Abstract
The COVID‐19 pandemic has placed considerable strain on healthcare workers showing high rates of stress and psychological health problems. Interventions are urgently needed to help healthcare workers perform under conditions of great risk and uncertainty. In particular, healthcare leadership is known to be critical to supporting healthcare workers to deal with an uncertain and distressing healthcare environment. This pilot study evaluated the impact of the R2 resilience program tailored for healthcare leaders working in a highly affected COVID‐19 area in Italy. Through two group cohorts, 21 healthcare leaders completed the intervention, with 17 participants providing pre‐ and post‐intervention assessment data. Sixty‐two staff members who benefitted from their coordinators' resilience‐focused leadership were also included in the study. Findings show that participation in R2 was associated with reduction in levels of perceived stress and burnout symptoms, and increases in rugged qualities, self‐efficacy and in social‐ecological resilience. Significant changes in rugged qualities, self‐efficacy and perceived stress were also detected in staff members. High rates of participants' program satisfaction have been detected. R2 is a promising intervention for healthcare professionals working in emergency settings designed to enhance the rugged qualities and resources required to deal with heightened exposure to stress.
Keywords: COVID‐19, healthcare workers, intervention, pandemic, R2 resilience program, resilience
1. INTRODUCTION
Originating as a cluster of unexplained cases of pneumonia in Wuhan, China, novel coronavirus disease – officially designated as COVID‐19 by the World Health Organization – has reached the level of a pandemic, affecting countries all around the world. To date (18th May 2021), 163,312,429 confirmed cases and 3,386,825 deaths attributable to this disease have been reported. Italy recorded 4.111.110 cases, representing one of the most affected countries worldwide with 122.833 deaths caused by COVID‐19. In particular, the region of Lombardy was the hardest hit by the virus, recording 826,762, almost one‐fourth of all coronavirus cases in the country, and 33,391 deaths (Ministero della Salute, 2021).
Studies conducted in Italy during the first COVID‐19 wave showed an average of 12% of all confirmed cases of COVID‐19 among healthcare workers, in line with other countries (International Council of Nurses (ICN), 2020; Sabetian et al., 2021). The INAIL report of 30 September 2020 (INAIL, 2020) showed that 70.3% (around 38,052 cases) out of 54,128 complaints about COVID‐19, concerned the ‘Health and Social Assistance’ sector. The most affected professionals were ‘health technicians’ such as nurses, midwives and professional educators (39.2% of the total cases), followed by qualified professions in health and social services (social health workers) (20%) and social assistance operators (careers) (8.9% of cases). To date (May, 2021), 122.717 responding health‐care workers have been infected, and 288 have died (Task Force COVID‐19, Dipartimento Malattie Infettive e Servizio di Informatica, 2021). In the wake of this global health crisis, stringent public health measures have been implemented to curtail the spread of COVID‐19 (Adhikari et al., 2020).
Widespread outbreaks of infectious disease, such as COVID‐19, are associated with psychological distress and symptoms of mental illness (Bao et al., 2020). In particular, healthcare workers are considered at higher risk of adverse mental health outcomes for several reasons: caring for COVID‐19 infected patients has meant shortages of protective equipment, long working hours, isolation from family, physical fatigue, and the pain of losing patients and colleagues (Kang et al., 2020). Specifically, healthcare workers who care for elderly parents or young children are affected by school closures, social distancing policies, in addition to physical and mental exhaustion and the fear of passing the infection to family members (The Lancet, 2020). Studies conducted in Italy showed that both frontline health‐care workers in Covid‐19 wards (Magnavita, Soave, et al., 2020) and staff from a local health unit (Magnavita, Tripepi, et al., 2020) developed high levels of stress, sleep disturbances, anxiety and depression, posttraumatic stress symptoms (Babore et al., 2020; Di Tella et al., 2020; Lasalvia, Bonetto et al., 2021) emotional burnout, relevant work‐related psychological pressure and somatic symptoms (Barello et al., 2020a, 2020b; Lasalvia, Amaddeo, et al., 2021). Similarly, previous studies conducted during the previous SARS pandemic found up to 50% of healthcare workers reporting acute psychological distress, burnout and posttraumatic stress while caring for their patients (Tam et al., 2004). These patterns suggest a critical need for healthcare organizations to support the mental health of their staff and maximize their resilience if they are to provide safe and effective care to their patients under challenging conditions (Adams & Walls, 2020; Banerjee, 2020; Dewey et al., 2020; Shanafelt et al., 2020).
Resilience is the ability to find and make use of internal and external resources to successfully cope when there has been exposure to risk or adversity (Cesana et al., 2018; Giordano, Cipolla, et al., 2019; Giordano & Ferrari, 2018; Ungar, 2008). Protective factors include individual assets (characteristics such as mastery, coping skills and self‐efficacy) (Ostafin & Proulx, 2020), as well as external resources such as personal and professional relationships (Giordano et al., 2020; Pipe et al., 2012) and a safe work environment. Resilience can, therefore, be considered a process that unfolds over time in the context of person–environment interactions (Egeland et al.,1993). This perspective suggests that it is a malleable process, and as such it is suitable for intervention (Giordano, Ragnoli & Brajda, 2019; Giordano, Ragnoli, Brajda et al., 2019; Giordano & Ungar, 2021). Recently, there has been interest in the development and evaluation of resilience building programs for healthcare workers (Grant et al., 2009), including populations like nurses in an oncology inpatient hospital unit (Pipe et al., 2012) and physicians at a tertiary care medical centre (Sood et al., 2011). Results from these program evaluations have shown that resilience‐promoting intervention protocols can yield adaptive changes such as reductions in stress, depression, anxiety and increased self‐efficacy.
While these programs have supported frontline staff to deal with workplace stressors, healthcare leadership (defined as the ability of supervisors to effectively and ethically influence others for the benefit of individual patients or populations as a whole [Hargett et al., 2017]) is known to be critical to supporting healthcare workers who must deal with an uncertain and distressing healthcare environment (Nicola et al., 2020). Shingler‐Nace (2020), for example, identifies five factors for successful leadership during the COVID‐19 pandemic: remaining calm, good communication, collaboration, coordination and providing psychosocial support to staff. In particular, having compassionate, open and highly communicative leaders may foster a sense of purpose that can act to strengthen a unified health approach among healthcare providers (Nicola et al., 2020). For healthcare workers dealing with COVID‐19, healthcare organization leaders that are reassuring and acknowledge their staffs' contributions are likely to be experienced as the most supportive (Howatt & Bradley, 2018; Pearce, 2020) with the potential for reinforcing social bonds, between colleagues and supervisors (Tam et al., 2004). Indeed, while healthcare workers may be inadequately prepared to cope with the stress caused by a serious public health crisis (Healy & Tyrrell, 2011), a positive attitude in the workplace which is modelled by supervisors has been found to reduce staff stress (Cai et al., 2020; Khalid et al., 2016), increase employee self‐efficacy and improve overall psychological wellbeing (Flesia et al., 2020; Proches, 2020). However, a recent study conducted in Italy during the COVID‐19 pandemic shows that an intrusive leadership style can trigger occupational stress, anxiety and depression in workers (Magnavita et al., 2021).
While some Western countries have incorporated psychological interventions into their protocols for managing disease outbreaks, this has not yet been the case in Italy, leading to the emergence and persistence of stress‐related disorders among healthcare workers. Furthermore, even when present, most interventions to support healthcare workers deal with pandemics have not yet been tested. The current study addresses this critical gap by evaluating the pilot implementation of a resilience curriculum for healthcare leaders dealing with the COVID‐19 pandemic, with the goal of improving psychological health and enhancing individual and work team resilience.
1.1. ‘R2 for leaders’ curriculum
The ‘R2 for Leaders’ program (www.resilienceresearch.org/R2) is an evidence‐informed resilience promoting curriculum for organization, business and educational institutions, built on promising practices that have been shown to enhance wellbeing among individuals experiencing stress and adversity. It integrates the principles of a social ecological approach to resilience developed by Dr. Michael Ungar and the Resilience Research Centre (RRC, n.d.) team at Dalhousie University (Halifax, Canada). The current adaptation of R2 is aimed at healthcare leaders and has the following goals:
Increase organizational capacity to build a resilient organization through a deeper understanding of individual ‘rugged’ qualities and external ‘resources’ (the two ‘R's’);
Help leaders integrate qualities of resilience into their organization's prevention programs including policies, procedures and the types of resources offered to workers;
Utilize a methodology to design programs that build resilience which are contextually specific.
