Abstract
Background:
Developments in genomics may improve patient consultations about weight management; however, optimal approaches for these communications are unstudied.
Purpose:
We assessed the influence of receiving generic, genomic information and of physician communication approach on overweight females in simulated clinical weight counseling interactions.
Methods:
200 participants were randomized to receive information about genomic or behavioral underpinnings of body weight from a virtual reality-based physician who used either a supportive or directive communication approach. Participants completed post-test self-report questionnaires.
Results:
Genomic explanations for body weight led patients to perceive less blame,[F (1,196)=47.68, p<.0001] and weight stigma, [F(1,196)=5.75, p=.017] in the consultation. They did not lead to negative outcomes in physician-patient interaction or affect health behavior-related attitudes and beliefs. Physician’s supportive or directive communication approach did not affect outcomes.
Conclusions:
Integrating genomic concepts into health care has potential to positively influence the patient-provider relationship while addressing longstanding challenges in weight management.
Trial registry:
Keywords: health care communication, weight management, obesity, genomics
Introduction
Rapid scientific advances have led medical professionals and researchers to envision a future practice built upon routine integration of genomics into the clinical encounter to guide care and prevention decisions (1, 2). Although most genomic tools are not ready for clinical implementation (1, 3), physicians have expressed interest in using genomic testing to predict and prevent disease (4). Obesity is a context in which genomic medicine could make substantial contributions to patient health, should the requisite discoveries be made (5, 6). Obesity was recently classified as a disease by the American Medical Association, and weight screening and counseling are recommended by the US Preventative Services Taskforce for inclusion in routine primary care practice. Yet, obesity management is an area with substantial challenges. There are limited evidence-based treatment options to support long-lasting weight loss (7–9), and a great deal of uncertainty on the part of physicians about how to communicate about weight with patients (10, 11). Weight-related counseling has been cited as a strain on the physician-patient relationship. In particular, patients have reported feeling blamed by providers because of their weight (12, 13). This is concerning as poor physician-patient relationships can lead to diminished care (14, 15).
Physicians also face uncertainty about how to communicate about genomics with patients (4, 16). Concerns are based, in part, on unanswered questions about potential patient sensitivities and reactions to genomic information (17, 18). This is likely to be true not only of personalized genomic test results, but also of generic information highlighting the influence of genomics on weight and weight change more broadly. Overweight individuals frequently find general discussions of genomics and weight self-relevant (19, 20). This is an important point because consideration of genomic factors in obesity in a general sense may arise sooner or more frequently than consideration of personalized test results as scientific advancement begins to allow us to use information about links between genomics and body weight to prevent and address weight gain. General information about genomic influences on weight and obesity is increasingly available through channels like the media (19, 21). Furthermore, within clinical interactions, notions of genomic predisposition to obesity are sometimes suggested or implied based, for example, on clinical family health history discussions.
Although yet to be tested, the provision of genomic information, even when not personalized, could potentially reduce overweight patients’ perceptions that their physicians blame them for their weight. Indeed, receipt of personalized genomic risk feedback with regard to weight has been found to reduce self-blame (20, 22). Theoretical models suggest that a reduction in perceptions of being blamed by the doctor could, in turn, lessen the degree to which patients report weight-based stigmatization and negative interpersonal treatment by providers (23, 24). This could be of great benefit as overweight patients frequently report the perception that physicians stigmatize them based on their weight, and this can lead to poorer patient-provider relationships (25, 26).
On the other hand, provision of genomic information could backfire, harming physician-patient relationships or reducing preventive health behavior among patients (3, 27, 28). Potential harm to the relationship hinges on the notion that communication about genomic underpinnings of weight could suggest that patients are biologically ‘defective’ or flawed (29, 30). This interpretation of genomic information could increase patients’ perceptions of stigma due to their biological or genetic makeup. This is conceptually distinct from weight stigma, but could likewise have detrimental effects on the encounter and the relationship. In addition, concerns have been raised that this information could undermine patients’ confidence in their ability to control their weight, or suggest that behavioral approaches to weight management are ineffective or less effective than biological ones (e.g., medication). This could be particularly detrimental for individuals who are motivated to and/or have tried to achieve a healthy weight but have struggled with the weight management or maintenance process. The need to tread lightly in clinical communication of genomic risk predictions to avoid such outcomes could place additional demands on providers in an already overstretched visit.
Influence of Physician Communication Approach
At present, we do not know whether integration of information about genomic underpinnings of weight will help or hinder primary care efforts to make weight management more effective. It is therefore crucial to investigate how variables in the clinical context can change or optimize the effect of genomic information provision. Such findings could guide us as to what kind of communication approach may best convey this information.
Supportive, partnership-oriented communication approaches (processes aimed at reaching shared understanding of medical problems and supporting patients psychologically and emotionally) have shown the capacity to lead to more positive relationships between patient and clinician and improvements in some health and clinical outcomes (31). A more directive, paternalistic communication approach (i.e., use of business-like language directing the patient to act on treatment goals in a more authoritarian manner (32)) may also be effective in promoting healthy behavior change (33). The relationship between communication approaches and patient outcomes can be complex, and depend upon patient preferences, provider and patient characteristics, and the disease context (34).
