Abstract
Objectives
The aim of this study was: (1) to adapt the time‐driven activity‐based costing (TDABC) method to emergency department (ED) ambulatory care; (2) to estimate the cost of care associated with frequently encountered ambulatory conditions; and (3) to compare costs calculated using estimated time and objectively measured time.
Methods
TDABC was applied to a retrospective cohort of patients with upper respiratory tract infections, urinary tract infections, unspecified abdominal pain, lower back pain and limb lacerations who visited an ED in Québec City (Canada) during fiscal year 2015–2016. The calculated cost of care was the product of the time required to complete each care procedure and the cost per minute of each human resource or equipment involved. Costing based on durations estimated by care professionals were compared to those based on objective measurements in the field.
Results
Overall, 220 care episodes were included and 3080 time measurements of 75 different processes were collected. Differences between costs calculated using estimated and measured times were statistically significant for all conditions except lower back pain and ranged from $4.30 to $55.20 (US) per episode. Differences were larger for conditions requiring more advanced procedures, such as imaging or the attention of ED professionals.
Conclusions
The greater the use of advanced procedures or the involvement of ED professionals in the care, the greater is the discrepancy between estimated‐time‐based and measured‐time‐based costing. TDABC should be applied using objective measurement of the time per procedure.
Keywords: emergency medicine, emergency service, financial Management, hospital/methods, hospital/organization & administration, Time‐driven activity‐based costing
1. INTRODUCTION
1.1. Background
Most developed countries are struggling with the urgency of balancing the ever‐growing medical needs of aging populations against limited availability of healthcare resources. 1 , 2 , 3 , 4 , 5 The challenge of providing care efficiently, meaning maximizing healthcare services and patient outcomes while minimizing resource use and costs, 6 , 7 is felt in all departments, including the emergency department (ED). However, most current ED costing systems (eg, relative intensity weights) do not inform decision makers sufficiently to allow easy detection of under‐utilization and over‐utilization of human or material resources and hence opportunities to improve the quality/cost ratio of the services provided. 8 , 9
1.2. Importance
To identify inefficient resource use, a reliable and precise costing method is needed. Time‐driven activity‐based costing (TDABC) has been proposed for this purpose. 10 , 11 TDABC determines patient costs by allocating all direct (eg, staff salaries) and overhead (eg, building maintenance) expenses to activities related to patient care. 12 , 13 Unlike traditional activity‐based costing methods, it uses time as a cost driver: expense is directly proportional to the time a patient spends receiving care. TDABC has been used successfully in many care settings, such as general surgery, 14 , 15 outpatient clinics, 16 and orthopedics, 17 but its use in the ED has seldom been examined. 8 Designed to estimate the cost of linear and homogenous care pathways, such as coronary bypass grafting, 18 TDABC requires adaptation for use in the ED setting, where illness severity varies considerably from low to high, and multiple paths of care (ambulatory care, stretchers, resuscitation) with little standardization between clinicians are the rule rather than the exception. Ambulatory care appears to be the most suitable ED section for initial testing of this costing method, because the paths of care are simpler, more linear, and more homogenous than in the stretcher area.
1.3. Goals of the investigation
Our aims were therefore (1) to adapt TDABC to ED ambulatory care; (2) to estimate the cost of care for frequently encountered ambulatory conditions; and (3) to compare the costs calculated using time estimated by care staff and time measured objectively.
2. METHODS
2.1. Study design and setting
Our study of the cost of ambulatory patient care in the ED comprised 2 phases:
Use of TDABC to estimate the cost of specific care procedures (eg, triage); and
Application of costs estimated in phase 1 to a retrospective cohort of patients to calculate the total cost of care for specific patient conditions.
The study took place during fiscal year 2015–2016 (April to March) at the CHUL, a tertiary care hospital located in Québec city (Canada) with a total ED census of approximately 77,000 adult and pediatric visits per year, including around 45,000 ambulatory patients. This ED is composed of 4 different areas each with its own staff, namely (1) the monitored stretcher area; (2) the unmonitored stretcher area (including a secure area for patients with mental health issues); (3) the resuscitation bay; and (4) the ambulatory area where patients with low‐acuity conditions not requiring a gurney are assessed. As explained in the introduction, this study focused on the latter.
Data collection and cost calculation were limited to the ED care episode, from patient arrival to discharge. We focused on 5 of the most common conditions seen in ED ambulatory care: (1) upper respiratory tract infection (URTI); (2) urinary tract infection (UTI); (3) lower back pain; (4) unspecified abdominal pain, defined as abdominal pain of undetermined cause upon discharge from the ED; and (5) minor lacerations on limbs, proximal or distal, necessitating only superficial closure without deep sutures or tendon repair. These conditions span the usual range of resource use intensity managed in most ED ambulatory care services.
2.2. Phase 1: The time‐driven activity‐based costing method
2.2.1. The steps constituting TDABC
The TDABC method estimates the cost of all procedures potentially applicable to patients throughout an ED care episode. In our case, this involved the following steps:
Process and resource mapping (eg, medical assessment) for each diagnosis through meetings with a team of experts representing all types of ED professionals and selected by the project steering committee (see Appendix SA1 for the composition of the team of experts).
Validation of process maps and durations by surveying the experts and by prospective in the field using time‐motion software (Laubrass UmtPlus Max, Appendix SA2).
