Abstract
Large numbers of microbes can be present in seminal fluid, and there are differences in the semen microbiota between normal and abnormal semen samples. To evaluate the semen microbiota in patients with leukocytospermia, 87 seminal fluid samples, including 33 samples with a normal seminal leukocyte count and 54 samples with leukocytospermia, were obtained for a cross-sectional analysis. Twenty samples with a normal seminal leukocyte count had normal sperm parameters (Control group), and 13 samples with a normal seminal leukocyte count were from asthenozoospermia patients (Ast group). However, 32 samples with leukocytospermia were from asthenozoospermia patients (LA group), and only 22 samples with leukocytospermia had normal sperm parameters (Leu group). The 16S ribosomal RNA (rRNA) gene sequencing method was used to sequence the microbiota in the seminal fluid, and multiple bioinformatics methods were utilized to analyze the data. Finally, the results showed that the worse sperm parameters were observed in the leukocytospermia-related groups. Semen microbiota analysis found that there was increased alpha diversity in the leukocytospermia-related groups. Firmicutes, Proteobacteria, Actinobacteria, and Bacteroidetes were the primary phyla in the seminal fluid. Two microbiota profiles, namely, Lactobacillus-enriched and Streptococcus-enriched groups, were identified in this study. The majority of the samples in the groups with a normal seminal leukocyte count could be categorized as Lactobacillus-enriched, whereas the majority of the leukocytospermia samples could be categorized as Streptococcus-enriched. Our study indicated that males with leukocytospermia have worse sperm parameters and a different semen microbiota composition compared to males with a normal seminal leukocyte count.
Keywords: 16S rRNA gene sequencing, asthenozoospermia, leukocytospermia, semen microbiota, sperm motility
INTRODUCTION
Leukocytospermia, which is defined by the World Health Organization (WHO) as a seminal leukocyte count of more than 1 × 106 ml−1, may indicate an obstruction or infection in the genitourinary tract.1 Several studies have found that leukocytospermia is closely related to sterility.1,2,3,4 Most of the evidence suggests that an increase in leukocyte count results in worse semen parameters such as lowered sperm count, concentration, and motility, and abnormal morphology, as more leukocytes, can increase reactive oxygen species (ROS), acrosomal damage, and DNA fragmentation. Consequently, a reduction in the seminal leukocyte count may have a favorable effect on sperm function.5,6 However, this idea remains controversial, as some studies have failed to associate leukocytospermia with decreased motility or fertilization ability.7,8,9 Therefore, further investigation is required to understand the relationship between leukocytospermia and sperm parameters.
Microbes, particularly bacteria, have been implicated in the pathogenesis of many human diseases. For a long time, microbes were considered exclusively harmful to human health. However, with the development of next-generation sequencing (NGS), researchers have realized that microbiomes play an important role not only in disease but also in maintaining human health. The microbiota in the gut, oral cavity, skin, and vagina are necessary for the immune response, energy metabolism, and pathological processes.10,11,12,13,14 Compared to studies pertaining to other locations in the body, reports on the microbiota in seminal fluid are relatively low, and most of them have focused on the relationship between sperm quality and microbiota. Hou et al.15 identified six groups of bacteria in seminal fluid, with Anaerococcus being significantly negatively correlated with sperm quality. Weng et al.16 found that seminal fluid samples could be categorized into three groups based on the predominance of Lactobacillus, Pseudomonas, or Prevotella, and most normal samples could be categorized in the Lactobacillus group. Baud et al.17 reported similar results, which indicated that semen samples broadly had three microbiota profiles, namely, Prevotella enriched, Lactobacillus enriched, and polymicrobial. Furthermore, vaginal microbiota were also found in the seminal fluid samples in that study. Pagliuca et al.18 study found that a relationship between microbiological evaluation and sperm DNA fragmentation in semen samples of patients undergoing fertility investigation.
The mechanism of leukocytospermia is still unclear, and bacterial infection may contribute to this process.19,20 Although the correlation between leukocyte count and bacterial infection of the semen remains controversial, treatment with antibiotics improves sperm parameters in patients with leukocytospermia, suggesting that the modulation of seminal microorganisms could affect sperm quality and fertilization ability.6,21,22
This study aimed to assess the relationship between leukocytospermia and sperm parameters in normal and asthenozoospermic males. Furthermore, we performed 16S ribosomal RNA (rRNA) gene sequencing on the MiSeq platform (Illumina Co., Ltd., San Diego, CA, USA) to analyze the composition of the semen microbiota in 87 samples, and the results related to the effects of leukocytospermia on the semen microbiota are described here.
PARTICIPANTS AND METHODS
Participants
For this retrospective study, patient medical records dated between December 2018 and December 2020 were obtained from Xiangya Hospital, Central South University (Changsha, China). The subjects were men seen for premarital checkups or patients with premature ejaculation and sterility. Because the influence of leukocytospermia on azoospermia and oligospermia (sperm concentration <15 × 106 ml−1) is minimal, the primary etiologies are endocrine abnormalities, intrinsic disorders of spermatogenesis, and obstruction of the ductal system.23,24,25 Patients with documented azoospermia and oligospermia were not included in this study. Patients with any other chronic diseases were excluded from this study. Data on age, medical history, semen volume, sperm concentration, progressive sperm motility, total sperm motility, sperm acrosin activity, and leukocytospermia were extracted from these records. The use of the hospital's database was approved by the Ethical Review Board at Xiangya Hospital, Central South University (No. 201906122).
Based on the WHO guidelines, asthenozoospermia was defined as a sperm concentration higher than 15 × 106 ml−1, with progressive sperm motility <32% or total sperm motility <40%. Leukocytospermia was defined as a seminal leukocyte count >1 × 106 ml−1.26 Sperm parameters including sperm concentration, progressive sperm motility, and total sperm motility were determined in our laboratory by a skilled technician. The seminal leukocyte count was stained using the peroxidase method, and acrosin was quantified using an enzyme-linked immunosorbent assay (ELISA) kit. Finally, the selected samples were categorized into four groups. The Control group included subjects with normal sperm parameters and a normal seminal leukocyte count, the asthenozoospermia (Ast) group included subjects with a normal seminal leukocyte count and asthenozoospermia, the leukocytospermia (Leu) group included subjects with normal sperm parameters, but with a seminal leukocyte count >1 × 106 ml−1, and the final group (LA group) included subjects with asthenozoospermia and a seminal leukocyte count >1 × 106 ml−1.
Sample collection
In addition to the retrospective study, a cross-sectional study with 87 subjects with normal sperm parameters or leukocytospermia was conducted at Xiangya Hospital, Central South University. As described above, subjects were divided into four groups: the Control group (n = 20), the Ast group (n = 13), the Leu group (n = 22), and the LA group (n = 32). Subjects were excluded if they had any systemic diseases (e.g., cardiac, pulmonary, digestive, neural, and renal diseases, hypertension, and diabetes) or any type of tumor, zoospermia, or oligospermia; a fever or any infection in the previous two months; a personal or family history of genetic or immune diseases; or a history of use of antibiotics, immunosuppressive drugs, or corticosteroids in the previous two months. All participants provided written informed consent. The study protocol was reviewed and approved by the Ethical Review Board at the Xiangya Hospital, Central South University (No. 201906122).
