by acupuncture with Ling Gui Ba Fa. Shanghai J. Acu‐Mox. 2015; 34: 22–24. [Google Scholar]
- 42. Zhan DW, Sun JH, Luo KT et al. Effects and efficacy observation of acupuncture on serum 5‐HT in patients with diarrhea‐predominant irritable bowel syndrome. Zhongguo Zhen Jiu 2014; 34: 135–138. [PubMed] [Google Scholar]
- 43. Wu XL, Wang YL, Sun JH et al. Clinical observation on acupuncture for diarrhea‐predominant irritable bowel syndrome patients in syndrome of liver‐stagnation and spleen‐deficiency and its impact on Th1/Th2. Zhongguo Zhen Jiu 2013; 33: 1057–1060. [PubMed] [Google Scholar]
- 44. Li H, Pei LX, Zhou JL, Sun JH. Controlled observation on the efficacy of acupuncture and western medicine on diarrhea‐type irritable bowel syndrome. WJAM 2013; 23: 11–16. [Google Scholar]
- 45. Ge JJ, Zeng KX. Efficacy observation on warm needling for 60 cases of diarrhea irritable bowel syndrome. WJAM 2013; 23: 43–51+45. [Google Scholar]
- 46. MacPherson H, Tilbrook H, Bland JM et al. Acupuncture for irritable bowel syndrome: primary care based pragmatic randomised controlled trial. BMC Gastroenterol. 2012; 12: 150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Chen YH, Chen XK, Yin XJ. Comparison of the therapeutic effects of electroacupuncture and probiotics combined with deanxit in treating diarrhea‐predominant irritable bowel syndrome. Chin. J. Integr. Tradit. West Med. 2012; 32: 594–598. [PubMed] [Google Scholar]
- 48. Sun JH, Wu XL, Xia C et al. Clinical evaluation of Soothing Gan and invigorating Pi acupuncture treatment on diarrhea‐predominant irritable bowel syndrome. Chin. J. Integr. Med. 2011; 17: 780–785. [DOI] [PubMed] [Google Scholar]
- 49. Shi ZM, Zhu YS, Wang QX, Lei MN. Comparative study on irritable bowel syndrome treated with acupuncture and western medicine. Zhongguo Zhen Jiu 2011; 31: 607–609. [PubMed] [Google Scholar]
- 50. Liu QQ, Wang ZK, Zhang W. Clinical observation on Geshanxiaoyao decoction combining acupuncture effect on the life quality of patients with irritable bowel syndrome. J. Zhejiang Chin. Med. Univ. 2010; 34: 510–1+3. [Google Scholar]
- 51. An G, Li N, Zhai G, Liu H, Sun J, Liang H. Evaluation of the therapeutic effect of acupuncture and moxibustion on irritable bowel syndrome. Shanghai J. Acu‐Mox. 2010; 29: 354–356. [Google Scholar]
- 52. Lembo AJ, Conboy L, Kelley JM et al. A treatment trial of acupuncture in IBS patients. Am. J. Gastroenterol. 2009; 104: 1489–1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Forbes A, Jackson S, Walter C, Quraishi S, Jacyna M, Pitcher M. Acupuncture for irritable bowel syndrome: a blinded placebo‐controlled trial. World J. Gastroenterol. 2005; 11: 4040–4044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Yin Y. Li Jiao Tong Fu's needling method for functional constipation: a randomized controlled study. Shanghai J. Acu‐Mox. 2019; 38. [Google Scholar]
- 55. Zhang C, Chen BG, Zhng XA. Observation on treating functional constipation of the Xuexu Changzao type by electroacupuncture at Baliao acupoint combined with the Mibaokang decoction. CJCM 2018; 10: 108–110. [Google Scholar]
- 56. Wu X, Zheng C, Xu X et al. Electroacupuncture for functional constipation: a multicenter, randomized, control trial. Evid. Based Complement. Alternat. Med. 2017; 2017: 1428943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Wang B, Chen Y, Chen S. Clinical observation of slow transit constipation treated with acupuncture and modified weitong xiaopi formula. Zhongguo Zhen Jiu 2017; 37: 130–134. [DOI] [PubMed] [Google Scholar]
- 58. Mao Z, Zhang H. Therapeutic observation of electroacupuncture and prucalopride succinate tablets for functional constipation. Shanghai J. Acu‐Mox. 2016; 35: 926–929. [Google Scholar]
- 59. Liu Z, Yan S, Wu J et al. Acupuncture for chronic severe functional constipation: a randomized trial. Ann. Intern. Med. 2016; 165: 761–769. [DOI] [PubMed] [Google Scholar]
