Abstract
Background
Brain-derived neurotrophic factor (BDNF) is essential for neuronal survival, differentiation, development, and plasticity. Evidence suggests that fluctuations in peripheral levels (i.e., plasma or serum) of BDNF are associated with eating behaviors. Nevertheless, the findings are inconsistent. The purpose of this study is to determine if serum or plasma levels of BDNF are altered in individuals with eating disorders (EDs) compared to controls.
Methods
We conducted a systematic search of the core electronic medical databases from inception to March 2022 and identified observational studies that compared individuals with EDs to controls without EDs on serum or plasma levels of BDNF. R version 4.0.4 was used for all visualizations and calculations.
Results
The current meta-analysis comprised 15 studies that fulfilled the inclusion criteria. Subjects with EDs (n = 795) showed lower BDNF levels compared to non-EDs controls (n = 552) (SMD: − 0.49, 95% CI [− 0.89; − 0.08], p-value = 0.01). Moreover, subgroup analysis was conducted based on the specimen (plasma and serum), which revealed no statistically significant difference in the levels of BDNF between the two subgroups (p-value = 0.92). Additionally, meta-regression results revealed that publication year, mean age of the individuals with EDs, NOS scores, and the number of individuals with EDs collectively accounted for 25.99% percent of the existing heterogeneity.
Conclusion
Lower BDNF levels are associated with EDs.
Supplementary Information
The online version contains supplementary material available at 10.1186/s40337-022-00630-w.
Keywords: Brain-derived neurotrophic factor, BDNF, Eating disorder, Anorexia nervosa, Bulimia nervosa, Binge eating disorder
Plain english summary
Brain-Derived Neurotrophic Factor, or BDNF for short, is one of the proteins in the body that regulates many functions of the brain, including how it develops and how its structure changes during its life. Neuropsychiatric disorders, including EDs, have been associated with changes in the amount of this protein in the body; but this is difficult to determine from one or two studies alone. In this review, we gathered information about the blood levels of BDNF in people suffering from ED and healthy people from several studies and compared them. This analysis showed that BDNF is lower in patients with ED. The significance of our review is that it might help understand the factors implicated in development of ED. It might also guide future studies to investigate decide whether BDNF can be used to predict ED relapse or remission.
Background
Eating disorders (EDs) are a heterogeneous group of conditions defined by pathological eating habits that are linked with weight changes and/or social behaviors that have a major impact on a person's quality of life and ability to function socially [1, 2]. In this context, “disordered eating” refers to difficulty maintaining a healthy weight and/or body image, such as persistent dieting and weight concerns [3]. Concordantly, weight, diet, and negative body image concerns all contribute to the risk factors for ED [4]. Anorexia nervosa (AN), bulimia nervosa (BN), and binge eating disorder (BED) are three of the most common EDs with lifetime prevalence rates of 0.5–1%, 1–3%, and 2–2.5%, respectively [5].
Studies have shown that people at risk of developing EDs are also more likely to have co-occurring psychological issues such as anxiety, depression, and insomnia [3], possibly hinting to an overlap of pathology between these disorders. In addition, people with ED may develop serious somatic symptoms (e.g., pain, shortness of breath, fatigue or weakness), and report a decreased general well-being and quality of life [6], increasing their risk of suicide [7] and death rates [8, 9].
Brain-derived neurotrophic factor (BDNF) is a neurotrophin that plays a critical role in activity-dependent neuronal plasticity [10, 11] with a significant effect on neuronal morphology and physiology, enhancing neurite sprouting and synaptic stability, as well as long-term potentiation [11]. BDNF may be produced by different cell types in the body, including vascular structures, the immune system, neurons, and glial cells [12–14]. It can be measured in plasma or blood, and might reflect CNS levels of the molecule [15–17].
BDNF has been strongly implicated as one of the important regulators of eating behavior and its disturbances are associated with EDs [18, 19]. For instance, animal studies have shown that knockouts of BDNF induce hyperphagia and obesity [20], and BDNF administration decreases food intake, increases energy expenditure, and reduces body weight [21, 22]. Moreover, the hypothalamus and the dorsal vagal complex, two major autonomic centers believed to regulate eating behavior and energy balance, show high levels of expression of BDNF and its receptor [21].
Several studies have successfully linked polymorphisms of the BDNF gene to EDs [23–25]. Systematic reviews and meta-analyses have found positive correlations between decreased circulating BDNF levels and disordered eating [26, 27] and other psychiatric conditions [28]. Most of these studies are genetic studies, and those that analyze circulating levels of BDNF are either carried out in regard to one type of ED, or are outdated. In this context, this systematic review and meta-analysis aims to analyze the plasma or serum BDNF concentrations in individuals with different types of ED compared to controls according to the most recent literature, in order to explore the utility of BDNF measurements in diagnosis, classification, and prognosis of EDs. Possible associations between BDNF and the type of ED are also investigated.
Material and methods
The current systematic review and meta-analysis was developed according to The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA 2020) guideline [29].
Literature search and selection criteria
MEDLINE, Scopus, EMBASE, and Web of Science databases were searched online till May 16th, 2022, accordingly, to retrieve relevant investigations. In addition to searching electronic databases, we also verified the reference list of all pertinent publications already retrieved. Our search strategy is depicted in the supplementary material (Additional file 1). Titles and abstracts were screened independently by two authors (PM and AK), and a third reviewer (SB) resolved the conflicts in screening.
There were two criteria for inclusion: (1) A study was designed as an observational one, measuring BDNF levels in individuals with EDs (AN, BN, BED) without any other neurological or neuropsychiatric disorders; and (2) The article provided sufficient data, including the total number of subjects in both ED and controls, as well as mean and standard deviation (SD) of BDNF levels. Also, no restrictions for language were applied.
Data extraction
The following data were extracted from each included article by one author (PM): (1) first author, year of publication, country of study, the assay used to measure BDNF levels, the type of specimen (serum, plasma, or blood), the number of subjects in the ED (e.g., AN, BN, BED) and control groups, the demographic characteristics of people with EDs and controls (e.g., age and gender), the mean and SD of BDNF levels in both the affected individuals and control groups, and the measurement scale used to calculate BDNF levels (e.g., pg./mL, ng/mL, or ng/mg).
