Abstract
Iodinated contrast media (ICM) have become one of the major causes of drug hypersensitivity reactions (HSRs) related to increasing numbers of ICM-based radiological imaging procedures. Strategies for diagnosing and preventing ICM-induced HSRs have not been uniformly standardized yet. However, advances have been made based on the results of recent research. A previous history of hypersensitivity to ICM is the most significant risk factor for developing HSR by ICM. Avoidance of culprit agents and premedication is the main strategy to prevent recurrences of HSRs in high-risk patients. In addition, we strongly recommend identifying sensitized ICM using skin tests to determine immunoglobulin E-mediated or delayed-type allergy and to guide the choice of an alternative contrast agent. ICM provocation test procedures have been established and are helpful in selected cases. In this paper, we review how to evaluate patients who have experienced immediate or delayed HSRs caused by ICM to minimize the risk of recurrence and discuss unmet needs that require further research.
Keywords: Contrast media, hypersensitivity, drug allergy, skin tests
INTRODUCTION
The number of reports with adverse reactions related to contrast agents has been rapidly increasing, reflecting increased numbers of imaging procedures using contrast agents. Iodinated contrast media (ICM) were the most common cause of drug anaphylaxis in Korea.1,2
According to the time of onset after exposure to ICM, hypersensitivity reactions (HSRs) to ICM can be categorized as either immediate reactions, which usually occur within 1 hour and up to 6 hours after exposure to ICM, or delayed reactions, which occur after 1 hour and up to several days following exposure.3 The prevalence of immediate reactions to the non-ionic low-osmolar ICMs currently used for intravascular enhancement has been reported to be about 0.2%–3%, and for delayed reactions about 1%–3%.4,5,6
Although various national and international societies have provided clinical guidelines for HSRs to ICMs, there are slight differences in recommendations regarding evaluation methods, use of premedication, and changes in ICM when administering ICMs.7,8 Furthermore, depending on the real-world situation, there may be differences in applying these guidelines to actual treatment in each medical facility. However, emerging evidence based on the clinical data on ICM-induced hypersensitivity indicates a central role in performing skin tests to more actively diagnose HSRs to ICMs and manage high-risk groups.8,9,10 In this review, we will introduce the latest knowledge on the diagnosis and treatment of immediate and delayed ICM-induced HSRs and look at how to utilize them in clinical practice settings.
DIAGNOSIS AND PREVENTION OF IMMEDIATE HSRs TO ICM
In the past, immediate HSRs to ICMs were considered to occur via non-immunological mechanisms. However, recent literature reporting positive skin tests in patients with more severe reactions suggests that a subgroup of immediate HSRs to ICMs may actually be immunoglobulin E (IgE)-mediated allergy.11,12,13
Clinical guidelines differ in diagnostic testing, the need for premedication to prevent HSR, changing the culprit ICM, and selection of alternative ICMs. While there is no specific recommendation in the guideline from the American College of Radiology, the position papers from European academic societies and expert guidelines recommend that an allergy test such as a skin test should be performed appropriately to differentiate an IgE-mediated allergic reaction and used to select an alternative ICM (Table 1).3 There are still many remaining unresolved issues such as determining the appropriate test target and optimal concentration of ICM, establishing an accurate test method and standardizing it, interpreting the cross-reactivity among ICMs and identifying the role of premedication such as antihistamines and steroids. In this section, we will review data on determining the appropriate skin test target, establishing an accurate skin test method, selecting a safe ICM by interpreting the cross-reactivity found in skin tests, and identifying the role of premedication.
Table 1. Diagnosis and prevention of immediate HSRs to ICM presented in each clinical guideline.
| Clinical guideline | Diagnosis | Premedication | Change and selection of alternative contrast agent |
|---|---|---|---|
| American College of Radiology7 | • No specific mention of a diagnostic test. | • Administering oral corticosteroids 12–13 hours before ICM exposure is recommended to patients who have previously experienced immediate HSRs to ICM. | • If culprit ICM is known in patients who have previously experienced immediate HSRs to ICM, a change of the ICM from the culprit to an alternative ICM is recommended. |
| • Performing skin tests routinely before CT scan with ICM is not recommended to predict immediate HSRs. | • If it is difficult to perform an ICM-related skin test, administering intravenous corticosteroid 4–5 hours before ICM exposure is recommended to patients who have previously experienced immediate HSRs to ICM. | • No specific mention of alternative ICM selection | |
| • No classification for severity of HSRs | |||
| European Society of Urogenital Radiology8 | • Consulting to allergist within 1–6 months is recommended for patients with a previous history of moderate to severe HSRs to ICM. | • Premedication is not recommended due to insufficient evidence. | • A change of the ICM from the culprit to an alternative ICM is recommended for patients who have previously experienced immediate HSRs to ICM |
| • Performing skin tests in consultation with an allergist can help to select an alternative ICM | |||
| European Academy of Allergy and Clinical Immunology (EAACI) position paper9 | • Skin test is recommended in all patients who have previously experienced immediate HSRs to ICM, except for emergent CT scan with ICM. | • Premedication is recommended for patients who have previously experienced immediate HSRs to ICM or have a difficult situation to perform a skin test due to an emergent CT scan with ICM. | • A change of the ICM from the culprit to a skin test-negative alternative ICM is recommended for patients who have previously experienced immediate HSRs to ICM. |
| • DPT can be used to identify suitable alternative ICMs in patients with a negative skin test. | • No classification for severity of HSRs | • Patients having experienced ICM-induced anaphylaxis are recommended to avoid CT scans with ICM. If it is necessary to perform a CT scan with ICM, a replacement to an alternative ICM and a preparation of emergency medicine are recommended. | |
| Spanish Society of Allergy and Clinical Immunology (SEAIC)10 | • Skin test is highly recommended for patients who have previously experienced immediate HSRs to ICM. | • The preventive effect of pretreatment is controversial. | • A replacement to an alternative ICM by skin test is recommended for patients who have previously experienced immediate HSRs to ICM. |
| • DPT is recommended to confirm an alternative ICM. |
HSR, hypersensitivity reaction; ICM, iodinated contrast media; DPT, drug provocation test.
