Abstract
Individuals' psychological distress is associated with disinhibited eating (external and emotional eating). The aim of the current study was to examine the moderating associations of COVID-19-related stress on parents' psychological distress (anxiety, hostility, depression) and external and emotional eating. One hundred and sixty U.S. parents of three- to five-year-old children (Mage = 34.08, SD = 6.76; 89 females) completed an online survey. After accounting for participant characteristics (i.e., age, BMI, sex), regression analyses showed that COVID-19 stress moderated the effects of anxiety, hostility, and depression on external eating. Additionally, findings showed that COVID-19 stress moderated hostility (but not anxiety or depression) on emotional eating. These findings suggest that unexpected stressors from the COVID-19 pandemic may exacerbate disinhibited eating among those individuals who experience psychological distress. This presents support for providing interventions that focus on healthy coping strategies and family well-being, support groups, and community resources (e.g., financial assistance) to alleviate external pressures during unprecedented times.
Keywords: External eating, Emotional eating, COVID-19, Stress, Anxiety, Hostility, Depression
“Some parents have had job and income losses, creating financial instability—and exacerbating parental stress.” -The Wall Street Journal (Peterson, 2021).
In early March 2020, the coronavirus disease 2019 (COVID-19) prompted schools and other businesses (including childcare programs) to close across the country due to enforced public health mandates and stay-at-home (SAH) orders (CDC, 2020a; CDC, 2020b; Review, 2020). The drastic negative outcomes for families of young children were numerous, including changes to family dynamics, childcare, work status, and financial security (e.g., Campbell, 2020; Heggeness & Fields, 2020; Moorman, 2021; Udalova, 2021). This elucidates that families experienced multi-faceted (family dynamics, childcare, work status, financial security) stress unique to the COVID-19 pandemic (henceforth referred to as COVID-19 stress), which may be associated with parents' psychological distress and disinhibited eating.
Disinhibited eating—a proclivity to lose control of one's eating either in response to emotional arousal or external circumstances—is an important consideration for health (Provencher et al., 2003; Young et al., 2017). Previous literature supports that psychological distress (anxiety, hostility, depression) is positively associated with disinhibited eating (Konttinen, 2020; Lattimore & Maxwell, 2004; Uğurlu et al., 2021). First, anxiety was found to be a strong predictor of disinhibited eating (Hussenoeder et al., 2021) and may be associated with the unique experiences of the COVID-19 pandemic. For instance, in a Mediterranean sample, Spanish participants who underwent stricter lockdown measures during the COVID-19 pandemic and who experienced greater anxiety also reported lower external eating (but not emotional eating; Papandreou et al., 2020). It is unknown why this is the case. It is likely that participants who underwent stricter public health policies may have experienced less COVID-19-related stress, as these individuals may have perceived that the stricter policies would provide a greater protection from getting the virus (akin to vehicle sanctions on the road leading to more safety behaviors [e.g., wearing seatbelts] and fewer accidents; Nordfjærn et al., 2011). In other words, COVID-19 stress may influence the effect of anxiety on disinhibited eating. Second, hostility (i.e., irritability, uncontrollable temper; Adawi et al., 2019) has been shown to predict disinhibited eating. Prior research indicates this relationship is strongest for participants with obesity and who experience weight fluctuations and dietary helplessness (Carmody et al., 1999). However, the literature regarding hostility and disinhibited eating behaviors is limited, especially among parent-specific samples. Lastly, higher levels of depression are associated with greater disinhibited eating (Konttinen et al., 2010; Marjaana Lindeman, 2001). Importantly, much of the research on depression and eating behaviors has focused on the association with eating disorders (binge eating) or obesity (Lazarevich et al., 2016; Mason & Lewis, 2014; Pinaquy et al., 2003) and lesser on disinhibited eating. Regardless, the tendency to overeat or lose control of one's eating in the presence of psychological distress is evident.
Additionally, research has linked psychological distress and general stress with eating behaviors (Groesz et al., 2012; Pellegrini et al., 2021; Şahan et al., 2021). Individuals who experience higher perceived stress are more likely to consume foods high in fat, experience a greater drive to eat, and report greater likelihood for eating under emotional distress and environmental cues (for review see Barrington et al., 2014; Joseph et al., 2018; O’Neill et al., 2020; Shen et al., 2020). Perceived stress and strong emotional states have also been shown to be related to increased emotional eating during the pandemic (Cecchetto et al., 2021; Shen et al., 2020), including among caregivers (Jordan et al., 2021). For instance, prior research has found that people changed their food habits during the SAH orders when confined to their homes (Haddad et al., 2020). Other studies have examined eating disorders (i.e., restricted eating, binge eating, purging) and stress levels during the COVID-19 pandemic (Phillipou et al., 2020; Rodgers et al., 2020) or examined psychological distress as a mediator (Ramalho et al., 2021). However, no studies to our knowledge have directly examined the influence of psychological distress on disinhibited eating (i.e., overeating in response to negative emotional states) as moderated by COVID-19 stress of parents of three- to five-year old children.
Two theories could explain the process of engaging in disinhibited eating under the presence of psychological distress and perceived stress. According to the Psychosomatic Theory, individuals prone to be emotional eaters (eating in response to external cues) respond to elevated stress or negative emotional arousal by engaging in excessive food consumption (Kaplan & Kaplan, 1957; Snoek et al., 2007). Second, Schachter's Externality Theory of Obesity posits that external eating is due to higher sensitivity to external cues, such as sight or smell of food, rather than internal cues such as hunger and satiety (Schachter, 1968, Schachter, 1974; Snoek et al., 2007). However, it is unknown whether the stress from an unknown/unfamiliar infectious disease (as opposed to common/familiar stressors of everyday life) will mitigate or exacerbate the relationship between psychological distress and disinhibited eating among parents of young children. Therefore, based on prior research and theoretical support, we predicted parents high in psychological distress (anxiety, hostility, depression) would demonstrate higher disinhibited eating (external eating, emotional eating) and this relationship may be exacerbated by the degree of COVID-19-related stress that participants experience.
