Abstract
Background:
Implant removal due to infection is one of the major causes failure following open reduction and internal fixation (ORIF). The aim of this study was to determine trends and predictors of infection-related implant removal following ORIF of extremities using a nationally representative database.
Methods:
Nationwide Inpatient Sample data from 2006 to 2017 was used to identify cases of ORIF following upper and lower extremity fractures, as well as cases that underwent infection-related implant removal following ORIF. Multivariate analysis was performed to identify independent predictors of infection-related implant removal, controlling for patient demographics and comorbidities, hospital characteristics, site of fracture, and year.
Results:
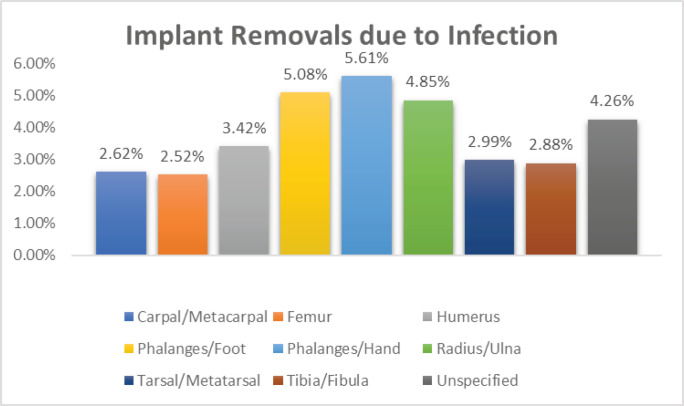
For all ORIF procedures, the highest rate of implant removal due to infection was the phalanges/hand (5.61%), phalanges/foot (5.08%), and the radius/ulna (4.85%). Implant removal rates due to infection decreased in all fractures except radial/ulnar fractures. Tarsal/metatarsal fractures (odds ratio (OR)=1.45, 95% confidence interval (CI): 1.02-2.05), and tibial fractures (OR=1.82, 95% CI: 1.45-2.28) were identified as independent predictors of infection-related implant removal. Male gender (OR=1.67, 95% CI: 1.49-1.87), Obesity (OR=1.85, 95% CI: 1.34-2.54), diabetes mellitus with chronic complications (OR=1.69, 95% CI: 1.13-2.54, P<0.05), deficiency anemia (OR=1.59, 95% CI: 1.14-2.22) were patient factors that were associated with increased infection-related removals. Removal of implant due to infection had a higher total charge associated with the episode of care (mean: $166,041) than non-infection related implant removal (mean: $133,110).
Conclusion:
Implant removal rates due to infection decreased in all fractures except radial/ulnar fractures. Diabetes, liver disease, and rheumatoid arthritis were important predictors of infection-related implant removal. The study identified some risk factors for implant related infection following ORIF, such as diabetes, obesity, and anemia, that should be studied further to implement strategies to reduce rate of infection following ORIF.
Key Words: Fracture, Implant removal, Infection-related implant removal, Infection, Septic hardware
Introduction
The medial collateral ligament (MCL) injury is the most common injury to the knee accounting for about 40% of knee injuries (1). The incidence of MCL injuries is 0.24/1000, with a 2:1 male to female ratio (2). In athletes, the incidence increases to 7.3/1000 population (3). The main medial static stabilizers of the knee are the superficial MCL, deep MCL, and posterior oblique ligament (POL) (4).
The MCL lies in the second layer in the medial aspect of the knee, the femoral attachment lies 1-mm proximal and 37 mm posterior to the medial femoral epicondyle, the distal bony attachment is located just anterior to the posteromedial crest of the tibia 42–71 mm from the tibial joint line, and the superficial MCL is the main medial static stabilizer of the knee all over the range of motion (4-6).
The deep MCL is a thickening of the joint capsule. It consists of two distinct components: the meniscofemoral ligament is distal and deep to the femoral attachment of the superficial MCL approximately 6-mm distal and 5-mm posterior to the medial epicondyle; the meniscotibial portion, which is shorter and thicker, attaches just distal to the edge of the articular surface of the medial tibial plateau (5,6).
The femoral attachment of the POL extends from the posterosuperior aspect of superficial attachment of MCL to the gastrocnemius tubercle and is divided into three components, superficial, capsular, and most importantly, the central arm (5-7). The central arm arises from the main tendon of the semimembranosus, directly attached to the posterior joint capsule and posterior meniscus, and blends its attachment on the tibia 5-mm below the tibial plateau (5,8). The POL is a valgus stabilizer when the knee is extended and has a role in maintaining rotational stability of the knee, especially in PCL-deficient knees (9).
The incidence of concomitant ligamentous injury with grade 3 MCL injury is about 80%, most of which are associated with anterior cruciate ligament (ACL) injury (10,11).
MCL is known for its good healing potential rather than intracapsular ligaments, so nonoperative treatment is the rule for treatment of MCL injuries in grades 1 and 2 and selected cases of grade 3 injuries (12, 13). Failed nonoperative treatment in grade 3 injuries leads to deterioration in knee function and subsequent osteoarthritis in 63% of cases after 10 years (14).
Several techniques have been described for MCL reconstruction however, no evidence supports one technique over the others (15).
This study aims to describe the minimally invasive reconstruction of the MCL of the knee and to evaluate the functional outcome and medial joint space opening 18 months postoperatively.
