Abstract
Vitamin has a major role in the functions of the immune system, and the efficacy of this vitamin in reducing inflammation has been identified. Considering the effects of vitamin D, this study research was performed for investigating the relationship between vitamin D and the severity of COVID-19 in children. This cross-sectional study was performed on 101 children infected with the new coronavirus from September 2020 to October 2021. Information on vitamin D levels, demographic factors, and clinical and laboratory findings were documented in information forms and prepared for statistical analyses. The average of children was 2.85 ± 0.85 years. Low oxygen saturation was observed in 35.3% of infected children. The level of involvement was higher in subjects with vitamin D levels higher than 30 and less than 10 ng/ml (p = 0.04). Clinical signs in cases with deficient and sufficient vitamin D levels were more severe in terms of tachypnea and tachycardia (p = 0.01). Children with vitamin D lower than 10 ng/ml showed more frequency (p = 0.02). Cases with moderate vitamin D had fewer gastrointestinal complications (p = 0.03). Also, oxygen levels were lower in children who had low levels of vitamin D (p = 0.02). Vitamin D levels were associated with levels of involvement, tachycardia, tachypnea, clinical signs, gastrointestinal problems, and O2 levels. Moderate vitamin D levels in children are a critical issue that should be considered.
Key Words: Vitamin D, COVID-19, coronavirus, children, pneumonia
Ethical Publication Statement
The author confirms that he has read the Journal's position on the issues involved in ethical publication and states that this report is consistent with those guidelines.
One of the most dangerous diseases worldwide is the new coronavirus disease (COVID-19). This virus causes inflammation in the airways, and a high percentage of cases need intensive care.1,2 The coronavirus has appeared two times in the last decade in the dangerous forms of MERS and SARS.3 Pneumonia is the most critical complication of COVID-19, and in patients with high severity, it is associated with an acute respiratory syndrome, and liver and kidney failure.4,5 The coronavirus 19 disease is milder in children than in adults. However, young people are not completely immune to the virus and they are not aware of the complications of the virus. Research has shown that newborns had more severe symptoms than older children.6 Vitamin D is among the effective vitamins in the inflammatory responses of the immune system, and unfortunately, previous findings demonstrate the deficiency of vitamin D in the Iranian population.7 Low concentrations of vitamin D increase the risk of coronavirus disease in children.8 Deficiency of this vitamin, by affecting liver function, increases the severity of coronavirus disease in people with risk factors such as obesity, diabetes, kidney and liver problems. Adequate levels of the vitamin can be suggested as a potential strategy for preventing and treating coronavirus disease.8, 9 Vitamin D is effective in decreasing the rate of microbial infections and mortality through various cellular mechanisms. This vitamin is also effective in decreasing the rate of common colds.10 One of the effective functions of this vitamin is the regulation of serum calcium concentrations, which has important functions in the body's metabolism.11 Vitamin D contributes to maintaining tight junctions, gap junctions, and cellular adhesions.9 It has been found that the role of cellular integration in infections by viruses and other microorganisms is highly important,12 and it also has a major role in reducing the structure of Th1 cytokines, which include tumor necrosis factor α and interferon γ.13 The innate immune system activates primary cytokines in individuals with coronavirus, and vitamin D enhances the specific function of the immune system to some extent by reducing the flow of cytokines,14 reducing primary inflammatory cytokines, and increasing the anti-inflammatory cytokines.15 Various studies have shown that coronavirus infection is related to incremented levels of proinflammatory cytokines and C-reactive proteins, and strategies to reduce the immune responses can be effective in reducing the severity of the COVID-19.14,16 Considering the effects of vitamin D on immunity and inflammation, the importance of children's health in society, and the high frequency of vitamin D deficiency in Iran, this research was performed for investigating the role of vitamin D on the severity of COVID-19 and its effects on infected children.
Material and Methods
Ethical considerations
All patients (patients' parents) signed informed consent to participate in this project. Researchers were committed to the confidentiality of patients' information at all stages of the project. This plan was approved by the Research Council of Iran University of Medical Sciences with the ethics code of IR.IUMS.FMD.REC.1400.003.
Study design
This cross-sectional analytical study was performed on 101 patients aged 1 month to 13 years referred to Hazrat Ali Asghar Hospital, who were tested positive for COVID-19 from September 2020 to October 2021. Eligible patients were enrolled in the project after receiving written consent from their parents.
