Abstract
Background
Skin‐related changes, such as fine lines, wrinkles, and acne scarring, are a source of distress to both men and women. Nanofractional radiofrequency delivers thermal energy to skin layers leading to dermal remodeling that can address skin conditions related to aging. The objective of this study was to evaluate the subject satisfaction of nanofractional radiofrequency for the treatment of facial wrinkles and acne scarring in both lighter and darker skin tones.
Materials and methods
30 subjects (skin types II‐VI) were enrolled in this prospective, evaluator‐blind study. The average age of subjects was 51.9 ± 13.5 years. Subjects received three treatments at 3‐ to 5‐week intervals on both sides of the face using the 80‐ or the 160‐pin tip disposables. Follow‐up visits were conducted at 6‐ and 12 weeks after the last treatment. Subject satisfaction was evaluated using a self‐assessment of a reduction of wrinkles or acne scars, and subject satisfaction questionnaire. Pain, tolerability, and safety were monitored throughout.
Results
Subjects treated for acne or wrinkles were satisfied with their treatment at both the 6‐week and 12‐week follow‐up visit (mean score 3.0; range 0 = very unsatisfied to 4 = very satisfied). The treatments were well tolerated at all treatment sessions, averaging a score of 3.5 on the tolerability scale (0 = very intolerable to 4 = very tolerable) with treatment‐associated pain reported to be mild (3.2 out of 10). There were no adverse events or unanticipated side effects.
Conclusions
This clinical study demonstrates subjects are satisfied with nanofractional radiofrequency treatments for improvement of their wrinkles and acne scars.
Keywords: acne scars, fractional radiofrequency, rhytids, wrinkles
1. INTRODUCTION
According to data collected from the American Society of Plastic Surgeons, 15.9 million minimally invasive cosmetic procedures were conducted in 2018, an increase of 2% from 2017 and a 228% from 2000. 1 These numbers show that non‐invasive procedures are outpacing surgical procedures. As a result, in order to meet this rising demand, physicians in the field must be prepared to provide safe and dependable nonsurgical rejuvenation. Part of the increase in non‐invasive procedures can be attributed to the rise in new technologies offered to patients and an increase in scientific knowledge of skin metabolism. 2 One of these newer and non‐invasive technologies is nanofractional radiofrequency. Nanofractional radiofrequency technology has been shown to improve skin laxity and to effectively treat various skin conditions related to aging, resulting in appearance alterations such as rhytids. 3
Patient satisfaction has increasingly received recognition as an important component to assessing quality of clinical care. 4 , 5 , 6 , 7 , 8 , 9 Patient satisfaction is the extent to which healthcare recipients perceive their experience and is a crucial indicator of perceived clinical outcomes. Additionally, it can play an influential role in patient retention, compliance, and medical malpractice claims. 10 Studies have shown that patients who are satisfied with their outcomes in the management of their chronic disease, go on to have improved outcomes when compared to those who are less satisfied. 11 , 12 In aesthetic procedures, satisfaction of patients may be one of the most important outcome metrics in determining if the patients will return for additional procedures. Understanding the factors that influence patient satisfaction (ie, procedural pain, treatment time) especially in aesthetic surgery, is essential for maintaining a successful practice. Knowing about these factors enables physicians to make changes to aspects of their treatment that are negatively impacting their patients' satisfaction.
The efficacy and safety of nanofractional radiofrequency in wrinkles and acne scarring have already been established in previously published studies. 2 , 7 , 13 , 14 , 15 , 16 , 17 The objective of this study was, therefore, to evaluate the satisfaction of the patient following treatment with a nanofractional radiofrequency device, in patients seeking treatment for facial rhytids and acne scarring.
2. MATERIALS AND METHODS
2.1. Participants
Data presented in this manuscript is a combination of two prospective, open‐label, single‐arm clinical studies conducted at one clinical center (New York, USA) between December 2018 and October 2019. The studies' protocols complied with the CONSORT 2010 statement for reporting controlled trial and the trials were conducted according to the Declaration of Helsinki and all its revisions. They were approved by the Institutional Review Board and registered to the ClinicalTrials.gov Registry (ID numbers: NCT03821324 and NCT03831477). All subjects provided written informed consent to participate in the trials.
