Abstract
Hepatocellular carcinoma (HCC) is a unique cancer entity that can be noninvasively diagnosed using imaging modalities without pathologic confirmation. In 2018, several major guidelines for HCC were updated to include hepatobiliary contrast agent magnetic resonance imaging (HBA-MRI) and contrast-enhanced ultrasound (CEUS) as major imaging modalities for HCC diagnosis. HBA-MRI enables the achievement of high sensitivity in HCC detection using the hepatobiliary phase (HBP). CEUS is another imaging modality with real-time imaging capability, and it is reported to be useful as a second-line modality to increase sensitivity without losing specificity for HCC diagnosis. However, until now, there is an unsolved discrepancy among guidelines on whether to accept “HBP hypointensity” as a definite diagnostic criterion for HCC or include CEUS in the diagnostic algorithm for HCC diagnosis. Furthermore, there is variability in terminology and inconsistencies in the definition of imaging findings among guidelines; therefore, there is an unmet need for the development of a standardized lexicon. In this article, we review the performance and limitations of HBA-MRI and CEUS after guideline updates in 2018 and briefly introduce some future aspects of imaging-based HCC diagnosis.
Keywords: Hepatocellular carcinoma, Diagnosis, Guideline, Magnetic resonance imaging, Diagnostic ultrasound
INTRODUCTION
Hepatocellular carcinoma (HCC) is the most common primary liver cancer, which exacts a heavy disease burden and is the third most common cause of cancer-related death worldwide [1-3]. HCC mainly occurs in patients with chronic liver disease, with chronic hepatitis B and C virus infections being the most common causes [1]. One unique and important characteristic in the diagnosis of HCC is that it can be diagnosed noninvasively by imaging modalities without pathologic confirmation in high-risk patients, which renders it imperative to correctly diagnose HCC on imaging [4]. Thus, guidelines have been established in many societies such as the American Association for the Study of Liver Diseases (AASLD), Liver Imaging Reporting and Data System (LI-RADS), the European Association for the Study of the Liver (EASL), the Asian Pacific Association for the Study of the Liver (APASL), and the Korean Liver Cancer Association-National Cancer Center (KLCA-NCC) to standardize the acquisition, interpretation, and reporting of imaging studies for HCC diagnosis [5-9]. These guidelines have been updated to reflect the latest updated evidence around 2018, which included hepatobiliary contrast agent magnetic resonance imaging (HBA-MRI) and contrast-enhanced ultrasound (CEUS) in the diagnostic algorithm of HCC [10]. These two modalities are included as diagnostic tests in several later updated guidelines from other societies, including the Society of Liver Cancer of China (2019) and the Taiwan Liver Cancer Association and the Gastroenterological Society of Taiwan (2020) [11,12]. Accordingly, since 2018, the application and performance of updated guidelines using HBA-MRI or CEUS for HCC diagnosis have been evaluated in several studies [13-20].
Therefore, in this article, we summarize the studies evaluating the performance and limitations of HBA-MRI and CEUS for HCC diagnosis, which reflect the updated guidelines. We also briefly introduce the future aspects of HCC imaging that have not yet been adopted in the guidelines, but are being actively studied recently, namely abbreviated MRI and CEUS for surveillance of HCC and deep learning for imaging-based diagnosis of HCC.
HBA-MRI FOR HCC DIAGNOSIS
Imaging properties of HBA-MRI
HBAs are specialized contrast agents that are taken up by functioning hepatocytes and are excreted in the bile [21]. There are two currently available gadolinium-based HBAs: gadoxetic acid (Gd-EOB-DTPA) and gadobenate dimeglumine (Gd-BOPTA). However, Gd-EOB-DTPA is more widely used than Gd-BOPTA because of its better pharmacokinetics for clinical use: a higher rate of biliary excretion (50% vs. 3–5%) and earlier window for hepatobiliary phase (HBP) imaging (10–40 vs. 60–120 minutes) [21-24]. Therefore, HBA-MRI refers to Gd-EOB-DTPA-enhanced MRI in this review, unless otherwise mentioned.
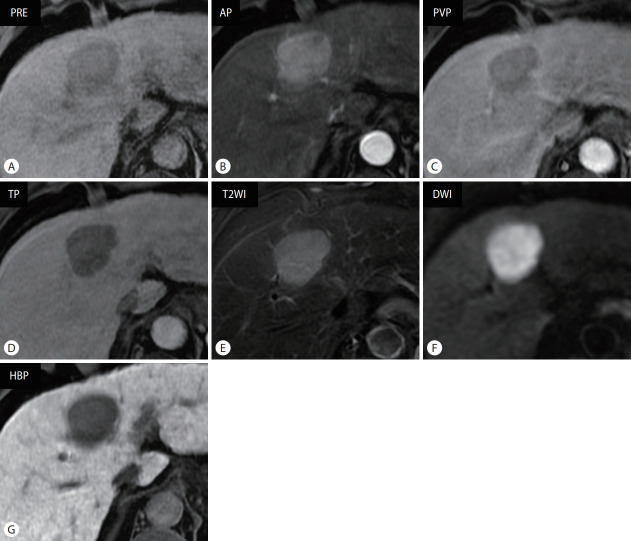
Since HBA is taken up by hepatocytes via organic anion transporting polypeptide 8 (OATP8), expression of OATP8 is the main factor determining signal intensity in HBP [21,25,26]. OATP8 expression is known to be reduced during hepatocarcinogenesis; OATP8 is highly expressed in regenerative nodules and low-grade dysplastic nodules and is less expressed in many high-grade dysplastic nodules and HCCs [25]. Therefore, most HCCs and some high-grade dysplastic nodules are hypointense in HBP, while most regenerative nodules, low-grade dysplastic nodules, some high-grade dysplastic nodules, and only a minor portion (5–12%) of HCCs are isointense or hyperintense in HBP (Fig. 1) [26]. One important point is that the reduction in the expression of OATP8 occurs prior to portal venous flow reduction and neo-arterialization, which implies that even early HCCs without definite arterial phase hyperenhancement (APHE) can be detected in HBP as hypointense lesions [25,26]. The ability to detect early HCCs is one of the strengths of HBAs compared to conventional extracellular contrast agents (ECAs) in the diagnosis of HCC. In addition, strongly enhancing hepatic parenchyma in HBP against hypointense HCCs facilitates the delineation of HCCs (Fig. 1) [26]. Meanwhile, HCC diagnosis using HBP alone may lead to misinterpretation because HBP hypointensity is not a specific finding for HCC, as it can also be found in other hepatic lesions, including premalignant lesions of HCC, other cirrhotic nodules, hemangioma, and non-HCC malignancies [26,27].
Figure 1.
Typical magnetic resonance imaging findings of hepatocellular carcinoma using hepatobiliary contrast agent in a 61-year-old male patient with chronic hepatitis B. Approximately 4-cm sized mass lesion in liver segment 4, which shows (A) hypointensity in precontrast T1-weighted image, (B) arterial phase hyperenhancement, and (C) portal venous phase (PVP) and (D) transitional phase (TP) washout. It shows (E) moderate hyperintensity in fat-suppressed T2-weighted image and (F) diffusion restriction. (G) In the hepatobiliary phase (HBP) image acquired 20 minutes after contrast administration, the mass is clearly visualized with hypointense lesion in contrast to hyperintense hepatic parenchyma. PRE, precontrast; AP, arterial phase; T2WI, T2-weighted image; DWI, diffusion-weighted image.
Diagnostic performance and limitations of HBA-MRI
Since HBP hypointensity is sensitive but not specific for HCC diagnosis, whether the use of HBP hypointensity as a major imaging feature for the definite diagnosis of HCC differs among guidelines, which may be attributed to several factors including different treatment policies [4-10]. Guidelines from Western societies such as AASLD, LI-RADS, and EASL do not accept HBP hypointensity as a major feature for the definite diagnosis of HCC to avoid false-positive diagnoses. However, the guidelines from Asian societies such as APASL and KLCA-NCC permit the definite diagnosis of HCC using a combination of APHE and HBP hypointensity, regardless of portal washout, to achieve high sensitivity to enable initiation of early locoregional treatment [4-10]. The use of HBP hypointensity for definite diagnosis of HCC, however, may reduce specificity because it is not a specific feature of HCC [26,27]. Therefore, to maintain specificity, Asian guidelines have additional exclusion criteria. For example, KLCA-NCC excludes lesions with marked T2 hyperintensity or targetoid appearance, with a reported specificity of up to 92.1% [9,13]. APASL also excludes cavernous hemangioma, but does not exclude targetoid lesions, which may result in specificity loss [8]. Multiple retrospective studies evaluating the diagnostic performance of HCC diagnostic algorithms according to the updated guidelines in 2018 reflect these differences: Western guidelines showed greater specificity (LI-RADS, 89–97.4%; EASL, 86–94.9%) but lower sensitivity (LI-RADS, 34.5–74.2%; EASL, 38.8–71.0%), while Asian guidelines showed greater sensitivity (APASL, 64–90.6%; KLCA-NCC, 65.5–86.1%) with relatively lower specificity (APASL, 73–83.9%; KLCA-NCC, 85–92.1%). Among Asian guidelines, APASL seems to be more sensitive but less specific than KLCA-NCC, as expected (Table 1) [13-16].
Table 1.
Discrepancy in diagnostic criteria and performance for HCC using HBA-MRI between Western and Asian societies
| Western societies |
Asian societies |
|||
|---|---|---|---|---|
| AASLD/LI-RADS 2018 | EASL 2018 | APASL 2017 | KLCA-NCC 2018 | |
| Diagnostic criteria for definite HCC | 1. For observation ≥ 20 mm: 1) APHE plus, 2) one or more additional major features* | APHE plus, washout at PVP | APHE plus, venous washout OR HBP hypointensity (excluding hemangioma) | APHE plus, washout at PVP, DP or HBP (excluding marked T2 hyperintense OR targetoid lesion) |
| 2. For observation between 10–19 mm: 1) APHE plus, 2) two or more additional major features* OR nonperipheral “washout” OR threshold growth | ||||
| Definite diagnosis using APHE and HBP hypointensity | Impossible | Impossible | Possible | Possible |
| Sensitivity | Relatively low | Relatively low | High† | High† |
| Jeon et al. [13] | 34.5 | 38.8 | 75.9 | 65.5 |
| Clarke et al. [14] | 45 | 44 | 64 | N/A |
| Hwang et al. [15] | 60–65 | 54 | 91–93 | 85 |
| Park et al. [16] | 67.7–74.2 | 65.2–71.0 | 89.4–90.6 | 82.3–86.1 |
| Specificity | High | High | Relatively low† | Relatively low† |
| Jeon et al. [13] | 97.4 | 92.1 | 78.9 | 92.1 |
| Clarke et al. [14] | 89 | 86 | 81 | N/A |
| Hwang et al. [15] | 92–95 | 91–94 | 73–78 | 85–88 |
| Park et al. [16] | 92.7–94.2 | 89.4–90.6 | 81.0–83.9 | 86.9–88.3 |
HCC, hepatocellular carcinoma; HBA, hepatobiliary contrast agent; MRI, magnetic resonance imaging; AASLD, American Association for the Study of Liver Diseases; LI-RADS, Liver Imaging Reporting and Data System; EASL, the European Association for the Study of the Liver; APASL, the Asian Pacific Association for the Study of the Liver; KLCA-NCC, Korean Liver Cancer Association-National Cancer Center; APHE, arterial phase hyperenhancement; PVP, portal venous phase; HBP, hepatobiliary phase; DP, delayed phase; N/A, not applicable.
