Abstract
Background:
Avascular necrosis (AVN) or osteonecrosis of the femoral head occurs as a result of a vascular supply disruption that could lead to hip osteoarthritis. Recently, several joint-preserving procedures have been suggested to improve the outcome of AVN, including hip arthroscopy. This systematic review aimed to investigate the role of hip arthroscopy to preserve hip joints suffering from AVN.
Methods:
This review was conducted to collect data on hip arthroscopy from the available literature for the management of AVN. The collected articles included those that were focused mainly on the management of AVN assisted by arthroscopy and published up to 2020 that were searched in four databases using such keywords as “Avascular Necrosis”, “AVN”, and “Osteonecrosis” in combination with “Hip Arthroscopy” or “Arthroscopic Hip Surgery”.
Results:
In total, 13 articles met the eligibility criteria, and no severe complications were reported after arthroscopy in patients with AVN. Moreover, the Harris scores were higher than 79 after the operation. The majority of the assessments showed that the use of arthroscopy was effective in the diagnosis and treatment of patients with AVN, except for one study, which had been performed on patients with stage IV AVN.
Conclusion:
The findings supported the idea that hip arthroscopy is effective in the treatment of AVN. This approach is becoming more popular for the diagnosis and treatment of hip disorders.
Key Words: Avascular necrosis of femoral head, Hip arthroscopy, Ischemic bone necrosis, Osteonecrosis
Introduction
Avascular necrosis (AVN) of the femoral head is a menacing disease in which the decreased blood flow to the femoral head leads to the death of bone cells and can result in articular surface collapse, and consequently, osteoarthritis (1, 2). Alcoholism, steroid use, unapproved weight gain medications, and hip trauma are the main causes of this condition (3-7). The pathogenesis of the avascular necrosis of the femoral head (AVNFH) is not well known (8).
Since AVNFH usually affects younger individuals (4, 9), it is of utmost importance to implement an early intervention to save the femoral head (FH) and prevent further arthritic changes (8). Several joint-preserving procedures have been recommended for the treatment of AVNFH. Some of these procedures, including core decompression with or without bone graft, aimed to prevent the collapse of the FH (10). Other procedures, such as trap door operation (2), focused on the restoration of the collapsed bone to support the cartilage. Rotational osteotomies with the goal to redirect the diseased bone from the weight-bearing area are the other type of joint preserving procedures (2). However, there have been no standard protocols for the treatment of AVNFH to retain the patient’s native hip joint (10, 11).
The majority of the hip preserving procedures are performed through open hip surgery, which is more or less associated with morbidity and risks. The role of hip arthroscopy in the diagnosis and treatment of AVNFH has been described in recent years (10). The present study aimed to review the current evidence on the therapeutic and diagnostic role of arthroscopy in patients with AVNFH.
Materials and Methods
A comprehensive search strategy was utilized to collect data based on the Cochrane Handbook for systematic reviews. Furthermore, the main stages in this study included the selection of eligibility criteria, searching databases, removal of unrelated articles, quality assessment, data extraction, and evaluation of the gathered data (12). It is worth mentioning that all published papers up to 15 October 2019 were searched in Google Scholar, PubMed, Scopus, and Medline databases.
Eligibility Criteria
A Participants-Intervention-Comparison-Outcome-Study design was utilized to select the eligibility criteria for this study. The inclusion criteria included 1) a clear description of the diagnostic and therapeutic role of the hip arthroscopy in patients with AVN of the hip, 2) sufficiency of the data, 3) sample size higher than 10 patients, and 4) investigations on human samples. On the other hand, in vitro and animal studies, non-clinical research, review articles, meta-analyses, expert opinions, editorial letters, case reports or case series, consensus statements, and qualitative investigations were excluded from the review process. In addition, the articles that were focused on the other therapeutic approaches or patients who underwent arthroplasty were removed from the study. In this study, even the non-randomized, non-blinded, and retrospective studies were included due to the dearth of the randomized clinical trial studies. Therefore, all case-control, prospective, and retrospective studies performed on human subjects were included to assess the role of hip arthroscopy in patients with AVN. In addition, the studies assessing the diagnostic and therapeutic role of hip arthroscopy in other diseases were excluded from the current study.
Literature Search
The search process was conducted in four electronic databases, including Google Scholar, PubMed, Scopus, and Medline up to March 2020. Moreover, the keywords that were used to accomplish the search process included “Avascular Necrosis”, “AVN”, and “Osteonecrosis”, in combination with “Hip Arthroscopy” or “Arthroscopic Hip Surgery”.
