Abstract
Objective
Problematic use of digital media and problematic use of the internet (PUI) in particular are growing problems in the general population. Moreover, studies have shown links between PUI and symptoms of attention-deficit/hyperactivity disorder (ADHD). This meta-analysis investigated whether children and adolescents with ADHD are more often affected by PUI compared to control groups.
Method
Multiple databases (EBSCOhost, Pubmed) were reviewed. Studies were eligible if individuals (aged 6–18 years) were diagnosed with ADHD, assessed on PUI-related measures, and compared to non-clinical or/and clinical controls without a diagnosis of ADHD. Out of 3,859 identified studies, 14 studies assessing 2,488 participants met all inclusion criteria. Four meta-analyses examining time-based and scale-based measures, different informants and non-clinical vs. clinical controls using random-effects models were performed. Funnel plots were used to investigate publication bias.
Results
The analyses revealed significantly more severe PUI in individuals with ADHD compared to controls, both when PUI was assessed via rating scale (scaled-based) and via units for time (time-based measures). Different informants (self- vs. parent-rating) had no impact on results. Differences in PUI between groups with ADHD and non-clinical controls were significant, whereas differences between ADHD and clinical controls were not. Due to the high heterogeneity observed and the small sample sizes, these latter findings should be interpreted cautiously.
Conclusion
Children and adolescents with ADHD show more severe PUI compared to non-clinical controls without ADHD. However, the small number of studies does not allow for a systematic comparison between ADHD and groups with other psychopathologies.
Keywords: problematic use of the internet, ADHD, children, adolescents, digital media, meta-analysis
Background
Problematic use of the internet/digital media
Problematic use of the internet (PUI) (or problematic internet use (PIU), sometimes also: pathological internet use) refers to all dysfunctional subtypes (e.g. excessive gaming, excessive use of social networks, excessive pornography viewing, cyberbullying, excessive gambling, cybershopping, etc.) linked to the use of digital media (Demetrovics, Szeredi, & Rózsa, 2008; Fineberg et al., 2018; Moretta, Buodo, Demetrovics, & Potenza, 2022). Although the term PUI should be confined to internet-related activity and its specific aspects (Dell’Osso et al., 2021), it sometimes includes digital activities that can also be performed offline (such as gaming) and digital devices that can be used offline (such as smart phones and tablets). For that reason, in our meta-analysis we expand the term problematic use of the internet to refer to a broader category i.e., problematic use of digital media. Internet use and problematic internet use can be understood as lying on a spectrum with an adaptive and a maladaptive end (Billieux et al., 2017; Davis, 2001). PUI thus needs to be considered as a highly complex construct (Caplan, 2007) and a distinction between dysfunctional or problematic internet use in contrast to “functional” use is challenging (see Joshi, Stubbe, Li, & Hilty, 2019). For the time being, a general definition and nomenclature for PUI is still lacking (Fineberg et al., 2018; Moretta et al., 2022). The term internet communication disorder has been created to subsume aspects of PUI that relate to the communication with others via digital media, including messenger or social media services or the use of smartphones (Wegmann, Ostendorf, & Brand, 2018). In the literature, the terms internet addiction (Brand, Young, & Laier, 2014; Young, 1998) or internet use disorder (IUD) (Holden, 2010) are frequently encountered. It has been argued that affected individuals show similar symptoms to people with substance dependence, leading to proposals that similar criteria should be adopted for the definition of PUI (Lu, Chou, Hsiao, Hu, & Yen, 2019; Tao et al., 2010), including, for instance, unsuccessful attempts to reduce consumption, continuous preoccupation, persistent use despite harmful consequences, neglect of other areas of life, psychological or physiological distress in reaction to withdrawal, etc. With the exception of gaming, so far, no other dysfunctional internet-related behavior has found its way into international classifications of diseases (Grant, Odlaug, & Chamberlain, 2017; King, Delfabbro, Billieux, & Potenza, 2020). In the DSM-5, internet gaming disorder is classified in section III “Conditions to further study”, and gambling disorder as a behavioral addiction within the category of “Substance related and Addictive Disorders” (APA, 2013). According to DSM-5, internet gaming disorder may also include behavioral addiction to offline-gaming. In the ICD-11 (Version 9/2020) (WHO, 2020), gambling disorder and gaming disorder (both online or offline) are categorized within the section on “Disorders due to substance use or addictive behaviors”, in contrast to “hazardous gaming”, which is categorized under “problems associated with health behaviors” and defined as a health risk arising from the frequency, the amount of time, neglect of other activities, risky behaviors or adverse consequences associated with gaming. Besides addiction, aspects of PUI have also been linked to other psychopathologies, such as obsessive-compulsive disorder (Chamberlain, Redden, Stein, Lochner, & Grant, 2017; Fineberg et al., 2018; Ioannidis et al., 2016), or disorders of impulse control (Fariba & Gokarakonda, 2020; Volpe, Dell’osso, Fiorillo, Mucic, & Aboujaoude, 2015). It has been proposed that it is not the intensity (i.e. amount of time), but rather the behavioral problems related to increased media use that might distinguish between pathological and non-pathological media use in youth, although the two are correlated (Boer, Stevens, Finkenauer, & van den Eijnden, 2020a; Van Den Eijnden, Koning, Doornwaard, Van Gurp, & Bogt, 2018). The term “problematic media use” would thus refer to addiction-like behaviors, such as emotional reactions to withdrawal of digital media or the feeling of psychological distress when media use is restricted. PUI often refers to the abuse of specific internet functions, such as gaming, and specific PUI may also occur offline. Generalized PUI, in contrast, involves a broader dysfunctional use of many possible facets of the internet with negative consequences for the individual's life. Generalized PUI has been linked to deficient self-regulation and has been discussed as a separate behavioral addiction (Brand et al., 2014; Caplan 2007; Moretta et al., 2022).
Estimates of PUI prevalence in the general population vary considerably between studies, countries (Darvesh et al., 2020; Durkee et al., 2012; Laconi et al., 2018), subtypes of PUI, and age and gender of participants (Anderson, Steen, & Stavropoulos, 2017; Carli et al., 2013), but have increased in recent years (Carbonell, Chamarro, Oberst, Rodrigo, & Prades, 2018; Kaess et al., 2016). Gaming disorder seems to have higher prevalence rates in Asia (10–15%) than in Western countries (1–10%) (Saunders et al., 2017), in males than in females, and in adolescents than in adults (Stevens, Dorstyn, Delfabbro, & King, 2020). In a large-scale German study, PUI was found in 6.1% of participants aged 11–21 years, with two prevalence peaks in the age groups 15–16 and 19–21 years (Lindenberg, Halasy, Szász-Janocha, & Wartberg, 2018). A recent Chinese survey in college students reported a prevalence of internet addiction of 7.2% in females and 8.17% in males (Shen et al., 2021). In an extensive meta-analysis that included findings from 31 countries and 131 epidemiological studies with 693,306 participants, the estimated prevalence rate of generalized internet addiction was 7.02% while that of internet gaming disorder lay at 2.47% (Pan, Chiu, & Lin, 2020).
A growing body of evidence points at an association between PUI and mental health disorders (Caplan, 2007; Fineberg et al., 2018; Spada, 2014; Young & Brand, 2017; Young, 1996, 1998), such as anxiety disorders and depression (Demirci, Akgönül, & Akpinar, 2015; Holmgren & Coyne, 2017; Hussain & Griffiths, 2019; Lo, Wang, & Fang, 2005; Ostovar et al., 2016; Woods & Scott, 2016; Younes et al., 2016), eating disorders (Çelik, Odacı, & Bayraktar, 2015; Ioannidis et al., 2021), autism spectrum disorder (ASD) (Macmullin, Lunsky, & Weiss, 2016; Paulus et al., 2020), or attention-deficit/hyperactivity disorder (ADHD) (Ceranoglu, 2018; Dullur, Krishnan, & Diaz, 2021; Nikkelen, Valkenburg, Huizinga, & Bushman, 2014; Wang et al., 2017; Werling et al., 2021a). The nature and function of these associations are not always clear and seem to vary according to the specific psychopathological problem. While some PUI behaviors may appear to be the consequence of the underlying psychopathological impairment, e.g. the avoidance of direct social contact in ASD or anxiety disorders, other psychopathological problems may also be aggravated or mediated by PUI, e.g. depression or eating disorders (Guo et al., 2020; Hinojo-Lucena, Aznar-Díaz, Cáceres-Reche, Trujillo-Torres, & Romero-Rodríguez, 2019; Ioannidis et al., 2021). According to meta-analyses on psychopathology and PUI, ADHD symptoms are typically associated with pathological internet use (100% of studies; Carli et al., 2013) and very often with internet gaming disorder (85% (González-Bueso et al., 2018), while symptoms associations of other psychopathologies are also very frequent (92% anxiety, 89% depression, 75% social phobia; González-Bueso et al., 2018; see also Andreassen et al., 2016). Besides psychopathological symptoms, internet gaming disorder has been linked to maladaptive coping with interpersonal problems or inappropriate attempts to restore psychosocial well-being (Cheng et al., 2018).
Attention-deficit hyperactivity disorder and PUI
ADHD is among the most common neurodevelopmental disorders worldwide with a prevalence between 2% and 7% in children and adolescents (Faraone et al., 2021; Polanczyk, Salum, Sugaya, Caye, & Rohde, 2015; Sayal, Prasad, Daley, Ford, & Coghill, 2018) and is characterized by symptoms of inattention and/or hyperactivity/impulsivity (APA, 2013). Since children and adolescents diagnosed with ADHD are highly responsive to immediate reward, sometimes lack self-efficacy and often lack emotional and cognitive self-regulation, they seem predisposed to develop an internet addiction (Barth & Renner, 2015; Ceranoglu, 2018). Neurobiologically, the mechanisms found to underlie internet gaming disorder, such as dopamine-mediated reward mechanisms, reduced brain activation in areas associated with impulse control and decision-making, and reduced connectivity in executive function networks (Weinstein & Lejoyeux, 2020) are also impaired in ADHD (Rubia, 2018).
A large number of studies have investigated the association between ADHD symptoms and PUI in correlation analyses in the general population or in samples with internet addiction or internet gaming addiction. In a meta-analysis on the association between internet addiction and ADHD symptoms, Wang and colleagues (Wang et al., 2017) identified 15 studies, consisting of two cohort studies and 13 cross-sectional studies, which included data from adolescents and adults, mostly from Asian countries. The authors analyzed groups with and without internet addiction regarding the occurrence or severity of ADHD symptoms and found a significant association of moderate size. More recently, Marin and colleagues (Marin, Nuñez, & de Almeida, 2021) reviewed the association between internet addiction and attention in adolescents in 44 studies and found that very few studies investigated attentional variables. In another systematic review, Dullur and colleagues (Dullur et al., 2021) identified 29 studies on the association between ADHD and gaming, comprising 15 studies with children and adolescents and 14 with adults. Eight of the studies with children and adolescents referred to community samples. The authors found consistent positive associations between ADHD symptoms and gaming, more often related to attention/inattention symptoms than to hyperactivity (Mazurek & Engelhardt, 2013; Panagiotidi & Overton, 2018). Problematic social media use has been found to be associated with ADHD symptoms, but to a lesser degree than with depression or anxiety (Barry, Sidoti, Briggs, Reiter, & Lindsey, 2017). Addictive smartphone use was reported to be more frequent in adolescents with ADHD than in non-ADHD individuals (OR 10.14) in a Korean community sample (Kim et al., 2019), and to be higher than in individuals with depression (OR 4.15) or anxiety disorders (OR 4.41). The relation between problematic use of cyberpornography in ADHD-samples compared to non-ADHD controls has only been investigated in adults (Niazof, Weizman, & Weinstein, 2019).
