Abstract
Objective
To assess national and regional trends and causes‐specific distribution of maternal mortality in India.
Design
Nationally representative cross‐sectional surveys.
Setting
All of India from 1997 to 2020.
Sample
About 10 000 maternal deaths among 4.3 million live births over two decades.
Methods
We analysed trends in the maternal mortality ratio (MMR) from 1997 through 2020, estimated absolute maternal deaths and examined the causes of maternal death using nationally representative data sources. We partitioned female deaths (aged 15–49 years) and live birth totals, based on the 2001–2014 Million Death Study to United Nations (UN) demographic totals for the country.
Main outcome measures
Maternal mortality burden and distribution of causes.
Results
The MMR declined in India by about 70% from 398/100 000 live births (95% CI 378–417) in 1997–98 to 99/100 000 (90–108) in 2020. About 1.30 million (95% CI 1.26–1.35 million) maternal deaths occurred between 1997 and 2020, with about 23 800 (95% CI 21 700–26 000) in 2020, with most occurring in poorer states (63%) and among women aged 20–29 years (58%). The MMRs for Assam (215), Uttar Pradesh/Uttarakhand (192) and Madhya Pradesh/Chhattisgarh (170) were highest, surpassing India’s 2016–2018 estimate of 113 (95% CI 103–123). After adjustment for education and other variables, the risks of maternal death were highest in rural and tribal areas of north‐eastern and northern states. The leading causes of maternal death were obstetric haemorrhage (47%; higher in poorer states), pregnancy‐related infection (12%) and hypertensive disorders of pregnancy (7%).
Conclusions
India could achieve the UN 2030 MMR goals if the average rate of reduction is maintained. However, without further intervention, the poorer states will not.
Tweetable abstract
We estimated that 1.3 million Indian women died from maternal causes over the last two decades. Although maternal mortality rates have fallen by 70% overall, the poorer states lag behind.
Keywords: Causes of maternal death, India, maternal mortality, trends in maternal mortality, UN goals
Tweetable abstract
We estimated that 1.3 million Indian women died from maternal causes over the last two decades. Although maternal mortality rates have fallen by 70% overall, the poorer states lag behind.
Introduction
The Government of India is a signatory to the United Nations (UN) Sustainable Development Goals (SDGs), which adopted a global maternal mortality ratio (MMR) target of fewer than 70 deaths per 100 000 live births by 2030. 1 This requires the reliable quantification of maternal deaths and trends and an understanding of the major causes of these deaths at the subnational level. India, similar to many countries with high maternal mortality, officially registers only a fraction of births, deaths and vital events. 2 , 3 Maternal deaths are concentrated in remote rural areas and are among the least likely to be recorded. 4 India, however, has had a functioning Sample Registration System (SRS) to monitor fertility and mortality covering over 1 million nationally representative homes for more than five decades.
The UN estimates that about 24 million children were born in 2017 in India, and about 35 000 mothers died during childbirth or shortly thereafter, giving an MMR of 145 per 100 000 live births. 5 This rate represented 12% of global maternal deaths. According to the World Health Organization (WHO), the worldwide MMR has fallen substantially from 342 in the year 2000 to 211 in 2017, reducing global maternal deaths from 451 000 to 295 000 during this period. 5 About 40% of this absolute decline was derived from fewer maternal deaths in India. 4
Here, we evaluate national and subnational levels and trends of maternal mortality over a 20‐year period in India by examining nearly 10 000 maternal deaths among 4.3 million live births identified in the SRS, and over 1500 maternal deaths assigned causes in the Million Death Study (MDS), a nationally representative, population‐based mortality survey. 6 , 7 We focus particularly on the rates of progress in the poorer states of India, which currently lag behind the national trends. A 2006 report, 4 based on maternal deaths captured in the SRS from 1997 to 2003, suggested that progress at that time was insufficient for India to meet the 2015 UN goals. We reassess that projection and point to how India can achieve the 2030 SDG 3.1.
Methods
Data source and design
We applied the WHO definitions of maternal death, namely the death of a woman while pregnant or within 42 days of terminating a pregnancy, irrespective of the site and duration of the pregnancy, from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes. 8 We selected nationally representative data sources to assess MMRs, and estimate maternal deaths and cause distribution. We extracted ten periodic MMR estimates (representing 2‐ or 3‐year periods from 1997 to 2018) for all of India, for major regions and for individual states from the SRS Special Bulletins on Maternal Mortality, 9 which provide subnational MMR statistics.
The SRS is a large‐scale continuous demographic survey conducted by the Registrar General of India since 1971 that provides national‐ and state‐level birth and death estimates. The current SRS covers about 8.1 million people selected from 8847 sample units (rural villages or urban blocks) in all states and union territories. 10 , 11 We also assembled complimentary information from other nationally representative MMR estimates from the National Family Health Surveys (NFHS) for 1998–1999, 12 the Indian Institute of Health and Family Welfare survey, 13 and the model‐based WHO/UN MMR estimates from 2000 to 2017. 14 These provided relevant maternal mortality data, albeit with limitations in methodology and under‐reporting. We extracted MMR estimates for 2010–2013 in three rounds of the Annual Health Survey (AHS), representative for nine poorer states, 15 , 16 , 17 which permitted a regional comparison of AHS and SRS estimates for this group of states.
We created two main categories of states: ‘poorer’ states, comprising eight Empowered Action Group states plus Assam (EAGA); and ‘Other’ states, consisting of richer states and union territories in the south and other regions, as defined by the SRS. 9 Within EAGA, we regrouped six previously partitioned major states into their original (pre‐1991) states to enable the consistent monitoring of trends over the two decades in: Uttar Pradesh combined with Uttarakhand, Bihar combined with Jharkhand, Madhya Pradesh combined with Chhattisgarh, Rajasthan, Orissa and Assam.
