Abstract
Background
Obesity is associated with stigma and discrimination. Health care providers should approach these patients professionally and without stigma, since treatment of obesity requires a relationship with mutual understanding between the doctor and patient.
Objective
To explore how patients and general practitioners (GPs) perceive obesity, using Q-methodology, which allows quantitative analysis of qualitative data.
Methods
A Q-methodology study, comprising 24 patients with obesity and 24 GPs. We created 48 statements with viewpoints on obesity. All participants sorted these statements in a forced grid with a quasi-normal distribution ranking from −5 (most disagree) to +5 (most agree). Subsequently, factor analysis was performed. Six patients were interviewed to explain their viewpoints.
Results
Analysis yielded 3 dominant groups (factors) of patients: (i) They acknowledge the importance of healthy lifestyle and feel mistreated by health care. (ii) They have a decreased quality of life, but do not blame health care, and (iii) They don’t need treatment and don’t have an impaired quality of life. For the GPs, the 3 dominant factors were: (i) They have understanding for the patients and feel that health care is insufficient, (ii) They believe that obesity may be hereditary but mainly is a lifestyle problem, and (iii) They believe obesity can be treated but is very difficult.
Conclusions
Viewpoints on obesity were different, both within and between the groups. Some GPs consider obesity mainly as a lifestyle problem, rather than a chronic disease. If patients and doctors can find mutual viewpoints on obesity, both patient satisfaction and a treatment strategy will be more effective.
Keywords: factor analysis (statistical), health communication, obesity, patient satisfaction, primary health care, qualitative research
Key messages.
Viewpoints on obesity differ, both within and between patients and GPs.
Different subgroups of viewpoints on obesity can be identified with Q-methodology.
Some GPs consider obesity a lifestyle problem, rather than a chronic disease.
Q-method is suitable for investigating subjective experiences and perspectives.
Introduction
The misconception that obesity is a lifestyle choice, that can be reversed simply by exercising willpower, has become cemented in the minds of the general public and much of the medical profession. However, obesity has now been acknowledged by the European Commission as a disease in its own right.1 The obesity pandemic is getting worse in both adults and children and adolescents.2 In Sweden, 15% of women and 16% of men suffer from obesity.3 It is a complex chronic metabolic disease with a multifactorial pathogenesis,4 associated with type 2 diabetes mellitus, nonalcoholic fatty liver disease, cardiovascular diseases, and different types of cancer.5 In addition, obesity has consequences for mental health as a result of weight stigma and discrimination, and may lead to social isolation.6 Current treatments for obesity comprise lifestyle changes including diet and exercise, drugs, psychotherapy, and bariatric surgery.7
The general practitioner (GP) is often the first doctor who meets the patient with obesity-related problems. However, as mentioned above, many GPs do not consider obesity as a serious medical condition that requires treatment,8 but rather as a lifestyle problem. This discrepancy has a negative impact on the relationship between doctors and patients. In addition, there is scepticism regarding the treatment options for obesity, but GPs still recommended them in order to maintain a good relationship with the patient.9 Previous research demonstrates the importance of good communication between GPs and patients to increase the probability that an intervention will become successful.10
One method to study people’s perspectives on a certain topic is via Q-methodology, which is a combined qualitative and quantitative method for investigating subjectivity.11,12 This method is well-established in the social sciences, but remains a relatively novel approach in the medical sciences. It provides a systematic procedure for examining the subjective components of human behaviour, where all the viewpoints of the subjects are clustered into different groups, called factors.11
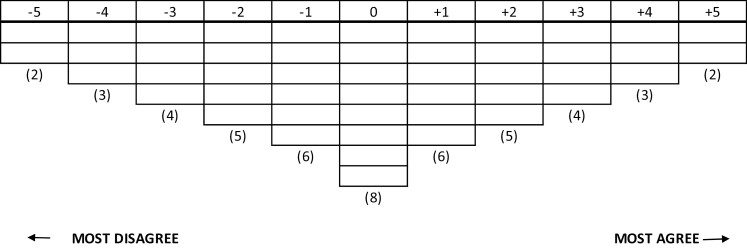
Firstly, the researcher gathers all kinds of opinions, beliefs, and information about a topic from different sources, such as previous research and interviews13 and creates statements about the topic. This is followed by an evaluation of the statements, performed by a group of experts within the topic, to increase the value and content, but also to minimize researcher bias. This evaluation leads to the creation of a so-called Q-set; the final set of statements that will be used. Secondly, the study population is selected, and the viewpoints of the participants should match the research question.14 Subsequently, the participants rank the statements from their individual perspective using a grid with a quasi-normal, forced distribution (see Fig. 1). The grid has the same number of cells as there are statements and has a rating scale from −5 to +5 which represents “most disagree” to “most agree.” All statements must be placed in the grid.11 In addition, qualitative information can be collected by interviewing participants about their most extreme rankings. When the ranking is completed, all responses are reduced to a few different factors.14 Each factor represents a distinct group of participants who share similar views.12 The number of extracted factors is usually between 3 and 6.14 Thereafter, a factor rotation is performed to make the factors more explainable. Each factor provides information that defines that factor.11
Fig. 1.