1. Methods
1.1. Participants and procedures
Participants (N = 175) were recruited from Prolific from April 24 through 27, 2020 (Prolific was found to have higher data quality as compared to other crowdsourcing platforms; Prolific, 2020; Palan & Schitter, 2018). Fifteen participants were excluded from the study for either completing the survey twice (i.e., duplicate IP address) or failed attention check questions (“How many words are in this sentence?”; “How many response options are in this question?”; and an open-ended inquiry regarding the purpose of the study; Oppenheimer et al., 2009). The remaining data (N = 160; 89 females) were used for analyses. The mean age of participants was 34.5 years old (SD = 6.8), identified as 81.3% white, 5.6% Black/African-American, 6.3% Asian, 0.6% Native Hawaiian/Pacific Islander, 3.8% bi- or multi-racial, and 2.5% as “other” or refused to answer, 83.3% non-Hispanic (16.7% Hispanic), lived primarily in California, U.S. (18.8%), and had at least a 4-year college degree (35%). Participants' self-reported height and weight were used to calculate Body Mass Index (BMI; M BMI = 27.1 kg/m2, SD = 6.8). A post hoc power analysis using G*Power (Faul et al., 2007) suggested that with N = 160, we have power = 0.97 to detect effect sizes ≥ 0.05 in multiple linear regression using six predictor variables.
The data collected were part of a larger study examining parenting and stress. Inclusion criteria consisted of the following: Participants must (a) be a parent of a child between the ages of three- and five-years old, (b) currently cohabiting or married with a partner, and (c) reside in the U.S. Additionally, the index child must not have had (d) any developmental delays or (e) any reported major medical problems/allergic reactions following ingestion of food. Eligible participants completed a 30-minute survey and were compensated with $5.00 USD (U.S. minimum hourly wage $7.25/h, Review, 2020). Participants self-recruited and completed the measures in the order described below. This study was approved by the university's Institutional Review Board.
1.2. Measures
1.2.1. Psychological distress
To measure psychological distress, we used the Brief Symptoms Inventory (BSI; Derogatis & Melisaratos, 1983). Participants rated their extent of feelings during the past 30-days using a 5-point scale (0 = not at all, 4 = extremely). The items correspond to three subscales: 1) Anxiety (six items; e.g., “Nervousness or shakiness inside”; α = 0.89), 2) Hostility (five items; e.g., “Temper outbursts that you could not control”; α = 0.83), and 3) Depression (five items; e.g., “Feeling hopeless about the future”; α = 0.92). Higher scores indicate more distress for the given symptom.
1.2.2. Disinhibited eating
To assess disinhibited eating, participants completed the Dutch Eating Behavior Questionnaire (DEBQ; van Strien et al., 1986). Participants rated two subscales: 1) emotional eating (13 items; e.g., “Do you have the desire to eat when you are irritated?”; α = 0.94), and 2) external eating (10 items; e.g., “If food tastes good to you, do you eat more than usual?”; α = 0.76) using a 5-point scale (1 = never, 5 = very often). Higher scores represent engaging more often with the given eating behavior.
1.2.3. COVID-19 stress
To measure the effect of the COVID-19 pandemic on families, a multi-faceted COVID-19 stress measure was created ad hoc and used for the purposes of this research. Participants rated the extent of agreement to four items using a 5-point Likert scale (1 = strongly disagree, 5 = strongly agree). Participants were asked to what extent the pandemic affected their family dynamic (“My family dynamic is affected by the pandemic of coronavirus”), financial situation (“My financial situation is affected by the pandemic of coronavirus”), childcare (“My childcare arrangement is affected by the pandemic of coronavirus”), and work (“My work is affected by the pandemic of coronavirus”). Items were assessed for reliability and validity1 and an overall COVID-19 Stress composite was created (α = 0.68). Higher scores reflect greater stress from the COVID-19 pandemic.
2. Results
Using SPSS 26, key study variables were checked for normality and missing data. Skewness and kurtosis for all key study variables fell within acceptable levels, [−2, +2] and [−7, +7], respectively. < 5 % of data was missing, so it was chosen to leave these cases as missing. Correlational analyses were conducted to examine whether participants' characteristics (age, BMI) were associated with key study variables (anxiety, hostility, depression, COVID-19 stress, external eating, and emotional eating; see Table 1 ). Independent sample t-tests were conducted and found that there were no parent sex differences on key study variables, all ps ≥ 0.236.
Table 1.
Correlations among key study variables (N = 160).
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. | Age | – | |||||||
| 2. | BMI (kg/m2) | −0.06 | – | ||||||
| 3. | BSI anxiety | −0.10 | 0.06 | – | |||||
| 4. | BSI hostility | −0.04 | 0.08 | 0.68⁎⁎⁎ | – | ||||
| 5. | BSI depression | −0.13 | 0.15 | 0.78⁎⁎⁎ | 0.73⁎⁎⁎ | – | |||
| 6. | Emotional eating | −0.01 | 0.35⁎⁎⁎ | 0.56⁎⁎⁎ | 0.44⁎⁎⁎ | 0.49⁎⁎⁎ | – | ||
| 7. | External eating | 0.04 | 0.16⁎ | 0.42⁎⁎⁎ | 0.27⁎⁎⁎ | 0.32⁎⁎⁎ | 0.63⁎⁎⁎ | – | |
| 8. | COVID-19 stress | 0.03 | −0.03 | 0.25⁎⁎ | 0.07 | 0.25⁎⁎ | 0.05 | 0.01 | – |
p < .05.
p < .01.
p < .001.
