Abstract
Background:
The incidence of contralateral anterior cruciate ligament (CACL) injuries after recovery from a first-time anterior cruciate ligament (ACL) disruption is high in women; however, little is known about the risk factors associated with this trauma.
Hypothesis:
Patient characteristics, strength, anatomic alignment, and neuromuscular characteristics of the contralateral uninjured leg at the time of the first ACL trauma are associated with risk of subsequent CACL injury, and these risk factors are distinct from those for a first-time ACL injury.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
Sixty-one women who suffered a first-time noncontact ACL injury while participating in high school or college sports and underwent measurement of potential risk factors on their contralateral limb soon after the initial ACL injury and before reconstruction were followed until either a CACL injury or an ACL graft injury occurred, or until the last date of contact.
Results:
Follow-up information was available for 55 (90.0%) of the 61 athletes and 11 (20.0%) suffered a CACL injury. Younger age, decreased participation in sport before the first ACL disruption, decreased anterior stiffness of the contralateral knee, and increased hip anteversion were associated with increases in the risk of suffering a CACL injury.
Conclusion:
A portion of CACL injury risk factors were modifiable (time spent participating in sport and increasing anterior knee stiffness with bracing), while others were nonmodifiable (younger age and increased hip anteversion). The relationship between younger age at the time of an initial ACL injury and increased risk of subsequent CACL trauma may be explained by younger athletes having more years available to be exposed to at-risk activities compared with older athletes. A decrease of anterior stiffness of the knee is linked to decreased material properties and width of the ACL, and this may explain why some women are predisposed to bilateral ACL trauma while others only suffer the index injury. The risk factors for CACL injury are unique to women who suffer bilateral ACL trauma compared with those who suffer unilateral ACL trauma. This information is important for the identification of athletes who may benefit from risk reduction interventions.
Keywords: knee, ACL, contralateral, trauma, injury prevention, risk factors
Complete disruption of the anterior cruciate ligament (ACL) and the associated concomitant injuries are among the most common knee injuries associated with sport and activity, with between 100,000 and 200,000 reported ACL ruptures in the United States annually.13 This a concern among women, as they are 2 times more likely to suffer ACL trauma in comparison with men when controlling for age, sport, and level of competition,7 and up to 23.7% of young women who suffer a unilateral ACL injury will suffer subsequent trauma to the contralateral ACL (CACL) within 2 years of full recovery and return to activity.22,35,43 Patients suffering bilateral ACL injuries return to sport at a decreased rate with a significant reduction in activity level.10 Even more concerning is that ACL trauma is associated with premature onset of posttraumatic osteoarthritis (PTOA),1,25,33 and this is problematic in young active individuals who place a high demand on their joints. Consequently, bilateral ACL injuries increase the risk of PTOA and create a considerable therapeutic challenge, as the management of PTOA in young active individuals through both surgical and nonsurgical approaches is only marginally successful.1 A more effective approach is to minimize the risk of suffering inciting CACL trauma. To accomplish this goal, a complete understanding of the risk factors associated with CACL injury is necessary for the development of interventions and to help identify patients at increased risk for CACL injury after primary ACL injury so that interventions can be targeted toward them.
Studies have established risk factors for first-time ACL injury and these include sport,7 level of play,7 athlete’s sex,7 family history of ACL injury,12 increased anteroposterior knee laxity,53,55 knee loading during landing from a jump,15,16 and specific measures of knee joint geometry.5,50,51,58 More recently, an investigation with multivariate analysis conducted to identify the independent predictors of first-time ACL injury revealed that family history of ACL injury, increased anteroposterior knee laxity, and increased body mass index (BMI) were associated with increased risk of injury in female high school and college athletes.55 Risk factors for CACL injury have not been studied to the same extent as those for a first-time ACL injury.26 Currently, young age, high activity level, and female sex have been shown to be factors associated with increased risk of suffering CACL injury.20,24,26,42,45,60
In addition, joint kinematics when landing from a jump, including less stable hip-ankle coordination and increased net intersegmental transverse plane hip internal rotation moment,34,36 and specific measures of knee joint geometry, including decreased femoral intercondylar notch width, tibial spine width and height, and articular cartilage thickness, have been identified as risk factors for CACL injury.22 It is likely that multiple factors influence the risk of suffering a CACL injury, and it is unclear if these factors are similar to or distinct from the risk factors for a first-time ACL injury. This served as the motivation for the current study, the purpose of which was to follow a cohort of female athletes who suffered a first-time noncontact ACL injury and returned to sport, identify those who subsequently suffered a noncontact CACL injury, and assess the effects of potential risk factors measured at the time of the first ACL injury on the risk of sustaining a CACL injury. We hypothesized that patient characteristics, joint laxity, anatomic alignment, and strength of the uninjured leg at the time of the first ACL injury are associated with increased risk of suffering a CACL injury, and these risk factors are distinct from risk factors for first-time ACL injury.
