Highlights
-
•
Cardiovascular disease (CVD) is the leading cause of morbidity and mortality in American women, but general knowledge and perception of risk in this population remains poor.
-
•
In this cross-sectional study of young women, significant gaps in knowledge and perception of CVD risk in individuals who have experienced an APO were identified along with general knowledge deficits related to pregnancy-related risk factors and CVD risk in young women.
-
•
These findings provide primary data to support the need for development and delivery of educational content on CVD risk to young women, particularly during the peripartum period.
Keywords: Cardiovascular disease, Pregnancy, Risk factors, Prevention
Abstract
Objective
Women who experience adverse pregnancy outcomes (APO) are at increased risk for cardiovascular disease (CVD); however, their knowledge of CVD risk is not well characterized. We aimed to evaluate knowledge and perception of CVD risk in young women and to determine whether these factors differ based on experience of an APO.
Methods
We conducted a cross-sectional study among women with a recent live birth at an urban medical center. Knowledge and perception of CVD risk were assessed through a self-administered online survey adapted from the American Heart Association Survey of Women's CVD Awareness.
Results
Of 5612 individuals contacted between 3/1/21 and 4/18/21, 714 completed the survey; the mean (SD) age was 34 (4) years and 25% reported an APO. While 62% of respondents identified CVD as the leading cause of death in women, there was no significant difference in CVD knowledge scores between participants who reported experiencing an APO and those who did not (6.9 vs 6.8 out of 10; p = 0.51). Participants who reported experiencing an APO had higher perception of personal risk for CVD (adjusted odds ratio, 2.64 [95% CI 1.83-3.80]) compared with participants who did not. Half of participants who experienced an APO reported perceiving average, or below average, risk for CVD and only 41 (22.5%) reported speaking with a healthcare professional about CVD within the past year.
Conclusions
Gaps remain in knowledge of CVD risk among young women, particularly after an APO. The peripartum period may represent a unique opportunity for targeted education when healthcare engagement is high.
1. Introduction
Cardiovascular disease (CVD) is the leading cause of morbidity and mortality in women, accounting for over 400,000 deaths each year in the United States [1]. Despite the significant burden of CVD, CVD knowledge and perception of risk among women remains poor. According to triennial survey data generated by the American Heart Association (AHA) Survey of Women's CVD Awareness, recognition of CVD as the leading cause of death in women declined from 65% in 2009 to 44% in 2019, with lower levels of awareness in younger women (25 to 34 years of age) [2]. Although awareness of CVD in young women has declined, the hospitalization rate for myocardial infarction in this subset of the population is rising, and CVD mortality rates among women aged 35-54 have plateaued in contrast with declining mortality rates in older groups [3], [4], [5].
There are limited data available on the knowledge and perception of CVD risk among young women, particularly among those who have experienced an adverse pregnancy outcome (APO). APOs represent an emerging group of risk factors for CVD that are particularly relevant for younger women. The common and inter-related disorders that comprise APOs include gestational diabetes mellitus (GDM), hypertensive disorders of pregnancy (HDP; gestational hypertension, preeclampsia, and eclampsia), preterm birth (PTB), and low birth weight (LBW; delivery of an infant <2500 grams); these disorders occur in approximately 20% of all pregnancies and are associated with increased risk of developing CVD, independent of traditional CVD risk factors [6]. Because these conditions resolve after delivery, awareness of the link between APOs and lifetime CVD risk remains incomplete. Further, monitoring and optimization of cardiovascular health following an APO is not consistently implemented, and the long-term cardiovascular risk associated with these complications may not be effectively communicated to the women who experience them [7,8].
Awareness of CVD risk is critical to prevention, particularly in young women who have experienced an APO, in whom primary prevention efforts may yield substantial long term benefit. To inform the design and delivery of effective educational initiatives in this population, existing research gaps must be addressed so that the current state of knowledge and perception of CVD risk among young women is better understood. The primary objective of this study was to investigate CVD knowledge and perception of CVD risk factors in individuals who had a live birth at a single urban medical center between January 1 and July 1, 2020. We sought to evaluate differences in CVD knowledge and risk perception between those who experienced an APO and those who did not, as well as differences by APO subtypes.
2. Methods
2.1. Study design and population sample
A cross-sectional study was conducted in our primary study sample of postpartum women using a self-administered online survey to assess general knowledge and perception of CVD risk. Information about the development of the survey instrument can be found in the Supplementary Material. The sampling frame consisted of all women who had a birthing hospitalization at Northwestern Memorial Hospital in Chicago, Illinois between January 1 and July 1, 2020 who had an email address listed in the electronic medical record (EMR), were older than 18 years of age at the time of delivery, and had a live birth outcome recorded after 28 weeks’ gestational age. Importantly, Northwestern Memorial Hospital currently has no existing educational programs that are systematically targeted at postpartum women who have experienced APOs. Recruitment and data collection in the primary sample took place between 3/1/2021 and 4/18/2021. Eligible participants were contacted electronically using the email on file in the EMR with an invitation to complete the survey. Prospective participants clicked on a URL to reach an online consent form; upon completion of the consent form, participants were automatically directed to the survey. Reminders were sent to all non-respondents at one- and two- week intervals following the initial recruitment email.
