Abstract
Polarized light imaging (PLI) is a new method which quantifies and visualizes nerve fiber direction. In this study, the educational value of PLI sections of the human brainstem were compared to histological sections stained with Luxol fast blue (LFB) using e‐learning modules. Mental Rotations Test (MRT) was used to assess the spatial ability. Pre‐intervention, post‐intervention, and long‐term (1 week) anatomical tests were provided to assess the baseline knowledge and retention. One‐on‐one electronic interviews after the last test were carried out to understand the students’ perceptions of the intervention. Thirty‐eight medical students, (19 female and 19 males, mean age 21.5 ± SD 2.4; median age: 21.0 years) participated with a mean MRT score of 13.2 ± 5.2 points and a mean pre‐intervention knowledge test score of 49.9 ± 11.8%. A significant improvement in both, post‐intervention and long‐term test scores occurred after learning with either PLI or LFB e‐learning module on brainstem anatomy (both P < 0.001). No difference was observed between groups in post‐intervention test scores and long‐term test scores (P = 0.913 and P = 0.403, respectively). A higher MRT‐score was significantly correlated with a higher post‐intervention test score (rk = 0.321; P < 0.05, respectively), but there was not a significant association between the MRT‐ and the long‐term scores (rk = −0.078; P = 0.509). Interviews (n = 10) revealed three major topics: Learning (brainstem) anatomy by use of e‐learning modules; The “need” of technological background information when studying brainstem sections; and Mnemonics when studying brainstem anatomy. Future studies should assess the cognitive burden of cross‐sectional learning methods with PLI and/or LFB sections and their effects on knowledge retention.
Keywords: gross anatomy education, histology education, neuroanatomy education, brainstem, Luxol fast blue, polarized light imaging, spatial ability, white matter
INTRODUCTION
Human neuroanatomy is crucial to the clinical diagnosis which makes understanding neuroanatomy of high importance to future clinicians (Frank and Danoff, 2007). Learning neuroanatomy is perceived to be challenging, requiring thorough basic science knowledge, understanding both gross anatomical and histological specimens with elicit help from atlases and properly designed learning applications (Fitzgerald et al., 2008). A recent review showed that several novel educational strategies are being applied in neuroanatomy including three‐dimensional (3D) teaching tools, applied neuroanatomy elective courses, equivalence‐based instruction‐rote learnings, mobile augmented reality applications, inquiry‐based clinical cases, cadaveric dissection, and social media were all used in the education of neuroanatomy to students (Sotgiu et al., 2020). More traditionally, neuroanatomy education has been carried out using cross‐sections of donor brains (Provo et al., 2002; Albanese, 2010). Cross‐sectional anatomy has the closest relationship with clinical radiology, both of which display anatomical information in two dimensions (Zimmermann et al., 2010). Like neuroanatomy, histology of the nervous system is regarded by students to be a difficult subject area (Garcia et al., 2019). The intricacy of the nervous system is complicated further by the various histological methods can be used to visualize different tissue properties (Pawlina and Ross, 2018). For example, in white matter visualization, various histological methods exist including myelin staining by Luxol fast blue (LFB) dye (Viktorov, 1978). Luxol fast blue is a copper phthalocyanine dye which is soluble in alcohol and attracted to the bases found in myelin sheath lipoproteins (Bruce‐Gregorios, 2006). In clinical practice, LFB is used to detect demyelination (Bruce‐Gregorios, 2006), although stained sections can be used as a teaching resource as well (Rubin et al., 2009; Roth et al., 2015). An alternative visualization method called polarized light imaging (PLI) uses polarized light on unstained sections and can quantify the orientation of nerve fibers. Polarized light imaging visualization is based on the birefringent capacity of the myelin sheath surrounding the axons (Axer et al., 2011a, 2011b). The advantage of PLI microscopy lies in providing detailed information concerning nerve fiber orientation and has only been used in research settings (Axer et al., 2007, 2011a, b; Mollink et al., 2017; Wiesmann et al., 2019; Henssen et al., 2019a, b). The use of PLI and the detailed information it provides has not been investigated in the educational setting.
An important component of anatomy education is spatial ability, which describes the inherent ability of the learner to orient and mentally manipulate an object in 2D and 3D manner (McGee, 1979; Linn and Petersen, 1985; Roach et al., 2021). Previous research showed that spatial ability was correlated with general anatomy knowledge assessments using practical examination, spatial multiple‐choice questions examination, and 3D synthesis of two‐dimensional views (Rochford, 1985). Later studies have reaffirmed the correlation between 3D synthesis and 2D sectional anatomy (Garg et al., 1999a, b; Hegarty and Kozhevnikov, 1999; Garg et al., 2002; Luursema et al., 2006, 2008; Hegarty et al., 2009; Nguyen et al., 2014). To assess spatial ability in students, most studies have used the well validated Mental Rotations Test (MRT) (Shepard and Metzler, 1971; Vandenberg and Kuse, 1978) and redrawn by Peters and colleagues (Peters et al., 1995). A recent meta‐analysis described a significant relationship between spatial ability and anatomy knowledge assessment using practical examination, 3D synthesis from two‐dimensional views, drawing of views, and cross‐sections. Relationships between spatial ability test and anatomy knowledge assessment using spatial multiple‐choice questions, however, have yet to be described (Langlois et al., 2017). A significant advantage in spatial ability for men was also observed in studies (Maccoby and Jacklin, 1974; Peters et al., 2007), as well as on a meta‐level (Voyer et al., 1995; Roach et al., 2021). Given the role of spatial and non‐spatial reasoning in learning anatomy, educators are encouraged to consider curriculum delivery modifications and a comprehensive assessment strategy to prevent disadvantaging individuals with low spatial ability. Due to the strong link between anatomy and spatial ability, improvements to anatomy curricula will not only help students to study anatomy more effectively but will also likely improve student spatial abilities (Hoyek et al., 2009; Vorstenbosch et al., 2013; Langlois et al., 2013, 2020).
A shift to the virtual teaching modalities has taken place due to the global devastation cause by the Coronavirus disease 2019 (Covid‐19) pandemic (Evans et al., 2020; Ravi, 2020). Even before the Covid‐19 pandemic, e‐learning modules had become increasingly popular in teaching health professional education, including anatomy education (Lewis et al., 2014). E‐learning is, by definition, a teaching method supported by digital technologies, including new multimedia technologies and the internet, which aims to improve the quality of learning by facilitating access to resources and services, as well as remote exchange and collaboration (Alonso et al., 2005). Therefore, the use of e‐learning modules could be of great value in the Covid‐19 pandemic. Despite these advantages educators must consider the spatial insights of the learners (Luursema et al., 2006, 2008). This study, therefore, set out to investigate the effect of e‐learning in anatomy education by use of different types of cross‐sections and aimed to correlate the learning effects with students’ spatial insights. For this, a complicated anatomical structure which is not regularly taught in the medical curriculum was chosen: the brainstem. The brainstem connects the cerebrum, cerebellum, and the spinal cord and furthermore contains nuclei for white matter tracts and source nuclei that impact the central nervous system functions. The brainstem contains afferent and efferent fibers that are part of projection tracts (i.e., the corticospinal tract). In contrast to white matter in the cerebrum, the brainstem does not contain commissural or association white matter tracts. The gray matter of the brainstem (neuronal cell bodies) can be found in clumps and clusters throughout its entire length to form the nuclei of the cranial nerves, the reticular formation, the pontine nuclei, and the medullary nuclei. The brainstem can be subdivided along its rostro‐caudal axis into the derivatives of the three primary embryological vesicles: (1) the midbrain, (2) the pons, and (3) the medulla oblongata (Nieuwenhuys et al., 2008; Angeles Fernández‐Gil et al., 2010; Mai and Paxinos, 2011; Mai et al., 2015; Sclocco et al., 2018). Sections of all three parts of the brainstem were used in this study.
The primary objective of this study was to evaluate the effect of spatial ability on cross‐sectional e‐learning brainstem anatomy. The secondary objective of this study examined the learning outcomes of students working with PLI images and learning outcomes of students working with LFB images. The hypothesis of this study was that students who have greater spatial ability as assessed by use of the MRT would perform better when learning 3D anatomy by use of photographs of cross‐sections in an e‐learning environment. In addition, it was thought that students who used PLI slices would outperform students who used LFB slices. It was assumed that PLI‐slices would increase students’ ability to construct a 3D overview of brainstem anatomy due to the fact that PLI provides fiber orientation information.
MATERIALS AND METHODS
Ethical Approval
Two histological datasets were retrieved from the anatomical collection of the department Medical Imaging, Anatomy division of the University Medical Center in Nijmegen, the Netherlands. All body donors signed a written informed consent permitting the use of their body and organs for scientific research and educational purposes. All protocols concerning the acquisition of data and tissue processing were approved by the CMO (Commissie Mensgebonden Onderzoek) region Arnhem‐Nijmegen, the Netherlands and are legislated under Dutch national law (BWBR0005009).
