Abstract
Acute otitis externa (AOE), also known as ‘swimmer's ear’, is a common acute problem. It is one of the most common ED presentations. Atypical organisms, recalcitrant disease and antibiotic options contribute to making AOE a clinical challenge. There are a number of red flags associated with AOE which require consideration when treating patients with AOE. We discuss an evidence‐based approach to management of AOE in the emergency setting, with indications for specialist referral.
Keywords: acute otitis externa, emergency medicine, topical treatment
Acute otitis externa (AOE), also known as ‘swimmer's ear’, is a common ED presentation; atypical organisms, recalcitrant disease and antibiotic options contribute to making AOE a clinical challenge. There are a number of red flags associated with AOE which require consideration when treating patients with AOE. We discuss an evidence‐based approach to management of AOE in the emergency setting, with indications for specialist referral.

Key findings.
Acute otitis externa is usually bacterial in origin.
Pseudomonas is the most common bacterium.
Ciprofloxacin is the only antimicrobial without risk of ototoxicity.
Multiple eardrop options are available in Australia for bacterial and fungal otitis externa.
Targeted use of eardrops is key in treatment; adjuncts may be needed.
Introduction
Otitis externa (OE), also known as ‘swimmer's ear’, refers to an inflammatory pathology of the external auditory canal (EAC) and is a common ED presentation. Depending on the infection history it can be acute (lasting less than 4–6 weeks), recurrent or chronic (lasting more than 3 months). 1 Acute OE (AOE) is one of the most common ED presentations.
The annual incidence is 0.4% in the USA, and 1% in the UK. 2 , 3 In tropical Australia, the annual incidence is greater than 1.5% because of the ambient humidity. 4 Incidence is increased by water sports, psoriasis, eczema, hygiene (cotton‐bud usage and ear syringing), immunosuppression, diabetes and narrow EACs. 4 , 5
Methods
Embase, Ovid‐Medline and Ovid‐PubMed databases were searched for literature specifically for management of AOE in the emergency setting using the search strategy in Table 1. The historical range from each database was explored; papers included were limited to those involving humans and published in the English language.
TABLE 1.
Search strategy employed for literature review
| Search strategy | Database | Results |
|---|---|---|
| 1. otitis externa.mp. or Otitis Externa | PubMed | 16 |
| 2. limit 1 to (english language and humans) | ||
| 3. acute.mp. | ||
| 4. Administration, Topical/ or topical.mp. | Medline | 11 |
| 5. ear drops.mp. | ||
| 6. 4 or 5 | ||
| 7. 2 and 3 and 6 | Embase | 2 |
| 8. emergency.mp. or Emergencies | ||
| 9. 7 and 8 |
Clinical presentation
Patients with AOE typically present with earache, itching, aural fullness or hearing impairment, and less commonly with painful lymphadenopathy. Ear discharge is often reported by patients as well. 6
A distinguishing feature between AOE and acute otitis media with discharge, is discomfort/pain upon pinna or tragal manipulation; this is because of contiguous stimulation of an inflamed EAC. Bacterial AOE has an oedematous, friable canal with or without debris/discharge (Fig. 1). Fungal AOE has a creamy discharge with or without fungal spores (black or white) or hyphae (Fig. 2). 7
Figure 1.