In this case, genomic information could be demotivating or motivating with respect to health behavior depending upon how it is interpreted by a patient. Use of a supportive approach may tip that balance such that genomic information is interpreted in a more motivating manner. For example, a supportive approach involves the direct offer of support and may therefore bolster patients’ self-efficacy (35) and increase patients’ perception that they have the resources to manage their weight. Similarly, genomic information could be interpreted in ways that benefit or damage the patient-physician relationship. Patients’ perceptions of weight stigmatization hinge on feelings that they are blamed for their condition and perceived as inferior. Because supportive communication revolves around demonstrating value and respect for patients, this approach could make patients more likely to interpret physician-provided genomic information in a de-stigmatizing light, and less likely to feel labeled by it. In this way, supportive, partnership-oriented versus more directive approaches may hold differing promise for mitigating potential negative effects or enhancing potential positive effects of discussing genomic information in these encounters (36, 37).
Hypotheses
To bring data to these questions, we conducted a randomized experiment assessing the influence of integrating generic genomic versus behavioral information into simulated, lab-based weight counseling interactions with overweight, female patients, while additionally testing the influence of physician communication approach (i.e., supportive or directive) on these processes. We hypothesized that overall, receipt of information about genomic factors in weight would be associated with both positive and negative interpersonal outcomes including reduced feelings of blame from the physician and reduced perceptions of weight stigmatization, but also increased participant perceptions that they were being labeled as biologically flawed. With respect to health-promoting attitudes and beliefs, although the literature is mixed, we hypothesized that, overall, genomic information would not be demotivating to participants. We expected physician communication approach would moderate these relationships. Although somewhat speculative, in terms of interpersonal outcomes, we hypothesized that a supportive communication approach would be associated with less perceived weight stigma and labeling among those who received genomic information. We further hypothesized that receiving genomic information via a supportive approach would be associated with higher levels of health-promoting attitudes and beliefs.
Method
The current study was a randomized experiment (NCT01443910). Overweight women received information related to the causes and management of overweight that focused on either genomics or personal behavior. This occurred in a simulated clinical encounter with a virtual reality-based primary care physician. The virtual physician used either a supportive or a directive approach to communicate this information. We employed a virtual reality-based simulation as opposed to using hypothetical vignettes or other traditional simulation approaches. Virtual reality allows for complete standardization between conditions even while the encounter is situated in a visually realistic clinical setting (38). Previous research has shown that experiences in virtual environments can be very compelling (39) and can elicit natural responses to interpersonal and clinical situations like the ones employed here (40–42).
Study Sample
Participants were recruited from the Washington, DC metropolitan area in 2012 through flyer and internet postings and word-of-mouth. The final sample for analysis was 200 women with a response rate of 75% (See Figure 1). We recruited women because females experience weight stigma more severely than men (43) and are more frequently the focus of research that describes negative experiences of overweight patients in health care settings (44).
Figure 1:
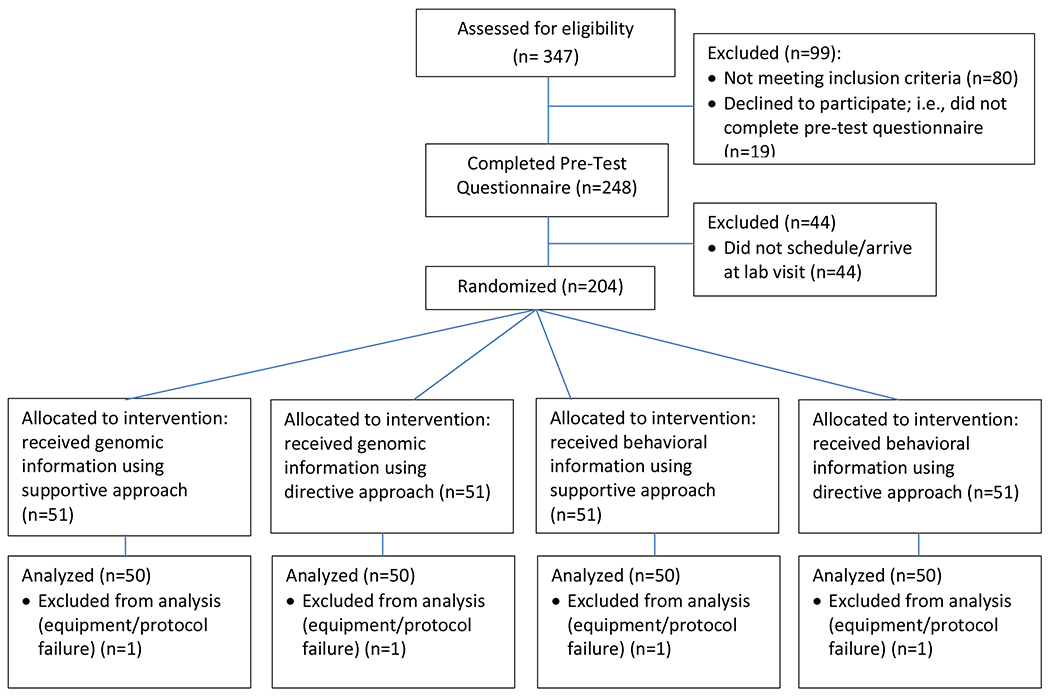
Study flow diagram
Using a 2 (genomic vs. behavioral information) X 2 (supportive vs. directive communication approach) design, fifty women were randomly assigned via random number generator to each of the four resulting conditions as they arrived in the lab. These included: receiving genomic information via supportive communication approach, receiving genomic information via directive communication, receiving behavioral information via supportive communication and receiving behavioral information via directive communication. Inclusion criteria included: being between 20 and 50 years old, having a self-reported body mass index of greater than or equal to 25 kg/m2, self-perception of being overweight, dissatisfaction with current weight status, and belief that they should lose weight. Individuals were ineligible if they had a history of eating disorder, were enrolled in a weight loss research trial, were health care providers or providers-in-training, or had received information about the purpose of the study from a previous participant. Exclusion criteria due to use of the virtual reality equipment included: having a vestibular or seizure disorder, a high propensity for motion sickness, known pregnancy, and/or uncorrected low vision or hearing. This study was approved by the Institutional Review Board of the National Human Genome Research Institute. Participants were compensated $75 by mailed check at the conclusion of the study.