Cause‐of‐death information (2007–2014) comes from MDS, a continuing, nationally representative, population‐based mortality survey conducted concurrently within the SRS. 18 , 19 The MDS collects data on the causes of death for all households in the SRS. We applied a modified WHO verbal autopsy tool that includes a local language narrative section describing the history prior to death, obtained from a family member of the deceased. We converted paper records to electronic records, and two trained general physicians independently and anonymously assigned an underlying cause of death using MDS guidelines. 20 We used International Classification of Diseases and Related Health Problems, 10th revision (ICD‐10) codes to determine the cause of death. 21 Any coding disagreements underwent a process of reconciliation and adjudication. The codes assigned by non‐specialist physicians were subsequently re‐reviewed by another group of specially trained obstetricians and physicians (RB, NC, MS, PS and JWS) to assign final maternal causes of death using the most recent WHO criteria. 22 A subteam (AS, TH, LR, NC and PS) reviewed the narratives to establish the planned and actual place of birth, and place of death, using a validated maternal data extraction tool. 23 Details of the MDS methodology, including the completeness of deaths captured and misclassification of causes, are published elsewhere. 3 , 24 , 25
Analyses
We computed MMR as maternal deaths per 100 000 live births by pooling the respective SRS sample number of maternal deaths and live births for each state, and derived 95% CIs using the delta method with a variance of Pf /[N * (1 – Pf )3] where Pf is the proportion of maternal deaths to live births. 5 , 26 , 27 For 2016–2018, we estimated the sample number of maternal deaths and live births by using the published SRS indicators for births and population, as the 2016–2018 SRS bulletins published only ratios and not the actual numbers of maternal deaths and live births. We projected MMRs for 2020 in India and major subnational regions (EAGA and other) assuming the average annual rate of reduction for the 20‐year period, with an upper and lower limit based on the 95% CI. 5 We excluded the 1997–1998 estimate for Gujarat because of an implausibly low MMR of 46. Finally, we used the trends over the study period to project MMRs in 2030 to determine the likelihood of meeting India’s goal for MMRs of <70 per 100 000 live births in the country as a whole and in each major state.
We estimated the absolute number of maternal deaths in India using UN Population Division 2019 estimates for deaths of women aged 15–49 years, and distributed the national total by state and region using the proportional distribution of MDS deaths, after applying survey weights. 28 We adjusted regional and state totals to match the UN national totals. This enabled the forward projections from 2016–2018 to 2019 and 2020. The use of UN demographic totals has the benefit of correcting for the slight undercounting in the ascertainment of adult female deaths in the SRS. 29
For a spatial analysis of the risk of maternal mortality, we geocoded maternal deaths and SRS live births for 2008–2011 to 7214 sampling units (after the exclusion of sampling units from smaller islands of India), as we had live birth data only at the SRS unit level for these years. We applied a geostatistical Bayesian Poisson model to estimate the spatially smoothed and risk‐adjusted MMR. 30 The geostatistical models adjusted for yearly time trends, urban/rural setting, subdistrict‐level female illiteracy, proportion of smokers from the sampling units and language regions (as a proxy for geographic regions). To account for potential spatial variation and sampling unit‐level variation, possibly as a result of factors that were not already included as covariates, we added smoothly varying spatial random effects (i.e. spatial autocorrelation or clustering) and independent unit‐level random effects. The geostatistical Bayesian model has been applied recently to snakebite mortality in India. 30 , 31 , 32
We analysed causes of maternal death from the MDS for 2007–2014 by extracting deaths that were assigned obstetric or pregnancy‐related ICD codes by trained physicians, according to WHO guidelines. We tabulated the main categories of maternal death causes and classified them further into two broad groups of direct and indirect causes. We assessed the distribution of causes of maternal deaths in India and compared this between poorer (Bihar and Uttar Pradesh) and richer (Maharashtra, Kerala and Tamil Nadu) states.
Results
We included 9573 maternal deaths among 4.3 million live births reported in India through the SRS from 1997–1998 to 2016–2018. About 58% (5517) of maternal deaths occurred among women aged 20–29 years, peaking at the ages of 20–24 years (Table 1). Nearly two‐thirds of maternal deaths (6057) occurred in EAGA states, with Uttar Pradesh/Uttarakhand contributing about 22% (2059), followed by Bihar/Jharkhand, with 12% (1113). About 37% (3519) of all maternal deaths occurred in the other states, led by West Bengal and Karnataka (Table 2). The concentration of maternal deaths in EAGA states was substantially higher than the proportion of total live births in these states (44%).
Table 1.
Characteristics of maternal deaths and live births in the Sample Registration System, 1997–2018: sample age distribution of maternal deaths
| Period | 1997–2018 | 1997–1998 | 1999–2001 | 2001–2003 | 2004–2006 | 2007–2009 | 2010–2012 | 2011–2013 | 2014–2016 | 2015–2017 | 2016–2018 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Age (years) | n (%) | ||||||||||
| All ages | 9573 (100) | 1589 | 1512 | 1383 | 1110 | 926 | 767 | 718 | 556 | 525 | 487 |
| 15–19 | 897 (9) | 191 | 181 | 166 | 111 | 83 | 54 | 43 | 22 | 21 | 24 |
| 20–24 | 3062 (32) | 461 | 438 | 401 | 344 | 333 | 299 | 251 | 195 | 179 | 161 |
| 25–29 | 2455 (26) | 334 | 318 | 290 | 289 | 250 | 215 | 237 | 189 | 179 | 156 |
| 30–34 | 1731 (18) | 318 | 302 | 277 | 211 | 130 | 130 | 108 | 89 | 84 | 83 |
| 35–39 | 942 (10) | 191 | 181 | 166 | 100 | 83 | 54 | 57 | 39 | 37 | 34 |
| 40–44 | 357 (4) | 64 | 60 | 55 | 44 | 46 | 15 | 14 | 17 | 21 | 19 |
| 45–49 | 81 (1) | 16 | 15 | 14 | 11 | 9 | 0 | 0 | 6 | 5 | 5 |
| Missing | 48 (<1) | ||||||||||
Numbers may not add up because of rounding (%) in the SRS; 48 maternal deaths were missing age.
Table 2.