Additional major features include enhancing “capsule”, nonperipheral “washout”, and threshold growth (≥50% in ≤6 months).
APASL criteria shows higher sensitivity but lower specificity than KLCA-NCC criteria since APASL does not exclude targetoid lesion unlike KLCA-NCC.
Despite the potential benefits of the sensitive detection of HCC using HBP images, HBA-MRI has several disadvantages compared to ECA-MRI. The absence of a true interstitial phase and a challenging arterial phase acquisition are the most problematic disadvantages. In HBA-MRI, extracellular-dominant and hepatocellular-dominant enhancements overlap at the transitional phase (TP; which corresponds to the delayed phase in ECA-MRI); therefore, hypointensity in TP may be either due to true washout or increased background parenchymal enhancement [26,28]. Therefore, Western guidelines such as AASLD, LI-RADS, and EASL do not include TP for washout assessment to maintain specificity when using HBA, which may entail decreased sensitivity for the detection of washout [5-7]. The strong parenchymal enhancement at the TP can also hinder detection of the “enhancing capsule,” which is one of the major imaging features of HCC. Previous studies showed a lower frequency of identifying the “enhancing capsule” in HCC when using HBA compared to ECA (31–47.4% vs. 73–87.4%) [29-31]. In addition, a smaller dose of HBA (0.025 mmol/kg) compared to ECA (0.1 mmol/kg) and the considerable occurrence of transient severe motion artifact due to impaired breath-hold ability after HBA administration may decrease the sensitivity for APHE detection [32,33]. These disadvantages may hamper the detection of major imaging features (i.e., APHE, delayed washout, and enhancing capsule) and may lead to a lower sensitivity for the definite diagnosis of HCC. Indeed, a few studies after the revision of the guidelines around 2018 showed that HBA-MRI is less sensitive than ECA-MRI for the definite diagnosis of HCC when applying LI-RADS (sensitivity, 67.3–71.2% vs. 78.9–83.1%), and comparable or less sensitive when applying EASL (sensitivity, 63.0– 67.5% vs. 71.5–76.2%) [29,34,35]. However, another study showed that HBA-MRI had comparable sensitivity to ECA-MRI when using the LI-RADS LR-5 criteria (78.1% vs. 73.7%) and a higher sensitivity than ECA-MRI for HCCs <20 mm (70.8% vs. 50.0%) [36]. Further studies are needed to determine the effect of these disadvantages of HBA on the diagnostic performance of HBA-MRI for HCC.
Several efforts have been made to improve the sensitivity of HBA-MRI using strict criteria such as LI-RADS, mainly in Asia, by altering the criteria or imaging sequences. For instance, a study showed that modifying the LI-RADS LR-5 criteria by extending “washout” to hypointensity in portal venous phase (PVP) or TP and “capsule” to either enhancing capsule appearance or non-enhancing capsule appearance in PVP or TP can increase sensitivity (79.2% vs. 60.4%) without significantly reducing the specificity (93.5% vs. 95.7%) [37]. Another study showed that using one of the independently significant ancillary features such as mild-moderate T2 hyperintensity, HBP hypointensity, non-enhancing “capsule,” or mosaic appearance to upgrade from LR-4 to LR-5 increased sensitivity (69.4–76.9% according to ancillary features used to upgrade vs. 66.2%) without a significant decrease in specificity (95.3–96.5% vs. 96.5%) [38]. The use of arterial subtraction images may overcome the weak APHE of HBA-MRI. Using arterial subtraction images can increase the detection rate of APHE in HCC (91.9% vs. 80.6%, compared to conventional arterial phase images) and increase the sensitivity of LI-RADS LR-5 for HCC diagnosis (64.1% vs. 55.9%) without a significant reduction in specificity (92.9% vs. 94.9%) [39]. Other studies reported that using later acquisition of PVP images after 70 seconds from the contrast injection detected more “washout” (83.6–84.1% vs. 50.9–64.6%) and enhancing “capsule” (27.6% vs. 19.8%) in HCC compared to using conventional PVP images, and may increase sensitivity (83.6% vs. 53.5%, LI-RADS; 82.8% vs. 50.0%, EASL) without a significant decrease in specificity (93.2% vs. 93.2%, both) for the diagnosis of HCC using the LI-RADS criteria [40,41]. The combined use of conventional and subtraction PVP images aided the detection of “washout” (detection frequency, 83% vs. 77%, compared to using conventional PVP only) and enhancing “capsule” (62% vs. 36%) [42]. However, these studies were performed retrospectively within a single center; a multi-center study with a prospective design is warranted to validate these promising results.
Gd-BOPTA-enhanced MRI
To our knowledge, only a few studies regarding MRI using Gd-BOPTA for the diagnosis of HCC have been published recently [43-46]. Similar to MRI using Gd-EOB-DTPA, HBP hypointensity on MRI using Gd-BOPTA is sensitive (sensitivity, 94.1%) but not specific (specificity, 26.9%) for HCC [44], and adding HBP hypointensity as a major feature for the definite diagnosis of HCC may increase the sensitivity for the detection of HCC using LI-RADS [44-46]. One study showed that APHE was seen similarly on MRI using Gd-BOPTA and Gd-EOB-DTPA (91.5% vs. 88.0%), while MRI using Gd-BOPTA detected more “washout” (60.2% vs. 45.3%) and enhancing “capsule” (50.2% vs. 33.3%); this is because as Gd-BOPTA is taken up by hepatocytes later than Gd-EOB-DTPA, the disadvantages related to TP, restricting the detection of “washout” in the portal phase only and hindering the detection of enhancing “capsule,” do not occur when using Gd-BOPTA [43]. However, as mentioned above, Gd-BOPTA has a disadvantage in that 60–120 minutes delay is needed to obtain HBP image, which may raise logistical issues [21]. Currently, there is no head-to-head comparison between Gd-BOPTA and Gd-EOB-DTPA for HCC diagnosis using recently modified criteria, warranting further investigation.
Comparison with other modalities: computed tomography (CT) and ECA-MRI
Although most major guidelines do not set the preferred imaging modalities among CT, ECA-MRI, and HBA-MRI for HCC diagnosis, previous meta-analyses have shown that HBA-MRI has a greater diagnostic accuracy with higher per-lesion sensitivity than CT (85–85.6% vs. 68–73.6%) and comparable specificity (94% vs. 93%) [47,48]. However, there have been mixed results regarding the comparison between HBA-MRI and ECA-MRI. Previous meta-analyses reported higher per-lesion sensitivity for HBA-MRI than ECA-MRI (85.6–87% vs. 74–77.5%), whereas more recent meta-analyses showed similar diagnostic performance for HBA-MRI and ECA-MRI (sensitivity, 76% vs. 72%; specificity, 92% vs. 92%) [47,49,50]. Caution is warranted in interpreting these results, as these differences in diagnostic accuracy may also stem from different study populations in different geographic regions (i.e., the proportion of subjects with chronic hepatitis B without cirrhosis) or different criteria for HCC diagnosis in each study, aside from using different contrast agent properties. For instance, in the latter meta-analysis, the sensitivity of HBA-MRI was 75% in the subgroup with hepatitis B while 59% in the subgroup with hepatitis C or alcoholic hepatitis, although there was no significant difference in sensitivity values between ECA-MRI and HBA-MRI in both subgroups [49]. In addition, the latter meta-analysis showed that HBA-MRI using the modified LI-RADS or EASL criteria with extended washout had higher sensitivity (83%) with reduced specificity (85%) than HBA-MRI or ECA-MRI using the conventional LI-RADS or EASL criteria (sensitivity, 66% and 68%; specificity, 91% and 94%, respectively) [49]. Another recent meta-analysis showed that HBA-MRI using strict criteria (i.e., accept washout in PVP only) had a lower sensitivity (63%) than HBA-MRI using extended criteria (i.e., extended washout to TP or HBP) (74%) or ECA-MRI (76%), while there were no significant differences in specificity (98%, 93%, and 96%, respectively) [51]. Therefore, further studies are needed to optimize the imaging criteria for HCC using HBA-MRI.
CEUS FOR HCC DIAGNOSIS
Imaging properties of CEUS
CEUS is another useful imaging modality for the diagnosis of focal hepatic lesions, which has been recognized recently as an important tool for HCC diagnosis in LI-RADS, EASL, APASL, and KLCA-NCC guidelines [6-9]. CEUS uses microbubble contrast agents with a diameter of 2–5 µm, which cannot pass through the vascular endothelium into the interstitial space [52]. Therefore, most ultrasound contrast agents (i.e., SonoVue/Lumason, Bracco, Milan, Italy and Definity/Luminity, Lantheus Medical Imaging, N. Billerica, MA, USA) are intravascular agents. One exception is Sonazoid (Daiichi-Sankyo, Tokyo, Japan; GE Healthcare, Chicago, IL, USA), taken up by Kupffer cells, which will be discussed later [53,54].
Due to the different pharmacokinetics of contrast agents used in ultrasound and CT/MRI, a substantial portion of intrahepatic cholangiocarcinomas (iCCAs) in cirrhotic livers show homogeneous APHE with washout in CEUS [55]. Therefore, diagnosing HCC solely by “APHE and washout” in CEUS can lead to the misdiagnosis of iCCA for HCC. However, several studies have shown different patterns of washout between HCC and iCCA in terms of timing and degree of washout; HCC usually shows late and mild washout (onset ≥60 seconds and less enhanced than liver but not devoid of enhancement), while iCCA shows early and marked washout (onset <60 seconds and virtually devoid of enhancement) (Fig. 2) [56-60]. Using the diagnostic criteria of “APHE with late and mild washout” for HCC by CEUS, many studies reported a good specificity (78.6–100%) but a lower sensitivity (38.6–92%) for HCC diagnosis, especially when compared to the conventional “APHE and washout” criteria or the subjective on-site diagnosis (Tables 2, 3) [17-20,61-68]. Several recent meta-analyses regarding CEUS LI-RADS reported a pooled sensitivity and specificity of 69–73% and 88–95% for LR-5, respectively [69-71].
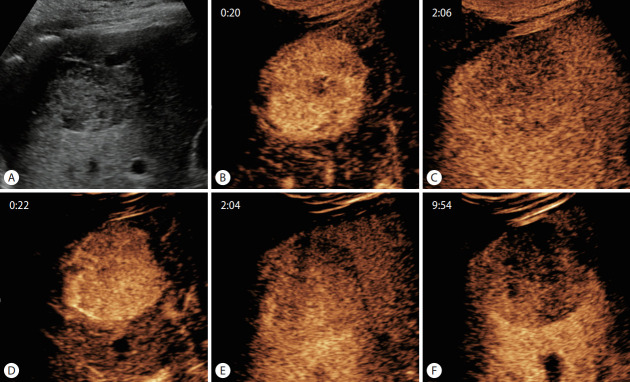
Figure 2.
Typical contrast-enhanced ultrasound findings of hepatocellular carcinoma using SonoVue and Sonazoid. (A) Approximately 4.5-cm sized hypoechoic mass in liver segment 6 on B-mode ultrasound. After administration of SonoVue, the mass shows (B) hyperenhancement in the arterial phase (20 seconds) and (C) mild washout in the delayed phase, but not devoid of enhancement (126 seconds). The same lesion enhanced with Sonazoid also shows (D) arterial phase hyperenhancement (22 seconds) and (E) mild delayed washout (124 seconds), as well as (F) clear hypointensity in the Kupffer phase (approximately 10 minutes after contrast administration).
