Abstract
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a viral pathogen that quickly became a global pandemic in the winter of 2020–2021. In response, governments issued social distancing orders to minimize transmission by reducing community contacts. We tested the efficacy of this social distancing at the state level during the first 2 months of the pandemic in the United States. We utilized data on daily SARS-CoV-2 case numbers and human community mobility (anonymized, aggregated cell phone location data stratified into six categories used as an index of social distancing), the date of government-issued social distancing orders, demographics, urbanization and public transportation. We implemented cross-correlation to identify lag times between declines in mobility and SARS-CoV-2 cases. Incorporating state-specific lag times, we tested for associations between case counts and mobility metrics using Bayesian multilevel models. Decreased mobility around grocery stores/ pharmacies, retail/recreation locations, transit stations and workplaces was correlated with decreases in SARS-CoV-2 cases with significant lag times of ≥21 days. Social distancing orders were associated with fewer cumulative SARS-CoV-2 cases when they were put in place earlier. Community mobility had already started declining prior to most social distancing orders, especially the more restrictive orders implemented later in the pandemic. Social distancing is an important tool that has been implemented throughout the pandemic to decrease SARS-CoV-2 transmission, although with significant social and economic impacts. Our results suggest that declines in cases were observed several weeks subsequent to implementation of social distancing measures, and that implementing social distancing earlier could potentially minimize the duration of time these policies need to be in effect. Our findings can inform ongoing management of this pandemic and other emerging infectious disease outbreaks by identifying areas where reductions in mobility are associated with reduced disease transmission, and the expected time frame between behavioural changes and measurable population outcomes.
Keywords: coronavirus, COVID-19, epidemic, pandemic, severe acute respiratory syndrome, social distancing
1 |. INTRODUCTION
A novel betacoronavirus emerged in December 2019 in Wuhan, Hubei province, China, where it caused a cluster of severe respiratory disease and pneumonia cases. It spread rapidly across the globe and was declared a pandemic by the World Health Organization in March 2020 (World Health Organization, 2020). The virus, named ‘severe acute respiratory syndrome coronavirus 2’ (SARS-CoV-2), caused the disease ‘COVID-19’ (Coronaviridae Study Group of the International Committee on Taxonomy of Viruses, 2020) and has been confirmed in nearly every country in the world and infected almost 270 million people (Johns Hopkins Coronavirus Resource Center, 2021).
The SARS-CoV-2 virus is highly contagious, with an instantaneous reproduction number (Rt) estimated at 3.1 (SD = 1.2) to 5.7 (SD = 2.5) across the United States of America (USA) during the first 2 weeks after 25 February 2020, when the pandemic was first introduced to the USA (Rubin et al., 2020). Person-to-person transmission is the driver of the current pandemic (Chan et al., 2020). Airborne transmission of respiratory secretions during close contact is currently believed to be the primary method of spread, although the role of other routes is still being investigated (Karia et al., 2020). The most common symptoms in people are fever, cough and fatigue, but a range of other symptoms are being identified that affect other organ systems (Grant et al., 2020). Due to high rates of pre-symptomatic and asymptomatic viral shedding (Li et al., 2020; Moghadas et al., 2020), transmission often occurs before infection is confirmed through diagnostic testing, posing challenges for contact tracing and quarantine.
The first positive case of SARS-CoV-2 in the USA was confirmed by the Centers for Disease Control and Prevention (CDC) on 20 January 2020 (Holshue et al., 2020), and all 50 states reported cases by mid-March 2020. Due to limited testing capabilities during the first months of the pandemic, testing was initially limited to individuals with fever and lower respiratory tract symptoms who also had a history of travel from China or close contact with a laboratory-confirmed SARS-CoV-2 patient within 14 days of symptom onset (Patel, 2020). Due to these limitations, community transmission in the USA went largely undetected during the early pandemic period.
To slow SARS-CoV-2 spread while testing capabilities increased, every state government in the USA instituted some kind of social distancing order (SDO) during March and April 2020. These SDOs varied in their scope, level of intensity and timing. Not all states enforced every type of SDO either; for example, only 38 states had instituted stay-at-home orders by April 30. This variation in the timing and location of SDOs provided an opportunity to investigate the impact of social distancing measures on the spread of SARS-CoV-2 at the state level.
Minimizing close contacts through social distancing is a key tool to rapidly decrease the propagation of directly transmitted pathogens, especially emerging infectious diseases for which vaccines are not yet available. Social distancing has limited the transmission of other infectious diseases, such as influenza (Fong et al., 2020), especially when distancing is instituted early in an epidemic and across a large proportion of the population (Kelso et al., 2009). However, widespread social distancing has significant impacts on livelihoods, social interactions, mental wellbeing and economies worldwide (Bonaccorsi et al., 2020; Brodeur et al., 2020; Fitzpatrick et al., 2020; Nicola et al., 2020; Rajkumar, 2020). Due to these far-reaching consequences, there is a need for critical scientific examination of the effectiveness of social distancing, especially during the early phases of response when strict social distancing would be most effective, but the epidemic potential of an emerging disease is not yet well characterized.
We hypothesized that social distancing, as measured by reductions in movement, resulted in subsequent declines in daily SARS-CoV-2 case incidence at the state level during the first 2 months of the pandemic in the USA. We expected that these case declines would occur after a temporal delay that varied by state, related to the timing of SDOs and the degree of mobility reduction achieved. We expected that the effect of social distancing on transmission was mediated by other factors that also increase contact among people, such as population size, number of people living in dense urban areas and public transportation use.
2 |. MATERIALS AND METHODS
2.1 |. Data collection
The daily count of new SARS-CoV-2 cases was reported by state public health websites and compiled by the COVID Tracking Project (The Atlantic Monthly Group, 2020d). Most states reported only laboratory-confirmed cases, but nine states combined these with ‘probable’ cases, defined as symptoms consistent with SARS-CoV-2 and a history of exposure to a SARS-CoV-2 patient or travel to an area with high SARS-CoV-2 prevalence, per the CDC case definition (Council of State & Territorial Epidemiologists, 2020). Both probable and confirmed cases, as reported by each state, were included in case incidence counts for modelling. Polymerase chain reaction (PCR) was the only diagnostic test widely available at the beginning of the pandemic (The Atlantic Monthly Group, 2020a), which reflects current or very recent infection. Some states began combining antibody test results (indicating previous infection) together with PCR test results in early May 2020 (The Atlantic Monthly Group, 2020c). We ended the study period on 30 April 2020 in order to better represent case incidence and not include previous infections. Each state entered the study on the first date they reported cumulative results from ≥10 tests (minimum date: 29 February 2020).
Inadequate testing during the early weeks of the epidemic resulted in apparent under-detection of cases. However, the relative trends of the epidemic curves are still useful for examining transmission patterns among states and correspond to similar trends in hospitalizations and deaths. Although hospitalization and mortality due to SARS-CoV-2 may be less likely to go undetected than infections, these measures are affected by additional confounders, such as comorbidities, disease severity and discrepancies in access to health care. Case counts are therefore a more appropriate index of new infections because they are more tightly associated temporally with transmission events.
State-issued SDOs (Institute for Health Metrics and Evaluation, University of Washington., 2020) included the closure of educational facilities, large gathering restrictions, initial closures of any businesses, closure of all non-essential businesses and stay-at-home orders. Cumulative SARS-CoV-2 cases in each state on the date SDOs went into effect was used as an index to reflect the timing of social distancing measures in relation to the level of transmission in each state, with fewer cases indicating that SDOs were enacted earlier.