As shown in Figure 1, the R2 model conceptualizes resilience as a process, shaped by key protective factors that help buffer against adversity. In particular, the impact of specific stressful life events and other daily hassles on the mental health and wellbeing of individuals is influenced by the interaction of two categories of resilience qualities: rugged qualities which are gratitude, self‐confidence, optimism, problem‐solving, mindfulness, sleep, nutrition and physical activity and resources which include structure, accountability, supportive relationships, a powerful identity, experiences of control, fair treatment, culture and the meeting of basic needs. Both sets of resilience factors were originally selected from a list of 52 well‐researched aspects of resilience which were identified through a scoping review conducted by the RRC. A two‐phase Delphi process with healthcare leaders in Canada narrowed the list to the 16 factors which became the focus of this version of the R2 program.
FIGURE 1.
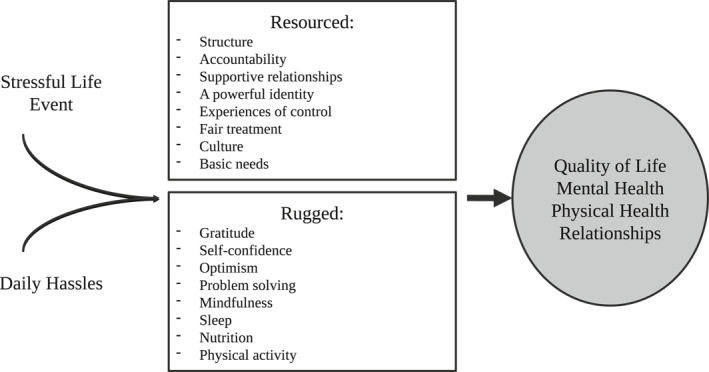
The R2 model
1.2. R2 for healthcare leaders
The Resilience Research Unit of the Catholic University of Milan, with the support of the RRC, adapted the Canadian version of R2 for Healthcare Leaders to the challenges facing service providers during the pandemic. Healthcare organizations had identified a need for professional development to deal with heightened stress in the workplace. Under normal circumstances, healthcare workers could seek release from workplace stress by spending more time with family or participating in social activities, both of which have been hampered by COVID‐19. Staff burnout from emotional distress has been reported anecdotally as a concern of healthcare leaders.
R2 follows a multisystemic resilience‐oriented approach, which normalizes and contextualizes both personal and work‐related stress, strengthens personal and organizational resources (i.e., making people more rugged and better resourced) for both individual and collective recovery, mobilizes self‐efficacy for ongoing adjustment and reduces exposure to the risk factors associated with burnout. In particular, the program focuses on enhancing and developing leadership capability in healthcare leaders, with the aim of equipping them to better lead their staff and their organizations more effectively during the pandemic. Specifically, the program aimed to help participants to:
Identify practices that support organizational and healthcare workers resilience;
Learn how to help staff navigate to, and negotiate for, resources in order to support mental health and wellbeing inside and outside the workplace;
Implement a methodology to build a resilience‐based prevention program.
Among the key protective factors considered in the R2 curriculum are 10 aspects of resilience which appear in the empirical literature on resilience in emergency settings (Cohen & McKay, 1984; Crane et al., 2020; Cutrona & Russell, 1988; Frink & Klimoski, 2004; Giordano et al., 2015; Kashdan & Rottenberg, 2010; Neimeyer, 2001; Shanafelt et al., 2020; Walsh, 2007) and a needs analysis conducted before the start of training. The 10 resilience factors include: (1) Gratitude and positive outlook, (2) Self‐confidence, (3) Flexibility, (4) Meaning making, (5) Mindfulness and self‐care, (6) Structure, (7) Accountability, (8) Supportive relationships, (9) A powerful identity and (10) Culture (see Table 1 for details). Indeed, the R2 program selects the rugged qualities and resources most likely to build resilience in a particular setting, ensuring the program is theoretically sound and matches the risks individuals experience. Within each session, the content, examples, group activities, and in‐session practice opportunities have been tailored for healthcare leaders dealing with COVID‐19. For example, in the ‘Culture’ session participants were invited to draw a symbol that represents the mission of the organization they belong to, and to reflect on how their collective mission has helped or hindered their capacity to deal with the pandemic. In the ‘Gratitude and positive outlook’ session, leaders were invited to propose to their team members their own ‘Gratitude journal’, writing down each day/week three things they felt grateful for and, if they wished, to share one of them with another team member.
TABLE 1.
R2 Resilience factors covered by the core curriculum
| Resilience resource | Impact in emergency contexts | Session content | Key messages |
|---|---|---|---|
| Gratitude and positive outlook | Gratitude supports resilience in emergency by helping individuals be content and focused and enabling their ability to deal with stress and challenges. In times of deepest despair, resilience involves ‘mastering the possible’, and acquiring a positive outlook on the future. |
|
|
| Self‐confidence | Self‐confidence supports resilience in emergency settings by generating feelings of kindness and care towards ourselves and by protecting individuals against damaging social comparisons, self‐conscious and rumination. |
|
|
| Flexibility | In emergency settings, flexibility is needed to learn how to deal with unforeseen challenges, reallocate roles and adapt to changed conditions. |
|
|
| Meaning making | Meaning reconstruction is considered a central process in healing following catastrophic events to gain perspective on experiences, make them more bearable and restore life purpose. |
|
|
| Mindfulness and self‐care | In emergency settings, both resources support resilience by allowing individuals to gain a greater knowledge of what is going on inside and around them and helping them to reconnect with what matters to them. |
|
|
| Structure | In emergency settings, structure supports resilience by acting as a buffer to chaos and reducing uncertainty and ambiguity in carrying out tasks and restores order, safety and stability. |
|
|
| Accountability | Accountability supports resilience in emergency settings by helping individuals to recognize the importance of duties and responsibilities in order to avoid unwanted consequences. |
|
|
| Supportive relationships | Supportive relationships enhance resilience in emergency settings by providing individuals with the support they need to work through stress and hardship, including emotional sustenance, self‐esteem building, provision of information and feedback, and tangible assistance. |
|
|
| A powerful identity | In emergency settings, a powerful identity supports resilience by reminding individuals of their strengths and enhancing personal and social agency. |
|
|
| Culture | In emergency settings, culture affects organizational resilience by grounding and orienting individuals, providing them with a sense of coherence and with foundations for collaborative learning and creative decision‐making. |
|
|
In this paper, we illustrate the pilot implementation of the R2 program with healthcare leaders working in the province of Bergamo – the part of Italy which has registered the highest number of cases in the country (Statista Research Department, 2020). We undertook this intervention as a first step towards investigating whether the R2 program can be employed as a resilience promoting curriculum for healthcare professionals in emergency settings. Here, we describe the Phase 1 pilot implementation of R2 conducted with healthcare leaders. Two questions are addressed by this intervention study:
Can R2 improve psychological adjustment among the healthcare leaders taking the program?
Can R2 enhance psychological adjustment and resilience resources among healthcare professionals belonging to the teams of the healthcare leaders who participate in the R2 program?
2. METHODS
2.1. Study design and procedure
A single group quasi‐experimental pretest ‐posttest design was employed in the study, with outcome measures assessed before and after the 12‐week R2 period. The baseline administration took place 1 week before the beginning of the program in April 2020, while the second administration was conducted in July 2020, 1 week after the end of the program.
This study is related to a COVID‐19 emergency program run by RiRes and the Italian NGO Cooperazione e Sviluppo (CESVI) in partnership with a cooperative which supports social and community enterprises working in Bergamo in the healthcare sector. Information about the R2 training was distributed to the cooperative's healthcare leaders through executives. Participation in the study was voluntary. Interested leaders were invited to take part in an e‐meeting facilitated by members of RiRes who explained the R2 12‐session training program and the monitoring study. Attendees were informed that their participation in the R2 program was not dependent upon their participation in the study. Healthcare leaders who opted to participate in the study completed a pre‐training assessment via the web (Qualtrics), which included an informed consent process and a battery of self‐report measures assessing psychological health and resilience.