After consultation of the university ethical review board, ethical approval was ruled as exempt because students participated voluntarily, data were handled in anonymized fashion and the results had no impact on their individual progression, anatomy grading, or any other study‐related outcome. The study was conducted in accordance with Helsinki Declaration as revised in 2013 (WMA, 2013) and was carried out in compliance with the Ethical Conduct of Clinical Studies. Written informed consent was obtained from the participants of the study.
Summarized Methodology of the Acquisition of the Used Datasets
Two human brainstem specimens used in this study were obtained from the individuals without history of neurological diseases. The PLI dataset was obtained from a serially sectioned brainstem, which was sliced using a HM 450 Sliding Microtome (Thermo Fisher Scientific Inc., Waltham, MA) at a thickness of 100 micrometers (µm). Detailed methods for PLI specimen processing have been described elsewhere (Mollink et al., 2019; Henssen et al., 2019a). The LFB dataset was obtained from brainstem serial sections using an LKB Bromma 2260 macrotome (LKB Instruments, Bromma, Sweden). The tissue was serially sectioned at 4 micrometers (µm) thickness and every 15th slice was kept for staining, resulting in an interplane resolution of 60 µm. Macrophotographs of all the sections (referred to hereafter as the histological slices) were taken with a Canon EOS 550D 18 MP CMOS APS‐C digital SLR camera (Canon Inc., Ōta, Tokyo, Japan) with a Canon 100 mm autofocus lens to digitize the data.
Study Design
Medicine students were eligible for inclusion after they studied gross neuroanatomy in the second bachelor’s year. In the Netherlands, during the bachelor’s program, students are taught basic sciences, including anatomy, during the first 3 years of their medical curriculum. During this preclinical program, all medical students receive 15 hours of gross neuroanatomy education; 10 hours of individual assignments, 2 hours of lectures, and 3 hours working with prosected specimens in the dissection rooms (Radboud Health Academy, 2019). Throughout the course a combination of case‐based learning and problem‐based learning methods are used. Students focus on the anatomy of the ventricular system, the basal ganglia, the limbic system, and the cerebellum. The function of the cranial nerves is also emphasized. Some students seek more in‐depth knowledge of neuroanatomy and sign up for an elective course on white matter anatomy (awarded two European Credit Transfer System points). Within this course, lectures (4 hours), self‐assignments (8 hours) and e‐learning modules on cerebral white matter anatomy (8 hours) are alternated with group assignments (10 hours) and hands‐on white matter dissection (15 hours). The final examination consists of a group report on the importance of understanding white matter anatomy in neurological deficits (e.g., multiple sclerosis) (14 hours) and an anatomical test (2 hours). Intrinsic brainstem anatomy, however, is not part of these curricular activities. Exclusion criteria for study participation included previous knowledge on brainstem anatomy, PLI microscopy, or LFB staining methods (e.g., acquired during research internships), students being unwilling to adhere to the study protocol and/or incomplete comprehension of the Dutch language. Students voluntarily signed up for this experiment and were, after inclusion, computer‐randomized over two groups using block randomization.
For this experiment, four e‐learning modules were constructed using the Lectora Online software (Courseware Company, Utrecht, the Netherlands). E‐learning modules were converted to Sharable Content Object Reference Model (SCORM) packages which were uploaded in the Brightspace a cloud‐based learning management system, released April 2020, (D2L Corporation, Kitchener, ON, Canada). In this learning management system, students were given access to different e‐learning modules in a defined chronological order. An overview of the study design is provided in Figure 1 and is discussed below. E‐learning modules were designed following the recommendations made by Van Nuland and Rogers (2016) with multimedia principles and e‐learning principles in mind.
Figure 1.
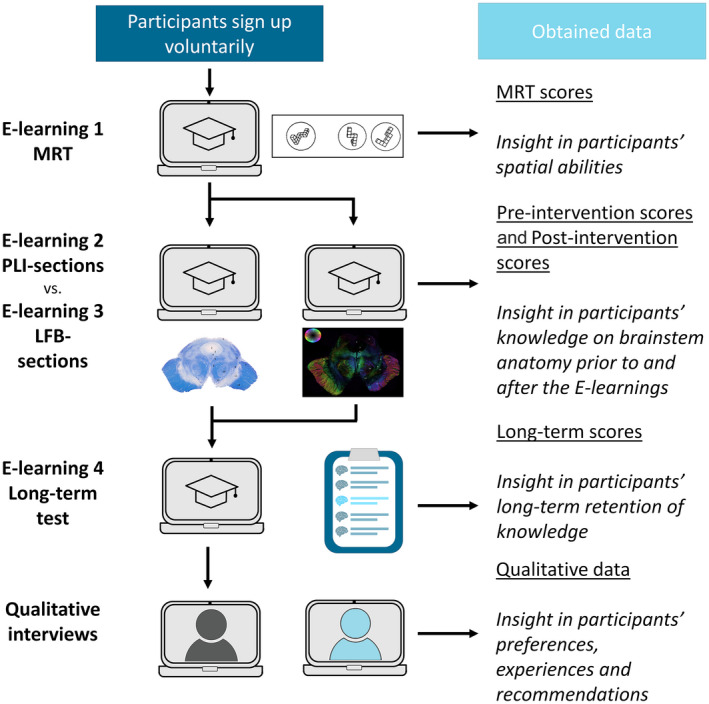
Study design. LFB, Luxol fast blue; MRT, Mental Rotations Test; and PLI, polarized light imaging.
The first e‐learning module contained a digitized version of the redrawn validated MRT (Vandenberg and Kuse, 1978; Peters, et al., 1995). This module adhered to the instructions of the MRT as proposed by Peters et al. (1995): (1) the written instructions were identical to those suggested in the cover text, (2) students had sufficient time to practice with examples of MRT‐questions, and (3) the three‐minute deadline to go through each section of the MRT was clearly announced prior to taking the test. In addition, an automatic timer was incorporated within the module which ensured that students were redirected to the “short break slide” after three minutes had passed. There was no possibility to students to go back and adapt answers after three minutes had passed or after they finished the last question by clicking the next slide button (Figure 2). Anonymized MRT results were sent to the principal investigator of this study (D.H.) after finishing the MRT e‐learning module. Students were awarded with a point when both of the stimulus figures that match the target figure were identified correctly. No credit was given for a single correct answer.
Figure 2.
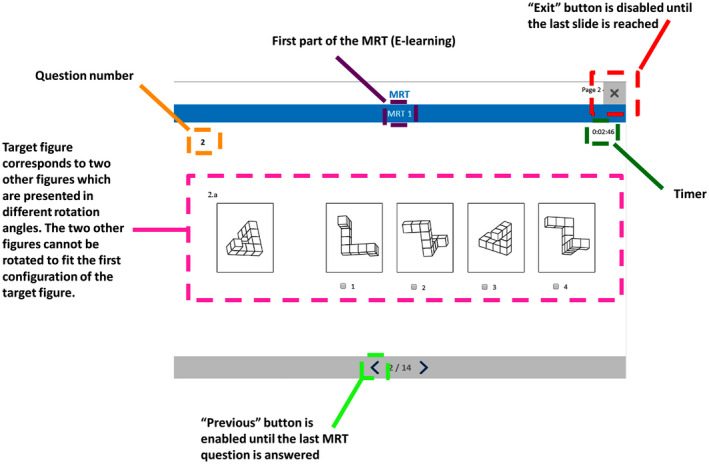
Example of a screenshot from the Mental Rotations Test e‐learning module with explanation of the elements and buttons. Screen capture is taken from the MRT e‐learning module. The title of the e‐learning module and paragraph in which the student is working is displayed in the center of the slide (highlighted in purple). On the left side, the student sees which question number he/she is working on (highlighted in orange). The slide shows a target figure on the left, and four stimulus figures on the right. In all problems sets there are two figures on the right which are rotated versions of the target figure, and two figures which cannot be made to match the target figure. The student has to determine which of the two figures are correct rotations of the target figure. The answer needs to be given by checking the boxes directly underneath the stimulus figures (highlighted in a pink). A single correct answer or a correct and an incorrect answer were not credited. The student can navigate using the arrow‐buttons in the bottom of the slide (highlighted in green; the backward button was disabled in various slides when this was regarded unfavorable). The timer on the right side of the figures shows the students the remaining amount of time to finish that specific part of the e‐learning module (highlighted in emerald). After finishing the e‐learning module, the exit button in the upper right corner was enabled to be used by students (highlighted in red). MRT, Mental Rotations Test.
The second e‐learning module comprised six chapters: (1) a pre‐intervention test on brainstem anatomy, (2) an introduction with to PLI microscopy and the tissue characteristics it is based upon, (3) a section discussing the anatomy of the midbrain using PLI images, (4) a section discussing the anatomy of the pons using PLI images, (5) a section discussing the anatomy of the medulla oblongata using PLI images, and (6) a post‐intervention test on brainstem anatomy.
