Abstract
Currently, the world is involved by a pandemic of severe acute respiratory syndrome coronavirus 2 (SARS CoV-2), which has been responsible for the deaths of hundreds of thousands of people so far. The consequences of infection with SARS-CoV-2 vary widely from asymptomatic to severe. Considering the increasing prevalence of different types of virus and acute infection with this disease, strategies to prevent mortality from COVID-19 should be seriously analyzed. In this study, the epidemiological, clinical and laboratory characteristics of patients with COVID-19 were investigated in order to identify risk factors for mortality. Chronic diseases such as chronic kidney disease (CKD), COPD, diabetes, hypertension, cardiovascular disease (CVD), cancer, increased D-dimer, male gender, old age, smoking and obesity are among the deadly risk factors associated COVID-19. Furthermore, lymphopenia and neutrophilia are often present in patients with SARS-CoV-2, and the ratio of absolute neutrophils to lymphocytes (NLR) was significantly increased in patients without bacterial infection. These findings could be used in the future to control and prevent disease, because timely identification of patients with risk of COVID-19 is important to provide better treatment strategies for reduction of mortality.
Key Words: Severe acute respiratory syndrome coronavirus 2, COVID 19, clinical features, mortality, prediction
Ethical Publication Statement
The author confirms that he has read the Journal's position on the issues involved in ethical publication and states that this report is consistent with those guidelines.
Over the past two decades, Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERSCoV) infections have negatively affected more than 10,000 patients and led to epidemics.1 Their responsible viruses belong to the beta-coronavirus family with a high mortality rate.1 In December 2019, a number of cases of pneumonia were reported in Wuhan City, Hubei Province, China, and studies attributed these cases to a new coronavirus, which was associated with severe pneumonia in some patients.2 No specific treatment has been identified for this new disease that was named COVID-19. Due to the very significant mortality rate compared to flu, the mortality rate of this disease has been reported between 2.2 to 3.7.3 In acute patients, the symptoms are usually associated withrespiratory dysfunction syndrome, which can eventually lead to death. The first symptoms of this disease are dry cough, fever and even fatigue. However, in some cases, there are no physical symptoms in infected people.4,5 Recent research shows that the most common comorbidities in patients with COVID-19 are diabetes, high blood pressure, and cardiovascular disease. Therefore, it is important for physicians to evaluate patients' clinical signs according to the effective factors and comorbidities.4-6 Studies show that the amounts of D-dimer, ferritin, AST, CRP, BUN, Cr, sodium, procalcitonin and NLR are statistically significant in predicting mortality,7 and it is well shown that the amount of NLR, which is easily calculated through a complete blood count, provides important information about the patient's inflammatory status in many diseases.7 In view of the above, the aim of this study was to examine the relationship between the clinical features of the disease and their mortality by examining related and parallel studies of the characteristics of patients with COVID-19.
Thus, the aim of this study was to examine the relationship between the clinical features of the disease and their mortality by examining related and parallel studies of the characteristics of patients with COVID-19.