Procedure
Individuals deemed eligible to participate were directed to a password-protected website to indicate their consent and complete the pre-test questionnaire. Participants were then scheduled to visit the lab for the in-person portion of the study. The study was described as an investigation into how patients feel about the techniques doctors use to talk about weight.
At the lab visit, participants were randomized to condition. One of three research assistants on the team guided participants through the study procedures and virtual interaction using a structured script. Participants took part in an interaction with a virtual physician in immersive virtual reality (Figure 2). They wore a head-mounted display that engulfed the field of view and presented 3D, stereoscopic visual stimuli that made up the virtual clinic room and its contents. They controlled their movement naturally within the virtual clinic room using physical body movement (e.g., turning their head, leaning forward). Participants were asked to put themselves into the shoes of the patient and respond to questions as if they were in a real doctor’s visit. Participants were informed that they could not ask the virtual physician questions.
Figure 2:
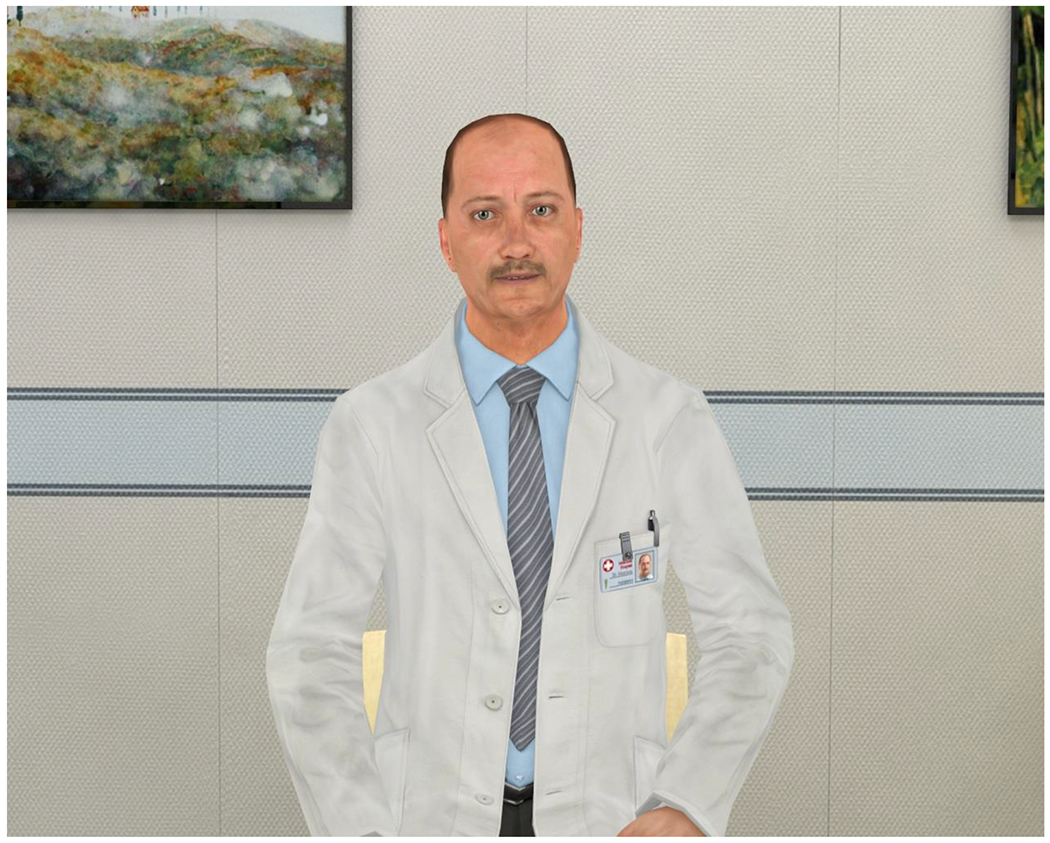
Screenshot of the virtual physician used in this trial
Participants were given an opportunity to look around in and acquaint themselves with the virtual doctor’s office. The research assistant answered any final questions and then triggered the beginning of the interaction with the virtual physician. The interaction consisted of a verbal discussion focusing on body weight and weight management within a primary care framework. The virtual physician presented weight counseling information consistent with condition (genomic or behavioral), he also asked the participant several contextually-appropriate questions during the course of the interaction (e.g., “what strategies have you tried to manage your weight?”). Participants verbally responded to these questions, and the research assistant triggered the virtual physician to acknowledge responses. In this way, the participant had a structured conversation with the virtual physician. The physician’s side of the conversation was controlled by the research assistant in that the research assistant triggered the physician’s speech. However, the content of that speech was consistent for all participants within each study condition. The physician was portrayed as a white male. This choice was made based on pilot testing in an attempt to strengthen the impact of the directive approach. The virtual reality system was created using the Vizard (Worldviz LLC, Santa Barbara, CA) software platform, and based on virtual reality-based clinical encounters developed for previous research projects (38).
The information provided by the virtual physician focused on either genomic factors or personal behavior as a primary causal factor in body weight and obesity. This information was communicated using either a supportive, partnership-oriented communication approach or a directive, information-oriented approach (34, 37). Details can be found in Table 1. Messages were developed based on recommended weight counseling approaches and in partnership with physician-consultants. After the virtual clinic interaction, participants completed a computerized post-test questionnaire. All post-test assessments were contained within this questionnaire. Finally, participants were debriefed and reminded of the generic nature of the information they were given by the virtual physician.