Selection of patients for skin testing
The use of skin tests or drug provocation tests (DPTs) as a prescreening for all patients scheduled to use ICM is not recommended because it is ineffective in predicting immediate-type HSRs in those without a previous history of HSRs.14,15 Instead, skin tests should be performed selectively for high-risk groups with a history of immediate HSR to ICM. There are other well-known minor risk factors of ICM-induced HSRs, including a history of asthma and other drug allergies, female and genetic predisposition such as HLA-DRB1*15:02 and a family history of hypersensitivity to ICMs.16,17,18 Recently, a history of hypersensitivity to gadolinium contrast agents has also been reported as a risk factor for hypersensitivity to ICMs.19
However, the risk of developing severe hypersensitivity in relation to these minor risk factors is relatively low; no current studies have presented a clear explanation between these minor risk factors and severe HSRs. Therefore, minor risk factors are no indication for performing skin tests. However, a history of severe HSR to ICM strongly correlates to the risk of severe recurrent HSR. Thus, whereas skin testing with ICM is strongly recommended for patients who have experienced severe systemic immediate HSRs such as anaphylaxis, it is not essential for patients with very mild reactions such as isolated localized urticaria, generalized pruritus, and isolated flushing as well as with toxic or unrelated reactions (e.g., heat sensation, nausea).9
Method of skin testing
Depending on the studies and methods used, the sensitivity, specificity, positive predictive value, and negative predictive value of skin tests for ICMs varied.11,20,21,22,23 In studies on immediate HSRs to ICM, the sensitivity and specificity of skin test was reported as 20% and 96%–100%, respectively.20,21 In addition, the positive predicted value of skin test in immediate HSRs to ICM was 17%–52%,11 and the negative predictive value was 94.2% in immediate HSRs.22 According to a meta-analysis of ICM skin test results in patients with immediate HSRs, the sensitivity of skin tests was different depending on the severity of HSRs to ICM. For example, the sensitivity of skin tests is about 12% in patients with urticaria, whereas it was 51.9% in those with anaphylaxis.11 In a recently published multicenter prospective study, the sensitivity of skin tests was 9.5%, 23%, 53%, and 100%, respectively, in those with immediate HSRs limited to the skin, severe systemic reactions, life-threatening reactions, and cardiac arrest, suggesting that severe HSRs would be based on IgE-mediated mechanism.24
Standardization of skin tests for ICM is a major task to be solved for accurate diagnosis and prevention. Currently, the recommended method of ICM-related skin testing is to begin with the skin prick test (SPT) using undiluted ICM. If the SPT is negative, then an intradermal test with a 1:10 diluted solution of ICMs is recommended. To verify the possibility of cross-reactivity among ICMs, it is recommended to perform SPT and intradermal tests with all ICMs available and relevant for the radiological departments.9,25 In addition to the methods, timing is an important factor in determining the sensitivity of the skin test. According to a position paper from European academic societies and expert guidelines based on a few studies, performing skin tests within 2–6 months after the onset of the index reaction showed higher sensitivity than tests performed afterward.20
Role of DPTs
DPT can be performed as a final step for confirmatory diagnosis. Older studies reported serious adverse reactions even after small test doses were injected before a planned imaging procedure, indirectly warning of the risk of a DPT.14,26 However, newer studies reported that DPT using ICMs could be safe and helpful in the diagnosis, provided that they are performed in institutions with experience in diagnosing HSRs to other drugs and in anaphylaxis treatment.23,27,28 DPT may play an important role in identifying safe alternative ICMs in patients who have experienced severe immediate HSRs, such as anaphylaxis. In patients with lower risk for a severe recurrent HSR, e.g., those with urticaria only, renewed exposure to a different skin test-negative ICM at a radiology department under emergency preparedness (when the following imaging procedure is indicated) may be sufficient. During DPT, careful monitoring is required for not only HSRs but also pharmacological toxic reactions. DPT should be avoided in patients with severe renal dysfunction, those taking nephrotoxic drugs, pregnant or lactating patients, or patients with hyperthyroidism. In most cases, the cumulative dose of the ICM given in DPT varied from 49.5 mL to 100 mL, and the injection was distributed over one or two days, depending on the study.9,10,23,27,28 A recent study suggested an uncomplicated two-step challenge with 5 mL and 30 mL; although 6.0% of patients who were negative in the challenge test experienced mild breakthrough reactions, none of these were severe reactions.29
Since there is still a lack of a consensus on when to implement ICM-related DPT and how to perform it in a standardized manner, additional discussion and validating studies on DPT in ICM hypersensitivity are necessary.