General characteristics and symptoms of COVID-19
Throughout history, many viral diseases have occurred that lead to severe and persistent fatigue, perhaps the most famous finding in Los Angeles (1934), Iceland (1948), London (1955) and Nevada (1984).8-11 In December 2019, cases of β-coronavirus-induced pneumonia were identified in Wuhan, China. At the beginning of the outbreak on January 12, 2020, the World Health Organization (WHO) named the virus coronavirus-2019.12 The SARS-CoV-2 genome sequence found in bats was 96.2% similar to MERS-CoV; The findings showed that mutations in the virus genome changed the host from bats to humans and made it possible to infect humans.13 The SARS-CoV-2 genome is closely similar to SARS-CoV and MERS-CoV, and the accumulated clinical and experimental data on previous viruses can be used to treat COVID-19. In addition, it can be predicted how the host's immune system will react to this particular virus and how the host responses can prevent the virus from becoming more prevalent.12 Studies show that SARS-CoV-2 disease occurs in humans, especially in the elderly and
The virus mainly occurs with the initial symptoms of fever, cough and body aches and affects the respiratory system. The clinical spectrum of COVID-19 varies from asymptomatic, to mild or severe pneumonia with respiratory failure.14 The site of primary infection with SARS-CoV-2 is unknown, and the pathogenesis of COVID-19 is still under investigation. For most patients, COVID-19 may only affect the lungs because it is a respiratory disease. The main mode of infection is human-to-human transmission through close contact, most of which is transmitted through the spread of airborne droplets by coughing or sneezing. For this reason, the rapid spread of SARS-CoV-2 with an original R0 of 2.6-2.2 has occurred, meaning that on average each individual has the potential to spread the infection to around 2.2 others.15
Clinical and bioclinical features of COVID-19 disease
Studies on the clinical and epidemiological features of COVID-19 have been performed in many countries. As one of the first studies,1 Huang et al. revealed the clinical manifestations of COVID-19 patients and concluded that patients in the intensive care unit (ICU) had higher plasma cytokine levels than non-ICU patients. In addition, other studies of clinical patients in patients with low disease severity were reviewed and their results showed that ICU patients were significantly older and were more likely to have some comorbidities.11,16,17 In addition, the study of 41 patients with severe COVID-19 showed high levels of proinflammatory cytokines including IL-2, IL-7, IL-10, G-CSF, IP-10, MCP-1, MIP-1A and α-TNF. These findings are consistent with SARS and MERS that the presence of lymphopenia and "cytokine storm" may play an important role in the pathogenesis of COVID-19. This "cytokine storm" can be the result of a viral infection and damage from pneumonia, which can lead to other complications such as pneumonitis, acute respiratory syndrome (ARDS), respiratory failure, shock, organ failure and even death.18
Studies by Chen et al. showed that old age, dyspnea, low hemoglobin levels, and underlying comorbidities were three to two times higher in ICU patients, respectively, and consequently their mortality rates were higher than those hospitalized in other wards of the hospital and outpatients. Li et al. also reported that the mortality rate of patients with hypertension, cerebrovascular disease, and diabetes was two, three, and two times higher in patients admitted to the intensive care unit respectively.19,20
COVID-19 risk factors (epidemiological, demographic and biochemical factors)
The challenge of COVID-19 is enormous due to its transmission complexity and proven lack of treatment. This will be more catastrophic for low- and middle-income countries due to high illiteracy, a very poor health care system, and a scarce intensive care unit. A series of studies have reported the clinical features of critical patients with COVID-19. Different clinical features and risk factors intended to identify the fatal consequences of the disease. Despite scientists' efforts to better understand the diagnostic and clinical features of the disease, the current understanding of the risk factors for COVID-19 is still ongoing.21 Evidence shows that the overall mortality rate from COVID-19 is 3.77 to 5.4%; However, this rate increases to 41.1 to 61.5% among severe or critical patients. To reduce overall mortality, it is essential to identify risk factors associated with disease severity and mortality in patients with COVID-19. Previous studies have shown that old age, underlying diseases, high D-dimer levels, and multivariate biochemical abnormalities are closely associated with disease severity or even death in COVID-19 patients.22 In various studies, laboratory findings show that cytokine storm, inflammation, acute