Abstract
Background
Ambulatory electromyographic (EMG) devices are increasingly being used in sleep bruxism studies. EMG signal acquisition, analysis and scoring methods vary between studies. This may impact comparability of studies and the assessment of sleep bruxism in patients.
Objectives
(a) To provide an overview of EMG signal acquisition and analysis methods of recordings from limited‐channel ambulatory EMG devices for the assessment of sleep bruxism; and (b) to provide an overview of outcome measures used in sleep bruxism literature utilising such devices.
Method
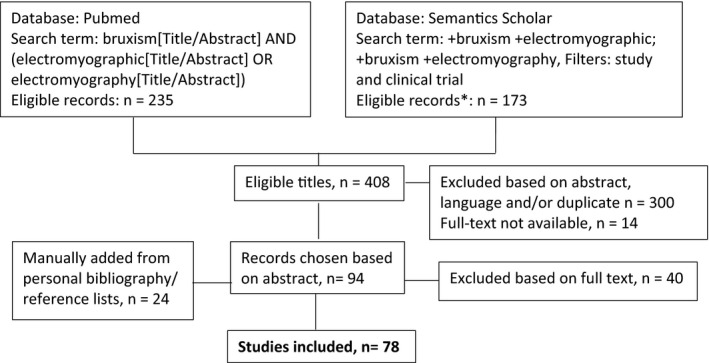
A scoping review of the literature was performed. Online databases PubMed and Semantics Scholar were searched for studies published in English until 7 October 2020. Data on five categories were extracted: recording hardware, recording logistics, signal acquisition, signal analysis and sleep bruxism outcomes.
Results
Seventy‐eight studies were included, published between 1977 and 2020. Recording hardware was generally well described. Reports of participant instructions in device handling and of dealing with failed recordings were often lacking. Basic elements of signal acquisition, for example amplifications factors, impedance and bandpass settings, and signal analysis, for example rectification, signal processing and additional filtering, were underreported. Extensive variability was found for thresholds used to characterise sleep bruxism events. Sleep bruxism outcomes varied, but typically represented frequency, duration and/or intensity of masticatory muscle activity (MMA).
Conclusion
Adequate and standardised reporting of recording procedures is highly recommended. In future studies utilising ambulatory EMG devices, the focus may need to shift from the concept of scoring sleep bruxism events to that of scoring the whole spectrum of MMA.
Keywords: ambulatory electromyographic device, limited channel device, masticatory muscle activity, sleep bruxism, surface electromyography
1. INTRODUCTION
Sleep bruxism is accompanied by masticatory muscle activity (MMA) during sleep, and its definition has received much attention over the years. 1 The most recent definition states that sleep bruxism is a masticatory muscle activity that is characterised as rhythmic (phasic) or non‐rhythmic (tonic) muscle contractions. 2 The term ‘rhythmic’ has extensively been used in the past to indicate MMA during sleep that is characterised by a repetitive pattern. 3 , 4 , 5 , 6 Rhythmic masticatory muscle activity (RMMA) has been considered the cardinal feature of sleep bruxism on electromyographic (EMG) traces derived from polysomnographic audio‐video (PSG‐AV) sleep laboratory studies. 3 , 4 , 5 In such studies, RMMA is distinguished from other types of MMA, more specifically from oro‐facial activities (OFAs; ie MMAs without characteristic patterns, such as swallowing, yawning and coughing) and from oro‐motor activities (OMAs; ie MMAs that are part of major movements, including head, neck or body movements). 3 , 7 , 8 Currently, sleep bruxism research is shifting towards adopting the more general term MMA, instead of RMMA. 9 , 10 This shift is driven by technical advancements and accumulating evidence in the field of ambulatory EMG recorders that are increasingly being used in sleep bruxism studies (eg 11 , 12 , 13 ). Their development is evolving, for example in terms of reduced size 14 and compatibility with other technologies, such as smartphone applications. 15 They allow for assessment of the whole spectrum of MMA, but are less able to discriminate between RMMA, OMA and OFA, compared to PSG‐AV. 3 Indeed, ambulatory EMG devices are known to overestimate sleep bruxism activity, compared to the gold standard, viz. PSG‐AV recordings. 16 However, they have obvious benefits compared to PSG‐AV, regarding costs and simplicity, and are therefore more pragmatic and important alternatives for the study of sleep bruxism on a larger scale. 17 Most importantly though, the shift towards assessment of the whole spectrum of MMA, instead of the more restricted RMMA, is driven by its clinical relevance. 9 It is plausible that clinical health outcomes, for example masticatory muscle pain, are related to EMG outcomes including, but not limited to, RMMA. Features of MMA, such as background EMG activity, 18 intensity and timing, 19 , 20 amplitude of activity 21 and variability of activity over time, 22 have been studied in relation to musculoskeletal signs and symptoms (for a comprehensive overview, see 23 ). The importance of addressing the continuum of MMA in order to understand its relation to specific clinical outcomes has been discussed extensively in previous publications. 2 , 9 , 10 , 24 , 25
Instrumental, assessment of MMA with the use of EMG, with or without positive self‐report and/or positive clinical inspection is needed to establish a ‘definite’ sleep bruxism diagnosis, according to the current bruxism diagnostic grading system. 2 , 10 The choice of criteria to score sleep bruxism on EMG recordings is a matter of ongoing discussion and research. 2 , 9
EMG recordings can be derived from attended or unattended (ie type 1 or type 2), PSG recordings, as well as limited‐channel, portable (ie type 3 and 4) EMG recorders 26 , 27 , 28 (Table 1). Once acquired, the EMG signal is scored to provide outcomes of MMA.
TABLE 1.
Types of sleep recording devices
| Type | Descriptiony 26 , 27 | Examples a |
|---|---|---|
| Type 1 | Full attended polysomnography (≥7 channels) in a laboratory setting | |
| Type 2 | Full unattended polysomnography (≥7 channels) | |
| Type 3 | Limited‐channel devices (usually 4–7 channels) |
Bruxoff (3 channels: 2 for bilateral masseter, 1 for ECG) TEAC‐HR‐10 J (3 channels: 1 for masseter, 1 respiratory, 1 for ECG) Myomonitor (4 channels: 2 for bilateral masseter, 2 for bilateral temporalis) |
| Type 4 | 1–2 channels |
Pro‐comp INFINITI (2 channels: 1 for masseter, 1 for ECG) EMG‐021/025, KTR2302B (2 channels for bilateral masseter) Grindcare (1 channel for temporalis) |
Abbreviation: ECG, electrocardiography.
Examples of electromyographic recorders included in this review.
EMG bursts are widely used as the basic elements of sleep bruxism outcome measures. 29 Various thresholds above which EMG activity is defined as a bruxism‐related burst have been used in literature, such as percentages of the maximum voluntary contraction (MVC) level, 11 , 29 , 30 , 31 , 32 multiplications of the baseline EMG activity 33 , 34 , 35 , 36 and recognition of a specific EMG pattern. 37 It is conceivable that the use of different thresholds for the assessment of the same EMG recording will lead to differences in the scoring of sleep bruxism outcomes, thus rendering comparison of studies difficult, if not impossible. Moreover, it may be hypothesised that the assessment of sleep bruxism in the clinic is impacted, since a patient may receive a different sleep bruxism diagnosis, depending on the threshold used to score an EMG recording.
After being scored, EMG bursts may be used to construct other measures of sleep bruxism events, such as sleep bruxism episodes. 29 To this end, the criteria from Reding, 6 which were adapted by Ware and Rugh, 38 and proposed as sleep bruxism criteria by Lavigne et al 29 (hereafter referred to as SB/research criteria) are currently widely used to define three types of episodes: phasic, tonic and mixed. 29 These criteria are based on EMG recordings as a part of PSG‐AV sleep laboratory assessments and have been transferred and used for the scoring of ambulatory EMG signals (eg 12 , 39 ), despite concerns regarding the validity of using these criteria in the absence of audiovisual recordings. 4 , 40 Furthermore, indices consisting of the number of EMG bursts or episodes per hour of sleep are commonly calculated. 11 , 22 , 29 , 32 , 37 Other indices may, amongst others, involve the number of EMG bursts or episodes per recording, 11 , 22 the total duration of those activities per hour of sleep, 11 , 32 the EMG area under the curve (AUC) per hour of sleep, 32 magnitude of muscle work over time, 19 the variability of activity over time 41 , 42 or the duration of the intervals between consecutive episodes. 20 Thus, a substantial variation in the expression of sleep bruxism EMG outcomes exists, without standardisation so far.
Besides variation in scoring of bruxism outcomes on an EMG signal, significant variation may also arise in the acquisition of the EMG signal itself, due to differences in technical specifications of EMG devices, for example in terms of electrode material and size, inter‐electrode distance, accepted impedance, amplification and filtering, and further processing of the EMG signal. 43 , 44 Improper technical characteristics may lead to the acquisition of unreliable EMG signal 43 and may further complicate comparison between studies. To this end, it has been recommended that studies adequately report on the technical aspects of EMG recordings, 45 but unfortunately this is not always the case. 46
Ambulatory EMG devices are indeed promising tools for future large‐scale studies of sleep bruxism, and MMA during sleep in general. 15 , 47 A substantial number of different devices are, or have been, available for research and/or commercial purposes. The validity of ambulatory EMG devices, compared to PSG recordings, has been addressed in previous literature reviews (see 16 , 48 , 49 ). However, a comprehensive overview of how sleep bruxism outcomes have been scored in studies uses ambulatory EMG recordings, and the technical aspects of these studies are lacking. Ideally, ambulatory EMG devices should allow for an accurate and uniform way to acquire EMG recordings and score EMG features of sleep bruxism in the natural environment of individuals. As a first step towards this goal, this paper was designed: (a) to provide an overview of EMG signal acquisition and analysis methods of recordings from type 4 ambulatory EMG devices for the assessment of sleep bruxism; and (b) to provide an overview of outcome measures used so far in sleep bruxism literature utilising such ambulatory EMG devices. The ultimate goal of this study is to provide information that can facilitate further development of a standardised tool for the assessment of sleep bruxism, 10 including protocols for recording, data acquisition and scoring that should be ideally applicable to all devices eventually used to study sleep bruxism. This would facilitate comparability of studies in the research setting, and the development and application of proper devices for use in clinical settings.
2. MATERIALS AND METHODS
A scoping review of the literature was performed. 50 , 51 Scoping reviews are specific types of reviews that allow structured mapping of evidence on a broad research question, and identification of gaps in existing literature. 50 , 51 They can also be used to identify the potential scope of a subsequent systematic review. 51 Scoping reviews differ from systematic reviews mainly in that they provide an overview of all existing literature on a particular topic, without quality assessment of the data. 50 , 51 To be suitable for inclusion in this scoping review, a study should fulfil the following criteria: (1) clinical study with the use of an ambulatory type 3 or 4 EMG recorder for the assessment of sleep bruxism, and (2) reports sleep bruxism outcomes. Only studies that reported data were included, viz. publications of study protocols, were excluded. Studies with type 1 or 2 devices 27 were also excluded. Online databases PubMed and Semantics Scholar were searched for studies published in English until 7 October 2020. Search terms and the inclusion flowchart are presented in Figure 1. Risk of bias assessment was not applicable for this review, 50 , 51 since the aim was to provide a comprehensive overview of all signal acquisition and scoring methods in the sleep bruxism literature. Data from the included studies were extracted into a worksheet. Table 2 provides an overview of the assessed variables. The search and inclusion procedures as well as data extraction were performed by one author (MT). When authors referred to another study, and the relevant information could indeed be found in the other study, it is reported as ‘refers to other’. It was not the purpose of the review to provide a thorough description of all technical specifications of EMG recordings, but rather, to limit itself to the reported items of the International Society of Electrophysiology and Kinesiology (ISEK). 45
FIGURE 1.
Search terms and inclusion flowchart
TABLE 2.
Extracted variables from included studies
| Category | Variable | Description of what was assessed |
|---|---|---|
| General study information | First author, year, journal | First author, year, journal |
| Study type | For example, cross‐sectional, case‐control | |
| Population | Adults/children | |
| Recording hardware | Description of EMG device | Authors’ description of type of EMG device |
| Commercial name of EMG device | Commercial name, description and/or manufacturer of EMG device | |
| Electrode type | Description of electrode | |
| Wireless electrode | Yes/no | |
| Number of channels | Number and site of channels | |
| Muscles | Which masticatory muscles were used for signal acquisition | |
| Picture of device | Present in publication; yes/no | |
| Use of additional instrumental methods to assess bruxism | For example, electrocardiographic activity, audiovisual recordings | |
| Recording logistics | Number of recording nights (not including the adaptation night) | Total number and, if applicable, number of recording sets (eg within 3 weeks, 3 sets of 4 recording nights) |
| Adaptation night before scoring | Yes/no | |
| Setting | Home/sleep laboratory | |
| Participant instructions device and electrode handling | How were participants instructed on using the device and handling the electrode | |
| Participant instructions device set‐up | If applicable, how were participants instructed to set‐up the device (eg performing MVC) | |
| Electrode placement | By participant of investigator | |
| How are failures dealt with | Which action followed if acquisition of the recording failed | |
| Signal acquisition | Amplification factor | How many times was the signal amplified |
| Impedance measurement | What data are provided on amplifier input and/or skin impedance | |
| Bandpass settings | What was the frequency range of the signal acquisition | |
| Notch filter | Frequency of additional notch filter | |
| A/D resolution | What was the resolution of the A/D converter | |
| Sampling rate | At which frequency was the signal sampled | |
| Signal analysis | Device output | Raw EMG signal/scored activity (viz. activity which was scored after automatic analysis of the EMG signal inside the EMG device) |
| Definition of analysis time | Which part of the signal was analysed | |
| EMG scoring software | Commercial name | |
| Rectification | Was the signal rectified | |
| Processing | Was the signal further processed, if yes, how | |
| Additional filtering | Was there any additional filtering performed in the analysis process | |
| Threshold for EMG scoring | Which threshold was used to score EMG events | |
| Definition of event | How was an event defined | |
| Sleep bruxism outcomes | Use of RMMA term as outcome variable | Yes/no |
| Diagnosis of ‘sleep bruxer’ through cut‐off criteria | Were cut‐off criteria used to define a bruxer, and if so, which | |
| Reported outcomes | Which sleep bruxism outcomes are reported |
Abbreviations: A/D, analog‐to‐digital; EMG, electromyographic; MVC, maximum voluntary contraction.
3. RESULTS
3.1. General study information
Seventy‐eight studies were included in this review (Figure 1). They were published between 1977 and 2020, with almost half (56%) having been published from the year 2013 on. Seventy‐six studies included adult populations. Study type characteristics are presented in Table 3.
TABLE 3.
Overview of study types
| Study type | n | First author & year |
|---|---|---|
| Algorithm development/cross‐sectional | 2 | Čadová 2014, Ikeda 1996 |
| Before‐after interventional | 9 | Castro Mattia 2018, Clark 1981, Kardachi 1977, Manfredini 2018, Needham 2013, Raphael 2013, Rugh 1981, Saueressig 2010, Zhou 2016 |
| Case‐control | 18 | Ahlberg 2008, Camara‐Souza 2018, Iwasaki 2015, Jonsgar 2015, Karakoulaki 2015, Kato 2018, Minakuchi 2014, Miyawaki 2003, Mude 2017, Nitschke 2011, Ohlmann 2018, Ono 2008, Palinkas 2019, Schmitter 2015, Shedden Mora 2012, Suganuma 2007, Wei 2017, Yachida 2012 |
| Controlled interventional | 2 | Rugh 1984 & 1989 |
| Cross‐sectional | 19 | Baba 2005, Clarke 1984 & 1984, Hammoudi 2019, Khawaja 2015, Manfredini 2011, 2016 & 2019, Matsuda 2016, Minakuchi 2016, Miyawaki 2004, Mizumori 2013, Murakami 2014, Nagamatsu‐Sakaguchi 2017, Ohlmann 2020, Po 2013, Takaoka 2017, Thymi 2019, Yamaguchi 2012 |
| Device development/case report | 1 | Yamaguchi 2018 |
| Device development/cross‐sectional | 2 | Haketa 2003, Stock 1983 |
| Device development/case‐control | 1 | Sakagami 2002 |
| Diagnostic validity | 7 | Castroflorio 2014 & 2015, Gallo 1997, Maeta 2019, Mainieri 2012, Shochat 2007, Stuginski‐Parbosa 2015 |
| Epidemiological | 2 | Gallo 1999, Minakuchi 2012 |
| Prospective cohort | 1 | Thymi 2020 |
| Randomised controlled trial | 13 | Abekura 2008, Baad‐Hansen 2007, Carvalho Bortoletto 2016, Conti 2014, Harada 2006, Jadidi 2008 & 2013, Lee 2010, Matsumoto 2015, Mohamed 1997, Saito‐ Murakami 2020, Shedden Mora 2013, Shimada 2019 |
| Reliability | 1 | Deregibus 2014 |
Abbreviation: n, number of studies.
