Abstract
Background/Aims
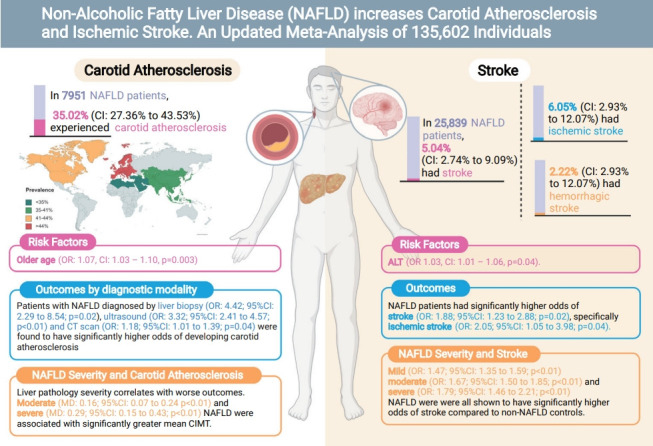
Non-alcoholic fatty liver disease (NAFLD) is associated with the development of cardiovascular disease. While existing studies have examined cardiac remodeling in NAFLD, there has been less emphasis on the development of carotid atherosclerosis and stroke. We sought to conduct a meta-analysis to quantify the prevalence, risk factors, and degree of risk increment of carotid atherosclerosis and stroke in NAFLD.
Methods
Embase and Medline were searched for articles relating to NAFLD, carotid atherosclerosis, and stroke. Proportional data was analysed using a generalized linear mixed model. Pairwise meta-analysis was conducted to obtain odds ratio or weighted mean difference for comparison between patients with and without NAFLD.
Results
From pooled analysis of 30 studies involving 7,951 patients with NAFLD, 35.02% (95% confidence interval [CI], 27.36–43.53%) had carotid atherosclerosis with an odds ratio of 3.20 (95% CI, 2.37–4.32; P<0.0001). Pooled analysis of 25,839 patients with NAFLD found the prevalence of stroke to be 5.04% (95% CI, 2.74–9.09%) with an odds ratio of 1.88 (95% CI, 1.23–2.88; P=0.02) compared to non-NAFLD. The degree of steatosis assessed by ultrasonography in NAFLD was closely associated with risk of carotid atherosclerosis and stroke. Older age significantly increased the risk of developing carotid atherosclerosis, but not stroke in NAFLD.
Conclusions
This meta-analysis shows that a stepwise increment of steatosis of NAFLD can significantly increase the risk of carotid atherosclerosis and stroke development in NAFLD. Patients more than a third sufferred from carotid atherosclerosis and routine assessment of carotid atherosclerosis is quintessential in NAFLD.
Keywords: Atherosclerosis, Stroke, Ischemic stroke, Nonalcoholic fatty liver disease
Graphical Abstract
INTRODUCTION
Nonalcoholic fatty liver disease (NAFLD) is the most common chronic liver disease affecting 22% to 30% of the global population [1,2]. NAFLD is characterized by the evidence of hepatic steatosis, either by imaging or histology, and the absence of secondary causes of hepatic lipid accumulation such as excessive alcohol consumption, long-term use of steatogenic medications, or monogenic hereditary disorders [3]. NAFLD encompasses a wide spectrum of disease ranging from simple steatosis to nonalcoholic steatohepatitis, a more progressive and advanced form of the disease characterized by inflammation, ballooning, and hepatocellular injury [4], which may subsequently progress to liver cirrhosis [5] and liver cancer [6]. The presence of NAFLD can result in a host of complications including the development of cardiovascular disease, extrahepatic or hepatic malignancy [7], and depression [8].
In NAFLD, the presence of chronic energy surplus causes lipo-toxicity, cell death, and inflammation [9], which can lead to the development of atherosclerosis [10] in the coronary, carotid, and peripheral arteries [11]. While current studies have predominantly focused on the development and progression of cardiac-related disease in NAFLD, the potential implications of carotid atherosclerosis are severe and predispose to the development of stroke. Stroke is the third-leading cause of disability and the second-leading cause of death worldwide [12]. Although common modifiable risk factors of stroke such as smoking, diet, and physical inactivity have been studied, there is still a limited understanding of stroke beyond its traditional risk factors [13], especially in the presence of metabolic dysfunction. Recent studies have found NAFLD to be an independent risk factor of stroke [14].
Current meta-analyses have focused on the association of NAFLD with coronary atherosclerosis and cardiovascular diseases [15-18]. However, a systematic analysis of the prevalence, risk factors, degree of steatosis in NAFLD and carotid atherosclerosis or stroke remains limited. Hence, this paper seeks to conduct an updated analysis of the associations of NAFLD with mean carotid intima-media thickness (CIMT), carotid atherosclerosis, stroke risk, and factors associated with these developments, with further subgroup analyses based on NAFLD severity and diagnostic modalities.
MATERIALS AND METHODS
Search strategy and inclusion criteria
This review adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses for its synthesis. Two electronic databases, MEDLINE, and Embase, were used to search all available records till 21st October 2021. The search strategy used search terms including ‘nonalcoholic fatty liver disease’, ‘hemorrhagic stroke’, ‘ischemic stroke’, ‘CIMT’, and other related terms in titles and abstracts. The full search strategy is included in Supplementary Material 1. References were imported into Endnote X9 for duplicate removal. References of the included articles and previous meta-analysis were also manually screened to ensure a comprehensive search.
Eligibility and selection criteria
Four authors (KEC, JQ, ASPT, and JX) independently screened abstracts and conducted full-text reviews to check the eligibility for inclusion, with disputes being resolved by obtaining the consensus of a fifth independent author (CHN). Only original articles were included, and reviews, commentaries, and editorials were excluded. Studies that were written or translated into the English language were included. NAFLD was defined as evidence of hepatic steatosis, either by imaging or histology and lack of secondary causes of hepatic fat accumulation such as significant alcohol consumption, long-term use of steatogenic medication or monogenic hereditary disorders [3]. Diagnosis of NAFLD was determined either from invasive methods, such as liver biopsy, or non-invasive methods including ultrasound and computed tomography (CT) scan. Blood-based diagnosis including NAFLD fibrosis score (NFS) was excluded from the analysis. Studies were included if they fulfilled the following criteria: one of the following outcomes 1) mean CIMT; 2) increased in CIMT, stenosis or plaques; and 3) stroke. Mean CIMT was defined as the average width of the intima-media layer of the carotid artery assessed by Duplex ultrasonography (DUS) [19]. Carotid arteriosclerosis was defined as the presence of carotid plaques/stenosis or an increase in CIMT. Stroke was defined as the presence of either ischemic and hemorrhagic stroke. For multiple studies inferring results from the same databases, duplicates were removed and only the most updated studies were included for analysis.
Data extraction and outcomes
NAFLD severity was graded according to ultrasound findings to maintain homogeneity. Mild NAFLD was defined as a slight diffuse increase in the hepatic parenchyma echogenicity with normal visualisation of the diaphragm and portal veins. Moderate NAFLD was defined as moderate diffuse increase in hepatic echogenicity, with slight impaired visualisation of the diaphragm and portal veins. Severe NAFLD was defined as a marked increase in hepatic echogenicity with poor or no visualisation of the diaphragm and portal veins [20,21]. Two pair of authors (KEC and ASPT; JQ and JL) independently extracted data including but not limited to 1) study characteristics such as: author, year, country, study design; 2) patient characteristics such as sample size, age, male gender, diagnostic criteria, severity of NAFLD, body mass index, presence of metabolic conditions including dyslipidemia and hypertension; and 3) clinical outcomes. Transformation of values was carried out using pre-existing formulae, in which mean and standard deviations were estimated from median and range using the widely adopted formula by Wan et al. [22] Blinded checking of the data by the authors was conducted to ensure accuracy of the data extracted and discrepancies in data were resolved through consensus.