Table 2.
Diagnostic performance of CEUS LI-RADS for HCC
| Study | Study type | Contrast agent | Diagnostic criteria | Sensitivity (%) | Specificity (%) |
|---|---|---|---|---|---|
| Terzi et al. [61] (2018) | Retrospective | SonoVue | LR-5 | 62.0 | 96.0‡ |
| Li et al. [62] (2019) | Retrospective | SonoVue | LR-5 | 89.1 | 80.4 |
| Makoyeva et al. [63] (2020) | Retrospective | Definity | LR-5 | 86.0 | 96.0 |
| LR-5/TIV | 92.0 | 96.0 | |||
| Huang et al. [17],* (2020) | Retrospective | SonoVue | LR-5 | 73.3 | 97.1 |
| Zheng et al. [64] (2020) | Retrospective | SonoVue | LR-5 | 75.0 | 96.0 |
| Modified LR-5† | 85.0 | 94.0 | |||
| Strobel et al. [19] (2021) | Prospective | Unmentioned | LR-5 | 65.2 | 78.6 |
| Li et al. [65] (2021) | Retrospective | SonoVue | LR-5 | 75.5 | 93.9 |
| Ding et al. [66] (2021) | Retrospective | SonoVue | LR-5 | 75.6 | 93.8 |
| Li et al. [67] (2021) | Retrospective | SonoVue | LR-5 | 49.6–64.3 | 85.3–91.7 |
| Ghiuchici et al. [68] (2021) | Retrospective | SonoVue | LR-5 | 71.9 | 94.3 |
| Schellhaas et al. [20] (2021) | Prospective | Unmentioned | LR-5/TIV | 64.0 | 78.9 |
| Zhou et al. [18] (2022) | Prospective | SonoVue | LR-5 | 38.6–63.6 | 92.7–100.0 |
CEUS, contrast-enhanced ultrasound; LI-RADS, Liver Imaging Reporting and Data System; HCC, hepatocellular carcinoma; TIV, tumor in vein.
All lesions are 20 mm or smaller.
Lesions with non-rim APHE and early but not punched-out washout are classified into LR-5 rather than LR-M.
Recalculated based on the data reported.
Table 3.
Comparison of diagnostic performance for HCC between CEUS LI-RADS and other diagnostic criteria
| Study | Study type | Contrast agent | LI-RADS |
“APHE and washout” |
On-site diagnosis† |
|||
|---|---|---|---|---|---|---|---|---|
| Sen (%) | Spe (%) | Sen (%) | Spe (%) | Sen (%) | Spe (%) | |||
| Huang et al. [17],* (2020) | Retrospective | SonoVue | 73.3 | 97.1 | 88.6 | 87.1 | N/A | N/A |
| Strobel et al. [19] (2021) | Prospective | Unmentioned | 65.2 | 78.6 | 74.3 | 63.0 | 91.5 | 67.4 |
| Schellhaas et al. [20] (2021) | Prospective | Unmentioned | 64.0 | 78.9 | 68.6 | 57.9 | 90.9 | 64.9 |
| Zhou et al. [18] (2022) | Prospective | SonoVue | 38.6–63.6 | 92.7–100.0 | 88.6–100.0 | 28.6–64.3 | N/A | N/A |
HCC, hepatocellular carcinoma; CEUS, contrast-enhanced ultrasound; LI-RADS, Liver Imaging Reporting and Data System; APHE, arterial phase hyperenhancement; Sen, sensitivity; Spe, specificity; N/A, not applicable.
All lesions are 20 mm or smaller.
Subjective on-site diagnosis of the examiner.
Advantages and limitations of CEUS
Despite the unsatisfactory sensitivity of CEUS due to the strict criteria for HCC diagnosis when used alone, CEUS has inherent advantages compared to CT/MRI. Unlike CT/MRI, which uses a predetermined scanning delay for the arterial phase, CEUS enables real-time arterial phase evaluation. Therefore, CEUS can be more sensitive when reevaluating APHE detection for lesions that lack APHE on CT/MRI due to mistiming [53,72,73]. Indeed, most major guidelines recommend using CEUS as a second-line modality when first-line examinations (i.e., CT or MRI) are inconclusive [7-9]. Several studies have shown that CEUS can depict more APHE and/or washout when used as a second-line modality for indeterminate lesions on CT/MRI (i.e., LR-3 or LR-4 lesions), and it can correctly upgrade the LI-RADS category from LR-3 or LR-4 to LR4, LR-5, or LR-M with few false positives [74-76]. In addition, arterioportal shunts or vascular pseudolesions are rarely visualized on CEUS, which are common pseudolesions mimicking true hepatic lesions and therefore inadequately categorized as LR-3 or LR-4 on CT/MRI [53,77,78]. Indeed, CEUS combined with grayscale ultrasound differentiated vascular pseudolesions such as arterioportal shunts from true nodules when MRI findings were inconclusive, with a small number of false negatives [75]. Another recent prospective study also showed the usefulness of CEUS as a second-line modality; although CEUS alone is less sensitive than HBA-MRI (60.8% vs. 72.2% and 86.1% according to EASL and KLCA-NCC guidelines, respectively), the additional use of CEUS for inconclusive lesions on HBA-MRI as a second-line modality can increase sensitivity (83.5% and 91.1% vs. 72.2% and 86.1% according to EASL and KLCA-NCC guidelines, respectively) with no additional false positives [79].
CEUS can also offer quantitative features of dynamic contrast enhancement by analyzing the time-intensity curve, and it may be used for differentiating HCCs from other hepatic tumors [80-84]. One study comparing quantitative CEUS parameters between HCC and focal nodular hyperplasia reported that maximum intensity and rise slope were higher in focal nodular hyperplasia, while rise time and time-to-peak were higher in HCC [82]. Two other studies reported differences in quantitative parameters, including washout time and maximum intensity between HCC and metastasis, and area under curves (AUCs) for washout time for differentiating HCC and metastasis are reported to be 0.780 and 0.922, respectively [83,84]. However, further studies are required to validate these results.
CEUS has several inherent limitations of ultrasound, such as operator dependency, limited sonic window, especially in patients with advanced cirrhosis, and limited capability for staging [54,85]. Several recent studies have shown mixed results for the inter-reader agreement of the CEUS LI-RADS criteria [18,62,63,67]. Inter-reader agreement of CEUS LI-RADS criteria has been reported to vary according to studies, ranging from moderate to excellent (κ=0.60–0.90) [18,62,63,67]. Among the imaging features of HCC on CEUS, inter-reader agreement was best in APHE (κ=0.65–0.83), followed by washout (κ=0.52–0.71), and ancillary features such as mosaic architecture (κ=0.124) or nodule-in-nodule appearance (κ=0.098) [18,62]. Another limitation is that CEUS permits the characterization of a limited number of targeted lesions on a single examination [60]. Thus, CEUS is not recommended for use in staging in LI-RADS, EASL, KLCA-NCC, and World Federation for Ultrasound in Medicine and Biology guidelines, and additional CT/MRI is required for staging even if HCC is diagnosed solely by CEUS [7,9,60,81].
Sonazoid-enhanced ultrasound
While LI-RADS, EASL, and KLCA-NCC allow only intravascular agents for HCC diagnosis, APASL accepts Sonazoid to diagnose HCC; nodules showing hypervascularity and/or Kupffer phase defects (discussed below) on Sonazoid-enhanced ultrasound can be diagnosed as HCC according to the APASL guideline [7-9,60]. Sonazoid is a liver-specific ultrasound contrast agent that is taken up by Kupffer cells after initial vascular distribution, enabling Kupffer phase (postvascular phase) imaging as well as vascular phase imaging [85]. Compared to intravascular agents, which use a low mechanical index (<0.1 MI), Sonazoid-enhanced ultrasound uses an intermediate mechanical index in the range of 0.2–0.3 due to its higher resistance to acoustic pressure [85]. With Sonazoid, imaging acquisition during the vascular phase, including the arterial phase and the PVP, is similar to that of intravascular agents, but following the vascular phase, an additional Kupffer phase, when microbubbles are accumulated in the Kupffer cells by phagocytosis, can be available [85]. Most malignant hepatic tumors, including HCCs, appear as non-enhancing or hypoenhancing defects in the Kupffer phase due to depletion of Kupffer cells, whereas most benign hepatocyte-origin tumors are iso- or hyperechoic at the Kupffer phase (Fig. 2). In addition, re-injection of Sonazoid in the Kupffer phase allows evaluation of arterial flow in Kupffer phase defect lesions; these properties may help increase the diagnostic performance of Sonazoid-enhanced ultrasound [85,86].
Sonazoid-enhanced ultrasound has several limitations related to the Kupffer phase. First, Kupffer phase defects may not be adequately evaluated in hyperechoic lesions when using low-mechanical index contrast imaging due to the influence of the background B-mode signal, which can result in false-negative nodules [87,88]. Second, a substantial portion of well-differentiated HCCs showed iso-enhancement in the Kupffer phase. One study using intraoperative CEUS showed that the proportion of hypoechogenicity in the Kupffer phase is significantly lower in well-differentiated HCCs than in moderately or poorly differentiated HCCs (54% vs. 92%), while another study reported that 83% of early HCCs were isoechoic at the Kupffer phase [89,90]. Lastly, similar to Gd-EOB-DTPA, theoretically, the additional enhancement via Kupffer cell uptake of bubbles during the TP of Sonazoid-enhanced ultrasound might cause the pseudo-washout effect (Table 4) [91].
Table 4.
Differences between SonoVue and Sonazoid for HCC diagnosis
| SonoVue | Sonazoid | |
|---|---|---|
| Composition | Gas: Sulfur hexafluoride | Gas: Perfluorobutane |
| Shell: mixture of DSPC and DPPG.Na | Shell: H-EPSNa | |
| Pharmacokinetics | Blood pool agent | Initial vascular distribution, then taken up by Kupffer cells |
| Image acquisition | Vascular phase only | Vascular and Kupffer phase ± re-injection technique |
| Advantages | Widely available | Allowing both vascular and Kupffer phase imaging |
| Widely studied with well-established diagnostic criteria | Re-injection technique may help increase diagnostic performance | |
| Stable time window of Kupffer phase: whole liver evaluation available | ||
| Disadvantages | No Kupffer phase imaging | Not yet available in some regions |
| Short time window of vascular phase: only limited number of lesions can be examined | Less studied than SonoVue | |
| Kupffer phase-related limitations: 1) false negative for hyperechoic lesions or well-differentiated HCCs, 2) theoretical pseudo-washout effect |
HCC, hepatocellular carcinoma; DSPC, distearoylphosphatidylcholine; DPPG.Na, dipalmitoyl phosphatidylglycerol sodium; H-EPSNa, hydrogenated egg phosphatidylserine sodium.