Materials and Methods
Data Source
We analyzed data from the Nationwide Inpatient Sample (NIS) from 2006 to 2017 to determine the trend and predicting factors of implant removal due to infection after ORIF. The NIS was chosen because it is the largest longitudinal national database in the United States, capturing 20% of hospitalizations annually. The database contains demographic, medical, and financial information associated with each episode of care from 1,051 hospitals across 15 states, and is maintained by the Healthcare Cost and Utilization project and the Agency for Healthcare Research and Quality(15,16). US population data was obtained from the census.gov website for each year (2006-2017)(17). This study was exempt from institutional board approval as all data was retrieved from the NIS.
Patient Selection
The NIS was queried from 2006 to 2017 for patients undergoing ORIF or implant removal each year using a method described by Lovald et al(1,18). Patients were identified via the Ninth Revision of the International Classification of Diseases (ICD-9 codes) for ORIF (79.8x) of the following humeral, radial/ulnar, carpal/metacarpal, femoral, tibial/fibula, tarsal/metatarsal fractures(19). Patients who underwent implant removal (78.6x) and those who developed infection following implant implantation (996.66 and 996.67) were identified as well. A total of 924,506 patients underwent ORIF, and 41,071 patients underwent remove of implant during the study period.
Data collection included demographic information (Age, gender, race), and medical comorbidities. Hospital factors including hospital size (small, medium, or large), type (academic urban, private urban, or rural), and financial data (length of stay, and hospital charges) were also collected. Lastly information regarding the implant, including indication for removal (aseptic or septic (ICD-9 code 996.66 and 996.67)), and location of implant were collected. In regards to the medical comorbidities collected, the conditions included in the Charlson Comorbidity Index (CCI) and the Elixhauser Comorbidity Measure (ECM), due to proven validity and common use in evaluating the NIS, and were identified using the ICD-9CM codes(20–22). The conditions included in these two indices are: age, alcohol abuse, drug abuse, liver disease (mild or severe), rheumatological conditions, peripheral vascular disease, chronic pulmonary disease, blood loss anemia, iron deficiency anemia, HIV/AIDS, solid organ tumor, lymphoma, metastatic disease, diabetes (uncomplicated or complicated), hemiplegia/paraplegia, and myocardial infarction.
Outcome Variables
The primary outcome measure of this study was impact of infection on implant removal following ORIF from 2006 to 2017. Additional secondary outcomes of this study were to identify independent predictors of implant removal due to infection, and the impact infection on the length of stay (LOS) and hospital charges in comparison with aseptic removal of implants.
Statistical Analysis
The impact of infection on implant removal on the LOS and hospital charges in comparison to aseptic implant removal was determined using Wilcoxon Rank-Sum Test. The rate of ORIF each year was determined using the NIS and census data. Similarly, the rate of aseptic implant removal and implant removal due to infection each year was determined using the NIS data and the census data to calculate rate per 100,000 of the national population. The removal of implant was further stratified by dividing the number of implant removals in a region of the body by the total number of ORIF procedures performed on that region each year. The removal of implant due to infection was further stratified by dividing the number of implant removals due to infection in a region of the body by the total number of implant removal procedures performed on that region each year.
Logistic regression analysis was performed, controlling for age, gender, ethnicity, medical comorbidities, hospital type and size, and fracture location to identify independent predictors of implant removal due to infection. Logistic regression was used to estimate the contribution of patient and hospital factors to the probability that a patient visit was for the removal of implant. The regressions included interaction terms between calendar year and site of implant/removal so that statistical comparisons could be made between different bones and the femur (used as reference due to its relatively high rate of fracture).
In order to estimate the incidence on a national population scale, the US population data was obtained from the census.gov, and used in conjunction with the population weight estimates provided by the NIS in order to generate national estimates of the outcomes. The hospital charged were adjusted to 2017 dollars using the inflation calculator provided by the US Bureau of Labor Statistics (23). We used R 2.15.1 (R Foundation for Statistical Computing, Vienna, Austria) for all analyses and the ‘rms’package within R for the logistic regression. In all analyses, p-values less than 0.05 were statistically significant.
Results
ORIF Procedures
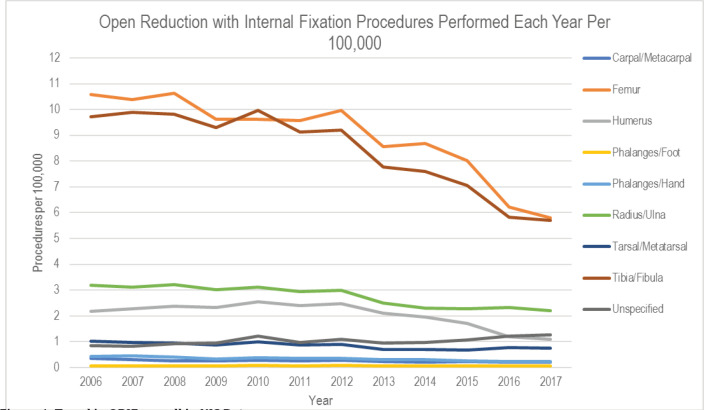
The rate of ORIF procedures were determined through using the NIS database from 2006 to 2017. During the 11-year study period, the overall rate of ORIF decreased from 28.4 to 17.3 per 100,000 (38.9%) [Table 1 and Figure 1]. This decrease was seen in the humerus (2.2 to 1.1 per 100,000, 50.2%), femur (10.6 to 5.8 per 100,000, 45.2%), phalanges/hand (0.43 to 0.24 per 100,000, 44.1%), and tibia/fibula (9.7 to 5.7 per 100,000, 41.3%). The most common location for ORIF was the femur (36.2%), followed by the tibia/fibula (34.0%), and radius/ulna (11.2%).
Table 1.