Statistical analysis
All analyses were conducted in R studio (version 5.0.0; The R Foundation, Indianapolis, IN, USA). A P-value ≤0.05 was considered as the threshold for statistical significance. Statistical heterogeneity was assessed via I2 and Cochran’s Q test values, where I2 values of 25%, 50% and 75% represented low, moderate and high degrees of heterogeneity, respectively [23,24]. A random effect model was used in all analyses regardless of heterogeneity measures as evidence has demonstrated more robust effect estimates with random effect compared to fixed-effect models [25,26]. An analysis of proportions was pooled using a generalized linear mixed model with Clopper-Pearson intervals [27,28]. To assess risk factors, a generalized mix model with a logit link and inverse variance weightage were used to derived the odds ratio (OR) [29]. Bivariate analysis of dichotomous variables was analysed in Paul Mantel ORs with and mean difference (MD) with inverse variance for continuous variables. A subgroup analysis was performed based on NAFLD diagnostic modality (ultrasound, CT, biopsy) and geographical location in the analysis of CIMT. Where possible, a sensitivity analysis was also performed on severity of NAFLD (i.e., mild, moderate, severe) based on ultrasound evaluation. Publication bias was examined based on asymmetry of the funnel plots (Supplementary Fig. 1) where sufficient studies were present (n>10) with Begg regression.
Quality assessment
Quality assessment of included articles was done with the Joanna Briggs Institute (JBI) critical appraisal tool (JBI Collaboration, Adelaide, Australia) [30]. The JBI assessment rates the quality of cohort studies on the premises of appropriateness of sample frame, sampling method, adequacy of sample size, data analysis, methods for identification and measurement of relevant condition, statistical analysis, and response rate adequacy.
RESULTS
Summary of included articles
The initial search from MEDLINE and Embase yielded a total of 1,095 articles. After the removal of 327 articles duplicated during the title abstract sieve, 768 articles were remained for abstract screening and a final total of 64 studies conducted between 1998 to 2019 were included in the meta-analysis (Fig. 1). The studies included were conducted in various countries including Algeria [31], China [32-39], Croatia [40], Egypt [41,42], Greece [43,44], India [45-49], Iran [50-57], Italy [58-66], Japan [67,68], Malaysia [69,70], Romania [71], Serbia [72], South Korea [73-78], Spain [79,80], Taiwan [81], Turkey [82-92], USA [93,94]. Additionally, one study [95] was a multicentre study based in Egypt [43]. A total of 135,602 patients were included in our analysis with 47,322 patients with NAFLD and 88,280 non-NAFLD controls. NAFLD defined by liver biopsy [44,82,84,86,87,90,92] was found in seven studies, and by non-invasive methods, including ultrasonography [31-43,45-81,83,85,86,88,89,91,93] in 57 studies and CT scan [94] in one study. All studies were assessed to have a high (n=46) or moderate (n=18) quality based on the JBI Critical Appraisal Checklist assessment tool (Supplementary Table 1). There was no evidence of publication bias (Fig. 2) with Begg regression (P=0.787).
Figure 1.
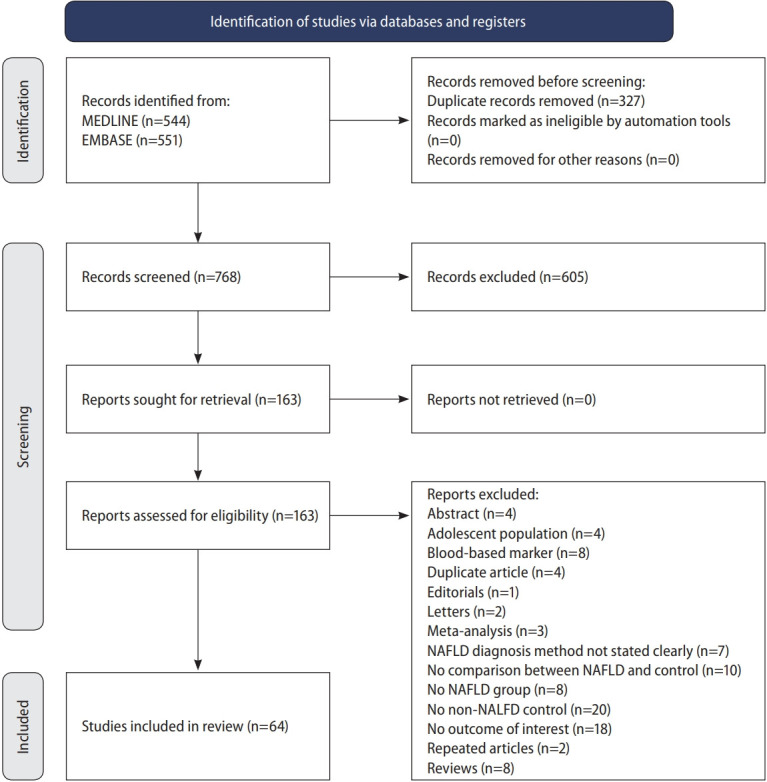
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow chart.
Figure 2.
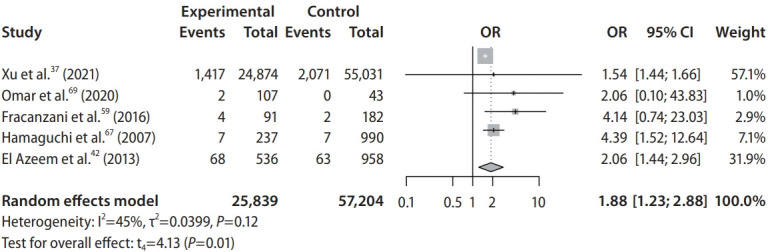
Forest plot on the odds of stroke in nonalcoholic fatty liver disease. OR, odds ratio; CI, confidence interval.
Carotid atherosclerosis
Prevalence and risk factors of carotid atherosclerosis
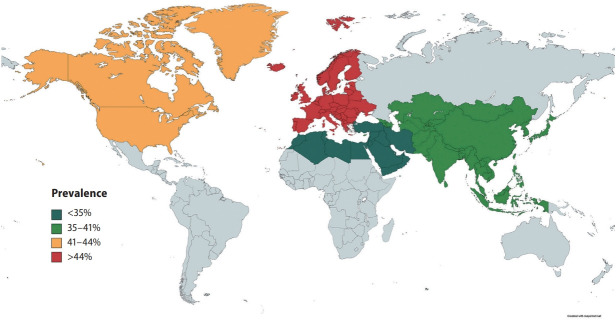
In pooled analysis of 7,951 patients with NAFLD, the prevalence of carotid atherosclerosis in NAFLD was found to be 35.02% (95% confidence interval [CI], 27.36–43.53%). When a subgroup analysis by geographical regions was conducted, the prevalence of carotid atherosclerosis in NAFLD was found to be the highest in Europe (44.72%; 95% CI, 31.02–59.28%; Fig. 3), followed by North America (41.02%; 95% CI, 37.50–44.63%), Asia (35.89%; 95% CI, 24.61–48.98%), and the lowest in the Middle East (19.21%; 95% CI, 12.58–28.21%). Table 1 summarizes the risk factor of carotid atherosclerosis in NAFLD. The presence of older age (OR, 1.07; 95% CI, 1.03–1.10; P=0.003) increases the risk of carotid atherosclerosis in NAFLD.
Figure 3.
Prevalence of carotid atherosclerosis by geographical region.
Table 1.
Risk factors of carotid atherosclerosis and stroke in NAFLD
| Carotid atherosclerosis |
Stroke |
|||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P-value | OR | 95% CI | P-value | |
| Age | 1.07 | 1.03 to 1.10 | 0.003* | 0.94 | 0.82 to 1.09 | 0.42 |
| Diabetes | 0.93 | 0.68 to 1.27 | 0.68 | 1.00 | 0.77 to 1.29 | 0.97 |
| Body mass index | 0.94 | 0.82 to 1.08 | 0.47 | 1.13 | 0.93 to 1.37 | 0.24 |
| Systolic blood pressure | 1.00 | 0.97 to 1.03 | 0.96 | 1.00 | 0.88 to 1.15 | 0.95 |
| Diastolic blood pressure | 1.03 | 0.96 to 1.10 | 0.47 | 1.30 | 0.72 to 2.35 | 0.32 |
| Alanine aminotransferase | 1.01 | 0.99 to 1.02 | 0.15 | 1.03 | 1.01 to 1.06 | 0.04* |
| Aspartate aminotransferase | 1.03 | 0.99 to 1.07 | 0.22 | - | - | - |
| HbA1c | 1.06 | 0.80 to 1.39 | 0.70 | - | - | - |
| Dyslipidemia | 1.01 | 0.74 to 1.39 | 0.93 | - | - | - |
NAFLD, nonalcoholic fatty liver disease; OR, odds ratio; CI, confidence interval; HbA1c, hemoglobin A1c.