Despite these limitations, a recent meta-analysis reported a good diagnostic performance for Sonazoid-enhanced ultrasound with pooled sensitivity and specificity of 90% and 97%, respectively, albeit with significant heterogeneity among studies [92]. There have been efforts to use Sonazoid using the CEUS LI-RADS criteria [91,93]. For instance, the modified CEUS LI-RADS LR-5 criteria, which included nodules ≥1 cm in size, non-rim and non-peripheral discontinuous globular APHE, late washout, and hypoenhancement in the Kupffer phase, showed sensitivity, specificity, and positive predictive value for modified LR-5 of 70.3%, 92.5%, and 93.8%, respectively, with miscategorization as LR-5 for two of 10 hemangiomas [93]. Even without the Kupffer phase, Sonazoid-enhanced ultrasound showed better sensitivity than SonoVue-enhanced CEUS (79% vs. 67%) with comparable specificity (both 100%) [91]. This difference possibly stemmed from the different washout profiles of the two contrast agents. Sonazoid-enhanced ultrasound showed a later washout time than SonoVue-enhanced CEUS (101 vs. 84 seconds), which may enable the detection of the late washout of HCCs more frequently. However, the reason for the different washout profiles between the two CEUS agents is not well known [91,94]. Until now, there has been no consensus regarding the diagnostic criteria for diagnosis of HCC on Sonazoid-enhanced ultrasound. Although the combination of APHE and Kupffer phase hypoenhancement of a hepatic lesion may provide high sensitivity, the downside would be a low specificity. Similar to HCC diagnostic criteria of KLCA-NCC guideline with HBA-MRI, it might be considered that the timing for determining late/mild washout criteria could be extended to Kupffer phase, only after excluding peripheral globular enhancement, rim APHE, rapid washout within 60 seconds, or marked washout (punchout appearance) within 2 minutes after contrast injection. In addition, contrast dosage and image acquisition methods vary between studies; either vendor-recommended dose or reduced dose can be used and late vascular phases or TP may or may not be obtained [85,91,93]. Based on the studies so far, Sonazoid-enhanced ultrasound is expected to be included as a diagnostic modality for HCC in 2022 KLCA-NCC guideline. Nevertheless, further studies are still warranted to validate these results, refine the diagnostic criteria, and standardize the protocol for Sonazoid-enhanced ultrasound.
FUTURE ASPECTS FOR HCC SURVEILLANCE AND DIAGNOSIS
Novel strategies for HCC surveillance: abbreviated MRI and CEUS
Current guidelines recommend surveillance in patients at risk of HCC with biannual ultrasound with or without serum alpha-fetoprotein measurement [5,7-9]. Previous studies, including randomized controlled trials, have shown that biannual surveillance of HCC using ultrasound significantly reduced overall or HCC-related mortality [95-97]. However, ultrasound has the limitation of low detection sensitivity for HCC, and a meta-analysis showed sensitivities for detecting early HCC in patients with cirrhosis of 63% and 45% using ultrasound with and without serum alpha-fetoprotein measurements, respectively [98,99]. Dynamic CT and MRI more sensitively detect HCC than ultrasound; however, the former has a risk of ionizing radiation exposure, while the latter has drawbacks in terms of cost and time effectiveness for HCC surveillance [98]. Therefore, novel strategies for HCC surveillance, abbreviated MRI and CEUS, have been studied to overcome the limitations of current surveillance modalities.
Abbreviated MRI is a simplified MRI protocol tailored to evaluate a specific disease. While complete liver MRI takes approximately 40 minutes to perform, abbreviated MRI involves only a few sequences necessary for HCC detection and is typically performed within 15 minutes, although it depends on the protocol [98]. Abbreviated MRI studies for HCC surveillance can be classified into three approaches: 1) non-contrast abbreviated MRI, typically consisting of T1-weighted in-phase/out-of-phase, T2-weighted, and diffusion-weighted imaging; 2) dynamic contrast-enhanced abbreviated MRI, typically consisting of pre-contrast, arterial, portal venous, and delayed phase imaging; and 3) HBP abbreviated MRI, typically consisting of HBP and T2-weighted imaging with or without diffusion-weighted imaging. Detailed information on the sequences, advantages, and disadvantages of each approach are beyond the scope of this paper and are available in another focused review [100].
To date, most studies regarding surveillance of HCC using abbreviated MRI have been performed retrospectively by simulating abbreviated MRI protocols from complete liver MRI. These retrospective, simulated studies have shown relatively good diagnostic performance (per-patient sensitivity, 61.5–92.1%; specificity, 76.4–100%) [101-110]. Recent meta-analyses reported pooled sensitivity and specificity of abbreviated MRI for detecting HCC of 86% and 94–96%, respectively, which were higher than those of ultrasound (sensitivity, 82% vs. 53%; specificity, 98% vs. 88%) [111,112]. However, few studies have focused on the performance of abbreviated MRI in a real surveillance setting [113]. Currently, prospective studies are ongoing, and they are expected to provide prospective data of abbreviated MRI that can validate the results of existing studies [114,115].
Sonazoid-enhanced ultrasound also has the potential to be used for the surveillance of HCC in high-risk patients. Sonazoid allows Kupffer phase imaging, which has a very stable time window of at least 60 minutes, and allows enough time to evaluate the entire liver for HCC surveillance [85,116]. A randomized controlled trial showed that Sonazoid-enhanced ultrasound can detect significantly smaller HCC nodules than B-mode ultrasound (13.0 vs. 16.7 mm) in patients with high risk for HCC development, even with shorter examination time (6.6 vs. 16.2 minutes) [117]. Although another prospective study did not find significant improvement in detecting early HCC by adding Sonazoid-enhanced ultrasound in routine ultrasound surveillance (detection rate, 1.1% vs. 0.8%), the false-referral rate was significantly reduced when CEUS was additionally used (1.1% vs. 4.4%) [116]. However, further studies regarding survival benefit and cost-effectiveness are warranted to clarify the benefits of CEUS in HCC surveillance. So far, the Asian Federation of Societies for Ultrasound in Medicine and Biology permits CEUS for HCC surveillance, especially in patients with very coarse liver parenchyma, while the World Federation for Ultrasound in Medicine and Biology does not recommend routine use of CEUS for HCC surveillance [81,85].
Deep learning in HCC diagnosis
Deep learning is a subset of machine learning that uses an architecture of artificial neural networks inspired by biological neural networks. Unlike classic machine learning methods, which depend on hand-engineered features, deep learning methods bypass feature engineering and learn features directly from data [118,119]. Deep learning has shown breakthrough performance improvements in various fields, including image analysis. A convolutional neural network is a deep learning architecture consisting of convolutional, pooling, and fully connected layers, which is the most commonly used architecture for processing images. Detailed information on deep learning and convolutional neural network is available in another focused review [118]. Regarding HCC imaging, deep learning has been studied not only for diagnosis but also for other fields such as segmentation, pathologic grading, and prediction of treatment response and prognosis [120]. In this article, we briefly introduce several studies on deep learning for the detection and diagnosis of HCC.
Deep learning algorithms for HCC diagnosis have been applied to multiple imaging modalities, including ultrasound, CT, and MRI. For ultrasound, Schmauch et al. [121] designed an ensemble model of ResNet50 and DenseNet to detect focal liver lesions from ultrasound and classified them as benign or malignant lesions, and reported AUCs of 0.935 and 0.916 in the test set for detection and classification, respectively. Yang et al. [122] developed another convolutional neural network model on ultrasound images combined with clinical information for the classification of focal liver lesions into benign or malignant lesions, which showed an AUC of 0.924 and higher sensitivity and specificity than expert radiologists on external datasets (86.5% vs. 76.1% and 85.5% vs. 76.9%, respectively). For CT, Yasaka et al. [123] trained a convolutional neural network model for the classification of liver masses into five categories (A, classic HCCs; B, malignant liver tumors other than classic and early HCCs; C, indeterminate masses or masslike lesions and rare benign liver masses other than hemangiomas and cysts; D, hemangiomas; and E, cysts), and the model showed an accuracy for the classification of liver masses of 84% and AUC differentiating A–B vs. C–E of 0.92. Another study on deep learning-based liver tumor classification on MRI showed 90.0% accuracy for differentiation between cysts, hemangiomas, focal nodular hyperplasias, HCCs, iCCAs, and colorectal cancer metastases and an AUC of 0.992 for HCC diagnosis, although only masses with typical imaging findings were included and the model was not externally validated [124]. More recent studies regarding deep learning algorithms showed comparable performance to radiologists for the classification of a liver mass on CT (accuracy for classification between HCC and non-HCC, 80.5% vs. 79.3%) or MRI (sensitivity and specificity for classification between benign and malignant, 91.9% vs. 89.1% and 94.1% vs. 90.4%, respectively) in external datasets [125,126]. In addition to classification, deep learning-based detection of HCCs on CT or MRI has been studied. One study developed a deep-learning algorithm for detecting HCCs on HBP images, which showed comparable performance to less-experienced radiologists on external datasets (sensitivity and specificity, 87% vs. 86% and 93% vs. 92%, respectively) [127]. Other studies also showed relatively good performance of deep-learning algorithms for detecting HCCs on CT (sensitivity, 92.0% and false-positive rate, 13.7%) or MRI (sensitivity, 89.7% and positive predictive value, 85.0% for lesions ≤2 cm) [128,129]. Regarding LI-RADS, one study reported that deep learning methods on MRI can distinguish between LR-3 and LR-4 or LR-5 lesions with an accuracy of 90% in the test set [130]. However, another study showed that the overall accuracy of the deep learning model for LI-RADS classification was only 41.2% and 47.7% in external CT and MRI datasets, respectively, although it had limitations in that only a small number of images were used for training [131]. Further investigations using larger multi-center data may be warranted to apply deep learning models in LI-RADS classification.
CONCLUSION
In recent years, several major guidelines for HCC have newly included HBA-MRI as the primary diagnostic test or CEUS as a second-line diagnostic test. Several studies have demonstrated that strongly enhanced hepatic parenchyma in HBP allows for better detection of HCC and staging of HCC. In addition, the usefulness of CEUS as a second-line modality has been reported to increase sensitivity without losing specificity. However, to date, there are significant discrepancies in the diagnostic criteria of HBA-MRI and preferred CEUS agents among major guidelines, which could be related to the prevalence of HCC and its treatment patterns in various regions. The application of novel surveillance strategies such as abbreviated MRI or CEUS and deep learning for HCC needs further validation in the near future. To resolve these issues, further large-scale prospective studies are required. Finally, the development and adoption of a universal lexicon for liver imaging would be necessary to decrease gaps between guidelines, enhance communication, and facilitate future scientific research.
Acknowledgments
We thank Sungeun Park and Hyo-Jin Kang for courtesy of the hepatobiliary MRI and CEUS images.
Abbreviations
- AASLD
the American Association for the Study of Liver Diseases
- APASL
the Asian Pacific Association for the Study of the Liver
- APHE
arterial phase hyperenhancement
- AUC
area under curve
- CEUS
contrast-enhanced ultrasound
- CT
computed tomography
- EASL
the European Association for the Study of the Liver
- ECA
extracellular contrast agent
- Gd-BOPTA
gadobenate dimeglumine
- Gd-EOB-DTPA
gadoxetic acid
- HBA-MRI
hepatobiliary contrast agent magnetic resonance imaging
- HBP
hepatobiliary phase
- HCC
hepatocellular carcinoma
- iCCA
intrahepatic cholangiocarcinoma
- KLCA-NCC
the Korean Liver Cancer Association-National Cancer Center
- LI-RADS
Liver Imaging Reporting and Data System
- OATP8
organic anion transporting polypeptide 8
- PVP
portal venous phase
- TP
transitional phase
Footnotes
Authors’ contributions
Study conception and design: Jeong Min Lee, Tae-Hyung Kim
Acquisition of data: Junghoan Park
Drafting of the manuscript: Junghoan Park
Critical revision of the manuscript: Jeong Min Lee, Tae-Hyung Kim, Jeong Hee Yoon
Conflicts of Interest
Jeong Min Lee received grants from Bayer Healthcare, Canon Healthcare, Philips Healthcare, GE Healthcare, CMS, Guerbet, Samsung Medison, Bracco, personal fees from Bayer Healthcare, Siemens Healthineer, Samsung Medison, Guerbet, outside the submitted work. Jeong Hee Yoon received personal fees from Bayer and Philips Healthcare. Other authors have no conflicts of interest.