3.2. Recording hardware
Various terms were used to describe the ambulatory EMG recorders, the most common being ‘portable EMG device’ 32 , 37 , 52 , 53 , 54 , 55 , 56 , 57 (n = 8; 10%), followed by ‘portable EMG recorder’ 58 , 59 , 60 , 61 and ‘portable single‐channel EMG device’ 33 , 62 , 63 , 64 (for each n = 4; 5%). All but two 59 , 65 studies provided a description of the devices’ components and/or information on their commercial names and/or manufacturers. Devices used more commonly were the ‘Grindcare’ in different versions 22 , 66 , 67 , 68 , 69 , 70 (n = 15; 19%), followed by the ‘Bitestrip’ 13 , 81 (n = 12; 15%), and the ‘Bruxoff’ 30 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 (n = 9; 12%) device (see online Appendix for overview). Pictures of devices were provided in 18 (23%) of the studies. 11 , 66 , 67 , 83 , 84 , 90 , 91 , 92 , 93 , 94 Eleven studies used additional instrumental methods to assess sleep bruxism, viz. audio recordings 54 (n = 1), video recordings 95 (n=1), audiovisual recordings 96 , 97 (n = 2) and electrocardiographic (ECG) activity 82 , 83 , 84 , 85 , 86 , 87 , 92 , 98 (n = 8, 10%).
Most studies (n = 44; 57%) utilised a single‐channel assembly, 13 , 14 , 22 , 31 , 57 , 60 , 61 , 62 , 63 , 64 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 90 , 91 , 95 , 96 , 97 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 and two and three channels were utilised in 13 (17%) 11 , 108 , 109 , 110 , 111 and 15 (19%) 19 , 98 , 112 , 113 , 114 , 115 , 116 studies, respectively, while two 53 , 117 studies used a four‐channel assembly (see online appendix for specifications of channel assemblies). The most prevalent recording site was the masseter muscle in 45 (58%) studies, 11 , 12 , 13 , 14 , 65 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 90 , 91 , 92 , 94 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 , 111 , 117 , 118 followed by the temporalis muscle in 21 (27%) studies, 15 , 22 , 66 , 67 , 69 , 70 , 71 , 93 , 95 , 96 , 97 and both muscles in 10 studies. 19 , 117 One study 119 did not provide details on the recording site, but referred to another publication instead.
Electrodes connected to the devices through wires were used in 52 (67%) studies, 11 , 12 , 19 , 22 , 30 , 31 , 32 , 33 , 53 , 54 , 56 , 57 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 102 , 105 , 106 , 107 , 108 , 109 , 110 , 111 , 112 , 117 , 118 while 17 (22%) studies 13 , 78 , 79 , 80 , 81 , 90 , 91 utilised wireless electrodes (see online appendix for overview of electrode descriptions). Four studies 101 , 113 , 116 , 119 did not describe the type of electrode, but referred the reader to another publication with description.
3.3. Recording logistics
Twenty‐five (32%) studies 12 , 14 , 82 , 83 , 85 , 88 , 90 , 91 , 92 , 94 , 96 , 97 , 99 , 100 , 105 , 108 , 117 based their analyses on single‐night recordings, and two studies did not clearly describe the number of recordings, 76 , 115 while all other studies (n = 51; 65%) 11 , 13 , 15 , 19 , 22 , 52 , 53 , 57 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 69 , 70 , 71 , 72 , 74 , 75 , 77 , 84 , 86 , 87 , 89 , 93 , 95 , 98 , 101 , 102 , 103 , 104 , 106 , 107 , 109 , 110 , 111 , 112 , 113 , 114 , 116 , 118 , 119 performed multiple night recordings, with a maximum of 70 recordings per participant 67 (see online appendix for overview of the number of recording nights per study). An adaptation night prior to scoring, that is a recording night which allowed participants to get accustomed to the recording procedure, the data of which were not used for further analyses, was performed in 17 (22%) of the studies. 9 , 85 , 90 , 91 , 92 , 96 , 97 , 108 , 109 In the vast majority (n = 63; 82%) of studies, recordings were performed at the home setting, 11 , 12 , 13 , 14 , 19 , 37 , 39 , 52 , 53 , 54 , 56 , 57 , 59 , 60 , 61 , 62 , 63 , 64 , 66 , 67 , 68 , 69 , 70 , 72 , 73 , 74 , 75 , 76 , 77 , 79 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 91 , 92 , 93 , 94 , 96 , 97 , 98 , 100 , 101 , 102 , 106 , 107 , 108 , 109 , 110 , 117 , 119 with four studies situated in a laboratory 33 , 78 , 80 , 90 and 11 studies not clearly describing the setting. 71 , 116 Placement of the electrode on the skin was performed by participants themselves in almost half of studies (n = 40; 52%). 11 , 12 , 13 , 14 , 52 , 53 , 56 , 57 , 59 , 60 , 63 , 64 , 66 , 67 , 68 , 69 , 70 , 73 , 74 , 75 , 76 , 82 , 84 , 92 , 93 , 94 , 102 , 105 , 106 , 109 , 118 In one study on children, the electrode was placed by the caregiver, 71 while in six studies the procedure was performed by the study investigators. 33 , 54 , 100 , 101 , 110 , 117 The description of who placed the electrode was unclear for 29 (37%) studies, 30 , 32 , 83 , 85 , 86 , 87 , 89 , 90 , 91 , 95 , 96 , 97 , 98 , 99 , 108 , 111 , 112 , 113 , 114 , 115 , 116 while two studies referred to another publication for a description. 9 , 119
Over half of the studies (n = 44; 56%) 11 , 12 , 13 , 14 , 39 , 52 , 53 , 56 , 59 , 60 , 63 , 64 , 65 , 66 , 69 , 70 , 71 , 73 , 74 , 75 , 76 , 80 , 82 , 84 , 87 , 92 , 93 , 94 , 95 , 102 , 105 , 107 , 109 , 110 , 114 , 117 , 119 reported that instructions were given to participants on how to handle the device and/or its components. Reports varied from brief statements, for example ‘subjects received instruction on how to handle the device as well as the placement of the electrodes’, 39 to more detailed descriptions, for example ‘participants were … instructed in its usage in a home environment using a mirror and an instruction manual over 15 min by two trained instructors’. 76 Thirty‐two studies (41%) 30 , 32 , 57 , 83 , 85 , 86 , 87 , 89 , 90 , 91 , 95 , 96 , 97 , 98 , 99 , 103 , 104 , 106 , 108 , 111 , 112 , 115 , 118 did not describe whether participants were given instructions on device handling, while for five studies 33 , 54 , 100 , 101 , 110 this information was not applicable, since the devices were mounted by the study investigators. As for set‐up procedures, for example performing an MVC at the start of the recording, these were described for 37 (47%) of the studies, 11 , 14 , 22 , 56 , 61 , 62 , 67 , 68 , 69 , 73 , 77 , 78 , 80 , 81 , 82 , 83 , 84 , 90 , 91 , 95 , 96 , 98 , 100 , 101 , 107 , 108 , 109 , 110 , 111 , 117 while the remaining 41 (53%) studies did not describe such procedures.
Certain actions were reported in case a recording failed; that is, recorded data were partially or completely insufficient for analysis. Additional instructions were given to participants in two studies, 11 , 109 while nine studies reported repeating failed recordings. 32 , 39 , 69 , 73 , 77 , 101 , 109 , 110 , 114 Nine studies 11 , 37 , 39 , 52 , 92 , 93 , 95 , 99 , 107 reported removing artefacts, for example arising from high noise levels, from the raw EMG signal prior to signal analysis. Recordings were completely discarded from further analysis in case of failure in 15 (19%) studies. 22 , 76 , 95 , 102 , 110 , 117 , 119 ‘Noisy signals were identified and excluded’ in one study, without further specification of the term ‘noisy signals’, that is reference to artefact or complete recording. 59 One study 14 reported evaluating signal quality and not finding artefacts, while another study 108 reported evaluating the signal for artefact, but without mentioning how these were dealt with. The remaining 45 (58%) studies did not report how failures were evaluated and/or dealt with.
3.4. Signal acquisition
The amplification factor of the signal during acquisition was described in only 19 (24%) studies 14 , 70 , 83 , 84 , 90 , 91 , 106 , 108 , 110 , 120 (Table 4). Different amplification factors were used for different devices, ranging from 250 90 , 115 to 50 000 times. 93
TABLE 4.
EMG signal acquisition characteristics
| Outcome | n | First author & year | |
|---|---|---|---|
| Amplification factor | 250× | 2 | Maeda, 2019, Stock 1983 |
| 256× | 1 | Yamaguchi 2018 | |
| 500× | 2 | Matsuda, 2016, Yamaguchi 2012 | |
| 800× | 4 | Stuginski‐Barbosa 2015, Thymi 2019, Yachida 2012, Zhou 2016 | |
| 2000× | 1 | Mohamed 1997 | |
| 3590× | 1 | Gallo 1999 | |
| 4300× | 3 | Castroflorio 2014 & 2015, Deregibus 2014 | |
| 5000× | 3 | Iwasaki 2015, Khawaja 2015, Wei 2017 | |
| 8692× | 1 | Po 2013 | |
| 50 000× | 1 | Sakagami 2002 | |
| Amplified signal, factor not described | 13 | Abekura 2008, Baad‐Hansen 2007, Baba 2005, Čadová 2014, Haketa 2003, Ikeda 1996, Karakoulaki 2015, Lee 2010, Manfredini 2011, Minakuchi 2012 & 2014, Nagamatsu‐Sakaguchi 2017, Shedden Mora 2012 | |
| Refers to other publication | 12 | Clarke 1984 & 1984, Gallo 1997, Kardachi 1977, Kato 2018, Manfredini 2016, 2018 & 2019, Nitschke 2011, Rugh 1989, Shedden Mora 2012, Thymi 2020 | |
| Not described | 34 | Ahlberg 2008, Camara‐Souza 2018, Carvalho Bortoletto 2016, Castro Mattia 2018, Clark 1981, Conti 2014, Harada 2006, Hammoudi 2019, Jadidi 2008 & 2013, Jonsgar 2015, Mainieri 2012, Matsumoto 2015, Minakuchi 2016, Miyawaki 2003 & 2004, Mizumori 2013, Mude 2017, Murakami 2014, Needham 2013, Ohlmann 2018 & 2020, Ono 2008, Palinkas 2019, Raphael 2013, Rugh 1981 & 1984, Saito‐Murakami 2020, Saueressig 2010, Schmitter 2015, Shimada 2019, Shochat 2007, Suganuma 2007, Takaoka 2017 | |
| Input and/or skin impedance | Amplifier 10 kΩ | 1 | Stock 1983 |
| Amplifier >2 MΩ | 1 | Mohamed 1997 | |
| Amplifier 250 MΩ | 3 | Iwasaki 2015, Khawaja 2015, Wei 2017 | |
| Skin <2 kΩ | 2 | Gallo, 1997 & 1999 | |
| Skin <10 kΩ | 3 | Jadidi 2008 & 2013, Takaoka 2017 | |
| Refers to other publication | 5 | Clarke 1984 & 1984, Kardachi 1977, Nitschke 2011, Rugh 1989 | |
| Not described | 63 | Abekura 2008, Ahlberg 2008, Baad‐Hansen 2007, Baba 2005, Čadová 2014, Camara‐Souza 2018, Carvalho Bortoletto 2016, Castro Mattia 2018, Castroflorio 2014 & 2015, Clark 1981, Conti 2014, Deregibus 2014, Haketa 2003, Hammoudi 2019, Harada 2006, Ikeda 1996, Jonsgar 2015, Karakoulaki 2015, Kato 2018, Lee 2010, Maeda 2019, Mainieri 2012, Manfredini 2011, 2016, 2018 & 2019, Matsuda 2016, Matsumoto 2015, Minakuchi 2012, 2014 & 2016, Miyawaki 2003 & 2004, Mizumori 2013, Mude 2017, Murakami 2014, Nagamatsu‐Sakaguchi 2017, Needham 2013, Ohlmann 2018 & 2020, Ono 2008, Palinkas 2019, Po 2013, Raphael 2013, Rugh 1981 & 1984, Saito‐Murakami 2020, Sakagami 2010, Saueressig 2010, Schmitter 2015, Shedden Mora 2012 & 2013, Shimada 2019, Shochat 2007, Stuginski‐Barbosa 2015, Suganuma 2007, Thymi 2019 & 2020, Yachida 2012, Yamaguchi 2012 & 2018, Zhou 2016 | |
| Bandpass settings | 5–500 Hz | 1 | Maeda 2019 |
| 5.3–450 Hz | 1 | Saito‐Murakami 2020 | |
| 10–400 Hz | 3 | Castroflorio 2014 & 2015, Deregibus 2014 | |
| 10–500 Hz | 3 | Shedden Mora 2012, Stock 1983, Yamaguchi 2012 | |
| 10–1000 Hz | 2 | Mude 2017, Kato 2018 | |
| 20–? Hz | 1 | Yamaguchi 2018 | |
| 20–500 Hz | 1 | Baad‐Hansen 2007 | |
| 20–600 Hz | 2 | Jadidi 2008 & 2013 | |
| 20–1000 Hz | 3 | Iwasaki 2015, Khawaja 2015, Wei 2017 | |
| 50–500 Hz | 2 | Čadová 2014, Gallo 1999 | |
| 70–500 Hz | 1 | Po 2013 | |
| 100–200 Hz | 1 | Sakagami 2010 | |
| 100–310 Hz | 1 | Mohamed 1997 | |
| 250–600 Hz | 1 | Raphael 2013 | |
| 250–610 Hz | 3 | Stuginski‐Barbosa 2015, Thymi 2019, Yachida 2012 | |
| 251–610 Hz | 1 | Zhou 2016 | |
| Refers to other publication | 9 | Clarke 1984 & 1984, Kardachi 1977, Manfredini 2016, 2018 & 2019, Nitschke 2011, Rugh 1989, Shedden Mora 2013, Thymi 2020 | |
| Not described | 42 | Abekura 2008, Ahlberg 2008, Baba 2005, Camara‐Souza 2018, Carvalho Bortoletto 2016, Castro Mattia 2018, Clark 1981, Conti 2014, Gallo 1997, Haketa 2003, Hammoudi 2019, Harada 2006, Ikeda 1996, Jonsgar 2015, Karakoulaki 2015, Lee 2010,, Mainieri 2012, Manfredini 2011, Matsuda 2016, Matsumoto 2015, Minakuchi 2012, 2014 & 2016, Miyawaki 2003 & 2004, Mizumori 2013, Murakami 2014, Nagamatsu‐Sakaguchi 2017, Needham 2013, Ohlmann 2018 & 2020, Ono 2008, Palinkas 2019, Rugh 1981 & 1984, Saueressig 2010, Schmitter 2015, Shimada 2019, Shochat 2007, Suganuma 2007, Takaoka 2017, | |
| Notch filter | 50 Hz | 2 | Saito‐Murakami 2020, Shedden Mora 2012 |
| 60 Hz | 3 | Kato 2018, Mohamed 1997, Mude 2017 | |
| Refers to other publication | 4 | Manfredini 2016 & 2018, Rugh 1989, Shedden Mora 2013 | |
| Not described | 69 | Abekura 2008, Ahlberg 2008, Baad‐Hansen 2007, Baba 2005, Čadová 2014, Camara‐Souza 2018, Carvalho Bortoletto 2016, Castro Mattia 2018, Castroflorio 2014 & 2015, Clark 1981, Clarke 1984 & 1984, Conti 2014, Deregibus 2014, Gallo 1997 & 1999, Haketa 2003, Hammoudi 2019, Harada 2006, Ikeda 1996, Iwasaki 2015, Jadidi 2008 & 2013, Jonsgar 2015, Karakoulaki 2015, Kardachi 1977, Khawaja 2015, Lee 2010, Maeda 2019, Mainieri 2012, Manfredini 2011, & 2019, Matsuda 2016, Matsumoto 2015, Minakuchi 2012, 2014 & 2016, Miyawaki 2003 & 2004, Mizumori 2013, Murakami 2014, Nagamatsu‐Sakaguchi 2017, Needham 2013, Nitschke 2011, Ohlmann 2018 & 2020, Ono 2008, Palinkas 2019, Po 2013, Raphael 2013, Rugh 1981 & 1984, Sakagami 2010, Saueressig 2010, Schmitter 2015, Shimada 2019, Shochat 2007, Stock 1983, Stuginski‐Barbosa 2015, Suganuma 2007, Takaoka 2017, Thymi 2019 & 2020, Wei 2017, Yachida 2012, Yamaguchi 2012 & 2018, Zhou 2016 | |
| A/D converter resolution | 8 bit | 7 | Castroflorio 2014 & 2015, Deregibus 2014, Gallo 1997 & 1999, Stock 1983, Yamaguchi 2012 |
| 10 bit | 2 | Po 2013, Raphael 2013 | |
| 12 bit | 2 | Maeda 2019, Yamaguchi 2018 | |
| 14 bit | 1 | Haketa 2003 | |
| 16 bit | 1 | Manfredini 2011 | |
| Refers to other publication | 7 | Clarke 1984 & 1984, Kato 2018, Manfredini 2016, 2018 & 2019, Nitschke 2011 | |
| Not described | 58 | Abekura 2008, Ahlberg 2008, Baad‐Hansen 2007, Baba 2005, Čadová 2014, Camara‐Souza 2018, Carvalho Bortoletto 2016, Castro Mattia 2018, Clark 1981, Conti 2014, Harada 2006, Hammoudi 2019, Ikeda 1996, Iwasaki 2015, Jadidi 2008 & 2013, Jonsgar 2015, Karakoulaki 2015, Kardachi 1977, Khawaja 2015, Lee 2010, Mainieri 2012, Matsuda 2016, Matsumoto 2015, Minakuchi 2012, 2014 & 2016, Miyawaki 2003 & 2004, Mizumori 2013, Mohamed 1997, Mude 2017, Murakami 2014, Nagamatsu‐Sakaguchi 2017, Needham 2013, Ohlmann 2018 & 2020, Ono 2008, Palinkas 2019, Rugh 1981, 1984 & 1989, Saito‐Murakami 2020, Sakagami 2010, Saueressig 2010, Schmitter 2015, Shedden Mora 2012 & 2013, Shimada 2019, Shochat 2007, Stuginski‐Barbosa 2015, Suganuma 2007, Takaoka 2017, Thymi 2019 & 2020, Wei 2017, Yachida 2012, Zhou 2016 | |
| Sampling rate | 10 Hz | 1 | Shedden Mora 2012 |
| 16 Hz | 1 | Saito‐Murakami 2020 | |
| 128 Hz | 1 | Murakami 2014 | |
| 200 Hz | 2 | Baba 2005, Haketa 2003 | |
| 800 Hz | 3 | Castroflorio 2014 & 2015, Deregibus 2014 | |
| 1000 Hz | 9 | Abekura 2008, Gallo 1997 & 1999, Harada 2006, Manfredini 2011, Matsuda 2016, Miyawaki 2003, Yamaguchi 2012 & 2018 | |
| 1001 Hz | 1 | Miyawaki 2004 | |
| 1002 Hz | 1 | Mizumori 2013 | |
| 1024 Hz | 1 | Lee 2010 | |
| 2000 Hz | 7 | Baad‐Hansen 2007, Čadová 2014, Iwasaki 2015, Jadidi 2008, Khawaja 2015, Po 2013, Raphael 2013 | |
| 2001 Hz | 1 | Jadidi 2013 | |
| 2048 Hz | 1 | Matsumoto 2015 | |
| 4000 Hz | 1 | Stock 1983 | |
| 22 050 Hz | 1 | Mude 2017 | |
| Refers to other publication | 9 | Clarke 1984 & 1984, Kato 2018, Manfredini 2016, 2018 & 2019, Nitschke 2011, Rugh 1989, Shedden Mora 2013 | |
| Not described | 38 | Ahlberg 2008, Camara‐Souza 2018, Carvalho Bortoletto 2016, Castro Mattia 2018, Clark 1981, Conti 2014, Hammoudi 2019, Ikeda 1996, Jonsgar 2015, Karakoulaki 2015, Kardachi 1977, Maeda 2019, Mainieri 2012, Minakuchi 2012, 2014 & 2016, Mohamed 1997, Nagamatsu‐Sakaguchi 2017, Needham 2013, Ohlmann 2018 & 2020, Ono 2008, Palinkas 2019, Rugh 1981 & 1984, Sakagami 2010, Saueressig 2010, Schmitter 2015, Shimada 2019, Shochat 2007, Stuginski‐Barbosa 2015, Suganuma 2007, Takaoka 2017, Thymi 2019 & 2020, Wei 2017, Yachida 2012, Zhou 2016 |
Abbreviation: n, number of studies.