Male and female subjects who met the inclusion criteria for nanofractional radiofrequency treatment of acne scarring and facial rhytids were enrolled. Subjects over the age of 21 and of any Fitzpatrick skin type (I‐VI) were eligible to participate. Exclusion criteria included the presence of a pacemaker or a defibrillator, metal implants in the treated anatomy, pregnancy, recent surgery in treatment area, and acute or chronic infection in the area. Women of child‐bearing age were required to use a reliable method of birth control at least three months prior to study enrollment.
2.2. Description of treatment
Skin in the treatment area was cleansed and dried prior to treatment. Treatments were performed using the Venus Viva™ (Venus Concept Inc, Toronto, Canada). Subjects were in a supine position for treatment. The distal section of the applicator on the device was cleaned and fitted with a new tip (80‐pin of up to 124 mJ/pin and 160‐pin of up to 62 mJ/pin) per practitioner preference. The 160‐pin tip was used for milder cases, whereas the 80‐pin tip was used for more severe cases. The applicator was held perpendicular to and in close contact with the skin surface for the duration of the treatment. Treatment parameters per case, such as voltage and pulse duration, were determined at the discretion of the primary investigator (N.S.). Nothing was applied to the treatment area immediately after the treatment. Furthermore, subjects were advised to not apply anything to the treated area for the 24 h period after the treatment and to avoid possible thermal or mechanical impact. Subjects were also instructed to use a high factor of sunscreen (SPF ≥ 30) to protect the treated area from direct sunlight beginning the next day and for the entire period of the study, which was approximately 6 months.
2.3. Outcome measures
Performance outcomes were the subjects' assessments of satisfaction with the treatment using a Subject Satisfaction Scale (SSS) at 6‐ and 12 weeks post‐treatment. Subject satisfaction was evaluated with the following 5‐point Likert scale: (4) very satisfied, (3) satisfied, (2) no opinion, (1) unsatisfied, and (0) very unsatisfied. Immediately after each treatment, subject discomfort was assessed using a 10 cm Visual Analog Scale (VAS) 18 , 19 on a scale from 0 cm (no pain) to 10 cm (pain as bad as it can be). Subjects were not permitted to view their previous VAS or SSS treatment scores. Additionally, following treatment, subject tolerability was recorded using a scale: (4) very tolerable, (3) tolerable, (2) having no opinion, (1) intolerable, and (0) very intolerable. All adverse events (AEs) were recorded up to the 12‐week post‐treatment visit.
Additional satisfaction analysis was in the form of a treatment evaluation questionnaire conducted at 6‐week follow‐up and 12‐week follow‐up. Subjects were asked what level of improvement they experienced (mild, moderate, or significant), whether they would recommend this treatment to a friend (yes or no), which treatment they experienced the started noticing changes in their skin (after the first treatment, after the second treatment, at the end of all treatments, or at follow‐up visits). Subjects with acne scars were asked where on their face, they saw the most reduction of scarring (nose, forehead, cheeks, or chin), and any other skin changes they noticed. Subjects with wrinkles were asked what specific changes they saw in their skin (smoother skin, softer skin, firmer skin, and improvement overall in wrinkles and fine lines) and which areas of the face had the most improvement of wrinkles (forehead, eyes, or mouth).
2.4. Statistical analysis
Quantitative data are presented as mean, median, and/or range, while qualitative data are presented as percentage (%). Unless otherwise stated, standard error (SE) was shown. Two‐sided Student's paired t test was used to test for changes from baseline to follow‐up visits at 6‐ and 12 weeks after the last treatment. p values less than 0.05 were considered statistically significant.