Concurrent to our recruitment of the primary analytic cohort, we simultaneously recruited a validation cohort of women admitted for labor and delivery at Northwestern Memorial Hospital between 3/12/21 and 5/3/21. Participants in this validation cohort were consented to the study, and then completed the same electronic survey via a tablet in the labor and delivery unit prior to giving birth.
All survey data were collected and managed using REDCap [9,10]. In both the primary and validation cohorts, the survey and all related materials were offered in the English language only. Informed consent was obtained from all participants. This study was approved by the Northwestern University Institutional Review Board.
2.2. Variables assessed
The primary exposure of interest was APO status. Self-reported APO status (including GDM, HDP, PTB, and LBW infant) was collected directly from survey responses (for definitions provided to participants, please refer to the survey provided in the Supplementary Material). In the validation cohort, only information on self-reported GDM and HDP was collected as participants completed the survey prior to giving birth and information about PTB and delivery of a LBW infant could not be ascertained. The primary outcomes of interest were general knowledge and perception of CVD risk. We defined CVD in this study as heart attack, coronary artery disease, heart failure, or stroke. A single question about relative risk perception was asked early in the survey to avoid introducing bias from other questions related to CVD later in the survey.
To assess general knowledge regarding CVD, participants were presented with a series of CVD risk factors and preventive behaviors, as well as factors that have no known impact on CVD risk and asked how each item affects the risk of heart disease for women in the general public. A knowledge score was calculated using the method applied by Wagner and colleagues in the Heart Disease Fact Questionnaire, wherein correct responses receive a value of one point and incorrect or “don't know/not sure” responses receive a score of zero points [11]. Possible scores, based only on the items with a known relationship to CVD risk, ranged from 0 to 10. Higher scores reflected greater knowledge of CVD risk factors and preventive behaviors. Additional questions were designed to assess CVD risk education and information sources; whether the respondent received routine preconception medical care; cardiovascular health before and during pregnancy; and sociodemographic factors. Participants were only asked about the pregnancy identified in the EMR in the described study period.
2.3. Statistical analysis
Descriptive statistics were calculated for all variables of interest. Normality of continuous variables was evaluated using quantile-quantile plots and the Shapiro-Wilk test. Differences between participants who self-reported an APO versus those who did not were compared using chi-squared or Fishers Exact tests for categorical covariates, two-sample t-tests for normal, continuous covariates, or Mann-Whitney U tests for non-parametric, continuous covariates. Linear regression was used to evaluate the association between self-reported APO status and knowledge of CVD risk, including adjustment for self-reported factors that reflected demographics (age), social determinants of health (race/ethnicity, income) and medical covariates (previous APO and time since giving birth). Self-reported race was included with the acknowledgement that this is a social construct. Logistic regression was used to evaluate the association of self-reported APO status with CVD risk perception (dichotomized as a binary outcome at the mean), including adjustment for self-reported factors that reflected demographics (age), social determinants of health (race/ethnicity, income) and medical covariates (previous APO and time since giving birth). Time since giving birth was included as a variable in both models to account for the potential effects of time on survey responses and to control for the effect of the COVID-19 pandemic on self-reported knowledge of CVD.
The potential effects of responder bias were assessed by comparing demographic characteristics of survey respondents with non-respondents using demographic and clinical information for all eligible participants obtained from the EMR (Northwestern Medicine Enterprise Data Warehouse [NMEDW]). We assessed demographic characteristics and CVD knowledge survey response patterns in the validation cohort using descriptive statistics. All tests of comparison and regression analyses for CVD knowledge and risk perception in the primary analytic sample were repeated within the validation sample. A two-sided p value<0.05 was used to indicate statistical significance. Statistical analysis was performed using SAS version 9.4.
3. Results
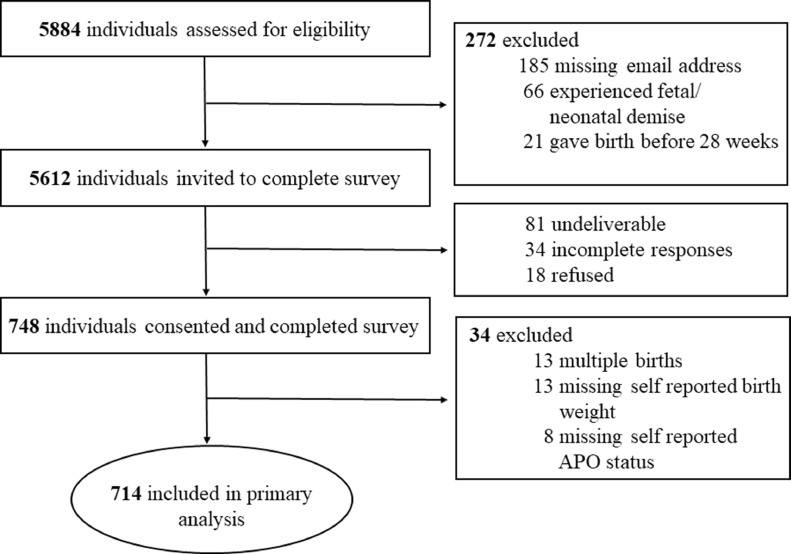
Of the 5,612 individuals who met criteria to be included in the primary analytic sample, 748 completed the survey (response rate of 13.3%: Fig. 1). Individuals who did not respond were significantly more likely to be younger and multiparous compared with survey respondents (Supplemental Table 1). A greater proportion of non-respondents identified as Hispanic, non-Hispanic Black, Asian, or other race/ethnicity compared with respondents, who primarily identified as non-Hispanic White. Non-respondents were also more likely to have public insurance compared with respondents. Similar prevalence of APOs were observed between the non-respondents (28%) and respondents (25%). In the validation cohort, among 222 eligible participants approached, 200 completed the survey and 18% reported an APO.
