Abstract
Bone remodeling replaces old and damaged bone with new bone through a sequence of cellular events occurring on the same surface without any change in bone shape. It was initially thought that the basic multicellular unit (BMU) responsible for bone remodeling consists of osteoclasts and osteoblasts functioning through a hierarchical sequence of events organized into distinct stages. However, recent discoveries have indicated that all bone cells participate in BMU formation by interacting both simultaneously and at different differentiation stages with their progenitors, other cells, and bone matrix constituents. Therefore, bone remodeling is currently considered a physiological outcome of continuous cellular operational processes optimized to confer a survival advantage. Bone remodeling defines the primary activities that BMUs need to perform to renew successfully bone structural units. Hence, this review summarizes the current understanding of bone remodeling and future research directions with the aim of providing a clinically relevant biological background with which to identify targets for therapeutic strategies in osteoporosis.
Subject terms: Osteoporosis, Bone, Homeostasis
Introduction
Despite the tremendous efforts of researchers studying bone remodeling for more than 50 years, the intrinsic spatial, biomolecular, and mechanotransduction complexities in bone remodeling continue to be debated. Initially, a two-stage process involving two types of cellular machinery was considered to be responsible for bone remodeling, in which bone formation by osteoblasts follows bone resorption by osteoclasts to achieve net bone mass equilibrium upon physiological maturity.1 However, recently identified cellular events, coordination pathways and anatomical structures have allowed a better understanding of the genesis, differentiation, activity, crosstalk and death of the entire cell population involved in bone remodeling.2 These discoveries have shed new light on the operational processes ensuring bone mass renewal without bone mass loss under physiological conditions. Bone remodeling is activated by local and systemic factors, supporting the concept that targeted remodeling is activated by local factors and that stochastic remodeling is activated by systemic factors, with these factors cooperating to maintain mechanical competence and meet concurrent metabolic demands. This new information implies that the determinants of the focal balance in bone mass after remodeling are the integrated effects of both mechanical and metabolic environmental conditions.
This review provides a novel integrated picture of the operational bone remodeling processes by describing, updating, and reexamining the current evidence and its biological plausibility. In this review, bone remodeling is described as a continuous flow of cellular signaling and connected events, not as a process comprising stages, as it has been historically presented.
Bone modeling, remodeling, and the mutual regulation of bone resorption and formation
In vertebrates, bone modeling and remodeling are essential processes that are activated throughout life and are regulated by distinct temporal cellular constituents that ensure functional bone adaptation and vertebrate survival. Bone modeling adapts bone shape to variable mechanical demands during growth and aging through cellular events that determine bone resorption and formation on opposing cortical and cancellous surfaces. This implies the existence of a modeling drift, which moves a bone structural unit over time in the direction defined by growth patterns, and adjusts the bone mass distribution to the stresses and strains induced by locomotion and physical activity.3 By bone remodeling, old or damaged bone is replaced with new bone through a sequence of cellular events occurring on the same surface without any change in bone shape.4
In the 1960s, Frost5 recognized that a forming osteon in mammalian compact bone consists of a group of synchronous cells, suggesting “control mechanisms which are functionally and temporally ordered, discontinuous and discrete”. Frost advanced the enlightening notion of a basic multicellular unit (BMU) as a transient anatomic structure in bone remodeling and introduced the quantum concept of bone remodeling, which is analogous to quantum theory in physics. Quantum physics explains the property of matter at the smallest scale. It defines the behavior of the minimum, discrete amount, i.e., the quantum, of any physical entity on the assumption that all phenomena in a submicroscopic system exhibit quantization.6 In an analogy, Frost intuitively defined a quantum of bone remodeling as a discrete change in bone mass resulting from the coordinated activity of an individual BMU at an anatomically discrete locus.1 The quantum concept conceived by Frost and later extended by Parfitt7 has had profound implications for the understanding of all aspects of bone pharmacology and physiopathology,8 particularly in the osteoporotic context.9 A remarkable idea of the early sixties that is in line with the modern theory that quantum biological phenomena can lead to evolutionary advantages.10
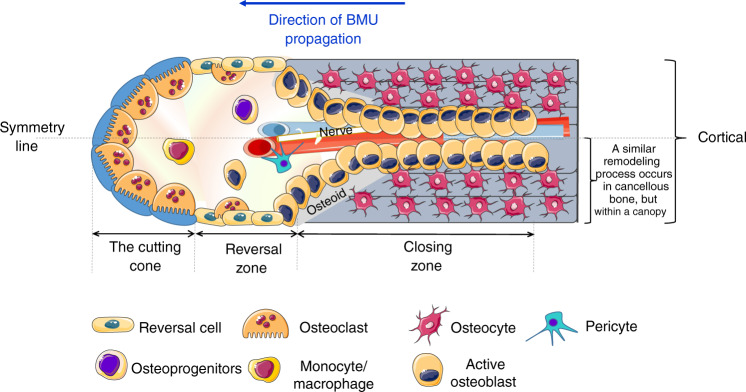
Frost recognized that the change in bone mass caused by the focal balance in each remodeling cycle of resorbed bone and formed bone is not an outcome of isolated “working” cell packets but is derived from the interacting parts of the whole BMU, which endures longer (9 months) than the lifespan of each single component.4 This implies a continuous and ordered cell supply that depends on the division frequency of each progenitor cell and the lifespan of each differentiated cell. A tightly maintained equilibrium between genesis and apoptosis is therefore critical for a properly functioning BMU.11 Recent advances have added complexity to the original BMU description. The number of cells considered to constitute a BMU has expanded to include all bone cells at all differentiation stages, interacting with their progenitors, T cells and bone matrix components. The BMU includes, in particular, a set of osteoclasts localized in the “cutting cone” followed by a set of cells, including reversal cells and osteoblasts, localized at the reversal zone; and a set of osteocytes localized in the closing zone. These cell sets constitute a secondary osteon around the neurovascular bundle wich is axially located with the connective matrix in the Haversian canal. A visualization of a complete BMU can be acquired only with a longitudinal section of cortical bone, where Haversian canals run parallel to the sectional plane (Fig. 1). Notably, the 3D trabecular network prevents the proper visualization of a complete BMU in cancellous bone.12
Fig. 1.
The cutting cone. The cutting cone originates in close proximity to neurovascular axial bundles and is generated by the propagation of the basic multicellular unit (BMU). The cutting cone consists of a set of osteoclasts, followed by a set of osteoblasts, reversal cells and secondary osteoclasts that cover the so-called reversal zone. At the end of the reversal zone, a set of osteocytes generate the closing zone. A line of symmetry divides in half the representation of a complete BMU in the cortex moving toward the longitudinal axis of the long bone. One-half of cortical BMU is similar to the BMU at the cancellous surface, although in cancellous bone, the BMU is separated from the marrow by a specific cell structure called the canopy
In bone remodeling, osteoblast–osteoclast interactions are necessary and must be coordinated in time and space to maintain the focal bone remodeling balance; this balance refers to the net amount of tissue resorbed and formed at each remodeling site (i.e., focal point) to maintain the structural integrity of the tissue. At maturity, the focal balance (neutral) in bone remodeling is determined by equal bone aliquots, which are removed and synthetized. In other periods in life or as a consequence of metabolic diseases, the focal balance can be negative (bone mass is lost) or positive (bone mass is gained). Focal coupling in bone remodeling strictly refers to the transfer of the information within the cell pool responsible for bone remodeling. This operational process couples the events necessary to remove and replace bone units under a hierarchy of time and space, independent of their focal balance; in fact, focal remodeling imbalance does not imply “uncoupling”. At each remodeling site, coupling indicates that the receptors on the osteoclast membrane as well as the regulatory factors released by osteoclasts are coupled with the sequential recruitment and differentiation of osteoblast lineage cells toward the mature phenotype, laying down the bone matrix and inducing mineralization. Coupling therefore implies that a commensurate change in bone formation follows any pathology- or therapy-related modification of bone resorption.
At each remodeling site, coupling is asynchronous: at any given time, bone is being resorbed at some sites, while it is being formed or is in the reversal phase from bone resorption to bone formation at other site. This implies that there is continuous focal transient loss of bone that is fully reversed in balanced remodeling; as the number of activated remodeling sites increases, the transient loss of bone, which is defined as the “virtual space” of bone remodeling, increases. As coupling takes place in different locations at different times, it requires local regulatory factors to transfer information among cells and tissue locations according to bone remodeling needs. Therefore, remodeling is defined as a dynamic physiological process executed through the coupled activity of osteoclasts and osteoblasts belonging to a BMU. Conversely, bone turnover is the outcome of bone remodeling that defines the amount of bone removed and formed within a given volume in a given time and is determined by the number of BMUs and by the focal balance within each BMU. As Parfitt said “Bone turnover refers to proportional bone volume replacement per unit time, and is usually expressed as percent/year […]. If bone turnover is 10%/year, then the mean lifetime of each moiety of bone is 10 years”.13
Osteocytes: tuning, initiation and termination of bone remodeling
Osteocytes are a relatively permanent phenotype of bone cells that Frost estimated to have a lifespan of ~25 years1 and play a master role in bone remodeling. Osteocytes represent more than 90% of bone cells in the adult skeleton14 with a average cell density highly dependent on the specie, bone anatomical site, and subiect analyzed.15 Recent studies performed using new imaging techniques have estimated that 19 000–28 500 cells per mm3 populate the human skeleton, accounting for ~42 billion individual cells.16 Osteocytes consist of a stellate body connected by slender cell processes (50–100 processes per cell). The asymmetrical “arborization” of dendrites polarizes toward bone surfaces, where the dendrites contact osteoblasts undergoing growth or remodeling or, during bone surface quiescence, bone lining cells. The term “arborization” was originally introduced by Marotti and Palumbo,17 and it now refers to “dendrogenesis”, the asymmetric and asynchronous formation of osteocyte dendrites. Short radiating dendrites extend toward mineralized surface, and long radiating dendrites extend toward the vasculature during the progressive translocation of cell bodies farther from the vascular surface due to the secretion of the osteoblastic lamina. Osteocytogenesis and dendrogenesis are discussed in a subsequent section (“The osteoblast pool: recruitment, expansion and osteocytogenesis”).
An adult human skeleton includes 23 trillion osteocyte connections with each other and with bone surface cells.16 These connections form a 3D protoplasmic network that constitutes a matrix-integrated functional syncytium, which does not cross cement lines but does establish direct contact with the bone marrow, resides in low-oxygen microenvironment and comprises multiple elements. During aging in both humans and rodents, this network deteriorates. Throughout aging, a large and linear reduction in dendrite number and cell body density directly related to the deterioration of cortical parameters has been observed.18 Since decreased osteocyte number accompanies reduced dendritic density, it has been suggested that dendrite loss might contribute to diminished osteocyte viability because a certain degree of locally and/or systemically triggered anabolic signaling through the osteocyte-lacunocanalicular system is lost (see below).18
The osteocyte-bone lining cell syncytium displays gap junctions (connexins) that allow the transfer of information between cells. Connexin43 (Cx43) is the most abundant connexin in osteocytes, and global knockout of Cx43 expression is lethal at birth.19 Conditional knockout of Cx43 in osteoblasts and osteocytes in mice led to various degrees of osteopenia depending on the differentiation state in which the deletion was induced,20,21 suggesting that functional Cx43 in osteoblasts and osteocytes is essential for normal bone mass acquisition and maintenance.
The osteocyte-bone lining cell syncytium is endowed within the lacunocanalicular network of cavities filled with bone extracellular fluid (BEF). BEF has a different ionic composition from systemic extracellular fluid (SEF)22 and establishes an extensive contact surface (215 m2, which is 120-fold the size of the trabecular network) with the mineralized matrix to allow efficient, short-term mineral exchange with SEF.23–26 This specific physical environment allows osteocytes to govern metabolic demands and mechanotransduction for bone mass adaptation.27 The strain-induced flow of BEF in the lacuno-canalicular network exerts a shear stress (fluid flow shear stress, FFSS) on osteocyte bodies, which undergo dendrogenesis to activate several classes of mechano-sensors regulating specific gene expression patterns.28
Osteocytes might sense FFSS through 1. “collagen hillocks”, which are collagen matrix projections in osteocyte canaliculi that directly link the matrix to osteocyte dendrites;29 2. β3 and β1 integrins, which participate to focal adhesion kinase (FAK) complex formation in osteocyte dendritic projections;30 3. primary cilia, which have a flow-sensing function that leads to increased osteoprotegerin (OPG)/receptor activator of nuclear factor kappa-B ligand (RANKL) ratio via a calcium-independent mechanism;31 4. connexin43, a component of gap junctions that mediates the transduction of mechanical signals;32 and 5. mechanosensitive ion channels, such as those composed of Piezo1, which are highly sensitive to osteocyte membrane tension.33
The deformation of the osteocyte cytoskeleton elicits Ca2+ influx signaling via the activation of TRPV4.34 The generation of Ca2+-dependent contractions of the cell membrane favors the production and release of extracellular vesicles (EVs) containing bone regulatory proteins.35 EVs are ubiquitous lipidic organelles that mediate the intercellular transfer of information through their cargo, which includes both proteins and nucleic acids.36 In osteocytes, EVs can be observed in proximity of the osteocytic network.37 In response to mechanical stimuli and subsequent Ca2+ influx, osteocyte lines have been observed to release EVs containing RANKL, OPG, and sclerostin.35
All the mechanical signals received by the osteocyte-bone lining cell syncytium modulate cell apoptosis and survival as well as the anabolic Wnt pathway in bone. Secreted Wnt protein stimulates target cell via the β-catenin-mediated (canonical) and β-catenin-independent (noncanonical) pathways. The canonical pathway has emerged as the predominant component of Wnt signaling in bone, positively affecting the entire osteoblast lineage.38 Wnt proteins bind to their receptors (Frizzled) and coreceptors (LRP5/6) to promote the stabilization of β-catenin in the cytoplasm, which translocates to the nucleus, where it induces the expression of osteogenesis-related genes.38,39 Many studies have demonstrated that β-catenin is required for bone formation and is activated during multiple stages of osteoblast differentiation to regulate both osteoblast and osteoclast.40–43 In fact, WNT–β-catenin signaling in osteoblasts and osteocytes indirectly represses osteoclast differentiation and bone resorption by stimulating the secretion of OPG.38
Mechanical signals activate the anabolic Wnt pathway in bone through the suppression of the Wnt receptor antagonist sclerostin (SOST). Recently, Sato et al.20,44 showed that FFSS induces the disruption of the FAK-integrin complex, thereby inhibiting histone deacetylase 4/5 (HDAC4/5), a negative regulator of SOST expression in osteocytes45 modulated by parathyroid hormone (PTH) treatment.46 Osteocytes can also decrease SOST expression after sensing decreases in oxygen levels.47
In vivo anatomical studies have suggested that the presence of apoptotic osteocytes at microdamaged sites correlates with the recruitment of osteoclasts at microcracks.48 In addition to their fundamental role as mechanosensors, osteocytes appear to be spatially, temporally and mechanistically linked to bone remodeling activation, particularly by regulating RANKL (as is discussed below). RANKL is routinely found as a membrane bound protein (mRANKL), but it can also be cleaved into a soluble form (sRANKL)49 or delivered via EVs.35 RANKL binds the receptor activator of nuclear factor kappa-B (RANK) on osteoclasts to induce osteoclastogenesis.50
In 2011, Nakashima et al.51 showed that the conditional deletion of RANKL expression in osteocytes using a DMP1 promoter caused a severe osteopetrotic phenotype. This osteopetrotic phenotype was confirmed by Xiong et al.,52 who in addition found that RANKL mRNA, isolated from total bone of DMP1-cre+, RANKLloxp/loxP mice, showed very little variation compared to that of wild type mice. The concentration of circulating sRANKL was unaltered compared to that in wild type animals. However, a 70% reduction in osteoclast number in the cancellous bone of these transgenic mice highlighted the relevance of local RANKL production.52 As the activation of Dmp1-Cre promoters is not exclusive to osteocytes,53 the conditional deletion of RANKL expression was performed under the control of the more specific SOST promoter. This conditional deletion generated a phenotype resembling the previous one, with a significant decrease in osteoclasts number in cancellous bone.54 Taken together, these in vivo studies confirmed that osteocytes produce RANKL and that osteocytic RANKL is fundamental to sustaining bone remodeling.
Whether osteocyte RANKL is soluble, is transferred via vesicles or is membrane-bound is not fully clear. Bonewald et al.14 first demonstrated that the MLO-Y4 osteocyte line expresses RANKL at the cell surface and at dendritic processes. MLO-Y4 cells and primary murine osteocytes cocultured with bone marrow precursors supported osteoclastogenesis, but their conditioned media alone did not have a similar effect,55 suggesting that cell–cell interactions between osteocytes and osteoclasts are needed for osteoclastogenesis. In a different study, the conditioned media of apoptotic MLO-Y4 cells increased osteoclast formation, osteoclast size and osteoclast precursor migration. Interestingly, in apoptotic MLO-Y4 cells, both RANKL mRNA and protein expression were upregulated, suggesting that the conditioned media of this cell culture might contain sRANKL.56 On the other hand, the conditioned media of a non apoptotic MLO-Y4 culture did not alter any of these aforementioned cell parameters.56 In another in vitro study, primary osteocytes were cocultured on a 3D collagen scaffold with osteoclast precursors separated by a porous membrane. Again, the osteocytes supported osteoclast formation, but the efficiency of their effect decreased with a decrease in the pore size of the membrane. Confocal microscopy showed that large pore membranes allow osteocyte dendrites to touch osteoclast precursors through the pores, but this contact was not observed when small-pore membranes were used.57 Therefore, the authors of this study hypothesized that under specific conditions, such as when osteocytes cannot physically touch OC precursors, osteocytes might support osteoclastogenesis by secreting EVs containing RANKL.58 Distinguish the exact localization and form of RANKL produced by osteocytes in vivo is particularly complicated, as the antibodies used for immunohistochemical analyses do not distinguish between the soluble and membrane forms. Therefore, to evaluate the form of RANKL that induces osteoclastogenesis, a mouse model was generated with a sheddase-resistant form of RANKL with no detectable sRANKL levels in the circulation. During growth, this lack of sRANKL did not cause bone mass alteration, but in the adult model mice, the number of osteoclasts was reduced with an increase in cancellous bone mass.59 However, mice lacking sRANKL expression and ovariectomized still displayed bone loss because of the lack of estrogen, indicating that, although mRANKL can support most RANKL functions, the soluble form is necessary to sustain bone remodeling under certain conditions.59 In support of this hypothesis, mice overexpressing sRANKL only in the liver, and therefore also in blood circulation, displayed a significant decrease in bone mass with an increase in the number of osteoclasts on cancellous bone surfaces during aging.60
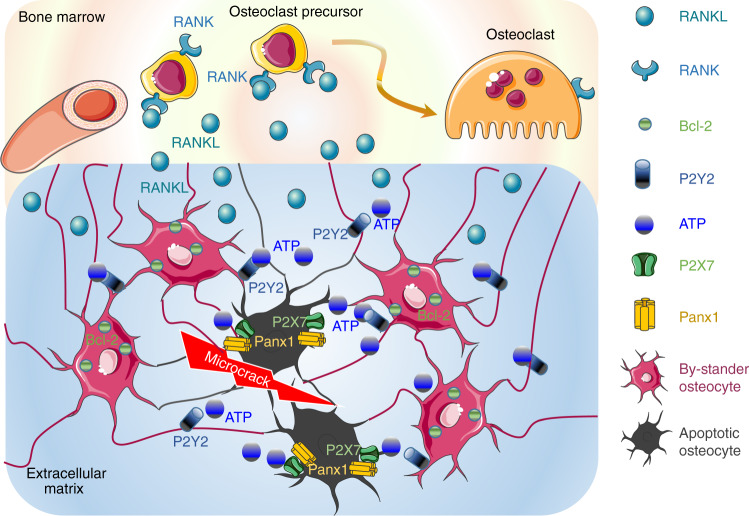
In vivo, osteocyte apoptosis is fundamental for initiating bone remodeling,61 independent of the stimulus causing osteocyte death such as estrogen loss,62 fatigue,63 or unloading.64 An in vivo immunohistochemical analysis showed that the RANKL signal in bone tissue was stronger in an area around 150–200 μm from the apopototc osteocytes.65 Interestingly, inhibiting apoptosis prevented the RANKL production by neighboring osteocytes, suggesting that “bone remodeling follows a common paradigm for localized tissue repair”, with different response-induced factor released from apoptotic osteocytes near the damage site and “bystander” osteocytes.63 MLO-Y4 cell apoptosis generated ATP release from cells via Pannexin 1 channels (PANX1) opening.66 The same phenotype was observed in mice treated with an inhibitor of the P2X7 receptor (P2X7R), which is a coactivator of PANX1.67 In periodontal ligament cells, ATP induced the upregulation of RANKL expression via a P2Y1 receptor-cyclooxygenase-dependent pathway.68 Since the release of ATP from apoptotic cells functions as a specific “find me” message for phagocytic cells,69 ATP release during osteocyte apoptosis might be a specific “find me” signal directed to neighboring osteocytes. Indeed, ATP from apoptotic osteocytes might bind P2Y2 receptors expressed on bystander osteocytes, which in turn might activate RANKL production and release67 (Fig. 2). Moreover, bystander osteocytes (in 1–2-mm proximity to the focal damage site) expressed the antiapoptotic protein BcL-2. This defense mechanism might be necessary to prevent osteoclastogenic signal damaging viable osteocytes70 (Fig. 2).