Healthcare leaders were invited to inform their staff members of their participation in the R2 program and its monitoring study and to invite them to take part to the survey, as indirect beneficiaries of the R2 program. Staff who consented were sent a web link to a survey before the start of the leaders' training and at the end of it. The staff members' participation was voluntary. The inclusion criterion was employment with the cooperative, and membership on a team coordinated by a leader who took part in the R2 program.
2.2. Participants
Participants for this pilot study were healthcare professionals drawn from a social and community enterprise specialized in providing healthcare services, education and social assistance to elderly people and at‐risk minors and mothers through homecare and day care assistance, social housing services and residential centres in the province of Bergamo.
Twenty‐one healthcare leaders were enrolled in the program which was implemented in two parallel group cycles: one with elderly care leaders and the other one with child protection and childcare coordinators. Two participants dropped out after attending the first two needs analysis meetings because of scheduling conflicts. Of the remaining 19 participants, 17 completed both the pre‐ and the post‐R2 program assessments. In comparing participants who completed the pre‐post protocols to those who did not, there were no differences in demographic variables, deployment experiences, outcome measures or number of group sessions attended (at least 85% for both groups).
Healthcare leaders invited all their staff members to take part in a separate survey to see if they indirectly benefitted from the resilience‐focused approach and techniques shown to their leaders. Thus, the final study population consisted of 17 leaders and 62 members of their staff, reporting a mean of 12.11 years of experience in the healthcare field. Among the respondents to the survey, 8 leaders and 49 healthcare workers were involved in elderly care and 9 leaders and 13 healthcare workers were involved in child protection and childcare services. Tables 2 and 3 summarize the descriptive statistics of the sample. More women (84.8%) than men participated. Participants reported a range of ‘Patients with Confirmed or Possible COVID‐19 Infection’ between 0 and 50 (M = 3.31).
TABLE 2.
Descriptive statistics – healthcare leaders
| Demographic data | Professional information | ||
|---|---|---|---|
| Age | Team | ||
| 20–30 years | 17.6% | Child Protection | 47.1% |
| 31–40 years | 29.4% | Elderly care | 52.9% |
| 41–50 years | 47.1% | ||
| 51–65 years | 5.9% | ||
| Gender | |||
| Female | 82.4% | ||
| Male | 17.6% | ||
TABLE 3.
Descriptive statistics – staff members
| Demographic data | Professional information | ||
|---|---|---|---|
| Age | Team | ||
| 20–30 years: | 12.9% | Child Protection | 21% |
| 31–40 years: | 22.6% | Elderly care | 79% |
| 41–50 years | 35.5% | Role | |
| 51–65 years | 29.1% | Coordinator | 21.5% (N = 17) |
| Nurse | 14.5% (N = 9) | ||
| Gender | Care Assistant | 41.9% (N = 26) | |
| Female | 85.5% | Family Assistant | 14.5% (N = 9) |
| Male | 14.5% | Volunteer | 4.8% (N = 3) |
| Educator | 24.2% (N = 15) | ||
| Total | 100% (N = 62) | ||
2.3. Intervention
The R2 program was delivered online using the Microsoft TEAMS platform, with two different parallel cycles involving two separate groups of healthcare leaders: the first with 9 elderly care leaders and the other with 12 child protection and childcare leaders. The curriculum began for both groups in April 2020, soon after the World Health Organization declared COVID‐19 a public health emergency. Both group cycles were implemented in 12 two‐hour weekly sessions over 3 months. The program was divided into two stages: the needs analysis, conducted during two two‐hour group remote meetings, followed by 10 R2 remote sessions.
2.3.1. Needs assessment
To initiate the R2 program, a needs analysis was conducted with participants to define the psychosocial needs of healthcare professionals dealing with a pandemic. Trainees were polled on the most relevant protective factors and processes that could support beneficiaries in dealing with COVID‐19 challenges (Shanafelt et al., 2020). A specific tool – Caught in a Thunderstorm (Castelli, 2013) – was used to do this. The risks/challenges/fears that trainees identify were written inside pictures of clouds drawn at the top of pieces of paper. For each cloud, trainees explained in both written form and through group discussion what and/or who has helped them deal with perceived barriers to wellbeing. These resources were then drawn as umbrellas at the bottom of the page. A process of personal reflection and small group and whole group reporting ensured that consensus was reached on the most important challenges and sources of resilience, much as a Delphi process (Brown, 1968) encourages stakeholders to prioritize issues in a community.
The main risks detected by participants were sadness, loneliness and relational distance, feelings of uncertainty and unpredictability, powerlessness and ineffectiveness, fear of collective selfishness and difficulties accepting the current situation. The main protective factors were peer and intimate relationships, personal skills, sense of personal agency, optimism and hope for the future, making meaning of personal and social experiences, organizational culture, mindfulness and flexibility. These protective factors oriented the selection of the exercises chosen to build resilience resources that were included as content for the 10 R2 sessions that followed the initial needs assessment process.
2.3.2. The R2 sessions
Ten 2‐h web sessions were conducted with participants. Each session was focused on one of the participants' self‐identified protective factors. Each session had five parts:
An initial supervision on the support healthcare leaders managed to provide to their teams during remote staff meetings, based on the previous R2 sessions;
A group reflection triggered by a selected video, a narration or photo, aimed at identifying whether and in which way the target resources have been a source of resilience in their own recovery process and for their team members;
Tailored workshops conducted during the sessions to facilitate self‐expression, shared meaning making and mastery of both suffering and resilience;
A group discussion in which healthcare leaders proposed different ways to introduce the target resource in the staff meetings (with consideration to time limitations);
Lessons learnt from the session.
2.3.3. Evaluation of outcomes
Healthcare leaders and their staff were assessed before the program began (T1) and at the end (T2) to assess change in mental health and wellbeing, resilience resources and work‐related stress. We hypothesized that participation in R2 would be associated with a significant increase in the positive outcomes of rugged resilience, resourced resilience and self‐efficacy and a significant decrease in general stress, work‐related stress and burnout symptoms, in both healthcare leaders and their staff members.
2.4. Measures
Demographics items included age, gender, service type, position, years of service at the current place of employment and number of Patients with Confirmed or Possible COVID‐19 Infection.
Program satisfaction was assessed using a pre‐ and post‐assessment questionnaire with a 3‐point Likert scale with participants at the end of the R2 program to rate general perceived usefulness and domains of acquired knowledge. At the post‐intervention assessment, participants also provided written responses to a series of multiple choice and open‐ended questions assessing their satisfaction with the program (e.g., What were your favourite/least favourite things about R2; Would you recommend this to other healthcare professionals? Why? Why not?).
Positive outcomes were assessed combining items from the General Self‐Efficacy Scale (GSE; Schwarzer & Jerusalem, 1995; Italian validation conducted by Sibilia et al., 1995), The Adult Resilience Measure (Liebenberg & Moore, 2018) and the Rugged Resilience Measure (Jefferies et al., 2020).
The General Self‐Efficacy Scale assesses individuals' general beliefs in their ability to respond to and control difficult or novel situations and to handle any related obstacles or setbacks. It consists of 10 items asking participants to rate their self‐efficacy with statements such as ‘I can usually handle whatever comes my way’, on a 4‐point scale (from 1 = does not describe me at all, to 4 = describes me to a great extent). All items were summed to create a total score, between 10 and 40. In the present study, the scale showed moderate reliability (Cronbach's alpha = 0.770).
Resilience was measured using two questionnaires: the 10‐item Rugged Resilience Measure (RRM; Jefferies et al., 2020), and the 17‐item Adult Resilience Measure Revised (ARM‐R; Liebenberg & Moore, 2018). The Rugged Resilience Measure is a measure of personal resilience, which consists of 10 self‐report items (e.g., perseverance, ‘I can keep going despite difficulties’; pride in achievements, ‘I take pride in things I have achieved’), rated on a 5‐point Likert scale ranging from ‘Not at all [like me]’ to ‘A lot [like me]’. Total score ranges from 10 to 50 with higher scores reflecting greater resilience. In the present study, the scale was found to have good internal consistency (Cronbach's alpha = 0.785).