Characteristics of maternal deaths and live births in the Sample Registration System, 1997–2018: maternal deaths and live births distribution by major state and region, 1997–2018
| State/Region | n (%) | Live births, in millions (%) |
|---|---|---|
| India | 9573 (100) | 4.3 (100) |
| EAGA* | 6057 (63) | 1.9 (44) |
| Uttar Pradesh/Uttarakhand | 2059 (22) | 0.6 (13) |
| Bihar/Jharkhand | 1113 (12) | 0.4 (9) |
| Madhya Pradesh/Chhattisgarh | 905 (9) | 0.3 (8) |
| Rajasthan | 894 (9) | 0.3 (6) |
| Assam | 546 (6) | 0.1 (3) |
| Orissa | 540 (6) | 0.2 (5) |
| Other states | 3519 (37) | 2.4 (56) |
| West Bengal | 437 (5) | 0.3 (7) |
| Karnataka | 408 (4) | 0.2 (5) |
| Andhra Pradesh | 288 (3) | 0.2 (5) |
| Gujarat | 287 (3) | 0.2 (6) |
| Maharashtra | 233 (2) | 0.2 (5) |
| Haryana | 214 (2) | 0.2 (4) |
| Tamil Nadu | 213 (2) | 0.2 (5) |
| Punjab | 188 (2) | 0.1 (3) |
| Kerala | 131 (1) | 0.2 (4) |
| Remaining states | 1120 (12) | 0.6 (14) |
Numbers may not add up because of rounding in the SRS results published for each state. *EAGA is the Empowered Action Group states plus Assam.
The MMR per 100 000 live births fell over the study period by more than 70%, from 398 (95% CI 378–417) in 1997–1998 to 113 (95% CI 103–123) in 2016–2018 (Figure 1), with an average annual rate of decline of 6.3% (95%CI 5.6–7.0%). Projecting the observed decline for a further 2 years, we estimate an MMR of 99 (95% CI 90–108) by 2020. Overall, we estimate that about 1.30 million (95% CI 1.26–1.35) maternal deaths occurred in India between 1997 and 2020. The EAGA states accounted for 952 000 maternal deaths, whereas about 317 400 maternal deaths occurred in the other states. The number of maternal deaths fell from 110 800 (95% CI 105 200–116 100) in 1997 to an estimated 23 800 (95% CI 21 700–26 000) in 2020 (Table S1). The proportion of maternal deaths among deaths in women aged 15–49 years fell from about 12% to below 4% during this time period. The MMR declines were broadly consistent with the WHO model‐based estimates (Figure 1) and correlated with the expansion of the percentage of births occurring in facilities as well as the decline in neonatal mortality (Pearson correlations of 93% and 98%, respectively, each P < 0.0001; Table S2).
Figure 1.
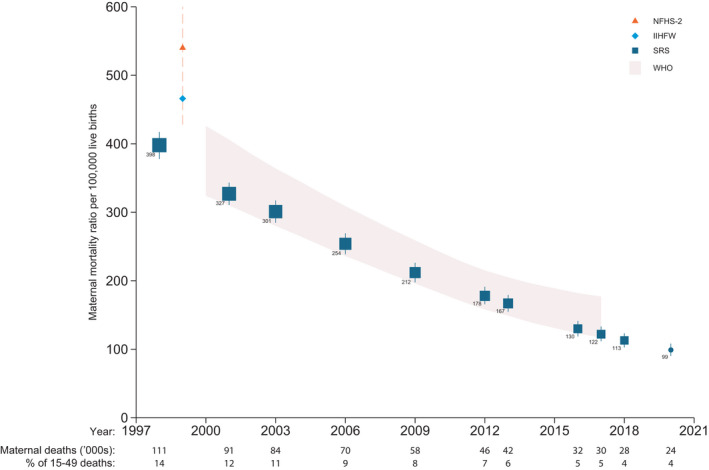
Trends in maternal mortality ratio (MMR) from 1998 to 2018 and projection for 2020 for India. Each year on the horizontal axis represents the last of each three‐year group for each MMR, except for 1998, which represents the second of two years. The pink bands represent the United Nations (UN)/World Health Organization (WHO) estimates. NFHS‐2 is the National Family Health Survey, 2nd round, and IIHFW is the Indian Institute of Health and Family Welfare survey. Absolute maternal deaths are scaled to the UN demographic totals for females at 15–49 years of age.
The percentage declines in MMR were similar in the EAGA states and in the other states (Figure 2), averaging 5.9% (95% CI 5.0–6.8%) in EAGA and 6.3% (95%CI 5.2–7.5%) in the other states. Projected MMRs per 100 000 live births for 2020 were 143 (95% CI 127–159) for the EAGA states and 68 (95% CI 58–77) for the other states. This amounts to 17 900 (95% CI 16 300–19 600) maternal deaths in the EAGA states and 5800 (95% CI 5300–6400) maternal deaths in the other states. The MMR in the EAGA states remained about twice as high as in the other states throughout the two decades. The proportion of deaths for maternal causes among females aged 15–49 years in the EAGA states fell from 20% in 1997 to about 7% in 2018. From 1997 to 2001, maternal deaths in Rajasthan accounted for nearly a third of all deaths in females aged 15–49 years (Table S1). The two states with the largest declines in MMRs were Bihar/Jharkhand (76%) and Maharashtra (72%), and the two states with the smallest declines were Haryana (33%) and Punjab (54%; Table S1).
Figure 2.
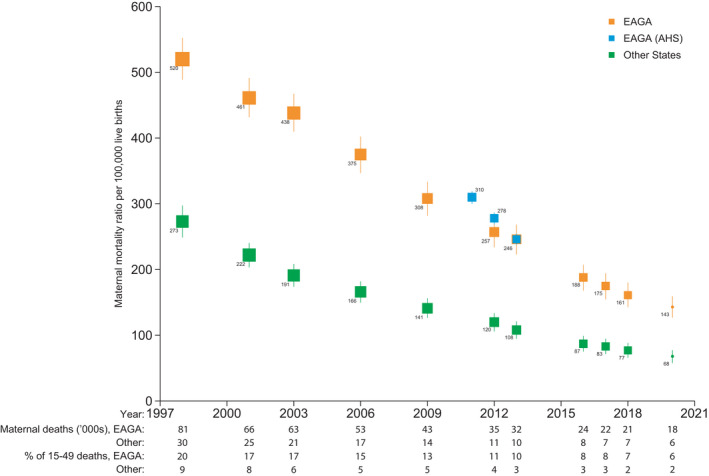
Trends in maternal mortality ratio from 1998 to 2018 and projection for 2020 for subnational regions of India. Each year on the horizontal axis represents the last of each three‐year group, except for 1998, which represents the last of two years. EAGA is the Empowered Action Group states plus Assam. Estimates for EAGA from the Annual Health Survey (AHS) data are for two‐year groups. Absolute maternal deaths are scaled to the United Nations demographic totals for females aged 15–49 years.