Score grid for Q-sorting.
The aim of our study was to analyse both the patients and the GPs perceptions about obesity using Q-methodology, and to compare them with each other.
Methods
Setting and data sources
We searched for opinions and viewpoints on obesity in different articles and in forums. This led to 52 statements. An expert group from the Obesity Unit (consisting of a doctor, a nurse, a dietician, a psychologist, and a physiotherapist) evaluated these statements and selected a Q-set comprising 48 statements. We transferred the Q-set to www.qmethodsoftware.com, and evaluated the statements to confirm that the language was understandable and that the Q-set could be distributed within the forced-choice grid without conflicts.
Twenty-four doctors, all GPs or GP residents (16 men and 8 women), and 24 patients with obesity (21 women and 3 men) were included. The number of participants is based on the convention that 1 needs roughly half as many participants as there are statements. Patients with obesity were recruited face to face via the obesity unit of the University hospital in Örebro. The participating GPs were recruited during a local primary health care conference. The inclusion criteria for the patients were: (i) body mass index >30 kg/m2 and (ii) that they had not started with a weight-loss program provided by the Obesity Unit, since we did not want them to be influenced by the information that they would receive during this program. All participants were informed about the purpose and procedure of the study and signed an informed consent. There was no dropping-out. For the patients, the Q-methodology data were collected at the Obesity Unit, Örebro University Hospital. For the GPs, the Q-methodology data were collected at their workplace. No other individuals were present during the data collection. One member of the research team (KB, female, medical doctor) also consecutively interviewed 6 patients to obtain qualitative information about their most extreme rankings, and field notes were made. No standard questionnaire was used for the interviews. The transcripts were not returned to the patients but were verified directly on the spot. Each interview took approximately 30 min. There was no earlier relationship between the participants and the research group. The research group was not biased in any way with respect to viewpoints regarding obesity.
Data analysis
Two members from the research team (QS and KB) imported the anonymized results in PQMethod software.8 The first step in the analysis was data reduction to summarize factors based on principal component analysis (PCA). The factors were extracted from both the patient and the GP group. We calculated the Z-scores, based on the factor scores from the PCA for every statement, which represented how much each factor agreed or disagreed on every statement.12 A Pearson’s correlation analysis was performed (SPSS Statistics version 25, IBM Corp, Armonk, NY) to compare the 2 groups, using the Z-scores from every statement from the patient and GP factors.
Results
We extracted 3 different factors from each group. Each factor represented a general viewpoint and was named after their distinguishing statements, as shown in Tables 1 and 2. Correlations between Z-scores for each statement between all factors are presented in Table 3.
Table 1.