Estimation of the annual capacity cost rate (in $/min) per resource (eg, nurses) and equipment (eg, X‐ray machine) as follows (Appendix SA3): Capacity cost rate = total annual expenditure/total minutes available for patient care per year. Annual expenses include compensation for hours worked, staff training and vacation, and equipment downtime and depreciation. Availability for patient care does not include staff vacation and training or time on breaks or equipment downtime. Student or resident involvement in patient care is highly variable. To improve the comparability of our results with those of non‐academic institutions, the cost of medical student training is not considered in our cost of care maps and models, in accordance with the approach adopted by the Canadian Institute for Health Information in its costing methodology. 19
Estimation of the annual cost of consumables (eg, gloves, needles, paper) in $/min in each department (eg, ED, radiology) involved in ED patient care, as follows (Appendix SA4): Cost of consumables = total annual cost/total staff‐minutes available for patient care.
Estimation of the overhead cost (eg, building maintenance) in $/min in each department involved in ED patient care, as follows (Appendix SA5): Overhead cost = annual overhead cost allocated/total staff‐minutes available for patient care.
Estimation of traceable supply costs (eg, medication, blood/urine analyses).
Calculation of the standard cost of each care procedure, by multiplying the duration by the sum of resource, consumable, and overhead costs, for example: Cost of ED triage = (nurse + consumables + overhead costs) × procedure duration = (0.77$/min + 0.07$/min + 0.17$/min) × 7.1 min = $7.17.
When applicable, the costs of traceable supplies (eg, medication) are added directly to this calculation (Appendix SA6).
2.2.2. Care process costs
The steps outlined above provide an estimation of the unit cost of each care procedure administered to ED ambulatory patients (eg, registration). The cost of minor laceration suturing by the physician was broken down to the cost per centimeter of wound and the cost of bronchodilator treatment, to the cost per puff administered.
2.2.3. TDABC approaches
The Bottom Line.
To improve emergency department (ED) costing systems, time‐driven activity‐based costing has been proposed. Using ambulatory care data from a low acuity Canadian ED, the study of 219 subjects found that, especially at higher cost of care, estimated times tend to underestimate true costs. Therefore, the authors recommend direct objective measurements from time stamps or logs in the ED.
Measurement of care process duration has been described previously as an optional step. In this study, direct observation was conducted between 2017 and 2019 by 12 different research assistants to measure the duration of ED care procedures. All measurements were prospective and not limited to the 5 patient conditions under study because the discharge diagnosis was not yet determined. Median duration was extracted from this database for each condition. Field measurement of certain short or rare procedures was not feasible. In these cases, cost was calculated using time estimated by the team of experts. To estimate the added value of an in‐situ time‐motion assessment, we generated 2 lists of care process costs using estimated duration (based on consensus among experts after three 6‐h in‐person meetings for mapping the 5 conditions under study) and using field measurement of care process median duration. The 2 lists of costs thus generated (estimated vs. measured) were used in the second phase to estimate the cost of each patient encounter.
2.2.4. Financial data sources
All financial data covering the study period, with the exception of data related to emergency physicians, were extracted from administrative databases and patient records by the accounting department at the local institution. The total annual cost for all ED physicians was obtained from a private billing agency hired by the local team (Agence de facturation MB inc.). This was used to calculate physician capacity cost using the method applied to the rest of the ED care staff. The participating ED is part of a universal, not‐for‐profit healthcare system where all hospital and physician expenses are covered by the government. Therefore, all costs estimated reflect the public payer perspective.
2.3. Phase 2: Retrospective cohort
2.3.1. Selection of participants
We reviewed the records of consecutive patients who visited the ED during fiscal year 2015–2016. Patients 18 years old and over, ambulatory throughout ED assessment, and discharged home from the ED with 1 of the 5 diagnoses of interest were included. Patients not covered by the provincial health insurance plan, having consulted for a similar problem in the previous 30 days, transferred from another ED or living in a long‐term care facility were excluded.
2.3.2. Measurements
Demographic and clinical data were retrieved retrospectively from local medical‐administrative records using a software tool or manually using a standardized abstraction form. The reliability of manual retrieval was tested by comparing reviews of 10% of the charts by 2 research assistants. The median weighted kappa statistic for manually collected variables was 0.85 (interquartile range [IQR], 0.57; 1), indicating strong inter‐observer agreement.
2.3.3. Outcomes
The primary outcome measurement was the mean cost of care for each condition of interest, based on time estimates by care professionals in comparison with objectively logged time. The secondary outcome measurement was the proportion of each cost element (eg, staff) relative to the total cost of care.
2.3.4. Analyses
Demographic characteristics and costs per condition are reported using means, medians, frequencies, and proportions, with 95% confidence intervals or IQRs where applicable. Measured times and estimated times were compared using a one‐sample Wilcoxon signed rank test. The cost per patient was calculated by summing the costs of all procedures performed during the ED episode, using both time values to calculate the unit cost, down to each centimeter of wound suturing and each puff of bronchodilator. Once the non‐Gaussian distribution of cost per patient was confirmed, the mean cost per condition was estimated and the 2 calculations were compared using bivariate generalized Gamma regression models with an Akaike information criterion. A Bland–Altman graph was plotted to visualize the agreement between costs based on estimated and measured times. Finally, the mean cost per patient for the whole cohort using measured time was broken down further to determine the proportions attributable to physicians, staff, diagnostic tests, treatments, consumables and overhead. Costs are reported in US dollars after applying the average conversion rate for the year 2016 according to the Bank of Canada (USD1 = CAD1.32). 20 All statistical tests were 2‐sided with the significance level set at P < 0.05 and were carried out using SAS Statistical Software v.9.4 (SAS Institute, Cary, NC). The study received approval from the CHU de Québec‐Université Laval research ethics committee (#2016‐2840).