A more complete understanding of risk factors specific to CACL injury, including both modifiable and nonmodifiable risk factors, will allow for the identification of individuals who will benefit the most from targeted injury prevention measures.
METHODS
This investigation was approved by our institutional review board and is an extension of previous work that was designed to examine the geometric characteristics of the knee that are risk factors for CACL injury among female athletes.22 Participants were recruited from a previous prospective cohort study of first-time noncontact (without contact to the knee or surrounding area) ACL injuries. That study collected data on injured athletes from 36 different high schools and colleges over a 4-year time interval.55 Study subjects competed in track and field, soccer, basketball, field hockey, or lacrosse and suffered a first-time, complete ACL rupture within the study period with no prior trauma to either knee. A first-time ACL rupture occurred in 109 study subjects (70 females and 39 males) during participation in high school or college sport at the varsity level and was confirmed with arthroscopic visualization at the time of ACL reconstruction (ACLR) and magnetic resonance imaging (MRI). Patients underwent ACLR and supervised rehabilitation and returned to sport and activity. To identify the athletes that suffered subsequent CACL injury, we attempted to obtain follow-up information on 88 (61 females and 27 males) of the 109 patients who had MR images of the uninjured contralateral knee (the knee at risk for injury in the current study) at the time of their initial ACL injury. We were able to contact 55 (90%) of 61 female patients and 24 (89%) of 27 male patients by mail, email, or telephone. The individuals were contacted after ACLR, rehabilitation, and return to sport and re-enrolled in the current study. Information was collected regarding subsequent CACL or ACL graft injury. Medical records were obtained and reviewed on participants that reported a CACL rupture to confirm that a complete, grade 3, noncontact CACL rupture occurred, which was determined via clinical examination, MRI, and arthroscopic visualization at the time of CACL reconstruction. In addition, the date of CACL injury was recorded. The current study focuses on female athletes because our previous work indicates that risk factors for ACL injury differ between men and women and there was only 1 CACL injury among the male athletes, precluding assessment of their risk factors.
After the first ACL disruption but before the initial ACLR, the injured patients visited our laboratory to undergo measurements of potential risk factors that were modifiable and nonmodifiable. Data for all study participants were collected by the same individual whose ability to reliably measure the risk factors was established before data collection by obtaining replicate measures on volunteers.48 The categories of potential risk factors that were considered included MR images of both knees, patient characteristics, joint laxity, lower extremity alignment, strength, and personality characteristics. The detailed methods and associated reliability used to obtain these measurements have been described,55 and the following is a brief overview of the protocol that was used. The same individual interviewed all study participants and documented