Abstract
Objective
To examine the hypothesis that PTSD with delayed expression in some cases occurs without subthreshold PTSD symptoms above background levels bridging the gap between the traumatic exposure(s) and the clinical diagnosis.
Methods
We performed systematic searches of peer‐reviewed papers in English referenced in Pubmed, Embase, or PsycINFO and ascertained 34 prospective studies of PTSD symptom trajectories identified by latent class growth statistical modeling. Studies with delayed and low‐stable trajectories provided appropriate data for this study. We computed the difference between the delayed trajectory PTSD symptom sumscore and the low‐stable PTSD sumscore at the observed points in time after the traumatic event(s).
Results
In 29 study populations, the latent class growth analyses displayed delayed trajectories, and in these, we identified 110 data points (% PTSD sumscore difference/months since traumatic exposure). The median PTSD symptom sumscore was 25% higher during the initial 6 months among individuals in the delayed trajectory compared to those in low‐stable trajectory. From this level, the difference widened and reached a plateau of 40–50% higher. The variation was large, and the baseline participation rate and loss to follow‐up were exceeding 25% in the majority of the studies. Heterogeneity of populations, measures, and analyses precluded formal meta‐analysis.
Conclusion
Delayed PTSD is preceded by PTSD symptoms during the first year in most cases. Still, few individuals may experience an asymptomatic delay. The results underpin the rationale for monitoring PTSD symptoms and may inform forensic assessments in that delayed PTSD without symptoms bridging the traumatic event is rare.
Keywords: forensic psychiatry, latent class growth analysis, partial PTSD, subthreshold PTSD, trajectory analysis, veterans
Summations
Subthreshold PTSD symptoms are present from the traumatic event until diagnosis in the vast majority of cases with delayed expression of PTSD, but data do not exclude asymptomatic delay intervals in some individuals.
Limitations
We were not able to arrive at a formal quantitative meta‐analytic estimate because of heterogeneity across populations, symptom scales, and latent growth analyses, but despite that, data converge and point in the same direction.
Only an unknown proportion of individuals in the delayed trajectories (if any) become clinical cases (best‐practice clinical diagnosis of PTSD at end of follow‐up rather than symptom reporting would have made a stronger case).
1. INTRODUCTION
Posttraumatic stress disorder (PTSD) emerged as a separate psychiatric diagnostic category among military veterans in the aftermath of the Vietnam War and was officially defined and recognized by the American Psychiatric Association in 1980. 1 The core elements of PTSD are the occurrence of intrusive memories, avoidant behavior/numbing, increased arousal, and—from 1994—impaired occupational and/or social functioning that develops after one or more exceptionally traumatic exposures. 2 It is clearly distinguished from acute stress disorder (also labeled combat stress reaction) by its more gradual development and symptoms that persist for a month or longer, but acute stress disorder is a strong predictor of PTSD. 3 , 4
Up to the early 2000s, it was thought that PTSD in the vast majority of cases would develop within the first few months after the potentially traumatic event. Later, three systematic reviews based upon numerous large prospective studies consistently demonstrated, that the onset of the disorder, defined as the time at which all diagnostic criteria are met, is delayed beyond 6 months in 20–30% of cases—more frequent in military personnel returning from deployment. 5 , 6 , 7 This knowledge disclosed an ambiguity in the definition of delayed‐onset PTSD, which can be understood as either a delay of the time at which the very first symptoms of the disorder occur (“out of the blue”) or as a delay of the time when all diagnostic criteria are fulfilled regardless of subthreshold symptoms during the delay interval (bridging symptoms). 5 , 8 In the latter case, delayed‐onset PTSD can be conceptualized as a disorder that develops gradually from an elevated level of PTSD symptoms during the initial months until the diagnostic threshold is crossed perhaps years later—or in other words—as essentially the same disorder as immediate onset PTSD but with slower development. However, in the former case, the disorder might be understood as a different diagnostic entity—perhaps with different determinants, prognostic factors, and options for treatment. 8
The PTSD diagnosis is different from most other psychiatric diagnoses in that the alleged cause of the disorder is included in the diagnostic criteria. The traumatic event is considered a necessary but not sufficient cause as most people who were exposed to a potentially traumatic event do not develop PTSD. It should be acknowledged, however, that causal links between traumatic events and PTSD have rarely been assessed by systematic epidemiological studies based upon unbiased estimates of risk relative to appropriate reference groups without exposure. A short time span from exposure to outcome is therefore important to establish a causal link in analogy with somatic injuries following accidents. A signature of the traumatic event(s) is present in two of the four PTSD symptom clusters (intrusive memories and avoidant behavior), but this may be secondary to psychiatric morbidity with other causes—such as major depression—and is not necessarily indicative of the cause of the disorder. Therefore, as the time of symptom onset becomes more and more distant from the exposure, the more it becomes uncertain if the disorder in fact is causally related to the trauma in question. On the other hand, if subthreshold PTSD symptoms bridge the traumatic event and the outcome and gradually develop into PTSD fulfilling all diagnostic criteria, the causal link to the trauma becomes more plausible.
So far it seems, that the scientific community at large, and the committees that have taken responsibility for the latest diagnostic classifications, endorse the view, that delayed‐onset PTSD should be understood as delayed onset of the disorder rather than delayed onset of the first symptoms. 9 , 10 Andrews et al stated in the first systematic review of delayed‐onset PTSD from 2007 that delayed‐onset PTSD in the absence of any prior symptoms is rare 5 and subsequent reviews arrived at the same conclusion even though data were limited. 6 , 7 The issue has also been specifically addressed in a study comparing characteristics of immediate and delayed‐onset PTSD 11 and retrospective cross‐sectional studies of military veterans 12 that all add to the limited evidence that delayed‐onset PTSD develops on top of subthreshold PTSD symptoms during the initial months following the traumatic event(s).
Nevertheless, the “bridging symptom” hypothesis is challenged by other studies. Several case reports from the 80s‐90s describe PTSD with onset many years after extremely traumatic war experiences in veterans that adapted well to civilian life after the war without display of psychiatric disorders. 13 , 14 , 15 Solomon et al reviewed 150 medical files of Israeli soldiers with delayed‐onset PTSD examined up to five years after the 1982 Lebanon War and report that in 10% of cases there were apparently no symptoms prior to the diagnosis. 12 O’Donnell et al found in a large prospective study of severely injured patients that the majority of patients with delayed‐onset PTSD diagnosed at least one year after the accidents had minimal symptoms during the initial months. 8 Finally, the diagnostic criteria requesting onset of the PTSD disorder within the first 6 months after the trauma in the vast majority of cases is relaxed in the latest diagnostic classifications issued by WHO. 16 However, the DSM criteria requiring that all diagnostic criteria are fulfilled within the first 6 months after the trauma, after which the delayed‐onset specifier is used, has not changed in DSM‐5. 17
Whether early subthreshold symptoms in delayed‐onset PTSD are present or not is important for monitoring and clinical practice, but is also of prime interest in forensic psychiatry, occupational medicine, and in the context of litigation. Thus, a recent verdict of a Danish court addressed a veteran case of delayed‐onset PTSD diagnosed 13 years after the alleged traumatic events and without obvious symptoms in parts of the delay interval. 18 This case was not approved by the Danish National Board of Occupational Injuries, mainly because the timing of PTSD symptoms relative to the traumatic event was not considered pertinent—an assessment that was contradicted by the verdict.
To the best of our knowledge, a systematic review explicitly weighting the observational evidence in support of or against the hypothesis, that PTSD, in some cases, occurs with delayed onset and without clinically relevant symptoms for a few to many years after the alleged causative traumatic event(s) has not been published earlier.
On this background, the objective of this review is to synthesize the scientific evidence addressing the time course of symptoms in PTSD with delayed expression, specifically whether delayed PTSD commonly occur without PTSD symptoms above background levels bridging the gap between the traumatic exposure(s) and the clinical diagnosis, and whether the symptom trajectory in delated‐onset PTSD is modified by the type of population, trauma severity, and taxing life events during follow‐up. To accomplish this, we evaluated prospective studies of PTSD symptom trajectories identified by latent growth mixture statistical modeling and equivalent statistical methods.