2.1. Associations among psychological distress, COVID-19 stress, and disinhibited eating
Six regression analyses controlling for participant characteristics were conducted to examine whether psychological distress (anxiety, hostility, depression) interacted with COVID-19 stress to predict disinhibited eating behaviors (external and emotional eating; see Table 2 ). All linear regressions met the assumptions of linear regression analyses. The predictor (anxiety, hostility, depression) and moderator variables (COVID-19 stress) were centered by subtracting the variable means. Interaction terms were created by multiplying the centered predictor variable by the centered moderator variable. InterActive (McCabe et al., 2018) was used to probe any significant interactions (moderator variable plotted at values of −2 SD, −1 SD, mean, +1 SD, +2 SD).
Table 2.
Regression analyses of the moderating effect of COVID-19 stress on psychological distress and disinhibited eating (N = 160).
| External eating |
Emotional eating |
|
|---|---|---|
| B (SE) | B (SE) | |
| R2 = 0.23, F (6, 147) = 7.50, p < .001 | R2 = 0.43, F (6, 147) = 18.41, p < .001 | |
| Constant | 3.28 (0.05) | 2.61 (0.07) |
| Age | 0.01 (0.01) | 0.01 (0.01) |
| Sex | 0.07 (0.09) | −0.03 (0.14) |
| BMI (kg/m2) | 0.01 (0.01) | 0.05 (0.01)⁎⁎⁎ |
| Anxiety | 0.28 (0.05)⁎⁎⁎ | 0.66 (0.08)⁎⁎⁎ |
| COVID-19 Stress | −0.09 (0.05) | −0.12 (0.08) |
| Anxiety × COVID-19 stress | 0.10 (0.05)⁎ | 0.05 (0.07) |
| R2 = 0.13, F (6, 147) = 3.68, p = .002 | R2 = 0.33, F (6, 147) = 12.31, p < .001 | |
| Constant | 3.29 (0.05) | 2.61 (0.07) |
| Age | 0.01 (0.01) | 0.01 (0.01) |
| Sex | 0.05 (0.10) | −0.06 (0.15) |
| BMI (kg/m2) | 0.01 (0.01) | 0.05 (0.01)⁎⁎⁎ |
| Hostility | 0.19 (0.06)⁎⁎ | 0.55 (0.09)⁎⁎⁎ |
| COVID-19 stress | −0.03 (0.05) | 0.003 (0.08) |
| Hostility × COVID-19 stress | 0.14 (0.05)⁎⁎ | 0.24 (0.08)⁎⁎ |
| R2 = 0.16, F (6, 147) = 4.51, p < .001 | R2 = 0.34, F (6, 147) = 12.51, p < .001 | |
| Constant | 3.28 (0.05) | 2.60 (0.08) |
| Age | 0.01 (0.01) | 0.01 (0.01) |
| Sex | 0.06 (0.10) | −0.04 (0.15) |
| BMI (kg/m2) | 0.01 (0.01) | 0.05 (0.01)⁎⁎⁎ |
| Depression | 0.15 (0.04)⁎⁎⁎ | 0.42 (0.07)⁎⁎⁎ |
| COVID-19 stress | −0.07 (0.05) | −0.09 (0.08) |
| Depression × COVID-19 stress | 0.10 (0.04)⁎⁎ | 0.12 (0.07) |
p < .05.
p < .01.
p < .001.
2.1.1. Anxiety
2.1.1.1. External eating
Findings showed that the interaction of anxiety and COVID-19 stress on external eating, B = 0.10, t(147) = 2.12, p = .035, was significant (see Fig. 1 ). At COVID-19 stress plotted 1 SD below the mean (B = 0.19, 95% CI = [0.05, 0.33], p = .007), at the mean (B = 0.28, 95% CI = [0.18, 0.38], p < .001), 1 SD above the mean (B = 0.37, 95% CI = [0.25, 0.49], p < .001), and 2 SD above the mean (B = 0.46, 95% CI = [0.28, 0.65], p < .001), anxiety had a significant positive influence on external eating. At COVID-19 stress plotted at 2 SD below the mean, anxiety did not significantly influence external eating (B = 0.10, 95% CI = [−0.11, 0.30], p = .342).
Fig. 1.
Two-way linear interaction effects for anxiety, COVID-19 stress, and external eating (N = 160).
2.1.1.2. Emotional eating
Findings showed that the interaction of anxiety and COVID-19 stress on emotional eating was not significant, B = 0.05, t(147) = 0.71, p = .481.
2.1.2. Hostility
2.1.2.1. External eating
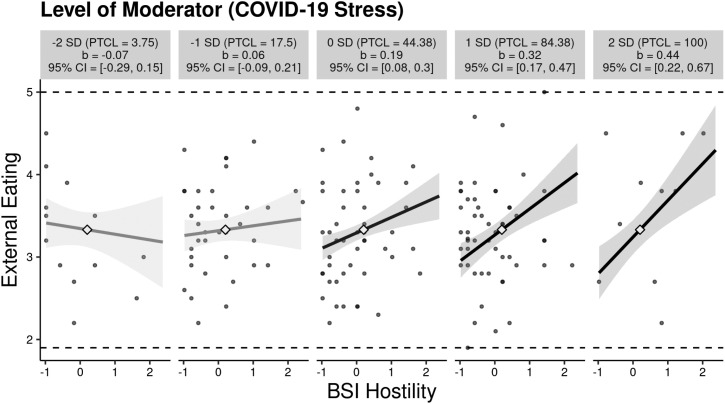
Findings showed that the interaction of hostility and COVID-19 stress on external eating, B = 0.14, t(147) = 2.65, p = .009, was significant (see Fig. 2 ). At COVID-19 stress plotted at the mean (B = 0.19, 95% CI = [0.08, 0.30], p = .001), 1 SD above the mean (B = 0.32, 95% CI = [0.17, 0.47], p < .001), and 2 SD above the mean (B = 0.44, 95% CI = [0.22, 0.67], p < .001), hostility had a significant positive influence on external eating. At COVID-19 stress plotted 2 SD below the mean (B = −0.07, 95% CI = [−0.29, 0.15], p = .537) and 1 SD below the mean (B = 0.06, 95% CI = [−0.09, 0.21], p = .423), hostility did not significantly influence external eating.