Human movement (‘mobility’), in the form of anonymized location data aggregated from individual mobile phones (Google, 2020), was used as an index of dynamic changes in social distancing over time. ‘Baseline’ was the median amount of movement for a particular day of the week summarized over 3 January–6 February 2020 and represented ‘normal’ mobility immediately prior to the pandemic. Mobility after 6 February was calculated as the proportionate change in daily mobility relative to baseline for each day of the week. Mobility data were stratified by six different location categories: residential areas (e.g. houses and apartments), grocery stores and pharmacies, retail and recreation, transit stations, workplaces, and parks. Residential measurements were quantified as the average number of hours that a person spent at their residence, while all other categories were quantified as the number of visitors to a given type of location.
We accounted for time-invariant, state-level variables that may influence disease transmission. These include population size (US Census Bureau, 2019) and density (people/km2; US Census Bureau, 2020); annual number of airplanes passengers (Bureau of Transportation Statistics, 2018c) and trips on public transportation (‘transit ridership’) (Bureau of Transportation Statistics, 2018b); number of airports (Bureau of Transportation Statistics, 2020); proportion of the population: in poverty (Semega et al., 2019), without health insurance (Berchick et al., 2019), classified as an essential worker or healthcare worker (United Way of the National Capital Area, 2020) and using public transportation for commuting (Bureau of Transportation Statistics, 2018a); and proportion of the population living in areas classified as urban (densely developed areas with ≥2,500 people), an urban cluster (2,500–50,000 people), or an urban area (≥50,000 people; US Census Bureau, 2018a). Race/ethnicity reflects the proportion of the population self-identifying as Black, Indigenous American, Hispanic/Latino or any ‘non-White’ race in the US Census (groups were not mutually exclusive; US Census Bureau, 2018b, 2018c). Covariates that were not proportions were scaled to range from 0 to 1 but retain the relative differences between values.
2.2 |. Data analyses
Data evaluation and statistics were performed in R version 4.0.4 (R Core Team, 2021). Seven-day centred means (moving windows) were generated for the daily count of new SARS-CoV-2 cases and mobility values to smooth out variation related to the day of the week (e.g. case reporting was lower and parks mobility was higher on weekends; The Atlantic Monthly Group, 2020b). This resulted in 53 ± 4 days (mean ± SD) of data per state. We used case numbers rather than another disease metric, such as proportion of positive tests, because these metrics would have shown a false decrease in disease burden during the first weeks of the pandemic due to the number of daily tests performed increasing exponentially at a much faster rate relative to the number of cases.
At the start of the pandemic, when case numbers were increasing and mobility was starting to decline, these variables were negatively correlated. This correlation switched to positive as case numbers started to decline in some states. Lag times between reductions in mobility and declines in new cases were calculated using cross-correlation between case counts and mobility. Two independent measures were considered: (a) the number of days until the inflection point from negative to positive correlation (‘minimal correlation’), which is hypothesized to be the amount of time it took for social distancing to contribute to initial declines in case numbers, and (b) the number of days until the maximum positive correlation, which could reflect the time it took for social distancing efforts to have maximal effects on case incidence.
The extent of social distancing that occurred prior to government-issued restrictions was calculated as the proportionate change in mobility that had already occurred on the day an SDO was put into place, relative to the maximum change in mobility each state achieved over the entire study period.
To test for associations between time-invariant, state-level predictors and pandemic severity, we implemented a Bayesian, negative binomial regression with a log link and no random effects. For these ‘cumulative case models’, the outcome was the cumulative count of cases in each state on 30 April. We tested for associations between predictors using Spearman’s rank correlation, and correlated variables (significant at p < .05) were not included in the same model. Models were compared using leave-one-out cross-validation information criterion (LOO IC) using the ‘loo’ package (Vehtari et al., 2017, 2020). The predictors in the top model were used in the next phase of modelling.
To test for associations between mobility and case counts, we implemented a Bayesian, multilevel, negative binomial regression with a log link and random effects, as follows:
For these ‘mobility models’, γijk represents the outcome of daily SARS-CoV-2 case counts and xlijk represents the time-varying predictor of daily mobility for each observation (i). Mobility was lagged by the number of days until maximum positive correlation as identified by cross-correlation analysis; this lag was unique for each state. We included random intercepts for each state (u0j) to account for resampling, and random slopes based on the number of days since a state entered the study (ulk) to account for different within-state relationships between mobility and case numbers and the temporal non-independence of these variables (Goldberg et al., 2016; Yang & Land, 2006). An autoregressive model was not implemented due to the overdispersed nature of the outcome variable necessitating the use of a negative binomial model, which accounts for variance in the data by use of an overdispersion parameter rather than Gaussian distributed residuals. Model building included running models with just mobility predictors, then adding time-invariant predictors (such as number of airports) from the top cumulative case models. Convergence of chains was assessed by checking that the potential scale reduction (R) equaled one and visually assessing the trace plots for evidence of non-convergence. Posterior predictive density plots were used to compare empirical values of the outcome variable to simulated replications (n = 1,000) of the outcome drawn from the model’s posterior predictive distribution.
Multiple mobility categories were not included together in the same models since they represented interrelated behaviours (e.g. as workplace mobility declined due to more people working from home, residential mobility inherently increased concurrently). Models containing the same mobility predictors were compared using LOO IC (Vehtari et al., 2017, 2020).
Regression models were implemented using the ‘brms’ package (Bürkner, 2017, 2018). Weak priors were selected for the intercept [Normal (0, 10)], beta [Normal (0, 1)] and shape [Gamma (0.01, 0.01)] parameters and each model contained four chains with 10,000 iterations each. The 95% highest density interval was used as the credible interval (CI).
3 |. RESULTS
We demonstrate a strong positive association between social distancing in the form of reduced community mobility and decreases in SARS-CoV-2 case incidence at the state level. Specifically, decreased movement around grocery stores/pharmacies, retail/recreation locations, transit stations and workplaces was most strongly associated with decreases in SARS-CoV-2 cases after significant lag times of 38–41 days. When put into place earlier, SDOs were associated with fewer cumulative cases, but community mobility had already began declining before SDOs were issued.
3.1 |. Trends in community mobility
Mobility for grocery stores/pharmacies showed a small spike of 18% (median) over baseline during the first three weeks of March in all states except Hawaii, corresponding to people shopping in preparation for stay-at-home orders and anticipated shortages. Mobility for grocery stores/pharmacies then declined to a maximum of 19% below baseline (median) and plateaued by April. Mobility in residential areas increased during the middle two weeks of March then plateaued to a maximum 18% above baseline (median), reflecting people staying at home more often. Mobility around parks was highly variable for all states and over time, with no consistent pattern, likely because many states had less restrictive policies regarding the use of outdoor spaces. The minimum use of parks ranged from 68% below to 20% above baseline (Figure 1, Table S1, Figure S1).
FIGURE 1.