Inclusion and exclusion criteria
Inclusion criteria were age between 1 month and 14 years, consent to participate in the study, and definite diagnosis of coronavirus disease. Exclusion criteria included decreased level of consciousness for reasons other than Covid-19 complications, chronic respiratory diseases, renal and hepatic diseases, history of chronic diseases, and the use of steroids and immunosuppressive drugs.
Procedure
After obtaining the necessary permits, the required information was extracted and recorded by referring to the hospital and studying children with coronavirus whose disease was confirmed by PCR or CT-Scan. Samples were selected through the available sampling method. The cases were monitored from the beginning of admission and the clinical course was completed by telephone after their discharge. In order to have easy access to the tests, the priority of choice was with the hospitalized patients. In case of the incompleteness of the information, the researcher received additional information through the phone calls, after providing a complete explanation about the study process. Then, after classifying the children in terms of disease severity, clinical and laboratory information were collected in the next step. During the study, the efficacy of vitamin D, the degree of fever, the severity of cough and shortness of breath, and possible gastrointestinal problems in patients were evaluated every forty-eight hours for two weeks. It should be noted that the evaluation of patients in the clinic was performed by nurses.
Data collection
Children were divided into 3 groups considering the severity of their diseases after being diagnosed with COVID-19: 1) non-severe pneumonia patients (cough with a respiratory rate of less than 60/min under 2 months of age, less than 50/min under one year, less than 40 for 1-4 years, and less than 30 for people over 5 years of age), and patients without risk factors in the history, examination, and laboratory test results, which were considered outpatients without the need for hospitalization. 2) Severe pneumonia patients (fever higher than or equal to 38.5 ° C, cyanosis, disturbance of level of consciousness, hypoxemia with 90% < SPO2 in room air, severe respiratory distress (including granting, difficult breathing, severe retraction, suprasternal retraction, intercostal or subcostal retractions, apnea, nasal flap jump, tachycardia, capillary refill time ≤ 2 seconds, mild to moderate dehydration symptoms, pneumonia with one of the warning signs), presence of danger signs in laboratory criteria and history (Existence of a score above 8 according to the protocols of the Ministry of Health), and the presence of Kawasaki-like symptoms), and this group of patients required hospitalization. 3) Severe pneumonia patients with symptoms of rapid breathing (higher than 60/min under 2 months of age, more than 50 per minute under one year, more than 40 for 1-4 years, and more than 30 for people over five years old), SPO2<90% in room air, tachypnea with shortness of breath, chest tightness, moaning, nasal flaps beating, and bruising of tongue and lips, decreased level of consciousness, significant change in vital signs requiring careful monitoring, inability to eat or drink, lack of communication when awake, excessive restlessness, and severe dehydration; this group required hospitalization in intensive care and supportive care units. All scores related to the extent of involvement were based on the COVID-19 flowchart for diagnosis and treatment at outpatient service levels. According to this guideline, according to the study population, the percentage of pulmonary involvement was classified was in 4 levels: less than 25%, 26 to 50, 51 to 75, and more than 75%.
Two cc blood samples were taken from all children immediately after the diagnosis to measure the level of vitamin D and other blood factors. Venous blood was collected in tubes that contained clot activator, and then were rapidly stored on ice. 60 minutes after collection, the samples were centrifuged at 10,000 rpm for 10 minutes. The plasma was isolated and analyzed at -80 °C. It should be noted that sampling was performed only once (immediately after diagnosis) and tests were performed in the hospital blood laboratory to assess vitamin D levels in three categories, including severe deficiency (less than 20), mild deficiency (21-30), and normal (more than 30 ng/ml).
Table 1.