the following patient characteristics: age at the time of first ACL injury, hours spent participating in sport per week, number of years participating in sport, family history of ACL injury, presence of chronic disease, race, weight, height, BMI, use of braces, use of medication, limb dominance, prior leg surgery, and prior injury to the lower extremity (knee, hip/thigh, lower leg, ankle/foot). The same examiner evaluated joint laxity. Ankle laxity was measured with the talar tilt test, generalized joint laxity was measured with the Beighton test,4 and knee laxity was measured with the KT-1000.11 The KT-1000 arthrometer is instrumented with load and displacement sensors that provide measurement of the anteroposterior load-displacement response of the contralateral knee. Data from the KT-1000 measurements were postprocessed with custom-written MATLAB software (MathWorks) to provide additional data on the anterior stiffness of the tibiofemoral joint (Figure 1). Lower extremity alignment (passive and active genu recurvatum, hamstring extensibility, standing quadriceps angle in the coronal plane, navicular drop, tibiofemoral angle in the coronal plane, pelvic angle, tibial torsion, hip anteversion, and length of the tibia and femur) was evaluated by the same investigator using an approach that has been described and shown to be reliable.48 The same investigator measured strength for all patients, and the peak torque developed during the test was used as the outcome. Trunk flexion and extension strength was measured isometrically with the Cybex system II.14 Knee muscle strength (flexion and extension evaluated at 30° and 15° of flexion) and ankle muscle strength (flexors and extensors) were measured isometrically with the Biodex system II. Hip strength was measured isometrically with a stabilized dynamometer.52 Personality characteristics were evaluated with the Temperament and Character Inventory,9 which was completed by the study participants. These data were used to assess each patient’s temperament (classified in 4 dimensions: Novelty Seeking, Harm Avoidance, Reward Dependence, and Persistence) and character (classified in 3 dimensions: Self-Directedness, Cooperativeness, and Self-Transcendence). The MRIs of the contralateral limb that were acquired at the time of the first ACL trauma were reviewed to confirm that the contralateral limb was normal and did not have evidence of prior injury to the articular cartilage of both patellofemoral and tibiofemoral joints, primary ligaments, joint capsule, and menisci. Measurements that were limb/knee specific were made on the contralateral, normal limb (ie, the limb that was at risk for injury or injured in the current study). Methods used for data collection have been published, and all have been shown to be reproducible and reliable.55
Figure 1.
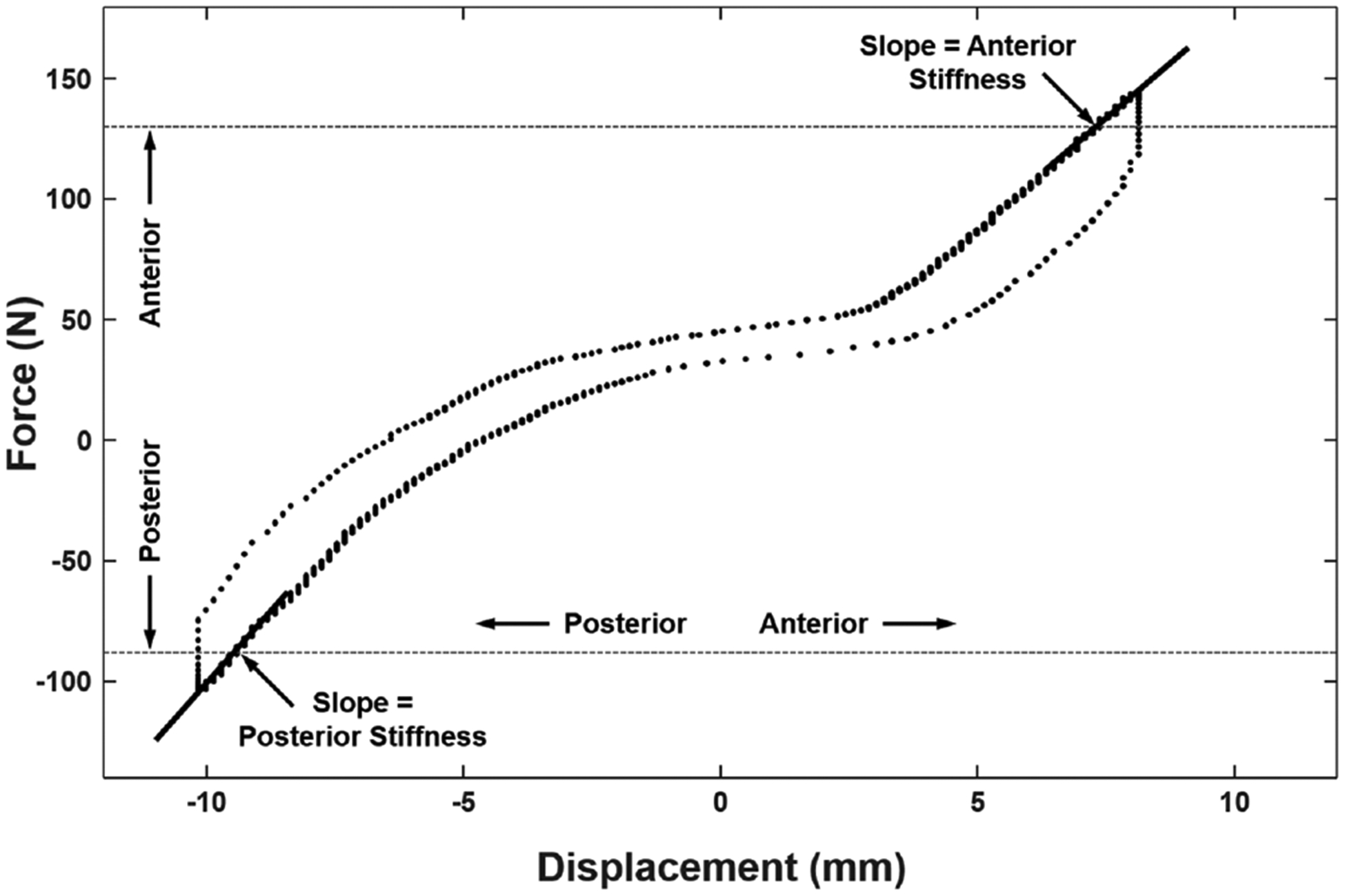
KT-1000 measurement of the anteroposterior load-displacement response of the knee. The anteriorposterior directed loads applied to the tibia, relative to the immobilized femur, are plotted on the vertical axis, and the resulting anteroposterior displacement of the tibia relative to the femur appears on the horizontal axis. The horizontal dashed lines identify the load limits of 130 N (anterior-directed load applied to the tibia) and −90 N (posterior-directed load applied to the tibia). These data were analyzed to evaluate anteroposterior laxity of the knee (the total tibiofemoral displacement produced by the 130 N anterior and −90 N posterior loads) and anterior and posterior stiffness of the knee (the slopes of the liner portion of the load-displacement response of the knee).