Seminal fluid was collected as per the WHO guidelines.26 The seminal fluid was collected by masturbation after 3 to 7 days of abstinence. Before sample collection, the hands and penises of the subjects were washed twice with soap. The seminal fluid was ejaculated into a sterile receptacle; 1 ml of seminal fluid sample was transferred to sterile microcentrifuge tubes and immediately stored at −80°C, and the rest of the sample was used for clinical tests. Venous blood samples from all subjects were collected, and white blood cell (WBC), hemoglobin (Hb), and platelet (PLT) counts were analyzed in our biochemistry laboratory.
Semen microbiota analysis
The QIAamp DNA mini kit (Qiagen Biotechology Co., Ltd., Dusseldorf, Germany) was used to extract genomic DNA, and the manufacturer's instructions were strictly followed. Bacterial DNA amplification was performed as previously described.27 Bacterial DNA was amplified via PCR (ABI GeneAmp® 9700, Boston, MA, USA) using custom-barcoded primers targeting the V3–V4 regions (338F: ACTCCTACGGGAGGCAGCAG, −806R: GGACTACHVGGGTWTCTAAT) of the 16S rRNA. Next, we purified the amplified sequences with the AxyPrep DNA Gel Extraction Kit and quantified the purified products with QuantiFluor™-ST (Promega Co., Madison, WI, USA). Finally, the TruSeqTM DNA Sample Prep Kit (Illumina Co., Ltd.) was used to construct the sequencing library, and the MiSeq platform was used to sequence the eligible library.
The raw sequences were analyzed by FLASH (https://ccb.jhu.edu/software/FLASH/index.shtm) for quality control and nonredundant gene building high-quality sequences reached a 97% nucleotide similarity were clustered into operational taxonomic units (OTUs). Nonredundant genes were stored in the Silva 138 release database (http://www.arb-silva.de) for species annotation and assessment, and the relative abundance was calculated at different levels (Domain, kingdom, Phylum, Class, Order, Family, Genus, and Species). Alpha diversity was evaluated using the Shannon index, ace index, and chao index with mothur software (https://www.mothur.org/wiki/Download_mothur). Beta diversity was analyzed using principal coordinate analysis (PCoA), with the Bray Curtis dissimilarity distance matrix at the OTU level by R software (https://www.r-project.org/). The relative abundance of genera was normalized by the log2 method. The microbiota clusters at the genus level were determined using the partitioning around medoids (PAM) algorithm with the Bray Curtis distance matrix. A heatmap of the top 15 most abundant genera was generated using R software. The semen microbiota analysis in our study was completed at Shanghai Majorbio Bio-pharm Technology Co., Ltd. (Shanghai, China). The experimental design is shown in Figure 1.
Figure 1.
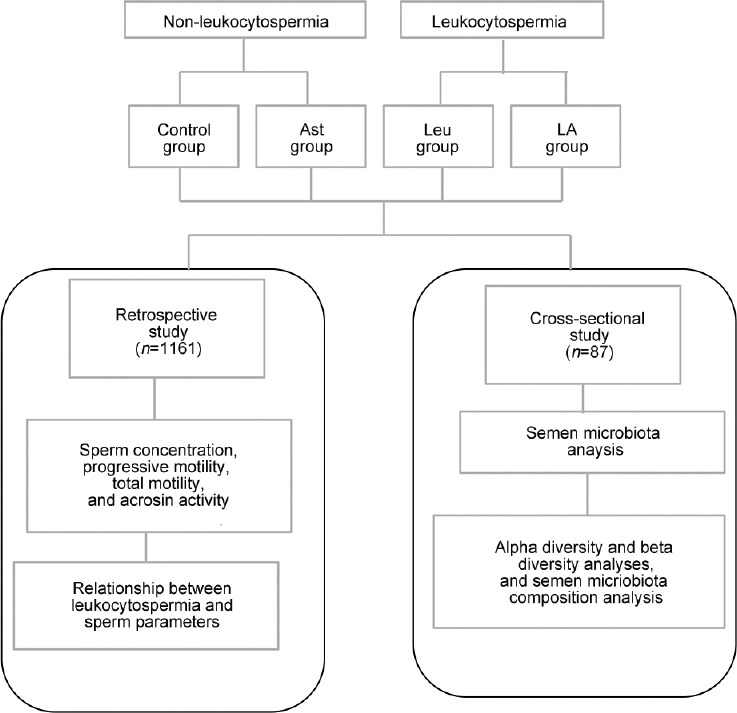
Experimental design. Ast group: asthenozoospermia patients with a normal seminal leukocyte count; Leu group: patients with leukocytospermia and normal sperm parameters; LA group: asthenozoospermia patients with leukocytospermia.
Statistical analyses
Differences in sperm parameters and detailed subject information between the Control and Leu groups or the Ast and LA groups in the retrospective study were evaluated using the nonparametric Kruskal–Wallis test followed by post hoc Wilcoxon rank sum test with continuity correction. Sequence number, alpha diversity indices, and the relative abundance of phyla were determined using Student's t-tests and expressed as the mean ± standard deviation (s.d.). All statistical analyses were conducted using SPSS 23.0 (SPSS Inc., Chicago, IL, USA). P < 0.05 was considered statistically significant.
RESULTS
Relationship between leukocytospermia and sperm parameters
Based on the inclusion criteria, a total of 1161 samples were selected for further analysis in the retrospective study. In total, 460 samples with a normal seminal leukocyte count and 701 samples with leukocytospermia were included in this study (Table 1 and Supplementary Table 1 (94.6KB, pdf) ). In the non-leukocytospermia groups, 66.1% of samples had normal sperm parameters, and only 33.9% of samples were from asthenozoospermia patients. However, 63.6% of samples with leukocytospermia fulfilled the diagnostic criteria for asthenozoospermia. Moreover, compared to the Leu group, the seminal leukocyte count was significantly increased by 20.0% in the LA group (P < 0.001).
Table 1.