Demographic and clinical features of children
| Variable | Parameter | Frequency | |
|---|---|---|---|
| Qty | % | ||
| Boy | 52 | 52.5 | |
| Gender | Girl | 47 | 47.5 |
| History of the use of Vitamin D | Yes | 45 | 45.5 |
| No | 54 | 54.5 | |
| Tachypnea | Yes | 38 | 38.4 |
| No | 61 | 61.7 | |
| Tachycardia | Yes | 46 | 46.5 |
| No | 53 | 53.5 | |
| Cough symptoms | Yes | 23 | 23.2 |
| No | 76 | 76.8 | |
| O2 level | 90-95 | 64 | 64.7 |
| <90 | 35 | 35.3 | |
| Gastrointestinal symptoms | Diarrhea | 74 | 86 |
| Vomiting | 59 | 69 | |
| Level of consciousness | Conscious | 85 | 85.9 |
| Confused | 12 | 12.1 | |
| Lethargic | 2 | 2.0 | |
The demographic information of cases and laboratory findings were documented in pre-designed forms and prepared for statistical analyses. The variables studied in this research included age, gender, degree of fever, shortness of breath, gastrointestinal function, and other underlying variables.
Biochemical analysis
Factors in children's plasma were assessed by high-performance liquid chromatography (HPLC) using Bio-Rad diagnostic kits (Bio-Rad, Munich, Germany), which are basically explained by the manufacturer. Other levels of biochemical-related metabolites were measured using Roche kits, Germany. Vitamin D levels were measured by chemiluminescence (DiaSorin Inc., Shanghai, Italy).
Statistical analysis
The data of this study included qualitative and quantitative variables, and descriptive and inferential statistical methods were implemented for analyzing the data through SPSS software version 25. In the first part of descriptive statistics, tables of frequency, as well as mean and standard deviation were used. In the second part, data analyses based on statistical inference were performed using the T-test and Chi-square test. P-values lower than 0.05 were assumed significant.
Results
Out of 101 children, 2 children were excluded from the study due to chronic diseases and dissatisfaction with participation, and 99 children were examined. The mean age was 2.85 ± 0.85 years, of which 52% were boys and 48% were girls. 46% of children had a history of taking vitamin D (as a therapeutic approach for children under the age of two and as a supplement for children over the age of two). Oxygen saturation of less than 90 was observed in 35.3% of affected children. The demographic and clinical findings can be found in Table 1. According to Figure 1, about 3% of the patients had bleeding and the others (97%) had no bleeding. Also, 5% of the patients had convulsions and the rest of them had no convulsions. About 42% of cases had dehydration and CRP levels more than 25 were reported in only 8% of children (Figure 2). Findings of the frequency of vitamin D levels by the age group showed that in 49 patients (52%) vitamin D levels were more than 30 ng/ml, and 65% of cases were over two years old. No statistically significant relationship was observed between age and vitamin D levels (p > 0.05). According to Table 3, the association among vitamin D levels and level of consciousness, levels of Ferritin, LDH, CRP, PLT, and dehydration in children was not significant (p > 0.05). But vitamin D deficiency was associated with higher involvement, tachycardia, tachypnea, clinical signs, gastrointestinal problems, and O2 levels (p < 0.01). The findings demonstrated that the level of involvement in cases with high and low levels of vitamin D was higher than others (p < 0.04). Further clinical signs were observed in children with severe vitamin D deficiency and high levels of this vitamin (p < 0.01). Regarding tachycardia and tachypnea, patients with vitamin D less than 10 ng/ml (severe vitamin D deficiency) showed a higher frequency (p < 0.02). In terms of gastrointestinal symptoms, children with moderate levels of vitamin D had fewer gastrointestinal complications. Oxygen levels were also lower in children with low levels of vitamin D (p < 0.02, p < 0.03). According to Table 4, 82.3% of the patients were hospitalized and 17.7% were outpatients. In 60 percent of the patients, the severity of the disease was at the hospital level, of which 18% had vitamin D lower than 20 and 82% had vitamin D above 20. 22% of patients had severe disease and required intensive care, of which 57% had vitamin D levels lower than 20 and 43% had vitamin D levels above 20. 18% had mild (outpatient) disease levels, of which 100% had more than 20 vitamin D. Statistical correlation findings demonstrated that vitamin D levels were considerably related with disease severity (p < 0.01). Findings of disease severity based on laboratory results showed that 54% had a disease severity between 5 and 7, 27% had a disease severity greater than 7, and 19% had a disease severity less than 5 (Table 5). Statistical correlation analyses showed that vitamin D levels were considerably related with disease severity based on laboratory results (p < 0.01). No mortality was observed in the patients of the present study.
Figure 1.