Statistical Analysis
The outcome of this study was the number of months between the first ACL injury and subsequent CACL injury. Participants who did not have a CACL injury were censored at the date of final contact. Patients who reinjured their reconstructed knee were included in the study, but their follow-up time was censored at the time of injury to the ipsilateral ACL graft because the risk factors for rupture after ACLR are different from those for injury to the healthy knee.23 Statistical methods were based on survival analysis, with a Cox regression used to model time to CACL injury, with each potential risk factor considered an independent variable to assess its univariate association with risk of CACL injury. Hazard ratios were determined relative to a 1 standard deviation (SD) decrease in the variable under consideration. The significance level of alpha was set at .05 a priori for all analyses. All statistical analyses were conducted using SAS version 9.2 (SAS Institute). A priori power calculations indicated that a sample of 55 patients with 10 CACL injuries during an average of 41.0 months of follow-up would provide at least 80% power to detect an association with risk if the true hazard ratio is 2.46 or larger per a 1 SD change in the independent variable.
RESULTS
Of the 55 female patients with follow-up information, 11 (20.0%) suffered a noncontact CACL injury for which they underwent reconstruction. Six (10.9%) women sustained an ipsilateral noncontact ACL graft injury, 1 of which occurred 1 month before the CACL injury. All patients suffering a graft injury were censored at their time of injury, so 10 CACL injuries were used in the statistical analysis. The mean time to CACL injury was 23.3 ± 11.2 months (range, 12.4–41.2 months). The mean follow-up interval for unilaterally injured patients was 45.0 ± 14.0 months (range, 7.3–71.5 months). With the exclusion of patients censored because of graft injury, the minimum follow-up was 24.1 months. All patients completed a supervised rehabilitation program administered through the rehabilitation clinic affiliated with their institution and returned to the same level of play and the same sports they participated in before the index injury.
Information for patient characteristics is included in Table 1. Of the 32 variables that were considered in this study (Tables 1 and 2), 4 were significantly associated with a risk of CACL injury after a first-time ACL injury (Table 3, Figure 1). A 1 SD decrease in anterior stiffness of the knee was associated with a 2.37-fold increase in the risk of CACL injury (P = .042). A 1-year decrease in age was associated with a 1.70-fold increase in the risk of CACL injury (P = .004). The number of hours per week spent participating in sport at the time of the initial ACL injury was also inversely associated with risk of CACL injury, with a 1.19-fold increase in risk for each 1 hour per week decrease in participation (P = .048). A 1 SD increase of hip anteversion was associated with a 2.38-fold increase in the risk of suffering a CACL injury (P = .017).
