Abstract
Background:
The purpose of this case series is to describe surgical decision making and clinical outcomes in posteriorly displaced radial head fractures with a major fragment (more than 50% of the head) located behind the humeral condyle. We also document the outcome of open reduction and internal fixation of completely displaced radial head fractures.
Methods:
A retrospective review of the ICUC® (Integrated Comprehensive Unchanged Complete) database was performed between 2012 and 2020. Patients were included if preoperative radiographs demonstrated a major radial head fracture fragment located posterior to the humeral condyle and a minimum of 2-year follow-up data was available.
Results:
Ten patients met inclusion criteria. Two patients had an associated elbow dislocation whereas 8 patients did not. All patients were found to have disruption of the lateral collateral ligament complex intraoperatively. Nine radial head fractures were successfully fixed with interfragmentary screws. One multi-fragmented radial head fracture could not be successfully stabilized with interfragmentary screw fixation and was resected. The average time to final follow-up was 4.8 years (range 2.2-8.1). At final follow-up, 6 patients demonstrated radiographic evidence of a healed radial head, 1 patient had avascular necrosis, and 2 had post-traumatic arthritis. None demonstrated radiographic instability. The average functional score was 0.64 (SD 0.81) and pain score was 0.45 (SD 0.93). The average elbow extension was 8 degrees (SD 11), elbow flexion was 139 degrees (SD 6), forearm supination was 60 degrees (SD 27), and forearm pronation was 69 degrees (SD 3).
Conclusion:
Recognition of a posteriorly displaced radial head fracture is essential, as it may be an indirect sign of elbow instability. This instability should be addressed during surgical intervention.
Key Words: Elbow, Elbow dislocation, Trauma, Radial head fracture
Introduction
Isolated radial head fractures found posterior to the lateral humeral condyle may conceal an occult elbow instability event with disruption of the lateral collateral ligamentous complex (LCL). Recognition of elbow instability is crucial as it may influence treatment decisions. Previous studies have investigated the correlation between radial head fracture size, amount of displacement, and elbow instability; however, there is a paucity of evidence on specific patterns of radial head fracture displacement and the associated ligamentous injuries and clinical outcomes (1–3). The purpose of this case series is to both describe surgical decision making and clinical outcomes in posteriorly displaced radial head fractures with a major fragment (more than 50% of the head) located behind the humeral condyle as well as document the successful outcome of open reduction and internal fixation of completely displaced radial head fractures. We hypothesize that a posteriorly displaced radial head fracture suggests either a dislocation on presentation or a subluxation event that upon self-reduction displaced the fracture posteriorly.
Materials and Methods
A retrospective review of the ICUC® (Integrated Comprehensive Unchanged Complete) database was performed of 1172 cases between 2012 and 2020 (4, 5). The ICUC database is an international collaboration of 4 leading medical centers in Europe and 1 in Uruguay spearheaded by the late Stephan Perren that is accessible online or via smartphone application to which autonomous participants submit operative cases including injury radiographs and CT scans, intra-operative photos of each surgical step, post-operative radiographs, and documentation of post-operative range of motion as well as outcome as scored on 4-point scales of patient pain and functional limitations (4, 5). The participants of this international database provided informed consent for medical use of the recorded images. Institutional Review Board approval was obtained.