Fig. 1.
Online survey recruitment diagram.
3.1. Analytic cohort
Of the 748 survey respondents in the primary online sample, 34 were excluded from analysis due to missing exposure data or self-reported multiple gestation (due to differences in the relationship between APO and CVD risk with multiple gestation), resulting in a final analytic sample of 714. One-fourth of respondents (n=182, 25%) reported experiencing an APO during the index pregnancy. There were no differences in age (p = 0.25) or education level (p = 0.13) between participants who reported experiencing an APO and those who did not (Table 1). A greater proportion of participants who reported experiencing an APO self-identified as Hispanic, non-Hispanic Black, Asian, or other race/ethnicity (35.9%) compared with participants with did not report experiencing an APO (21.9%). Participants who reported experiencing an APO were more likely to report a lower household income and to report that they were uninsured or on public insurance at the time of the survey. There was no difference in reported tobacco use between the groups (p = 0.09), but participants who reported an APO reported a higher median BMI prior to pregnancy (24.8, interquartile range [IQR] 22.5-29.1) compared with those who did not (22.9, IQR 21.0-25.8). Across the study sample, most participants reported participating in exercise at least one day per week, both before and during pregnancy. A higher proportion of participants who reported experiencing an APO also reported being prescribed aspirin during pregnancy (30.2%) compared with participants who did not report experiencing an APO (15.6%).
Table 1.
Demographics of 714 survey respondents by adverse pregnancy outcome status.
| Characteristic, N (%) | Adverse Pregnancy Outcome* (n=182) | No Adverse Pregnancy Outcome (n=532) | p-value1 |
|---|---|---|---|
| Age, years, mean (SD) | 35 (4) | 34 (4) | 0.25 |
| Race/Ethnicity* | 0.002 | ||
| ▒Black | 9 (5.0) | 19 (3.6) | |
| ▒White | 116 (64.1) | 416 (78.2) | |
| ▒Hispanic | 35 (19.3) | 49 (9.2) | |
| ▒Asian | 15 (8.3) | 36 (6.8) | |
| ▒Other | 6 (3.3) | 12 (2.2) | |
| Education⁎⁎ | 0.13 | ||
| ▒High school or below | 7 (3.9) | 15 (2.8) | |
| ▒Vocational/trade | 2 (1.1) | 7 (1.3) | |
| ▒College | 170 (93.4) | 509 (95.7) | |
| Annual Household Income | 0.01 | ||
| ▒<$35,000 | 16 (8.8) | 19 (3.6) | |
| ▒$35,000-49,999 | 3 (1.7) | 12 (2.3) | |
| ▒$50,000-74,999 | 11 (6.0) | 22 (4.1) | |
| ▒$75,000-99,999 | 12 (6.6) | 32 (6.0) | |
| ▒>$100,000 | 125 (68.7) | 423 (79.5) | |
| ▒Decline to answer | 15 (8.2) | 24 (4.5) | |
| Insurance Status at Time of Survey | 0.02 | ||
| ▒Commercial insurance | 163 (89.6) | 505 (94.9) | |
| ▒Public insurance | 12 (6.6) | 22 (4.1) | |
| ▒No insurance | 3 (1.7) | 2 (0.4) | |
| ▒Decline to answer | 4 (2.2) | 3 (0.6) | |
| Primiparous | 121 (66.5) | 286 (53.8) | 0.003 |
| Time elapsed since delivery, days, mean(SD) | 376 (51.6) | 372 (52.3) | 0.37 |
| Previous APO | 44 (24.2) | 40 (7.5) | <0.001 |
| Pre-pregnancy BMI, kg/m2, median (IQR) | 24.8 (22.5-29.1) | 22.9 (21.0-25.8) | <0.001 |
| Reported Tobacco Use | 11 (6.0) | 17 (3.2) | 0.09 |
| Weekly exercise, pre-pregnancy | 0.20 | ||
| ▒<1 day/week | 25 (13.7) | 61 (11.5) | |
| ▒1-4 days/week | 119 (65.4) | 318 (59.8) | |
| ▒>5 days/week | 37 (20.3) | 148 (27.8) | |
| ▒Advised by physician not to exercise | 1 (0.6) | 5 (0.9) | |
| Weekly exercise, during pregnancy | 0.001 | ||
| ▒<1 day/week | 66 (37.9) | 158 (30.0) | |
| ▒1-4 days/week | 97 (55.8) | 296 (56.3) | |
| ▒>5 days/week | 11 (6.3) | 72 (13.7) | |
| ▒Advised by physician not to exercise | 8 (4.4) | 6 (1.1) | |
| Aspirin prescribed during pregnancy | 55 (30.2) | 83 (15.6) | <0.001 |
| Aspirin use | |||
| ▒Daily | 48 (87.3) | 66 (79.5) | 0.55 |
| ▒Sometimes | 4 (7.3) | 9 (10.9) | |
| ▒Never | 3 (5.4) | 8 (9.6) |
APO: Adverse Pregnancy Outcome; BMI: Body Mass Index; IQR: Inter Quartile Range.