Between 2008 and 2011, three‐quarters of India’s maternal deaths identified in the MDS were clustered in rural areas of the EAGA states (Figure 3). After adjusting for female literacy, rural/urban status, smoking prevalence, language and spatial clustering effects, we noted particular ‘hotspots’ of higher risk‐adjusted maternal death rates in 2008–2011 (the period during which such analyses were possible) in central Uttar Pradesh, in Assam and in other north‐eastern states, and in the tribal areas that border Bihar, Madhya Pradesh and Chhattisgarh. During these years, over 22% of India’s estimated 26 million live births occurred in areas with a risk‐adjusted MMR of 70 or below, which is the SDG target for 2030. Over two‐thirds of births occurred in areas with a risk‐adjusted MMR ranging from 71 to 200, and 10% occurred in subareas with a risk‐adjusted MMR exceeding 201. The highest risk‐adjusted MMRs of ≥251 occurred in populations with only 0.7% of live births.
Figure 3.
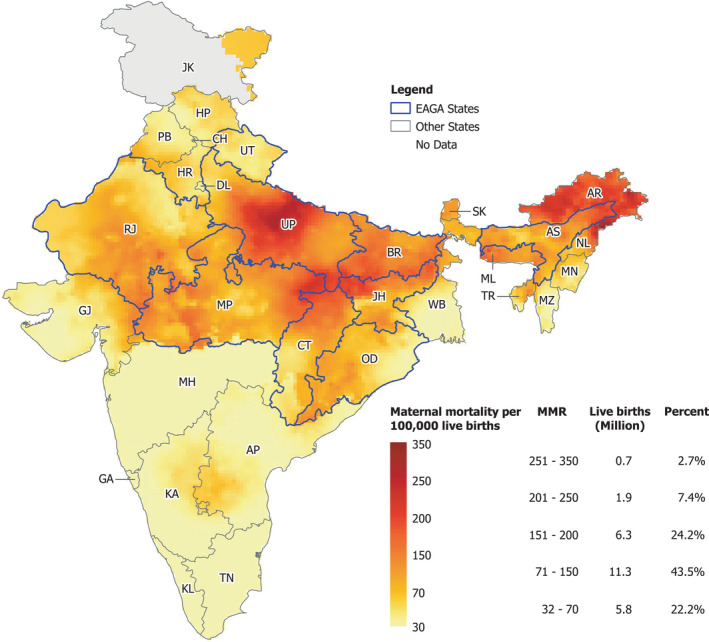
Spatial distribution of risk‐adjusted maternal mortality ratios (MMRs) in rural areas of India in 2008–2011. The risk of maternal death is adjusted for female literacy, rural/urban status, smoking prevalence, language and spatial clustering effects. States/union territories in India: AP, Andhra Pradesh; AR, Arunachal Pradesh; AS, Assam; BR, Bihar; CH, Chandigarh; CT, Chhattisgarh; DL, Delhi; GA, Goa; GJ, Gujarat; HR, Haryana; HP, Himachal Pradesh; JH, Jharkhand; JK, Jammu and Kashmir; KA, Karnataka; KL, Kerala; MP, Madhya Pradesh; MH, Maharashtra; MN, Manipur; ML, Meghalaya; MZ, Mizoram; NL, Nagaland; OR, Orissa; PB, Punjab; RJ, Rajasthan; SK, Sikkim; TN, Tamil Nadu; TR, Tripura; UL, Uttarakhand; UP, Uttar Pradesh; WB, West Bengal.
At the end of the study period, in 2016–2018, Assam had the highest MMR at 215, followed by Uttar Pradesh/Uttarakhand at 192. Maharashtra and Kerala had the lowest MMRs, at 46 and 43, respectively (Figure 4). Based on the trends in Figure 1, the MMRs for Assam and Uttar Pradesh/Uttarakhand were about 9 years behind the national ratios of 2016–2018, and Madhya Pradesh/Chhattisgarh was 6 years behind. Of the national total of 23 800 maternal deaths projected for 2020, Uttar Pradesh/Uttarakhand had 7600 maternal deaths, followed by Bihar/Jharkhand with 3500 and Madhya Pradesh/Chhattisgarh with 3100 (Table S1).
Figure 4.
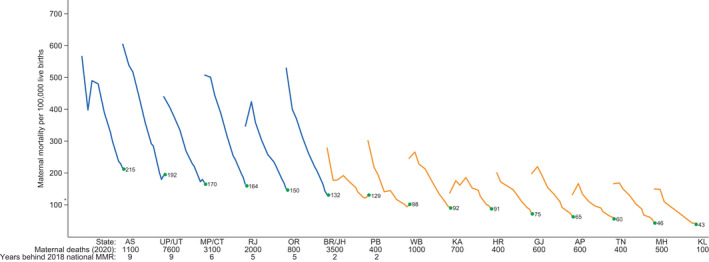
Trends in maternal mortality ratio (MMR) in major states (1998–2018) and estimated maternal deaths (2020). Each line starts in 1998 and ends in 2018. *National MMR. The number of years lagging behind the 2018 national MMR is derived from the trends in Figure 1. See Figure 3 for state abbreviations. The blue MMR trend lines represent trends in poorer states (the EAGA states).
At the current average rates of progress, we project that by 2030 India’s overall MMR will meet and exceed the UN SDG target, reaching an MMR of 52 (95% CI 47–56), based mostly on progress in the other states, which we project to reach an MMR of 35 (95% CI 30–40). By contrast, we project that the EAGA states will most likely not meet the SDG target, reaching an MMR of only 78 (95% CI 69–87). To examine the possible reported effects of the interruption of maternal services as a result of the COVID‐19 pandemic, 33 we posited that the MMR would remain unchanged for 2020 and 2021 and would then continue to decline at the previous rate of progress. In this scenario, by 2030 MMRs would reach 59 (95% CI 54–64) for India overall, 88 (95% CI 78–98) in the EAGA states and 40 (95% CI 34–46) in the other states.