Fig. 2.
The “find me” message from apoptotic osteocytes. Under fatigue failure, osteocytes undergo apoptosis, whereas the osteocytes surrounding the apoptotic osteocytes, the “bystander osteocytes”, show upregulation of the antiapoptotic protein BcL-2, which protects them from death. Apoptotic osteocytes activate the Panx1/P2XR pathway to induce the release of ATP into the extracellular compartment as a specific “find me” signal. ATP binds P2Y2 receptors on bystander osteocytes, which in turn produce and release RANKL at the interface with the bone marrow. RANKL promotes the recruitment of osteoclast progenitors and osteoclastogenesis
As osteocytes are deeply embedded in the bone matrix, osteocyte apoptosis or autophagic death causes secondary necrosis due to inhibited phagocytosis by scavenger cells. Necrotic osteocytes release damage-associated molecular pattern (DAMP) proteins after the cell membrane is disrupted.61 DAMP proteins flow through the canalicular network and reach the bone/marrow interface, where they bind to pattern recognition receptors (PRRs) on bone marrow cells.71 When activated by DAMP–PRR binding, monocytes and macrophages produce proinflammatory cytokines, such as TNFα, IL-6, and IL-1.72 These cytokines in turn stimulate the expression of RANKL in osteoblasts,73 enhancing the osteoclastogenesis previously activated by the release of ATP by apoptotic osteocytes.66 DAMPs can directly regulate osteoclast formation by activating the membrane-bound C-type lectin receptor Mincle. Mincle activation triggers calcium signaling and oxidative phosphorylation in osteoclasts, inducing osteoclast differentiation.74
Under physiological conditions, osteocytes exert an inhibitory effect on osteoclasts by contributing to the osteoblast production of OPG via Wnt signaling.75,38 OPG functions as a soluble decoy receptor that binds RANKL, preventing its interaction with RANK expressed by osteoclast progenitors. The major cell source of OPG is still debated, as it depends on the bone compartment and on the age of the subject considered. In addition to osteocytes, other cells can be sources of OPG or RANKL; these cells are osteoprogenitors, osteoblasts49 or cells of the immune system (B and T cells),76 which are all simultaneously present in a BMU. Nevertheless, OPG released by mature osteoblasts and/or osteocytes may constitute the termination signal of the resorption phase in the remodeling cycle.77
In addition to microcrack-induced signals to activate the healing of microdamage foci through targeted remodeling, osteocytes sense systemic and local stimuli that affect their functions and survival. When exposed to a stimulus, osteocytes release several factors affecting (1) bone remodeling at stochastic loci, (2) matrix mineralization, (3) lacunocanalicular remodeling, (4) mineral homeostasis, and (5) fat metabolism and myogenesis (Table 1).
Table 1.
Systemic and local factors influencing osteocyte function
| Stimuli (Systemic/Local) | Features affected (Local) | Factors released (Local/Systemic) | Final outcome (Systemic/Local) |
|---|---|---|---|
|
PTH Estrogens 1,25(OH)2D3 Irisin Calcitonin Senescence TGF-β1 Pi pO2 |
Life-Span Network formation Secretome Mechanotrasduction |
Sclerostin, DKK1, FGF23, DMP1, Phex, MEPE, Sema 3A RANKL, OPG SASPs, TGF-β1 OCN |
• Bone Remodeling Balance • Matrix Mineralization • Perilacunocanalicular Remodeling • Errors correction in Ca2+/P homeostasis • Energy metabolism • Myogenesis • Oxidative stress |
Major systemic and local stimuli that influence osteocyte activity, the functions affected, the factors released upon exposure to the stimuli, and the impact on the system
PTH/PTH-related peptide (PTHrP)
Under physiological conditions, osteocytes integrate the responses of bone to mechanical loading and PTH, since the mechanotransduction process requires PTH receptor 1 (PTHR1) activation to downregulate SOST expression. SOST expression downregulation positively fine-tunes the bone remodeling balance by promoting osteoblast expansion.78 When PTHR1 on osteocytes is activated by chronically high PTH concentrations or when PTHR1 is constitutively active, osteocytes initiate bone remodeling by expanding the osteoclast pool through the release of RANKL,79 particularly within the bone cortex.80 In contrast, when PTHR1 is deleted, RANKL release and subsequent osteoclastogenesis do not occur.81
Interestingly, in addition to BMU activation, three hours after PTH exposure, demineralization of the bone matrix surrounding osteocytes accompanied by compensatory mineral deposition has been observed.82 The same outcome was observed in cases of excess PTH concentrations both in rats83 and humans84 and under PTH modulation after exercise.85 This process is mediated by osteocytes and is called perilacunar remodeling (i.e., “osteocytic osteolysis”); it was initially recognized during lactation. Perilacunar remodeling has been associated with the activation of PTH-related peptide (PTHrP)–PTHR1 signaling, which induces matrix resorptive activity in osteocytes similar to that in osteoclasts.86 Perilacunar remodeling integrated with bone remodeling contributes to the maintenance of bone quality. Perilacunar remodeling is an additional component of the long-term error correction mechanism to maintain plasma calcium levels, in addition to the homeostatic regulatory mechanism in osteoclasts (RANKL-mediated). The efficiency of this additional and independent component of bone remodeling in calcium homeostasis under PTH regulation remains unclear because of the lack of a relationship between serum PTH and osteocyte lacuna characteristics.87
Nevertheless, as has been recently discussed,88 osteocytes per sé function independently of associated endocrine loops and exhibit an evolutionary advantage in mineral homeostasis, which is particularly highlighted in the rapid minute-to-minute regulation of the BEF-[Ca2+] in teleosts,89 as well as in mammals.26,90
Osteocytes, through PTHR1 activation, might counteract age-related bone mass loss. In fact, during aging, as well as under the action of several stressors [see Farr et al.91 for a review], senescent osteocytes accumulate in the bone microenvironment and acquire a distinctive proinflammatory secretome, termed the senescence-associated secretory phenotype (SASP),92 which leads to imbalanced bone remodeling with increased resorption and decreased formation. When PTHR1 was deleted in mouse osteocytes in vivo (Dmp1-PPRKO), the affected mice displayed age-dependent osteopenia related to a decrease in osteoblast activity with a parallel rise in osteoclast number and activity. The imbalanced bone remodeling in these animals was partially due to a sclerostin-dependent decrease in osteoblast activity and the lack of osteocyte protection from oxidative stress.93
Estrogen
Osteocytes respond to estrogen by producing the protein semaphorin 3A (Sema3A). Sema3A released into the bone microenvironment binds to its receptor on osteocytes and promotes their survival. The autocrine loop initiated via Sema3A is mainly triggered in the mature cell stage, which is the dominant characteristic of cells in the adult skeleton and is critical in bone remodeling balance, counteracting age-related bone loss. Autocrine loop impairment caused by estrogen deficiency induces an osteoporosis phenotype.94 In addition to its effects on bone remodeling, estrogen regulates mechanotransduction in osteocytes by affecting FFSS,95 Wnt/β-catenin expression,96 and Cx43 expression.97 Its removal triggers osteocyte apoptosis and alters the oxidative microenvironment, leading to the loss of osteocyte resistance to oxidative stress.
TGF-β1
Recently, osteocyte-intrinsic TGF-β1 signaling was discovered as a regulator of lacuno-canalicular remodeling. The suppression of TGF-β1 signaling in osteocytes, either pharmacologically (by TGF-β receptor type I kinase inhibitors) or genetically (by specific deletion of the receptor TβRII in DMP1-cre mice), leads to the reduction osteocyte dendrites length and total lacuno-canalicular area. The deterioration of the lacuno-canalicular network was accompanied by the decrease in the gene expression of Sost, and metalloproteases Mmp2, 13, 14, which are involved in the lacuno-canalicular remodeling, and by the reduction of fracture resistance in cortical bone despite no differences in cortical thickness and geometry, and increase in trabecular bone mass, likely due to the observed decrease in osteoclasts number and surface.98 The observation that lacuno-canalicular remodeling is an essential component of bone mechanical competence sustains the view that osteocytes play an evolutionarily conserved role in bone quality control.98
1,25(OH)2D3
In addition to its systemic effects, 1,25(OH)2D3 binds to VDR in osteocytes in an autocrine manner, and as they mature, osteocytes acquire the capacity to convert physiological levels of 25(OH)D to 1,25(OH)2D3.99 The exact role of 1,25(OH)2D3 in osteocyte metabolism is still uncharacterized. However, recent observations have pointed out that 1,25(OH)2D3 a) stimulates the production of fibroblast factor 23 (FGF23) in osteocyte-like cells;100 the hormone FGF23 is primarily involved in phosphate homeostasis and vitamin D synthesis; b) modulates matrix mineralization by downregulating dentin matrix protein-1 (DMP-1);101 and c) regulates osteocyte perilacunar remodeling and canalicular organization through the activation of matrix resorption genes.102
Phosphate
The establishment of X-linked hypophosphatemia (XLH) mouse models, characterized by elevated serum FGF23 levels, which caused decreased 1,25(OH)2D3 levels and hypophosphatemia, led to the discovery of the role played by phosphate in osteocyte functioning, which is triggered in response to disruption of plasma phosphate homeostasis.103 How osteocytes sense phosphate levels and subsequently regulate perilacunar remodeling103 and FGF23 and 1,25(OH)2D3 synthesis104 is still unclear. However, as has been previously discussed,105 the phosphate-sensing mechanism in osteocytes may involve the activation of FGFR1 and high-affinity Na+-Pi cotransporters.
Calcitonin
Osteocytes express specific calcitonin receptors, which are progressively lost with age.106 Calcitonin can potentially modify the osteocyte production of sclerostin and FGF23.107
Irisin
Irisin, a myokine produced by muscles, reduces osteocyte apoptosis and increases osteocyte number.108 These effects suggest a regulatory loop involving osteocytes and muscle metabolism, particularly since osteocytes inhibit skeletal muscle differentiation by producing a large number of cytokines, which might permeate the periosteum or diffuse into the circulation to negatively regulate myogenesis109.
These findings indicate that osteocytes can be considered the “social” coordinators of bone cells because they are responsible for maintaining bone physiological responsiveness to mechanical and metabolic demands. When osteocytic coordination fails, severe osteoporosis develops.110
Bone lining cells (blcs), canopy cells and pericytes: composition of the vascular bone remodeling compartment (brc)
BLCs, derived from the final differentiation of osteoblasts, are located on quiescent trabecular, endosteal, and endocortical surfaces at the end of bone formation. BLCs are a cell population that differs from both marrow cells111 and osteoblasts. BLCs are flattened and exibits lower synthetic activity, with little cytoplasm or endoplasmic reticulum,112 but they retain a social attitude. Similar to osteocytes, BLCs express intercellular adhesion molecule-1 (ICAM-1) to maintain functional contact with osteoblasts, osteoclast precursors113 and mature osteoclasts.114 They cover quiescent bone surfaces that are not undergoing remodeling, but they are not “quiescent” as the older literature suggests. Although their specific function has not yet been fully defined, BLCs might form an epithelial-like membrane that functions as an ion partition system between bone and systemic extracellular fluids in Ca2+ homeostasis.26,90,115 Indeed, the BLC membrane expresses tight junction membrane proteins that are responsive to metabolic demands such as chronic metabolic acidosis.116 Moreover, BLCs stain positive for osteoblast markers such as alkaline phosphatase, (ALP) osteocalcin (OCN), and osteonectin, in agreement with their osteogenic potential. BLCs are covered by a thin layer of mesenchyme-derived cells called bone marrow envelope (BME) cells that morphologically resemble BLCs and, similar to BLCs, are considered osteoprogenitors.2
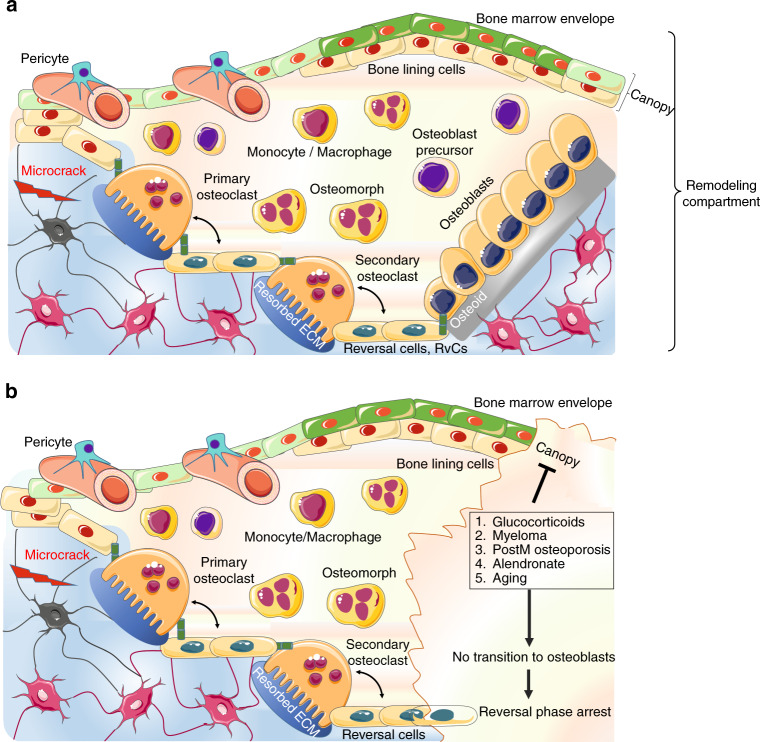
When the remodeling starts, BME cells and BLCs form a protective structure known as the canopy, which separates osteoclasts and osteoblasts from bone marrow117 (Fig. 3). At the bone remodeling site, BLCs disconnect from the underlying osteocytes through gap junction disruption, and digest fibrillary collagen, the most abundant component in the bone extracellular matrix (ECM), which is tightly packed in a helical structure to provide mechanical stability and confer resistance against proteolysis.118 To be degraded, fibrillary collagen usually requires the activation of the cysteine protease cathepsin K and members of the matrix metalloproteinase (MMP) family.119 While osteoclasts express both of these enzymes types, which contribute differently to bone resorption,120 BLCs do not express cathepsin K but can efficiently remove nonmineralized fibrillary collagen (present either on the quiescent bone surface or in resorption lacunae after osteoclastic activity)113 mediated through their highly active MMPs.121
Fig. 3.
The bone remodeling compartment (BRC). a The BRC provides the correct microenvironment to link bone formation and resorption through local signaling. The bone marrow envelope (BME) is a layer of cells of mesenchymal origin and a reservoir for osteoprogenitors that covers the layer of bone lining cells (BLCs). Once remodeling is initiated, osteoclasts lift the BME from the BLC, inducing BME cells to form a structure called the canopy. The canopy separates the remodeling site from the remainder of the bone marrow to allow osteoclast and osteoblast precursors to enter the blood compartment. After resorption, osteoclasts either undergo apoptosis or dedifferentiate into osteomorphs. The resorbed surface is then colonized by secondary osteoclasts and reversal cells. Reversal cells are osteoblast progenitors that digest fibrillar collagen remnants, similar to BLCs. Secondary osteoclasts and reversal cells provide the basis for the recruitment and expansion of osteoblastic pools (b) except under certain counteracting conditions, such as glucocorticoid or alendronate treatment, myeloma, or postmenopausal osteoporosis
The generation of the canopy allows the formation of the bone remodeling compartment (BRC), which is considered an essential component of the BMU itself, as it provides a microenvironment to link bone formation and resorption through local signaling.122
The BRC is generated in the proximity of the microvasculature123 (Fig. 3). Although it is unclear how the BRC is formed, several lines of evidence have suggested that the BRC favors a direct connection between bone cells and sinusoids, which might provide reservoirs of osteoprogenitors.122
In support of this hypothesis, an increased presence of capillaries covering human cancellous bone has been found at remodeling sites in an area within 50 µm from the canopy surface.124 This coverage has also been observed on cortical bone remodeling sites.4
The tight link between BRCs and capillaries, which are coated with pericytes, allows capillary-BRC canopy interactions to induce BMU development at bone remodeling sites117 (Fig. 3). Pericytes, first identified as cells covering microvessels/capillaries and maintaining local homeostasis and angiogenesis, support the mesenchymal niche and can be considered osteoprogenitors.125 It has been hypothesized that pericytes first move from capillaries to the canopy and then to the bone surface, where they differentiate into mature osteoblasts during bone remodeling.126 It is also plausible that the vascularization of the BRC favors the recruitment of osteoprogenitors circulating in the peripheral blood.127
Recently, a specific capillary subtype that supports perivascular osteoprogenitor differentiation by producing Nogging via Notch/Dll 4 signaling has been termed type H vessel, which express both CD31 and Endomucin at high levels. Type H vessels are surrounded by abundant osteoprogenitors (Osterix-positive cells) and are located both in the metaphysis, close to the growth plate, and in the diaphysis (periosteum and endosteum).128,129 During bone remodeling, the release of platelet-derived growth factor type BB (PDGF-BB) from preosteoclasts induces an increase in endothelial cell recruitment and assembly, with a subsequent rise in the number of type H vessels. Simultaneously, PDGF-BB triggers the recruitment of osteoprogenitors from vessels to the bone surface.130 The formation of H vessels is supported by the production of the slit homolog 3 (SLIT3) protein in osteoclasts,131 which also enhances H vessel branching.131–133
Type H vessels respond to the administration of intermittent anabolic PTH (iPTH), which promotes the detachment of leptin receptor-expressing (LepR+) cells, which are pericytes that can differentiate into osteoprogenitors,134 from CD31hi/Edmhi vessels. Pericyte migration contributes to the osteoprogenitor recruitment to the BRC during PTH-induced bone remodeling.135 Notably, anabolic responses to iPTH as well as sclerostin inhibitor treatments, decline with time,136 as it is conceivable that the precursor pool tends to be exhausted after major stimulation.