2. METHODS
2.1. Literature search
Two authors (JPB and JHJ) assisted by a scientific librarian searched Medline, Embase, and PsycINFO for prospective epidemiological studies with longitudinal analysis of trajectories of PTSD symptoms measured at least three times after exposure to traumatic events on 5 January 2021. An initial search in Medline with terms combining posttraumatic stress disorder and symptom trajectory (for details, see Supplementary Material, Appendix S1) captured 21 of 25 eligible papers identified from a review. 19 Three papers were not identified because the journals were not indexed by Medline, and one relevant paper was not captured. An updated search with slightly updated search terms captured all relevant indexed articles. Hereby, we were assured that the updated search term had appropriate coverage. Subsequently, we identified, respectively, 558, 557, and 403 original eligible papers in these three databases, in total 718 after removing duplicates.
Inclusion criteria were as follows:
PTSD symptoms defined according to DSM‐III+ / ICD‐10+ criteria
≥ 100 participants
≥ 1 year of follow‐up
≥ 3 measurement points
trajectory analysis (latent class growth analysis)
adult populations (>=18 years)
Exclusion criteria were as follows:
Birth‐related PTSD
Partner violence (but not assault and rape), restriction to ICD‐10 eligible trauma
Childhood abuse, to ensure prospective data
After sifting of titles and abstracts 97 papers remained for full‐text reading and the final sample fulfilling the in‐ and exclusion criteria included 33 papers reporting PTSD trajectories in 41 populations. Moreover, one paper was identified from other sources 20 so the final sample had 34 papers and 42 populations. Consensus between authors was reached by discussion. Medline search strings, the Prisma flow chart, a table listing reasons for exclusion of 64 papers selected for full‐text reading, and the Prisma checklist are provided in Appendices S1–S3. The protocol is registered at www.crd.york.ac.uk/prospero (CRD42021227447) and adheres with the Prisma Guidelines for systematic reviews.
2.2. Data extraction
Two authors (JPB and JHJ) systematically extracted information about study populations, design, baseline participation, attrition from baseline to the last follow‐up, trauma characteristics, number of follow‐up assessments, the methods for exposure and outcome ascertainment, quantitative measures of PTSD symptoms, and statistical methods applied for latent class growth modeling.
When available, we extracted crude and adjusted risk estimates (RR or equivalent with 95% CI) for effects of trauma severity and posttraumatic stressful life events on the risk of being on the delayed trajectory versus low‐stable trajectory. We also screened for information on interactive effects of stressful life events on the trauma PTSD association in delayed‐onset PTSD.
Time and PTSD sum score data points were retrieved from tables when available, otherwise obtained as approximate values by readouts of graphs of trajectories measured with 1/10 mm accuracy by Adobe Pro software by two authors, JPB and JHJ). All extracted data were transferred to a datasheet and made available for summary statistics created by SAS Studio software 9.04. 21 As a measure of interrater reliability we computed the Pearson correlation coefficients (n = 110, low‐stable trajectory: r = 0.994, p < 0.0001; delayed trajectory: r = 0.995, p < 0.0001).
2.3. Data synthesis
2.3.1. Criteria for homogeneity across studies
The homogeneity of the PTSD trajectories was evaluated by inspection of the trajectory graphs by two authors (JPB and JHJ), who reached consensus by discussion. First, it was decided if a delayed trajectory was displayed or not. A delayed trajectory was defined as a trajectory with an increasing PTSD symptom sumscore across time, which may/may not reach a plateau at a higher level during the follow‐up period. Second, it was evaluated whether the trajectories were typical or not. A typical study used a PTSD symptom scale based upon the DSM‐IV/DSM‐IV‐TR criteria and was defined by four trajectories (low stable, improving, delayed, and high stable). It was furthermore requested that the proportion of individuals on the delayed trajectory was within the range of 5–15%. Two larger studies that subdivided trajectories into for instance slowly and fast improving trajectories were allowed in the typical category. 22 , 23 One of these also displayed two delayed categories (monotonically increase and relieved‐worsening). 22 Studies displaying (1) the typical four symptom trajectories (low stable, improving, delayed, and high stable) and (2) a delayed trajectory with a prevalence of 5–15% were designated as having higher homogeneity, otherwise lower homogeneity.
2.3.2. Stratification
Descriptive summary statistics were stratified by type of population defined by (1) military personnel (2) professionals such as police, firefighters, rescue personnel, construction and cleaning workers, and medical workers, and (3) people exposed to trauma in civilian life.
2.3.3. The measure of PTSD symptoms
The PTSD symptom sumscore at a given assessment (point in time synchronized with the traumatic event(s)) for the delayed trajectory was subtracted from the corresponding value for the stable low trajectory. In order to compare trajectories based upon different PTSD symptom scales, the difference between the delayed and the stable low trajectory was taken as a percentage of the entire scale range. An example: The mean PTSD sumscore on the posttraumatic disorder symptom checklist (PCL—the most often used scale with 17 items corresponding to the DSM‐IV/DSM‐IV‐TR symptoms and rated from 1 (not at all) to 5 (always), range 17–85) was 21 for the low‐stable trajectory and 32 for the delayed‐onset trajectory 1 month after the traumatic event. The difference at this time‐point, 32–21 = 11, was taken as a percentage of the range of this scale, which is from 17 to 85: 11/(85–17) = 16,2%. It was assumed that moving a given percentage on one scale is equivalent to moving the same percentage on another scale.
The mean values of the score differences between delayed and low‐stable trajectories weighted by the size of the baseline population were tabulated by months in relation to the traumatic event and stratified by type of population and homogeneity of studies (higher/lower). For an overview, the same data are also presented in scatterplots with lines joining average values.
2.3.4. Bias and confounding
We are not aware of any transparent and standard assessment tool that is appropriate for assessment of quality and bias related to the specific research questions addressed here. As recommended by some epidemiologists, 24 we have for purposes of this specific review identified issues of major importance for potential bias. PTSD trajectories may be distorted by selection bias, attrition bias, common method bias, number/timing of assessments, and duration of follow‐up. Estimates of relative risk of delayed PTSD trajectories according to trauma severity and interaction between exposure to the primary trauma and later stressful life events may, in addition, be biased by confounding by baseline characteristics (sex, age, socio‐economic status, family occurrence of psychiatric disorder, history of mental disorder, childhood abuse, and physical health including for example brain injury). All factors were dichotomized (present yes/no). The risk of selection and attrition bias was considered more likely if the baseline participation rate was <75% or unknown or the proportion of baseline participants completing the last follow‐up assessment was <75% or unknown.
3. RESULTS
3.1. Characteristics
We identified 34 prospective studies (42 study populations) of trauma exposed populations with PTSD symptom trajectory analysis. 22 , 23 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 Key characteristics for each study are listed in Supplementary Material (Appendix S4) and summarized in Table 1. Brief summary descriptions of each study are provided in Supplementary Material (Appendix S5).
TABLE 1.
Summary of study characteristics by type of study populations (n = 42), 34 papers
| Characteristic | Military | Professionals | Civilians |
|---|---|---|---|
| Number of study populations, n | 20 | 5 | 17 |
| Publication year, n | |||
| 2000–2010 | 2 | 0 | 4 |
| 2011–2015 | 9 | 1 | 7 |
| 2016–2020 | 9 | 4 | 6 |
| Region, n | |||
| USA | 12 | 4 | 7 |
| Europe | 2 | 0 | 4 |
| Other | 6 | 1 | 6 |
| Traumatic event(s), n | |||
| Deployment/combat | 21 | 0 | 0 |
| Terror | 0 | 4 | 5 |
| Disaster | 0 | 1 | 5 |
| Injury/disease | 0 | 0 | 6 |
| Study size, n | |||
| 100‐<500 | 9 | 0 | 6 |
| 500‐<3000 | 3 | 2 | 1 |
| 3000+ | 8 | 3 | 10 |
| Men, % mean (range) | 93.9 (72–100) | 67.7 (41–86) | 43.6 (0–82) |
| Age, years, mean at baseline (range) | 31.6 (23–59) | 43.4 (40–45) | 41.0 (20–70) |
| Number of assessments, mean (range) | 3.9 (3–6) | 3.6 (3–4) | 3.5 (3–7) |
| Duration of follow‐up, months (mean, range) | 130 (7–420) | 112 (54–144) | 43 (12–144) |
| Method of data collection, % | |||
| Questionnaire | 17 | 4 | 8 |
| Interview | 0 | 1 | 8 |
| Expert | 3 | 0 | 1 |
| PTSD symptom scale, % | |||
| PCL | 11 | 5 | 4 |
| CAPS | 4 | 0 | 2 |
| Other | 5 | 0 | 11 |
| PTSD symptom trajectory, % (mean) | |||
| No delayed‐onset track, n | 3 | 0 | 10 |
| Resilient, mean % | 74.9 | 71.1 | 63.8 |
| Delayed‐onset, mean % | 11.9 | 11.1 | 8.3 |
| Other, mean % | 13.2 | 17.8 | 27.9 |
| High homogeneity, % | 52.9 | 60.0 | 70,5 |
| Participation at baseline <75%, % | 80 | 80 | 70 |
| Attrition from baseline to latest follow‐up >25%, % | 85 | 80 | 65 |
The majority of studies were carried out in the USA during the past 5–10 years and most addressed military deployment. Therefore, young men are overrepresented. The number of assessments spanned 3–7 and the duration of follow‐up was longer than 5 years in 45% of studies and longer than 10 years in 29% of studies.