The ARM‐R(Liebenberg & Moore, 2018) is a measure of social‐ecological resilience which explores interpersonal, community and cultural resources which allow people to achieve positive outcomes despite significant adverse experiences. The scale uses a 5‐point Likert scale (‘To what extent do the sentences below describe you?’ where 1 = ‘Not at all’ and 5 = ‘A lot’; e.g., ‘I am aware of my own strengths’; ‘I know where to get help in my community’). Total score ranges from 17 to 85. The scale shows fairly high reliability (Cronbach's alpha = 0.882), with higher scores from the summed items indicating greater socio‐ecological resilience. RRM and ARM did not exist in Italian versions; therefore, it was independently translated in Italian by a professional translator. The integrity of the items was then verified using back‐translation (Vallerand, 1989). Discrepancies with the original English version were noted, and the Italian version was adjusted accordingly.
Negative outcomes were assessed as follows. Burnout was measured using two items from the Maslach Burnout Inventory Emotional Exhaustion (MBI:EE), a non‐proprietary measure, validated to measure burnout in healthcare settings (Dolan et al., 2015). It includes two items: ‘I feel burned out from my work’ rated on a 5‐point Liker scale, ranging from 1 (Never) to 5 (Every day) and ‘I feel like I'm burning out from my work’, rated on a 5‐point Liker scale, ranging from 1 (Not at all) to 5 (A lot). Total score ranges from 5 to 10. In the present study, the scale showed moderate reliability (Cronbach's alpha = 0.672).
General stress was measured using The Perceived Stress Scale (PSS‐10) (Cohen, 1988; Cohen et al., 1983), a self‐report instrument consisting of 10 items to assess how unpredictable and uncontrollable respondents felt their lives to be and how over‐loaded they were day‐to‐day. Each of the items on the PSS‐10 are rated on a 5‐point Likert scale, ranging from 0 (never) to 4 (very often). Total score ranges from 0 to 40 with the scale showing moderate reliability (Cronbach's alpha = 0.604).
Work‐Related Stress was assessed using the Management Standards Indicator Tool (MSIT), a 35‐item self‐report measure of the psychosocial work environment designed to assist organizations with psychosocial risk assessment. Responses to most items are given on a 5‐point Likert scale: 1 (never), 2 (seldom), 3 (sometimes), 4 (often) and 5 (always). Items are worded so that low scores are indicative of high (and potentially harmful) exposures. The instrument has been validated and translated into Italian (Magnavita, 2012). However, in the study, 13 items were excluded as they were not considered relevant in a pandemic scenario and to reduce the overall length of the survey to avoid response burden. Total score ranges from 35 to 175. Despite the reduced number of items, the scale maintained fairly high reliability (Cronbach's alpha = 0.882).
2.5. Data analysis
Analyses were conducted using SPSS Statistics for Windows version 22.0. This study employed a single group pre‐post intervention design. Subscales of the GSE, RRM, ARM, PSS, MSIT and MBI:EE served as outcome variables. Pre‐post distributions were analysed using paired‐samples t‐tests. Standardized mean differences (with Hedges adjustment for a small sample size) and 95% confidence intervals were used to examine the relative size of the intervention effect across the different measures. For small sample sizes (<50), the Hedge's Corrected version of the Cohen's d (Hedges and Olkin 1985), has been computed to correct for biases. Cohen's standards (large [0.8], medium [0.5] and small [0.2]) were used to interpret the magnitude of intervention effects (Cohen, 1998). Descriptive statistics were used to analyse sociodemographic data.
3. RESULTS
3.1. Program satisfaction
Results showed high rates of general perceived usefulness for the R2 program (M = 2,5; SD = 0.52). In particular the program provided participants with skills related to interaction and dialogue with their staff (M = 2,42; SD = 0.51) and strengthened personal resources (M = 2,58; SD = 0.67) and team resources (M = 2,5; SD = 0.52). Final open‐ended comments reported specific benefits attributed to the program such as:
Improvement in interpersonal relationships with other leaders (‘I felt less alone and supported by my colleague, like never before’)
Growth in self‐awareness (‘The program allowed me to take some time to reflect on what is happening inside and around me, on my actions and reactions, in both personal and professional field’).
3.2. Mental health and resilience
First, a paired‐samples t‐test was used to compare the scores of both negative outcomes (general stress, work‐related stress and burnout) and positive outcomes (rugged resilience, resourced resilience and self‐efficacy) in the leaders directly involved in the program. Results showed statistically significant differences in the three positive outcome measures: in the rugged resilience (RRM) scores between pre‐ (M = 29.37, SD = 3.59) and post‐R2 (M = 34.69, SD = 3.66), t(16) = −4.53, p = 0.00, in the resourced resilience (ARM) between pre‐ (M = 59.65, SD = 4.68) and post‐R2 (M = 65.18, SD = 5.85); t(17) = −4.37, p = 0.00 and in self‐efficacy (GSE) between pre‐ (M = 26.37, SD = 2.06) and post‐R2 (M = 29.5, SD = 2.39); t(16) = −4.75, p = 0.00.
Regarding negative outcomes, results showed a significant decrease in general stress (PSS) between pre‐ (M = 35.94, SD = 3.32) and post‐R2 (M = 33.25, SD = 2.72), t(16) = 2.47, p = 0.026 and burnout symptoms (MBI:EE) between pre‐ (M = 6.31, SD = 1.35) and post‐R2 (M = 5.37, SD = 1.2); t(16) = 2.61, p = 0.020. No differences were found in the leaders' work‐related stress (MSIT) between pre‐ (M = 50.5, SD = 15.33) and post‐R2 (M = 50.56, SD = 15.17), t(16) = −0.44, p = 0.966 (Table 4).
TABLE 4.
Changes in outcome measures from pre‐ to post‐R2 intervention – healthcare leaders
| Construct (measure) | Pre‐R2 | Post‐R2 | t | p | Pre‐ to post‐Hedge's g |
|---|---|---|---|---|---|
| M (SD) | M (SD) | ||||
| Rugged resilience (RRM) (n = 16) | 29.37 (3.59) | 34.69 (3.66) | −4.53 | 0.00** | 1.09 |
| Self‐efficacy (GSE) (n = 16) | 26.37 (2.06) | 29.5 (2.39) | −4.75 | 0.00** | 1.228 |
| Resourced resilience (ARM) (n = 17) | 59.65 (4.68) | 65.18 (5.85) | −4.37 | 0.00** | 1.157 |
| General stress (PSS) (n = 16) | 35.94 (3.32) | 33.25 (2.72) | 2.47 | 0.026* | −0.384 |
| Burnout symptoms (MBI:EE) (n = 16) | 6.31 (1.35) | 5.37 (1.2) | 2.61 | 0.020* | −0.30 |
| Work‐related stress (MSIT) (n = 16) | 50.5 (15.33) | 50.56 (15.17) | −0.44 | 0.966 | ‐ |
Note: *p < 0.05, **p < 0.001.
Abbreviations: ARM, Adult Resilience Measure; GSE, General Self‐Efficacy; MBI:EE, Maslach Burnout Inventory Emotional Exhaustion; MSIT, Management Standards Indicator Tool; PSS, Perceived Stress Scale; RRM, Rugged Resilience Measure.
Next, a paired‐samples t‐test was used to compare the scores of both negative outcomes (general stress, work‐related stress and burnout) and positive outcomes (rugged resilience, resourced resilience and self‐efficacy) among staff members. Results showed statistically significant differences in two positive outcomes measures: the rugged resilience (RRM) scores between pre‐ (M = 32.19, SD = 4.54) and post‐R2 (M = 35.32, SD = 4.14); t(62) = −5.90, p = 0.00, and self‐efficacy (GSE) between pre‐ (M = 28.27, SD = 3.19) and post‐R2 (M = 30.35, SD = 3.10); t(62) = −4.18, p = 0.00. Although not significant, the resourced resilience (ARM) measure showed an increase between pre‐ (M = 62.87, SD = 8.93) and post‐R2 (M = 63.66, SD = 8.70); t(62) = −0.68, p = 0.499.