Table 1:
Information Provided and Communication Approach used by Virtual Doctor in Study Conditions
| Information Type | Genomic | • Body weight has a sizeable heritable component • Weight is controlled in part by genes interacting with and influencing one’s behavior and environment • Individuals with a genomic predisposition for obesity may be at a higher risk for lifelong obesity and may need to work harder than other people to maintain a healthy weight • Importance of diet and physical activity for weight management • Importance of realistic weight loss goals |
| Behavioral | • Body weight has a sizeable personal behavior component and is largely under personal control • Weight is controlled by energy in versus energy out, but this balance can be complicated • Individuals who are already overweight may be at higher risk for lifelong obesity, and may need to work harder than other people to maintain a healthy weight • Importance of diet and physical activity for weight management • Importance of realistic weight loss goals |
|
| Communication Approach | Supportive | • Nonverbal behavior: positive facial expressions • Paralinguistic behavior: vocal emphasis on supportive message elements • Non-substantive verbal responses: more supportive in nature (e.g., “I know this topic can be a little sensitive”; “I’ll be here to help you work through any issues or setbacks you have”) |
| Directive | • Nonverbal behavior: neutral facial expressions • Paralinguistic behavior: vocal emphasis on directive message elements • Non-substantive verbal responses: more directive in nature (e.g., “I know this topic isn’t fun to talk about”; “It’s important that you work through any setbacks that you have”) |
Measures
Perceived Blame
Participants’ perceptions that the physician blamed them for their weight were measured at post-test using a 3-item scale (e.g., “this doctor believes that my weight problem is my fault”; Cronbach’s alpha = 0.90). Items were assessed on a 1-7 scale (strongly disagree to strongly agree).
Perceived Physician Weight Stigmatization and Labeling
Participants’ perceptions that the physician stigmatized them due to their weight were measured using a 3-item scale (e.g., “this doctor thinks less of me because of my weight”; Cronbach’s alpha =0.76). Items were assessed on a 1-7 scale (strongly disagree to strongly agree).
Participants’ perceptions that the physician negatively labeled them based on the causes of their overweight were measured using seven items developed based on a measure by Esplen and colleagues (45). This scale assessed reactions to “the information the doctor gave me” so that it could be administered to participants in all conditions (e.g., “the information the doctor gave me made me feel labeled”; Cronbach’s alpha = 0.90). Items were assessed on a 1-7 scale (strongly disagree to strongly agree).
Health Behavior-Relevant Beliefs and Attitudes
Patient confidence in their ability to lose weight was measured at pre- and post-test with the following item: “how confident are you that you can lose weight?” Participants’ perceptions of the effectiveness of eight weight management strategies (e.g., medication, dieting) were assessed individually using a scale developed by Ogden and Flanagan (46). These were assessed on a 1-5 scale (not at all effective to very effective).
Statistical Analysis
We conducted a factor analysis with an oblique rotation to assess factor loadings for items assessing perceived effectiveness of weight management strategies. We created scales based on the three factors that emerged: biological strategies (medication, surgery; Cronbach’s alpha = 0.63), behavioral strategies (dieting, exercise; Cronbach’s alpha = 0.61), and interpersonal strategies (counseling, support group, consultation with a physician; Cronbach’s alpha = 0.72). One item (policy change) was dropped because it did not load on any factor. We assessed the effect of the manipulation on each outcome independently using analysis of variance. We conducted a repeated measures analysis of variance for patient confidence as this variable was assessed at both pre-test and post-test.
Results
Demographics
Demographics did not vary by condition (Table 2). Of the 200 women who completed the experiment, 70.5% met BMI criteria for being overweight but not obese; 29.5% met criteria for obesity. Participants were 35.1 years old on average (SD=9.6). 56.5% were college graduates. 54.5% self-identified as Black/African American, 29.5% as white, 4.0% as Hispanic/Latino, 4.5% as Asian, and 7.5% as “other”. Demographics of women who completed the pre-test questionnaire, but did not complete the study did not differ from those who did complete the study (data not shown).
Table 2:
Participant demographics by condition.
| Information: Genomic | Information: Behavioral | Significance testa | |||
|---|---|---|---|---|---|
| Communication: Supportive | Communication: Directive | Communication: Supportive | Communication: Directive | ||
| Body mass index (kg/m2) | 34.38 (6.68) | 33.59 (6.22) | 33.89 (8.09) | 35.42 (7.94) | p=.61 |
| Age (years) | 34.0 (9.4) | 35.9 (9.0) | 34.2 (8.2) | 36.1 (11.6) | p=.58 |
| Race: white | 26% | 32% | 30% | 30% | p=.93 |
| Race: Black | 54% | 54% | 54% | 56% | |
| Race: % other | 20% | 14% | 16% | 14% | |
| College graduate | 56% | 64% | 60% | 46% | p =.30 |
significance tests were F-tests for continuous variables and chi square tests for categorical ones
Perceived Blame
There was a main effect for both information type [F (1,196)=47.68, p<.0001] and communication approach [F(1,196)=27.25, p<.0001] on the extent to which participants felt that the doctor blamed them for their weight (see Table 3 for means). Participants who received information about genomics, and those who met with a doctor using a supportive approach perceived less blame. The interaction was not significant.