Distinguishing statements for the patient factors and their rank scores.
| Factor | Statement | Factor 1 | Factor 2 | Factor 3 |
|---|---|---|---|---|
| Patient factor 1 | 41. Health care providers treat patients with obesity worse than those without | 5 | −1 | 1 |
| 7. Individuals with obesity have knowledge about healthy food | 2 | −1 | 0 | |
| 9. Individuals with obesity understand the importance of eating healthy | 2 | 0 | 0 | |
| 43. Individuals with obesity have an impaired quality of life | 1 | 4 | −2 | |
| 17. Regular meals protect against obesity | 0 | 1 | 2 | |
| 19. At least 30 min physical activity per day protects against weight gain | 0 | 2 | 2 | |
| 1. Obesity can be prevented | 0 | 2 | 5 | |
| 15. By reducing energy-rich food, weight loss will occur | −1 | 1 | 2 | |
| 8. Individuals with obesity have healthy food habits | −1 | −5 | 1 | |
| 13. Obesity is more common among people with higher education and income | −2 | −3 | −5 | |
| 48. Individuals with obesity who increase their physical activity lose weight | −2 | 3 | 1 | |
| Patient factor 2 | 43. Individuals with obesity have an impaired quality of life | 1 | 4 | −2 |
| 28. Early childhood is the time when food- and exercise habits are established | 0 | 3 | 0 | |
| 30. If you have parents who have obesity, you will develop obesity yourself | −1 | 1 | −2 | |
| 47. Individuals with obesity receive enough support from healthcare | −4 | 0 | −3 | |
| 44. Use of certain drugs leads to obesity | 2 | 0 | 4 | |
| 36. Individuals with obesity have knowledge about the risks with obesity | 3 | 0 | 3 | |
| 40. Doctors have too little knowledge about obesity | 3 | −1 | 2 | |
| 41. Health care providers treat patients with obesity worse than those without | 5 | −1 | 1 | |
| 24. Alcohol consumption does not increase the risk of weight gain | −1 | −2 | 0 | |
| 46. Weight loss does not provide increased quality of life | 0 | −4 | 1 | |
| 8. Individuals with obesity have healthy food habits | −1 | −5 | 1 | |
| Patient factor 3 | 21. Physical activity improves health regardless of weight | 3 | 2 | 5 |
| 5. Obesity is not hereditary | −2 | −2 | 3 | |
| 18. Obesity is often used as an excuse for not exercising | −3 | −1 | 1 | |
| 8. Individuals with obesity have healthy food habits | −1 | −5 | 1 | |
| 41. Health care providers treat patients with obesity worse than those without | 5 | −1 | 1 | |
| 3. Obesity is a person’s own choice | −5 | −4 | 0 | |
| 34. Individuals with obesity need treatment | 2 | 3 | −1 | |
| 37. Individuals with obesity are not interested in their weight | −4 | −3 | −1 | |
| 39. Abuse in childhood increases the risk of obesity | 1 | 1 | −1 | |
| 43. Individuals with obesity have an impaired quality of life | 1 | 4 | −2 | |
| 45. Obesity is an eating disorder | 1 | 0 | −3 | |
| 38. Individuals with obesity often feel bad mentally | 4 | 4 | −4 | |
| 33. Obesity is a lifelong disease | 1 | 1 | −4 |
Bold value shows the rank score of significant statements for the specified patient factor.
Table 2.
Distinguishing statements for the GP factors and their rank scores.
| Factor | Statement | Factor 1 | Factor 2 | Factor 3 |
|---|---|---|---|---|
| GP factor 1 | 41. Health care providers treats patients with obesity worse than those without weight problem | 3 | −3 | −2 |
| 9. Individuals with obesity understand the importance of eating healthy | 2 | 0 | 0 | |
| 40. Doctors have too little knowledge about obesity | 1 | −1 | −1 | |
| 35. There is no effective treatment for obesity | 0 | −2 | −4 | |
| 48. Individuals with obesity who increase their exercise will lose weight | −2 | 3 | 0 | |
| 37. Individuals with obesity are not interested of their weight | −4 | −1 | −2 | |
| 3. Obesity is a person’s own choice | −4 | 0 | 0 | |
| GP factor 2 | 45. Obesity is an eating disorder | −1 | 4 | −2 |
| 48. Individuals with obesity who increase their exercise will lose weight | −2 | 3 | 0 | |
| 23. Smoking increases the risk of weight gain | −1 | 1 | −3 | |
| 25. The public judges individuals with obesity | 4 | 1 | 4 | |
| 13. Obesity is more common among people with higher education and income | −5 | 0 | −5 | |
| 26. To lose weight is easy | −5 | −2 | −4 | |
| 7. Individuals with obesity have knowledge about healthy food | 0 | −2 | 2 | |
| 24. Alcohol consumption does not increase the risk of weight gain | −2 | −4 | −2 | |
| 5. Obesity is not hereditary | −2 | −5 | −3 | |
| GP factor 3 | 11. It is enough to change food habits to lose weight | −1 | −3 | 2 |
| 46. Weight loss does not provide increased quality of life | −3 | −4 | 0 | |
| 48. Individuals with obesity who increase their exercise will lose weight | −2 | 3 | 0 | |
| 17. Regular meals protect against obesity | 2 | 3 | 0 | |
| 33. Obesity is a lifelong disease | 1 | 2 | −1 | |
| 6. Individuals with obesity have an unhealthy lifestyle | −2 | −1 | −4 | |
| 32. 5–10% weight loss is not enough to live longer | −3 | −1 | −5 |
Bold value shows the rank score of significant statements for the specified patient factor.