BLCs do not exclusively represent a final differentiation stage of the osteogenic line; they can also be osteoblast precursors.137 A study by Matic et al.137 led to the development of a model in which osteoclasts initiate osteoprogenitor cell expansion (see following section) by activating osteoprogenitor reservoirs located in proximity to the eroded bone surface consisting of BLCs, canopy cells and pericytes.120
Hence, BLCs favor the initiation of bone formation by supporting the recruitment of bone-forming osteoblasts from the canopy upon the release of osteoclastic factors supporting bone formation, independently of bone resorption (see following section). The osteoclast-canopy interface is therefore the physical site where the coupling of bone resorption to bone formation occurs.117
Osteoclasts
Resorbing osteoclasts: osteoclastogenesis and excavation of resorption lacunae
Osteoclasts are responsible for bone resorption, a process that is accomplished in a fairly short time relative to that required for bone formation. Osteoclasts originate from the hematopoietic monocyte-macrophage lineage, residing within the granulocyte-macrophage colony-forming unit. Osteoclastogenesis starts in the bone marrow upon the release of RANKL and macrophage colony-stimulating factor (M-CSF) from osteocytes and vascular endothelial cells close to the bone surface.138 It then extends toward the bone surface through the layer of BLCs along an “osteogenesis route”, likely guided by physical (i.e., collagen) and biochemical (i.e., sphingosine-1-phosphate, S1P) signals.139 In vitro experiments have shown that osteoclasts access bone surfaces by directly displacing the cells present on the bone surface.140 TGF-β1 is important for inducing cytoskeletal reorganization via the p38 pathway in osteoblastic cells, which elongate to generate cell-free areas.141 The inhibition of c-src and subsequent actin organization in osteoclast precursors prevent osteoclasts from migrating through the osteoblast layer.142 Metalloproteinase (MMP) inhibitors prevent both osteoblast elongation and the subsequent generation of cell-free areas143 and directly act on osteoclasts by preventing their migration through the cell layer.141 However, in osteoclasts, MMP inhibitors did not affect actin organization per sé,142 although they had been previously demonstrated to prolong the podosome lifespan in these cells.144 MMP inhibitor administration fully prevented osteoclast recruitment in the diaphysis core in vivo145 as well as osteoclast migration through collagen in vitro.146 Among MMPs, MMP-14 and MMP-9 seem to play a major role in osteoclast migration. MMP-14, also known as MT1-MMP, is expressed in all skeletal cells but is more abundant in osteoclasts.147 MT1-MMP-knockout (KO) mice usually die couple of months after birth, and display a severe phenotype that includes delayed ossification, unclosed sutures and unremoved cartilage.148 MMP-14 is highly expressed on osteoclast podosomes,149 and it digests interstitial collagen as well as other ECM molecules.150 MMP-9-KO mice showed reduced osteoclast invasion into the core of developing bones,151 and in vitro, osteoclasts lacking MMP9 did not migrate.152 However, very recently, it has been demonstrated that osteoclasts lacking either MMP9 or MMP14 alone (in this case conditionally deleted in the myeloid population) did not show altered fusion and function, or any defects in bone resorption. Only the deletion of both MMP9 and MMP14 generated a reduction in bone resorption areas and in type I collagenolysis activity.153
The fusion of the earliest osteoclast precursors into multinucleated, mature osteoclasts is a critical process in osteoclastogenesis, as the number of nuclei per cell determines osteoclast aggressiveness.154 The presence of distinct giant hypernucleated osteoclasts per sé in patients undergoing long-term treatment with nitrogen bisphosphonates (NBPs), as discovered by Weinstein et al.155 and confirmed by others,156 did not necessarily indicate an increase in osteoclast aggressiveness. These osteoclasts indeed showed decreased resorption competency and prolonged apoptosis characteristics. A recent study with transmission electron microscopy demonstrated that NBPs first induce osteoclast apoptosis and then the formation of newly differentiated osteoclasts that can anchor the bone surface but cannot form a clear zone or ruffled border.157 NPBs induce osteoclasts to acquire a nonresorbing phenotype by inhibiting c-Src, which is essential for cytoskeletal construction,158 and by stimulating dendritic cell-specific transmembrane protein (DC-STAMP),159 which is necessary for cell fusion.
Under physiological conditions, osteoclast fusion requires immobility and heterogeneity between fusion partners; fusion can only occur at the bone surface and must be completed for successful resorption.139 As reviewed elsewhere,160 heterogeneity is an integral feature of osteoclast fusion and may be related to the capacity of fusion precursors to adapt to specific bone microenvironments. Fusion also requires RANKL, which is highly expressed by BLCs;161 osteoblasts in the growing skeleton; and osteocyte arborizations that reach the bone surface in adults.51,52 sRANKL or mRANKL produced by osteogenic cells binds to RANK on osteoclast precursors to activate intracellular signaling of tumor necrosis factor receptor-associated factors (TRAFs), especially TRAF 2, 5, 6, which are adapter molecules that trigger NF-κB activation.162 NF-κBs are transcription factors that were originally discovered as regulators of B lymphocyte differentiation163 and that play important roles in innate and adaptative immune responses.164 Mice lacking both NF-κB 1 and 2 display, among other features, severe osteopetrosis165 due to an accumulation of osteoclast precursors.166 NF-κBs can activate canonical signaling and noncanonical signaling pathways in osteoclasts. Canonical NF-κB signaling activation is very fast, initiated within one hour of RANKL binding, and leads to the induction of NFATc1 expression.167 NFATc1 is a transcription factor that plays a master role in osteoclastogenesis168 by regulating the expression of osteoclast-specific genes such as cathepsin K, DC-STAMP, and tartrate-resistant acid phosphatase (TRAP) or that of osteoclast-associated receptor (OSCAR) and other genes involved in OC resorptive functions.169 The role of the Nf-κB noncanonical pathway in osteoclastogenesis is controversial. Global deletion of single molecules involved in the Nf-κB noncanonical pathway did not affect osteoclast numbers in vivo,170 whereas conditional deletion of TRAF3, an inhibitor of the noncanonical pathway, in osteoclast precursors resulted in increased osteoclast formation and bone resorption in mice.171
The discovery of a forward signaling induced by RANKL binding to its receptor RANK on osteoclast precursors led to the development of denosumab (DMAB), a human monoclonal antibody that binds RANKL and inhibits osteoclastogenesis. Recently, a second receptor for RANKL, the leucine-rich repeat-containing G protein-coupled receptor LGR4, was discovered on the osteoclast membrane. The extracellular domain of LGR4 binds RANKL and inhibits NFATC1 expression, thus blocking osteoclastogenesis.172 Very recently, a variant of RANKL with changes in a few amino acids in the RANK binding site was developed. This variant still activates LGR4 signaling and inhibits osteoclastogenesis. Moreover, it has been observed that this variant acts as an immunogen triggering the production of anti‐RANKL antibodies, and its use might reduce the risks linked to the abrupt suspension of denosumab use.173,70 The balance achieved among RANK, RANKL, OPG, and LGR4 fine tunes bone resorption in the bone remodeling process, and the pharmacological modulation of this balance has critical therapeutic potential in osteoporosis.172
In addition to RANKL/RANK, LGR4 and M-CSF signaling174 guiding and balancing the early steps of osteoclastogenesis, other factors act in concert to determine the osteoclastic mature cell phenotype, including β3-integrin,175 NR4A1,176 immunoreceptor tyrosine-based activation motif-containing proteins (ITAMs), DNAX-activating protein and the Fcγ receptor.177 Additionally, Toll-like receptors (TLRs) expressed on osteoclast progenitors178 promote differentiation toward the mature cell phenotype, as observed in inflammatory osteolytic diseases.179
WNT proteins such as Wnt5A in the noncanonical pathway have been outlined as key elements in osteoclastogenesis. WNT5a produced by osteoblasts supports osteoclastogenesis by stimulating RANK expression in osteoclast precursors,180 promoting osteoclast fusion,181 and supporting actin ring formation and bone resorption via c-Src.182 Since WNT5a enhances osteogenic pathway of Wnt/β-catenin activation in osteoblasts,183 it was thought that WNT5a produced by osteoblasts might affect both resorption and formation. However, recent studies have led to modifications of this previous assumption as they demonstrated that, after RANKL stimulation, osteoclast precursors also produce and secrete a unique phosphorylated form of WNT5A. Furthermore, deletion of this phosphorylated form of WNT5a in mature osteoclasts led to reduced bone formation in male mice.184 Hence, it is speculated that in the BRC, osteoblast WNT5a first supports osteoclastogenesis; then, as the osteoclast precursors differentiate, WNT5a expression increases, leading to the subsequent enhancement of osteoclast fusion and activity. In later stages, WNT5a production by mature osteoclasts fosters osteoblastogenesis because WNT5a cooperates with canonical Wnt signaling. The subsequent expansion of the osteoblast pool might therefore fulfill the resorption cavity at the proper time and space, suggesting that Wnt5a is a clastokine that maintains osteoclast–osteoblast coupling in physiological bone remodeling.
The cytoskeletal and membrane organization of osteoclasts characterizes their differentiation state. Mature osteoclasts are polarized cells with an apical membrane facing bone and an opposite basolateral membrane facing plasma. Both apical and basolateral membrane domains are essential structures for resorbing osteoclasts.185 Critical functional features of the apical membrane domain are the sealing zone and the ruffled border. The sealing zone establishes contact with the bone surface and delimits the resorption lacunae (i.e., Howship’s lacunae). The ruffled border membrane allows large vesicle transport, the delivery of hydrochloric acid (by vacuolar-type H + ATPase186) and chloride ion channel-7 (CLC-7),187 and the release of several lysosomal proteases, such as cathepsin K, TRAP, and MMPs.188 After endocytosis, the products derived from matrix degradation are transported through the cell within vesicles for further intracellular degradation and exocytosed on the opposite site through the secretory domain at the basolateral membrane.189 Thus, the osteoclasts never lose their tight attachment to the bone surface when resorption occurs. The interaction with the matrix is mediated by the integrin complex α5β3, which recognizes RGD motifs in proteins such as fibronectin,190 osteopontin (OPN)191 and bone sialoprotein.192 By binding to RGD motifs, the α5β3 complex is activated and clusters at the ruffled border,193 thus allowing the activation of focal adhesion complexes and the formation of the sealing zone during resorption.194 It has been hypothesized that integrin β3 contains two motifs with different affinities (high and low) for Ca2+ concentrations. A normal Ca2+ concentration in BEF maintains low-affinity domain activation, which does not maintain a strong attachment between β3 and RGD. When Ca2+ concentrations diminish, such as when osteocytes are injured, the high affinity site is the only one activated; this motif induces αvβ3 clustering, which allows osteoclasts to strongly adhere to the matrix and initiate bone resorption.195
The overall fate of osteoclasts (i.e., recruitment, differentiation, fusion and apoptosis, see below), is tightly controlled by the process coordinating bone remodeling, in which osteoclasts are also providers of multiple coupling signals196 for osteoblast formation.
Resorbing osteoclasts: the release of bone matrix factors
The bone ECM resorbed by osteoclasts contains inorganic and organic compounds. A growing body of evidence in ECM biology suggests that several organic proteins of the matrix regulate the quantum of BMU activity. While the only inorganic components of the ECM are apatite and trace elements, proteomic analysis have led to the identification of more than 100 organic ECM proteins,197 with collagen type I (Coll-1) and noncollagenous proteins (NCPs) being the major constituents. NCPs can bind growth factors, membrane receptors, and adhesion molecules, forming an intrinsic biochemical signaling network within each BMU. NCPs comprise several Gla proteins, including bone-Gla protein (i.e., Osteocalcin, OCN), matrix-Gla protein (MGP), protein-S, Gla-rich protein (GRP), periostin, and periostin-like factor (PLF), as reviewed elsewhere.198 In addition to OCN, whose hormonal effects were previously established in animal models,199 Gla proteins exhibit several functions supporting bone metabolism through γ-carboxylation-dependent and γ-carboxylation-independent mechanisms, ranging from the regulation of cell adhesion and activity to the modulation of calcium concentrations in the extracellular space. Gla proteins act in concert with glycoproteins such as osteonectin, thrombospondins and R-spondins, sialoprotein and matrix extracellular phosphoglycoprotein (MEPE) and DMP1 to control mineralization, synergistically with FGF23 and PHEX produced by osteocytes (see Lin et al.200 for review).
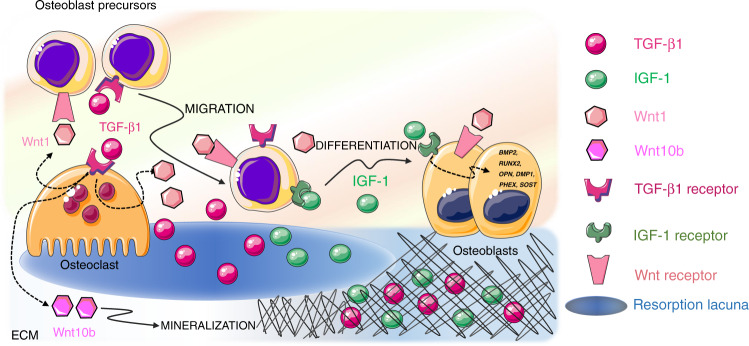
Two major factors released by the ECM influence bone remodeling and BMU activity: transforming growth factor-β (TGF-β) and insulin growth factor-1 (IGF-1). Together, TGF-β and IGF-1 influence the recruitment and differentiation of osteoblast lineage cells (Fig. 4), favor bone matrix mineralization, and regulate osteoclast activity. For these reasons, they are acknowledged as “coupling factors”.
Fig. 4.
Released extracellular matrix (ECM) factors. Two major factors are released by the ECM upon bone resorption and cooperate to regulate bone remodeling and BMU activity: TGF-β1 and IGF-1. After release from the matrix, active TGF-β1 acts both on osteoblasts and osteoclasts to induce osteoblast precursor migration to the site of resorption and osteoclast production of Wnt1, which promotes osteoblast recruitment and/or differentiation at sites of bone resorption, and Wint10b, which promotes matrix mineralization. IGF-1 supports the recruitment of osteoblast progenitors and promotes osteoblast differentiation and matrix mineralization by inducing the transcription of osteogenesis‐related genes such as DMP1, PHEX, SOST, BMP2, RUNX2, OPN, and OCN
TGF-β
TGF-β1 is one of the most abundant cytokines in the bone matrix.201 TGF-β1, which is a member of the TGF superfamily that includes bone morphogenetic proteins (BMPs), binds to specific TGF receptors (TGFR1-2) in osteoblasts, where it activates the synthesis of collagen and the expression of RUNX2, a master transcription factor regulating osteoblast proliferation and differentiation. TGF-β1 release and activation, resulting from the activity of metalloproteinases and interaction with integrins, are prerequisites for the exertion of TGF-β1 effects on bone cells. This occurs during bone resorption since osteoclasts lower the pH in resorption lacunae and secrete cathepsin K, thus releasing and activating TGF-β1.202 When osteoclasts actively resorb bone, TGF-β1 is released in the lacunae, thus playing a crucial role in the balance between bone formation and resorption. First, active TGF-β1 induces osteoblast precursor migration to the site of resorption203 without affecting the differentiation of cells.204 Since TGF-β1 alone is not able to promote osteoblast differentiation,205 cooperative pathways need to be activated to foster an osteogenic environment at resorption surfaces within the BRC. A cooperation pathway is provided by the osteoclast itself. In addition to activating and releasing TGF-β1 from the bone matrix, osteoclasts express specific receptors for TGF-β1. Osteoclastic TGF-β1 receptor signaling stimulates the production of Wnt1, which promotes osteoblast recruitment and/or differentiation at sites of bone resorption. Since impaired TGF-β1 receptor signaling in osteoclasts has detrimental effects on bone mass in mouse models, it is likely that the release of Wnt1 constitutes a coupling pathway.206 Moreover, TGF-β1 favors RANKL production in osteoblast precursors by inducing TRAF3 degradation. The expression of TRAF3, which is an inhibitor of noncanonical Nf-κB signaling, in osteoblast precursors favors the stabilization of β-catenin and, therefore, their differentiation into mature osteoblasts. In the absence of TRAF3 expression, Nf-κB noncanonical signaling is activated with an increase in RANKL production and therefore is associated with osteoclastogenesis.207 With matrix resorption progression, the concentration of TGF-β1 increases, and TGF-β1 activates a negative feedback loop in osteoclastogenesis. High TGF-β1 expression inhibits the migration of osteoclast precursors208 by suppressing RANKL expression and by stimulating OPG production in osteoblasts.209 A reduced RANKL/OPG ratio indeed results in reduced osteoclastogenesis. In the absence of osteoclast survival factors such as RANKL, TGF-β1 leads to osteoclast apoptosis via the upregulation of Bim expression.210 This proapoptotic effect of TGF-β1 on osteoclasts is consistent with the crucial role it plays in the reversal of bone resorption to bone formation. Indeed, TGF-β1 release enhances Wnt10b expression and secretion to stimulate osteoblast-directed mineralization. TGF-β1 therefore has a dual effect on osteoblasts by directly recruiting their progenitors to the bone surface and by indirectly promoting matrix mineralization through osteoclast-derived Wnt10b.211
IGF1
IGF-1 is the most abundant growth factor deposited in the bone ECM.212 Osteocytes in particular secrete large amounts of IGF1, which is incorporated in the bone matrix.213 Since IGF-1 is produced under loading, it might contribute to the mechanotransduction process.214 Whether released by cell secretion or bone ECM degradation, IGF1 is a local autocrine/paracrine regulator of bone remodeling and does not contribute to the circulating IGF-I pool. IGF-1 acts primarily as a migratory signal and as a differentiation factor for osteoblast precursors, rather than as a proliferation factor. IGF-1 recruits progenitor cells of the osteoblastic lineage215 and promotes osteoblast differentiation and matrix mineralization by upregulating the osteogenesis‐related genes DMP1, PHEX, SOST, BMP2, RUNX2, OPN, and OCN.216 Moreover, IGF-1 released from the bone matrix during bone resorption establishes an osteogenic microenvironment by activating mechanistic target of rapamycin (mTOR) signaling,217 which is critical for cellular energy metabolism and cell migration.218 Recent studies have confirmed that IGF-1-dependent activation of mTOR induces human dental pulp stem cell (DPSC) differentiation toward an osteoblastic phenotype.219
Since TGF-β1 and IGF1 do not remain accessible long enough to affect the complete refilling of the resorption cavity,220 their action might be limited to the early phases of remodeling, when osteoclasts are still actively resorbing the bone matrix.
Anabolic osteoclasts: a bridge from bone resorption to formation
The resorption of the bone ECM is necessary, but not sufficient, to induce the stimulus provided by osteoclasts to osteoblasts during remodeling. Currently, available evidence indicates that osteoclasts can support bone formation independent of their resorption activity. The paradoxical concept of “anabolic osteoclasts” was articulated after the original observation that human osteoblasts exposed to conditioned media from human osteoclasts increased bone nodule formation.221 The finding that the transplantation of nonfunctional osteoclasts in irradiated skeletally mature 3-month-old wild-type mice induced a high trabecular bone volume, increased bone strength, and an increased bone formation rate in trabecular bone222 supports this concept. The anabolic role of osteoclasts can be observed in both humans and mice with osteoclast-rich osteopetrosis (OPT), a disease resulting from mutations of either the V-ATPase subunit or the ClC-7 chloride channel that abrogate the osteoclastic acidification process, which is essential for resorption activity. Under these conditions, no factors stored in bone were released from the unresorbed bone matrix, but the long-surviving osteoclasts, fused into large abnormal multinucleated cells, provided an osteogenic milieu.223 In fact, in models of osteoclast-rich OPT, bone formation is maintained or enhanced despite the impairment of resorption activity,224 thus providing evidence that nonresorbing osteoclasts promote/maintain bone formation. Findings following the pharmacologic blockage of cathepsin K in osteoclasts (Odanacatib) are in line with this view. In patients treated with Odanacatib, although osteoclast bone resorption was impaired, the osteoclast number was increased to be more than twofold higher than that after placebo treatment by month 60, and bone formation, after a transient reduction, was maintained.225
In contrast to “osteoclast-rich” OPT, active bone formation is lacking in “osteoclast-poor” OPT (due to TNFRSF11A mutations226) or dysosteosclerosis (DSS) (an OPT of unknown etiology227). Indeed, bone histomorphometric analysis showed no linear single or double tetracycline labels under these conditions.