Quality assessment and risk of bias
The quality of included studies was assessed using the Newcastle–Ottawa scale (NOS), which was developed for observational studies. The NOS is constructed to evaluate three major features of observational studies: sample selection, case–control comparability, and exposure. Scores on this scale range from 0 to 9 [30]. Studies with a star rating of 7–9 were considered of the best quality, a rating of 4–6 stars a poor quality, and a rating of fewer than four the lowest quality [31]. Two authors (SB and PM) independently evaluated the quality of the included studies using the NOS. Different checklists were used based on the study design.
Quantitative analysis
R version 4.0.4 (R Core Team [2020]. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria) was used for all calculations and visualizations. "meta" (version 4.17–0), "metafor" (version 2.4–0), "dmetar" (version 0.0–9), and "tidyverse" were utilized (version 1.3.0). R was used to create all forest and the drapery plots. Statistical significance was defined as a p-value of < 0.05.
The effect size was quantified using the standardized mean difference (SMD). The analytical model was composed of fixed effects and random effects, interchangeably. If the values reported in the manuscript were expressed as a median and interquartile range (IQR) or median and range and we were unable to obtain the mean and standard deviation (SD) from the authors, we converted these values using the statistical methods suggested by Luo et al. [32] and Wan et al. [33]. The Q statistic and the I2 index were used to determine heterogeneity. According to Cochrane standards, an I2 < 40% value indicates that inconsistency across studies is not significant. We intended to utilize the fixed effects model in this instance. If the I2 estimates varied by more than 40%, we expected to analyze using the random effects technique. To further elucidate the sources of heterogeneity, we performed a sensitivity analysis on meta-analyses with substantial heterogeneity, including ten or more papers. We removed one study each time and recalculated the effect size (Leave-One-Out Analyses).
The degree of asymmetry in the funnel plot and Egger's test [34] are used to identify publication bias. Indeed, funnel plots are often used to visually reveal publication bias. By contrast, the Egger's test is an objective statistic that enables users to validate visual cues provided by funnel plots. When there was evidence of publication bias, we used the trim-and-fill procedure to adjust the effect sizes [35].
Results
Selection of studies
The search strategy retrieved a total yield of 1,308 studies. After removing the duplicates, 745 studies remained. The screening identified 32 potentially eligible studies, and 14 original studies met the criteria to be included in the meta-analysis. No further studies that were appropriate for inclusion were identified via hand searching and checking the references. Figure 1 illustrates the process of study selection according to the PRISMA guidelines.
Fig. 1.
Flow diagram summarizing the selection of eligible studies based on the PRISMA guidelines
Study characteristics & major findings of the included studies
Table 1 demonstrates the basic characteristics of the included studies in the meta-analysis. Levels of BDNF were measured in 14 studies from 2002 to 2022, all of which included control groups. 1,454 total observations, including 722 cases and 466 controls, were retrieved from the included studies. A total female predominancy was observed among the subjects with a 1188 to 0 female to male ratio. All the studies reported findings on one of the ED types, either Anorexia Nervosa (AN) or Bulimia Nervosa (BN). Regarding the four studies with longitudinal designs, the baseline levels of BDNF were analyzed [36–39]. The overall standardized mean difference (SMD) between ED individuals and the controls was − 0.49 [ − 0.0.9–0.08] (Fig. 2).
Table 1.
Baseline Characteristics of Included Studies
| Study ID | Patients | Controls | Main significant findings | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Author, Year | Country | Study design | BDNF measurement method | Source (serum, plasma) | No. (Type of ED) | Diagnostic Criteria | BDNF levels (mean ± SD), ng/ml |
No | BDNF levels (mean ± SD), ng/ml |
|
| Nakazato et al., 2002 | Japan | Cross-sectional | BDNF Emax Immunoassay System kit (Promega, Madison, WI) | Serum | 12 (AN-R, AN-BP) | DSM-IV | 24.9 ± 6.75 | 21 | 61.4 ± 19.5 |
Lower BDNF levels in AN and BN patients compared to controls Lower BDNF levels in AN patients compared to BN patients Positive correlation between BDNF levels and BMI in all subjects |
| Nakazato et al., 2002 | Japan | Cross-sectional | BDNF Emax Immunoassay System kit (Promega, Madison, WI) | Serum | 18 (BN) | DSM-IV | 38.4 ± 15.3 | 21 | 61.4 ± 19.5 | |
| Nakazato et al., 2006 | Japan | Longitudinal | BDNF Emax Immunoassay System kit (Promega, Madison, WI, USA) | Serum | 13 (AN-R, AN-BP) | DSM-IV | 14.5 ± 4.4 | 17 | 14.5 ± 4.4 |
Lower BDNF levels in AN patients compared to controls No difference in BDNF levels in AN patients before and after partial weight recovery Positive correlation between BDNF levels and ED symptom scores (EDI-2) in all subjects Positive correlation between BDNF levels and BMI in all subjects |
| Nakazato et al., 2009 | Japan | Cross-sectional | Emax Immunoassay System kit (Promega, Madison, WI, USA) | Serum | 29 (AN-R, AN-BP) | DSM-IV | 11.7 ± 4.9 | 28 | 15.1 ± 5.5 |
Lower BDNF levels in AN patients compared to controls Lower BDNF levels in AN patients compared to patients who recovered from AN Higher rate of set-shifting errors (WCST) in AN patients No correlation between BDNF levels and WCST performance |