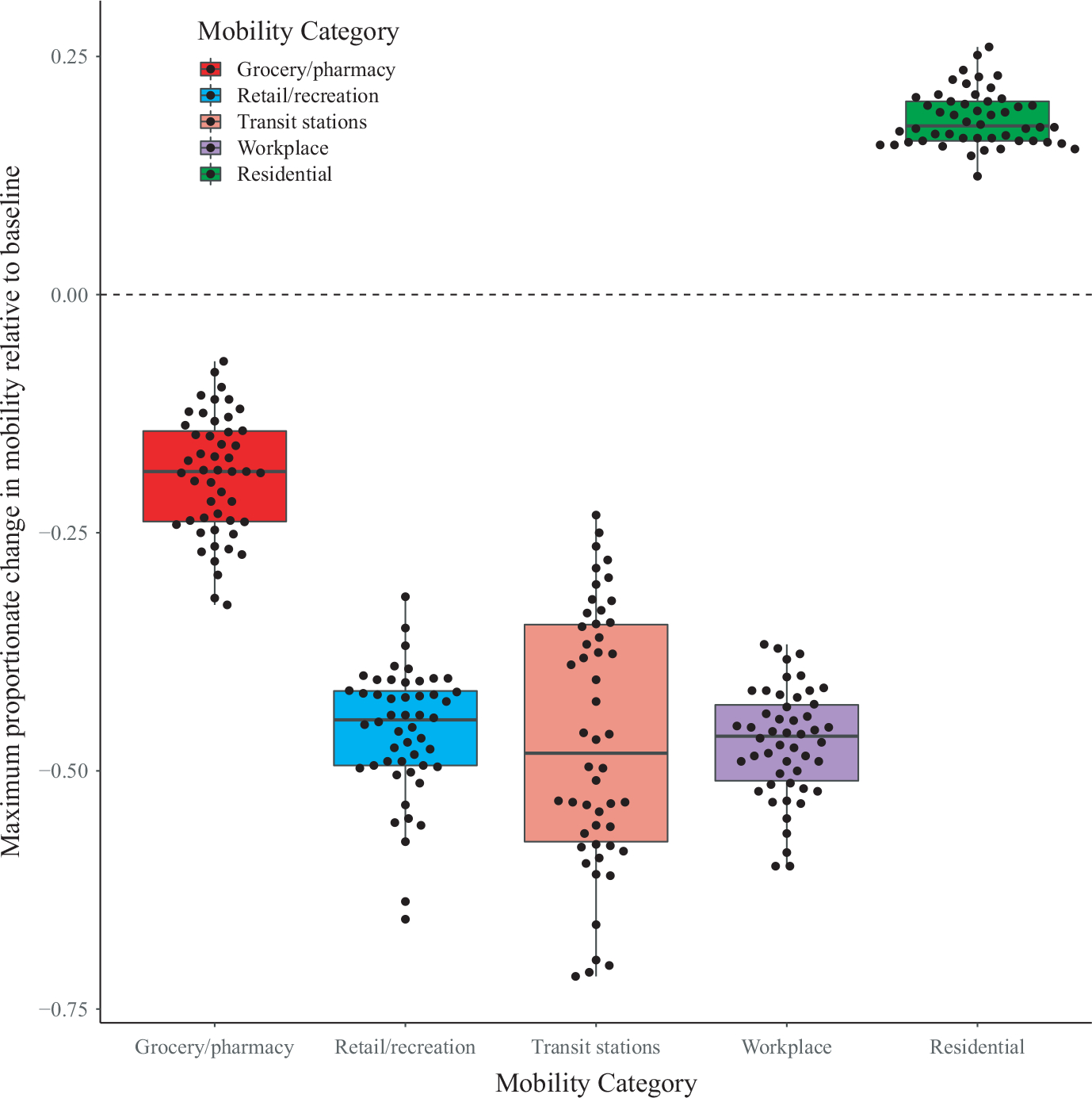
Maximum proportional change in mobility compared with baseline (baseline = 0) achieved by each state, over the course of the study period (29 February-30 April 2020). Each data point represents the value for one state, and box and whisker plots compare the distribution of values among states within each mobility category. Mobility was measured as one of five categories based on the type of locations used by the public: grocery and pharmacy locations, retail and recreation locations, transit stations, workplaces and residential areas (e.g. houses and apartments). Residential mobility increased over the course of the study period (positive values relative to baseline), while all other mobility categories decreased (negative values relative to baseline). Note: Parks were not included in this figure because mobility around parks was highly variable and fluctuated erratically over time for all states
Mobility around retail/recreation locations, transit stations and workplaces were extremely correlated (R2 = .88–.90, p ≤ .001). Mobility in these categories declined in near parallel to a maximum of 45%, 48% and 46% below baseline respectively (median; Figure 1, Table S1, Figure S1). These categories represent areas that were avoided as the public became aware of the pandemic and were commonly closed when SDOs took effect.
Mobility started changing across all states and mobility categories at the beginning of the study, very often before SDOs were implemented (Figure S1). Social distancing orders that tended to occur earlier (e.g. large gathering restrictions, closure of educational facilities and initial businesses) had more variability in the degree of mobility reduction that had already occurred at the time they were instituted (Figure S2a–c). Non-essential services tended to be closed later (17 March-3 April), by which time 33 of 34 states had already reached ≥70% of the maximal change in residential mobility, ≥60% of the maximum change in retail/recreational mobility, ≥60% of the maximal change in transit station mobility and ≥69% of the maximal changes in workplace mobility (Figure S2d). By the time of stay-at-home orders (19 March-7 April), 100% of 38 states had already reached ≥70% of the maximal change in residential mobility, ≥60% of the maximum change in retail/recreational mobility, ≥68% of the maximal change in transit station mobility and ≥69% of the maximal changes in workplace mobility (Figure S2e). Parks and grocery stores/pharmacies were not included in this analysis due to these categories having more variable patterns of use during the time period in which SDOs were enacted. Four SDOs were not enacted by every state: gathering restrictions (enacted by 49 states), stay-at-home orders (enacted by 38 states), any business closure (enacted by 47 states) and closure of non-essential services (enacted by 34 states).
3.2 |. Temporal correlation between mobility and case count
Grocery stores/pharmacies, transit stations, retail/recreation locations and workplaces generally had a negative correlation with cases at the start of the study when mobility was declining and cases were increasing. Minimal correlation occurred after a 21-to 23-day lag and maximal positive correlation peaked after a 38- to 41-day lag (median; Figure 2, Table S2, Figure S3a–d). Residential mobility initially had a positive correlation with cases, peaking after a 2-day lag, and minimal correlation occurring after a 23-day lag when cases were declining but residential mobility had plateaued and remained high (Figure 2, Table S2, Figure S3e). Parks mobility had variable correlations with cases numbers, both between states and over time, with most states having undulating cross-correlation curves as park use fluctuated (Figure 2, Table S2, Figure S3f).
FIGURE 2.