Sperm parameters in the nonleukocytospermia and leukocytospermia groups
| Variable | Non-leukocytospermia | Leukocytospermia | ||
|---|---|---|---|---|
|
|
|
|||
| Control | Ast | Leu | LA | |
| Patient, n (%) | 304 (66.1) | 156 (33.9) | 255 (36.4) | 446 (63.6) |
| Leukocytospermia (×106 ml−1) | 0.70 (0.50–0.90) | 0.73 (0.60–0.90) | 1.40 (1.10–1.50)ab | 1.68 (1.20–1.70)ab |
| Age (year) | 30.6 (28.0–33.8) | 30.2 (28.0–33.0) | 30.0 (27.0–33.0) | 30.5 (28.0–33.0) |
| Semen volume (ml) | 3.0 (1.5–4.5) | 3.1 (2.0–4.0) | 3.0 (2.0–4.0) | 3.0 (1.5–4.0) |
| Sperm concentration (×106 ml−1) | 195.6 (140.8–237.9) | 106.7 (61.8–140.8)a | 177.4 (132.8–207.2)ab | 96.4 (64.0–122.2)ab |
| Progressive sperm motility (%) | 44.0 (37.4–49.3) | 24.6 (21.6–29.6)a | 39.6 (34.6–43.2)ab | 22.7 (18.2–28.5)ab |
| Total sperm motility (%) | 67.5 (60.3–74.7) | 43.1 (38.6–50.2)a | 61.9 (55.1–68.5)ab | 40.5 (35.0–48.0)ab |
| Sperm acrosin activity (×106 µIU−1) | 108.0 (95.3–118.3) | 75.0 (56.9–91.2)a | 96.6 (83.8–106.9)ab | 63.7 (50.8–72.0)ab |
aThe Ast, Leu or LA group compared to the Control group, P<0.001; bThe Leu or LA group compared to the Ast group, P<0.001. Data are shown as median (IQR). Ast group: asthenozoospermia patients with a normal seminal leukocyte count; Leu group: patients with leukocytospermia and normal sperm parameters; LA group: asthenozoospermia patients with leukocytospermia; IQR: interquartile range
No significant differences in age or ejaculated volume were observed among the four groups (Table 1). The other four sperm parameters, including sperm concentration, progressive sperm motility, total sperm motility, and sperm acrosin activity, were significantly decreased in the groups with leukocytospermia (all P < 0.001). Compared to those of the Control group, sperm concentration, progressive sperm motility, total sperm motility, and sperm acrosin activity were significantly decreased in the Leu group by 10.2%, 11.2%, 9.5%, and 11.8%, respectively. Similarly, compared to those of the Ast group, sperm concentration, progressive sperm motility, total sperm motility, and sperm acrosin activity decreased in the LA group by 10.7%, 8.4%, 6.4%, and 17.7%, respectively. These results indicated that samples from patients with leukocytospermia had worse sperm parameters than samples with a normal seminal leukocyte count.
Patient information
Detailed information on the samples from the 87 subjects who were included in the cross-sectional study is given in (Supplementary Table 2 (108.5KB, pdf) ). We did not observe any differences in age, WBC, Hemoglobin, PLT, or smoking ratio among the groups. Similar to the retrospective study, sperm parameters, including sperm concentration, progressive sperm motility, total sperm motility, and sperm acrosin activity, were found to be significantly decreased in the leukocytospermia-related groups (all P < 0.05; Figure 2 and Supplementary Table 3).
Figure 2.
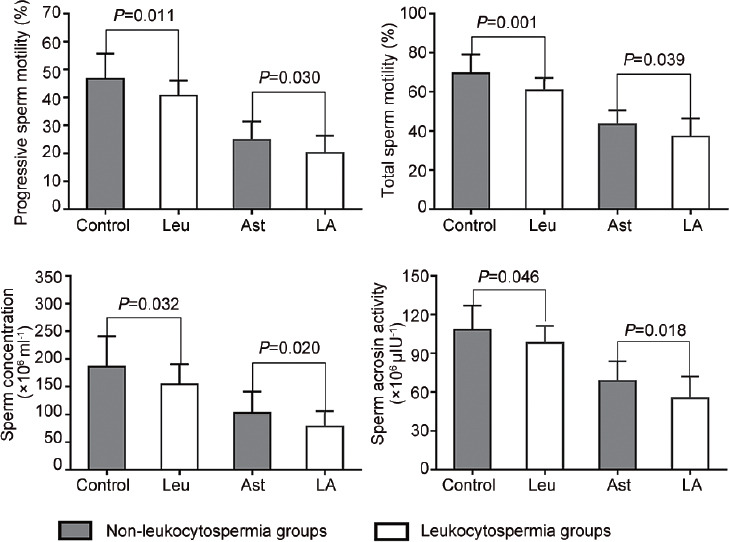
Sperm parameters of the 87 subjects. The leukocytospermia groups had worse sperm parameters. Ast group: asthenozoospermia patients with a normal seminal leukocyte count; Leu group: patients with leukocytospermia and normal sperm parameters; LA group: asthenozoospermia patients with leukocytospermia.
Supplementary Table 3.
Detailed patient information for sperm microbiota analysis
| Control group | Asthenozoospermia group | Leukocytospermia group | LA group | |
|---|---|---|---|---|
| Number | 20 | 13 | 22 | 32 |
| Age (year), median (IQR)* | 29.0 (27.3–30.0) | 31.2 (29.0–33.5) | 29.3 (26.8–30.3) | 32.4 (28.3–37.8) |
| Semen volume (ml), median (IQR) | 3.4 (2.1–4.9) | 3.8 (3.0–4.5) | 3.8 (3.0–5.0) | 3.8 (3.0–4.5) |
| WBC (109 l−1), median (IQR)* | 7.0 (6.0–7.9) | 6.8 (5.8–7.5) | 7.0 (5.4–8.2) | 6.8 (5.6–7.0) |
| Hemoglobin (g l−1), median (IQR)* | 147.4 (134.8–160.2) | 149.4 (137.3–157.5) | 147.5 (130.0–159.0) | 151.4 (145.0–161.0) |
| PLT (1012 l−1), median (IQR)* | 222.6 (192.5–253.3) | 223.5 (201.5–248.8) | 234.7 (201.5–248.8) | 219.3 (200.0–234.0) |
| Smoking ratio (%)* | 25.0 | 30.7 | 27.3 | 25.8 |
*No significant difference between each group. LA group: asthenozoospermia patients with leukocytospermia; IQR: interquartile range; WBC: white blood cell; PLT: pallet
Semen microbiota analysis at the OTU level
A total of 3 945 550 high-quality sequences were detected, and 15 937 OTUs were clustered from the 87 semen samples (Supplementary Table 4 (1MB, pdf) ). We found that the number of OTUs in the LA group was as high as 10 679, and only 5399 OTUs were identified in the Ast group (Figure 3a). The number of OTUs in the Control group was 8107 and that in the Leu group was 8855. The Leu group had 1780 unique OTUs, and 2896 unique OTUs existed in the LA groups. However, only 1513 and 666 unique OTUs were identified in the Control and Ast groups, respectively. The Shannon index, ace index, and chao index were used to assess the alpha diversity of the semen microbiota. Compared to the Control group, the Shannon index was found to be significantly increased (P < 0.05), and the ace index and chao index were slightly increased in the Leu group (Figure 3b). Similar results were observed in the Ast and LA groups, indicating that semen samples from subjects with leukocytospermia had increased alpha diversity (Figure 3b). To examine the bacterial community structure in all semen samples, a beta diversity analysis was performed with PCoA at the OTU level. However, the semen samples could not be separated into their four groups by PCoA (Figure 3c).
Figure 3.
