To the Editor:
The COVID-19 pandemic has challenged the health system but has provided opportunities for improvement. Affected regions have experienced an unprecedented shortage in ICU beds and qualified staff, therefore requiring the transfer of patients.1 Regions far away from large urban centers are more likely to be overwhelmed because of fewer resources.2 A guideline and consensus statement recently published in Chest by Dichter et al3 has proposed as a strategy to face new mass critical surge response that the load could be balanced across regions before the hospitals are overwhelmed and the standard routine affected.3 A regional command center to coordinate the transfers is necessary, but as far as we know the experiences described in this regard are scarce.4 The goal of this study was to describe the flow and the characteristics of the patients with severe COVID-19 who were transferred by a regional command center in the first four pandemic waves.
Methods
A prospective observational study was conducted in Catalonia from March 15, 2020 to July 1, 2021. Hospitalized patients with severe COVID-19 transferred to an ICU managed by the Emergency Medical System (EMS) of Catalonia from a centralized regional command center were included. This study has been approved by the Ethics and Clinical Research Committee of the Institut d'Investigació Sanitària Pere Virgili (107/2020).
The population of Catalonia is 7,739,758, of whom 42.8% is concentrated in the Barcelona metropolitan area (BMA). In February 2020, 63.2% of ICU beds were located in the BMA, mostly in five hospitals. Thirteen percent of the total ICU beds are in private hospitals. The EMS is part of the Catalan public health system, which centralizes and coordinates all interhospital transfers. During the pandemic, the hospital network was divided into five subregions in the form of clusters in which each hospital has a higher-level hospital as a reference. Each cluster is made up of eight to 10 hospitals, creating a radial network that ends at a high-level hospital in the BMA.
Requests for transfer are made when the clinical situation of the patient requires therapeutic resources that are not available in the sending hospital. A team of health care technicians, nurses, and doctors, which varies between five and 10 people depending on demand, participates in the coordination of the transfers. Since the beginning of the pandemic, this team has been reinforced by a specialist in the care of patients who are critically ill. Using information from the phone call and electronic health records, the team assesses the transfer request, provides clinical advice to clinicians onsite, prioritizes the transfers, assigns the most appropriate resource for the transfer, selects the destination hospital, facilitates the return to the hospital of origin, provides logistical support for transfers with extracorporeal membrane oxygenation therapy, and distributes electro-medical equipment. To help establish severity and priority, a predictive model of critical events composed by seven clinical variables obtained in the first assessment has been developed and validated, the interhospital transfers for COVID-19 patients (TIHCOVID) Scale.5 ICU allocation of patients with severe COVID-19 is done initially within each cluster until it reaches its overload limit and then to other clusters according to the direction of the health care authorities. The team continuously monitors the availability of ICU beds. All transfer requests, their priority, and their real-time management status is made available to the entire team. In times of crisis, these data are displayed on a large screen.
Results
During the study period, the regional command center assessed 3,051 interhospital transfer requests for patients with severe COVID-19. Three hundred fifty-four patients (11.6%) did not require transfer, and 2,697 transfers were carried out.