Fig. 2.
Two-way linear interaction effects for hostility, COVID-19 stress, and external eating (N = 160).
2.1.2.2. Emotional eating
Findings showed that the interaction of hostility and COVID-19 stress on emotional eating, B = 0.24, t(147) = 2.84, p = .005, was significant (see Fig. 3 ). At COVID-19 stress plotted 1 SD below the mean (B = 0.33, 95% CI = [0.10, 0.56], p = .005), at the mean (B = 0.54, 95% CI = [0.37, 0.72], p < .001), 1 SD above the mean (B = 0.76, 95% CI = [0.53, 0.99], p < .001), and 2 SD above the mean (B = 0.97, 95% CI = [0.62, 1.32], p < .001), hostility had a significant positive influence on emotional eating. At COVID-19 stress plotted at 2 SD below the mean (B = 0.12, 95% CI = [−0.23, 0.46], p = .508), hostility did not significantly influence emotional eating.
Fig. 3.
Two-way linear interaction effects for hostility, COVID-19 stress, and emotional eating (N = 160).
2.1.3. Depression
2.1.3.1. External eating
Findings showed that the interaction of depression and COVID-19 stress on external eating, B = 0.10, t(147) = 2.41, p = .017, was significant (see Fig. 4 ). At COVID-19 stress plotted at the mean (B = 0.15, 95% CI = [0.07, 0.24], p = .001), 1 SD above the mean (B = 0.25, 95% CI = [0.14, 0.35], p < .001), and 2 SD above the mean (B = 0.34, 95% CI = [0.18, 0.51], p < .001), depression had a significant positive influence on external eating. At COVID-19 stress plotted at 2 SD below the mean (B = −0.04, 95% CI = [−0.23, 0.16], p = .716) and 1 SD below the mean (B = 0.06, 95% CI = [−0.07, 0.19], p = .362), depression did not significantly influence external eating.
Fig. 4.
Two-way linear interaction effects for depression, COVID-19 stress, and external eating (N = 160).
2.1.3.2. Emotional eating
Findings showed that the interaction of depression and COVID-19 stress on emotional eating was not significant, B = 0.12, t(147) = 1.82, p = .071.
3. Discussion
The present study examined the associations among psychological distress (anxiety, hostility, depression), COVID-19 stress, and disinhibited eating (external, emotional eating) of parents of three- to five-year old children. Findings showed that COVID-19 stress moderated the associations between 1) anxiety and external eating, 2) hostility and external eating, and 3) depression and external eating. Additionally, it was found that COVID-19 stress moderated the associations between hostility (but not anxiety and depression) and emotional eating.
First, COVID-19 stress moderated the associations between psychological distress (anxiety, hostility, depression) and external eating. Specifically, it was found that individuals with anxiety (hostility, depression) who experienced greater COVID-19 stress reported more external eating than counterparts who experienced lower COVID-19 stress. Findings support Schachter's Externality Theory of Obesity (Schachter, 1968, Schachter, 1974; Snoek et al., 2007) and that of prior work. For example, adults living in the United Kingdom with uncontrolled eating before the pandemic and who experienced higher health anxiety during the pandemic reported an increased intake of high energy density snack foods (Coulthard et al., 2021). Importantly, our findings extended prior work by Papandreou et al. (2020) who found that greater psychological distress (i.e., anxiety) was associated with lower external eating in locations with stricter public health policies during COVID-19. Stricter health policies could lessen the stress experienced by citizens overall. Indeed, we found that among individuals with high psychological distress, lower (vs. higher) levels of COVID-19 stress was associated with lower external eating. However, there was still a significant positive association among high anxiety and external eating under lower levels of COVID-19 stress, suggesting individuals with high anxiety (vs. hostility, depression) may be more prone to external eating while experiencing stressors of the COVID-19 pandemic.
Second, COVID-19 stress moderated the association between hostility (but not anxiety and depression) and emotional eating. The lack of moderating associations between anxiety/depression and emotional eating could be that among individuals who tend to emotionally overeat, COVID-19 stress did not impose a significant amount of additional stress. Indeed, findings from prior work found that among adults who tended to emotionally overeat before the pandemic, COVID-19 health anxiety did not predict increased emotional overeating (Coulthard et al., 2021). In addition, previous studies also found that emotional overeating did not differ between individuals from two Mediterranean countries who experienced differential lockdown measures and pandemic severity (Papandreou et al., 2020). However, it was found that high COVID-19 stress predicted higher emotional eating in individuals that reported high hostility. One possibility, and consistent with the Psychosomatic Theory (Kaplan & Kaplan, 1957; Snoek et al., 2007), is that individuals with hostility are more likely to use escape-avoidance coping, which may include eating to regulate negative affect (Vandervoort, 2006).
3.1. Limitations and future directions
Although this study is novel in understanding how psychological distress and COVID-19 stress relate to disinhibited eating, there are some limitations. First, results of this study may have limited generalizability. Respondents were mostly white and upper-class participants. Racial/ethnic minorities and families with lower socioeconomic status may experience the negative effects of the COVID-19 pandemic differently than white or upper-class participants due to higher food insecurity and stress rates (Breslau et al., 2021; Kandiah et al., 2021; Lauren et al., 2021; Lund, 2021). It is possible that the adverse effects of COVID-19 would exacerbate the relationships between psychological distress and disinhibited eating among minority groups and those with low income such that those at risk for food insecurity may decrease their disinhibited eating. Additionally, participants were parents of three- to five-year old children. Parents of children in the home during SAH orders (particularly those with young children) encountered increased stress levels (Kowal et al., 2020) and other obstacles (e.g., childcare, remote learning) sui generis of other household structures.