REFERENCES
- 1.Yang JD, Hainaut P, Gores GJ, Amadou A, Plymoth A, Roberts LR. A global view of hepatocellular carcinoma: trends, risk, prevention and management. Nat Rev Gastroenterol Hepatol. 2019;16:589–604. doi: 10.1038/s41575-019-0186-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ozakyol A. Global epidemiology of hepatocellular carcinoma (HCC epidemiology) J Gastrointest Cancer. 2017;48:238–240. doi: 10.1007/s12029-017-9959-0. [DOI] [PubMed] [Google Scholar]
- 3.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 4.Tang A, Cruite I, Mitchell DG, Sirlin CB. Hepatocellular carcinoma imaging systems: why they exist, how they have evolved, and how they differ. Abdom Radiol (NY) 2018;43:3–12. doi: 10.1007/s00261-017-1292-3. [DOI] [PubMed] [Google Scholar]
- 5.Marrero JA, Kulik LM, Sirlin CB, Zhu AX, Finn RS, Abecassis MM, et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the American Association for the Study of Liver Diseases. Hepatology. 2018;68:723–750. doi: 10.1002/hep.29913. [DOI] [PubMed] [Google Scholar]
- 6.Chernyak V, Fowler KJ, Kamaya A, Kielar AZ, Elsayes KM, Bashir MR, et al. Liver imaging reporting and data system (LI-RADS) version 2018: imaging of hepatocellular carcinoma in at-risk patients. Radiology. 2018;289:816–830. doi: 10.1148/radiol.2018181494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.European Association for the Study of the Liver EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2018;69:182–236. doi: 10.1016/j.jhep.2018.03.019. [DOI] [PubMed] [Google Scholar]
- 8.Omata M, Cheng AL, Kokudo N, Kudo M, Lee JM, Jia J, et al. Asia-Pacific clinical practice guidelines on the management of hepatocellular carcinoma: a 2017 update. Hepatol Int. 2017;11:317–370. doi: 10.1007/s12072-017-9799-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Korean Liver Cancer Association (KLCA) National Cancer Center (NCC) 2018 Korean Liver Cancer Association-National Cancer Center Korea practice guidelines for the management of hepatocellular carcinoma. Korean J Radiol. 2019;20:1042–1113. doi: 10.3348/kjr.2019.0140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim TH, Kim SY, Tang A, Lee JM. Comparison of international guidelines for noninvasive diagnosis of hepatocellular carcinoma: 2018 update. Clin Mol Hepatol. 2019;25:245–263. doi: 10.3350/cmh.2018.0090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhou J, Sun H, Wang Z, Cong W, Wang J, Zeng M, et al. Guidelines for the diagnosis and treatment of hepatocellular carcinoma (2019 edition) Liver Cancer. 2020;9:682–720. doi: 10.1159/000509424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shao YY, Wang SY, Lin SM, Diagnosis Group. Systemic Therapy Group Management consensus guideline for hepatocellular carcinoma: 2020 update on surveillance, diagnosis, and systemic treatment by the Taiwan Liver Cancer Association and the Gastroenterological Society of Taiwan. J Formos Med Assoc. 2020;120:1051–1060. doi: 10.1016/j.jfma.2020.10.031. [DOI] [PubMed] [Google Scholar]
- 13.Jeon SK, Lee JM, Joo I, Yoo J, Park JY. Comparison of guidelines for diagnosis of hepatocellular carcinoma using gadoxetic acid-enhanced MRI in transplantation candidates. Eur Radiol. 2020;30:4762–4771. doi: 10.1007/s00330-020-06881-y. [DOI] [PubMed] [Google Scholar]
- 14.Clarke CGD, Albazaz R, Smith CR, Rowe I, Treanor D, Wyatt JI, et al. Comparison of LI-RADS with other non-invasive liver MRI criteria and radiological opinion for diagnosing hepatocellular carcinoma in cirrhotic livers using gadoxetic acid with histopathological explant correlation. Clin Radiol. 2021;76:333–341. doi: 10.1016/j.crad.2020.12.007. [DOI] [PubMed] [Google Scholar]
- 15.Hwang SH, Park MS, Park S, Lim JS, Kim SU, Park YN. Comparison of the current guidelines for diagnosing hepatocellular carcinoma using gadoxetic acid-enhanced magnetic resonance imaging. Eur Radiol. 2021;31:4492–4503. doi: 10.1007/s00330-020-07468-3. [DOI] [PubMed] [Google Scholar]
- 16.Park SH, Shim YS, Kim B, Kim SY, Kim YS, Huh J, et al. Retrospective analysis of current guidelines for hepatocellular carcinoma diagnosis on gadoxetic acid-enhanced MRI in at-risk patients. Eur Radiol. 2021;31:4751–4763. doi: 10.1007/s00330-020-07577-z. [DOI] [PubMed] [Google Scholar]
- 17.Huang JY, Li JW, Lu Q, Luo Y, Lin L, Shi YJ, et al. Diagnostic accuracy of CEUS LI-RADS for the characterization of liver nodules 20 mm or smaller in patients at risk for hepatocellular carcinoma. Radiology. 2020;294:329–339. doi: 10.1148/radiol.2019191086. [DOI] [PubMed] [Google Scholar]
- 18.Zhou H, Zhang C, Du L, Jiang J, Zhao Q, Sun J, et al. Contrast-enhanced ultrasound liver imaging reporting and data system in diagnosing hepatocellular carcinoma: diagnostic performance and interobserver agreement. Ultraschall Med. 2022;43:64–71. doi: 10.1055/a-1168-6321. [DOI] [PubMed] [Google Scholar]
- 19.Strobel D, Jung EM, Ziesch M, Praktiknjo M, Link A, Dietrich CF, et al. Real-life assessment of standardized contrast-enhanced ultrasound (CEUS) and CEUS algorithms (CEUS LI-RADS®/ESCULAP) in hepatic nodules in cirrhotic patients-a prospective multicenter study. Eur Radiol. 2021;31:7614–7625. doi: 10.1007/s00330-021-07872-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schellhaas B, Bernatik T, Bohle W, Borowitzka F, Chang J, Dietrich CF, et al. Contrast-enhanced ultrasound algorithms (CEUS-LI-RADS/ESCULAP) for the noninvasive diagnosis of hepatocellular carcinoma - a prospective multicenter DEGUM study. Ultraschall Med. 2021;42:178–186. doi: 10.1055/a-1198-4874. [DOI] [PubMed] [Google Scholar]
- 21.Seale MK, Catalano OA, Saini S, Hahn PF, Sahani DV. Hepatobiliary-specific MR contrast agents: role in imaging the liver and biliary tree. Radiographics. 2009;29:1725–1748. doi: 10.1148/rg.296095515. [DOI] [PubMed] [Google Scholar]
- 22.Vanhooymissen IJSML, Thomeer MG, Braun LMM, Gest B, van Koeverden S, Willemssen FE, et al. Intrapatient comparison of the hepatobiliary phase of Gd-BOPTA and Gd-EOB-DTPA in the differentiation of hepatocellular adenoma from focal nodular hyperplasia. J Magn Reson Imaging. 2019;49:700–710. doi: 10.1002/jmri.26227. [DOI] [PubMed] [Google Scholar]
- 23.Frydrychowicz A, Lubner MG, Brown JJ, Merkle EM, Nagle SK, Rofsky NM, et al. Hepatobiliary MR imaging with gadoliniumbased contrast agents. J Magn Reson Imaging. 2012;35:492–511. doi: 10.1002/jmri.22833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. American College of Radiology (ACR). The LI-RADS® v2018 Manual. ACR web site, < https://www.acr.org/-/media/ACR/Files/Clinical-Resources/LI-RADS/LI-RADS-2018-Manual-5Dec18.pdf>. Accessed 28 Jun 2021.