The third e‐learning module was identical to the second except that all references to PLI were replaced by references to LFB. The chapter introducing PLI microscopy was replaced by a chapter introducing LFB staining with approximately similar information load. Figures from PLI microscopy were replaced by corresponding LFB slices (Figure 3). Finally, wherever the word “PLI” or “polarized light imaging” was printed, it was replaced by “LFB” or “Luxol fast blue.” The third module was identical in length to the second module; both e‐learning modules comprised 41 slides.
Figure 3.
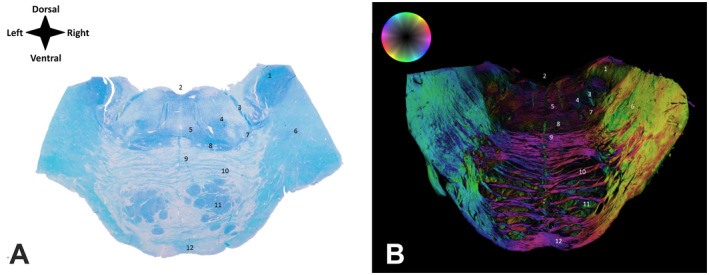
Cross‐sections of the pons at the level of the facial loop. A, Section of the pons stained in Luxol fast blue. Anatomical orientation is depicted in the upper right corner the panel; B, Unstained section of the pons visualized in the polarized light (polarized light imaging). Color‐coded fiber‐orientation‐map wheel in the panel B provides information on the orientation of fibers in the section. Numerical labels correspond to the same structures on both panels: 1 = Inferior cerebellar peduncle; 2 = Cerebral aquaduct/Fourth ventricle; 3 = Facial tract; 4 = Abducens tract; 5 = Medial longitudinal fasciculus; 6 = Middle cerebellar peduncle; 7 = Lateral lemniscus; 8 = Medial lemniscus; 9 = Dorsal pontine decussation; 10 = Pontocerebellar fibers; 11 = Pontine nuclei with corticonuclear tract, corticobulbar tract and corticospinal tract; and 12 = Ventral pontine decussation.
The fourth e‐learning module comprised a final follow‐up test with identical questions as the pre‐intervention and post‐intervention tests. In this module, the questions were provided in a randomized order. Anonymized test results of the fourth module were sent to the principal investigator of this study (D.H.) after finishing the e‐learning module. No correction for guessing was carried out.
Testing Procedure and Questions
The tests used in either one of the e‐learning modules contained solely questions testing anatomical knowledge. No questions on the technical background of the methods of LFB or PLI were present. No images were presented in the test slides. Students could not navigate to other chapters when filling in the different tests. The pre‐intervention and post‐intervention tests were identical and comprised 20 two‐choice questions. Sixteen of these questions referred to relationships of different structures in the same level of the brainstem (8:4:4 ratio regarding questions on midbrain, pontine, and medullary anatomy, respectively). Four questions tested the craniocaudal orientation of structures. Anonymized results of the pre‐intervention test and post‐intervention test were sent to the principal investigator of this study (D.H.) after finishing the e‐learning module. Examples of questions are provided in the Supporting Information File.
Questions tested the knowledge of relationships between structures in the same slice and relationships on the craniocaudal axis. The questions were designed based on previous empirical experience and scientific articles produced by this research team (Kooloos et al., 2014; Henssen et al., 2020). Based on Bloom’s taxonomy, the tests assessed learning information belonging to the application dimension. Learners were tested whether or not they were capable of implementing abstractions that were both similar and different from the learning situation (Bloom, 1956). All questions were first‐order multiple‐choice questions and had two‐answer options. None of the questions were accompanied by figures or pictures.
The first e‐learning module was combined with the second or third module. Students were provided with four hours to complete both e‐learning modules at home as this experiment was conducted during Covid‐19 pandemic. The fourth e‐learning module was made available exactly one week after completion of the first and second or first and third e‐learning modules. This module was also completed at home. Every slide in the chapters designed for anatomy learning provided a section of the human brainstem using PLI or LFB. Encompassing text was provided to guide students when studying these images and to help them appreciate the anatomical structures visible. Examples of the slides from e‐learning modules are depicted in Figure 4.
Figure 4.
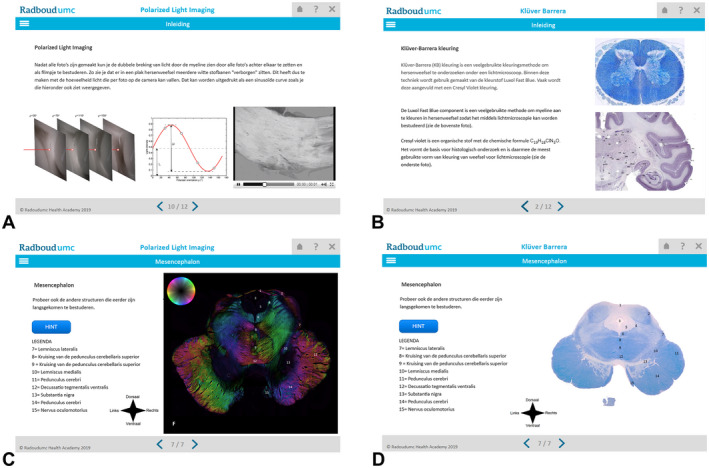
Examples of captured screens from the different e‐learning modules. Panels A and C show images from the e‐learning module utilizing polarized light imaging; Panels B and D show images from the e‐learning module utilized Luxol fast blue‐stained sections.
Qualitative Interviews and Assessment
After finishing the e‐learning experience, ten students were willing to participate in a short, semi‐structured qualitative interview. Electronic, face‐to‐face interviews were conducted using Skype, version 8.65.0.78 (Skype Technologies, Luxembourg City, Luxembourg). All interviews were video‐recorded. Prior to the interviews, a separate informed consent was signed by the participants. The interviewer conducted the interviews as near as normal conversation using open‐ended questions. All interviews were conducted in a semi‐structures fashion by use of open‐ended questions to obtain insights on experiences of students when working with LFB‐slides, PLI‐slides, and e‐learning modules to study 3D brainstem anatomy. A topic list was constructed prior to the interviews by the two investigators. Elucidated topics were: (1) Views on digital learning during the Covid‐19 pandemic, (2) The value of the used microscopy technique to study brainstem anatomy, (3) The balance between providing technical background of the microscopy technique and brainstem anatomy, (4) Advantages and disadvantages of either microscopy technique, and (5) Learning strategies and examination strategies used by the students.
The interviews were semi‐structured and guided by the five open‐ended questions: (1) How did you experience the e‐learning modules as study resource during the Covid‐19 pandemic?, (2) How did you feel about the technique that you used in your study and what can you remember about the specifics of this technique?, (3) Where the technical slides presented in the right proportion with regard to the slides which discussed the anatomy of the brainstem?, (4) What advantages or disadvantages do you recognize for the technique you studied brainstem anatomy with?, and (5) How did you feel about the follow‐up test and which strategies did you use to answer the questions? An inductive iterative process was performed during the interviews using the constant comparative method, indicating that the interview could be steered in a different direction when a new topic arose. When unclear, additional questions were asked to ensure proper understanding of the interviewees meaning.
The recordings of each interview were transcribed verbatim and analyzed using direct content analysis. Starting after the first interview had taken place; transcriptions were coded line‐by‐line, through which a code list was created. Coding was continued after each interview.
Coding and analysis were carried out independently by one of the researchers (D.H.), who met periodically with the other researcher (A.v.C.v.W.) to discuss codes and themes until consensus was reached. The coding process was performed using Atlas.ti software, version 8.2.29.0 (ATLAS.ti Scientific Software Development GmbH, Berlin, Germany). The constructed codebook could be organized into categories and themes (see Supporting Information File). Discrepancies and interpretations were discussed by the researchers. The codes were grouped to enable the recognition of in order to recognize.
Statistical Analysis
The statistical package SPSS Statistics, version 25 (IBM Corp., Armonk, NY) was used for statistical analyses of the data of the questionnaire. The Cronbach’s alpha test was carried out to assess whether the used assessments were internally consistent (i.e., assessing reliability). Internal consistency and thus reliability, is generally regarded acceptable when ≥ 0.7. Kendall’s tau B was used to assess the association between the MRT results and (1) the post‐intervention test scores and (2) the long‐term test scores. The Shapiro–Wilk test was applied to test normality of the acquired data. Descriptive statistical data (e.g., test‐scores and MRT‐scores) were represented as mean with ± standard deviation (±SD) if normally distributed, and/or as a median with range Q1/Q3 if not normally distributed. Categorical data (e.g., gender, PLI/LFB‐group, and academic year) were reported as frequency (n) and as percentage of the total (%).