While meta-analytical association studies or systematic reviews have identified associations between ADHD symptoms and aspects of PUI, no meta-analysis to date has focused exclusively on studies with ADHD patients. Such studies are usually case control studies, in which internet related problems in children and adolescents with a diagnosis of ADHD and in non-ADHD controls – clinical or healthy – are directly compared. Although case control-studies in general show lower generalizability than population studies, they nevertheless have the advantage of relating explicitly to clinically referred groups and can thus provide a frame of reference for clinicians who are treating patients with ADHD and its diverse comorbidities. ADHD symptoms, on the other hand, also exist in the general population (Heidbreder, 2015; Salum et al., 2014) and a large proportion of children and adolescents with PUI may present elevated ADHD symptoms without reaching a diagnostic threshold or a need for ADHD treatment. In addition, the role of PUI in the development or aggravation of ADHD symptoms is subject of ongoing debate. A longitudinal study found an association of PUI in non-ADHD adolescents with the development of ADHD symptoms over two years (Ra et al., 2018). With regard to social media, in a Dutch community sample, Boer and colleagues (Boer, Stevens, et al., 2020a) found that problematic social media use predicted an increase of attentional problems one or two years later. Conversely, attention problems did not predict an increase in problematic social media use. While a causality between increased media use and the subsequent development of ADHD is doubtful (see Sibley & Coxe, 2018), it is plausible that the adverse effects of excessive media use - with lack of sleep and exposure to fast-paced and violent content - may lead to ADHD like behaviors which could erroneously be diagnosed as ADHD (Lissak, 2018). It is also possible that frequent media use and the continuous experience of fast and immediate responses may result in a cognitive style in which non-digital actions or interactions are perceived as understimulating and boring (Nikkelen et al., 2014). This, in turn, may lead to increased symptoms of ADHD (Baumgartner, van der Schuur, Lemmens, & tePoel, 2017).
Objective and research questions
The main goal of this meta-analysis was to compare PUI in children and adolescents diagnosed with ADHD to age-matched non-clinical or clinical groups. More specifically, we sought to investigate whether internet use/digital media use in individuals with ADHD differs from that of nonclinical controls or clinical groups with other psychopathological disorders in terms of frequency of use or severity of related problem behaviors. A further question to investigate was whether these differences vary according to the age of the participants. Finally, we wished to examine whether reported differences in PUI depend on the informant. Self-ratings and parent-ratings may both be subject to bias. When conducting self-ratings, children or adolescents may be unaware of or unwilling to admit the true extent of their problems, while parents may simply not know how much time their child is actually spending on the internet.
Methods
Criteria for considering studies for meta-analysis and outcome measures
This meta-analysis investigated case-control studies on PUI that compared individuals with a diagnosis of attention-deficit hyperactivity disorder with age matched controls.
To be considered for inclusion in the meta-analysis, a group of children and/or adolescents, age range 6–18 years and without any specific comorbidity, had to be compared with a) controls from the general population without ADHD (non-clinical controls), and/or b) clinical controls with psychopathological disorders other than ADHD, and/or c) individuals with another specific psychopathological disorder plus comorbid ADHD regarding time- or score-related measures of PUI. The diagnosis of ADHD had to be explicitly based on a standard clinical assessment or the ADHD group had to be recruited in child and adolescent psychiatry or other clinical contexts where a preceding clinical diagnostic process could be assumed. Furthermore, all studies had to report a quantitative measure of the internet/media use in form of a rating scale (scaled score) and/or of the time unit spent on the internet/with media per day or week (timed score), as well as the required statistical information (group size, mean and standard deviation or equivalent). Studies had to be published in peer-reviewed journals. Studies written in a language other than English or German, as well as neuroscientific studies or case studies were excluded, as were studies with ADHD diagnoses deduced from self-assessment questionnaires instead of clinical diagnostic procedures. Also, studies with samples exceeding the age range of 6–18 years were excluded, studies with no “pure” ADHD group, and studies that did not contain a direct group comparison, e. g. such as studies exclusively relying on correlational analyses.
The primary outcome investigated in the meta-analysis was the frequency/intensity of internet/digital media use or the severity of problematic internet/media use. PUI data could be based on parents' report or self-report.
Search methods
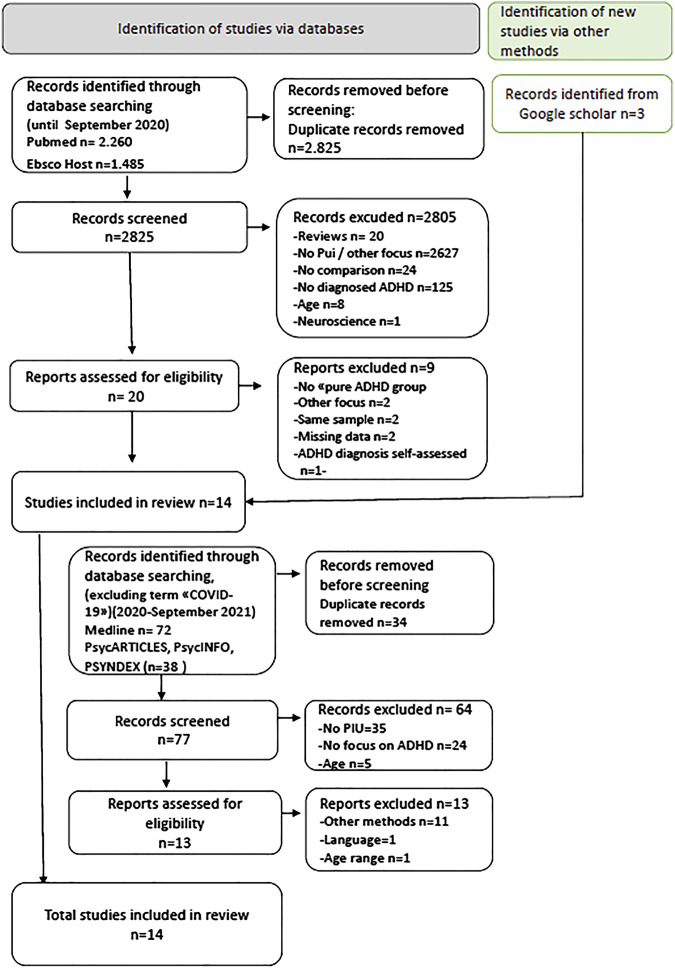
A systematic literature search was conducted by two independent researchers (SK and RD) and checked by the first author (Fig. 1). Potential keywords and databases were identified, discussed, and then selected by SK, RD and the first author. Keywords used in the search string included (ADHD OR Attention deficit hyperactivity disorder OR inattention OR Hyperkinetic disorder) AND (Problematic Internet use OR PUI OR Gaming OR Internet OR Smartphone OR Computer OR Social networking OR Social media OR Facebook OR YouTube OR WhatsApp OR Gaming Disorder OR Mobile phone OR PC OR Tablet OR Video game OR Screen media OR Digital OR Internet addiction) AND (children OR adolescents OR boys OR girls OR teenager OR youth OR teens OR students). The search was conducted in the following databases: EBSCOhost (including PsycARTICLES, PSYNDEX, PsycINFO) and PubMed (including Medline). Additionally, Google Scholar was used for specific searches. The last search was conducted on September 16th, 2020. To update the meta-analysis, a second electronic research was performed in October 2021, covering studies published from September 2020 to September 2021. The same key words and data bases were used as before, with one exception: Studies containing the key words “COVID-19” or “pandemic” were excluded. It has been shown that internet/digital media use had considerably changed under pandemic conditions in children and adolescents with ADHD (e.g. Werling, Walitza, & Drechsler, 2021a) and other psychopathologies (Werling, Walitza, Grünblatt, & Drechsler, 2021b) and we believe that the impact of COVID-19 on PUI should be investigated separately. This second search was conducted by two independent researchers (AW and RD).
Fig. 1.
Flow chart of the search process
Data collection and analysis
All papers that met the inclusion criteria were again checked by the two independent researchers (RD, SK) and by AW (2020) and by two researchers (AW, RD) in 2021. The final inclusion of studies was based on the consensus of all three researchers (2020) or of two researchers (2021), respectively. All data were managed using RevMan 5.4 (Nordic Cochrane Center, 2014). The sample sizes, means, and standard deviations from all studies were extracted. If values were missing or incomplete, the respective study authors were contacted and asked to contribute missing data to be included in the meta-analysis. Papers by authors who did not provide missing data in time, were excluded from the quantitative analysis. The search strategy was visualized in a flow chart according to PRISMA recommendations (Page, Moher, & McKenzie, 2021).
For the measurement of group and subgroup differences, standardized mean differences were used based on the specifics of the comparison. Random-effect models (DerSimonian & Laird, 1986) were applied for all analyses, as some heterogeneity was expected. The main reason to decide in favor of random-effect models lay in the expected differences between the samples examined in the studies and in the variety of measures (different scales and time units) used for the analyses. Results were visualized by forest tree plots. Risk of bias was visualized by funnel plots Figure A1 and A2 (Appendix).
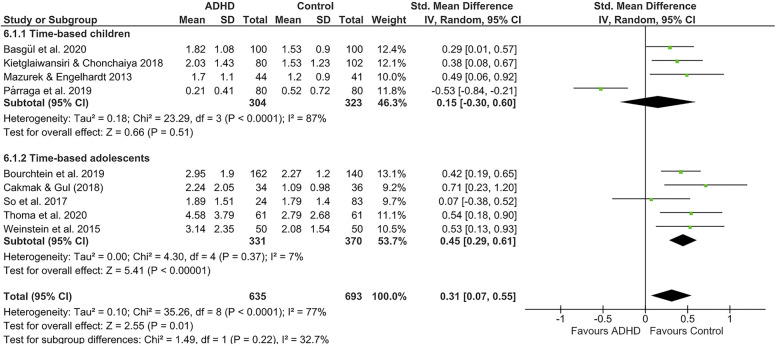
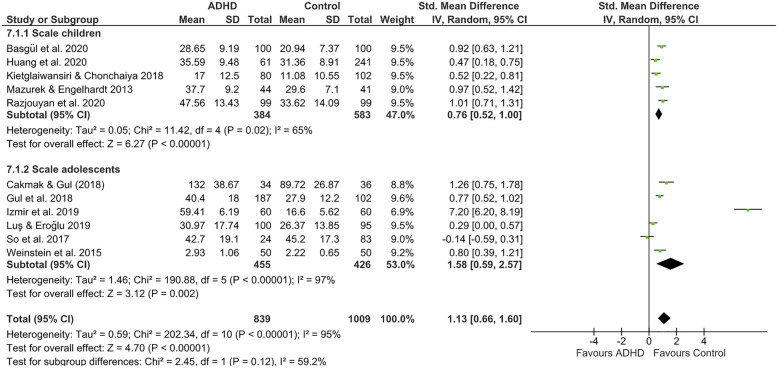
One main analysis was performed for time-based and one for scale-based measurements of PUI (Figs 2 and 3). Additionally, both analyses were divided into subgroups of children (age mean of ADHD group <12 years) and adolescents (age mean >12 years). Additional analyses were conducted comparing parent- and self-rated studies and studies with healthy (non-clinical) vs. clinical controls. For all studies that indicated a substantial amount of heterogeneity (I 2 > 50%) (Patsopoulos, Evangelou, & Ioannidis, 2008), a sensitivity analysis was performed. Only results after removal of studies that resulted in substantial change will be reported.
Fig. 2.
Time-based analyses of PUI in children and adolescents with ADHD compared to controls
Fig. 3.
Scale-based analyses of PUI in children and adolescents with ADHD compared to controls
Quality assessment
The classification of methodological qualities was assessed by two independent raters (AW, RD) with a modified tool for the evaluation of case control studies (Critical Appraisal tools for JBI Systematic Review; Moola et al., 2020). In this checklist, studies are evaluated according to 10 methodological criteria, with focus on methodological aspects particularly relevant for case-control studies, such as matching and comparability of groups (Supplementary material).
Results
Study selection
The electronic search in 2020 led to 1,485 hits on EBSCOhost (including PsycARTICLES, PsycINFO, PSYNDEX, MEDLINE) and 2,260 hits on PubMed (including MEDLINE). Four additional studies were identified through search in Google Scholar after the removal of duplicates, the abstracts of all articles were screened based on the predefined inclusion and exclusion criteria. For a detailed description of the inclusion and exclusion process see Fig. 1.
In the 2020 search, after reviewing a total of 3,748 studies, 920 duplicates were removed. 2,627 studies that did not address ADHD in children or adolescents and studies that did not investigate PUI were excluded. Additionally, reviews, neuroscientific studies, and studies in languages other than English or German were also excluded (see flowchart, Fig. 1). Next, all titles and abstracts fulfilling our inclusion criteria were reviewed and assessed for eligibility. Of these, two studies were excluded as they did not include a group with ADHD as the primary diagnosis. Four studies had to be excluded from the quantitative analysis due to missing data or different statistical approaches, e.g. without direct comparison of groups (Bioulac, Arfi, & Bouvard, 2008; Enagandula, Singh, Adgaonkar, Subramanyam, & Kamath, 2018; Kahraman & Demirci, 2018; Restrepo et al., 2020). A further study had to be excluded because the ADHD diagnosis was self-assessed (Nie, Zhang, Chen, & Li, 2016). Two studies were excluded as their results were based on the same study sample as another study already included in the analysis (Engelhardt, Mazurek, & Sohl, 2013; So et al., 2019). Ultimately, 14 studies remained eligible for the quantitative analysis (Fig. 1, Table 1). The second search in 2021 on PsycARTICLES, PsycINFO, PSYNDEX, MEDLINE, including publications from September 2020 to September 2021 and using the same search terms as before, but excluding COVID-19 or pandemic, led to 77 hits after the removal of 34 duplicates. 64 studies did not fulfill the criteria (no PUI n = 35, no ADHD focus n = 24, different age n = 5). Among the remaining 11 PUI studies on ADHD, only two studies used the requested methods, but one study had to be excluded because the age range did not fulfill the criteria, besides missing statistical information (Masi et al., 2021), the second study was published in Spanish (Menendez-García et al., 2020). In consequence, no new study was included in the meta-analysis.