3. RESULTS
3.1. Characteristics of study subjects
The study focused on 219 subjects (patients) representing 220 ED care episodes, 1 patient having presented twice with clinically unrelated lacerations, 6 months apart. Table 1 lists the recorded characteristics of the patients. The mean age of the cohort was 37.1 years. Women represented more than 60% of the patients in each condition category except superficial limb lacerations, in which men represented 67.6% of the patients. Most participants were of low‐acuity (59.4% with scores of 4 or 5 on the Canadian Triage and Acuity Scale) and presented no significant comorbidities (82.3% with score 0 on the Charlson Comorbidity Index). Median length of ED stay varied from 3.7 h for patients with an upper respiratory tract infection to 7.3 h for patients with unspecified abdominal pain.
TABLE 1.
Characteristics of patients (N = 219)
| Characteristics c | Upper respiratory tract infection | Urinary tract infection | Lower back pain | Unspecified abdominal pain | Laceration (limb) | Total |
|---|---|---|---|---|---|---|
| No. | 49 | 47 | 44 | 46 | 33 (34) a | 219 (220) a |
| Mean age (SD), y | 33.3 (10.2) | 36.3 (17.9) | 42.2 (18.2) | 36.8 (15.2) | 37.2 (18.7) | 37.1 (16.2) |
| Female | 38 (77.6) | 43 (91.5) | 27 (61.4) | 29 (63.0) | 10 (30.3) | 147 (67.1) |
| Charlson index | ||||||
| 0 | 40 (81.6) | 41 (87.2) | 36 (81.8) | 33 (71.7) | 30 (90.9) | 180 (82.2) |
| 1 | 7 (14.3) | 2 (4.3) | 4 (9.1) | 9 (19.6) | 0 (0) | 22 (10.0) |
| ≥2 | 2 (4.1) | 4 (8.5) | 4 (9.1) | 4 (8.7) | 3 (9.1) | 17 (7.8) |
| No. of drugs used regularly | ||||||
| Not recorded | 0 (0) | 0 (0) | 0 (0) | 1 (2.2) | 5 (15.1) | 6 (2.7) |
| 0 | 28 (57.1) | 25 (53.2) | 26 (59.1) | 26 (56.5) | 23 (69.7) | 128 (58.5) |
| 1 | 6 (12.3) | 12 (25.5) | 6 (13.6) | 9 (19.6) | 2 (6.1) | 35 (16.0) |
| ≥2 | 15 (30.6) | 10 (21.3) | 12 (27.3) | 10 (21.7) | 3 (9.1) | 50 (22.8) |
| Median h spent in ED (IQR) | 3.7 (2.0; 6.0) | 4.5 (3.0; 7.3) | 4.4 (2.8; 6.1) | 7.3 (5.8; 8.9) | 5.2 (3.7; 6.8) | 5.2 (3.2; 7.4) |
| Acuity: CTAS b | ||||||
| 2 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (2.9) | 1 (0.5) |
| 3 | 14 (28.6) | 22 (46.8) | 18 (40.9) | 23 (50.0) | 11 (32.4) | 88 (40.0) |
| 4 | 29 (59.2) | 22 (46.8) | 26 (59.1) | 22 (47.8) | 22 (64.7) | 121 (55.0) |
| 5 | 6 (12.2) | 3 (6.4) | 0 (0) | 1 (2.2) | 0 (0) | 10 (4.5) |
| Mean systolic pressure (SD) | 127.5 (15.1) | 132.4 (21.8) | 132.7 (15.5) | 131.6 (16.2) | 135.1 (13.3) | 131.6 (16.9) |
| Mean heart rate (SD) | 94.2 (13.3) | 85.8 (12.1) | 82.5 (15.3) | 82.8 (11.0) | 85.0 (10.8) | 86.3 (13.4) |
| Mean laceration length in cm (SD) | N/A | N/A | N/A | N/A | 5.2 (4.4) | N/A |
Abbreviations: CTAS, Canadian Triage and Acuity Scale; ED, emergency department; IQR, interquartile range; SD, standard deviation; N/A, not applicable.
For mean age, sex, Charlson index, and number of drugs used regularly, N =33 patients for a total of 219; for median hours spent in ED, acuity, mean systolic pressure, mean heart rate, and mean laceration length, N = 34 care episodes for a total of 220.
Canadian Triage and Acuity Scale (2 = emergent; 3 = urgent; 4 = less urgent; 5 = non urgent).
All data are presented as number and percentage [N (%)] unless otherwise indicated.
3.2. Process maps and durations
Process maps were developed with the team of experts for each condition of interest. All maps are available online (Appendix SA7). More than 300 h of direct observation recorded between 2017 and 2019 yielded 3080 measurements of the duration of procedures grouped into 75 categories. Table 2 compares the estimated and measured durations of the main ED care procedures. Compared to objective time measurement, the care professionals we surveyed tended to underestimate the duration of procedures such as triage and venipuncture and overestimate the time required for X‐rays, ultrasound, computed tomography (CT) scans and other ancillary tests.
TABLE 2.