Selection of safe alternative ICMs
Several studies published in recent years have shown that solely changing the culprit ICM to another ICM reduced the risk for recurrence of immediate acute HSRs and that this procedure was even more effective than premedication without changing the culprit ICM.30,31,32 In patients with a history of immediate HSR to ICM, re-exposure to the causative ICM without premedication resulted in the recurrence of an immediate reaction in 31.1% of cases. The recurrence rate was reduced to 12% when the ICM was changed and further decreased to 7.6% with premedication combined with ICM change.33 Currently, international guidelines from North America and Europe recommend that patients who experienced HSRs to ICMs avoid the causative agent and change to another ICM. Some studies suggested that a common N-(2,3-dihydroxypropyl) carbamoyl side chain might be important for cross-reactivity between ICM.22,34 Therefore, in patients who experienced a severe index HSR to ICM, using skin test-negative ICM without a common side-chain resulted in lower recurrence of HSR on re-exposure.13
The basophil activation test (BAT) can be a complementary tool to diagnose immediate HSR to ICM with a good correlation with ST and DPT results. However, the degree of its additional benefit still has not been sufficiently demonstrated.23,35
There is still insufficient understanding of cross-reactivity between different ICMs and, consequently, considerable disagreement in determining how to select the most suitable alternative ICM.13,33 Therefore, it is necessary to conduct a large-scale prospective study with sufficient numbers in each ICM subgroup.33
Effectiveness of premedication
Some studies have reported a reduction of recurrent HSRs to ICM with premedication without significant short-term adverse effects.30,33 There is no standardized premedication protocol for preventing immediate HSR to low osmolar contrast media in patients with a history of HSR to the same type of ICM. Lee et al.30 reported the severity-based stratified prophylaxis regimens reduced the risk of breakthrough reactions in patients with a history of HSR to ICM; antihistamine only for mild index HSRs, a combination of antihistamine and single-dose corticosteroid (methylprednisolone 40 mg) for moderate index HSRs, and a combination of antihistamine and multiple-dose corticosteroid (methylprednisolone 40 mg) for severe index HSRs. However, premedication cannot completely prevent the recurrence of an immediate HSR, especially severe HSRs such as anaphylaxis.36,37 As premedication, systemic steroids and antihistamines are widely used, but standard premedication protocols detailing drug choice, dosage, and interval and frequency of administration before ICM re-exposure have not been properly established. Park et al.33 reported that the combined use of antihistamines and corticosteroids did not show significant additional benefit compared to the treatment with antihistamines alone in patients with mild HSRs. In addition, increasing the frequency of corticosteroid use rather than the cumulative dose helped reduce ICM-induced HSRs.30 Jung et al.38 reported that the frequency of immediate HSRs was lower in the group treated with two sequential corticosteroid injections than in patients only receiving a single steroid regimen. Summarizing the above results, antihistamine alone is sufficient for premedication for patients with mild immediate HSRs. On the other hand, it is effective to administer steroids repeatedly in patients with severe immediate HSR. However, the premedication strategy for severe ICM-induced HSR is not yet established. Further studies are necessary to clarify which patients require premedication.
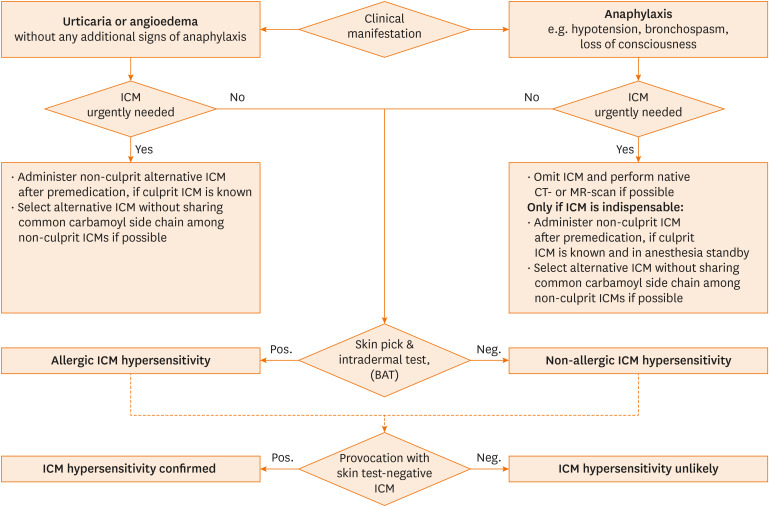
Strategies to prevent immediate HSRs to ICM (Fig. 1)
Fig. 1. Algorithm for patients with immediate hypersensitivity reactions to ICM.
ICM, iodinated contrast media; BAT, basophil activation test; Pos., positive; Neg., negative.
Taking an accurate history of clinical symptoms, severity, type, and amount of contrast agent, treatment, and outcomes is essential for risk stratification and developing individual strategies to prevent recurrence.
1) If ICM is urgent for patients with a history of severe HSRs such as severe laryngeal edema accompanied by breathing difficulties, airway obstruction, hypotension, and loss of consciousness, avoid using ICM and perform computed tomography (CT) without contrast media or instead consider alternative tests such as magnetic resonance imaging (MRI) as the first option.
2) If the acute use of ICM is unavoidable before allergy testing is possible, replace the culprit with a different ICM under cover of premedication. If the causative agent is unknown, premedication and close monitoring are required. As there is a higher risk for recurrent reactions, install emergency preparedness. For patients with previous severe HSRs and unavoidable ICM use, apply an individual risk-benefit analysis for the patient and have full-scale emergency treatment options immediately available (e.g., anesthesia emergency team on standby).
3) Skin tests should be performed with culprit ICM (if known) and alternative ICMs. Completely avoid the causative agent and any other skin test-positive ICMs and administer a skin test-negative ICM. In patients with less severe reactions, contrasted imaging using a skin test-negative ICM with a different structure from the culprit is possible under emergency treatment availability with or without premedication, depending on the severity of the reaction.
4) Consider confirming non-reactivity through intravenous DPT with skin test-negative ICMs prior to use of ICM, which is recommended particularly after severe reactions. Compared to renewed exposure to an ICM at the radiology department, it appears safer to give fractionated doses of ICM through DPT in a department experienced in handling anaphylaxis.