Data were collected by self‐report questionnaires in the majority of studies (69%), but structured interviews by telephone or face‐to‐face were feasible for example in studies of consecutive series of injured patients. The posttraumatic stress disorder checklist (PCL) with 17 items corresponding to DSM‐IV/DSM‐IV‐TR PTSD symptoms was the scale used most often to quantify PTSD symptom intensity (42.9%), but in total 8 different scales were applied—all with reference to the DSM‐IV/DSM‐IV‐TR classification.
About 75% of studies suffered from low baseline participation rates and/or high loss to follow‐up (Table 1).
3.2. PTSD trajectories
In 13 study populations, the latent class growth analyses did not reveal delayed symptom trajectories. In the 29 populations with delayed trajectories, the homogeneity was considered higher according to the specified criteria in 17 populations (59%). Characteristics of studies with and without delayed symptom trajectories are displayed in Supplementary Material (Appendix S5).
In total, 110 data points (PTSD sumscore/months since traumatic exposure) were extracted from studies with delayed trajectories. In military personnel, the median PTSD symptom sumscore was about 25% higher at 12 months postdeployment compared to levels before and during deployment in individuals on the delayed trajectory (Table 2, crude median 34.8%–9.3% = 25.5%, weighted median 35.1%–8.0% = 27.1%). From this level, the difference widened and reached a plateau 40–50% higher after return from deployment (Table 2, Figure 1A). The trajectories in the subsample of more homogeneous studies (44 of the 64 observations) were much alike the trajectories in the entire sample of military personnel, but with less variation (Table 2).
TABLE 2.
Crude and weighted a mean difference of PTSD symptom sumscore between delayed and low‐stable trajectories across follow‐up given as percentage of scale range. Stratification on homogeneity of studies and type of population
| Months after trauma | High homogeneity n = 75 | High and low homogeneity n = 110 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean | Weighted mean | median | Min‐max | n | Mean | Weighted mean | Median | Min‐max | |
| Military | ||||||||||
| Before/during | 9 | 10.6 | 9.2 | 6.6 | 0.4–33.9 | 14 | 11.2 | 9.3 | 8.0 | 0.4–33.9 |
| >0 – 6 | 9 | 14.5 | 13.4 | 11.6 | 3.3–28.4 | 10 | 16.2 | 14.8 | 13.5 | 3.3–30.7 |
| > 6–12 | 8 | 23.2 | 24.7 | 28.2 | 2.4–41.0 | 11 | 28.7 | 34.8 | 35.1 | 2.4–50.6 |
| >12–36 | 7 | 27.5 | 11.9 | 14.2 | 7.8–56.9 | 8 | 24.6 | 10.2 | 11.8 | 3.9–56.9 |
| >36–60 | 4 | 31.9 | 29.8 | 33.3 | 16.8–44.0 | 6 | 37.4 | 40.8 | 39.8 | 16.8–50.1 |
| >60–120 | 5 | 39.6 | 39.5 | 38.9 | 24.5–54.2 | 8 | 38.1 | 39.2 | 40.9 | 6.7–54.2 |
| >120 | 2 | 53.8 | 53.8 | 53.8 | 50.9–56.8 | 8 | 38.0 | 38.4 | 40.8 | 1.2–56.8 |
| Professionals | ||||||||||
| Before/during | ||||||||||
| >0–6 | 0 | |||||||||
| > 6–12 | 0 | |||||||||
| >12–36 | 3 | 12,5 | 18.0 | 19.6 | −2.1–20.1 | 6 | 19.2 | 19.2 | −19.8 | −1.2–35.9 |
| >36–60 | 1 | 36.6 | 36.6 | 36.6 | ‐ | 3 | 32.4 | 36.0 | 39.2 | 24.6–36.6 |
| >60–120 | 5 | 30.4 | 39.2 | 37.1 | 7.7–51.3 | 7 | 32.9 | 40.9 | 37.1 | 7.7–51.3 |
| >120 | 1 | 26.5 | 26.5 | 26.5 | ‐ | 2 | 46.2 | 49.4 | 46.2 | 26.5–65.9 |
| Civilians | ||||||||||
| Before/during | 1 | 7.5 | 7.5 | 7,5 | ‐ | 2 | 10.8 | 11.2 | 10.8 | 7.5–14.1 |
| >0 – 6 | 8 | 13,3 | 25,7 | 12,0 | 3,5–26.1 | 9 | 12.3 | 14.6 | 10.2 | 3.5–26.1 |
| > 6–12 | 4 | 26,1 | 28.4 | 27,6 | 14.6–34.8 | 6 | 25.4 | 28.3 | 27.4 | 14.6–34.8 |
| >12–36 | 5 | 36.1 | 34.6 | 41,2 | 13.8–60.4 | 6 | 34.8 | 32.5 | 34.5 | 13.8–60.4 |
| >36–60 | 0 | 1 | 9.7 | 9.7 | 9.7 | ‐ | ||||
| >60–120 | 2 | 20.8 | 19.0 | 20,8 | 10.3–31.3 | 2 | 20.8 | 17.0 | 10.3 | 10.3–31.3 |
| >120 | 1 | 39.0 | 39.0 | 39.0 | ‐ | 1 | 39.0 | 39.0 | 39.0 | ‐ |
Mean weighted by sample size.
FIGURE 1.
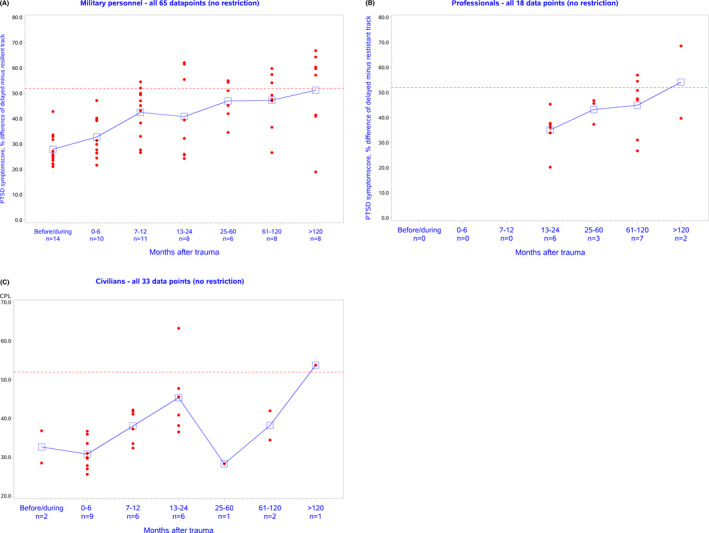
(A–C) Scatter plots and mean crude differences of PTSD symptom sumscore between delayed and low‐stable trajectories across follow‐up given as percentage of scale range. No restriction by level of homogeneity. Dotted line indicates level of probable PTSD. (A) Military personnel; (B) Professionals; (C) Civilians
Compared to military personnel, the trajectories among civilians were different with a higher initial level of PTSD symptom sumscores and a flatter slope (Table 2, Figure 1C). Professionals seemed in between, but data for this group were sparse (Table 2, Figure 1B). The corresponding plots with restriction to studies with higher homogeneity were similar. In all groups, the variation was large as indicated by the scatter plots (Figure 1A‐C).