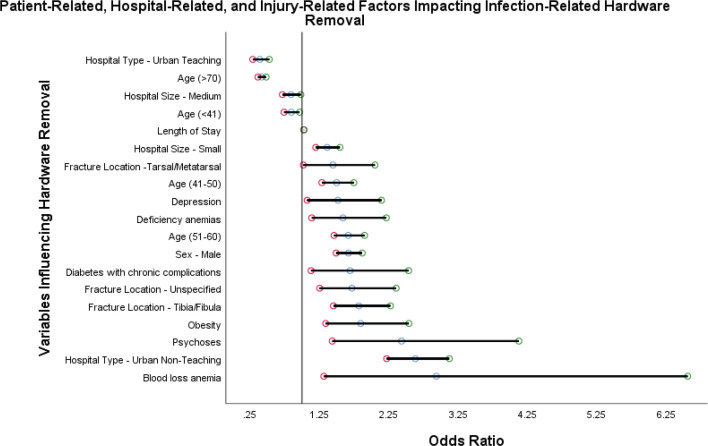
Predictors of Implant removal due to infection
| Predictors of Implant Removal | Odds Ratio | 95% CI Lower Limit | 95% CI Upper Limit | P-Value |
|---|---|---|---|---|
| Blood loss anemia | 2.94 | 1.32 | 6.56 | <0.001 |
| Hospital Type - Urban Non-Teaching | 2.63 | 2.22 | 3.12 | <.0001 |
| Psychoses | 2.43 | 1.44 | 4.13 | <0.001 |
| Obesity | 1.85 | 1.34 | 2.54 | <0.001 |
| Fracture Location - Tibia/Fibula | 1.82 | 1.45 | 2.28 | <.0001 |
| Fracture Location - Unspecified | 1.72 | 1.25 | 2.36 | <0.001 |
| Diabetes with chronic complications | 1.69 | 1.13 | 2.54 | <0.05 |
| Sex - Male | 1.67 | 1.49 | 1.87 | <.0001 |
| Age (51-60) | 1.67 | 1.46 | 1.90 | <.0001 |
| Deficiency anemias | 1.59 | 1.14 | 2.22 | <0.01 |
| Depression | 1.52 | 1.07 | 2.15 | <0.05 |
| Age (41-50) | 1.50 | 1.29 | 1.75 | <.0001 |
| Fracture Location -Tarsal/Metatarsal | 1.45 | 1.02 | 2.05 | <0.05 |
| Hospital Size - Small | 1.36 | 1.20 | 1.55 | <.0001 |
| Length of Stay | 1.03 | 1.03 | 1.03 | <.0001 |
| Age (<41) | 0.85 | 0.74 | 0.97 | <0.05 |
| Hospital Size - Medium | 0.84 | 0.72 | 0.98 | <0.05 |
| Age (>70) | 0.42 | 0.36 | 0.48 | <.0001 |
| Hospital Type - Urban Teaching | 0.39 | 0.29 | 0.53 | <.0001 |
Figure 1.
Trend in ORIF overall in NIS Data
Trends in Implant Removal
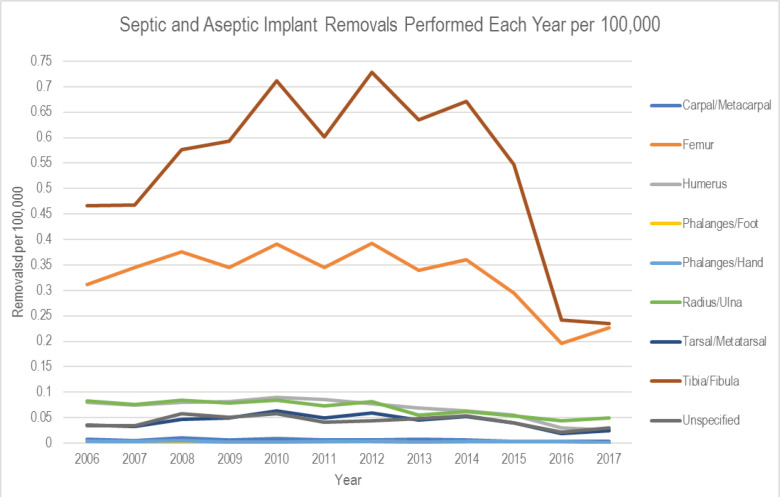
The rate of implant removal across the study period decreased from 1.02 to 0.60 per 100,000 (41.7%). The greatest decrease was seen in the phalanges/foot (-81.6%), humerus (-68.4%), and phalanges/hands (-63.3%) [Figure 2]. The highest rate of implant removal for any reason was removal from the radius/ulna (21.0%), followed by the hands/phalanges (16.5%) and carpal/metacarpal (13.5%).
Figure 2.
Trend in Implant removal by body region
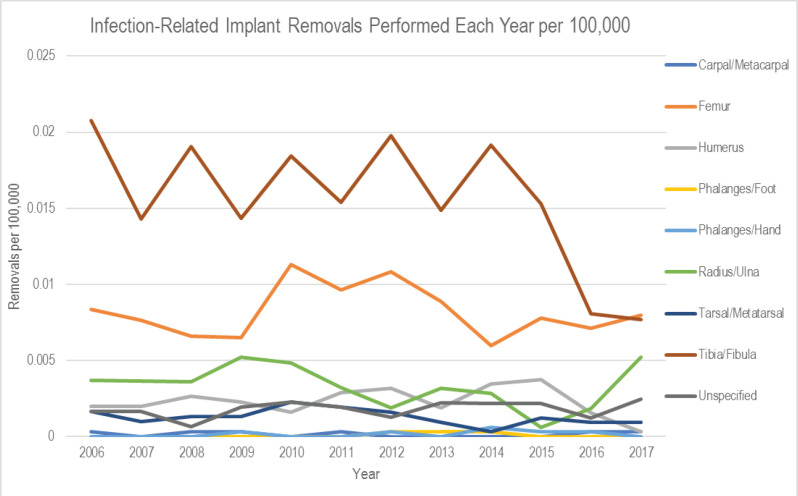
Trends in Infection-Related Implant Removal
The rate of infection-related implant removal across the study period decreased from 0.039 to 0.025 per 100,000 (41.7%). The greatest decrease was seen in the humerus (-84.7%), tibia/fibula (-63.0%), and tarsal/metatarsal (-44.9%) [Figure 3]. There was an increase in the rate of infection-related implant for the radius/ulna (41.9%, 0.0037 to 0.0052). The highest rate of implant removal due to infection was the phalanges/hand (5.61%), phalanges/foot (5.08%), and the radius/ulna (4.85%) [Figure 4]. The most common implant location associated with infection-related implant removal was the phalanges/hand (22.0%) and carpal/metacarpal (22.0%), followed by the humerus (11.0%).