heart damage, acute liver damage, and acute renal failure are also seen in dead patients. Death has been due to ARDS in the majority of deceased patients.21 In a study performed on 4021 patients, the mortality rate of patients aged 60 years and older was 5.3% and this rate was reported to be 1.4% for patients under 60 years of age. Meanwhile, according to data reported from Wuhan, the mortality rate from COVID-19 in patients 60 years and older was 63.6%. This mortality rate is documented by the claim that its prevalence is much higher in the elderly and mortality is directly related to age.4 Figure 1 shows the proportion of each population group at high risk of COVID-19 infection.22 According to this figure, people living in a nursing home, whether permanently or temporarily, are at high risk of infection or death of COVID-19; Of course, they are less likely to be hospitalized. In terms of comorbid conditions, people with ESRD or dementia/Alzheimer's are at higher risk. People with underlying diseases are also at higher risk for infection and hospitalization or death. The number of underlying individuals with very severe underlying diseases by presenting pneumonia. The mean age of COVID-19 disease is 47 to 59 years, of which 41.9 to 45.7% of patients are women.13 diseases is more closely related to the complications of the disease and the increased probability of death.22
Given the status of chronic obstructive pulmonary disease (COPD) patients and its association with COVID-19 mortality, studies have argued that COPD patients with COVID-19 show higher rates of hospitalization and mortality. And this could be due to viral infections in COPD patients where systemic inflammation increases with slow improvement in reported symptoms. In addition to the effects of the coronavirus, patients with COPD have a number of comorbidities, some of which are associated with an increased risk of hospitalization.27,28 The analysis of systematic studies also demonstrated that the mortality of patients admitted to COVID-19 hospital with diabetes is higher compared to patients without diabetes. Therefore, patients with diabetes and COVID-19 often require invasive ventilation care and are referred to the intensive care unit (ICU) because of the potential for acute respiratory distress syndrome (ARDS).29-38 As a result, diabetes determines the severity and mortality of COVID-19 patients.29,30 Elevated procalcitonin and ferritin in the serum of infected patients is an unfavorable prognostic factor for the patient. In SARS-CoV-2 infection, an increase in the concentration of D-dimer resulting from fibrin decay (FDP) has been also observed, which affects the cascade function of blood clotting factors as the disease progresses, consequently leading to Increased clotting time of prothrombin (PT) and activated partial thromboplastin time (APTT). Therefore, having a high D-dimer significantly increases the probability of mortality. Studies show that high levels of D-dimer increase the risk of severe infection and mortality. In addition, a study in China found that increased D-dimer levels during hospitalization were associated with the worst long-term outcomes. Therefore, the use of D-dimer levels as an indicator of disease severity may be useful, especially in COVID-19 patients who are unable to perform specific imaging.31-33 Changes in hematological parameters also occur in patients with COVID-19 disease and can, to some extent, predict their mortality. In fact, studies revealed that lymphopenia and neutrophilia are more common in patients with SARS-CoV-2, and the ratio of absolute neutrophils to lymphocytes (NLR) is also significantly increased in patients without bacterial infection.33
Analysis of other studies suggests that comorbidities, gender, age, smoking, obesity, acute kidney damage, and D-dimer are important risk factors for this disease. A meta-analysis of current regional reports of patients with coronavirus infection highlights the impact of complications, comorbidities, and demographic variables on coronavirus mortality. These results have important clinical implications such as clinical management and specific preventive measures for patients with coronary heart disease.23 Women with COVID-19 disease have fewer hospitalizations and deaths than men. The results of the meta-analysis also showed that male sex appear to be a risk factor for COVID-19 mortality. In the adaptive immune system, men have fewer CD8 + T cells, CD4 T4 cells, and reduced B cell production than women. In addition, some of the genes involving in regulation of immune systems are located on the X chromosome, and increased expression of TLR7 in ill women may be capable of increasing disease tolerance in their body and reducing the duration of the disease. The results of a systematic study also confirmed that obesity is associated with death in patients with COVID-19 disease.24-26
Figure 1.