Duration in minutes of the main care procedures applied to ambulatory patients as estimated by care professionals and measured in the ED
| Care professionals' estimates a | Field measurement | |||
|---|---|---|---|---|
| Procedure | No. | Median (IQR) | P value b | |
| Clerk | ||||
| Registration | 4 | 75 | 2.3 (1.6; 2.8) | <0.0001 |
| Nurse | ||||
| Pre‐triage | 1 | 74 | 1.0 (0.8; 1.3) | 0.50 |
| Triage | ||||
| All conditions c | N/A | 187 | 7.1 (5.5; 9.3) | N/A |
| Upper respiratory tract infections | 4 | 17 | 6.9 (4.8; 8.7) | 0.001 |
| Urinary tract infections | 4 | 17 | 6.4 (5.6; 10.4) | <0.0001 |
| Lower back pain | 4 | 24 | 7.7 (6.0; 8.9) | <0.0001 |
| Unspecified abdominal pain | 6 | 36 | 7.3 (5.0; 9.6) | 0.03 |
| Limb laceration d | 12 | 4 | 7.5 (6.1; 9.6) | 0.14 |
| Venipuncture | 3.5 | 165 | 6.1 (4.1; 9.3) | <0.0001 |
| ED physician | ||||
| Initial assessment | ||||
| All conditions c | N/A | 139 | 7.9 (4.6; 12.8) | N/A |
| Upper resp. tract infections | 7 | 16 | 7.0 (6.0; 11.0) | 0.35 |
| Urinary tract infections | 5 | 18 | 7.6 (4.6; 12.5) | 0.007 |
| Lower back pain | 7 | 11 | 9.4 (5.3; 15.6) | 0.16 |
| Unspecified abdominal pain | 7 | 18 | 9.1 (4.7; 12.8) | 0.16 |
| Limb laceration | 5 | 5 | 6.1 (4.0; 8.7) | 0.50 |
| Point‐of‐care ultrasound | 5 | 32 | 5.9 (4.7; 8.4) | 0.01 |
| Limb wound repair‐stich, per cm | 4.5 | 18 | 6.2 (4.1; 9.3) | 0.03 |
| Limb wound repair‐glue, per cm | 1.5 | 4 | 3.1 (2.8; 4.0) | 0.07 |
| Nursing assistant | ||||
| Room disinfection | 2 | 61 | 1.28 (0.9; 2.3) | 0.02 |
| Patient transport to imaging (one way) | 7.5 | 13 | 3.95 (3.5; 5) | 0.002 |
| Respiratory therapist | ||||
| β‐agonist therapy, per puff | 2 | 11 | 1.5 (0.7; 2.1) | 0.06 |
| Spirometry | 21 | 14 | 20.1 (11.8; 32.3) | 0.73 |
| X‐ray e | ||||
| Chest | 7 | 75 | 5.1 (3.1; 7.1) | <0.0001 |
| Lumbar spine | 7 | 12 | 5.9 (3.7; 7.6) | 0.12 |
| Abdomen | 9 | 11 | 6.1 (4.8; 8.0) | 0.02 |
| Ultrasound e | ||||
| Abdomen, complete | 10 | 9 | 16.4 (14.4; 20.1) | 0.02 |
| Abdomen, limited | 5 | 9 | 8.1 (5.4; 12.2) | 0.03 |
| Pelvic and surface | 10 | 16 | 13.3 (11.9; 15.0) | 0.008 |
| CT scan f | ||||
| Abdomen with IV contrast | 15 | 49 | 4.5 (3.3; 7.3) | <0.0001 |
| Abdomen without contrast | 8 | 12 | 2.7 (2.5; 3.9) | 0.002 |
| Head without contrast | 8 | 30 | 2.2 (2.0; 3.2) | <0.0001 |
| Other ancillary tests | ||||
| ECG | 8 | 82 | 4.6 (3.8; 6.1) | <0.0001 |
Abbreviations: CT, computed tomography; ED, emergency department; IQR, interquartile range; N/A, not applicable.
Estimated by consensus among a panel of experts.
Two‐sided one‐sample Wilcoxon signed rank test.
Including all measurements for patients with targeted and non‐targeted diagnoses.
Including tetanus booster, wound cleansing, and dressing.
Measured from patient entry into the X‐ray/ultrasound room to patient exit into the hallway.
Time of imaging, excluding patient preparation, set‐up, and transport.
3.3. Capacity cost rates and cost of care estimates
Table 3 shows the capacity cost rates of the different cost elements involved in the care of ED patients, including the departments of radiology and respiratory therapy. More details on the allocation of consumables and overhead expenses to patient care are provided as online supplementary material (Appendices SA8 and SA9).
TABLE 3.
Capacity cost rates of ED cost elements ($US/min)
| Cost element | Capacity cost rate |
|---|---|
| Human resources | |
| Nurses | 0.77 |
| Nursing assistants | 0.50 |
| Clerks | 0.42 |
| ED physicians | 3.89 |
| Imaging technicians | 0.59 |
| Respiratory therapists | 0.66 |
| Equipment | |
| X‐ray | 0.16 |
| Ultrasound | 0.11 |
| CT scan | 0.61 |
| Consumables | |
| ED | 0.07 |
| Imaging | 0.11 |
| Respiratory therapy | 0.05 |
| Overhead | |
| ED | 0.17 |
| Radiology | 0.03 |
| Respiratory therapy department | 0.04 |
Abbreviations: CT, computed tomography; ED, emergency department.
3.4. TDABC approaches: Estimated time versus measured time
Table 4 compares the mean costs of care per patient per condition based on estimated time and on measured time. The difference between the 2 estimates is statistically significant except for lower back pain and ranges in absolute terms from $4.30 to $55.20 (US). The Bland–Altman plot (Figure 1) shows that higher the cost of care, the higher is the difference between the 2 TDABC approaches. These differences follow the trend noted earlier for the difference between estimated and measured times, that is, estimated time (and hence cost) is lower than measured time for acts by professionals and higher for imaging and ancillary tests.
TABLE 4.