- 60. Liu K, Cai GF, Shang LL, Sun H. Effect of abdominal electroacupuncture on functional constipation. JCAM 2016; 32: 42–44. [Google Scholar]
- 61. Zheng HB, Chen Y. A clinical randomized controlled trial of acupuncture at the combination of back‐shu point and front‐mu point of large intestine meridian in the treatment of functional constipation. PJCM 2015: 57–59. [Google Scholar]
- 62. Xu HF, Zhang HX. Therapeutic observation of electroacupuncture for functional constipation. Shanghai J. Acu‐Mox. 2015: 214–217. [Google Scholar]
- 63. Zhang C, Liu Z‐L, Zhou Y et al. Clinical effect assessment on therapy of electric acupuncture of yangming meridian for functional constipation with slow transmission. Chin. J. Basic Med. Tradit. Chin. Med. 2013; 19: 684–686. [Google Scholar]
- 64. Zhang C, Guo L, Guo X, Li G, Guo X. Short and long‐term efficacy of combining Fuzhengliqi mixture with acupuncture in treatment of functional constipation. J. Tradit. Chin. Med. 2013; 33: 51–59. [DOI] [PubMed] [Google Scholar]
- 65. Peng WN, Wang L, Liu Z, S, et al. Analysis on follow‐up efficacy and safety of slow transit constipation treated with individualized deep puncture at Tianshu (ST 25): a multi‐central randomized controlled trial. Zhongguo Zhen Jiu 2013; 33: 865–869. [PubMed] [Google Scholar]
- 66. Guo LK, Zhang CX, Guo XF. Acupuncture combined with Chinese herbal medicine Plantain and Senna granule in treatment of functional constipation: a randomized, controlled trial. Zhong Xi Yi Jie He Xue Bao 2011; 9: 1206–1214. [DOI] [PubMed] [Google Scholar]
- 67. Yang DL, Liu ZS. Observation of deep acupuncture at tianshu for functional constipation. Beijing J. Tradit. Chin. Med. 2010; 29: 366–368. [Google Scholar]
- 68. Wang CW, He HB, Li N et al. Observation on therapeutic effect of electroacupuncture at Tianshu (ST 25) with deep needling technique on functional constipation. Zhongguo Zhen Jiu 2010; 30: 705–708. [PubMed] [Google Scholar]
- 69. Zhang ZL, Ji XQ, Zhao SH et al. Multi‐central randomized controlled trials of electroacupunture at Zhigou (TE 6) for treatment of constipation induced by stagnation or deficiency of qi. Zhongguo Zhen Jiu 2007; 27: 475–478. [PubMed] [Google Scholar]
- 70. Manheimer E, Cheng K, Wieland LS et al. Acupuncture for treatment of irritable bowel syndrome. Cochrane Database Syst. Rev. 2012; 5: Cd005111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Yu Z. Neuromechanism of acupuncture regulating gastrointestinal motility. World J. Gastroenterol. 2020; 26: 3182–3200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Lan L, Zeng F, Liu GJ et al. Acupuncture for functional dyspepsia. Cochrane Database Syst. Rev. 2014; 10: CD008487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Wang L, Xu M, Zheng Q et al. The Effectiveness of Acupuncture in Management of Functional Constipation: A Systematic Review and Meta‐Analysis. Evid. Based Complement. Alternat. Med. 2020; 2020: 6137450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Takakura N, Yajima H. A double‐blind placebo needle for acupuncture research. BMC Complement. Altern. Med. 2007; 7: 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Sox HC, Lewis RJ. Pragmatic trials: practical answers to “real world” questions. JAMA 2016; 316: 1205–1206. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Risk of bias graph: review authors' judgments about each risk of bias item presented as percentages across all included studies.
Figure S2. Risk of bias summary: review authors' judgments about each risk of bias items for each included study.
Figure S3. Funnel plot of comparison, IBS, irritable bowel syndrome; FD, functional dyspepsia; FC, functional constipation.
Table S1. Characteristics of the included studies.
Table S2. Types of sham acupuncture.
Table S3. Trim and fill analysis.
Table S4. Search strategies.