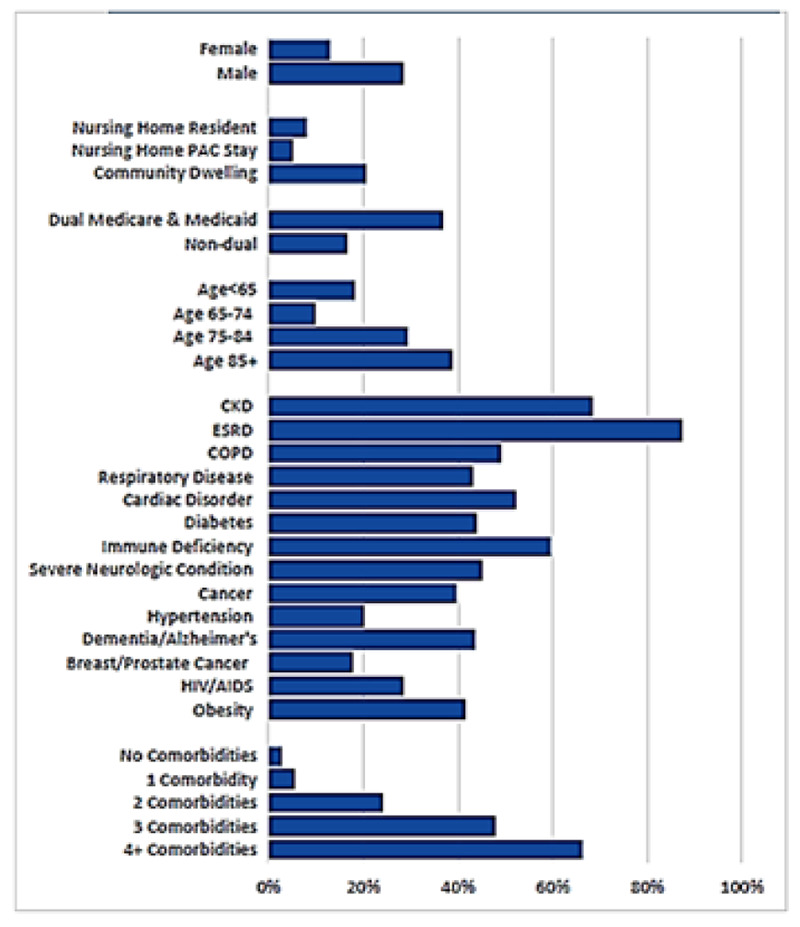
Percentage of mortality from infection.22
Table 1.
Clinical characteristics and mortality from COVID-19
| Findings | Methodology | Title | Author/yeas |
|---|---|---|---|
| Most COVID-19-related deaths were due to old age. Hematologically, lymphocytopenia and increased neutrophil to lymphocyte ratio were found in COVID-19 deceased patients. Similarly, elevated D-dimer and ferritin at admission were risk factors for death in adult patients with COVID-19. Assessing these factors upon admission may help us in determining the risk and early testing for severe COVID-19 cases, so that every effort can be made to manage COVID-19 rapidly and prevent mortality. | This was a retrospective and observational study involving all patients admitted to Sukraraj Tropical and Infectious Diseases Hospital, whose transcriptase reverse polymerase chain reaction was positive for SARS-COV-2. The medical records of deceased patients from January 2020 to January 2021 were evaluated. | Clinical Mortality Review of COVID-19 Patients at Sukraraj Tropical and Infectious Disease Hospital, Nepal; A Retrospective Study | Bastola et al., 2021.34 |
| COVID-19 infection is associated with significant mortality, mainly in elderly patients with underlying diseases. Significant effects of age, gender, and underlying diseases such as diabetes, renal impairment, renal disease, and heart disease increase the risk of death in patients with COVID-19. | Articles published as of March 23, 2020, are written in English and reporters of COVID-19 mortality have been reviewed. Random effects model with 95% CI was used to calculate the odds ratio (OR) and risk ratio (HR) | Factors associated with mortality in Covid-19 patients: a systematic review and meta-analysis | Sepandi et al., 2020.35 |
| The inflammatory response to cytokines is increased in most critically ill COVID-19 patients. Chloroquine (hydroxy) monotherapy was not associated with a risk of mortality, and the use of ACE inhibitors or ARBs was associated with a reduced risk of mortality in patients with COVID-19. | The identified common risk factors were extracted and the relevant publications were searched by PubMed until June 26, 2020. Then, COVID-19 mortality risk factors were analyzed and compared with the retracted articles. | Risk factors of COVID-19 mortality: a systematic review of current literature and lessons from recent retracted articles | Lee et al., 2020.36 |
| A comparison of leukocyte counting methods has not yet been developed in the group of patients admitted to intensive care units and helps to increase the number of complete automatic blood counting tests in patients with COVID-19. Assessing the production and increase in the number of light chains in a patient's body, especially kappa-type chains, may be a predictor in assessing the severity of COVID-19 and its future consequences. | CBC was analyzed in 735 ICU admitted COVID-19 cases, COVID- 19 cases, non-ICU cases and ICU cases. FLC concentrations were analyzed in 133 cases. | Cell Population Data and Serum Polyclonal Immunoglobulin Free Light Chains in the Assessment of COVID-19 Severity | Małecka-Giełdowska et al., 2021.37 |