Regarding negative outcomes, results showed a significant decrease in general stress (PSS) between pre‐ (M = 33.03, SD = 3.67) and post‐R2 (M = 30.53, SD = 3.95); t(62) = 3.80, p = 0.00 and in work‐related stress (MSIT) between pre‐ (M = 50.18, SD = 10.56) and post‐R2 (M = 46.93, SD = 10.75); t(60) = 2.25, p = 0.028, while the decrease in burnout symptoms (MBI:EE) between pre‐ (M = 4.7, SD = 1.63) and post‐R2 (M = 4.35, SD = 1.64). [t(60) = 1.68, p = 0.098] was not significant (Table 5).
TABLE 5.
Changes in outcome measures from pre‐ to post‐R2 intervention – staff members
| Construct (measure) | Pregroup | Postgroup | t | p | d |
|---|---|---|---|---|---|
| M (SD) | M (SD) | ||||
| Rugged resilience (RRM) (n = 62) | 32.19 (4.54) | 35.32 (4.14) | −5.90 | 0.00** | 0.751 |
| Self‐efficacy (GSE) (n = 62) | 28.27 (3.19) | 30.35 (3.10) | −4.18 | 0.00** | 0.531 |
| Resourced resilience (ARM) (n = 62) | 62.87 (8.93) | 63.66 (8.70) | −0.68 | 0.499 | ‐ |
| General stress (PSS) (n = 62) | 33.03 (3.67) | 30.53 (3.95) | 3.80 | 0.00** | −0.378 |
| Burnout symptoms (MBI:EE) (n = 60) | 4.7 (1.63) | 4.35 (1.64) | 1.68 | 0.098 | ‐ |
| Work‐related stress (MSIT) (n = 60) | 50.18 (10.56) | 46.93 (10.75) | 2.25 | 0.028* | −0.29 |
Note: *p < 0.05, **p < 0.001.
Abbreviations: ARM, Adult Resilience Measure; GSE, General Self‐Efficacy; MBI:EE, Maslach Burnout Inventory Emotional Exhaustion; MSIT, Management Standards Indicator Tool; PSS, Perceived Stress Scale; RRM, Rugged Resilience Measure.
4. DISCUSSION
To our knowledge, this is the first study exploring the implementation of a resilience promoting curriculum (R2 program) for healthcare leaders dealing with a pandemic. Furthermore, while several studies have explored community, worksite and population‐specific stress reduction programs (Aikens et al., 2014; Werneburg et al., 2011) little empirical attention has been given to enhance the resilience of healthcare employees (Mills et al., 2018). Data from this Phase 1 pilot study suggest that the R2 program has the potential to support healthcare leaders dealing with the COVID‐19 pandemic. Their resilience, in turn, appears to exert a positive effect on the resilience of their staff. However, as this was a single‐arm, non‐randomized intervention, with a small sample size, results need to be interpreted conservatively.
Participation in the R2 program was associated with a significant increase in each positive outcome. In particular, results for the healthcare leaders showed a significant increase with a large effect size in the two measures of rugged and resourced resilience targeted during the program, and in personal self‐efficacy where there was a medium effect size. These results are in line with other studies on resilience‐focused programs with healthcare professionals that report a significant increase in resilience resources (Werneburg et al., 2018) and self‐efficacy (Tarantino et al., 2013) at the end of training. Regarding staff members, results were similar, reporting a large effect size for the increase in rugged resilience, a medium effect size related to the increase of self‐efficacy and a small (but not statistically significant) increase in resources related to resilience.
Based on these results, we believe the R2 program has potential to build resilience by strengthening the rugged factors that reside within individuals, including self‐efficacy and the resources that support employees in healthcare settings to deal with adversity. Importantly, healthcare leaders managed to embrace a multisystemic perspective during the R2 sessions and reflect on the relevant resilience factors in their own recovery process, with these changes translating into improvements in their staff members' wellbeing. While this pilot study lacks a control group, its results suggest the need for future evaluations of similar programs conducted as randomized control trials with a larger sample size.
Regarding negative outcomes, a significant decrease in personal stress and in burnout were reported for both leader and staff groups. However, considering the staff member group separately, the decrease in burnout symptoms did not reach significance. These results are in line with other studies conducted on healthcare workers involved in resilience enhancing programs who have reported lower levels of adverse outcomes (Maunder et al., 2006), stress (Sood et al., 2011; Werneburg et al., 2018) and a decrease in burnout symptoms (Mistretta et al., 2018). Other studies, like that by Tubbert (2016), have shown that healthcare professionals working in medical settings (a hospital's emergency room) can improve their resilience and positively influence their personal and professional lives by being taught the skills to handle stress. In this study, however, staff members showed a non‐significant decrease in burnout symptoms. This may be due to the shortage of time that they were in contact with their supervisors during the pandemic, or the lack of opportunities during staff meetings to reflect on their personal and collective recovery process. Furthermore, the small sample size may have accounted for the non‐significant results.
5. IMPLICATIONS
The COVID‐19 pandemic has highlighted the need for healthcare professionals to deal with heightened stress in the workplace. Given the high levels of impairments experienced by frontline health‐care workers and their difficulties in coping with workplace stress which has been exacerbated by social distancing measures outside of work hours, organizations need to implement programs that can effectively support the mental health of their staff and maximize their resilience.
Resilience is the ability to find and apply resources for support, engage in successful coping, or employ other accessible protective factors where there has been exposure to risk or adversity. In the case of healthcare workers dealing with pandemics, responsive exchanges with healthcare organization leaders can help them build the skills they need to manage stress (Howatt & Bradley, 2018; Pearce, 2020; Tubbert, 2016). These leaders, therefore, must themselves have the capacity to deal with complex and stressful work environments while also demonstrating support for their staff and patients.
R2 is a multisystemic resilience‐oriented approach which helps healthcare leaders strengthen access to personal and organizational resources. Implementation of the R2 model is intended to address the following three generalized principles to build a resilient healthcare organization:
Applying a participatory approach to program design which integrates providers' perceptions of possible solutions to complex problems (Giordano et al., 2021; Giordano & Ungar, 2021). In order to identify practices that support organizational and healthcare workers' resilience, the R2 program involved healthcare leaders in selecting the rugged qualities and resources most likely to build resilience in their particular settings during the pandemic. Furthermore, during each R2 session, participants were invited to elaborate key messages to be delivered to their staff, based on the operationalization of the target resources in their working setting (see Table 1). Indeed, before effective approaches can be developed that support healthcare professionals, it is critical to understand their specific sources of anxiety and fear and the resources that are most relevant to them (Shanafelt et al., 2020).
Healthcare leaders can be mentors to their staff, helping them navigate to, and negotiate for, resources in order to support mental health and wellbeing. Starting from the assumption that, if adequately trained, healthcare leaders could better lead their staff and their organizations more effectively during the pandemic, the results of this study suggest that leaders trained in R2 may be better able to build resilience and increase wellbeing in both themselves and their staff.
A resilience framework can be a useful basis for an organization's mental health support programs during a pandemic.
Reflecting these principles in action, participants in the R2 program suggested a number of changes to the program. Specifically, they recommended that the number of sessions (in this trial there were 12) be reduced given the level of commitment required during a very stressful period in their lives. Indeed, during the last sessions they felt less engaged due to the physical and emotional fatigue they experienced after the first months of the pandemic. For this reason, a second R2 implementation, which took place began in November 2020 was reduced to eight sessions. Second, more support is being offered to participants to help them adapt the program content to meetings with their staff and developing strategies to influence the overall resilience of their healthcare settings.
6. CONCLUSION
Resilience it not only a quality within individuals but grows from access to, and use of, the resources needed to support mental health and wellbeing (Giordano, Ragnoli, Brajda, et al., 2019; Ungar & Theron, 2019). Resilience in healthcare professionals following an emergency results from the combination of personal ruggedness and access to resources, with the organization or environment in which they work playing a central role in predicting wellbeing. Indeed, several studies affirm that supportive work environments within healthcare organizations can enhance resilience processes even in the most challenging of situations (Lowe, 2013). In particular, healthcare leaders can play a central role in enhancing resilience in their staff: efforts to hear, protect, prepare, support, form authentic and relational bonds, and care during a crisis is fundamental for staff wellbeing (Shanafelt et al., 2020).