Patients were included in this study if preoperative radiographs demonstrated a major radial head fracture fragment (greater than 50% of the head) located posterior to the humeral condyle (OTA classification 2R1A-C), a minimum of 2-year follow-up data was available, and the patient was able to be contacted by telephone to evaluate patient reported clinical outcomes (PROMs). PROMs were assessed by functional limitation (FL) and pain (graded on a numerical scale 0 to 4, with 0 denoting zero functional limitation/no pain and 4 as unable to do any activity/maximum pain). In contrast to existing PROMs (e.g. the Disabilities of the Arm, Shoulder, and Hand (DASH) score or Patient-Rated Wrist Evaluation (PRWE) score), which are limited to specific anatomic regions, the ICUC database created the FL score to assess a patient’s self-reported functional outcome without limiting to specific goals or activities, as each patient may have different ultimate functional demands (4). FL was assessed on a scale from 0 to 4, with 0 denoting zero functional limitation, 1 meaning the patient can do most activities, 2 denoting that the patient can only do certain activities, 3 as unable to do most activities, and 4 as unable to do any activity. Range of motion of the elbow was assessed at final follow-up via clinical photos with a goniometer as previously validated (6). Range of motion was recorded in degrees rather than as a percentage of the patient’s contralateral side in order to compare results to a functional arc of elbow range of motion, which Morrey et al. previously established is 30 to 130 degrees of extension-flexion and 100 degrees of forearm rotation (50 degrees of pronation and 50 degrees of supination) (7). Additionally, the following patient characteristics were obtained through chart review: age, gender, current smoking status, medical comorbidities, employment status, hand dominance, surgical fixation, number of displaced radial head fracture fragments, and need for further procedures.
Results
Ten patients were identified with a major radial head fracture fragment located posterior to the humeral condyle with 2-year follow-up [Table 1]. Two patients had an associated dislocated elbow (Mason type IV) [Figure 1A-C] whereas eight patients did not have radiographic evidence of a dislocated elbow on presentation (Mason type III) [Figure 2A-C]. The mean age was forty-one years (range 15-70) with eight males and two females. All patients were found to have disruption of the lateral soft tissue attachments to the lateral column including the lateral collateral ligament complex. This allowed the elbow to be hinged open to permit careful retrieval of the displaced radial head fragment.
Table 1.
Patient Demographics and Injury
| Case | Age (years) | Gender (M/F) | Laterality of Injured Extremity | Mason Classification | Number of Radial Head Fragments | Surgery | Additional surgery required (Y/N) | Secondary Surgery | Patient Reported Outcomes at Final Follow-up* |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 20 | M | Left | IV | 1 | ORIF with screws, bone anchors, and ex fix | N | FL = 1; P = 0 | |
| 2 | 45 | M | Right | IV | 3 | ORIF with screws, bone anchors, and ex fix | Y | Radial head resection | FL=1; P=1 |
| 3 | 20 | M | Right | III | 1 | ORIF with screws and bone anchors | N | FL = 0; P = 0 | |
| 4 | 70 | M | Right | III | 2 | ORIF with screws and bone anchors | N | FL = 0; P = 0 | |
| 5 | 20 | M | Left | III | 2 | ORIF with screws and bone anchors | N | FL = 0, P = 0 | |
| 6 | 55 | M | Right | III | 2 | Radial head resection | N | FL = 0; P = 0 | |
| 7 | 60 | F | Left | III | 1 | ORIF with screws and bone anchors | Y | Removal of hardware | FL = 0; P = 0 |
| 8 | 45 | M | Right | III | 2 | ORIF with screws and bone anchors | Y | Removal of hardware | FL = 2; P = 3 |
| 9 | 55 | F | Right | III | 2 | ORIF with screws and bone anchors | Y | Removal of hardware | FL = 0; P = 0 |
| 10 | 15 | M | Right | III | 2 | ORIF with screws and bone anchors | N | FL = 1; P = 0 |
Abbreviations: M = Male; F = Female; ORIF = open reduction internal fixation; FL = functional limitation score; P = pain score
*Functional limitation and pain scores are rated on a scale from 0 to 4, with zero as no pain or functional limitation and 4 as unable to do any activity/maximum pain
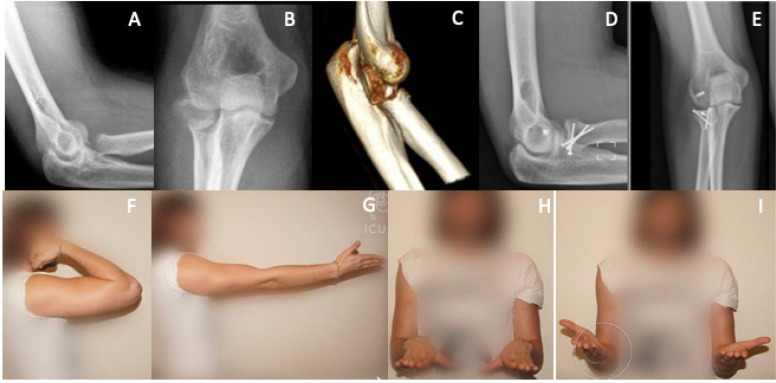
Figure 1.