Therefore, these “anabolic osteoclasts” might produce a pool of signals that activate bone formation and that can be a) released into the BRC, b) shuttled to osteoblasts, and c) transferred by receptor binding.
Information released into the BRC
Several osteoclast-derived factors released into the BRC have been identified and validated in genetically modified mouse models. These factors include cardiotrophin-1 (CT-1),228 S1P,229 Wnt10B, BMP6,230 collagen triple helix repeat-containing 1 (CTHRC1),231 complement factor 3a (C3a),232 and leukemia inhibitory factor (LIF).233 However, not all of these identified factors are responsible for coupling in bone remodeling, nor are they produced only by osteoclasts due to macrophage contamination in vitro and the presence in vivo of immunocompetent cells within the remodeling compartment. Whether these factors exhibit similar effects in humans remains unclear; however, a recent study shed some light on this controversy. Bone biopsy samples taken from postmenopausal women treated with DMAB were analyzed by RNA sequencing, and the results were compared to those obtained from bone biopsy samples of untreated subjects. The comparison revealed potential osteoclast-derived coupling factors in humans: LIF, CREG2, CST3, CCBE1, and dipeptidyl peptidase-4 (DPP4), a highly conserved cell surface peptidase. The reduction in osteoclast-derived DPP4 in the DMAB-treated group was associated with a significant increase in glucagon-like peptide-1 (GLP)−1 in the serum compared to that in the placebo-treated group, suggesting that DPP4, in addition to its function as a coupling factor, might constitute a potential link between bone remodeling and energy metabolism.234
Mature human osteoclasts also secrete SLIT3, a chemorepellent originally identified as a regulator of axon crossing in the brain. Osteoclast-derived SLIT3 stimulates the migration and proliferation of osteoblast lineage cells via the activation of β-catenin and suppresses osteoclastogenesis in an autocrine manner.131 SLIT3 contributes to the initial establishment of the osteogenic environment after resorption and meets the requirements to be considered a coupling factor, as i) SLIT3 production increases during osteoclast differentiation and ii) SLIT3 is necessary for osteoblast precursor migration.235 Considering that bone greatly contributes to SLIT3 levels in plasma, SLIT3 might be considered a novel biomarker of bone turnover and a candidate for the treatment of osteoporosis because it plays active roles in both bone resorption and formation through its opposite effects.
Information shuttled to osteoblasts
The coupling of osteoclasts to osteoblasts and related functions involve not only the secretion of factors in the BRC but also the production of specific EVs, released by bone cells. EVs have emerged as important intercellular regulators since they function as messengers from osteoclasts to osteoblasts, and vice versa.236
EVs exhibit an evolutionary advantage over the paracrine pathway activated by released factors because they can protect their message (mRNAs and proteins, including cytokines, etc.) from degradation and might therefore play critical roles in fine-tuning bone remodeling.
Osteogenic cells trigger hematopoietic precursor differentiation into osteoclasts by secreting RANKL. In addition, through a less-characterized mechanism, osteoclasts stimulate osteoblasts using the same RANKL–RANK pathway acting in reverse mode; that is, RANKL acts as the receptor. In fact, osteoclasts release EVs (between 25 and 120 nm in diameter) that carry RANK. These vesicles were initially thought to be negative paracrine regulators of osteoclastogenesis.237 However, a recent study demonstrated that vesicular RANK binds to RANKL on the osteoblast surface (and possibly on osteocytes) and triggers the mTOR-dependent stimulation of Runx2238 (Fig. 5). This finding suggests a previously unknown scenario in which actively resorbing osteoclasts promote the differentiation of neighboring osteoblast precursors into mature bone-forming cells. The physiological importance of the messages shuttled by EVs has been confirmed by the observation that osteoblasts do not efficiently deposit bone ECM when RANKL reverse signaling is suppressed.238
Fig. 5.
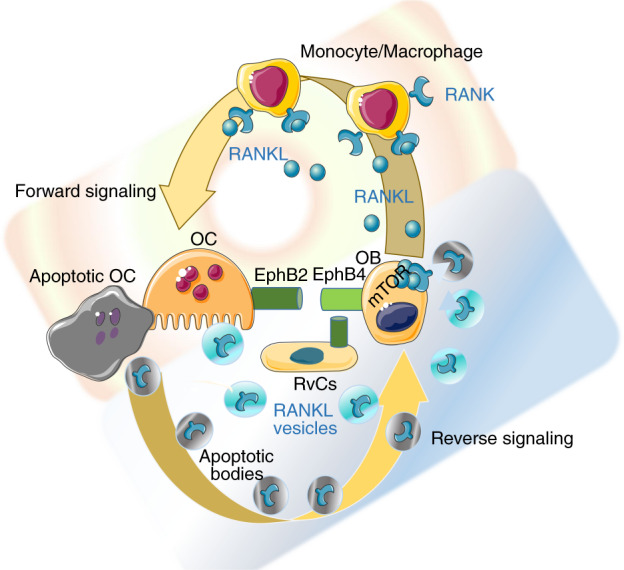
Anabolic osteoclasts. Osteoblasts stimulate osteoclastogenesis by producing RANKL as a forward signal. However, osteoclasts can act as anabolic cells by generating positive reverse signaling in osteoblasts. Both resorbing and apoptotic osteoclasts can release extracellular vesicles (EVs) that contain RANK. Once discharged from EVs, RANK binds RANKL clusters on the osteoblast membrane and activates osteogenesis via the mTOR pathway. In addition, EphrinB2 signaling from osteoclasts to EphB4 on osteoblasts/bone lining cells (BLCs)/reversal cells favors osteogenic differentiation
The discovery of the reverse signaling induced by RANK on osteoclasts binding to RANKL on osteoblasts indicates new pharmacological possibilities. Interestingly, the administration of a specific peptide, W9, to prevent RANKL-RANK signaling has been shown to exert a bone anabolic effect in vivo by inducing uncoupling.239 Therefore, DMAB may activate RANKL reverse signaling,240 explaining the continuous increase in bone mineral density (BMD) observed at the 10-year follow-up of DMAB-treated individuals.241 However, experimental evidence supporting the hypothesis of the bimodal effects of DMAB on RANKL-RANK signaling during bone remodeling is lacking because remodeling-based bone formation is severely suppressed in the femur of DMAB-treated subjects.242 It is more likely that DMAB blocks RANKL expressed on bone marrow mesenchymal stem cells (BMSCs),243 through which it negatively regulates osteogenic differentiation.244 According to a hypothesis suggested by Wang et al.,243 the DMAB-related abrogation of RANKL-induced inhibition of osteoblast precursors might underlie the activation of modeling-based bone formation242 and sustain the increase in BMD over time, as previously observed.241
RANKL monomers expressed on osteoblasts are not activated by RANK238 or by OPG, as indicated by the deletion of RANK or OPG failing to reduce bone formation.245 In contrast, the multimeric assembly of RANKL can activate reverse signaling. In fact, OP3-4, a RANKL-binding peptide that induces the clustering of RANKL on the cell membrane, induces the activation of RANKL reverse signaling.246 RANKL clustering on early osteoblasts may therefore be required for the activation of RANKL reverse signaling in resorption lacunae, similar to the effect of shuttling RANK in osteoclast EVs during bone remodeling (Fig. 5) or that of an anti-RANKL antibody-containing leucine zippers, which induce trimer formation.238
Some of the exosomes released by osteoclasts at the end of the two-week cell life span contribute to signal transfer during remodeling. In fact, apoptotic osteoclasts produce large amounts of apoptotic bodies. Apoptotic bodies are subcellular membrane-bound EVs containing fragments of nucleus, endoplasmic reticulum and mitochondria that assemble in a random manner and are involved in intercellular crosstalk.247 Osteoclast-derived apoptotic bodies contain osteoclast differentiation factors, such as RANK and RANKL (Fig. 5). In contrast, osteoblast-derived apoptotic bodies contain specific osteogenic factors, such as BMPs, OPN, OCN and bone ALP (BALP). By mapping the whole-proteome signatures of osteoclast-derived apoptotic bodies, the apoptotic bodies content was confirmed to be consistent with that of their parent cells in terms of both proteome signatures and biological functions.248 During remodeling, osteoclast-derived apoptotic bodies containing miR-214-3p are delivered to osteoblasts and serve as intercellular messengers that inhibit osteoblast differentiation and subsequent bone formation.249 Recently, the roles of osteoclast-derived apoptotic bodies have been more precisely characterized, and their effects have been found to be determined by the differentiation state of parental cells.250 For example, apoptotic bodies derived from mononuclear preosteoclasts undergoing apoptosis deliver PDGF-BB to recipient endothelial progenitor cells (EPCs), and since PDGF-BB is a proangiogenic factor,130 preosteoclast derived apoptotic bodies promote angiogenesis. However, apoptotic bodies derived from multinucleated mature osteoclasts promote osteogenesis via RANKL reverse signaling.
Therefore, in addition to well-studied osteoclast–osteoblast coupling, the involvement of osteoclast-derived apoptotic bodies promotes the transition from bone resorption to formation during bone remodeling. Although the mechanism by which apoptotic bodies delivery is controlled within each BMU is unclear, mature osteoclasts derived apoptotic bodies further connect the disappearance of osteoclasts from resorption lacunae with the incoming osteogenic process involving osteoblast recruitment, migration and differentiation, contributing to the reversal of cellular activity in reverting from bone resorption to bone formation.
Information transferred by receptor binding
The communication route between osteoclasts and osteoblasts involves a bidirectional signaling pathway mediated by EphrinB2‐EphB4 that links the suppression of osteoclastogenesis to osteogenesis within each BMU.251 EphrinBs are transmembrane proteins with cytoplasmic domains that are preferential ligands for the tyrosine kinase receptor EphB. EphrinB2 expression in osteoclasts is associated with RANKL-induced osteoclast differentiation, whereas EphB4 is constitutively expressed in osteoblasts. Signaling from EphrinB2 in mature osteoclasts to EphB4 in osteoblast precursors stimulates osteogenic differentiation (Fig. 5), whereas signaling from EphB4 in osteoblasts to EphB2 in osteoclasts inhibits the differentiation of osteoclast precursors. EphrinB2–EphB4 bidirectional signaling must function locally and requires direct cell‐cell contact since both receptors are anchored to the cell membrane, as shown with goldfish scale model of bone remodeling.252 In humans, the role of EphrinB2 and EphB4 in bone remodeling has been debated because osteoclasts actively resorbing bone, and osteoblasts forming bone do not directly get in contact in the BRC. As a result the cell–cell interaction mediated by EphrinB2 and EphB4 might be limited to the precursor stage, when osteoclastogenesis and osteoblastogenesis are simultaneously regulated, or (as suggested previously253) to the mature osteoclast stage, in which direct contact is realized with the BLCs surrounding the canopy. Under PTH1R activation, EphrinB2 expressed on osteoclasts has been suggested to affect EphrinB4 on the osteoblast/BLC surface to induce osteoblast commitment and promote osteoblast differentiation.254
Intermediate cell phenotypes: osteomorphs and reversal cells tuning and coupling bone remodeling
The orderly genesis and apoptosis of both osteoclasts and osteoblasts are essential for physiological bone homeostasis during bone remodeling. Possible intermediate phenotypes may be appropriate targets for coupling factors by providing a temporal connection between osteoclasts and osteoblasts. In the traditional view, osteoclasts were thought to live for two weeks11 before undergoing apoptosis; it was therefore assumed that during bone remodeling, the osteoclast resorption phase within a single BMU was temporally limited by the osteoclast life span, ending with the completion of its bone-resorbing activity. However, the observation that osteoclasts can survive longer by fusing with circulating monocytes with access to BRC255 has challenged this view. While osteoclast apoptosis is a rare event requiring high energy expenditure for the removal of the apoptotic debris, osteoclast disassembly into smaller unresorbing cells, which can revert to functional osteoclasts when needed, is a more efficient process. Two observations support the latter view: first, primary osteoclasts have been identified at the cutting cone and secondary osteoclasts have been shown to establish a functional link with reversal cells (Figs. 1 and 3) as focal bone remodeling progresses within a single BRC,256 and second, osteoclasts have recently been shown to be recycled into osteomorphs. Osteomorphs have been described as highly motile osteoclast daughter cells that remain in the adjacent bone marrow and retain the ability to fuse back into functional osteoclasts.257
The discovery of a transient cell stage of osteoclasts (i.e., the osteomorph) that can undergo phenotype reversion, analogous to what occurs in osteoblasts (i.e., BLCs), implies the presence of two reacting components of the BMU that can rapidly adjust the operational process of bone remodeling. This implication is clinically relevant to osteoporosis therapy. For example, BLCs can react to PTH exposure by quickly reverting to osteoblasts and thus expand the osteoblastic pool258 to fill resorption lacunae, similar to process in the “anabolic window” after teriparatide and abaloparatide administration.259 Similarly, exposure to RANKL might allow osteomorphs to rapidly fuse and recycle back into functional osteoclasts. Since RANKL inhibition by DMAB results in osteomorph accumulation,257 the reconstitution of RANKL signaling, as occurs upon DMAB discontinuation, can activate massive bone resorption over a very short time scale, leading to rebound fractures.260 This rebound effect is not fully inhibited by bisphosphonate therapy,261 probably because osteomorphs first accumulate at bone sites and are thus not accessible to potent bisphosphonate treatment. After osteoclasts are no longer active and disappear, the Howship’s lacunae remain covered with undigested nonmineralized collagen matrix. Mononucleated cells colonize these eroded surfaces (ESs), covering 80% them.262 These cells, called reversal cells,263 lack specific cell identification markers. The available literature has identified the cells appearing at the resorption lacunae as osteoclasts264 or, more recently, as osteoblasts.265 Indeed, the reversal cells express osteoblast lineage cell markers such as Runx2, ALP, and Col3, but not TRAcP or CatK.265 Indeed, reversal cells express osteoblast markers such as Runx2, ALP, and Col3 but not TRAcP or CatK.265 Abdelgawad et al.266 showed that the immunoreactivity of these cells for osteoclast-derived TRAcP is attributable to TRAcP taken up by osteoblast lines from neighboring osteoclasts and does not represent the acquisition of an osteoclastic phenotype. Moreover, Abdelgawad et al.266 observed that early reversal cells, located in close proximity to resorbing osteoclasts and forming direct cellular contacts with neighboring osteoclasts through short cytoplasmic extensions, are osteoblast progenitors with the capacity to digest fibrillar collagen remnants, similar to BLCs.113 In particular, reversal cells have been shown to be distributed among osteoclasts in the resorption surface far from the pockets of osteoclasts at the cutting cone tip. New resorption events might occur after the primary excavation of the resorption cavity/canal when reversal cells have colonized ES.256 In contrast, osteoclasts have never been observed at the bone formation wall, suggesting that bone resorption continues until bone formation takes place. Lassen et al.’s256 findings indicate that a pure reversal period, as commonly depicted following a halt in resorption,8 does not take place. In contrast, it is conceivable that the expanded pool of reversal cells, initially interacting with bystander osteoclasts in the same time and space, gradually switch off further resorption and form an osteogenic environment, activating bone formation later, when osteoclasts are completely absent.
The dynamic events described here support the view that the operational process of bone remodeling is a continuous physiological entity. All events, from the formation of the bone remodeling compartment with canopy cells to the colonization of a reversal zone by reversal cells in the early period of bone remodeling, generate the environment necessary for the recruitment and expansion of the osteoblast pool and subsequent refilling of resorption lacunae (Fig. 3).
The osteoblastic cells pool: recruitment, expansion and osteocytogenesis
Osteoblasts are cuboidal-shaped cells on bone surfaces. Osteoblasts have traditionally been considered the cell responsible for the production of the organic components of the bone matrix and its consequent mineralization because they synthetize and secrete matrix components such as collagen type I, OCN, osteonectin, bone sialoprotein, OPN, proteoglycans, and ALP.267 In vivo, a set of osteoblasts, all with similar morphologies, lay down osteoid on active bone-forming surfaces.268 The dense endoplasmic reticulum of these cells indicates high synthetic activity, and the extensive contacts among these osteoblasts, osteocytes and BLCs indicate their extensive intercellular connections.269
Marotti et al.270 hypothesized that in human bone physiology, osteoblasts can participate in two different types of osteogenesis: static and dynamic osteogenesis. Static osteogenesis occurs in the mesenchymal tissue to initiate intramembranous ossification to generate primary trabecula during growth. This osteogenesis type is thus independent of the loading environment and will be subject to later osteoclast resorption. Static osteogenesis involves stationary osteoblasts, which are pluristratified and polarized in all directions. These osteoblasts differentiate into osteocytes in the exact same site where they had been originated from the mesenchymal precursors.271 Dynamic osteogenesis takes place to thicken the primitive trabeculae generated in the context of static osteogenesis, and it is therefore the type of osteogenesis activated in response to metabolic and mechanical demand. The osteoblasts participating in dynamic osteogenesis are arranged in an epithelial-like manner within a single cell layer. They all are polarized in the same direction, and they maintain contacts with osteocytic dendrites as they move from the mineralization front toward the vascular surface.271 In the adult skeleton, physiological bone remodeling involves only dynamic osteogenesis, which refill resorption lacunae.
Osteoblastic cells contribute not only to osteogenesis but also to osteoclastogenesis by producing RANKL. The same osteogenic cells may accomplish this dual function at different stages of maturation. Immature osteoblasts respond to bone regulatory factors in a pro-osteoclastogenic manner, but during the maturation process, they lose RANKL expression and do not support osteoclastogenesis.272 Moreover, as cells mature, they secrete more ECM and exert local inhibitory control over osteoclastogenesis by releasing the osteoclastogenic inhibitor OPG.77 Osteoblasts are considered the major sources of OPG in cancellous bone, acting in concert with osteocytes and other cells to modulate the RANKL/RANK ratio and reduce resorption by osteoclasts. This inhibitory activity is mandatory for the correct shift from bone resorption to bone formation and protects newly formed bone against untimely resorption.77 Cawley’s study stressed the concept “that the local concentration of OPG near the cell surface is a key factor in its ability to block the activity of RANKL”.
The osteoblast lineage derives from the differentiation of mesenchymal cells in the stromal compartment of bone marrow (BM). The bone marrow stroma contains self-renewing, multipotent progenitors that can give rise to osteoblasts, thus ensuring a reservoir of bone-forming cells for bone growth, modeling and remodeling.273 Anatomically, the BM stroma is part of the skeleton and is present in all bones except auditory ossicles, which therefore do not undergo remodeling.274 The definition of skeletal stem cells and their physiological significance and terminology associated with them have been debated.273–275 A self-renewing stromal progenitor, originally referred to as an “osteogenic” or “stromal”/”stem” cell (BMSC), corresponds to a specific type of perivascular cell in mammalian bone marrow. The characterization of pericytes as multipotent progenitors is evolving. Nevertheless, Sacchetti et al.276 pointed out that only BM vessel-residing cells defined as pericytes have the ability to differentiate into osteoblasts during physiological bone remodeling. Since tissue-specific mesodermal progenitors show tissue-specific commitments in vivo, the native skeletogenic potential is thus intrinsic to the progenitor/stem cell set found in the skeleton.277
Upon the initiation of bone remodeling, as previously discussed, the formation of BRCs by BLCs/canopy cells establishes a direct connection with the vascular sinus closely covering bone-forming surfaces, allowing pericyte detachment and differentiation toward the osteogenic phenotype.