Study Selection, Data Extraction, and Study Design
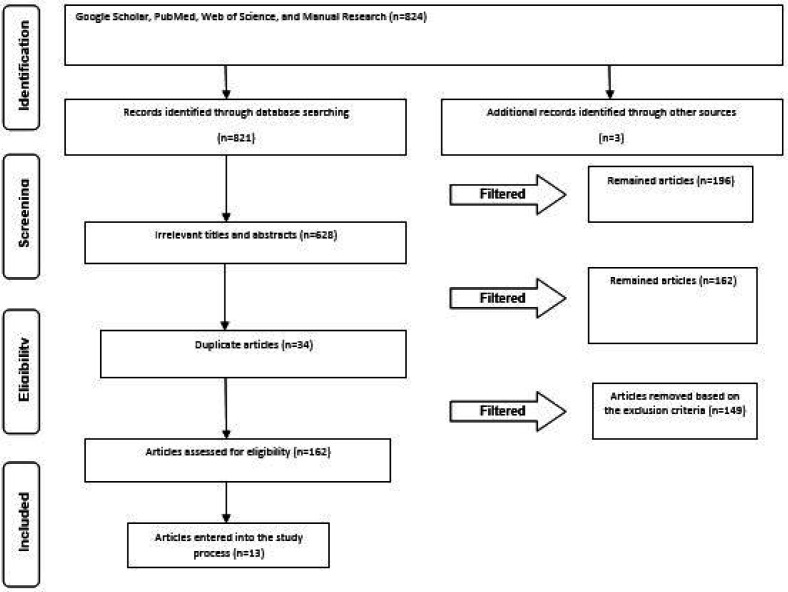
This systematic review focused on the studies with an emphasis on the diagnostic and therapeutic role of hip arthroscopy in patients with AVN of the hip. The search process was carried out using the selected keywords and searching in four electronic databases, including Google Scholar, PubMed, Scopus, and Medline, up to March 2020. In the next step, the number of papers in each database was determined, and the titles and abstracts were then reviewed and screened for relevancy. The selection process was performed based on consistency with the eligibility criteria. In the screening stage, the articles inconsistent with the study objectives were removed after reviewing the title and abstract of each article. Subsequently, the full-text version of the selected articles was obtained for final screening. It should be mentioned that two researchers separately reviewed the titles and abstracts of all articles and were continuously in contact with each other to consult and exchange the required information. Furthermore, they discussed the results obtained from papers and determined the eligibility criteria with mutual agreement. Following that, the researchers extracted the information related to the study objectives and recorded them in a researcher-made form. Figure 1 depicts a PRISMA flow diagram presenting the stages of the paper selection.
Figure 1.
PRISMA flowchart representing the study selection process
Risk of Bias and Quality Assessment
Based on Cochrane’s risk of bias tool, the risk of bias in the included studies was assessed in eight domains, including bias due to confounders, selection of participants, measurement of intervention, missing data, selective reporting, measurement outcome, departure form intended intervention, and other sources (13).
Results
In total, 824 articles were found in the first search, out of which 628 papers were excluded due to irrelevancy, and a total of 196 articles remained after the primary investigation. Another 34 articles were removed from the study since they were duplicates. Furthermore, the articles investigating other hip joint diseases than AVN were excluded from this study (n=51). Other excluded studies were experimental or in vitro articles (n=0), studies just reporting a technique (n=16), studies assessing the complication of arthroscopy in patients with hip joints problems (n=19), studies with a sample size of fewer than 10 people (n=6), editorial letters (n=1), books (n=2), narrative articles and reviews (n=31), and case reports (n=23). Eventually, 13 articles remained to be included in this review [Figure 1].
No randomized double-blind clinical trials were found in this study. Accordingly, only pre-and post-intervention, as well as comparative studies were included in this review. The included studies were performed in five different regions, the most frequent (53.8%) of which were China (n=7). Moreover, three studies were conducted in European countries, including Germany (n=1), Switzerland (n=1), and Poland (n=1). A total of three (23%) studies were carried out in the USA, and no study was found to be conducted in South America and Africa. The included studies (n=13) were performed on 799 patients (895 hips) with AVN (stages I-III). The mean age of the patients was 44 years, and the majority of the studies included more males than female patients. No severe complications were reported after arthroscopy in the patients with AVN, and Harris scores were higher than 79 after arthroscopy. The mean follow-up duration after operation ranged from 12 months to 2.5 years. Furthermore, multiple small-diameter drilling decompression combined with arthroscopy was utilized in some studies (10, 14, 15).
Arthroscopic core decompression combined with autogenous cancellous bone graft and bone morphogenetic protein was applied in a study conducted by Zhuo et al. (16). The patients in a study performed by Guo et al. underwent drilling decompression with a 3.5-mm Steinmann pin under the C-arm X-ray monitoring. Synovectomy and cartilage trimming were performed through hip arthroscopy combined with hip arthrosynovitis or cartilage trauma (17). This was similar to the method adopted by Sekiya et al. (18)
Ellenrieder et al. performed core decompression using a guiding sleeve via a lateral approach. In this technique, a central drill hole was used to curettage the necrotic area through the insertion of the autogenous bone cylinders (19). Similarly, multihole decompression and arthroscopic debridement were performed in a study conducted by Xue-Zhong et al. (20). The arthroscopy procedures in a study carried out by Liu et al. consisted of the removal of loose bodies, debridement, and biopsy (21). In a study performed by Majewski et al., an incision was placed 2 cm ventral and caudal to the greater trochanter. Moreover, the joint was filled with 10-20 ml Ringer’s Lactate solution over a puncture needle providing enough joint space to pass the blunt trocar without traction (22).