Comparison of the mean costs of care ($US) per condition according to time‐driven activity‐based costing based on time estimates and time measurements
| Conditions | TE a | TM b | Difference TE‐TM | P value |
|---|---|---|---|---|
| Upper respiratory tract infection | 64.2 (58.4 to 70.0) | 53.7 (47.9 to 59.6) | 10.5 (9.9 to 11.0) | <0.001 |
| Urinary tract infection | 63.9 (52.9 to 74.9) | 67.1 (57.7 to 76.6) | −3.2 (−5.7 to −0.8) | 0.005 |
| Lower back pain | 90.1 (71.2 to 108.9) | 85.7 (70.4 to 101.1) | 4.3 (−0.2 to 9.0) | 0.07 |
| Unspecified abdominal pain | 211.0 (183.1 to 238.9) | 160.9 (147.2 to 190.6) | 50.2 (41.7 to 58.7) | <0.001 |
| Superficial limb laceration | 142.8 (109.1 to 176.5) | 194.8 (148.1 to 241.5) | −52.0 (−68.0 to −36.0) | <0.001 |
Abbreviations: CI, confidence interval; ED, emergency department; TE, Time estimates by care professionnals; TM, time measurements on the field; US, United States.
Note: Time‐driven activity‐based costing requires 2 parameters: the capacity cost rate ($/min) of resources involved in patient care and the duration (min) of procedures provided to patients. The costs of the care procedures are obtained by multiplying the first with the second as in the following example: Cost of ED triage = capacity cost rates of nurse, consumables and overhead (1.02$/min + 0.09$/min + 0.22$/min) × triage duration (7.1 min) = $9.44. This table compares the cost estimates obtained from the durations estimated with 2 different approaches. All data are presented as mean (95% CI).
Time‐driven activity‐based costing from time estimates by care professionals.
Time‐driven activity‐based costing from field measurements of time.
FIGURE 1.
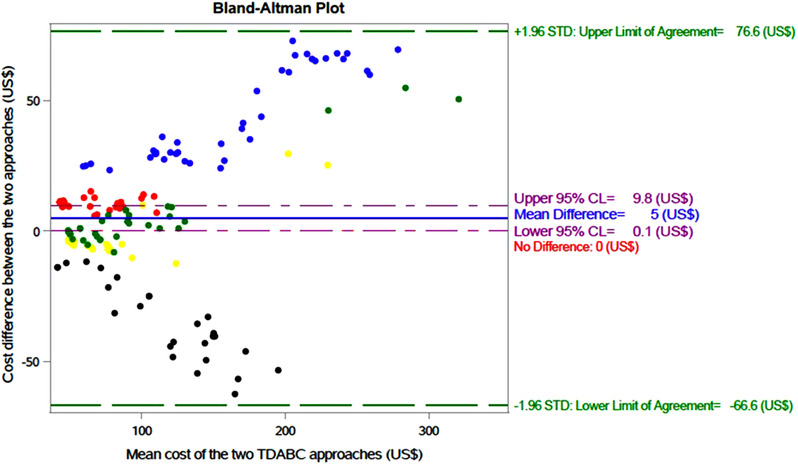
Bland–Altman plot of the agreement between costing ($US) of ambulatory patient care based on estimated and measured procedure times in the emergency department. Dots represent the individual study subjects of the 5 conditions under study. Abbreviations: CL, confidence limit; STD, standard deviation; TDABC: time‐driven activity‐based costing.
At the population level, for the year under study, the differences in mean costs of care (in absolute terms) calculated using the 2 approaches are $1421 for urinary tract infection (n = 444), $1926 for lower back pain (n = 448), $4400 for URTI (n = 419), $36,660 (n = 705) for superficial limb laceration and $56,575 for unspecified abdominal pain (n = 1127). Based on the average of these differences, we estimate that the 2 costings could differ by approximately $509,744 for the population of ED ambulatory adult patients as a whole (n = 21,204).
3.5. Proportions of the overall cost associated with each cost element
Staff (eg, nurses, radiology technicians) and physicians (ED physicians, radiologists) account for more than 86% of the average cost of care for ambulatory patients (Figure 2).
FIGURE 2.
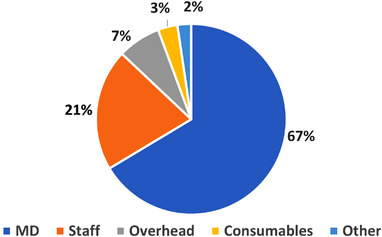
Proportions of the different cost elements in the total cost of ambulatory patient care in the emergency department. Proportions based on the 5 conditions under study. MD: emergency physicians, radiologists and cardiologists (ECG reading). Staff: nurses, nursing assistants, clerks, respiratory therapists, medical imaging technologists. Other: Labs, medication and imaging devices (depreciation and maintenance).