- 25.Choi JY, Lee JM, Sirlin CB. CT and MR imaging diagnosis and staging of hepatocellular carcinoma: part I. Development, growth, and spread: key pathologic and imaging aspects. Radiology. 2014;272:635–654. doi: 10.1148/radiol.14132361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Choi JY, Lee JM, Sirlin CB. CT and MR imaging diagnosis and staging of hepatocellular carcinoma: part II. Extracellular agents, hepatobiliary agents, and ancillary imaging features. Radiology. 2014;273:30–50. doi: 10.1148/radiol.14132362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Joo I, Lee JM, Lee DH, Jeon JH, Han JK, Choi BI. Noninvasive diagnosis of hepatocellular carcinoma on gadoxetic acid-enhanced MRI: can hypointensity on the hepatobiliary phase be used as an alternative to washout? Eur Radiol. 2015;25:2859–2868. doi: 10.1007/s00330-015-3686-3. [DOI] [PubMed] [Google Scholar]
- 28.Zech CJ, Ba-Ssalamah A, Berg T, Chandarana H, Chau GY, Grazioli L, et al. Consensus report from the 8th international forum for liver magnetic resonance imaging. Eur Radiol. 2020;30:370–382. doi: 10.1007/s00330-019-06369-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Min JH, Kim JM, Kim YK, Cha DI, Kang TW, Kim H, et al. Magnetic resonance imaging with extracellular contrast detects hepatocellular carcinoma with greater accuracy than with gadoxetic acid or computed tomography. Clin Gastroenterol Hepatol. 2020;18:2091–2100. doi: 10.1016/j.cgh.2019.12.010. e7. [DOI] [PubMed] [Google Scholar]
- 30.Min JH, Kim JM, Kim YK, Kang TW, Lee SJ, Choi GS, et al. Prospective intraindividual comparison of magnetic resonance imaging with gadoxetic acid and extracellular contrast for diagnosis of hepatocellular carcinomas using the liver imaging reporting and data system. Hepatology. 2018;68:2254–2266. doi: 10.1002/hep.30122. [DOI] [PubMed] [Google Scholar]
- 31.Son J, Hwang SH, Park S, Han K, Chung YE, Choi JY, et al. Imaging features of hepatocellular carcinoma: quantitative and qualitative comparison between MRI-enhanced with Gd-EOB-DTPA and Gd-DTPA. Invest Radiol. 2019;54:494–499. doi: 10.1097/RLI.0000000000000562. [DOI] [PubMed] [Google Scholar]
- 32.Tamada T, Ito K, Sone T, Yamamoto A, Yoshida K, Kakuba K, et al. Dynamic contrast-enhanced magnetic resonance imaging of abdominal solid organ and major vessel: comparison of enhancement effect between Gd-EOB-DTPA and Gd-DTPA. J Magn Reson Imaging. 2009;29:636–640. doi: 10.1002/jmri.21689. [DOI] [PubMed] [Google Scholar]
- 33.Well L, Weinrich JM, Adam G, Bannas P. Transient severe respiratory motion artifacts after application of gadoxetate disodium: what we currently know. Rofo. 2018;190:20–30. doi: 10.1055/s-0043-120116. [DOI] [PubMed] [Google Scholar]
- 34.Lee S, Kim MJ, Kim SS, Shin H, Kim DY, Choi JY, et al. Retrospective comparison of EASL 2018 and LI-RADS 2018 for the noninvasive diagnosis of hepatocellular carcinoma using magnetic resonance imaging. Hepatol Int. 2020;14:70–79. doi: 10.1007/s12072-019-10002-3. [DOI] [PubMed] [Google Scholar]
- 35.Min JH, Kim JM, Kim YK, Kim H, Cha DI, Kang TW, et al. EASL versus LI-RADS: intra-individual comparison of MRI with extracellular contrast and gadoxetic acid for diagnosis of small HCC. Liver Int. 2021;41:2986–2996. doi: 10.1111/liv.15012. [DOI] [PubMed] [Google Scholar]
- 36.Kim YY, Kim YK, Min JH, Cha DI, Kim JM, Choi GS, et al. Intraindividual comparison of hepatocellular carcinoma washout between MRIs with hepatobiliary and extracellular contrast agents. Korean J Radiol. 2021;22:725–734. doi: 10.3348/kjr.2020.1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hwang SH, Park S, Han K, Choi JY, Park YN, Park MS. Optimal lexicon of gadoxetic acid-enhanced magnetic resonance imaging for the diagnosis of hepatocellular carcinoma modified from LI-RADS. Abdom Radiol (NY) 2019;44:3078–3088. doi: 10.1007/s00261-019-02077-1. [DOI] [PubMed] [Google Scholar]
- 38.Lee S, Kim SS, Bae H, Shin J, Yoon JK, Kim MJ. Application of liver imaging reporting and data system version 2018 ancillary features to upgrade from LR-4 to LR-5 on gadoxetic acid-enhanced MRI. Eur Radiol. 2021;31:855–863. doi: 10.1007/s00330-020-07146-4. [DOI] [PubMed] [Google Scholar]
- 39.Kim DH, Choi SH, Byun JH, Kang JH, Lim YS, Lee SJ, et al. Arterial subtraction images of gadoxetate-enhanced MRI improve diagnosis of early-stage hepatocellular carcinoma. J Hepatol. 2019;71:534–542. doi: 10.1016/j.jhep.2019.05.005. [DOI] [PubMed] [Google Scholar]
- 40.Kang HJ, Lee JM, Jeon SK, Jang S, Park S, Joo I, et al. Intraindividual comparison of dual portal venous phases for non-invasive diagnosis of hepatocellular carcinoma at gadoxetic acid-enhanced liver MRI. Eur Radiol. 2021;31:824–833. doi: 10.1007/s00330-020-07162-4. [DOI] [PubMed] [Google Scholar]
- 41.Baek KA, Kim SS, Shin HC, Hwang JA, Choi SY, Lee WH, et al. Gadoxetic acid-enhanced MRI for diagnosis of hepatocellular carcinoma in patients with chronic liver disease: can hypointensity on the late portal venous phase be used as an alternative to washout? Abdom Radiol (NY) 2020;45:2705–2716. doi: 10.1007/s00261-020-02553-z. [DOI] [PubMed] [Google Scholar]
- 42.Chung JW, Yu JS, Choi JM, Cho ES, Kim JH, Chung JJ. Subtraction images from portal venous phase gadoxetic acid-enhanced MRI for observing washout and enhancing capsule features in LI-RADS version 2018. AJR Am J Roentgenol. 2020;214:72–80. doi: 10.2214/AJR.18.20797. [DOI] [PubMed] [Google Scholar]
- 43.Allen BC, Ho LM, Jaffe TA, Miller CM, Mazurowski MA, Bashir MR. Comparison of visualization rates of LI-RADS version 2014 major features with IV gadobenate dimeglumine or gadoxetate disodium in patients at risk for hepatocellular carcinoma. AJR Am J Roentgenol. 2018;210:1266–1272. doi: 10.2214/AJR.17.18981. [DOI] [PubMed] [Google Scholar]
- 44.De Gaetano AM, Catalano M, Pompili M, Marini MG, Rodríguez Carnero P, et al. Critical analysis of major and ancillary features of LI-RADS v2018 in the differentiation of small (≤ 2 cm) hepatocellular carcinoma from dysplastic nodules with gadobenate dimeglumine-enhanced magnetic resonance imaging. Eur Rev Med Pharmacol Sci. 2019;23:7786–7801. doi: 10.26355/eurrev_201909_18988. [DOI] [PubMed] [Google Scholar]
- 45.Li Y, Chen J, Weng S, Yan C, Ye R, Zhu Y, et al. Hepatobiliary phase hypointensity on gadobenate dimeglumine-enhanced magnetic resonance imaging may improve the diagnosis of hepatocellular carcinoma. Ann Transl Med. 2021;9:55. doi: 10.21037/atm.2020.02.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhang Y, Tang W, Xie S, Chen J, Zhang L, Rong D, et al. The role of lesion hypointensity on gadobenate dimeglumine-enhanced hepatobiliary phase MRI as an additional major imaging feature for HCC classification using LI-RADS v2018 criteria. Eur Radiol. 2021;31:7715–7724. doi: 10.1007/s00330-021-07807-y. [DOI] [PubMed] [Google Scholar]
- 47.Hanna RF, Miloushev VZ, Tang A, Finklestone LA, Brejt SZ, Sandhu RS, et al. Comparative 13-year meta-analysis of the sensitivity and positive predictive value of ultrasound, CT, and MRI for detecting hepatocellular carcinoma. Abdom Radiol (NY) 2016;41:71–90. doi: 10.1007/s00261-015-0592-8. [DOI] [PubMed] [Google Scholar]
- 48.Li J, Wang J, Lei L, Yuan G, He S. The diagnostic performance of gadoxetic acid disodium-enhanced magnetic resonance imaging and contrast-enhanced multi-detector computed tomography in detecting hepatocellular carcinoma: a meta-analysis of eight prospective studies. Eur Radiol. 2019;29:6519–6528. doi: 10.1007/s00330-019-06294-6. [DOI] [PubMed] [Google Scholar]
- 49.Kim DW, Choi SH, Kim SY, Byun JH, Lee SS, Park SH, et al. Diagnostic performance of MRI for HCC according to contrast agent type: a systematic review and meta-analysis. Hepatol Int. 2020;14:1009–1022. doi: 10.1007/s12072-020-10100-7. [DOI] [PubMed] [Google Scholar]
- 50.Lee YJ, Lee JM, Lee JS, Lee HY, Park BH, Kim YH, et al. Hepatocellular carcinoma: diagnostic performance of multidetector CT and MR imaging-a systematic review and meta-analysis. Radiology. 2015;275:97–109. doi: 10.1148/radiol.14140690. [DOI] [PubMed] [Google Scholar]
- 51.Feng Z, Zhao H, Guan S, Wang W, Rong P. Diagnostic performance of MRI using extracellular contrast agents versus gadoxetic acid for hepatocellular carcinoma: a systematic review and meta-analysis. Liver Int. 2021;41:1117–1128. doi: 10.1111/liv.14850. [DOI] [PubMed] [Google Scholar]
- 52.Wilson SR, Burns PN. Microbubble-enhanced US in body imaging: what role? Radiology. 2010;257:24–39. doi: 10.1148/radiol.10091210. [DOI] [PubMed] [Google Scholar]
- 53.Kim TK, Noh SY, Wilson SR, Kono Y, Piscaglia F, Jang HJ, et al. Contrast-enhanced ultrasound (CEUS) liver imaging reporting and data system (LI-RADS) 2017 - a review of important differences compared to the CT/MRI system. Clin Mol Hepatol. 2017;23:280–289. doi: 10.3350/cmh.2017.0037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kim TH, Yoon JH, Lee JM. Emerging role of hepatobiliary magnetic resonance contrast media and contrast-enhanced ultrasound for noninvasive diagnosis of hepatocellular carcinoma: emphasis on recent updates in major guidelines. Korean J Radiol. 2019;20:863–879. doi: 10.3348/kjr.2018.0450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vilana R, Forner A, Bianchi L, García-Criado A, Rimola J, de Lope CR, et al. Intrahepatic peripheral cholangiocarcinoma in cirrhosis patients may display a vascular pattern similar to hepatocellular carcinoma on contrast-enhanced ultrasound. Hepatology. 2010;51:2020–2029. doi: 10.1002/hep.23600. [DOI] [PubMed] [Google Scholar]
- 56.Liu GJ, Wang W, Lu MD, Xie XY, Xu HX, Xu ZF, et al. Contrast-enhanced ultrasound for the characterization of hepatocellular carcinoma and intrahepatic cholangiocarcinoma. Liver Cancer. 2015;4:241–252. doi: 10.1159/000367738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Han J, Liu Y, Han F, Li Q, Yan C, Zheng W, et al. The degree of contrast washout on contrast-enhanced ultrasound in distinguishing intrahepatic cholangiocarcinoma from hepatocellular carcinoma. Ultrasound Med Biol. 2015;41:3088–3095. doi: 10.1016/j.ultrasmedbio.2015.08.001. [DOI] [PubMed] [Google Scholar]
- 58.Wildner D, Bernatik T, Greis C, Seitz K, Neurath MF, Strobel D. CEUS in hepatocellular carcinoma and intrahepatic cholangiocellular carcinoma in 320 patients - early or late washout matters: a subanalysis of the DEGUM multicenter trial. Ultraschall Med. 2015;36:132–139. doi: 10.1055/s-0034-1399147. [DOI] [PubMed] [Google Scholar]
- 59.Chen LD, Ruan SM, Liang JY, Yang Z, Shen SL, Huang Y, et al. Differentiation of intrahepatic cholangiocarcinoma from hepatocellular carcinoma in high-risk patients: a predictive model using contrast-enhanced ultrasound. World J Gastroenterol. 2018;24:3786–3798. doi: 10.3748/wjg.v24.i33.3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. American College of Radiology (ACR). CEUS LI-RADS® v2017 CORE. ACR web site, < https://www.acr.org/-/media/ACR/Files/RADS/LI-RADS/CEUS-LI-RADS-2017-Core.pdf>. Accessed 28 Jun 2021.