DIAGNOSIS AND PREVENTION OF DELAYED HSRs TO ICM
Most delayed-type HSRs to ICM manifest as mild to moderate uncomplicated maculopapular rashes. Very rarely, severe cutaneous adverse reactions (SCAR), such as acute generalized exanthematous pustulosis, Stevens-Johnson syndrome, or toxic epidermal necrolysis, may occur.39,40 Delayed HSRs are T-cell-mediated type IV allergic reactions that occur several hours to several days after the administration of ICM and last for several days to several weeks. However, most delayed HSRs occur within one week.41 The incidence of delayed HSR was significantly higher in nonionic dimer contrast media users than in nonionic monomer users.42 Delayed HSRs were reported to have more frequent cross-reactivity between ICMs than immediate HSRs. Although there is no evidence to prove the efficacy of premedication in patients with delayed hypersensitivity to ICM, several studies have reported that premedication with systemic corticosteroids may reduce reaction rate and severity in patients with a previous history of delayed-type HSRs. However, breakthrough reactions do occur, and the variable onset of delayed-type reactions makes it difficult to select the appropriate time to administer the premedication. In this section, we will review the clinical meaning of the skin test in ICM-induced delayed hypersensitivity and the role of premedication in ICM-induced delayed hypersensitivity.
Skin tests in delayed-type HSRs
In patients having had a suspected delayed-type rash to ICM, skin tests such as patch tests and intradermal tests with delayed reading can be helpful to confirm T-cell-mediated HSRs and may help choose alternative ICMs which may be tolerated. International guidelines emphasize the proactive implementation of the ICM skin test (Table 2). Yoon et al.11 reported that the overall test positivity rate was 26%, of which 7% was for the SPT, 22% for the delayed reading of the intradermal test, and 16% for the patch test, respectively. To overcome the low sensitivity rate, the combination of intradermal test with delayed reading and patch test can be attempted at the same time.11 In addition, the skin test sensitivity can be increased by testing with a higher concentration of ICM used in intradermal tests with delayed reading compared to the concentrations used for immediate reading.20 When skin tests in 1:10 concentration were negative, 70% of the patients showed positive delayed reading results without any side effects in the intradermal test performed with the undiluted stock solution.43
Table 2. Diagnosis and prevention of delayed HSRs to ICM presented in each clinical guideline.
| Clinical guideline | Diagnosis | Premedication | Change and selection of alternative contrast agent |
|---|---|---|---|
| American College of Radiology7 | • No specific mention of diagnostic test | • Premedication is not recommended for patients who have experienced mild delayed HSRs with skin symptoms. | • If culprit ICM is known in patients who have previously experienced delayed HSRs to ICM, a change of the ICM from the culprit to an alternative ICM is recommended. |
| • No specific mention of alternative ICM selection | |||
| European Society of Urogenital Radiology8 | • Patch and intradermal tests with delayed reading are recommended for patients who have previously experienced delayed HSRs to ICM. | • Premedication is generally not recommended. | • A change of the ICM from the culprit to a skin test-negative alternative ICM is recommended for patients who have previously experienced delayed HSRs to ICM. |
| European Academy of Allergy and Clinical Immunology (EAACI) position paper9 | • Skin test is recommended in all patients who have previously experienced delayed HSRs to ICM, except for emergent CT scan with ICM. | • Premedication is not recommended due to insufficient evidence. | • A change of the ICM from the culprit to a skin test-negative alternative ICM is recommended for patients who have previously experienced delayed HSRs to ICM. |
| • DPT can be used to identify proper alternative ICMs in patients with a negative skin test. | • Patients with the experience of ICM-induced severe cutaneous adverse reactions are recommended to avoid CT scans with ICM. | ||
| • DPT is recommended after considering the risks and benefits. | |||
| Spanish Society of Allergy and Clinical Immunology (SEAIC)10 | • Patch and intradermal tests with delayed reading are recommended for patients who have previously experienced delayed hypersensitivity. | • The preventive effect of pretreatment is controversial. | • A change of the ICM from the culprit to a skin test-negative alternative ICM is recommended for patients who have previously experienced delayed HSRs to ICM. |
| • DPT can be used to evaluate culprit ICM in case negative skin test. | |||
| • In severe cutaneous adverse reaction experienced patients, DPT with culprit ICM is contraindicated. |
HSR, hypersensitivity reaction; ICM, iodinated contrast media; DPT, drug provocation test.
The timing of the intradermal test with delayed reading is also an important determinant of sensitivity. According to Brockow et al.,20 intradermal tests with delayed reading showed a high positivity rate of 48% when performed 1 to 6 months after the recovery of delayed-type HSR, whereas it dropped to 23% when performed thereafter. These data suggest that the combination of intradermal test with delayed reading and patch test can be used to diagnose ICM-induced delayed-type hypersensitivity. To increase the sensitivity of ICM-induced delayed-type hypersensitivity, it is important to conduct skin tests with various concentrations of ICMs and perform skin tests at an appropriate time.
The role of DPT in delayed HSRs
As described above, skin testing showed relatively low sensitivity and high cross-reactivity with other ICMs in patients with delayed hypersensitivity to ICM.11 This limits the value of the skin test and reduces the negative predictive value. Around half of the patients showed hypersensitivity on DPT when exposed to skin test-negative ICM.43,44 Therefore, in delayed HSRs, the culprit ICM should not be readministered, and a structurally different ICM should be chosen. DPT can play a role in accurately diagnosing and selecting safe alternative ICMs in patients with delayed-type HSRs. ICM-related DPT should be performed under close monitoring and careful consideration of the risk of other pharmacological toxic reactions such as renal function deterioration.