4. LIMITATIONS
This study has certain limitations. First, it focuses on a single Canadian institution. The use of TDABC in other EDs with different protocols or care pathways may require further adaptation. However, because this study was conducted in a Canadian setting using methods developed in the United States, equivalent application of TDABC is likely to be feasible in most EDs in developed countries. In addition, we have transparently reported the unit costs and times used in our analyses, making it easier for the reader to assess the generalizability of our cost estimates. For example, using the median of average salaries by US state in the 2015–2016 ACEP Emergency Physician Compensation Report, 21 we estimate that emergency physician costs should be increased by 50% to better reflect the U.S context. Similar approximations derived from additional sources could be made for other expenses. Second, medical students were excluded from the cost estimates because the time they spend on direct patient care is inconsistent. This choice allows comparison of our results to studies in other jurisdictions where costing does not include training expenses (medical or other healthcare). Furthermore, we did measure durations of procedures involving medical students and residents. We estimated that their assessments of patients with review by the supervising physician cost respectively $17.36 and $11.87 (US), compared to $33.27 when the attending physician alone did the assessment. However, because their involvement in ED care is variable and primarily for educational purposes, we believe that the influence of medical students and residents on costs should be the subject of a focused study. Third, because untraceable supplies (eg, stitches) and overhead cannot be tracked for each patient, we allocated these based on the time for which the care professionals were occupied with each episode. This may have resulted in cost overestimation for acts such as assessment by the physician and underestimation for acts such as wound repair, which require more consumables. However, because consumables and overhead represent small proportions of the overall cost of care (3% and 7%, respectively), the impact of these inaccuracies on the cost estimates was likely minimal. This minor simplification made TDABC easier to use without compromising the goal of the study. Finally, care costs were calculated before the coronavirus disease 2019 (COVID‐19) pandemic. Again, although overall costs likely have increased since then (eg, systematic use of personal protective equipment), the adaptations of TDABC proposed in this study remain relevant and applicable in the post‐COVID context.
5. DISCUSSION
We have adapted and used TDABC to estimate the cost of care for a wide spectrum of ambulatory conditions frequently encountered in the ED. The accuracy of this method depends directly on that of the estimations of the time spent completing each care procedure, which can be either estimated by surveying care professionals or measured directly in the field. This study showed that the greater the use of resources, the greater is the discrepancy between the cost estimates based on these 2 alternatives. Researchers or managers wishing to use TDABC to estimate the cost of ED care should prefer objective measurements of time, either from time stamps in ED information software or from logs kept by direct observers in field studies.
To the best of our knowledge, this is the first study to estimate the cost of the entire ED care pathway for several categories of ambulatory patients. This significantly increases the level of complexity of applying TDABC because ED care encompasses a very wide range of medical, surgical, and administrative procedures. Few previous studies involving TDABC in the ED have examined as many specific care procedures, services or activities, such as CT scanning of the abdomen and pelvis, 22 medical scribes, 23 post‐discharge nurse calls, 24 or billing. 25 We found 1 study in which TDABC was applied to costing the entire in‐hospital care pathway of pediatric appendicitis including its ED component. 26 However, overhead was not considered, and the consumables cost was estimated roughly for the full hospital care pathway without calculating specifically for the ED. In all TDABC studies conducted in that ED, time data were collected using a mixture of approaches and some objective measurements of process duration. However, the number and variation of field measurements were seldom disclosed, nor was it explained how time measured was used alongside time estimated by clinicians or experts. Time data collection is a major issue in TDABC studies. 27 Although many institutions have ED information systems or other real‐time location tracking systems that provide time stamps, 28 these rarely cover all activities that need to be assessed throughout the ED care pathway. Our study confirms that: (1) estimated times are not reliable enough for accurate costing of ED care; and (2) the time taken to execute short, frequent, overlapping, or rare procedures is hard to measure in the field. Accordingly, our findings suggest that TDABC should be applied using objective measures of process duration. However, depending on the reliability and accuracy required for the analysis, the use of a mixed approach for collecting time data may be more pragmatic and feasible. Thus, complex, frequent and expensive procedures should be costed using objective and reliable time measurements, whereas durations of short, inexpensive or rare procedures could be estimated by surveying care professionals. 10 , 29
This study focused on 5 frequent ambulatory care conditions treated in a fully mature universal healthcare system. The costs calculated differ significantly from similar estimates in recent studies conducted in the United States. In a study focused on the years 2012–2015, Ho et al. 30 estimated that visits to a hospital ED in Texas for an upper respiratory tract infection and a urinary tract infection costed $1074 and $2122 compared to $54 and $68 ($US) in our study. The costs for venipuncture, chest X‐ray, and abdominal/pelvic CT scan were $12, $194, and $1625 compared to $5, $20, and $132, respectively. Other studies conducted in the United States have revealed similar differences 31 , 32 although of lesser magnitude. However, these studies used charges and insurance claims, which have been shown to overestimate true costs. 33 , 34 Moreover, greater involvement of private insurers and for‐profit organizations in the provision of care 35 , 36 as well as higher wages in the United States 37 may also explain these differences in the cost of care. Meanwhile, little research has been published on the cost of ED ambulatory care in Canada. According to Campbell et al. (2005), ED care for an upper respiratory tract infection and a urinary tract infection cost respectively $115.57 and $160.72 ($US, based on $CA 2005 value) 20 , 38 in Ontario, which is still higher than what we calculated, even though the Ontario and Quebec healthcare systems are very similar. Two reasons might explain the difference. First, the Ontarian cost estimates included any subsequent return visit within 2 weeks, whereas our analysis was limited to the ED visit itself. In addition, more than 39% of all ED patients did subsequently visit a care setting within 14 days, which likely increased the average costs reported. Second, TDABC is known to produce lower cost estimates than other costing methods. 9 , 17 Using time as a cost driver, TDABC considers only the resource consumed to care for the patient and does not incorporate costs associated with unused capacity, which are often captured by conventional costing methods. It also assumes that an increase in the number of patients in the ED that results in an increase in the number of care processes performed will increase costs proportionally, regardless of the number of care professionals actually available in the field. Further comparative studies are needed to determine the conditions under which each method is most appropriate.