Table 3.
Correlations between Z-scores for each statement between all factors according to Pearson’s correlation analysis (P values).
| Patient factor 1 | Patient factor 2 | Patient factor 3 | |
|---|---|---|---|
| GP factor 1 | 0.808 | 0.773 | 0.568 |
| GP factor 2 | 0.421 | 0.770 | 0.262 |
| GP factor 3 | 0.471 | 0.792 | 0.509 |
The table shows that the correlations between the factors varied. Patient factor 1 had the highest correlation (r = 0.808, P = <0.001) with GP factor 1. However, it has a weak correlation with other GP factors. Patient factor 2 correlated well with all GP factors, meanwhile, patient factor 3 had a moderate correlation with 2 GP factors and the lowest correlation with GP factor 2.
Table 4 shows the statements where the different patients and GP factors agreed and disagreed on most. The extracted factors from the patients explained 62% of the variance of the original Q-sorts and the extracted 3 factors from the GPs also explained 62% of the variance. In factor analysis, this is considered as a valid and acceptable proportion of variance explained by a construct.
Table 4.
Statements where the different patients and GP factors agreed and disagreed on most.
| Group and factor number | Significantly loaded statements | Z-Score |
|---|---|---|
| Patients factor 1 | 25. The public judges individuals with obesity | 1.617 |
| 41. Health care providers treat patients with obesity worse than those without | 1.516 | |
| 27. To keep the weight stable after weight loss is difficult | 1.384 | |
| 2. Individuals with obesity are lazy | −1.830 | |
| 3. Obesity is a person’s own choice | −1.941 | |
| 42. Individuals with obesity do not want to lose weight | −2.061 | |
| Patients factor 2 | 27. To keep the weight stable after weight loss is difficult | 1.900 |
| 25. The public judges individuals with obesity | 1.573 | |
| 14. Obesity is a disease with several different causes | 1.474 | |
| 10. Snacks eating do not lead to obesity | −1.435 | |
| 8. Individuals with obesity have healthy food habits | −1.462 | |
| 26. To lose weight is easy | −1.960 | |
| Patients factor 3 | 21. Physical activity improves health regardless of weight | 1.857 |
| 1. Obesity can be prevented | 1.569 | |
| 44. Use of certain drugs leads to obesity | 1.445 | |
| 33. Obesity is a lifelong disease | −1.522 | |
| 13. Obesity is more common among people with higher education and income | −1.584 | |
| 26. To lose weight is easy | −1.778 | |
| GPs factor 1 | 21. Physical activity improves health, regardless of weight | 2.019 |
| 27. To keep the weight stable after weight loss is difficult | 1.637 | |
| 44. Use of certain drugs leads to obesity | 1.360 | |
| 42. Individuals with obesity do not want to lose weight | −1.529 | |
| 26. To lose weight is easy | −1.627 | |
| 13. Obesity is more common among people with higher education and income | −1.807 | |
| GPs factor 2 | 21. Physical activity improves health, regardless of weight | 2.079 |
| 14. Obesity is a disease with several different causes | 2.052 | |
| 28. Early childhood is the time where food- and exercise habits are developed | 1.323 | |
| 24. Alcohol consumption does not increase the risk of weight gain | −1.688 | |
| 5. Obesity is not hereditary | −1.914 | |
| 22. Stress does not increase the risk of weight gain | −2.001 | |
| GPs factor 3 | 21. Physical activity improves health, regardless of weight | 1.996 |
| 27. To keep the weight stable after weight loss is difficult | 1.860 | |
| 25. The public judges individuals with obesity | 1.594 | |
| 26. To lose weight is easy | −1.742 | |
| 32. 5–10% weight loss is not enough to live longer | −1.849 | |
| 13. Obesity is more common among people with higher education and income | −2.014 |
The table shows the similarities and differences between the patient factors and GP factors. Among the patients, many personal statements were ranked highly. Among the GPs, medical facts about obesity were ranked highly. The majority disagreed with statement 26 and the majority agreed with statement 27. All GP factors and 1 patient factor agreed the most with statement 21, meanwhile 2 patient factors and 1 GP factor ranked statement 25 very highly.