We undertook this study as a first step towards investigating whether the R2 program can be employed as a resilience‐promoting curriculum for people working in emergency response settings such as the COVID‐19 pandemic. However, results of this study are limited by the simple pre‐post repeated measures design without a control group and the small sample size. Furthermore, the issue of demand characteristics may have influenced staff members who were aware of their leaders' participation, and thus may have felt the need to respond favourably, and the leaders themselves, who might have felt pressured to respond favourably given the time they invested in the training. Finally, the small sample size whose selection was based on naturally occurring groups threatens the validity and generalizability of this study's results. More research is required with larger samples to determine the true effectiveness of the R2 program. A second implementation with new teams of Italian healthcare workers has been conducted during the second wave of COVID‐19. Study results are forthcoming. The lack of research examining resilience development programs in a population of healthcare providers during public health crises makes future research in this field extremely timely.
7. IMPACT STATEMENT
This study suggests that resilience programs like R2, when tailored to the needs of healthcare workers exposed to adversity, may be helpful in reducing employee stress and improving resilience. Indeed, resilience is not only a quality within individuals but can be developed through access to the resources needed to support mental health and wellbeing during conditions of extreme stress like a pandemic.
CONFLICT OF INTEREST STATEMENT
The authors declare that there is no conflict of interest.
ETHICAL STATEMENT
Research procedures were reviewed and approved by the Scientific Committee of the Department of Psychology – Resilience Research Unit (RiRes) of the Università Cattolica del Sacro Cuore.
ACKNOWLEDGMENTS
This research did not receive any specific grant from funding agencies in the public, commercial or not‐for‐profit sectors.
Open Access Funding provided by Universita Cattolica del Sacro Cuore within the CRUI–CARE Agreement.
Giordano, F. , Cipolla, A. , & Ungar, M . (2022). Building resilience for healthcare professionals working in an Italian red zone during the COVID‐19 outbreak: A pilot study. Stress and Health, 38(2), 234–248. 10.1002/smi.3085
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- Adams, J. G. , & Walls, R. M. (2020). Supporting the health care workforce during the COVID‐19 global epidemic. Journal of the American Medical Association, 323(15), 1439–1440. 10.1001/jama.2020.3972 [DOI] [PubMed] [Google Scholar]
- Adhikari, S. P. , Meng, S. , Wu, Y. J. , Mao, Y. P. , Ye, R. X. , Wang, Q. Z. , Sun, C. , Sylvia, S. , Rozelle, S. , Raat, H. , & Zhou, H. (2020). Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID‐19) during the early outbreak period: A scoping review. Infectious Disease of Poverty, 9(29). 10.1186/s40249-020-00646-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aikens, K. A. , Astin, J. , Pelletier, K. R. , Levanovich, K. , Baase, C. , Park, Y. Y. , & Bodnar, C. M. (2014). Mindfulness goes to work: Impact of an online workplace intervention. Journal of Occupational and Environmental Medicine, 56(7), 721–731. 10.1097/JOM.0000000000000209 [DOI] [PubMed] [Google Scholar]
- Babore, A. , Lombardi, L. , Viceconti, M. L. , Pignataro, S. , Marino, V. , Crudele, M. , Candelori, C. , Bramanti, S. M. , & Trumello, C. (2020). Psychological effects of the COVID‐2019 pandemic: Perceived stress and coping strategies among healthcare professionals. Psychiatry Research, 293, 113366. 10.1016/j.psychres.2020.113366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banerjee, D. (2020). The COVID‐19 outbreak: Crucial role the psychiatrists can play. Asian Journal of Psychiatry, 50, 102014. 10.1016/j.ajp.2020.102014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bao, Y. , Sun, Y. , Meng, S. , Shi, J. , & Lu, L. (2020). 2019‐nCoV epidemic: Address mental health care to empower society. Lancet, 395(10224), e37–e38. 10.1016/S0140-6736(20)30309-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barello, S. , Palamenghi, L. , & Graffigna, G. (2020. a). Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID‐19 pandemic. Psychiatry Research, 290, 113129. 10.1016/j.psychres.2020.113129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barello, S. , Palamenghi, L. , & Graffigna, G. (2020. b). Stressors and resources for healthcare professionals during the Covid‐19 pandemic: Lesson learned from Italy. Frontiers in Psychology, 11. 10.3389/fpsyg.2020.02179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown, B. B. (1968). Delphi process: A methodology used for the elicitation of opinions of experts. The RAND Corporation. [Google Scholar]
- Cai, H. , Tu, B. , Ma, J. , Chen, L. , Fu, L. , Jiang, Y. , & Zhuang, Q. (2020). Psychological impact and coping strategies of frontline medical staff in hunan between january and march 2020 during the outbreak of coronavirus disease 2019 (COVID‐19) in Hubei, China. Medical Science Monitor, 26. e9241711. 10.12659/2FMSM.924171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castelli, C. (2013). Tutori di resilienza. Guida orientativa per interventi psicoeducativi. EDUCatt Università Cattolica. [Google Scholar]
- Cesana, M. L. , Giordano, F. , Boerchi, D. , Rivolta, M. , & Castelli, C. (2018). Drawing to reconstruct: Pilot study on acknowledging prisoners’ internal and external resources in a penitentiary institution. World Futures, 74, 392–411. 10.1080/02604027.2018.1445913 [DOI] [Google Scholar]
- Cohen, J. (1998). Statistical power analysis for the behavioral sciences. 2nd ed. Lawrence Erlbaum Associates. [Google Scholar]
- Cohen, S. (1988). Perceived stress in a probability sample of the United States. In Spacapan S. & Oskamp S. (Eds.), The Claremont Symposium on Applied Social Psychology. The social psychology of health (pp. 31–67). Sage Publications, Inc. [Google Scholar]
- Cohen, S. , Kamarck, T. , & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 385–396. 10.2307/2136404 [DOI] [PubMed] [Google Scholar]
- Cohen, S. , & McKay, G. (1984). Social support, stress, and the buffering hypothesis: A theoretical analysis. In Baum A., Taylor S. E., & Singer J. G. (Eds.), Handbook of Psychology and Health (Vol. 4, pp. 253–267). Hillsdale, NJ: Erlbaum. [Google Scholar]
- Crane, M. F. , Kangas, M. , Karin, E. , Searle, B. , & Chen, D. (2020). Leveraging the experience of stressors: The role of adaptive systematic self‐reflection, anxiety. Stress & Coping, 33(3), 231–247. 10.1080/10615806.2020.1732359 [DOI] [PubMed] [Google Scholar]
- Cutrona, C. E. , & Russell, D. W. (1988). The provisions of social relationships and adaptation to stress. In Jones W. H. & Perlman D. (Eds.), Advances in Personal Relationships (Vol. 1, pp. 37–67). Greenwich, CT: JAI Press. [Google Scholar]
- Dewey, C. , Hingle, S. , Goelz, E. , & Linzer, M. (2020). Supporting clinicians during the COVID‐19 pandemic. Annals of Internal Medicine, 172(11), 752–753. 10.7326/M20-1033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Tella, M. , Romeo, A. , Benfante, A. , & Castelli, L. (2020). Mental health of healthcare workers during the COVID‐19 pandemic in Italy. Journal of Evaluation in Clinical Practice, 26(6), 1583–1587. 10.1111/jep.13444 [DOI] [PubMed] [Google Scholar]
- Dolan, E. D. , Mohr, D. , Lempa, M. , Joos, S. , Fihn, S. D. , Nelson, K. M. , & Helfrich, C. D. (2015). Using a single item to measure burnout in primary care staff: A psychometric evaluation. Journal of General Internal Medicine, 30(5), 582–587. 10.1007/s11606-014-3112-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egeland, B. , Carlson, E. , & Sroufe, L. A. (1993). Resilience as process. Development and Psychopathology, 5(4), 517–528. 10.1017/S0954579400006131 [DOI] [Google Scholar]