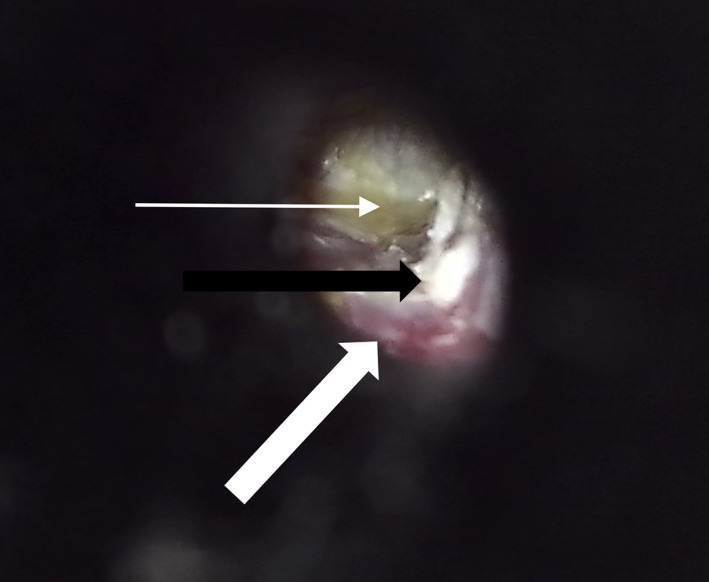
Otoscopic view of acute bacterial otitis externa during aural toilet. Thin white arrow shows purulent exudate pooling next to the tympanic membrane. Thick white arrow shows the erythematous and friable external auditory canal mucosa typical of bacterial acute otitis externa. Thick black arrow shows residual debris in the external auditory canal.
Figure 2.
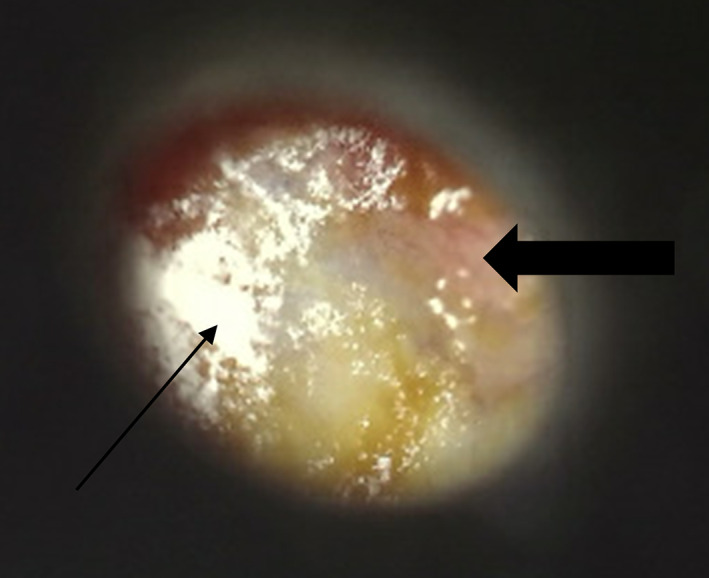
Otoscopic view of fungal otitis externa. Thin arrow shows white fungal hyphae. Thick arrow shows an inflamed tympanic membrane.
Complications of AOE
Proximally contiguous infection can cause inflammation of the ear drum (myringitis) which can lead to perforation.
Distally contiguous disease can cause periauricular cellulitis, perichondritis of the pinna, regional facial cellulitis and systemic toxicity. 5
In immunocompromised patients and diabetics, malignant/necrotising OE can lead to temporal bone osteomyelitis. 8 , 9
Pathogens
Topical management of AOE
Topical antibiotics for AOE are highly effective and are the mainstay of treatment. 11 Eardrops available in Australia are listed in Table 2. Multi‐agent eardrops with steroids are better for AOE with myringitis or granulation. 12 A guideline is shown in Figure 3 to aid in both diagnosis and management of AOE.
TABLE 2.