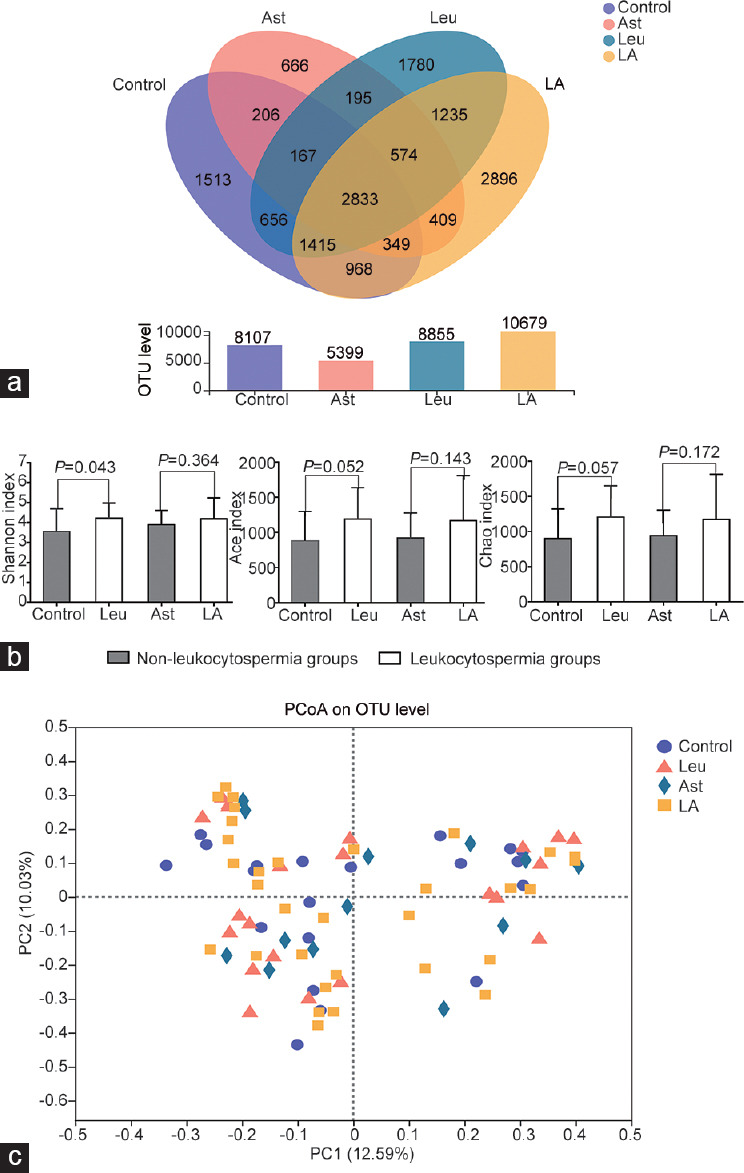
Semen microbiota was analyzed at the OTU level. (a) Venn diagram of Control, Leu, Ast, and LA groups at the OTU level. The leukocytospermia-related groups had more OTUs. (b) Alpha diversity analysis. The leukocytospermia-related groups had an increase in alpha diversity. (c) PCoA of the microbial composition. No significant separation between the different groups at the OTU level. Ast group: asthenozoospermia patients with a normal seminal leukocyte count; Leu group: patients with leukocytospermia and normal sperm parameters; LA group: asthenozoospermia patients with leukocytospermia; OTU: operational taxonomic unit; PCoA: principal coordinate analysis.
Semen microbiota analysis at the phylum level
To further investigate the sperm microbial composition, we analyzed the results at the phylum level. Firmicutes, Proteobacteria, Actinobacteria, and Bacteroidetes were the primary phyla in every group (Figure 4a). We did not observe significant differences in the proportion of these three phyla (including Firmicutes, Proteobacteria, and Actinobacteria) among the four groups (Figure 4a and 4b). In the Control group, the composition of Firmicutes, Proteobacteria, and Actinobacteria accounted for 38.7%, 26.3% and 13.6%, respectively. The composition of Firmicutes, Proteobacteria, and Actinobacteria in the Leu group was 37.6%, 25.0%, and 13.4%, respectively. Similarly, the proportions of these three phyla were 35.3%, 28.9%, and 18.1% in the Ast group and 41.2%, 25.2%, and 12.6% in the LA group (Figure 4a). However, the relative abundance of Bacteroidetes was different in each group. The proportion of Bacteroidetes in the Control group was 3.9% but that in the Leu group was 9.4% (Figure 4a). Compared to the Control group, Bacteroidetes was significantly increased in the Leu group (P < 0.05; Figure 4b). As a result, the ratio of Firmicutes/Bacteroidetes was significantly decreased in the Leu group. Compared to that in the Ast group, the relative abundance of Bacteroidetes moderately increased in the LA group, accompanied by a slight decrease in the ratio of Firmicutes/Bacteroidetes (Figure 4b).
Figure 4.
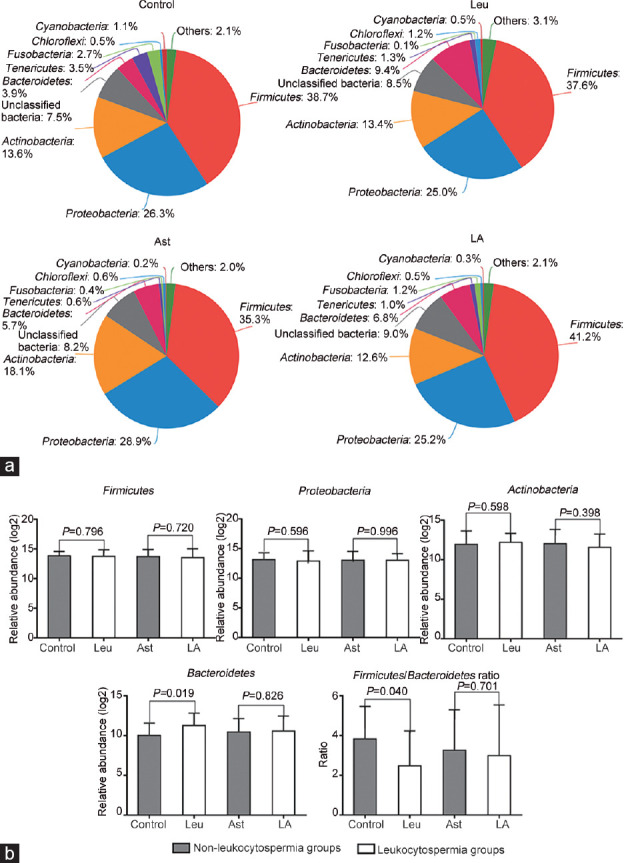
Semen microbiota at the phylum level. (a) Pie plot of the main semen microbiota at the phylum level. Firmicutes, Proteobacteria, Actinobacteria, and Bacteroidetes were the primary phyla. (b) Relative abundances of the different phyla in each group. Leukocytospermia-related groups had a different semen microbiota composition, with an increase in Bacteroidetes and a decrease in the Firmicutes/Bacteroidetes ratio. Ast group: asthenozoospermia patients with a normal seminal leukocyte count; Leu group: patients with leukocytospermia and normal sperm parameters; LA group: asthenozoospermia patients with leukocytospermia.