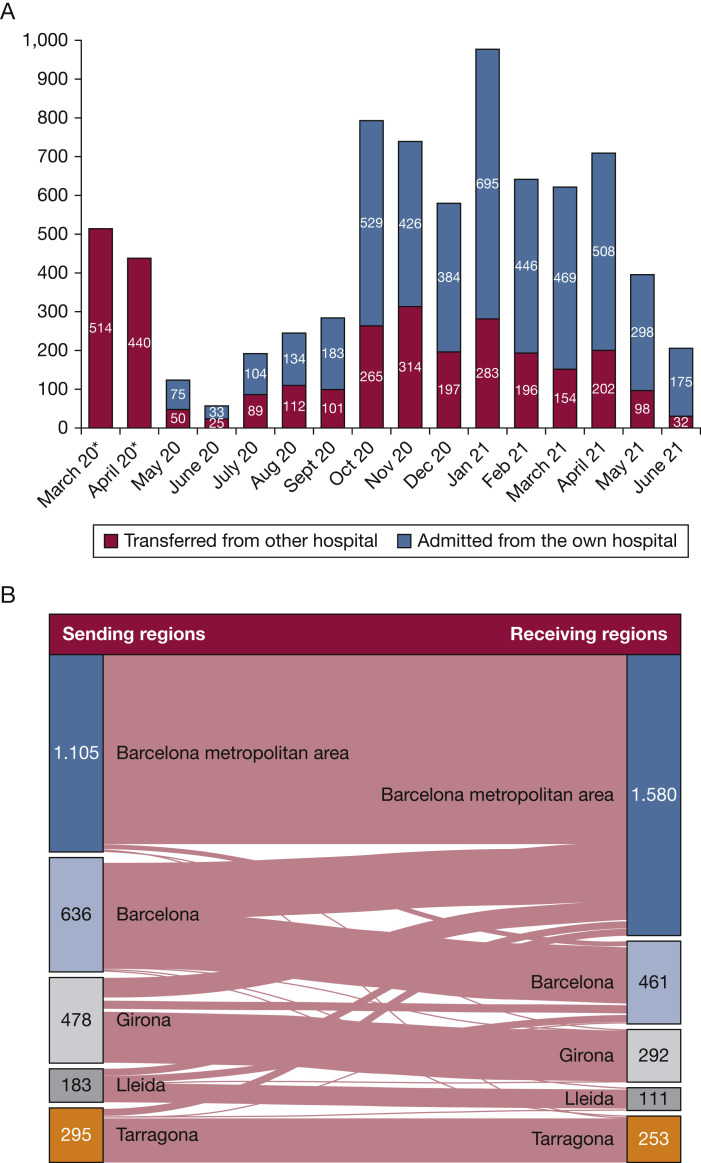
The highest number of transfers occurred during March and April 2020, as shown in Figure 1A. The average monthly percentage of ICU admissions transferred from other hospitals was 30.6%, with a range between 15.5% and 40%.6 Figure 1B shows the flow of patients between the different provinces and the BMA. The highest flow of patients was recorded in the BMA, which received 506 (32.0%) patients from outside its area and sent out only 31 (2.8%). The province of Barcelona transferred 311 (48.9%) patients out of its area, Girona 190 (39.7%), Lleida 74 (40.4%), and Tarragona 46 (15.6%). The growth in demand for transfers in each province was asymmetrical and staggered, requiring transfers between the different clusters during severe surge. Only 28% of patients came from a hospital with an ICU service. Table 1 shows the clinical characteristics of patients transferred during the first four waves of the COVID-19 pandemic. The hospital mortality was 29.2%. No adverse events related to transport or critical events during transport were reported.
Figure 1.
Number and flow of patients transferred during the pandemic. A, Number of patients admitted per month to the ICUs in Catalonia according to their origin. ∗Data on admitted ICU patients from their own hospital in March and April 2020 were not available. B, Flow of patients with severe COVID-19 transferred to an ICU in Catalonia. The number of inhabitants by area and provinces were: Barcelona metropolitan area (3,239,337), Barcelona (2,465,360), Tarragona (826,930), Girona (771,779), and Lleida (436,352).
Table 1.