3. RESULTS
3.1. Patient demographics
Thirty (30) subjects were enrolled in the study, one subject did not meet inclusion/exclusion criteria and one subject experienced an adverse event not related to study treatment, therefore, 28 subjects completed treatments and 22 completed all follow‐ups (Figure 1). Of the 28 subjects, 15 were indicated to get treatment for wrinkles and 13 were indicated for acne scars. The mean age and standard deviation (SD) at study consent were 51.9 ± 13.5 years. Twenty‐six (26) subjects (92.9%) were female and 2 (7.1%) were male. Nine (9) subjects had Fitzpatrick skin type II (32.1%), 6 had type III (21.4%), 9 had type IV (32.1%), 3 had type V (10.7%), and 1 had type VI (3.6%) (Table 1).
FIGURE 1.
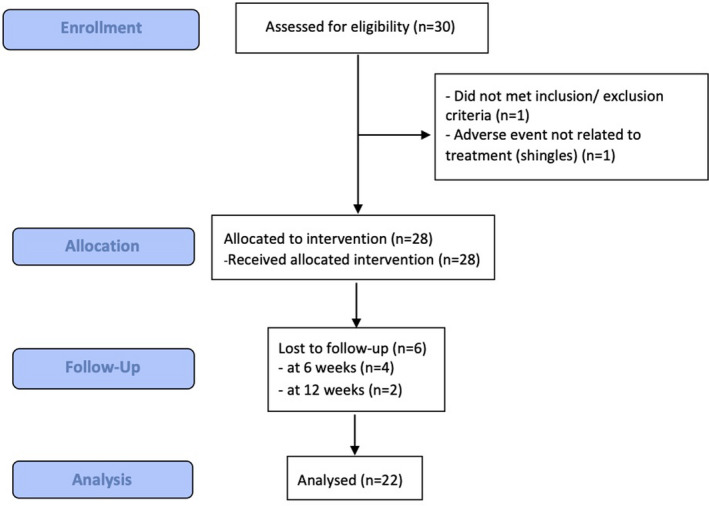
Study overview. A flow chart representing patient enrollment
TABLE 1.
Demographic data of participants
| Demographic data |
Results (N = 28) |
|---|---|
| Age, mean (SD) (years) | 51.9 (13.5) |
| Age, range (years) | 27–75 |
| Gender, n (%) | |
| Female | 26 (92.9) |
| Male | 2 (7.1) |
| Race | |
| Caucasian | 23 (82.1) |
| Asian | 3 (10.7) |
| Black or African Descent | 1 (3.6) |
| Asian/Caucasian | 1 (3.6) |
| Ethnicity | |
| Non‐Hispanic | 5 (17.9) |
| Hispanic | 23 (82.1) |
| Fitzpatrick skin type | |
| II | 9 (32.1) |
| III | 6 (21.4) |
| IV | 9 (32.1) |
| V | 3 (10.7) |
| VI | 1 (3.6) |
| Indication | |
| Acne scars | 13 (46.4) |
| Wrinkles | 15 (53.6) |
| Applicator type | |
| 80‐pin | 16 (57.1) |
| 160‐pin | 12 (42.9) |
3.2. Secondary outcomes: Subject satisfaction
Subjects were consistently satisfied with their treatment, with mean scores of 3 out of 4 (SE 0.2) at 6 weeks and 3 out of 4 (0.3) at 12 weeks after the last treatment. Over 70% of subjects reported post‐treatment improvement of either a mild (35%), moderate (20%), or significant (15%) nature to their treatment areas at 6 weeks. That improved to 77% at 12 weeks, with mild (31.8%), moderate (18.2%), or significant (27.3%) improvement. By week 12, 100% of subjects reported they would recommend this treatment to a friend.
The greatest number of subjects started noticing changes in their skin following their second treatment (38%), followed by a group that began noticing changes following their first treatment (24%), at follow‐up visits (24%), and at the end of treatments (14%) (Figure 2). The most reported subjects specific anatomical improvement for wrinkle indications was an improvement in the forehead area (frown lines) around the eyes (crow's feet), and around the mouth (marionette lines) (Figure 3). Furthermore, in subjects with acne indications, resolved cystic acne, additionally with a healthier skin texture, and less dry feeling and looking skin were reported by subjects at 6‐week and 12‐week follow‐up. Acne scar reduction did not significantly change between 6‐week follow‐up and 12‐week follow‐up (Figure 4).