Two-sample t-test, chi-squared test, Fisher's exact test, or Mann Whitney U test.
Adverse Pregnancy Outcomes include hypertensive disorders of pregnancy (gestational hypertension, preeclampsia, eclampsia), gestational diabetes, preterm birth, and delivery of a low birth weight infant.
One participant declined to report race/ethnicity and four declined to report education.
Nearly two-thirds of participants identified CVD as the leading cause of death in women (62.1% in the APO group and 61.7% in the non-APO group; Supplemental Table 2). There was no significant difference in mean CVD knowledge scores between participants who reported experiencing an APO and those who did not (6.9 vs 6.8; p = 0.51; Table 2). The proportion of participants who correctly identified traditional CVD risk factors and preventive behaviors was also similar between groups. Nearly all participants (>96%) correctly identified obesity, hypertension, and smoking as CVD risk factors. Most respondents also identified regular exercise (>94%) and low cholesterol (>70%) as risk-lowering factors, while a minority (<46%) recognized breastfeeding as a factor associated with lower risk of CVD. No significant differences were noted between groups in the identification of APOs as CVD risk factors (Table 2). Most participants correctly identified HDP (>75%) and GDM (>76%) as CVD risk factors. Frequency of recognition was lower in both groups for the correct identification of PTB (<16%) and delivery of a LBW infant (<11%).
Table 2.
Cardiovascular disease knowledge and risk perception by adverse pregnancy outcome status.
| Response, N (%) | Adverse Pregnancy Outcome (n=182) | No Adverse Pregnancy Outcome (n=532) | p-value1 |
|---|---|---|---|
| Total CVD Knowledge Score, mean (SD)* | 6.9 (1.5) | 6.8 (1.4) | 0.51 |
| Correctly Identified CVD Risk Factors | |||
| ▒Hypertension | 179 (98.4) | 518 (97.4) | 0.58 |
| ▒Overweight/Obesity | 176 (96.7) | 521 (97.9) | 0.35 |
| ▒Smoking | 175 (96.2) | 519 (97.6) | 0.32 |
| ▒Hypertensive Disorders of Pregnancy | 144 (79.1) | 401 (75.4) | 0.30 |
| ▒Gestational Diabetes | 139 (76.4) | 410 (77.1) | 0.85 |
| ▒Preterm Birth | 28 (15.4) | 59 (11.1) | 0.13 |
| ▒Low Birth Weight | 20 (11.0) | 40 (7.5) | 0.15 |
| Correctly Identified CVD Preventive Factors | |||
| ▒Regular Exercise | 172 (94.5) | 522 (98.1) | 0.01 |
| ▒Low Cholesterol Level | 129 (70.9) | 400 (75.2) | 0.25 |
| ▒Breastfeeding | 85 (46.7) | 212 (39.9) | 0.11 |
| Personal CVD Risk Perception | <0.001 | ||
| ▒Much higher than average | 11 (6.0) | 17 (3.2) | |
| ▒Somewhat higher than average | 80 (44.0) | 120 (22.6) | |
| ▒Average | 63 (34.6) | 197 (37.0) | |
| ▒Somewhat lower than average | 20 (11.0) | 139 (26.1) | |
| ▒Much lower than average | 8 (4.4) | 59 (11.1) | |
| Self-Reported CVD Knowledge | 0.26 | ||
| ▒Very well informed | 7 (3.9) | 19 (3.6) | |
| ▒Well informed | 20 (11.0) | 59 (11.1) | |
| ▒Moderately informed | 68 (37.4) | 162 (30.5) | |
| ▒A little informed | 61 (33.5) | 180 (33.8) | |
| ▒Not at all informed | 26 (14.3) | 112 (21.1) | |
| Intend to Follow Up with Physician | 88 (48.4) | 184 (34.6) | 0.001 |
| Regarding CVD Risk | |||
| ▒Family Doctor | 74 (40.7) | 150 (28.2) | |
| ▒OB/Gyn | 29 (15.9) | 71 (13.4) | |
| ▒Cardiologist | 15 (8.2) | 26 (4.9) | |
| ▒Nurse Practitioner | 8 (4.4) | 12 (2.3) | |
| ▒Nurse | 1 (0.6) | 4 (0.8) | |
| ▒Other | 2 (1.1) | 2 (0.4) |
CVD: Cardiovascular Disease.
Two-sample t-test, chi-squared test, or Fisher's exact test.
Possible CVD knowledge score ranged from 0 to 10, with higher scores reflecting greater knowledge of CVD risk factors and preventive behaviors.