The majority of the studies showed the effectiveness of arthroscopy in the diagnosis and treatment of patients with AVN, except for one article, which was performed on patients with stage IV of AVN.
Table 1 tabulates the data extracted from each study including time and place of the study, sample size, age, male to female ratio, stages of AVN, complications after arthroscopy, follow-up, and outcomes (23).
Table 1.
Data extracted from each included study
|
Authors
(years) Reference |
Country | Type of study | Sample size | Group | Age | Female/Male | Stage | Complication | Harris scores after operation | Follow-up | Outcome | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Li et al. (2017) (5) |
China | Retrospective analysis | 60 patients (98 hips) | A1:26 cases/43 hips B2: 34 cases/55 hips |
A:37.4 B:35.2 |
A:15/11 B:18/16 |
Early-stage (I and II stage) | No sever complication | A:82.07 B:75.79 P<0.005 |
57.6 months | Drilling decompression combined with hip arthroscopy is effective in the treatment of patients with early-stage of AVNFH | |
| Li et al. (2017) (8) |
China | Prospective, Case-control |
91 patients (127hip) | HA: 39 cases/53 hips C:52 cases/74 hips |
Two groups were matched | Two groups were matched | Early-stage | Temporary sciatic nerve apraxia during operation in 2 cases | HA:83.3 C: 76.61 P<0.005 |
HA:39 C:34 |
Improvement in pain relief and hip function in patients who underwent hip arthroscopy. | |
| Guo et al. (2018) (12) |
China | Prospective, Case-control |
76 patients(76 hips) | HA3:38 C4:38 |
HA:43.9 C:44.6 |
HA:8/27 C:12/29 |
Early-stage (stage II) | No sever complication | HA:86.72 C:78.62 P<0.005 |
30 months | Using the arthroscopic-guided core decompression method can improve results in patients with AVN. | |
| Wang et al. (2007) (9) |
China | Prospective, Before-after | 226 patients (383 hips), | -- | 36.5 | 57/169 | -- | Progress in the staging of clinical course and collapse of the femoral head in patients with low Harris scores and Hydrops articuli. |
Before operation:68 After: 79 P<0.005 |
35 months | Excellent curative effect was found in the majority of hips. The AVNFH was improved by hip arthroscopy through scavenging pain-producing substances, removing the cartilage chips caused by isolation or undermining dissection, and correcting internal environment disorder. | |
| Ellenrieder et al. (2013) (14) |
Germany | Prospective, Before-after | 53 patients (56 hips) | -- | 44 | 39/14 | Steinberg stages I-III | No sever complication | -- | 33 months | In case of cartilage defects or potential collapse of the femoral head, arthroscopy of the hip joint was performed. The success rate was reported in 86% of patients treated with Steinberg stages I-III. | |
| Majewski et al. (2010) (17) |
Switzerland | Prospective, Before after | 11 patients | -- | 13 years | 7/3 | Idiopathic femur head necrosis | No iatrogenic cartilage injury, no infection, no wound-healing problem, and no neurovascular complication | -- | 1-year follow-up | An average increase in hip motion of flexion, abduction, adduction, external rotation, and internal rotation was reported in patients who underwent arthroscopy | |
| XUE-ZHONG et al. (2007) (15). |
China | Retrospective study | 72 patients (80 hips) | HA: 41 cases/ 46 hips C:31 cases/34 hips |
Two groups were matched | -- | (stages 0, I, ) | No sever complication | -- | -- | Success rate was higher in multihole core decompression and arthroscopic debridement in the management of AVNFH, compared to the traditional group | |
| Liu et al. (2002) (16) |
China | Prospective, Before-after |
16 patients with avascular necrosis | -- | 17 to 64 years. | 33%/77% | -- | No sever complication | Harris hip scores increased by 27 on average. (P<0.005) |
-- | The patients with avascular necrosis reported no pain after arthroscopy and the Harris hip scores increased by 27 on average | |
| Zhuo (2012) (11) |
China | Prospective, Before-after |
28 patients (33 hips) | -- | 1-3 years | -- | -- | No sever complication | 85.67- 81.33 | followed up 2.5 years | Better results in patients who underwent arthroscopic core decompression combined with autogenous cancellous bone graft and BMP compared to traditional closed core decompression in terms of pain and hip function improvement, as well as slowing down the process of femoral head necrosis | |
| Przybył et al (2017) (18) |
Poland | 14 patients Prospective, Before-after | 14 patients (14 hips) | -- | -- | -- | -- | No sever complication | -- | 12 months | A good outcome was reported in the arthroscopic treatment of avascular necrosis produced at 6 and 12 months after the surgery. | |
| O’Leary et al. (2001) (10) |
USA | Retrospective | 83 patients (86 hips) | -- | 29.2 | 37%/67% | -- | No sever complication | -- | 30 months | Improvement was reported in only 40% of AVN patients over 30 months. | |
| Sekiya et al (2000) (13) |
USA | Prospective study | 23 hips | -- | -- | -- | -- | -- | -- | -- | A weak correlation was observed among the results obtained from plain radiographs, magnetic resonance imaging, and arthroscopy, indicating poor correlation among the current imaging techniques in terms of the staging of AVN. | |
| Ruch et al. (2001) (19) |
USA | Prospective study | 46 patients (52 hips) | -- | -- | -- | -- | -- | -- | -- | Based on the obtained results, arthroscopy of the hip was a success in a diagnosis of osteochondral degeneration that was not detected by plain radiographs or magnetic resonance imaging. | |
Determination of the Risk of Bias
In total, 13 articles were carefully reviewed in this study considering the risk of bias in eight domains, and Cochrane guidelines were followed to assess the quality of the included studies. To assess the risk of bias, low and high risks of bias were marked as “Yes” and “No”, respectively. Moreover, unclear or unknown risk of bias was specified as “Unclear”. Figure 2 illustrates the quality assessment of the selected articles.