Table 1.
Characteristics of included studies (alphabetic order)
| Author (year of publication), country | Age range (years) | PUI type | ADHD Group n
Age mean years (SD) Male/female |
Control Group n
Age mean years (SD) Male/female Type of control group |
Instrument/parameter (informant) | Results used for meta-analysis ADHD group M (SD) compared to control group M (SD) |
|
Basgul et al. (2020)
Turkey |
10–13 | Gaming |
n = 100 11.53 (1.03) 82m/18f |
n = 100 11.83 (0.98) 60m/40f Non-clinical |
Scale: Computer Game Addiction Scale for Children (CGASC); Time: Daily total playing time (hr) (SR) |
PUI- Scale (score): ADHD group 28.65 (9.19) > Control group 20.94 (7.37) PUI-Time (hr): ADHD group ∼1.82 (1.08), Control group ∼1.53 (0.90)a) |
|
Bourchtein et al. (2019)
USA |
12–14 | Technology use |
n = 162 13.17 (0.41) 105m/57 f School sample, but regular diagnostic procedure for ADHD |
n = 140 13.18 (0.40) 62m/78f Non-clinical |
Time: Total media time (min.) (PR) or rated on a 6-point Likert scale (SR) | PUI-Time (min) (PR): ADHD group 177.07 (114.35) > Control group 136.16 (72.33) PUI-Time (Likert scaled score) (SR): ADHD group 7.08 (4.17) > Control group 5.93 (2.69) |
|
Çakmak and Gul (2017)
Turkey |
12–16 | Internet use |
n = 34 13.50 (1.41) 23m/11f |
n = 36 13.50y (1.42) 23m/13f Non-clinical |
Scale: Online Cognition Scale (OCS) (PR); Time: Weekly internet use (hr per week))(PR) |
PUI-Scale (score): ADHD group 132 (38.67) > Control group 89.72 (26.87) PUI-Time (hr per week) ADHD group 15.73 (14.36) (hr per day =2.24 (2.05)) > Control group 7.66 (6.90) (hr per day = 1.09 (0.98)) |
|
Gul et al., (2018)
Turkey |
13–19 | Facebook overuse and addiction |
n = 187 14.9 (1.7) 95/92 |
n = 102 14.9 (1.4) 50/52, Clinical control (first referral, non-ADHD) |
Scale: Bergen Facebook Addiction Scale (BFAS) (SR) | PUI-Scale (score): ADHD group 40.4 (18.0) > Control group 27.9 (12.2) |
|
Huang et al. (2020)
Taiwan |
9–12 | Smartphone addiction |
n = 61 10.64 (1.00) 50m/11f |
n = 241 11.08 (0.81) 114m/127f Non-clinical |
Scale: Smartphone Addiction Proneness scale (SAPS) adapted for parents (PR) | PUI-Scale (score): ADHD group 35.59 (9.48) > Control group 31.36 (8.91) |
|
Izmir et al. (2019)
Turkey |
13–17 | Internet addiction |
n = 60 15.10 (1.86) Combined n = 25 Inattentive n=25 Hyperactive/impulsive n=10 |
n = 60 14.31 (2.23) No information on gender no ADHD; no other psychiatric diagnosis (/non-clinical/clinical?) |
Scale: Internet Addiction Diagnostic Questionnaire (IADQ) Young (1998) (SR) |
PUI-Scale (score): ADHD total group 59.41 (6.19)b) > Control group16.60 (5.62) |
|
Kietglaiwansiri and Chonchaiya (2018)
Thailand |
6–19 | Video game use |
n = 80 ∼9.83 (2.96) 65m/15f |
n = 102 ∼10.0 (1.48) 51m/51f Non-clinical |
Scale: Game Addiction Screen-ing Test (GAST); Time: PC time (PR) |
PUI-Scale (score): ADHD group ∼17.0 (12.5) > Control group ∼11.08 (10.55) PUI-Time: Weekday PC time (hr) ADHD group ∼2.03 (1.43) > Control group ∼1.53 (1.23) |
|
Luş and Eroğlu (2019)
Turkey |
12–17 | Internet addiction |
n = 100 12–14y n=69 15–17y n=30 78m/21f |
n = 95 12–14y n=51 15–17y n=44 34m/61f Non-ADHD clinical control (first referral) |
Scale: Young Internet Addiction Scale (IAT) (SR) | PUI-Scale (score): ADHD group 30.97 (17.74) > Control group 26.37 (13.85) |
|
Mazurek and Engelhardt (2013)
USA |
8–18 | Video Game use |
n = 44 11.10 (2.40) 44m/0 |
1. n = 41, 12.20 (1.40) 41m/0, Non-clinical 2. n = 56, 11.70 (2.20) 56/0, ASD |
Scale: Problem Video Game Playing Test (PVGT, King et al. 2011) adapted for parents (PR); Time: Video Game time, hr day−1 (PR) |
PUI-Scale (score) ADHD group 37.70 (9.20) > Control group 29.60 (7.10); ASD group 41.2 (12.7) > Control group 29.60 (7.10) PUI-Time (hr): ADHD group 1.70 (1.10) = Control group 1.20 (0.90); ASD group 2.1 (1.3) > Control group 1.20 (0.90) |
| Párraga et al. (2019) Spain | 6–16 | Video game playing |
n = 80 10.10 (2.39) 55m/25f |
n = 80 9.78 (2.38) 31m/49f Non-clinical |
Time: Questionnaire about the child's lifestyle habits: Playing video game time (hr day−1) (PR). |
PUI-Time (hr): ADHD group 0.21 (0.40) < Control group 0.52 (0.72) |
|
Razjouyan et al. (2020)
Iran |
Elementary school children | Internet addiction (video game addiction) |
n = 99 No information on age mean 66m/33f |
n = 99 No information on age mean approx.50m/50f Non-clinical |
Scale: Young's Internet Addiction Test (YIAT) (SR) | PUI-Scale (score): ADHD group 47.56 (13.43) > Control group 33.62 (14.09) |
|
So et al. (2017)
Japan |
12–15 | Internet addiction |
n = 24 14m/10f No information on mean age |
1. ASD: n = 83; 54m/29f 2. ADHD+ASD: n = 25; 15m/10f |
Scale: YIAT Time: internet time (hr) rated on 3-point-Likert scale (SR) | PUI-Scale (score): ADHD group 42.7 (19.1) = ASD group 45.2 (17.3) PUI-Time (hr): ADHD group ∼1.89 (1.51) = ASD group ∼1.79 (1.40) |
|
Thoma et al. (2020)
Germany |
8–18 | Screen based media use (time) |
n = 61 12.93 (2.13) 38m/23f |
n = 61; 2.97 (2.22) 38m/23f Non-clinical |
Time: Total media use schooldays (min). Screen time-based sedentary behavior questionnaire (Rey-López et al., 2012); (SR) | PUI-Time (min): ADHD group 275.2 (227.4) > Control group 167.7 (161.3) |
|
Weinstein et al. (2015)
Israel |
13–15 | Internet addiction (video game addiction) |
n = 50 13.75 (0.80) 50/0 Special school students with formal diagnosis of ADHD |
n = 50 14.0 (0.60) 50/0 Special school students, non-ADHD |
Scale: Young's Internet Addiction Test (IAT) Time: hours spent on internet per day (4-point Likert scale) (SR) | PUI-Scale (score): ADHD group 2.93 (1.06) > Control group 2.22 (0.65) PUI-Time (hr): ADHD group ∼3.14 (2.35) > Control group ∼2.08 (1.54) |
Notes: PR =Parent rating, SR= Self rating; ASD: Autism Spectrum Disorder. M= mean, SD= standard deviation. Estimated time data (based on recoded scores) or transformed values are indicated by ∼. “ADHD group > control group” indicates significantly higher PUI values in ADHD, “ADHD group < control group” indicates significantly lower PUI values in ADHD group; “ADHD group = Control group” indicates no significant difference. a) not statistically compared. b) ADHD score calculated from 3 subtype scores. Studies are listed in alphabetic order of authors.
Study description
All 14 studies contained a comparison between a group of children and adolescents diagnosed with ADHD and a group of controls without ADHD, drawn from the general population or from another clinically referred group or special school students. When studies contained more than one control group – i.e. non-clinical controls and controls with other psychopathology – the non-clinical control group was used for the analyses (except for the clinical controls subgroup analysis). Study characteristics including authors, country of origin, type of PUI investigated in the study, description of samples, used PUI measures and study results are depicted in Table 1. Studies differed with regard to sample size, objective, and form and completeness of provided data (Table S1., Supplementary material). The studies by Bourchtein et al. (2019) and Thoma et al. (2020) investigated the relation between digital media use and sleep; Párraga et al. (2019) investigated life-style habits including the use of digital media. Izmir, Ipci, and Ercan (2019) investigated PUI and aggression in ADHD subtypes. The other studies were directly related to the investigation of subtypes of PUI in ADHD and controls (Table 1).
PUI in the included studies was assessed either by the duration of the internet/digital media use, e.g. minutes, hours, daily, weekly use (=time-based measures) (Bourchtein et al., 2019; Párraga et al., 2019; Thoma et al., 2020) or with Likert scales indicating the severity of PUI (=scale-based measures) (Gul, Yurumez Solmaz, Gul, & Oner, 2018; Huang, Hu, Shyu, & Yeh, 2020; Izmir et al., 2019; Luş & Eroğlu, 2019, Razjouyan, Khademi, Dorandish, & Davari-Ashtiani, 2020) (Tables 1 and 2). Six studies reported results of both approaches to measure PUI (Bourchtein et al., 2019; Basgul, Bekar, & Lus, 2020; Çakmak & Gul, 2017; Kietglaiwansiri & Chonchaiya, 2018; Mazurek & Engelhardt, 2013; So et al., 2017). Another study also assessed both but reported incomplete time-based data (Izmir et al., 2019). Kietglaiwansiri and Chonchaiya (2018) presented age and results as median and quartiles, which we transformed into means and standard deviation using the formula published by Wan and co-authors (Wan, Wang, Liu, & Tong, 2014). In three studies, the time spent on digital media was indicated on Likert scales with time ranges (Kietglaiwansiri & Chonchaiya, 2018; So et al., 2017; Weinstein, Yaacov, Manning, Danon, & Weizman, 2015). In these cases, when the distribution of responses on the Likert scale was available, estimated time means were derived by recoding time ranges into estimated mean values and by calculating group means and standard deviations (e. g. Likert scale points: A = less than 1 h; B = 1–3 h; C = more than 3 h; were recoded into: A = 0.5 h; B = 2 h; C = 4 h). These estimated results are indicated on Table 1 by “∼”. When weekday and weekend use time were both reported, we opted for the weekday time, because it represents the more critical factor for daily life functioning.
Table 2.
Summary of characteristics of included studies
| Characteristics | Included studies |
| Publication year range | 2013–2021 |
| Participants (n) | 2,488 |
| Range of age means | 9.5–16.41 years |
| Studies with children (age mean <12 years) | 6 (SR: 2) |
| Studies with adolescents (age mean >12 years) | 8 (SR: 6, SR + PR: 1) |
| Studies scale-based/time-based/both | 5/3/6 |
| Studies on general internet or media use/PUI/gaming/other | 3/6/4/2 |
| Studies with one or more clinical (or not typically developing) control groups | 5 |
| No. of countries | 10 |
Note. SR= Self-rating, PR= Parent rating.