Table 3:
Unadjusted Means and Standard Deviations of Health Behavior-Related, Interpersonal, and Self-Blame Variables
| Genomic Information | Behavioral Information | Main Effect Information Type, p value and partial η2a | Main Effect Communication Approach p value and partial η2 b | Interaction, p value and partial η2 | |||
|---|---|---|---|---|---|---|---|
| Supportive Communication | Directive Communication | Supportive Communication | Directive Communication | ||||
| Perceived blame | 2.84 (1.50) | 3.93 (1.59) | 4.31 (1.68) | 5.53 (1.49) | p<.0001 / .20 | p<.0001/ .12 | p=.78/ .000 |
| Weight stigma perceptions | 1.85 (.99) | 2.17 (1.29) | 2.0 (1.01) | 2.82 (1.41) | p=.017 / .029 | p<.001/ .055 | p=.14 / .011 |
| Labeling perceptions | 2.09 (1.20) | 2.26 (1.29) | 2.01 (1.06) | 2.57 (1.49) | p=.52/ .002 | p=.039/ .022 | p=.28/ .006 |
| Weight loss confidence c, | 4.72 (1.68) | 5.14 (1.60) | 4.88 (1.38) | 5.24 (1.60) | p=.73/ .001 | p=.057/ .018 | p=.91/ .000 |
| Perceived treatment effectiveness: biological | 3.03 (.98) | 3.05 (1.2) | 2.96 (.96) | 2.80 (1.1) | p=.29/ .006 | p=.64/ .001 | p=.55/ .002 |
| Perceived treatment effectiveness: lifestyle | 4.47 (.77) | 4.52 (.75) | 4.66 (.52) | 4.66 (.54) | p=.076/ .016 | p=.79/ .000 | p=.79/ .000 |
| Perceived treatment effectiveness: interpersonal | 3.54 (.96) | 3.50 (.94) | 3.37 (.82) | 3.52 (.70) | p=.53/ .002 | p=.64/ .001 | p=.43/ .003 |
Main effects from 2-way ANOVA comparing the two information type conditions
Main effects from 2-way ANOVA comparing the two communication approach conditions
Repeated measures ANOVAs used for this variable
Perceived Physician Weight Stigmatization and Labeling
There was a main effect of information type and a main effect of communication approach on participants’ perceptions that they had been stigmatized by the doctor based on weight. Participants who received genomic information [F(1,196)=5.75, p=.017], and those who met with a supportive doctor [F(1,196)=11.49, p=.0008], perceived that the doctor was less stigmatizing. The interaction was not significant.
There was a main effect of communication approach on participants’ perceptions that they were labeled due to the information that the doctor gave them, F(1,196)=4.32, p=.039. Participants who met with a doctor who used a directive approach had increased perceptions of labeling. There was no main effect of information type and no interaction.
Health Behavior-Relevant Attitudes and Beliefs
Repeated measures analysis of variance revealed a significant effect of time on participant confidence for weight management following the encounter, F(1,195)=266.52, p<.0001. Confidence at post-test was significantly increased over baseline by an average of 1.29 scale points. There were no significant effects of condition.
There were no significant main effects or interactions predicting participants’ effectiveness ratings for any of the three types of weight management strategies (biological, lifestyle, or interpersonal). The main effect of information type on lifestyle strategies approached, but did not reach significance, F(1,196)=3.19, p=.076, such that lifestyle efficacy beliefs tended to be lower among those who received genomic rather than behavioral information.
Discussion
Genomic medicine could pave the way for significant advances in preventive health care related to common conditions like obesity. However, questions remain about the potential influence of genomic information on patients, and what will be required of physicians for effective communication. The current study brought data to these questions in the context of weight management, a clinical area that is both pressing and challenging. Current findings suggest reason for optimism. Communicating about generic genomic explanations for body weight led patients to perceive less blame and weight stigma in the clinical consultation. Importantly, this occurred with little evidence of negative effects in terms of physician-patient interaction and the attitudes and beliefs that underlie healthy patient behavior.
Surveys of physicians and other health care providers have demonstrated that clinicians can stereotype and hold biases against their overweight patients (47–49). This situation can not only sour the therapeutic relationship, but has also been connected with poorer patient outcomes through delay or avoidance of care (50). Psychological theories have suggested a connection between blaming an individual for causing her medical condition and stigmatization (23, 24). The current findings are the first empirical evidence supporting the potential for genomic information provision to reduce perceived blame and the extent to which patients feel stigmatized by physicians based on their weight. Although the effects of genomic information provision on perceived stigma were relatively modest, the effects on perceived blame were quite strong. There may be other benefits of this robust reduction in perceived blame for the patient-provider relationship that went unexplored in the current study. In all, future communications integrating genomic messages appear to have the added benefit of improving relationships between physicians and their overweight patients.
The capacity for genomic information communication to bolster the therapeutic relationship is important. However, these benefits would not be sufficient to counter concerns and warnings raised in the literature about potential negative effects of discussing genomics in the context of obesity. Communicating that one might be genetically predisposed to be obese could be stigmatizing in its own right, possibly undercutting benefits ascribed to blame reduction. Genomic information can be perceived to label patients as flawed or ‘defective’. A similar phenomenon has been demonstrated in the realm of mental illness (29, 30), however, this had never been tested in the context of obesity. The current analysis demonstrated no support for this concern. Perceived labeling and stigmatization due to the information provided by the physician was not heightened when genomic predisposition information was communicated.