Reports on impedance conditions were scarcer (Table 4). Five studies reported an amplifier input impedance of 10 kΩ, 115 >2 106 and 250 MΩ. 19 , 59 , 60 Another five studies reported on skin impedance measurements, that is <2 99 , 110 and <10 kΩ. 37 , 52 , 69
The frequency range of signal sampling, that is bandpass settings, was described in 27 studies (35%) 14 , 19 , 54 , 59 , 60 , 61 , 67 , 70 , 83 , 84 , 90 , 93 , 95 , 100 , 102 , 106 , 108 , 110 , 111 , 115 (Table 4). Similar to the amplification factor, bandpass settings varied between different devices. As for additional notch filtering, two studies reported a 50 Hz notch filter, 95 , 102 while another three studies reported a 60 Hz notch filter during analysis of the signal 54 , 100 , 106 (Table 4).
The resolution of the analog voltage to digital (A/D) signal converter was reported in 13 (17%) studies 11 , 14 , 30 , 33 , 67 , 83 , 84 , 90 , 99 , 108 , 110 , 115 , 117 and ranged between 8 bit 83 , 84 , 99 , 115 and 16 bit (Table 4). Data on sampling rates were provided in 31 (40%) studies 11 , 14 , 19 , 59 , 67 , 83 , 84 , 91 , 92 , 95 , 96 , 97 , 99 , 102 , 105 , 107 , 108 , 109 , 110 , 111 , 112 , 115 , 117 (Table 4). Frequencies varied between 10 Hz 102 and 22050 Hz, 54 with the majority of studies utilising frequencies of approximately 1000 14 , 33 , 53 , 91 , 92 , 96 , 97 , 99 , 107 , 110 , 112 , 117 and 2000 Hz 19 , 32 , 37 , 52 , 59 , 67 , 108 , 109 , 111 (n = 12 and 9, respectively).
3.5. Signal analysis
Analysis of the acquired signal was performed either automatically by the EMG device, or as a separate step, after EMG data were transferred from the device to a computer. In the first case, built‐in software analysed and scored the signal, and thus, the output of the EMG device was scored activity, which was reported in 30 (38%) studies. 13 , 22 , 31 , 69 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 88 , 93 , 103 , 104 , 113 , 114 , 115 , 116 In 30 (38%) studies, 19 , 30 , 68 , 70 , 83 , 84 , 90 , 91 , 92 , 96 , 97 , 98 , 100 , 101 , 102 , 107 , 108 , 109 , 111 , 117 , 118 , 119 the output of the EMG device was raw EMG activity. In seven studies, the signal was stored in the device after undergoing some form of processing, for example rectification, 32 , 95 , 99 , 110 , 112 or if certain conditions were met, for example only recording EMG activity with an amplitude >5 μV. 11 Studies performing analysis of raw EMG data reported the use of 10 different software programs, viz. the Bruxmeter software, 30 , 82 , 83 , 84 , 87 the Myomonitor software, 53 the Bruxism analysing software MTS50011, 96 , 97 Sound Engine software, 54 Chart 5, 91 SmartAnalyzer, 117 Biograph Infinity, 109 custom‐made algorithms in the MatLab software, 19 , 57 , 59 , 60 , 70 , 108 , 111 LabVIEW 102 , 119 and Jaws. 32 Six studies reported the use of a custom software without further specification. 11 , 39 , 95 , 98 , 107 , 110
Thirty (38%) studies 11 , 13 , 30 , 76 , 77 , 78 , 80 , 81 , 83 , 90 , 91 , 95 , 96 , 97 , 100 , 101 , 102 , 107 , 109 , 110 , 112 , 116 , 117 provided some description of which part of the signal was analysed, for example “the first and last 15 mins … of each night's recording were excluded from analysis”. 32 There were three main ways of choosing a part of the signal for analysis, namely exclusion of a pre‐defined period of recording time (n = 10), 30 , 32 , 78 , 96 , 97 , 100 , 107 , 109 , 112 , 116 device functioning for only a set amount of time (n = 10) 13 , 117 and utilisation of diaries with self‐reported recording times (n = 6). 11 , 39 , 60 , 101 , 102 , 110 The four remaining studies used adjunctive measurements to help define which part of the signal should be analysed, viz. concomitant PSG, 33 , 83 , 90 and actigraphy. 91
Signal rectification was performed in 17 (22%) studies 11 , 32 , 37 , 39 , 52 , 92 , 93 , 95 , 97 , 99 , 100 , 104 , 106 , 110 , 112 , 117 (Table 5). Other signal processing procedures were described in 23 studies 29%), 11 , 19 , 95 , 96 , 97 , 98 , 99 , 100 , 102 , 107 , 108 , 109 , 110 , 111 , 117 for example signal smoothing through root mean square conversion (n = 10) 19 , 32 , 53 , 67 , 95 , 98 , 100 , 102 , 108 , 117 (Table 5). Furthermore, additional filtering of the signal prior to scoring bruxism was described in five studies 19 , 54 , 90 , 100 , 101 (Table 5).
TABLE 5.
Rectification, signal processing and additional filtering of EMG signal
| Outcome | n | First author & year | |
|---|---|---|---|
| Rectification | yes | 17 | Abekura 2008, Baad‐Hansen 2007, Baba 2005, Gallo 1997 & 1999, Haketa 2003, Jadidi 2008 & 2013, Kato 2018, Manfredini 2011, Miyawaki 2003 & 2004, Mizumori 2013, Mohamed 1997, Rugh 1989, Saito‐Murakami 2020, Sakagami 2010 |
| Refers to other publication | 1 | Nitschke 2011 | |
| Not described | 60 | Ahlberg 2008, Čadová 2014, Camara‐Souza 2018, Carvalho Bortoletto 2016, Castro Mattia 2018, Castroflorio 2014 & 2015, Clark 1981, Clarke 1984 & 1984, Conti 2014, Deregibus 2014, Hammoudi 2019, Harada 2006, Ikeda 1996, Iwasaki 2015, Jonsgar 2015, Karakoulaki 2015, Kardachi 1977, Khawaja 2015, Lee 2010, Maeda 2019, Mainieri 2012, Manfredini 2016, 2018 & 2019, Matsuda 2016, Matsumoto 2015, Minakuchi 2012, 2014 & 2016, Mude 2017, Murakami 2014, Nagamatsu‐Sakaguchi 2017, Needham 2013, Ohlmann 2018 & 2020, Ono 2008, Palinkas 2019, Po 2013, Raphael 2013, Rugh 1981 & 1984, Saueressig 2010, Schmitter 2015, Shedden Mora 2012 & 2013, Shimada 2019, Shochat 2007, Stock 1983, Stuginski‐Barbosa 2015, Suganuma 2007, Takaoka 2017, Thymi 2019 & 2020, Wei 2017, Yachida 2012, Yamaguchi 2012 & 2018, Zhou 2016 | |
| Processing | Averaged signal | 2 | Gallo 1997, Harada 2006 |
| Averaged at 16 Hz | 1 | Matsumoto 2015 | |
| Averaged with moving interval of 1 ms and window time of 19 ms | 2 | Miyawaki 2003 & 2004 | |
| Converted to absolute value and smoothed with a width of 15 sampling points | 1 | Matsuda 2016 | |
| Converted to absolute values and smoothed by a width of 101 points (.1 s) | 1 | Maeda 2019 | |
| Root mean square | 5 | Baad‐Hansen 2007, Ikeda 1996, Manfredini 2011, Raphael 2013, Saito‐Murakami 2020 | |
| Root mean square amplitude values calculated over 125‐ms contiguous rectangular windows | 1 | Po 2013 | |
| Root mean square conversion in 0.125‐sec segments, and 0.0625‐sec overlap of time segments | 1 | Lee 2010 | |
| Root mean square conversion in 128‐ms time‐windows | 1 | Iwasaki 2015 | |
| Root mean square conversion with integration time of 10 ms | 1 | Kato 2018 | |
| Root mean square with average factor of 100 ms | 1 | Shedden Mora 2012 | |
| Integrated signal, integration time 0.5 s | 1 | Gallo 1999 | |
| Integrated signal, integration time was the entire duration of sleep | 1 | Mohamed 1997 | |
| Integrated signal, but method not described | 2 | Čadová 2014, Mizumori 2013 | |
| Performed, but method not described | 2 | Baba 2005, Haketa 2003 | |
| Refers to other publication | 3 | Nitschke 2011, Rugh 1989, Shedden Mora 2013 | |
| Not described | 52 | Abekura 2008, Ahlberg 2008, Camara‐Souza 2018, Carvalho Bortoletto 2016, Castro Mattia 2018, Castroflorio 2014 & 2015, Clark 1981, Clarke 1984 & 1984, Conti 2014, Deregibus 2014, Hammoudi 2019, Jadidi 2008 & 2013, Jonsgar 2015, Karakoulaki 2015, Kardachi 1977, Khawaja 2015, Mainieri 2012, Manfredini 2016, 2018 & 2019, Minakuchi 2012, 2014 & 2016, Miyawaki 2003 & 2004, Mude 2017, Murakami 2014, Nagamatsu‐Sakaguchi 2017, Needham 2013, Ohlmann 2018 & 2020, Ono 2008, Palinkas 2019, Rugh 1981 & 1984, Sakagami 2010, Saueressig 2010, Schmitter 2015, Shimada 2019, Shochat 2007, Stock 1983, Stuginski‐Barbosa 2015, Suganuma 2007, Takaoka 2017, Thymi 2019 & 2020, Wei 2017, Yachida 2012, Yamaguchi 2012 & 2018, Zhou 2016 | |
| Additional filtering | 200 Hz low‐pass filter and 60 Hz notch filter | 1 | Mude 2017 |
| 500 Hz low‐pass filter and 60 Hz notch filter | 1 | Kato 2018 | |
| 20 Hz high pass filter | 2 | Maeda 2019, Matsuda 2016 | |
| Low‐level noise | 1 | Iwasaki 2015 | |
| Refers to other publication | 2 | Nitschke 2011, Rugh 1989 | |
| Not described | 71 | Abekura 2008, Ahlberg 2008, Baad‐Hansen 2007, Baba 2005, Čadová 2014, Camara‐Souza 2018, Carvalho Bortoletto 2016, Castro Mattia 2018, Castroflorio 2014 & 2015, Clark 1981, Clarke 1984 & 1984, Conti 2014, Deregibus 2014, Gallo 1997 & 1999, Haketa 2003, Hammoudi 2019, Harada 2006, Ikeda 1996, Jadidi 2008 & 2013, Jonsgar 2015, Karakoulaki 2015, Kardachi 1977, Khawaja 2015, Lee 2010, Mainieri 2012, Manfredini 2011, 2016, 2018 & 2019, Matsumoto 2015, Minakuchi 2012, 2014 & 2016, Miyawaki 2003 & 2004, Mizumori 2013, Mohaer 1997, Murakami 2014, Nagamatsu‐Sakaguchi 2017, Needham 2013, Ohlmann 2018 & 2020, Ono 2008, Palinkas 2019, Po 2013, Raphael 2013, Rugh 1981 & 1984, Saito‐Murakami 2020, Sakagami 2010, Saueressig 2010, Schmitter 2015, Shedden Mora 2012 & 2013, Shimada 2019, Shochat 2007, Stock 1983, Stuginski‐Barbosa 2015, Suganuma 2007, Takaoka 2017, Thymi 2019 & 2020, Wei 2017, Yachida 2012, Yamaguchi 2012 & 2018, Zhou 2016 |
Abbreviation: n, number of studies.
Twenty‐five different thresholds were used for scoring of events on the EMG signal, the most common being a percentage of the MVC (Table 6). Forty‐two studies (54%) 11 , 12 , 14 , 22 , 56 , 61 , 62 , 64 , 67 , 68 , 69 , 71 , 73 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 86 , 87 , 88 , 91 , 95 , 96 , 97 , 98 , 100 , 105 , 107 , 109 , 111 used a percentage of the MVC, ranging from 3% 32 to 50%, 11 with six of these studies using a 20% of 60% MVC threshold. 22 , 31 , 56 , 61 , 62 , 67 Six studies used a multiplication of the background EMG activity, viz. two times, 22 , 54 , 91 three times, 70 three standard deviations 92 and four standard deviations. 60 One study 90 used a combination of the above, that is >2 times baseline amplitude, and amongst those, bursts that exceeded 5%, 10% and 20% MVC. Fourteen studies 19 , 110 , 115 , 117 , 118 , 119 used other thresholds, that is 1, 106 10, 102 , 119 20, 103 , 104 , 118 100 μV, 65 20% of the highest occurring bursts, 99 percentages of 20 N bite‐force thresholds, 19 , 59 the maximum amplitude of the signal of stimulated artefacts, 110 the average root mean square of muscle activity during three swallowing movements, 117 an A/D converter‐related threshold 115 and a spectrogram‐based frequency and power threshold. 108 Three studies 37 , 52 , 112 did not utilise a threshold for EMG scoring. Integrated EMG values per hour of sleep were used as outcome variables in one study 112 and recognition of pre‐sampled EMG patterns in the other two 37 , 52 (Table 6).
TABLE 6.