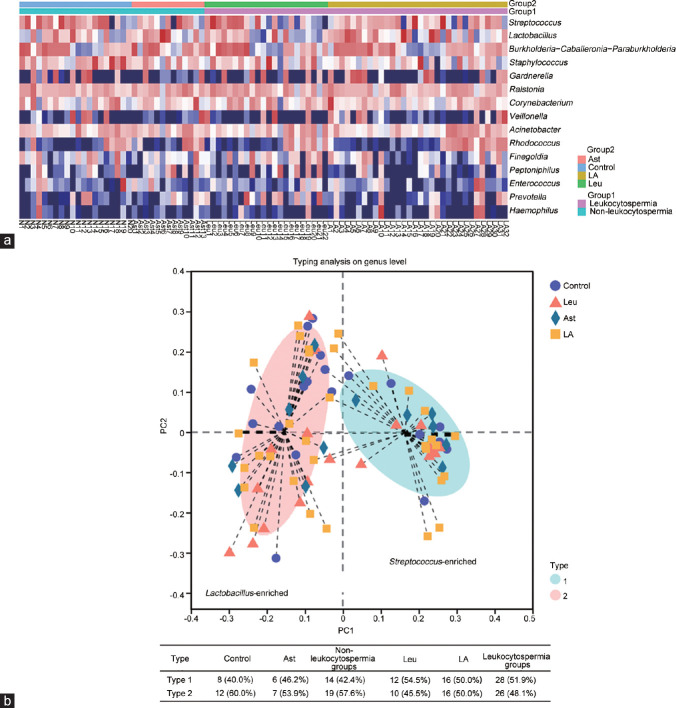
Semen microbiota analysis at the genus level
At the genus level, the composition of the semen microbiota was analyzed. Overall, the top 15 most abundant genera in the semen were Streptococcus, Lactobacillus, Burkholderia-Caballeronia-Paraburkholderia, Staphylococcus, Gardnerella, Ralstonia, Corynebacterium, Veillonella, Acinetobacter, Rhodococcus, Finegoldia, Peptoniphilus, Enterococcus, Prevotella, and Haemophilus (Figure 5a), and most of these genera are also found in the vagina.12,28,29,30,31,32,33 Microbiota profile analysis revealed that the seminal genera were clustered into two main groups: Lactobacillus-enriched and Streptococcus-enriched groups (Figure 5b); 60.0% of Control subjects and 53.9% of Ast subjects belonged to the Lactobacillus-enriched group, whereas only 45.5% of Leu subjects and 50.0% of LA subjects belonged to the Lactobacillus-enriched group. In other words, 57.6% of non-leukocytospermia subjects but only 48.1% of leukocytospermia subjects belonged to Lactobacillus-enriched group. In contrast, 51.9% of leukocytospermia subjects and only 42.4% of subjects with normal seminal leukocyte counts exhibited to Streptococcus-enriched group. This indicated that there was a decrease in Lactobacillus and an increase in Streptococcus in samples from subjects with leukocytospermia.
Figure 5.
Semen microbiota on the genus level. (a) Heatmap of top 15 most abundant genera. Most of the semen microbiota was also been found in the vagina. (b) Community cluster of semen microbiota in each sample at the genus level. The semen samples clustered into two main groups Lactobacillus-enriched and Streptococcus-enriched, 57.6% of the samples in the groups with a normal seminal leukocyte count could be categorized as Lactobacillus-enriched, with 48.1% of leukocytospermia-related samples being Lactobacillus-enriched. In contrast, 51.9% of the leukocytospermia samples could be categorized as Streptococcus-enriched, whereas only 42.4% of the non-leukocytospermia samples were Streptococcus-enriched. Ast group: asthenozoospermia patients with a normal seminal leukocyte count; Leu group: patients with leukocytospermia and normal sperm parameters; LA group: asthenozoospermia patients with leukocytospermia.
DISCUSSION
In this retrospective study, based on the diagnostic criteria of asthenozoospermia and leukocytospermia, 1161 samples were obtained and categorized into four groups. The results revealed that samples from subjects with leukocytospermia in the Leu and LA groups had lower sperm quality, indicating that the seminal leukocyte count was negatively correlated with sperm parameters not only in normal males but also in asthenozoospermic males. These results are consistent with those of previous studies1,2,3,34 and reconfirmed the relationship between leukocytospermia and sperm parameters.
Owing to the results indicating an important effect of sperm microbes on seminal leukocyte count and sperm parameters, we used 16S rRNA gene sequencing to identify the microbiota in additional 87 seminal samples. Several studies have observed that higher alpha diversity in the gut, skin, and oral cavity is beneficial for human health.35,36,37 However, this rule does not seemingly apply to the microbiota in genital tract, and some studies have found that higher diversity of microbiota is a negative factor for sperm health.38,39 Semen from men with chronic prostatitis/chronic pelvic pain syndrome has been shown to have a higher species diversity than that of healthy men, and women with bacterial vaginosis have communities that are more polymicrobial.40,41 In this study, the results showed that alpha diversity increased in the leukocytospermia-related groups. A possible reason for this could be the increased microbes in samples from subjects with leukocytospermia.
Although there are multiple microbiota communities in different parts of the urogenital tract in males, Firmicutes, Proteobacteria, Actinobacteria, and Bacteroidetes are the most abundant in seminal fluid.37,40 We found that Firmicutes, Proteobacteria, Actinobacteria, and Bacteroidetes were the major phyla in sperm samples, and this result supported the above conclusion. It is well known that these four phyla are also abundant at other body sites.42,43 A study of 1135 Dutch participants showed that Firmicutes, Proteobacteria, Bacteroidetes, and Actinobacteria are the dominant bacterial communities in the gut, and other studies have found that Firmicutes, Proteobacteria, Actinobacteria, and Bacteroidetes are the most abundant phyla in the oral tract, skin, and vagina.43,44,45 Disorder in the dominant phyla has a severe effect on host health, and several studies have indicated that obesity, diabetes, and cardiovascular diseases are associated with an increase in the Firmicutes phylum and a relatively lower abundance of the Bacteroidetes phylum in the gut.46 Another study found that azoospermic men associated with a decreased of Bacteroidetes.47 However, different results are found in another study that compared with healthy men, patients with prostatitis have a higher abundance of Bacteroidetes in seminal fluid.40 In this study, the results showed that a significant increase of Bacteroidetes was observed in the Leu group, with a slight increase in the LA group. Correspondingly, the ratio of Firmicutes/Bacteroidetes was decreased in the subjects with leukocytospermia. Hence, this study found that leukocytospermia-related groups have a different microbiota composition at the phylum level.