Second, this study used a cross-sectional design and collected data during the beginning of the COVID-19 pandemic. We did not measure perceived psychological distress or general stress prior to the pandemic or assess transference from one type of stressor to another (especially considering time of data collection). It is possible that, for some participants, psychological distress was linear from pre-pandemic to time of data collection or that eating behaviors differed for individuals with lower (vs. higher) psychological distress before the COVID-19 pandemic (Breslau et al., 2021). Future studies would benefit from considering pre-pandemic circumstances within their measures. Relatedly, the COVID-19 Stress measure could be evaluating differing COVID-19 psychosocial factors rather than stress levels caused by the pandemic. Even though the measure was assessed for psychometric integrity1, it would have been beneficial to evaluate participants on the psychosocial impact of COVID-19 rather than on COVID-19 stress level, specifically.
Third, results are indicative of perceived behaviors and not on actual behavior (e.g., documentation or physiological measurements in real time). Prior research on self-perception indicates people generally are not as accurate about interpersonal perception and behavioral indices (for review see Dunning, 2005; Epley & Dunning, 2006; Vazire & Mehl, 2008; Wilson & Dunn, 2004). Future research should consider taking a more direct approach (e.g., ecological momentary assessment). Lastly, the order of self-report measures was not counterbalanced. Counterbalancing has shown to strengthen internal consistency and validity in numerous domains and research designs (e.g., Luce et al., 2007; Young et al., 2003). Future research should consider counterbalancing self-report measures.
3.2. Implications and conclusions
Our research has theoretical and applied implications. First, our findings are relevant to theoretical perspectives on eating due to external cues and elevated stress or emotional arousal (e.g., Psychosomatic Theory, Schachter's Externality Theory of Obesity; Kaplan & Kaplan, 1957; Schachter, 1968; Snoek et al., 2007). Second, this research contributes to our understanding of how the pandemic has affected parents and families (particularly those with young children) and may be key to reducing psychological distress and disinhibited eating. Gaining an in-depth understanding of how external cues and emotional factors affect dietary-relevant behaviors has become increasingly important as dietary health concerns for families continues to rise, particularly during the COVID-19 pandemic (Aksoy et al., 2021; Dunn et al., 2020). Third, our findings that COVID-19 stress moderated factors of psychological distress and disinhibited eating can aid in the creation of interventions, dietary health-relevant advertisements, and communications related to dietary health and stress reduction. For instance, practitioners and mental health professionals can provide interventions that focus on healthy coping strategies and family well-being, support groups, and community resources (e.g., financial assistance) to alleviate external pressures during unprecedented times. As families settle into a “new normal” with new, emerging SARS-CoV-2 variants (CDC, 2020a) and businesses and schools resume to full capacity, parents continue to face multi-faceted COVID-19 stress (changes to family dynamics, childcare, work status, and financial security) including increased psychological distress and disinhibited eating (Canady, 2020; Freisthler et al., 2021).
CRediT authorship contribution statement
Noelle K. Herzog: Methodology, Validation, Formal analysis, Investigation, Resources, Data curation, Writing – original draft, Writing – review & editing, Visualization, Project administration. Adelyn Sherrard: Validation, Formal analysis, Resources, Data curation, Writing – original draft, Writing – review & editing, Visualization. Tyler C. Kemmerley: Investigation, Writing – original draft. Cin Cin Tan: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Resources, Data curation, Writing – original draft, Writing – review & editing, Visualization, Supervision, Project administration, Funding acquisition.
Declaration of competing interest
The authors declare no conflicts of interest in preparing this article.
Acknowledgments
All phases of this study were supported by the Dean's Office of the College of Arts and Letters at the University of Toledo as part of the author, Cin Cin Tan, Ph.D.'s research start-up package.
Footnotes
Due to the slightly low Cronbach's alpha (DeVellis, 2012) and to explore the factorial structure, all four items of the COVID-19 Stress instrument (rs > 0.19, ps ≤ 0.018) were subjected to a principal components analysis with oblique rotation (direct oblimin). Component 1 explained 51.28% of the variance with factor loadings from 0.658 to 0.766. The Kaiser-Meyer-Olkin (KMO = 0.63) measure with a significant Bartlett's test of sphericity, χ2 (6) = 116.12, p < .001, indicated that it was appropriate to use the factor analytic model on this set of data (Abdi & Williams, 2010; Field, 2009). Additionally, even though the Cronbach's alpha of 0.68 can be considered marginally low in some instances with a cut off value of ≥ 0.70 (DeVellis, 2012), a growing amount of literature proposes that strictly adhering to the arbitrary threshold of 0.70 may allow for flawed reporting (Berger & Hänze, 2015) and offer limited evidence of reliability (Gardner, 1995; Taber, 2018) in some instances. To assess validity of the COVID-19 Stress instrument, we reviewed scale items for criterion validity. Since this data was a part of a larger study, participants had also completed the Perceived Stress Scale (PSS-4; Cohen et al., 1983). Sample item included, “In the last 2 weeks, how often have you felt difficulties were piling up so high that you could not overcome them?”. To have good criterion validity, we expected test items from the PSS-4 and the COVID-19 Stress scale to be correlated. Test items were significantly correlated (r = 0.35, p < .001). Therefore, by providing additional factor analysis as complimentary evidence, the authors are confident that the scale in question adequately provides reliable support for a COVID-19 stress dimension.