Thresholds for scoring EMG events
| Outcome | n | First author& year | |
|---|---|---|---|
| % MVC | 3%, 10% and 20% MVC | 1 | Baad‐Hansen 2007 |
| 5% MVC | 1 | Čadová 2014 | |
| 10% MVC | 11 | Camara‐Souza 2018, Castroflorio 2014 & 2015, Deregibus 2014, Harada 2006, Manfredini 2011 & 2018, Matsumoto 2015, Miyawaki 2003 & 2004, Ohlmann 2018 | |
| 10% MVC (selected amongst 3%, 10% and 20% MVC) | 1 | Ikeda 1996 | |
| 10% and 20% MVC | 3 | Lee 2010, Matsuda 2016, Takaoka 2017 | |
| 20% MVC | 7 | Baba 2005, Jonsgar 2015, Kato 2018, Ono 2008, Saito‐Murakami 2020, Thymi 2020, Yamaguchi 2018 | |
| 20% of 60% MVC | 6 | Conti 2014, Raphael 2013, Schmitter 2015, Stuginski‐Barbosa 2015, Yachida 2012, Zhou 2016 | |
| 20% & 50% MVC | 1 | Haketa 2003 | |
| 30% MVC | 11 | Ahlberg 2008, Carvalho‐Bortoletto 2016, Castro Mattia 2018, Karakouliaki 2015, Mainieri 2012, Minakuchi 2014, Murakami 2014, Nagamatsu‐Sakaguchi 2017, Palinkas 2019, Saueressig 2010, Shochat 2007 | |
| Multiplication of background activity | > 2x baseline EMG activity during resting | 1 | Matsuda 2016 |
| 2× baseline activity | 1 | Yamaguchi 2012 | |
| 2× baseline noise level during resting conditions of the mandible at the beginning of the recording | 1 | Mude 2017 | |
| >3× amplitude of background noise | 1 | Thymi 2019 | |
| >3× resting state standard deviations | 1 | Mizumori 2013 | |
| 4× standard deviation of background EMG activity while awake | 1 | Wei 2017 | |
| >2× baseline amplitude, and amongst those 5%, 10% and 20% MVC | 1 | Maeda 2019 | |
| Other thresholds | 1 μV | 1 | Mohamed 1997 |
| 10 μV | 2 | Shedden Mora 2012 & 2013 | |
| 20 μV | 3 | Rugh 1981, 1984 & 1989 | |
| 100 μV | 1 | Clark 1981 | |
| 20% of highest occurring bursts | 1 | Gallo 1997 | |
| 5–9, 10–24, 25–49, 50–79 and ≥80% of 20 N force in each 128‐ms time‐window | 1 | Iwasaki 2015 | |
| 4 magnitude thresholds (10%, 25%, 50% and 20% of 20 N bite force) and 6 duration points (1, 2, 5, 10, 15 and 20 s) | 1 | Khawaja 2015 | |
| Maximum amplitude of the signals of the stimulated artefacts | 1 | Gallo 1999 | |
| Average RMS of muscle activity during three swallowing movements | 1 | Manfredini 2011 | |
| Whenever the fourth least significant bit of the analogue‐to‐digital convertor was active, a bruxing episode was occurring | 1 | Stock 1983 | |
| 0.625 Hz peak frequency and 2% relative power | 1 | Po 2013 | |
| Not applicable | Signal recognition algorithm | 3 | Jadidi 2008 & 2013, Takaoka 2017 |
| Integrated EMG values of each analysed period | 1 | Abekura 2008 | |
| Refers to other publication | 3 | Manfredini 2016, Nitschke 2011, Shimada 2019 | |
| Not described | 10 | Clarke 1984 & 1984, Hammoudi 2019, Kardachi 1977, Minakuchi 2012 & 2016, Needham 2013, Ohlman 2020, Sakagami 2002, Suganuma 2007 |
Abbreviations: MVC, maximum voluntary contraction; n, number of studies; RMS, root mean square.
Bruxism events were defined in various ways (see online appendix for a complete overview). Out of the 78 included studies, only nine (12%) 32 , 63 , 66 , 74 , 75 , 89 , 113 , 114 , 116 did not provide a description of how bruxism events were defined. Another five studies 14 , 61 , 68 , 85 , 100 referred to other publications for a description. Two studies did not utilise events, but integrated EMG values per hour of sleep, 112 and cumulative EMG activity divided by the duration of sleep 106 as measures of muscle activity. The remaining 62 (79%) studies provided descriptions of bruxism event definitions. Of those, five 12 , 39 , 54 , 94 , 99 used the SB/research criteria 29 to score EMG events. Another eight studies 56 , 57 , 64 , 84 , 96 , 97 , 102 , 119 used these criteria to score types of bruxism episodes, but based on a different threshold than the 20% MVC of the 1996 publication. 29 The remaining 49 (63%) studies used a variety of ways to define a bruxism event 11 , 13 , 19 , 22 , 53 , 59 , 60 , 62 , 65 , 67 , 69 , 70 , 71 , 72 , 73 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 86 , 87 , 90 , 91 , 92 , 93 , 95 , 98 , 101 , 103 , 104 , 105 , 107 , 108 , 109 , 110 , 111 , 112 , 115 , 117 , 118 (see Appendix S1). Definitions of events were based on criteria of EMG thresholds, duration of EMG activity above the threshold and interval between subsequent supra‐threshold activity. With the exception of two studies, 37 , 52 all abovementioned studies with descriptions of bruxism event definitions (n = 60) included a threshold in their description of the event. Of these, 41 (53%) reported an additional duration criterion for the definition of an event, 11 , 12 , 13 , 19 , 54 , 56 , 57 , 59 , 60 , 64 , 65 , 67 , 69 , 70 , 73 , 78 , 79 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 102 , 105 , 107 , 108 , 109 , 110 , 111 , 115 , 118 , 119 and 22 reported a threshold, duration and interval criterion. 11 , 12 , 79 , 90 , 91 , 95 , 96 , 97 , 98 , 99 , 105 , 107 , 109 , 110 , 111 Eight studies used outcomes related to cardiac activity in the definition of a bruxism event. 30 , 82 , 83 , 84 , 86 , 87 , 88 , 98 Two studies 37 , 52 used a pattern recognition algorithm for the definition of events.
3.6. Sleep bruxism outcomes
The term RMMA was used in the context of sleep bruxism outcome variables in nine studies. 33 , 57 , 83 , 84 , 91 , 96 , 97 , 108 Twenty‐four studies (31%) 12 , 13 , 79 , 80 , 81 , 82 , 85 , 87 , 89 , 90 , 94 , 105 used cut‐off criteria to define sleep bruxers. Of those, 13 studies used criteria to grade the severity of bruxism 13 , 87 , 89 , 90 (Table 7).
TABLE 7.
Cut‐off values and grading criteria for defining sleep bruxers
| Outcome | n | First author & year | |
|---|---|---|---|
| Cut‐off | >2 episodes/h | 1 | Camara‐Souza 2018 |
| ≥2 episodes/h | 2 | Murakami 2014, Schmitter 2015 | |
| >4 episodes/h | 3 | Castroflorio 2015, Manfredini 2016, Mude 2017 | |
| >25 events/h | 1 | Takaoka 2017 | |
| SB/research criteria | 2 | Ono 2008, Suganuma 2007 | |
| 5.5 EMG‐episode/h, 32.2 EMG‐burst‐all/h and 26.4 EMG‐burst‐5%/h | 1 | Maeda 2019 | |
| 18 EMG/h or higher in three consecutive nights and 19 EMG/h or higher in five consecutive nights | 1 | Stuginski‐Barbosa 2015 | |
| Cut‐off and grading | >2 episodes/h for moderate and >4 episodes/h for intense/severe sleep bruxism | 2 | Ohlman 2018 & 2020 |
| 0 = <40 events; 1 = 40–74 events; 2 = 75–124 events; and 3 = ≥125 events (0–2: non‐severe SB, score 3: severe SB) | 1 | Nagamatsu‐Sakaguchi 2017 | |
| 0 = <40 events; 1 = 40–74 events; 2 = 75–124 events; and 3 = ≥125 events | 2 | Saueressig 2010 | |
| 0 = <30 events, 1 = 31–60 events, 2 = 61–100 events and 3 = ≥100 events | 3 | Carvalho Bortoletto 2016, Karakoulaki 205, Minakuchi 2012 | |
| 0 = <30 events, 1 = 31–60 events, 2 = 61–100 events and 3 = ≥100 events (0–1 normal controls, 2–3 severe SB) | 1 | Minakuchi 2014 | |
| 0 = no bruxism (≤39 episodes), 1 = mild bruxism (40–74 episodes), 2 = moderate bruxism (75–124 episodes) and 3 = severe bruxism (≥125 episodes) | 3 | Ahlberg 2008, Mainieri 2012, Palinkas 2019 | |
| SB frequency score in four grades (0, 1, 2 and 3) | 1 | Minakuchi 2016 |
Abbreviations: EMG, electromyographic, h, hour, n, number of studies, SB, sleep bruxism.
There were three main groups of sleep bruxism outcome variables: frequency, duration and intensity of masticatory muscle activity. Frequency variables were most commonly assessed, with 71 (91%) studies 11 , 12 , 13 , 14 , 22 , 30 , 31 , 32 , 33 , 37 , 52 , 53 , 54 , 56 , 57 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 101 , 102 , 103 , 104 , 105 , 107 , 108 , 109 , 110 , 111 , 113 , 114 , 115 , 116 , 117 , 118 , 119 reporting at least one frequency variable, followed by duration and intensity variables, which were reported in 28 (36%) 11 , 19 , 77 , 91 , 92 , 93 , 96 , 98 , 100 , 101 , 102 , 107 , 108 , 109 , 110 , 111 , 113 , 115 , 117 , 118 , 119 and 20 (26%) 32 , 56 , 98 , 101 , 106 , 107 , 109 , 110 , 111 , 112 , 113 , 115 , 117 studies, respectively. Forty‐six (59%) studies 12 , 13 , 14 , 22 , 57 , 62 , 65 , 66 , 67 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 94 , 95 , 97 , 99 , 103 , 104 , 105 , 114 , 116 reported on frequency variables only, while three studies 19 , 39 , 100 reported on only duration measures, and two 106 , 112 solely on intensity. Twenty‐two studies 11 , 32 , 77 , 91 , 92 , 93 , 96 , 98 , 101 , 102 , 107 , 108 , 109 , 110 , 111 , 113 , 115 , 117 , 118 , 119 reported on the combination of two or more variables of frequency, duration and intensity. An overview of reported outcomes is provided in Table 8.
TABLE 8.
Types of sleep bruxism outcome variables based on frequency, duration and intensity of masticatory muscle activity
| First author & year | Frequency | Duration | Intensity |
|---|---|---|---|
| Abekura 2008 | Integrated EMG values/h (μV*s) | ||
| Ahlberg 2008 | Score based on events/recording | ||
| Baad‐Hansen 2007 | Events/h | EMG duration/h | EMG AUC/h |
| Baba 2005 | Total duration of muscle activity/h, averaged across the 5‐night study period | ||
| Čadová 2014 | Activity/h | Duration of activity (s) | Mean amplitude of contraction episode (%MVC) |
| Max amplitude of contraction episode (%MVC) | |||
| Integral under the signal curve of contraction episode (%MVC) (%MVC*s) | |||
| Camara‐Souza 2018 | Episodes/h | ||
| Carvalho Bortoletto 2016 | Score based on events/recording | ||
| Castro Mattia 2018 | Score based on events/recording | ||
| Castroflorio 2014 | Episodes/h | ||
| Episodes/ night | |||
| Castroflorio 2015 | Episodes/h | ||
| Episodes/ night | |||
| Clark 1981 | Activity/h | ||
| Clarke 1984 | Events/night | ||
| Clarke 1984 | Events/night | Duration of events | Intensity of bruxing as a factor of force and duration |
| Total n of seconds bruxing/night | |||
| Conti 2014 | EMG events/h | ||
| Deregibus 2014 | Episodes/h | ||
| Episodes/ night | |||
| Gallo 1997 | Number of episodes | ||
| Gallo 1999 | Episodes/h | Duration of episodes | Mean amplitudes of episodes |
| episodes/night | Intervals between episodes | Maximum amplitudes of episodes | |
| Integral (= muscle work, %MVC) | |||
| Haketa 2003 | Events/h | Event duration/h | |
| Events/night | Event duration/night | ||
| Event duration | |||
| Hammoudi 2019 | EMG grinds/hour | EMG burst duration | Intensity |
| EMG grinds total n | |||
| EMG episodes/h | |||
| EMG episodes total n | |||
| EMG bursts/h | |||
| EMG bursts total n | |||
| Harada 2006 | Events/h | % event duration/night | total EMG activity |
| Ikeda 1996 | Events/h | Mean EMG duration/ event | mean peak EMG level (%MVC) |
| Iwasaki 2015 | Duty factor, that is the amount of time each muscle was activated at specific magnitudes during a given time, % | ||
| Jadidi 2008 | SRA events | ||
| Jadidi 2013 | SRA events | ||
| Jonsgar 2015 | Episodes/h | Mean burst duration | |
| Episodes total n | |||
| Grinds/h | |||
| Grinds total n | |||
| Bursts/h | |||
| Bursts total n | |||
| Karakoulaki 2015 | Score based on events/recording | ||
| Kardachi 2017 | n of bruxing units | ||
| Kato 2018 | Cumulative duration of each episode | ||
| Cumulative duration of episodes/h | |||
| Khawaja 2015 | Duty factor for duration of muscle activity threshold | Duty factor for magnitude of muscle activity threshold | |
| Lee 2010 | Events/h | ||
| Maeda 2019 | Episodes/h | ||
| Bursts/h | |||
| Mainieri 2012 | Score based on events/recording | ||
| Manfredini 2011 | Events/recording | Total MMA duration (s)/recording | |
| Total MMA duration (s)/hour | Integrated EMG signal (μV x s)/recording | ||
| Manfredini 2016 | Episodes/h | integrated EMG signal (μV x s)/hour | |
| Manfredini 2018 | Episodes/h | ||
| Phasic sleep‐time masticatory muscle activity/h | |||
| Tonic sleep‐time masticatory muscle activity/h | |||
| Mixed sleep‐time masticatory muscle activity/h | |||
| Sleep‐time masticatory muscle activity total number | |||
| Manfredini 2019 | Episodes/h | ||
| Phasic sMMA events/h | |||
| Tonic sMMA events/h | |||
| Mixed sMMA events/h | |||
| Total sMMA events/night | |||
| Matsuda 2016 | Coefficient of variation of interval duration | n‐IEMG (integral values normalised by individual MVC) | |
| Coefficient of variation of burst duration | n‐RMS (root mean square normalised by individual MVC) | ||
| Coefficient of variation of cycle time | |||
| Interval duration | |||
| Burst duration | |||
| Matsumoto 2015 | Events/h | % event duration/night | total EMG activity |
| Minakuchi 2012 | Score based on events/recording | ||
| Minakuchi 2014 | Score based on events/recording | ||
| Minakuchi 2016 | Score based on events/recording | ||
| Miyawaki 2003 | Episodes/h | Episode duration | |
| Miyawaki 2004 | RMMA episodes/h | ||
| Short‐burst episode/h | |||
| Clenching episode/h | |||
| Other EMG episodes/h | |||
| Mizumori 2013 | Events/h | Event duration | |
| Events/night | |||
| Bursts/event | |||
| Mohamed 1997 | Cumulative EMG activity (μV.s) divided by the duration of sleep (min) | ||
| Mude 2017 | Phasic episodes/h | ||
| Tonic episodes/h | |||
| Mixed episodes/h | |||
| Murakami 2014 | Events/h | ||
| Events/night | |||
| Nagamatsu‐Sakaguchi 2017 | Score based on events/recording | ||
| Needham 2013 | Number of clenching/grinding episodes/week | ||
| Nitschke 2011 | Activity periods/h | Activity periods duration | Mean amplitudes (%MVC) |
| Activity periods/night | Max amplitudes (%MVC) | ||
| Time integral (%MVC) | |||
| Ohlmann 2018 | Episodes/h | ||
| Ohlmann 2020 | Episodes/h | ||
| Ono 2008 | Episodes/h | ||
| Episodes/night | |||
| Burst/episode | |||
| Bruxism/h | |||
| Palinkas 2019 | Score based on events/recording | ||
| Po 2013 | RMMA episode frequency (Hz) | Pooled RMMA episodes duration | |
| episodes/ night | |||
| Raphael 2013 | Events/ min | ||
| Rugh 1981 | Mean number of events | Mean duration of events | |
| Rugh 1984 | EMG units | ||
| Rugh 1989 | μV/sec | ||
| Saito‐Murakami 2020 | Events/recording | ||
| Sakagami 2002 | episodes/h | Total bruxism time/h | |
| Bruxism lasting time | |||
| Saueressig 2010 | Score based on events/ recording | ||
| Schmitter 2015 | Episodes/h | Burst duration | Intensity |
| Bursts/h | |||
| Shedden Mora 2012 | Rhythmic NMMA episodes/h | rhythmic NMMA episode duration/h | |
| EMG bursts/h | EMG bursts duration/h | ||
| Burst/episode | |||
| Shedden Mora 2013 | Bursts/h | Durations of bursts/h | |
| Shimada 2019 | Events/h | ||
| Shochat 2007 | Events/recording | ||
| Stock 1983 | n episodes | Duration (not further specified) | Severity (not further specified) |
| Stuginski‐Barbosa 2015 | Events/h | ||
| Total number of events | |||
| Coefficient of variation from the multiple night recordings (CV =SD/mean) | |||
| Suganuma 2007 | Episodes/h | ||
| Episodes/night | |||
| Burst/episode | |||
| Bruxism/h | |||
| Takaoka 2017 | Events/h | ||
| Thymi 2019 | Events/recording | ||
| Events/h | |||
| Coefficient of variation (CV = SD/mean) | |||
| Thymi 2020 | Episodes/h | Bruxism time index (% time bruxing/total sleep time) | |
| Wei 2017 | Clench episodes/h | Mean clench duration | Mean clench bite‐force |
| Clench episodes number | Clench‐related temporalis duty factor (sum of clench episode durations / total recording time) | ||
| Yachida 2012 | Events/h | ||
| Number of events | |||
| Night‐to‐night variability (CV = SD/mean) | |||
| Yamaguchi 2012 | Episodes/h | ||
| Episodes/night | |||
| Yamaguchi 2018 | Bursts/h | ||
| Zhou 2016 | Events/h | Intensity of the EMG (area under EMG curve) |
Abbreviation: AUC, area under the curve; CV, coefficient of variation; EMG, electromyographic; h, hour; MVC, maximum voluntary contraction; n, number; NMMA, nocturnal masticatory muscle activity; RMMA, rhythmic masticatory muscle activity; SD, standard deviation; sMMA, surface masticatory muscle activity; SRA, signal recognition analysis.