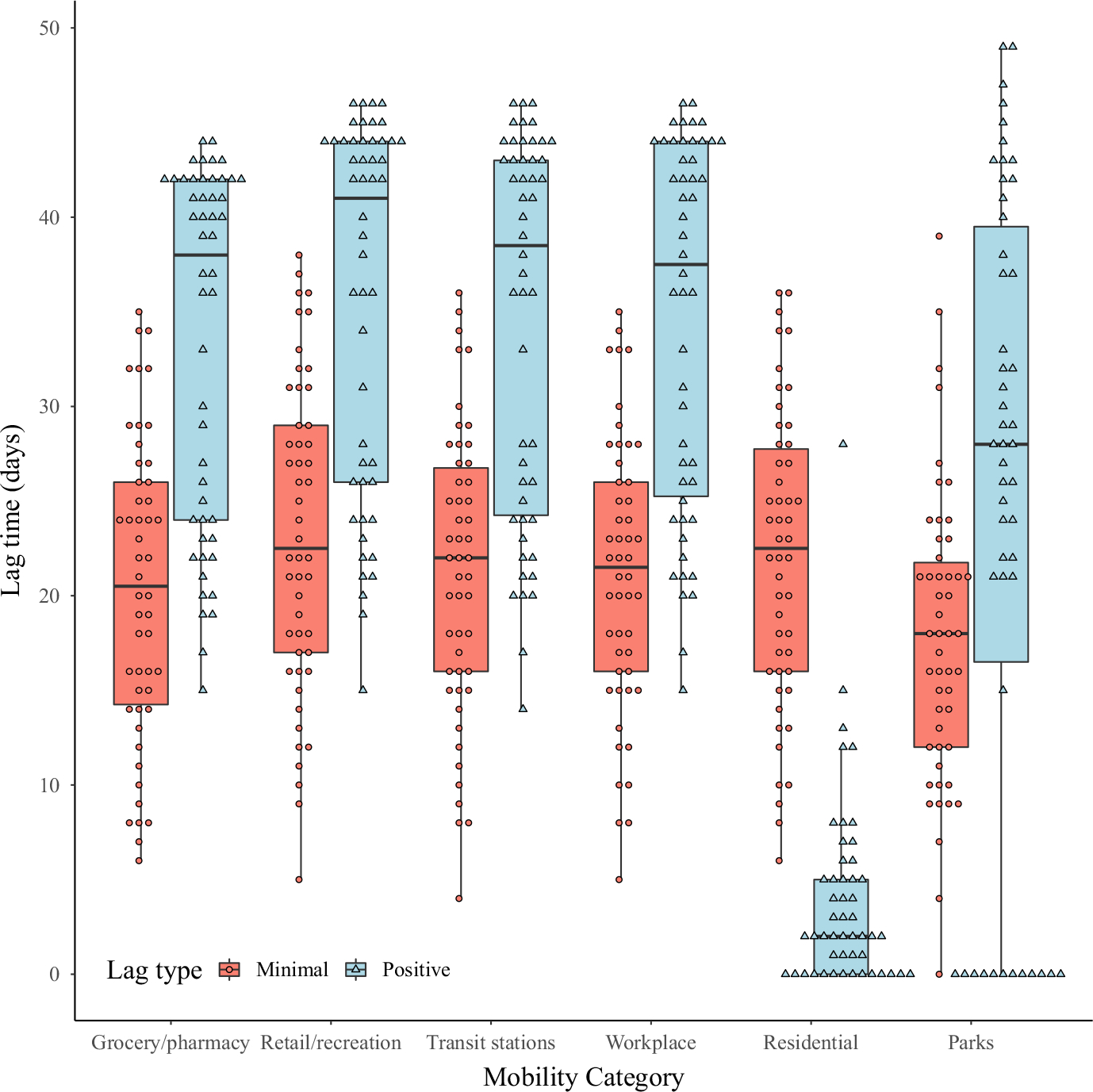
Lag time (in days) between reductions in daily mobility measurements and declines in daily case incidence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the United States, as estimated from cross-correlation analyses. Each data point represents the value for one state, and box and whisker plots compare the distribution of values among states within each mobility category and lag type. Two independent measures were considered: (a) the number of days until the inflection point from negative to positive correlation (‘minimal correlation’), which is hypothesized to be the amount of time it took for social distancing to contribute to initial declines in case numbers, and (b) the number of days until the maximum positive correlation, which could reflect the time it took for social distancing efforts to have maximal effects on case incidence. Mobility was measured as one of six categories based on the type of locations used by the public: grocery and pharmacy locations, retail and recreation locations, transit stations, workplaces, residential areas (e.g. houses and apartments) and parks
3.3 |. The associations of mobility with SARS-CoV-2 cases
Significant positive associations with cumulative SARS-CoV-2 case counts were detected for population size and density, population in poverty, population living in any type of urban centre, population commuting on public transportation, transit ridership, number of airports, airline passengers and the number of SARS-CoV-2 cases on the day the following SDOs were enacted: educational facility closure, stay-at-home orders, initial business closure and non-essential services closure (Table S3). The top cumulative case model contained the population living in an urban area (β = 36.47, 95% CI = 10.83–107.26) and the number of airports (β = 1.68, 95% CI = 1.30–2.22, R2 Bayes = 0.3, LOO IC = 741.1), and these variables were included in mobility models (Table S3).
Once urban area and airports were controlled for, lagged mobility around grocery stores/pharmacies (β = 2.25, 95% CI = 2.02–2.51), retail/recreation locations (β = 1.46, 95% CI = 1.32–1.62), transit stations (β = 1.46, 95% CI = 1.32–1.66) and workplaces (β = 1.72, 95% CI = 1.51–1.97) had positive associations with daily SARS-CoV-2 case count (Figure 3, Table S4). Parks were not associated with case count (β = 1.04, 95% CI = 0.90–1.20). Models had very similar point estimates, and LOO IC values regardless of whether urban area and the number of airports were included (Table S4).
FIGURE 3.