TABLE 1.
Summary of Continuous Measurements Obtained at the Time of the First ACL Injury (n = 55)a
| Mean | SD | Minimum | Maximum | |
|---|---|---|---|---|
| Patient Characteristics | ||||
| Height, cm | 167.8 | 6.74 | 154.9 | 180.3 |
| Weight, kg | 65.9 | 9.65 | 50.3 | 90.7 |
| BMI, kg/m2 | 23.3 | 2.66 | 19.3 | 30.4 |
| Age at first ACL injury, y | 17.1 | 2.14 | 13 | 21 |
| Age at final follow-up, y | 20.28 | 2.67 | 15.18 | 25.21 |
| Follow-up interval, mo | 41.0 | 15.9 | 7.3 | 71.5 |
| Hours/week participating in sport | 9.35 | 6.37 | 2 | 48 |
| Years of sport participation | 7.76 | 3.67 | 1 | 16 |
| LE alignment | ||||
| Standing quadriceps angle, deg | 11.7 | 4.24 | 0 | 20 |
| Tibiofemoral angle, deg | 10.3 | 3.44 | 4 | 19 |
| Navicular drop, mm | 8.73 | 3.93 | 1.85 | 19.6 |
| Pelvic angle, deg | 6.25 | 4.46 | −5 | 17 |
| Tibial torsion, deg | 12.9 | 4.81 | 0 | 25 |
| Hip anteversion, deg | 8.45 | 4.63 | −8 | 19 |
| Hamstring extensibility, deg | 15.2 | 10.2 | −11 | 41 |
| Genu recurvatum (active), deg | −8.45 | 4.4 | −19 | 0 |
| Genu recurvatum (passive), deg | −9.49 | 4.59 | −21 | −1 |
| Tibial length, cm | 37.3 | 2.11 | 33.3 | 43 |
| Femur length, cm | 43.6 | 2.56 | 38.3 | 48.6 |
| Joint laxity | ||||
| AP displacement, mm | 14.95 | 2.91 | 8.65 | 22.28 |
| Posterior stiffness, N/mm | 22.67 | 3.76 | 12.76 | 30.96 |
| Anterior stiffness, N/mm | 19.1 | 19.08 | 10.63 | 31.61 |
| Beighton score | 3.29 | 2.56 | 0 | 9 |
| Strength, Nm | ||||
| Hip flexion | 129.7 | 29.9 | 37.9 | 214 |
| Hip extension | 118.2 | 32.1 | 64.7 | 221.9 |
| Hip abduction | 120.2 | 25.7 | 65.6 | 170.8 |
| Hip adduction | 123.1 | 22.1 | 85.8 | 172.5 |
| Hip internal rotation | 19.2 | 5.03 | 10.8 | 32.5 |
| Hip external rotation | 21.5 | 5.03 | 13.6 | 36.6 |
| Knee flexion 15° | 77.8 | 19.6 | 35.1 | 114.8 |
| Knee flexion 30° | 69.1 | 19.8 | 27.1 | 110.4 |
| Knee extension 15° | 87.6 | 32.7 | 26.9 | 190.3 |
| Knee extension 30° | 128.8 | 32.4 | 74.5 | 203.5 |
| Trunk flexion | 112 | 30.1 | 39.3 | 185.7 |
| Trunk extension | 133.6 | 37 | 33.9 | 231.8 |
| Ankle dorsiflexion | 26.7 | 11.5 | 11.3 | 82.9 |
| Ankle plantarflexion | 83.2 | 23 | 23.2 | 126.8 |
| Personality | ||||
| Novelty seeking | 60.7 | 10.5 | 43 | 92 |
| Harm avoidance | 51.4 | 11.3 | 27 | 78 |
| Reward dependence | 71.6 | 9.21 | 42 | 90 |
| Persistence | 75.9 | 10.9 | 47 | 95 |
| Self-directedness | 74.4 | 11.4 | 43 | 93 |
| Cooperativeness | 79 | 9.13 | 58 | 93 |
| Self-transcendence | 43 | 9.33 | 21 | 67 |
ACL, anterior cruciate ligament; AP, anteroposterior; BMI, body mass index; LE, lower extremity.