Analyses stratified by duration of follow‐up (<=/> 5 years) did not indicate that the difference in PTSD symptom levels during the initial year was less in studies with long follow‐up compared to short follow‐up [27.0% (SE 2.5) versus 24.4% (SE 2.2)].
3.3. Trauma severity and stressful life events
Six studies reported a significant higher risk of a delayed trajectory in individuals with more severe exposure to trauma than in individuals with lower traumatic exposure with relative risk spanning 1.07 (95% CI 1.02–1.12) and 3.58 (95% CI 2.95–4.34), 23 , 39 , 41 , 46 , 48 , 53 Table 3. One study did not observe increased risk according to the severity of combat experience in either a group with combat stress reaction and another without, 37 adjusted OR 0.96 (95% CI 0.63–1.48) and 0.87 (95% CI 0.55–1.36). Moreover, four studies did not observe significant associations between indicators of trauma severity and delayed‐onset trajectory but did not report relative risks. 28 , 29 , 30 , 31 The studies used different measures of frequency or severity of traumatic events and therefore computing a common average risk estimate is not appropriate. Most studies relied on perceived threat which introduces risk of common method bias. Risk estimates in nine studies were adjusted for demographic and socio‐economic factors, but none were adjusted for all a priory defined potential confounding factors.
TABLE 3.
Risk of delayed‐onset trajectory according to frequency or severity of traumatic event(s). Adjusted OR with 95% CI
| Reference | Population | Trauma ascertainment | Exposure contrast | OR | 95%CI | Adjustment a |
|---|---|---|---|---|---|---|
| Dickstein 2010 (74) | Peacekeeping soldiers | Peacekeeping event scale | Combat exposure yes/no | No significant effect | NR | 4 |
| Karstoft 2013 (83) | Deployed soldiers with combat stress reaction | Perceived severity of battle, 4‐ point scale | Severity of battle vs none | 0.96 | 0.63–1.48 | Adjustment by latent class |
| Deployed soldiers without combat stress reaction | Perceived severity of battle, 4‐ point scale | Severity of battle vs none | 0.87 | 0.55–1.36 | Adjustment by latent class | |
| Deployed soldiers with combat stress reaction | Perceived combat life threat, 5 point scale | Level of threat | 1.90 | 1.08–3.35 | Adjustment by latent class | |
| Deployed soldiers without combat stress reaction | Perceived combat life threat, 5 point scale | Level of threat | 0.95 | (0.64–1.43) | Adjustment by latent class | |
| Lowe 2014 (85) | Urban residents | Telephone interview 20 item trauma questionnaire during life | Number of traumatic events | 1.13 | 1.04–1.22 | Adjustment for years since events |
| Bryant 2015 (73) | Injured patients | Records | Injury severity score 1–5 | No significant effect | NR | 5 |
| Maslow 2015 (87) | 9/11 rescue, recovery, and clean‐up workers | Telephone interview, ad hoc questionnaire on 7 traumatic exposures | Fear injured/killed yes/no b | 3.58 | 2.95–4.34 | 4 |
| Bromet 2016 (101) | 9/11 responders, police | Six items on WTC exposure severity | Intermediate (3–4) versus (0–2) | 2.8 | 1.4–5.6 | 5 |
| Six items on WTC exposure severity | High (5–6) versus low (0–2) | 4.8 | 2.4–9.8 | 5 | ||
| 9/11 responders, non‐traditional | Six items on WTC exposure severity | Intermediate (3–4) versus low (0–2) | 1.9 | 1.2–2.9 | 5 | |
| Six items on WTC exposure severity | High (5–6) versus low (0–2) | 3.4 | 1.9–6.2 | 5 | ||
| Eekhout 2016 (76) | Deployed soldiers | Deployment stressor list, 19 items | Level of deployment stressors | Significantly increased | NR | Adjustment? |
| Feder 2016 (70) | World Trade Center Police | World Trade Center exposure inventory, 10 items | Count of 10 exposures | 1.13 | 1.03–1.23 | Adjustment? |
| World Trade Center non‐traditional | World Trade Center exposure inventory, 10 items | Count of 10 exposures | 1.14 | 1.07–1.22 | Adjustment? | |
| (68)Welch 2016 (99) | Residents and area workers | Telephone interview, ad hoc questionnaire on 7 traumatic exposures | Threat 9/11 injury/death yes/no b | 1.44 | 1.21–1.71 | 5 |
| Donoho 2017 (75) | Deployed soldiers | Ad hoc 5 items | Combat exposure yes/no | No significant effect | NR | 6 |
| Polusny 2017 (94) | National Guard soldiers | Deployment risk and resilience Inventory | Combat exposure, scale? | 1.07 | 1.02–1.12 | Adjustment? |
| Palmer 2019 (92) | Deployed soldiers | Records on parent unit equivalent with role in combat | Combat role versus support role | 3.13 | 1.85–5.26 | 3 |
| Lowe 2020(68) | Injured patients | Records | Exposed to assault versus motor vehicle accident | 2.67 | 1.32–5.4 | 4 |
NR, not reported; NS: p> 0.05.
Number of determinants adjusted for by analysis or design from the following list of 6 categories of established potential confounders: sex, age, socio‐economic position, previous mental health, previous somatic health, childhood abuse.
Five other 9/11 trauma direct and indirect trauma exposure indices were all significantly related to the delayed‐onset trajectory.
Five studies reported increased risk of a delayed trajectory by exposure to stressful life events during the follow‐up period with relative risk spanning 1.23 (95% CI 1.03–1.45) and 7.77 (95% CI 5.15–11.7), 23 , 28 , 39 , 41 , 48 Table 4. The severity of the traumatic exposure was measured by different trauma inventories with 2–20 items, some addressing the specific traumatic events in question. No studies reported effects of interaction between the trauma and post‐trauma stressors.
TABLE 4.
Risk of delayed‐onset trajectory according to post‐trauma stressor frequency or severity. Adjusted OR with 95% CI
| Reference | Population | Trauma ascertainment | Exposure contrast | OR | 95%CI | Adjustment a |
|---|---|---|---|---|---|---|
| Lowe 2014 | Urban residents | Telephone interview 20 item trauma questionnaire during life | Number of traumatic events 2 years after baseline interview | 1.69 | 1.43–1.99 | Adjustment for years since events |
| Bryant 2015 | Injured patients | Self‐report (Recent Life Events Questionnaire) | Traumatic or aversive stressful life events past 12 months during follow‐up | 1.55 | 1.31–1.84 | 5 (only bivariate significant included) |
| Traumatic or aversive stressful life events past 24 months during follow‐up | 1.05 | 0.90–1.11 | 5 (only bivariate significant included) | |||
| Maslow 2015 | 9/11 rescue. recovery and clean‐up workers | Telephone interview. ad hoc questionnaire on 7 traumatic exposures | Loss of job due to 9/11 yes/no | 7.77 | 5.15–11.72 | 4 |
| Feder 2016 | World Trade Center Police | Web‐based survey on life stressors at follow‐up | n of 3 additional life stressors since 9/11 | 1.42 | 1.09–1.86 | Adjustment? |
| World Trade Center non‐traditional | Web‐based survey on life stressors at follow‐up | n of 3 additional life stressors since 9/11 | 1.23 | 1.03–1.45 | Adjustment? | |
| Polusny 2017 | National Guard soldiers | Deployment risk and resilience Inventory | Postdeployment stressful life events | 1.44 | 1.05–1.96 | Adjustment? |
Number of determinants adjusted for by analysis or design from the following list of 6 categories of established potential confounders: sex, age, socio‐economic position, previous mental health, previous somatic health, childhood abuse.
4. DISCUSSION
The trajectory analyses demonstrate substantial heterogeneity of average PTSD symptoms following a potentially traumatic event as also described in earlier reviews. 19 , 20 The typical course is not dichotomous with a low stable (resistant/resilient) and an improving (recovering) trajectory, but also includes high stable (chronic), worsening (delayed), and sometimes fluctuating symptom trajectories. The trajectory analyses were performed during past two decades and all studies applied PTSD symptom inventories based upon DSM‐IV/DSM‐IV‐TR criteria. Although not less than eight different instruments and symptom scoring algorithms were used to quantify PTSD symptoms, the comparability across studies seems high because the same set of 17 specified PTSD symptoms was predominant.