FIGURE 2.
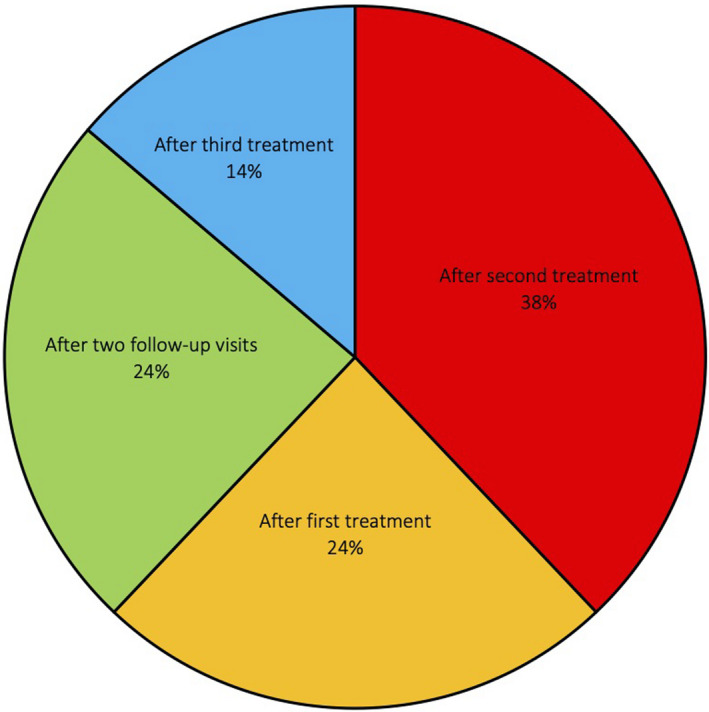
Treatment evaluation questionnaire, question: “When did the subject notice changes in their skin?”
FIGURE 3.
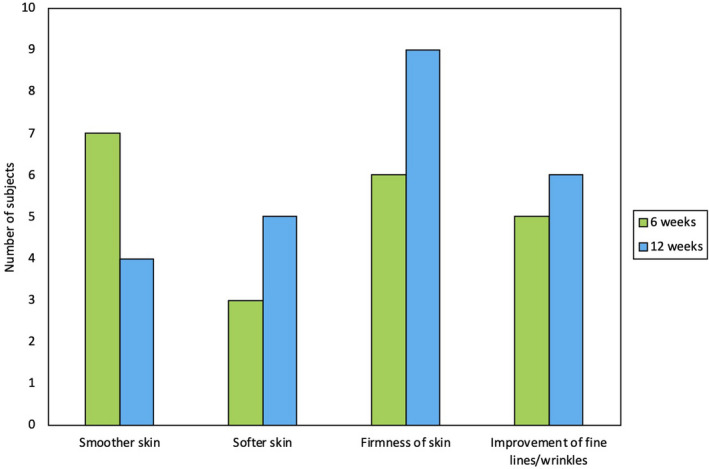
Treatment evaluation questionnaire for wrinkles, question: “What specific changes did the subject see in their skin,” between two follow‐up visits, at 6 weeks and 12 weeks
FIGURE 4.