TABLE 2.
Summary of Categorical Measurements Obtained at the Time of the First ACL Injury (n = 55)a
| No. of Patients | Percentage | |
|---|---|---|
| Race | ||
| White | 48 | 87.3 |
| Nonwhite | 7 | 12.7 |
| Leg dominance | ||
| Right | 52 | 94.5 |
| Left | 3 | 5.5 |
| Other conditions | ||
| Chronic illness | 48 | 87.3 |
| Medication use | 7 | 12.7 |
| Brace use | 20 | 36.4 |
| History | ||
| Prior hip/thigh injury | 5 | 9.1 |
| Prior knee injury | 15 | 27.3 |
| Prior leg injury | 5 | 9.1 |
| Prior ankle/foot injury | 24 | 43.6 |
| Prior leg surgery | 4 | 7.3 |
| Parent with ACL injury | 14 | 25.5 |
| Laxity | ||
| Morton toe | 21 | 38.2 |
| Ankle anterior drawer 1 + | 12 | 21.8 |
| Ankle anterior drawer 2 + | 4 | 7.3 |
| Talar tilt | 9 | 16.4 |
ACL, anterior cruciate ligament.
TABLE 3.
Significant (P < .05) Associations With the Risk of CACL Injury From the Univariate Cox Regression Analysis
| HR | 95% CI | P Value | |
|---|---|---|---|
| Agea | 1.70 | 1.17–2.63 | .004 |
| Hours/week of sport participationa | 1.19 | 1.00–1.45 | .048 |
| Hip anteversionb | 2.38 | 1.16–5.14 | .017 |
| Anterior knee stiffnessa | 2.37 | 1.03–6.60 | .042 |
Hazard ratios (HRs) with corresponding 95% CIs indicating the increase in risk of contralateral anterior cruciate ligament (CACL) injury per 1-year decrease in age, 1 hour per week decrease in sport participation, or 1 SD decrease in anterior stiffness of the knee.
HRs with corresponding 95% CIs indicating the increase in risk of CACL injury per 1 SD increase of the variable.
DISCUSSION
The findings from this investigation support our hypothesis, as we identified 4 risk factors measured after a first-time ACL injury that were associated with an increased risk of subsequently suffering a noncontact CACL injury in women. One, younger age, confirmed results from prior studies20,24,26,42,45,59 and 3 (decreased anterior stiffness of the tibiofemoral joint, decreased hours per week of sport participation, and increased hip anteversion) had not been previously identified. Decreased hours per week of sport participation is modifiable, and it may be possible to increase anterior stiffness of the knee with a brace; however, younger age and increased hip anteversions are nonmodifiable.
Increased anteroposterior laxity of the tibiofemoral joint has been shown to be associated with an increased risk of suffering a first-time ACL injury,53,55 but in the current study it was not related to risk of suffering a subsequent CACL injury. Instead, we found an inverse relationship between anterior stiffness of the knee and risk of CACL injury (ie, decreased anterior stiffness was associated with an increased risk of suffering CACL injury). Anteroposterior laxity and stiffness of the knee were evaluated simultaneously with the KT-1000 arthrometer, which was used to measure the anteroposterior directed loads applied to the tibiofemoral joint by the examiner and the resulting displacements of the tibia relative to the femur (ie, the complete load vs displacement response of the tibiofemoral joint) (Figure 1). These data were processed to characterize anteroposterior laxity (the anteroposterior displacement of the tibia relative to the femur produced by corresponding 130 N anterior and −90 N posterior directed loads applied to the knee) and anterior stiffness of the tibiofemoral joint (the slope of the linear region of the load-displacement response) (Figure 1). Anteroposterior laxity and anterior stiffness of the tibiofemoral joint were derived from the same load-displacement relationship; however, they provided different insights into the biomechanics of the joint and the underlying mechanisms of injury associated with individuals who suffer bilateral ACL trauma in comparison with unilateral ACL trauma. Anteroposterior laxity is an assessment of the ligaments that span the tibiofemoral joint (primarily the anterior and posterior cruciate ligaments in a normal knee) and how they restrain anteroposterior loading of the joint.27 Anterior stiffness of the knee is an evaluation of how anterior displacement of the tibia relative to the femur is restrained by the ACL,28 and it provides insight into ACL biomechanics, which are influenced by the orientation of the ACL relative to the load applied to the knee, and the material and geometric properties of the ACL.6,56
Our finding that a decrease in anterior stiffness of the tibiofemoral joint was associated with increased risk of suffering CACL injury suggests that there may be a unique subset of women with a first-time ACL injury who are predisposed to bilateral trauma based on inferior material properties of the ACL, smaller ACL size (volume and cross-sectional area), abnormal orientation of the ACL relative to the intersegmental loads transmitted across the knee, or some combination of these variables. When considered with the earlier work of Levins et al,22 which revealed that decreased femoral notch width was significantly associated with increased risk of CACL injury, this introduces the hypothesis that a decrease in the size of the femoral notch is associated with a smaller size of the ACL, inferior structural properties of the ligament, or a combination of both, and this could be one of the underlying mechanisms associated with increased risk of