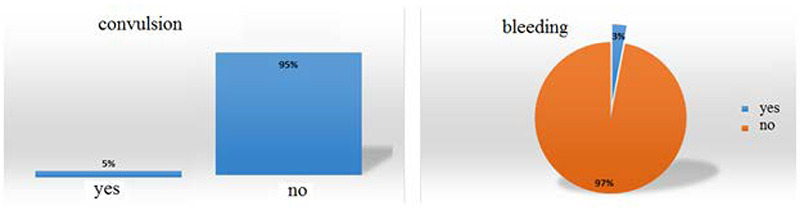
Frequency percentage of bleeding and convulsion
Figure 2.
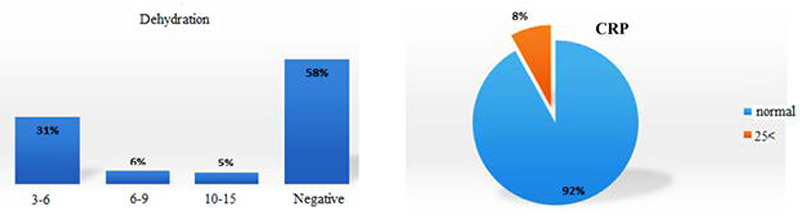
Frequency percentage of dehydration and CRP
Discussion
In addition to the roles of vitamin D in regulating calcium and phosphorus homeostasis and its efficacy on the intestine, kidneys, and bones, its role in immune system function has been previously identified. This issue has made it important to pay attention to the effective roles of this vitamin in acute and chronic diseases.8 In the present study, for the first time, the relationship between vitamin D and the severity of COVID-19 in children under 12 years of age was investigated. The findings of our study demonstrated that levels of this vitamin in individuals were related to tachycardia and tachypnea, gastrointestinal symptoms, and oxygen levels. Children with normal vitamin D levels also had diseases with lower severity, lower rate of involvement, and fewer gastrointestinal symptoms. This showed that patients with high and low vitamin D levels had more severe symptoms, and sufficient levels of vitamin D could be effective in decreasing symptoms and the rate of involvement of patients. A similar study in Iran demonstrated that the serum levels of vitamin D in the group of cases with coronavirus disease was considerably lower compared to the healthy group.17 Another study on the importance of vitamin D in cases with coronavirus disease demonstrated that despite the effects of vitamin D on the cytokine response, supplementary concentrations of this vitamin can be used to reduce the severe immune response.18 In another study, the severity of COVID-19 in children was categorized into five categories, including asymptomatic, mild, moderate, severe, and critical (very severe), considering the clinical signs, laboratory results, and chest radiographic findings. They showed that the levels of this vitamin in patients were considerably lower in comparison to the controls (p <0.001). In addition, the degree of fever was much higher in patients with low levels of this vitamin compared to cases with adequate vitamin D levels, and there was a reverse correlation between fever and vitamin D. In general, their results showed that the level of vitamin D in the pediatric population may be effective in the rate and severity of coronavirus disease.19 Limited research has been conducted on the association of vitamin D with coronavirus in children, but the findings on influenza and colds have shown that the levels of this vitamin can be effective. Camargo et al. have studied the role of vitamin D in reducing the symptoms of influenza and stated that vitamin D supplementation reduces the risk of developing severe respiratory diseases.20 Furthermore, Rondanell et al. in 2018, showed that vitamin D can reduce the symptoms of colds by increasing adaptive immunity in different parts of the immune system.10 The findings of the present study demonstrated that levels of vitamin D were related to levels of involvement, tachycardia, tachypnea, clinical signs, gastrointestinal problems, and O2 levels. Other similar findings indicated the efficacy of vitamin D on clinical symptoms in children with coronavirus.19,21 The effects of vitamin D on reducing the severity and symptoms and gastrointestinal problems of COVID-19 in adults has also been reported in several studies.22-24 However, little research has been done on children, and studies in the age group of children have not yet examined the efficacy of vitamin D on these variables. In this research, no significant relationship was observed among vitamin D levels and the level of consciousness, as well as Ferritin, LDH, CRP, and PLT levels. In other studies, similar results were observed.25, 26 In the study of the effects of vitamin D on the disease, it was observed that this vitamin plays a major role in the effective activation of innate immunity by modulating the immune system. The production of antimicrobial peptides (defensins and catalysidines) after the stimulation of toll-like receptors by pathogenic lipopeptides depends on adequate levels of vitamin D, and in various articles, a link has been found between vitamin D deficiency and