Figure 3.
Trend in Implant Removal due to infection by body region
Figure 4.
Implant Removals due to Infection
Predictors of Infection-Related Implant Removals
Logistic regression analysis was performed to identify independent predictors of implant removal due to infection [Figure 5]. In terms of body region, tarsal/metatarsal fractures (odds ratio (OR)=1.45, 95% confidence interval (CI): 1.02-2.05, P<0.05), and tibial fractures (OR=1.82, 95% CI: 1.45-2.28, P<0.001) were identified as independent predictors of infection-related implant removal. Medical comorbidities determined to be significant predictors included obesity (OR=1.85, 95% CI: 1.34-2.54, P<0.001), diabetes mellitus with chronic complications (OR=1.69, 95% CI: 1.13-2.54, P<0.05), deficiency anemia (OR=1.59, 95% CI: 1.14-2.22, P<0.01), psychosis (OR=2.43. 95% CI: 1.44-4.13, P<0.001), and depression (OR=1.52, 95% CI: 1.07-2.15, P<0.05). Patients who were male were noted to be approximately 67% more likely to undergo removal due to infection (OR= 1.67, 95% CI: 1.49-1.87 P<0.001).
Figure 5.
Predictors of infection related implant removal
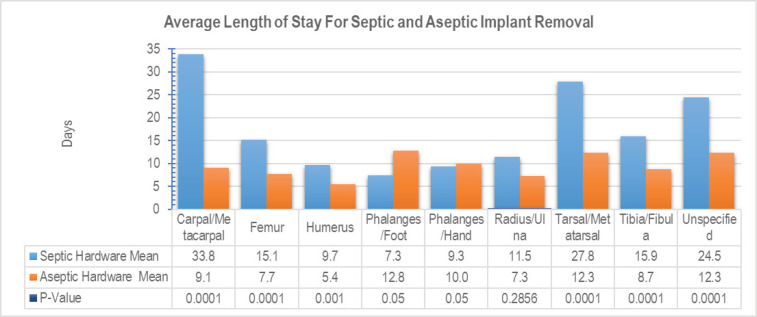
Length of Stay Hospital Charges
Patients undergoing removal of implant due to infection had a significantly longer length of stay (mean: 17.2) than non-infection related implant removal (mean: 9.5 days) [Figure 6]. The longest mean length of stay for infection-related implant removal was seen with carpal/metacarpal (33.8 days), and for non-infectious implant removal was seen with phalanges/foot (12.8 days). The greatest difference in mean days for length of stay for infection-related versus non-infection related implant removal was seen between tarsal/metatarsal removals (15.5 days, 27.8 days vs. 12.3 days).
Figure 6.
Average Length of Stay following Aseptic versus Septic Implant Removal
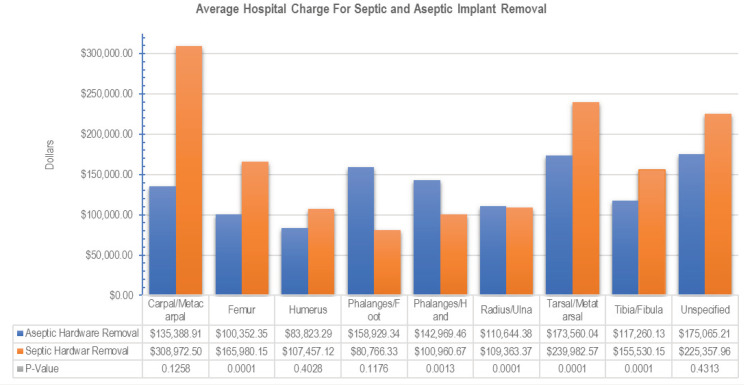
Hospital Charges
Patients undergoing removal of implant due to infection had a higher total charge associated with their episode of care (mean: $166,041) than non-infection related implant removal (mean: $133,110) [Figure 7]. The greatest average of total charges for infection-related implant removal was seen with carpal/metacarpal ($308,973), and for non-infectious implant removal was seen with tarsal metatarsal ($173,560). The greatest difference in mean total charges for infection-related versus non-infection related implant removal was seen between carpal/metacarpal removals ($173,586, $308,973 vs. $135,389).
Figure 7.
Hospital Charges following Aseptic versus Septic Implant Removal
Discussion
Postoperative infection is a significant source of morbidity and mortality leading to poor functional outcomes, and places significant strain on the global healthcare system resources (24,25). Implant infections are a common complication after ORIF, but few studies have examined the trends and predictors of implant infection in these patients, with the available studies suggesting ORIF implant infection rates exceeding periprosthetic joint infection rates in arthroplasty patients(26–31). Our study investigated the patients undergoing ORIF, and the impact of infection on the need for implant removal with the goal of determining the incidence, trends, economic burden, and predictors of implant infection following ORIF.