Cells with true osteogenic potential can also circulate.278 Cells with multiple potential differentiation routes similar to those of BMSCs can enter the circulation, and although the mechanism by which they enter the circulation is unclear, they circulate in physiologically significant numbers, correlate with markers of bone formation and increase during bone growth.127 Characterization of these cells deserves further study, and circulating skeletal progenitors might form an additional pool of osteoblast precursors for bone remodeling and/or tissue repair. In fact, fractures result in the mobilization of mesenchymal osteogenic progenitors into the circulation to promote fracture healing, even in very old patients.279 Although circulating osteoprogenitor fate and function are determined by the homing of these cells to focal sites and their exposure to microenvironment signaling,280 their presence per sé in the blood has important implications for regenerative medicine.281
The average lifespan of active osteoblasts is 3 months.4 When bone matrix formation ends and the subsequent matrix mineralization process completes the primary phase, mature osteoblasts undergo three possible fates. Between 60% and 80% of osteoblasts at resorption lacunae die via apoptosis.282 Cells at all differentiation stages undergo apoptosis, which continues throughout the osteoblast life span and is regulated by Wnt signaling, PTH and mechanical stimulation.61 Osteoblast apoptosis is key to regulating the extent and duration of bone formation and is the target of catabolic and anabolic regulatory factors affecting bone mass. Apoptosis exerts a significant effect on the number of osteoblasts producing bone matrix at a bone formation site.283 The balance between the expression of proapoptotic factors Bim and Bak and the prosurvival factor Bcl determines the osteoblast life span and, therefore, bone volume and strength.284 Estrogens and androgens also exert effects on bone cell life span. In particular, they exert antiapoptotic effects on osteoblasts and osteocytes and proapoptotic effects on osteoclasts. Interestingly, estrogen receptors or the androgen receptor can transmit antiapoptotic signals with similar efficiency, regardless of whether the ligand is an estrogen or an androgen.285 p53, a potent tumor suppressor, is also critically involved in determining osteoblast life span, as it induces apoptosis, inhibits osteoblast proliferation and stimulates osteoblast differentiation through the Akt–FoxOs pathway286 to regulate bone remodeling.287
The remaining osteoblasts (those on the bone trabecular endosteal and endocortical surfaces) might differentiate into BLCs, which are characterized by lower biosynthetic activity and a flat morphology, or they might remain embedded in the matrix, undergo the active process of osteocytogenesis,288 and become osteocytes (5%–20% of mature osteoblasts). Osteocytogenesis requires proteolytic activity to deepen the osteoid. Collagenase-resistant type I collagen in the bone matrix increased the osteocyte apoptosis rate.289 Additionally, the deletion of the metalloproteinase MT-MMP1 generated an altered osteocytic network in mice.290 Osteocytogenesis requires cytoskeleton plasticity to form dendrites (dendrogenesis). Although the entire dendrogenesis process has not yet been elucidated, one factor known to be necessary in the dendrogenesis of osteoid osteocytes (the late osteoblast/early osteocyte that undergoes the transition to mature osteocytes288) is E11/gp38 or podoplanin (Pdpn), a transmembrane glycoprotein. The conditional deletion of PDNP in mice generated a decreased number and length of osteocyte processes.291 Recently, it has been shown that SP7 (Osterix) is also necessary to support dendrogenesis because it regulates Osteocrine.292
With the progression of osteocytogenesis, osteoid osteocytes start expressing specific cytoskeletal markers (fimbrin and destrin) and factors for mineralizing the surrounding matrix (Phex and MEPE) until they become mineralizing osteocytes (expressing Dmp1). The cell terminally differentiate into mature osteocytes producing SOST and FGF23.288
The differentiation of osteoblasts into osteocytes at the end of the bone remodeling process is essential to reestablish mechanical competence. Therefore, 9.1 million osteocytes are replaced daily during bone remodeling.16 Hence, osteocytes can be considered dynamic cells capable of reconstituted mechanical sensitivity after replacement293 as well as the inhibitory control over osteoclastogenesis via the local production of OPG.77
Conclusions: bone remodeling as a continuous flow of information and connected events
Current evidence on bone remodeling has indicated the complexity of this process by showing how events and effectors are connected and coordinated to ensure the removal of old bone and maintain bone mechanical competence. Recent findings have shown that bone remodeling is a physiological process consisting of continuous operations with fast reactive components that confer survival advantage. After BRC formation, local coordinating factors and events, acting in concert in time and space and responding to metabolic and mechanical regulators, affect the final quantum of BMU activity. This complete picture overwrites the classical view of bone remodeling organized in discrete stages. The current knowledge indicates that each BMU component is critical for different mechanisms depending on the specific differentiation stage of the cell. All the signals discussed in the present review affect the remodeling process. The outcome depends on the cells generating the stimulus, and the way in which the stimulus is transferred. Understanding how the events determining the focal balance between bone resorption and formation unfold within each BMU provides necessary biological background information that will help to better identify targets of therapeutic approaches to osteoporosis.
Acknowledgements
We thank Springer Nature Author Services for providing highly professional editing.
Competing interests
The authors declare no competing interests.
References
- 1.Frost, H. M. Bone remodeling dynamics (Charles C Thomas Company, 1963).
- 2.Delaisse JM, et al. Re-thinking the bone remodeling cycle mechanism and the origin of bone loss. Bone. 2020;141:115628. doi: 10.1016/j.bone.2020.115628. [DOI] [PubMed] [Google Scholar]
- 3.Maggiano CM, Maggiano IS, Tiesler VG, Chi-Keb JR, Stout SD. Methods and theory in bone modeling drift: comparing spatial analyses of primary bone distributions in the human humerus. J. Anat. 2016;228:190–202. doi: 10.1111/joa.12383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Parfitt AM. Osteonal and hemi-osteonal remodeling: the spatial and temporal framework for signal traffic in adult human bone. J. Cell. Biochem. 1994;55:273–286. doi: 10.1002/jcb.240550303. [DOI] [PubMed] [Google Scholar]
- 5.Frost HM. A synchronous group of mammalian cells whose in vivo behavior can be studied. Henry Ford. Hosp. Med. Bull. 1965;13:161–172. [PubMed] [Google Scholar]
- 6.Feynman, R., Leighton, R. & Sands, M. The Feynman lectures on physics (Addison-Wesley Pub. Co., 1964).
- 7.Parfitt AM. The cellular basis of bone remodeling: the quantum concept reexamined in light of recent advances in the cell biology of bone. Calcif. Tissue Int. 1984;36:S37–S45. doi: 10.1007/BF02406132. [DOI] [PubMed] [Google Scholar]
- 8.Eriksen EF. Normal and pathological remodeling of human trabecular bone: three dimensional reconstruction of the remodeling sequence in normals and in metabolic bone disease. Endocr. Rev. 1986;7:379–408. doi: 10.1210/edrv-7-4-379. [DOI] [PubMed] [Google Scholar]
- 9.Parfitt AM. The quantum concept of bone remodeling and turnover: implications for the pathogenesis of osteoporosis. Calcif. Tissue Int. 1979;28:1–5. doi: 10.1007/BF02441211. [DOI] [PubMed] [Google Scholar]
- 10.Marais A, et al. The future of quantum biology. J. R. Soc. Interface. 2018;15:20180640. doi: 10.1098/rsif.2018.0640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Manolagas SC. Birth and death of bone cells: basic regulatory mechanisms and implications for the pathogenesis and treatment of osteoporosis. Endocr. Rev. 2000;21:115–137. doi: 10.1210/edrv.21.2.0395. [DOI] [PubMed] [Google Scholar]
- 12.Jilka RL. Biology of the basic multicellular unit and the pathophysiology of osteoporosis. Med. Pediatr. Oncol. 2003;41:182–185. doi: 10.1002/mpo.10334. [DOI] [PubMed] [Google Scholar]
- 13.Parfitt AM. Misconceptions (2): turnover is always higher in cancellous than in cortical bone. Bone. 2002;30:807–809. doi: 10.1016/S8756-3282(02)00735-4. [DOI] [PubMed] [Google Scholar]
- 14.Bonewald, L. F. & Marcus, D. F. R. In Osteoporosis 3rd edn (eds Nelson, D. & Rosen, C.) 170–189 (Elsevier, 2008).
- 15.Metz LN, Martin RB, Turner AS. Histomorphometric analysis of the effects of osteocyte density on osteonal morphology and remodeling. Bone. 2003;33:753–759. doi: 10.1016/S8756-3282(03)00245-X. [DOI] [PubMed] [Google Scholar]
- 16.Buenzli PR, Sims NA. Quantifying the osteocyte network in the human skeleton. Bone. 2015;75:144–150. doi: 10.1016/j.bone.2015.02.016. [DOI] [PubMed] [Google Scholar]
- 17.Marotti G, Palumbo C. The mechanism of transduction of mechanical strains into biological signals at the bone cellular level. Eur. J. Histochem. 2007;51:15–19. [PubMed] [Google Scholar]
- 18.Tiede-Lewis LM, et al. Degeneration of the osteocyte network in the C57BL/6 mouse model of aging. Aging. 2017;9:2190–2208. doi: 10.18632/aging.101308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lecanda F, et al. Connexin43 deficiency causes delayed ossification, craniofacial abnormalities, and osteoblast dysfunction. J. Cell Biol. 2000;151:931–944. doi: 10.1083/jcb.151.4.931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chung DJ, et al. Low peak bone mass and attenuated anabolic response to parathyroid hormone in mice with an osteoblast-specific deletion of connexin43. J. Cell Sci. 2006;119:4187–4198. doi: 10.1242/jcs.03162. [DOI] [PubMed] [Google Scholar]
- 21.Zhang Y, et al. Enhanced osteoclastic resorption and responsiveness to mechanical load in gap junction deficient bone. PLoS One. 2011;6:e23516. doi: 10.1371/journal.pone.0023516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Green J. Role of bone in regulation of systemic acid-base balance. Miner. Electrolyte Metab. 1994;20:7–30. [PubMed] [Google Scholar]
- 23.Bushinsky DA, Chabala JM, Levi-Setti R. Ion microprobe analysis of mouse calvariae in vitro: evidence for a “bone membrane”. Am. J. Physiol. Endocrinol. Metab. 1989;256:E152–E158. doi: 10.1152/ajpendo.1989.256.1.E152. [DOI] [PubMed] [Google Scholar]
- 24.Bushinsky DA, Gavrilov K, Chabala JM, Featherstone JD, Levi-Setti R. Effect of metabolic acidosis on the potassium content of bone. J. Bone Miner. Res. 1997;12:1664–1671. doi: 10.1359/jbmr.1997.12.10.1664. [DOI] [PubMed] [Google Scholar]
- 25.Rubinacci A, Benelli FD, Borgo E, Villa I. Bone as an ion exchange system: evidence for a pump-leak mechanism devoted to the maintenance of high bone K+ Am. J. Physiol. Endocrinol. Metab. 2000;278:E15–E24. doi: 10.1152/ajpendo.2000.278.1.E15. [DOI] [PubMed] [Google Scholar]
- 26.Dedic C, et al. Calcium fluxes at the bone/plasma interface: acute effects of parathyroid hormone (PTH) and targeted deletion of PTH/PTH-related peptide (PTHrP) receptor in the osteocytes. Bone. 2018;116:135–143. doi: 10.1016/j.bone.2018.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rubinacci A, et al. Bone as an ion exchange system: evidence for a link between mechanotransduction and metabolic needs. Am. J. Physiol. Endocrinol. Metab. 2002;282:E851–E864. doi: 10.1152/ajpendo.00367.2001. [DOI] [PubMed] [Google Scholar]
- 28.Qin L, Liu W, Cao H, Xiao G. Molecular mechanosensors in osteocytes. Bone Res. 2020;8:23. doi: 10.1038/s41413-020-0099-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McNamara LM, Majeska RJ, Weinbaum S, Friedrich V, Schaffler MB. Attachment of osteocyte cell processes to the bone matrix. Anat. Rec. 2009;292:355–363. doi: 10.1002/ar.20869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cabahug-Zuckerman P, et al. Potential role for a specialized β(3) integrin-based structure on osteocyte processes in bone mechanosensation. J. Orthop. Res. 2018;36:642–652. doi: 10.1002/jor.23792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Malone, A. M. D. et al. Primary cilia mediate mechanosensing in bone cells by a calcium-independent mechanism. Proc. Natl. Acad. Sci. USA. 104, 13325–13330 (2007). [DOI] [PMC free article] [PubMed]
- 32.Plotkin LI, Speacht TL, Donahue HJ. Cx43 and mechanotransduction in bone. Curr. Osteoporos. Rep. 2015;13:67–72. doi: 10.1007/s11914-015-0255-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang L, et al. Mechanical sensing protein PIEZO1 regulates bone homeostasis via osteoblast-osteoclast crosstalk. Nat. Commun. 2020;11:282. doi: 10.1038/s41467-019-14146-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lyons JS, et al. Microtubules tune mechanotransduction through NOX2 and TRPV4 to decrease sclerostin abundance in osteocytes. Sci. Signal. 2017;10:eaan5748. doi: 10.1126/scisignal.aan5748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Morrell AE, et al. Mechanically induced Ca(2+) oscillations in osteocytes release extracellular vesicles and enhance bone formation. Bone Res. 2018;6:6. doi: 10.1038/s41413-018-0007-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Colombo M, Raposo G, Théry C. Biogenesis, secretion, and intercellular interactions of exosomes and other extracellular vesicles. Annu. Rev. Cell Dev. Biol. 2014;30:255–289. doi: 10.1146/annurev-cellbio-101512-122326. [DOI] [PubMed] [Google Scholar]
- 37.Kamel-ElSayed SA, Tiede-Lewis LM, Lu Y, Veno PA, Dallas SL. Novel approaches for two and three dimensional multiplexed imaging of osteocytes. Bone. 2015;76:129–140. doi: 10.1016/j.bone.2015.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Baron R, Kneissel M. Wnt signaling in bone homeostasis and disease: from human mutations to treatments. Nat. Med. 2013;19:179–192. doi: 10.1038/nm.3074. [DOI] [PubMed] [Google Scholar]
- 39.Karner CM, Long F. Wnt signaling and cellular metabolism in osteoblasts. Cell. Mol. Life Sci. 2017;74:1649–1657. doi: 10.1007/s00018-016-2425-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Day TF, Guo X, Garrett-Beal L, Yang Y. Wnt/β-catenin signaling in mesenchymal progenitors controls osteoblast and chondrocyte differentiation during vertebrate skeletogenesis. Dev. Cell. 2005;8:739–750. doi: 10.1016/j.devcel.2005.03.016. [DOI] [PubMed] [Google Scholar]
- 41.Hu H, et al. Sequential roles of Hedgehog and Wnt signaling in osteoblast development. Development. 2005;132:49–60. doi: 10.1242/dev.01564. [DOI] [PubMed] [Google Scholar]
- 42.Song L, et al. Loss of Wnt/β-catenin signaling causes cell fate shift of preosteoblasts from osteoblasts to adipocytes. J. Bone Miner. Res. 2012;27:2344–2358. doi: 10.1002/jbmr.1694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gaur T, et al. Canonical Wnt signaling promotes osteogenesis by directly stimulating Runx2 gene expression. J. Biol. Chem. 2005;280:33132–33140. doi: 10.1074/jbc.M500608200. [DOI] [PubMed] [Google Scholar]
- 44.Sato T, et al. A FAK/HDAC5 signaling axis controls osteocyte mechanotransduction. Nat. Commun. 2020;11:3282. doi: 10.1038/s41467-020-17099-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wein MN, et al. HDAC5 controls MEF2C-driven sclerostin expression in osteocytes. J. Bone Miner. Res. 2015;30:400–411. doi: 10.1002/jbmr.2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wein MN, et al. SIKs control osteocyte responses to parathyroid hormone. Nat. Commun. 2016;7:13176. doi: 10.1038/ncomms13176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stegen S, et al. Osteocytic oxygen sensing controls bone mass through epigenetic regulation of sclerostin. Nat. Commun. 2018;9:2557. doi: 10.1038/s41467-018-04679-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Verborgt O, Gibson GJ, Schaffler MB. Loss of osteocyte integrity in association with microdamage and bone remodeling after fatigue in vivo. J. Bone Miner. Res. 2000;15:60–67. doi: 10.1359/jbmr.2000.15.1.60. [DOI] [PubMed] [Google Scholar]
- 49.Boyce BF, Xing L. Functions of RANKL/RANK/OPG in bone modeling and remodeling. Arch. Biochem. Biophys. 2008;473:139–146. doi: 10.1016/j.abb.2008.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Holliday LS, Patel SS, Rody WJ., Jr. RANKL and RANK in extracellular vesicles: surprising new players in bone remodeling. Extracell. Vesicles Circ. Nucleic Acids. 2021;2:18–28. doi: 10.20517/evcna.2020.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nakashima T, et al. Evidence for osteocyte regulation of bone homeostasis through RANKL expression. Nat. Med. 2011;17:1231–1234. doi: 10.1038/nm.2452. [DOI] [PubMed] [Google Scholar]
- 52.Xiong J, et al. Matrix-embedded cells control osteoclast formation. Nat. Med. 2011;17:1235–1241. doi: 10.1038/nm.2448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lim J, Burclaff J, He G, Mills JC, Long F. Unintended targeting of Dmp1-Cre reveals a critical role for Bmpr1a signaling in the gastrointestinal mesenchyme of adult mice. Bone Res. 2017;5:16049. doi: 10.1038/boneres.2016.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Xiong J, et al. Osteocytes, not osteoblasts or lining cells, are the main source of the RANKL required for osteoclast formation in remodeling bone. PLoS One. 2015;10:e0138189. doi: 10.1371/journal.pone.0138189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhao S, et al. MLO-Y4 osteocyte-like cells support osteoclast formation and activation. J. Bone Miner. Res. 2002;17:2068–2079. doi: 10.1359/jbmr.2002.17.11.2068. [DOI] [PubMed] [Google Scholar]
- 56.Al-Dujaili SA, et al. Apoptotic osteocytes regulate osteoclast precursor recruitment and differentiation in vitro. J. Cell. Biochem. 2011;112:2412–2423. doi: 10.1002/jcb.23164. [DOI] [PubMed] [Google Scholar]
- 57.Honma M, et al. RANKL subcellular trafficking and regulatory mechanisms in osteocytes. J. Bone Miner. Res. 2013;28:1936–1949. doi: 10.1002/jbmr.1941. [DOI] [PubMed] [Google Scholar]