Dependent t tests were used to test the differences between pre‐intervention scores, post‐intervention scores, and long‐term scores. Two sample t tests were carried out to compare the mean test‐results between different groups. The two‐sample t test is generally used to test whether two population means are comparable or different. In educational research, a common application is to test whether a new teaching method is superior to the standard teaching method in two comparable groups of students (Snedecor and Cochrane, 1989). Effect sizes were reported using Cohen’s d. The Chi‐Square test was used to determine whether there was an association between categorical data. When data were not specified, these participants were excluded from the corresponding analyses.
RESULTS
Normally Distributed Test‐Data in a Representative Cohort Using Reliable and Consistent Tests
In total, 38 students (19 females and 19 males) studying medicine participated in this study. Age was found to be non‐normally distributed (P < 0.05). Median age showed to be 21.0 years (Q1: 20 years; Q3: 23 years). The majority of students were second‐year bachelor students (65.8%); 21.1% of the students were first‐year Master students, 2.6% of the students were second‐year Master students, and 10.5% of the students were third‐year Master students. MRT scores, pre‐intervention test scores, post‐intervention test scores, and long‐term test scores were found to be normally distributed (P = 0.679; P = 0.086; P = 0.129; P = 0.107, respectively). A Cronbach’s alpha of 0.905 was found for the MRT test which indicated that the MRT e‐learning module to test spatial ability was reliable and internally consistent. The pre‐intervention test, post‐intervention test, and long‐term test were found to be internally consistent and thus reliable with a Cronbach’s alpha of 0.713, 0.728, and 0.739, respectively.
The mean MRT score showed to be 13.2 ± SD 5.2 points (Table 1). The MRT scores of the males were not significantly different from those of the females (P = 0.134). Based on the demographics, the students were considered representative of the cohort of students at this university medical center. Although not formally tested, the researchers recognize that the included students most probably were more interested in neuroanatomy than the average medical student.
Table 1.
Sex Differences of Mental Rotations Test Scores and Knowledge Test Scores
| MRT/Test Score | Total (n = 38) Mean (±SD) | Males (n = 19) Mean (±SD) | Females (n = 19) Mean (±SD) | P‐value |
|---|---|---|---|---|
| MRT test score (points) | 13.2 (±5.2) | 15.2 (±4.0) | 11.2 (±5.5) | 0.134 a |
| Pre‐intervention test (%) | 49.9 (±11.8) | 50.8 (±13.1) | 48.7 (±10.4) | 0.630 a |
| Post‐intervention test score (%) | 77.9 (±14.5) | 82.1 (±13.8) | 73.7 (±14.3) | 0.937 a |
| Long‐term test score (%) | 66.5 (±16.2) | 65.8 (±16.0) | 67.1 (±16.1) | 0.700 a |
Independent t test; MRT = Mental Rotations Test.
Improvement After E‐Learning; No Differences Between Microscopy Visualization Techniques
In the total group, the mean pre‐intervention test score showed to be 49.87 ± 11.77%. The mean post‐intervention test score showed to be 77.89 ± 14.50%, indicating a significant improvement after learning brainstem anatomy through either e‐learning module (P < 0.001; Cohen’s d = −2.13). The long‐term test score showed to be 66.45 ± 16.23%, which indicated a significant improvement compared to the pre‐intervention test score (P < 0.001; Cohen’s d = −1.18) and a significant diminishment compared to the post‐intervention test (P < 0.001; Cohen’s d = 0.74). Nineteen students were included in the PLI group and 19 students were included in the LFB group. Baseline characteristics per group are depicted in Table 2. No significant differences were found between the baseline characteristics of the students in each group. Pre‐intervention scores were not significantly different between the two groups (P = 0.497; Cohen’s d = 0.20) Post‐intervention test scores in the PLI group (78.16 ± 10.70%) were not significantly different from those in the LFB group (77.63 ± 17.82%) (P = 0.913; Cohen’s d = 0.04). Long‐term test scores in the PLI group (68.68 ± 17.78%) were not significantly different from those in the LFB group (64.21 ± 14.65%) (P = 0.403; Cohen’s d = 0.30) (Figure 5).
Table 2.
Baseline Characteristics of the Participating Students
| Characteristics | Total n (%) | PLI Group n (%) | LFB Group n (%) | P‐value |
|---|---|---|---|---|
| Number of students | 38 (100.0) | 19 (100.0) | 19 (100.0) | |
| Age (years) | 21.5 (±2.37) | 21.84 ± 2.97 | 21.21 ± 1.58 | 0.420 a |
| Mean (±SD) | ||||
| Sex | ||||
| Female | 19 (50.0) | 8 (42.1) | 11 (57.9) | 0.330 b |
| Male | 19 (50.0) | 11 (57.9) | 8 (42.1) | |
| Class | 0.501 b | |||
| Bachelor (Second year) | 25 (65.8) | 11 (57.9) | 14 (73.7) | 0.549 b |
| Master (First year) | 8 (21.1) | 4 (21.1) | 4 (21.1) | >0.999 b |
| Master (Second year) | 1 (2.6) | 1 (5.3) | 0 (0) | N/A |
| Master (Third year) | 4 (10.5) | 3 (15.8) | 1 (5.3) | 0.317 b |
Independent t test.
Chi‐Square test; LFB, Luxol fast blue; PLI, Polarized light imaging.
Figure 5.
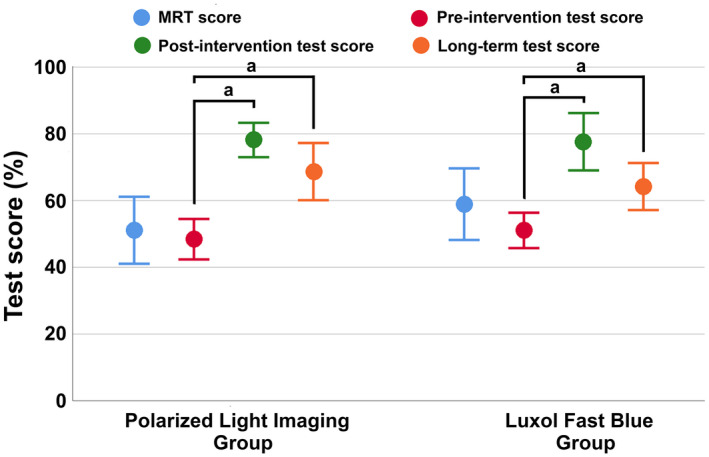
Students’ performance on mental rotation test (MRT) and knowledge tests. Results are presented in means % ± SD (95%‐C.I.) for both groups. a P < 0.05.
There was no significant difference in knowledge on the mesencephalon as assessed by the post‐intervention test (P = 0.449; Cohen’s d = −0.25) or the long‐term test (P = 0.455; Cohen’s d = 0.25). There was no significant difference in knowledge on the pons as assessed by the post‐intervention test (P = 0.855; Cohen’s d = 0.06) or the long‐term test (P = 0.384; Cohen’s d = 0.29). Finally, there was no significant difference in knowledge on the medulla as assessed by the post‐intervention test (P = 0.098; Cohen’s d = 0.56) or the long‐term test (P = 0.702; Cohen’s d = 0.13). With regard to knowledge of the craniocaudal relations of structures, there was no significant difference in knowledge as assessed by the post‐intervention test (P = 0.636; Cohen’s d = −0.16) or the long‐term test (P = 0.886; Cohen’s d = −0.05).
Mental Rotations Test Scores Positively Correlate with Knowledge Test‐Scores
A significant correlation could be found between the MRT score and pre‐ and post‐intervention test scores (rk = 0.236; P = 0.050 and rk = 0.321; P < 0.05, respectively). There was no significant correlation between MRT scores and the long‐term scores (rk = −0.078; P = 0.509).
In addition, there was a significant correlation between the pre‐intervention test score and the post‐intervention test score (rk = 0.310; P < 0.05). The pre‐intervention test score and long‐term test score, however, were not correlated (rk = 0.159; P = 0.197). Furthermore, a higher post‐intervention score did not correlate with a higher long‐term score (rk = 0.195; P = 0.108).
Qualitative Results
Ten students were willing to participate in the qualitative interview part of this study (five males; five females; mean age 21.13 ± 1.96 years). Six students worked with the PLI e‐learning module; four students worked with the LFB e‐learning module. From the qualitative analysis of students' interviews, 22 codes were derived, which could be divided into three overarching themes: (1) Learning anatomy by use of e‐learning modules, (2) The “need” of technological background information when studying brainstem sections, and (3) Mnemonics when studying brainstem anatomy.