Clinical Characteristics of Patients Transferred in the First Four COVID-19 Pandemic Waves
| Characteristic | All Patients (N = 1,468) (Waves 1-4) | First Wavec (n = 450) | Second/Third/Fourth Waved (n = 1,018) | P |
|---|---|---|---|---|
| Age, mean (SD), y | 60.6 (12.5) | 60.1 (12.3) | 61.0 (12.8) | .702 |
| Male sex | 1,029 (70.1) | 311 (69.1) | 718 (70.5) | .326 |
| Hypertension | 756 (51.5) | 218 (51.2) | 538 (52.8) | .069 |
| Diabetes mellitus | 392 (26.7) | 113 (25.2) | 279 (27.4) | .660 |
| Obesity (BMI ≥ 30) | 383 (26.1) | 116 (26.0) | 267 (26.2) | .821 |
| Active smoking | 106 (7.2) | 22 (4.9) | 84 (8.3) | .031 |
| Respiratory backgrounda | 352 (24.0) | 91 (20.1) | 261 (25.6) | .019 |
| Comorbidities b | 247 (16.8) | 82 (18.0) | 165 (16.2) | .103 |
| Clinical frailty scale (CFS) | .034 |
|||
| 1 | 184 (12.5) | 75 (16.7) | 109 (10.7) | |
| 2 | 716 (48.8) | 209 (46.4) | 507 (49.8) | |
| 3 | 514 (35.0) | 147 (32.7) | 367 (36.1) | |
| ≥4 | 54 (3.7) | 19 (4.2) | 35 (3.5) | |
| Nonintubated before transfer | 448 (30.5) | 66 (14.7) | 382 (37.5) | < .001 |
| Only oxygen mask | 51 (3.5) | 21 (4.7) | 30 (2.9) | |
| HNF | 177 (12.0) | 23 (5.1) | 154 (15.1) | |
| NIV | 57 (3.9) | 15 (3.3) | 42 (4.1) | |
| Both HNF and NIV | 163 (11.1) | 7 (1.6) | 156 (15.3) | |
| Intubated before transfer | 1020 (69.5) | 384 (85.3) | 636 (62.5) | < .001 |
| Oxygen mask prior intubation | 376 (25.6) | 233 (51.8) | 143 (14.0) | |
| HNF prior intubation | 267 (18.2) | 74 (16.4) | 193 (18.9) | |
| NIV prior intubation | 228 (15.5) | 67 (14.9) | 161 (15.8) | |
| Both HNF and NIV prior intubation | 149 (10.2) | 10 (2.2) | 139 (13.7) | |
| PAo2/Fio2 ratio, mean (SD) | 117.4 (52.6) | 113.2 (55.1) | 119.3 (50.3) | .010 |
| Need for pronation prior transfer | 248 (16.9) | 112 (24.9) | 136 (13.3) | < .001 |
| Acidosis or shock | 185 (19.4) | 67 (14.9) | 118 (11.6) | < .001 |
| Acute renal failure | 388 (26.4) | 108 (24.0) | 280 (27.5) | .044 |
| ICU at issuing hospital | 417 (28.4) | 129 (28.7) | 288 (28.3) | .580 |
| Location before transfer: | ||||
| ICU | 128 (8.7) | 57 (12.7) | 71 (7.0) | .025 |
| ED | 1,095 (74.6) | 314 (69.8) | 781 (76.7) | .038 |
| Semi-critical care unit | 245 (16.7) | 79 (17.5) | 166 (16.3) | .464 |
| Days of ICU stay after transfer, mean (SD) | 18.6 (14.4) | 19.3 (16.7) | 18.2 (13.4) | .297 |
| High risk of death according to TIHCOVID scale | 305 (20.8) | 102 (22.7) | 203 (19.9) | < .001 |
| Hospital mortality | 429 (29.2) | 152 (33.8) | 277 (27.2) | < .001 |
Values are No. (%) for categorical variables and mean (SD) for continuous variables. The Student t or the χ2 were used to compare the subgroups. Test were two-tailed, and P values below .05 were considered statistically significant. HNF = high nasal flow; NIV = noninvasive mechanical ventilation; TIHCOVID = interhospital transfers for COVID-19 patient.
Asthma, COPD GOLD class A-B, OSA/hypopnea syndrome.
Includes COPD GOLD class C-D, pulmonary fibrosis, cerebral vascular accident with sequelae, heart failure with New York Heart Association functional class III-IV, neurodegenerative diseases, active cancer, and Child B-C cirrhosis.
March 14, 2020 through April 30, 2020.