Studies employed diverse rating scales or questionnaires for the measurement of different aspects of PUI (Tables 1 and 2). To measure technology use among adolescents, Bourchtein et al. (2019) used time duration in minutes as well as Likert-scaled time measures: While parents indicated in minutes how much time their child spent using different communication media, the adolescents answered four similar questions on a Likert scale. In the study by Huang et al. (2020), parents of participants completed the Smartphone Addiction Proneness scale (SAPS) (Kim, Lee, Lee, Nam, & Chung, 2014), adapted for parents. The Internet Addiction Diagnostic Questionnaire (IADQ), which was used by Izmir et al. (2019), is a self-report instrument of eight items and based on the DSM-IV-TR criteria for pathological gambling (Young, 1996, 1998). Four studies used Young's Internet Addiction Test (YIAT or IAT, Young, 1998) (Luş & Eroğlu, 2019; Razjouyan et al., 2020b; So et al., 2017; Weinstein et al., 2015). This self-report questionnaire is composed of 20 questions with a total score ranging from 20 to 100. In the study by Mazurek and Engelhardt (2013), parents were asked to report the number of hours per day which their child spends gaming and to complete a modified version of the Problem Video Game Playing Test (PVGT) (King, Delfabbro, & Zajac, 2011). The remaining studies used scales such as the Online Cognition Scale (OCS) (Davis, Flett, & Besser, 2002), the Bergen Facebook Addiction Scale (BFAS) (Andreassen, TorbjØrn, Brunborg, & Pallesen, 2012) or the Game Addiction Screening Test (GAST) (Pornnoppadol, Sornpaisarn, Khamklieng, & Pattanaamorn, 2014) (Table 1). Five of the studies presented parent-rated data, eight self-rated data and one study provided both (Tables 1 and 2).
Methodological study quality
Studies' quality was heterogeneous (details are presented in Supplementary material). A clinical diagnosis of ADHD was a criterion for inclusion in the meta-analysis and many studies reported that clinical ADHD diagnoses were established in psychiatric hospitals or outpatient units, but without describing the diagnostic procedure any further. Five out of 14 studies did not explicitly assess or exclude comorbidities in the ADHD group, and seven in the control group. Despite the fact that the subtypes of PUI are known to be gender-specific, e.g. with higher rates of problematic gaming in boys, only five studies showed an appropriate matching for sex (Çakmak & Gul, 2017; Gul et al., 2018; Párraga et al., 2019, So et al., 2017; Thoma et al., 2020) or included only boys (Mazurek & Engelhardt, 2013; Weinstein et al., 2015) (Supplementary material). The remaining studies did not control or match for sex or the male/female ratio was not reported.
Analyses
The two main analyses investigated PUI differences between ADHD and controls separately for time-based and scale-based measures. Both analyses were further subdivided into studies with children (ADHD age mean under 12 years) and adolescents (age mean over 12 years). The next subgroup analyses were conducted separately for parent-rated and self-rated measures. The overall analysis of these two subgroup analyses constitutes an overall analysis of this meta-analysis, including all 14 studies. Finally, a subgroup analysis was performed for studies which compared ADHD patients not with healthy controls, but with other clinical or psychopathological groups, or special school students, respectively. This subgroup analysis was contrasted with the analysis of all studies comparing individuals with ADHD to non-clinical controls. Whenever necessary, sensitivity analyses were performed (Table 3).
Table 3.
Effect sizes and results for main and subgroups differences and results of sensitivity analyses
| Effects of comparison | Hetero- Subgroup geneity differences | |||||||
| Studies (K) | Participants (n) | SMD | 95% CI | Z | P | I 2 | P | |
| 1. Time-based all | 9 | 1,328 | 0.31 | 0.07–0.55 | 2.55 | 0.01 | 77% | 0.22 |
| Children | 4 | 627 | 0.15 | −0.30–0.60 | 0.66 | 0.51 | 87% | |
| Adolescents | 5 | 701 | 0.45 | 0.29–0.61 | 5.41 | <0.001 | 7% | |
| 1. SA Time-based all b) | 8 | 1,168 | 0.41 | 0.29–0.53 | 6.84 | <0.001 | 0% | 0.48 |
| Children b) | 3 | 467 | 0.36 | 0.18–0.54 | 3.85 | <0.001 | 0% | |
| 2. Scale-based all | 11 | 1,848 | 1.13 | 0.66–1.60 | 4.70 | <0.001 | 95% | 0.12 |
| Children | 5 | 967 | 0.76 | 0.52–1.00 | 6.27 | <0.001 | 65% | |
| Adolescents | 6 | 881 | 1.58 | 0.59–2.57 | 3.12 | 0.002 | 95% | |
| 2. SA Scale-based all a) | 10 | 1,728 | 0.68 | 0.46–0.90 | 6.14 | <0.001 | 76% | 0.45 |
| Adolescents a) | 5 | 761 | 0.59 | 0.19–0.98 | 6.14 | <0.001 | 83% | |
| 3. Parent- vs. self-rated all | 14 | 2,252 | 0.91 | 0.63–1.31 | 4.39 | <0.001 | 95% | 0.05 |
| Parent-rated | 6 | 921 | 0.49 | 0.05–0.93 | 2.19 | <0.001 | 90% | |
| Self-rated | 8 | 1,331 | 1.27 | 0.63–1.91 | 3.87 | <0.001 | 95% | |
| 3. SA Parent- vs. self-rated all a), b) | 12 | 1,972 | 0.64 | 0.46–0.83 | 4.54 | <0.001 | 74% | 0.81 |
| Parent-rated b) | 5 | 761 | 0.67 | 0.39–0.94 | 4.79 | <0.001 | 67% | |
| Self-rated a) | 7 | 1,211 | 0.62 | 0.35–0.89 | 4.54 | <0.001 | 79% | |
| 4. Non-clinical vs. clinical controls all | 14 | 2,452 | 0.84 | 0.46–1.23 | 4.33 | <0.001 | 95% | 0.01 |
| Clinical controls | 5 | 791 | 0.29 | −0.14, 0.72 | 1.34 | 0.180 | 87% | |
| Non-clinical (healthy) controls | 9 | 1,661 | 1.20 | 0.65–1.76 | 4.25 | <0.001 | 96% | |
| 4. SA Clinical controls vs. non-clinical controls all a),b) | 12 | 2,172 | 0.55 | 0.33–0.76 | 5.03 | <0.001 | 81% | 0.09 |
| Non-clinical (healthy) controls a), b) | 7 | 1,381 | 0.70 | 0.48–0.92 | 6.29 | <0.001 | 71% | |
Note. SA = Sensitivity analysis; Italics: sensitivity analysis; a) Izmir et al. (2019) removed; b) Párraga et al. (2019) removed.
Time-based measures
The SMD (standardized mean differences) for the overall time-based analysis including nine studies was 0.31 (95% CI: 0.07, 0.55), indicating that children and adolescents with ADHD spend more time on media than controls (Fig. 2). Heterogeneity was high (I 2 = 77%), but sensitivity analysis revealed that it was reduced to 0% when the study by Párraga et al. (2019) was removed (Table 3). When children and adolescents were considered separately, effects in the children's group were small (SMD of 0.15, 95% CI: −0.30, 0.60) and heterogeneity was important (I 2 = 87%). Again, sensitivity analysis showed that the removal of Párraga et al.’s (2019) study led to a larger effect (SMD=0.36, 95% CI: 0.18, 0.54) with longer internet times in children with ADHD than in controls, and no heterogeneity (I 2 = 0%). In the adolescent subgroup analysis of the time spent on media, SMD was moderate (0.45, 95% CI: 0.29, 0.61). Taken together, it can be concluded that adolescents with ADHD spend more time on media than do non-affected controls, and that most results from studies with children point in the same direction.
Scale-based measures
The overall SMD of 11 scale-based studies comparing participants with and without ADHD was large (1.31, 95% CI: 0.66, 1.60) and indicated higher severity of problematic internet/media use in ADHD compared to controls (Table 2, Fig. 4). Similar results were obtained when children and adolescents were considered separately. In both subgroups, individuals with ADHD obtained higher scores on PUI scales than did controls, indicating more severe PUI. The SMD was large for adolescents (1.58, 95% CI: 0.59, 2.57) and moderate for children (0.76, 95% CI: 0.52, 1.00), but subgroup differences were not significant (P < 0.12) (Table 3). Heterogeneity was very high for the overall analysis (I 2 = 97%) and was reduced to 76% when the study by Izmir et al. (2019) was removed (Table 3).
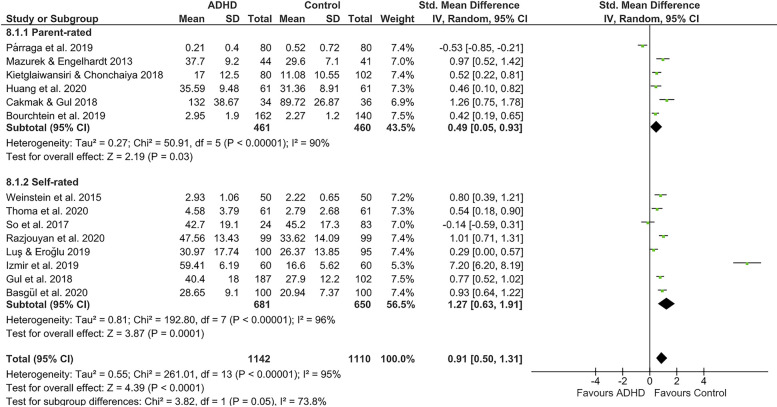
Fig. 4.
Parent-rated and self-rated measures of PUI in groups with ADHD compared to controls
Parent- vs. self-rated measures
All 14 selected studies were entered into this analysis, which therefore represents an overall analysis, with both time-based and scale-based measures. If time and scale parameters were available in the same study, we opted for the scale-based score. Six studies using parent-rated measures resulted in a SMD of 0.49 (95% CI: 0.05, 0.93) between participants with and without ADHD. Heterogeneity was elevated (I 2 = 90%) and was reduced to 67% after removal of the study by Párraga et al. (2019) (Table 3). Eight studies with self-rated measures had a large SMD (1.27, 95% CI: 0.63, 1.91). Heterogeneity was elevated (I 2 = 96%) and was reduced to 79% after the removal of the study by Izmir et al. (2019). Effects of studies with self- and parent-rated PUI differed marginally (P = 0.05) when all 14 studies were considered, with larger effects for self-rated studies, but no longer differed after the removal of the studies by Izmir et al. (2019) and Párraga et al. (2019) (parent-rated SMD 0.67, 95% CI: 0.39, 0.94), self-rated SMD 0.62, 95% CI: 0.35, 0.89; subgroup differences: P < 0.0.81; Table 3.
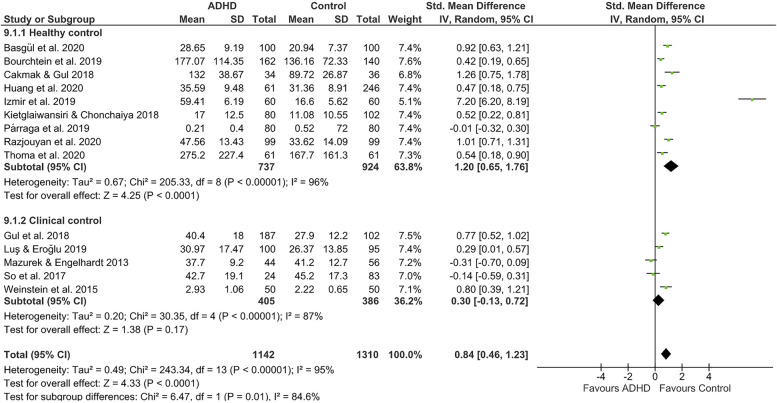
ADHD compared to other clinical groups
Five studies included clinical control groups or special school students. In two studies, children and adolescents with ADHD were compared to patients with autism spectrum disorder (ASD) (Mazurek & Engelhardt, 2013; So et al., 2017). In two other studies, controls were individuals referred to child and adolescent psychiatry (first time referral) without a diagnosis of ADHD, which may include all possible kinds of psychopathology as well as no diagnosis (Gul et al., 2018; Luş & Eroğlu, 2019). Weinstein et al. (2015) compared students with a diagnosis of ADHD enrolled in a special school for students with learning or behavioral problems to other special school students without ADHD as the control group. The analysis revealed that the SMD between the ADHD groups and the clinical comparison groups was small (0.30, 95 % CI: -0.13, 0.72) (Fig. 5, Table 3) and heterogeneity was elevated (I 2 = 87%). As shown in the forest plot and by negative SMDs, both studies with ASD patients (Mazurek & Engelhardt, 2013; So et al., 2019) indicated less severe PUI in the ADHD group than in the ASD group. When ADHD vs. clinical subgroup effects were compared to ADHD vs. non-clinical subgroup effects, subgroup differences were significant (P < 0.001).