Figure 2.
Quality assessment of the studies included in the review
Discussion
Arthroscopic surgery of the hip is a very useful and facilitating technique in the treatment of different hip diseases. The use of hip arthroscopy in the treatment of AVNFH has been explained in different studies; however, there is no consensus on the role of arthroscopy in the diagnosis and treatment of the AVNFH (8). This systematic review attempted to answer three main questions based on the current literature.
Is arthroscopy beneficial in the treatment of patients with avascular necrosis of the femoral head?
The reviewed literature showed the beneficial effect of arthroscopy on patients with AVNFH. Ellenrieder et al. showed the improvement of the hip function following hip arthroscopy for AVN in 86% of patients with stages I-III of AVNFH (19). In a study performed by Majewski et al., arthroscopy in patients with AVNFH led to an average increase in hip motion (flexion, abduction, adduction, external rotation, and internal rotation) (22). In the same line, Wang et al. conducted a study on 226 patients with AVNFH (383 hips). Based on the obtained results, the Harris score was significantly increased after the operation, and excellent and medium curative effects were found in 69.5% (Harris score>80) and 24.5% (Harris score between 70 and 79) of the hips, respectively. However, only 6% of the patients experienced poor results (Harris score<69). Lie et al. showed that hip arthroscopy and decompression were associated with an improvement in pain and hip range of movement and function in six months (10). Similarly, Guo et al. conducted a study to evaluate the effects of arthroscopy-guided core decompression and bone grafting on 76 patients with early-stage AVNFH (i.e., stage II). According to their results, the patients who underwent arthroscopy obtained better imaging outcomes and higher Harris hip scores, compared to the control group (17).
The AVNFH was improved by hip arthroscopy through scavenging pain-producing substances, removing the cartilage chips caused by isolation or undermining dissection, and correcting internal environment disorder (15). In the same line, Liu et al. performed a study to determine the diagnostic and therapeutic value of arthroscopy in 16 patients with AVN. In this study, the arthroscopic procedure consisted of the removal of loose bodies, debridement, and biopsy. An average increase was reported in the Harris hip scores (27 points), and patients had no pain after arthroscopy (21).
Several arthroscopic procedures have been described for the retreatment of patients with AVNFH. Trapdoor and light bulb approaches are among the two most common open surgeries (24, 25). These approaches can be used as a predictable preservation technique in the pre-collapse stage. Muscular preservation, decreased recovery times, as well as reduced postoperative pain and infection are the main advantages of the light bulb as an arthroscopic surgery technique, compared to open procedures (26). Based on the results of a study conducted by Rosenwaser et al., the light bulb approach and autologous iliac bone grafting had a high rate of clinical success (25). Additionally, the light bulb approach was utilized in a study conducted by Wang et al., and the survival rate was estimated to be 85% in patients with stage IIA and IIB of AVN. Moreover, the corresponding value was determined at 60% in patients with stage IIIA and IIC of AVN (27).
Other studies described arthroscopic procedures for decompression. Li et al. evaluated the effectiveness of multiple small-diameter drilling decompression combined with hip arthroscopy in the treatment of patients with AVNFH. Based on the obtained results, the patients who underwent hip arthroscopy and decompression obtained higher Harris scores, compared to those who underwent drilling decompression alone. They showed hip arthroscopy as an effective technique in the treatment of patients with early-stage AVNFH, and no serious complications were reported during follow-ups. These findings were consistent with the results of another study performed by Li et al. which revealed that hip arthroscopy was effective in slowing down the process of femoral head necrosis and delaying the need for total hip arthroplasty in patients with AVNFH (14).