| Yamada et al., 2012 | Japan | Cross-sectional and longitudinal | ELISA kit (Quantikine, R & D Systems, Minneapolis, MN, USA) | Plasma | 16 (BN) | DSM-IV | 1.89 ± 1.67 | 10 | 6.57 ± 6.09 |
Lower BDNF levels in BN patients compared to controls Increased BDNF levels following inpatient treatment, suggesting that lower BDNF in BN is associated with abnormal eating behaviors, especially binge eating |
| Dmitrzak-Weglarz et al., 2013 | Poland | Cross-sectional | DuoSet ELISA Development Kits (R&D Systems) – | Serum | 46 (AN-R) | ICD-10 and DSM-IV | 23.72955 ± 8.245963 | 45 | 22.22206 ± 5.938468 |
No difference in BDNF levels in AN patients compared with controls No correlation between BDNF levels and BMI or severity of depression symptoms (BDI) in all subjects Correlations between BDNF levels and patient personality dimensions (TCI) |
| Dmitrzak-Weglarz et al., 2013 | Poland | Cross-sectional | DuoSet ELISA Development Kits (R&D Systems) – | Serum | 14 (AN-BP) | ICD-10 and DSM-IV | 23.32821 ± 8.078747 | 45 | 22.22206 ± 5.938468 | |
| Zwipp et al., 2014 | Germany | Cross-sectional and longitudinal | Enzyme-Linked Immunosorbent Assay kits (ELISA; 181 Promega Inc., Madison, WI, USA) | Serum | 55 (AN) | DSM-IV | 6.6165 ± 3.4158 | 52 | 6.7008 ± 2.7814 |
Higher BDNF levels in patients who recovered from AN compared to acutely underweight AN patients Increased BDNF levels with short-term weight gain in acutely underweight AN patients Inverse association of BDNF with psychomotor speed (TMT) in acutely underweight AN patients but not in controls Acutely underweight AN patients with higher BDNF also had lower lifetime BMI, indicating that serum BDNF levels in patients with AN vary with the stage of illness Changes in BDNF levels may have different context-dependent effects, including the modulation of cognitive functioning in acutely underweight patients; as BDNF has pleiotropic functions |
| Eddy et al., 2015 | USA | Cross-sectional | immunoassay (ELISA, R&D Systems, Inc) | Serum | 50 (AN-R) | DSM-V | 13.6 ± 0.9 | 22 | 14.6 ± 0.8 |
Higher BDNF levels in AN-BP than AN-R No difference in BDNF levels in AN-BP compared to AN-R after controlling for BMI No difference in BDNF levels in AN patients compared to controls No correlation between BDNF levels and BMI in all subjects Positive association between BDNF levels and frequency of purging in all subjects |
| Eddy et al., 2015 | USA | Cross-sectional | immunoassay (ELISA, R&D Systems, Inc) | Serum | 25 (AN-BP) | DSM-V | 17.2 ± 1.5 | 22 | 14.6 ± 1.4 | |
| Homan et al., 2015 | Switzerland | Randomized, double-blind, placebo-controlled, crossover study | BDNF Emax Immunoassay Kit (Promega, Switzerland) | Plasma | 20 (Remitted BN) | DSM-IV | 3.058 ± 1.5066 | 27 | 2.383 ± 1.2814 |
Positive correlation between AMPT–induced differences in BDNF levels with the AMPT–induced differences in reward learning across sample Higher BDNF levels in patients with remitted BN compared to controls across conditions Higher BDNF levels in the morning before compared with after a standardized breakfast across groups and conditions |
| Rybakowski et al., 2017 | Poland | Longitudinal | n/a | Serum | 76 (AN) | n/a | 28.94 ± 7.19 | 30 | 34.66 ± 7.4 |
Lower BDNF levels in acute AN Normalization of BDNF levels after weight recovery in AN Negative correlation between BDNF levels and body weight in acute AN but not AN after partial weight recovery No correlation between BDNF levels and psychopathological symptoms (HDRS, BDI and YBOCS) in either acute AN or AN after partial weight recovery No evidence found to support a role of serum BDNF levels in the modulation of depressive and obsessive–compulsive symptoms of AN |
| Matsumoto et al., 2017 | Japan | Cross-sectional | Human BDNF ELISA kits (Aviscera Bioscience, Santa Clara, CA, USA) | Serum | 19 (AN-R, AN-BP) | DSM-IV | 13.96 ± 6.02 | 22 | 16.58 ± 3.5 |
No difference in proBDNF and mBDNF levels among AN patients, BN patients, and controls Correlation between proBDNF and MMP-9 levels in both ED patients and controls Positive correlation between mBDNF levels and IGT performance in BN patients but not in AN patients |
| Matsumoto et al., 2017 | Japan | Cross-sectional | Human BDNF ELISA kits (Aviscera Bioscience, Santa Clara, CA, USA) | Serum | 28 (BN) | DSM-IV | 14.99 ± 4.9 | 22 | 12.57 ± 12.54 | |
| Mancuso et al., 2020 | USA | Cross-sectional | ELISA (EMD Millipore: Billerica, MA) | Serum | 36 (AN-R, AN-BP) | K-SADS PL and EDE | 2.7313 ± 0.4153 | 32 | 3.7928 ± 0.4575 |
Lower fasting BDNF levels in AN patients compared with controls Lower BDNF AUC after breakfast in AN patients compared with controls Positive association between BDNF AUC and kilocalories consumed during CTT in AN patients (particularly AN-R) |
| Tyszkiewicz-Nwafor et al., 2020 | Poland | Longitudinal | BDNF DuoSet (cat. No DY 248) and TrkB DuoSet (cat. No DY 397–5) ELISA Development Kit (R&D System, Minneapolis, MN, USA) | Serum | 42 (AN) | ICD-10, DSM-IV and DSM-V | 28.66 ± 6.7 | 30 | 34.66 ± 7.4 |
Increased BDNF levels in AN patients after partial weight recovery compared with before, but lower levels compared with controls at two-time points Negative correlation between BDNF levels and the severity of ED symptoms (EAT-26) No correlation between BDNF levels and depressive and obsessive–compulsive symptoms (HDRS, BDI, YBOCS) for either malnourished patients or partially weight recovered AN patients |
| Borsdorf et al., 2021 | Germany | Longitudinal | Quantikine ELISA (R&D Systems Inc.) | Serum | 149 (AN) | DSM-IV | 17.36 ± 6.57 | 79 | 14.08 ± 0.75 |
Lower BDNF levels in AN patients at admission compared with controls Continuous increase in BDNF levels, reaching supranormal levels at 2.5-year follow-up Inverse association between BDNF levels with ED psychopathology (BDI-II, SCAS, MROAS, SIAB-EX) at discharge Positive association between BDNF levels with previous weight gain at 1-year follow-up |