Although various protocols of DPT have been reported, there is still no consensus on standardized provocation protocols such as the amount of ICM and the time interval between steps.
In vitro test for delayed HSRs to ICM
A lymphocyte transformation test (LTT), which measures the proliferation of circulating drug-specific memory T cells, may be an additional diagnostic tool to detect the culprit ICM of delayed HSRs to ICM.45 The sensitivity of LTT ranges from 13% to 75%,46 and it can be positive even 10–20 years after delayed HSR since LTT evaluates drug-specific memory T cell response in the peripheral blood.45 However, since memory T cell reactivity was reduced in some patients 3–4 years after delayed HSR, it is recommended to perform LTT within 2–3 years of the onset of delayed HSR.45 Despite its promising aspects, LTT is tedious, less sensitive than the skin test, and has mostly been performed for experimental research.
Effectiveness of premedication
The usefulness of premedication for delayed HSR is still lacking. Although a case report has claimed that corticosteroid premedication is effective in ICM-induced maculopapular rash,47 there are no cohort studies to evaluate the efficacy of premedication for delayed HSR. Therefore, several guidelines suggest
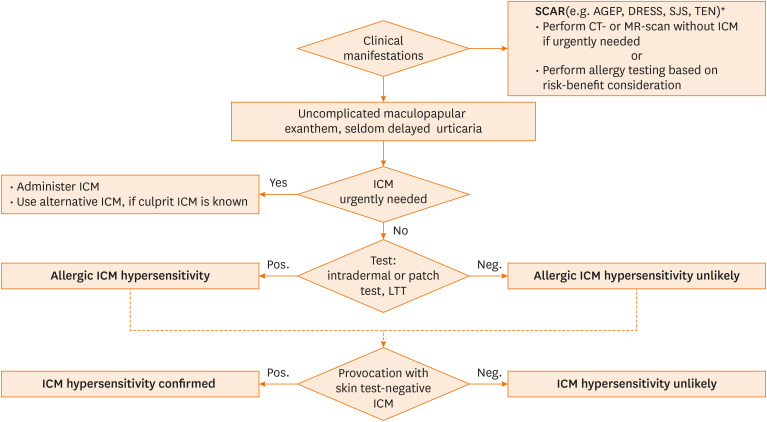
Strategies to prevent delayed HSRs to ICM (Fig. 2)
Fig. 2. Algorithm for patients with delayed hypersensitivity reactions to ICM.
SCAR, severe cutaneous adverse reaction; AGEP, acute generalized exanthematous pustulosis; DRESS, drug reaction with eosinophilia and systemic symptoms; SJS, Stevens-Johnson-syndrome; TEN, toxic epidermal necrolysis; CT, computed tomography; MR, magnetic resonance; ICM, iodinated contrast media; LTT, lymphocyte transformation test; Pos., positive; Neg., negative.
1) For all patients who have experienced delayed onset exanthems to ICMs, it is essential to take an accurate history, including clinical symptoms, severity, type of contrast agent, the amount used, treatment, and outcome results.
2) If patients have experienced SCAR such as acute generalized erythematous pustulosis, drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome, Stevens-Johnson syndrome, or toxic epidermal necrolysis, ICM use should be prohibited, and CT without ICM or alternative tests such as MRI should be performed. Skin tests are generally possible, but DPT should be performed exceptionally after thorough consideration of the risks and benefits for the individual patients.
3) In patients who have experienced an uncomplicated maculopapular rash, skin tests should be performed unless an imaging test using ICM is urgently needed. If ICM use is urgently required for a patient who has experienced an uncomplicated maculopapular rash, avoid using the causative contrast agent and change to another ICM. If the culprit agent is not known and skin tests are not possible, a CT scan can be considered after risk-benefit analysis and receiving the informed consent of the patient, because there is an increased risk for another maculopapular rash, but not for life-threatening anaphylaxis or SCAR.
4) When performing skin tests, as many types of ICM as possible, including the causative agent, should be tested with delayed readings of the intradermal tests and patch tests. Regardless of the test result, the culprit agent should be avoided. If any of the ICMs is positive in the skin test, it is recommended to avoid using skin test-positive agents and replace them with skin test-negative contrast agents. If the skin test is negative to all substances including the culprit, this test does not aid in indicating which ICM may be better tolerated.
5) DPT can be considered as the next step. If the DPT is negative, that ICM is highly likely to be safe when administered intravenously on a CT scan.
6) There is insufficient evidence on the effectiveness of premedication in preventing delayed-type HSRs. Thus, substituting the ICM with another skin-test-negative ICM rather than premedication should be the strategy to avoid further reactions. Nevertheless, premedication can be considered in individual patients with higher risk and severe exanthema. A short-term prescription of topical and oral steroids is recommended if symptoms recur after leaving the medical facility.3
UNMET NEEDS
There are still many controversies and unmet needs concerning ICM hypersensitivity. Recent guidelines indicate the need for skin testing, particularly for patients with severe allergic reactions and anaphylaxis, to select a safe alternative ICM that shall be tolerated in the future.3 However, since the majority of patients with a mild degree of immediate ICM hypersensitivity do not react to any ICM in skin tests, the mechanism of the reaction remains unclear. Furthermore, since BAT and LTT are not available beyond the experimental setting, their potential roles are not validated.
Premedication may reduce minor adverse reactions, such as pruritus and urticaria, but not anaphylaxis.48 Moreover, effective premedication strategies remain unknown. There is little consensus regarding whether and for whom premedication is helpful and which premedication should be administered. Multicenter studies including large numbers of patients are needed to determine the impact of different premedication protocols on clinical outcomes.