References
- Abdi H., Williams L.J. Principal component analysis. WIREs. Computational Statistics. 2010;2(4):433–459. doi: 10.1002/wics.101. [DOI] [Google Scholar]
- Adawi M., Zerbetto R., Re T.S., Bisharat B., Mahamid M., Amital H., Del Puente G., Bragazzi N.L. Psychometric properties of the brief symptom inventory in nomophobic subjects: Insights from preliminary confirmatory factor, exploratory factor, and clustering analyses in a sample of healthy Italian volunteers. Psychology Research and Behavior Management. 2019;12:145–154. doi: 10.2147/PRBM.S173282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aksoy N.C., Kabadayi E.T., Alan A.K. An unintended consequence of Covid-19: Healthy nutrition. Appetite. 2021;166 doi: 10.1016/j.appet.2021.105430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrington W.E., Beresford S.A.A., McGregor B.A., White E. Perceived stress and eating behaviors by sex, obesity status, and stress vulnerability: Findings from the vitamins and lifestyle (VITAL) study. Journal of the Academy of Nutrition and Dietetics. 2014;114(11):1791–1799. doi: 10.1016/j.jand.2014.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berger R., Hänze M. Impact of expert teaching quality on novice academic performance in the jigsaw cooperative learning method. International Journal of Science Education. 2015;37(2):294–320. [Google Scholar]
- Breslau J., Finucane M.L., Locker A.R., Baird M.D., Roth E.A., Collins R.L. A longitudinal study of psychological distress in the United States before and during the COVID-19 pandemic. Preventive Medicine. 2021;143 doi: 10.1016/j.ypmed.2020.106362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell A.M. An increasing risk of family violence during the Covid-19 pandemic: Strengthening community collaborations to save lives. Forensic Science International: Reports. 2020;2 doi: 10.1016/j.fsir.2020.100089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canady V.A. APA stress report amid COVID-19 points to parental challenges. Mental Health Weekly. 2020;30(22):3–4. doi: 10.1002/mhw.32385. [DOI] [Google Scholar]
- Carmody T.P., Brunner R.L., Jeor S.T.S. Hostility, dieting, and nutrition attitudes in overweight and weight-cycling men and women. International Journal of Eating Disorders. 1999;26(1):37–42. doi: 10.1002/(SICI)1098-108X(199907)26:1<37::AID-EAT5>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- CDC . Centers for Disease Control and Prevention; 2020. Coronavirus disease 2019 (COVID-19)https://www.cdc.gov/coronavirus/2019-ncov/science/about-epidemiology/identifying-source-outbreak.html February 11. [Google Scholar]
- CDC . Centers for Disease Control and Prevention; 2020. Covid-19 archived webpage.https://www.cdc.gov/coronavirus/2019-nCoV/index.html February 11. [Google Scholar]
- Cecchetto C., Aiello M., Gentili C., Ionta S., Osimo S.A. Increased emotional eating during COVID-19 associated with lockdown, psychological and social distress. Appetite. 2021;160 doi: 10.1016/j.appet.2021.105122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24(4):385–396. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- Coulthard H., Sharps M., Cunliffe L., van den Tol A. Eating in the lockdown during the Covid 19 pandemic; self-reported changes in eating behaviour, and associations with BMI, eating style, coping and health anxiety. Appetite. 2021;161 doi: 10.1016/j.appet.2020.105082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis L.R., Melisaratos N. The brief symptom inventory: An introductory report. Psychological Medicine. 1983;13(3):595–605. doi: 10.1017/S0033291700048017. [DOI] [PubMed] [Google Scholar]
- DeVellis R.F. 3rd ed. Sage Publications; Thousand Oaks, CA: 2012. Scale development. [Google Scholar]
- Dunn C.G., Kenney E., Fleischhacker S.E., Bleich S.N. Feeding low-income children during the Covid-19 pandemic. New England Journal of Medicine. 2020;382(18) doi: 10.1056/NEJMp2005638. [DOI] [PubMed] [Google Scholar]
- Dunning D. Psychology Press; New York: 2005. Self-insight: Roadblocks and detours on the path to knowing thyself. [Google Scholar]
- Epley N., Dunning D. The mixed blessings of self-knowledge in behavioral prediction: Enhanced discrimination but exacerbated bias. Personality and Social Psychology Bulletin. 2006;32:641–655. doi: 10.1177/0146167205284007. [DOI] [PubMed] [Google Scholar]
- Faul F., Erdfelder E., Lang A.G., Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods. 2007;39:175–191. doi: 10.3758/BF03193146. [DOI] [PubMed] [Google Scholar]
- Field A. (2nd ed.). Sage; 2009. Discovering statistics using SPSS. [Google Scholar]
- Freisthler B., Gruenewald P.J., Tebben E., Shockley McCarthy K., Price Wolf J. Understanding at-the-moment stress for parents during COVID-19 stay-at-home restrictions. Social Science & Medicine. 2021;279 doi: 10.1016/j.socscimed.2021.114025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner P.L. Measuring attitudes to science: Unidimensionality and internal consistency revisited. Research in Science Education. 1995;25(3):283–289. [Google Scholar]
- Groesz L.M., McCoy S., Carl J., Saslow L., Stewart J., Adler N., Laraia B., Epel E. What is eating you? Stress and the drive to eat. Appetite. 2012;58(2):717–721. doi: 10.1016/j.appet.2011.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haddad C., Zakhour M., Bou Kheir M., Haddad R., Al Hachach M., Sacre H., Salameh P. Association between eating behavior and quarantine/confinement stressors during the coronavirus disease 2019 outbreak. Journal of Eating Disorders. 2020;8(1):40. doi: 10.1186/s40337-020-00317-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heggeness M., Fields J. Census.Gov; 2020. Working moms bear brunt of home schooling while working during COVID-19.https://www.census.gov/library/stories/2020/08/parents-juggle-work-and-child-care-during-pandemic.html [Google Scholar]