Radial head fracture with a posteriorly dislocated fragment without evidence of elbow dislocation on injury films (A-C) Injury films show the posteriorly dislocated radial head fracture fragment and likely subluxated ulnohumeral joint, better visualized on the 3-dimensional CT scan. (D-F) Postoperative radiographs after primary fixation of the radial head and repair of the LCL complex, showing a healed radial head and concentric ulnohumeral at final follow-up without evidence of avascular necrosis or instability
Figure 2.
Radiographs of patient with posteriorly dislocated radial head fracture with associated elbow dislocation. (A-C) Injury films show the posteriorly dislocated radial head fracture fragment, dislocated elbow joint without evidence of a coronoid fracture, better visualized on the 3-dimensional CT scan. (D-E) Immediate postoperative radiographs, showing fixation of the radial head fracture fragment and LCL complex. Notably, the elbow was still unstable intraoperatively and required temporary application of external fixation across the elbow joint. (F) Postoperative radiographs after external fixator removal, showing a healed radial head and concentric ulnohumeral without evidence of avascular necrosis or instability
Nine radial head fractures were successfully fixed with interfragmentary screws including three complete fractures of the radial head that were separated from the radial neck. The goal for interfragmentary screw fixation was a minimum of two screws starting proximally in the radial head segment with fixing it distally into the radial neck and shaft. The fractures were initially reduced with pointed reduction forceps and held with K wires. Countersinking was important to prevent prominent screw heads. Screws averaging 1.5mm in diameter were ultimately utilized for fixation. If possible, a third screw was utilized to provide additional fixation in multiple planes. Range of motion of the elbow was assessed to ensure the screws do not cause any blocks to motion. One patient with a 2 fragment radial head fracture could not be successfully stabilized with interfragmentary screw fixation and was simply resected acutely.
All ten patients had the LCL and overlying disrupted lateral musculature reattached to the humeral lateral column using bone anchors. Two patients were noted intraoperatively to demonstrate persistent elbow instability and required temporary application of external fixation across the elbow joint [Figure 2]. The medial collateral ligament (MCL) was not repaired in any patient; rather the surgeons in this case series chose to apply a static external fixation device if the elbow demonstrated persistent instability after repair of the lateral collateral ligamentous complex. The average time to final follow-up was 4.8 years (range 2.2-8.1). At final follow-up, six patients demonstrated radiographic evidence of a healed radial head, one patient had avascular necrosis, and two had post-traumatic arthritis (both had radiocapitellar arthritis, while one patient also had concurrent ulnohumeral arthritis). Four patients required secondary surgeries: three underwent removal of hardware for symptomatic hardware and one underwent a radial head resection secondary to radial head avascular necrosis [Table 1]. No patients demonstrated radiographic instability. The average functional score was 0.64 (SD 0.81) and pain score was 0.45 (SD 0.93) [Table 2]. The average elbow extension was 8 degrees (SD 11), elbow flexion was 139 degrees (SD 6), forearm supination was 60 degrees (SD 27), and forearm pronation was 69 degrees (SD 3).
Table 2.
Clinical Outcomes at Final Follow-Up
| Clinical Outcome Measure | Score |
| Functional Limitation | 0.5 ± 0.7 |
| Pain | 0.4 ± 0.9 |
Data expressed as mean ± standard deviation
Discussion
The correlation between radial head fracture size, amount of displacement, and elbow instability have previously been studied; however, there is a paucity of evidence on specific patterns of radial head fracture displacement and the associated ligamentous injuries and clinical outcomes (1–3). In this study, we specifically focused on radial head fractures with a major fragment (>50%) located posterior to the lateral condyle. Our data suggest that this fracture pattern may be a pathognomonic sign of an associated occult elbow instability event, even without radiographic evidence of a dislocated elbow, as all of our patients with this injury pattern sustained concomitant LCL injuries requiring repair.