Similar levels of self-reported CVD knowledge were observed in both groups, with most participants reporting that they were ‘a little informed’ or ‘moderately informed’ about heart disease in women. However, significant differences in risk perception were noted, with 91 (48%) participants in the APO group reporting that their personal risk of heart disease was ‘somewhat higher’ or ‘much higher’ than the average individual, compared with 137 (25.8%) in the non-APO group. A higher proportion of participants who reported experiencing an APO also reported intent to follow up with a physician regarding their risk for CVD (48.4%) compared with individuals who did not report an APO (34.6%); most of these participants reported intent to follow up with their family physician, with only 15 women who experienced an APO (8%) and 26 women who did not experience an APO (5%) planning to contact a cardiologist.
There was no significant univariate association between APO status and CVD knowledge score (p = 0.51) or after adjustment for age, race/ethnicity, income, previous APO, and time elapsed since giving birth (p = 0.32, Table 3). A significant univariate association between APO status and risk perception was observed (odds ratio [OR] = 2.88, [95% CI 2.03-4.09]) and remained significant after adjustment for age, race/ethnicity, income, previous APO, and time elapsed since giving birth (adjusted OR = 2.64, [95% CI 1.83-3.80]).
Table 3.
Association of adverse pregnancy outcome status with cardiovascular disease knowledge and risk perception.
| Dependent Variable | ß coefficient (95% CI) | p-value |
|---|---|---|
| CVD Knowledge Score | ||
| ▒Model 1 | 0.08 (-0.16, 0.32) | 0.51 |
| ▒Model 2* | 0.13 (-0.12, 0.38) | 0.32 |
| Odds Ratio (95% CI) | ||
| Relative Risk Perception⁎⁎ | ||
| ▒Model 1 | 2.88 (2.03-4.09) | <0.001 |
| ▒Model 2* | 2.64 (1.83-3.80) | <0.001 |
CVD: Cardiovascular Disease.
Adjusted for age, race/ethnicity, income, previous adverse pregnancy outcome, and days post delivery.
Modeled as a binary variable, with those reporting higher than average risk compared to those reporting average or lower than average risk.
The CVD knowledge score was similar across APO subtypes, ranging from a mean of 6.3 in those who reported GDM to a mean of 7.1 in those who reported PTB (Supplemental Table 3). Among participants who experienced HDP, 79.5% correctly identified hypertension during pregnancy as a risk factor for CVD. Similarly, 71.1% of participants who reported GDM correctly identified GDM as a risk factor for CVD. In contrast, among participants who experienced PTB, only 15.4% recognized PTB as a risk factor for CVD, and only 12.5% of participants with a LBW infant recognized this experience as a maternal risk factor for CVD. Risk perception also differed between groups, with greater proportions of participants who reported experiencing HDP (55.1%) and GDM (57.9%) reporting a higher than average personal risk of heart disease compared with those who reported experiencing PTB (34.6%) or delivering a LBW infant (37.6%). In all APO subtypes, intention to follow up with a physician regarding CVD risk was higher compared with participants who did not report experiencing an APO.
Table 4 lists self-reported sources of information on CVD in women among all study participants. In both groups, higher proportions of participants reported receiving information about CVD from the internet, television, or social media than from a healthcare professional. Only 22.5% of participants who experienced an APO reported speaking with a healthcare professional about CVD within the past year.
Table 4.
Sources of information on cardiovascular disease in women by adverse pregnancy outcome status.
| Response, N (%) | Adverse Pregnancy Outcome (n=182) | No Adverse Pregnancy Outcome (n=532) | p-value1 |
|---|---|---|---|
| Magazine or newspaper | 27 (14.8) | 74 (13.9) | 0.76 |
| Radio | 14 (7.7) | 28 (5.3) | 0.23 |
| Television | 45 (24.7) | 99 (18.6) | 0.08 |
| Doctor, nurse or healthcare professional | 41 (22.5) | 92 (17.3) | 0.12 |
| Internet | 59 (32.4) | 166 (31.2) | 0.76 |
| Social Media | 44 (24.2) | 103 (19.4) | 0.17 |
| Podcast | 2 (1.1) | 19 (3.6) | 0.12 |
| Friend or Relative | 27 (14.8) | 86 (16.2) | 0.67 |
| Other | 10 (5.5) | 28 (5.3) | 0.90 |
| Did not see, hear, or read about CVD in women | 55 (30.2) | 203 (38.2) | 0.05 |
CVD: Cardiovascular Disease.
Chi-squared test or Fisher's exact test.
3.2. Validation cohort
Of the 200 respondents recruited in person, one was excluded due to missing survey data resulting in a final sample of 199 in the sample recruited prior to delivery. The validation cohort was qualitatively more diverse than the sample recruited electronically, but reported CVD knowledge and relative risk perception were similar across both samples (Supplemental Tables S4–S7). There was no significant relationship observed between APO status and cardiovascular disease knowledge or risk perception in the validation cohort (Supplemental Table S8).
4. Discussion
In this cross-sectional survey of young women, we found that two-thirds of participants correctly identified heart disease as the leading cause of death in women. Most participants accurately identified traditional risk factors for CVD. However, recognition of APOs as CVD risk factors differed by APO subtype; most participants associated HDP and GDM with CVD risk, but few recognized PTB or delivery of a LBW infant as CVD risk factors. Although participants who experienced an APO reported higher CVD risk perception than those who did not, there was no association between self-reported APO status and CVD knowledge score. These findings suggest that significant gaps remain in the overall perception of personal CVD risk in individuals who have experienced an APO along with knowledge deficits related to pregnancy-related risk factors and CVD risk more generally.