Similarly, and contrary to concerns, communication of genomic information and the accompanying reduction in perceived blame was not beneficial for or detrimental to the attitudes and beliefs that underlie patients’ health-promoting behavior. There is a body of literature that has demonstrated positive, negative, and frequently no change in health behavior following provision of genomic information (51–53). Previous work has also linked higher levels of self-blame and perceived stigmatization to poorer health behavior and weight outcomes (20, 53, 54). However, the effect of physician-provided weight-related genomic information in a clinical context had not been investigated. It appears that, in this context, the sizeable effects of genomic information provision on perceived blame were not sufficient to move the needle with respect to health behavior-related beliefs and attitudes. It may be that perceptions of blame stemming from an individual function differently from self-blame or from more global perceptions of stigma and discrimination.
The current study included overweight women who were dissatisfied with their current weight, and though currently overweight, most had attempted weight loss throughout their lifetime. These individuals, therefore, may have been particularly vulnerable to potential effects of genomic explanations in undercutting motivation. Rather, patients’ confidence in their ability to manage their weight was increased from pre-test regardless of the physician’s explanation. This supports previous findings which suggest that patients are not deterministic about genetics. Rather, they understand that genes influence health outcomes together and in interaction with the environment and individual behavior (19, 55, 56).
We had hypothesized that the effects of genomic information provision would vary depending upon the provider’s communication approach. The final piece of good news is that genomic information provision had the same positive interpersonal effects, and same lack of negative effects, regardless of the communication approach used. Good communication practices are always recommended (57), and in this case, a supportive approach led to independent benefits for patient perceptions of the physician-patient relationship. However, this finding suggests that, at least in the current context, genomic predisposition may not be as sensitive a topic as sometimes feared. Therefore, accommodations in communication practices may not be necessary to convey this information to its biggest benefit.
Like all studies, the current study has both strengths and limitations. First, the encounter between the participant and the physician was a simulated interaction. Real-world encounters are more complex and variable, and thus the influence of the factors studied here may be less clear-cut. However, validation work has shown the appropriateness of using virtual reality to study social processes (40, 41), and by simulating the encounter we were able to identify causal relationships in an area that is otherwise difficult to interrogate. Unlike many other studies assessing the clinical influence of genomic information, the current sample had a large proportion of African-American participants and included individuals with a range of education levels. The study did, however, only include women who were dissatisfied with their weight. Providers are encouraged to counsel all patients with obesity about their weight (58). Future research should include a wider diversity of participants – men and women with variable beliefs about their need to lose weight. Finally, we created or adapted several measures used in the current study. In many cases, this study was the first to investigate these concepts and suitable measures did not exist. In future work, measures of these concepts should be further developed and psychometrically tested. The addition of direct measures of health behavior may have also improved the study. However, given the negligible effects found for the related, measured variables, it is unlikely that we would have observed changes in behavior.
As scientific knowledge about both the genomic underpinnings of obesity and the mechanisms through which genes influence weight continues to grow, links between genomics and body weight become increasingly relevant to health care. In addition, general notions of genomic predisposition to obesity can be implied through family health history discussions or conveyed through the media (19, 21). As such, the implications of the current study may have immediate relevance to clinical practice. In all, the discussion of genomic underpinnings of weight in the health care environment has great potential to positively influence the relationship between patients and providers, while also addressing challenges in clinical weight management.
Acknowledgements
This research was supported by the Intramural Research Program of the National Human Genome Research Institute, National Institutes of Health. This work is based on data collected in the Immersive Virtual Environment Testing Area of the Social and Behavioral Research Branch, NHGRI, NIH. The authors thank Colleen McBride, PhD and Howard Gordon, MD for advice and feedback during study development and editorial comments on a previous version of this manuscript. We thank Aanand Naik, MD for feedback during study development. We also acknowledge Peter Hanna, Stephanie Browning, and Maie Lee for assistance with data collection.
References
- 1.Freero. Clinical application of whole-genome sequencing: Proceed with care JAMA. 2014;311(10):1017–9. [DOI] [PubMed] [Google Scholar]
- 2.Manolio T, Chisholm R, Ozenberger B, Roden D, Williams M, Wilson R, et al. Implementing genomic medicine in the clinic: The future is here. Genetics in Medicine. 2013;15(4):258–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Loos R. Genetic determinants of common obesity and their value in prediction. Best Practice and Research Clinical Endocrinology and MEtabloism. 2012;26(2):211–26. [DOI] [PubMed] [Google Scholar]