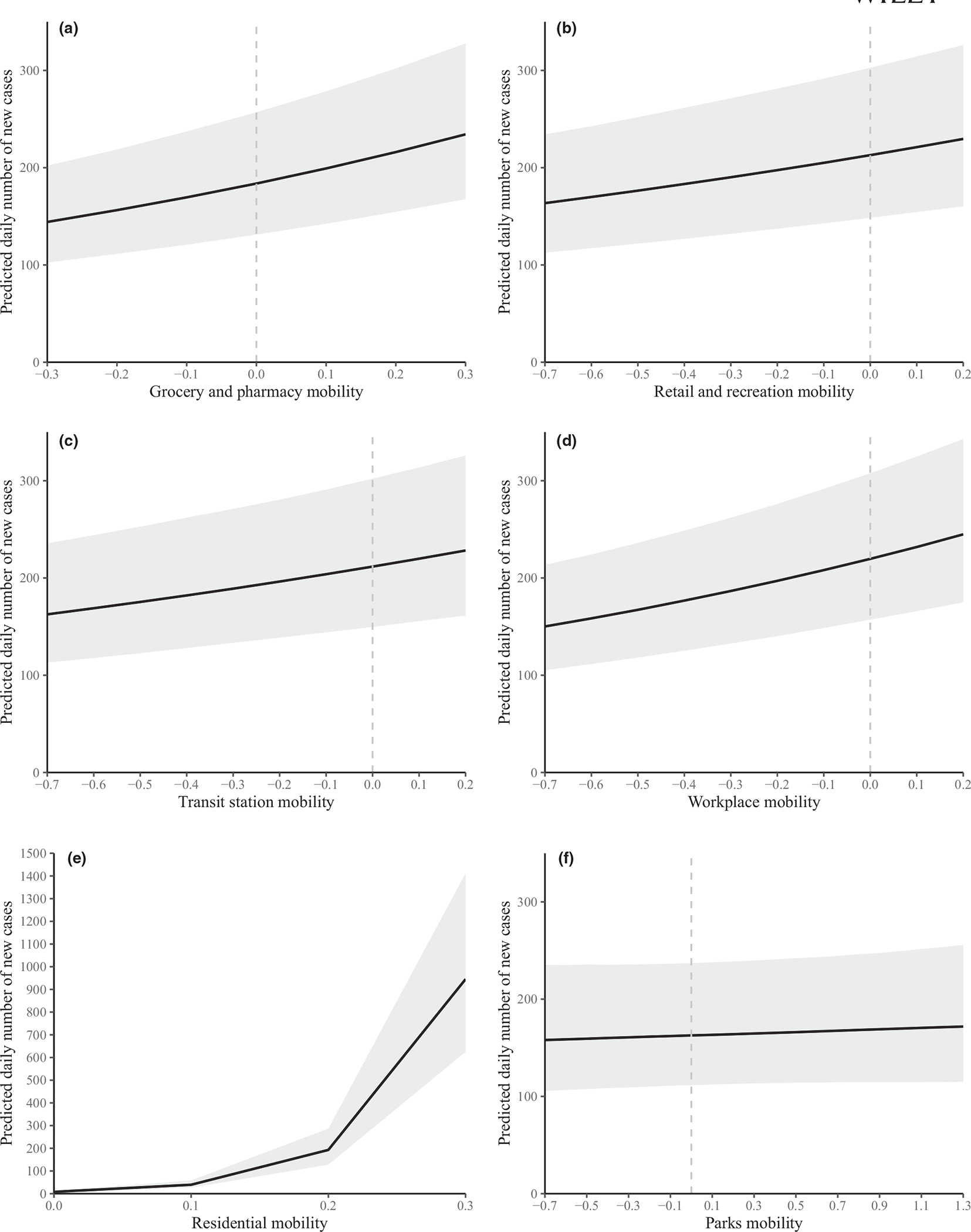
Plot of predictions from the final six ‘mobility models’, each testing the association between reductions in community mobility (as measured by anonymized location data aggregated from mobile phones) and the daily number of new severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) cases. Each model measured mobility in one of six categories based on the type of locations used by the public: (a) grocery stores and pharmacies, (b) retail and recreation locations, (c) transit stations, (d) workplaces, (e) residential areas (e.g. houses, apartments) and (f) parks. The proportion of the population living in an urban area and the number of airports were also controlled for as covariates. The state was used as a random intercept and the number of days since a state entered the study was used as the random slope
Mobility around residential areas was also positively associated with case count but the point estimates, 95% CI, and LOO IC were extremely large (β = 80,515,75.63, 95% CI = 5,488,097.66-11,874,990.68, LOO IC = 24,601.4; Figure 3, Table S4). These unrealistic estimates were due to case numbers continuing to increase exponentially as the residential mobility curve plateaued once people were spending a peak number of hours at home. As there are only 24 hr in a day, there was a limit to the increase in time someone could spend at home, compared with case numbers which could theoretically increase to include the entire population of a state. We expect that increased time spent at home would not be a predictor of cases but rather a public reaction to increasing case numbers, although more time spent at home could in turn contribute to eventual reductions in overall community transmission.
4 |. DISCUSSION
This study is unique in incorporating data at daily timesteps to demonstrate that reductions in mobility specifically around grocery store/pharmacies, retail/recreation locations, transit stations and workplaces are associated with subsequent declines in SARS-CoV-2 cases. These are areas with a high degree of mixing among people from different households, and minimizing these interactions can be expected to slow the transmission of SARS-CoV-2. Our results support other studies using complimentary techniques to show that decreases in SARS-CoV-2 cases are associated with social distancing and/or the implementation of SDOs (Courtemanche et al., 2020; Dave et al., 2020; Friedson et al., 2020; Matrajt & Leung, 2020). Social distancing is a tool that can be implemented rapidly (compared with vaccine development) but is economically and socially costly, and unlikely to end an epidemic when used as a solitary strategy. This is especially true in the face of highly contagious and rapidly mutating pathogens, as demonstrated by the spread of highly transmissible SARS-CoV-2 variants (Washington et al., 2021).
The inflection point of correlation between SARS-CoV-2 cases and mobility occurred 3 weeks after initial reductions in mobility, and it took 5 to 6 weeks to see maximum correlation. These lag times are supported by previous work using difference-in-difference and synthetic control approaches to estimate that it took >3 weeks for cumulative cases counts to decline substantially after stay-at-home orders were put in place (Dave et al., 2020; Friedson et al., 2020). Lags between mobility and case detection may be due to several biological, logistical and social factors. The virus incubation period, delays and limits to testing, and pre-symptomatic or asymptomatic transmission events would all contribute to delays in case detection after infection. Decreasing mobility will decrease new transmission events, but daily case counts may not decline immediately due to recently acquired infections, which will continue to be detected as people start to feel ill and get tested. Although reductions in mobility can reduce new infections between households, the increased amount of time that people spend at home may increase within-household transmission secondary to household members being in close contact more often (Leclerc et al., 2020). Anticipated lag times, adjusted for evolving changes in testing availability, should be communicated to the public to manage expectations about the expected duration of social distancing interventions.
Lag times could be reduced through multiple mechanisms. Widely available testing early during an epidemic will provide individuals with the information they need to make informed decisions about personal behaviours such as isolation and quarantine (Funk et al., 2009). There is likely a feedback loop between the public perception of growing case numbers leading to declines in mobility, with these reductions in mobility subsequently leading to declines in case numbers. The directionality of this two-way interaction between behaviour and disease transmission likely changed over the course of our study period. If the goal is to motivate timely changes in public behaviours to reduce disease transmission, increased transparency and public communication regarding current epidemic conditions might also increase the speed and degree of mobility reduction prior to government guided SDOs.
Indeed, we found that the public had already started reducing their mobility by the time state-level SDOs were put into place, especially the more restrictive orders that occurred later in the pandemic. This is supported by event study regression analysis that found no effect of state-level stay-at-home orders on social mixing indices, and emergency declarations accounted for only 12% of social mixing reductions after 5 days, though this increased to 45% after 20 days (Gupta et al., 2020). This lack of state-level SDO impact may reflect unmeasured local ordinances and/or individual behaviour changes in response to news coverage of the pandemic. Cancellation of popular events may have encouraged the public to alter their behaviour ahead of SDOs, such as the cancellation of the remainder of the National Basketball Association season on 11 March in response to a player testing positive for SARS-CoV-2. However, our results demonstrate that SDOs were relatively more effective when put into place earlier, when there were fewer people infected, similar to work that found early adoption of stay-at-home orders resulted in the largest declines in SARS-CoV-2 cases (Dave et al., 2020). Despite this mixed support for direct effects, SDOs likely encouraged the public to continue social distancing by reinforcing the severity of the pandemic threat to public health and reducing opportunities for activities outside the home.
Important non-pharmaceutical interventions to control SARS-CoV-2 transmission were implemented concurrently or subsequently to SDOs, such as the use of facial coverings, staying >6 feet apart and frequent hand washing. These actions have reduced transmission of SARS-CoV-2 and other pathogens (Chu et al., 2020; Fong et al., 2020; Lyu & Wehby, 2020; Telles et al., 2021), and public awareness of these recommended interventions increased over time (Lin et al., 2020), although there was geographic and demographic variation in compliance (Fisher, 2020). Mask use and city-wide sanitation measures may have been an important mechanism by which South Korea and China were able to keep case numbers low relative to other countries which also implemented social and physical distancing orders around the same time (Telles et al., 2021). The use of non-pharmaceutical interventions and declines in mobility are likely not independent, and there may have been additive or multiplicative interactions among these behaviours.