| Keeler et al., 2022 | UK | Cross-sectional | U-PLEX Human BDNF assay (Meso Scale Discovery, Maryland, USA) | Serum | 56 (AN-R, AN-BP) | DSM-V | 5.354 ± 2.616 | 51 | 8.323 ± 2.595 |
Lower BDNF levels in AN patients compared to controls and patients recovering from AN Negative association of BDNF with depression and ED psychopathology in the whole sample, but not in AN patients BDNF serum concentrations may be a state marker of AN, but do not reflect symptom severity In acute AN, BDNF levels seem to be linked to TNF-α signaling |
BDNF: Brain-Derived Neurotrophic Factor; proBDNF: precursor Brain-Derived Neurotrophic Factor; mBDNF: mature Brain-Derived Neurotrophic Factor; ED: Eating Disorder; AN: Anorexia Nervosa; BN: Bulimia Nervosa; AN-R: Anorexia Nervosa Restricting subtype; AN-BP: Anorexia Nervosa Binge-eating/Purging subtype; YFAS: Yale Food Addiction Scale; ELISA: Enzyme-Linked Immunosorbent Assay; BMI: Body Mass Index; DSM: Diagnostic and Statistical Manual of Mental Disorders; ICD: International Classification of Diseases; K-SADS PL: Schedule for Affective Disorders and Schizophrenia for School Age Children-Present and Lifetime Version; EDE: Eating Disorder Examination; HDRS: Hamilton Depression Rating Scale; BITE: Bulimic Investigatory Test, Edinburgh; EDI: Eating Disorder Inventory; WCST: Wisconsin Card Sorting Test; TCI: Temperament and Character Inventory; TMT: Trail Making Test; AMPA: Alpha-methyl-para-tyrosine; MMP: Matrix Metalloproteinase; IGT: Iowa Gambling Task; SNP: Single Nucleotide Polymorphism; AUC: Area Under Curve; CTT: Cookie Taste Test; EAT: Eating Attitudes Test; BDI: Beck Depression Inventory; YBOCS: Yale-Brown Obsessive–Compulsive Scale; SCAS: Spence Children’s Anxiety Scale; MROAS: Morgan–Russell Outcome Assessment Schedule; SIAB-EX: Structured Interview for Anorexia and Bulimia-Expert Interview
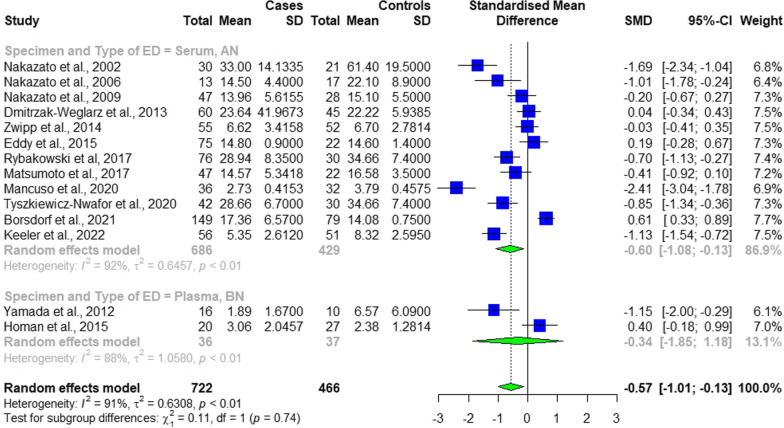
Fig. 2.
The forest plot of the subgroup analysis based on the specimen and type of ED, denoting a statistically significant difference in the level of BDNF between participants with and without eating disorder, but not between the two subgroups
Except for four studies [37, 40–42], all the other included ones reported a negative association between the level of BDNF and the presence of any type of eating disorders, meaning the levels of BDNF was lower among ED individuals compared to healthy controls (Table 1). None of the four studies reported the opposite recruited sex-matched controls. In fact, except for Borsdorf et al. [37] study, having age-matched controls, the other three studies did not provide information on the detailed characteristics of their control groups.
The methodological quality of studies
In the present study, nine studies achieved above 6 stars, six studies achieved 6 stars, and one study achieved 5 stars (Table 2). The median NOS score for included studies was 6.57 (IQR = 1, mean ± SD = 6.57 ± 0.75, range: 5–8) out of 9, which shows an estimated moderate to good quality. One study (7.14%) [43] had high risks of bias (scores 0–5), twelve studies (85.71%) [36, 38–42, 44–48] had moderate [34, 39] risks of bias (scores 6–7), and one study (7.14%) [37] had low risks of bias (scores 8–9) in their methodological quality (Table 2).
Table 2.
Quality assessment of the included studies based on the NOS checklist (adapted for cross sectional studies)
| Author, Year | QUESTION 1 | QUESTION 2 | QUESTION 3 | QUESTION 4 | QUESTION 5 | QUESTION 6 | QUESTION 7 | Overall |
|---|---|---|---|---|---|---|---|---|
| Nakazato et al., 2002 | * | * | * | ** | * | * | 7 | |
| Nakazato et al., 2006 | * | * | ** | * | * | 6 | ||
| Nakazato et al., 2009 | * | * | * | ** | * | * | 7 | |
| Yamada et al., 2012 | * | * | * | * | * | 5 | ||
| Dmitrzak-Weglarz et al., 2013 | * | * | * | ** | * | * | 7 | |
| Zwipp et al., 2014 | * | * | * | * | * | * | 6 | |
| Eddy et al., 2015 | * | * | * | ** | * | * | 7 | |
| Homan et al., 2015 | * | * | ** | * | * | 6 | ||
| Rybakowski et al., 2017 | * | * | * | * | ** | * | 7 | |
| Matsumoto et al., 2017 | * | * | * | ** | * | * | 7 | |
| Mancuso et al., 2020 | * | * | * | ** | * | * | 7 | |
| Tyszkiewicz-Nwafor et al., 2020 | * | * | * | * | * | * | 6 | |
| Borsdorf et al., 2021 | * | * | * | * | ** | * | * | 8 |
| Keeler et al., 2022 | * | * | * | ** | * | 6 |
Selection: Questions 1 to 4, Comparability: Question 5, Outcome: Questions 6 and 7
*, ** The NOS checklist uses a "star system" to assess the quality of studies, with the number of stars indicating the overall score in that particular domain, i.e., Selection, Comparability, and Outcome
Comparison of BDNF Levels between Individuals with EDs and Controls
In all studies, levels of BDNF were compared between individuals with EDs (N = 722) and controls (N = 466). The cumulative number of female and male participants was 1188 and 0, respectively. The mean age was 19.99 ± 6.8 and 22.15 ± 8.48 for participants with EDs and controls, respectively.
A statistically significant difference was observed comparing the levels of BDNF between participants with EDs and controls (SMD − 0.5667, 95% CI [ − 1.0067; − 0.1267], p-value = 0.0116, Fig. 2). Two sets of subgroup analysis were conducted:
First, based on the specimen (plasma and serum), which revealed that there was not a statistically significant difference in the levels of BDNF between the two subgroups (p-value = 0.7425, Fig. 2).
Second, based on ED type. As such, studies were categorized into two subgroups based on the type of EDs that studies’ sample size had: Bulimia Nervosa (BN) and Anorexia Nervosa (AN), and Obesity Associated with ED. This analysis demonstrated that there was not a statistically significant difference between the two subgroups (p-value = 0.7425, Fig. 2).