4. DISCUSSION
This scoping review provided a comprehensive overview of type 3 and 4 ambulatory EMG signal acquisition and analysis methods, and outcome measures used to date in sleep bruxism literature. Results showed a growing number of studies using ambulatory EMG devices for the assessment of sleep bruxism, especially in the past decade. This finding may reflect technological developments and an overall compliance with the recommendations given by an international group of experts to establish a definitive assessment of sleep bruxism through instrumental methods. 1 , 2
4.1. Recording hardware
Hardware was generally well described in all but two studies. 59 , 65 It is a quite straightforward recommendation that ambulatory EMG devices should have a simple design, with a minimum number of components and wires, for compliance and uncomplicated use in the home setting. For example, cable motion artefacts in the EMG signal can occur as a result of using wired electrodes. 43 Besides, wired and/or voluminous devices may be considered uncomfortable to wear during sleep, especially in the case of multiple night recordings. New, wireless type 4 devices that allow for whole night recordings have been introduced, 14 , 15 and their further development and validation against standardised PSG‐AV assessments is recommended. Future developments may even include wireless type 2 and 3 recording devices, 121 allowing for concomitant assessments of, for example, electroencephalographic (EEG) and breathing. The masseter muscle was the site of preference in 58% of included studies. 11 , 12 , 13 , 14 , 65 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 90 , 91 , 92 , 94 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 , 111 , 117 , 118 The choice of recording site, that is temporalis or masseter muscle, can be guided by practical aspects, such as the presence of facial hair. It can be argued that both sites can provide valid data in terms of masticatory muscle activity during sleep, as long as appropriate impedance levels are assured 122 and recordings undergo thorough quality control for signal‐to‐noise ratios.
4.2. Recording logistics
Sleep bruxism has a time‐variant nature, 41 , 42 which obviously requires multiple recordings to capture this particular feature. Multiple night recordings were performed in the majority of included studies, 11 , 13 , 15 , 19 , 22 , 52 , 53 , 57 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 69 , 70 , 71 , 72 , 74 , 75 , 77 , 84 , 86 , 87 , 89 , 93 , 95 , 98 , 101 , 102 , 103 , 104 , 106 , 107 , 109 , 110 , 111 , 112 , 113 , 114 , 116 , 118 , 119 showing that ambulatory EMG devices are well suited for such assessments.
Proper instructions to participants for handling an EMG device and/or its components are important to enable its flawless functioning and were given in 57% of included studies. 11 , 12 , 13 , 14 , 39 , 52 , 53 , 56 , 59 , 60 , 63 , 64 , 65 , 66 , 69 , 70 , 71 , 73 , 74 , 75 , 76 , 80 , 82 , 84 , 87 , 92 , 93 , 94 , 95 , 102 , 105 , 107 , 109 , 110 , 114 , 117 , 119 Correct placement of the device is crucial in order to obtain good recordings and prevention of artefacts due to, for example, improper skin cleaning that could result in high skin‐electrode impedance. 43 Therefore, it is recommended that the use of the device is trained with participants, either face‐to‐face or through tele‐medicine, and written and/or recorded instructions are provided for reference at home.
Set‐up procedures, that is performance of grimaces, MVCs, etc., for reference purposes were applicable for 47% of included studies. 11 , 14 , 22 , 56 , 61 , 62 , 67 , 68 , 69 , 73 , 77 , 78 , 80 , 81 , 82 , 83 , 84 , 90 , 91 , 95 , 96 , 98 , 100 , 101 , 107 , 108 , 109 , 110 , 111 , 117 Such procedures may be source of variability and can complicate study protocols. 68 In line with the recommendation of the use of simple devices, it can be suggested that only simple and sufficiently standardised set‐up procedures should be preferred, if not avoided altogether.
Finally, on the topic of recording logistics, it is notable that 58% of the studies 12 , 13 , 19 , 30 , 71 , 72 , 74 , 75 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 94 , 96 , 97 , 98 , 100 , 103 , 104 , 105 , 106 , 111 , 112 , 113 , 115 , 116 , 118 did not report on how failures were dealt with. Failures in ambulatory EMG recordings can be divided in two categories. The first is quite straightforward, namely the failure of performance of a part or the entire recording due to detachment or improper placement of the electrode. 22 , 62 , 68 , 73 The second is the presence of artefacts in the EMG signal as a result of high noise levels. 43 Failures can be prevented by adequate device handling and tackled with pre‐set quality criteria, which should include a minimal number of recording nights, and a minimal number of recording hours with acceptable signal‐to‐noise ratio. Ideally, ambulatory EMG recorders should have built‐in features for automatic quality checks of proper placement and connection of the electrode, good functioning of the device, impedance measurements and signal‐to‐noise ratio. Smartphone technologies can be developed to facilitate these functions. 15 It is recommended that future studies employ and report quality criteria based on which recordings are considered failures, in line with similar recommendations given by the American Academy of Sleep Medicine (AASM) for the performance of Out of Centre Sleep Testing (OCST). 123 The OCST standards 123 are an excellent example of comprehensive quality reporting of ambulatory sleep recordings. Similar standards for ambulatory EMG recordings of masticatory muscle activity would be a valuable development in the field.
4.3. Signal acquisition
Adequate reporting on signal acquisition features in EMG studies is recommended by the International Society of Electrophysiology and Kinesiology (ISEK). 45 It allows the reader to identify whether the signal was acquired in a correct way, and facilitates comparison between different studies. Results of the present study show that basic elements of signal acquisition, that is amplifications factors, impedance, bandpass settings, notch filtering, A/D converter resolution and sampling rates, were largely underreported. Underreporting of methodology in EMG studies of masticatory muscles has been described previously. In their systematic review of EMG studies published in 2004, Armijo‐Olivo et al. found that less than 50% of the items proposed by ISEK were reported in approximately 91% of assessed studies. 46 As the authors of this review state, maximum word counts and editorial limitations may contribute to underreporting, and online appendices may help overcome this issue. 46 Moreover, it may be hypothesised that authors’ (lack of) knowledge of the recording processes may affect the way these are reported in a publication.
In addition, quite some variability was encountered amongst studies for certain signal acquisition variables. It is beyond the scope of this review to recommend the ideal features of signal acquisition from the masticatory muscles. The reader is referred to other publications, for example. 43 , 44 , 45 , 122 , 124 Here, some brief comments will be made. Surface EMG measures very small amplitudes, that is microvolt to millivolt, and appropriate amplification is needed, in order to allow proper processing and recording of the signal. 43 , 122 Furthermore, external interfering signals with a so‐called ‘common mode’, that is equal in phase and amplitude, need to be eliminated during the amplification process in order to reduce noise in the EMG signal. 122 , 125 Amplification factors of at least 500 122 and 1000, 124 with a high common mode rejection ratio, that is >95 dB, 44 , 122 have been recommended. In the present review, only three studies reported amplification factors smaller than the recommended 500. 14 , 90 , 115 Furthermore, bandpass settings starting from 5–10 Hz (high pass) 45 to 400–500 Hz (low pass) 45 , 122 have been recommended for surface EMG. In the present review, bandpass settings ranging from 5–500 Hz 90 to 251–610 Hz 61 were encountered. In a number of studies, the high pass filter may have been too high, with a possible consequence of amplitude loss and introduction of artefacts. 43 , 126 Moreover, as per the Nyquist theorem, the signal sampling rate should be at least twice the highest frequency cut‐off of the bandpass filter, 43 , 45 and even higher sampling rates are preferred. Consequently, for surface EMG, sampling rates of at least 1000 Hz are advised, 45 , 125 though up to 5000 Hz sampling has also been recommended. 43 Sampling rates in studies included in the present review were mainly around 1000 14 , 33 , 53 , 91 , 92 , 96 , 97 , 99 , 107 , 110 , 112 , 117 and 2000 Hz, 19 , 32 , 37 , 52 , 59 , 67 , 108 , 109 , 111 that is within acceptable limits.
4.4. Signal analysis
There was an equal number of studies in which EMG devices produced raw EMG signal vs devices in which activity was automatically scored (38% 19 , 30 , 68 , 70 , 83 , 84 , 90 , 91 , 92 , 96 , 97 , 98 , 100 , 101 , 102 , 107 , 108 , 109 , 117 , 118 , 119 and 38%, 13 , 22 , 31 , 69 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 88 , 93 , 103 , 104 , 111 , 113 , 114 , 115 , 116 respectively). Providing scored output has the obvious benefit of simplifying the data collection process. Moreover, it can help reduce investigator‐related measurement errors. 98 However, this requires consensus on the topic of the ideal sleep bruxism scoring method, which, as will be discussed further on, is not yet the case. Furthermore, one should be mindful of the fact that skipping evaluation of the raw EMG signal poses the risk of scoring low quality signal, in terms of signal‐to‐noise ratio and presence of other artefacts.
Importantly, ambulatory type 4 EMG recordings are well known for their inability to correctly identify the actual amount of sleeping time compared to PSG assessments. 3 , 4 Subsequently, investigators are forced to implement alternative methods for defining sleep time in a recording. The current review showed that only a minority of studies, viz. 38%, 11 , 13 , 30 , 76 , 77 , 78 , 80 , 81 , 83 , 90 , 91 , 95 , 96 , 97 , 100 , 101 , 102 , 107 , 109 , 110 , 112 , 116 , 117 provided some description of which part of the signal was analysed as sleep time. Different methods were used, the most important being excluding a pre‐defined amount of time from the start and/or end of the recording, 30 , 32 , 78 , 96 , 97 , 100 , 107 , 109 , 112 , 116 device functioning for only a set amount of time, 13 , 117 and subjective sleep diaries. 11 , 39 , 60 , 101 , 102 , 110 Having different criteria for choosing the length of the recording to be analysed can be an important source of variation amongst different studies. Alongside, abovementioned methods have their limitations, such as excluding actual sleep time for the first two methods, and biased subjective reports and/or forgetting to fill out diaries for the third. Future investigations may consider the use of evolving technologies of wrist‐worn personal health monitoring devices 127 , 128 to define sleep time and overcome these issues. Alternatively, it is advised that studies at least include a description of analysis time in their publications. Other interesting developments are found in the field of portable PSG devices, that is self‐applicable electrode sets that allow for electroencephalographic (EEG) recordings, based on which sleep‐wake states can be discriminated more accurately. 121 , 129 As the authors of these publications suggest, further development and simplifications of these devices and electrodes may prove extremely useful for the field of at‐home assessments of sleep bruxism, and possible also other sleep disorders. 121 , 129
The variables rectification, signal processing and additional filtering of the EMG signal were largely left undescribed in the included studies. As discussed for the topic of signal acquisition variables, it is recommended that publications include descriptions of these procedures. 45 , 46
Twenty‐five different thresholds were used for scoring the sleep bruxism events, with a percentage of the MVC being the most common. The lack of unanimous thresholds to score sleep bruxism events is a topic that has been discussed for over two decades in the field. 10 , 98 The %MVC method started to be used for scoring sleep bruxism events in PSG studies in the mid‐80 s by Phillips et al. 130 These authors, as well as Okeson et al. in 1990, 131 used a 40% MVC threshold to score bruxism events, based on the belief that a smaller threshold would be confused with swallowing. 130 , 131 A 20% MVC criterion was used in the widely implemented scoring criteria proposed in 1996 by Lavigne et al. 29 As the authors of this PSG study state, this threshold ‘was the most frequently associated, when controlled with audio‐video signals, to the beginning of a bruxism episode’. 29 However, in the same year, Ikeda et al. argued that, based on the results of their EMG‐ECG study on the development of criteria to score bruxism events, a 10% MVC threshold should be utilised, with 20% and 40% MVC thresholds being too high. 98 Despite these findings, thresholds of both 10% MVC 34 and 20% MVC 42 were adopted in future publications, and, as seen from the results of the present study, also other values have been used over the years in EMG studies, for example 30% MVC, 71 and 20% of 60% MVC. 62 The use of the multiplication of baseline EMG activity was introduced by the AASM in 2007, 132 with the recommendation to use a threshold of at least two times the baseline amplitude of background EMG of chin EMG activity. This recommendation was kept in subsequent versions of the AASM scoring manual. 133 Raphael et al. used twice the amplitude of relaxed EMG levels while awake in their PSG study, published in 2012, 134 and further work. 135 A few other authors used multiplications of baseline activity in their studies in the following years, for example Mizumori et al. 92 and Maluly et al. 136
Thus, so far, it can be concluded that %MVC thresholds are widely implemented in sleep bruxism research, and that little consensus exists amongst research groups as for the ideal MVC threshold for scoring sleep bruxism events. Furthermore, multiplications of baseline EMG activity have been recommended and implemented to a lesser extent than the %MVC threshold, perhaps due to the fact that this approach is relatively novel as compared to the %MVC method.
Ideally, a single threshold should exist to be used amongst research groups, and future studies are encouraged to focus on establishing this. Here, several issues that affect the choice of such a threshold will be discussed. An ideal threshold should be valid, that is adequately distinguish events from non‐events. In PSG‐AV recordings, this means distinguishing MMAs related to sleep bruxism, from other muscle activities, that is OFAs and OMAs. 3 , 7 , 8 Limited availability of PSG facilities and growing use of ambulatory EMG recorders has led to a thorough revision of concepts regarding how masticatory muscle activity should be assessed within the construct of bruxism. 9 Registrations performed by ambulatory EMG recorders in general assess only MMA, with some exceptions with simultaneous audio recordings (eg 96 ), and assessment of cardiac activity (eg 84 ). Therefore, they do not allow for relating MMAs to grinding sounds, microarousals or other activities such as swallowing, yawning and/or other body movements, as is the case for PSG‐AV recordings. Subsequently, strictly taken, OFAs and OMAs cannot yet be scored based on ambulatory EMG recordings. Even so, ambulatory EMG recorders allow for recording the full spectrum of masticatory muscle activity during sleep, and, as argued in the Background section, are very potent alternatives for PSG‐AV for large‐scale studies and/or multiple night recordings. Given the above, it seems reasonable to suggest the use of a different scoring strategy for PSG‐ and EMG‐derived recordings. This follows the line of reasoning by Manfredini et al. 9 who suggested that a clear distinction should be made between sleep bruxism scored on PSG‐AV recordings, that is PSG/SB, and masticatory muscle activity scored on ambulatory EMG recordings, that is EMG/MMA. As pointed out in the same publication, 9 the definition of a sleep bruxism event may need to shift from the concept of events being related to microarousals as an exclusive association, 137 to events being a part of a spectrum of MMA in broader sense, that is unrelated to other sleep variables, such as microarousals. 9 Instead, EMG/MMA events, and the thresholds used to score them, may need to be defined based on which clinical outcome is investigated, for example tooth wear and pain 9 , 10 This topic will be elaborated in the next section of this discussion.