In summary, applying TDABC to the ED setting, where disease severity varies widely and standardization of care is minimal, raises major challenges. To overcome these challenges, this study suggests that (1) TDABC cost estimates should be based on objective time measurements whenever possible, and (2) consumables and overhead expenses, which represent a small proportion of the total cost of care, may be allocated with minimal loss of precision using time rather than inventory associated with an average ED care pathway as recommended in the original TDABC methodology. Because the focus of this study was ambulatory patients, the next step will be to adapt TDABC to costing the entire care pathway for patients requiring stretchers or treated in the resuscitation area.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
AUTHOR CONTRIBUTIONS
Simon Berthelot, Myriam Mallet, Henry T. Stelfox, and Lynne Moore designed the study. Simon Berthelot and Myriam Mallet supervised its conduct. Myriam Mallet, Sébastien Blais, Mélanie Létourneau, Amélie Pineault, Justine Boulet, Christian Boilard, Camille Fortier, Benoît Huard, Akram Mokhtari, Annika Lesage, Émilie Lévesque, Laurence Baril, Pascale Olivier, Keven Vachon, Olivia Yip, Mathieu Bouchard, and Adrien Vézo collected the financial, organizational, and clinical data. Simon Berthelot, David Simonyan, and Jason R. Guertin carried out the statistical analyses. Simon Berthelot drafted the initial manuscript. All authors proofread the manuscript and approved its submitted version. Simon Berthelot assumes responsibility for the integrity of the data used in this study and the accuracy of its analysis.
Supporting information
Supporting Information
ACKNOWLEDGMENTS
This study was supported by the Fonds de recherché du Québec‐Santé, the Centre de recherché du CHU de Québec‐Université Laval, the Canadian Association of Emergency Physicians, and the Département de médecine familiale et de médecine d'urgence, Université Laval.
Biography
Simon Berthelot, MD, MSc, is an Associate Professor in the Department of Family Medicine and Emergency Medicine at Université Laval in Québec, Canada.

Berthelot S, Mallet M, Blais S, et al. Adaptation of time‐driven activity‐based costing to the evaluation of the efficiency of ambulatory care provided in the emergency department. JACEP Open. 2022;3:e12778. 10.1002/emp2.12778
Supervising Editor: Christian Tomaszewski, MD, MS
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see https://www.icmje.org). The authors have stated that no such relationships exist.
REFERENCES
- 1. Iacobucci G. Financial crisis is inevitable in the NHS by 2015–16, King's Fund says. BMJ. 2014;348:g3048. [DOI] [PubMed] [Google Scholar]
- 2. Iacobucci G. UK spending on healthcare lowest of G7 countries. BMJ. 2014;348:g3063. [DOI] [PubMed] [Google Scholar]
- 3. Organisation de coopération et de développement économiques. Impact de la crise économique sur les systèmes de santé. 2015. Published 2013. Accessed 31 janvier 2015. http://www.oecd.org/fr/sante/impact‐de‐la‐crise‐economique‐sur‐les‐systemes‐de‐sante.htm
- 4. Commission de révision permanente des programmes. Cap sur la performance . In: Bibliothèque et Archives nationales du Québec; 2015:1‐71. [Google Scholar]
- 5. Canadian Institute for Health Information. Tendances des dépenses nationales de santé : Comment les dépenses de santé varient‐elles d'une province et d'un territoire à l'autre? Accessed November 3, 2015. https://www.cihi.ca/fr/depenses‐et‐main‐doeuvre‐de‐la‐sante/depenses/tendances‐des‐depenses‐nationales‐de‐sante/bddns2015‐sujet6
- 6. Canadian Institute for Health Information. A Performance Measurement Framework for the Canadian Health System. Published 2013. Accessed April 13, 2022. https://secure.cihi.ca/free_products/HSP_Framework_Technical_Report_EN.pdf
- 7. Health Quality Council of Alberta. Alberta Quality Matric for Health. Published 2005. Accessed April 13, 2022. https://hqca.ca/wp‐content/uploads/2021/12/HQCA_11X8_5_Matrix.pdf
- 8. Yun BJ, Prabhakar AM, Warsh J, et al. Time‐driven activity‐based costing in emergency medicine. Ann Emerg Med. 2015;67(6):765‐772. [DOI] [PubMed] [Google Scholar]
- 9. Palsis JA, Brehmer TS, Pellegrini VD, Drew JM, Sachs BL. The cost of joint replacement: comparing two approaches to evaluating costs of total hip and knee arthroplasty. J Bone Joint Surg Am. 2018;100(4):326‐333. [DOI] [PubMed] [Google Scholar]
- 10. Kaplan RS, Porter ME. How to solve the cost crisis in health care. Harv Bus Rev. 2011;89(9):46‐42, 54, 56‐61 passim. [PubMed] [Google Scholar]
- 11. Kaplan RS. Improving value with TDABC. Healthc Financ Manage. 2014;68(6):76‐83. [PubMed] [Google Scholar]
- 12. Canadian Institute for Health Information. Document technique sur la Base de données canadienne sur les coûts par patient : Méthodologie SIG d’établissement des coûts par patient, novembre 2011. Published 2011. Accessed 16 septembre 2015. https://www.cihi.ca/fr/MIS_PATIENT_COST_METH_fr.pdf
- 13. Sutherland JM. Pricing hospital care: global budgets and marginal pricing strategies. Health Policy. 2015;119(8):1111‐1118. [DOI] [PubMed] [Google Scholar]
- 14. Kirkpatrick JR, Marks S, Slane M, et al. Using value‐based analysis to influence outcomes in complex surgical systems. J Am Coll Surg. 2015;220(4):461‐468. [DOI] [PubMed] [Google Scholar]