Learning (brainstem) anatomy by use of e‐learning modules
Students were interviewed during the Covid‐19 pandemic, which caused them to have electronic study materials only to study anatomy. In practice, such electronic study materials mainly comprised various forms of online lectures. Therefore, using e‐learning modules on a new anatomical topic elicited interest in students from both the PLI group and the LFB group. Students complimented the researchers on the lay‐out and usability of the e‐learning modules. However, all participants also complained on lack of hands‐on activities when working with electronic study materials only. Especially when keeping in mind that most second‐year students saw their unique (the only course in the Netherlands) white matter brain dissection assignments being replaced by electronic education, it is not surprising that participants complained about this. Six students, however, expressed that they felt more “in control” when working with the e‐learning modules. They explained this by stating that the structure provided by the e‐learning modules helped them to create a logical overview of the subject. By dividing the brainstem into three regions along the craniocaudal axis, they felt that the complex anatomy became more compartmentalized. Then, each of the three regions was studied in depth in two dimensions with clear instructions and helpful hint‐buttons. By clicking these hint‐buttons, more information regarding a certain topic appeared. The feedback they received from the e‐learning module helped them maintain their attention and stay well‐focused: “I liked the e‐learnings a lot! When at home making assignments, this was a nice change in educational material to work with, even though it was just an experiment” [Student #15; PLI group], “I could determine my own learning pace with the e‐learnings. When E‐visiting a lecture, the professor speeds up or slows down at exactly the wrong moments. Then I just get lost.” [Student #3; LFB group], and “They looked nice, the e‐learnings. And they were functioning quite well; I did not really experience any technical disturbances.” [Student #14; LFB group].
The “need” of technological background information when studying brainstem sections
When asked to explain what the participants remembered from the technological information on PLI or LFB, all students expressed that they found this information rather profound and beyond their level of knowledge. They disclosed that they were less interested by this technical background. Although all participants explained that they understood that they needed some information on the methodology used to obtain the brainstem slices, they did not feel that it was obligatory to know “all the details.” In general, students expressed the need to understand “how to read” the presented figures. For example, in the PLI group students expressed that they only needed to know why there was a small circle in the left upper corner of the PLI figure. This color‐coded fiber‐orientation‐map wheel helped them to understand the direction of the fiber pathway. In LFB staining method group, students did not express this need to understand “how to read” the presented figures. These participants stated that all they needed to know was that LFB stained the myelin coverings of the axons, thereby making it a white matter staining method: “I did not really focus on the technical slides on PLI to be honest. I just wanted to understand it in such a way that I could understand the colorful PLI pictures” [student #28; PLI group], “I studied the LFB slides and I just remembered: ‘blue means white matter trajectories.’ That was enough for me to finish the e‐learning module and fill in the test. I think my test scores were rather O.K., so for me it worked” [student #3; LFB group].
Mnemonics when studying brainstem anatomy
When asked on their tactics how they filled in the post‐intervention test, students expressed that they had the information on brainstem anatomy fresh in their minds. Clustering information in the e‐learning module and during the tests by brainstem region (e.g., mesencephalon) enabled students to increase their knowledge retention. Students expressed that they could use this retention of knowledge during the post‐intervention test. They “simply remembered which structured was located lateral or medial.” However, after 1 week, students of the PLI group disclosed the use of a different mnemonic. During the long‐term test, all students in the PLI group explained that they visualized the sections of the brainstem in color, enabling them to distinguish different white matter tracts. The students explicitly explained that the visualized colors of the white matter tracts in the PLI figures were not necessarily needed for the students to learn correctly the fiber orientation of the tracts: “I liked it that the brainstem was categorized into three regions. That made it easier to comprehend. I liked it that some ‘old acquaintances’ in anatomy, for example the corticospinal tract, could be observed as well. And by following the corticospinal tract through the brainstem, it became clear where it decussates. Something I never really could picture by the way.” [Student #31; PLI group], “Well, I just pictured the PLI figures when making the last test after one week. I cannot imagine that the colors I remembered really represented the colors in the real PLI‐slides, to be honest. I just visualized the medial lemniscus as a purple structure, whereas the corticospinal tract was blue in my imagination. Probably these colors are incorrect, but it helped me!” [Student #7; PLI group], and “Well, all structures were blue‐ish. So I just tried to remember which tract was medial and which one ran lateral. It was not that difficult to remember after all.” [Student #32; LFB group].
DISCUSSION
This study showed that brainstem anatomy can be learned by use of different types of slices and was not affected by visualization technique. More specifically, students who learned brainstem anatomy by use of PLI sections did not outperform or underperform students who learned the same topic using LFB sections. However, spatial ability was found to have a significant positive correlation with the direct learning outcomes. There was, however, no significant correlation between MRT‐scores and long‐term scores.
Different Types of Sections in E‐Learning Modules for Brainstem Anatomy
It is already well‐known that the use of sections is an effective study method to learn neuroanatomy (Pani et al., 2013; Henssen et al., 2020). Nevertheless, cross‐sectional learning is also known to be considered difficult (Brunken et al., 2003; Anglin et al., 2004; Wilson, 2015) and it requires significant cognitive effort on behalf of the learner (Küçük et al., 2016; Henssen et al., 2020). Current results are, therefore, in line with the available literature. However, few studies have investigated the effect of different microscopy techniques (including different histological stains) on learning outcomes. In 2009, Rubin and colleagues studied the effect of grayscale images versus colored images of stained tissues in students suffering from color‐deficiency (Rubin et al., 2009). They emphasized that grayscale images provided information on the texture of tissues and the contrasts between tissues. This enabled color‐deficient students to learn histologic architecture, compensating for their deficiency by focusing tissue structures rather than on color variation (Rubin et al., 2009). Based upon this article, it is believed that the LFB‐stained sections in the e‐learning modules might be educational as they provided students with structural characteristics of the white matter tracts. Although lacking the information on fiber orientation, LFB‐stained sections might have encouraged students to consider structural characteristics that may otherwise be overshadowed in the brightly colored PLI images, similar to the explanation as proposed by Rubin et al. (2009). In addition, these results concur with evidence that visual ability and spatial ability play different distinct roles in anatomy education (Hegarty and Kozhevnikov, 1999; Kozhevnikov et al., 2002). These studies showed that low‐spatial visualizers interpreted graphs as pictures and mostly relied on visual (iconic) imagery, whereas high‐spatial visualizers constructed more schematic images and manipulated them spatially (Hegarty and Kozhevnikov, 1999; Kozhevnikov et al., 2002). As PLI and LFB were using visual cues, a role of visual abilities in the outcomes of the present study is expected. Although not investigated quantitatively, the qualitative interviews gave rise to such interactions and reaffirmed the findings of Hegarty and Kozhevnikov (1999) and Kozhevnikov et al. (2002).
E‐Learning Approaches to Study Sectional Anatomy and the Effects of Spatial Ability on Learning Outcomes
Correlation analysis showed that spatial ability was positively correlated with direct post‐intervention results. These results indicate that students with lower spatial abilities were disadvantaged by the e‐learning modules. This is in agreement with previous publications; previous work has showed that performance when working with e‐learning modules was correlated with the spatial insights of the learner (Luursema et al., 2006, 2008). More specifically, they found that stereopsis enabled students to perform significantly better on identification and localization tasks. Also, participants with lower spatial ability scores benefited more from the stereoptic tools than those with higher spatial ability scores (Luursema et al., 2006, 2008; Bogomolova et al., 2020; Wainman et al., 2020). Additionally, a recent meta‐analysis showed that stereopsis is an important distinguishing elements of 3D visualization technologies as this has a significant positive effect on acquisition of anatomical knowledge when using an interactive 3D environment (Bogomolova et al., 2021). However, long‐term outcomes have not been evaluated in these studies. In the present study, the correlation between MRT‐scores and learning outcome was not found in the test results 1 week after learning, whereas the MRT‐scores were correlated with the post‐intervention test scores. This suggests that spatial ability was influenced by visual abilities of the students and that visual abilities might have played a more important role than spatial ability. The lack of correlation between spatial ability and long‐term test outcomes may possibly be explained by an improvement of spatial abilities during the experiment itself. Such a practice effect has been described with students using the MRT (Peters et al., 1995) and spatial abilities have also been found to be trained by anatomy instruction and mental rotations training on an individual study level (Hoyek et al., 2009; Vorstenbosch et al., 2013), as well as on a meta‐level (Langlois et al., 2013, 2020). Furthermore, present results show no significant differences between males and females were found in spatial ability. This is not in line with the scientific literature on this topic in which males have been found to have increased spatial abilities in the field of anatomy education (Garg et al., 1999a, b; Lufler et al., 2012; Langlois et al., 2013; Vorstenbosch et al., 2013).
Multiple‐Choice Questions to Assess Anatomical Knowledge
In this study the specific multiple‐choice questions could have affected the outcome. Guillot et al. (2007) hypothesized that the anatomy examination does not only evaluate the acquisition and retention of the anatomy knowledge. They stated that such examination also assesses students’ visuo‐spatial abilities. This statement was strengthened by their observation that the higher performance of male students in the anatomy examination contrasted with their decreased success in their academic education when compared to their female colleagues. Therefore, they concluded that these observations would seem to confirm an independent external factor in their experiments, which may have influenced the outcomes (Guillot et al., 2007). This concurs with other studies where authors stated that specific mental rotation training may lead to higher scores in anatomy questions requiring spatial ability (Hoyek et al., 2009). The lack of visual representations in spatial multiple‐choice questions could have disadvantaged learners with lower spatial ability because providing visual clues eliminates the need for cognitively demanding mental rotations (Keedy et al., 2011).