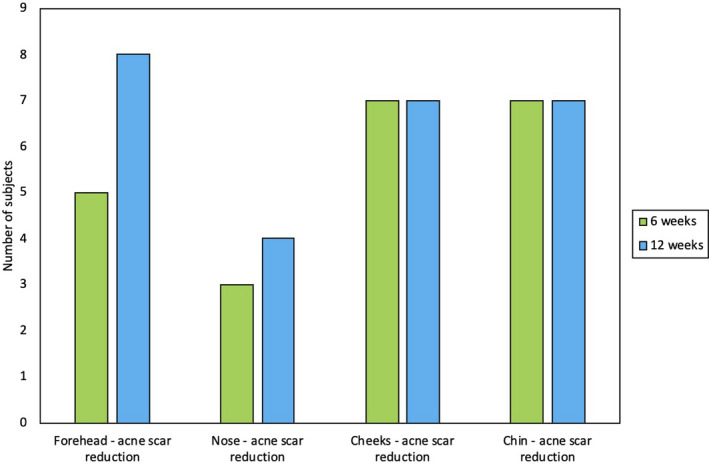
Treatment evaluation questionnaire for acne scars, question: “What specific changes did the subject see in their skin,” between two follow‐up visits, at 6 weeks and 12 weeks
3.3. Safety outcomes: Pain, tolerability, and adverse events
The treatments were well tolerated at all treatment sessions, subjects with acne scars reported a VAS pain score of 3.2 (SE 0.4) out of 10 which correlates to “mild pain” and subjects with wrinkles reported a pain score of 3.2 (SE 0.3) out of 10 which also correlates to “mild pain.” VAS scores for both the 80‐pin (up to 124 mJ/pin) and 160‐pin (u to 62 mJ/pin) were also considered “mild pain” (80‐pin mean VAS was 3.2 and 160‐pin mean VAS was 3.3). The average tolerability between all three treatments was consistently rated as “tolerable” to “very tolerable,” subjects treated for acne scars averaged scored their tolerability 3.5 out of 4.0, while subjects treated for wrinkles scored treatment tolerability an average of 3.6 out of 4.0. There were no reports of adverse events or unanticipated side effects during the duration of the study (Table 2, Figure 2).
TABLE 2.
Average satisfaction with treatment results at follow‐up using the Subject Satisfaction Scale (SSS)
| Time point | 6 weeks | 12 weeks | SSS rating | p‐value |
|---|---|---|---|---|
| Mean (SE) | 3.0 (0.2) | 3.0 (0.3) | 3 = Satisfied | p = 0.70 |
SSS: (4) very satisfied, (3) satisfied, (2) no opinion, (1) unsatisfied, and (0) very unsatisfied.
Abbreviation: SE, standard error.
4. DISCUSSION
This was a prospective, evaluator‐blinded study of nanofractional radiofrequency for the treatment and reduction of wrinkles and acne scarring for 28 subjects. Subjects were consistently satisfied with their treatment at both follow‐up visits. Moreover, none of the subjects experienced any adverse events and pain was consistently rated low between all treatment visits and at follow‐up visits (Table 3).
TABLE 3.
Average pain assessed using the Visual Analog Score (VAS)
| Indication | Mean (SE) | VAS rating |
|---|---|---|
| Wrinkles | 3.2 (0.4) | Mild pain |
| Acne scars | 3.2 (0.3) | Mild pain |
No pain: 0–0.4 cm, Mild pain: 0.5–4.4 cm, Moderate pain: 4.5–7.5 cm, and Severe pain: 7.6–10 cm.
Abbreviation: SE, standard error.
Fractional radiofrequency devices remain a dominant technology in the non‐invasive management of skin aging, as it is a safe and effective treatment for a broad range of skin conditions. 20 The technology also carries a significant number of advantages that may be associated with patients' satisfaction, when compared to more invasive technologies. The mechanism of action created with nanofractional radiofrequency is a non‐homogeneous thermal wound on the skin that is delivered directly to the reticular dermis, while deeper areas of the skin are left intact. This results in faster wound healing all while causing less pain to the patient than more invasive procedures. 21 Furthermore, histological findings revealed that procollagen I, III, and elastin levels improved after treatment. 3 The technology is also inclusive to all skin types; it has shown positive clinical results on wrinkles, skin texture, and pores without post‐inflammatory hyperpigmentation in Asian population samples. 15 , 22 , 23 , 24 The study included here included subjects with darker skin tones and results in those subjects were not significantly different from those with lighter skin tones. Both groups of subjects were consistently satisfied with their treatments.