Eardrops available for use in Australia for acute otitis externa
| Brand name | Active ingredients | Indication | Dosage/duration |
|---|---|---|---|
| Single agent | |||
| Ciloxan† | Ciprofloxacin 0.3% | CSOM, OE, discharging grommets | Five drops, twice a day, until a few days after symptoms have cleared |
| Soframycin‡, § | Framycetin 0.5% | OE | Three drops, thrice a day, until a few days after symptoms have cleared |
| Multi‐agent with steroid | |||
| Sofradex/Otodex‡, § | Dexamethasone 0.05%, framycetin 0.5%, gramicidin 0.005% | CSOM, OE | Three drops, three to four times a day, until a few days after symptoms have cleared |
| Locacorten Vioform§, ¶ | Flumetasone 0.02%, clioquinol 1% | Fungal OE, bacterial OE | Three drops, twice a day, until a few days after symptoms have cleared |
| Ciprofloxacin HC¶ | Hydrocortisone 1%, ciprofloxacin 0.2% | CSOM, OE, discharging grommets | Three drops, twice a day, until a few days after symptoms have cleared |
| Kenacomb Otic‡, §/Otocomb Otic‡, § | Triamcinolone 0.1%, neomycin 0.25%, gramicidin 0.025%, nystatin 100 000 units/g | OE (including fungal), CSOM | Three drops, twice to thrice a day, until a few days after symptoms have cleared |
PBS, Pharmaceutical Benefits Scheme (authority required).
PBS (general).
Should not be used in patient with tympanic membrane perforations.
Non‐PBS.
CSOM, chronic suppurative otitis media; OE, otitis externa.
Figure 3.
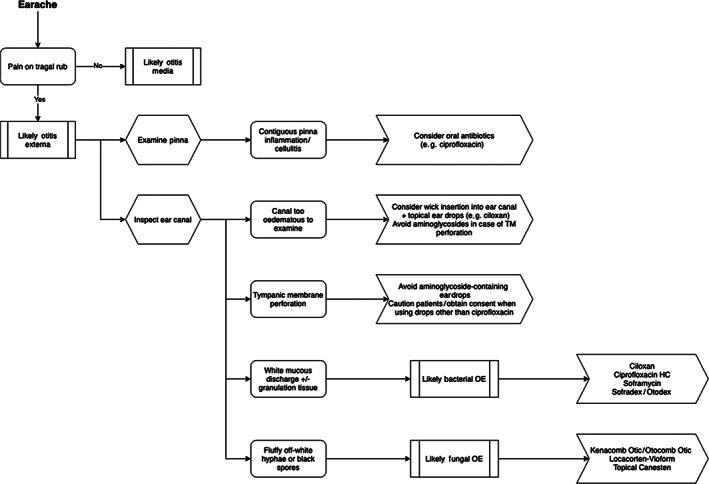
Management guidelines with topical antibiotics for acute otitis externa in the primary care setting. TM, tympanic membrane.
Bacterial AOE
EAC swab should be taken.
Start with a topical treatment with pseudomonal coverage.
If tympanic membrane perforation is suspected, or the membrane cannot be seen, we recommend ciprofloxacin as it is the only antibiotic option that does not cause ototoxicity.
Fungal AOE
Choices such as Ciloxan (Novartis Pharma AG, Basel, Switzerland) and Soframycin (Sanofi‐Aventis, Paris, France) will be ineffective.
Locacorten Vioform (Novartis, Dorval, QC, Canada), Kenacomb Otic (Bristol Meyers Squibb, New York, NY, USA)/Otocomb Otic and topical Canesten (clotrimazole) are appropriate choices.
Anecdotally, gramicidin‐containing compounds are less effective than the other options listed.
Fungal OE often requires referral to ear, nose and throat (ENT) specialists for ear toileting.
Adjuncts to topical antibiotics
Severe cases of AOE may need wick insertion into the EAC to ease eardrop administration. Wicks must be completely inserted in the ear canal, and not prolapse out. Recent evidence indicates that wicks may remain in situ for up to 5 days. 13 Systemic antibiotics may be indicated where contiguous infection of the pinna, or folliculitis is concerned – those with anti‐pseudomonal coverage are wise given that P. aeruginosa is isolated in up to 55% of cases. 14
Advice on how to administer drops
Patients should be advised on how to properly administer drops to provide maximum efficacy. Eardrops should be placed in the EAC with the head in a dependent position, with tragal‐pumping to allow maximum drop penetration (Fig. 4).