Fig. 5.
Analyses of PUI in groups with ADHD compared with non-clinical (healthy) versus clinical controls
The non-clinical group was composed of the nine remaining studies, with six scale-based and three time-based study results. In the study by Izmir et al. (2019) the control group was obviously recruited from clinically referred children, who had not received a diagnosis according to DSM-5. We decided here to categorize them as non-clinical. Overall effects within the ADHD vs. non-clinical group were large (SMD = 1.20, 95% CI: 0.65, 1.76) but heterogeneity was high (I 2 = 96%). The removal of the study by Izmir et al. (2019) reduced heterogeneity to 81%, and the additional removal of the study by Párraga et al. reduced heterogeneity further to 71%. After the removal of both studies from the non-clinical subgroup, only a trend for subgroup differences for ADHD vs. healthy and ADHD vs. clinical controls remained (Chi2 = 2.79, P < 0.09) (Table 3).
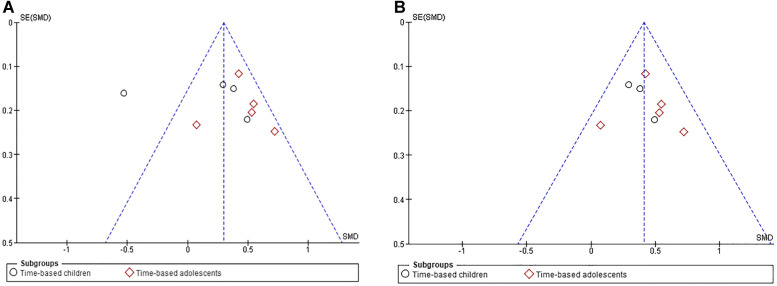
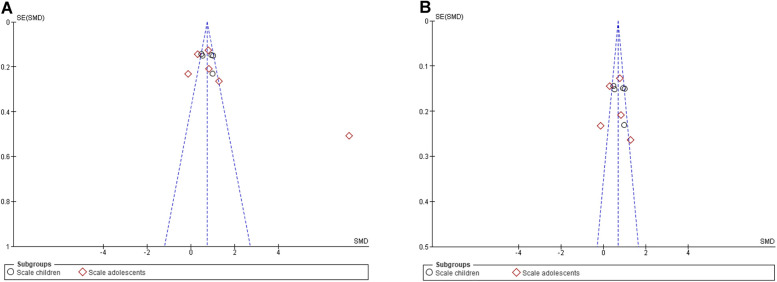
Analysis of bias
The two main analyses (time-based and scale-based group comparison) were analyzed by funnel plots for the estimation of publication bias. The time-based analysis was asymmetric with more studies tending towards the right, but symmetry improved after the removal of the study by Párraga et al. (Fig. A1). The funnel plot of the scale-based analyses showed a more symmetrical pattern, which was further improved after the study by Izmir et al. was removed (Fig. A2). In consequence, after removal of two critical studies identified by the sensitivity analysis, funnel plots did not provide strong evidence of publication bias, but given the small number of studies, this interpretation must be treated with caution (Sterne et al., 2011). The study by Párraga et al. (2019) differed from the other studies insofar as lifestyle habits rather than Internet addiction were assessed. The computer time indicated by parents for their children with ADHD was extremely low (approx. 0.2 h per day) and significantly lower than that indicated for control children (0.51 h per day). The study authors pointed out that this finding was unexpected and in contrast to other reports on media time in ADHD. A possible explanation may be that Párraga et al. (2019) examined only families with high socio-economic status, which may lead to higher academic pressure (Owens, 2020, 2021) and to a stricter control of screen time. It is possible that in this particular group, parents of schoolchildren with ADHD (age mean 10.10 years) tended to control their child's media time more rigorously compared to parents of healthy control children. In the study by Izmir et al. (2019), heterogeneity was added to the analysis not because the results showed a reverse effect, but because the effect was unexpectedly high. The study was characterized by low scores on the IADQ in the control group (mean = 16.69) and mean daily internet times of approximately 1 h (not included in the analysis because of incomplete data), which is low for typical teenagers aged between 13 and 17 years. Moreover, the focus of the study was not on the comparison to a control group, but on the association between symptoms of PUI and aggression in adolescents with subtypes of ADHD.
Discussion
The present meta-analysis revealed that individuals with a diagnosis of ADHD had higher PUI values both in time-based and in scale-based measures compared to controls, indicating that youth with ADHD spend more time on digital media and have more severe symptoms of problematic internet use compared to age-matched healthy controls. Neither time-based nor scale-based results differed significantly when the results from children and adolescent were compared. In consequence, enhanced PUI measures do not seem to depend on the age of ADHD participants.
Similarly, differences between the ADHD groups and controls were present irrespective of the source of information: parent-ratings and self-ratings led to equivalent results, at least after the removal of two studies which were responsible for increased heterogeneity. Nevertheless, there was a certain overlap between age groups and informant groups, as the majority of parent-rated results came from studies with children, and the majority of self-rated measures from studies with adolescents. Thus, in order to draw more general conclusions regarding the impact of the informant, it would be necessary to contrast studies with participants of the same age group. For the time being, such studies are still lacking. While all study findings showed that youth with a diagnosis of ADHD differed in PUI intensity or severity from healthy/nonclinical control samples, conclusions regarding other clinical groups were less evident. We identified only four studies which included a direct comparison between ADHD and other clinical groups without ADHD. A fifth study (Weinstein et al., 2015) used special school students as controls, which we included in the “clinical” group, as these students did not belong to a typically developing population of children. The comparison between the subgroup of studies with healthy controls and clinical controls resulted in a significant difference between the subgroup effects. Thus, the severity of PUI in individuals with ADHD differed significantly from the PUI severity in healthy controls but not from clinical controls. More specifically, the two studies contrasting ASD (without comorbid ADHD) and ADHD showed more severe PUI impairment in ASD, while the other three studies with clinical controls showed effects with stronger impairment in the ADHD subgroup.
Most main and subgroup analyses indicated high heterogeneity between studies, which was expected given the high variability of samples, of measures, and the differing recruitment procedures for control participants. Sensitivity analyses showed that two studies in particular were partly responsible for this heterogeneity, which was considerably reduced by their removal: Párraga et al. (2019) and Izmir et al. (2019). The fact that only half of the included studies were appropriately matched for sex may be considered a serious confound, since digital habits, preferences and also problematic use and its consequences can differ considerably between the sexes (Derevensky et al., 2019; Durkee et al., 2012; Kim, Kim, Choi, Kim, & Kim, 2020).
In summary, this first meta-analysis directly comparing PUI measures in children and adolescents with a clinical diagnosis of ADHD and controls suggests that individuals with ADHD differ from healthy individuals regarding PUI intensity and severity. This is consistent with the literature reporting strong associations between ADHD symptoms and PUI (Boer, van den Eijnden, et al., 2020b; Carli et al., 2013; Kahraman & Demirci, 2018; Kim et al., 2019; Ko, Yen, Chen, Yeh, & Yen, 2009; Ozturk, Ekinci, Ozturk, & Canan, 2013; Panagiotidi & Overton, 2020; Zhang et al., 2015). In contrast to most other reviews, this meta-analysis excluded studies which were solely based on correlational analyses of ADHD symptoms and PUI but used studies that compared clinically diagnosed children and adolescents with ADHD and control groups. While no causal inference can be drawn from this type of investigation, the clinical diagnosis of ADHD appears nevertheless to be a risk factor for PUI/the overuse of digital media. This is in line with neuropsychological and neurobiological models of ADHD, which relate ADHD behavioral problems to deficits in self-regulation and reward processing (Rubia, 2018), deficits that may also contribute to the development of PUI (Brand et al., 2014). However, dysfunctions characteristic for PUI may be largely transdiagnostic (Restrepo et al., 2020). The differentiation of hypothetical ADHD-specific PUI patterns from those of other psychopathological disorders will require further analyses focusing on qualitative and quantitative aspects of digital media-related behaviors in ADHD. Besides comorbidity, possible gender-specific differences and age-specific trajectories of PUI should also be taken into account. From a clinical perspective, the results suggest that the screening for PUI – or at least an exploration of digital media behavior - should be an integral part of the clinical ADHD assessment.
Limitations
The inclusion of only 14 studies in the present analysis, encompassing 2,488 participants, was probably the biggest drawback of the meta-analysis, causing several limitations. Given the small number and heterogeneity of subgroups, especially of clinical control group studies, caution is warranted when drawing conclusions on clinical controls and on parent-vs. self-rated measures. A confound of age group and informant cannot be excluded. Due to a lack of studies on this topic, it was not possible to conduct an analysis of ADHD groups with and without comorbidities, as had originally been planned. It also remains a methodological problem that most studies did not address the aspect of comorbidity at all; therefore, we cannot assume that the studies summarized in this meta-analysis only included cases of “pure” ADHD. In consequence, the specific impact of clinically diagnosed ADHD in contrast to or in combination with other psychopathological disorders could not be answered satisfactorily and further studies on this specific topic are needed. Similarly, only very few studies differentiated between different presentations of ADHD. As already discussed, several studies did not take into account differences in the sex ratio of groups. Finally, different subtypes of PUI and different measures are included here in the same analyses.
Conclusion
This meta-analytical investigation was able to identify group differences between individuals diagnosed with ADHD and healthy controls. These results contribute to the assumption that children and adolescents diagnosed with ADHD are at risk for PUI. Nevertheless, a higher risk of PUI does not appear to be limited to ADHD, and other clinical groups should also be screened for PUI during routine psychiatric assessments. Problematic internet/digital media use in diagnosed clinical groups and its association with psychopathological disorders – not only symptoms - remains insufficiently researched in child and adolescent psychiatry. In particular, the role of comorbidities in the development of PUI in ADHD requires further investigation.
Funding sources
No financial support was received for this review and the study was not registered.
Authors' contribution
AW, RD and SW concept and design of the study; AW, SK, SE, RD data extraction, statistical analysis; AW, SK, SE, RD analysis and interpretation; AW, RD and SK drafting and revising the article; all authors contributed to the critical revision of the article. The corresponding author (AW) affirms that she had access to all data from the study, both what is reported and what is unreported, and also that she had complete freedom to direct its analysis and its reporting, without influence from the sponsors. The corresponding author (AW) also affirms that there was no editorial direction or censorship from the sponsors.
Conflict of interest
S. Walitza has received in the last 5 years royalties from Thieme Hogrefe, Kohlhammer, Springer, Beltz. Her work was supported in the last 5 years by the Swiss National Science Foundation (SNF), diff. EU FP7s, Bfarm Germany, ZInEP, Hartmann Müller Stiftung, Olga Mayenfisch, Gertrud Thalmann, Vontobel, Unicentia, Erika Schwarz Fonds. Outside professional activities and interests are declared under the link of the University of Zurich https://www.uzh.ch/prof/ssl-dir/interessenbindungen/client/web/. RD has received royalties from Hogrefe and her work has been supported by the SNF in the last 5 years. The other authors declare no conflict of interest.
Supplementary Materials
Appendix
Fig. A1.
Funnel plots of studies based on time-based PUI measures in children and adolescents with ADHD compared to controls, A. all included studies, B. after removal of the study by Párraga et al., 2019
Fig. A2.
Funnel plots of studies based on scale-based PUI measures in children and adolescents with ADHD compared to controls. A. all included studies, B. after removal of the study by Izmir et al., 2019
Contributor Information
Anna Maria Werling, Email: anna.werling@pukzh.ch.
Sajiv Kuzhippallil, Email: sajiv.kuzhippallil@pukzh.ch.
Sophie Emery, Email: sophie.emery@pukzh.ch.
Susanne Walitza, Email: susanne.walitza@pukzh.ch.
Renate Drechsler, Email: renate.drechsler@kjpd.uzh.ch.
Acknowledgements
The authors appreciate the support and collaboration of the European Network for Problematic Usage of the Internet of the COST Action CA16207 (European Cooperation in Science and Technology).