Guadilla et al. indicated the viability of the core decompression and bone grafting in the treatment of patients with AVN. This approach helps avoid open surgery in these patients (26). In a study performed by Xue-Zhong et al., the effectiveness of multi-hole core decompression and arthroscopic debridement was investigated in the management of AVNFH. The results revealed that the group who underwent the modified techniques obtained a higher success rate (86.9%), compared to the group who underwent traditional treatment (58.8%) (20).
In another study carried out by Zhuo et al., 28 patients (33 hips) with early-stage AVNFH underwent arthroscopic minimally invasive surgery (i.e., arthroscopic core decompression) to determine the effectiveness of this management technique. It should be noted that arthroscopy was combined with autogenous cancellous bone graft and bone morphogenetic protein or simply closed core decompression. The obtained results indicated pain relief and improved hip function in all patients after six months. Additionally, the mean Harris score of the patients who underwent arthroscopy combined with autogenous cancellous bone graft was 85.67. Moreover, those who underwent arthroscopy utilizing bone morphogenetic protein or simply closed core decompression obtained a score of 81.33. Improvement in pain and hip function, as well as delays in the process of femoral head necrosis, was observed in patients who underwent arthroscopic core decompression combined with autogenous cancellous bone graft and bone morphogenetic protein, compared to those who underwent traditional closed core decompression (16).
The included studies in this review confirmed the effectiveness of arthroscopy in the treatment of patients with early-stage AVNFH; however, as anticipated, this procedure failed to show beneficial effects on patients with advanced AVN.
The AVNFH is not only a bone disease, it also involves the hip joint in the process. Therefore, the secondary pathological changes in the hip joint should be considered in addition to the decompression of the FH for the treatment of AVNFH (10). Regardless of the causative factors, such as idiopathic conditions, high-stress trauma, high-dose corticosteroid administration, or alcohol abuse, the treatment of AVN includes the activation of the biological process, which is dictated by the disease stage and size of the lesion (28). Li et al. showed less joint effusion in patients with stage I AVN, whereas this condition appears in stage II AVN (10). The management of early-stage AVNFH is of utmost importance, and multiple small-diameter drilling decompression combined with hip arthroscopy is a comprehensive therapy for these patients. Based on a study conducted by Li et al., hip arthroscopy is used to directly visualize the condition of the joint and remove synovial hypertrophy. They eliminated the agents causing inflammation by rinsing with physiological saline solution (10), which decreased the intra-articular pressure and improved the functions of the joint as well as its internal environment (29). Moreover, it led to the recovery of joint activity and blocked the vicious inflammatory cycle (30). According to some studies, the rate of penetrating cartilage can be decreased by arthroscopy (31-34).
The main indicators for using hip arthroscopy in the treatment of patients with early-stage AVN include failures in conservative treatment, remarkable synovial hyperplasia, effusion, and articular cartilage damage diagnosed by magnetic resonance imaging (MRI), as well as corpus liberum in the articular cavity or labrum injury with mechanical symptoms (10).
Is arthroscopy an applicable diagnostic approach for the management of patients with avascular necrosis?
The choice of treatment for AVN depends on MRI and radiography outcomes (28). Although plain radiographs and MRI images are commonly used to diagnose and determine the stages of AVNFH, they are not appropriate approaches to diagnose early articular cartilage damage (35, 36). The results confirmed the advantages of arthroscopy for the diagnosis of AVN, compared to MRI and radiography. In total, two studies made a comparison between the diagnostic value of arthroscopy and other techniques, such as MRI (18, 33).
Ruch et al. conducted a study to evaluate the correlation between plain radiographs, MRI, and diagnostic arthroscopy in the staging of the AVNFH. A moderate correlation was reported between MRI and plain radiographs, MRI and arthroscopy, as well as plain radiographs and arthroscopy in this study.
Based on the obtained results, the arthroscopy efficiently diagnosed the osteochondral degeneration that was not detected by plain radiographs or MRI (18). In another study carried out by Sekiya et al., the diagnostic accuracy of the hip arthroscopy was evaluated in patients with AVN. They showed a weak correlation among the results obtained from plain radiographs, MRI, and arthroscopy. Accordingly, a poor correlation was reported among the findings of the current imaging techniques in terms of the staging of AVN. Due to the insufficiency of MRI in assessing the articular cartilage, arthroscopy is required for accurate evaluation and staging, especially in patients in advanced stages of AVN (33).
The MRI findings on the articular cartilage of the hip joint during traction were compared with the arthroscopic results in a study conducted by Nakanishi et al. The obtained results indicated that MRI outcomes corresponded well with the arthroscopic findings of all cases suffering from osteonecrosis and advanced osteonecrosis (37). However, this study was not entered in this review due to the small sample size (i.e., fewer than 10 patients).
Hip arthroscopy is considered a gold standard for the diagnosis of intra-articular hip pathology (38). Based on one study performed by Sekiya et al., only 36% of the damage observed by hip arthroscopy can be diagnosed by MRI (18). Hip arthroscopy offers some advantages, compared to other techniques. Direct observation and size determination of the damaged articular surface is possible by this approach (33). Moreover, this technique can be used to determine the stage of this disease (18). The hip arthroscopy is more accurate in pathology diagnosis, with no evidence in MRI or plain radiography. This technique is useful in the identification of patients with remarkable joint damage who might not benefit from core decompression (26, 39).