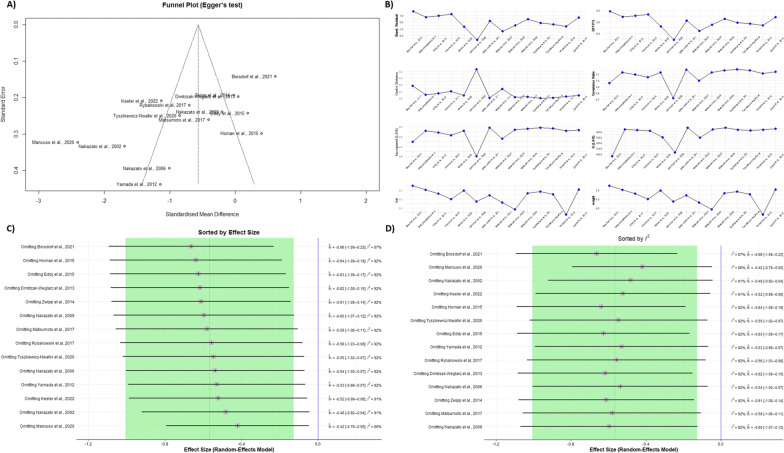
Between-study heterogeneity
The Eggers’ test did not indicate the presence of substantial funnel plot asymmetry (p-value = 0.0100, Fig. 3A). The between-study heterogeneity was statistically significant (p-value = < 0.0001). Its variance was estimated at τ2 = 0.6308 [0.2969; 1.7793], with an I2 value of 91.2% [86.9%; 94.0%]. The prediction interval ranged from g = − 2.3650 to 1.2317, indicating that negative intervention effects cannot be ruled out for future studies (Fig. 3B).
Fig. 3.
A The funnel plot showing no evidence of publication bias, statistically supported by Egger’s regression test. B The influence analysis plot, showing different influence diagnostics including: Externally Standardized Residuals, DFFITS Value, Cook’s Distance, Covariance Ratio, Leave-One-Out τ2 and Q Values, and Hat Value and Study Weight. Ceave-One-Out sensitivity analysis result, sorted by effect sizes from low to high. D Leave-One-Out sensitivity analysis result, sorted by heterogeneity as measured by I2 from low to high
Outliers’ identification and sensitivity analysis
An influence analysis was done to detect any influential cases, which identified three studies as outliers [37, 44, 46], and the p-value raised from 0. 0116 to 0.0118. Consequently, we conducted a sensitivity analysis to identify whether the influential cases have affected the significancy level of the meta-analyses. To do so, each time, we omitted one study and recalculated the effect size (leave-one-out analysis). Sensitivity analysis showed that the effect size remained significant after omitting each study (Fig. 3C, D).
Univariate and multivariate meta-regression analysis
To identify the source of heterogeneity, a meta-regression analysis was conducted. Number of individuals with EDs, the year of publication, and the mean age of ED individuals accounted for 24.56, 49.99, and 84.39 percent of heterogeneity, respectively. On the other hand, the NOS scores of the included studies did not play a part in the observed heterogeneity of the data per se. A multivariate meta-regression analysis was done to rule out the existence of any possible overlaps between the number of individuals with EDs and the other three mentioned variables that did not contribute as much to the heterogeneity, revealing publication year and the number of individuals with EDs contributed to 34.37 percent of the heterogeneity, NOS scores and number of individuals with EDs contributed to 42.58 percent of the heterogeneity, and mean age of individuals with EDs and their sample size contributed to 51.41 percent of the heterogeneity. Finally, all the four variables including publication year, mean age of the individuals with EDs, NOS scores, and the number of individuals with EDs collectively accounted for 66.8 percent of heterogeneity in the data (Table 3).
Table 3.
Meta − regression of BDNF levels in persons with EDs and healthy controls
| Moderator | No. of comparisons | No. of subjects | Meta-regression | R2 analog (proportion of variance explained) | ||||
|---|---|---|---|---|---|---|---|---|
| ED | HC | Estimated Intercept | 95% CI | p-value | ||||
| No. of persons with EDs | 14 | 722 | 466 | − 1.2303 | − 1.9597 | − 0.5009 | 0.0331 | 24.56% |
| Age (mean, years) | 14 | 722 | 466 | 0.6128 | − 0.0624 | 1.2880 | < 0.0001 | 84.39% |
| Publication year | 14 | 722 | 466 | − 1.6911 | − 2.9995 | − 0.3826 | 0.0013 | 46.99% |
| NOS score | 14 | NA | NA | − 1.1455 | − 2.9337 | 0.6426 | 0.4344 | 0.00% |
| All moderators combined (Multiple Meta − Regression) | 13 | NA | NA | 51.8716 | − 157.1692 | 260.9124 | 0.1098 | 66.80% |
Discussion
To the best of our knowledge, the current study is the first systematic review and meta-analysis comparing the levels of BDNF in people with eating disorders (EDs) to people without a history of EDs. The main finding of our study is that BDNF levels are significantly lower among individuals with EDs compared to healthy controls. Previous systematic reviews assessed the levels of BDNF in individuals with AN [24, 27, 47] and BN [26] separately, showing that levels of BDNF are lower among affected individuals. Given the dynamic nature of EDs, our study takes a more comprehensive approach and compares: First, persons with EDs of any kind to healthy controls; Second, the discrepancies in the levels of BDNF between different types of ED.
Our findings demonstrate that people with EDs generally have a lower level of serum and plasma BDNF compared to healthy controls. Several hypotheses can be proposed to explain lower BDNF blood levels in people with EDs. Since BDNF plays a crucial role in the nervous system's growth, regulation, and maintenance, its level alterations can affect neurological functions, including hunger and satiety, both directly and via indirect pathways [49, 50]. Both of these pathways can eventually lead to disturbances in eating habits and give rise to respective disorders. Previous research has provided a large amount of evidence emphasizing BDNF’s control of feeding, with specific attention to the central effects [51]. Nevertheless, BDNF levels might also reflect other pathophysiological mechanisms associated with EDs and be secondary to other underlying factors.