Alongside with the issue of threshold validity, one should be mindful of factors which may influence its reliable acquisition. An overview of such factors will be given here, in order to assist the ongoing discussion on the choice of an ideal threshold. Using the MVC as a reference value to normalise EMG data is a common and practical way in EMG analysis to overcome the issue of variability in amplitudes between and within individuals. 122 , 125 , 138 It allows for the expression of the magnitudes of EMG tasks as percentages of a reference value, instead of μV or mV. 139 In the dental field, an MVC is relatively easy to perform, for example by having the participant clench in the maximal intercuspal occlusion, or on materials such as rubber tubing, wax or cotton rolls. 140 Differences in acquisition methods may affect the magnitude of the MVC. Mapelli et al. showed that clenching on an arch‐shaped wax pad of 2 mm thickness produces MVCs of significantly higher amplitude and with better test–retest repeatability than clenching on cotton rolls of 10 mm thickness. 140 Moreover, the lack of appropriate training and instruction of participants in performing maximal contractions have an important influence on the MVC 45 , 138 and will most likely lead to submaximal contractions, 139 and consequently to an overestimation of sleep bruxism events. Encouragement of study participants and visual feedback of provoked EMG activity can lead to achieving actual MVCs in healthy, pain‐free individuals. 139 In the home setting, such encouragement and feedback are not readily available, and investigators have little control on whether MVCs are performed correctly. In fact, it has been shown that MVCs can altogether be forgotten to be performed by a substantial number of study participants, resulting in not scorable recordings and subsequent data loss. 68 New technologies, such as smartphone apps and online platforms, can prove extremely useful in this context, 15 through providing reminders and instruction videos for performing the MVCs, and even real‐time feedback regarding the EMG/MVC level. 141
Pain is another important factor that can influence the acquisition of an MVC. It is recommended that the MVC normalisation method is used in healthy individuals without pain and/or injuries, since these conditions will most likely lead to the performance of submaximal contractions. 122 , 139 This is unfortunate for sleep bruxism studies, in which individuals with pain in the masticatory system are often investigated. It has been shown that the force, measured in N, which is exerted during maximal contraction on force transducers, is decreased in individuals with pain in the masticatory system, compared to pain‐free controls. 142 , 143 In addition, Manfredini et al. found that in individuals with myofascial pain the level of EMG activity of masticatory muscles was significantly lower compared to pain‐free controls, during maximum clenching on cotton rolls. 144 On the other hand, Lobbezoo et al. found that even though the EMG amplitude of a MVC in maximal intercuspal occlusion and on biting on a bilateral bite‐fork was lower in individuals with pain in the masticatory muscles compared to pain‐free controls, this difference was not statistically significant. 145 The authors do mention, however, that this lack of statistical significance may be related to the small sample size. 145 Furthermore, Giannakopoulos et al. found an increase in maximum biting EMG activity in intercuspation after pain‐reduction following treatment of non‐dysfunctional myofascial TMD pain. 146 Thus, it remains plausible that the MVC in masticatory muscles is affected by the presence of pain and that subsequently, a sleep bruxism scoring threshold that relies on MVC is not ideal in samples with pain. More research on the exact differences between the overall MVC levels of patients with pain as compared to pain‐free individuals might allow the use of an ‘adjusted’ MVC threshold, that is an MVC threshold that is adjusted depending on the presence of pain. As another alternative, the use of submaximal EMG levels can be considered 122 and has indeed been used in a number of studies included in this review. 22 , 31 , 56 , 61 , 62 , 67 However, this method too can be sensitive for errors and will require careful training of study participants, as well as close monitoring of correct performance through, for example, real‐time feedback practices, as discussed above.
On the other hand, the multiplication of the amplitude of background EMG has the advantage of being less demanding for the participant, hereby overcoming the issues of submaximal ‘maximal’ contractions, forgetting to perform MVCs, and influences of different MVC acquisition methods. In this sense, it may be an interesting threshold to be used in cases where cooperation is challenging, such as paediatric populations and individuals with developmental disabilities. This method has been recommended by the AASM 132 , 133 for scoring sleep bruxism activity in PSG‐AV recordings and seems a promising alternative for the %MVC methods. However, EMG activity of masticatory muscles is found to be higher during wakefulness, compared to sleep. 147 What is more, the levels of background activity have been associated with the presence of chronic pain both during sleep, 18 as well as wakefulness. 148 More specifically, Raphael et al. 18 showed in a PSG study a small, but statistically significant elevation of background EMG activity of masticatory muscles during sleep in patients with myofascial TMD pain, compared to controls. Moreover, the AASM guidelines 132 , 133 recommend a period of at least 3 s of stable background EMG before a sleep bruxism event can be scored. However, variation of background EMG activity over the course of a night may occur, as a result of sweat, secretions of sebaceous glands and changes in conductance, with possible influences on scoring of events. As for muscle activity during wakefulness, Bodéré et al. 148 found increased masticatory muscle EMG activity at rest for individuals with different types of oro‐facial pain, that is myofascial and neuropathic, compared to controls. On the other hand, other studies have not found differences in EMG activity of masticatory muscles at rest in individuals with TMD pain 149 or headache, 150 compared to pain‐free controls, nor between the EMG activity of masticatory muscles on the painful and non‐painful sites in patients with unilateral myofascial pain. 151 Thus, it is possible that the presence of pain is positively associated with differences in background EMG activity in sleep and awake states, and if so, using it as a threshold to score sleep bruxism events will lead to underdiagnosing sleep bruxism in individuals with pain.
Other thresholds, such as specific EMG amplitudes (μV), 65 , 102 , 103 , 104 , 106 , 118 , 119 percentages of the highest occurring bursts, 99 or bite‐force thresholds, 19 , 59 and the mean amplitude of swallowing movements 117 were encountered in included studies. EMG amplitude data are known to be influenced by a number of factors and can greatly vary between and within individuals 122 ; therefore, thresholds based on absolute amplitude values, such as 10 μV, are discouraged. The use of swallowing movements, 117 percentages of highest occurring bursts, 99 as well as percentages of bite‐force with corresponding EMG values 19 , 59 deserve further research. The latter may be interesting specifically in the field of investigating clinical outcomes such as tooth wear and other dental complications, in which the degree of force applied to the dental tissues and/or materials is relevant for the occurrence of complications.
Taken together, based on the above discussion on factors with impact on MVC and background EMG activity values, it can be suggested that the MVC method is suitable for normalising EMG data, and as such a good threshold candidate. On the other hand, it has the drawbacks that its acquisition is influenced by participant cooperation and the presence of pain. A multiplication of background EMG activity is less depending on participant compliance, but may also be influenced by wake–sleep state, as well as the presence of pain. Alternatives include, amongst others, percentages of highest occurring bursts, swallowing, etc. Clearly, more research is needed before broad consensus can be reached on this topic.
4.5. Sleep bruxism outcomes
The results of this review showed that sleep bruxism outcome variables fell into three categories, viz. representing frequency, duration and intensity of MMA, or a combination of two or more categories. Current visions on sleep bruxism assessment support that different sleep bruxism variables, representing different expressions of muscle work, could be related to different clinical outcomes. 9 , 10 As a speculative example, it may be plausible that when investigating pain as a health outcome, frequency and duration of MMA are important predictor variables, whereas duration and intensity could be more relevant in a study on tooth wear or failures of dental restorations. In the latter case, the duration and type of tooth contact would also be interesting predictor variables. A pivotal first step for further development of this concept is the choice of an appropriate threshold for scoring activity on the EMG signal. Next steps could include the classification of EMG devices according to the type of MMA outcomes they are able to asses, in a way similar to the classification of obstructive sleep apnoea devices for out‐of‐centre testing. 152
Furthermore, it was found that the RMMA term was used as a sleep bruxism outcome variable in nine studies. 33 , 57 , 83 , 84 , 91 , 96 , 97 , 108 As discussed above, defining only RMMA’s based on ambulatory EMG devices while ignoring other forms of MMA may not be a representative approach. Instead, clearly defined criteria for scoring EMG/MMA may be more relevant for future studies on the association between sleep bruxism (and sleep MMA in the broader sense) and health outcomes.
Taken together, and in line with previous publications, 9 , 10 it is emphasised that in the field of research with ambulatory EMG recordings a) the focus may need to shift from the concept of scoring sleep bruxism, to that of scoring the whole spectrum of masticatory muscle activity, and b) masticatory muscle activity variables should carefully be selected, based on the assessed health outcome.
4.6. Strengths and limitations
This scoping review has several strengths, the most important of which is its relevance for revealing the evolution of sleep bruxism research. It is the first review that provided a comprehensive and structured overview of signal acquisition and analysis methods used in sleep bruxism studies utilising ambulatory EMG recorders in the past five decades. As such, its results can form a reference point for the rapidly evolving research field of sleep bruxism and can assist researchers, and the industry, in the design and conduct of high‐quality future studies, and in the further development of ambulatory EMG recorders. Furthermore, the results of the study also highlighted the diversity in sleep bruxism outcomes, the importance of scoring the whole spectrum of masticatory muscle activity during sleep and the subsequent need for working towards clearly defined scoring criteria.
Limitations need to be acknowledged as well. The most important is that relevant articles that did assess masticatory muscle activity during sleep but did not use the term ‘bruxism’ may possibly have been missed by our search strategy. This is a limitation that needs to be accepted, since the starting point and main aim of the review was to address the topic of sleep bruxism. The issue of assessing sleep bruxism activity vs. the whole spectrum of masticatory muscle activity was extensively addressed in the discussion of this review, arguing that indeed, in the field of ambulatory EMG recordings, it may be more fruitful and clinically relevant to shift the focus towards a standardised assessment of the whole spectrum of MMA.
5. CONCLUSION
The main conclusions of this scoping review per topic are as follows:
Recording hardware: Recording hardware was generally well described, and it is recommended that future studies continue to do so. Further development of simple, and if possible, wireless devices is encouraged.
Recording logistics: Ambulatory EMG devices are well suited for multiple night recordings. Reports of participant instructions in device handling and dealing with failed recordings were often lacking. Proper reporting hereof is recommended.
Signal acquisition: Basic elements of signal acquisition, for example amplifications factors, impedance and bandpass settings, were generally underreported. It is recommended that studies follow established surface EMG signal acquisition guidelines, and adequately report on those, or refer to a paper describing these.
Signal analysis: The part of the signal that was analysed, and rectification, signal processing and additional filtering of the signal were often underreported. Here too, adequate reporting it is highly recommended. Extensive variability was found for thresholds use to define sleep bruxism events, and further research on the topic that takes into consideration the limitations of each type of threshold is highly recommended.
Sleep bruxism outcomes: Outcomes represented frequency, duration and intensity of masticatory muscle activity, or a combination of two or more categories. Future studies need to take into consideration that variables scored on a signal acquired by an ambulatory EMG device are different entities than those scored by PSG recordings. Finally, it is recommended that the focus may need to shift from the concept of scoring sleep bruxism events to that of scoring the whole spectrum of MMA.
CONFLICT OF INTEREST
Dr. Aarab reports grants from Sunstar Suisse SA and TKI Health Holland related to this work, and grants from SomnoMed‐Goedegebuure and Vivisol BV outside of this work. Dr. Ahlberg has nothing to disclose. Dr. Baba has nothing to disclose. Dr. Carra has nothing to disclose. Dr. De Laat has nothing to disclose. Dr. Gallo has nothing to disclose. Dr. Lavigne reports free access to recording devices without any financial link. Dr. Lobbezoo reports grants from Sunstar Suisse SA, SomnoMed‐Goedegebuure, Airway Management and Vivisol BV outside of this work. Dr. Manfredini has nothing to disclose. Dr. Svensson reports personal fees from Sunstar Suisse SA outside of this work. Dr. Thymi reports grants from Sunstar Suisse SA and TKI Health Holland related to this work.
AUTHOR CONTRIBUTIONS
All co‐authors actively took part in the conceptualisation and preparation of this manuscript. MT performed the analysis of data and drafted a first version of the manuscript. FL, GA, JA, KB, MCC, LG, AL, DM, GL and PS revised the manuscript.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1111/joor.13170.
Supporting information
Supinfo S1
Appendix S2
ACKNOWLEDGEMENTS
This review is in part based on a closed meeting about the development of EMG standards and criteria for the assessment of bruxism, held in Bordeaux, France, on 17 March 2018 hosted by Sunstar Suisse SA. The authors want to thank Bart Bervoets, technician at the Academic Centre for Dentistry Amsterdam (ACTA), for his valuable and critical input on this manuscript.
Thymi M, Lobbezoo F, Aarab G, et al. Signal acquisition and analysis of ambulatory electromyographic recordings for the assessment of sleep bruxism: A scoping review. J Oral Rehabil. 2021;48:846–871. 10.1111/joor.13170
DATA AVAILABILITY STATEMENT
The data that were used for the synthesis of results in this manuscript are available as an online appendix.