Arthroscopy is associated with substantial increases in both diagnostic sensitivity and accuracy in drilling the necrotic area compared with conventional open surgery. Moreover, specificity in determining the condition of cartilage and labrum facilitates intra-operative decisions regarding further treatments (30).
Is arthroscopy a safe approach in the treatment of patients with avascular necrosis?
Based on several studies, the development of AVN is one of the postoperative complications following hip arthroscopy caused by excessive traction weight and time (40). Therefore, it is necessary to select a safer mid-anterior or anterolateral surgical approach to decrease the level of damage to the femoral artery and femoral nerve (18). Similarly, the traction weight and time should be taken into account to prevent injury to the perineal area during hip arthroscopy (41). Due to the relationship between the outcome of core decompression surgery and the time of postoperative non-weight bearing, it is necessary to develop a rehabilitation training program after hip arthroscopy to enhance hip function (42). Rupp et al. performed a study to determine the risk of AVNFH after arthroscopic femoroplasty extending to the posterolateral femoral neck. No evidence of AVNFH has been observed in patients who underwent MRI evaluation after femoroplasty. Due to the lack of association between avascular necrosis and femoroplasty of the posterolateral vascular region of the FH, arthroscopic posterolateral femoroplasty can be used in these patients without worries about the incidence of AVN (43). This finding was confirmed in another study conducted by Christopher et al., which was performed to assess the complications in patients who underwent hip arthroscopy. Cases with AVN after hip arthroscopy have been rare to date (44). Based on one study conducted by Chan et al., only one case with AVN was reported in 530 hips that underwent arthroscopy (45).
It is of significant importance to choose an appropriate treatment for AVNFH (34, 46). Based on the obtained results of the included articles in this study, no severe complication was observed among patients with AVN who underwent arthroscopy. However, Wang et al. reported progress in the staging of clinical course and collapse of the FH in patients with low Harris scores and hydrops articuli (15). Moreover, Li et al. revealed temporary sciatic nerve apraxia during operation in 2 out of 91 patients with AVN who underwent arthroscopy (14).
One of the main advantages of hip arthroscopy is the safety of the technique. However, this method is accompanied by post-operative complications (47), most of which are injury to perineal skin, nerve palsy, vascular injury, compartment syndrome, hematoma, and infection which are observed in 4% of the hip arthroscopy surgeries (48, 49). Several studies assessed the risk of arthroscopy and post-operative complication of this approach in patients with AVN. Since the mentioned studies did not meet the eligibility criteria, a summary of this issue was reported in this review.
Arthroscopy can be used as an adjunct procedure in patients with early-stage AVN for both diagnostic and therapeutic purposes. The utilization of hip arthroscopy in patients with AVNFH allows the surgeon to make a better diagnosis and develop a proper treatment. It also makes it possible for the surgeon to treat intra-articular pathology associated with AVNFH and perform head-preserving surgical procedures, such as core decompression with or without bone grafting or light bulb operation in a less invasive manner.
Suggestion and Limitations
Some interfering factors, such as age, associated comorbidities, and surgeon experience are considered among the affecting factors. The majority of the articles in this review included patients in the same age groups; however, all interference variables were not assessed, which might affect the obtained results of the reviewed studies. Therefore, it is suggested that future studies assess the therapeutic and diagnostic role of arthroscopy among patients with AVN in different stages considering possible confounding variables. Moreover, due to the lack of homogeneity in the studies to assess the hypothesis, some studies were retrospective in nature, which could affect the outcomes in this study.
Table 2.
Quality assessment of the studies included in the review
|
Authors
(years) Reference |
Bias due to confounders | Bias due to the selection of participants | Bias due to the measurement of intervention | Bias due to missing data | Incomplete outcome data | Free of selective reporting | Other sources of bias |
|---|---|---|---|---|---|---|---|
| Li et al. (7) | Yes | Yes | Yes | Yes | Yes | No | Yes |
| Li et al. (11) | No | No | No | No | No | Unclear | No |
| Guo et al. (14) | No | No | No | Yes | No | Yes | No |
| Wang et al. (12) | No | No | Yes | Yes | Yes | Unclear | Yes |
| Ellenrieder et al. (16) | No | No | No | No | No | Yes | No |
| Majewski et al. (19) | No | No | No | No | No | No | No |
| Xue-Zhong et al. (17) | Yes | Yes | No | No | No | No | Yes |
| Liu et al. (18) | No | No | No | No | No | Yes | Unclear |
| Zhuo et al. (13) | No | No | No | No | No | Yes | No |
| Przybył et al. (47) | Yes | No | No | No | No | Yes | Unclear |
| O’Leary et al. (48) | Yes | Yes | Yes | Yes | No | Yes | No |
| Sekiya et al. (15) | No | No | No | No | No | Yes | No |
| Ruch et al. (30) | No | No | No | No | No | Yes | No |
Conflict of interest:
The authors declare that they have no conflict of interest regarding the publication of this study.