| Potential risk factors such as advanced age, high SOFA score and d-dimer greater than 1 μg/ml can assist physicians in diagnosing patients with poor prognosis in the early stages. | In this retrospective cohort study, all adult hospitalized died patients with a positive COVID-19 test by January 31, 2020, were included in the study. Demographic, clinical, therapeutic and laboratory data, including serial samples for viral RNA detection, were extracted from electronic medical records and compared between survivors and non-survivors. | Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study | Zhou et al., 2021.31 |
| The mean age of death due to COVID-19 was 63±15 years and 85.1% of them were male. The most common clinical complaints were cough, fever, and shortness of breath. The most common manifestation of chest CT scan was bilateral involvement. Among COVID-19 deaths, 13.5% developed myocarditis and 4.7% developed respiratory complications (such as pneumothorax). According to the findings, 54.1% died due to cardiac arrest and 44.6% due to respiratory arrest. | A cross-sectional and retrospective descriptive study was performed by reviewing the medical records of 149 patients who died of COVID-19. Their diagnosis was confirmed by chest CT scan or PCR-RT. Independent t-test was used to compare quantitative variables and chi-square test was used to analyze qualitative variables. | Clinical Features and Paraclinical Findings of Patients Died of COVID-19 in a Referral Hospital in Sari, Iran | Ghasemian et al., 2020.38 |
Clinical features and mortality from COVID-19
So far, there are several studies on the clinical relationship between COVID-19 disease and related deaths. Some of them are summarized in Table 1. In addition to risk factors such as age, diabetes, hypertension, renal disorders, kidney disease and heart disease, the findings demonstrated other clinical factors involving in mortality.34,35 COVID-19 is currently a public health emergency of concern to international health organizations.36-38 The rapid development of COVID-19 has led to a large number of patients being infected in a short period of time. Elderly patients are at high risk of progressing to more severe illness or even death. A review of various studies showed that most of the deaths due to COVID-19 are related to old age, male gender and multiple comorbidities. Lymphocytopenia and increased neutrophil to lymphocyte ratio were found to be involved in COVID-19 mortality. Similarly, elevated D-dimer and ferritin at admission were risk factors for death in adult patients with COVID-19. Assessing these factors at admission may be helpful in assessing risk and testing early for severe COVID-19 cases, leading to rapid management of COVID-19 and prevention of mortality.
In conclusion, the selection of appropriate clinical indicators for early identification and class treatment of COVID-19 patients is very important.
Acknowledgments
None.
List of acronyms
- APTT
activated partial thromboplastin time
- ARDS
acute respiratory distress syndrome
- CKD
chronic kidney disease
- COPD
chronic obstructive pulmonary disease
- COVID-19
a disease due to coronavirus 2
- CVD
cardiovascular disease
- ICU
intensive care unit
- MERSCoV
Middle East Respiratory Syndrome
- NLR
neutrophils to lymphocytes
- PT
prothrombin
- SARS
Severe acute respiratory syndrome
- SARS CoV-2
severe acute respiratory syndrome coronavirus 2
Funding Statement
Funding: The author received no specific funding for this work.