- Hussenoeder F.S., Conrad I., Engel C., Zachariae S., Zeynalova S., Glaesmer H., Hinz A., Witte V., Tönjes A., Löffler M., Stumvoll M., Villringer A., Riedel-Heller S.G. Analyzing the link between anxiety and eating behavior as a potential pathway to eating-related health outcomes. Scientific Reports. 2021;11(1):14717. doi: 10.1038/s41598-021-94279-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordan A.K., Barnhart W.R., Studer-Perez E.I., Kalantzis M.A., Hamilton L., Musher-Eizenman D.R. ‘Quarantine 15’: Pre-registered findings on stress and concern about weight gain before/during COVID-19 in relation to caregivers' eating pathology. Appetite. 2021;166 doi: 10.1016/j.appet.2021.105580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph P.V., Davidson H.R., Boulineaux C.M., Fourie N.H., Franks A.T., Abey S.K., Henderson W.A. Eating behavior, stress, and adiposity: Discordance between perception and physiology. Biological Research for Nursing. 2018;20(5):531–540. doi: 10.1177/1099800418779460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandiah J., Saiki D., Jones J. Eating behaviors of American adults during the COVID-19 pandemic. 2021;5(1) doi: 10.32892/jmri.248. [DOI] [Google Scholar]
- Kaplan H.I., Kaplan H.S. The psychosomatic concept of obesity. Journal of Nervous and Mental Disease. 1957;125:181–201. doi: 10.1097/00005053-195704000-00004. [DOI] [PubMed] [Google Scholar]
- Konttinen H. Emotional eating and obesity in adults: The role of depression, sleep and genes. Proceedings of the Nutrition Society. 2020;79(3):283–289. doi: 10.1017/S0029665120000166. [DOI] [PubMed] [Google Scholar]
- Konttinen H., Männistö S., Sarlio-Lähteenkorva S., Silventoinen K., Haukkala A. Emotional eating, depressive symptoms and self-reported food consumption. A population-based study. Appetite. 2010;54(3):473–479. doi: 10.1016/j.appet.2010.01.014. [DOI] [PubMed] [Google Scholar]
- Kowal M., Coll-Martín T., Ikizer G., Rasmussen J., Eichel K., Studzińska A., Koszałkowska K., Karwowski M., Najmussaqib A., Pankowski D., Lieberoth A., Ahmed O. Who is the Most stressed during the COVID-19 pandemic? Data from 26 countries and areas. Applied Psychology: Health and Well-Being. 2020;12(4):946–966. doi: 10.1111/aphw.12234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lattimore P., Maxwell L. Cognitive load, stress, and disinhibited eating. Eating Behaviors. 2004;5(4):315–324. doi: 10.1016/j.eatbeh.2004.04.009. [DOI] [PubMed] [Google Scholar]
- Lauren B.N., Silver E.R., Faye A.S., Rogers A.M., Woo-Baidal J.A., Ozanne E.M., Hur C. Predictors of households at risk for food insecurity in the United States during the COVID-19 pandemic. Public Health Nutrition. 2021;24(12):3929–3936. doi: 10.1017/S1368980021000355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarevich I., Irigoyen Camacho M.E., Zepeda Zepeda M., Velázquez-Alva M.d.C. Relationship among obesity, depression, and emotional eating in young adults. Appetite. 2016;107:639–644. doi: 10.1016/j.appet.2016.09.011. [DOI] [PubMed] [Google Scholar]
- Luce K.H., Winzelberg A.J., Das S., Osborne M.I., Bryson S.W., Taylor C.B. Reliability of self-report: Paper versus online administration. Computers in Human Behavior. 2007;23(3):1384–1389. doi: 10.1016/j.chb.2004.12.008. [DOI] [Google Scholar]
- Lund E.M. Even more to handle: Additional sources of stress and trauma for clients from marginalized racial and ethnic groups in the United States during the COVID-19 pandemic. Counselling Psychology Quarterly. 2021;34(3–4):321–330. doi: 10.1080/09515070.2020.1766420. [DOI] [Google Scholar]
- Marjaana Lindeman K.S. Emotional eating and eating disorder psychopathology. Eating Disorders. 2001;9(3):251–259. doi: 10.1080/10640260127552. [DOI] [PubMed] [Google Scholar]
- Mason T.B., Lewis R.J. Profiles of binge eating: The interaction of depressive symptoms, eating styles, and body mass index. Eating Disorders. 2014;22(5):450–460. doi: 10.1080/10640266.2014.931766. [DOI] [PubMed] [Google Scholar]
- McCabe C.J., Kim D.S., King K.M. Improving present practices in the visual display of interactions. Advances in Methods and Practices in Psychological Science. 2018;1(2):147–165. doi: 10.1177/2515245917746792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moorman J.D. The privilege of childcare: An intersectional analysis of the COVID-19 U.S. Childcare crisis and its implications for CAM research. Journal of Children and Media. 2021;15(1):41–43. doi: 10.1080/17482798.2020.1860102. [DOI] [Google Scholar]
- Nordfjærn T., Jørgensen S., Rundmo T. A cross-cultural comparison of road traffic risk perceptions, attitudes towards traffic safety and driver behaviour. Journal of Risk Research. 2011;14(6):657–684. doi: 10.1080/13669877.2010.547259. [DOI] [Google Scholar]
- O’Neill J., Kamper-DeMarco K., Chen X., Orom H. Too stressed to self-regulate? Associations between stress, self-reported executive function, disinhibited eating, and BMI in women. Eating Behaviors. 2020;39 doi: 10.1016/j.eatbeh.2020.101417. [DOI] [PubMed] [Google Scholar]
- Oppenheimer D.M., Meyvis T., Davidenko N. Instructional manipulation checks: Detecting satisficing to increase statistical power. Journal of Experimental Social Psychology. 2009;45(4):867–872. doi: 10.1016/j.jesp.2009.03.009. [DOI] [Google Scholar]
- Palan S., Schitter C. Prolific.ac—A subject pool for online experiments. Journal of Behavioral and Experimental Finance. 2018;17:22–27. doi: 10.1016/j.jbef.2017.12.004. [DOI] [Google Scholar]