Disclaimer:
It should be noted that the present study is informational; therefore, the described strategies might not be suitable for other conditions or purposes.
Acknowledgments
Hereby, the authors extend their gratitude to authorities and staff in Ghaem Hospital Research Center, Mashhad, Iran, for cooperation in this study.
References
- 1.Liang MH, Cullen KE, Larson MG, Thompson MS, Schwartz JA, Fossel AH, et al. Cost-effectiveness of total joint arthroplasty in osteoarthritis. Arthritis Rheum. 1986 Aug;29(8):937–43. doi: 10.1002/art.1780290801. [DOI] [PubMed] [Google Scholar]
- 2.Jonsson B, Larsson SE. Functional improvement and costs of hip and knee arthroplasty in destructive rheumatoid arthritis. Scand J Rheumatol. 1991;20(5):351–7. doi: 10.3109/03009749109096811. [DOI] [PubMed] [Google Scholar]
- 3.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007 Apr;89(4):780–5. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 4.Della Valle CJ, Mesko NW, Quigley L, Rosenberg AG, Jacobs JJ, Galante JO. Primary total hip arthroplasty with a porous-coated acetabular component A concise follow-up, at a minimum of twenty years, of previous reports. J Bone Joint Surg Am. 2009 May;91(5):1130–5. doi: 10.2106/JBJS.H.00168. [DOI] [PubMed] [Google Scholar]
- 5.Engh CA, Hopper RH, Engh CA. Long-term porous-coated cup survivorship using spikes, screws, and press-fitting for initial fixation. J Arthroplasty. 2004 Oct;19(7 Suppl 2):54–60. doi: 10.1016/j.arth.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 6.Udomkiat P, Dorr LD, Wan Z. Cementless hemispheric porous-coated sockets implanted with press-fit technique without screws: average ten-year follow-up. J Bone Joint Surg Am. 2002 Jul;84(7):1195–200. doi: 10.2106/00004623-200207000-00016. [DOI] [PubMed] [Google Scholar]
- 7.Eskelinen A, Remes V, Helenius I, Pulkkinen P, Nevalainen J, Paavolainen P. Uncemented total hip arthroplasty for primary osteoarthritis in young patients: a mid-to long-term follow-up study from the Finnish Arthroplasty Register. Acta Orthop. 2006 Feb;77(1):57–70. doi: 10.1080/17453670610045704. [DOI] [PubMed] [Google Scholar]
- 8.Utting MR, Raghuvanshi M, Amirfeyz R, Blom AW, Learmonth ID, Bannister GC. The Harris-Galante porous-coated, hemispherical, polyethylene-lined acetabular component in patients under 50 years of age: a 12- to 16-year review. J Bone Joint Surg Br. 2008 Nov;90(11):1422–7. doi: 10.1302/0301-620X.90B11.20892. [DOI] [PubMed] [Google Scholar]
- 9.Bobyn JD, Toh KK, Hacking SA, Tanzer M, Krygier JJ. Tissue response to porous tantalum acetabular cups: a canine model. J Arthroplasty. 1999 Apr;14(3):347–54. doi: 10.1016/s0883-5403(99)90062-1. [DOI] [PubMed] [Google Scholar]
- 10.Bobyn JD, Stackpool GJ, Hacking SA, Tanzer M, Krygier JJ. Characteristics of bone ingrowth and interface mechanics of a new porous tantalum biomaterial. J Bone Joint Surg Br. 1999 Sep;81(5):907–14. doi: 10.1302/0301-620x.81b5.9283. [DOI] [PubMed] [Google Scholar]
- 11.Nakashima Y, Mashima N, Imai H, Mitsugi N, Taki N, Mochida Y, et al. Clinical and radiographic evaluation of total hip arthroplasties using porous tantalum modular acetabular components: 5-year follow-up of clinical trial. Mod Rheumatol. 2013 Jan;23(1):112–8. doi: 10.1007/s10165-012-0618-9. [DOI] [PubMed] [Google Scholar]
- 12.Komarasamy B, Vadivelu R, Bruce A, Kershaw C, Davison J. Clinical and radiological outcome following total hip arthroplasty with an uncemented trabecular metal monoblock acetabular cup. Acta Orthop Belg. 2006 Jun;72(3):320–5. [PubMed] [Google Scholar]
- 13.Mulier M, Rys B, Moke L. Hedrocel trabecular metal monoblock acetabular cups: mid-term results. Acta Orthop Belg. 2006 Jun;72(3):326–31. [PubMed] [Google Scholar]
- 14.Macheras G, Kateros K, Kostakos A, Koutsostathis S, Danomaras D, Papagelopoulos PJ. Eight- to ten-year clinical and radiographic outcome of a porous tantalum monoblock acetabular component. J Arthroplasty. 2009 Aug;24(5):705–9. doi: 10.1016/j.arth.2008.06.020. [DOI] [PubMed] [Google Scholar]