- 4.Haga S, Carrig M, O’Daniel J, Orlando L, Killeya-Jones L, Ginsburg G, et al. Genomic risk profiling: Attitudes and use in personal and clinical care of primary care physicians who offer risk profiling. Journal of General Internal Medicine. 2011;26(8):834–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Agurs-Collins T, Khoury M, Simon-Morton D, Olster D, Harris J, Milner J. Public health genomics: Translating obesity genomics into population health benefits. Obesity. 2008;16(S3):S85–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.El-Sayed Moustafa J, Froguel P. From obesity genetics to the future of personalized obesity therapy. Nature Reviews Endocrinology. 2013;9(7):402–13. [DOI] [PubMed] [Google Scholar]
- 7.Douketis J, Macie C, Thabane L, Williamson D. Systematic review of long-term weight loss studies in obese adults: clinical significance and applicability to clinical practice. International Journal of Obesity. 2005;29(10):1153–67. [DOI] [PubMed] [Google Scholar]
- 8.Anderson J, Konz E, Frederich R, Wood C. Long-term weight-loss maintenance: A meta-analysis of US studies. American Journal of Clinical Nutrition. 2001;74(5):579–84. [DOI] [PubMed] [Google Scholar]
- 9.Kraschnewski J, Boan J, Esposito J, Sherwood N, Lehman E, Kephart D, et al. Long-term weight loss maintenance in the United States. International Journal of Obesity. 2010;34(11):1644–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chisholm A, Hart J, Lam V, Peters S. Current challenges of behavior change talk for medical professionals and trainees. Patient Education and Counseling. 2012;87(3):389–94. [DOI] [PubMed] [Google Scholar]
- 11.Kushner R Barriers to providing nutrition counseling by physicians: A survey of primary care practitioners. Preventive Medicine. 1995;24(6):546–52. [DOI] [PubMed] [Google Scholar]
- 12.Ruelaz A, Diefenbach P, Simon B, Lanto A, Arterburn D, Shekelle P. Perceived barriers to weight management in primary care: Perspectives of patients and providers. Journal of General Internal Medicine. 2007;22(4):518–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Friedman K, Ashmore J, Applegate K. Recent experiences of weight-based stigmatiation in a weight loss surgery population: Psychological and behavioral correlates. Obesity. 2008;16(S2):S69–74. [DOI] [PubMed] [Google Scholar]
- 14.Safran D, Taira D, Rogers W, Kosinski M, Ware J, Tarlov A. Linking primary care performance to outcomes of care. Journal of Family Practice. 1998;46(3):213–20. [PubMed] [Google Scholar]
- 15.Stewart M, Brown J, Donner A, McWhinney I, Oates J, Weston W, et al. The impact of patient-centered care on outcomes. Journal of Family Practice. 2000;49(9):796–804. [PubMed] [Google Scholar]
- 16.Suther S, Goodson P. Barriers to the provision of genetic services by primary care physicians. A systematic review of the literature. Genetics in Medicine. 2003;5(2):70–6. [DOI] [PubMed] [Google Scholar]
- 17.Najafzadeh M, Davis J, Joshi P, Marra C. Barriers for integrating personalized medicine into clinical practice: A qualitative analysis. American Journal of Medical Genetics. 2013;161A(4):758–63. [DOI] [PubMed] [Google Scholar]
- 18.Wilkes M The case against marketing genetic tests to primary care doctors to promote test ordering. Journal of General Internal Medicine. 2011;26(8):824–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Persky S, Sanderson S, Koehly L. Online communication about genetics and body weight: implications for health behavior and internet-based education. Journal of Health Communication. 2013;18(2):241–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Conradt M, Dierk J-M, Schlumberger P, Albohn C, Rauh E, Hinney A, et al. A consultation with genetic information about obesity decreases self-blame about eating and leads to realistic weight loss goals in obese individuals. Journal of Psychosomatic Research. 2009;66(4):287–95. [DOI] [PubMed] [Google Scholar]
- 21.Yoo J, Kim J. Obesity in the new media: A content analysis of obesity videos on YouTube. Health Communication. 2012;27(1):89–97. [DOI] [PubMed] [Google Scholar]
- 22.Meisel S, Wardle J. ‘Battling my biology’: Psychological effects of genetic testing for risk of weight gain. Journal of Genetic Counseling. 2014;23(2):179–86. [DOI] [PubMed] [Google Scholar]
- 23.Weiner B, Perry R, Magnusson J. An attributional analysis of reactions to stigmas. Journal of Personality and Social Psychology. 1998;55(5):736–48. [DOI] [PubMed] [Google Scholar]
- 24.Crandall C Prejudice against fat people: Ideology and self-interest. Journal of Personality and Social Psychology. 1994. 66:882–94. [DOI] [PubMed] [Google Scholar]
- 25.Puhl RM, Moss-Racusin CA, Schwartz MB. Internalization of weight bias: Implications for binge eating and emotional well-being. Obesity. 2007;15(1):19–23. [DOI] [PubMed] [Google Scholar]
- 26.Friedman KE, Ashmore JA, Applegate KL. Recent experiences of weight-based stigmatization in a weight loss surgery population: Psychological and behavioral correlates. Obesity. 2008;16(Suppl 2):S69–S74. [DOI] [PubMed] [Google Scholar]
- 27.Hall W, Matthews R, Morley K. Being more realistic about the public health impact of genomic medicine. PLos Medicine. 2010;7(10):e1000347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Flinter F Should we sequence everyone’s genome? No. British Medical Journal. 2013;346:f31–2. [Google Scholar]
- 29.Phelan JC. Genetic bases of mental illness - a cure for stigma? Trends in Neurosciences. 2002;25(8):430–1. [DOI] [PubMed] [Google Scholar]
- 30.Angermeyer M, Holzinger A, Carta M, Schomerus G. Biogenetic explanations and public acceptance of mental illness: Systematic review of population studies. British Journal of Psychiatry. 2011;199(5):367–72. [DOI] [PubMed] [Google Scholar]