Our study extends upon recent work by focusing on a key subset of the population who are at a time in their life when they are highly engaged with the healthcare system (e.g., pregnancy and the postpartum period) with 1 in 4 reporting an APO, consistent with national prevalence rates [12,13]. We found that a higher proportion of women in our study (62%) correctly identified heart disease as the leading cause of death in women compared with the latest national survey data reported by the AHA, in which only 44% of participants answered this question correctly [2]. This finding may be related to several factors, including respondent bias related to the survey introduction focusing on heart disease, recruitment at an academic medical center, and a high proportion of participants with at least a college education (95%) compared with the latest AHA sample (62%). However, nearly four in ten participants did not correctly identify heart disease as the leading cause of death in women, indicating that continued educational efforts are necessary. In addition to women in the postpartum period, other populations to focus on for future educational intervention efforts include women who are receiving mammography for breast cancer screening, as well as those receiving cervical cancer screening or contraceptive counseling, as these also represent periods of high engagement with the healthcare system [14].
Previous studies designed to characterize CVD risk awareness in women who have experienced an APO have focused exclusively on individuals who experienced HDP (primarily preeclampsia). While studies conducted prior to 2016 generally reported a lack of awareness in individuals who experienced HDP regarding their long term CVD risk [[15], [16], [17], [18]], a more recent survey found that 63% of individuals who experienced preeclampsia were aware of the association between preeclampsia and CVD [19], which was consistent with our findings among those who experienced HDP. Similar rates of recognition were also observed in our sample and previous studies focusing on awareness of GDM as a risk factor for future health complications [20]. In contrast, we note for the first time low levels of awareness of CVD risk in individuals who have experienced PTB or delivery of a LBW infant. In recent years, the AHA and the American College of Obstetrics and Gynecology (ACOG) have updated their guidelines to include HDP and GDM as major risk factors for CVD, and to recommend annual screening in these individuals. However, these guidelines do not yet include other APO subtypes (e.g., PTB, delivery of a LBW infant) despite emerging data on the association between these risk factors and CVD [[21], [22], [23], [24]]. Our study findings support the need for educational programming in women who have experienced all subtypes of APO in order to improve knowledge and perception of CVD risks and encourage the initiation of risk-reducing behaviors earlier in the life course.
Inaccurate levels of risk perception were observed across the sample of participants who reported experiencing an APO, even in those who correctly identified APO as a personal risk factor for CVD. While the majority of participants who experienced GDM and HDP correctly identified these disorders as CVD risk factors, only half reported increased personal risk for CVD, with lower levels of risk perception observed in all other subgroups. This disconnect between knowledge and risk perception has important implications for the development of targeted educational initiatives in this population. While the high level of CVD knowledge observed in our sample is encouraging, our findings suggest that this knowledge does not always translate to accurate perception of personal risk. Further, most participants reported receiving information on CVD from sources other than a healthcare professional (e.g., the internet, social media, or television), with a minority reporting that they learned about CVD from a physician. These findings are consistent with a recent study by Burgess and Feliu, who surveyed 241 women with a recent history of preeclampsia and found that a majority reported learning of the association between CVD and preeclampsia through internet sources [19]. Our results are also consistent with the findings reported by Seely and colleagues, who conducted focus groups in twenty women aged 18-50 years with a history of preeclampsia and reported that women who had experienced preeclampsia favored web-based programs as a method by which to receive education on CV risk reduction strategies [18]. These data suggest dissemination of information and preventive interventions through web-based or app-based tools may be promising avenues to enhance awareness of CVD risk and risk-lowering interventions. Further research is needed to better understand the quality, content, and delivery mechanisms of existing educational initiatives in women who have experienced an APO
Strengths of this study include the use of the EMR to generate the sampling frame for online survey delivery in the primary analytic sample, which allowed us to reach a broad number of postpartum patients and examine differences between respondents and non-respondents to evaluate the potential for nonresponse bias. While there were differences between respondents and non-respondents, similar prevalence of APOs were observed. Second, the study limited data collection to individuals who had given birth in the past year to minimize the risk of recall bias, in contrast with the majority of studies in the literature that utilize self-report of APO status decades after pregnancy. Third, examination of differences between individuals who had and had not experienced APOs along with each APO subtype revealed important differences that have not previously been characterized. Fourth, similar findings were observed with a validation cohort that was recruited during admission for labor and delivery.
This study also has several limitations that must be acknowledged. The utilization of a self-administered survey relied on self-report of APO and health history, which introduces the potential for recall bias into our study design. Second, responders differed from non-responders and the overall response rate was low. It is possible that the online delivery of the survey in the primary sample may have been a barrier due to differential internet access by socioeconomic status. Third, our study recruited participants from a single institution, introducing the potential for response bias in our sample. Fourth, the sample was recruited from an academic health center and the survey was only available in English. Thus, our findings may not be generalizable to the overall population. Future research should consider broader, more community-engaged approaches to recruitment and incorporate data collection instruments in multiple languages.