- 58.Honma M, Ikebuchi Y, Suzuki H. Mechanisms of RANKL delivery to the osteoclast precursor cell surface. J. Bone Miner. Metab. 2021;39:27–33. doi: 10.1007/s00774-020-01157-3. [DOI] [PubMed] [Google Scholar]
- 59.Xiong J, et al. Soluble RANKL contributes to osteoclast formation in adult mice but not ovariectomy-induced bone loss. Nat. Commun. 2018;9:2909. doi: 10.1038/s41467-018-05244-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mizuno A, et al. Transgenic mice overexpressing soluble osteoclast differentiation factor (sODF) exhibit severe osteoporosis. J. Bone Miner. Metab. 2002;20:337–344. doi: 10.1007/s007740200049. [DOI] [PubMed] [Google Scholar]
- 61.Komori T. Cell death in chondrocytes, osteoblasts, and osteocytes. Int. J. Mol. Sci. 2016;17:2045. doi: 10.3390/ijms17122045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Emerton KB, et al. Osteocyte apoptosis and control of bone resorption following ovariectomy in mice. Bone. 2010;46:577–583. doi: 10.1016/j.bone.2009.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kennedy OD, Laudier DM, Majeska RJ, Sun HB, Schaffler MB. Osteocyte apoptosis is required for production of osteoclastogenic signals following bone fatigue in vivo. Bone. 2014;64:132–137. doi: 10.1016/j.bone.2014.03.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Aguirre JI, et al. Osteocyte apoptosis is induced by weightlessness in mice and precedes osteoclast recruitment and bone loss. J. Bone Miner. Res. 2006;21:605–615. doi: 10.1359/jbmr.060107. [DOI] [PubMed] [Google Scholar]
- 65.Kennedy OD, et al. Activation of resorption in fatigue-loaded bone involves both apoptosis and active pro-osteoclastogenic signaling by distinct osteocyte populations. Bone. 2012;50:1115–1122. doi: 10.1016/j.bone.2012.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kringelbach TM, Aslan D, Novak I, Schwarz P, Jørgensen NR. UTP-induced ATP release is a fine-tuned signalling pathway in osteocytes. Purinergic Signal. 2014;10:337–347. doi: 10.1007/s11302-013-9404-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cheung WY, et al. Pannexin-1 and P2X7-receptor are required for apoptotic osteocytes in fatigued bone to trigger RANKL production in neighboring bystander osteocytes. J. Bone Miner. Res. 2016;31:890–899. doi: 10.1002/jbmr.2740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Luckprom P, Wongkhantee S, Yongchaitrakul T, Pavasant P. Adenosine triphosphate stimulates RANKL expression through P2Y1receptor-cyclo-oxygenase-dependent pathway in human periodontal ligament cells. J. Periodontal. Res. 2010;45:404–411. doi: 10.1111/j.1600-0765.2009.01256.x. [DOI] [PubMed] [Google Scholar]
- 69.Elliott MR, et al. Nucleotides released by apoptotic cells act as a find-me signal to promote phagocytic clearance. Nature. 2009;461:282–286. doi: 10.1038/nature08296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Verborgt O, Tatton NA, Majeska RJ, Schaffler MB. Spatial distribution of bax and Bcl-2 in osteocytes after bone fatigue: complementary roles in bone remodeling regulation? J. Bone Miner. Res. 2002;17:907–914. doi: 10.1359/jbmr.2002.17.5.907. [DOI] [PubMed] [Google Scholar]
- 71.Takeuchi O, Akira S. Pattern recognition receptors and inflammation. Cell. 2010;140:805–820. doi: 10.1016/j.cell.2010.01.022. [DOI] [PubMed] [Google Scholar]
- 72.Messmer D, et al. High mobility group box protein 1: an endogenous signal for dendritic cell maturation and Th1 polarization. J. Immunol. 2004;173:307–313. doi: 10.4049/jimmunol.173.1.307. [DOI] [PubMed] [Google Scholar]
- 73.Mori T, et al. IL-1β and TNFα-initiated IL-6-STAT3 pathway is critical in mediating inflammatory cytokines and RANKL expression in inflammatory arthritis. Int. Immunol. 2011;23:701–712. doi: 10.1093/intimm/dxr077. [DOI] [PubMed] [Google Scholar]
- 74.Andreev D, et al. Osteocyte necrosis triggers osteoclast-mediated bone loss through macrophage-inducible C-type lectin. J. Clin. Investig. 2020;130:4811–4830. doi: 10.1172/JCI134214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Glass DA, et al. Canonical Wnt signaling in differentiated osteoblasts controls osteoclast differentiation. Dev. Cell. 2005;8:751–764. doi: 10.1016/j.devcel.2005.02.017. [DOI] [PubMed] [Google Scholar]
- 76.Walsh MC, Choi Y. Biology of the RANKL-RANK-OPG system in immunity, bone, and beyond. Front. Immunol. 2014;5:511. doi: 10.3389/fimmu.2014.00511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Cawley KM, et al. Local production of osteoprotegerin by osteoblasts suppresses bone resorption. Cell Rep. 2020;32:108052. doi: 10.1016/j.celrep.2020.108052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Delgado-Calle J, et al. Control of bone anabolism in response to mechanical loading and PTH by distinct mechanisms downstream of the PTH receptor. J. Bone Miner. Res. 2017;32:522–535. doi: 10.1002/jbmr.3011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ben-Awadh AN, et al. Parathyroid hormone receptor signaling induces bone resorption in the adult skeleton by directly regulating the RANKL gene in osteocytes. Endocrinology. 2014;155:2797–2809. doi: 10.1210/en.2014-1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Rhee Y, et al. PTH receptor signaling in osteocytes governs periosteal bone formation and intracortical remodeling. J. Bone Miner. Res. 2011;26:1035–1046. doi: 10.1002/jbmr.304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Saini V, et al. Parathyroid hormone (PTH)/PTH-related peptide type 1 receptor (PPR) signaling in osteocytes regulates anabolic and catabolic skeletal responses to PTH. J. Biol. Chem. 2013;288:20122–20134. doi: 10.1074/jbc.M112.441360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hongo H, et al. Osteocytic osteolysis in PTH-treated wild-type and rankl(-/-) mice examined by transmission electron microscopy, atomic force microscopy, and isotope microscopy. J. Histochem. Cytochem. 2020;68:651–668. doi: 10.1369/0022155420961375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tazawa K, et al. Osteocytic osteolysis observed in rats to which parathyroid hormone was continuously administered. J. Bone Miner. Metab. 2004;22:524–529. doi: 10.1007/s00774-004-0519-x. [DOI] [PubMed] [Google Scholar]
- 84.Misof BM, et al. Bone matrix mineralization and osteocyte lacunae characteristics in patients with chronic kidney disease—mineral bone disorder(CKD-MBD) J. Musculoskelet. Neuronal Interact. 2019;19:196–206. [PMC free article] [PubMed] [Google Scholar]
- 85.Gardinier JD, Al-Omaishi S, Morris MD, Kohn DH. PTH signaling mediates perilacunar remodeling during exercise. Matrix Biol. 2016;52-54:162–175. doi: 10.1016/j.matbio.2016.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Qing H, et al. Demonstration of osteocytic perilacunar/canalicular remodeling in mice during lactation. J. Bone Miner. Res. 2012;27:1018–1029. doi: 10.1002/jbmr.1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Misof BM, et al. No role of osteocytic osteolysis in the development and recovery of the bone phenotype induced by severe secondary hyperparathyroidism in vitamin D receptor deficient mice. Int. J. Mol. Sci. 2020;21:7989. doi: 10.3390/ijms21217989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Davesne D, et al. The phylogenetic origin and evolution of acellular bone in teleost fishes: insights into osteocyte function in bone metabolism. Biol. Rev. Camb. Philos. Soc. 2019;94:1338–1363. doi: 10.1111/brv.12505. [DOI] [PubMed] [Google Scholar]
- 89.Hung JT, et al. Assessing the ability of zebrafish scales to contribute to the short-term homeostatic regulation of [Ca2+] in the extracellular fluid during calcemic challenges. Fish. Sci. 2019;85:943–959. doi: 10.1007/s12562-019-01353-9. [DOI] [Google Scholar]
- 90.Marenzana M, Shipley AM, Squitiero P, Kunkel JG, Rubinacci A. Bone as an ion exchange organ: evidence for instantaneous cell-dependent calcium efflux from bone not due to resorption. Bone. 2005;37:545–554. doi: 10.1016/j.bone.2005.04.036. [DOI] [PubMed] [Google Scholar]
- 91.Farr JN, Kaur J, Doolittle ML, Khosla S. Osteocyte cellular senescence. Curr. Osteoporos. Rep. 2020;18:559–567. doi: 10.1007/s11914-020-00619-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Farr JN, et al. Identification of senescent cells in the bone microenvironment. J. Bone Miner. Res. 2016;31:1920–1929. doi: 10.1002/jbmr.2892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Uda Y, et al. Parathyroid hormone signaling in mature osteoblasts/osteocytes protects mice from age-related bone loss. Aging. 2021;13:25607–25642. doi: 10.18632/aging.203808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hayashi M, et al. Autoregulation of osteocyte Sema3A orchestrates estrogen action and counteracts bone aging. Cell Metab. 2019;29:627–637.e5. doi: 10.1016/j.cmet.2018.12.021. [DOI] [PubMed] [Google Scholar]
- 95.Sharma D, et al. The effects of estrogen deficiency on cortical bone microporosity and mineralization. Bone. 2018;110:1–10. doi: 10.1016/j.bone.2018.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Jackson E, et al. Osteocyte Wnt/β-catenin pathway activation upon mechanical loading is altered in ovariectomized mice. Bone Rep. 2021;15:101129. doi: 10.1016/j.bonr.2021.101129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ma L, et al. Connexin 43 hemichannels protect bone loss during estrogen deficiency. Bone Res. 2019;7:11. doi: 10.1038/s41413-019-0050-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Dole NS, et al. Osteocyte-intrinsic TGF-β signaling regulates bone quality through perilacunar/canalicular remodeling. Cell Rep. 2017;21:2585–2596. doi: 10.1016/j.celrep.2017.10.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Turner AG, Hanrath MA, Morris HA, Atkins GJ, Anderson PH. The local production of 1,25(OH)2D3 promotes osteoblast and osteocyte maturation. J. Steroid Biochem. Mol. Biol. 2014;144:114–118. doi: 10.1016/j.jsbmb.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 100.Yashiro M, et al. Active vitamin D and vitamin D analogs stimulate fibroblast growth factor 23 production in osteocyte-like cells via the vitamin D receptor. J. Pharm. Biomed. Anal. 2020;182:113139. doi: 10.1016/j.jpba.2020.113139. [DOI] [PubMed] [Google Scholar]
- 101.Nociti FH, Jr., et al. Vitamin D represses dentin matrix protein 1 in cementoblasts and osteocytes. J. Dent. Res. 2014;93:148–154. doi: 10.1177/0022034513516344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Rolvien T, et al. Vitamin D regulates osteocyte survival and perilacunar remodeling in human and murine bone. Bone. 2017;103:78–87. doi: 10.1016/j.bone.2017.06.022. [DOI] [PubMed] [Google Scholar]
- 103.Yuan Y, et al. Impaired 1,25 dihydroxyvitamin D3 action and hypophosphatemia underlie the altered lacuno-canalicular remodeling observed in the Hyp mouse model of XLH. PLoS One. 2021;16:e0252348. doi: 10.1371/journal.pone.0252348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ito N, Findlay DM, Anderson PH, Bonewald LF, Atkins GJ. Extracellular phosphate modulates the effect of 1α,25-dihydroxy vitamin D3 (1,25D) on osteocyte like cells. J. Steroid Biochem. Mol. Biol. 2013;136:183–186. doi: 10.1016/j.jsbmb.2012.09.029. [DOI] [PubMed] [Google Scholar]
- 105.Takashi Y, Fukumoto S. Phosphate-sensing and regulatory mechanism of FGF23 production. J. Endocrinol. Investig. 2020;43:877–883. doi: 10.1007/s40618-020-01205-9. [DOI] [PubMed] [Google Scholar]
- 106.Gooi JH, et al. Decline in calcitonin receptor expression in osteocytes with age. J. Endocrinol. 2014;221:181–191. doi: 10.1530/JOE-13-0524. [DOI] [PubMed] [Google Scholar]
- 107.Davey RA, Findlay DM. Calcitonin: physiology or fantasy? J. Bone Miner. Res. 2013;28:973–979. doi: 10.1002/jbmr.1869. [DOI] [PubMed] [Google Scholar]
- 108.He Z, et al. Irisin inhibits osteocyte apoptosis by activating the Erk signaling pathway in vitro and attenuates ALCT-induced osteoarthritis in mice. Bone. 2020;141:115573. doi: 10.1016/j.bone.2020.115573. [DOI] [PubMed] [Google Scholar]
- 109.Wood CL, Pajevic PD, Gooi JH. Osteocyte secreted factors inhibit skeletal muscle differentiation. Bone Rep. 2017;6:74–80. doi: 10.1016/j.bonr.2017.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Du JH, et al. The function of Wnt ligands on osteocyte and bone remodeling. J. Dent. Res. 2019;98:930–938. doi: 10.1177/0022034519854704. [DOI] [PubMed] [Google Scholar]
- 111.Miller SC, Bowman BM, Smith JM, Jee WSS. Characterization of endosteal bone-lining cells from fatty marrow bone sites in adult beagles. Anat. Rec. 1980;198:163–173. doi: 10.1002/ar.1091980204. [DOI] [PubMed] [Google Scholar]
- 112.Miller SC, de Saint-Georges L, Bowman BM, Jee WS. Bone lining cells: structure and function. Scanning Microsc. 1989;3:953–960. [PubMed] [Google Scholar]
- 113.Everts V, et al. The bone lining cell: its role in cleaning howship’s lacunae and initiating bone formation. J. Bone Miner. Res. 2002;17:77–90. doi: 10.1359/jbmr.2002.17.1.77. [DOI] [PubMed] [Google Scholar]
- 114.Bloemen V, de Vries TJ, Schoenmaker T, Everts V. Intercellular adhesion molecule-1 clusters during osteoclastogenesis. Biochem. Biophys. Res. Commun. 2009;385:640–645. doi: 10.1016/j.bbrc.2009.05.145. [DOI] [PubMed] [Google Scholar]
- 115.Talmage RV. Morphological and physiological considerations in a new concept of calcium transport in bone. Am. J. Anat. 1970;129:467–476. doi: 10.1002/aja.1001290408. [DOI] [PubMed] [Google Scholar]
- 116.Wongdee K, Riengrojpitak S, Krishnamra N, Charoenphandhu N. Claudin expression in the bone-lining cells of female rats exposed to long-standing acidemia. Exp. Mol. Pathol. 2010;88:305–310. doi: 10.1016/j.yexmp.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 117.Andersen TL, et al. A physical mechanism for coupling bone resorption and formation in adult human bone. Am. J. Pathol. 2009;174:239–247. doi: 10.2353/ajpath.2009.080627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Fields GB. Interstitial collagen catabolism. J. Biol. Chem. 2013;288:8785–8793. doi: 10.1074/jbc.R113.451211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Sprangers S, Everts V. Molecular pathways of cell-mediated degradation of fibrillar collagen. Matrix Biol. 2019;75-76:190–200. doi: 10.1016/j.matbio.2017.11.008. [DOI] [PubMed] [Google Scholar]
- 120.Delaissé JM, et al. Matrix metalloproteinases (MMP) and cathepsin K contribute differently to osteoclastic activities. Microsc. Res. Tech. 2003;61:504–513. doi: 10.1002/jemt.10374. [DOI] [PubMed] [Google Scholar]
- 121.Shi J, et al. Membrane-type MMPs enable extracellular matrix permissiveness and mesenchymal cell proliferation during embryogenesis. Dev. Biol. 2008;313:196–209. doi: 10.1016/j.ydbio.2007.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Parfitt AM. The bone remodeling compartment: a circulatory function for bone lining cells. J. Bone Miner. Res. 2001;16:1583–1585. doi: 10.1359/jbmr.2001.16.9.1583. [DOI] [PubMed] [Google Scholar]
- 123.Hauge EM, Qvesel D, Eriksen EF, Mosekilde L, Melsen F. Cancellous bone remodeling occurs in specialized compartments lined by cells expressing osteoblastic markers. J. Bone Miner. Res. 2001;16:1575–1582. doi: 10.1359/jbmr.2001.16.9.1575. [DOI] [PubMed] [Google Scholar]
- 124.Kristensen HB, Andersen TL, Marcussen N, Rolighed L, Delaisse JM. Increased presence of capillaries next to remodeling sites in adult human cancellous bone. J. Bone Miner. Res. 2013;28:574–585. doi: 10.1002/jbmr.1760. [DOI] [PubMed] [Google Scholar]
- 125.Díaz-Flores L, et al. Pericytes. Morphofunction, interactions and pathology in a quiescent and activated mesenchymal cell niche. Histol. Histopathol. 2009;24:909–969. doi: 10.14670/HH-24.909. [DOI] [PubMed] [Google Scholar]
- 126.Delaisse JM. The reversal phase of the bone-remodeling cycle: cellular prerequisites for coupling resorption and formation. Bonekey Rep. 2014;3:561. doi: 10.1038/bonekey.2014.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Eghbali-Fatourechi GZ, et al. Circulating osteoblast-lineage cells in humans. N. Engl. J. Med. 2005;352:1959–1966. doi: 10.1056/NEJMoa044264. [DOI] [PubMed] [Google Scholar]
- 128.Kusumbe AP, Ramasamy SK, Adams RH. Coupling of angiogenesis and osteogenesis by a specific vessel subtype in bone. Nature. 2014;507:323–328. doi: 10.1038/nature13145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Ramasamy SK, Kusumbe AP, Wang L, Adams RH. Endothelial Notch activity promotes angiogenesis and osteogenesis in bone. Nature. 2014;507:376–380. doi: 10.1038/nature13146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Xie H, et al. PDGF-BB secreted by preosteoclasts induces angiogenesis during coupling with osteogenesis. Nat. Med. 2014;20:1270–1278. doi: 10.1038/nm.3668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Kim BJ, et al. Osteoclast-secreted SLIT3 coordinates bone resorption and formation. J. Clin. Investig. 2018;128:1429–1441. doi: 10.1172/JCI91086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Qiu H, Xiao W, Yue J, Wang L. Heparan sulfate modulates Slit3-induced endothelial cell migration. Methods Mol. Biol. 2015;1229:549–555. doi: 10.1007/978-1-4939-1714-3_43. [DOI] [PubMed] [Google Scholar]
- 133.Geutskens SB, et al. Control of human hematopoietic stem/progenitor cell migration by the extracellular matrix protein Slit3. Lab. Investig. 2012;92:1129–1139. doi: 10.1038/labinvest.2012.81. [DOI] [PubMed] [Google Scholar]
- 134.Zhou BO, Yue R, Murphy MM, Peyer JG, Morrison SJ. Leptin-receptor-expressing mesenchymal stromal cells represent the main source of bone formed by adult bone marrow. Cell Stem Cell. 2014;15:154–168. doi: 10.1016/j.stem.2014.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Caire R, et al. Parathyroid hormone remodels bone transitional vessels and the leptin receptor‐positive pericyte network in mice. J. Bone Miner. Res. 2019;34:1487–1501. doi: 10.1002/jbmr.3728. [DOI] [PubMed] [Google Scholar]
- 136.Ominsky MS, et al. Differential temporal effects of sclerostin antibody and parathyroid hormone on cancellous and cortical bone and quantitative differences in effects on the osteoblast lineage in young intact rats. Bone. 2015;81:380–391. doi: 10.1016/j.bone.2015.08.007. [DOI] [PubMed] [Google Scholar]