- 31.Epstein RM, Street RL Jr.. Patient-Centered Communication in Cancer Care: Promoting Healing and Reducing Suffering. In: National Cancer Institute N, editor. Bethesda, MD: 2007. [Google Scholar]
- 32.Grugaard PK, Finset A. Trait anxiety and reactions to patient-centered and doctor-centered styles of communication: an experimental study. Psychosomatic Medicine. 2000;62(33–9). [DOI] [PubMed] [Google Scholar]
- 33.Kinmonth A, Woodcock A, Griffin S, Spiegal N, Campbell M. Randomised controlled trial of patient centred care of diabetes in general practice: impact on current wellbeing and future disease risk. The Diabetes Care From Diagnosis Research Team. BMJ. 1998;317(7167):1202–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Swenson S, Buell S, Zettler P, White M, Ruston D, Lo B. Patient-centered communication: Do patients really prefer it?. Journal of General Internal Medicine. 2004;19(11):1069–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bray S, Saville P, Brawley L. Determinants of clients’ efficacy in their interventionists and effects on self-perceptions for exercise in cardiac rehabilitation. Rehabilitation Psychology. 2013;58(2):185–95. [DOI] [PubMed] [Google Scholar]
- 36.Epstein R, Street RJ. Patient-centered communication in cancer care: Promoting healing and reducing suffering. In: Institute NC, editor. 7 ed. Bethesda, MD: NIH Publication; 2007. [Google Scholar]
- 37.Graugaard P, Finset A. Trait anxiety and reactions to patient-centered and doctor-centered styles of communications: An experimental study. Psychosomatic Medicine. 2000;62(1):33–9. [DOI] [PubMed] [Google Scholar]
- 38.Persky S Employing immersive virtual environments for innovative experiments in health care communication. Patient Education and Counseling. 2011;82(3):313–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bailenson JN, Blascovich J, Beall AC, Loomis JM. Interpersonal distance in immersive virtual environments. Personality and Social Psychology Bulletin. 2003;29:1–15. [DOI] [PubMed] [Google Scholar]
- 40.McCall C, Blascovich J. How, when, and why to use digital experimental virtual environments to study social behavior. Social and Personality Psychology Compass. 2009;3:1–15. [Google Scholar]
- 41.Blascovich J, Loomis J, Beall A, Swinth K, Hoyt C, Bailenson J. Immersive virtual environment technology as a research tool for social psychology. Psychological Inquiry. 2002;13:103–25. [Google Scholar]
- 42.Raij AB, Johnsen K, Dickerson RF, Lok BC, Cohen MS, Duerson M, et al. Comparing interpersonal interactions with a virtual human to those with a real human. IEEE Transactions on Visualization and Computer Graphics. 2007;13(3):1–15. [DOI] [PubMed] [Google Scholar]
- 43.Tiggemann M, Rothblum ED. Gender differences in social consequences of perceived overweight in the United States and Australie. Sex Roles. 1988;18:75–86. [Google Scholar]
- 44.Puhl RM, Heuer CA. The stigma of obesity: A review and update. Obesity. 2009;17(5):941–64. [DOI] [PubMed] [Google Scholar]
- 45.Esplen M, Stuckless N, Hunter J, Liede A, Metcalfe K, Glendon G, et al. The BRCA Self-Concept Scale: A new instrument to measure self-concept in BRCA1/2 mutation carriers. Psycho-Oncology. 2009;18(11):1216–29. [DOI] [PubMed] [Google Scholar]
- 46.Ogden J, Flanagan Z. Beliefs about the causes and solutions to obesity: A comparison of GPs and lay people. Patient Education and Counseling. 2008;71(1):72–8. [DOI] [PubMed] [Google Scholar]
- 47.Foster G, Wadden T, Markis A, Davidson D, RS S, Allison D, et al. Primary care physicians’ attitudes about obesity and its treatment. Obesity Research. 2003;11(10):1168–77. [DOI] [PubMed] [Google Scholar]
- 48.Jay M, Kalet A, Ark T, McCacken M, Messito M, Richter R, et al. Physicians’ attitudes about obesity and their associations with competency and specialty: A cross-sectional study. BMC Health Services Research. 2009;9(106). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Budd G, Mariotti M, Graff D, Falkenstein K. Health care professionals’ attitudes about obesity: An integrative review. Applied Nursing Research. 2011;24:127–37. [DOI] [PubMed] [Google Scholar]
- 50.Amy N, Aalborg A, Lyons P, Keranen L. Barriers to routine gynecological cancer screening for White and African-American obese women. International Journal of Obesity. 2006;30(1):147–55. [DOI] [PubMed] [Google Scholar]
- 51.Marteau T, French D, Griffin S, Prevost A, Sutton S, Watkinson C, et al. Does communicating DNA-based risk estimates motivate people to change their behaviour? 2010. [DOI] [PubMed] [Google Scholar]
- 52.McBride C, Sanderson S, Kaphingst K, Koehly L. The Behavioral Response to Personalized Genetic Information: Will Genetic Risk Profiles Motivate Individuals and Families to Choose More Healthful Behaviors? Annual Review of Public Health. 2010;31:89. [DOI] [PubMed] [Google Scholar]
- 53.Vartanian L, Shaprow J. Effects of weight stigma on exercise motivation and behavior: A preliminary investigation among college-aged females. Journal of Health Psychology. 2008;13(1):131–8. [DOI] [PubMed] [Google Scholar]
- 54.Major B, Hunger J, Bunyan D, Miller C. The ironic effects of weight stigma. Journal of Experimental Social Psychology. 2014;51:74–80. [Google Scholar]
- 55.Brogan A, D H. The structure of the causal attribution belief network of patients with obesity. British Journal of Health Psychology. 2009;14:35–48. [DOI] [PubMed] [Google Scholar]
- 56.Parrott R, Silk K, Condit C. Diversity in lay perceptions of the sources of human traits: Genes, environments, and personal behaviors. Social Science and Medicine. 2003;56:1099–109. [DOI] [PubMed] [Google Scholar]
- 57.American Medical Association. An Ethical Force Program concensus report: Improving communication - Improving care Chicago, IL: AMA, 2006. [Google Scholar]
- 58.Moyer V. Screening for and management of obesity in adults: U.S. Preventive Services Task Force recommendation statment. Annals of Internal Medicine. 2012;157(5):373–8. [DOI] [PubMed] [Google Scholar]