Previous studies have demonstrated an association between displaced or comminuted radial head fractures and ligamentous injury (8–11). One study found an associated lateral ulnar collateral ligament or medial collateral ligament injury in up to 80% of patients on MRI, although MRI findings have been shown not to correlate with clinical symptoms in patients with radial head fractures thus necessitating clinical correlation (9,10). Our study builds upon this data by demonstrating isolated posteriorly dislocated radial head fractures correlated with LCL instability intraoperatively, substantiating the radiographic findings previously demonstrated. Additionally, the data in this study supports those previously reported by Tarallo et. al, whose retrospective review found an LCL avulsion in 60% of unstable radial head fractures intra-operatively (10). Our case series augments this data by focusing specifically on posteriorly dislocated radial head fragments on presentation relative to the lateral condyle; moreover, our study also provides a clinical follow-up regarding the outcomes of treatment.
As all of the patients with major radial head fracture fragments posterior to the humeral condyle in our study were found to have concomitant disruption of the lateral soft attachments to the lateral column including the lateral collateral ligamentous complex, we believe this fracture pattern represents the footprint of an elbow dislocation or subluxation, as at some point the elbow may have been subluxated or dislocated and subsequently self-reduced. Thus, this type of fracture pattern may represent a variant of the modified Mason type 4 fracture, necessitating surgeon vigilance to recognize concurrent ligamentous injuries and address any instability during surgical intervention. This includes intraoperative assessment of elbow stability after repair of the lateral collateral ligamentous complex, as two of the ten patients in this series demonstrated persistent instability and required temporary application of an external fixator. While none of the patients underwent MCL repair, this may be an alternative option to the external fixator if clinically indicated.
Additionally, despite patients reporting minimal pain or functional limitations after ORIF at final follow-up, there was a high rate of secondary surgery associated with ORIF. In this case series, four patients required secondary surgeries: three underwent removal of hardware for symptomatic hardware and one underwent a radial head resection secondary to radial head avascular necrosis. Notably, the literature remains controversial regarding optimal surgical treatment of Mason type III and IV fractures (12–18). Ring et al. previously concluded that fixation is best reserved for minimally comminuted fractures with 3 or fewer articular fragments while prosthetic arthroplasty should be performed for more complex and comminuted fractures (16). Furthermore, in a prospective randomized control trial for 45 patients with Mason Type 3 radial head fractures, Chen et al. demonstrated improved outcomes at 2-year follow-up for the radial head replacement cohort compared with ORIF (19). Similarly, Vannabouathong et al. concluded in their systematic review that radial head arthroplasties can lead to better function and reduced postoperative complications compared to open reduction internal fixation in displaced radial head fractures (18). Kachooei et al. demonstrated in their systematic review at 10% rate of removal or revision of the radial head arthroplasty, primarily due to elbow arthrolysis (20). This is significantly less than the rate of secondary surgery in our series. Furthermore, there is a paucity of data comparing range of motion or clinical outcomes in radial head arthroplasty and ORIF in modified Mason Type 4 fractures. Al-Burdeni et al. retrospectively compared outcomes in modified Mason type III and IV at an average follow-up of 15 months, reporting no difference in regaining functional range of motion and similar complication rates (21). However, this was a limited sample size (n=36 patients) with a short follow-up period with selection bias. Similarly, the meta-analysis by Sun et al. comparing radial head arthroplasty and ORIF in modified Mason type III and IV fractures showed higher satisfaction rates and better Broberg and Morrey elbow scores in the arthroplasty group, but no differences in QuickDASH scores or other complications (22). While our patients reported good clinical outcomes despite the high secondary surgery rate, further studies are needed to establish the optimal intervention in this injury pattern that maximizes patient outcomes.