- 137.Matic I, et al. Quiescent bone lining cells are a major source of osteoblasts during adulthood. Stem Cells. 2016;34:2930–2942. doi: 10.1002/stem.2474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Collin-Osdoby P, et al. Receptor activator of NF-kappa B and osteoprotegerin expression by human microvascular endothelial cells, regulation by inflammatory cytokines, and role in human osteoclastogenesis. J. Biol. Chem. 2001;276:20659–20672. doi: 10.1074/jbc.M010153200. [DOI] [PubMed] [Google Scholar]
- 139.Søe K, Delaisse JM, Borggaard XG. Osteoclast formation at the bone marrow/bone surface interface: importance of structural elements, matrix, and intercellular communication. Semin. Cell Dev. Biol. 2020;112:8–15. doi: 10.1016/j.semcdb.2020.05.016. [DOI] [PubMed] [Google Scholar]
- 140.Ferrier J, Xia SL, Lagan E, Aubin JE, Heersche JNM. Displacement and translocation of osteoblast-like cells by osteoclasts. J. Bone Miner. Res. 1994;9:1397–1405. doi: 10.1002/jbmr.5650090911. [DOI] [PubMed] [Google Scholar]
- 141.Karsdal MA, Fjording MS, Foged NT, Delaissé JM, Lochter A. Transforming growth factor-β-induced osteoblast elongation regulates osteoclastic bone resorption through a p38 mitogen-activated protein kinase- and matrix metalloproteinase-dependent pathway. J. Biol. Chem. 2001;276:39350–39358. doi: 10.1074/jbc.M008738200. [DOI] [PubMed] [Google Scholar]
- 142.Saltel F, et al. Transmigration: a new property of mature multinucleated osteoclasts. J. Bone Miner. Res. 2006;21:1913–1923. doi: 10.1359/jbmr.060821. [DOI] [PubMed] [Google Scholar]
- 143.Perez-Amodio S, Beertsen W, Everts V. (Pre-)osteoclasts induce retraction of osteoblasts before their fusion to osteoclasts. J. Bone Miner. Res. 2004;19:1722–1731. doi: 10.1359/JBMR.040509. [DOI] [PubMed] [Google Scholar]
- 144.Kajita M, et al. Membrane-type 1 matrix metalloproteinase cleaves CD44 and promotes cell migration. J. Cell Biol. 2001;153:893–904. doi: 10.1083/jcb.153.5.893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Blavier L, Delaisse JM. Matrix metalloproteinases are obligatory for the migration of preosteoclasts to the developing marrow cavity of primitive long bones. J. Cell Sci. 1995;108:3649–3659. doi: 10.1242/jcs.108.12.3649. [DOI] [PubMed] [Google Scholar]
- 146.Sato T, Foged NT, Delaissé JM. The migration of purified osteoclasts through collagen is inhibited by matrix metalloproteinase inhibitors. J. Bone Miner. Res. 1998;13:59–66. doi: 10.1359/jbmr.1998.13.1.59. [DOI] [PubMed] [Google Scholar]
- 147.Andersen TL, et al. A scrutiny of matrix metalloproteinases in osteoclasts: evidence for heterogeneity and for the presence of MMPs synthesized by other cells. Bone. 2004;35:1107–1119. doi: 10.1016/j.bone.2004.06.019. [DOI] [PubMed] [Google Scholar]
- 148.Holmbeck K, et al. MT1-MMP-deficient mice develop dwarfism, osteopenia, arthritis, and connective tissue disease due to inadequate collagen turnover. Cell. 1999;99:81–92. doi: 10.1016/S0092-8674(00)80064-1. [DOI] [PubMed] [Google Scholar]
- 149.Sato T, et al. Identification of the membrane-type matrix metalloproteinase MT1-MMP in osteoclasts. J. Cell Sci. 1997;110:589–596. doi: 10.1242/jcs.110.5.589. [DOI] [PubMed] [Google Scholar]
- 150.Ohuchi E, et al. Membrane type 1 matrix metalloproteinase digests interstitial collagens and other extracellular matrix macromolecules. J. Biol. Chem. 1997;272:2446–2451. doi: 10.1074/jbc.272.4.2446. [DOI] [PubMed] [Google Scholar]
- 151.Engsig MT, et al. Matrix metalloproteinase 9 and vascular endothelial growth factor are essential for osteoclast recruitment into developing long bones. J. Cell Biol. 2000;151:879–889. doi: 10.1083/jcb.151.4.879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Chellaiah MA, Ma T. Membrane localization of membrane type 1 matrix metalloproteinase by CD44 regulates the activation of pro-matrix metalloproteinase 9 in osteoclasts. Biomed. Res. Int. 2013;2013:302392. doi: 10.1155/2013/302392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Zhu L, et al. Osteoclast-mediated bone resorption is controlled by a compensatory network of secreted and membrane-tethered metalloproteinases. Sci. Transl. Med. 2020;12:eaaw6143. doi: 10.1126/scitranslmed.aaw6143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Møller AMJ, et al. Aging and menopause reprogram osteoclast precursors for aggressive bone resorption. Bone Res. 2020;8:27. doi: 10.1038/s41413-020-0102-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Weinstein RS, Roberson PK, Manolagas SC. Giant osteoclast formation and long-term oral bisphosphonate therapy. N. Engl. J. Med. 2009;360:53–62. doi: 10.1056/NEJMoa0802633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Jobke B, Milovanovic P, Amling M, Busse B. Bisphosphonate-osteoclasts: changes in osteoclast morphology and function induced by antiresorptive nitrogen-containing bisphosphonate treatment in osteoporosis patients. Bone. 2014;59:37–43. doi: 10.1016/j.bone.2013.10.024. [DOI] [PubMed] [Google Scholar]
- 157.Takagi Y, et al. Effect of nitrogen-containing bisphosphonates on osteoclasts and osteoclastogenesis: an ultrastructural study. Microscopy. 2021;70:302–307. doi: 10.1093/jmicro/dfaa073. [DOI] [PubMed] [Google Scholar]
- 158.Liu H, et al. Histochemical evidence of zoledronate inhibiting c-src expression and interfering with CD44/OPN-mediated osteoclast adhesion in the tibiae of mice. J. Mol. Histol. 2015;46:313–323. doi: 10.1007/s10735-015-9620-9. [DOI] [PubMed] [Google Scholar]
- 159.Yagi M, et al. DC-STAMP is essential for cell-cell fusion in osteoclasts and Foreign body giant cells. J. Exp. Med. 2005;202:345–351. doi: 10.1084/jem.20050645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Takito J, Nakamura M. Heterogeneity and actin cytoskeleton in osteoclast and macrophage multinucleation. Int. J. Mol. Sci. 2020;21:6629. doi: 10.3390/ijms21186629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Streicher C, et al. Estrogen regulates bone turnover by targeting RANKL expression in bone lining cells. Sci. Rep. 2017;7:6460. doi: 10.1038/s41598-017-06614-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Takayanagi H. Osteoimmunology: shared mechanisms and crosstalk between the immune and bone systems. Nat. Rev. Immunol. 2007;7:292–304. doi: 10.1038/nri2062. [DOI] [PubMed] [Google Scholar]
- 163.Karin M, Greten FR. NF-κB: linking inflammation and immunity to cancer development and progression. Nat. Rev. Immunol. 2005;5:749–759. doi: 10.1038/nri1703. [DOI] [PubMed] [Google Scholar]
- 164.Hayden MS, West AP, Ghosh S. NF-κB and the immune response. Oncogene. 2006;25:6758–6780. doi: 10.1038/sj.onc.1209943. [DOI] [PubMed] [Google Scholar]
- 165.Franzoso G, et al. Requirement for NF-kappaB in osteoclast and B-cell development. Genes Dev. 1997;11:3482–3496. doi: 10.1101/gad.11.24.3482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Xing L, et al. NF-κB p50 and p52 expression is not required for RANK-expressing osteoclast progenitor formation but is essential for RANK- and cytokine-mediated osteoclastogenesis. J. Bone Miner. Res. 2002;17:1200–1210. doi: 10.1359/jbmr.2002.17.7.1200. [DOI] [PubMed] [Google Scholar]
- 167.Asagiri M, et al. Autoamplification of NFATc1 expression determines its essential role in bone homeostasis. J. Exp. Med. 2005;202:1261–1269. doi: 10.1084/jem.20051150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Ishida N, et al. Large scale gene expression analysis of osteoclastogenesis in vitro and elucidation of NFAT2 as a key regulator. J. Biol. Chem. 2002;277:41147–41156. doi: 10.1074/jbc.M205063200. [DOI] [PubMed] [Google Scholar]
- 169.Takayanagi H, et al. Induction and activation of the transcription factor NFATc1 (NFAT2) integrate RANKL signaling in terminal differentiation of osteoclasts. Dev. Cell. 2002;3:889–901. doi: 10.1016/S1534-5807(02)00369-6. [DOI] [PubMed] [Google Scholar]
- 170.Ruocco MG, et al. I{kappa}B kinase (IKK){beta}, but not IKK{alpha}, is a critical mediator of osteoclast survival and is required for inflammation-induced bone loss. J. Exp. Med. 2005;201:1677–1687. doi: 10.1084/jem.20042081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Xiu Y, et al. Chloroquine reduces osteoclastogenesis in murine osteoporosis by preventing TRAF3 degradation. J. Clin. Investig. 2014;124:297–310. doi: 10.1172/JCI66947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Luo J, et al. LGR4 is a receptor for RANKL and negatively regulates osteoclast differentiation and bone resorption. Nat. Med. 2016;22:539–546. doi: 10.1038/nm.4076. [DOI] [PubMed] [Google Scholar]
- 173.Ko YJ, et al. A novel modified RANKL variant can prevent osteoporosis by acting as a vaccine and an inhibitor. Clin. Transl. Med. 2021;11:e368. doi: 10.1002/ctm2.368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Yang X, Pande S, Scott C, Friesel R. Macrophage colony-stimulating factor pretreatment of bone marrow progenitor cells regulates osteoclast differentiation based upon the stage of myeloid development. J. Cell. Biochem. 2019;120:12450–12460. doi: 10.1002/jcb.28512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Faccio R, Takeshita S, Zallone A, Ross FP, Teitelbaum SL. c-Fms and the αvβ3 integrin collaborate during osteoclast differentiation. J. Clin. Investig. 2003;111:749–758. doi: 10.1172/JCI200316924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Scholtysek C, et al. NR4A1 regulates motility of osteoclast precursors and serves as target for the modulation of systemic bone turnover. J. Bone Miner. Res. 2018;33:2035–2047. doi: 10.1002/jbmr.3533. [DOI] [PubMed] [Google Scholar]
- 177.Koga T, et al. Costimulatory signals mediated by the ITAM motif cooperate with RANKL for bone homeostasis. Nature. 2004;428:758–763. doi: 10.1038/nature02444. [DOI] [PubMed] [Google Scholar]
- 178.Souza PPC, Lerner UH. Finding a toll on the route: the fate of osteoclast progenitors after toll-like receptor activation. Front. Immunol. 2019;10:1663. doi: 10.3389/fimmu.2019.01663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Yim M. The role of toll-like receptors in osteoclastogenesis. J. Bone Metab. 2020;27:227–235. doi: 10.11005/jbm.2020.27.4.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Maeda K, et al. Wnt5a-Ror2 signaling between osteoblast-lineage cells and osteoclast precursors enhances osteoclastogenesis. Nat. Med. 2012;18:405–412. doi: 10.1038/nm.2653. [DOI] [PubMed] [Google Scholar]
- 181.Kobayashi Y, et al. Wnt16 regulates osteoclast differentiation in conjunction with Wnt5a. Biochem. Biophys. Res. Commun. 2015;463:1278–1283. doi: 10.1016/j.bbrc.2015.06.102. [DOI] [PubMed] [Google Scholar]
- 182.Uehara S, et al. Protein kinase N3 promotes bone resorption by osteoclasts in response to Wnt5a-Ror2 signaling. Sci. Signal. 2017;10:eaan0023. doi: 10.1126/scisignal.aan0023. [DOI] [PubMed] [Google Scholar]
- 183.Okamoto M, et al. Noncanonical Wnt5a enhances Wnt/β-catenin signaling during osteoblastogenesis. Sci. Rep. 2014;4:4493. doi: 10.1038/srep04493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Roberts JL, et al. Deletion of Wnt5a in osteoclasts results in bone loss through decreased bone formation. Ann. N. Y. Acad. Sci. 2020;1463:45–59. doi: 10.1111/nyas.14293. [DOI] [PubMed] [Google Scholar]
- 185.Akisaka T. The ruffled border and attachment regions of the apposing membrane of resorbing osteoclasts as visualized from the cytoplasmic face of the membrane. J. Electron Microsc. 2006;55:53–61. doi: 10.1093/jmicro/dfl012. [DOI] [PubMed] [Google Scholar]
- 186.Yao G, Feng H, Cai Y, Qi W, Kong K. Characterization of vacuolar-ATPase and selective inhibition of vacuolar-H(+)-ATPase in osteoclasts. Biochem. Biophys. Res. Commun. 2007;357:821–827. doi: 10.1016/j.bbrc.2007.04.082. [DOI] [PubMed] [Google Scholar]
- 187.Kornak U, et al. Loss of the ClC-7 chloride channel leads to osteopetrosis in mice and man. Cell. 2001;104:205–215. doi: 10.1016/S0092-8674(01)00206-9. [DOI] [PubMed] [Google Scholar]
- 188.Delaissé JM, et al. Proteinases in bone resorption: obvious and less obvious roles. Clin. Chim. Acta. 2000;291:223–234. doi: 10.1016/S0009-8981(99)00230-2. [DOI] [PubMed] [Google Scholar]
- 189.Stenbeck G, Horton MA. Endocytic trafficking in actively resorbing osteoclasts. J. Cell Sci. 2004;117:827–836. doi: 10.1242/jcs.00935. [DOI] [PubMed] [Google Scholar]
- 190.Helfrich MH, Nesbitt SA, Dorey EL, Horton MA. Rat osteoclasts adhere to a wide range of rgd (arg-gly-asp) peptide-containing proteins, including the bone sialoproteins and fibronectin, via a β3 integrin. J. Bone Miner. Res. 1992;7:335–343. doi: 10.1002/jbmr.5650070314. [DOI] [PubMed] [Google Scholar]
- 191.Faccio R, et al. Activation of αvβ3 integrin on human osteoclast-like cells stimulates adhesion and migration in response to osteopontin. Biochem. Biophys. Res. Commun. 1998;249:522–525. doi: 10.1006/bbrc.1998.9180. [DOI] [PubMed] [Google Scholar]
- 192.Ross FP, et al. Interactions between the bone matrix proteins osteopontin and bone sialoprotein and the osteoclast integrin alpha v beta 3 potentiate bone resorption. J. Biol. Chem. 1993;268:9901–9907. doi: 10.1016/S0021-9258(18)98430-9. [DOI] [PubMed] [Google Scholar]
- 193.Faccio R, et al. Localization and possible role of two different alpha v beta 3 integrin conformations in resting and resorbing osteoclasts. J. Cell Sci. 2002;115:2919–2929. doi: 10.1242/jcs.115.14.2919. [DOI] [PubMed] [Google Scholar]
- 194.Duong LT, Lakkakorpi P, Nakamura I, Rodan GA. Integrins and signaling in osteoclast function. Matrix Biol. 2000;19:97–105. doi: 10.1016/S0945-053X(00)00051-2. [DOI] [PubMed] [Google Scholar]
- 195.Xiang B, et al. The osteoclasts attach to the bone surface where the extracellular calcium concentration decreases. Cell Biochem. Biophys. 2016;74:553–558. doi: 10.1007/s12013-016-0757-2. [DOI] [PubMed] [Google Scholar]
- 196.Sims NA, Martin TJ. Osteoclasts provide coupling signals to osteoblast lineage cells through multiple mechanisms. Annu. Rev. Physiol. 2020;82:507–529. doi: 10.1146/annurev-physiol-021119-034425. [DOI] [PubMed] [Google Scholar]
- 197.Jiang X, et al. Method development of efficient protein extraction in bone tissue for proteome analysis. J. Proteome Res. 2007;6:2287–2294. doi: 10.1021/pr070056t. [DOI] [PubMed] [Google Scholar]
- 198.Rubinacci A. Expanding the functional spectrum of vitamin K in bone. Focus on: “vitamin K promotes mineralization, osteoblast to osteocyte transition, and an anti-catabolic phenotype by γ-carboxylation-dependent and -independent mechanisms”. Am. J. Physiol. Cell Physiol. 2009;297:C1336–C1338. doi: 10.1152/ajpcell.00452.2009. [DOI] [PubMed] [Google Scholar]
- 199.Mizokami A, Kawakubo-Yasukochi T, Hirata M. Osteocalcin and its endocrine functions. Biochem. Pharmacol. 2017;132:1–8. doi: 10.1016/j.bcp.2017.02.001. [DOI] [PubMed] [Google Scholar]
- 200.Lin X, Patil S, Gao YG, Qian A. The bone extracellular matrix in bone formation and regeneration. Front. Pharmacol. 2020;11:757. doi: 10.3389/fphar.2020.00757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Hering S, et al. TGFβ1 and TGFβ2 mRNA and protein expression in human bone samples. Exp. Clin. Endocrinol. Diabetes. 2001;109:217–226. doi: 10.1055/s-2001-15109. [DOI] [PubMed] [Google Scholar]
- 202.Oursler MJ. Osteoclast synthesis and secretion and activation of latent transforming growth factor β. J. Bone Miner. Res. 1994;9:443–452. doi: 10.1002/jbmr.5650090402. [DOI] [PubMed] [Google Scholar]
- 203.Tang Y, et al. TGF-beta1-induced migration of bone mesenchymal stem cells couples bone resorption with formation. Nat. Med. 2009;15:757–765. doi: 10.1038/nm.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Alliston T, Choy L, Ducy P, Karsenty G, Derynck R. TGF-beta-induced repression of CBFA1 by Smad3 decreases cbfa1 and osteocalcin expression and inhibits osteoblast differentiation. EMBO J. 2001;20:2254–2272. doi: 10.1093/emboj/20.9.2254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Breen EC, et al. TGF? alters growth and differentiation related gene expression in proliferating osteoblasts in vitro, preventing development of the mature bone phenotype. J. Cell. Physiol. 1994;160:323–335. doi: 10.1002/jcp.1041600214. [DOI] [PubMed] [Google Scholar]
- 206.Weivoda MM, et al. Osteoclast TGF-β receptor signaling induces Wnt1 secretion and couples bone resorption to bone formation. J. Bone Miner. Res. 2016;31:76–85. doi: 10.1002/jbmr.2586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Li J, et al. TGFβ-induced degradation of TRAF3 in mesenchymal progenitor cells causes age-related osteoporosis. Nat. Commun. 2019;10:2795. doi: 10.1038/s41467-019-10677-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Kim JS, et al. Transforming growth factor-β1 regulates macrophage migration via RhoA. Blood. 2006;108:1821–1829. doi: 10.1182/blood-2005-10-009191. [DOI] [PubMed] [Google Scholar]
- 209.Takai H, et al. Transforming growth factor-β stimulates the production of osteoprotegerin/osteoclastogenesis inhibitory factor by bone marrow stromal cells. J. Biol. Chem. 1998;273:27091–27096. doi: 10.1074/jbc.273.42.27091. [DOI] [PubMed] [Google Scholar]
- 210.Houde N, Chamoux E, Bisson M, Roux S. Transforming growth factor-beta1 (TGF-beta1) induces human osteoclast apoptosis by up-regulating Bim. J. Biol. Chem. 2009;284:23397–23404. doi: 10.1074/jbc.M109.019372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Ota K, et al. TGF-β induces Wnt10b in osteoclasts from female mice to enhance coupling to osteoblasts. Endocrinology. 2013;154:3745–3752. doi: 10.1210/en.2013-1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Seck T, et al. Concentration of insulin-like growth factor (IGF)-I and -II in iliac crest bone matrix from pre- and postmenopausal women: relationship to age, menopause, bone turnover, bone volume, and circulating IGFs. J. Clin. Endocrinol. Metab. 1998;83:2331–2337. doi: 10.1210/jcem.83.7.4967. [DOI] [PubMed] [Google Scholar]
- 213.Lean JM, Mackay AG, Chow JW, Chambers TJ. Osteocytic expression of mRNA for c-fos and IGF-I: an immediate early gene response to an osteogenic stimulus. Am. J. Physiol. Endocrinol. Metab. 1996;270:E937–E945. doi: 10.1152/ajpendo.1996.270.6.E937. [DOI] [PubMed] [Google Scholar]