- Flesia, L. , Monaro, M. , Mazza, C. , Fietta, V. , Colicino, E. , Segatto, B. , & Roma, P. (2020). Predicting perceived stress related to the Covid‐19 outbreak through stable psychological traits and machine learning models. Journal of Clinical Medicine, 9(10), 3350. 10.3390/jcm9103350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frink, D. D. , & Klimoski, R. J. (2004). Advancing accountability theory and practice: Introduction to the human resource management review special edition [Editorial]. Human Resource Management Review, 14(1), 1–17. 10.1016/j.hrmr.2004.02.001 [DOI] [Google Scholar]
- Giordano, F. , Caravita, S. C. S. , & Jefferies, P. (2020). Social‐ecological resilience moderates the effectiveness of avoidant coping in children exposed to adversity: An exploratory study in Lithuania. Frontiers in Psychology, 11, 536353. 10.3389/fpsyg.2020.536353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giordano, F. , Cipolla, A. , Ragnoli, F. , & Bruno, F. B. (2019). Transit migration and trauma: The detrimental effect of interpersonal trauma on Syrian children in transit in Italy. Psychological Injury and Law, 12, 76–87. 10.1007/s12207-019-09345-x [DOI] [Google Scholar]
- Giordano, F. , Cipolla, A. , & Ungar, M. (2021). Tutor of resilience: A model for psychosocial care following experiences of adversity. Frontiers in Psychiatry, 12, 559154. 10.3389/fpsyt.2021.559154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giordano, F. , & Ferrari, C. (2018). Resilience in children victims of violence: An intervention project with adolescents in Lithuania [processi di resilienza in minori vittime di violenza: Un progetto di intervento con adolescenti in Lituania]. Maltrattamento e Abuso all’Infanzia, 20(2), 105–116. 10.3280/MAL2018-002007 [DOI] [Google Scholar]
- Giordano, F. , Orenti, A. , Lanzoni, M. , Marano, G. , Biganzoli, E. , Castelli, C. , & Baubet, T. (2015). Trauma and temporal discontinuity in children victims of natural disasters. The Test de trois dessins: Avant, pendant et avenir. [Trauma e discontinuità temporale nei minori vittime di disastri naturali. Il Test de trois dessins: Avant, pendant et avenir]. Maltrattamento e Abuso all’Infanzia, 17(2), 87–116. 10.3280/MAL2015-002005 [DOI] [Google Scholar]
- Giordano, F. , Ragnoli, F. , & Brajda, B. F. (2019). Data on resilience and trauma‐related symptoms in Lithuanian children victims of violence. Data in Brief, 23, 10379. 10.1016/j.dib.2019.103791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giordano, F. , Ragnoli, F. , Brajda, B. F. , & Boerchi, D. (2019). Testing assisted resilience approach therapy (ARAT) with children victims of violence. Children and Youth Services Review, 96, 286–293. 10.1016/j.childyouth.2018.11.050 [DOI] [Google Scholar]
- Giordano, F. , & Ungar, M. (2021). Principle‐driven program design versus manualized programming in humanitarian settings. Child Abuse & Neglect, 111, 104862. 10.1016/j.chiabu.2020.104862 [DOI] [PubMed] [Google Scholar]
- Grant, A. M. , Curtayne, L. , & Burton, G. (2009). Executive coaching enhances goal attainment, resilience and workplace well‐being: A randomised controlled study. The Journal of Positive Psychology, 4(5), 396–407. 10.1080/17439760902992456 [DOI] [Google Scholar]
- Hargett, C. W. , Doty, J. P. , Hauck, J. N. , Webb, A. M. B. , Cook, S. H. , Tsipis, N. E. , Neumann, J. A. , Andolsek, K. M. , & Taylor, D. C. (2017). Developing a model for effective leadership in healthcare: A concept mapping approach. Journal of Healthcare Leadership, 28(9), 69–78. http://10.2147/JHL.S141664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Healy, S. , & Tyrrell, M. (2011). Stress in emergency departments: Experiences of nurses and doctors. Emergency Nurse, 19(4), 31–37. 10.7748/en2011.07.19.4.31.c8611 [DOI] [PubMed] [Google Scholar]
- Hedges, L. , & Olkin, I. (1985). Statistical methods in meta‐analysis. Statistics in Medicine, 20. 10.2307/1164953 [DOI] [Google Scholar]
- Howatt, B. , & Bradley, L. (2018). Supporting healthcare workers' mental health is good for patient care. The Globe and Mail. Retrieved December 14, 2020 from https://www.theglobeandmail.com/business/careers/workplace‐award/article‐supporting‐healthcare‐workers‐mental‐health‐is‐good‐for‐patient‐care/ [Google Scholar]
- INAIL . (2020). I dati sulle denunce da COVID‐19. Available online at: https://www.inail.it/cs/internet/docs/alg‐scheda‐tecnica‐contagi‐covid‐30‐settembre‐2020.pdf [Google Scholar]
- International Council of Nurses (ICN) . (2020). ICN calls for data on healthcare worker infection rates and deaths. Retrieved December 14, 2020 from https://www.icn.ch/news/icn‐calls‐data‐healthcare‐worker‐infection‐rates‐and‐deaths#:∼:text=It%20shows%20that%2C%20on%20average,infected%20healthcare%20workers%20of%20210%2C000 [Google Scholar]
- Jefferies, P. , Vanstone, R. , & Ungar, M. (2020). The rugged resilience measure: Validation of a brief measure of personal resilience [unpublished manuscript]. Resilience Research Centre, Dalhousie University. [Google Scholar]
- Kang, L. , Ma, S. , Chen, M. , Yang, J. , Wang, Y. , Li, R. , Yao, L. , Bai, H. , Cai, Z. , Yang, B. X. , Hu, S. , Zhang, K. , Wang, G. , Ma, C. , & Liu, Z. (2020). Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross‐sectional study. Brain, Behavior, and Immunity, 87, 11–17. 10.1016/j.bbi.2020.03.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashdan, T. B. , & Rottenberg, J. (2010). Psychological flexibility as a fundamental aspect of health. Clinical Psychology Review, 30(7), 865–878. 10.1016/j.cpr.2010.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalid, I. , Khalid, T. J. , Qabajah, M. R. , Barnard, A. G. , & Qushmaq, I. A. (2016). Healthcare workers emotions, perceived stressors and coping strategies during a MERS‐CoV outbreak. Clinical Medicine and Research, 14(1), 7–14. 10.3121/cmr.2016.1303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasalvia, A. , Amaddeo, F. , Porru, S. , Carta, A. , Tardivo, S. , Bovo, C. , & Bonetto, C. (2021). Levels of burn‐out among healthcare workers during the COVID‐19 pandemic and their associated factors: A cross‐sectional study in a tertiary hospital of a highly burdened area of north‐east Italy. BMJ Open, 11(1), e045127. 10.1136/bmjopen-2020-045127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasalvia, A. , Bonetto, C. , Porru, S. , Carta, A. , Tardivo, S. , Bovo, C. , Ruggeri, M. , & Amaddeo, F. (2021). Psychological impact of COVID‐19 pandemic on healthcare workers in a highly burdened area of north‐east Italy. Epidemiology and Psychiatric Sciences, 30. 10.1017/S2045796020001158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liebenberg, L. , & Moore, J. C. (2018). A social ecological measure of resilience for adults: The RRC‐ARM. Social Indicators Research, 136(1), 1–19. 10.1007/s11205-016-1523-y [DOI] [Google Scholar]
- Lowe, L. D. (2013). Creating a caring work environment and fostering nurse resilience. International Journal for Human Caring, 17(4), 52–59. 10.20467/1091-5710.17.4.52 [DOI] [Google Scholar]
- Magnavita, N. (2012). Validation of the Italian version of the HSE indicator tool. Occupational Medicine, 62(4), 288–294. 10.1093/occmed/kqs025 [DOI] [PubMed] [Google Scholar]