References
- Anderson, E. L. , Steen, E. , & Stavropoulos, V. (2017). Internet use and problematic internet use: A systematic review of longitudinal research trends in adolescence and emergent adulthood. International Journal of Adolescence and Youth , 22(4), 430–454. Routledge. 10.1080/02673843.2016.1227716. [DOI] [Google Scholar]
- Andreassen, C. S , Billieux, J. , Griffiths, M. D. , Kuss, D. J , Demetrovics, Z. , Mazzoni, E. , & Pallesen, S. (2016). The relationship between addictive use of social media and video games and symptoms of psychiatric disorders: A large-scale cross-sectional study. Psychology of Addictive Behaviors , 30(2), 252–262. 10.1037/adb0000160. [DOI] [PubMed] [Google Scholar]
- Andreassen, C. S. , TorbjØrn, T. , Brunborg, G. S. , & Pallesen, S. (2012). Development of a Facebook addiction scale. Psychological Reports , 110(2), 501–517. 10.2466/02.09.18.PR0.110.2.501-517. [DOI] [PubMed] [Google Scholar]
- APA (2013). Diagnostic and statistical manual of mental disorders (5th ed.). [Google Scholar]
- Barry, C. T. , Sidoti, C. L. , Briggs, S. M. , Reiter, S. R. , & Lindsey, R. A. (2017). Adolescent social media use and mental health from adolescent and parent perspectives. Journal of Adolescence , 61, 1–11. 10.1016/j.adolescence.2017.08.005. [DOI] [PubMed] [Google Scholar]
- Barth, G. M. , & Renner, T. J. (2015). ADHS und Mediensucht bei Kindern und Jugendlichen. SUCHT , 61(5), 293–301. 10.1024/0939-5911.a000385. [DOI] [Google Scholar]
- Basgul, S. S. , Bekar, B. , & Lus, M. G. (2020). Associations between computer game addiction and attention deficit and hyperactivity disorder - an emprical study. ADDICTA: The Turkish Journal on Addictions , 7(2), 122–128. 10.5152/addicta.2020.20142. [DOI] [Google Scholar]
- Baumgartner, S. E. , van der Schuur, W. A. , Lemmens, J. S. , & te Poel, F. (2017). The relationship between media multitasking and attention problems in adolescents: Results of two longitudinal studies. Human Communication Research , 44(1), 3–30. 10.1111/hcre.12111. [DOI] [Google Scholar]
- Billieux, J. , King, D. L. , Higuchi, S. , Achab, S. , Bowden-Jones, H. , Hao, W. , … Poznyak, V. (2017). Functional impairment matters in the screening and diagnosis of gaming disorder. Journal of Behavioral Addictions , 6(3), 285–289. Akademiai Kiado Rt. 10.1556/2006.6.2017.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bioulac, S. , Arfi, L. , & Bouvard, M. P. (2008). Attention deficit/hyperactivity disorder and video games: A comparative study of hyperactive and control children. European Psychiatry , 23(2), 134–141. 10.1016/j.eurpsy.2007.11.002. [DOI] [PubMed] [Google Scholar]
- Boer, M. , Stevens, G. , Finkenauer, C. , & van den Eijnden, R. (2020a). Attention deficit hyperactivity disorder-symptoms, social media use intensity, and social media use problems in adolescents: Investigating directionality. Child Development , 91(4), e853–e865. 10.1111/cdev.13334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boer, M. , van den Eijnden, R. J. J. M. , Boniel-Nissim, M. , Wong, S. L. , Inchley, J. C. , Badura, P. , … Stevens, G. W. J. M. (2020b). Adolescents’ intense and problematic social media use and their well-being in 29 countries. Journal of Adolescent Health , 66(6), S89–S99. 10.1016/j.jadohealth.2020.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourchtein, E. , Langberg, J. M. , Cusick, C. N. , Breaux, R. P. , Smith, Z. R. , & Becker, S. P. (2019). Featured article: Technology use and sleep in adolescents with and without attention-deficit/hyperactivity disorder. Journal of Pediatric Psychology , 44(5), 517–526. 10.1093/jpepsy/jsy101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brand, M. , Young, K. S. , & Laier, C. (2014). Prefrontal control and internet addiction: A theoretical model and review of neuropsychological and neuroimaging findings. Frontiers in Human Neuroscience , 8(MAY), Frontiers Media S. A. 10.3389/fnhum.2014.00375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Çakmak, F. H. , & Gul, H. (2017). Factors associated with problematic İnternet use among children and adolescents with attention deficit hyperactivity disorder. Northern Clinics of Istanbul , 5(4), 302. 10.14744/nci.2017.92668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caplan, S. E. (2007). Relations among loneliness, social anxiety, and problematic internet use. Cyberpsychology and Behavior , 10(2), 234–242. 10.1089/cpb.2006.9963. [DOI] [PubMed] [Google Scholar]
- Carbonell, X. , Chamarro, A. , Oberst, U. , Rodrigo, B. , & Prades, M. (2018). Problematic use of the internet and smartphones in university students: 2006–2017. International Journal of Environmental Research and Public Health , 15(3). 10.3390/ijerph15030475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carli, V. , Durkee, T. , Wasserman, D. , Hadlaczky, G. , Despalins, R. , Kramarz, E. , … Kaess, M. (2013). The association between pathological internet use and comorbid psychopathology: A systematic review. Psychopathology, 46(1), 1–13, Psychopathology. 10.1159/000337971. [DOI] [PubMed] [Google Scholar]
- Çelik, Ç. B. , Odacı, H. , & Bayraktar, N. (2015). Is problematic internet use an indicator of eating disorders among Turkish university students? Eating and Weight Disorders , 20(2), 167–172. 10.1007/s40519-014-0150-3. [DOI] [PubMed] [Google Scholar]
- Ceranoglu, T. A. (2018). Inattention to problematic media use habits: Interaction between digital media use and attention-deficit/hyperactivity disorder. Child and Adolescent Psychiatric Clinics of North America , 27(2), 183–191. W.B. Saunders. 10.1016/j.chc.2017.11.009. [DOI] [PubMed] [Google Scholar]
- Chamberlain, S. R. , Redden, S. A. , Stein, D. J. , Lochner, C. , & Grant, J. E. (2017). Impact of obsessive-compulsive personality disorder symptoms in Internet users. Annals of Clinical Psychiatry : Official Journal of the American Academy of Clinical Psychiatrists , 29(3), 173–181. 10.17863/CAM.12541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng, Y. S. , Tseng, P. T. , Lin, P. Y. , Chen, T. Y. , Stubbs, B. , Carvalho, A. F. , … Wu, M. K. (2018). Internet addiction and its relationship with suicidal behaviors: A meta-analysis of multinational observational studies. Journal of Clinical Psychiatry , 79(4). 10.4088/JCP.17r11761. [DOI] [PubMed] [Google Scholar]
- Darvesh, N. , Radhakrishnan, A. , Lachance, C. C. , Nincic, V. , Sharpe, J. P. , Ghassemi, M. , … Tricco, A. C. (2020). Exploring the prevalence of gaming disorder and internet gaming disorder: A rapid scoping review. Systematic reviews , 9(1), BioMed Central Ltd. 10.1186/s13643-020-01329-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis, R. A. (2001). Cognitive-behavioral model of pathological Internet use. Computers in Human Behavior , 17(2), 187–195. 10.1016/S0747-5632(00)00041-8. [DOI] [Google Scholar]
- Davis, R. A. , Flett, G. L. , & Besser, A. (2002). Validation of a new scale for measuring problematic internet use: Implications for pre-employment screening. Cyberpsychology and Behavior , 5(4), 331–345. 10.1089/109493102760275581. [DOI] [PubMed] [Google Scholar]
- Dell'Osso, B. , Di Bernardo, I. , Vismara, M. , Piccoli, E. , Giorgetti, F. , Molteni, L. , … Viganò, C. (2021). Managing problematic usage of the internet and related disorders in an era of diagnostic transition: An updated review. Clinical Practice and Epidemiology in Mental Health: CP & EMH , 17, 61–74. 10.2174/1745017902117010061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demetrovics, Z. , Szeredi, B. , & Rózsa, S. (2008). The three-factor model of internet addiction: The development of the problematic internet use questionnaire. Behavior Research Methods , 40(2), 563–574. 10.3758/BRM.40.2.563. [DOI] [PubMed] [Google Scholar]
- Demirci, K. , Akgönül, M. , & Akpinar, A. (2015). Relationship of smartphone use severity with sleep quality, depression, and anxiety in university students. Journal of Behavioral Addictions , 4(2), 85–92. 10.1556/2006.4.2015.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derevensky, J. L. , Hayman, V. , & Gilbeau, L. (2019). Behavioral addictions: Excessive gambling, gaming, Internet, and smartphone use among children and adolescents. Pediatric Clinics , 66(6), 1163–1182. 10.1016/j.pcl.2019.08.008 [DOI] [PubMed] [Google Scholar]
- DerSimonian, R. , & Laird, N. (1986). Meta-analysis in clinical trials. Controlled Clinical Trials , 7(3), 177–188. 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- Dullur, P. , Krishnan, V. , & Diaz, A. M. (2021). A systematic review on the intersection of attention-deficit hyperactivity disorder and gaming disorder. Journal of Psychiatric Research , 133, 212–222, Elsevier Ltd. 10.1016/j.jpsychires.2020.12.026. [DOI] [PubMed] [Google Scholar]
- Durkee, T. , Kaess, M. , Carli, V. , Parzer, P. , Wasserman, C. , Floderus, B. , … Wasserman, D. (2012). Prevalence of pathological internet use among adolescents in Europe: Demographic and social factors. Addiction , 107(12), 2210–2222. 10.1111/j.1360-0443.2012.03946.x. [DOI] [PubMed] [Google Scholar]
- Enagandula, R. , Singh, S. , Adgaonkar, G. , Subramanyam, A. , & Kamath, R. (2018). Study of internet addiction in children with attention-deficit hyperactivity disorder and normal control. Industrial Psychiatry Journal , 27(1), 110. 10.4103/ipj.ipj_47_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engelhardt, C. R. , Mazurek, M. O. , & Sohl, K. (2013). Media use and sleep among boys with autism spectrum disorder, adhd, or typical development. Pediatrics , 132(6), 1081–1089. 10.1542/peds.2013-2066. [DOI] [PubMed] [Google Scholar]
- Faraone, S. V. , Banaschewski, T. , Coghill, D. , Zheng, Y. , Biederman, J. , Bellgrove, M. A. , … Wang, Y. (2021). The world federation of ADHD international consensus statement: 208 evidence-based conclusions about the disorder. Neuroscience and Biobehavioral Reviews , Elsevier Ltd, 10.1016/j.neubiorev.2021.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fariba, K. , & Gokarakonda, S. (2020). Impulse control disorders. Psychiatry . https://scholarlycommons.hcahealthcare.com/psychiatry/17. [PubMed] [Google Scholar]
- Fineberg, N. A. , Demetrovics, Z. , Stein, D. J. , Ioannidis, K. , Potenza, M. N. , Grünblatt, E. , … Chamberlain, S. R. (2018). Manifesto for a European research network into problematic usage of the internet. European Neuropsychopharmacology , 28(11), 1232–1246. 10.1016/j.euroneuro.2018.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Bueso, V. , Santamaría, J. J. , Fernández, D. , Merino, L. , Montero, E. , & Ribas, J. (2018). Association between internet gaming disorder or pathological video-game use and comorbid psychopathology: A comprehensive review. International Journal of Environmental Research and Public Health , 15(4), MDPI AG. 10.3390/ijerph15040668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant, J. E. , Odlaug, B. L. , & Chamberlain, S. R. (2017). Gambling disorder, DSM-5 criteria and symptom severity. Comprehensive Psychiatry , 75, 1–5. 10.1016/j.comppsych.2017.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gul, H. , Yurumez Solmaz, E. , Gul, A. , & Oner, O. (2018). Facebook overuse and addiction among Turkish adolescents: Are ADHD and ADHD-related problems risk factors? Psychiatry and Clinical Psychopharmacology , 28(1), 80–90. 10.1080/24750573.2017.1383706. [DOI] [Google Scholar]
- Guo, W. , Tao, Y. , Li, X. , Lin, X. , Meng, Y. , Yang, X. , … Li, T. (2020). Associations of internet addiction severity with psychopathology, serious mental illness, and suicidality: Large-sample cross-sectional study. Journal of Medical Internet Research , 22(8). 10.2196/17560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heidbreder, R. (2015). ADHD symptomatology is best conceptualized as a spectrum: A dimensional versus unitary approach to diagnosis. ADHD Attention Deficit and Hyperactivity Disorders , 7(4), 249–269, Springer-Verlag Wien. 10.1007/s12402-015-0171-4. [DOI] [PubMed] [Google Scholar]