Also, provocation tests with ICM have been used mainly in patients with a history of severe reactions to identify alternative ICMs in a safer setting.49 On the other hand, in less severe cases, skin test-negative ICM reexposition at the radiology department may also suffice when the ICM is needed for diagnosis.
CONCLUSION
HSRs to ICM are a significant concern arising with the increased use of contrast-enhanced imaging modalities. To prevent recurrent HSRs to ICM, avoidance of the culprit ICM, substituting with other structurally different ICMs and considering premedication are generally recommended. Additionally, skin tests and DPT can provide a helpful risk assessment of whether certain ICMs may be safe alternatives. However, as the negative predictive value of these tests is not 100%, these tests cannot completely exclude the reactivity of ICM on the following systemic exposure. Unfortunately, skin tests, DPT, and premedication protocols are not standardized. Therefore, well-planned prospective studies with a large number of patients are required to validate the value of these tests on hypersensitivity to ICM in the future.
Footnotes
Disclosure: There are no financial or other issues that might lead to a conflict of interest.
References
- 1.Cho MK, Moon M, Kim HH, Kang DY, Lee JY, Cho SH, et al. Analysis of individual case safety reports of drug-induced anaphylaxis to the Korea adverse event reporting system. Allergy Asthma Respir Dis. 2020;8:30–35. [Google Scholar]
- 2.Moon IJ, Kim SR, Koh BS, Leem DW, Park KH, Lee JH, et al. Drug-induced anaphylaxis in a single Korean tertiary hospital. Korean J Med. 2015;88:281–287. [Google Scholar]
- 3.Brockow K. Allergy to radiocontrast dye. Immunol Allergy Clin North Am. 2022;42:391–401. doi: 10.1016/j.iac.2021.12.001. [DOI] [PubMed] [Google Scholar]
- 4.Brockow K, Christiansen C, Kanny G, Clément O, Barbaud A, Bircher A, et al. Management of hypersensitivity reactions to iodinated contrast media. Allergy. 2005;60:150–158. doi: 10.1111/j.1398-9995.2005.00745.x. [DOI] [PubMed] [Google Scholar]
- 5.Park C, Bae Y, Choi S, Kim T, Jung Y, Cho Y, et al. Incidence, clinical manifestations, and outcome of adverse reactions to intravenous radio-contrast media following computed tomography (Ct) in general population. Ann Allergy Asthma Immunol. 2009;103:A44. [Google Scholar]
- 6.Hosoya T, Yamaguchi K, Akutsu T, Mitsuhashi Y, Kondo S, Sugai Y, et al. Delayed adverse reactions to iodinated contrast media and their risk factors. Radiat Med. 2000;18:39–45. [PubMed] [Google Scholar]
- 7.ACR Committee on Drugs and Contrast Media. ACR manual on contrast media. Reston (VA): American College of Radiology; 2020. [Google Scholar]
- 8.Contrast Media Safety Committee. ESUR guidelines on contrast agents European Society of Urogenital Radiology 2019; version 10.0. Wien: Contrast Media Safety Committee; 2019. [Google Scholar]
- 9.Torres MJ, Trautmann A, Bohm I, Scherer K, Barbaud A, Bavbek S, et al. Practice parameters for diagnosing and managing iodinated contrast media hypersensitivity. Allergy. 2021;76:1325–1339. doi: 10.1111/all.14656. [DOI] [PubMed] [Google Scholar]
- 10.Rosado Ingelmo A, Doña Diaz I, Cabañas Moreno R, Moya Quesada MC, García-Avilés C, García Nuñez I, et al. Clinical practice guidelines for diagnosis and management of hypersensitivity reactions to contrast media. J Investig Allergol Clin Immunol. 2016;26:144–155. doi: 10.18176/jiaci.0058. [DOI] [PubMed] [Google Scholar]
- 11.Yoon SH, Lee SY, Kang HR, Kim JY, Hahn S, Park CM, et al. Skin tests in patients with hypersensitivity reaction to iodinated contrast media: a meta-analysis. Allergy. 2015;70:625–637. doi: 10.1111/all.12589. [DOI] [PubMed] [Google Scholar]
- 12.Kim MH, Lee SY, Lee SE, Yang MS, Jung JW, Park CM, et al. Anaphylaxis to iodinated contrast media: clinical characteristics related with development of anaphylactic shock. PLoS One. 2014;9:e100154. doi: 10.1371/journal.pone.0100154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sohn KH, Seo JH, Kang DY, Lee SY, Kang HR. Finding the optimal alternative for immediate hypersensitivity to low-osmolar iodinated contrast. Invest Radiol. 2021;56:480–485. doi: 10.1097/RLI.0000000000000765. [DOI] [PubMed] [Google Scholar]
- 14.Yamaguchi K, Katayama H, Takashima T, Kozuka T, Seez P, Matsuura K. Prediction of severe adverse reactions to ionic and nonionic contrast media in Japan: evaluation of pretesting. A report from the Japanese Committee on the Safety of Contrast Media. Radiology. 1991;178:363–367. doi: 10.1148/radiology.178.2.1987594. [DOI] [PubMed] [Google Scholar]