4.1. Studies with delayed PTSD trajectories
In 29 of the 42 study populations, a delayed PTSD trajectory was revealed. The latent class grow analyses are explorative and do not allow predefined specific hypotheses with respect to the time course of symptoms. Although this data‐driven approach is a limitation, the data do consistently indicate that individuals on track to develop PTSD satisfying all diagnostic criteria have on average elevated symptom levels already during the first year after the potential traumatic events. However, several limitations need to be acknowledged. First, the variation in time‐specific PTSD symptom levels across study populations is large and quantitative data on variation within studies are only provided in few studies. 20 , 22 , 36 , 55 , 56 Therefore, a formal meta‐analysis with statistical evaluation of the initial difference of PTSD symptom levels between delayed and low‐stable trajectories could not be performed. However, in each of the studies with applicable information, the delayed trajectory was highly significantly above the low‐stable trajectory, also in the initial phase. Insufficient statistical power may not be an issue, but the confidence limits for the magnitude of the difference cannot be computed. Second, although the average level of PTSD symptoms is substantially elevated during the first year after the potentially traumatic event(s) in individuals on the delayed trajectory, there may still be some (probably few) with a silent course of symptoms, that are hidden within the entire group of people on the delayed trajectory. Third, studies with short follow‐up periods are not informative with respect to occurrence of delayed‐onset PTSD with a long interval without symptoms. Nevertheless, 14 populations with follow‐up exceeding 5 years were also characterized with substantially elevated average PTSD symptom levels during the initial years. Fourth, it should be acknowledged that only an unreported and probably unknown proportion of individuals with worsening symptoms become clinical cases, and these persons may have a trajectory that deviates from the average. Fifth, stressful life events during follow‐up may be a major determinant for delayed‐onset of PTSD, 57 but is not accounted for by the trajectory analyses. If stressful life events during follow‐up are important, failure to account for these may decrease chances to detect delayed‐onset PTSD without bridging symptoms.
Baseline participation and loss to follow‐up exceeded 30% in the majority of trajectory analysis studies, but it is hard to speculate how selection and attrition issues would systematically bias differences between delayed and low‐stable trajectories toward falsely larger values. Moreover, 13 studies reporting results of drop‐out analyses did not raise concern for systematic bias of trajectory analyses. 27 , 31 , 36 , 38 , 42 , 43 , 44 , 46 , 48 , 49 , 53 , 58 , 59 In summary, the trajectory analyses revealing delayed trajectories consistently indicate that individuals on the delayed trajectory had on average 25–30% higher initial PTSD symptom levels relative to individuals on the low‐stable trajectory.
4.2. Studies without delayed PTSD trajectories
In 13 of the 42 study populations, the latent growth analysis did not result in a delayed type of PTSD symptom trajectory characterized by an increasing level of symptoms across time, which may/may not reach a plateau at a high level during the follow‐up period. There are several reasons why the statistical modeling may not identify this type of trajectory even when delayed‐onset cases without bridging symptoms are present in the sample. First, the sample size may be too small to allow detection of an infrequent trajectory 20 : the proportion of studies with less than 500 participants was 46% in studies without delayed‐onset trajectories and 31% in those with. Second, the follow‐up period may be too short. Case reports suggest that delayed‐onset PTSD can develop several years and even decades after the assumed traumatizing event 13 , 14 , 15 , 60 , 61 , 62 , 63 , 64 : The average duration of follow‐up was 66.7 months in studies not displaying delayed‐onset trajectories and 105.5 months in those that did. Third, contextual factors may influence reporting of PTSD symptoms—for instance military personal and professionals may be reluctant to acknowledge and report PTSD symptoms because it may be incompatible with the organizational climate and job performance: the majority of studies revealing a delayed trajectory addressed military personnel and other professionals (76% versus 24%). Finally, loss to follow‐up may be differential, because people, that experience worsening PTSD symptoms, may be less likely to participate in the later follow‐up assessments. However, no major difference was found in the proportion of loss to follow‐up in studies with and without delayed trajectories (65% versus 60%), but many studies did not provide data on loss to follow‐up (41% and 23%, respectively). In summary, the trajectory analyses failing to demonstrate delayed trajectories do not provide strong evidence against the occurrence of delayed‐onset PTSD without bridging symptoms.
4.3. Previous literature
The results of the trajectory analyses are supported by a range of prospective epidemiological studies with quantitative data on PTSD symptom intensity during the initial months after the trauma and later individual clinical diagnosis of PTSD with delayed expression. 4 , 8 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 But findings seem to contrast with several earlier case reports from the last decades of the 20th century describing PTSD in military veterans that were diagnosed with PTSD up to 40 years after severe traumatic experiences supposed to be necessary but not sufficient causes of the disorder. 12 , 13 , 14 , 15 , 60 , 61 , 63 , 64 , 75 , 76 However, case reports provide only weak evidence for causal relations. Of notice, all case reports describe direct traumatic exposures at the absolute extreme of life‐threatening experiences, and all seemed to be triggered by recent life events often with specific reminders of the initial traumas.
4.4. Clinical relevance of subsyndromal PTSD symptoms
Are 25–30% higher initial PTSD symptom levels marginal or clinically relevant? The symptom inventory most often used in the included studies is the posttraumatic disorder checklist PCL with 17 items corresponding to the 17 PTSD symptoms in the DSM‐IV symptom clusters BD. 77 Respondents indicate how much they have been bothered the last month on a scale ranging from 1 (not at all) to 5 (extremely) and accordingly, the sumscore across all 17 items is from 17 through 85. In the 18 PTSD trajectory studies using the PCL scale, the average score during the first year post‐trauma was 22.4 in the low‐stable group and 41.5 in the delayed group. This may be benchmarked with a score of ≥44 or ≥50 that has been suggested as appropriate cutoffs for identifying probable PTSD. 77 , 78
Subthreshold PTSD has consistently been associated with elevated levels of depression and suicidal ideation in veteran populations 79 and other professional groups. 80 For instance, a Korean cross‐sectional study of 45 698 current firefighters found a prevalence of PTSD according to DSM‐5 criteria of 2.6% and subthreshold PTSD defined by 6 different sets of symptoms in 1.8–18%. 81 Subthreshold PTSD by all definitions was significantly associated with suicidal behavior, depression, alcohol use problems, and functional impairment—even in the most relaxed definitions of subthreshold PTSD based upon at least one DSM‐5 symptom from each of the five symptom clusters, B‐F rated 2 or higher (moderately to extremely). Similarly, McLaughlin et al found that the presence of two DSM‐5 symptoms from any of the symptom clusters was strongly related to clinically significant distress or impairment and comorbid disorders with odds ratios 9.7 (95% CI 2.2–42.7) and 3.0 (95% CI 1.7–5.2), respectively. 82 This study was based upon cross‐sectional WHO administered data from 13 countries including 23 936 individuals. All data in these studies were self‐reported. Finally, meta‐analytic findings suggest that subthreshold PTSD may develop into delayed‐onset PTSD. 7 Among individuals initially classified as having subthreshold PTSD, 26.2% developed delayed‐onset PTSD compared to 4.1% of individuals with less or no initial symptoms. Summing up, considering the level of initial PTSD symptoms in delayed‐onset PTSD and several studies of clinical correlates of subthreshold PTSD, it seems likely that bridging symptoms in delayed‐onset PTSD often are of clinical relevance.
4.5. Heterogeneity across populations
The trajectory data suggest that PTSD symptoms among individuals on the delayed trajectory increase at a lower rate among military personnel, but lacking information on variability and large heterogeneity across studies precludes meta‐analysis and statistical evaluation. Moreover, we were not able to evaluate how treatment intervention in the initial phase as debriefing might influence the symptom trajectories.
4.6. Implications of trauma severity
It is generally acknowledged and psychologically plausible that trauma severity and frequency are related to increased risk of PTSD, 10 but the evidence is less substantial when it comes to delayed‐onset PTSD. Findings in prospective studies are mixed with some studies reporting increased risk and others no risk. Comparison of studies is difficult because of different measures of trauma severity. The same applies to effect of post‐trauma stressful life events. Since exposure is included in the definition of PTSD, cases with less severe exposure may not be labeled PTSD causing more severe events to appear riskier—given that less severe exposures are true causes of delayed‐onset PTSD. Moreover, common method bias because of self‐reported trauma exposure would bias risk estimates in the same direction and cannot be ruled out with confidence.