Future Directions in Neuroanatomy Education
Several studies highlighted a perceived difficulty of understanding neuroanatomy among medical students (Zinchuk et al., 2010; Gupta et al., 2013; Matthias et al., 2013; Pakpoor et al., 2014). Previous studies have also found that participants with higher levels of interest in the studied subject reported higher levels of knowledge acquisition (Javaid et al., 2018). This suggested that teaching tools aimed at increasing interest could also increase knowledge retention. One of the methods to increase students’ interests could be the use of advances from other scientific domains. These advances should, however, first be tested for their potential educational benefits. Simultaneously, more appealing teaching methods should be searched for. Such appealing teaching methods could include various forms of 3D modeling, including augmented realty (Allen et al., 2016; Moro et al., 2017; Barmaki et al., 2019; Bork et al., 2019; Henssen et al., 2020), virtual reality (Birbara et al., 2020; Kurul et al., 2020; Birbara and Pather, 2021), and 3D‐printing (Backhouse et al., 2019; Young et al., 2019). Three‐dimensional models have also been used to teach brainstem anatomy to students, although most of these applications focused on cranial nerve anatomy (Yeung et al., 2011; Richardson‐Hatcher et al., 2014).
Limitations of the Study
The relatively small cohort enrolled in this study should be regarded as one of its limitations.
Another limitation is that cognitive load was not included as one of the parameters. The cognitive load theory was aimed to develop optimal instructional design principles and strategies while keeping the human cognitive architecture in mind (Sweller, 1988). It is assumed that the human cognitive system has a limited working memory (five to nine novel elements) (Miller, 1956; Ockelford, 2002) and that working memory actively processes no more than two to four new elements simultaneously (Baddeley and Hitch, 1974; Ockelford, 2002). It also assumes that almost all new information is lost after approximately 20 seconds without rehearsal. The theory emphasizes that these rules only apply to novel information, obtained through sensory memory (Sweller, 1988; Van Merriënboer and Sweller, 2010). In anatomy education, the cognitive load theory also plays an important role (Brunken et al., 2003; Anglin et al., 2004; Wilson, 2015; Henssen et al., 2020).
In addition, the period between the post‐intervention test and the long‐term test was relatively short and future studies should expand this window between tests to assess longer term knowledge retention. However, it emerged that studying brainstem anatomy by use of cross‐sections is a valuable method, especially for students with good spatial insight.
Another limitation of the present study is formed by the lack of a control group not subjected to any educational intervention. By including this group, it would be possible see if improvement would occur without any educational intervention as a practice effect. However, the educational interventions used in this study (e‐learning modules using PLI slides vs. LFB‐slides) covered a topic that was not discussed in the curriculum at this university medical center. Therefore, the authors believe that an improvement over time without any education intervention was unlikely to occur. The lack of this control group, however, must be considered a limitation of the present study.
CONCLUSIONS
This study shows that learning brainstem anatomy by use of e‐learning modules with digitized cross‐sections is a valuable study method. This study method was found especially effective for students with higher spatial ability. No differences in learning outcome were observed between students who studied brainstem anatomy with PLI sections and LFB sections. Qualitatively, the brightly colored PLI sections remained visualizable for students, in contrast to the LFB sections. Future studies should include cognitive load as an additional outcome measure to assess the cognitive burden of cross‐sectional learning methods and their effects on knowledge retention.
NOTES ON CONTRIBUTORS
ANNE‐MARIE VAN CAPPELLEN VAN WALSUM, M.D. Ph.D., is an assistant professor of anatomy and associate principal lecturer in the Department of Medical Imaging at the Radboud University Medical Centre in Nijmegen, the Netherlands. She teaches and coordinates anatomy and neuroanatomy courses for medical, biomedical, and technical medicine students. Her research interest is in studying the anatomy and pathology of white matter brain networks with innovative imaging techniques.
DYLAN J.H.A. HENSSEN, M.D., Ph.D., is a second‐year resident and post‐doctoral researcher in the Department of Radiology and Nuclear Medicine at the Radboud University Medical Centre in Nijmegen, the Netherlands. He focuses on neuroanatomy and radiology education and his research interest is in application of augmented and virtual reality and other innovative three‐dimensional imaging techniques in clinical and educational settings.
Supporting information
Supplementary Material
Supplementary Material
Acknowledgments
The authors declare that they have no conflict of interest in the conduction of this research.
No funding was received for conducting this research. All data, including the SCORM packages of the [Dutch] e‐learning modules (with the exception of the MRT e‐learning module) can be acquired upon reasonable request by contacting the corresponding author.
LITERATURE CITED
- Albanese M. 2010. The gross anatomy laboratory: A prototype for simulation‐based medical education. Med Educ 44:7–9. [DOI] [PubMed] [Google Scholar]
- Allen LK, Eagleson R, de Ribeaupierre S. 2016. Evaluation of an online three‐dimensional interactive resource for undergraduate neuroanatomy education. Anat Sci Educ 9:431–439. [DOI] [PubMed] [Google Scholar]
- Alonso F, López G, Manrique D, Viñes JM. 2005. An instructional model for web‐based e‐learning education with a blended learning process approach. Br J Educ Technol 36:217–235. [Google Scholar]
- Angeles Fernández‐Gil M, Palacios‐Bote R, Leo‐Barahona M, Mora‐Encinas JP. 2010. Anatomy of the brainstem: A gaze into the stem of life. Semin Ultrasound CT MR 31:196–219. [DOI] [PubMed] [Google Scholar]
- Anglin GJ, Vaez H, Cunningham KL. 2004. Visual representations and learning: The role of static and animated graphics. In: Jonassen DH (Editor). Handbook of Research on Educational Communications and Technology. 2nd Ed. New York, NY: Lawrence Erlbaum Associate Publishers. p 865–916. [Google Scholar]
- Axer M, Amunts K, Grässel D, Palm C, Dammers J, Axer H, Pietrzyk U, Zilles K. 2011a. A novel approach to the human connectome: Ultra‐high resolution mapping of fiber tracts in the brain. NeuroImage 54:1091–1101. [DOI] [PubMed] [Google Scholar]
- Axer M, Axer H, Grassel D, Amunts K, Zilles K, Pietrzyk U. 2007. Nerve fiber mapping of the human visual cortex using polarized light imaging (PLI). In: Yu B. (Editor). 2007 IEEE Nuclear Science Symposium Conference Record: Nuclear Science Symposium and Medical Imaging Conference (2007 NSS/MIC); Honolulu, HI, 2007 October 26 ‐ November 2. p 4345–4347. Institute of Electrical and Electronics Engineers (IEEE), Piscataway, NJ. [Google Scholar]
- Axer M, Grässel D, Kleiner M, Dammers J, Dickscheid T, Reckfort J, Hütz T, Eiben B, Pietrzyk U, Zilles K, Amunts K. 2011b. High‐resolution fiber tract reconstruction in the human brain by means of three‐dimensional polarized light imaging. Front Neuroinform 5:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Backhouse S, Taylor D, Armitage JA. 2019. Is this mine to keep? Three‐dimensional printing enables active, personalized learning in anatomy. Anat Sci Educ 12:518–528. [DOI] [PubMed] [Google Scholar]
- Baddeley A, Hitch G. 1974. Working memory. Psychol Learn Motiv 8:47–89. [Google Scholar]
- Barmaki R, Yu K, Pearlman R, Shingles R, Bork F, Osgood GM, Navab N. 2019. Enhancement of anatomical education using augmented reality: An empirical study of body painting. Anat Sci Educ 12:599–609. [DOI] [PubMed] [Google Scholar]
- Birbara NS, Pather N. 2021. Real or not real: The impact of the physical fidelity of virtual learning resources on learning anatomy. Anat Sci Educ (in press; 10.1002/ase.2022). [DOI] [PubMed] [Google Scholar]