- 15.Kim SH, Jo EJ, Kim MY, Lee SE, Kim MH, Yang MS, et al. Clinical value of radiocontrast media skin tests as a prescreening and diagnostic tool in hypersensitivity reactions. Ann Allergy Asthma Immunol. 2013;110:258–262. doi: 10.1016/j.anai.2013.01.004. [DOI] [PubMed] [Google Scholar]
- 16.Lee SY, Kang DY, Kim JY, Yoon SH, Choi YH, Lee W, et al. Incidence and risk factors of immediate hypersensitivity reactions associated with low-osmolar iodinated contrast media: a longitudinal study based on a real-time monitoring system. J Investig Allergol Clin Immunol. 2019;29:444–450. doi: 10.18176/jiaci.0374. [DOI] [PubMed] [Google Scholar]
- 17.Cha MJ, Kang DY, Lee W, Yoon SH, Choi YH, Byun JS, et al. Hypersensitivity reactions to iodinated contrast media: a multicenter study of 196 081 patients. Radiology. 2019;293:117–124. doi: 10.1148/radiol.2019190485. [DOI] [PubMed] [Google Scholar]
- 18.Chung SJ, Kang DY, Lee W, Lee SB, Kim S, Lee SE, et al. HLA-DRB1*15: 02 is associated with iodinated contrast media-related anaphylaxis. Invest Radiol. 2020;55:304–309. doi: 10.1097/RLI.0000000000000644. [DOI] [PubMed] [Google Scholar]
- 19.Ahn YH, Kang DY, Park SB, Kim HH, Kim HJ, Park GY, et al. Allergic-like hypersensitivity reactions to gadolinium-based contrast agents: an 8-year cohort study of 154 539 patients. Radiology. 2022;303:329–336. doi: 10.1148/radiol.210545. [DOI] [PubMed] [Google Scholar]
- 20.Brockow K, Romano A, Aberer W, Bircher AJ, Barbaud A, Bonadonna P, et al. Skin testing in patients with hypersensitivity reactions to iodinated contrast media - a European multicenter study. Allergy. 2009;64:234–241. doi: 10.1111/j.1398-9995.2008.01832.x. [DOI] [PubMed] [Google Scholar]
- 21.Goksel O, Aydın O, Atasoy C, Akyar S, Demirel YS, Misirligil Z, et al. Hypersensitivity reactions to contrast media: prevalence, risk factors and the role of skin tests in diagnosis--a cross-sectional survey. Int Arch Allergy Immunol. 2011;155:297–305. doi: 10.1159/000320760. [DOI] [PubMed] [Google Scholar]
- 22.Schrijvers R, Breynaert C, Ahmedali Y, Bourrain JL, Demoly P, Chiriac AM. Skin testing for suspected iodinated contrast media hypersensitivity. J Allergy Clin Immunol Pract. 2018;6:1246–1254. doi: 10.1016/j.jaip.2017.10.040. [DOI] [PubMed] [Google Scholar]
- 23.Salas M, Gomez F, Fernandez TD, Doña I, Aranda A, Ariza A, et al. Diagnosis of immediate hypersensitivity reactions to radiocontrast media. Allergy. 2013;68:1203–1206. doi: 10.1111/all.12214. [DOI] [PubMed] [Google Scholar]
- 24.Clement O, Dewachter P, Mouton-Faivre C, Nevoret C, Guilloux L, Bloch Morot E, et al. Immediate hypersensitivity to contrast agents: the French 5-year CIRTACI study. EClinicalMedicine. 2018;1:51–61. doi: 10.1016/j.eclinm.2018.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brockow K. Medical algorithm: diagnosis and treatment of radiocontrast media hypersensitivity. Allergy. 2020;75:1278–1280. doi: 10.1111/all.14147. [DOI] [PubMed] [Google Scholar]
- 26.Higashi TS, Kuniyasu Y, Takizawa K, Ikeuchi T, Kai Y. The consideration and performing of pretesting of contrast medium: surveying in Kanagawa. Nippon Igaku Hoshasen Gakkai Zasshi. 1993;53:1324–1330. [PubMed] [Google Scholar]
- 27.Böhm I, Schild HH. A practical guide to diagnose lesser-known immediate and delayed contrast media-induced adverse cutaneous reactions. Eur Radiol. 2006;16:1570–1579. doi: 10.1007/s00330-006-0202-9. [DOI] [PubMed] [Google Scholar]
- 28.Prieto-García A, Tomás M, Pineda R, Tornero P, Herrero T, Fuentes V, et al. Skin test-positive immediate hypersensitivity reaction to iodinated contrast media: the role of controlled challenge testing. J Investig Allergol Clin Immunol. 2013;23:183–189. [PubMed] [Google Scholar]
- 29.Ahn KM, Ahn YH, Cho MK, Kang DY, Lee SY, Kang HR. Validation of practical pathway in patients with anaphylaxis to low osmolar contrast media: a retrospective cohort study. J Allergy Clin Immunol Pract. 2022 doi: 10.1016/j.jaip.2022.03.030. [DOI] [PubMed] [Google Scholar]
- 30.Lee SY, Yang MS, Choi YH, Park CM, Park HW, Cho SH, et al. Stratified premedication strategy for the prevention of contrast media hypersensitivity in high-risk patients. Ann Allergy Asthma Immunol. 2017;118:339–344.e1. doi: 10.1016/j.anai.2016.11.027. [DOI] [PubMed] [Google Scholar]
- 31.Abe S, Fukuda H, Tobe K, Ibukuro K. Protective effect against repeat adverse reactions to iodinated contrast medium: premedication vs. changing the contrast medium. Eur Radiol. 2016;26:2148–2154. doi: 10.1007/s00330-015-4028-1. [DOI] [PubMed] [Google Scholar]
- 32.Park HJ, Park JW, Yang MS, Kim MY, Kim SH, Jang GC, et al. Re-exposure to low osmolar iodinated contrast media in patients with prior moderate-to-severe hypersensitivity reactions: a multicentre retrospective cohort study. Eur Radiol. 2017;27:2886–2893. doi: 10.1007/s00330-016-4682-y. [DOI] [PubMed] [Google Scholar]