References
- 1.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020. Feb 15;395(10223):497-506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li Q Guan X Wu P Wang X Zhou L Tong Y Ren R Leung KSM Lau EHY Wong JY Xing X Xiang N Wu Y Li C Chen Q Li D Liu T Zhao J Liu M Tu W Chen C Jin L Yang R Wang Q Zhou S Wang R Liu H Luo Y Liu Y Shao G Li H Tao Z Yang Y Deng Z Liu B Ma Z Zhang Y Shi G Lam TTYWu JTGao GFCowling BJYang B Leung GMFeng Z. Early Transmission Dynamics in Wuhan, China of Novel Coronavirus-Infected Pneumonia. N Engl J Med. 2020. Mar 26;382(13):1199-1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ; HLH Across Speciality Collaboration, UK. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020. Mar 28;395(10229):1033-1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Genc Yavuz B, Colak S, Guven R, Altundag İ, Seyhan AU, Gunay Inanc R. Clinical Features of the 60 Years and Older Patients Infected with 2019 Novel Coronavirus: Can We Predict Mortality Earlier? Gerontology. 2021;67(4):433-440. doi: 10.1159/000514481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Vito A, Geremia N, Fiore V, Princic E, Babudieri S, Madeddu G. Clinical features, laboratory findings and predictors of death in hospitalized patients with COVID-19 in Sardinia, Italy. Eur Rev Med Pharmacol Sci. 2020. Jul;24(14):7861-7868. doi: 10.26355/eurrev_2020 07_22291. [DOI] [PubMed] [Google Scholar]
- 6.Vaira LA, Deiana G, Fois AG, Pirina P, Madeddu G, De Vito A, Babudieri S, Petrocelli M, Serra A, Bussu F, Ligas E, Salzano G, De Riu G. Objective evaluation of anosmia and ageusia in COVID-19 patients: Single-center experience on 72 cases. Head Neck. 2020. Jun;42(6):1252-1258. doi: 10.1002/hed.26204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Faria SS, Fernandes PC Jr, Silva MJ, Lima VC, Fontes W, Freitas-Junior R, Eterovic AK, Forget P. The neutrophil-to-lymphocyte ratio: a narrative review. Ecancermedicalscience. 2016. Dec 12;10:702. doi: 10.3332/ecancer.2016.702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sigurdsson B. A new clinical entity? Lancet 1956;267:789–790. doi: 10.1016/S0140-6736(56)91252-1 [Google Scholar]
- 9.Boffey P. Fatigue ‘Virus’ Has Experts More Baffled and Skeptical Than Ever. New York, NY: New York Times; .1987. Available online at: www.nytimes.com/1987/07/28/science/fatigue-virus-has-experts-morebaffled-and-skeptical-than-ever.html (accessed July 28, 1987). [Google Scholar]
- 10.Steinbrook R. 160 Victims at Lake Tahoe: Chronic Flu-Like Illness a Medical Mystery Story. Los Angeles, CA: Los Angeles Times. 1986. Available online at: http://articles.latimes.com/1986-06-07/news/mn-9956_1_lake-tahoe (Accessed June 7, 1986).\ [Google Scholar]
- 11.Hyde B. The Clinical and Scientific Basis of ME/CFS. Ottawa, ON: Nightingale Research Foundation, 1992. [Google Scholar]
- 12.Lu R Zhao X Li J Niu P Yang B Wu H Wang W Song H Huang B Zhu N Bi Y Ma X Zhan F Wang L Hu T Zhou H Hu Z Zhou W Zhao L Chen J Meng Y Wang J Lin Y Yuan J Xie Z Ma J Liu WJWang D Xu W Holmes ECGao GFWu G Chen W Shi W Tan W. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020. Feb 22;395(10224):565-574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhou P Yang XL Wang XG Hu B Zhang L Zhang W Si HR Zhu Y Li B Huang CL Chen HD Chen J Luo Y Guo H Jiang RD Liu MQ Chen Y Shen XR Wang X Zheng XS Zhao K Chen QJ Deng F Liu LLYan B Zhan FXWang YYXiao GFShi ZL. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020. Mar;579(7798):270-273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pradyumna P, Ritika P. Chronic Fatigue Syndrome After COVID-19 Infection: A Call for Action. Erciyes Med J 2021; 43(1):98–9 • DOI: 10.14744/etd.2020.06767. [Google Scholar]