4.7. Stressful life events
Of particular interest from an etiological point of view are studies of interaction between the primary trauma and later occurrence of stressful life events. The studies reviewed here do not contribute evidence on this and only few prospective epidemiological studies have so far explicitly addressed this issue. A study of 814 Dutch soldiers deployed in Afghanistan with 26 months postdeployment follow‐up assessment, postdeployment stressors prospectively predicted a steeper PTSD symptom trajectory in high combat exposed soldiers compared to low combat exposed soldiers. 57 Another study examined PTSD symptom trajectories among World Trade Center Health Registry enrollees some of which later were exposed to Hurricane Sandy that struck New York in 2013. 83 Among individuals with 9/11 traumatic exposure, those who also experienced high exposure to Hurricane Sandy were at higher risk of probable delayed‐onset PTSD than those with low Hurricane Sandy exposure. These results are compatible with the hypothesis that Hurricane Sandy may have exacerbated subthreshold or previously resolved symptoms of 9/11‐related PTSD. It seems that that ongoing stressors may play a central role in explaining the trajectory of posttraumatic stress over time, and that factors beyond the experience of stressors and traumas may account for sex and ethnic differences in posttraumatic stress risk. 84 Even neurobiological mechanistic insight supports the plausibility of sensitization and triggering effects of renewed traumatic exposure (Smid et al., submitted for publication), there is an obvious need to corroborate these findings in epidemiologic studies.
5. CONCLUSION
In summary, several large epidemiological studies of populations exposed to trauma with prospective collection of outcome data provide consistent evidence that individuals with delayed PTSD symptoms have on average about 25–30% higher symptoms during the initial months compared to individuals with a low‐stable trajectory. This applies to both military personnel, professionals, and civilians and is not restricted to studies with shorter follow‐up. These findings do not exclude that few persons without PTSD symptoms bridging the traumatic exposure and the PTSD diagnosis are hidden in the average and typical trajectories. To examine the long‐term unbiased risk of PTSD, we need prospective controlled studies with a measure of PTSD symptoms, that is defined independently of specific traumatic events. Findings indicating effects of trauma severity and post‐trauma stressful life events on the occurrence of delayed‐onset PTSD are sparse and/or conflicting and replication in studies explicitly designed to address these issues is needed.
The results underpin the rationale for monitoring PTSD symptoms during the initial periods after traumatic events in order to identify persons at risk of later development of PTSD. Moreover, our findings inform forensic assessments that PTSD with delayed expression rarely develops in the absence of any symptoms bridging the interval between exposure to the traumatic event and onset of full‐blown PTSD.
CONFLICTS OF INTERESTS
None declared.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1111/acps.13372.
Supporting information
Supplementary Material
ACKNOWLEDGMENT
The Danish Work Environment Fund provided a grant for the study on 17 December 2020 (J.nr. 20205100927). Research librarian Elizabeth Bengtsen is thanked for skillful assistance with literature searching and with getting access to full‐text papers.
Bonde JPE, Jensen JH, Smid GE, et al. Time course of symptoms in posttraumatic stress disorder with delayed expression: A systematic review. Acta Psychiatr Scand.2022;145:116–131. doi: 10.1111/acps.13372
DATA AVAILABILITY STATEMENT
All data included in this paper are available from public sources. A file with readings from figures in original articles may be provided by mail to the corresponding author.
REFERENCES
- 1. Diagnostic and Statistical Manual of Mental Disorders 3th ed. DSM III 1980. Washington, DC: Amercian Psychiatric Association; 1980. [Google Scholar]
- 2. Brewin CR. "I wouldn't start from here"–an alternative perspective on PTSD from the ICD‐11: comment on Friedman (2013). J Trauma Stress. 2013;26(5):557‐559. [DOI] [PubMed] [Google Scholar]
- 3. Solomon Z, Shklar R, Singer Y, Mikulincer M. Reactions to combat stress in Israeli veterans twenty years after the 1982 Lebanon war. J Nerv Ment Dis. 2006;194(12):935‐939. [DOI] [PubMed] [Google Scholar]
- 4. Bryant RA, Harvey AG. Delayed‐onset posttraumatic stress disorder: a prospective evaluation. Aust N Z J Psychiatry. 2002;36(2):205‐209. [DOI] [PubMed] [Google Scholar]
- 5. Andrews B, Brewin CR, Philpott R, Stewart L. Delayed‐onset posttraumatic stress disorder: a systematic review of the evidence. Am J Psychiatry. 2007;164(9):1319‐1326. [DOI] [PubMed] [Google Scholar]
- 6. Smid GE, Mooren TT, van der Mast RC, Gersons BP, Kleber RJ. Delayed posttraumatic stress disorder: systematic review, meta‐analysis, and meta‐regression analysis of prospective studies. J Clin Psychiatry. 2009;70(11):1572‐1582. [DOI] [PubMed] [Google Scholar]
- 7. Utzon‐Frank N, Breinegaard N, Bertelsen M, et al. Occurrence of delayed‐onset post‐traumatic stress disorder: a systematic review and meta‐analysis of prospective studies. Scand J Work Environ Health. 2014;40(3):215‐229. [DOI] [PubMed] [Google Scholar]
- 8. O'Donnell ML, Varker T, Creamer M, et al. Exploration of delayed‐onset posttraumatic stress disorder after severe injury. Psychosom Med. 2013;75(1):68‐75. [DOI] [PubMed] [Google Scholar]
- 9. Friedman MJ, Resick PA, Bryant RA, Brewin CR. Considering PTSD for DSM‐5. Depress Anxiety. 2011;28(9):750‐769. [DOI] [PubMed] [Google Scholar]
- 10. Friedman MJ, Resick PA, Bryant RA, Strain J, Horowitz M, Spiegel D. Classification of trauma and stressor‐related disorders in DSM‐5. Depress Anxiety. 2011;28(9):737‐749. [DOI] [PubMed] [Google Scholar]
- 11. Andrews B, Brewin CR, Stewart L, Philpott R, Hejdenberg J. Comparison of immediate‐onset and delayed‐onset posttraumatic stress disorder in military veterans. J Abnorm Psychol. 2009;118(4):767‐777. [DOI] [PubMed] [Google Scholar]
- 12. Solomon Z, Kotler M, Shalev A, Lin R. Delayed onset PTSD among Israeli veterans of the 1982 Lebanon War. Psychiatry. 1989;52(4):428‐436. [DOI] [PubMed] [Google Scholar]
- 13. Ramchandani D. Distinguishing features of delayed‐onset posttraumatic stress disorder. Bull Menninger Clin. 1990;54(2):247‐254. [PubMed] [Google Scholar]
- 14. Pomerantz AS. Delayed onset of PTSD: delayed recognition or latent disorder? Am J Psychiatry. 1991;148(11):1609. [DOI] [PubMed] [Google Scholar]
- 15. Herrmann N, Eryavec G. Delayed onset post‐traumatic stress disorder in World War II veterans. Can J Psychiatry. 1994;39(7):439‐441. [DOI] [PubMed] [Google Scholar]
- 16. World Health Organisation . International Classification of Diseases 11th Revision, ICD‐11. The Global Standard for Diagnostic Health Information. Geneva: World Health Organisation; 2018. [Google Scholar]
- 17. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 18. Vestre landsret dom afsagt den 26 . juni 2020 (In Danish). Danske Domstole. https://elmer‐adv.dk/wp‐content/uploads/2020/10/Vestre‐Landsrets‐dom‐af‐26.‐juni‐2020‐anonymiseret.pdf. Accessed 26.6.2020,