P-value ≤0.05 denotes statistical significance.
Comparative outcomes
A summary of comparative results can be found in Table 2. When compared to non-NAFLD controls, patients with NAFLD were shown to have significantly higher risk of carotid atherosclerosis (OR, 3.20; 95% CI, 2.37–4.32; P<0.0001). Subgroup analysis by diagnostic modality similarly demonstrated that patients with NAFLD diagnosed by liver biopsy (OR, 4.42; 95% CI, 2.29–8.54; P=0.02), ultrasound (OR, 3.32; 95% CI, 2.41–4.57; P<0.01), and CT scan (OR, 1.18; 95% CI, 1.01–1.39; P=0.04) had significantly higher risk of developing carotid atherosclerosis as compared to non-NAFLD controls. Patients with NAFLD were also found to have a significantly greater mean CIMT than those without NAFLD (MD, 0.12; 95% CI, 0.08–0.17; P<0.0001). Subgroup analysis of mean CIMT based on the severity of NAFLD revealed that liver pathology severity correlates with the worse outcomes. Patients suffering from moderate NAFLD (MD, 0.16; 95% CI, 0.07–0.24; P<0.01) and severe NAFLD (MD, 0.29; 95% CI, 0.15–0.43; P<0.01) had significant increase in mean CIMT but not in mild NAFLD (MD, -0.04; 95% CI, -0.28 to 0.20; P=0.76).
Table 2.
Comparative outcomes between NAFLD and non-NAFLD
| Total | Effect size | 95% CI | P-value | I2 (%) | Cochran Q | |
|---|---|---|---|---|---|---|
| Mean CIMT | 46,686 | MD: 0.12 | 0.08 to 0.17 | <0.0001* | 98.60 | 0.00 |
| Carotid atherosclerosis | 23,793 | OR: 3.20 | 2.37 to 4.32 | <0.0001* | 87.80 | <0.01 |
| Overall stroke | 83,043 | OR: 1.88 | 1.23 to 2.88 | 0.02* | 45.30 | 0.12 |
| Hemorrhagic stroke | 1,968 | OR: 1.85 | 0.20 to 17.40 | 0.18 | 0.00 | 0.54 |
| Ischemic stroke | 82,146 | OR: 2.05 | 1.05 to 3.98 | 0.04* | 57.30 | 0.07 |
NAFLD, nonalcoholic fatty liver disease; CI, confidence interval; CIMT, carotid intima-media thickness; MD, mean difference; OR, odds ratio.
P-value ≤0.05 denotes statistical significance.
Stroke
Prevalence and risk factors of stroke
In pooled analysis of 25,839 individuals with NAFLD, the incidence of stroke in NAFLD was found to be 5.04% (95% CI, 2.74–9.09%). Specifically, the incidence of ischemic stroke in NAFLD was 6.05% (95% CI, 2.93–12.07%) while the incidence of hemorrhagic stroke was found to be 2.22% (95% CI, 0.22–18.77%). In NAFLD, there was no significant factor affecting the presence of stroke aside from an increase level of alanine aminotransferase (ALT) (OR, 1.03; 95% CI, 1.01–1.06; P=0.04).
Comparative outcomes
Patients with NAFLD were shown to have significantly higher risk of developing stroke (OR, 1.88; 95% CI, 1.23–2.88; P=0.02; Fig. 2, Table 2) when compared to non-NAFLD controls. Specifically, patients with NAFLD were found to have significantly higher risk of developing ischemic stroke (OR, 2.05; 95% CI, 1.05–3.98; P=0.04) when compared to non-NAFLD controls. However, comparisons between NAFLD and non-NAFLD controls found that there was no significant difference in the risk of developing hemorrhagic stroke (OR, 1.85; 95% CI, 0.20–17.40; P=0.18). Subgroup analysis classified by the severity of NAFLD found that patients suffering from mild (OR, 1.47; 95% CI, 1.35–1.59; P<0.01), moderate (OR, 1.67; 95% CI, 1.50–1.85; P<0.01), and severe (OR, 1.79; 95% CI, 1.46–2.21; P<0.01). NAFLD were all shown to have significantly higher risk of developing stroke when compared to non-NAFLD controls.
DISCUSSION
The presence of NAFLD has been associated with an increase in atherogenic dyslipidemia [96,97] leading to the development of cardiovascular complications such as myocardial infarctions [98] and cerebrovascular accident [7]. While previous studies have demonstrated the association between NAFLD, carotid atherosclerosis [81] and increased stroke risks [37], the current findings further expand on the published literature by providing a contemporaneous analysis on the prevalence of carotid atherosclerosis and stroke in NAFLD, risks factors, and the influence of NAFLD severity and diagnostic modality. Significantly, the degree of steatosis in NAFLD can influence the progression of CIMT and stroke, with severe steatosis resulting in the highest odds of events.
In our meta-analysis, the prevalence of carotid atherosclerosis in NAFLD was found to be 35.02% (95% CI, 27.36– 43.53%) and stroke was 5.04% (95% CI, 2.74–9.09%). Subgroup analysis based on geographical regions found the prevalence of carotid atherosclerosis in NAFLD to be highest in the West. While the geographical regions are not a representation of ethnicity, the prevalence of CIMT have been found to be higher in the Caucasian population [99]. In the analysis of risk factors, the presence of hyperlipidemia and diabetes did not significantly increase the risk of stroke or carotid atherosclerosis in NAFLD. Only older age increased the risk of carotid atherosclerosis while ALT increased the risk of stroke in NAFLD. These results, however, should be interpreted with caution as these findings do not discount the possibility that hyperlipidemia and diabetes may have not been significant due to insufficient statistical power arising from the limited sample size in the risk factor analysis. However, the presence of NAFLD could potentially increase the risk of stroke and CIMT independently with more severe steatosis significantly increasing the rate of events.
While the presence of carotid atherosclerosis does not necessarily translate into an event of ischemic stroke, the presence of carotid atherosclerosis increases the risk of ischemic stroke by 20% [100]. The presence of carotid plaques has also been associated with cerebral atrophy and reduced cognitive ability [101]. In turn, while more than a third of patients with NAFLD sufferred from carotid atherosclerosis, only 5.04% (95% CI, 2.74–9.09%) of patients with NAFLD suffered from a stroke with twice the risk (OR, 1.88; 95% CI, 1.23–2.88; P=0.02) compared to those without NAFLD. Specifically, the presence of NAFLD was found to result in significantly higher risk of developing ischemic stroke (OR, 2.05; 95% CI, 1.05– 3.98; P=0.04) but not in hemorrhagic stroke (OR, 1.85; 95% CI, 0.20–17.40; P=0.18). While the incidence of stroke in NAFLD is rather minute, the presence of NAFLD resulted in twice the risk of stroke and the implications of which can be devastating [102]. Additionally, it is important that we do not undermine the presence of subclinical carotid atherosclerosis, evidently more prevalent in NAFLD as it represents prime therapeutic targets to prevent morbidity and mortality associated with clinically evident disease (i.e., stroke).
Prevailing guidelines by the American Association for the Study of Liver Diseases (AASLD) [103] and the European Association for the Study of the Liver (EASL) [104] have highlighted the importance of cardiovascular risk evaluation in NAFLD. However, the use of CIMT for NAFLD has yet to be endorsed or routinely recommended for NAFLD. Yet, the DUS is a safe, easy, and cost-effective screening investigative tool that can be routinely employed in the clinic [105,106], and has a sensitivity and specificity of 90% and 94% for carotid artherosclerosis [107]. Additionally, the DUS can double as a screening modality for coronary artery disease (CAD) with a respective sensitivity and specificity of 78% and 75% for CAD [108]. CAD is a known complication of NAFLD, and recent estimates suggest the prevalence of CAD to be 38.7% and 55.4%, respectively [10]. With the strong correlation between coronary and carotid atherosclerosis with NAFLD, future studies should assess the cost effectiveness and viability for routine DUS evaluation for NAFLD.