- 15.Wu F, Zhao S, Yu B, Chen YM, Wang W, Song ZG. A new coronavirus associated with human respiratory disease in China. Nature. 2020. 10.1038/s41586-020-2008-3 [Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Farrell TW, Ferrante LE, Brown T, Francis L, Widera E, Rhodes R, Rosen T, Hwang U, Witt LJ, Thothala N, Liu SW, Vitale CA, Braun UK, Stephens C, Saliba D. AGS Position Statement: Resource Allocation Strategies and Age-Related Considerations in the COVID-19 Era and Beyond. J Am Geriatr Soc. 2020. Jun;68(6):1136-1142. doi: 10.1111/jgs.16537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Osmani F. Analysis of students satisfaction with virtual education in Medical Science University during the pandemic outbreak of COVID-19. Int J Assess Tools Educ. 2021;8(1):1–8. [Google Scholar]
- 18.Nicholls JM, Poon LL, Lee KC, Ng WF, Lai ST, Leung CY, Chu CM, Hui PK, Mak KL, Lim W, Yan KW, Chan KH, Tsang NC, Guan Y, Yuen KY, Peiris JS. Lung pathology of fatal severe acute respiratory syndrome. Lancet. 2003. May 24;361(9371):1773-8. doi: 10.1016/s0140-6736(03)13413-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen J, Qi T, Liu L, Ling Y, Qian Z, Li T. Clinical progression of patients with COVID-19 in Shanghai, China. J Infect. 2020. doi: 10.1016/j.jinf.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li B, Yang J, Zhao F, Zhi L, Wang X, Liu L. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020;109(5):531-8. doi: 10.1007/ s00392-020-01626-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang XB, Hu L, Ming Q, Wei XJ, Zhang ZY, Chen LD, Wang MH, Yao WZ, Huang QF, Ye ZQ, Cai YQ, Zeng HQ. Risk factors for mortality of coronavirus disease-2019 (COVID-19) patients in two centers of Hubei province, China: A retrospective analysis. PLoS One. 2021. Jan 28;16(1):e0246030. doi: 10.1371/journal.pone.0246030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mehta HB, Li S, Goodwin JS. Risk Factors Associated With SARS-CoV-2 Infections, Hospitalization, and Mortality Among US Nursing Home Residents. JAMA Netw Open. 2021. Mar 1;4(3):e216315. doi: 10.1001/jamanetworkopen.2021.6315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dessie ZG, Zewotir T. Mortality-related risk factors of COVID-19: a systematic review and meta-analysis of 42 studies and 423,117 patients. BMC Infect Dis. 2021. Aug 21;21(1):855. doi: 10.1186/s12879-021-06536-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Scully EP, Haverfield J, Ursin RL, Tannenbaum C, Klein SL. Considering how biological sex impacts immune responses and COVID-19 outcomes. Nat Rev Immunol. 2020. Jul;20(7):442-447. doi: 10.1038/s41577-020-0348-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hewagama A, Patel D, Yarlagadda S, Strickland FM, Richardson BC. Stronger inflammatory / cytotoxic T-cell response in women identified by microarray analysis. Genes Immun. 2009. Jul;10(5):509-16. doi: 10.1038/gene.2009.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Abdullah M, Chai PS, Chong MY, Tohit ER, Ramasamy R, Pei CP, Vidyadaran S. Gender effect on in vitro lymphocyte subset levels of healthy individuals. Cell Immunol. 2012;272(2):214-9. doi: 10.1016/j.cellimm.2011.10.009. [DOI] [PubMed] [Google Scholar]