Complications after open reduction and internal fixation are an incredibly common postoperative problem orthopaedic surgeons contend with daily (2,28,29,32–36). While some of these complications can be managed conservatively, certain complications, such as infection or implant irritation, benefit from removal of the implant. The overall rate of implant removal is high, 13-27%, with removal of implant accounting for nearly 6% of orthopaedic procedures (37–40). One such reason for removal of implant, especially in the hands (carpal, metacarpals, and phalanges) is due to patient’s feeling stiffness in the area near the implant, tendon disruption, poor healing, and infection (41). While infection can occur with any implantable device, infection of implant following ORIF is particularly devastating and can lead to significant morbidity, including amputation or permanent disability (6,7,10,42). Multiple factors contribute to a patients risk implant infection following ORIF, including the location of the fractures, medical comorbidities like lupus and rheumatic disease, and if the fracture was open or closed (13,29,43–45). Furthermore, comorbidities or medications that impair wound healing can further slow healing already impaired by the fracture, increasing the risk of developing a surgical site infection, implant infection, or pin site infection(33). While antibiotic therapy can treat minor infections, definitive treatment in most patients requires removal of the implant(25). Fracture location is an important variable contributing to implant infection. Lower extremity fractures, particularly in the ankle and the tibial plateau, have incredibly high rates of postoperative wound complications (28,30). Fortunately, several studies have found the rate of implant removal and implant removal for infection, to be decreasing over the previous two decades(39,40). Our study results are in line with the literature, finding the rate of ORIF procedures, the rate of implant removal and infection-related implant removal to have decreased during the study period. Additionally, our study results were similar to the literature finding the highest removal rates due infection of the implant seen following carpal/metacarpal and phalanges/hand fracture ORIF.
The decrease in need for removal of implant, and the reduction in rate of infection-related implant is most likely due to advances and improvements in pre/peri/postoperative management of these patients. The results of our study also highlighted multiple predisposing factors to implant removal due to infection following ORIF. The medical comorbidities, including diabetes mellitus, liver disease, and rheumatoid arthritis, are well known risk factors for postoperative infection. Diabetes mellitus results is a well-known risk factor for complication due to immune dysfunction in the setting of hyperglycemic environments, and impaired wound healing (13,45). Liver disease is also a well-established risk factor for postoperative infections (46). Management of rheumatological conditions poses a nebulous decision for both the patient and the surgeon as not only can the rheumatological conditions themselves lead to increased risk of infection, the treatment modalities commonly used also can increase the risk of infection (43,47,48). These comorbidities make these patients less than ideal candidates for surgical repair, especially if treatment will be ORIF of the tibia or of tarsal fractures. However, the nature of these injuries often requires surgery for definitive management without long term functional decline and disability (49,50). The protective role of female gender being associated with decreased rates of implant removal due to infection remains controversial. Multiple studies have reported conflicting findings, with some showing female gender to decrease risk of infection, and others showing higher rates of infection (10,51–54). The role of gender is theorized to be in part to differences in sex hormone levels, particularly testosterone. Testosterone has been shown to have immune-modulatory and immune-suppressive effects, ultimately leading to a less robust antibody and immune response to infection in men than in females (55,56).
While we believe our study has the potential to have a positive impact with regards to infection-related implant removal, we understand it is not without limitations. The utilization of a national database provided a multi-year, incredibly comprehensive pool of data from institutions across the country. However, large databases have inherent errors within the systems that can lead to errors when analyzing the data (57). For this reason, the NIS was chosen in place of the American College of Surgeons National Surgical Quality Improvement Program and National Hospital Discharge Survey, as these databases have lower reports of in-hospital morbidity (58). Furthermore, there remains discrepancies between different databases regarding incidence of injuries and procedures (16). Another limitation is the inability to capture the removal of implant in all patients undergoing this procedure as an outpatient. However, it is our belief that most patients undergoing implant removal, especially when due to infection of the implant, will have the procedure done as an impatient. Lastly, the ICD-9 coding system does not differentiate the specific location of the ORIF procedure or removal of the implant, yielding only general locations.
Despite these limitations, we believe our study has several strengths. The main strength of our study is the review of more than 900,000 implants associated with multiple types of fractures. Our studies analyzed the trends of implant removal due to aseptic and septic indications in fracture in all the extremities. The additionally analysis of medical comorbidities, hospital factors, and financial data associated with each episode of care creates a comprehensive study that provides a comprehensive epidemiological analysis of implant removal following ORIF. The current study provides a multi-year analysis of a large national database assessing the trends in ORIF procedures, and aseptic and septic removal of implant following ORIF for eight fracture locations. The results indicate the highest rate of infection-related removal of implant is seen following ORIF of tarsal and tibial fractures. Lastly, the study reinforced the current literature indicating the increased risk of infection associated with diabetes mellitus, liver disease, and rheumatological conditions.
Implant removal rates due to infection decreased in all fractures except radial/ulnar fractures. Diabetes, liver disease, obesity, anemia, depression, and rheumatoid arthritis were significant predictors of infection-related implant removal. Identification of the trends and predictors of implant-related infection is only a first step. These medical conditions must be appropriately managed medically, and further studies investigating possible “best practice” guidelines for medical co-management and optimization of these patients are necessary in order to decrease their risk for implant-related infection.
Funding:
No funding was received for this research study. We have no conflicts of interest to disclose.