Satisfaction‐related outcome measures are critical components of all medical procedures. A patient‐centered measure of satisfaction is especially important for aesthetic procedures because patients usually have several options when it comes to selecting a procedure or a physician. Physicians can demonstrate the value of its services in the current era of quality assurance and continuous improvement by developing better scientific metrics to evaluate patients' perceptions of these new technologies and their interactions with this specialty.
Fractional radiofrequency has been shown to improve skin texture 25 and successfully treated acne and acne scars. 23 , 24 , 26 , 27 It can induce wrinkle reduction, laxity, and skin contouring improvement. 28 Our results in this clinical trial, along with previous efficacy results backed by appropriate safety profile, support these findings. 2 , 7 , 13 , 14 , 15 , 16 , 17 Additionally, nanofractional radiofrequency has been shown to improve skin roughness in over 70% of patients, 29 which is similar to the results shown in this study, where a noticeable change in skin smoothness was one of the most commonly reported outcomes post‐treatment. A main advantage of nanofractional radiofrequency is that it involves no risk, is not time consuming and downtime is short. The treatment's safety profile is outstanding, with minimal discomfort and side effects. Our satisfaction results show that skin firmness was the most common textural change subjects reported (most noticeable at 12 weeks). At 12 weeks, all subjects would recommend this treatment to a friend. The reported pain was rated as mild although no anesthetic or pain treatment was used before and during treatment. Comfortable treatments with no pain are an advantage for both the treating physician and the patient both. Subjects recorded high levels of satisfaction with the procedure, which lasted for at least 12 weeks after treatment.
This study was not without limitations. It was performed at a single center with a relatively small number of subjects and with a dermatologist who is familiar with energy‐based devices. Furthermore, there was no control group in this analysis. Unfortunately, this is often the case in studies involving radiofrequency devices in which no specific gold standard has been established. 30 It would be worthwhile to investigate the feasibility of using a placebo group or a split‐face study, as a control group, which would be very close to the actual procedure but without delivering the energy (no heat generated by RF).
Subjective criteria must be met in the context of cosmetic procedures where subjects pursue treatments among other things due to perceived dissatisfaction. However, by studying subject satisfaction through qualitative means, we gain a unique understanding that can ultimately enhance healthcare practices. Therefore, it is important to integrate qualitative data into future research models.
5. CONCLUSIONS
In conclusion, our results suggest that patients are consistently satisfied with nanofractional radiofrequency treatments. The satisfaction is likely derived from that nanofractional radiofrequency treatments showed prolonged improvements in overall skin quality and pigmentation criteria. The nanofractional radiofrequency device may be a viable alternative for fractional laser devices, for the treatment of rhytids for patients looking for shorter recovery times and looking to avoid the drawbacks of fractional laser treatments.
ETHICS STATEMENT
All subjects gave their informed consent for inclusion before they participated in the study. The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by local IRB.
CONFLICT OF INTEREST
SA, AS, and KM have nothing to disclose. NS is principal investigator of Venus Concept Inc and owns stock in the company.
AUTHOR CONTRIBUTIONS
SA, AS, KM, and NS contributed to the analysis and review of the manuscript for scientific accuracy.
Arruda S, Swearingen A, Medrano K, Sadick N. Subject satisfaction following treatment with nanofractional radiofrequency for the treatment and reduction of acne scarring and rhytids: A prospective study. J Cosmet Dermatol. 2021;20:3475–3481. 10.1111/jocd.14455
Funding information
This study was sponsored by Venus Concept, Inc. Funding for open access charge: Venus Concept Inc.
DATA AVAILABILITY STATEMENT
Qualified researchers may request access to the data that support the findings of this study from Venus Concept Inc. by contacting rmays@venusconcept.com.
REFERENCES
- 1. 2018 Plastic Surgery Statistics Report. Plastic Surgery. Published online 2018:25.