Subsequently, we analyzed the composition of the semen microbiota at the genus level. Streptococcus, Burkholderia-Caballeronia-Paraburkholderia, Lactobacillus, Staphylococcus, Gardnerella, Ralstonia, Corynebacterium, Veillonella, Acinetobacter, Rhodococcus, Finegoldia, Peptoniphilus, Enterococcus, Prevotella, and Haemophilus were the most abundant genera in the sperm samples. Some 16S rRNA-based NGS studies have produced similar results.15,16,17,48,49,50,51 Interestingly, the majority of these genera can also be found in the vaginal microbiota.12,29,30,31,32,33,38,49 Studies have demonstrated that bacteria are shared among partners, and young men with no sexual experience have been shown to have a lower bacterial concentration and lower bacterial diversity in their semen than sexually experienced men of the same age.52 Correspondingly, an abnormal semen microbiota could generate disorders of vaginal bacteria and finally influence the fertility.38,49 In our study, the presence of these bacteria in males may be attributed to the exchange of bacteria in the reproductive tracts between sexual partners. However, a distinction in the seminal microbiota at the genus level was not observed between the non-leukocytospermia and leukocytospermia groups.
The samples in this study could be clustered into two groups, namely, Lactobacillus-enriched and Streptococcus-enriched groups. Furthermore, we found that most of the subjects with normal seminal leukocyte counts exhibited to the Lactobacillus-enriched group. Our results corroborate those of previous studies that have used NGS to analyze semen microbiota and found that normal samples had a higher abundance of Lactobacillus.15,16,17 Lactobacillus is usually considered to be beneficial for human health, and it has been isolated from the gut, skin, oral cavity, and vagina.53,54 Lactobacillus species are the most commonly found microbes in the vagina of healthy women. These microbes can produce large amounts of lactic acid, maintaining the normal microenvironment of the vagina.53,55,56 Some studies have found that transplantation of Lactobacillus in subjects with vaginosis was effective.55,56 The genus Streptococcus comprises more than one hundred species and is a prevalent human pathogen causing pneumonia, otitis media, bacteremia, and meningitis.57 Some studies revealed that patients with prostatitis had a higher relative abundance of Streptococcus in their seminal fluid.58,59 Our study found that more subjects with leukocytospermia belonged to the Streptococcus-enriched group, while more subjects with non-leukocytospermia belonged to the Lactobacillus-enriched group. However, the cluster relationship in this study was weak, and more samples should be collected for further study to verify these results. Changes of seminal microbiota in leukocytospermia-related groups were observed, so we could infer that if the abnormal semen microbiota are corrected in patients with leukocytospermia, there might be an improvement in their sperm parameters and benefit for the treatment of sterility.
CONCLUSION
This study provided evidence indicating that males with leukocytospermia have worse sperm parameters. The results of semen microbiota analysis showed that the leukocytospermia-related groups had a higher alpha diversity. Firmicutes, Proteobacteria, Actinobacteria, and Bacteroidetes were the primary phyla in the seminal fluid. The Bacteroidetes phylum was more prevalent in leukocytospermia-related subjects. Several bacterial genera, including Streptococcus, Lactobacillus, Burkholderia-Caballeronia-Paraburkholderia, Staphylococcus, Gardnerella, Ralstonia, Corynebacterium, Veillonella, Acinetobacter, Rhodococcus, Finegoldia, Peptoniphilus, Enterococcus, Prevotella, and Haemophilus, were abundantly found in sperm samples, and most of these genera have been previously found in the vaginal microbiota. Moreover, subjects with leukocytospermia have a characteristic semen microbiota composition, with a decrease in Lactobacillus and an increase in Streptococcus.
AUTHOR CONTRIBUTIONS
This study was designed by YY, XJQ, DSW, and LLZ. YY, JKL, TT, YHL, and CHZ collected the sperm samples. YY, XJQ, and LLZ collected the clinical data. The data were analyzed by YY, DSW, HL, and LLZ. The draft was written by YY and critically reviewed by all the authors. All authors read and approved the final manuscript.
COMPETING INTERESTS
All authors declare no competing interests.
ACKNOWLEDGMENTS
This work was supported by Youth Foundation of National Natural Science Foundation of China (No. 81703963 and No. 81202807), the Natural Science Foundation of Hunan (No. 2018JJ2667 and No. 2019JJ40511), and the Scientific Research Project of Chinese Traditional Medicine Administration Bureau in Hunan Province (No. 201806).
Supplementary Information is linked to the online version of the paper on the Asian Journal of Andrology website.
REFERENCES
- 1.Henkel R, Offor U, Fisher D. The role of infections and leukocytes in male infertility. Andrologia. 2021;53:e13743. doi: 10.1111/and.13743. [DOI] [PubMed] [Google Scholar]
- 2.Mupfiga C, Fisher D, Kruger T, Henkel R. The relationship between seminal leukocytes, oxidative status in the ejaculate, and apoptotic markers in human spermatozoa. Syst Biol Reprod Med. 2013;59:304–11. doi: 10.3109/19396368.2013.821540. [DOI] [PubMed] [Google Scholar]
- 3.Eldamnhoury EM, Elatrash GA, Rashwan HM, El-Sakka AI. Association between leukocytospermia and semen interleukin-6 and tumor necrosis factor-alpha in infertile men. Andrology. 2018;6:775–80. doi: 10.1111/andr.12513. [DOI] [PubMed] [Google Scholar]
- 4.Moubasher A, Sayed H, Mosaad E, Mahmoud A, Farag F, et al. Impact of leukocytospermia on sperm dynamic motility parameters, DNA and chromosomal integrity. Cent European J Urol. 2018;71:470–5. doi: 10.5173/ceju.2018.1724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oliva A, Multigner L. Ketotifen improves sperm motility and sperm morphology in male patients with leukocytospermia and unexplained infertility. Fertil Steril. 2006;85:240–3. doi: 10.1016/j.fertnstert.2005.06.047. [DOI] [PubMed] [Google Scholar]
- 6.Jung JH, Kim MH, Kim J, Baik SK, Koh SB, et al. Treatment of leukocytospermia in male infertility: a systematic review. World J Mens Health. 2016;34:165–72. doi: 10.5534/wjmh.2016.34.3.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kaleli S, Oçer F, Irez T, Budak E, Aksu MF. Does leukocytospermia associate with poor semen parameters and sperm functions in male infertility.The role of different seminal leukocyte concentrations? Eur J Obstet Gynecol Reprod Biol. 2000;89:185–91. doi: 10.1016/s0301-2115(99)00204-3. [DOI] [PubMed] [Google Scholar]