- 19. Galatzer‐Levy IR, Huang SH, Bonanno GA. Trajectories of resilience and dysfunction following potential trauma: A review and statistical evaluation. Clin Psychol Rev. 2018;63:41‐55. [DOI] [PubMed] [Google Scholar]
- 20. Lowe SR, Ratanatharathorn A, Lai BS, et al. Posttraumatic stress disorder symptom trajectories within the first year following emergency department admissions: pooled results from the International Consortium to predict PTSD. Psychol Med. 2021;51(7):1129‐1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Inc. SI . SAS Studio. 9.04 ed, vol 1. Cary: SAS Institute Inc; 2012. ‐2018. [Google Scholar]
- 22. Andersen SB, Karstoft KI, Bertelsen M, Madsen T. Latent trajectories of trauma symptoms and resilience: the 3‐year longitudinal prospective USPER study of Danish veterans deployed in Afghanistan. J Clin Psychiatry. 2014;75(9):1001‐1008. [DOI] [PubMed] [Google Scholar]
- 23. Feder A, Mota N, Salim R, et al. Risk, coping and PTSD symptom trajectories in World Trade Center responders. J Psychiatr Res. 2016;82:68‐79. [DOI] [PubMed] [Google Scholar]
- 24. Rothman KJ, Greenland S. Modern Epidemiology. Philadelphia: Lippincott‐Raven; 2008. [Google Scholar]
- 25. Adams SW, Allwood MA, Bowler RM. Posttraumatic stress trajectories in world trade center tower survivors: hyperarousal and emotional numbing predict symptom change. J Trauma Stress. 2019;32(1):67‐77. [DOI] [PubMed] [Google Scholar]
- 26. Armour C, Shevlin M, Elklit A, Mroczek D. A latent growth mixture modeling approach to PTSD symptoms in rape victims. Traumatology (Tallahass Fla). 2012;18(1):20‐28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Boasso AM, Steenkamp MM, Nash WP, Larson JL, Litz BT. The relationship between course of PTSD symptoms in deployed U.S. Marines and degree of combat exposure. J Trauma Stress. 2015;28(1):73‐78. [DOI] [PubMed] [Google Scholar]
- 28. Bryant RA, Nickerson A, Creamer M, et al. Trajectory of post‐traumatic stress following traumatic injury: 6‐year follow‐up. Br J Psychiatry. 2015;206(5):417‐423. [DOI] [PubMed] [Google Scholar]
- 29. Dickstein BD, Suvak M, Litz BT, Adler AB. Heterogeneity in the course of posttraumatic stress disorder: trajectories of symptomatology. J Trauma Stress. 2010;23(3):331‐339. [DOI] [PubMed] [Google Scholar]
- 30. Donoho CJ, Bonanno GA, Porter B, Kearney L, Powell TM. A decade of war: prospective trajectories of posttraumatic stress disorder symptoms among deployed US military personnel and the influence of combat exposure. Am J Epidemiol. 2017;186(12):1310‐1318. [DOI] [PubMed] [Google Scholar]
- 31. Eekhout I, Reijnen A, Vermetten E, Geuze E. Post‐traumatic stress symptoms 5 years after military deployment to Afghanistan: an observational cohort study. Lancet Psychiatry. 2016;3(1):58‐64. [DOI] [PubMed] [Google Scholar]
- 32. Galovski TE, Peterson ZD, Fox‐Galalis A. Trajectories of posttraumatic stress and depression in police and community members following the violence during civil unrest in ferguson. Missouri. Am J Community Psychol. 2018;62(3–4):433‐448. [DOI] [PubMed] [Google Scholar]
- 33. Ginzburg K, Ein‐Dor T. Posttraumatic stress syndromes and health‐related quality of life following myocardial infarction: 8‐year follow‐up. Gen Hosp Psychiatry. 2011;33(6):565‐571. [DOI] [PubMed] [Google Scholar]
- 34. Habibović M, Denollet J, Pedersen SS. Posttraumatic stress and anxiety in patients with an implantable cardioverter defibrillator: Trajectories and vulnerability factors. Pacing Clin Electrophysiol. 2017;40(7):817‐823. [DOI] [PubMed] [Google Scholar]
- 35. Hobfoll SE, Mancini AD, Hall BJ, Canetti D, Bonanno GA. The limits of resilience: distress following chronic political violence among Palestinians. Soc Sci Med. 2011;72(8):1400‐1408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Johannesson KB, Arinell H, Arnberg FK. Six years after the wave. Trajectories of posttraumatic stress following a natural disaster. J Anxiety Disord. 2015;36:15‐24. [DOI] [PubMed] [Google Scholar]
- 37. Karstoft KI, Armour C, Elklit A, Solomon Z. Long‐term trajectories of posttraumatic stress disorder in veterans: the role of social resources. J Clin Psychiatry. 2013;74(12):e1163‐e1168. [DOI] [PubMed] [Google Scholar]
- 38. Le Brocque RM, Hendrikz J, Kenardy JA. Parental response to child injury: examination of parental posttraumatic stress symptom trajectories following child accidental injury. J Pediatr Psychol. 2010;35(6):646‐655. [DOI] [PubMed] [Google Scholar]
- 39. Lowe SR, Galea S, Uddin M, Koenen KC. Trajectories of posttraumatic stress among urban residents. Am J Community Psychol. 2014;53(1–2):159‐172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Lowe SR, Joshi S, Pietrzak RH, Galea S, Cerdá M. Mental health and general wellness in the aftermath of Hurricane Ike. Soc Sci Med. 2015;124:162‐170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Maslow CB, Caramanica K, Welch AE, Stellman SD, Brackbill RM, Farfel MR. Trajectories of scores on a screening instrument for PTSD among world trade center rescue, recovery, and clean‐up workers. J Trauma Stress. 2015;28(3):198‐205. [DOI] [PubMed] [Google Scholar]
- 42. Nash WP, Boasso AM, Steenkamp MM, Larson JL, Lubin RE, Litz BT. Posttraumatic stress in deployed Marines: prospective trajectories of early adaptation. J Abnorm Psychol. 2015;124(1):155‐171. [DOI] [PubMed] [Google Scholar]
- 43. Norris FH, Tracy M, Galea S. Looking for resilience: understanding the longitudinal trajectories of responses to stress. Soc Sci Med. 2009;68(12):2190‐2198. [DOI] [PubMed] [Google Scholar]
- 44. Orcutt HK, Erickson DJ, Wolfe J. The course of PTSD symptoms among Gulf War veterans: a growth mixture modeling approach. J Trauma Stress. 2004;17(3):195‐202. [DOI] [PubMed] [Google Scholar]
- 45. Orcutt HK, Bonanno GA, Hannan SM, Miron LR. Prospective trajectories of posttraumatic stress in college women following a campus mass shooting. J Trauma Stress. 2014;27(3):249‐256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Palmer L, Thandi G, Norton S, et al. Fourteen‐year trajectories of posttraumatic stress disorder (PTSD) symptoms in UK military personnel, and associated risk factors. J Psychiatr Res. 2019;109:156‐163. [DOI] [PubMed] [Google Scholar]
- 47. Pietrzak RH, Van Ness PH, Fried TR, Galea S, Norris FH. Trajectories of posttraumatic stress symptomatology in older persons affected by a large‐magnitude disaster. J Psychiatr Res. 2013;47(4):520‐526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Polusny MA, Erbes CR, Kramer MD, et al. Resilience and posttraumatic stress disorder symptoms in national guard soldiers deployed to Iraq: A prospective study of latent class trajectories and their predictors. J Trauma Stress. 2017;30(4):351‐361. [DOI] [PubMed] [Google Scholar]
- 49. Porter B, Bonanno GA, Frasco MA, Dursa EK, Boyko EJ. Prospective post‐traumatic stress disorder symptom trajectories in active duty and separated military personnel. J Psychiatr Res. 2017;89:55‐64. [DOI] [PubMed] [Google Scholar]
- 50. Sterling M, Hendrikz J, Kenardy J. Compensation claim lodgement and health outcome developmental trajectories following whiplash injury: A prospective study. Pain. 2010;150(1):22‐28. [DOI] [PubMed] [Google Scholar]