- 27.Hurst JR, Skolnik N, Hansen GJ, Anzueto A, Donaldson GC, Dransfield MT, Varghese P. Understanding the impact of chronic obstructive pulmonary disease exacerbations on patient health and quality of life. Eur J Intern Med. 2020. Mar;73:1-6. doi: 10.1016/j.ejim.2019.12.014. [DOI] [PubMed] [Google Scholar]
- 28.Williams NP, Ostridge K, Devaster JM, Kim V, Coombs NA, Bourne S, Clarke SC, Harden S, Abbas A, Aris E, Lambert C, Tuck A, Williams A, Wootton S, Staples KJ, Wilkinson TMA; AERIS Study Group. Impact of radiologically stratified exacerbations: insights into pneumonia aetiology in COPD. Respir Res. 2018. Jul 28;19(1):143. doi: 10.1186/s12931-018-0842-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fadini GP, Morieri ML, Longato E, Avogaro A. Prevalence and impact of diabetes among people infected with SARS-CoV-2. J Endocrinol Invest. 2020. Jun;43(6):867-869. doi: 10.1007/s40618-020-01236-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang B, Li R, Lu Z, Huang Y. Does comorbidity increase the risk of patients with COVID-19: evidence from meta-analysis. Aging (Albany NY). 2020. Apr 8;12(7):6049-6057. doi: 10.18632/aging.103000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020. Mar 28;395(10229):1054-1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shah S, Shah K, Patel SB, Patel FS, Osman M, Velagapudi P, Turagam MK, Lakkireddy D, Garg J. Elevated D-Dimer Levels Are Associated With Increased Risk of Mortality in Coronavirus Disease 2019: A Systematic Review and Meta-Analysis. Cardiol Rev. 2020. Nov/Dec;28(6):295-302. doi: 10.1097/CRD.0000000000000330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Małecka-Giełdowska M, Fołta M, Wi´sniewska A, Czyz˙ ewska E, Ciepiela O. Cell Population Data and Serum Polyclonal Immunoglobulin Free Light Chains in the Assessment of COVID-19 Severity. Viruses 202; 13;1381. 10.3390/v13071381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bastola A, Shrestha S, Nepal R, Maharjan K, Shrestha B, Chalise BS, Thapa P, Balla P, Sapkota A, Shah P. Clinical Mortality Review of COVID-19 Patients at Sukraraj Tropical and Infectious Disease Hospital, Nepal; A Retrospective Study. Trop Med Infect Dis.2021; 6:137. 10.3390/tropicalmed6030137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sepandi M, Taghdir M, Alimohamadi Y, Afrashteh S, Hosamirudsari H. Factors Associated with Mortality in COVID-19 Patients: A Systematic Review and Meta-Analysis. Iran J Public Health. 2020. Jul;49(7):1211-1221. doi: 10.18502/ijph.v49i7.3574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lee KH, Kim JS, Hong SH, Seong D, Choi YR, Ahn YT, Kim KS, Kim SE, Lee S, Sim W, Kim D, Jun B, Yang JW, Yon DK, Lee SW, Kim MS, Dragioti E, Li H, Jacob L, Koyanagi A, Abou Ghayda R, Shin JI, Smith L. Risk factors of COVID-19 mortality: a systematic review of current literature and lessons from recent retracted articles. Eur Rev Med Pharmacol Sci. 2020. Dec;24(24):13089-13097. doi: 10.26355/eurrev_202012_24216. [DOI] [PubMed] [Google Scholar]
- 37.Małecka-Giełdowska M, Fołta M, Wiśniewska A, Czyżewska E, Ciepiela O. Cell Population Data and Serum Polyclonal Immunoglobulin Free Light Chains in the Assessment of COVID-19 Severity. Viruses. 2021. Jul 15;13(7):1381. doi: 10.3390/v13071381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ghasemian R, Alizadeh-Navaei R, Boskabadi J, Rezaei Kalantari K. Clinical Features and Paraclinical Findings of Patients Died of COVID-19 in a Referral Hospital in Sari, Iran, February 2020-May 2020. J Mazandaran Univ Med Sci. 2021; 31(198) :119-132. Article in Persian. [Google Scholar]