In conclusion, important gaps in awareness and risk perception were identified that should be used to inform the development of educational interventions aimed at improving risk perception and awareness of pregnancy related risk factors for CVD in this population. Because pregnancy occurs early in a woman's life, typically before the onset of clinical symptoms of CVD, it represents a unique and opportune time to assess and discuss risk for developing CVD across the lifetime and to initiate risk-reduction strategies. Developing educational programs that effectively focus on CVD health in young mothers, who often must balance many competing demands on their time in their role as caregivers, is imperative [2]. While evidence exists regarding risk reduction for CVD after an APO with primary prevention through routine screening and lifestyle modifications [21,[25], [26], [27]], knowledge of the link between APO and CVD and an accurate perception of personal CVD risk are critical to prevention.
Sources of funding
Research reported in this publication was supported, in part, by the National Institutes of Health's National Center for Advancing Translational Sciences, Grant Number UL1TR001422, SSK was funded by NHLBI HL161514. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
CRediT authorship contribution statement
Lauren Beussink-Nelson: Conceptualization, Methodology, Software, Investigation, Formal analysis, Writing – original draft, Writing – review & editing. Abigail S. Baldridge: Software, Validation, Formal analysis, Data curation, Writing – review & editing. Elizabeth Hibler: Conceptualization, Writing – review & editing. Natalie A. Bello: Writing – review & editing. Kelly Epps: Writing – review & editing. Kenzie A. Cameron: Writing – review & editing. Donald M. Lloyd-Jones: Writing – review & editing. Holly C. Gooding: Writing – review & editing. Janet M. Catov: Writing – review & editing. Janet W. Rich-Edwards: Writing – review & editing. Lynn M. Yee: Writing – review & editing. Paloma Toledo: Methodology, Investigation, Writing – review & editing. Jennifer M. Banayan: Methodology, Investigation, Writing – review & editing. Sadiya S. Khan: Conceptualization, Methodology, Resources, Writing – review & editing, Supervision.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
The authors would like to thank Karen Robb of the American Heart Association and Dr. Elizabeth Walker for assistance with development of the survey instrument. We would also like to thank Carla Albrecht, BSN, Mary Jane Jones, BSN, Joanna Gala, BSN, Yvonne Jekels, BSN, Alicia Sanchez, BSN, Adina E. Suchar, MSN, RN, Erin Roselle, BSN, Alyssa Santi, BSN, and Valarie Sampram, BSN for their assistance with recruitment for this project.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.ajpc.2022.100364.
Appendix. Supplementary materials
References
- 1.Virani S.S., Alonso A., Benjamin E.J., Bittencourt M.S., Callaway C.W., Carson A.P., et al. Heart disease and stroke statistics-2020 update: a report from the American heart association. Circulation. 2020;141:e139–e596. doi: 10.1161/CIR.0000000000000757. [DOI] [PubMed] [Google Scholar]
- 2.Cushman M., Shay C.M., Howard V.J., Jiménez M.C., Lewey J., McSweeney J.C., et al. Ten-year differences in women’s awareness related to coronary heart disease: results of the 2019 American Heart Association National Survey: a special report from the American Heart Association. Circulation. 2021;143:239–e248. doi: 10.1161/CIR.0000000000000907Circulation. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wilmot K.A., O'Flaherty M., Capewell S., Ford E.S., Vaccarino V. Coronary heart disease mortality declines in the United States from 1979 through 2011: evidence for stagnation in young adults, especially women. Circulation. 2015;132:997–1002. doi: 10.1161/CIRCULATIONAHA.115.015293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arora S., Stouffer G.A., Kucharska-Newton A.M., Qamar A., Vaduganathan M., Pandey A., et al. Twenty year trends and sex differences in young adults hospitalized with acute myocardial infarction. Circulation. 2019;139:1047–1056. doi: 10.1161/CIRCULATIONAHA.118.037137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ford E.S., Capewell S. Coronary heart disease mortality among young adults in the U.S. from 1980 through 2002: concealed leveling of mortality rates. J Am Coll Cardiol. 2007;50:2128–2132. doi: 10.1016/j.jacc.2007.05.056. [DOI] [PubMed] [Google Scholar]
- 6.Lane-Cordova A.D., Khan S.S., Grobman W.A., Greenland P., Shah S.J. Long-term cardiovascular risks associated with adverse pregnancy outcomes: JACC review topic of the week. J Am Coll Cardiol. 2019;73:2106–2116. doi: 10.1016/j.jacc.2018.12.092. [DOI] [PubMed] [Google Scholar]
- 7.Wilkins-Haug L., Celi A., Thomas A., Frolkis J., Seely E.W. Recognition by women's health care providers of long-term cardiovascular disease risk after preeclampsia. Obstet Gynecol. 2015;125:1287–1292. doi: 10.1097/AOG.0000000000000856. [DOI] [PubMed] [Google Scholar]