Regarding the direct pathway by which decreased BDNF levels mediate disruption of eating habits, it has been suggested that single nucleotide polymorphisms (SNPs) in the BDNF gene increase the susceptibility to the development of binge eating disorder, and people with EDs have an amplified level of genetically-altered BDNF molecules. Such functional polymorphisms are often associated with lower blood levels of BDNF. Due to the high prevalence of this specific mutation, it has been more examined than other BDNF gene SNPs, specifically regarding weight regain. In a study conducted by Nonino et al., the detection of allele frequency of rs6265 SNP in the BDNF gene indicated an elevated risk for the development of BED in individuals with relapse to obesity in the postoperative period of bariatric surgery [52]. Not only is it presumed that an association between the frequency of SNPs within the BDNF gene and the risk of ED onset exists, but it has also been suggested that such polymorphisms can contribute to episodes of EDs exacerbations in people already diagnosed with EDs. Montelenoe et al. have also demonstrated that the rs6365 polymorphism of the BDNF gene is significantly associated with binge eating behavior in women with bulimia nervosa or binge eating disorder [53]. This is particularly important in designing more efficient treatment plans to battle ED.
BDNF levels can alter neuronal function in an indirect manner as well. A growing body of evidence suggests that BDNF is involved in depression, as its levels are significantly reduced in depressed individuals [54]. As such, lower BDNF levels raises the vulnerability to depression, with which eating disorder frequently co-exist as they share common biological mechanisms [55, 56]. Furthermore, it has been shown that antidepressant agents up-regulate the expression of the BDNF gene [55, 57]. Therefore, the assumption that dysregulated levels of BDNF can indirectly, using depression as a mediator, put individuals at higher risk for developing EDs is further confirmed.
Recent findings have also provided evidence in favor of the interplay between BDNF, insulin, insulin’s counter-regulatory hormones, including catecholamines, and leptin levels in people with EDs [58]. They suggest that leptin and BDNF levels are sensitive to the depletion of catecholamine reserve. Under physiological circumstances, exhaustion of catecholamine stores in the body, such as the pre-prandial situations, causes the BDNF levels to fall drastically and then surge again once the individual is in a postprandial state inducing appetite suppression [42]. In people with EDs, the above mechanism loses sensitivity to catecholamine depletion and shows more preference towards the pre-prandial states, leading to significantly lower levels of BDNF, which can, in turn, initiate the downstream cascade of pathological dysregulations observed in ED conditions.
As mentioned earlier in the discussion, not only do disrupted BDNF levels give rise to the occurrence of EDs, they can impact the severity of their symptoms [36]. Additionally, recent studies suggest that on a hypothetical spectrum of disordered eating behaviors, individuals with more extreme symptoms had significantly lower BDNF levels as well [18, 41]. Further research is required to determine whether there is a causal relation between BDNF levels and the severity of symptoms or whether they are both secondary to another underlying factor contributing to the disorder's pathophysiology.
One interesting aspect of the present study is that it suggests persons with EDs, regardless of their exact type, do not differ much in terms of BDNF levels. This is contrary to the findings of some of the included studies and may, in part, be due to the larger sample sizes of those included studies whose findings were in line with the above argument.
The present study has some strengths and limitations that merit comment. It is the first meta-analysis comparing the level of BDNF in individuals across the eating disorder spectrum to healthy controls. It sheds some light on the importance of BDNF as a member of the neurotrophin family of growth factors as an underlying attributable risk factor for eating disorders. However, there are some limitations, too. Further research is required to estimate the prevalence of depression and BDNF levels simultaneously to depict a more detailed picture of the interplay between depression and BDNF levels in the context of eating disorders, and to reach a clear understanding of the delicate interactions between BDNF levels and the entire nervous system to unravel the full scope of physiological, biochemical, and even anatomical influences this factor has on hunger regulation. Also, due to the lack of information in included studies, we were unable to subgroup the findings based on the applied diagnostic methods, which could lead to more precise results or even illuminate possible sources of bias. Another notable limitation could be the fact that all the individuals in the included studies are female. This hinders our ability to reach generalizable findings and also to perform a meta-regression analysis with sex as one of the variables since it has only of class of item.
Conclusion
This study showed that lower levels of blood BDNF are associated with the presence of EDs. Whether or not a causative relationship exists between the two phenomena is a question for further research to address. Considering the burden of EDs mentioned in previous studies and the possible role of altered BDNF levels in the onset and progression of EDs, interventions targeting the restoration of BDNF level to normal are deemed beneficial in the affected people.
Supplementary Information
Additional file 1. Summary of search strategies customized for each data bank.
Acknowledgements
Not applicable
Abbreviations
- AN
Anorexia nervosa
- BDNF
Brain-derived neurotrophic factor
- BED
Binge eating disorder
- BN
Bulimia nervosa
- CNS
Central nervous system
- EDs
Eating disorders
- NOS
Newcastle–Ottawa scale
- RAN
Restricting type anorexia nervosa
- SNPs
Single nucleotide polymorphisms
Author contributions
PS: drafting of the manuscript/ study conception and design/ data acquisition, SB: drafting of the manuscript/ analysis and data interpretation, PM: data acquisition/ critical revision, AK: data acquisition, OM and AT: critical revision, NR: study conception and design/ critical revision. All authors read and approved the final manuscript.
Funding
Not applicable.