- 33.Park SJ, Kang DY, Sohn KH, Yoon SH, Lee W, Choi YH, et al. Immediate mild reactions to CT with iodinated contrast media: strategy of contrast media readministration without corticosteroids. Radiology. 2018;288:710–716. doi: 10.1148/radiol.2018172524. [DOI] [PubMed] [Google Scholar]
- 34.Lerondeau B, Trechot P, Waton J, Poreaux C, Luc A, Schmutz JL, et al. Analysis of cross-reactivity among radiocontrast media in 97 hypersensitivity reactions. J Allergy Clin Immunol. 2016;137:633–635.e4. doi: 10.1016/j.jaci.2015.07.035. [DOI] [PubMed] [Google Scholar]
- 35.Trcka J, Schmidt C, Seitz CS, Bröcker EB, Gross GE, Trautmann A. Anaphylaxis to iodinated contrast material: nonallergic hypersensitivity or IgE-mediated allergy? AJR Am J Roentgenol. 2008;190:666–670. doi: 10.2214/AJR.07.2872. [DOI] [PubMed] [Google Scholar]
- 36.Freed KS, Leder RA, Alexander C, DeLong DM, Kliewer MA. Breakthrough adverse reactions to low-osmolar contrast media after steroid premedication. AJR Am J Roentgenol. 2001;176:1389–1392. doi: 10.2214/ajr.176.6.1761389. [DOI] [PubMed] [Google Scholar]
- 37.Davenport MS, Cohan RH, Caoili EM, Ellis JH. Repeat contrast medium reactions in premedicated patients: frequency and severity. Radiology. 2009;253:372–379. doi: 10.1148/radiol.2532090465. [DOI] [PubMed] [Google Scholar]
- 38.Jung JW, Choi YH, Park CM, Park HW, Cho SH, Kang HR. Outcomes of corticosteroid prophylaxis for hypersensitivity reactions to low osmolar contrast media in high-risk patients. Ann Allergy Asthma Immunol. 2016;117:304–309.e1. doi: 10.1016/j.anai.2016.07.010. [DOI] [PubMed] [Google Scholar]
- 39.Brockow K. Immediate and delayed reactions to radiocontrast media: is there an allergic mechanism? Immunol Allergy Clin North Am. 2009;29:453–468. doi: 10.1016/j.iac.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 40.Rydberg J, Charles J, Aspelin P. Frequency of late allergy-like adverse reactions following injection of intravascular non-ionic contrast media. A retrospective study comparing a non-ionic monomeric contrast medium with a non-ionic dimeric contrast medium. Acta Radiol. 1998;39:219–222. doi: 10.1080/02841859809172183. [DOI] [PubMed] [Google Scholar]
- 41.Kang DY, Lee SY, Ahn YH, Yoon SH, Choi YH, Lee W, et al. Incidence and risk factors of late adverse reactions to low-osmolar contrast media: a prospective observational study of 10,540 exposures. Eur J Radiol. 2022;146:110101. doi: 10.1016/j.ejrad.2021.110101. [DOI] [PubMed] [Google Scholar]
- 42.Schild HH, Kuhl CK, Hübner-Steiner U, Böhm I, Speck U. Adverse events after unenhanced and monomeric and dimeric contrast-enhanced CT: a prospective randomized controlled trial. Radiology. 2006;240:56–64. doi: 10.1148/radiol.2393050560. [DOI] [PubMed] [Google Scholar]
- 43.Torres MJ, Gomez F, Doña I, Rosado A, Mayorga C, Garcia I, et al. Diagnostic evaluation of patients with nonimmediate cutaneous hypersensitivity reactions to iodinated contrast media. Allergy. 2012;67:929–935. doi: 10.1111/j.1398-9995.2012.02840.x. [DOI] [PubMed] [Google Scholar]
- 44.Vernassiere C, Trechot P, Commun N, Schmutz JL, Barbaud A. Low negative predictive value of skin tests in investigating delayed reactions to radio-contrast media. Contact Dermat. 2004;50:359–366. doi: 10.1111/j.0105-1873.2004.00367.x. [DOI] [PubMed] [Google Scholar]
- 45.Pichler WJ, Tilch J. The lymphocyte transformation test in the diagnosis of drug hypersensitivity. Allergy. 2004;59:809–820. doi: 10.1111/j.1398-9995.2004.00547.x. [DOI] [PubMed] [Google Scholar]
- 46.Gómez E, Ariza A, Blanca-López N, Torres MJ. Nonimmediate hypersensitivity reactions to iodinated contrast media. Curr Opin Allergy Clin Immunol. 2013;13:345–353. doi: 10.1097/ACI.0b013e328362b926. [DOI] [PubMed] [Google Scholar]
- 47.Romano A, Artesani MC, Andriolo M, Viola M, Pettinato R, Vecchioli-Scaldazza A. Effective prophylactic protocol in delayed hypersensitivity to contrast media: report of a case involving lymphocyte transformation studies with different compounds. Radiology. 2002;225:466–470. doi: 10.1148/radiol.2251011654. [DOI] [PubMed] [Google Scholar]
- 48.Sánchez-Borges M, Aberer W, Brockow K, Celik GE, Cernadas J, Greenberger PA, et al. Controversies in Drug Allergy: Radiographic Contrast Media. J Allergy Clin Immunol Pract. 2019;7:61–65. doi: 10.1016/j.jaip.2018.06.030. [DOI] [PubMed] [Google Scholar]
- 49.Moreno EG, Mayorga C, La’zaro M, Campano’n MV, Da’vila I. Hypersensitivity reactions to iodinated contrast media: is it a true allergy. Curr Treat Options Allergy. 2018;5:103–117. [Google Scholar]