Strengths and limitations
This study provides an up-to-date comprehensive assessment of the association between NAFLD, carotid atherosclerosis and increased stroke risk, including the prevalence, risk factors, and severity of steatosis. However, there are several limitations. Although liver biopsy has higher sensitivity and specificity in the diagnosis of NAFLD, majority of studies utilized non-invasive, imaging-based investigations rather than biopsy to diagnose NAFLD. In addition, while modalities such as CT or Fibroscan may be more accurate in grading NAFLD severity, grading of NAFLD severity was limited to ultrasonographic findings to maintain homogeneity with majority of studies utilizing ultrasonography (89.1%) and is similar to our previous meta-analysis [109]. We were also unable to assess the effects of stage of fibrosis on CIMT or stroke due to lack of granularity in the reported data. Lastly, the included studies were largely retrospective and are subjected to inherent limitations of the study design such as selection bias.
Conclusions
Patients with NAFLD were found to be associated with increased carotid atherosclerosis and stroke prevalence. While the prevalence of stroke in NAFLD may be low, the severe consequences highlight the importance for CIMT evaluation in NAFLD. Routine screening for carotid atherosclerosis, guided by the severity of hepatic steatosis, among patients with NAFLD might aid in the reduction of stroke.
Acknowledgments
All authors have made substantial contributions to all of the following: (1) the conception and design of the study, or acquisition of data, or analysis and interpretation of data, (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted. No writing assistance was obtained in the preparation of the manuscript. The manuscript, including related data, figures and tables has not been previously published and that the manuscript is not under consideration elsewhere. This research meets the ethical guidelines, including adherence to the legal requirements of the study country.
Abbreviations
- AASLD
the American Association for the Study of Liver Diseases
- ALT
alanine aminotransferase
- CAD
coronary artery disease
- CI
confidence interval
- CIMT
carotid intima-media thickness
- CT
computed tomography
- DUS
Duplex ultrasonography
- EASL
the European Association for the Study of the Liver
- JBI
Joanna Briggs Institute
- MD
mean difference
- NAFLD
non-alcoholic fatty liver disease
- NFS
NAFLD fibrosis score
- OR
odds ratio
Study Highlights
• Out of 7,951 NAFLD patients, 35.02% had carotid atherosclerosis with an OR of 3.20.
• The prevalence of stroke in NAFLD patients was 5.04% with an OR of 1.88.
• The routine assessment of carotid atherosclerosis is quintessential in NAFLD.
Footnotes
Authors’ contributions
Conceptualization: Mark Muthiah, Arun J Sanyal, Cheng Han Ng
Data curation: Ansel Shao Pin Tang, Kai En Chan, Jingxuan Quek, Cheng Han Ng
Formal analysis: Ansel Shao Pin Tang, Kai En Chan, Jingxuan Quek, Jieling Xiao, Phoebe Tay
Supervision: Margaret Teng, Keng Siang Lee, May Zin Myint, Benjamin Tan, Vijay K Sharma, Darren Jun Hao Tan, Wen Hui Lim, Daniel Huang, Nicholas WS Chew, Mohammad Shadab Siddiqui, Mark Muthiah, Arun J Sanyal, Cheng Han Ng
Validation: Ansel Shao Pin Tang, Kai En Chan, Jingxuan Quek, Jieling Xiao, Phoebe Tay, Margaret Teng, Keng Siang Lee, May Zin Myint, Benjamin Tan, Vijay K Sharma, Darren Jun Hao Tan, Wen Hui Lim, Daniel Huang, Apichat Kaewdech, Nicholas WS Chew, Mohammad Shadab Siddiqui, Mark Muthiah, Arun J Sanyal, Cheng Han Ng
Writing, original draft: Ansel Shao Pin Tang, Kai En Chan, Jingxuan Quek, Cheng Han Ng
Writing, review, and editing: Ansel Shao Pin Tang, Kai En Chan, Jingxuan Quek, Jieling Xiao, Phoebe Tay, Margaret Teng, Keng Siang Lee, Snow Yunni Lin, May Zin Myint, Benjamin Tan, Vijay K Sharma, Darren Jun Hao Tan, Wen Hui Lim, Daniel Huang, Apichat Kaewdech, Nicholas WS Chew, Mohammad Shadab Siddiqui, Mark Muthiah, Arun J Sanyal, Cheng Han Ng
All authors have read and approved the final version of the manuscript for submission.
Conflicts of Interest
AJS is President of Sanyal Biotechnology and has stock options in Genfit, Akarna, Tiziana, Indalo, Durect and Galmed. He has served as a consultant to Astra Zeneca, Nitto Denko, Enyo, Ardelyx, Conatus, Nimbus, Amarin, Salix, Tobira, Takeda, Jannsen, Gilead, Terns, Birdrock, Merck, Valeant, Boehringer-Ingelheim, Lilly, Hemoshear, Zafgen, Novartis, Novo Nordisk, Pfizer, Exhalenz and Genfit. He has been an unpaid consultant to Intercept, Echosens, Immuron, Galectin, Fractyl, Syntlogic, Affimune, Chemomab, Zydus, Nordic Bioscience, Albireo, Prosciento, Surrozen and Bristol Myers Squibb. His institution has received grant support from Gilead, Salix, Tobira, Bristol Myers, Shire, Intercept, Merck, Astra Zeneca, Malinckrodt, Cumberland and Norvatis. He receives royalties from Elsevier and UptoDate. MN has been on the advisory board for 89BIO, Gilead, Intercept, Pfizer, Novo Nordisk, Blade, EchoSens, Fractyl, Terns, Siemens and Roche diagnostic; MN has received research support from Allergan, BMS, Gilead, Galmed, Galectin, Genfit, Conatus, Enanta, Madrigal, Novartis, Pfizer, Shire, Viking and Zydus; MN is a minor shareholder or has stocks in Anaetos, Rivus Pharma and Viking.
All other authors do not have any conflict of interest to declare.
SUPPLEMENTAL MATERIAL
Supplementary material is available at Clinical and Molecular Hepatology website (http://www.e-cmh.org).
Search strategy
Summary of included articles
Funnel plots of publication bias.