- 61.Terzi E, Iavarone M, Pompili M, Veronese L, Cabibbo G, Fraquelli M, et al. Contrast ultrasound LI-RADS LR-5 identifies hepatocellular carcinoma in cirrhosis in a multicenter restropective study of 1,006 nodules. J Hepatol. 2018;68:485–492. doi: 10.1016/j.jhep.2017.11.007. [DOI] [PubMed] [Google Scholar]
- 62.Li J, Ling W, Chen S, Ma L, Yang L, Lu Q, et al. The interreader agreement and validation of contrast-enhanced ultrasound liver imaging reporting and data system. Eur J Radiol. 2019;120:108685. doi: 10.1016/j.ejrad.2019.108685. [DOI] [PubMed] [Google Scholar]
- 63.Makoyeva A, Kim TK, Jang HJ, Medellin A, Wilson SR. Use of CEUS LI-RADS for the accurate diagnosis of nodules in patients at risk for hepatocellular carcinoma: a validation study. Radiol Imaging Cancer. 2020;2:e190014. doi: 10.1148/rycan.2020190014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zheng W, Li Q, Zou XB, Wang JW, Han F, Li F, et al. Evaluation of contrast-enhanced US LI-RADS version 2017: application on 2020 liver nodules in patients with hepatitis B infection. Radiology. 2020;294:299–307. doi: 10.1148/radiol.2019190878. [DOI] [PubMed] [Google Scholar]
- 65.Li S, Zhou L, Chen R, Chen Y, Niu Z, Qian L, et al. Diagnostic efficacy of contrast-enhanced ultrasound versus MRI liver imaging reporting and data system (LI-RADS) for categorising hepatic observations in patients at risk of hepatocellular carcinoma. Clin Radiol. 2021;76:161.e1–161.e10. doi: 10.1016/j.crad.2020.10.009. [DOI] [PubMed] [Google Scholar]
- 66.Ding J, Long L, Zhang X, Chen C, Zhou H, Zhou Y, et al. Contrast-enhanced ultrasound LI-RADS 2017: comparison with CT/MRI LI-RADS. Eur Radiol. 2021;31:847–854. doi: 10.1007/s00330-020-07159-z. [DOI] [PubMed] [Google Scholar]
- 67.Li W, Li L, Zhuang BW, Ruan SM, Hu HT, Huang Y, et al. Interreader agreement of CEUS LI-RADS among radiologists with different levels of experience. Eur Radiol. 2021;31:6758–6767. doi: 10.1007/s00330-021-07777-1. [DOI] [PubMed] [Google Scholar]
- 68.Ghiuchici AM, Dănilă M, Popescu A, Şirli R, Moga T, Topan M, et al. Contrast-enhanced ultrasound algorithm (ACR CEUS LI-RADSv 2017)- a valuable tool for the noninvasive diagnosis of hepatocellular carcinoma in patients with chronic liver disease. Med Ultrason. 2021;23:383–389. doi: 10.11152/mu-2887. [DOI] [PubMed] [Google Scholar]
- 69.Son JH, Choi SH, Kim SY, Lee SJ, Park SH, Kim KW, et al. Accuracy of contrast-enhanced ultrasound liver imaging reporting and data system: a systematic review and meta-analysis. Hepatol Int. 2020;14:1104–1113. doi: 10.1007/s12072-020-10102-5. [DOI] [PubMed] [Google Scholar]
- 70.Shin J, Lee S, Bae H, Chung YE, Choi JY, Huh YM, et al. Contrast-enhanced ultrasound liver imaging reporting and data system for diagnosing hepatocellular carcinoma: a meta-analysis. Liver Int. 2020;40:2345–2352. doi: 10.1111/liv.14617. [DOI] [PubMed] [Google Scholar]
- 71.Li J, Yang L, Ma L, Lu Q, Luo Y. Diagnostic accuracy of contrast-enhanced ultrasound liver imaging reporting and data system (CEUS LI-RADS) for differentiating between hepatocellular carcinoma and other hepatic malignancies in high-risk patients: a meta-analysis. Ultraschall Med. 2021;42:187–193. doi: 10.1055/a-1309-1568. [DOI] [PubMed] [Google Scholar]
- 72.Maruyama H, Takahashi M, Ishibashi H, Yoshikawa M, Yokosuka O. Contrast-enhanced ultrasound for characterisation of hepatic lesions appearing non-hypervascular on CT in chronic liver diseases. Br J Radiol. 2012;85:351–357. doi: 10.1259/bjr/20440141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sugimoto K, Moriyasu F, Shiraishi J, Saito K, Taira J, Saguchi T, et al. Assessment of arterial hypervascularity of hepatocellular carcinoma: comparison of contrast-enhanced US and gadoxetate disodium-enhanced MR imaging. Eur Radiol. 2012;22:1205–1213. doi: 10.1007/s00330-011-2372-3. [DOI] [PubMed] [Google Scholar]
- 74.Kang HJ, Kim JH, Joo I, Han JK. Additional value of contrast-enhanced ultrasound (CEUS) on arterial phase non-hyperenhancement observations (≥2 cm) of CT/MRI for high-risk patients: focusing on the CT/MRI LI-RADS categories LR-3 and LR-4. Abdom Radiol (NY) 2020;45:55–63. doi: 10.1007/s00261-019-02132-x. [DOI] [PubMed] [Google Scholar]
- 75.Hu J, Bhayana D, Burak KW, Wilson SR. Resolution of indeterminate MRI with CEUS in patients at high risk for hepatocellular carcinoma. Abdom Radiol (NY) 2020;45:123–133. doi: 10.1007/s00261-019-02181-2. [DOI] [PubMed] [Google Scholar]
- 76.Tan Z, Teoh WC, Wong KM, Wansaicheong GK, Sandrasegaran K. Analysis of comparative performance of CEUS and CECT/MR LI-RADS classification: can CEUS dichotomize LI-RADS indeterminate lesions on CT or MRI? Clin Imaging. 2020;62:63–68. doi: 10.1016/j.clinimag.2020.02.002. [DOI] [PubMed] [Google Scholar]
- 77.Kim TK, Choi BI, Han JK, Chung JW, Park JH, Han MC. Nontumorous arterioportal shunt mimicking hypervascular tumor in cirrhotic liver: two-phase spiral CT findings. Radiology. 1998;208:597–603. doi: 10.1148/radiology.208.3.9722834. [DOI] [PubMed] [Google Scholar]
- 78.Yu JS, Kim KW, Jeong MG, Lee JT, Yoo HS. Nontumorous hepatic arterial-portal venous shunts: MR imaging findings. Radiology. 2000;217:750–756. doi: 10.1148/radiology.217.3.r00dc13750. [DOI] [PubMed] [Google Scholar]
- 79.Kang HJ, Lee JM, Yoon JH, Han JK. Role of contrast-enhanced ultrasound as a second-line diagnostic modality in noninvasive diagnostic algorithms for hepatocellular carcinoma. Korean J Radiol. 2021;22:354–365. doi: 10.3348/kjr.2020.0973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Dietrich CF, Averkiou MA, Correas JM, Lassau N, Leen E, Piscaglia F. An EFSUMB introduction into dynamic contrast-enhanced ultrasound (DCE-US) for quantification of tumour perfusion. Ultraschall Med. 2012;33:344–351. doi: 10.1055/s-0032-1313026. [DOI] [PubMed] [Google Scholar]
- 81.Dietrich CF, Nolsøe CP, Barr RG, Berzigotti A, Burns PN, Cantisani V, et al. Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS) in the liver - update 2020 - WFUMB in cooperation with EFSUMB, AFSUMB, AIUM, and FLAUS. Ultraschall Med. 2020;41:562–585. doi: 10.1055/a-1177-0530. [DOI] [PubMed] [Google Scholar]
- 82.Pei XQ, Liu LZ, Xiong YH, Zou RH, Chen MS, Li AH, et al. Quantitative analysis of contrast-enhanced ultrasonography: differentiating focal nodular hyperplasia from hepatocellular carcinoma. Br J Radiol. 2013;86:20120536. doi: 10.1259/bjr.20120536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Yue WW, Wang S, Xu HX, Sun LP, Guo LH, Bo XW, et al. Parametric imaging with contrast-enhanced ultrasound for differentiating hepatocellular carcinoma from metastatic liver cancer. Clin Hemorheol Microcirc. 2016;64:177–188. doi: 10.3233/CH-162060. [DOI] [PubMed] [Google Scholar]
- 84.Lu Q, Zhang XL, Han H, Huang BJ, Ding H, Wang WP. Value of perfusion parameters for differentiating hepatocellular carcinoma and liver metastasis with hypervascularity and a normal hepatic background on contrast-enhanced ultrasound imaging. J Ultrasound Med. 2019;38:2601–2608. doi: 10.1002/jum.14957. [DOI] [PubMed] [Google Scholar]
- 85.Lee JY, Minami Y, Choi BI, Lee WJ, Chou YH, Jeong WK, et al. The AFSUMB consensus statements and recommendations for the clinical practice of contrast-enhanced ultrasound using Sonazoid. J Med Ultrasound. 2020;28:59–82. doi: 10.4103/JMU.JMU_124_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kudo M. Defect reperfusion imaging with Sonazoid®: a breakthrough in hepatocellular carcinoma. Liver Cancer. 2016;5:1–7. doi: 10.1159/000367760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Duisyenbi Z, Numata K, Nihonmatsu H, Fukuda H, Chuma M, Kondo M, et al. Comparison between low mechanical index and high mechanical index contrast modes of contrast-enhanced ultrasonography: evaluation of perfusion defects of hypervascular hepatocellular carcinomas during the postvascular phase. J Ultrasound Med. 2019;38:2329–2338. doi: 10.1002/jum.14926. [DOI] [PubMed] [Google Scholar]
- 88.Goto E, Masuzaki R, Tateishi R, Kondo Y, Imamura J, Goto T, et al. Value of post-vascular phase (Kupffer imaging) by contrast-enhanced ultrasonography using Sonazoid in the detection of hepatocellular carcinoma. J Gastroenterol. 2012;47:477–485. doi: 10.1007/s00535-011-0512-9. [DOI] [PubMed] [Google Scholar]
- 89.Arita J, Hasegawa K, Takahashi M, Hata S, Shindoh J, Sugawara Y, et al. Correlation between contrast-enhanced intraoperative ultrasound using Sonazoid and histologic grade of resected hepatocellular carcinoma. AJR Am J Roentgenol. 2011;196:1314–1321. doi: 10.2214/AJR.10.4310. [DOI] [PubMed] [Google Scholar]
- 90.Numata K, Fukuda H, Miwa H, Ishii T, Moriya S, Kondo M, et al. Contrast-enhanced ultrasonography findings using a perflubutane-based contrast agent in patients with early hepatocellular carcinoma. Eur J Radiol. 2014;83:95–102. doi: 10.1016/j.ejrad.2013.09.025. [DOI] [PubMed] [Google Scholar]
- 91.Kang HJ, Lee JM, Yoon JH, Lee K, Kim H, Han JK. Contrast-enhanced US with sulfur hexafluoride and perfluorobutane for the diagnosis of hepatocellular carcinoma in individuals with high risk. Radiology. 2020;297:108–116. doi: 10.1148/radiol.2020200115. [DOI] [PubMed] [Google Scholar]
- 92.Yang Y, Liu C, Yan J, Liu K. Perfluorobutane contrast-enhanced ultrasonography for the diagnosis of HCC: a systematic review and meta-analysis. Abdom Radiol (NY) 2021;46:4619–4628. doi: 10.1007/s00261-021-03141-5. [DOI] [PubMed] [Google Scholar]
- 93.Sugimoto K, Kakegawa T, Takahashi H, Tomita Y, Abe M, Yoshimasu Y, et al. Usefulness of modified CEUS LI-RADS for the diagnosis of hepatocellular carcinoma using sonazoid. Diagnostics (Basel) 2020;10:828. doi: 10.3390/diagnostics10100828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kim TK, Jang HJ. Emerging evidence of the utility of perfluorobutane-enhanced US as a diagnostic test for hepatocellular carcinoma. Radiology. 2020;297:117–119. doi: 10.1148/radiol.2020202763. [DOI] [PubMed] [Google Scholar]