- Birbara NS, Sammut C, Pather N. 2020. Virtual reality in anatomy: A pilot study evaluating different delivery modalities. Anat Sci Educ 13:445–457. [DOI] [PubMed] [Google Scholar]
- Bloom BS (Editor). 1956. Taxonomy of Educational Objectives: The Classification of Educational Goals. Handbook 1: Cognitive Domain. 1st Ed. New York, NY: David McKay Co, Inc. 201 p. [Google Scholar]
- Bogomolova K, Ham IJ, Dankbaar ME, van der Broek WW, Hovlus SE, van der Hage JA, Hierck BP. 2020. The effect of stereoscopic augmented reality visualization on learning anatomy and the modifying effect of visual‐spatial abilities: A double‐center randomized controlled trial. Anat Sci Educ 13:558–567. [DOI] [PubMed] [Google Scholar]
- Bogomolova K, Hierck BP, Looijen AE, Pilon JM, Putter H, Wainman B, Hovius SE, van der Hage JA. 2021. Stereoscopic three‐dimensional visualisation technology in anatomy learning: A meta‐analysis. Med Educ (in press; 10.1111/medu.14352). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bork F, Stratmann L, Enssle S, Eck U, Navab N, Waschke J, Kugelmann D. 2019. The benefits of an augmented reality magic mirror system for integrated radiology teaching in gross anatomy. Anat Sci Educ 12:585–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce‐Gregorios JH. 2006. Histophatologic Techniques. 2nd Ed. Quezon City, Philippines: Goodwill Trading Co., Inc. 356 p. [Google Scholar]
- Brunken R, Plass JL, Leutner D. 2003. Direct measurement of cognitive load in multimedia learning. Educ Psychol 38:53–61. [DOI] [PubMed] [Google Scholar]
- Evans DJ, Bay BH, Wilson TD, Smith CF, Lachman N, Pawlina W. 2020. Going virtual to support anatomy education: A STOPGAP in the midst of the Covid‐19 pandemic. Anat Sci Educ 13:279–283. [DOI] [PubMed] [Google Scholar]
- Fitzgerald JE, White MJ, Tang SW, Maxwell‐Armstrong CA, James DK. 2008. Are we teaching sufficient anatomy at medical school? The opinions of newly qualified doctors. Clin Anat 21:718–724. [DOI] [PubMed] [Google Scholar]
- Frank JR, Danoff D. 2007. The CanMEDS initiative: Implementing an outcomes‐based framework of physician competencies. Med Teach 29:642–647. [DOI] [PubMed] [Google Scholar]
- Garcia M, Victory N, Navarro‐Sempere A, Segovia Y. 2019. Students' views on difficulties in learning histology. Anat Sci Educ 12:541–549. [DOI] [PubMed] [Google Scholar]
- Garg AX, Norman GR, Eva KW, Spero L, Sharan S. 2002. Is there any real virtue of virtual reality? The minor role of multiple orientations in learning anatomy from computers. Acad Med 77:S97–S99. [DOI] [PubMed] [Google Scholar]
- Garg A, Norman GR, Spero L, Maheshwari P. 1999a. Do virtual computer model hinder anatomy learning? Acad Med 74:S87–S89. [DOI] [PubMed] [Google Scholar]
- Garg A, Norman G, Spero L, Taylor I. 1999b. Learning anatomy: Do new computer models improve spatial understanding? Med Teach 21:519–522. [Google Scholar]
- Guillot A, Champely S, Batier C, Thiriet P, Collet C. 2007. Relationship between spatial abilities, mental rotation and functional anatomy learning. Adv Health Sci Educ Theory Prac 12:491–507. [DOI] [PubMed] [Google Scholar]
- Gupta NB, Khadilkar SV, Bangar SS, Patil TR, Chaudhari CR. 2013. Neurology as career option among postgraduate medical students. Ann Indian Acad Neurol 16:478–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hegarty M, Keehner M, Khooshabeh P, Montello DR. 2009. How spatial abilities enhance, and are enhanced by, dental education. Learn Individ Differ 19:61–70. [Google Scholar]
- Hegarty M, Kozhevnikov M. 1999. Types of visual‐spatial representations and mathematical problem solving. J Educ Psychol 91:684–689. [Google Scholar]
- Henssen DJ, Derks B, van Doorn M, Verhoogt NC, Staats P, Vissers K, Van Cappellen van Walsum AM. 2019b. Visualizing the trigeminovagal complex in the human medulla by combining ex‐vivo ultra‐high resolution structural MRI and polarized light imaging microscopy. Sci Rep 9:11305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henssen DJ, Mollink J, Kurt E, van Dongen R, Bartels RH, Gräβel D, Kozicz T, Axer M, Van Cappellen van Walsum AM. 2019a. Ex vivo visualization of the trigeminal pathways in the human brainstem using 11.7T diffusion MRI combined with microscopy polarized light imaging. Brain Struct Funct 224:159–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henssen DJ, van den Heuvel L, De Jong G, Vorstenbosch MA, van Cappellen van Walsum AM, Van den Hurk MM, Kooloos JG, Bartels RH. 2020. Neuroanatomy learning: Augmented reality vs. cross‐sections. Anat Sci Educ 13:353–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyek N, Collet C, Rastello O, Fargier P, Thiriet P, Guillot A. 2009. Enhancement of mental rotation abilities and its effect on anatomy learning. Teach Learn Med 21:201–206. [DOI] [PubMed] [Google Scholar]
- Javaid MA, Chakraborty S, Cryan JF, Schellekens H, Toulouse A. 2018. Understanding neurophobia: Reasons behind impaired understanding and learning of neuroanatomy in cross‐disciplinary healthcare students. Anat Sci Educ 11:81–93. [DOI] [PubMed] [Google Scholar]
- Keedy AW, Durack JC, Sandhu P, Chen EM, O’Sullivan PS, Breiman RS. 2011. Comparison of traditional methods with 3D computer models in the instruction of hepatobiliary anatomy. Anat Sci Educ 4:84–91. [DOI] [PubMed] [Google Scholar]
- Kooloos JG, Schepens‐Franke AN, Bergman EM, Donders RA, Vorstenbosch MA. 2014. Anatomical knowledge gain through a clay‐modeling exercise compared to live and video observations. Anat Sci Educ 7:420–429. [DOI] [PubMed] [Google Scholar]
- Kozhevnikov M, Hegarty M, Mayer RE. 2002. Revising the visualizer‐verbalizer dimension: Evidence of two types of visualizers. Cognit Instruct 20:47–77. [Google Scholar]
- Küçük S, Kapakin S, Göktaş Y. 2016. Learning anatomy via mobile augmented reality: Effects on achievement and cognitive load. Anat Sci Educ 9:411–421. [DOI] [PubMed] [Google Scholar]
- Kurul R, Ögün MN, Neriman Narin A, Avci Ş, Yazgan B. 2020. An alternative method for anatomy training: Immersive virtual reality. Anat Sci Educ 13:648–656. [DOI] [PubMed] [Google Scholar]
- Langlois J, Bellemare C, Toulouse J, Wells GA. 2017. Spatial abilities and anatomy knowledge assessment: A systematic review. Anat Sci Educ 10:235–241. [DOI] [PubMed] [Google Scholar]
- Langlois J, Bellemare C, Toulouse J, Wells GA. 2020. Spatial abilities training in anatomy education: A systematic review. Anat Sci Educ 13:71–79. [DOI] [PubMed] [Google Scholar]
- Langlois J, Wells GA, Lecourtois M, Bergeron G, Yetisir E, Martin M. 2013. Sex differences in spatial abilities of medical graduates entering their residency programs. Anat Sci Edu 6:368–375. [DOI] [PubMed] [Google Scholar]
- Lewis KO, Cidon MJ, Seto TL, Chen H, Mahan JD. 2014. Leveraging e‐learning in medical education. Curr Probl Pediatr Adolesc Health Care 44:150–163. [DOI] [PubMed] [Google Scholar]
- Linn MC, Petersen AC. 1985. Emergence and characterization of sex differences in spatial ability: A meta‐analysis. Child Dev 56:1479–1498. [PubMed] [Google Scholar]
- Lufler RS, Zumwalt AC, Romney CA, Hoagland TM. 2012. Effect of visual‐spatial ability on medical students' performance in a gross anatomy course. Anat Sci Educ 5:3–9. [DOI] [PubMed] [Google Scholar]
- Luursema JM, Vervey WB, Kommers PA, Annema J‐H. 2008. The role of stereopsis in virtual anatomical learning. Interact Comput 20:455–460. [Google Scholar]
- Luursema JM, Vervey WB, Kommers PA, Geelkerken RH, Vos HJ. 2006. Optimizing conditions for computer‐assisted anatomical learning. Interact Comput 18:1123–1138. [Google Scholar]
- Maccoby EE, Jacklin CN. 1974. The Psychology of Sex Differences. Volume I. 1st Ed. Stanford, CA: Stanford University Press. 416 p. [Google Scholar]
- Mai JK, Majtanik M, Paxinos G. 2015. Atlas of the Human Brain. 4th Ed. London, UK: Academic Press. 456 p. [Google Scholar]
- Mai JK, Paxinos G (Editors). 2011. The Human Nervous System. 3rd Ed. London, UK: Academic Press. 1428 p. [Google Scholar]
- Matthias AT, Nagasingha P, Ranasinghe P, Gunatilake SB. 2013. Neurophobia among medical students and non‐specialist doctors in Sri Lanka. BMC Med Educ 13:164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGee MG. 1979. Human spatial abilities: Psychometric studies and environmental, genetic, hormonal, and neurological influences. Psychol Bull 86:889–918. [PubMed] [Google Scholar]