REFERENCES
- 1.Lim GEH, Tang A, Ng CH, Chin YH, Lim WH, Tan DJH, et al. An observational data meta-analysis on the differences in prevalence and risk factors between MAFLD vs NAFLD. Clin Gastroenterol Hepatol. 2021 Dec 4; doi: 10.1016/j.cgh.2021.11.038. doi: 10.1016/j.cgh.2021.11.038. [DOI] [PubMed] [Google Scholar]
- 2.Huang DQ, El-Serag HB, Loomba R. Global epidemiology of NAFLD-related HCC: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2021;18:223–238. doi: 10.1038/s41575-020-00381-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67:328–357. doi: 10.1002/hep.29367. [DOI] [PubMed] [Google Scholar]
- 4.Wong C, Yaow CYL, Ng CH, Chin YH, Low YF, Lim AYL, et al. Sodium-glucose co-transporter 2 inhibitors for non-alcoholic fatty liver disease in Asian patients with type 2 diabetes: a meta-analysis. Front Endocrinol (Lausanne) 2021;11:609135. doi: 10.3389/fendo.2020.609135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li B, Zhang C, Zhan YT. Nonalcoholic fatty liver disease cirrhosis: a review of its epidemiology, risk factors, clinical presentation, diagnosis, management, and prognosis. Can J Gastroenterol Hepatol. 2018;2018:2784537. doi: 10.1155/2018/2784537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Michelotti GA, Machado MV, Diehl AM. NAFLD, NASH and liver cancer. Nat Rev Gastroenterol Hepatol. 2013;10:656–665. doi: 10.1038/nrgastro.2013.183. [DOI] [PubMed] [Google Scholar]
- 7.Muthiah MD, Cheng Han N, Sanyal AJ. A clinical overview of non-alcoholic fatty liver disease: a guide to diagnosis, the clinical features, and complications-What the non-specialist needs to know. Diabetes Obes Metab. 2022;24 Suppl 2:3–14. doi: 10.1111/dom.14521. [DOI] [PubMed] [Google Scholar]
- 8.Xiao J, Lim LKE, Ng CH, Tan DJH, Lim WH, Ho CSH, et al. Is fatty liver associated with depression? A meta-analysis and systematic review on the prevalence, risk factors, and outcomes of depression and non-alcoholic fatty liver disease. Front Med (Lausanne) 2021;8:691696. doi: 10.3389/fmed.2021.691696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Muthiah MD, Cheng Han N, Sanyal AJ. A clinical overview of non-alcoholic fatty liver disease: a guide to diagnosis, the clinical features, and complications-what the non-specialist needs to know. Diabetes Obes Metab. 2022;24 Suppl 2:3–14. doi: 10.1111/dom.14521. [DOI] [PubMed] [Google Scholar]
- 10.Toh JZK, Pan XH, Tay PWL, Ng CH, Yong JN, Xiao J, et al. A meta-analysis on the global prevalence, risk factors and screening of coronary heart disease in nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2021 Sep 21; doi: 10.1016/j.cgh.2021.09.021. doi: 10.1016/j.cgh.2021.09.021. [DOI] [PubMed] [Google Scholar]
- 11.Zou Y, Li X, Wang C, Wang J, Wang F, Ma L, et al. Association between non-alcoholic fatty liver disease and peripheral artery disease in patients with type 2 diabetes. Intern Med J. 2017;47:1147–1153. doi: 10.1111/imj.13549. [DOI] [PubMed] [Google Scholar]
- 12.GBD 2017 DALYs and HALE Collaborators Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1859–1922. doi: 10.1016/S0140-6736(18)32335-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hopewell JC, Clarke R. Emerging risk factors for stroke: what have we learned from mendelian randomization studies? Stroke. 2016;47:1673–1678. doi: 10.1161/STROKEAHA.115.010646. [DOI] [PubMed] [Google Scholar]
- 14.Hu J, Xu Y, He Z, Zhang H, Lian X, Zhu T, et al. Increased risk of cerebrovascular accident related to non-alcoholic fatty liver disease: a meta-analysis. Oncotarget. 2017;9:2752–2760. doi: 10.18632/oncotarget.22755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ampuero J, Gallego-Durán R, Romero-Gómez M. Association of NAFLD with subclinical atherosclerosis and coronary-artery disease: meta-analysis. Rev Esp Enferm Dig. 2015;107:10–16. [PubMed] [Google Scholar]
- 16.Zhou YY, Zhou XD, Wu SJ, Fan DH, Van Poucke S, Chen YP, et al. Nonalcoholic fatty liver disease contributes to subclinical atherosclerosis: a systematic review and meta-analysis. Hepatol Commun. 2018;2:376–392. doi: 10.1002/hep4.1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Veracruz N, Hameed B, Saab S, Wong RJ. The association between nonalcoholic fatty liver disease and risk of cardiovascular disease, stroke, and extrahepatic cancers. J Clin Exp Hepatol. 2021;11:45–81. doi: 10.1016/j.jceh.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Madan SA, John F, Pyrsopoulos N, Pitchumoni CS. Nonalcoholic fatty liver disease and carotid artery atherosclerosis in children and adults: a meta-analysis. Eur J Gastroenterol Hepatol. 2015;27:1237–1248. doi: 10.1097/MEG.0000000000000429. [DOI] [PubMed] [Google Scholar]
- 19.Heiss G, Sharrett AR, Barnes R, Chambless LE, Szklo M, Alzola C. Carotid atherosclerosis measured by B-mode ultrasound in populations: associations with cardiovascular risk factors in the ARIC study. Am J Epidemiol. 1991;134:250–256. doi: 10.1093/oxfordjournals.aje.a116078. [DOI] [PubMed] [Google Scholar]
- 20.Al Rifai M, Silverman MG, Nasir K, Budoff MJ, Blankstein R, Szklo M, et al. The association of nonalcoholic fatty liver disease, obesity, and metabolic syndrome, with systemic inflammation and subclinical atherosclerosis: the multi-ethnic study of atherosclerosis (MESA) Atherosclerosis. 2015;239:629–633. doi: 10.1016/j.atherosclerosis.2015.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Idilman IS, Akata D, Hazirolan T, Doganay Erdogan B, Aytemir K, Karcaaltincaba M. Nonalcoholic fatty liver disease is associated with significant coronary artery disease in type 2 diabetic patients: a computed tomography angiography study 2. J Diabetes. 2015;7:279–286. doi: 10.1111/1753-0407.12172. [DOI] [PubMed] [Google Scholar]
- 22.Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/ or interquartile range. BMC Med Res Methodol. 2014;14:135. doi: 10.1186/1471-2288-14-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 24.Fletcher J. What is heterogeneity and is it important? BMJ. 2007;334:94–96. doi: 10.1136/bmj.39057.406644.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bell A, Fairbrother M, Jones K. Fixed and random effects models: making an informed choice. Qual Quant. 2019;53:1051–1074. [Google Scholar]
- 26.Tufanaru C, Munn Z, Stephenson M, Aromataris E. Fixed or random effects meta-analysis? Common methodological issues in systematic reviews of effectiveness. Int J Evid Based Healthc. 2015;13:196–207. doi: 10.1097/XEB.0000000000000065. [DOI] [PubMed] [Google Scholar]
- 27.Clopper CJ, Pearson ES. The use of confidence or fiducial limits illustrated in the case of the binomial. Biometrika. 1934;26:404–413. [Google Scholar]
- 28.Schwarzer G, Chemaitelly H, Abu-Raddad LJ, Rücker G. Seriously misleading results using inverse of Freeman-Tukey double arcsine transformation in meta-analysis of single proportions. Res Synth Methods. 2019;10:476–483. doi: 10.1002/jrsm.1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ng CH, Tan DJH, Lim XC, Yong JN, Syn N, Soon GST, et al. A diagnostic test meta-analysis evaluating imaging-based and blood biomarker-based assessment tools for fibrosis after liver transplantation. Liver Transpl. 2022;28:659–669. doi: 10.1002/lt.26345. [DOI] [PubMed] [Google Scholar]
- 30.Munn Z, Moola S, Riitano D, Lisy K. The development of a critical appraisal tool for use in systematic reviews addressing questions of prevalence. Int J Health Policy Manag. 2014;3:123–128. doi: 10.15171/ijhpm.2014.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Taharboucht S, Guermaz R, Brouri M, Chibane A. Subclinical atherosclerosis and arterial stiffness in nonalcoholic fatty liver disease: a case-control study in Algerian population. J Med Vasc. 2021;46:129–138. doi: 10.1016/j.jdmv.2021.03.008. [DOI] [PubMed] [Google Scholar]