The time-invariant, state-level variables represented different but overlapping aspects of population density and clustering, all of which had positive correlations with case numbers, although likely for different reasons. For example, larger airports, especially those with a high number of international routes, could lead to higher risk of initial seeding of disease into a state, whereas numerous urban centres may contribute to sustained disease transmission once introduced. There are also intricate relationships between poverty, race, ethnicity, livelihood, health care access and urbanization, as demonstrated by urbanization mediating the association between human immunodeficiency virus (HIV) prevalence and poverty levels, and racial/ethnic disparities in HIV prevalence being reduced once poverty was controlled for (Mackey et al., 2021; Vaughan et al., 2014; Walton & Willyard, 2020). Although we controlled for these factors in our modelling, variables as measured did not greatly improve model fit, demonstrating that most of the variability in the data was explained by the mobility parameters and state-level groupings. Although this association between higher human densities and more SARS-CoV-2 cases is intuitive, some areas with high population densities, such as Taiwan, have been largely successful in controlling their outbreaks through proactive testing, contact tracing, strict social distancing, widely available face masks and limited international travel (Wang et al., 2020).
Park mobility was not significantly associated with SARS-CoV-2 cases, likely because people could utilize these areas while still physically distancing. Recent evidence demonstrates that outdoor spaces are low risk for SARS-CoV-2 transmission and support the use of outdoor spaces to improve physical and mental wellbeing during the pandemic (Bulfone et al., 2021; Leclerc et al., 2020).
Mobile phone data not only provide a wealth of information but also introduce potential biases if there are different mobility behaviours between people who have mobile phones compared with those who do not. Mobile phone use in the USA is high, with 81% of people owning a smartphone, but smartphone use was lower among older age groups and lower education and income levels (Taylor & Silver, 2019), groups which were disproportionally impacted by SARS-CoV-2 (Killerby et al., 2020; Leclerc et al., 2020).
This study demonstrates that social distancing, in the form of mobility reductions, is associated with subsequent declines in SARS-CoV-2 cases, albeit with significant lag times of 3 weeks or more. This decline, in combination with the fact that our study showed that the public made significant mobility reductions prior to state-level SDOs, highlights the importance of early and accurate public health communication to inform individuals of preventative measures they can personally implement, especially in the absence of government-mandated guidelines. Social distancing is likely to be most effective when done proactively at the start of an epidemic, which should be communicated to the public to encourage support and compliance with SDOs. Social distancing can be an effective epidemic response tool to slow transmission while developing testing and hospital capacity, quarantine protocols and pharmaceutical interventions, such as vaccinations.
Supplementary Material
Impacts.
Reductions in community mobility around workplaces, transit stations, retail/recreation locations and grocery store/pharmacies were associated with subsequent declines in SARS-CoV-2 cases, but these declines in cases occurred after lag times of three weeks or more. Park visitation was not associated with SARS-CoV-2 case numbers.
Mobility metrics declined prior to government-issued social distancing orders, but early implementation of these orders was correlated with lower cumulated SARS-CoV-2 cases.
Social distancing can be an effective epidemic response tool to slow transmission while developing other control measures, such as vaccinations.
ACKNOWLEDGEMENTS
We thank Laura H. Backus, Peter J. Sebastian, Sarah T. Abusaa, Jose Pablo Gomez, Cristin C. Young, Pranav S. Pandit and Rima D. Shrestha for their support and scientific advice. Research reported in this publication was supported by the United States National Institutes of Health (grant number: T32 OD 011147) and the National Institute of Allergy and Infectious Diseases of the National Institutes of Health (award number: U01AI151814). Content is solely the responsibility of the authors.
Funding information
National Institutes of Health, Grant/Award Number: T32 OD 011147; National Institute of Allergy and Infectious Diseases of the National Institutes of Health, Grant/Award Number: U01 AI1 51814
Footnotes
CONFLICT OF INTERESTS
The authors declare they have no conflicts of interest.
ETHICS STATEMENT
This manuscript does not contain any studies with human participants or animals performed by any of the authors. The data used in this study are publicly available, anonymous and aggregated. Therefore, Institutional Review Board approval was not required, and informed consent was not possible.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of the article at the publisher’s website.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are openly available in Mendeley Data at https://data.mendeley.com/datasets/bjpjr25gdj.1.
REFERENCES
- Berchick ER, Barnett JC, & Upton RD (2019). Health insurance in the United States: 2018 (No. P60–267(RV); Current Population Reports, p. 44). U.S. Census Bureau. https://www.census.gov/data/tables/2019/demo/health-insurance/p60-267.html [Google Scholar]
- Bonaccorsi G, Pierri F, Cinelli M, Flori A, Galeazzi A, Porcelli F, Schmidt AL, Valensise CM, Scala A, Quattrociocchi W, & Pammolli F (2020). Economic and social consequences of human mobility restrictions under COVID-19. Proceedings of the National Academy of Sciences of the United States of America, 117(27), 15530–15535. 10.1073/pnas.2007658117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brodeur A, Gray DM, Islam A, & Bhuiyan S (2020). A literature review of the economics of Covid-19 (SSRN Scholarly Paper ID 3636640). Social Science Research Network, https://papers.ssrn.com/abstract=3636640 [Google Scholar]
- Bulfone TC, Malekinejad M, Rutherford GW, & Razani N (2021). Outdoor transmission of SARS-CoV-2 and other respiratory viruses: A systematic review. The Journal of Infectious Diseases, 223(4), 550–561. 10.1093/infdis/jiaa742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bureau of Transportation Statistics (2018a). Commute mode. https://cms.bts.gov/commute-mode [Google Scholar]
- Bureau of Transportation Statistics (2018b). State transportation by the numbers. https://cms.bts.gov/content/state-transportion-numbers
- Bureau of Transportation Statistics. (2018c). U.S. airline traffic by airport. https://cms.bts.gov/us-airline-traffic-airport
- Bureau of Transportation Statistics (2020). Part 139 Airports. https://cms.bts.gov/part-139-airports
- Bürkner P-C (2017). brms: An R package for Bayesian multilevel models using Stan. Journal of Statistical Software, 80(1), 1–28. 10.18637/jss.v080.i01 [DOI] [Google Scholar]
- Bürkner P-C (2018). Advanced Bayesian multilevel modeling with the R package brms. The R Journal, 10(1), 395–411. 10.32614/RJ-2018-017 [DOI] [Google Scholar]