- Hinojo-Lucena, F. J. , Aznar-Díaz, I. , Cáceres-Reche, M. P. , Trujillo-Torres, J. M. , & Romero-Rodríguez, J. M. (2019). Problematic internet use as a predictor of eating disorders in students: A systematic review and meta-analysis study. Nutrients , 11(9), MDPI AG. 10.3390/nu11092151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holden, C. (2010). Behavioral addictions debut in proposed DSM-V. Science , 327(5968), 935, American Association for the Advancement of Science. 10.1126/science.327.5968.935. [DOI] [PubMed] [Google Scholar]
- Holmgren, H. G. , & Coyne, S. M. (2017). Can’t stop scrolling!: Pathological use of social networking sites in emerging adulthood. Addiction Research and Theory , 25(5), 375–382. 10.1080/16066359.2017.1294164. [DOI] [Google Scholar]
- Huang, Y. C. , Hu, S. C. , Shyu, L. Y. , & Yeh, C. B. (2020). Increased problematic smartphone use among children with attention-deficit/hyperactivity disorder in the community: The utility of Chinese version of Smartphone Addiction Proneness Scale. Journal of the Chinese Medical Association , 83(4), 411–416. 10.1097/JCMA.0000000000000278. [DOI] [PubMed] [Google Scholar]
- Hussain, Z. , & Griffiths, M. D. (2019). The associations between problematic social networking site use and sleep quality, attention-deficit hyperactivity disorder, depression, anxiety and stress. International Journal of Mental Health and Addiction . 10.1007/s11469-019-00175-1. [DOI] [Google Scholar]
- Ioannidis, K. , Chamberlain, S. R. , Treder, M. S. , Kiraly, F. , Leppink, E. W. , Redden, S. A. , … Grant, J. E. (2016). Problematic internet use (PIU): Associations with the impulsive-compulsive spectrum. An application of machine learning in psychiatry. Journal of Psychiatric Research , 83, 94–102. 10.1016/j.jpsychires.2016.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ioannidis, K. , Hook, R. W. , Grant, J. E. , Czabanowska, K. , Roman-Urrestarazu, A. , & Chamberlain, S. R. (2021). Eating disorders with over-exercise: A cross-sectional analysis of the mediational role of problematic usage of the internet in young people. Journal of Psychiatric Research , 132, 215–222. 10.1016/j.jpsychires.2020.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Izmir, S. B. I. , Ipci, M. , & Ercan, E. S. (2019). Internet use and aggression in adolescents with attention deficit hyperactivity disorder. Dusunen Adam , 32(3), 185–193. 10.14744/DAJPNS.2019.00028. [DOI] [Google Scholar]
- Joshi, S. V. , Stubbe, D. , Li, S. T. T. , & Hilty, D. M. (2019). The use of technology by youth: Implications for psychiatric educators. Academic Psychiatry , 43(1), 101–109. 10.1007/s40596-018-1007-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaess, M. , Parzer, P. , Brunner, R. , Koenig, J. , Durkee, T. , Carli, V. , … Wasserman, D. (2016). Pathological internet use is on the rise among European adolescents. Journal of Adolescent Health , 59(2), 236–239. 10.1016/j.jadohealth.2016.04.009. [DOI] [PubMed] [Google Scholar]
- Kahraman, Ö. , & Demirci, E. Ö. (2018). Internet addiction and attention-deficit–hyperactivity disorder: Effects of anxiety, depression and self-esteem. Pediatrics International , 60(6), 529–534. 10.1111/ped.13573. [DOI] [PubMed] [Google Scholar]
- Kietglaiwansiri, T. , & Chonchaiya, W. (2018). Pattern of video game use in children with attention-deficit–hyperactivity disorder and typical development. Pediatrics International , 60(6), 523–528. 10.1111/ped.13564. [DOI] [PubMed] [Google Scholar]
- Kim, K. M. , Kim, H. , Choi, J. W. , Kim, S. Y. , & Kim, J. W. (2020). What types of internet services make adolescents addicted? Correlates of problematic internet use. Neuropsychiatric disease and treatment , 16, 1031–1041. 10.2147/NDT.S247292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, D. , Lee, Y. , Lee, J. , Nam, J. K. , & Chung, Y. (2014). Development of Korean smartphone addiction proneness scale for youth. PloS One , 9(5), e97920. 10.1371/journal.pone.0097920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, S. G. , Park, J. , Kim, H. T. , Pan, Z. , Lee, Y. , & McIntyre, R. S. (2019). The relationship between smartphone addiction and symptoms of depression, anxiety, and attention-deficit/hyperactivity in South Korean adolescents. Annals of General Psychiatry , 18(1). 10.1186/s12991-019-0224-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King, D. L. , Delfabbro, P. H. , Billieux, J. , & Potenza, M. N. (2020). Problematic online gaming and the COVID-19 pandemic. Journal of Behavioral Addictions , 9(2), 184–186. 10.1556/2006.2020.00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King, D. L. , Delfabbro, P. H. , & Zajac, I. T. (2011). Preliminary validation of a new clinical tool for identifying problem video game playing. International Journal of Mental Health and Addiction , 9(1), 72–87. 10.1007/s11469-009-9254-9. [DOI] [Google Scholar]
- Ko, C. H. , Yen, J. Y. , Chen, C. S. , Yeh, Y. C. , & Yen, C. F. (2009). Predictive values of psychiatric symptoms for internet addiction in adolescents: A 2-year prospective study. Archives of Pediatrics and Adolescent Medicine , 163(10), 937–943. 10.1001/archpediatrics.2009.159. [DOI] [PubMed] [Google Scholar]
- Laconi, S. , Kaliszewska-Czeremska, K. , Gnisci, A. , Sergi, I. , Barke, A. , Jeromin, F. , … Kuss, D. J. (2018). Cross-cultural study of problematic internet use in nine European countries. Computers in Human Behavior , 84, 430–440. 10.1016/j.chb.2018.03.020. [DOI] [Google Scholar]
- Lindenberg, K. , Halasy, K. , Szász-Janocha, C. , & Wartberg, L. (2018). A phenotype classification of internet use disorder in a large-scale high-school study. International Journal of Environmental Research and Public Health , 15(4). 10.3390/ijerph15040733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lissak, G. (2018). Adverse physiological and psychological effects of screen time on children and adolescents: Literature review and case study. Environmental Research , 164, 149–157. 10.1016/j.envres.2018.01.015. [DOI] [PubMed] [Google Scholar]
- Lo, S. K. , Wang, C. C. , & Fang, W. (2005). Physical interpersonal relationships and social anxiety among online game players. Cyberpsychology and Behavior , 8(1) 15–20, Cyberpsychol Behav. 10.1089/cpb.2005.8.15. [DOI] [PubMed] [Google Scholar]
- Lu, W. H. , Chou, W. J. , Hsiao, R. C. , Hu, H. F. , & Yen, C. F. (2019). Correlations of internet addiction severity with reinforcement sensitivity and frustration intolerance in adolescents with attention-deficit/hyperactivity disorder: The moderating effect of medications. Frontiers in Psychiatry , 10(APR). 10.3389/fpsyt.2019.00268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luş, M. , & Eroğlu, M. Z. (2019). Internet addiction among adolescents with attention-deficit/hyperactivity disorder. Cukurova Medical Journal , 44(1), 140-147. 10.17826/cumj.551351. [DOI] [Google Scholar]
- Macmullin, J. A. , Lunsky, Y. , & Weiss, J. A. (2016). Plugged in: Electronics use in youth and young adults with autism spectrum disorder. Autism , 20(1), 45–54, SAGE Publications Ltd. 10.1177/1362361314566047. [DOI] [PubMed] [Google Scholar]
- Marin, M. G. , Nuñez, X. , & de Almeida, R. M. M. (2021). Internet addiction and attention in adolescents: A systematic review. Cyberpsychology, Behavior, and Social Networking , 24(4), 237–249. 10.1089/cyber.2019.0698. [DOI] [PubMed] [Google Scholar]
- Masi, L. , Abadie, P. , Herba, C. , Emond, M. , Gingras, M. P. , & Amor, L. B. (2021). Video games in ADHD and non-ADHD children: Modalities of use and association with ADHD symptoms. Frontiers in Pediatrics , 9, 632272. 10.3389/fped.2021.632272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazurek, M. O. , & Engelhardt, C. R. (2013). Video game use in boys with autism spectrum disorder, ADHD, or typical development. Pediatrics , 132(2), 260–266. 10.1542/peds.2012-3956. [DOI] [PubMed] [Google Scholar]
- Menendez-García, A. , Jiménez-Arroyo, A. , Rodrigo-Yanguas, M. , Marin-Vila, M. , Sánchez-Sánchez, F. , Roman-Riechmann, E. , & Blasco-Fontecilla, H. (2020). Internet, video game and mobile phone addiction in children and adolescents diagnosed with ADHD: A case-control study. Adicciones , 1469-1469. 10.20882/adicciones.1469. [DOI] [PubMed] [Google Scholar]
- Moola, S. , Munn, Z. , Tufanaru, C. , Aromataris, E. , Sears, K. , Sfetcu, R , … Mu, .P.-F. (2020). Chapter 7: Systematic reviews of etiology and risk. In Aromataris E., & Munn Z. (Eds.), JBI manual for evidence synthesis . JBI. Available from: https://synthesismanual.jbi.global. [Google Scholar]
- Moretta, T. , Buodo, G. , Demetrovics, Z. , & Potenza, M. N. (2022). Tracing 20 years of research on problematic use of the internet and social media: Theoretical models, assessment tools, and an agenda for future work. Comprehensive Psychiatry , 112, 152286. 10.1016/j.comppsych.2021.152286. [DOI] [PubMed] [Google Scholar]
- Niazof, D. , Weizman, A. , & Weinstein, A. (2019). The contribution of ADHD and attachment difficulties to online pornography use among students. Comprehensive Psychiatry , 93, 56–60. 10.1016/j.comppsych.2019.07.002. [DOI] [PubMed] [Google Scholar]
- Nie, J. , Zhang, W. , Chen, J. , & Li, W. (2016). Impaired inhibition and working memory in response to internet-related words among adolescents with internet addiction: A comparison with attention-deficit/hyperactivity disorder. Psychiatry Research , 236, 28–34. 10.1016/j.psychres.2016.01.004. [DOI] [PubMed] [Google Scholar]
- Nikkelen, S. W. C. , Valkenburg, P. M. , Huizinga, M. , & Bushman, B. J. (2014). Media use and ADHD-related behaviors in children and adolescents: A meta-analysis. Developmental Psychology , 50(9), 2228–2241. 10.1037/a0037318. [DOI] [PubMed] [Google Scholar]
- Ostovar, S. , Allahyar, N. , Aminpoor, H. , Moafian, F. , Nor, M. B. M. , & Griffiths, M. D. (2016). Internet addiction and its psychosocial risks (depression, anxiety, stress and loneliness) among Iranian adolescents and young adults: A structural equation model in a cross-sectional study. International Journal of Mental Health and Addiction , 14(3), 257–267. 10.1007/s11469-015-9628-0. [DOI] [Google Scholar]
- Owens, J. (2020). Social class, diagnoses of attention-deficit/hyperactivity disorder, and child well-being. Journal of Health and Social Behavior , 61(2), 134–152. 10.1177/0022146520924810. [DOI] [PubMed] [Google Scholar]
- Owens, J. (2021). Parental intervention in school, academic pressure, and childhood diagnoses of ADHD. Social Science & Medicine , 272, 113746. 10.1016/j.socscimed.2021.113746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozturk, F. O. , Ekinci, M. , Ozturk, O. , & Canan, F. (2013). The relationship of affective temperament and emotional-behavioral difficulties to internet addiction in Turkish teenagers. ISRN Psychiatry , 2013, 1–6. 10.1155/2013/961734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page, M. J. , Moher, D. , & McKenzie, J. E. (2021). Introduction to PRISMA 2020 and implications for research synthesis methodologists. Research Synthesis Methods , 13(2), 156–163. PMID: 34693644. 10.1002/jrsm.1535. [DOI] [PubMed] [Google Scholar]
- Panagiotidi, M. , & Overton, P. (2018). The relationship between internet addiction, attention deficit hyperactivity symptoms and online activities in adults. Comprehensive Psychiatry , 87, 7–11. 10.1016/j.comppsych.2018.08.004. [DOI] [PubMed] [Google Scholar]
- Panagiotidi, M. , & Overton, P. (2020). Attention deficit hyperactivity symptoms predict problematic mobile phone use. Current Psychology , 1–7. 10.1007/s12144-020-00785-2. [DOI] [Google Scholar]