October 17, 2020 through April 30, 2021.
Discussion
The regional command center managed a third of the ICU admissions in Catalonia. The most densely populated area received the highest number of transfers of patients with severe COVID-19. Differences in management and outcomes were found between the first and subsequent waves as in other larger ICU series.7 Another collaborative network between public, private, and federal hospitals in Arizona shared ICU resources, hiring ambulance transfer services and from the beginning had to cope with the heterogeneity of the various actors.8 The current study describes the structure of an integrated command center within the public health network based on a previous structure that had been dedicated to the interhospital transfer, which is not common in all EMS. This proves its usefulness and has facilitated its rapid implementation and operational functioning as a “single regional ICU.”
The leadership of a critical care specialist provided clinical support and facilitated decision-making regarding the suitability of the therapeutic effort, especially for those centers that did not have an ICU. The mortality rate of patients transferred was similar to other national and international series supporting the safety of transfers.9
The regional command center has enabled real-time monitoring of demand and available ICU resources across the territory in an effective way and provides clear information improving the communication among all actors. Although its effect on patient outcomes remains to be established, our data indicate that the regional command center has performed as a transfer hub capable of early load balancing to prevent overcrowding and crisis care during the mass critical pandemic surge.10
Acknowledgments
Financial/nonfinancial disclosures: None declared.
References
- 1.Guillon A., Laurent E., Godillon L., Kimmoun A., Grammatico-Guillon L. Inter-regional transfers for pandemic surges were associated with reduced mortality rates. Intensive Care Med. 2021;47(7):798–800. doi: 10.1007/s00134-021-06412-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Miller I.F., Becker A.D., Grenfell B.T., Metcalf C.J.E. Disease and healthcare burden of COVID-19 in the United States. Nat Med. 2020;26(8):1212–1217. doi: 10.1038/s41591-020-0952-y. [DOI] [PubMed] [Google Scholar]
- 3.Dichter J.R., Devereaux A.V., Sprung C.L., et al. Mass critical care surge response during COVID-19. Chest. 2021;161(2):429–447. doi: 10.1016/j.chest.2021.08.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arabi Y.M., Azoulay E., Al-Dorzi H.M., et al. How the COVID-19 pandemic will change the future of critical care. Intensive Care Med. 2021;47(3):282–291. doi: 10.1007/s00134-021-06352-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Solà S., Jacob J., Azeli Y., Trenado J., Morales-Álvarez J., Jiménez-Fàbrega F.X. Priority in interhospital transfer of patients with severe COVID-19: development and prospective validation of a triage tool. Emergencias. 2022;34(1):29–37. [PubMed] [Google Scholar]
- 6.Salut/Dades COVID Generalitat de Catalunya. https://dadescovid.cat/
- 7.Carbonell R., Urgelés S., Rodríguez A., et al. COVID-19 SEMICYUC Working Group Mortality comparison between the first and second/third waves among 3,795 critical COVID-19 patients with pneumonia admitted to the ICU: a multicentre retrospective cohort study. Lancet Reg Health Eur. 2021;11 doi: 10.1016/j.lanepe.2021.100243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Villarroel L., Christ C.M., Smith L., et al. Collaboration on the Arizona surge line: how Covid-19 became the impetus for public, private, and federal hospitals to function as one system. NEJM Catal Innov Care Deliv. 2021;12 [Google Scholar]
- 9.COVID-ICU Group on behalf of the REVA Network and the COVID-ICU Investigators Clinical characteristics and day-90 outcomes of 4244 critically ill adults with COVID-19: a prospective cohort study. Intensive Care Med. 2021;47(1):60–73. doi: 10.1007/s00134-020-06294-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kadri S.S., Sun J., Lawandi A., et al. Association between caseload surge and COVID-19 survival in 558 U.S. hospitals, March to August 2020. Ann Intern Med. 2021;174(9):1240–1251. doi: 10.7326/M21-1213. [DOI] [PMC free article] [PubMed] [Google Scholar]