A total of 1565 maternal deaths among 35 295 female deaths at ages 15–49 years recorded in the MDS from 2007 to 2014 were available for the analyses of cause of death. (The causes of maternal deaths from 2001 to 2003 have already been published. 34 ) These 2007–2014 deaths had similar age and regional distributions to the overall and periodic samples of maternal deaths in the SRS. The leading causes of death were obstetric haemorrhage (47%), pregnancy‐related infection (12%) and hypertensive disorders of pregnancy (7%) (Table 3). Nationally, obstetric haemorrhage caused about 11 200 (95% CI 10 600–11 900) maternal deaths in 2020, and pregnancy‐related infection caused 2800 (95% CI 2400–3300), hypertensive disorders caused 1600 (95% CI 1300–2000) and abortion (termination of pregnancy) caused 1200 (95% CI 900–1500) maternal deaths. The leading causes of maternal deaths were similarly distributed between the periods before (2007–2009) and after (2010–2013) the introduction of the National Health Mission, a national programme dedicated to improving maternal and child health outcomes. 35 , 36 Obstetric haemorrhage was the leading cause of maternal death in all states, but represented a notably higher proportion in Bihar, Uttar Pradesh and Uttarakhand than in Maharashtra, Tamil Nadu and Kerala (Figure 3, 5), where the proportion of maternal deaths linked to hypertensive disorders was higher. Based on the review of the verbal autopsy narrative section, 457 (29%) of 1565 maternal deaths had planned to give birth at home, and of these 139 (30%) died in a health facility or en route. Of the 727 deaths of women who planned to give birth at a facility, 568 (78%) died in a facility, 68 (9%) died at home and 57 (8%) died en route to the facility (Table 4). Overall, about half of the maternal deaths occurred in health facilities (51.4%), about a third occurred at home (30.2%) or en route to a health facility (8.4%), and for the remainder, the place of death was unknown (10.0%).
Table 3.
Causes of maternal death in the Million Death Study from 2007 to 2014, and projected national totals for 2020
| Cause of death (ICD‐10 codes) | Sample | Proportion (95% CI) | National totals in 2020 (95% CI) |
|---|---|---|---|
| Direct causes | |||
| Haemorrhage | 735 | 47.2 (44.4–50.0) | 11 200 (10 600–11 900) |
| (O44, O45, O46, O67, O72, O20, O71) | |||
| Pregnancy‐related infection | 183 | 12 (10.2–14.0) | 2800 (2400–3300) |
| (A34, O23, O41, O85, O86, O91) | |||
| Hypertensive disorders | 109 | 6.7 (5.4–8.2) | 1600 (1300–2000) |
| (O15, O10, O11, O12, O13, O14, O16) | |||
| Abortion | 78 | 4.9 (3.8–6.2) | 1200 (900–1500) |
| (O00, O01, O03, O04, O05, O06, O07) | |||
| Other Direct Causes | 313 | 19.6 (17.4–21.9) | 4700 (4100–5200) |
| (O26, O75, O90, O22, O87, O88, O24, X61–X76, F53, O21, O26) | |||
| Indirect causes | 147 | 9.8 (8.2–11.6) | 2300 (2000–2800) |
| (O98, A00/B99, O99, C00/N99, R00/R99) | |||
| Total | 1565 | 100 | 23 800 |
| (21 700–26 000) |
Sample proportions are weighted for sampling probability and national totals are rounded to the nearest hundred.
Figure 5.
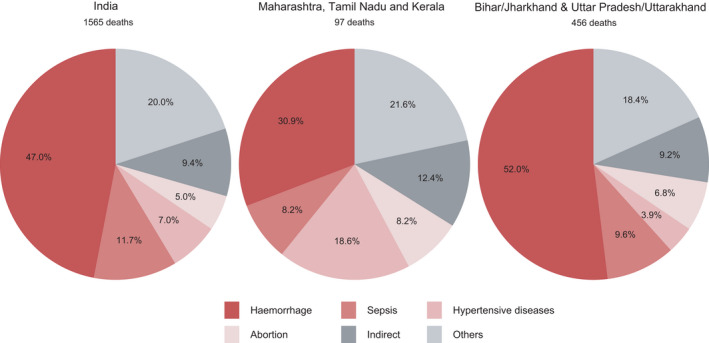
Causes of maternal death in India and in selected states, 2007–2014: sepsis (pregnancy‐related infections); others (other obstetric complications); HDP (hypertensive disorders of pregnancy).
Table 4.
Place of death by planned place of birth and location
| Place of death | |||||
|---|---|---|---|---|---|
| Health facility | Home | Unknown | En route | Total | |
| Planned place of birth (%) | |||||
| Health facility | 568 (78.1) | 68 (9.4) | 34 (4.7) | 57 (7.8) | 727 (100) |
| Home | 94 (20.6) | 273 (59.7) | 45 (9.8) | 45 (9.8) | 457 (100) |
| Unknown | 78 (35.3) | 52 (23.5) | 73 (33.0) | 18 (8.1) | 221 (100) |
| Complication occurred before the onset of labour | 65 (40.6) | 79 (49.4) | 4 (2.5) | 12 (7.5) | 160 (100) |
| Type of residence (%) | |||||
| Rural | 608 (48.6) | 398 (31.8) | 127 (10.2) | 117 (9.4) | 1250 (100) |
| Urban | 197 (62.5) | 74 (23.5) | 29 (9.2) | 15 (4.8) | 315 (100) |
| Region (%) | |||||
| EAGA | 445 (47.9) | 337 (36.2) | 58 (6.2) | 90 (9.7) | 930 (100) |
| Others | 360 (56.7) | 135 (21.3) | 98 (15.4) | 42 (6.6) | 635 (100) |
| Total | 805 | 472 | 156 | 132 | 1565 |
Proportions are row percentages.