- 8.Cavagna M, Oliveira JB, Petersen CG, Mauri AL, Silva LF, et al. The influence of leukocytospermia on the outcomes of assisted reproductive technology. Reprod Biol Endocrinol. 2012;10:44. doi: 10.1186/1477-7827-10-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Castellini C, D’Andrea S, Martorella A, Minaldi E, Necozione S, et al. Relationship between leukocytospermia, reproductive potential after assisted reproductive technology, and sperm parameters: a systematic review and meta-analysis of case-control studies. Andrology. 2020;8:125–35. doi: 10.1111/andr.12662. [DOI] [PubMed] [Google Scholar]
- 10.Qin J, Li R, Raes J, Arumugam M, Burgdorf KS, et al. A human gut microbial gene catalogue established by metagenomic sequencing. Nature. 2010;464:59–65. doi: 10.1038/nature08821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Egert M, Simmering R, Riedel CU. The association of the skin microbiota with health, immunity, and disease. Clin Pharmacol Ther. 2017;102:62–9. doi: 10.1002/cpt.698. [DOI] [PubMed] [Google Scholar]
- 12.Fettweis JM, Serrano MG, Brooks JP, Edwards DJ, Girerd PH, et al. The vaginal microbiome and preterm birth. Nat Med. 2019;25:1012–21. doi: 10.1038/s41591-019-0450-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Oh J, Unutmaz D. Immune cells for microbiota surveillance. Science. 2019;366:419–20. doi: 10.1126/science.aaz4014. [DOI] [PubMed] [Google Scholar]
- 14.Yao Y, Yan L, Chen H, Wu N, Wang W, et al. Cyclocarya paliurus polysaccharides alleviate type 2 diabetic symptoms by modulating gut microbiota and short-chain fatty acids. Phytomedicine. 2020;77:153268. doi: 10.1016/j.phymed.2020.153268. [DOI] [PubMed] [Google Scholar]
- 15.Hou D, Zhou X, Zhong X, Settles ML, Herring J, et al. Microbiota of the seminal fluid from healthy and infertile men. Fertil Steril. 2013;100:1261–9. doi: 10.1016/j.fertnstert.2013.07.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weng SL, Chiu CM, Lin FM, Huang WC, Liang C, et al. Bacterial communities in semen from men of infertile couples: metagenomic sequencing reveals relationships of seminal microbiota to semen quality. PLoS One. 2014;9:e110152. doi: 10.1371/journal.pone.0110152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baud D, Pattaroni C, Vulliemoz N, Castella V, Marsland BJ, et al. Sperm microbiota and its impact on semen parameters. Front Microbiol. 2019;10:234. doi: 10.3389/fmicb.2019.00234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pagliuca C, Cariati F, Bagnulo F, Scaglione E, Carotenuto C, et al. Microbiological evaluation and sperm DNA fragmentation in semen samples of patients undergoing fertility investigation. Genes (Basel) 2021;12:654. doi: 10.3390/genes12050654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lackner JE, Herwig R, Schmidbauer J, Schatzl G, Kratzik C, et al. Correlation of leukocytospermia with clinical infection and the positive effect of antiinflammatory treatment on semen quality. Fertil Steril. 2006;86:601–5. doi: 10.1016/j.fertnstert.2006.01.032. [DOI] [PubMed] [Google Scholar]
- 20.Punab M, Lõivukene K, Kermes K, Mändar R. The limit of leucocytospermia from the microbiological viewpoint. Andrologia. 2003;35:271–8. [PubMed] [Google Scholar]
- 21.Brunner RJ, Demeter JH, Sindhwani P. Review of guidelines for the evaluation and treatment of leukocytospermia in male infertility. World J Mens Health. 2019;37:128–37. doi: 10.5534/wjmh.180078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pajovic B, Pajovic L, Vukovic M. Effectiveness of antibiotic treatment in infertile patients with sterile leukocytospermia induced by tobacco use. Syst Biol Reprod Med. 2017;63:391–6. doi: 10.1080/19396368.2017.1373158. [DOI] [PubMed] [Google Scholar]
- 23.Cocuzza M, Alvarenga C, Pagani R. The epidemiology and etiology of azoospermia. Clinics (Sao Paulo) 2013;68(Suppl 1):15–26. doi: 10.6061/clinics/2013(Sup01)03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Magharehabed M, Almadani N, Askari M, Naji M, Akbari A, et al. Rare case of an oligospermic male with 46,XX/46,XY tetragametic chimerism. Andrologia. 2019;51:e13290. doi: 10.1111/and.13290. [DOI] [PubMed] [Google Scholar]
- 25.Dong WW, Huang HL, Yang W, Liu J, Yu Y, et al. Testis-specific Fank1 gene in knockdown mice produces oligospermia via apoptosis. Asian J Androl. 2014;16:124–30. doi: 10.4103/1008-682X.122592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.WHO . 5th ed. Geneva: World Health Organization; 2010. WHO Laboratory Manual for the Examination and Processing of Human Semen. [Google Scholar]
- 27.Yao Y, Chen H, Yan L, Wang W, Wang D. Berberine alleviates type 2 diabetic symptoms by altering gut microbiota and reducing aromatic amino acids. Biomed Pharmacother. 2020;131:110669. doi: 10.1016/j.biopha.2020.110669. [DOI] [PubMed] [Google Scholar]
- 28.Jie Z, Chen C, Hao L, Li F, Song L, et al. Life history recorded in the vagino-cervical microbiome along with multi-omics? Genomics Proteomics Bioinformatics. 2021 doi: 10.1016/j.gpb.2021.01.005. doi: 10.1016/j.gpb.2021.01.005. [Online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Glaeser SP, Doijad S, Hijazin M, Chakraborty T, Falsen E, et al. Varibaculum anthropi sp.nov. represented by three genetically different genomovars isolated from clinical material and emended description of the genus Varibaculum. Syst Appl Microbiol. 2016;39:546–52. doi: 10.1016/j.syapm.2016.09.002. [DOI] [PubMed] [Google Scholar]
- 30.Diop K, Andrieu C, Michelle C, Armstrong N, Bittar F, et al. Characterization of a new Ezakiella isolated from the human vagina: genome sequence and description of Ezakiella massiliensis sp.nov. Curr Microbiol. 2018;75:456–63. doi: 10.1007/s00284-017-1402-z. [DOI] [PubMed] [Google Scholar]
- 31.Majidzadeh M, Fatahi-Bafghi M. Current taxonomy of Rhodococcus species and their role in infections. Eur J Clin Microbiol Infect Dis. 2018;37:2045–62. doi: 10.1007/s10096-018-3364-x. [DOI] [PubMed] [Google Scholar]