respiratory disorders. Many studies have considered it important to provide randomized controlled trials to investigate this preventive effect.27 Regulatory T cells have a major role in the immune system by identifying and killing viruses. A biological study demonstrated that vitamin D can be effective in reducing coronavirus infection by activating regulatory T cells. They showed that many patients with coronavirus suffer from vitamin D deficiency, so by adding this vitamin to patients' diets, this reduction in T cells can be compensated.28 Vitamin D deficiency is a frequent problem that has considerable health consequences, and the effect of this vitamin on the immune system is less known. Nutrition and supplements are the major sources of this vitamin in winter because exposure to sunlight is not enough to produce vitamin D.27 Recent studies have shown that as the coronavirus pandemic increases, children are more likely to be trapped at home, and prolonged stay at home leads to an increment in the number of children with low levels of vitamin D during March and June 2020, in comparison with the same months in previous years.19,28,29 These findings indicate the importance of sunlight in the natural increase of vitamin D reserves in children.30-32 In general, in the present study, high vitamin D levels had a considerable relation with the severity of symptoms and a higher rate of involvement in patients with coronavirus disease, which indicates that controlled intake of vitamin D can have better effects on the immune system and prevention of excessive intake should be considered. One of the limitations of this research was the lack of access to the patients during the study, which was solved by appropriate planning. It is suggested that the efficacy of vitamin D on the recovery of children with coronavirus would be measured in future clinical trials. Also, the present study was conducted in one center, and conducting this research in several centers can lead to more accurate results.
Table 2.
Distribution of Levels of vitamin D by age group
| Vitamin D levels (ng/mL) | p-value | |||||
|---|---|---|---|---|---|---|
| Age | Less than 10 | 10-20 | 21-30 | More than 30 | Total | |
| Under two years | 45.0% | 47.7% | 46.0% | 53.7% | 47.4% | 0.20 |
| More than two years | 55.0% | 52.3% | 54.0% | 46.3% | 52.6% | |
| Total | 100% | 100% | 100% | 100% | 100% | |
Table 3.
Relationship among vitamin D levels and the studied parameters
| Variable | Parameter | Vitamin D levels (ng/mL) | p-value | |||
| Less than 10 | 10-20 | 21-30 | More than 30 | |||
|---|---|---|---|---|---|---|
| Conscious | 18% | 23% | 39% | 18% | 0.09 | |
| Level of consciousness | Confused | 12% | 27% | 23% | 21% | |
| Lethargic | 15% | 30% | 30% | 25% | ||
| Normal based on age | 11% | 29% | 26% | 34% | ||
| 150-500 | 14% | 25% | 27% | 32% | 17.0 | |
| Ferritin level | More than 500 | 12% | 24% | 28% | 36% | |
| Less than 500 | 13% | 27% | 24% | 36% | ||
| LDH level | 500-1000 | 15% | 24% | 28% | 33% | 31.0 |
|
|
More than 1000 | 16% | 25% | 28% | 31% | |
| Less than 25 | 11% | 24% | 31% | 34% | ||
| 26-50 | 20% | 20% | 25% | 35% | ||
| Level of involvement | 51-75 | 34% | 21% | 24% | 31% | 04.0 |
| More than 75 | - | 100 | - | - | ||
| Less than 40 | 13% | 27% | 33% | 27% | ||
| CRP levels | 40-70 | 17% | 25% | 35% | 33% | |
| More than 70 | 18% | 28% | 25% | 29% | ||
| Thrombocytopenia | 22% | 29% | 26% | 23% | ||
| PLT levels | Thrombocytosis | 27% | 26% | 27% | 20% | 17.0 |
| Yes | 33% | 29% | 20% | 18% | ||
| Tachypnea | No | 24% | 21% | 32% | 23% | 02.0 |
| Tachycardia | Yes | 31% | 32% | 19% | 18% | |
|
|
No | 26% | 21% | 32% | 23% | 02.0 |
| Degree of fever | 23% | 25% | 24% | 28% | ||
| Clinical symptoms | PR | 28% | 20% | 28% | 25% | 01.0 |
|
|
RR | 26% | 21% | 25% | 28% | |
| Diarrhea | 20% | 24% | 31% | 34% | ||
| Gastrointestinal problems | Vomiting | 32% | 23% | 25% | 20% | 0.02 |
|
|
Bloody diarrhea | 29% | 26% | 20% | 25% | |
| 3-6 | 13% | 37% | 23% | 27% | ||
| Dehydration | 6-9 | 25% | 35% | 15% | 25% | 52.0 |
|
|
10-15 | 25% | 35% | 15% | 25% | |
| Negative | 17% | 25% | 35% | 33% | ||
| O2 levels | 90-95 | 12% | 23% | 22% | 43% | 03.0 |
|
|
<90 | 27% | 26% | 27% | 20% | |
Table 4.