References
- 1.S D I. Complications and hardware removal after open reduction and internal fixation of humeral fractures. J Trauma J Trauma . 2011;70(5):1273–8. doi: 10.1097/TA.0b013e318215bedd. [DOI] [PubMed] [Google Scholar]
- 2.Beharrie AW, Beredjiklian PK, Bozentka DJ. Functional outcomes after open reduction and internal fixation for treatment of displaced distal radius fractures in patients over 60 years of age. J Orthop Trauma. 2004 Dec;18(10):680–6. doi: 10.1097/00005131-200411000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Chirodian N, Arch B, Parker MJ. Sliding hip screw fixation of trochanteric hip fractures: Outcome of 1024 procedures. Injury [Internet]. 2005 Jun;36(6):793–800. doi: 10.1016/j.injury.2005.01.017. [DOI] [PubMed] [Google Scholar]
- 4.Grawe B, Le T, Lee T, Wyrick J. Open Reduction and Internal Fixation (ORIF) of Complex 3- and 4-Part Fractures of the Proximal Humerus: Does Age Really Matter? Geriatr Orthop Surg Rehabil. 2012 Mar;3(1):27–32. doi: 10.1177/2151458511430662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Südkamp N, Bayer J, Hepp P, Voigt C, Oestern H, Kääb M, et al. Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate Results of a prospective, multicenter, observational study. J Bone Joint Surg Am. 2009 Jun;91(6):1320–8. doi: 10.2106/JBJS.H.00006. [DOI] [PubMed] [Google Scholar]
- 6.Metsemakers WJ, Kuehl R, Moriarty TF, Richards RG, Verhofstad MHJ, Borens O, et al. Infection after fracture fixation: Current surgical and microbiological concepts. Injury [Internet]. 2018 Mar;49(3):511–22. doi: 10.1016/j.injury.2016.09.019. [DOI] [PubMed] [Google Scholar]
- 7.Rightmire E, Zurakowski D, Vrahas M. Acute Infections After Fracture Repair. Clin Orthop Relat Res [Internet]. 2008 Feb;466(2):466–72. doi: 10.1007/s11999-007-0053-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chitnis AS, Vanderkarr M, Sparks C, McGlohorn J, Holy CE. Complications, Health Care Resource Utilization and Costs Associated with Type III Open Fractures of the Tibial Shaft Requiring Open Reduction and Internal Fixation. Value in Health [Internet]. 2018 May;21:S177. [Google Scholar]
- 9.Uhthoff HK, Poitras P, Backman DS. Internal plate fixation of fractures: short history and recent developments. J Orthop Sci [Internet]. 2006 Mar;11(2):118–26. doi: 10.1007/s00776-005-0984-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rasouli MR, Viola J, Maltenfort MG, Shahi A, Parvizi J, Krieg JC. Hardware Removal Due to Infection after Open Reduction and Internal Fixation: Trends and Predictors. Arch Bone Jt Surg [Internet]. 2015 Jul;3(3):184–92. [PMC free article] [PubMed] [Google Scholar]
- 11.Otchwemah R, Grams V, Tjardes T, Shafizadeh S, Bäthis H, Maegele M, et al. Bacterial contamination of open fractures - pathogens, antibiotic resistances and therapeutic regimes in four hospitals of the trauma network Cologne, Germany. Injury. 2015 Oct;46(108):S104–S108. doi: 10.1016/S0020-1383(15)30027-9. [DOI] [PubMed] [Google Scholar]
- 12.Calkins TE, Culvern C, Nam D, Gerlinger TL, Levine BR, Sporer SM, et al. Dilute Betadine Lavage Reduces the Risk of Acute Postoperative Periprosthetic Joint Infection in Aseptic Revision Total Knee and Hip Arthroplasty: A Randomized Controlled Trial. J Arthroplasty. 2020 Feb;35(2):538–543. doi: 10.1016/j.arth.2019.09.011. [DOI] [PubMed] [Google Scholar]
- 13.Casqueiro J, Casqueiro J, Alves C. Infections in patients with diabetes mellitus: A review of pathogenesis. Indian J Endocrinol Metab. 2012 Mar;16 Suppl 1:S27–36. doi: 10.4103/2230-8210.94253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meidani M, Naeini AE, Rostami M, Sherkat R, Tayeri K. Immunocompromised patients: Review of the most common infections happened in 446 hospitalized patients. J Res Med Sci. 2014 Mar;19(Suppl 1):S71–73. [PMC free article] [PubMed] [Google Scholar]
- 15.Healthcare Cost and Utilization Project (HCUP) [Internet] [[cited 2019 Sep 14]]. Available from: https://www.ahrq.gov/data/hcup/index.html.
- 16.Bohl DD, Basques BA, Golinvaux NS, Baumgaertner MR, Grauer JN. Nationwide Inpatient Sample and National Surgical Quality Improvement Program give different results in hip fracture studies. Clin Orthop Relat Res. 2014 Jun;472(6):1672–80. doi: 10.1007/s11999-014-3559-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Census.gov [Internet] [ [cited 2020 Feb 16]]. Available from: https://www.census.gov.
- 18.Lovald S, Mercer D, Hanson J, Cowgill I, Erdman M, Robinson P, et al. Hardware removal after fracture fixation procedures in the femur. J Trauma Acute Care Surg. 2012 Jan;72(1):282–7. doi: 10.1097/TA.0b013e318219fea9. [DOI] [PubMed] [Google Scholar]
- 19.ICD-9-CM Volume 1 Diagnosis Codes [Internet] [[cited 2020 Jan 19]]. Available from: http://www.icd9data.com/2015/Volume1/default.htm.