REFERENCES
- 1. Lobbezoo F, Ahlberg J, Glaros AG, et al. Bruxism defined and graded: an international consensus. J Oral Rehabil. 2013;40(1):2‐4. [DOI] [PubMed] [Google Scholar]
- 2. Lobbezoo F, Ahlberg J, Raphael KG, et al. International consensus on the assessment of bruxism: report of a work in progress. J Oral Rehabil. 2018;45:837–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Carra MC, Huynh N, Lavigne G. Sleep bruxism: a comprehensive overview for the dental clinician interested in sleep medicine. Dent Clin North Am. 2012;56(2):387‐413. [DOI] [PubMed] [Google Scholar]
- 4. Carra MC, Huynh N, Lavigne GJ. Diagnostic accuracy of sleep bruxism scoring in absence of audio‐video recording: a pilot study. Sleep Breath. 2015;19(1):183‐190. [DOI] [PubMed] [Google Scholar]
- 5. Lavigne GJ, Rompre PH, Poirier G, Huard H, Kato T, Montplaisir JY. Rhythmic masticatory muscle activity during sleep in humans. J Dent Res. 2001;80(2):443‐448. [DOI] [PubMed] [Google Scholar]
- 6. Reding GR, Zepelin H, Robinson JE Jr, Zimmerman SO, Smith VH. Nocturnal teeth‐grinding: all‐night psychophysiologic studies. J Dent Res. 1968;47(5):786‐797. [DOI] [PubMed] [Google Scholar]
- 7. Kato T, Thie NMR, Montplaisir JY, Lavigne G. Bruxism and orofacial movements during sleep. Dent Clin North Am. 2001;45(4):657‐684. [PubMed] [Google Scholar]
- 8. Dutra KM, Pereira FJ Jr, Rompre PH, Huynh N, Fleming N, Lavigne GJ. Oro‐facial activities in sleep bruxism patients and in normal subjects: a controlled polygraphic and audio‐video study. J Oral Rehabil. 2009;36(2):86‐92. [DOI] [PubMed] [Google Scholar]
- 9. Manfredini D, Ahlberg J, Wetselaar P, Svensson P, Lobbezoo F. The bruxism construct: from cut‐off points to a continuum spectrum. J Oral Rehabil. 2019;46:991–997. [DOI] [PubMed] [Google Scholar]
- 10. Manfredini D, Ahlberg J, Aarab G, et al. Towards a Standardized Tool for the Assessment of Bruxism (STAB)—overview and general remarks of a multidimensional bruxism evaluation system. J Oral Rehabil. 2020;47:549–556. [DOI] [PubMed] [Google Scholar]
- 11. Haketa T, Baba K, Akishige S, Fueki K, Kino K, Ohyama T. Utility and validity of a new EMG‐based bruxism detection system. Int J Prosthodont. 2003;16:422‐428. [PubMed] [Google Scholar]
- 12. Ono Y, Suganuma T, Shinya A, Furuya R, Baba K. Effects of sleep bruxism on periodontal sensation and tooth displacement in the molar region. Cranio. 2008;26(4):282‐286. [DOI] [PubMed] [Google Scholar]
- 13. Minakuchi H, Sogawa C, Hara ES, et al. Comparison of platelet serotonin transporter activity in subjects with severe sleep bruxism and control. J Prosthodont Res. 2014;58(4):217‐222. [DOI] [PubMed] [Google Scholar]
- 14. Yamaguchi T, Mikami S, Saito M, Okada K, Gotouda A. A newly developed ultraminiature wearable electromyogram system useful for analyses of masseteric activity during the whole day. J Prosthodont Res. 2018;62(1):110‐115. [DOI] [PubMed] [Google Scholar]
- 15. Thymi M, Verhoeff M, Visscher C, Lobbezoo F. Patient‐based experiences with the use of an ambulatory electromyographic device for the assessment of masticatory muscle activity during sleep. J Oral Rehabil. 2020;47:557–566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Casett E, Réus JC, Stuginski‐Barbosa J, et al. Validity of different tools to assess sleep bruxism: a meta‐analysis. J Oral Rehabil. 2017;44(9):722‐734. [DOI] [PubMed] [Google Scholar]
- 17. Carra MC, Huynh NT, El‐Khatib H, Remise C, Lavigne G. Sleep bruxism, snoring, and headaches in adolescents: short‐term effects of a mandibular advancement appliance. Sleep Med. 2013;14:656‐661. [DOI] [PubMed] [Google Scholar]
- 18. Raphael K, Janal MN, Sirois DA, et al. Masticatory muscle sleep background EMG activity is elevated in myofascial TMD patients. J Oral Rehabil. 2013;40(12):883‐891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Iwasaki LR, Gonzalez YM, Liu H, Marx DB, Gallo LM, Nickel JC. A pilot study of ambulatory masticatory muscle activities in temporomandibular joint disorders diagnostic groups. Orthod Craniofac Res. 2015;18(Suppl. 1):146‐155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Muzalev K, Lobbezoo F, Janal MN, Raphael KG. Inter‐episode sleep bruxism intervals and myofascial face pain. Sleep. 2017;40(8): zsx078. 10.1093/sleep/zsx078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Camparis CM, Formigoni G, Teixeira MJ, Bittencourt LR, Tufik S, de Siqueira JT. Sleep bruxism and temporomandibular disorder: clinical and polysomnographic evaluation. Arch Oral Biol. 2006;51(9):721‐728. [DOI] [PubMed] [Google Scholar]
- 22. Yachida W, Castrillon EE, Baad‐Hansen L, et al. Craniofacial pain and jaw‐muscle activity during sleep. J Dent Res. 2012;91(6):562‐567. [DOI] [PubMed] [Google Scholar]
- 23. Baad‐Hansen L, Thymi M, Lobbezoo F, Svensson P. To what extent is bruxism associated with musculoskeletal signs and symptoms? A systematic review. J Oral Rehabil. 2019;46(9):845‐861. [DOI] [PubMed] [Google Scholar]
- 24. Raphael KG, Santiago V, Lobbezoo F. Is bruxism a disorder or a behaviour? Rethinking the international consensus on defining and grading of bruxism. J Oral Rehabil. 2016;43(10):791‐798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Raphael KG, Santiago V, Lobbezoo F. Bruxism is a continuously distributed behaviour, but disorder decisions are dichotomous (Response to letter by Manfredini, De Laat, Winocur, & Ahlberg (2016)). J Oral Rehabil. 2016;43(10):802‐803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Association ASD . ASDA standards of practice: portable recording in the assessment of obstructive sleep apnea. Sleep. 1994;17(4):372‐377. [DOI] [PubMed] [Google Scholar]
- 27. Collop NA, Anderson WM, Boehlecke B, et al. Clinical guidelines for the use of unattended portable monitors in the diagnosis of obstructive sleep apnea in adult patients. Portable Monitoring Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2007;3(7):737‐747. [PMC free article] [PubMed] [Google Scholar]
- 28. Koyano K, Tsukiyama Y, Ichiki R, Kuwata T. Assessment of bruxism in the clinic. J Oral Rehabil. 2008;35(7):495‐508. [DOI] [PubMed] [Google Scholar]
- 29. Lavigne GJ, Rompre PH, Montplaisir JY. Sleep bruxism: validity of clinical research diagnostic criteria in a controlled polysomnographic study. J Dent Res. 1996;75(1):546‐552. [DOI] [PubMed] [Google Scholar]
- 30. Castroflorio T, Bargellini A, Rossini G, Cugliari G, Deregibus A, Manfredini D. Agreement between clinical and portable EMG/ECG diagnosis of sleep bruxism. J Oral Rehabil. 2015;42(10):759‐764. [DOI] [PubMed] [Google Scholar]
- 31. Stuginski‐Barbosa J, Porporatti AL, Costa YM, Svensson P, Conti PC. Diagnostic validity of the use of a portable single‐channel electromyography device for sleep bruxism. Sleep Breath. 2016;20(2):695‐702. [DOI] [PubMed] [Google Scholar]
- 32. Baad‐Hansen L, Jadidi F, Castrillon E, Thomsen PB, Svensson P. Effect of a nociceptive trigeminal inhibitory splint on electromyographic activity in jaw closing muscles during sleep. J Oral Rehabil. 2007;34(2):105‐111. [DOI] [PubMed] [Google Scholar]
- 33. Yamaguchi T, Abe S, Rompre PH, Manzini C, Lavigne GJ. Comparison of ambulatory and polysomnographic recording of jaw muscle activity during sleep in normal subjects. J Oral Rehabil. 2012;39(1):2‐10. [DOI] [PubMed] [Google Scholar]
- 34. Lavigne GJ, Rompre PH, Poirier G, Huard H, Kato T, Montplaisir JY. Rhythmic masticatory muscle activity during sleep in humans. J Dent Res. 2001;80(2):443‐448. [DOI] [PubMed] [Google Scholar]
- 35. Saito M, Yamaguchi T, Mikami S, et al. Weak association between sleep bruxism and obstructive sleep apnea. A sleep laboratory study. Sleep Breath. 2015;20(2):703‐709. [DOI] [PubMed] [Google Scholar]
- 36. Muzalev K, Visscher CM, Koutris M, Lobbezoo F. Long‐term variability of sleep bruxism and psychological stress in patients with jaw‐muscle pain: report of two longitudinal clinical cases. J Oral Rehabil. 2018;45(2):104‐109. [DOI] [PubMed] [Google Scholar]
- 37. Jadidi F, Castrillon E, Svensson P. Effect of conditioning electrical stimuli on temporalis electromyographic activity during sleep. J Oral Rehabil. 2008;35(3):171‐183. [DOI] [PubMed] [Google Scholar]
- 38. Ware JC, Rugh JD. Destructive bruxism: sleep stage relationship. Sleep. 1988;11(2):172‐181. [DOI] [PubMed] [Google Scholar]
- 39. Baba K, Haketa T, Sasaki Y, Ohyama T, Clark GT. Association between masseter muscle activity levels recorded during sleep and signs and symptoms of temporomandibular. J Orofac Pain. 2005;19(3):226‐231. [PubMed] [Google Scholar]
- 40. Miettinen T, Myllymaa K, Muraja‐Murro A, et al. Polysomnographic scoring of sleep bruxism events is accurate even in the absence of video recording but unreliable with EMG‐only setups. Sleep Breath. 2020;24(3):893‐904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Van Der Zaag J, Lobbezoo F, Visscher CM, Hamburger HL, Naeije M. Time‐variant nature of sleep bruxism outcome variables using ambulatory polysomnography: implications for recognition and therapy evaluation. J Oral Rehabil. 2008;35(8):577‐584. [DOI] [PubMed] [Google Scholar]
- 42. Lavigne GJ, Guitard F, Rompre PH, Montplaisir JY. Variability in sleep bruxism activity over time. J Sleep Res. 2001;10:237‐244. [DOI] [PubMed] [Google Scholar]
- 43. Tankisi H, Burke D, Cui L, et al. Standards of instrumentation of EMG. Clin Neurophysiol. 2020;131:243‐258. [DOI] [PubMed] [Google Scholar]
- 44. Hugger A, Hugger S, Schindler HJ. Surface electromyography of the masticatory muscles for application in dental practice. Current evidence and future developments. Int J Comput Dentistry. 2008;11:81‐106. [PubMed] [Google Scholar]
- 45. Merletti R. Standards for reporting EMG data. J Electromyogr Kinesiol. 1999;9(1):III–IV. [Google Scholar]
- 46. Armijo‐Olivo S, Gadotti I, Kornerup M, Lagravère M, Flores‐Mir C. Quality of reporting masticatory muscle electromyography in 2004: a systematic review. J Oral Rehabil. 2007;34:397‐405. [DOI] [PubMed] [Google Scholar]
- 47. Lobbezoo F, Aarab G, Ahlers MO, et al. Consensus‐based clinical guidelines for ambulatory electromyography and contingent electrical stimulation in sleep bruxism. J Oral Rehabil. 2020;47(2):164‐169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Manfredini D, Ahlberg J, Castroflorio T, Poggio CE, Guarda‐Nardini L, Lobbezoo F. Diagnostic accuracy of portable instrumental devices to measure sleep bruxism: a systematic literature review of polysomnographic studies. J Oral Rehabil. 2014;41(11):836‐842. [DOI] [PubMed] [Google Scholar]
- 49. Yamaguchi T, Mikami S, Maeda M, et al. Portable and wearable electromyographic devices for the assessment of sleep bruxism and awake bruxism: a literature review. Cranio. 2020;1–9. [DOI] [PubMed] [Google Scholar]
- 50. Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J. 2009;26(2):91‐108. [DOI] [PubMed] [Google Scholar]
- 51. Armstrong R, Hall BJ, Doyle J, Waters E. Cochrane update. ‘Scoping the scope’ of a cochrane review. J Public Health. 2011;33(1):147‐150. [DOI] [PubMed] [Google Scholar]
- 52. Jadidi F, Castrillon EE, Nielsen P, Baad‐Hansen L, Svensson P. Effect of contingent electrical stimulation on jaw muscle activity during sleep: a pilot study with a randomized controlled trial design. Acta Odontol Scand. 2013;71(5):1050‐1062. [DOI] [PubMed] [Google Scholar]
- 53. Lee SJ, McCall WD Jr, Kim YK, Chung SC, Chung JW. Effect of botulinum toxin injection on nocturnal bruxism: a randomized controlled trial. Am J Phys Med Rehabil. 2010;89(1):16‐23. [DOI] [PubMed] [Google Scholar]
- 54. Mude AH, Kawakami S, Kato S, Minagi S. Properties of tonic episodes of masseter muscle activity during waking hours and sleep in subjects with and without history of orofacial pain. J Prosthodont Res. 2018;62(2):234‐238. [DOI] [PubMed] [Google Scholar]
- 55. Saueressing AC, Mainieri VC, Grossi PK, et al. Analysis of the influence of a mandibular advancement device on sleep and sleep bruxism scores by means of the BiteStrip and the Sleep Assessment Questionnaire. Int J Prosthodont. 2010;23(3):204‐213. [PubMed] [Google Scholar]
- 56. Schmitter M, Kares‐Vrincianu A, Kares H, Bermejo JL, Schindler HJ. Sleep‐associated aspects of myofascial pain in the orofacial area among Temporomandibular Disorder patients and controls. Sleep Med. 2015;16(9):1056‐1061. [DOI] [PubMed] [Google Scholar]
- 57. Shimada A, Castrillon EE, Svensson P. Revisited relationships between probable sleep bruxism and clinical muscle symptoms. J Dent. 2019;S0300–5712(19):30022‐30023. [DOI] [PubMed] [Google Scholar]
- 58. Abekura H, Yokomura M, Sadamori S, Hamada T. The initial effects of occlusal splint vertical thickness on the nocturnal EMG activities of masticatory muscles in subjects with a bruxism habit. Int J Prosthodont. 2008;21(2):116‐120. [PubMed] [Google Scholar]
- 59. Khawaja SN, McCall W, Dunford R, et al. Infield masticatory muscle activity in subjects with pain‐related temporomandibular disorders diagnoses. Orthod Craniofac Res. 2015;18(Suppl. 1):137‐145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Wei F, Van Horn MH, Coombs MC, et al. A pilot study of nocturnal temporalis muscle activity in TMD diagnostic groups of women. J Oral Rehabil. 2017;44(7):517‐525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Zhou W‐N, Fu H‐Y, Du Y‐F, et al. Short‐term effects of repetitive transcranial magnetic stimulation on sleep bruxism ‐ a pilot study. Int J Oral Sci. 2016;8(1):61‐65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Conti PC, Stuginski‐Barbosa J, Bonjardim LR, Soares S, Svensson P. Contingent electrical stimulation inhibits jaw muscle activity during sleep but not pain intensity or masticatory muscle pressure pain threshold in self‐reported bruxers: a pilot study. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;117(1):45‐52. [DOI] [PubMed] [Google Scholar]
- 63. Hammoudi W, Trulsson M, Smedberg JI, Svensson P. Phenotypes of patients with extensive tooth wear—a novel approach using cluster analysis. J Dent. 2019;82:22‐29. [DOI] [PubMed] [Google Scholar]
- 64. Jonsgar C, Hordvik PA, Berge ME, Johansson AK, Svensson P, Johansson A. Sleep bruxism in individuals with and without attrition‐type tooth wear: an exploratory matched case‐control electromyographic study. J Dent. 2015;43(12):1504‐1510. [DOI] [PubMed] [Google Scholar]
- 65. Clark GT, Beemsterboer P, Rugh JD. The treatment of nocturnal bruxism using contingent EMG feedback with an arousal task. Behav Res Ther. 1981;19:451‐455. [DOI] [PubMed] [Google Scholar]
- 66. Needham R, Davies SJ. Use of the Grindcare(R) device in the management of nocturnal bruxism: a pilot study. Br Dent J. 2013;215(1):E1. [DOI] [PubMed] [Google Scholar]
- 67. Raphael KG, Janal MN, Sirois DA, Svensson P. Effect of contingent electrical stimulation on masticatory muscle activity and pain in patients with a myofascial temporomandibular disorder and sleep bruxism. J Orofac Pain. 2013;27(1):21‐31. [DOI] [PubMed] [Google Scholar]
- 68. Thymi M, Visscher CM, Wismeijer D, Lobbezoo F. Associations between sleep bruxism and (peri‐)implant complications: lessons learned from a clinical study. BDJ Open. 2020;6(1): 10.1038/s41405-020-0028-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Takaoka R, Ishigaki S, Yatani H, Ogata S, Hayakawa K. Evaluation of genetic factors involved in nocturnal electromyographic activity of masticatory muscles in twins. Clin Oral Investig. 2017;21(1):319‐325. [DOI] [PubMed] [Google Scholar]
- 70. Thymi M, Shimada A, Lobbezoo F, Svensson P. Clinical jaw‐muscle symptoms in a group of probable sleep bruxers. J Dent. 2019;85:81‐87. [DOI] [PubMed] [Google Scholar]
- 71. Carvalho Bortoletto C, da Silva C, FdCCS M, et al. Evaluation of electromyographic signals in children with bruxism before and after therapy with Melissa Officinalis L—a randomized controlled clinical trial. J Phys Ther Sci. 2016;28:738‐742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Castro Mattia PR, Panitz Selaimen CM, Teixeira ER, Fagondes SC, Grossi ML. The effects of sleeping with or without prostheses on sleep quality, sleep bruxism, and signs of obstructive sleep apnea syndrome: a pilot study. Int J Prosthodont. 2018;31(3):197‐205. [DOI] [PubMed] [Google Scholar]
- 73. Karakoulaki S, Tortopidis D, Andreadis D, Koidis P. Relationship between sleep bruxism and stress determined by saliva biomarkers. Int J Prosthodont. 2015;28(5):467‐474. [DOI] [PubMed] [Google Scholar]
- 74. Minakuchi H, Sakaguchi C, Hara ES, et al. Multiple sleep bruxism data collected using a self‐contained EMG detector/analyzer system in asymptomatic healthy subjects. Sleep Breath. 2012;16:1069‐1072. [DOI] [PubMed] [Google Scholar]
- 75. Minakuchi H, Sogawa C, Miki H, et al. Sleep bruxism frequency and platelet serotonin transporter activities in young adult subjects. Sleep Breath. 2016;20(1):271‐276. [DOI] [PubMed] [Google Scholar]