There are several limitations to our study. The main limitation of our data is the small sample size of this retrospective case series, as only ten patients were included. While the incidence of an isolated posteriorly dislocated radial head fracture is uncommon, larger studies are necessary to support our findings. Additionally, our data come from an international database that utilizes a different assessment for PROMs, which may limit direct comparisons to studies using more well-known PROMs such as QuickDASH or PROMIS scores. Lastly, the majority of patients included were male with a significant range in age at time of injury; thus, the generalizability of our findings may be limited. However, despite these limitations, our study may provide a foundation upon which future studies can be conducted.
Surgeon vigilance is essential in recognition of the radiologic finding of a posteriorly displaced radial head fracture on pre-operative imaging, as it may be an indirect sign of elbow instability. Recognition is essential in order to identify concomitant elbow injuries and address this instability during surgical intervention. Additionally, primary fixation of radial head fracture in this injury pattern is associated with good patient-reported outcomes despite a high revision rate.
References
- 1.Beingessner DM, Dunning CE, Gordon KD, Johnson JA, King GJW. The effect of radial head fracture size on elbow kinematics and stability. J Orthop Res off Publ Orthop Res Soc. 2005;23(1):210–7. doi: 10.1016/j.orthres.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 2.Capo JT, Shamian B, Francisco R, Tan V, Preston JS, Uko L, et al. Fracture pattern characteristics and associated injuries of high-energy, large fragment, partial articular radial head fractures: a preliminary imaging analysis. J Orthop Traumatol. 2015;16(2):125–31. doi: 10.1007/s10195-014-0331-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rineer CA, Guitton TG, Ring D. Radial head fractures: loss of cortical contact is associated with concomitant fracture or dislocation. J Shoulder Elbow Surg. 2010;19(1):21–5. doi: 10.1016/j.jse.2009.05.015. [DOI] [PubMed] [Google Scholar]
- 4.Regazzoni P, Giannoudis PV, Lambert S, Fernandez A, Perren SM. The ICUC® app: Can it pave the way for quality control and transparency in medicine? Injury. 2017;48(6):1101–3. doi: 10.1016/j.injury.2017.04.058. [DOI] [PubMed] [Google Scholar]
- 5.Regazzoni P, Südkamp N, Fernandez A, Perren SM. A new way to learn and analyze surgical interventions. Orthopedics and Trauma Surgery messages and news. 2016 [Google Scholar]
- 6.Blonna D, Zarkadas PC, Fitzsimmons JS, O’Driscoll SW. Validation of a photography-based goniometry method for measuring joint range of motion. J Shoulder Elbow Surg. 2012;21(1):29–35. doi: 10.1016/j.jse.2011.06.018. [DOI] [PubMed] [Google Scholar]
- 7.Morrey BF, Askew LJ, Chao EY. A biomechanical study of normal functional elbow motion. J Bone Joint Surg Am. 1981;63(6):872–7. [PubMed] [Google Scholar]
- 8.O’Driscoll SW, Bell DF, Morrey BF. Posterolateral rotatory instability of the elbow. J Bone Joint Surg Am. 1991;73(3):440–6. [PubMed] [Google Scholar]
- 9.Itamura J, Roidis N, Mirzayan R, Vaishnav S, Learch T, Shean C. Radial head fractures: MRI evaluation of associated injuries. J Shoulder Elbow Surg. 2005;14(4):421–4. doi: 10.1016/j.jse.2004.11.003. [DOI] [PubMed] [Google Scholar]
- 10.Kaas L, van Riet RP, Turkenburg JL, Vroemen JPAM, van Dijk CN, Eygendaal D. Magnetic resonance imaging in radial head fractures: most associated injuries are not clinically relevant. J Shoulder Elbow Surg. 2011;20(8):1282–8. doi: 10.1016/j.jse.2011.06.011. [DOI] [PubMed] [Google Scholar]