- 2. Bohnert K, Dorizas A, Sadick N. Prospective, pilot evaluation of the performance of nanofractional radiofrequency for improvement of skin texture via skin resurfacing. J Cosmet Dermatol. 2018;17(1):61‐65. 10.1111/jocd.12398 [DOI] [PubMed] [Google Scholar]
- 3. Shin JM, Kim JE. Radiofrequency in clinical dermatology. Med Lasers. 2013;2(2):49‐57. 10.25289/ML.2013.2.2.49 [DOI] [Google Scholar]
- 4. Ali ST, Feldman SR. Patient satisfaction in dermatology: a qualitative assessment. Dermatol Online J. 2014;20(2). https://doi.org/https://escholarship.org/uc/item/5tc6b5f3 [PubMed] [Google Scholar]
- 5. Gibbons C, Singh S, Gibbons B, et al. Using qualitative methods to understand factors contributing to patient satisfaction among dermatology patients: a systematic review. J Dermatol Treat. 2018;29(3):290‐294. 10.1080/09546634.2017.1364688 [DOI] [PubMed] [Google Scholar]
- 6. Poulos GA, Brodell RT, Mostow EN. Improving quality and patient satisfaction in dermatology office practice. Arch Dermatol. 2008;144(2):263‐265. 10.1001/archdermatol.2007.58 [DOI] [PubMed] [Google Scholar]
- 7. Ray M, Gold M. A Retrospective study of patient satisfaction following a trial of nano‐fractional RF treatment. J Drugs Dermatol. 2015;14(11):1268‐1271. [PubMed] [Google Scholar]
- 8. Salins CAD, Brenaut E, Misery L, Roguedas‐Contios AM. Factors influencing patient satisfaction: assessment in outpatients in dermatology department. J Eur Acad Dermatol Venereol. 2016;30(10):1823‐1828. 10.1111/jdv.13652 [DOI] [PubMed] [Google Scholar]
- 9. Wang Y‐C, Ganzorig B, Wu C‐C, et al. Patient satisfaction with dermatology teleconsultation by using MedX. Comput Methods Programs Biomed. 2018;167:37‐42. 10.1016/j.cmpb.2018.10.015 [DOI] [PubMed] [Google Scholar]
- 10. Prakash B. Patient satisfaction. J Cutan Aesthet Surg. 2010;3(3):151‐155. 10.4103/0974-2077.74491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kirsner RS, Federman DG. Patient satisfaction. Quality of care from the patients' perspective. Arch Dermatol. 1997;133(11):1427‐1431. 10.1001/archderm.133.11.1427 [DOI] [PubMed] [Google Scholar]
- 12. Kaplan SH, Greenfield S, Ware JE. Assessing the effects of physician‐patient interactions on the outcomes of chronic disease. Med Care. 1989;27(3 Suppl):S110‐127. 10.1097/00005650-198903001-00010 [DOI] [PubMed] [Google Scholar]
- 13. Eubanks S, Solomon J. In press. Published online 2021.
- 14. Kilmer S, Kang A. In press. Published online 2021.