- 95.Zhang BH, Yang BH, Tang ZY. Randomized controlled trial of screening for hepatocellular carcinoma. J Cancer Res Clin Oncol. 2004;130:417–422. doi: 10.1007/s00432-004-0552-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Yeh YP, Hu TH, Cho PY, Chen HH, Yen AM, Chen SL, et al. Evaluation of abdominal ultrasonography mass screening for hepatocellular carcinoma in Taiwan. Hepatology. 2014;59:1840–1849. doi: 10.1002/hep.26703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Mittal S, Kanwal F, Ying J, Chung R, Sada YH, Temple S, et al. Effectiveness of surveillance for hepatocellular carcinoma in clinical practice: a United States cohort. J Hepatol. 2016;65:1148–1154. doi: 10.1016/j.jhep.2016.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.An JY, Peña MA, Cunha GM, Booker MT, Taouli B, Yokoo T, et al. Abbreviated MRI for hepatocellular carcinoma screening and surveillance. Radiographics. 2020;40:1916–1931. doi: 10.1148/rg.2020200104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Tzartzeva K, Obi J, Rich NE, Parikh ND, Marrero JA, Yopp A, et al. Surveillance imaging and alpha fetoprotein for early detection of hepatocellular carcinoma in patients with cirrhosis: a meta-analysis. Gastroenterology. 2018;154:1706–1718. doi: 10.1053/j.gastro.2018.01.064. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Brunsing RL, Fowler KJ, Yokoo T, Cunha GM, Sirlin CB, Marks RM. Alternative approach of hepatocellular carcinoma surveillance: abbreviated MRI. Hepatoma Res. 2020;6:59. doi: 10.20517/2394-5079.2020.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Marks RM, Ryan A, Heba ER, Tang A, Wolfson TJ, Gamst AC, et al. Diagnostic per-patient accuracy of an abbreviated hepatobiliary phase gadoxetic acid-enhanced MRI for hepatocellular carcinoma surveillance. AJR Am J Roentgenol. 2015;204:527–535. doi: 10.2214/AJR.14.12986. [DOI] [PubMed] [Google Scholar]
- 102.Besa C, Lewis S, Pandharipande PV, Chhatwal J, Kamath A, Cooper N, et al. Hepatocellular carcinoma detection: diagnostic performance of a simulated abbreviated MRI protocol combining diffusion-weighted and T1-weighted imaging at the delayed phase post gadoxetic acid. Abdom Radiol (NY) 2017;42:179–190. doi: 10.1007/s00261-016-0841-5. [DOI] [PubMed] [Google Scholar]
- 103.Chan MV, McDonald SJ, Ong YY, Mastrocostas K, Ho E, Huo YR, et al. HCC screening: assessment of an abbreviated non-contrast MRI protocol. Eur Radiol Exp. 2019;3:49. doi: 10.1186/s41747-019-0126-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Kim JS, Lee JK, Baek SY, Yun HI. Diagnostic performance of a minimized protocol of non-contrast MRI for hepatocellular carcinoma surveillance. Abdom Radiol (NY) 2020;45:211–219. doi: 10.1007/s00261-019-02277-9. [DOI] [PubMed] [Google Scholar]
- 105.Vietti Violi N, Lewis S, Liao J, Hulkower M, Hernandez-Meza G, Smith K, et al. Gadoxetate-enhanced abbreviated MRI is highly accurate for hepatocellular carcinoma screening. Eur Radiol. 2020;30:6003–6013. doi: 10.1007/s00330-020-07014-1. [DOI] [PubMed] [Google Scholar]
- 106.Whang S, Choi MH, Choi JI, Youn SY, Kim DH, Rha SE. Comparison of diagnostic performance of non-contrast MRI and abbreviated MRI using gadoxetic acid in initially diagnosed hepatocellular carcinoma patients: a simulation study of surveillance for hepatocellular carcinomas. Eur Radiol. 2020;30:4150–4163. doi: 10.1007/s00330-020-06754-4. [DOI] [PubMed] [Google Scholar]
- 107.Park HJ, Jang HY, Kim SY, Lee SJ, Won HJ, Byun JH, et al. Non-enhanced magnetic resonance imaging as a surveillance tool for hepatocellular carcinoma: comparison with ultrasound. J Hepatol. 2020;72:718–724. doi: 10.1016/j.jhep.2019.12.001. [DOI] [PubMed] [Google Scholar]
- 108.Khatri G, Pedrosa I, Ananthakrishnan L, de Leon AD, Fetzer DT, Leyendecker J, et al. Abbreviated-protocol screening MRI vs. complete-protocol diagnostic MRI for detection of hepatocellular carcinoma in patients with cirrhosis: an equivalence study using LI-RADS v2018. J Magn Reson Imaging. 2020;51:415–425. doi: 10.1002/jmri.26835. [DOI] [PubMed] [Google Scholar]
- 109.Jalli R, Jafari SH, Sefidbakht S, Kazemi K. Comparison of the accuracy of DWI and ultrasonography in screening hepatocellular carcinoma in patients with chronic liver disease. Iran J Radiol. 2015;12:e12708. doi: 10.5812/iranjradiol.12708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Han S, Choi JI, Park MY, Choi MH, Rha SE, Lee YJ. The diagnostic performance of liver MRI without intravenous contrast for detecting hepatocellular carcinoma: a case-controlled feasibility study. Korean J Radiol. 2018;19:568–577. doi: 10.3348/kjr.2018.19.4.568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Kim DH, Choi SH, Shim JH, Kim SY, Lee SS, Byun JH, et al. Metaanalysis of the accuracy of abbreviated magnetic resonance imaging for hepatocellular carcinoma surveillance: non-contrast versus hepatobiliary phase-abbreviated magnetic resonance imaging. Cancers (Basel) 2021;13:2975. doi: 10.3390/cancers13122975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Gupta P, Soundararajan R, Patel A, Kumar-M P, Sharma V, Kalra N. Abbreviated MRI for hepatocellular carcinoma screening: a systematic review and meta-analysis. J Hepatol. 2021;75:108–119. doi: 10.1016/j.jhep.2021.01.041. [DOI] [PubMed] [Google Scholar]
- 113.Brunsing RL, Chen DH, Schlein A, Wolfson T, Gamst A, Mamidipalli A, et al. Gadoxetate-enhanced abbreviated MRI for hepatocellular carcinoma surveillance: preliminary experience. Radiol Imaging Cancer. 2019;1:e190010. doi: 10.1148/rycan.2019190010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kim HA, Kim KA, Choi JI, Lee JM, Lee CH, Kang TW, et al. Comparison of biannual ultrasonography and annual non-contrast liver magnetic resonance imaging as surveillance tools for hepatocellular carcinoma in patients with liver cirrhosis (MAGNUS-HCC): a study protocol. BMC cancer. 2017;17:877. doi: 10.1186/s12885-017-3819-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.An C, Kim DY, Choi JY, Han KH, Roh YH, Kim MJ. Noncontrast magnetic resonance imaging versus ultrasonography for hepatocellular carcinoma surveillance (MIRACLE-HCC): study protocol for a prospective randomized trial. BMC Cancer. 2018;18:915. doi: 10.1186/s12885-018-4827-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Park JH, Park MS, Lee SJ, Jeong WK, Lee JY, Park MJ, et al. Contrast-enhanced US with perfluorobutane for hepatocellular carcinoma surveillance: a multicenter diagnostic trial (SCAN) Radiology. 2019;292:638–646. doi: 10.1148/radiol.2019190183. [DOI] [PubMed] [Google Scholar]
- 117.Kudo M, Ueshima K, Osaki Y, Hirooka M, Imai Y, Aso K, et al. B-mode ultrasonography versus contrast-enhanced ultrasonography for surveillance of hepatocellular carcinoma: a prospective multicenter randomized controlled trial. Liver Cancer. 2019;8:271–280. doi: 10.1159/000501082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Chartrand G, Cheng PM, Vorontsov E, Drozdzal M, Turcotte S, Pal CJ, et al. Deep learning: a primer for radiologists. Radiographics. 2017;37:2113–2131. doi: 10.1148/rg.2017170077. [DOI] [PubMed] [Google Scholar]
- 119.Park HJ, Park B, Lee SS. Radiomics and deep learning: hepatic applications. Korean J Radiol. 2020;21:387–401. doi: 10.3348/kjr.2019.0752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Castaldo A, De Lucia DR, Pontillo G, Gatti M, Cocozza S, Ugga L, et al. State of the art in artificial intelligence and radiomics in hepatocellular carcinoma. Diagnostics (Basel) 2021;11:1194. doi: 10.3390/diagnostics11071194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Schmauch B, Herent P, Jehanno P, Dehaene O, Saillard C, Aubé C, et al. Diagnosis of focal liver lesions from ultrasound using deep learning. Diagn Interv Imaging. 2019;100:227–233. doi: 10.1016/j.diii.2019.02.009. [DOI] [PubMed] [Google Scholar]
- 122.Yang Q, Wei J, Hao X, Kong D, Yu X, Jiang T, et al. Improving B-mode ultrasound diagnostic performance for focal liver lesions using deep learning: a multicentre study. EBioMedicine. 2020;56:102777. doi: 10.1016/j.ebiom.2020.102777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Yasaka K, Akai H, Abe O, Kiryu S. Deep learning with convolutional neural network for differentiation of liver masses at dynamic contrast-enhanced CT: a preliminary study. Radiology. 2018;286:887–896. doi: 10.1148/radiol.2017170706. [DOI] [PubMed] [Google Scholar]
- 124.Hamm CA, Wang CJ, Savic LJ, Ferrante M, Schobert I, Schlachter T, et al. Deep learning for liver tumor diagnosis part I: development of a convolutional neural network classifier for multi-phasic MRI. Eur Radiol. 2019;29:3338–3347. doi: 10.1007/s00330-019-06205-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Wang M, Fu F, Zheng B, Bai Y, Wu Q, Wu J, et al. Development of an AI system for accurately diagnose hepatocellular carcinoma from computed tomography imaging data. Br J Cancer. 2021;125:1111–1121. doi: 10.1038/s41416-021-01511-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Zhen SH, Cheng M, Tao YB, Wang YF, Juengpanich S, Jiang ZY, et al. Deep learning for accurate diagnosis of liver tumor based on magnetic resonance imaging and clinical data. Front Oncol. 2020;10:680. doi: 10.3389/fonc.2020.00680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Kim J, Min JH, Kim SK, Shin SY, Lee MW. Detection of hepatocellular carcinoma in contrast-enhanced magnetic resonance imaging using deep learning classifier: a multi-center retrospective study. Sci Rep. 2020;10:9458. doi: 10.1038/s41598-020-65875-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Yang CJ, Wang CK, Fang YD, Wang JY, Su FC, Tsai HM, et al. Clinical application of mask region-based convolutional neural network for the automatic detection and segmentation of abnormal liver density based on hepatocellular carcinoma computed tomography datasets. PLoS One. 2021;16:e0255605. doi: 10.1371/journal.pone.0255605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Zheng R, Wang L, Wang C, Yu X, Chen W, Li Y, et al. Feasibility of automatic detection of small hepatocellular carcinoma (≤2 cm) in cirrhotic liver based on pattern matching and deep learning. Phys Med Biol. 2021;66:085014. doi: 10.1088/1361-6560/abf2f8. [DOI] [PubMed] [Google Scholar]
- 130.Wu Y, White GM, Cornelius T, Gowdar I, Ansari MH, Supanich MP, et al. Deep learning LI-RADS grading system based on contrast enhanced multiphase MRI for differentiation between LR-3 and LR-4/LR-5 liver tumors. Ann Transl Med. 2020;8:701. doi: 10.21037/atm.2019.12.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Yamashita R, Mittendorf A, Zhu Z, Fowler KJ, Santillan CS, Sirlin CB, et al. Deep convolutional neural network applied to the liver imaging reporting and data system (LI-RADS) version 2014 category classification: a pilot study. Abdom Radiol (NY) 2020;45:24–35. doi: 10.1007/s00261-019-02306-7. [DOI] [PMC free article] [PubMed] [Google Scholar]