suffering a CACL injury.22 Alternatively, it is possible that a decrease in femoral notch size is associated with increased impingement of the ACL against the roof of the notch, and this is the underlying mechanism that increases the risk of suffering a CACL injury. To gain insight into the underlying biomechanics associated with noncontact CACL injury, and test the before-mentioned hypotheses, multivariate analysis with a much larger sample size is necessary to determine if the increased risk of CACL injury is independently influenced by biomechanical properties of the ACL (which would be indicated by decreased anterior stiffness of the knee as an independent risk factor), ACL geometry (represented by decreased volume and cross-sectional area of the ACL as an independent risk factor), impingement of the ACL against the femoral notch (characterized by decreased size of the femoral notch), or a combination of these variables.
It is intuitive that an ACL with increased capacity to resist anterior displacement of the tibia relative to the femur will be less likely to rupture; however, there are limited published data on the association between knee joint stiffness and the risk of knee ligament injury. Schmitz et al44 reported decreased knee stiffness in women compared with men, and this led them to conclude that decreased knee stiffness is likely one of many factors contributing to the increased rate of ACL and CACL injuries experienced by women in comparison with men.5,20,26,29,35,60 Our study focused on women, as they are at elevated risk of suffering ACL trauma in comparison with men,7 and future work is needed to determine if anterior stiffness of the tibiofemoral joint is associated with risk of CACL injury in men.
Hip alignment was also related to risk of suffering CACL trauma; specifically, increased femoral anteversion was associated with increased risk of injury. This finding supports prior work that reported increased femoral anteversion is associated with an increased risk of first-time ACL injury in athletes3 and the general population.46 The finding of a direct relationship between increased femoral anteversion and increased risk of CACL injury may be linked to the prior work by Paterno et al,36 who reported that increased transverse plane hip internal rotation moment during the initial landing phase of the drop vertical jump maneuver is highly predictive of an individual suffering a second ACL trauma to either the CACL or ACL graft. This provides support for the hypothesis that the mechanism by which hip alignment contributes to risk of ACL injury is through altered biomechanics. For example, excessive femoral anteversion has been directly implicated in altering lower extremity kinematics such that risk of ACL injury is increased.21,30,31,36 Nguyen et al31 identified femoral anteversion as a contributing characteristic to valgus collapse during the single-leg squat. Likewise, Kaneko and Sakuraba21 reported that increased femoral anteversion was associated with lower hip flexion angle, higher valgus alignment, and greater rectus femoris muscle activity on single-step landing, all factors that contributed to greater anterior tibial displacement upon landing. Additionally, in a study of 19 female athletes performing cutting maneuvers, the only significant predictor of knee abduction during the cutting task was hip adduction, a risk factor associated with ACL injury.18 Support for this finding can be derived from the work of Powers,37 who reported that increased internal rotation and adduction of the hip during weightbearing activity acts to move the knee medially in relation to the foot, and in turn with the foot fixed to the floor, the knee abducts and creates dynamic valgus about the joint. This positioning of the knee during cutting maneuvers has been identified as a common mechanism of noncontact ACL injury,19 providing additional support for the concept that hip alignment is an important factor associated with ACL and CACL injuries. Moreover, increased femoral anteversion has been associated with increased anterior laxity of the knee,47 a well-established risk factor for ACL injury.15,16,38,53,55
Younger age at the time of the initial ACL injury was significantly associated with increased risk of CACL trauma, and this relationship may be explained by the fact that an athlete’s age is correlated with exposure to athletics, with younger athletes having more years available to be exposed to at-risk activity associated with high school and collegiate sports in comparison with older athletes. Consequently, younger age and the associated increased exposure to sport may explain, at least in part, the increased risk of CACL injury.55 Similarly, our analysis indicated that the risk of subsequent CACL injury was inversely associated with the hours per week of participation in sport before the initial ACL injury, which may be an indicator of future exposure to sport because the younger athletes had fewer hours of participation in sport. Alternatively, it may be that decreased participation in sport before the first ACL injury is related to the extent to which an individual is willing and able to participate in rehabilitation after ACLR and return to sport with normal neuromuscular control and function.