- 32.Fall NS, Lo CI, Fournier PE, Sokhna C, Raoult D, et al. Arcanobacterium ihumii sp. nov., Varibaculum vaginae sp. nov. and Tessaracoccus timonensis sp. nov., isolated from vaginal swabs from healthy Senegalese women. New Microbes New Infect. 2019;31:100585. doi: 10.1016/j.nmni.2019.100585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mortaki D, Gkegkes ID, Psomiadou V, Blontzos N, Prodromidou A, et al. Vaginal microbiota and human papillomavirus: a systematic review. J Turk Ger Gynecol Assoc. 2020;21:193–200. doi: 10.4274/jtgga.galenos.2019.2019.0051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhang QF, Zhang YJ, Wang S, Wei Y, Li F, et al. The effect of screening and treatment of Ureaplasma urealyticum infection on semen parameters in asymptomatic leukocytospermia: a case-control study. BMC Urol. 2020;20:165. doi: 10.1186/s12894-020-00742-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stanislawski MA, Lozupone CA, Wagner BD, Eggesbø M, Sontag MK, et al. Gut microbiota in adolescents and the association with fatty liver: the EPOCH study. Pediatr Res. 2018;84:219–27. doi: 10.1038/pr.2018.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Younge NE, Araújo-Pérez F, Brandon D, Seed PC. Early-life skin microbiota in hospitalized preterm and full-term infants. Microbiome. 2018;6:98. doi: 10.1186/s40168-018-0486-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu XX, Jiao B, Liao XX, Guo LN, Yuan ZH, et al. Analysis of salivary microbiome in patients with Alzheimer's disease. J Alzheimers Dis. 2019;72:633–40. doi: 10.3233/JAD-190587. [DOI] [PubMed] [Google Scholar]
- 38.Altmäe S, Franasiak JM, Mändar R. The seminal microbiome in health and disease. Nat Rev Urol. 2019;16:703–21. doi: 10.1038/s41585-019-0250-y. [DOI] [PubMed] [Google Scholar]
- 39.Lundy SD, Sangwan N, Parekh NV, Selvam MK, Gupta S, et al. Functional and taxonomic dysbiosis of the gut, urine, and semen microbiomes in male infertility. Eur Urol. 2021;79:826–36. doi: 10.1016/j.eururo.2021.01.014. [DOI] [PubMed] [Google Scholar]
- 40.Mändar R, Punab M, Korrovits P, Türk S, Ausmees K, et al. Seminal microbiome in men with and without prostatitis. Int J Urol. 2017;24:211–6. doi: 10.1111/iju.13286. [DOI] [PubMed] [Google Scholar]
- 41.Vodstrcil LA, Twin J, Garland SM, Fairley CK, Hocking JS, et al. The influence of sexual activity on the vaginal microbiota and Gardnerella vaginalis clade diversity in young women. PLoS One. 2017;12:e0171856. doi: 10.1371/journal.pone.0171856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Egert M, Simmering R. The microbiota of the human skin. Adv Exp Med Biol. 2016;902:61–81. doi: 10.1007/978-3-319-31248-4_5. [DOI] [PubMed] [Google Scholar]
- 43.Zhernakova A, Kurilshikov A, Bonder MJ, Tigchelaar EF, Schirmer M, et al. Population-based metagenomics analysis reveals markers for gut microbiome composition and diversity. Science. 2016;352:565–9. doi: 10.1126/science.aad3369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Arweiler NB, Netuschil L. The oral microbiota. Adv Exp Med Biol. 2016;902:45–60. doi: 10.1007/978-3-319-31248-4_4. [DOI] [PubMed] [Google Scholar]
- 45.Dréno B, Araviiskaia E, Berardesca E, Gontijo G, Sanchez Viera M, et al. Microbiome in healthy skin, update for dermatologists. J Eur Acad Dermatol Venereol. 2016;30:2038–47. doi: 10.1111/jdv.13965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Magne F, Gotteland M, Gauthier L, Zazueta A, Pesoa S, et al. The firmicutes/bacteroidetes ratio: a relevant marker of gut dysbiosis in obese patients? Nutrients. 2020;12:1475. doi: 10.3390/nu12051474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Alfano M, Ferrarese R, Locatelli I, Ventimiglia E, Ippolito S, et al. Testicular microbiome in azoospermic men-first evidence of the impact of an altered microenvironment. Hum Reprod. 2018;33:1212–7. doi: 10.1093/humrep/dey116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lundy SD, Vij SC, Rezk AH, Cohen JA, Bajic P, et al. The microbiome of the infertile male. Curr Opin Urol. 2020;30:355–62. doi: 10.1097/MOU.0000000000000742. [DOI] [PubMed] [Google Scholar]
- 49.Mändar R, Punab M, Borovkova N, Lapp E, Kiiker R, et al. Complementary seminovaginal microbiome in couples. Res Microbiol. 2015;166:440–7. doi: 10.1016/j.resmic.2015.03.009. [DOI] [PubMed] [Google Scholar]
- 50.Chen H, Luo T, Chen T, Wang G. Seminal bacterial composition in patients with obstructive and non-obstructive azoospermia. Exp Ther Med. 2018;15:2884–90. doi: 10.3892/etm.2018.5778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Monteiro C, Marques PI, Cavadas B, Damião I, Almeida V, et al. Characterization of microbiota in male infertility cases uncovers differences in seminal hyperviscosity and oligoasthenoteratozoospermia possibly correlated with increased prevalence of infectious bacteria. Am J Reprod Immunol. 2018;79:e12838. doi: 10.1111/aji.12838. [DOI] [PubMed] [Google Scholar]
- 52.Mändar R, Türk S, Korrovits P, Ausmees K, Punab M. Impact of sexual debut on culturable human seminal microbiota. Andrology. 2018;6:510–2. doi: 10.1111/andr.12482. [DOI] [PubMed] [Google Scholar]
- 53.Gustafsson RJ, Ahrné S, Jeppsson B, Benoni C, Olsson C, et al. The Lactobacillus flora in vagina and rectum of fertile and postmenopausal healthy Swedish women. BMC Womens Health. 2011;11:17. doi: 10.1186/1472-6874-11-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.O’Callaghan J, O’Toole PW. Lactobacillus: host-microbe relationships. Curr Top Microbiol Immunol. 2013;358:119–54. doi: 10.1007/82_2011_187. [DOI] [PubMed] [Google Scholar]
- 55.Kroon SJ, Ravel J, Huston WM. Cervicovaginal microbiota, women's health, and reproductive outcomes. Fertil Steril. 2018;110:327–36. doi: 10.1016/j.fertnstert.2018.06.036. [DOI] [PubMed] [Google Scholar]
- 56.Lev-Sagie A, Goldman-Wohl D, Cohen Y, Dori-Bachash M, Leshem A, et al. Vaginal microbiome transplantation in women with intractable bacterial vaginosis. Nat Med. 2019;25:1500–4. doi: 10.1038/s41591-019-0600-6. [DOI] [PubMed] [Google Scholar]
- 57.Andam CP, Hanage WP. Mechanisms of genome evolution of Streptococcus. Infect Genet Evol. 2015;33:334–42. doi: 10.1016/j.meegid.2014.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Magri V, Wagenlehner FM, Montanari E, Marras E, Orlandi V, et al. Semen analysis in chronic bacterial prostatitis: diagnostic and therapeutic implications. Asian J Androl. 2009;11:461–77. doi: 10.1038/aja.2009.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ivanov IB, Kuzmin MD, Gritsenko VA. Microflora of the seminal fluid of healthy men and men suffering from chronic prostatitis syndrome. Int J Androl. 2009;32:462–7. doi: 10.1111/j.1365-2605.2008.00878.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.