- 20.Ranson WA, Neifert SN, Cheung ZB, Mikhail CM, Caridi JM, Cho SK. Predicting In-Hospital Complications After Anterior Cervical Discectomy and Fusion: A Comparison of the Elixhauser and Charlson Comorbidity Indices. World Neurosurg. 2020 Feb;:134:e487–96. doi: 10.1016/j.wneu.2019.10.102. [DOI] [PubMed] [Google Scholar]
- 21.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998 Jan;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 23.CPI Inflation Calculator [Internet] [[cited 2020 Nov 27]]. Available from: https://www.bls.gov/data/inflation_calculator.htm.
- 24.Helwig P, Morlock J, Oberst M, Hauschild O, Hübner J, Borde J, et al. Periprosthetic joint infection--effect on quality of life. Int Orthop. 2014 May;38(5):1077–81. doi: 10.1007/s00264-013-2265-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Darouiche RO. Treatment of Infections Associated with Surgical Implants. http://dx.doi.org/101056/NEJMra035415 [Internet]. 2009 Oct 8. [[cited 2020 Apr 7]]. Available from: https://www.nejm.org/doi/pdf/10.1056/NEJMra035415.
- 26.Zalavras CG, Christensen T, Rigopoulos N, Holtom P, Patzakis MJ. Infection following operative treatment of ankle fractures. Clin Orthop Relat Res. 2009 Jul;467(7):1715–20. doi: 10.1007/s11999-009-0743-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Younger AS, Duncan CP, Masri BA. Treatment of infection associated with segmental bone loss in the proximal part of the femur in two stages with use of an antibiotic-loaded interval prosthesis. J Bone Joint Surg Am. 1998 Jan;80(1):60–9. doi: 10.2106/00004623-199801000-00011. [DOI] [PubMed] [Google Scholar]
- 28.Momaya AM, Hlavacek J, Etier B, Johannesmeyer D, Oladeji LO, Niemeier TE, et al. Risk factors for infection after operative fixation of Tibial plateau fractures. Injury. 2016 Jul;47(7):1501–5. doi: 10.1016/j.injury.2016.04.011. [DOI] [PubMed] [Google Scholar]
- 29.Morris BJ, Unger RZ, Archer KR, Mathis SL, Perdue AM, Obremskey WT. Risk factors of infection after ORIF of bicondylar tibial plateau fractures. J Orthop Trauma. 2013 Sep;27(9):e196–200. doi: 10.1097/BOT.0b013e318284704e. [DOI] [PubMed] [Google Scholar]
- 30.Henkelmann R, Frosch K-H, Glaab R, Lill H, Schoepp C, Seybold D, et al. Infection following fractures of the proximal tibia - a systematic review of incidence and outcome. BMC Musculoskelet Disord. 2017 Nov;18(1):481. doi: 10.1186/s12891-017-1847-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shahi A, Kheir MM, Tarabichi M, Hosseinzadeh HRS, Tan TL, Parvizi J. Serum D-Dimer Test Is Promising for the Diagnosis of Periprosthetic Joint Infection and Timing of Reimplantation. J Bone Joint Surg Am. 2017 Sep;99(17):1419–27. doi: 10.2106/JBJS.16.01395. [DOI] [PubMed] [Google Scholar]
- 32.Lovald S, Mercer D, Hanson J, Cowgill I, Erdman M, Robinson P, et al. Complications and hardware removal after open reduction and internal fixation of humeral fractures. J Trauma. 2011 May;70(5):1273–7; discussion 1277–1278. doi: 10.1097/TA.0b013e318215bedd. [DOI] [PubMed] [Google Scholar]
- 33.Chung KC, Mathews AL. Management of Complications of Distal Radius Fractures. Hand Clin [Internet]. 2015 May;31(2):205–15. doi: 10.1016/j.hcl.2014.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Macera A, Carulli C, Sirleo L, Innocenti M. Postoperative Complications and Reoperation Rates Following Open Reduction and Internal Fixation of Ankle Fracture. Joints [Internet]. 2018 May;6(2):110–5. doi: 10.1055/s-0038-1653949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Leroux T, Wasserstein D, Henry P, Khoshbin A, Dwyer T, Ogilvie-Harris D, et al. Rate of and Risk Factors for Reoperations After Open Reduction and Internal Fixation of Midshaft Clavicle Fractures: A Population-Based Study in Ontario, Canada. J Bone Joint Surg Am. 2014 Jul;96(13):1119–25. doi: 10.2106/JBJS.M.00607. [DOI] [PubMed] [Google Scholar]
- 36.Yasui Y, Shimozono Y, Hung CW, Marangon A, Wollstein A, Gianakos AL, et al. Postoperative Reoperations and Complications in 32,307 Ankle Fractures With and Without Concurrent Ankle Arthroscopic Procedures in a 5-Year Period Based on a Large U. S. Healthcare Database. J Foot Ankle Surg. 2019 Jan;58(1):6–9. doi: 10.1053/j.jfas.2018.03.030. [DOI] [PubMed] [Google Scholar]
- 37.Böstman O, Pihlajamäki H. Routine implant removal after fracture surgery: a potentially reducible consumer of hospital resources in trauma units. J Trauma. 1996 Nov;41(5):846–9. doi: 10.1097/00005373-199611000-00013. [DOI] [PubMed] [Google Scholar]
- 38.Naumann MG, Sigurdsen U, Utvåg SE, Stavem K. Incidence and risk factors for removal of an internal fixation following surgery for ankle fracture: A retrospective cohort study of 997 patients. Injury. 2016 Aug;47(8):1783–8. doi: 10.1016/j.injury.2016.05.011. [DOI] [PubMed] [Google Scholar]