- Chan J-W, Yuan S, Kok K-H, To K-W, Chu H, Yang J, Xing F, Liu J, Yip C-Y, Poon R-S, Tsoi H-W, Lo S-F, Chan K-H, Poon V-M, Chan W-M, Ip JD, Cai J-P, Cheng V-C, Chen H, … Yuen K-Y (2020). A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: A study of a family cluster. The Lancet, 395(10223), 514–523. 10.1016/S0140-6736(20)30154-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ, Chu DK, Akl EA, El-harakeh A, Bognanni A, Lotfi T, Loeb M, Hajizadeh A, Bak A, Izcovich A, Cuello-Garcia CA, Chen C, Harris DJ, Borowiack E, … Schünemann HJ (2020). Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: A systematic review and meta-analysis. The Lancet, 395(10242), 1973–1987. 10.1016/S0140-6736(20)31142-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coronaviridae Study Group of the International Committee on Taxonomy of Viruses (2020). The species severe acute respiratory syndrome-related coronavirus: Classifying 2019-nCoV and naming it SARS-CoV-2. Nature Microbiology, 5(4), 1–9. 10.1038/s41564-020-0695-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Council of State and Territorial Epidemiologists. (2020). Standardized surveillance case definition and national notification for 2019 novel coronavirus disease (COVID-19) (Interim-20-ID-01; CSTE Position Statement(s), p. 10). https://wwwn.cdc.gov/nndss/conditions/coronavirus-disease-2019-covid-19/case-definition/2020/
- Courtemanche C, Garuccio J, Le A, Pinkston J, & Yelowitz A (2020). Strong social distancing measures in the United States reduced the COVID-19 growth rate. Health Affairs, 39(7), 1237–1246. 10.1377/hlthaff.2020.00608 [DOI] [PubMed] [Google Scholar]
- Dave DM, Friedson AI, Matsuzawa K, & Sabia JJ (2020). When do shelter-in-place orders fight COVID-19 best? Policy heterogeneity across states and adoption time (Working Paper No. 27091; Working Paper Series). National Bureau of Economic Research. 10.3386/w27091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher KA, Barile JP, Guerin RJ, Vanden Esschert KL, Jeffers A, Tian LH, Garcia-Williams A, Gurbaxani B, Thompson WW, & Prue CE (2020). Factors associated with cloth face covering use among adults during the COVID-19 pandemic–united States, April and May 2020. Morbidity and Mortality Weekly Report, 69(28), 933–937. 10.15585/mmwr.mm6928e3 [DOI] [PubMed] [Google Scholar]
- Fitzpatrick KM, Harris C, & Drawve G (2020). Fear of COVID-19 and the mental health consequences in America. Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1), S17–S21. 10.1037/tra0000924 [DOI] [PubMed] [Google Scholar]
- Fong MW, Gao H, Wong JY, Xiao J, Shiu EYC, Ryu S, & Cowling BJ (2020). Nonpharmaceutical measures for pandemic influenza in nonhealthcare settings—Social distancing measures. Emerging Infectious Diseases, 26(5), 976–984. 10.3201/eid2605.190995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedson AI, McNichols D, Sabia JJ, & Dave D (2020). Did California’s shelter-in-place order work? Early coronavirus-related public health effects (Working Paper No. 26992; Working Paper Series). National Bureau of Economic Research. 10.3386/w26992 [DOI] [Google Scholar]
- Funk S, Gilad E, Watkins C, & Jansen VAA (2009). The spread of awareness and its impact on epidemic outbreaks. Proceedings of the National Academy of Sciences of the United States of America, 106(16), 6872–6877. 10.1073/pnas.0810762106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg SB, Rousmaniere T, Miller SD, Whipple J, Nielsen SL, Hoyt WT, & Wampold BE (2016). Do psychotherapists improve with time and experience? A longitudinal analysis of outcomes in a clinical setting. Journal of Counseling Psychology, 63(1), 1–11. 10.1037/cou0000131 [DOI] [PubMed] [Google Scholar]
- Google LLC (2020). Google COVID-19 community mobility reports. https://www.google.com/covid19/mobility/
- Grant MC, Geoghegan L, Arbyn M, Mohammed Z, McGuinness L, Clarke EL, & Wade RG (2020). The prevalence of symptoms in 24,410 adults infected by the novel coronavirus (SARS-CoV-2; COVID-19): A systematic review and meta-analysis of 148 studies from 9 countries. PLoS One, 15(6), e0234765. 10.1371/journal.pone.0234765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta S, Nguyen TD, Rojas FL, Raman S, Lee B, Bento A, Simon KI, & Wing C (2020). Tracking public and private responses to the COVID-19 epidemic: Evidence from state and local government actions. In NBER Working Papers (No. 27027; Working Paper). National Bureau of Economic Research. https://ideas.repec.org/p/nbr/nberwo/27027.html [Google Scholar]
- Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, Spitters C, Ericson K, Wilkerson S, Tural A, Diaz G, Cohn A, Fox L, Patel A, Gerber SI, Kim L, Tong S, Lu X, Lindstrom S … Washington State 2019-nCoV Case Investigation Team (2020). First case of 2019 novel coronavirus in the United States. The New England Journal of Medicine, 382(10), 929–936. 10.1056/NEJMoa2001191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute for Health Metrics and Evaluation, University of Washington. (2020). COVID-19 projections. https://covid19.healthdata.org/projections
- Johns Hopkins Coronavirus Resource Center (2021). COVID-19 Map. Johns Hopkins Coronavirus Resource Center, https://coronavirus.jhu.edu/map.html [Google Scholar]
- Karia R, Gupta I, Khandait H, Yadav A, & Yadav A (2020). COVID-19 and its modes of transmission. SN Comprehensive Clinical Medicine, 2(10), 1798–1801. 10.1007/s42399-020-00498-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelso JK, Milne GJ, & Kelly H (2009). Simulation suggests that rapid activation of social distancing can arrest epidemic development due to a novel strain of influenza. BMC Public Health, 9(1), 117. 10.1186/1471-2458-9-117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killerby ME, Link-Gelles R, Haight SC, Schrodt CA, England L, Gomes DJ, Shamout M, Pettrone K, O’aughlin K, Kimball A, Blau EF, Burnett E, Ladva CN, Szablewski CM, Tobin-D’Angelo M, Oosmanally N, Drenzek C, Murphy DJ, Blum JM, … Wong KK (2020). Characteristics associated with hospitalization among patients with COVID-19–Metropolitan Atlanta, Georgia, March-April 2020. Morbidity and Mortality Weekly Report, 69(25), 790. 10.15585/mmwr.mm6925e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leclerc QJ, Fuller NM, Knight LE, Funk S, Knight GM & CMMID COVID-19 Working Group (2020). What settings have been linked to SARS-CoV-2 transmission clusters? Wellcome Open Research, 5, 83. 10.12688/wellcomeopenres.15889.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li R, Pei S, Chen B, Song Y, Zhang T, Yang W, & Shaman J (2020). Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV-2). Science, 368(6490), 489–493. 10.1126/science.abb3221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Y-H, Liu C-H, & Chiu Y-C (2020). Google searches for the keywords of “wash hands” predict the speed of national spread of COVID-19 outbreak among 21 countries. Brain, Behavior, and Immunity, 87, 30–32. 10.1016/j.bbi.2020.04.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyu W, & Wehby GL (2020). Community use of face masks and COVID-19: Evidence from a natural experiment of state mandates in the US. Health Affairs, 39(8), 1419–1425. 10.1377/hlthaff.2020.00818 [DOI] [PubMed] [Google Scholar]