Discussion
Main findings
This comprehensive documentation of nearly 10 000 maternal deaths using nationally representative data from India over a 20‐year period finds that maternal mortality has been substantial in India, totalling nearly 1.3 million deaths over this time period, but that MMRs have fallen by nearly 70% over the period. Although India fell short of the 2015 UN goal, it is likely to meet the 2030 goal of 70 or fewer maternal deaths per 100 000 live births. However, without further efforts in the poorest EAGA states – currently the location of over 60% of maternal deaths – India is unlikely to achieve the national goal of all states meeting the SDG. Indeed, these poorer states are particularly vulnerable to the disruption that the COVID‐19 pandemic might cause in the delivery of health services. Maternal deaths are concentrated in selected rural areas of Uttar Pradesh and Assam, and in tribal areas overlapping a few northern states, pointing to the need for focal intervention in these areas.
Strengths and limitations
Our analysis provides the largest study yet to document trends in maternal mortality in India. We use robust nationally representative survey data paired with geospatial analyses to show the marked variation in maternal death risk across the country. We demonstrate that the poorer states need to accelerate their rates of progress in reducing maternal mortality if the whole of India is to achieve the UN SDGs. Our analyses have some limitations, however. Maternal deaths remain a reasonably uncommon cause of death. Reliable measurement of trends requires large sample sizes. Indeed, NFHS surveys prior to 1997 showed increases in maternal mortality, but this was with fewer than 50 maternal deaths being available for analyses. 4 Hence, some of the state‐level estimates relying on small numbers of recorded deaths may be similarly unreliable. If the SRS had undercounted the overall number of female deaths at 15–49 years of age, we might have also undercounted the absolute maternal deaths (but less likely the MMR). However, independent demographic assessments find that the SRS has a high coverage of expected births, 37 but undercounts deaths in females older than 5 years by 8–11%. 38 , 39 , 40 We correct for this possible undercounting in absolute deaths by using the UN totals of deaths at 15–49 years of age, to which we apply the SRS proportions of deaths. The causes of death based on verbal autopsy are subject to misclassification. 25 However, we minimised such misclassification by having a central panel with at least two skilled obstetrical experts re‐review all maternal deaths. Overall, our analyses provide useful evidence to inform health policies and strategies for tackling maternal mortality in India.
Interpretation
The reductions in maternal deaths reflect successful initiatives by the government and stakeholders through the Child Survival and Safe Motherhood programme (1992), the Reproductive and Child Health Program (1997) and the National Health Mission (2005). 35 , 41 Our analyses reveal that MMR fell at a faster rate than neonatal mortality (in the first month of life), which is particularly sensitive to access to delivery in facilities. 24 , 42 However, although the reduced number of maternal deaths correlated with an expansion of the percentage of births occurring in facilities, driven mostly by the Janani Suraksha Yojana, a conditional cash transfer programme to increase deliveries in health facilities, maternal death declines did not accelerate after the introduction of this scheme. Our findings suggest that the quality of emergency obstetric care is a major driver of maternal mortality. Even planned facility births ended in a substantial proportion of deaths occurring at home or en route to facilities. Earlier analyses of maternal deaths by cause from 2001 to 2003 reached similar conclusions. 34 The high proportion of deaths occurring in facilities among women who planned to give birth in a health facility suggest unanticipated emergency obstetrical scenarios, particularly haemorrhage.
The leading cause of maternal death at the national and subnational level remains obstetric haemorrhage. 34 , 43 The proportion of deaths resulting from obstetric haemorrhage has increased in poorer states compared with 2001–2003 estimates, 34 suggesting that persistent underlying medical conditions, including severe anaemia, as well as delayed recognition and management, may exacerbate postpartum bleeding. 44 In rich states, hypertensive disorders of pregnancy caused a significant proportion of maternal deaths, highlighting a need to improve efforts to prevent, diagnose and treat this condition. Given the substantial interstate variations in maternal deaths, there may be a role for state‐specific maternal health interventions to reduce maternal mortality. 13 , 42 , 45
The COVID‐19 pandemic has the potential to reverse gains in maternal mortality in India by reducing access to antenatal care services and institutional births. However, representative national and regional level evidence on the impact on maternal mortality are lacking as data are still emerging. The effects of COVID‐19 on maternal health outcomes on health facilities in rural areas remain poorly understood. 46 , 47 Recent increases in maternal deaths reported to the national Health Management Information System were mostly linked to other/unknown causes, probably reflecting the effects of COVID‐19 infection among pregnant women. 47 It remains uncertain whether COVID‐19 effects have had an impact on maternal care prevention and treatment services, which would increase the MMR.
Conclusion
India has made great strides in implementing interventions that have improved maternal health in the country. However, attention is needed in three areas. First, we need policies that recognise and monitor the subnational disparities, particularly in the EAGA states and the rural and tribal areas, where the majority of maternal deaths occur (and which might be particularly affected by disruptions in delivery resulting from the COVID‐19 pandemic). 33 This argues for additional targeted efforts to improve access and address quality gaps in these hotspots. Second, educational programmes should inform women about the benefits of care and planned births at health facilities. Finally, for these areas and nationally a continuing reliable estimation of maternal deaths is needed, including ensuring that the SRS results on causes of death are published in a timely manner. Unfortunately, the last release of MDS mortality data was from 2014. Additional research in the EAGA states is required to identify the drivers of maternal mortality and effective interventions. By prioritising improvements in maternal health outcomes in the EAGA states, India can accelerate the overall decline in MMR and ensure that each state achieves the 2030 SDG goal and continues to improve beyond that date.
Disclosure of interests
None declared. Completed disclosure of interests form available to view online as supporting information.
Contribution to authorship
PJ conceived and developed the study idea and design. CM, AS, UR and SHF analysed the data. CM performed the literature review. NC, JWS, PS, RB, MS and PJ coded the causes. AS, PS, MS, TH and LR extracted data from the narratives. PJ and CM wrote the initial draft, and all authors revised and approved the final draft for publication.
Details of ethics approval
This study was approved by St. Michael’s Hospital Research Ethics Board (ref. no. REB 04‐268; 5 February 2004).
Funding
This study was supported by a Canadian Institutes of Health Research Foundation grant (FDN 154277). PJ is supported by a Canada Research Chair and Endowed Chair at the University of Toronto.
Acknowledgement
We thank Hellen Gelband for her helpful suggestions.
Data Availability Statement
Data, partially derived from public domain resources, are available on request from the authors.
Supporting information
Table S1. National and regional indicators for maternal mortality in India, 1997–2018.