- Papandreou C., Arija V., Aretouli E., Tsilidis K.K., Bulló M. Comparing eating behaviours, and symptoms of depression and anxiety between Spain and Greece during the COVID-19 outbreak: Cross-sectional analysis of two different confinement strategies. European Eating Disorders Review. 2020;28(6):836–846. doi: 10.1002/erv.2772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pellegrini C.A., Webster J., Hahn K.R., Leblond T.L., Unick J.L. Relationship between stress and weight management behaviors during the COVID-19 pandemic among those enrolled in an internet program. Obesity Science & Practice. 2021;7(1):129–134. doi: 10.1002/osp4.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson A. Loneliness, anxiety and loss: The Covid pandemic’s terrible toll on kids. Wall Street Journal. 2021 https://www.wsj.com/articles/pandemic-toll-children-mental-health-covid-school-11617969003 April 9. [Google Scholar]
- Phillipou A., Meyer D., Neill E., Tan E.J., Toh W.L., Van Rheenen T.E., Rossell S.L. Eating and exercise behaviors in eating disorders and the general population during the COVID-19 pandemic in Australia: Initial results from the COLLATE project. International Journal of Eating Disorders. 2020;53(7):1158–1165. doi: 10.1002/eat.23317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinaquy S., Chabrol H., Simon C., Louvet J.-P., Barbe P. Emotional eating, alexithymia, and binge-eating disorder in obese women. Obesity Research. 2003;11(2):195–201. doi: 10.1038/oby.2003.31. [DOI] [PubMed] [Google Scholar]
- Prolific . 2020. Prolific | Online participant recruitment for surveys and market research.https://prolific.co/ [Google Scholar]
- Provencher V., Drapeau V., Tremblay A., Després J.-P., Lemieux S. Eating behaviors and indexes of body composition in men and women from the Québec family study. Obesity Research. 2003;11(6):783–792. doi: 10.1038/oby.2003.109. [DOI] [PubMed] [Google Scholar]
- Ramalho S.M., Trovisqueira A., de Lourdes M., Gonçalves S., Ribeiro I., Vaz A.R., Conceição E. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity. 2021. The impact of COVID-19 lockdown on disordered eating behaviors: The mediation role of psychological distress; pp. 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Review E.D. [Newsletters]. US Department of Education (ED) 2020. 2020 | U.S. Department of Education.https://www2.ed.gov/news/newsletters/edreview/2020/0320.html [Google Scholar]
- Rodgers R.F., Lombardo C., Cerolini S., Franko D.L., Omori M., Fuller-Tyszkiewicz M., Linardon J., Courtet P., Guillaume S. The impact of the COVID-19 pandemic on eating disorder risk and symptoms. International Journal of Eating Disorders. 2020;53(7):1166–1170. doi: 10.1002/eat.23318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Şahan E., Eroğlu M.Z., Sertçelik S. Eating behaviors, depression, and anxiety levels of pre bariatric surgery patients with obesity comorbid with or without attention deficit and hyperactivity disorder. Brain and Behavior. 2021;11(1) doi: 10.1002/brb3.1915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schachter S. Obesity and eating. Science. 1968;161(3843):751–756. doi: 10.1126/science.161.3843.751. [DOI] [PubMed] [Google Scholar]
- Schachter S. Lawrence Erlbaum Associates; 1974. Obese humans and rats. [Google Scholar]
- Shen W., Long L.M., Shih C.-H., Ludy M.-J. A humanities-based explanation for the effects of emotional eating and perceived stress on food choice motives during the COVID-19 pandemic. Nutrients. 2020;12(9):2712. doi: 10.3390/nu12092712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snoek H.M., Strien T.V., Janssens J.M.A.M., Engels R.C.M.E. Emotional, external, restrained eating and overweight in Dutch adolescents. Scandinavian Journal of Psychology. 2007;48(1):23–32. doi: 10.1111/j.1467-9450.2006.00568.x. [DOI] [PubMed] [Google Scholar]
- van Strien T., Frijters J.E.R., Bergers G.P.A., Defares P.B. The dutch eating behavior questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. International Journal of Eating Disorders. 1986;5(2):295–315. doi: 10.1002/1098-108X(198602)5:2<295::AID-EAT2260050209>3.0.CO;2-T. [DOI] [Google Scholar]
- Taber K.S. The use of Cronbach’s alpha when developing and reporting research instruments in science education. Research in Science Education. 2018;48(6):1273–1296. doi: 10.1007/s11165-016-9602-2. [DOI] [Google Scholar]
- Udalova V. The United States Census Bureau; 2021. Initial impact of COVID-19 on U.S. economy more widespread than on mortality.https://www.census.gov/library/stories/2021/03/initial-impact-covid-19-on-united-states-economy-more-widespread-than-on-mortality.html [Google Scholar]
- Uğurlu Y.K., Değirmenci D.M., Durgun H., Uğur H.G. The examination of the relationship between nursing students’ depression, anxiety and stress levels and restrictive, emotional, and external eating behaviors in COVID-19 social isolation process. Perspectives in Psychiatric Care. 2021;57(2):507–516. doi: 10.1111/ppc.12703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandervoort D.J. Hostility and health: Mediating effects of belief systems and coping styles. Current Psychology. 2006;25(1):50–66. doi: 10.1007/s12144-006-1016-2. [DOI] [Google Scholar]
- Vazire S., Mehl M.R. Knowing me, knowing you: The accuracy and unique predictive validity of self-ratings and other-ratings of daily behavior. Journal of Personality and Social psychology. 2008;95(5):1202. doi: 10.1037/a0013314. [DOI] [PubMed] [Google Scholar]
- Wilson T.D., Dunn E.W. Self-knowledge: Its limits, value, and potential for improvement. Annual Review of Psychology. 2004;55:493–518. doi: 10.1146/annurev.psych.55.090902.141954. [DOI] [PubMed] [Google Scholar]
- Young D.A., Campbell Z., Zakzanis K.K., Weinstein E. A comparison between an interview and a self-report method of insight assessment in chronic schizophrenia. Schizophrenia Research. 2003;63(1):103–109. doi: 10.1016/S0920-9964(02)00378-X. [DOI] [PubMed] [Google Scholar]
- Young H.A., Cousins A.L., Watkins H.T., Benton D. Is the link between depressed mood and heart rate variability explained by disinhibited eating and diet? Biological Psychology. 2017;123:94–102. doi: 10.1016/j.biopsycho.2016.12.001. [DOI] [PubMed] [Google Scholar]