Figure 4.

Visual representation of how to administer topical antibiotics to external auditory canal. Note that the head is in a dependent position, with demonstration of tragal pumping. 15
The role of ear toilet
In patients with discharge that occludes the canal, ear toilet should be considered, especially if infection is recalcitrant or not adequately cleared with gentle tissue spears. It is important that ear toilet is performed only by ENT surgeons, or physicians with advanced training to avoid iatrogenic injury to the tympanic membrane or ossicles.
Specific considerations
Perforated tympanic membrane
If there is a perforated tympanic membrane, aminoglycoside‐containing medications should be avoided because of their potential to cause ototoxicity. 16
These medications include framycetin (Soframycin/Sofradex/Otodex) and neomycin (Kenacomb Otic/Otocomb Otic).
The only current topical treatment without risk of ototoxicity is ciprofloxacin.
Locacorten Vioform is labelled ‘contraindicated’ in patients with tympanic membrane perforations; however, in clinical practice it is widely used and extremely effective.
If Locacorten Vioform is used, counsel patients on potential for hearing impairment and vertigo, and immediately discontinue use if these symptoms are reported.
Patients should also be counselled that the use of steroid‐containing drops can cause discomfort when applied to the middle ear.
Pregnancy
As listed in the Australian Medicines Handbook, all of the eardrops listed above are listed as “safe to use” in pregnancy.
If concerned, however, referral to an ENT specialist is recommended for ongoing ear toilet and topical administration of antimicrobial mixtures.
Prevention of recurrent disease
Dry ear precautions
Particularly so in those with narrow/tortuous ear canals, moisture accumulation is a significant risk factor for the development of recurrent or recalcitrant infections. 1 , 17
For those whose hobbies involve water sports, particular care must be taken to prevent water exposure to the canals.
Good ear hygiene after‐the‐fact using acidifying/astringent eardrops, or even alcohol‐containing drops can hasten drying of the ear canal to prevent infection.
Avoiding EAC trauma
Specialist referral guidelines
Emergency treatment
If the EAC is occluded secondary to inflammation, then wick placement in the ED is recommended.
If there is associated perichondritis, particularly so with children, hospitalisation may be necessary for i.v. antibiotics.
In poorly controlled diabetics and immunocompromised patients at risk of developing malignant OE, early referral and treatment is recommended to prevent temporal bone osteomyelitis.
ENT specialist referral
AOE refractory to at least 2 weeks of topical therapy, specialist ENT referral is needed.
Patients who develop complications, particularly a perforated tympanic membrane.
Red flags
- Perichondritis
- Tenderness, erythema and swelling of the auricle.
- Facial cellulitis
- Swelling of the facial soft‐tissue which may track down towards the jaw.
- Malignant OE
- Excruciating pain disproportionate to examination findings, granulation tissue seen in the EAC.
- EAC squamous cell carcinoma
- Abnormal lesion in the EAC not responding to antimicrobial treatment.
- Intracranial infection (abscess/meningitis)
- Altered consciousness, photophobia, headaches, visual symptoms, neck stiffness.
Conclusion
AOE is an extremely common ENT infection.
There are several topical antibiotics available.
Treatment is usually straightforward.
Prompt referral to an ENT specialist is recommended if the patient is acutely unwell or there are red flags.
Competing interests
None declared.
Hershil Khatri, BMedSt, MD, Principal House Officer; Johnson Huang, MBBS, MPhil, Principal House Officer; Emily Guazzo, MBBS, DipAdvSurgAnat, FRACS (ORL‐HNS), Surgeon; Craig Bond, BMed (Hons), MBBS, FRACS (ORL‐HNS), Surgeon.