Table S2. Proportions of maternal death and health facility births, 1997–2018.
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Meh C, Sharma A, Ram U, Fadel S, Correa N, Snelgrove JW, Shah P, Begum R, Shah M, Hana T, Fu SH, Raveendran L, Mishra B, Jha P. Trends in maternal mortality in India over two decades in nationally representative surveys. BJOG 2022; 10.1111/1471-0528.16888.129:550–561.
References
- 1. WHO . Strategies toward ending preventable maternal mortality (EPMM) [Internet]. Geneva, Switzerland: World Health Organization; 2015. [http://www.who.int/reproductivehealth/topics/maternal_perinatal/epmm/en/]. Accessed 24 September 2020. [Google Scholar]
- 2. Jha P. Reliable direct measurement of causes of death in low‐ and middle‐income countries. BMC Med 2014;12:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gomes M, Begum R, Sati P, Dikshit R, Gupta PC, Kumar R, et al. Nationwide mortality studies to quantify causes of death: relevant lessons from India's million death study. Health Aff 2017;36:1887–95. [DOI] [PubMed] [Google Scholar]
- 4. Registrar General India, Centre for Global Health Research . Maternal Mortality in India: 1997–2003 Trends, Causes and Risk Factors [Internet]. New Delhi, India: Registrar General India, Centre for Global Health Research; 2006. [http://www.cghr.org/wordpress/wp‐content/uploads/RGI‐CGHR‐Maternal‐Mortality‐in‐India‐1997–2003.pdf]. Accessed 21 November 2020. [Google Scholar]
- 5. WHO . Trends in Maternal Mortality 2000 to 2017: Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Geneva, Switzerland: World Health Organization; 2019. [Google Scholar]
- 6. Dhingra N, Jha P, Sharma VP, Cohen AA, Jotkar RM, Rodriguez PS, et al. Adult and child malaria mortality in India: a nationally representative mortality survey. Lancet 2010;376:1768–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Menon GR, Singh L, Sharma P, Yadav P, Sharma S, Kalaskar S, et al. National Burden Estimates of healthy life lost in India, 2017: an analysis using direct mortality data and indirect disability data. Lancet Glob Heal 2019;7:e1675–84. [DOI] [PubMed] [Google Scholar]
- 8. WHO . The WHO Application of ICD‐10 to Deaths during Pregnancy, Childbirth and the Puerperium: ICD‐MM. Geneva, Switzerland: WHO; 2012. [Google Scholar]
- 9. Office of the Registrar General & Census Commissioner India . Sample Registration System [Internet]. New Delhi, India: Office of the Registrar General & Census Commissioner India; 2020 [https://censusindia.gov.in/2011‐Common/Sample_Registration_System.html]. Accessed October 19 2020. [Google Scholar]
- 10. Office of the Registrar General India . Sample Registration [Internet]. Office of the Registrar General India ; 2021. [New Delhi, India: https://censusindia.gov.in/Vital_Statistics/SRS/Sample_Registration_System.html]. Accessed July 11 2021. [Google Scholar]
- 11. Office of the Registrar General India . SRS Bulletin Sample Registration System Office of the Registrar General, India. New Delhi, India: Office of the Registrar General India; 2020. [https://censusindia.gov.in/vital_statistics/SRS_Bulletins/SRSBulletin_2018.pdf]. Accessed 10 July 2021. [Google Scholar]
- 12. IIPS . National Family Health Survey (NFHS‐2), 1998‐99. Mumbai, India: International Institute for Population Sciences (IIPS) and ORC Macro; 2000. [Google Scholar]
- 13. Vora KS, Mavalankar DV, Ramani KV, Upadhyaya M, Sharma B, Iyengar S, et al. Maternal health situation in India: a case study. J Heal Popul Nutr 2009;27:184–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. WHO . Maternal Mortality ‐ Estimates by Country [Internet]. Geneva, Switzerland: Global Health Observatory Data Repository; 2016. [https://apps.who.int/gho/data/view.main.1390]. Accessed 19 October 2020. [Google Scholar]
- 15. Office of the Registrar General and Census Commissioner India . Annual Health Survey. Bulletins 2010–11 [Internet]. New Delhi, India: Office of the Registrar General and Census Commissioner India; 2011. [https://www.censusindia.gov.in/vital_statistics/AHSBulletins/ahs.html]. Accessed 19 October 2020. [Google Scholar]
- 16. Office of the Registrar General and Census Commissioner India . Annual Health Survey. Bulletins 2011–12 [Internet]. New Delhi, India: Office of the Registrar General and Census Commissioner India; 2012. [https://www.censusindia.gov.in/vital_statistics/AHSBulletins/ahs2011.html. Accessed 19 October 2020. [Google Scholar]
- 17. Office of the Registrar General and Census Commissioner India . Annual Health Survey(AHS) 2nd Updation. Bulletins 2012–2013 [Internet]. New Delhi, India: Office of the Registrar General and Census Commissioner India; 2013. [https://www.censusindia.gov.in/vital_statistics/AHSBulletins/AHS_2nd_Updation_Bulletins.html]. Accessed 19 October 2020. [Google Scholar]
- 18. Collaborators for the Million Death Study . Causes of neonatal and child mortality in India: a nationally representative mortality survey. Lancet 2010;376:1853–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jha P, Gajalakshmi V, Gupta PC, Kumar R, Mony P, Dhingra N, et al. Prospective study of one million deaths in India: rationale, design, and validation results. Avila MH, editor. PLoS Med 2005;3:e18. 10.1371/journal.pmed.0030018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. RGI‐CGHR . Prospective study of Million Deaths in India: Technical Document No VIII: Health Care Professional's Manual for Assigning Causes of Death Based on RHIME Household Reports [Internet]. New Delhi, India: RGI‐CGHR; 2011. [http://www.cghr.org:8080/cme2‐training/reference/MDS_manual.pdf]. Accessed 30 November 2020. [Google Scholar]
- 21. WHO . International Statistical Classification of Diseases and Related Health Problems 10th Revision [Internet]. Geneva, Switzerland: WHO; 2011. [www.who.int]. Accessed 19 October 2020. [Google Scholar]
- 22. World Health Organization . The WHO Application of ICD‐10 to Deaths during Pregnancy, Childbirth and the Puerperium: ICD‐MM. Geneva, Switzerland: WHO Library. 2012. [Google Scholar]