- 32.Guo K, Zhang L, Lu J, Yu H, Wu M, Bao Y, et al. Non-alcoholic fatty liver disease is associated with late but not early atherosclerotic lesions in Chinese inpatients with type 2 diabetes. J Diabetes Complications. 2017;31:80–85. doi: 10.1016/j.jdiacomp.2016.09.008. [DOI] [PubMed] [Google Scholar]
- 33.Huang Y, Bi Y, Xu M, Ma Z, Xu Y, Wang T, et al. Nonalcoholic fatty liver disease is associated with atherosclerosis in middle-aged and elderly Chinese. Arterioscler Thromb Vasc Biol. 2012;32:2321–2326. doi: 10.1161/ATVBAHA.112.252957. [DOI] [PubMed] [Google Scholar]
- 34.Li X, Shi H, Wang Z, Chang L, Zhang M, Dong X. Arterial stiffness is increased in nondiabetic, nonhypertensive postmenopausal women with nonalcoholic fatty liver disease. J Hypertens. 2017;35:1226–1234. doi: 10.1097/HJH.0000000000001285. [DOI] [PubMed] [Google Scholar]
- 35.Tu S, Zhao R, Fang H, Wang L, Shao A, Sheng J. Association between non-alcoholic fatty liver disease and intracerebral hemorrhage. Cell Transplant. 2019;28:1033–1038. doi: 10.1177/0963689719840025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang B, Zhao Z, Liu S, Wang S, Chen Y, Xu Y, et al. Impact of diabetes on subclinical atherosclerosis and major cardiovascular events in individuals with and without non-alcoholic fatty liver disease. Diabetes Res Clin Pract. 2021;177:108873. doi: 10.1016/j.diabres.2021.108873. [DOI] [PubMed] [Google Scholar]
- 37.Xu J, Dai L, Zhang Y, Wang A, Li H, Wang Y, et al. Severity of nonalcoholic fatty liver disease and risk of future ischemic stroke events. Stroke. 2021;52:103–110. doi: 10.1161/STROKEAHA.120.030433. [DOI] [PubMed] [Google Scholar]
- 38.Zhang L, Guo K, Lu J, Zhao F, Yu H, Han J, et al. Nonalcoholic fatty liver disease is associated with increased carotid intima-media thickness in type 1 diabetic patients. Sci Rep. 2016;6:26805. doi: 10.1038/srep26805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zheng J, Zhou Y, Zhang K, Qi Y, An S, Wang S, et al. Association between nonalcoholic fatty liver disease and subclinical atherosclerosis: a cross-sectional study on population over 40 years old. BMC Cardiovasc Disord. 2018;18:147. doi: 10.1186/s12872-018-0877-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mikolasevic I, Racki S, Zaputovic L, Lukenda V, Sladoje-Martinovic B, Orlic L. Nonalcoholic fatty liver disease (NAFLD) and cardiovascular risk in renal transplant recipients. Kidney Blood Press Res. 2014;39:308–314. doi: 10.1159/000355808. [DOI] [PubMed] [Google Scholar]
- 41.Assem M, Amin M, Khalafallah O, Hussien A, Saif A, Mousa S. Hypoadiponectinemia as a marker of increased cardiovascular risk in patients with non-alcoholic fatty liver disease: correlation with albumin/creatinine ratio. Arch Endocrinol Metab. 2021;65:93–97. doi: 10.20945/2359-3997000000307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.El Azeem HA, Khalek el-SA, El-Akabawy H, Naeim H, Khalik HA, Alfifi AA. Association between nonalcoholic fatty liver disease and the incidence of cardiovascular and renal events. J Saudi Heart Assoc. 2013;25:239–246. doi: 10.1016/j.jsha.2013.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tziomalos K, Giampatzis V, Bouziana SD, Spanou M, Papadopoulou M, Pavlidis A, et al. Association between nonalcoholic fatty liver disease and acute ischemic stroke severity and outcome. World J Hepatol. 2013;5:621–626. doi: 10.4254/wjh.v5.i11.621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vlachopoulos C, Manesis E, Baou K, Papatheodoridis G, Koskinas J, Tiniakos D, et al. Increased arterial stiffness and impaired endothelial function in nonalcoholic fatty liver disease: a pilot study. Am J Hypertens. 2010;23:1183–1189. doi: 10.1038/ajh.2010.144. [DOI] [PubMed] [Google Scholar]
- 45.Agarwal AK, Jain V, Singla S, Baruah BP, Arya V, Yadav R, et al. Prevalence of non-alcoholic fatty liver disease and its correlation with coronary risk factors in patients with type 2 diabetes. J Assoc Physicians India. 2011;59:351–354. [PubMed] [Google Scholar]
- 46.Mishra S, Yadav D, Gupta M, Mishra H, Sharma P. A study of carotid atherosclerosis in patients with non-alcoholic fatty liver disease. Indian J Clin Biochem. 2013;28:79–83. doi: 10.1007/s12291-012-0286-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rampally V, Biri SK, Nair IK, Vadlakonda A. Determination of association between nonalcoholic fatty liver disease and carotid artery atherosclerosis among nondiabetic individuals. J Family Med Prim Care. 2020;9:1182–1186. doi: 10.4103/jfmpc.jfmpc_957_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rasool A, Dar W, Latief M, Dar I, Sofi N, Khan MA. Nonalcoholic fatty liver disease as an independent risk factor for carotid atherosclerosis. Brain Circ. 2017;3:35–40. doi: 10.4103/bc.bc_28_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Thakur ML, Sharma S, Kumar A, Bhatt SP, Luthra K, Guleria R, et al. Nonalcoholic fatty liver disease is associated with subclinical atherosclerosis independent of obesity and metabolic syndrome in Asian Indians. Atherosclerosis. 2012;223:507–511. doi: 10.1016/j.atherosclerosis.2012.06.005. [DOI] [PubMed] [Google Scholar]
- 50.Fadaei R, Meshkani R, Poustchi H, Fallah S, Moradi N, Panahi G, et al. Association of carotid intima media thickness with atherogenic index of plasma, apo B/apo A-I ratio and paraoxonase activity in patients with non-alcoholic fatty liver disease. Arch Physiol Biochem. 2019;125:19–24. doi: 10.1080/13813455.2018.1429475. [DOI] [PubMed] [Google Scholar]
- 51.Hanafi MG, Cina M, Zakerkish M, Rahim F, Saki-Malehi A, Nissi Q. Correlation between non-alcoholic fatty liver disease and carotid Intima-Media thickness in patient with type II diabetes. Int J Osteoporos Metab Disord. 2015;8:35–41. [Google Scholar]
- 52.Lankarani KB, Mahmoodi M, Lotfi M, Zamiri N, Heydari ST, Ghaffarpasand F, et al. Common carotid intima-media thickness in patients with non-alcoholic fatty liver disease: a population-based case-control study. Korean J Gastroenterol. 2013;62:344–351. doi: 10.4166/kjg.2013.62.6.344. [DOI] [PubMed] [Google Scholar]
- 53.Mohammadi A, Bazazi A, Ghasemi-Rad M. Evaluation of atherosclerotic findings in patients with nonalcoholic fatty liver disease. Int J Gen Med. 2011;4:717–722. doi: 10.2147/IJGM.S25753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mohammadi A, Bazazi A, Maleki-Miyandoab T, Ghasemi-Rad M. Evaluation of relationship between grading of fatty liver and severity of atherosclerotic finding. Int J Clin Exp Med. 2012;5:251–256. [PMC free article] [PubMed] [Google Scholar]
- 55.Mohammadi A, Sedani HH, Ghasemi-Rad M. Evaluation of carotid intima-media thickness and flow-mediated dilatation in middle-aged patients with nonalcoholic fatty liver disease. Vasc Health Risk Manag. 2011;7:661–665. doi: 10.2147/VHRM.S26011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mohammadzadeh A, Shahkarami V, Shakiba M, Sabetrasekh P, Mohammadzadeh M. Association of non-alcoholic fatty liver disease with increased carotid intima-media thickness considering other cardiovascular risk factors. Iran J Radiol. 2019;16:e14260. [Google Scholar]
- 57.Nahandi MZ, Khoshbaten M, Ramazanzadeh E, Abbaszadeh L, Javadrashid R, Shirazi KM, et al. Effect of non-alcoholic fatty liver disease on carotid artery intima-media thickness as a risk factor for atherosclerosis. Gastroenterol Hepatol Bed Bench. 2014;7:55–62. [PMC free article] [PubMed] [Google Scholar]
- 58.Fracanzani AL, Burdick L, Raselli S, Pedotti P, Grigore L, Santorelli G, et al. Carotid artery intima-media thickness in nonalcoholic fatty liver disease. Am J Med. 2008;121:72–78. doi: 10.1016/j.amjmed.2007.08.041. [DOI] [PubMed] [Google Scholar]