Factor 1 (patients): have knowledge about healthy food- and exercise habits and feel mistreated by health care providers
Nine patients showed knowledge about lifestyle changes that lead to weight loss but they do not have good experiences with these lifestyle changes. In contrast to the other patients’ viewpoints, these patients strongly feel that health care is mistreating them.
One patient said:
I received documentation about a gastric bypass when I sought care for a urinary tract infection. They only think that I have to train more, eat a low-calorie diet or should have a gastric bypass. You do not get help or support for anything else.
Factor 2 (patients): suffering from obesity for a long time but do not blame health care providers
Seven patients with obesity highlighted that early childhood is the time when food- and exercise habits are developed and that there is a hereditary component. These patients confirm that obesity affects their quality of life. They believe that doctors have sufficient knowledge about obesity and that they receive support from health care providers. One patient said:
“I have had problems with my weight and hypothyroidism since birth and even though I am told to eat right and despite doing so, you are criticized that you do not. Throughout my whole childhood, I have eaten according to the plate model but I am still not properly treated.”
This patient explained that she felt criticized by her environment and although she felt that she was not treated adequately, she understood how difficult it is to treat obesity.
Factor 3 (patients): do not think that obesity has an impact on the quality of life and do not think they need any help
Five patients believed that obesity does not affect the quality of life and that it is not a hereditary condition. Although they are aware of their condition, they do not think they need treatment, and in contrast to other viewpoints, they do not think that obesity is a lifelong disease. One patient said:
I think obesity depends on many things, both medications but also life situation. I think that if you look backward and look when you became obese, you can relate it to something that happened during that time.
Factor 1 (GP): understand the patients and believe that health care provides insufficient support
Ten doctors believed they have insufficient knowledge about obesity and that health care providers treat the patients with obesity worse than those without obesity. There is a certain understanding for these patients. Distinguishing for this viewpoint is that they are not sure whether there is an effective treatment for obesity.
Factor 2 (GP): believe that obesity is hereditary and an eating disorder
Four doctors believed that obesity is an eating disorder, as well as a hereditary condition. They agreed the least with the statement that people with obesity are negatively judged and disagreed the least with the statement that losing weight is easy.
Factor 3 (GPs): obesity is not a lifelong disease but it is difficult to lose weight
Seven doctors believed that patients with obesity have a healthy lifestyle and that it is sufficient to change food habits to lose weight. However, they do not have an opinion regarding whether weight loss increases the quality of life or whether exercise leads to weight loss. Distinguishing from the other viewpoints, they believe that obesity is not a lifelong disease.
Discussion
Several studies have shown the importance of good communication between GPs and patients.10 In our study we focussed on the different perspectives on obesity both within and between GPs and patients. Our findings show some differences and similarities in ranking between the distinguishing statements for the patients and GPs, leading to 6 different factors on obesity. Three factors from patients and 3 factors from GPs were considered important in this study.