Association among vitamin D levels and disease severity based on clinical findings
| Disease severity based on clinical findings | p-value | ||||
|---|---|---|---|---|---|
| Outpatient (mild) | Hospitalization (moderate) | ICU (severe) | hospitalization | 0.000 | |
| Vitamin levels less than 10 | 0.0% | 25.0% | 75.0% | ||
| Vitamin levels between 10-20 | 0.0% | 50.0% | 50.0% | ||
| Vitamin levels between 21-30 | 4.2% | 70.8% | 25.0% | ||
| Vitamin levels more than 30 | 32.0% | 62.0% | 6.0% | ||
| Total | 17.7% | 60.4% | 21.9% | ||
Table 5.
Association among vitamin D levels and disease severity based on laboratory results
| Disease severity based on laboratory results | p-value | |||
|---|---|---|---|---|
| Score ≤4 | Score : 5-7 | Score >7 | ||
| Vitamin levels less than 10 | 0.0% | 25.0% | 75.0% | 0.000 |
| Vitamin levels between 10-20 | 0.0% | 33.3% | 66.7% | |
| Vitamin levels between 21-30 | 3.8% | 61.5% | 34.6% | |
| Vitamin levels more than 30 | 35.3% | 58.8% | 5.9% | |
| Total | 19.2% | 53.5% | 27.3% | |
In conclusion, the present study showed that vitamin D levels were associated with levels of involvement, tachycardia, tachypnea, clinical signs, gastrointestinal problems, and O2 levels. Therefore, vitamin D can be effective in reducing the severity of COVID-19. The most important finding of the present study was the importance of moderate levels of vitamin D and their effects on clinical symptoms and important health factors, and this issue should be considered by health officials.
Acknowledgements
The authors would like to thank Aliasghar clinical research development center for editorial and search assistance.
List of acronyms
- COVID-19
Coronavirus Disease 2019
- CRP
C-Reactive Protein
- CT-Scan
Computed tomography scan
- HPLC
High-performance liquid chromatography
- LDH
Lactate Dehydrogenase
- MERS
Middle East. respiratory syndrome
- PCR
polymerase chain reaction
- PLT
platelet
- SARS
Severe acute respiratory syndrome
- SPO2
Saturation of peripheral oxygen
Funding Statement
Funding: The authors received no specific funding for this work.
Contributor Information
Pegah Karimian, Email: Karimian.p@iums.ac.ir.
Motahareh Sadat Tahami, Email: motahareh.s.tahami@gmail.com.
Shirin Sayyahfar, Email: sayyahfar.sh@iums.ac.ir.