- 59.Fracanzani AL, Tiraboschi S, Pisano G, Consonni D, Baragetti A, Bertelli C, et al. Progression of carotid vascular damage and cardiovascular events in non-alcoholic fatty liver disease patients compared to the general population during 10 years of follow-up. Atherosclerosis. 2016;246:208–213. doi: 10.1016/j.atherosclerosis.2016.01.016. [DOI] [PubMed] [Google Scholar]
- 60.Mantovani A, Mingolla L, Rigolon R, Pichiri I, Cavalieri V, Zoppini G, et al. Nonalcoholic fatty liver disease is independently associated with an increased incidence of cardiovascular disease in adult patients with type 1 diabetes. Int J Cardiol. 2016;225:387–391. doi: 10.1016/j.ijcard.2016.10.040. [DOI] [PubMed] [Google Scholar]
- 61.Neri S, Signorelli SS, Scuderi R, Bruno M, Bertino G, Clementi A, et al. Carotid intima-media thickness and liver histology in hemodialysis patients with nonalcoholic fatty liver disease. Int J Angiol. 2011;20:149–156. doi: 10.1055/s-0031-1283218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ramilli S, Pretolani S, Muscari A, Pacelli B, Arienti V. Carotid lesions in outpatients with nonalcoholic fatty liver disease. World J Gastroenterol. 2009;15:4770–4774. doi: 10.3748/wjg.15.4770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Salvi P, Ruffini R, Agnoletti D, Magnani E, Pagliarani G, Comandini G, et al. Increased arterial stiffness in nonalcoholic fatty liver disease: the Cardio-GOOSE study. J Hypertens. 2010;28:1699–1707. doi: 10.1097/HJH.0b013e32833a7de6. [DOI] [PubMed] [Google Scholar]
- 64.Targher G, Bertolini L, Padovani R, Rodella S, Arcaro G, Day C. Differences and similarities in early atherosclerosis between patients with non-alcoholic steatohepatitis and chronic hepatitis B and C. J Hepatol. 2007;46:1126–1132. doi: 10.1016/j.jhep.2007.01.021. [DOI] [PubMed] [Google Scholar]
- 65.Targher G, Bertolini L, Padovani R, Rodella S, Zoppini G, Zenari L, et al. Relations between carotid artery wall thickness and liver histology in subjects with nonalcoholic fatty liver disease. Diabetes Care. 2006;29:1325–1330. doi: 10.2337/dc06-0135. [DOI] [PubMed] [Google Scholar]
- 66.Targher G, Bertolini L, Padovani R, Zoppini G, Zenari L, Falezza G. Associations between liver histology and carotid intima-media thickness in patients with nonalcoholic fatty liver disease. Arterioscler Thromb Vasc Biol. 2005;25:2687–2688. doi: 10.1161/01.ATV.0000189299.61568.79. [DOI] [PubMed] [Google Scholar]
- 67.Hamaguchi M, Kojima T, Takeda N, Nagata C, Takeda J, Sarui H, et al. Nonalcoholic fatty liver disease is a novel predictor of cardiovascular disease. World J Gastroenterol. 2007;13:1579–1584. doi: 10.3748/wjg.v13.i10.1579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mori T, Yoshioka K, Tanno Y. Non-alcoholic fatty liver disease frequency and associated factors at admission of acute stroke. Hepatol Int. 2022;16:81–88. doi: 10.1007/s12072-021-10253-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Omar N, Koshy M, Hanafiah M, Hatta SFWM, Shah FZM, Johari B, et al. Relationships between severity of steatosis with glycemic control and carotid intima-media thickness among diabetic patients with ischemic heart disease. J Res Med Sci. 2020;25:64. doi: 10.4103/jrms.JRMS_560_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Tan EC, Tai MS, Chan WK, Mahadeva S. Association between non-alcoholic fatty liver disease evaluated by transient elastography with extracranial carotid atherosclerosis in a multiethnic Asian community. JGH Open. 2018;3:117–125. doi: 10.1002/jgh3.12114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Silaghi CA, Silaghi H, Crăciun AE, Fărcaș A, Colosi HA, Cosma DT, et al. Age, abdominal obesity, and glycated hemoglobin are associated with carotid atherosclerosis in type 2 diabetes patients with nonalcoholic fatty liver disease. Med Ultrason. 2015;17:300–307. doi: 10.11152/mu.2013.2066.173.cas. [DOI] [PubMed] [Google Scholar]
- 72.Stolic RV, Trajkovic GZ, Kostic MM, Sovtic SR, Odalovic AM, Krdzic BD, et al. Correlation between nonalcoholic fatty liver and cardiovascular disease in elderly hemodialysis patients. Int Urol Nephrol. 2016;48:883–889. doi: 10.1007/s11255-016-1237-8. [DOI] [PubMed] [Google Scholar]
- 73.Hong HC, Hwang SY, Ryu JY, Yoo HJ, Seo JA, Kim SG, et al. The synergistic impact of nonalcoholic fatty liver disease and metabolic syndrome on subclinical atherosclerosis. Clin Endocrinol (Oxf) 2016;84:203–209. doi: 10.1111/cen.12940. [DOI] [PubMed] [Google Scholar]
- 74.Kang JH, Cho KI, Kim SM, Lee JY, Kim JJ, Goo JJ, et al. Relationship between nonalcoholic fatty liver disease and carotid artery atherosclerosis beyond metabolic disorders in nondiabetic patients. J Cardiovasc Ultrasound. 2012;20:126–133. doi: 10.4250/jcu.2012.20.3.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kim HC, Kim DJ, Huh KB. Association between nonalcoholic fatty liver disease and carotid intima-media thickness according to the presence of metabolic syndrome. Atherosclerosis. 2009;204:521–525. doi: 10.1016/j.atherosclerosis.2008.09.012. [DOI] [PubMed] [Google Scholar]
- 76.Kim JH, Kim SY, Jung ES, Jung SW, Koo JS, Kim JH, et al. Carotid intima-media thickness is increased not only in non-alcoholic fatty liver disease patients but also in alcoholic fatty liver patients. Digestion. 2011;84:149–155. doi: 10.1159/000326854. [DOI] [PubMed] [Google Scholar]
- 77.Kim SK, Choi YJ, Huh BW, Park SW, Lee EJ, Cho YW, et al. Nonalcoholic fatty liver disease is associated with increased carotid intima-media thickness only in type 2 diabetic subjects with insulin resistance. J Clin Endocrinol Metab. 2014;99:1879–1884. doi: 10.1210/jc.2013-4133. [DOI] [PubMed] [Google Scholar]
- 78.Moon SH, Noh TS, Cho YS, Hong SP, Hyun SH, Choi JY, et al. Association between nonalcoholic fatty liver disease and carotid artery inflammation evaluated by 18F-fluorodeoxyglucose positron emission tomography. Angiology. 2015;66:472–480. doi: 10.1177/0003319714537872. [DOI] [PubMed] [Google Scholar]
- 79.Serra-Planas E, Aguilera E, Castro L, Rodríguez R, Salinas I, Lucas A, et al. Low prevalence of non-alcoholic fatty liver disease in patients with type 1 diabetes is associated with decreased subclinical cardiovascular disease. J Diabetes. 2017;9:1065–1072. doi: 10.1111/1753-0407.12539. [DOI] [PubMed] [Google Scholar]
- 80.Zizza A, Guido M, Tumolo MR, De Donno A, Bagordo F, Grima P. Atherosclerosis is associated with a higher risk of hepatic steatosis in HIV-infected patients. J Prev Med Hyg. 2017;58:E219–E224. [PMC free article] [PubMed] [Google Scholar]
- 81.Wang CC, Lin SK, Tseng YF, Hsu CS, Tseng TC, Lin HH, et al. Elevation of serum aminotransferase activity increases risk of carotid atherosclerosis in patients with non-alcoholic fatty liver disease. J Gastroenterol Hepatol. 2009;24:1411–1416. doi: 10.1111/j.1440-1746.2009.05872.x. [DOI] [PubMed] [Google Scholar]
- 82.Arinc H, Sarli B, Baktir AO, Saglam H, Demirci E, Dogan Y, et al. Serum gamma glutamyl transferase and alanine transaminase concentrations predict endothelial dysfunction in patients with non-alcoholic steatohepatitis. Ups J Med Sci. 2013;118:228–234. doi: 10.3109/03009734.2013.814734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ayaz T, Kirbas A, Durakoglugil T, Durakoglugil ME, Sahin SB, Sahin OZ, et al. The relation between carotid intima media thickness and serum osteoprotegerin levels in nonalcoholic fatty liver disease. Metab Syndr Relat Disord. 2014;12:283–289. doi: 10.1089/met.2013.0151. [DOI] [PubMed] [Google Scholar]