- 11.Tarallo L, Porcellini G, Merolla G, Pellegrini A, Giorgini A, Catani F. Isolated displaced type II partial articular radial head fracture: correlation of preoperative imaging with intraoperative findings of lateral ulnar collateral ligament tear. J Shoulder Elbow Surg. 2020;29(1):132–8. doi: 10.1016/j.jse.2019.07.006. [DOI] [PubMed] [Google Scholar]
- 12.Grewal R, MacDermid JC, Faber KJ, Drosdowech DS, King GJW. Comminuted radial head fractures treated with a modular metallic radial head arthroplasty. Study of outcomes. J Bone Joint Surg Am. 2006;88(10):2192–200. doi: 10.2106/JBJS.E.00962. [DOI] [PubMed] [Google Scholar]
- 13.Moro JK, Werier J, MacDermid JC, Patterson SD, King GJ. Arthroplasty with a metal radial head for unreconstructible fractures of the radial head. J Bone Joint Surg Am. 2001;83(8):1201–11. doi: 10.2106/00004623-200108000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Clembosky G, Boretto JG. Open Reduction and Internal Fixation Versus Prosthetic Replacement for Complex Fractures of the Radial Head. J Hand Surg. 2009;34(6):1120–3. doi: 10.1016/j.jhsa.2008.12.031. [DOI] [PubMed] [Google Scholar]
- 15.Koslowsky TC, Mader K, Gausepohl T, Pennig D. Reconstruction of Mason type-III and type-IV radial head fractures with a new fixation device: 23 patients followed 1-4 years. Acta Orthop. 2007;78(1):151–6. doi: 10.1080/17453670610013565. [DOI] [PubMed] [Google Scholar]
- 16.Ring D, Quintero J, Jupiter JB. Open reduction and internal fixation of fractures of the radial head. J Bone Joint Surg Am. 2002;84(10):1811–5. doi: 10.2106/00004623-200210000-00011. [DOI] [PubMed] [Google Scholar]
- 17.Duckworth AD, Wickramasinghe NR, Clement ND, Court-Brown CM, McQueen MM. Radial head replacement for acute complex fractures: what are the rate and risks factors for revision or removal? Clin Orthop. 2014;472(7):2136–43. doi: 10.1007/s11999-014-3516-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vannabouathong C, Akhter S, Athwal GS, Moro J, Bhandari M. Interventions for displaced radial head fractures: network meta-analysis of randomized trials. J Shoulder Elbow Surg. 2019;28(3):578–86. doi: 10.1016/j.jse.2018.10.019. [DOI] [PubMed] [Google Scholar]
- 19.Chen X, Wang S, Cao L, Yang G, Li M, Su J. Comparison between radial head replacement and open reduction and internal fixation in clinical treatment of unstable, multi-fragmented radial head fractures. Int Orthop. 2011;35(7):1071–6. doi: 10.1007/s00264-010-1107-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kachooei AR, Baradaran A, Ebrahimzadeh MH, Dijk CN van, Chen N. The Rate of Radial Head Prosthesis Removal or Revision: A Systematic Review and Meta-Analysis. J Hand Surg. 2018;43(1):39–53. doi: 10.1016/j.jhsa.2017.08.031. [DOI] [PubMed] [Google Scholar]
- 21.Al-Burdeni S, Abuodeh Y, Ibrahim T, Ahmed G. Open reduction and internal fixation versus radial head arthroplasty in the treatment of adult closed comminuted radial head fractures (modified Mason type III and IV) Int Orthop. 2015;39(8):1659–64. doi: 10.1007/s00264-015-2755-1. [DOI] [PubMed] [Google Scholar]
- 22.Sun H, Duan J, Li F. Comparison between radial head arthroplasty and open reduction and internal fixation in patients with radial head fractures (modified Mason type III and IV): a meta-analysis. Eur J Orthop Surg Traumatol Orthop Traumatol. 2016;26(3):283–91. doi: 10.1007/s00590-016-1739-1. [DOI] [PubMed] [Google Scholar]