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Parnian Shobeiri, Sara Bagherieh and Parsa Mirzayi have contributed equally
References
- 1.Hay P, et al. Burden and health-related quality of life of eating disorders, including avoidant/restrictive food intake disorder (ARFID), in the Australian population. J Eat Disord. 2017;5(1):1–10. doi: 10.1186/s40337-017-0149-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pohjolainen V, et al. Long-term health-related quality of life in eating disorders. Qual Life Res. 2016;25(9):2341–2346. doi: 10.1007/s11136-016-1250-5. [DOI] [PubMed] [Google Scholar]
- 3.Aspen V, et al. Psychiatric co-morbidity in women presenting across the continuum of disordered eating. Eat Behav. 2014;15(4):686–693. doi: 10.1016/j.eatbeh.2014.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stice E, et al. An 8-year longitudinal study of the natural history of threshold, subthreshold, and partial eating disorders from a community sample of adolescents. J Abnorm Psychol. 2009;118(3):587–597. doi: 10.1037/a0016481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Edition F. Diagnostic and statistical manual of mental disorders. Am Psychiatric Assoc. 2013;21:591–643. [Google Scholar]
- 6.Sanftner JL. Quality of life in relation to psychosocial risk variables for eating disorders in women and men. Eat Behav. 2011;12(2):136–142. doi: 10.1016/j.eatbeh.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 7.Keski-Rahkonen A, Mustelin L. Epidemiology of eating disorders in Europe: prevalence, incidence, comorbidity, course, consequences, and risk factors. Curr Opin Psychiatry. 2016;29(6):340–345. doi: 10.1097/YCO.0000000000000278. [DOI] [PubMed] [Google Scholar]
- 8.Smink FR, Van Hoeken D, Hoek HW. Epidemiology of eating disorders: incidence, prevalence and mortality rates. Curr Psychiatry Rep. 2012;14(4):406–414. doi: 10.1007/s11920-012-0282-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arcelus J, et al. Mortality rates in patients with anorexia nervosa and other eating disorders: a meta-analysis of 36 studies. Arch Gen Psychiatry. 2011;68(7):724–731. doi: 10.1001/archgenpsychiatry.2011.74. [DOI] [PubMed] [Google Scholar]
- 10.Park H, Poo M-M. Neurotrophin regulation of neural circuit development and function. Nat Rev Neurosci. 2013;14(1):7–23. doi: 10.1038/nrn3379. [DOI] [PubMed] [Google Scholar]
- 11.Zagrebelsky M, Korte M. Form follows function: BDNF and its involvement in sculpting the function and structure of synapses. Neuropharmacology. 2014;76:628–638. doi: 10.1016/j.neuropharm.2013.05.029. [DOI] [PubMed] [Google Scholar]
- 12.Braun A, et al. Cellular sources of enhanced brain-derived neurotrophic factor production in a mouse model of allergic inflammation notice to professional recruitment and announcement advertisers. Am J Respir Cell Mol Biol. 1999;21(4):537–546. doi: 10.1165/ajrcmb.21.4.3670. [DOI] [PubMed] [Google Scholar]
- 13.Karege F, Schwald M, Cisse M. Postnatal developmental profile of brain-derived neurotrophic factor in rat brain and platelets. Neurosci Lett. 2002;328(3):261–264. doi: 10.1016/s0304-3940(02)00529-3. [DOI] [PubMed] [Google Scholar]
- 14.Le Blanc J, et al. Platelets selectively regulate the release of BDNF, but not that of its precursor protein, proBDNF. Front Immunol. 2020 doi: 10.3389/fimmu.2020.575607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Teixeira AL, et al. Circulating levels of brain-derived neurotrophic factor: correlation with mood, cognition and motor function. Biomark Med. 2010;4(6):871–887. doi: 10.2217/bmm.10.111. [DOI] [PubMed] [Google Scholar]
- 16.Woods SP, et al. Brain-derived neurotrophic factor (BDNF) is associated with depressive symptoms in older adults with HIV disease. J Neurovirol. 2021;27(1):70–79. doi: 10.1007/s13365-020-00916-2. [DOI] [PubMed] [Google Scholar]
- 17.Mourão AM, et al. Plasma levels of brain-derived neurotrophic factor are associated with prognosis in the acute phase of ischemic stroke. J Stroke Cerebrovasc Dis. 2019;28(3):735–740. doi: 10.1016/j.jstrokecerebrovasdis.2018.11.013. [DOI] [PubMed] [Google Scholar]
- 18.Saito S, et al. Low serum BDNF and food intake regulation: a possible new explanation of the pathophysiology of eating disorders. Prog Neuropsychopharmacol Biol Psychiatry. 2009;33(2):312–316. doi: 10.1016/j.pnpbp.2008.12.009. [DOI] [PubMed] [Google Scholar]
- 19.Monteleone P, Maj M. Dysfunctions of leptin, ghrelin, BDNF and endocannabinoids in eating disorders: beyond the homeostatic control of food intake. Psychoneuroendocrinology. 2013;38(3):312–330. doi: 10.1016/j.psyneuen.2012.10.021. [DOI] [PubMed] [Google Scholar]
- 20.Kernie SG, Liebl DJ, Parada LF. BDNF regulates eating behavior and locomotor activity in mice. EMBO J. 2000;19(6):1290–1300. doi: 10.1093/emboj/19.6.1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nakagawa T, et al. Brain-derived neurotrophic factor regulates glucose metabolism by modulating energy balance in diabetic mice. Diabetes. 2000;49(3):436–444. doi: 10.2337/diabetes.49.3.436. [DOI] [PubMed] [Google Scholar]
- 22.Tsuchida A, et al. Acute effects of brain-derived neurotrophic factor on energy expenditure in obese diabetic mice. Int J Obes Relat Metab Disord. 2001;25(9):1286–1293. doi: 10.1038/sj.ijo.0801678. [DOI] [PubMed] [Google Scholar]
- 23.Ribasés M, et al. Association of BDNF with anorexia, bulimia and age of onset of weight loss in six European populations. Hum Mol Genet. 2004;13(12):1205–1212. doi: 10.1093/hmg/ddh137. [DOI] [PubMed] [Google Scholar]
- 24.Abou Al Hassan S, Cutinha D, Mattar L. The impact of COMT, BDNF and 5-HTT brain-genes on the development of anorexia nervosa: a systematic review. Eat Weight Disord. 2021;26(5):1323–1344. doi: 10.1007/s40519-020-00978-5. [DOI] [PubMed] [Google Scholar]
- 25.Manfredi L, et al. A systematic review of genetic polymorphisms associated with binge eating disorder. Nutrients. 2021 doi: 10.3390/nu13030848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Phillips K, Keane K, Wolfe BE. Peripheral brain derived neurotrophic factor (BDNF) in bulimia nervosa: a systematic review. Arch Psychiatr Nurs. 2014;28(2):108–113. doi: 10.1016/j.apnu.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 27.Brandys MK, et al. A meta-analysis of circulating BDNF concentrations in anorexia nervosa. World J Biol Psychiatry. 2011;12(6):444–454. doi: 10.3109/15622975.2011.562244. [DOI] [PubMed] [Google Scholar]
- 28.Molendijk ML, et al. Serum BDNF concentrations as peripheral manifestations of depression: evidence from a systematic review and meta-analyses on 179 associations (N=9484) Mol Psychiatry. 2014;19(7):791–800. doi: 10.1038/mp.2013.105. [DOI] [PubMed] [Google Scholar]