- 84.Aygun C, Kocaman O, Sahin T, Uraz S, Eminler AT, Celebi A, et al. Evaluation of metabolic syndrome frequency and carotid artery intima-media thickness as risk factors for atherosclerosis in patients with nonalcoholic fatty liver disease. Dig Dis Sci. 2008;53:1352–1357. doi: 10.1007/s10620-007-9998-7. [DOI] [PubMed] [Google Scholar]
- 85.Başar O, Akbal E, Köklü S, Tuna Y, Koçak E, Başar N, et al. Increased H-FABP concentrations in nonalcoholic fatty liver disease. Possible marker for subclinical myocardial damage and subclinical atherosclerosis. Herz. 2013;38:417–422. doi: 10.1007/s00059-012-3714-x. [DOI] [PubMed] [Google Scholar]
- 86.Cetindağlı I, Kara M, Tanoglu A, Ozalper V, Aribal S, Hancerli Y, et al. Evaluation of endothelial dysfunction in patients with nonalcoholic fatty liver disease: association of selenoprotein P with carotid intima-media thickness and endothelium-dependent vasodilation. Clin Res Hepatol Gastroenterol. 2017;41:516–524. doi: 10.1016/j.clinre.2017.01.005. [DOI] [PubMed] [Google Scholar]
- 87.Colak Y, Karabay CY, Tuncer I, Kocabay G, Kalayci A, Senates E, et al. Relation of epicardial adipose tissue and carotid intimamedia thickness in patients with nonalcoholic fatty liver disease. Eur J Gastroenterol Hepatol. 2012;24:613–618. doi: 10.1097/MEG.0b013e3283513f19. [DOI] [PubMed] [Google Scholar]
- 88.Colak Y, Senates E, Yesil A, Yilmaz Y, Ozturk O, Doganay L, et al. Assessment of endothelial function in patients with nonalcoholic fatty liver disease. Endocrine. 2013;43:100–107. doi: 10.1007/s12020-012-9712-1. [DOI] [PubMed] [Google Scholar]
- 89.Kemaloglu C, Kemaloglu MD. Non alcoholic fatty liver disease is a predictor of subclinical carotid atherosclerosis in the presence of metabolic syndrome. Nepal Heart J. 2019;16:39–45. [Google Scholar]
- 90.Kilciler G, Genc H, Tapan S, Ors F, Kara M, Karadurmus N, et al. Mean platelet volume and its relationship with carotid atherosclerosis in subjects with non-alcoholic fatty liver disease. Ups J Med Sci. 2010;115:253–259. doi: 10.3109/03009734.2010.500062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kucukazman M, Ata N, Yavuz B, Dal K, Sen O, Deveci OS, et al. Evaluation of early atherosclerosis markers in patients with nonalcoholic fatty liver disease. Eur J Gastroenterol Hepatol. 2013;25:147–151. doi: 10.1097/MEG.0b013e32835a58b1. [DOI] [PubMed] [Google Scholar]
- 92.Ozturk K, Uygun A, Guler AK, Demirci H, Ozdemir C, Cakir M, et al. Nonalcoholic fatty liver disease is an independent risk factor for atherosclerosis in young adult men. Atherosclerosis. 2015;240:380–386. doi: 10.1016/j.atherosclerosis.2015.04.009. [DOI] [PubMed] [Google Scholar]
- 93.Gill C, Vatcheva KP, Pan JJ, Smulevitz B, McPherson DD, Fallon M, et al. Frequency of nonalcoholic fatty liver disease and subclinical atherosclerosis among young mexican americans. Am J Cardiol. 2017;119:1717–1722. doi: 10.1016/j.amjcard.2017.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Oni E, Budoff MJ, Zeb I, Li D, Veledar E, Polak JF, et al. Nonalcoholic fatty liver disease is associated with arterial distensibility and carotid intima-media thickness: (from the multi-ethnic study of atherosclerosis) Am J Cardiol. 2019;124:534–538. doi: 10.1016/j.amjcard.2019.05.028. [DOI] [PubMed] [Google Scholar]
- 95.Brea A, Mosquera D, Martín E, Arizti A, Cordero JL, Ros E. Nonalcoholic fatty liver disease is associated with carotid atherosclerosis: a case-control study. Arterioscler Thromb Vasc Biol. 2005;25:1045–1050. doi: 10.1161/01.ATV.0000160613.57985.18. [DOI] [PubMed] [Google Scholar]
- 96.Siddiqui MS, Sterling RK, Luketic VA, Puri P, Stravitz RT, Bouneva I, et al. Association between high-normal levels of alanine aminotransferase and risk factors for atherogenesis. Gastroenterology. 2013;145:1271–1279. doi: 10.1053/j.gastro.2013.08.036. e1-e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Siddiqui MS, Fuchs M, Idowu MO, Luketic VA, Boyett S, Sargeant C, et al. Severity of nonalcoholic fatty liver disease and progression to cirrhosis are associated with atherogenic lipoprotein profile. Clin Gastroenterol Hepatol. 2015;13:1000–1008. doi: 10.1016/j.cgh.2014.10.008. e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Patel S, Siddiqui MB, Roman JH, Zhang E, Lee E, Shen S, et al. Association between lipoprotein particles and atherosclerotic events in nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2021;19:2202–2204. doi: 10.1016/j.cgh.2020.09.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Rockman CB, Hoang H, Guo Y, Maldonado TS, Jacobowitz GR, Talishinskiy T, et al. The prevalence of carotid artery stenosis varies significantly by race. J Vasc Surg. 2013;57:327–337. doi: 10.1016/j.jvs.2012.08.118. [DOI] [PubMed] [Google Scholar]
- 100.Liu J, Zhu Y, Wu Y, Liu Y, Teng Z, Hao Y. Association of carotid atherosclerosis and recurrent cerebral infarction in the Chinese population: a meta-analysis. Neuropsychiatr Dis Treat. 2017;13:527–533. doi: 10.2147/NDT.S124386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Ammirati E, Moroni F, Magnoni M, Rocca MA, Messina R, Anzalone N, et al. Extent and characteristics of carotid plaques and brain parenchymal loss in asymptomatic patients with no indication for revascularization. Int J Cardiol Heart Vasc. 2020;30:100619. doi: 10.1016/j.ijcha.2020.100619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Haacke C, Althaus A, Spottke A, Siebert U, Back T, Dodel R. Long-term outcome after stroke: evaluating health-related quality of life using utility measurements. Stroke. 2006;37:193–198. doi: 10.1161/01.STR.0000196990.69412.fb. [DOI] [PubMed] [Google Scholar]
- 103.Choudhary NS, Duseja A. Screening of cardiovascular disease in nonalcoholic fatty liver disease: whom and how? J Clin Exp Hepatol. 2019;9:506–514. doi: 10.1016/j.jceh.2019.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.European Association for the Study of the Liver (EASL) European Association for the Study of Diabetes (EASD) European Association for the Study of Obesity (EASO) EASL-EASDEASO clinical practice guidelines for the management of nonalcoholic fatty liver disease. Obes Facts. 2016;9:65–90. doi: 10.1159/000443344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Bots ML, Grobbee DE. Intima media thickness as a surrogate marker for generalised atherosclerosis. Cardiovasc Drugs Ther. 2002;16:341–351. doi: 10.1023/a:1021738111273. [DOI] [PubMed] [Google Scholar]
- 106.Kasliwal RR, Bansal M, Desai D, Sharma M. Carotid intimamedia thickness: current evidence, practices, and Indian experience. Indian J Endocrinol Metab. 2014;18:13–22. doi: 10.4103/2230-8210.126522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Jahromi AS, Cinà CS, Liu Y, Clase CM. Sensitivity and specificity of color duplex ultrasound measurement in the estimation of internal carotid artery stenosis: a systematic review and metaanalysis. J Vasc Surg. 2005;41:962–972. doi: 10.1016/j.jvs.2005.02.044. [DOI] [PubMed] [Google Scholar]
- 108.Zaidi NR, Gilani SA, Mehboob R, Waseem H, Hassan A. Diagnostic accuracy of carotid intima media thickness by B-mode ultrasonography in coronary artery disease patients. Arch Med Sci Atheroscler Dis. 2020;5:e79–e84. doi: 10.5114/amsad.2020.95651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Toh JZK, Pan XH, Tay PWL, Ng CH, Yong JN, Xiao J, et al. A meta-analysis on the global prevalence, risk factors and screening of coronary heart disease in nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2021 Sep 21; doi: 10.1016/j.cgh.2021.09.021. doi: 10.1016/j.cgh.2021.09.021. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search strategy
Summary of included articles
Funnel plots of publication bias.