- 51. Sakuma A, Ueda I, Shoji W, Tomita H, Matsuoka H, Matsumoto K. Trajectories for post‐traumatic stress disorder symptoms among local disaster recovery workers following the great East Japan earthquake: Group‐based trajectory modeling. J Affect Disord. 2020;274:742‐751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Wang C, Rapp P, Darmon D, et al. Utility of P300 ERP in monitoring post‐trauma mental health: A longitudinal study in military personnel returning from combat deployment. J Psychiatr Res. 2018;101:5‐13. [DOI] [PubMed] [Google Scholar]
- 53. Welch AE, Caramanica K, Maslow CB, Brackbill RM, Stellman SD, Farfel MR. Trajectories of PTSD among lower manhattan residents and area workers following the 2001 world trade center disaster, 2003–2012. J Trauma Stress. 2016;29(2):158‐166. [DOI] [PubMed] [Google Scholar]
- 54. Zerach G, Karstoft KI, Solomon Z. Hardiness and sensation seeking as potential predictors of former prisoners of wars’ posttraumatic stress symptoms trajectories over a 17‐year period. J Affect Disord. 2017;218:176‐181. [DOI] [PubMed] [Google Scholar]
- 55. Pietrzak RH, Feder A, Singh R, et al. Trajectories of PTSD risk and resilience in World Trade Center responders: an 8‐year prospective cohort study. Psychol Med. 2014;44(1):205‐219. [DOI] [PubMed] [Google Scholar]
- 56. Sterling M, Hendrikz J, Kenardy J. Similar factors predict disability and posttraumatic stress disorder trajectories after whiplash injury. Pain. 2011;152(6):1272‐1278. [DOI] [PubMed] [Google Scholar]
- 57. Smid GE, Kleber RJ, Rademaker AR, van Zuiden M, Vermetten E. The role of stress sensitization in progression of posttraumatic distress following deployment. Soc Psychiatry Psychiatr Epidemiol. 2013;48(11):1743‐1754. [DOI] [PubMed] [Google Scholar]
- 58. Gouweloos‐Trines J, Te Brake H, Sijbrandij M, Boelen PA, Brewin CR, Kleber RJ. A longitudinal evaluation of active outreach after an aeroplane crash: Screening for post‐traumatic stress disorder and depression and assessment of self‐reported treatment needs. Eur J Psychotraumatol. 2019;10(1):1554406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Wang J, Ursano RJ, Gonzalez OI, et al. Association of suicidal ideation with trajectories of deployment‐related PTSD symptoms. Psychiatry Res. 2018;267:455‐460. [DOI] [PubMed] [Google Scholar]
- 60. Christenson RM, Walker JI, Ross DR, Maltbie AA. Reactivation of traumatic conflicts. Am J Psychiatry. 1981;138(7):984‐985. [DOI] [PubMed] [Google Scholar]
- 61. Hamilton JW. Unusual long‐term sequelae of a traumatic war experience. Bull Menninger Clin. 1982;46(6):539‐541. [PubMed] [Google Scholar]
- 62. Van Dyke C, Zilberg NJ, McKinnon JA. Posttraumatic stress disorder: a thirty‐year delay in a World War II veteran. Am J Psychiatry. 1985;142(9):1070‐1073. [DOI] [PubMed] [Google Scholar]
- 63. Pary R, Turns D, Tobias CR. A case of delayed recognition of posttraumatic stress disorder. Am J Psychiatry. 1986;143(7):941. [DOI] [PubMed] [Google Scholar]
- 64. Richmond JS, Beck JC. Posttraumatic stress disorder in a World War II veteran. Am J Psychiatry. 1986;143(11):1485‐1486. [DOI] [PubMed] [Google Scholar]
- 65. McFarlane AC. The aetiology of post‐traumatic stress disorders following a natural disaster. Br J Psychiatry. 1988;152(1):116‐121. [DOI] [PubMed] [Google Scholar]
- 66. Green MM, McFarlane AC, Hunter CE, Griggs WM. Undiagnosed post‐traumatic stress disorder following motor vehicle accidents. Med J Aust. 1993;159(8):529‐534. [DOI] [PubMed] [Google Scholar]
- 67. Buckley TC, Blanchard EB, Hickling EJ. A prospective examination of delayed onset PTSD secondary to motor vehicle accidents. J Abnorm Psychol. 1996;105(4):617‐625. [DOI] [PubMed] [Google Scholar]
- 68. Gray MJ, Bolton EE, Litz BT. A longitudinal analysis of PTSD symptom course: delayed‐onset PTSD in Somalia peacekeepers. J Consult Clin Psychol. 2004;72(5):909‐913. [DOI] [PubMed] [Google Scholar]
- 69. Hepp U, Moergeli H, Buchi S, et al. Post‐traumatic stress disorder in serious accidental injury: 3‐year follow‐up study. Br J Psychiatry. 2008;192(5):376‐383. [DOI] [PubMed] [Google Scholar]
- 70. Berninger A, Webber MP, Niles JK, et al. Longitudinal study of probable post‐traumatic stress disorder in firefighters exposed to the World Trade Center disaster. Am J Ind Med. 2010;53(12):1177‐1185. [DOI] [PubMed] [Google Scholar]
- 71. Goodwin L, Jones M, Rona RJ, Sundin J, Wessely S, Fear NT. Prevalence of delayed‐onset posttraumatic stress disorder in military personnel: is there evidence for this disorder?: Results of a prospective UK cohort study. J Nerv Ment Dis. 2012;200(5):429‐437. [DOI] [PubMed] [Google Scholar]
- 72. Bryant RA, O'Donnell ML, Creamer M, McFarlane AC, Silove D. A multisite analysis of the fluctuating course of posttraumatic stress disorder. JAMA Psychiatry. 2013;70(8):839‐846. [DOI] [PubMed] [Google Scholar]
- 73. Horesh D, Solomon Z, Keinan G, Ein‐Dor T. The clinical picture of late‐onset PTSD: A 20‐year longitudinal study of Israeli war veterans. Psychiatry Res. 2013;12:10. [DOI] [PubMed] [Google Scholar]
- 74. North CS, Oliver J. Analysis of the longitudinal course of PTSD in 716 survivors of 10 disasters. Soc Psychiatry Psychiatr Epidemiol. 2013;48(8):1189‐1197. [DOI] [PubMed] [Google Scholar]
- 75. Lim LC. Delayed emergence of post‐traumatic stress disorder. Singapore Med J. 1991;32(1):92‐93. [PubMed] [Google Scholar]
- 76. Briggs AC. A case of delayed post‐traumatic stress disorder with ‘organic memories’ accompanying therapy. Br J Psychiatry. 1993;163:828‐830. [DOI] [PubMed] [Google Scholar]
- 77. Brewin CR. Systematic review of screening instruments for adults at risk of PTSD. J Trauma Stress. 2005;18(1):53‐62. [DOI] [PubMed] [Google Scholar]
- 78. Ruggiero KJ, Del Ben K, Scotti JR, Rabalais AE. Psychometric properties of the PTSD Checklist‐Civilian Version. J Trauma Stress. 2003;16(5):495‐502. [DOI] [PubMed] [Google Scholar]
- 79. Bergman HE, Przeworski A, Feeny NC. Rates of subthreshold PTSD among U.S. military veterans and service members. A Literature Review. Mil Psychol. 2017;29(2):117‐127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Brancu M, Mann‐Wrobel M, Beckham JC, et al. Subthreshold posttraumatic stress disorder: A meta‐analytic review of DSM‐IV prevalence and a proposed DSM‐5 approach to measurement. Psychol Trauma. 2016;8(2):222‐232. [DOI] [PubMed] [Google Scholar]
- 81. Kim JI, Oh S, Park H, Min B, Kim JH. The prevalence and clinical impairment of subthreshold PTSD using DSM‐5 criteria in a national sample of Korean firefighters. Depress Anxiety. 2020;37(4):375‐385. [DOI] [PubMed] [Google Scholar]
- 82. McLaughlin KA, Koenen KC, Friedman MJ, et al. Subthreshold posttraumatic stress disorder in the world health organization world mental health surveys. Biol Psychiatry. 2015;77(4):375‐384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Gargano LM, Li J, Millien L, Alper H, Brackbill RM. Exposure to multiple disasters: The long‐term effect of Hurricane Sandy (October 29, 2012) on NYC survivors of the September 11, 2001 World Trade Center attack. Psychiatry Res. 2019;273:719‐724. [DOI] [PubMed] [Google Scholar]
- 84. Galatzer‐Levy IR, Brown AD, Henn‐Haase C, Metzler TJ, Neylan TC, Marmar CR. Positive and negative emotion prospectively predict trajectories of resilience and distress among high‐exposure police officers. Emotion. 2013;13(3):545‐553. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
Data Availability Statement
All data included in this paper are available from public sources. A file with readings from figures in original articles may be provided by mail to the corresponding author.