Data availability statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
References
- 1. Boustred N. Practical guide to otitis externa. Aust. Fam. Physician 1999; 28: 217–21. [PubMed] [Google Scholar]
- 2. Guthrie RM, Bailey BJ, Witsell DL et al. Diagnosis and treatment of acute otitis externa an interdisciplinary update. Ann. Otol. Rhinol. Laryngol. 1999; 108: 2–18. [PubMed] [Google Scholar]
- 3. Rowlands S, Devalia H, Smith C, Hubbard R, Dean A. Otitis externa in UK general practice: a survey using the UK general practice research database. Br. J. Gen. Pract. 2001; 51: 533–8. [PMC free article] [PubMed] [Google Scholar]
- 4. Balch G, Heal C, Cervin A, Gunnarsson R. Oral corticosteroids for painful acute otitis externa (swimmer's ear): a triple‐blind randomised controlled trial. Aust. J. Gen. Pract. 2019; 48: 565–72. [DOI] [PubMed] [Google Scholar]
- 5. Kaushik V, Malik T, Saeed SR. Interventions for acute otitis externa. Cochrane Database Syst. Rev. 2010; (1): CD004740. [DOI] [PubMed] [Google Scholar]
- 6. Rosenfeld RM, Brown L, Cannon CR et al. Clinical practice guideline: acute otitis externa. Otolaryngol. Head Neck Surg. 2006; 134: S4–23. [DOI] [PubMed] [Google Scholar]
- 7. Martin TJ, Kerschner JE, Flanary VA. Fungal causes of otitis externa and tympanostomy tube otorrhoea. Int. J. Pediatr. Otorhinolaryngol. 2005; 69: 1503–8. [DOI] [PubMed] [Google Scholar]
- 8. Mirza N. Otitis externa. Management in the primary care office. Postgrad. Med. 1996; 99: 157–8. [PubMed] [Google Scholar]
- 9. Hern JD, Almeyda J, Thomas DM, Main J, Patel KS. Malignant otitis externa in HIV and AIDS. J. Laryngol. Otol. 1996; 110: 770–5. [DOI] [PubMed] [Google Scholar]
- 10. Roland PS, Stroman DW. Microbiology of acute otitis externa. Laryngoscope 2002; 112: 1166–77. [DOI] [PubMed] [Google Scholar]
- 11. Rosenfeld RM, Singer M, Wasserman JM, Stinnett SS. Systematic review of topical antimicrobial therapy for acute otitis externa. Otolaryngol. Head Neck Surg. 2006; 134: 24–48. [DOI] [PubMed] [Google Scholar]
- 12. Sander R. Otitis externa: a practice guide to treatment and prevention. Am. Fam. Physician 2001; 63: 927–37. [PubMed] [Google Scholar]
- 13. Bola S, Rashid M, Hickey S. Optimising the use of otowicks in otitis externa. J. Laryngol. Otol. 2017; 131: 809–12. [DOI] [PubMed] [Google Scholar]
- 14. Cheffins R, Heal C, Rudolphy S, Evans R, Veitch C. Acute otitis externa: management by GP s in North Queensland. Aust. Fam. Physician 2009; 38: 262–6. [PubMed] [Google Scholar]
- 15. Alcon Laboratories . Ciprodex – Full Prescribing Information. 2003. [Updated 2019; Cited 28 Sep 2020.] Available from URL: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/021537s017lbl.pdf [Google Scholar]
- 16. Leis JA, Rutka JA, Gold WL. Aminoglycoside‐induced ototoxicity. Can. Med. Assoc. J. 2015; 187: E52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wright DN, Alexander JM. Effect of water on the bacterial flora of swimmers' ears. Arch. Otolaryngol. 1974; 99: 15–8. [DOI] [PubMed] [Google Scholar]
- 18. Hobson JC, Lavy JA. Use and abuse of cotton buds. J. R. Soc. Med. 2005; 98: 360–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bird S. Ear syringing: minimising the risks. Aust. Fam. Physician 2008; 37: 359–60. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.