References
- 1.Zumla A, Hui DS, Perlman S. Middle East respiratory syndrome. Lancet. 2015. Sep 5;386(9997):995-1007. doi: 10.1016/S0140-6736(15)60454-8. Epub 2015 Jun 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Napoli RD. Evaluation and Treatment Coronavirus (COVID-19) [Updated 2020 Mar 20]. In StatPearls; StatPearls: Petersburg, FL, USA, 2020. [Google Scholar]
- 3.Peiris JS. Severe Acute Respiratory Syndrome (SARS). J Clin Virol. 2003;28(3):245-247. doi:10.1016/j.jcv.2003.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Imperial College London. Report 2: estimating the potential total number of novel coronavirus cases in Wuhan City, China. Jan 2020. https://www.imperial.ac.uk/mrc-globalinfectiousdisease-analysis/news--wuhan-coronavirus. [Google Scholar]
- 5.Yin Y, Wunderink RG. MERS, SARS and other coronaviruses as causes of pneumonia. Respirology. 2018. Feb;23(2):130-137. doi: 10.1111/resp.13196. Epub 2017 Oct 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cruz A, Zeichner S. COVID-19 in children: initial characterization of the pediatric disease. Pediatrics. 2020; doi:10.1542/peds.2020-0834. [DOI] [PubMed] [Google Scholar]
- 7.Tabrizi R, Moosazadeh M, Akbari Dabbaghmanesh MH, Mohamadkhani M, Asemi Z, et al. High prevalence of vitamin D deficiency among Iranian population: a systematic review and meta-analysis. Iran J Med Sci 2018; 43(2): 125-139 (Persian). [PMC free article] [PubMed] [Google Scholar]
- 8.Nadiger M, Hassor S, Totapally B. Vitamin d levels in children with COVID-19 admitted to the PICU. Critical Care Medicine. 49 (SUPPL 1):54, 2021. [Google Scholar]
- 9.Schwalfenberg GK. A review of the critical role of vitamin D in the functioning of the immune system and the clinical implications of vitamin D deficiency. Mol Nutr Food Res. 2011. Jan;55(1):96-108. doi: 10.1002/mnfr.201000174. Epub 2010 Sep 7. [DOI] [PubMed] [Google Scholar]
- 10.Rondanelli M., Miccono A., Lamburghini S., Avanzato I., Riva A., Allegrini P., Faliva M.A., Peroni G., Nichetti M., Perna S. Self-Care for Common Colds: The Pivotal Role of Vitamin D, Vitamin C, Zinc, and Echinacea in Three Main Immune Interactive Clusters (Physical Barriers, Innate and Adaptive Immunity) Involved during an Episode of Common Colds-Practical Advice on Dosages and on the Time to Take These Nutrients/Botanicals in order to Prevent or Treat Common Colds. Evid Based Complement Alternat Med. 2018, 2018, 5813095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Holick MF. Vitamin D deficiency. N Engl J Med. 2007. Jul 19;357(3):266-81. doi: 10.1056/NEJMra 070553. [DOI] [PubMed] [Google Scholar]
- 12.Rossi GA, Fanous H, Colin AA. Viral strategies predisposing to respiratory bacterial superinfections. Pediatr Pulmonol. 2020. Apr;55(4):1061-1073. doi: 10.1002/ppul.24699. Epub 2020 Feb 21. [DOI] [PubMed] [Google Scholar]
- 13.Sharifi A, Vahedi H, Nedjat S, Rafiei H, Hosseinzadeh-Attar MJ. Effect of single-dose injection of vitamin D on immune cytokines in ulcerative colitis patients: a randomized placebo-controlled trial. APMIS. 2019. Oct;127(10):681-687. doi: 10.1111/apm.12982. Epub 2019 Jul 26. [DOI] [PubMed] [Google Scholar]
- 14.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020. Feb 15;395(10223):497-506. doi: 10.1016/S0140-6736(20)30183-5. Epub 2020 Jan 24. Erratum in: Lancet. 2020 Jan 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gombart AF, Pierre A, Maggini S. A Review of Micronutrients and the Immune System-Working in Harmony to Reduce the Risk of Infection. Nutrients. 2020. Jan 16;12(1):236. doi: 10.3390/nu12010236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. Clinical Characteristics of 138 Hospitalized Patients with 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020. Mar 17;323(11):1061-1069. doi: 10.1001/jama.2020.1585. Erratum in: JAMA. 2021 Mar 16;325(11): 1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Azadeh H, Hedayatizadeh-Omran A, Saeedi M, Vahedi-Larijani L, Mehravaran H, Heydari K. Serum Vitamin D Concentrations in CoVID19 Patients. J Mazandaran Univ Med Sci. 2021; 31(195) :30-36. URL: http://jmums.mazums.ac.ir/article-1-16104-en.html [Google Scholar]