Comparison to existing literature
Patient factor 1 underlined their belief of the importance of combining diet and exercise for an effective weight loss15 even though other studies suggest that also behavioural strategies such as self-monitoring are required for a successful result.16 Besides that, this group agreed strongly on the statement that health care providers treat patients with obesity worse than those without obesity, which the other groups did not. This patient factor had a high correlation with GP factor 1. The correlation between patient factor 1 and the other GP factors was much lower, which may be explained by the fact that these GPs did not highlight statements that were associated with discrimination and lack of knowledge about obesity. Instead, they highlighted medical facts about obesity, which these patients did not take into consideration.
In patient factor 2, this group seemed to have struggled with obesity for a long time and they were unsure whether health care providers could do more for them. This patient group believed that patients with obesity have unhealthy eating habits, and they were neutral about their knowledge regarding obesity-associated health risks. They confirmed that doctors have adequate knowledge about obesity, and did not feel that they were treated any differently than patients without obesity. This is in line with studies in which patients with obesity reported positive experiences with health care.17 They also confirmed that obesity has an impact on quality of life, thus confirming previous research regarding the relationship between obesity and a decreased quality of life.18 This viewpoint had a similar correlation with all the GP viewpoints, which means that they share similar opinions about these statements.
Patient factor 3 differed from the other patient factors and showed a believe that patients with obesity neither need treatment, nor have an impaired quality of life. This shows that there are patients with obesity who are less affected by their condition. These patients strongly disagreed on the statement that patients with obesity suffer from impaired mental health, although previous studies demonstrate that obesity and depression often coexist and are interrelated.19,20 They also disagreed on the statement that obesity is a hereditary condition, and they were neutral about obesity as being a persons’ own choice, as well as that they agreed on that patients with obesity have healthy food habits. These patients neither seemed to feel bad about having obesity, nor did they want any help and nor did they consider obesity as a lifelong disease, which almost all other viewpoints did, except GP factor 3. Patient factor 3 had the lowest correlation with all GP viewpoints, especially with GP factor 2, who strongly agreed on obesity as an eating disorder and strongly agreed on obesity as a hereditary condition. Obviously, this group do not consider obesity as a chronic metabolic disease.
Strengths and limitations
We used a method that is well established in the social sciences, but remains a relatively novel approach in medical sciences. The major strength of this method is that Q-methodology allows statistical interpretation of qualitative data and provides a powerful method to investigate differences and similarities in viewpoints between doctors and patients regarding their condition.
There are some limitations. Selection bias may have been introduced. The GPs who participated may have been more interested in obesity and were motivated to make a change, compared with the GPs that did not choose to participate. Secondly, the participating patients may have had more negative experiences with health care providers and they may experience a more impaired health and participated for this reason.
Conclusions
We showed that viewpoints on obesity are different, both within and between patients and GPs. A patient may have completely different viewpoints regarding his/her condition than the GP. Some GPs show viewpoints that are not supported by the current knowledge, such as considering obesity mainly as a lifestyle problem, rather than a chronic disease. In addition, our findings show that a considerable number of patients feel stigmatized because of their obesity, and experience impaired quality of life. For these reasons, awareness of these differences is relevant for clinical practice; if the GP and the patient are able to find mutual viewpoints about obesity, patient satisfaction will improve and a treatment and/or support strategy will be more effective.
Acknowledgements
We thank the professionals at the Obesity Unit at the Örebro University Hospital for their support with the review of the Q-sort statements.
Contributor Information
Qays Shahed, Department of Internal Medicine, Faculty of Medicine and Health, Örebro University, Örebro, Sweden.
Karolina Baranowska, Department of Internal Medicine, Faculty of Medicine and Health, Örebro University, Örebro, Sweden.
Marije C Galavazi, Department of Internal Medicine, Faculty of Medicine and Health, Örebro University, Örebro, Sweden.
Yang Cao, Department of Clinical Epidemiology and Biostatistics, School of Medical Sciences, Örebro University, Örebro, Sweden.
Michiel A van Nieuwenhoven, Department of Internal Medicine, Division of Gastroenterology, Faculty of Medicine and Health, Örebro University, Örebro, Sweden.
Funding
The study was funded by departmental resources.
Ethical approval
Ethical approval was granted by the Etikprövningsmyndigheten Uppsala (Dnr 2019-04756).