- 76. Nagamatsu‐Sakaguchi C, Minakuchi H, Clark GT, Kuboki T. Relationship between the frequency of sleep bruxism and the prevalence of signs and symptoms of temporomandibular disorders in an adolescent population. Int J Prosthodont. 2008;21:292‐298. [PubMed] [Google Scholar]
- 77. Saueressig AC, Mainieri VC, Grossi PK, et al. Analysis of the influence of a mandibular advancement device on sleep and sleep bruxism scores by means of the BiteStrip and the Sleep Assessment Questionnaire. Int J Prosthodont. 2010;23:204‐213. [PubMed] [Google Scholar]
- 78. Shochat T, Gavish A, Arons E, et al. Validation of the BiteStrip screener for sleep bruxism. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104(3):e32‐e39. [DOI] [PubMed] [Google Scholar]
- 79. Ahlberg K, Savolainen A, Paju S, et al. Bruxism and sleep efficiency measured at home with wireless devices. J Oral Rehabil. 2008;35(8):567‐571. [DOI] [PubMed] [Google Scholar]
- 80. Mainieri VC, Saueressig AC, Pattussi MP, Fagondes SC, Grossi ML. Validation of the Bitestrip versus polysomnography in the diagnosis of patients with a clinical history of sleep bruxism. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113(5):612‐617. [DOI] [PubMed] [Google Scholar]
- 81. Palinkas M, Seidel Coscarella L, Hiromo Hotta T, et al. Influence of sleep bruxism severity on masticatory efficiency: electromyographic analysis. Arch Ital Biol. 2019;157(2–3):59‐65. [DOI] [PubMed] [Google Scholar]
- 82. Camara‐Souza MB, de Figueredo OMC, Rodrigues Garcia RCM. Association of sleep bruxism with oral health‐related quality of life and sleep quality. Clin Oral Investig. 2019;23(1):245‐251. [DOI] [PubMed] [Google Scholar]
- 83. Castroflorio T, Deregibus A, Bargellini A, Debernardi C, Manfredini D. Detection of sleep bruxism: comparison between an electromyographic and electrocardiographic portable holter and polysomnography. J Oral Rehabil. 2014;41(3):163‐169. [DOI] [PubMed] [Google Scholar]
- 84. Deregibus A, Castroflorio T, Bargellini A, Debernardi C. Reliability of a portable device for the detection of sleep bruxism. Clin Oral Investig. 2014;18(8):2037‐2043. [DOI] [PubMed] [Google Scholar]
- 85. Manfredini D, Arreghini A, Lombardo L, et al. Assessment of anxiety and coping features in bruxers: a portable electromyographic and electrocardiographic study. J Oral Facial Pain Headache. 2016;30(3):249‐254. [DOI] [PubMed] [Google Scholar]
- 86. Manfredini D, Lombardo L, Vigiani L, Arreghini A, Siciliani G. Effects of invisible orthodontic retainers on masticatory muscles activity during sleep: a controlled trial. Prog Orthod. 2018;19(1):24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Ohlmann B, Bomicke W, Habibi Y, Rammelsberg P, Schmitter M. Are there associations between sleep bruxism, chronic stress, and sleep quality? J Dent. 2018;74:101‐106. [DOI] [PubMed] [Google Scholar]
- 88. Manfredini D, Lombardo L, Visentin A, Arreghini A, Siciliani G. Correlation between sleep‐time masseter muscle activity and tooth wear: an electromyographic study. J Oral Facial Pain Headache. 2019;33(2):199‐204. [DOI] [PubMed] [Google Scholar]
- 89. Ohlmann B, Waldecker M, Leckel M, et al. Correlations between sleep bruxism and temporomandibular disorders. J Clin Med. 2020;9(2):611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Maeda M, Yamaguchi T, Mikami S, et al. Quantitative analyses of jaw‐opening muscle activity during the active phase of jaw‐closing muscles in sleep bruxism. J Sleep Res, 2019, 29(6):e12922 . [DOI] [PubMed] [Google Scholar]
- 91. Matsuda S, Yamaguchi T, Mikami S, Okada K, Gotouda A, Sano K. Rhythm and amplitude of rhythmic masticatory muscle activity during sleep in bruxers ‐ comparison with gum chewing. Cranio. 2016;34(4):234‐241. [DOI] [PubMed] [Google Scholar]
- 92. Mizumori T, Sumiya M, Kobayashi Y, Inano S, Yatani H. Prediction of sleep bruxism events by increased heart rate. Int J Prosthodont. 2013;26(3):239‐243. [DOI] [PubMed] [Google Scholar]
- 93. Sakagami R, Horri T, Ino S, Matoba K, Kato H, Kawanami M. Development of a portable bruxism monitoring and analysis device equipped with a microcomputer and its practical application. Front Med Biol Engng. 2002;11(4):295‐306. [DOI] [PubMed] [Google Scholar]
- 94. Suganuma T, Ono Y, Shinya A, Furuya R. The effect of bruxism on periodontal sensation in the molar region: a pilot study. J Prosthetic Dentistry. 2007;98(1):30‐35. [DOI] [PubMed] [Google Scholar]
- 95. Saito‐Murakami K, Sato M, Otsuka H, Miura H, Terada N, Fujisawa M. Daytime masticatory muscle electromyography biofeedback regulates the phasic component of sleep bruxism. J Oral Rehabil. 2020;47(7):827‐833. [DOI] [PubMed] [Google Scholar]
- 96. Miyawaki S, Tanimoto Y, Araki Y, Katayama A, Fujii A, Takano‐Yamamoto T. Association between nocturnal bruxism and gastroesophageal reflux. Sleep. 2003;26(7):888‐892. [DOI] [PubMed] [Google Scholar]
- 97. Miyawaki S, Tanimoto Y, Araki Y, Katayama A, Imai M, Takano‐Yamamoto T. Relationships among nocturnal jaw muscle activities, decreased esophageal pH, and sleep positions. Am J Orthod Dentofacial Orthop. 2004;126(5):615‐619. [DOI] [PubMed] [Google Scholar]
- 98. Ikeda T, Nishigawa K, Kondo K, Takeuchi H, Clark GT. Criteria for the detection of sleep‐associated bruxism in humans. J Orofac Pain. 1996;10:270‐282. [PubMed] [Google Scholar]
- 99. Gallo L, Lavigne G, Rompre PH, Palla S. Reliability of scoring EMG orofacial events polysomnography compared with ambulatory recordings. J Sleep Res. 1997;6:259‐263. [DOI] [PubMed] [Google Scholar]
- 100. Kato S, Ekuni D, Kawakami S, Mude AH, Morita M, Minagi S. Relationship between severity of periodontitis and masseter muscle activity during waking and sleeping hours. Arch Oral Biol. 2018;90:13‐18. [DOI] [PubMed] [Google Scholar]
- 101. Nitschke I, Meier L, Farella M, Palla S, Gallo LM. Nocturnal masseter electromyographic activity of complete denture wearers. Gerodontology. 2012;29(2):e595‐e601. [DOI] [PubMed] [Google Scholar]
- 102. Shedden Mora M, Weber D, Borkowski S, Rief W. Nocturnal masseter muscle activity is related to symptoms and somatization in temporomandibular disorders. J Psychosom Res. 2012;73(4):307‐312. [DOI] [PubMed] [Google Scholar]
- 103. Rugh JD, Barghi N, Drago CJ. Experimental occlusal discrepancies and nocturnal bruxism. J Prosthet Dent. 1984;51:548‐553. [DOI] [PubMed] [Google Scholar]
- 104. Rugh JD, Graham GS, Smith JC, Ohrbach RK. Effects of canine versus molar occlusal splint guidance on nocturnal bruxism and craniomandibular symptomatology. J Craniomandib Disord. 1989;3:203‐210. [PubMed] [Google Scholar]
- 105. Murakami T, Masaki C, Takahashi H, et al. Sleep bruxism is affected by peripheral benzodiazepine receptor gene polymorphisms. Int J Stomatol Occlusion Med. 2014;7(1):13‐17. [Google Scholar]
- 106. Mohamed SE, Christensen LV, Penchas J. A randomized double‐blind clinical trial of the effect of amitriptyline on nocturnal masseteric motor activity (sleep bruxism). Cranio. 1997;15(4):326‐332. [DOI] [PubMed] [Google Scholar]
- 107. Harada T, Ichiki R, Tsukiyama Y, Koyano K. The effect of oral splint devices on sleep bruxism: a 6‐week observation with an ambulatory electromyographic recording device. J Oral Rehabil. 2006;33(7):482‐488. [DOI] [PubMed] [Google Scholar]
- 108. Po JM, Gallo LM, Michelotti A, Farella M. Comparison between the rhythmic jaw contractions occurring during sleep and while chewing. J Sleep Res. 2013;22(5):593‐599. [DOI] [PubMed] [Google Scholar]
- 109. Matsumoto H, Tsukiyama Y, Kuwatsuru R, Koyano K. The effect of intermittent use of occlusal splint devices on sleep bruxism: a 4‐week observation with a portable electromyographic recording device. J Oral Rehabil. 2015;42(4):251‐258. [DOI] [PubMed] [Google Scholar]
- 110. Gallo LM, Salis Gross SS, Palla S. Nocturnal masseter EMG activity of healthy subjects in a natural environment. J Dent Res. 1999;78(8):1436‐1444. [DOI] [PubMed] [Google Scholar]
- 111. Čadová M, Gallo LM. Electromyographic signal analysis tool: masseter electromyography activity in a natural environment. Russ J Biomech. 2014;18(4):374‐382. [Google Scholar]
- 112. Abekura H, Yokomura M, Sadamori S, Hamada T. The initial effects of occlusal splint vertical thickness on the nocturnal EMG activities of masticatory muscles in subjects with a bruxism habit. Int J Prosthodont. 2008;21:116‐120. [PubMed] [Google Scholar]
- 113. Clarke NG, Townsend DR, Carey SE. Bruxing patterns in man during sleep. J Oral Rehabil. 1984;11:123‐127. [DOI] [PubMed] [Google Scholar]
- 114. Kardachi BJ, Clarke NG. The use of biofeedback to control bruxism. J Periodontol. 1977;48(10):639‐642. [DOI] [PubMed] [Google Scholar]
- 115. Stock P, Clarke NG. Monitoring bruxism. Med Biol Eng Comput. 1983;21:295‐300. [DOI] [PubMed] [Google Scholar]
- 116. Clarke NG, Townsend DR. Distribution of nocturnal bruxing patterns is man. J Oral Rehabil. 1984;11:529‐534. [DOI] [PubMed] [Google Scholar]
- 117. Manfredini D, Fabbri A, Peretta R, Guarda‐Nardini L, Lobbezoo F. Influence of psychological symptoms on home‐recorded sleep‐time masticatory muscle activity in healthy subjects. J Oral Rehabil. 2011;38(12):902‐911. [DOI] [PubMed] [Google Scholar]
- 118. Rugh JD, Johnson RW. Temporal analysis of nocturnal bruxism during EMG feedback. J Periodontol. 1981;52(5):263‐265. [DOI] [PubMed] [Google Scholar]
- 119. Shedden Mora M, Weber D, Neff A, Rief W. Biofeedback‐based cognitive‐behavioral treatment compared with occlusal splint for temporomandibular disorder a randomized controlled trial. Clin J Pain. 2013;29:1057‐1065. [DOI] [PubMed] [Google Scholar]
- 120. Sakagami R, Horii T, Ino S, Matoba K, Kato H, Kawanami M. Development of a portable bruxism monitoring and analysis device equipped with a microcomputer and its practical implication. Front Med Biol Eng. 2002;11(4):295‐306. [DOI] [PubMed] [Google Scholar]
- 121. Miettinen T, Myllymaa K, Westeren‐Punnonen S, et al. Success rate and technical quality of home polysomnography with self‐applicable electrode set in subjects with possible sleep bruxism. IEEE J Biomed Health Inform. 2018;22(4):1124‐1132. [DOI] [PubMed] [Google Scholar]
- 122. Konrad P. The ABC of EMG: A Practical Introduction to Kinesiological Electromyography. , 1.4 ed. Arizona, USA: Noraxon U.S.A., Inc.; 2006. [Google Scholar]
- 123. Medicine AAoS . Standards for Accreditation of Out of Center Sleep Testing (OCST) in Adult Patients. 2011.
- 124. Wang J, Tang L, Bronlund J. Surface EMG signal amplification and filtering. Int J Comput Appl. 2013;82(1):15‐22. [Google Scholar]
- 125. Hugger A, Hugger S, Schindler H. Surface electromyography of the masticatory muscles for application in dental practice. Current evidence and future developments. Int J Comput Dent. 2008;11:81‐106. [PubMed] [Google Scholar]
- 126. van Boxtel A. Optimal signal bandwidth for the recording of surface EMG activity of facial, jaw, oral, and neck muscles. Psychophysiology. 2001;38:22‐34. [PubMed] [Google Scholar]
- 127. Mantua J, Gravel N, Spencer R. Reliability of sleep measures from four personal health monitoring devices compared to research‐based actigraphy and polysomnography. Sensors. 2016;16(5):646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Haghayegh S, Khoshnevis S, Smolensky M, Diller K, Castriotta R. Accuracy of wristband Fitbit models in assessing sleep: systematic review and meta‐analysis. J Med Internet Res. 2019;21(11):e16273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Myllymaa S, Lepola P, Töyräs J, et al. New disposable forehead electrode set with excellent signal quality and imaging compatibility. J Neurosci Methods. 2013;215(1):103‐109. [DOI] [PubMed] [Google Scholar]
- 130. Phillips BA, Okeson J, Paesani D, Gilmore R. Effect of sleep position on sleep apnea and parafunctional activity. Chest. 1986;90(3):424‐429. [DOI] [PubMed] [Google Scholar]
- 131. Okeson J, Phillips B, Berry D, Cook Y, Paesani DA, Galante J. Nocturnal bruxing events in healthy geriatric subjects. J Oral Rehabil. 1990;17:411‐418. [DOI] [PubMed] [Google Scholar]
- 132. Iber C, Ancoli‐Israel S, Chesson A, Quan SF. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications. Westchester, IL: American Academy of Sleep Medicine; 2007. [Google Scholar]
- 133. Berry R, Albertario C, Harding S, et al. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications. Version 2.5. Darien, IL: American Academy of Sleep Medicine; 2018. [Google Scholar]
- 134. Raphael KG, Sirois DA, Janal MN, et al. Sleep bruxism and myofascial temporomandibular disorders. J Am Dent Assoc. 2012;143(11):1223‐1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Raphael KG, Janal MN, Sirois DA, et al. Masticatory muscle sleep background electromyographic activity is elevated in myofascial temporomandibular disorder patients. J Oral Rehabil. 2013;40(12):883‐891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Maluly M, Andersen ML, Dal‐Fabbro C, et al. Polysomnographic study of the prevalence of sleep bruxism in a population sample. J Dent Res. 2013;92(7 Suppl.):97S‐103S. [DOI] [PubMed] [Google Scholar]
- 137. Lavigne GJ, Khoury S, Abe S, Yamaguchi T, Raphael K. Bruxism physiology and pathology: an overview for clinicians. J Oral Rehabil. 2008;35(7):476‐494. [DOI] [PubMed] [Google Scholar]
- 138. Burden A, Bartlett R. Normalisation of EMG amplitude: an evaluation an comparison of old and new methods. Med Eng Phys. 1999;21:247‐257. [DOI] [PubMed] [Google Scholar]
- 139. Burden A. How should we normalize electromyograms obtained from healthy participants? What we have learned from over 25 years of research. J Electromyogr Kinesiol. 2010;20(6):1023‐1035. [DOI] [PubMed] [Google Scholar]
- 140. Mapelli A, Tartaglia GM, Connelly ST, Ferrario VF, De Felicio CM, Sforza C. Normalizing surface electromyographic measures of the masticatory muscles: comparison of two different methods for clinical purpose. J Electromyogr Kinesiol. 2016;30:238‐242. [DOI] [PubMed] [Google Scholar]
- 141. Prasad S, Paulin M, Cannon RD, Palla S, Farella M. Smartphone‐assisted monitoring of masticatory muscle activity in freely moving individuals. Clin Oral Investig. 2019;23:3601–3611. [DOI] [PubMed] [Google Scholar]
- 142. Testa M, Geri T, Pitance L, et al. Alterations in jaw clenching force control in people with myogenic temporomandibular disorders. J Electromyogr Kinesiol. 2018;43:111‐117. [DOI] [PubMed] [Google Scholar]
- 143. Kogawa EM, Calderon PS, Lauris JR, Araujo CR, Conti PC. Evaluation of maximal bite force in temporomandibular disorders patients. J Oral Rehabil. 2006;33(8):559‐565. [DOI] [PubMed] [Google Scholar]
- 144. Manfredini D, Cocilovo F, Favero L, Ferronato G, Tonello S, Guarda‐Nardini L. Surface electromyography of jaw muscles and kinesiographic recordings: diagnostic accuracy for myofascial pain. J Oral Rehabil. 2011;38(11):791‐799. [DOI] [PubMed] [Google Scholar]
- 145. Lobbezoo F, van der Glas H, van der Bilt A, Buchner R, Bosman F. Sensitivity of the jaw‐jerk reflex in patients with myogenous temporomandibular disorder. Arch Oral Biol. 1996;41(6):553‐563. [DOI] [PubMed] [Google Scholar]
- 146. Giannakopoulos NN, Rauer AK, Hellmann D, Hugger S, Schmitter M, Hugger A. Comparison of device‐supported sensorimotor training and splint intervention for myofascial temporomandibular disorder pain patients. J Oral Rehabil. 2018;45(9):669‐676. [DOI] [PubMed] [Google Scholar]
- 147. Okura K, Kato T, Montplaisir JY, Sessle BJ, Lavigne GJ. Quantitative analysis of surface EMG activity of cranial and leg muscles across sleep stages in human. Clin Neurophysiol. 2006;117(2):269‐278. [DOI] [PubMed] [Google Scholar]
- 148. Bodere C, Tea SH, Giroux‐Metges MA, Woda A. Activity of masticatory muscles in subjects with different orofacial pain conditions. Pain. 2005;116(1–2):33‐41. [DOI] [PubMed] [Google Scholar]
- 149. Nicholson RA, Townsend DR, Gramling SA. Influence of a scheduled‐waiting task on EMG reactivity and oral habits among facial pain patients and no‐pain controls. Appl Psychophysiol Biofeedback. 2000;25(4):203‐219. [DOI] [PubMed] [Google Scholar]
- 150. Ong JC, Nicholson RA, Gramling SA. EMG reactivity and oral habits among young adult headache sufferers and painfree controls in a scheduled‐waiting task. Appl Psychophysiol Biofeedback. 2003;28(4):255‐265. [DOI] [PubMed] [Google Scholar]
- 151. Manfredini D, Cocilovo F, Stellini E, Favero L, Guarda‐Nardini L. Surface electromyography findings in unilateral myofascial pain patients: comparison of painful vs non pain. Pain Med. 2013;14:1848‐1853. [DOI] [PubMed] [Google Scholar]
- 152. Collop NA, Tracy SL, Kapur V, et al. Obstructive sleep apnea devices for out‐of‐center (OOC) testing: technology evaluation. J Clin Sleep Med. 2011;7(5):531‐548. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supinfo S1
Appendix S2
Data Availability Statement
The data that were used for the synthesis of results in this manuscript are available as an online appendix.