- 15. Oker F, Ozyapici H. A new costing model in hospital management: time‐driven activity‐based costing system. Health Care Manag (Frederick). 2013;32(1):23‐36. [DOI] [PubMed] [Google Scholar]
- 16. Demeere N, Stouthuysen K, Roodhooft F. Time‐driven activity‐based costing in an outpatient clinic environment: development, relevance and managerial impact. Health Policy. 2009;92(2‐3):296‐304. [DOI] [PubMed] [Google Scholar]
- 17. Akhavan S, Ward L, Bozic KJ. Time‐driven activity‐based costing more accurately reflects costs in arthroplasty surgery. Clin Orthop Relat Res. 2015;474(1):8‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Erhun F, Mistry B, Platchek T, Milstein A, Narayanan VG, Kaplan RS. Time‐driven activity‐based costing of multivessel coronary artery bypass grafting across national boundaries to identify improvement opportunities: study protocol. BMJ Open. 2015;5(8):e008765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Canadian Institute for Health Information. Canadian Patient Cost Database Technical Document: MIS Patient Costing Methodology January 2019. Published 2019. Accessed January 29, 2021. https://www.cihi.ca/sites/default/files/document/mis_patient_cost_meth_en_0.pdf
- 20. Bank of Canada. Historical Noon and Closing Rates. Accessed June 11, 2021. https://www.bankofcanada.ca/rates/exchange/legacy‐noon‐and‐closing‐rates/?_ga=2.71813523.1060196855.1623203547‐1844222510.1623203547
- 21. American College of Emergency Physicians. 2015 Emergency Physician Compensation Report Highlights Regional Salary Trends. Published 2015. Accessed April 19, 2022. https://www.acepnow.com/article/2015‐emergency‐medicine‐compensation‐report‐released/2/
- 22. Anzai Y, Heilbrun ME, Haas D, et al. Dissecting costs of CT study: application of TDABC (time‐driven activity‐based costing) in a Tertiary Academic Center. Acad Radiol. 2017;24(2):200‐208. [DOI] [PubMed] [Google Scholar]
- 23. Heaton HA, Nestler DM, Barry WJ, et al. A time‐driven activity‐based costing analysis of emergency department scribes. Mayo Clin Proc Innov Qual Outcomes. 2019;3(1):30‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Liu Y, Luciani‐Mcgillivray I, Hughes M, Raja AS, Kaplan RS, Yun BJ. Time‐driven activity‐based costing of emergency department postdischarge nurse calls. J Healthc Manag. 2020;65(6):419‐428. [DOI] [PubMed] [Google Scholar]
- 25. Tseng P, Kaplan RS, Richman BD, Shah MA, Schulman KA. Administrative costs associated with physician billing and insurance‐related activities at an academic health care system. JAMA. 2018;319(7):691‐697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Yu YR, Abbas PI, Smith CM, et al. Time‐driven activity‐based costing: a dynamic value assessment model in pediatric appendicitis. J Pediatr Surg. 2017;52(6):1045‐1049. [DOI] [PubMed] [Google Scholar]
- 27. Etges A, Ruschel KB, Polanczyk CA, Urman RD. Advances in value‐based healthcare by the application of time‐driven activity‐based costing for inpatient management: a systematic review. Value Health. 2020;23(6):812‐823. [DOI] [PubMed] [Google Scholar]
- 28. Yoo S, Kim S, Kim E, Jung E, Lee KH, Hwang H. Real‐time location system‐based asset tracking in the healthcare field: lessons learned from a feasibility study. BMC Med Inform Decis Mak. 2018;18(1):80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Keel G, Savage C, Rafiq M, Mazzocato P. Time‐driven activity‐based costing in health care: a systematic review of the literature. Health Policy. 2017;121(7):755‐763. [DOI] [PubMed] [Google Scholar]
- 30. Ho V, Metcalfe L, Dark C, et al. Comparing utilization and costs of care in freestanding emergency departments, hospital emergency departments, and urgent care centers. Ann Emerg Med. 2017;70(6):846‐857e843. [DOI] [PubMed] [Google Scholar]
- 31. Galarraga JE, Mutter R, Pines JM. Costs associated with ambulatory care sensitive conditions across hospital‐based settings. Acad Emerg Med. 2015;22(2):172‐181. [DOI] [PubMed] [Google Scholar]
- 32. Mehrotra A, Liu H, Adams JL, et al. Comparing costs and quality of care at retail clinics with that of other medical settings for 3 common illnesses. Ann Intern Med. 2009;151(5):321‐328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Finkler SA. The distinction between cost and charges. Ann Intern Med. 1982;96(1):102‐109. [DOI] [PubMed] [Google Scholar]
- 34. Wan W, Itri J. Charge master: friend or foe? Curr Probl Diagn Radiol. 2016;45(2):122‐127. [DOI] [PubMed] [Google Scholar]
- 35. The Commonwealth Fund. International Health Care System Profiles: United States. Published 2020. Accessed May 25, 2021. https://www.commonwealthfund.org/international‐health‐policy‐center/countries/united‐states
- 36. The Commonwealth Fund. International Health Care System Profiles: Canada. Published 2020. Accessed May 25, 2021. https://www.commonwealthfund.org/international‐health‐policy‐center/countries/canada
- 37. Organization for Economic Cooperation and Development. Average wages. Published 2021. Accessed May 25, 2021. https://data.oecd.org/earnwage/average‐wages.htm
- 38. Statistics Canada. Consumer Price Index, annual average, not seasonally adjusted. Accessed June 11, 2021. https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1810000501&pickMembers%5B0%5D=1.2&cubeTimeFrame.startYear=2005&cubeTimeFrame.endYear=2016&referencePeriods=20050101%2C20160101&request_locale=en
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information