- 39.Fenelon C, Murphy EP, Galbraith JG, Kearns SR. The burden of hardware removal in ankle fractures: How common is it, why do we do it and what is the cost? A ten-year review. Foot Ankle Surg. 2019 Aug;25(4):546–9. doi: 10.1016/j.fas.2018.05.006. [DOI] [PubMed] [Google Scholar]
- 40.Partio N, Huttunen TT, Mäenpää HM, Mattila VM. Reduced incidence and economic cost of hardware removal after ankle fracture surgery: a 20-year nationwide registry study. Acta Orthopaedica [Internet]. 2020 Feb;0(0):1–5. doi: 10.1080/17453674.2020.1733749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kollitz KM, Hammert WC, Vedder NB, Huang JI. Metacarpal fractures: treatment and complications. Hand (N Y) [Internet]. 2014 Mar;9(1):16–23. doi: 10.1007/s11552-013-9562-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bonnevialle P. Operative treatment of early infection after internal fixation of limb fractures (exclusive of severe open fractures) Orthopaedics & Traumatology: Surgery & Research [Internet]. 2017 Feb;103(1, Supplement):S67–73. doi: 10.1016/j.otsr.2016.06.019. [DOI] [PubMed] [Google Scholar]
- 43.Botha-Scheepers SA, Sarembock B. Infections in the management of rheumatic diseases: An update. S Afr Med J. 2015 Dec;105(12):1076. doi: 10.7196/samj.2015.v105i12.10220. [DOI] [PubMed] [Google Scholar]
- 44.Xu Y-Q, Zhu Y-L, Fan X-Y, Jin T, Li Y, He X-Q. Implant-Related Infection in the Tibia: Surgical Revision Strategy with Vancomycin Cement [Internet] The Scientific World Journal. 2014:e124864. doi: 10.1155/2014/124864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lee D, Lee R, Gowda NB, Probasco WV, Stake S, Ibrahim G, et al. Impact of diabetes mellitus on surgical complications in patients undergoing revision total knee arthroplasty: Insulin dependence makes a difference. Journal of Clinical Orthopaedics and Trauma [Internet]. 2020 Jan;11(1):140–6. doi: 10.1016/j.jcot.2019.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cheruvattath R, Balan V. Infections in Patients With End-stage Liver Disease. J Clin Gastroenterol. 2007 Apr;41(4):403–11. doi: 10.1097/01.mcg.0000248018.08515.f9. [DOI] [PubMed] [Google Scholar]
- 47.Caporali R, Caprioli M, Bobbio-Pallavicini F, Montecucco C. DMARDS and infections in rheumatoid arthritis. Autoimmun Rev. 2008 Dec;8(2):139–43. doi: 10.1016/j.autrev.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 48.Lacaille D, Guh DP, Abrahamowicz M, Anis AH, Esdaile JM. Use of nonbiologic disease-modifying antirheumatic drugs and risk of infection in patients with rheumatoid arthritis. Arthritis Rheum. 2008 Aug;59(8):1074–81. doi: 10.1002/art.23913. [DOI] [PubMed] [Google Scholar]
- 49.MedicalAdvisoryBoard [Internet] [[cited 2020 Feb 16]]. Available from: https://www.courts.ri.gov/Courts/workerscompensationcourt/MedicalAdvisoryBoard/Pages/Protocols.aspx.
- 50.Manidakis N, Dosani A, Dimitriou R, Stengel D, Matthews S, Giannoudis P. Tibial plateau fractures: functional outcome and incidence of osteoarthritis in 125 cases. Int Orthop [Internet]. 2010 Apr;34(4):565–70. doi: 10.1007/s00264-009-0790-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cohen B, Choi YJ, Hyman S, Furuya EY, Neidell M, Larson E. Gender Differences in Risk of Bloodstream and Surgical Site Infections. J Gen Intern Med [Internet]. 2013 Oct;28(10):1318–25. doi: 10.1007/s11606-013-2421-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Namba RS, Inacio MCS, Paxton EW. Risk factors associated with surgical site infection in 30,491 primary total hip replacements. J Bone Joint Surg Br. 2012 Oct;94(10):1330–8. doi: 10.1302/0301-620X.94B10.29184. [DOI] [PubMed] [Google Scholar]
- 53.Li C, Renz N, Trampuz A. Management of Periprosthetic Joint Infection. Hip Pelvis [Internet]. 2018 Sep;30(3):138–46. doi: 10.5371/hp.2018.30.3.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Thangarajah T, Prasad PSV, Narayan B. Surgical Site Infections Following Open Reduction and Internal Fixation of Ankle Fractures. Open Orthop J [Internet]. 2009 Jul;:3:56–60. doi: 10.2174/1874325000903010056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Taneja V. Sex Hormones Determine Immune Response. Front Immunol [Internet]. 2018 Aug;:9. doi: 10.3389/fimmu.2018.01931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jørgensen TN. Sex disparities in the immune response. Cell Immunol. 2015 Apr;294(2):61–2. doi: 10.1016/j.cellimm.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 57.Memtsoudis SG. Limitations Associated with the Analysis of Data from Administrative Databases. Anesthes [Internet]. 2009 Aug;111(2):449–449. doi: 10.1097/ALN.0b013e3181adf739. [DOI] [PubMed] [Google Scholar]
- 58.Weis A, Anderson J, Chang D. Comparing the National Surgical Quality Improvement Program With the Nationwide Inpatient Sample Database | Research, Methods, Statistics | JAMA Surgery | JAMA Network [Internet] [[cited 2020 Jan 19]]. Available from: https://jamanetwork.com/journals/jamasurgery/fullarticle/2300997. [DOI] [PubMed]