- 15. Nitayavardhana S, Wanitphakdeedecha R, Ng JNC, Eimpunth S, Manuskiatti W. The efficacy and safety of fractional radiofrequency nanoneedle system in the treatment of atrophic acne scars in Asians. J Cosmet Dermatol. 2020;19(7):1636‐1641. 10.1111/jocd.13484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Artzi O, Cohen S, Verner I, et al. Radio peel‐synergism between nano‐fractional radiofrequency and 20% trichloroacetic acid chemical peeling. Dermatol Surg. 2019;45(5):711‐717. 10.1097/DSS.0000000000001918 [DOI] [PubMed] [Google Scholar]
- 17. Goel A, Gatne V. Use of nanofractional radiofrequency for the treatment of acne scars in Indian skin. J Cosmet Dermatol. 2017;16(2):186‐192. 10.1111/jocd.12311 [DOI] [PubMed] [Google Scholar]
- 18. Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short‐Form McGill Pain Questionnaire (SF‐MPQ), Chronic Pain Grade Scale (CPGS), Short Form‐36 Bodily Pain Scale (SF‐36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken). 2011;63(Suppl 11):S240‐S252. 10.1002/acr.20543 [DOI] [PubMed] [Google Scholar]
- 19. Aun C, Lam YM, Collett B. Evaluation of the use of visual analogue scale in Chinese patients. Pain. 1986;25(2):215‐221. 10.1016/0304-3959(86)90095-3 [DOI] [PubMed] [Google Scholar]
- 20. Weiss RA, Weiss MA, Munavalli G, Beasley KL. Monopolar radiofrequency facial tightening: a retrospective analysis of efficacy and safety in over 600 treatments. J Drugs Dermatol. 2006;5(8):707‐712. [PubMed] [Google Scholar]
- 21. Hruza G, Taub AF, Collier SL, Mulholland SR. Skin rejuvenation and wrinkle reduction using a fractional radiofrequency system. J Drugs Dermatol. 2009;8(3):259‐265. [PubMed] [Google Scholar]
- 22. Vejjabhinanta V, Wanitphakdeedecha R, Limtanyakul P, Manuskiatti W. The efficacy in treatment of facial atrophic acne scars in Asians with a fractional radiofrequency microneedle system. J Eur Acad Dermatol Venereol. 2014;28(9):1219‐1225. 10.1111/jdv.12267 [DOI] [PubMed] [Google Scholar]
- 23. Lee HS, Lee DH, Won CH, et al. Fractional rejuvenation using a novel bipolar radiofrequency system in Asian skin. Dermatol Surg. 2011;37(11):1611‐1619. 10.1111/j.1524-4725.2011.02134.x [DOI] [PubMed] [Google Scholar]
- 24. Yeung CK, Chan NPY, Shek SYN, Chan HHL. Evaluation of combined fractional radiofrequency and fractional laser treatment for acne scars in Asians. Lasers Surg Med. 2012;44(8):622‐630. 10.1002/lsm.22063 [DOI] [PubMed] [Google Scholar]
- 25. Kaminaka C, Uede M, Matsunaka H, Furukawa F, Yamamoto Y. Clinical studies of the treatment of facial atrophic acne scars and acne with a bipolar fractional radiofrequency system. J Dermatol. 2015;42(6):580‐587. 10.1111/1346-8138.12864 [DOI] [PubMed] [Google Scholar]
- 26. Peterson JD, Palm MD, Kiripolsky MG, Guiha IC, Goldman MP. Evaluation of the effect of fractional laser with radiofrequency and fractionated radiofrequency on the improvement of acne scars. Dermatol Surg. 2011;37(9):1260‐1267. 10.1111/j.1524-4725.2011.02110.x [DOI] [PubMed] [Google Scholar]
- 27. Bloom BS, Emer J, Goldberg DJ. Assessment of safety and efficacy of a bipolar fractionated radiofrequency device in the treatment of photodamaged skin. J Cosmet Laser Ther. 2012;14(5):208‐211. 10.3109/14764172.2012.724534 [DOI] [PubMed] [Google Scholar]
- 28. Sadick NS, Nassar AH, Dorizas AS, Alexiades‐Armenakas M. Bipolar and Multipolar Radiofrequency. Dermatol Surg. 2014;40:S174. 10.1097/DSS.0000000000000201 [DOI] [PubMed] [Google Scholar]
- 29. Cho SI, Chung BY, Choi MG, et al. Evaluation of the clinical efficacy of fractional radiofrequency microneedle treatment in acne scars and large facial pores. Dermatol Surg. 2012;38(7 Pt 1):1017‐1024. 10.1111/j.1524-4725.2012.02402.x [DOI] [PubMed] [Google Scholar]
- 30. de Araújo AR, Soares VPC, da Silva FS, da Moreira TS. Radiofrequency for the treatment of skin laxity: mith or truth. An Bras Dermatol. 2015;90(5):707‐721. 10.1590/abd1806-4841.20153605 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Qualified researchers may request access to the data that support the findings of this study from Venus Concept Inc. by contacting rmays@venusconcept.com.