- 18.Weir EK, Thenappan T, Bhargava M, Chen Y. Does vitamin D deficiency increase the severity of COVID-19?. Clin Med (Lond). 2020;20(4):e107-e108. doi:10.7861/clinmed.2020-0301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yılmaz K, Şen V. Is vitamin D deficiency a risk factor for COVID-19 in children?. Pediatr Pulmonol. 2020;55(12):3595-3601. doi:10.1002/pp ul.25106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Camargo CA Jr, Ganmaa D, Frazier AL, et al. Randomized trial of vitamin D supplementation and risk of acute respiratory infection in Mongolia. Pediatrics. 2012;130(3):e561–e567. doi:10.1542/ peds.2011-3029 [DOI] [PubMed] [Google Scholar]
- 21.Gavriela AFeketea, Vasiliki Vlacha, Bocsan Ioana Corina, et al. Vitamin D in Corona Virus Disease 2019 (COVID-19) Related Multisystem Inflammatory Syndrome in Children. Frontiers in Immunology. 2021:12. 607.DOI=10.3389/fimmu .2021.64854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Munshi R, Hussein MH, Toraih EA, Elshazli RM, Jardak C, Sultana N, et al. Vitamin D insufficiency as a potential culprit in critical COVID-19 patients. J Med Virol. 2021;93:733–40. doi.org/10. 1002/jmv.26360. [DOI] [PubMed] [Google Scholar]
- 23.Merzon E, Tworowski D, Gorohovski A, Vinker S, Cohen AG, Green I, et al. Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study. FEBS J. 2020;287:3693–702. doi.org/10. 1111/febs.15495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maghbooli Z, Sahraian MA, Ebrahimi M, Pazoki M, Kafan S, Tabriz HM, et al. Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection. PLoS ONE. 2020;15:e0239799. doi.org/10.1371/journal.pone.0239799. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 25.Güven M, Gültekin H. The effect of high-dose parenteral vitamin D3 on COVID-19-related inhospital mortality in critical COVID-19 patients during intensive care unit admission: an observational cohort study. Eur J Clin Nutr. 2021. Sep;75(9):1383-1388. doi: 10.1038/s41430-021-00984-5. Epub 2021 Jul 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hastie CE, Pell JP, Sattar N. Vitamin D and COVID-19 infection and mortality in UK Biobank. Eur J Nutr. 2021;60(1):545-548. doi: 10.1007/s 00394-020-02372-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Laaksi I. Vitamin D and respiratory infection in adults. Proc Nutr Soc. 2012. Feb;71(1):90-7. doi: 10.1017/S0029665111003351. Epub 2011 Nov 25. [DOI] [PubMed] [Google Scholar]
- 28.Chen G, Wu D, Guo W, Cao Y, Huang D, Wang H, Wang T, Zhang X, Chen H, Yu H, Zhang X, Zhang M, Wu S, Song J, Chen T, Han M, Li S, Luo X, Zhao J, Ning Q. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest. 2020. May 1;130(5):2620-2629. doi: 10.1172/JCI137244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jafari R, Cegolon L, Torkaman M, Kashaki M, Dehghanpoor F, Cheraghalipoor F, Javanbakht M. A 6 months old infant with fever, dyspnea and poor feeding diagnosed with COVID-19. Travel Med Infect Dis. 2020. Jul-Aug;36:101789. doi: 10.1016/j.tmaid.2020.101789. Epub 2020 Jun 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Panfili FM, Roversi M, D'Argenio P, Rossi P, Cappa M, Fintini D. Possible role of vitamin D in Covid-19 infection in pediatric population. J Endocrinol Invest. 2021. Jan;44(1):27-35. doi: 10.1007/s40618-020-01327-0. Epub 2020 Jun 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shafiee S, Cegolon L, Khafaei M, Gholami N, Zhao S, Khalesi N, Moosavian H, Fathi S, Izadi M, Ghadian A, Javanbakht M, Javanbakht A, Akhavan-Sigari R. Gastrointestinal cancers, ACE-2/TMPRSS2 expression and susceptibility to COVID-19. Cancer Cell Int. 2021. Aug 16;21(1):431. doi: 10.1186/s12935-021-02129-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yu L, Ke HJ, Che D, Luo SL, Guo Y, Wu JL. Effect of Pandemic-Related Confinement on Vitamin D Status Among Children Aged 0-6 Years in Guangzhou, China: A Cross-Sectional Study. Risk Manag Healthc Policy. 2020. Nov 19;13:2669-2675. doi: 10.2147/RMHP.S282495. [DOI] [PMC free article] [PubMed] [Google Scholar]