- 15.Banerjee S, Issa K, Kapadia BH, Pivec R, Khanuja HS, Mont MA. Systematic review on outcomes of acetabular revisions with highly-porous metals. Int Orthop. 2014 Apr;38(4):689–702. doi: 10.1007/s00264-013-2145-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bobyn JD, Poggie RA, Krygier JJ, Lewallen DG, Hanssen AD, Lewis RJ, et al. Clinical validation of a structural porous tantalum biomaterial for adult reconstruction. J Bone Joint Surg Am. 2004; Suppl 2:123–9. doi: 10.2106/00004623-200412002-00017. [DOI] [PubMed] [Google Scholar]
- 17.Kamada T, Mashima N, Nakashima Y, Imai H, Takeba J, Miura H. Mid-term clinical and radiographic outcomes of porous tantalum modular acetabular components for hip dysplasia. J Arthroplasty. 2015 Apr;30(4):607–10. doi: 10.1016/j.arth.2014.11.007. [DOI] [PubMed] [Google Scholar]
- 18.Harris WH, White RE. Socket fixation using a metal-backed acetabular component for total hip replacement A minimum five-year follow-up. J Bone Joint Surg Am. 1982 Jun;64(5):745–8. [PubMed] [Google Scholar]
- 19.Harris WH, Penenberg BL. Further follow-up on socket fixation using a metal-backed acetabular component for total hip replacement A minimum ten-year follow-up study. J Bone Joint Surg Am. 1987 Oct;69(8):1140–3. [PubMed] [Google Scholar]
- 20.Shirazi-Adl A, Dammak M, Paiement G. Experimental determination of friction characteristics at the trabecular bone/porous-coated metal interface in cementless implants. J Biomed Mater Res. 1993 Feb;27(2):167–75. doi: 10.1002/jbm.820270205. [DOI] [PubMed] [Google Scholar]
- 21.Wegrzyn J, Kaufman KR, Hanssen AD, Lewallen DG. Performance of Porous Tantalum vs Titanium Cup in Total Hip Arthroplasty: Randomized Trial with Minimum 10-Year Follow-Up. J Arthroplasty. 2015 Jun;30(6):1008–13. doi: 10.1016/j.arth.2015.01.013. [DOI] [PubMed] [Google Scholar]
- 22.Baad-Hansen T, Kold S, Nielsen PT, Laursen MB, Christensen PH, Soballe K. Comparison of trabecular metal cups and titanium fiber-mesh cups in primary hip arthroplasty: a randomized RSA and bone mineral densitometry study of 50 hips. Acta Orthop. 2011 Apr;82(2):155–60. doi: 10.3109/17453674.2011.572251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ayers DC, Greene M, Snyder B, Aubin M, Drew J, Bragdon C. Radiostereometric analysis study of tantalum compared with titanium acetabular cups and highly cross-linked compared with conventional liners in young patients undergoing total hip replacement. J Bone Joint Surg Am. 2015 Apr;97(8):627–34. doi: 10.2106/JBJS.N.00605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Meneghini RM, Ford KS, McCollough CH, Hanssen AD, Lewallen DG. Bone remodeling around porous metal cementless acetabular components. J Arthroplasty. 2010 Aug;25(5):741–7. doi: 10.1016/j.arth.2009.04.025. [DOI] [PubMed] [Google Scholar]
- 25.Laaksonen I, Lorimer M, Gromov K, Eskelinen A, Rolfson O, Graves SE, et al. Trabecular metal acetabular components in primary total hip arthroplasty. Acta Orthop. 2018 Jun;89(3):259–64. doi: 10.1080/17453674.2018.1431445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Matharu GS, Judge A, Pandit HG, Murray DW. Which factors influence the rate of failure following metal-on-metal hip arthroplasty revision surgery performed for adverse reactions to metal debris? an analysis from the National Joint Registry for England and Wales. Bone Jt J. 2017 Aug;99-B(8):1020–7. doi: 10.1302/0301-620X.99B8.BJJ-2016-0889.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Poggie RA, Brown TD, Pedersen DR. Finite elements analysis of peri-acetabular stress of cemented, metal-backed, and porous tantalum backed acetabular components. Trans Orthop Res Soc. 1999 [Google Scholar]
- 28.Wilkinson JM, Peel NF, Elson RA, Stockley I, Eastell R. Measuring bone mineral density of the pelvis and proximal femur after total hip arthroplasty. J Bone Joint Surg Br. 2001 Mar;83(2):283–8. doi: 10.1302/0301-620x.83b2.10562. [DOI] [PubMed] [Google Scholar]
- 29.Tokarski AT, Novack TA, Parvizi J. Is tantalum protective against infection in revision total hip arthroplasty? Bone Jt J. 2015 Jan;97-B(1):45–9. doi: 10.1302/0301-620X.97B1.34236. [DOI] [PubMed] [Google Scholar]