- Magnavita, N. , Soave, P. M. , Ricciardi, W. , & Antonelli, M. (2020). Occupational stress and mental health of anesthetists during the COVID‐19 pandemic. International Journal of Environmental Research and Public Health, 17, 8245. 10.3390/ijerph17218245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magnavita, N. , Tripepi, G. , & Chiorri, C. (2021). Telecommuting, off‐time work, and intrusive leadership in workers’ well‐being. International Journal of Environmental Research and Public Health, 18, 3330. 10.3390/ijerph18073330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magnavita, N. , Tripepi, G. , & Di Prinzio, R. R. (2020). Symptoms in health care workers during the COVID‐19 epidemic. A cross‐sectional survey. International Journal of Environmental Research and Public Health, 17(14), 5218. 10.3390/ijerph17145218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maunder, R. G. , Lancee, W. J. , Balderson, K. E. , Bennett, J. P. , Borgundvaag, B. , Evans, S. , Fernandes, C. M. B. , Goldbloom, D. S. , Gupta, M. , Hunter, J. J. , McGillis Hall, L. , Nagle, L. M. , Pain, C. , Peczeniuk, S. S. , Raymond, G. , Read, N. , Rourke, S. B. , Steinberg, R. J. , Stewart, T. E. , Veldhorst, G. , & Wasylenki, D. (2006). Long‐term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerging Infectious Diseases, 12(12), 1924–1932. 10.3201/eid1212.060584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills, J. , Wand, T. , & Fraser, J. A. (2018). Exploring the meaning and practice of self‐care among palliative care nurses and doctors: A qualitative study. BMC Palliative Care, 17(63). 10.1186/s12904-018-0318-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministero della salute . (2021). COVID‐19 situazione Italia. Retrieved May 19, 2021 from https://opendatadpc.maps.arcgis.com/apps/dashboards/b0c68bce2cce478eaac82fe38d4138b1 [Google Scholar]
- Mistretta, E. G. , Davis, M. C. , Temkit, M. , Lorenz, C. , Darby, B. , & Stonnington, C. M. (2018). Resilience training for work‐related stress among health care workers: Results of a randomized clinical trial comparing in‐person and smartphone‐delivered interventions. Journal of Occupational and Environmental Medicine, 60(6), 559–568. 10.1097/JOM.0000000000001285 [DOI] [PubMed] [Google Scholar]
- Neimeyer, R. A. (2001). Meaning reconstruction and the experience of loss. American Psychological Association. [Google Scholar]
- Nicola, M. , Sohrabi, C. , Mathew, G. , Kerwan, A. , Al‐Jabir, A. , Griffin, M. , Agha, M. , & Agha, R. (2020). Health policy and leadership models during the COVID‐19 pandemic: A review. International Journal of Surgery, 81, 122–129. http://10.1016/j.ijsu.2020.07.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostafin, B. D. , & Proulx, T. (2020). Meaning in life and resilience to stressors. Anxiety, Stress & Coping, 33(6), 603–622. 10.1080/10615806.2020.1800655 [DOI] [PubMed] [Google Scholar]
- Pearce, K. (2020). In fight against COVID‐19, nurses face high‐stakes decisions, moral distress. The Hub. https://hub.jhu.edu/2020/04/06/covid‐nursing‐cynda‐rushton‐qa/ [Google Scholar]
- Pipe, T. B. , Buchda, V. L. , Launder, S. , Hudak, B. , Hulvey, L. , Karns, K. E. , & Pendergast, D. (2012). Building personal and professional resources of resilience and agility in the healthcare workplace. Stress and Health, 28, 11–22. 10.1002/smi.1396 [DOI] [PubMed] [Google Scholar]
- Proches, C. G. (2020). How leadership matters in healthcare – especially in a crisis. The Conversation. https://theconversation.com/how‐leadership‐matters‐in‐healthcare‐especially‐in‐a‐crisis‐141321 [Google Scholar]
- Resilience Research Center . (n.d.). Build your resilience with R2. Retrieved from https://resilienceresearch.org/r2/ [Google Scholar]
- Sabetian, G. , Moghadami, M. , Hashemizadeh Fard Haghighi, L. , Shahriarirad, R. , Javad Fallahi, M. , Asmarian, M. , & Sadat Moeini, Y. (2021). COVID‐19 infection among healthcare workers: A cross‐sectional study in southwest Iran. Virology Journal, 18, 58. 10.1186/s12985-021-01532-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarzer, R. , & Jerusalem, M. (1995). Generalized self‐efficacy scale. In Weinman J., Wright S., & Johnston M. (Eds.), Measures in health psychology: A user’s portfolio (pp. 35–37). Nfer‐Nelson. [Google Scholar]
- Shanafelt, T. , Ripp, J. , & Trockel, M. (2020). Understanding and addressing sources of anxiety among health care professionals during the COVID‐19 pandemic. Journal of the American Medical Association, 323(21), 2133–2134. 10.1001/jama.2020.5893 [DOI] [PubMed] [Google Scholar]
- Shingler‐Nace, A. (2020). COVID‐19. When leadership calls. Nurse Leader, 8(3), 202–203. 10.1016/j.mnl.2020.03.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibilia, L. , Schwarzer, R. , & Jerusalem, M. (1995). Italian adaptation of the general self‐efficacy scale: Self‐efficacy generalized. http://userpage.fu‐berlin.de/health/italian.htm [Google Scholar]
- Sood, A. , Prasad, K. , Schroeder, D. , & Varkey, P. (2011). Stress management and resilience training among department of medicine faculty: A pilot randomized clinical trial. Journal of General Internal Medicine, 26(8), 858–861. 10.1007/s11606-011-1640-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statista Research Department . (2020). Provinces with the highest number of coronavirus (COVID‐19) cases in Italy as of July 20, 2021. https://www.statista.com/statistics/1109295/provinces‐with‐most‐coronavirus‐cases‐in‐italy/ [Google Scholar]
- Tam, C. W. , Pang, E. P. , Lam, L. C. , & Chiu, H. F. (2004). Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: Stress and psychological impact among frontline healthcare workers. Psychological Medicine, 34(7), 1197–1204. 10.1017/S0033291704002247 [DOI] [PubMed] [Google Scholar]
- Tarantino, B. , Earley, M. , Audia, D. , D'Adamo, C. , & Berman, B. (2013). Qualitative and quantitative evaluation of a pilot integrative coping and resiliency program for healthcare professionals. Explore, 29(1), 44–47. 10.1016/j.explore.2012.10.002 [DOI] [PubMed] [Google Scholar]
- Task force COVID‐19‐Dipartimento Malattie Infettive e Servizio di Informatica . (2021). Istituto Superiore di Sanità. Epidemia COVID‐19. Retrieved May 2021 from https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino‐sorveglianza‐integrata‐COVID‐19_24‐febbraio‐2021.pdf. Retrieved February 2021 from https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino‐sorveglianza‐integrata‐COVID‐19_28‐luglio‐2020.pdf [Google Scholar]
- The Lancet . (2020). COVID‐19: Protecting health‐care workers. Lancet, 395, 922. 10.1016/S0140-6736(20)30644-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tubbert, S. J. (2016). Resiliency in emergency nurses. Journal of Emergency Nurses, 42(1), 47–52. 10.1016/j.jen.2015.05.016 [DOI] [PubMed] [Google Scholar]
- Ungar, M. (2008). Resilience across cultures. British Journal of Social Work, 38(2), 218–235. 10.1093/bjsw/bcl343 [DOI] [Google Scholar]
- Ungar, M. , & Theron, L. (2019). Resilience and mental health: How multisystemic processes contribute to positive outcomes. The Lancet Psychiatry, 7(5), 441–448. 10.1016/S2215-0366(19)30434-1 [DOI] [PubMed] [Google Scholar]
- Vallerand, R. J. (1989). Vers une mèthodologie de validation trans‐culturelle de questionnaires psychologiques: Implications pour la recherché en langue française. Psychologie Canadienne, 30, 662–680. [PubMed] [Google Scholar]
- Walsh, F. (2007). Traumatic loss and major disasters: Strengthening family and community resilience. Family Process, 46(2), 207–227. 10.1111/j.1545-5300.2007.00205.x [DOI] [PubMed] [Google Scholar]
- Werneburg, B. L. , Herman, L. L. , Preston, H. R. , Rausch, S. M. , Warren, B. A. , Olsen, K. D. , & Clark, M. M. (2011). Effectiveness of a multidisciplinary worksite stress reduction programme for women. Stress and Health, 27, 356–364. 10.1002/smi.1380 [DOI] [Google Scholar]
- Werneburg, B. L. , Jenkins, S. M. , Friend, J. L. , Berkland, B. E. , Clark, M. M. , Rosedahl, J. K. , Preston, H. R. , Daniels, D. C. , Riley, B. A. , Olsen, K. D. , & Sood, A. (2018). Improving resiliency in healthcare employees. American Journal of Health Behavior, 42(1), 39–50. 10.5993/AJHB.42.1.4 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