- Miller G. 1956. The magical number seven, plus or minus two: Some limits on our capacity for processing information. Psychol Rev 63:81–97. [PubMed] [Google Scholar]
- Mollink J, Hiemstra M, Miller KL, Huszar IN, Jenkinson M, Raaphorst J, Wiesmann M, Ansorge O, Pallebage‐Gamarallage M, van Cappellen van Walsum AM. 2019. White matter changes in the perforant path area in patients with amyotrophic lateral sclerosis. Neuropathol Appl Neurobiol 45:570–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mollink J, Kleinnijenhuis M, Cappellen van Walsum AV, Sotiropoulos SN, Cottaar M, Mirfin C, Heinrich MP, Jenkinson M, Pallebage‐Gamarallage M, Ansorge O, Jbabdi S, Miller KL. 2017. Evaluating fibre orientation dispersion in white matter: Comparison of diffusion MRI, histology and polarized light imaging. NeuroImage 157:561–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moro C, Štromberga Z, Raikos A, Stirling A. 2017. The effectiveness of virtual and augmented reality in health sciences and medical anatomy. Anat Sci Educ 10:549–559. [DOI] [PubMed] [Google Scholar]
- Nguyen N, Mulla A, Nelson AJ, Wilson TD. 2014. Visuospatial anatomy comprehension: The role of spatial visualization ability and problem‐solving strategies. Anat Sci Educ 7:280–288. [DOI] [PubMed] [Google Scholar]
- Nieuwenhuys R, Voogd J, van Huijzen C. 2008. The Human Central Nervous System: A Synopsis and Atlas. 4th Ed. Berlin, Germany: Springer‐Verlag. 981 p. [Google Scholar]
- Ockelford A. 2002. The magical number two, plus or minus one: Some limits on our capacity for processing musical information. Music Sci 6:185–219. [Google Scholar]
- Pakpoor J, Handel AE, Disanto G, Davenport RJ, Giovannoni G, Ramagopalan SV, Association of British Neurologists . 2014. National survey of UK medical students on the perception of neurology. BMC Med Educ 14:225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pani JR, Chariker JH, Naaz F. 2013. Computer‐based learning: Interleaving whole and sectional representation of neuroanatomy. Anat Sci Educ 6:11–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pawlina W, Ross MH. 2018. Histology: A Text and Atlas: With Correlated Cell and Molecular Biology. 8th Ed. Baltimore, MD: Wolters Kluwer Health. 928 p. [Google Scholar]
- Peters M, Laeng B, Latham K, Jackson M, Zaiyouna R, Richardson C. 1995. A redrawn Vandenberg and Kuse Mental Rotations Test: Different versions and factors that affect performance. Brain Cogn 28:39–58. [DOI] [PubMed] [Google Scholar]
- Peters M, Manning JT, Reimers S. 2007. The effects of sex, sexual orientation, and digit ratio (2D:4D) on mental rotation performance. Arch Sex Behav 36:251–260. [DOI] [PubMed] [Google Scholar]
- Provo J, Lamar C, Newby T. 2002. Using a cross‐section to train veterinary students to visualize anatomical structures in three dimensions. J Res Sci Teach 39:10–34. [Google Scholar]
- Radboud Health Academy . 2019. Radboud University Medical Center Studiecatalogus 2019/2020. Radboud University Medical Center, Nijmegen, the Netherlands. URL: https://healthacademy.radboudumc.nl/studiecatalogus/#/ [accessed 20 December 2020]. [Google Scholar]
- Ravi KS. 2020. Dead body management in times of Covid‐19 and its potential impact on the availability of cadavers for medical education in India. Anat Sci Educ 13:313–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson‐Hatcher A, Hazzard M, Ramirez‐Yanez G. 2014. The cranial nerve skywalk: A 3D tutorial of cranial nerves in a virtual platform. Anat Sci Educ 7:469–478. [DOI] [PubMed] [Google Scholar]
- Roach VA, Mi M, Mussell J, Van Nuland SE, Lufler RS, DeVeau K, Dunham SM, Husmann P, Herriott HL, Edwards DN, Doubleday AF, Wilson BM, Wilson AB. 2021. Correlating spatial ability with anatomy assessment performance: A meta‐analysis. Anat Sci Educ (in press; 10.1002/ase.2029). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rochford K. 1985. Spatial learning disabilities and underachievement among university anatomy students. Med Educ 19:13–26. [DOI] [PubMed] [Google Scholar]
- Roth JA, Wilson TD, Sandig M. 2015. The development of a virtual 3D model of the renal corpuscle from serial histological sections for e‐learning environments. Anat Sci Educ 8:574–583. [DOI] [PubMed] [Google Scholar]
- Rubin LR, Lackey WL, Kennedy FA, Stephenson RB. 2009. Using color and grayscale images to teach histology to color‐deficient medical students. Anat Sci Educ 2:84–88. [DOI] [PubMed] [Google Scholar]
- Sclocco R, Beissner F, Bianciardi M, Polimeni JR, Napadow V. 2018. Challenges and opportunities for brainstem neuroimaging with ultrahigh field MRI. NeuroImage 168:412–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shepard RN, Metzler J. 1971. Mental rotation of three‐dimensional objects. Science 171:701–703. [DOI] [PubMed] [Google Scholar]
- Snedecor GW, Cochran WG. 1989. Statistical Methods. 8th Ed. Ames, IA: Iowa State University Press. 503 p. [Google Scholar]
- Sotgiu MA, Mazzarello V, Bandiera P, Madeddu R, Montella A, Moxham B. 2020. Neuroanatomy, the Achille's heel of medical students. A systematic analysis of educational strategies for the teaching of neuroanatomy. Anat Sci Educ 13:107–116. [DOI] [PubMed] [Google Scholar]
- Sweller J. 1988. Cognitive load during problem‐solving ‐ Effects on learning. Cognit Sci 12:257–285. [Google Scholar]
- Van Merriënboer JJG, Sweller J. 2010. Cognitive load theory in health professional education: Design principles and strategies. Med Educ 44:85–93. [DOI] [PubMed] [Google Scholar]
- Van Nuland SE, Rogers KA. 2016. The anatomy of e‐learning tools: Does software usability influence learning outcomes? Anat Sci Educ 9:378–390. [DOI] [PubMed] [Google Scholar]
- Vandenberg SG, Kuse AR. 1978. Mental rotations, a group test of three‐dimensional spatial visualization. Percept Motor Skill 47:599–604. [DOI] [PubMed] [Google Scholar]
- Viktorov IV. 1978. Rapid method of combined staining of myelinated fibers and brain cells. Arkh Patol 40:73–76. [PubMed] [Google Scholar]
- Vorstenbosch MA, Klaassen TP, Donders AR, Kooloos JG, Bolhuis SM, Laan RF. 2013. Learning anatomy enhances spatial ability. Anat Sci Educ 6:257–262. [DOI] [PubMed] [Google Scholar]
- Voyer D, Voyer S, Bryden MP. 1995. Magnitude of sex differences in spatial abilities: A meta‐ analysis and consideration of critical variables. Psychol Bull 117:250–270. [DOI] [PubMed] [Google Scholar]
- Wainman B, Pukas G, Wolak L, Mohanraj S, Lamb J, Norman GR. 2020. The critical role of stereopsis in virtual and mixed reality learning environments. Anat Sci Educ 13:401–412. [DOI] [PubMed] [Google Scholar]
- Wiesmann M, Guardia GS, Janssen E, Veltien A, Mollink J, Dederen PJ, Heerschap A, Kiliaan AJ, de Leeuw FE. 2019. Inflammation, demyelination, and their role in cerebral small vessel disease. A postmortem combined (ultra‐) high‐field MRI, polarized light imaging, and immunohistochemistry approach. J Cerebr Blood Flow Metabol 39:393–394. [Google Scholar]
- Wilson TD. 2015. Role of image and cognitive load in anatomical multimedia. In: Chan LK, Pawlina W (Editors). Teaching Anatomy: A Practical Guide. 1st Ed. New York, NY: Springer International Publishing. p 237–246. [Google Scholar]
- WMA . 2013. World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 310:2191–2194. [DOI] [PubMed] [Google Scholar]
- Yeung JC, Fung K, Wilson TD. 2011. Development of a computer‐assisted cranial nerve simulation from the visible human dataset. Anat Sci Educ 4:92–97. [DOI] [PubMed] [Google Scholar]
- Young JC, Quayle MR, Adams JW, Bertram JF, McMenamin PG. 2019. Three‐dimensional printing of archived human fetal material for teaching purposes. Anat Sci Educ 12:90–96. [DOI] [PubMed] [Google Scholar]
- Zimmermann E, Germershausen C, Greupner J, Schnapauff D, Rief M, Grigoryev M, Wollenberg U, Dewey M. 2010. Improvement of skills and knowledge by a hands‐on cardiac CT course: Before and after evaluation with a validated questionnaire and self‐assessment. Rofo 182:589–593. [DOI] [PubMed] [Google Scholar]
- Zinchuk AV, Flanagan EP, Tubridy NJ, Miller WA, McCullough LD. 2010. Attitudes of us medical trainees towards neurology education: “Neurophobia” ‐ A global issue. BMC Med Educ 10:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
Supplementary Material