- 29.Page MJ, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 31.Lo CK-L, Mertz D, Loeb M. Newcastle-ottawa scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol. 2014;14(1):45. doi: 10.1186/1471-2288-14-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Luo D, et al. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. 2018;27(6):1785–1805. doi: 10.1177/0962280216669183. [DOI] [PubMed] [Google Scholar]
- 33.Wan X, et al. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14(1):1–13. doi: 10.1186/1471-2288-14-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Egger M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Duval S, Tweedie R. Trim and fill: a simple funnel-plot–based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455–463. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 36.Nakazato M, et al. No change between the serum brain-derived neurotrophic factor in female patients with anorexia nervosa before and after partial weight recovery. Prog Neuropsychopharmacol Biol Psychiatry. 2006;30(6):1117–1121. doi: 10.1016/j.pnpbp.2006.04.017. [DOI] [PubMed] [Google Scholar]
- 37.Borsdorf B, et al. BDNF levels in adolescent patients with anorexia nervosa increase continuously to supranormal levels 2.5 years after first hospitalization. J Psychiatry Neurosci JPN. 2021;46(5):568–578. doi: 10.1503/jpn.210049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tyszkiewicz-Nwafor M, et al. Brain-derived neurotrophic factor and oxytocin signaling in association with clinical symptoms in adolescent inpatients with anorexia nervosa-a longitudinal study. Front Psychiatry. 2019;10:1032. doi: 10.3389/fpsyt.2019.01032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rybakowski F, et al. Brain derived neurotrophic factor gene Val66Met and -270C/T polymorphisms and personality traits predisposing to anorexia nervosa. Neuro Endocrinol Lett. 2007;28(2):153–158. [PubMed] [Google Scholar]
- 40.Dmitrzak-Weglarz M, et al. BDNF Met66 allele is associated with anorexia nervosa in the Polish population. Psychiatr Genet. 2007;17(4):245–246. doi: 10.1097/YPG.0b013e3280991229. [DOI] [PubMed] [Google Scholar]
- 41.Eddy KT, et al. Appetite regulatory hormones in women with anorexia nervosa: binge-eating/purging versus restricting type. J Clin Psychiatry. 2015;76(1):19–24. doi: 10.4088/JCP.13m08753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Homan P, et al. The role of BDNF, leptin, and catecholamines in reward learning in bulimia nervosa. Int J Neuropsychopharmacol. 2014 doi: 10.1093/ijnp/pyu092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yamada H, et al. Recovery of low plasma BDNF over the course of treatment among patients with bulimia nervosa. Psychiatry Res. 2012;198(3):448–451. doi: 10.1016/j.psychres.2011.12.015. [DOI] [PubMed] [Google Scholar]
- 44.Nakazato M, et al. Possible involvement of brain-derived neurotrophic factor in eating disorders. IUBMB Life. 2012;64(5):355–361. doi: 10.1002/iub.1012. [DOI] [PubMed] [Google Scholar]
- 45.Zwipp J, et al. Serum brain-derived neurotrophic factor and cognitive functioning in underweight, weight-recovered and partially weight-recovered females with anorexia nervosa. Prog Neuropsychopharmacol Biol Psychiatry. 2014;54:163–169. doi: 10.1016/j.pnpbp.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 46.Mancuso C, et al. Changes in appetite-regulating hormones following food intake are associated with changes in reported appetite and a measure of hedonic eating in girls and young women with anorexia nervosa. Psychoneuroendocrinology. 2020;113:104556–104556. doi: 10.1016/j.psyneuen.2019.104556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Keeler JL, et al. Growth factors in anorexia nervosa: a systematic review and meta-analysis of cross-sectional and longitudinal data. World J Biol Psychiatry. 2022 doi: 10.1080/15622975.2021.2015432. [DOI] [PubMed] [Google Scholar]
- 48.Matsumoto J, et al. Altered serum level of matrix metalloproteinase-9 and its association with decision-making in eating disorders. Psychiatry Clin Neurosci. 2017;71(2):124–134. doi: 10.1111/pcn.12490. [DOI] [PubMed] [Google Scholar]
- 49.Cheng CM, et al. Predictive roles of brain-derived neurotrophic factor Val66Met polymorphism on antidepressant efficacy of different forms of prefrontal brain stimulation monotherapy: a randomized, double-blind, sham-controlled study. J Affect Disord. 2022;297:353–359. doi: 10.1016/j.jad.2021.10.077. [DOI] [PubMed] [Google Scholar]
- 50.Tomoda T, et al. BDNF controls GABA(A)R trafficking and related cognitive processes via autophagic regulation of p62. Neuropsychopharmacology. 2022;47(2):553–563. doi: 10.1038/s41386-021-01116-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rios M. BDNF and the central control of feeding: accidental bystander or essential player? Trends Neurosci. 2013;36(2):83–90. doi: 10.1016/j.tins.2012.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nonino CB et al. DRD2 and BDNF polymorphisms are associated with binge eating disorder in patients with weight regain after bariatric surgery. In: Eating and Weight Disorders: Studies on Anorexia, Bulimia and Obesity; 2021. [DOI] [PubMed]
- 53.Monteleone P, et al. The 196G/A (val66met) polymorphism of the BDNF gene is significantly associated with binge eating behavior in women with bulimia nervosa or binge eating disorder. Neurosci Lett. 2006;406(1):137. doi: 10.1016/j.neulet.2006.07.040. [DOI] [PubMed] [Google Scholar]
- 54.Ristevska-Dimitrovska G, et al. Different serum BDNF levels in depression: results from BDNF studies in FYR Macedonia and Bulgaria. Psychiatr Danub. 2013;25(2):123–127. [PubMed] [Google Scholar]
- 55.Milaneschi Y, et al. Depression and obesity: evidence of shared biological mechanisms. Mol Psychiatry. 2019;24(1):18–33. doi: 10.1038/s41380-018-0017-5. [DOI] [PubMed] [Google Scholar]
- 56.Yang T, et al. The Role of BDNF on Neural Plasticity in Depression. Front Cell Neurosci. 2020 doi: 10.3389/fncel.2020.00082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bayer SJ, Yang GS, Lyon DE. Genetic variation associated with depressive symptoms in breast cancer patients: a systematic review. Cancer Nurs. 2022;45(1):E197–e205. doi: 10.1097/NCC.0000000000000903. [DOI] [PubMed] [Google Scholar]
- 58.Aliasghari F, Yaghin NL, Mahdavi R. Relationship between hedonic hunger and serum levels of insulin, leptin and BDNF in the Iranian population. Physiol Behav. 2019;199:84–87. doi: 10.1016/j.physbeh.2018.11.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Summary of search strategies customized for each data bank.
Data Availability Statement
Not applicable.