- Mackey K, Ayers CK, Kondo KK, Saha S, Advani SM, Young S, Spencer H, Rusek M, Anderson J, Veazie S, Smith M, & Kansagara D (2021). Racial and ethnic disparities in COVID-19–related infections, hospitalizations, and deaths: A systematic review. Annals of Internal Medicine, 174(3), 362–373. 10.7326/M20-6306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matrajt L, & Leung T (2020). Evaluating the effectiveness of social distancing interventions to delay or flatten the epidemic curve of coronavirus disease. Emerging Infectious Diseases, 26(8), 1740–1748. 10.3201/eid2608.201093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moghadas SM, Fitzpatrick MC, Sah P, Pandey A, Shoukat A, Singer BH, & Galvani AP (2020). The implications of silent transmission for the control of COVID-19 outbreaks. Proceedings of the National Academy of Sciences of the United States of America, 117(30), 17513–17515. 10.1073/pnas.2008373117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicola M, Alsafi Z, Sohrabi C, Kerwan A, Al-Jabir A, Iosifidis C, Agha M, & Agha R (2020). The socio-economic implications of the coronavirus pandemic (COVID-19): A review. International Journal of Surgery, 78, 185–193. 10.1016/j.ijsu.2020.04.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel A, Jernigan DB, Abdirizak F, Abedi G, Aggarwal S, Albina D, Allen E, Andersen L, Anderson J, Anderson M, Anderson T, Anderson K, Bardossy AC, Barry V, Beer K, Bell M, Berger S, Bertulfo J, Biggs H, … Yousef A (2020). Initial public health response and interim clinical guidance for the 2019 novel coronavirus outbreak: United States, December 31, 2019 – February 4, 2020. Morbidity and Mortality Weekly Report, 69(5), 140–146. 10.15585/mmwr.mm6905e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team (2021). R: A language and environment for statistical computing. R Foundation for Statistical Computing. https://www.R-project.org/
- Rajkumar RP (2020). COVID-19 and mental health: A review of the existing literature. Asian Journal of Psychiatry, 52, 102066. 10.1016/j.ajp.2020.102066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin D, Huang J, Fisher BT, Gasparrini A, Tam V, Song L, Wang X, Kaufman J, Fitzpatrick K, Jain A, Griffis H, Crammer K, Morris J, & Tasian G (2020). Association of Social Distancing, Population Density, and Temperature with the instantaneous reproduction number of SARS-CoV-2 in counties across the United States. JAMA Network Open, 3(7), e2016099. 10.1001/jamanetworkopen.2020.16099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semega J, Kollar M, Creamer J, & Mohanty A (2019). Income and poverty in the United States: 2018 (No. P60–266; Current Population Reports, p. 88). U.S. Census Bureau. https://www.census.gov/data/tables/2019/demo/income-poverty/p60-266.html [Google Scholar]
- Taylor K, & Silver L (2019). Smartphone ownership is growing rapidly around the world, but not always equally (p. 47). Pew Research Center: https://www.pewresearch.org/global/2019/02/05/smartphone-ownership-is-growing-rapidly-around-the-world-but-not-always-equally/
- Telles CR, Roy A, Ajmal MR, Mustafa SK, Ahmad MA, de la Serna JM, Frigo EP, & Rosales MH (2021). The impact of COVID-19 management policies tailored to airborne SARS-CoV-2 transmission: Policy analysis. JMIR Public Health and Surveillance, 7(4), e20699. 10.2196/20699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Atlantic Monthly Group (2020a). Data definitions. The COVID Tracking Project, https://covidtracking.com/about-data/data-defitions
- The Atlantic Monthly Group (2020b). Data FAQ. The COVID Tracking Project, https://covidtracking.com/about-data/faq
- The Atlantic Monthly Group (2020c). Position statement on antibody data reporting. The COVID Tracking Project, https://covidtracking.com/blog/antibody-data-reporting
- The Atlantic Monthly Group (2020d). The COVID Tracking Project. The COVID Tracking Project, https://covidtracking.com/
- United Way of the National Capital Area. (2020). U.S. States with the most essential workers. https://unitedwaynca.org/blog/us-states-with-the-most-essential-workers/
- US Census Bureau (2018a). 2010 census urban area lists record layouts. https://www.census.gov/programs-surveys/geography/techical-documentation/records-layout/2010-urban-lists-record-layout.html
- US Census Bureau. (2018b). 2018 American Community Survey 1-year estimates, Hispanic or Latino origin by race. Table B03002, https://data.census.gov/cedsci/table?q=hispanic&g=0100000US.04000.001&hidePreview=true&tid=ACSDT1Y2018.B03002&t=Hispanic%20or%20Lat?ino&vintage=2018&moe=false&tp=false
- US Census Bureau. (2018c). 2018 American Community Survey 1-year estimates, race. Table B02001, https://data.census.gov/cedsci/table?table=DP05&tid=ACSDT1Y2018.B02001&g=0100000US.04000.001&lastDisplayedRow=29&vintage=2018&cid=S0201_001E&hidePreview=false&moe=true&t-p=true&t=Race%20and%20Ethnicity
- US Census Bureau. (2019). State population totals and components of change 2010–2019. https://www.census.gov/data/tables/timesseries/demo/popest/2010s-state-total.html
- US Census Bureau. (2020). State area measurements and internal point coordinates. https://www.census.gov/geographies/reference-files2010/geo/state-area.html
- Vaughan AS, Rosenberg E, Shouse RL, & Sullivan PS (2014). Connecting race and place: A county-level analysis of white, Black, and Hispanic HIV prevalence, poverty, and level of urbanization. American Journal of Public Health, 104(7), e77–e84. 10.2105/AJPH.2014.301997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vehtari A, Gabry J, Magnusson M, Yao Y, Bürkner P, Paananen T, & Gelman A (2020). loo: Efficient leave-one-out cross-validation and WAIC for Bayesian models. R package version 2.4.1. https://mc-stan.org/loo/ [Google Scholar]
- Vehtari A, Gelman A, & Gabry J (2017). Practical Bayesian model evaluation using leave-one-out cross-validation and WAIC. Statistics and Computing, 27(5), 1413–1432. 10.1007/s11222-016-9696-4 [DOI] [Google Scholar]
- Walton TW, & Willyard KA (2020). Small area health insurance estimates: 2018 (No. P30–07; Current Population Reports, p. 13). US Census Bureau. https://www.census.gov/library/publications/2020/demo/p30-07.html [Google Scholar]
- Wang CJ, Ng CY, & Brook RH (2020). Response to COVID-19 in Taiwan: Big data analytics, new technology, and proactive testing. Journal of the American Medical Association, 323(14), 1341–1342. 10.1001/jama.2020.3151 [DOI] [PubMed] [Google Scholar]
- Washington NL, Gangavarapu K, Zeller M, Bolze A, Cirulli ET, Schiabor Barrett KM, Larsen BB, Anderson C, White S, Cassens T, Jacobs S, Levan G, Nguyen J, Ramirez JM, Rivera-Garcia C, Sandoval E, Wang X, Wong D, Spencer E, … Andersen KG (2021). Emergence and rapid transmission of SARS-CoV-2 B.1.1.7 in the United States. Cell, 184(10), 2587–2594.e7. 10.1016/j.cell.2021.03.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2020). Coronavirus Disease 2019 (COVID-19) Situation Report—51 (p. 9).
- Yang Y, & Land KC (2006). A mixed models approach to the age-period-cohort analysis of repeated cross-section surveys, with an application to data on trends in verbal test scores. Sociological Methodology, 36(1), 75–97. 10.1111/j.1467-9531.2006.00175.x [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are openly available in Mendeley Data at https://data.mendeley.com/datasets/bjpjr25gdj.1.