- 8.Brener A., Lewnard I., Mackinnon J., Jones C., Lohr N., Konda S., et al. Missed opportunities to prevent cardiovascular disease in women with prior preeclampsia. BMC Womens Health. 2020;20:217. doi: 10.1186/s12905-020-01074-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harris P.A., Taylor R., Minor B.L., Elliott V., Fernandez M., O'Neal L., et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95 doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wagner J., Lacey K., Chyun D., Abbott G. Development of a questionnaire to measure heart disease risk knowledge in people with diabetes: the Heart Disease Fact Questionnaire. Patient Educ Couns. 2005;58:82–87. doi: 10.1016/j.pec.2004.07.004. [DOI] [PubMed] [Google Scholar]
- 12.Simeone R.M., Downing K.F., Wallace B., Galang R.R., DeSisto C.L., Tong V.T., et al. Changes in rates of adverse pregnancy outcomes during the COVID-19 pandemic: a cross-sectional study in the United States, 2019-2020. J Perinatol. 2022;42:617–623. doi: 10.1038/s41372-022-01327-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Osterman M., Hamilton B., Martin J.A., Driscoll A.K., Valenzuela C.P. Births: final data for 2020. Natl Vital Stat Rep. 2021;70:1–50. [PubMed] [Google Scholar]
- 14.Cameron N.A., Khan S.S. Leveraging mammography as a unique opportunity for cardiovascular health promotion. Circ Cardiovasc Imaging. 2022;15 doi: 10.1161/CIRCIMAGING.122.013977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spratling P.M., Pryor E.R., Moneyham L.D., Hodges A.L., White-Williams C.L., Martin J.N., Jr. Effect of an educational intervention on cardiovascular disease risk perception among women with preeclampsia. J Obstetr Gynecol Neonat Nurs. 2014;43:179–189. doi: 10.1111/1552-6909.12296. [DOI] [PubMed] [Google Scholar]
- 16.Traylor J., Chandrasekaran S., Limaye M., Srinivas S., Durnwald C.P. Risk perception of future cardiovascular disease in women diagnosed with a hypertensive disorder of pregnancy. J Mater Fetal Neonat Med. 2016;29:2067–2072. doi: 10.3109/14767058.2015.1081591. [DOI] [PubMed] [Google Scholar]
- 17.Brown M.C., Bell R., Collins C., Waring G., Robson S.C., Waugh J., et al. Women’s perception of future risk following pregnancies complicated by preeclampsia. Hypertens Pregnancy. 2013;32:60–73. doi: 10.3109/10641955.2012.704108. [DOI] [PubMed] [Google Scholar]
- 18.Seely E.W., Rich-Edwards J., Lui J., Nicklas J.M., Saxena A., Tsigas E., et al. Risk of future cardiovascular disease in women with prior preeclampsia: a focus group study. BMC Pregnancy Childbirth. 2013;13:240. doi: 10.1186/1471-2393-13-240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Burgess A., Feliu K. Women's knowledge of cardiovascular risk after preeclampsia. Nurs Women's Health. 2019;23:424–432. doi: 10.1016/j.nwh.2019.07.001. [DOI] [PubMed] [Google Scholar]
- 20.Zera C.A., Nicklas J.M., Levkoff S.E., Seely EW. Diabetes risk perception in women with recent gestational diabetes: delivery to the postpartum visit. J Mater Fetal Neonat Med. 2013;26:691–696. doi: 10.3109/14767058.2012.746302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mosca L., Benjamin E.J., Berra K., Bezanson J.L., Dolor R.J., Lloyd-Jones D.M., et al. Effectiveness-based guidelines for the prevention of cardiovascular disease in women–2011 update: a guideline from the American heart association. Circulation. 2011;123:1243–1262. doi: 10.1161/CIR.0b013e31820faaf8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bushnell C., McCullough L.D., Awad I.A., Chireau M.V., Fedder W.N., Furie K.L., et al. Guidelines for the prevention of stroke in women: a statement for healthcare professionals from the American heart association/American stroke association. Stroke. 2014;45:1545–1588. doi: 10.1161/01.str.0000442009.06663.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hypertension in pregnancy Report of the American college of obstetricians and gynecologists’ task force on hypertension in pregnancy. Obstetr Gynecol. 2013;122:1122–1131. doi: 10.1097/01.AOG.0000437382.03963.88. [DOI] [PubMed] [Google Scholar]
- 24.ACOG Committee opinion no. 736: optimizing postpartum care. Obstet Gynecol. 2018;131:e140–ee50. doi: 10.1097/AOG.0000000000002633. [DOI] [PubMed] [Google Scholar]
- 25.Scholten R.R., Hopman M.T., Lotgering F.K., Spaanderman M.E. Aerobic exercise training in formerly preeclamptic women: effects on venous reserve. Hypertension. 2015;66:1058–1065. doi: 10.1161/HYPERTENSIONAHA.115.05786. [DOI] [PubMed] [Google Scholar]
- 26.Timpka S., Stuart J.J., Tanz L.J., Rimm E.B., Franks P.W., Rich-Edwards J.W. Lifestyle in progression from hypertensive disorders of pregnancy to chronic hypertension in nurses' health study II: observational cohort study. BMJ. 2017;358:j3024. doi: 10.1136/bmj.j3024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Berks D., Hoedjes M., Raat H., Duvekot J.J., Steegers E.A.P., Habbema J.D.F. Risk of cardiovascular disease after pre-eclampsia and the effect of lifestyle interventions: a literature-based study. BJOG. 2013;120:927–931. doi: 10.1111/1471-0528.12191. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.