- Pan, Y. C. , Chiu, Y. C. , & Lin, Y. H. (2020). Systematic review and meta-analysis of epidemiology of internet addiction. Neuroscience and Biobehavioral Reviews , 118, 612–622, Elsevier Ltd. 10.1016/j.neubiorev.2020.08.013. [DOI] [PubMed] [Google Scholar]
- Párraga, J. L. , Pérez, B. C. , López-Martín, S. , Albert, J. , MartínFernández-Mayoralas, D. , Fernández-Perrone, A. L. , … Fernández-Jaén, A. (2019). Attention-deficit/hyperactivity disorder and lifestyle habits in children and adolescents. Actas Espanolas de Psiquiatria , 47(4), 158–164. https://europepmc.org/article/med/31461155. [PubMed] [Google Scholar]
- Patsopoulos, N. A. , Evangelou, E. , & Ioannidis, J. P. A. (2008). Sensitivity of between-study heterogeneity in meta-analysis: Proposed metrics and empirical evaluation. International Journal of Epidemiology , 37(5), 1148–1157. 10.1093/ije/dyn065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulus, F. W. , Sander, C. S. , Nitze, M. , Kramatschek-Pfahler, A.-R. , Voran, A. , & Von Gontard, A. (2020). Gaming Disorder and Computer-Mediated Communication in Children and Adolescents with Autism Spectrum Disorder , 48(2), 113–122. 10.1024/1422-4917/a000674. [DOI] [PubMed] [Google Scholar]
- Polanczyk, G. V. , Salum, G. A. , Sugaya, L. S. , Caye, A. , & Rohde, L. A. (2015). Annual research review: A meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. Journal of Child Psychology and Psychiatry and Allied Disciplines , 56(3), 345–365. 10.1111/jcpp.12381. [DOI] [PubMed] [Google Scholar]
- Pornnoppadol, C. , Sornpaisarn, B. , Khamklieng, K. , & Pattanaamorn, S. (2014). The development of game addiction screening test (GAST). Journal of the Psychiatric Association of Thailand , 59(1), 3–7. [Google Scholar]
- Ra, C. K. , Cho, J. , Stone, M. D. , De La Cerda, J. , Goldenson, N. I. , Moroney, E. , … Leventhal, A. M. (2018). Association of digital media use with subsequent symptoms of attention-deficit/hyperactivity disorder among adolescents. JAMA - Journal of the American Medical Association , 320(3), 255–263. 10.1001/jama.2018.8931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Razjouyan, K. , Khademi, M. , Dorandish, Z. , & Davari-Ashtiani, R. (2020). An investigation into the frequency of addiction to video games in children with attention-deficit hyperactivity disorder. Journal of Family Medicine and Primary Care , 9(2), 669. 10.4103/jfmpc.jfmpc_464_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Restrepo, A. , Scheininger, T. , Clucas, J. , Alexander, L. , Salum, G. A. , Georgiades, K. , … Milham, M. P. (2020). Problematic internet use in children and adolescents: Associations with psychiatric disorders and impairment. BMC Psychiatry , 20(1). 10.1186/s12888-020-02640-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rey-López, J. P. , Ruiz, J. R. , Ortega, F. B. , Verloigne, M. , Vicente-Rodriguez, G. , Gracia-Marco, L. , … Gómez Lorente, J. J. (2012). Reliability and validity of a screen time-based sedentary behaviour questionnaire for adolescents: The HELENA study. European Journal of Public Health , 22(3), 373–377. 10.1093/eurpub/ckr040. [DOI] [PubMed] [Google Scholar]
- Rubia, K. (2018). Cognitive neuroscience of attention deficit hyperactivity disorder (ADHD) and its clinical translation. Frontiers in human neuroscience , 12, 100. 10.3389/fnhum.2018.00100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salum, G. A. , Sonuga-Barke, E. , Sergeant, J. , Vandekerckhove, J. , Gadelha, A. , Moriyama, T. S. , … Rohde, L. A. P. (2014). Mechanisms underpinning inattention and hyperactivity: Neurocognitive support for ADHD dimensionality. Psychological Medicine , 44(15), 3189–3201. 10.1017/S0033291714000919. [DOI] [PubMed] [Google Scholar]
- Saunders, J. B. , Hao, W. , Long, J. , King, D. L. , Mann, K. , Fauth-Bühler, M. , … Poznyak, V. (2017). Gaming disorder: Its delineation as an important condition for diagnosis, management, and prevention. Journal of Behavioral Addictions , 6(3), 271–279, Akademiai Kiado Rt. 10.1556/2006.6.2017.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayal, K. , Prasad, V. , Daley, D. , Ford, T. , & Coghill, D. (2018). ADHD in children and young people: Prevalence, care pathways, and service provision. The Lancet Psychiatry , 5(2), 175–186, Elsevier Ltd. 10.1016/S2215-0366(17)30167-0. [DOI] [PubMed] [Google Scholar]
- Shen, Y. , Wang, L. , Huang, C. , Guo, J. , De Leon, S. A. , Lu, J. P. , … Zhang, X. Y. (2021). Sex differences in prevalence, risk factors and clinical correlates of internet addiction among Chinese college students. Journal of Affective Disorders , 279, 680–686. 10.1016/j.jad.2020.10.054. [DOI] [PubMed] [Google Scholar]
- Sibley, M. H. , & Coxe, S. J. (2018). Digital media use and ADHD symptoms. JAMA - Journal of the American Medical association , 320(24), 2599, American Medical Association. 10.1001/jama.2018.18095. [DOI] [PubMed] [Google Scholar]
- So, R. , Makino, K. , Fujiwara, M. , Hirota, T. , Ohcho, K. , Ikeda, S. , … Inagaki, M. (2017). The prevalence of internet addiction among a Japanese adolescent psychiatric clinic sample with autism spectrum disorder and/or attention-deficit hyperactivity disorder: A cross-sectional study. Journal of Autism and Developmental Disorders , 47(7), 2217–2224. 10.1007/s10803-017-3148-7. [DOI] [PubMed] [Google Scholar]
- So, R. , Makino, K. , Hirota, T. , Fujiwara, M. , Ocho, K. , Ikeda, S. , … Inagakip, M. (2019). The 2-year course of internet addiction among a Japanese adolescent psychiatric clinic sample with autism spectrum disorder and/or attention-deficit hyperactivity disorder. Journal of Autism and Developmental Disorders , 49(11), 4515–4522. 10.1007/s10803-019-04169-9. [DOI] [PubMed] [Google Scholar]
- Spada, M. M. (2014). An overview of problematic Internet use. Addictive Behaviors , 39(1), 3–6 Addict Behav 10.1016/j.addbeh.2013.09.007. [DOI] [PubMed] [Google Scholar]
- Sterne, J. A. , Sutton, A. J. , Ioannidis, J. P. , Terrin, N. , Jones, D. R. , Lau, J. , … Higgins, J. P. (2011). Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ (Clinical Research ed.) , 343, d4002. 10.1136/bmj.d4002. [DOI] [PubMed] [Google Scholar]
- Stevens, M. W. R. , Dorstyn, D. , Delfabbro, P. H. , & King, D. L. (2020). Global prevalence of gaming disorder: A systematic review and meta-analysis. Australian and New Zealand Journal of Psychiatry . SAGE Publications Inc. 10.1177/0004867420962851. [DOI] [PubMed] [Google Scholar]
- Tao, R. , Huang, X. , Wang, J. , Zhang, H. , Zhang, Y. , & Li, M. (2010). Proposed diagnostic criteria for internet addiction. Addiction , 105(3), 556–564. 10.1111/j.1360-0443.2009.02828.x. [DOI] [PubMed] [Google Scholar]
- Thoma, V. K. , Schulz-Zhecheva, Y. , Oser, C. , Fleischhaker, C. , Biscaldi, M. , & Klein, C. (2020). Media use, sleep quality, and ADHD symptoms in a community sample and a sample of ADHD patients aged 8 to 18 years. Journal of Attention Disorders , 24(4), 576–589. 10.1177/1087054718802014. [DOI] [PubMed] [Google Scholar]
- Van Den Eijnden, R. , Koning, I. , Doornwaard, S. , Van Gurp, F. , & Bogt, T. T. (2018). The impact of heavy and disordered use of games and social media on adolescents’ psychological, social, and school functioning. Journal of Behavioral Addictions , 7(3), 697–706. 10.1556/2006.7.2018.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volpe, U. , Dell’osso, B. , Fiorillo, A. , Mucic, D. , & Aboujaoude, E. (2015). Internet-related psychopathology: Clinical phenotypes and perspectives in an evolving field. Psychopathology of Addictions Journal of Psychopathology , 21. [Google Scholar]
- Wang, C. Y. , Wu, Y. C. , Su, C. H. , Lin, P. C. , Ko, C. H. , & Yen, J. Y. (2017). Association between Internet gaming disorder and generalized anxiety disorder. Journal of Behavioral Addictions , 6(4), 564–571. 10.1556/2006.6.2017.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, B. qian , Yao, N. qi , Zhou, X. , Liu, J. , & Lv, Z. tao (2017). The association between attention deficit/hyperactivity disorder and internet addiction: A systematic review and meta-analysis. BMC Psychiatry , 17(1). 10.1186/s12888-017-1408-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wan, X. , Wang, W. , Liu, J. , & Tong, T. (2014). Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Medical Research Methodology , 14(1). 10.1186/1471-2288-14-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wegmann, E. , Ostendorf, S. , & Brand, M. (2018). Is it beneficial to use internet-communication for escaping from boredom? Boredom proneness interacts with cue-induced craving and avoidance expectancies in explaining symptoms of internet-communication disorder. PloS One , 13(4). 10.1371/journal.pone.0195742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstein, A. , & Lejoyeux, M. (2020). Neurobiological mechanisms underlying internet gaming disorder. Dialogues in Clinical Neuroscience , 22(2), 113–126, Les Laboratoires Seriver. 10.31887/DCNS.2020.22.2/aweinstein. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstein, A. , Yaacov, Y. , Manning, M. , Danon, P. , & Weizman, A. (2015). Internet addiction and attention deficit hyperactivity disorder among schoolchildren. Israel Medical Association Journal , 17(12), 731–734. https://europepmc.org/article/med/26897972. [PubMed] [Google Scholar]
- Werling, A. M. , Walitza, S. , & Drechsler, R. (2021a). Impact of the COVID-19 lockdown on screen media use in patients referred for ADHD to child and adolescent psychiatry: An introduction to problematic use of the internet in ADHD and results of a survey. Journal of Neural Transmission , 128(7), 1033–1043. 10.1007/s00702-021-02332-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werling, A. M. , Walitza, S. , Grünblatt, E. , & Drechsler, R. (2021b). Media use before, during and after COVID-19 lockdown according to parents in a clinically referred sample in child and adolescent psychiatry: Results of an online survey in Switzerland. Comprehensive Psychiatry , 109, 152260. 10.1016/j.comppsych.2021.152260. [DOI] [PubMed] [Google Scholar]
- Woods, H. C. , & Scott, H. (2016). #Sleepyteens: Social media use in adolescence is associated with poor sleep quality, anxiety, depression and low self-esteem. Journal of Adolescence , 51, 41–49. 10.1016/j.adolescence.2016.05.008. [DOI] [PubMed] [Google Scholar]
- World Health Organization (2020). ICD-11 for mortality and morbidity statistics. 2020. https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/411470068.
- Younes, F. , Halawi, G. , Jabbour, H. , Osta, N. E. , Karam, L. , Hajj, A. , & Khabbaz, L. R. (2016). Internet addiction and relationships with insomnia, anxiety, depression, stress and self-esteem in university students: A cross-sectional designed study. PloS One , 11(9). 10.1371/journal.pone.0161126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young, K. S. (1996). Psychology of computer use: XL. Addictive use of the internet - a case that breaks the stereotype. Psychological Reports , 79(3 PART 1), 899–902. 10.2466/pr0.1996.79.3.899. [DOI] [PubMed] [Google Scholar]
- Young, K. S. (1998). Internet addiction: The emergence of a new clinical disorder. Cyberpsychology and Behavior , 1(3), 237–244. 10.1089/cpb.1998.1.237. [DOI] [Google Scholar]
- Young, K. S. , & Brand, M. (2017). Merging theoretical models and therapy approaches in the context of internet gaming disorder: A personal perspective. Frontiers in Psychology , 8(OCT), 1853, Frontiers Media S.A. 10.3389/fpsyg.2017.01853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, Y. , Mei, S. , Li, L. , Chai, J. , Li, J. , Du, H. , & Weinstein, A. M. (2015). The relationship between impulsivity and internet addiction in Chinese college students: A moderated mediation analysis of meaning in life and self-esteem. PloS One , 10(7). 10.1371/journal.pone.0131597. [DOI] [PMC free article] [PubMed] [Google Scholar]