Conflict of interest
None declared.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
- 1. Burki T. European Commission classifies obesity as a chronic disease [published online ahead of print, 2021 Jun 1]. Lancet Diabetes Endocrinol. 2021;9(7):418. doi: 10.1016/S2213-8587(21)00145-5 [DOI] [PubMed] [Google Scholar]
- 2. Engin A. The definition and prevalence of obesity and metabolic syndrome. Adv Exp Med Biol. 2017;960:1–17. [DOI] [PubMed] [Google Scholar]
- 3. Statistik om övervikt och fetma—Folkhälsomyndigheten. n.d. Övervikt och fetma. [accessed 2020 Oct 22]. https://www.folkhalsomyndigheten.se/folkhalsorapportering-statistik/tolkad-rapportering/folkhalsans-utveckling/resultat/halsa/overvikt-och-fetma/ [Google Scholar]
- 4. Manna P, Jain SK. Obesity, oxidative stress, adipose tissue dysfunction, and the associated health risks: causes and therapeutic strategies. Metab Syndr Relat Disord. 2015;13(10):423–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Goossens GH. The metabolic phenotype in obesity: fat mass, body fat distribution, and adipose tissue function. Obes Facts. 2017;10(3):207–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Brewis A, SturtzSreetharan C, Wutich A. Obesity stigma as a globalizing health challenge. Global Health. 2018;14(1):20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Natvik E, Råheim M, Andersen JR, Moltu C. Living a successful weight loss after severe obesity. Int J Qual Stud Health Well-being. 2018;13(1):1487762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Schwenke M, Luppa M, Welzel FD, Löbner M, Luck-Sikorski C, Kersting A, Blüher M, Riedel-Heller SG. Attitudes and treatment practice of general practitioners towards patients with obesity in primary care. BMC Fam Pract. 2020;21(1):169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Epstein L, Ogden J. A qualitative study of GPs’ views of treating obesity. Br J Gen Pract. 2005;55(519):750–754. [PMC free article] [PubMed] [Google Scholar]
- 10. Ogden J, Bandara I, Cohen H, Farmer D, Hardie J, Minas H, Moore J, Qureshi S, Walter F, Whitehead MA. General practitioners’ and patients’ models of obesity: whose problem is it? Patient Educ Couns. 2001;44(3):227–233. [DOI] [PubMed] [Google Scholar]
- 11. Akhtar-Danesh N. Qfactor: a command for Q-methodology analysis. Stata J. 2018;18(2):432–446. [Google Scholar]
- 12. Zabala A, Pascual U. Bootstrapping Q methodology to improve the understanding of human perspectives. PLoS One. 2016;11(2):e0148087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Klooster P, Visser M, de Jong M. Comparing two image research instruments: the Q-sort method versus the Likert attitude questionnaire. Food Qual Prefer. 2008;19(5):511–518. [Google Scholar]
- 14. Watts S. Develop a Q methodological study. Educ Prim Care. 2015;26(6):435–437. [DOI] [PubMed] [Google Scholar]
- 15. Ramage S, Farmer A, Eccles KA, McCargar L. Healthy strategies for successful weight loss and weight maintenance: a systematic review. Appl Physiol Nutr Metab. 2014;39(1):1–20. [DOI] [PubMed] [Google Scholar]
- 16. Berg C, Forslund HB. The influence of portion size and timing of meals on weight balance and obesity. Curr Obes Rep. 2015;4(1):11–18. [DOI] [PubMed] [Google Scholar]
- 17. Thomas SL, Hyde J, Karunaratne A, Herbert D, Komesaroff PA. Being ‘fat’ in today’s world: a qualitative study of the lived experiences of people with obesity in Australia. Health Expect. 2008;11(4):321–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kolotkin RL, Andersen JR. A systematic review of reviews: exploring the relationship between obesity, weight loss and health-related quality of life. Clin Obes. 2017;7(5):273–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nigatu YT, Bültmann U, Schoevers RA, Penninx BWJH, Reijneveld SA. Does obesity along with major depression or anxiety lead to higher use of health care and costs? A 6-year follow-up study. Eur J Public Health. 2017;27(6):965–971. [DOI] [PubMed] [Google Scholar]
- 20. Lupinno FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BWJH, Zitman FG. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67(3):220–229. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.