- 214.Lau KHW, et al. Osteocyte-derived insulin-like growth factor I is essential for determining bone mechanosensitivity. Am. J. Physiol. Endocrinol. Metab. 2013;305:E271–E281. doi: 10.1152/ajpendo.00092.2013. [DOI] [PubMed] [Google Scholar]
- 215.Fiedler J, Brill C, Blum WF, Brenner RE. IGF-I and IGF-II stimulate directed cell migration of bone-marrow-derived human mesenchymal progenitor cells. Biochem. Biophys. Res. Commun. 2006;345:1177–1183. doi: 10.1016/j.bbrc.2006.05.034. [DOI] [PubMed] [Google Scholar]
- 216.Yuan Y, et al. Gene expression profiles and bioinformatics analysis of insulin-like growth factor-1 promotion of osteogenic differentiation. Mol. Genet. Genom. Med. 2019;7:e00921. doi: 10.1002/mgg3.921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Xian L, et al. Matrix IGF-1 maintains bone mass by activation of mTOR in mesenchymal stem cells. Nat. Med. 2012;18:1095–1101. doi: 10.1038/nm.2793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Liu L, Parent CA. Review series: TOR kinase complexes and cell migration. J. Cell Biol. 2011;194:815–824. doi: 10.1083/jcb.201102090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Feng X, et al. Insulin-like growth factor 1 can promote proliferation and osteogenic differentiation of human dental pulp stem cells via mTOR pathway. Dev. Growth Differ. 2014;56:615–624. doi: 10.1111/dgd.12179. [DOI] [PubMed] [Google Scholar]
- 220.Sims NA, Martin TJ. Coupling signals between the osteoclast and osteoblast: how are messages transmitted between these temporary visitors to the bone surface? Front. Endocrinol. 2015;6:41. doi: 10.3389/fendo.2015.00041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Karsdal MA, Neutzsky-Wulff AV, Dziegiel MH, Christiansen C, Henriksen K. Osteoclasts secrete non-bone derived signals that induce bone formation. Biochem. Biophys. Res. Commun. 2008;366:483–488. doi: 10.1016/j.bbrc.2007.11.168. [DOI] [PubMed] [Google Scholar]
- 222.Thudium CS, et al. A comparison of osteoclast-rich and osteoclast-poor osteopetrosis in adult mice sheds light on the role of the osteoclast in coupling bone resorption and bone formation. Calcif. Tissue Int. 2014;95:83–93. doi: 10.1007/s00223-014-9865-4. [DOI] [PubMed] [Google Scholar]
- 223.Neutzsky-Wulff AV, et al. Severe developmental bone phenotype in ClC-7 deficient mice. Dev. Biol. 2010;344:1001–1010. doi: 10.1016/j.ydbio.2010.06.018. [DOI] [PubMed] [Google Scholar]
- 224.Henriksen K, et al. Dissociation of bone resorption and bone formation in adult mice with a non-functional V-ATPase in osteoclasts leads to increased bone strength. PLoS One. 2011;6:e27482. doi: 10.1371/journal.pone.0027482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.McClung MR, et al. Odanacatib for the treatment of postmenopausal osteoporosis: results of the LOFT multicenter, randomised, double blind, placebo-controlled trial and LOFT Extension study. Lancet Diabetes Endocrinol. 2019;7:899–911. doi: 10.1016/S2213-8587(19)30346-8. [DOI] [PubMed] [Google Scholar]
- 226.Guerrini MM, et al. Human osteoclast-poor osteopetrosis with hypogammaglobulinemia due to TNFRSF11A (RANK) mutations. Am. J. Hum. Genet. 2008;83:64–76. doi: 10.1016/j.ajhg.2008.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Whyte MP, et al. Dysosteosclerosis presents as an “osteoclast-poor” form of osteopetrosis: comprehensive investigation of a 3-year-old girl and literature review. J. Bone Miner. Res. 2010;25:2527–2539. doi: 10.1002/jbmr.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Walker EC, et al. Cardiotrophin-1 is an osteoclast-derived stimulus of bone formation required for normal bone remodeling. J. Bone Miner. Res. 2008;23:2025–2032. doi: 10.1359/jbmr.080706. [DOI] [PubMed] [Google Scholar]
- 229.Meshcheryakova A, Mechtcheriakova D, Pietschmann P. Sphingosine 1-phosphate signaling in bone remodeling: multifaceted roles and therapeutic potential. Expert Opin. Ther. Targets. 2017;21:725–737. doi: 10.1080/14728222.2017.1332180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Pederson L, Ruan M, Westendorf JJ, Khosla S, Oursler MJ. Regulation of bone formation by osteoclasts involves Wnt/BMP signaling and the chemokine sphingosine-1-phosphate. Proc. Natl Acad. Sci. USA. 2008;105:20764–20769. doi: 10.1073/pnas.0805133106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Takeshita S, et al. Osteoclast-secreted CTHRC1 in the coupling of bone resorption to formation. J. Clin. Investig. 2013;123:3914–3924. doi: 10.1172/JCI69493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Matsuoka K, Park KA, Ito M, Ikeda K, Takeshita S. Osteoclast-derived complement component 3a stimulates osteoblast differentiation. J. Bone Miner. Res. 2014;29:1522–1530. doi: 10.1002/jbmr.2187. [DOI] [PubMed] [Google Scholar]
- 233.Cornish J, Callon KE, Edgar SG, Reid IR. Leukemia inhibitory factor is mitogenic to osteoblasts. Bone. 1997;21:243–247. doi: 10.1016/S8756-3282(97)00144-0. [DOI] [PubMed] [Google Scholar]
- 234.Weivoda MM, et al. Identification of osteoclast-osteoblast coupling factors in humans reveals links between bone and energy metabolism. Nat. Commun. 2020;11:87. doi: 10.1038/s41467-019-14003-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Kim BJ, Koh JM. Coupling factors involved in preserving bone balance. Cell. Mol. Life Sci. 2019;76:1243–1253. doi: 10.1007/s00018-018-2981-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Liu M, Sun Y, Zhang Q. Emerging role of extracellular vesicles in bone remodeling. J. Dent. Res. 2018;97:859–868. doi: 10.1177/0022034518764411. [DOI] [PubMed] [Google Scholar]
- 237.Huynh N, et al. Characterization of regulatory extracellular vesicles from osteoclasts. J. Dent. Res. 2016;95:673–679. doi: 10.1177/0022034516633189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Ikebuchi Y, et al. Coupling of bone resorption and formation by RANKL reverse signalling. Nature. 2018;561:195–200. doi: 10.1038/s41586-018-0482-7. [DOI] [PubMed] [Google Scholar]
- 239.Furuya Y, et al. Stimulation of bone formation in cortical bone of mice treated with a receptor activator of nuclear factor-κB ligand (RANKL)-binding peptide that possesses osteoclastogenesis inhibitory activity. J. Biol. Chem. 2013;288:5562–5571. doi: 10.1074/jbc.M112.426080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Portal-Núñez S, et al. Unexpected bone formation produced by RANKL blockade. Trends Endocrinol. Metab. 2017;28:695–704. doi: 10.1016/j.tem.2017.06.003. [DOI] [PubMed] [Google Scholar]
- 241.Bone HG, et al. 10 years of denosumab treatment in postmenopausal women with osteoporosis: results from the phase 3 randomised FREEDOM trial and open-label extension. Lancet Diabetes Endocrinol. 2017;5:513–523. doi: 10.1016/S2213-8587(17)30138-9. [DOI] [PubMed] [Google Scholar]
- 242.Dempster DW, et al. Modeling‐based bone formation in the human femoral neck in subjects treated with denosumab. J. Bone Miner. Res. 2020;35:1282–1288. doi: 10.1002/jbmr.4006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Wang L, Huang B, Chen X, Su J. New insight into unexpected bone formation by denosumab. Drug Discov. Today. 2020;25:1919–1922. doi: 10.1016/j.drudis.2020.09.001. [DOI] [PubMed] [Google Scholar]
- 244.Chen X, Zhi X, Wang J, Su J. RANKL signaling in bone marrow mesenchymal stem cells negatively regulates osteoblastic bone formation. Bone Res. 2018;6:34. doi: 10.1038/s41413-018-0035-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Amizuka N, et al. Defective bone remodelling in osteoprotegerin-deficient mice. J. Electron Microsc. 2003;52:503–513. doi: 10.1093/jmicro/52.6.503. [DOI] [PubMed] [Google Scholar]
- 246.Sone E, et al. The induction of RANKL molecule clustering could stimulate early osteoblast differentiation. Biochem. Biophys. Res. Commun. 2019;509:435–440. doi: 10.1016/j.bbrc.2018.12.093. [DOI] [PubMed] [Google Scholar]
- 247.Pitt JM, Kroemer G, Zitvogel L. Extracellular vesicles: masters of intercellular communication and potential clinical interventions. J. Clin. Investig. 2016;126:1139–1143. doi: 10.1172/JCI87316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Ma Q, et al. Osteoclast-derived apoptotic bodies show extended biological effects of parental cell in promoting bone defect healing. Theranostics. 2020;10:6825–6838. doi: 10.7150/thno.45170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Li D, et al. Osteoclast-derived exosomal miR-214-3p inhibits osteoblastic bone formation. Nat. Commun. 2016;7:10872. doi: 10.1038/ncomms10872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Ma Q, et al. Osteoclast-derived apoptotic bodies couple bone resorption and formation in bone remodeling. Bone Res. 2021;9:5. doi: 10.1038/s41413-020-00121-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Zhao C, et al. Bidirectional ephrinB2-EphB4 signaling controls bone homeostasis. Cell Metab. 2006;4:111–121. doi: 10.1016/j.cmet.2006.05.012. [DOI] [PubMed] [Google Scholar]
- 252.Tazaki Y, et al. RANKL, Ephrin-Eph and Wnt10b are key intercellular communication molecules regulating bone remodeling in autologous transplanted goldfish scales. Comp. Biochem. Physiol. A Mol. Integr. Physiol. 2018;225:46–58. doi: 10.1016/j.cbpa.2018.06.011. [DOI] [PubMed] [Google Scholar]
- 253.Matsuo K, Otaki N. Bone cell interactions through Eph/ephrin: bone modeling, remodeling and associated diseases. Cell Adhes. Migr. 2012;6:148–156. doi: 10.4161/cam.20888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Allan EH, et al. EphrinB2 regulation by PTH and PTHrP revealed by molecular profiling in differentiating osteoblasts. J. Bone Miner. Res. 2008;23:1170–1181. doi: 10.1359/jbmr.080324. [DOI] [PubMed] [Google Scholar]
- 255.Jacome-Galarza CE, et al. Developmental origin, functional maintenance and genetic rescue of osteoclasts. Nature. 2019;568:541–545. doi: 10.1038/s41586-019-1105-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Lassen NE, et al. Coupling of bone resorption and formation in real time: new knowledge gained from human haversian BMUs. J. Bone Miner. Res. 2017;32:1395–1405. doi: 10.1002/jbmr.3091. [DOI] [PubMed] [Google Scholar]
- 257.McDonald MM, et al. Osteoclasts recycle via osteomorphs during RANKL-stimulated bone resorption. Cell. 2021;184:1330–1347.e13. doi: 10.1016/j.cell.2021.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Kim SW, et al. Intermittent parathyroid hormone administration converts quiescent lining cells to active osteoblasts. J. Bone Miner. Res. 2012;27:2075–2084. doi: 10.1002/jbmr.1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Makino A, et al. Frequent administration of abaloparatide shows greater gains in bone anabolic window and bone mineral density in mice: a comparison with teriparatide. Bone. 2021;142:115651. doi: 10.1016/j.bone.2020.115651. [DOI] [PubMed] [Google Scholar]
- 260.Zanchetta MB, et al. Significant bone loss after stopping long-term denosumab treatment: a post FREEDOM study. Osteoporos. Int. 2018;29:41–47. doi: 10.1007/s00198-017-4242-6. [DOI] [PubMed] [Google Scholar]
- 261.Sølling AS, Harsløf T, Langdahl B. Treatment with zoledronate subsequent to denosumab in osteoporosis: a randomized trial. J. Bone Miner. Res. 2020;35:1858–1870. doi: 10.1002/jbmr.4098. [DOI] [PubMed] [Google Scholar]
- 262.Baron R, Vignery A, Van Tran P. The significance of lacunar erosion without osteoclasts: studies on the reversal phase of the remodeling sequence. Metab. Bone Dis. Relat. Res. 1980;2:35–40. [Google Scholar]
- 263.Dempster DW, et al. Standardized nomenclature, symbols, and units for bone histomorphometry: a 2012 update of the report of the ASBMR histomorphometry nomenclature committee. J. Bone Miner. Res. 2013;28:2–17. doi: 10.1002/jbmr.1805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Yamamoto T, Yamagata A, Nagai H. A histochemical study of tartrate-resistant acid phosphatase activity in rat osteoblasts. Acta Histochem. Cytochem. 1996;29:221–225. doi: 10.1267/ahc.29.221. [DOI] [Google Scholar]
- 265.Andersen TL, et al. Understanding coupling between bone resorption and formation. Am. J. Pathol. 2013;183:1–12. doi: 10.1016/j.ajpath.2013.03.006. [DOI] [PubMed] [Google Scholar]
- 266.Abdelgawad ME, et al. Early reversal cells in adult human bone remodeling: osteoblastic nature, catabolic functions and interactions with osteoclasts. Histochem. Cell Biol. 2016;145:603–615. doi: 10.1007/s00418-016-1414-y. [DOI] [PubMed] [Google Scholar]
- 267.Rosenberg N, Rosenberg O, Soudry M. Osteoblasts in bone physiology-mini review. Rambam Maimonides Med. J. 2012;3:e0013. doi: 10.5041/RMMJ.10080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Florencio-Silva R, Sasso GRDS, Sasso-Cerri E, Simões MJ, Cerri PS. Biology of bone tissue: structure, function, and factors that influence bone cells. Biomed. Res. Int. 2015;2015:421746. doi: 10.1155/2015/421746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Yellowley CE, Li Z, Zhou Z, Jacobs CR, Donahue HJ. Functional gap junctions between osteocytic and osteoblastic cells. J. Bone Miner. Res. 2000;15:209–217. doi: 10.1359/jbmr.2000.15.2.209. [DOI] [PubMed] [Google Scholar]
- 270.Marotti G, Ferretti M, Palumbo C, Benincasa M. Static anddynamic bone formation and the mechanism of collagen fiberorientation. Bone. 1999;25:156. [Google Scholar]
- 271.Ferretti M, Palumbo C. The osteocyte: from “prisoner” to “orchestrator”. J. Funct. Morphol. Kinesiol. 2021;6:28. doi: 10.3390/jfmk6010028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Atkins GJ, et al. RANKL expression is related to the differentiation state of human osteoblasts. J. Bone Miner. Res. 2003;18:1088–1098. doi: 10.1359/jbmr.2003.18.6.1088. [DOI] [PubMed] [Google Scholar]
- 273.Bianco P, Robey PG. Skeletal stem cells. Development. 2015;142:1023–1027. doi: 10.1242/dev.102210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Palumbo C, Cavani F, Sena P, Benincasa M, Ferretti M. Osteocyte apoptosis and absence of bone remodeling in human auditory ossicles and scleral ossicles of lower vertebrates: a mere coincidence or linked processes? Calcif. Tissue Int. 2012;90:211–218. doi: 10.1007/s00223-012-9569-6. [DOI] [PubMed] [Google Scholar]
- 275.Bianco P, et al. The meaning, the sense and the significance: translating the science of mesenchymal stem cells into medicine. Nat. Med. 2013;19:35–42. doi: 10.1038/nm.3028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Sacchetti B, et al. No identical “mesenchymal stem cells” at different times and sites: human committed progenitors of distinct origin and differentiation potential are incorporated as adventitial cells in microvessels. Stem Cell Rep. 2016;6:897–913. doi: 10.1016/j.stemcr.2016.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Sacchetti B. Post-natal “mesenchymal” stem cells: the assayable skeletal potency. J. Stem Cells Regen. Med. 2019;15:12–15. doi: 10.46582/jsrm.1501004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Kuznetsov SA, et al. Circulating skeletal stem cells. J. Cell Biol. 2001;153:1133–1140. doi: 10.1083/jcb.153.5.1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Alm JJ, et al. Circulating plastic adherent mesenchymal stem cells in aged hip fracture patients. J. Orthop. Res. 2010;28:1634–1642. doi: 10.1002/jor.21167. [DOI] [PubMed] [Google Scholar]
- 280.Canalis E. The fate of circulating osteoblasts. N. Engl. J. Med. 2005;352:2014–2016. doi: 10.1056/NEJMe058080. [DOI] [PubMed] [Google Scholar]
- 281.Feehan J, Nurgali K, Apostolopoulos V, Al Saedi A, Duque G. Circulating osteogenic precursor cells: building bone from blood. EBioMedicine. 2019;39:603–611. doi: 10.1016/j.ebiom.2018.11.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Manolagas SC, Parfitt AM. What old means to bone. Trends Endocrinol. Metab. 2010;21:369–374. doi: 10.1016/j.tem.2010.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Weinstein RS, Jilka RL, Parfitt AM, Manolagas SC. Inhibition of osteoblastogenesis and promotion of apoptosis of osteoblasts and osteocytes by glucocorticoids. Potential mechanisms of their deleterious effects on bone. J. Clin. Investig. 1998;102:274–282. doi: 10.1172/JCI2799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Moriishi T, et al. Overexpression of BCLXL in osteoblasts inhibits osteoblast apoptosis and increases bone volume and strength. J. Bone Miner. Res. 2016;31:1366–1380. doi: 10.1002/jbmr.2808. [DOI] [PubMed] [Google Scholar]
- 285.Manolagas SC, Kousteni S, Jilka RL. Sex steroids and bone. Recent Prog. Horm. Res. 2002;57:385–409. doi: 10.1210/rp.57.1.385. [DOI] [PubMed] [Google Scholar]
- 286.Wang X, et al. p53 functions as a negative regulator of osteoblastogenesis, osteoblast-dependent osteoclastogenesis, and bone remodeling. J. Cell Biol. 2006;172:115–125. doi: 10.1083/jcb.200507106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Liu H, Li B. p53 control of bone remodeling. J. Cell. Biochem. 2010;111:529–534. doi: 10.1002/jcb.22749. [DOI] [PubMed] [Google Scholar]
- 288.Bonewald LF. The amazing osteocyte. J. Bone Miner. Res. 2011;26:229–238. doi: 10.1002/jbmr.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Zhao W, Byrne MH, Wang Y, Krane SM. Osteocyte and osteoblast apoptosis and excessive bone deposition accompany failure of collagenase cleavage of collagen. J. Clin. Investig. 2000;106:941–949. doi: 10.1172/JCI10158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Holmbeck K, et al. The metalloproteinase MT1-MMP is required for normal development and maintenance of osteocyte processes in bone. J. Cell Sci. 2005;118:147–156. doi: 10.1242/jcs.01581. [DOI] [PubMed] [Google Scholar]
- 291.Staines KA, et al. Hypomorphic conditional deletion of E11/podoplanin reveals a role in osteocyte dendrite elongation. J. Cell. Physiol. 2017;232:3006–3019. doi: 10.1002/jcp.25999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Wang JS, et al. Control of osteocyte dendrite formation by Sp7 and its target gene osteocrin. Nat. Commun. 2021;12:6271. doi: 10.1038/s41467-021-26571-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Lerebours C, Buenzli PR. Towards a cell-based mechanostat theory of bone: the need to account for osteocyte desensitisation and osteocyte replacement. J. Biomech. 2016;49:2600–2606. doi: 10.1016/j.jbiomech.2016.05.012. [DOI] [PubMed] [Google Scholar]