- 23. Montgomery AL, Morris SK, Kumar R, Jotkar R, Mony P, Bassani DG, et al. Capturing the context of maternal deaths from verbal autopsies: a reliability study of the maternal data extraction tool (M‐DET). PLoS One 2011;6:e14637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Fadel SA, Rasaily R, Awasthi S, Begum R, Black RE, Gelband H, et al. Changes in cause‐specific neonatal and 1–59‐month child mortality in India from 2000 to 2015: a nationally representative survey. Lancet 2017;390:1972–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Aleksandrowicz L, Malhotra V, Dikshit R, Gupta PC, Kumar R, Sheth J, et al. Performance criteria for verbal autopsy‐based systems to estimate national causes of death: development and application to the Indian Million Death Study. BMC Med 2014;12:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. WHO . Maternal Mortality Ratio (per 100 000 Live Births) [Internet]. Geneva, Switzerland: WHO; 2021. [https://www.who.int/data/gho/indicator‐metadata‐registry/imr‐details/26]. Accessed 7 February 2021 [Google Scholar]
- 27. Miller R. Survival Analysis, 2nd edn. New York, USA: John Wiley & Sons, Ltd; 2011. [Google Scholar]
- 28. UN Economic & Social Affairs . World Population Prospects 2019 [Internet]. New York, USA: Department of Economic and Social Affairs. World Population Prospects 2019. 2019. [https://population.un.org/wpp/Download/Standard/Population/]. [Google Scholar]
- 29. Gerland P. UN population division's methodology in preparing base population for projections: case study for India. Asian Popul Stud 2014;10:274–303. [Google Scholar]
- 30. Brown PE. Model‐based geostatistics the easy way. J Stat Softw 2015;63 (12):1–24. [Google Scholar]
- 31. Brown P, Izawa Y, Balakrishnan K, Fu SH. Mortality from Particulate Matter 2.5 in India: National Retrospective Cohort Study. Environmental Health Perspectives (in press). [Google Scholar]
- 32. Suraweera W, Warrell D, Whitaker R, Menon G, Rodrigues R, Fu SH, et al. Trends in snakebite deaths in India from 2000 to 2019 in a nationally representative mortality study. Elife 2020;9:e54076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kumari V, Mehta K, Choudhary R. COVID‐19 outbreak and decreased hospitalisation of pregnant women in labour. The Lancet Global Health 2020;8:e1116–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Montgomery AL, Ram U, Kumar R, Jha P. Maternal mortality in India: causes and healthcare service use based on a nationally representative survey. PLoS One 2014;9:e83331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Akseer N, Kamali M, Arifeen SE, Malik A, Bhatti Z, Thacker N, et al. Progress in maternal and child health: how has South Asia fared? BMJ 2017;357:j1608. [DOI] [PubMed] [Google Scholar]
- 36. Jha P & Laxminarayan R. Choosing Health: An entitlement for all Indians [Internet]. New Delhi, India. 2009 [http://www.cghr.org/wp‐content/uploads/2011/06/Choosing‐Health‐report‐FINAL.pdf]. Accessed 27 November 2020.
- 37. Yadav AK, Ram F. Assessment of completeness of birth registrations (5+) by sample registration system (SRS) of India and major states. Demogr India 2015;44 (1&2):111–8. [Google Scholar]
- 38. Fadel SA, Boschi‐Pinto C, Yu S, Reynales‐Shigematsu LM, Menon GR, Newcombe L, et al. Trends in cause‐specific mortality among children aged 5–14 years from 2005 to 2016 in India, China, Brazil, and Mexico: an analysis of nationally representative mortality studies. Lancet 2019;393:1119–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Yadav AK, Ram F. There is a glaring gender bias in death registrations in India. Economic & Political Weekly 2019;54 (51): 1–6. [Google Scholar]
- 40. Bhat PNM. Completeness of India's sample registration system: An assessment using the general growth balance method. Popul Stud (NY) 2002;56:119–34 [DOI] [PubMed] [Google Scholar]
- 41. Shah P, Shah S, Kutty RV, Modi D. Changing epidemiology of maternal mortality in rural India: time to reset strategies for MDG‐5. Trop Med Int Heal 2014;19:568–75. 10.1111/tmi.12282 [DOI] [PubMed] [Google Scholar]
- 42. Horwood G, Opondo C, Choudhury SS, Rani A, Nair M. Risk factors for maternal mortality among 1.9 million women in nine empowered action group states in India: secondary analysis of Annual Health Survey data. BMJ Open 2020;10:e038910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Gupta SD, Khanna A, Gupta R, Sharma NK, Sharma ND. Maternal mortality ratio and predictors of maternal deaths in selected desert districts in Rajasthan. A community‐based survey and case control study. Women's Heal Issues 2010;20:80–5. [DOI] [PubMed] [Google Scholar]
- 44. Parks S, Hoffman MK, Goudar SS, Patel A, Saleem S, Ali SA, et al. Maternal anaemia and maternal, fetal, and neonatal outcomes in a prospective cohort study in India and Pakistan. BJOG An Int J Obstet Gynaecol 2019;126:737–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Kumar S. Reducing maternal mortality in India: policy, equity, and quality issues. Indian J Public Health 2010;54:57. [DOI] [PubMed] [Google Scholar]
- 46. Chmielewska B, Barratt I, Townsend R, Kalafat E, van der Meulen J, Gurol‐Urganci I, et al. Effects of the COVID‐19 pandemic on maternal and perinatal outcomes: a systematic review and meta‐analysis. Lancet Glob Heal 2021;9 (6):e759–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.S R. Deaths by ‘Unknown Causes’ On National Health Mission Portal 2X Official Covid Toll [Internet]. Mumbai, India. 2021 [https://www.indiaspend.com/covid‐19/deaths‐unknown‐causes‐national‐health‐mission‐portal‐covid‐toll‐760219]. Accessed 14 July 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. National and regional indicators for maternal mortality in India, 1997–2018.
Table S2. Proportions of maternal death and health facility births, 1997–2018.
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Data Availability Statement
Data, partially derived from public domain resources, are available on request from the authors.