None of the strength variables tested were significantly associated with risk of CACL injury. This is contrary to prior literature, which reported that decreased lower extremity strength had a significant association with an increased risk of traumatic knee injury in women, including ACL rupture, in a prospective study of 225 high school–aged athletes in Sweden.41
Our study had strengths and potential limitations. An important strength of this work was the prospective study design. This approach allowed all measurements to be acquired from the contralateral leg soon after the initial ACL injury, before the patients underwent ACLR and rehabilitation. Therefore, we were able to capture data pertaining to the knee of interest before a CACL injury occurred, and at a time point that is relevant for informing a patient about the underlying mechanisms associated with an increased risk of suffering this injury. The patients underwent MRI examination of their contralateral limb at the time of the first ACL injury, and all were found to have normal tibiofemoral and patellofemoral joints. In addition, the study focused on CACL injuries and did not combine CACL injuries with graft injuries, as the risk factors for trauma may be different between ligaments and grafts. In addition, our study focused on female athletes and did not include men because the risk factors for a first-time ACL injury are different between the sexes,55 and this may be the case for CACL injuries. There are potential limitations associated with this study, including the number of CACL injuries that occurred during the surveillance period of the study. While our sample size of CACL injuries is small, it is similar to those in prior reports that have used the same prospective cohort study design. This may have limited the statistical power to detect associations with hazard ratios under 2.4, and there was insufficient statistical power for multivariate analysis. While the univariate results of the current study remain valid, multivariate analysis would allow for a greater understanding of the combination of independent risk factors that increase the risk of suffering a CACL injury.50,51,55 Exposure to sport was not measured and used in our analysis; however, all study participants recovered from their ACLR and returned to preinjury sports at the same level of competition. Another potential limitation was the variability between surgical technique and rehabilitation protocol—performed and prescribed by 10 different surgeons—which limits the understanding of the influence of surgery and rehabilitation on the contralateral limb. However, only 1 CACL injury occurred within the first 12 months after primary ACLR, indicating that the variability between surgeons and rehabilitation programs likely did not have a significant effect on the outcome. It is important for us to highlight that our approach was to measure the risk factors for CACL injury soon after the first noncontact ACL injury and before reconstruction, as this is the time point when clinicians and athletes need to establish a plan to prevent subsequent injuries of the same kind. Bilateral neuromuscular and proprioceptive changes have been shown to occur after ACLR and rehabilitation,8,39,54 and consequently it is possible that the contralateral limb underwent deconditioning8,54 and this produced a change in compensatory biomechanics over time.17,40 However, it is unclear to what extent variations between rehabilitation protocols among participants in the present study had an effect on the contralateral limb. Consequently, more research is needed to fully characterize patients’ neuromuscular control and proprioception as they return to sport and activity to understand the interaction between rehabilitation and the risk factors for CACL injury. At the current point in time, this represents a challenge because there are no universally accepted guidelines for return to preinjury sport and activity after ACL injury and reconstruction.
The objective of this investigation was to determine the risk factors for CACL injury in female athletes at the time of unilateral first-time noncontact ACL injury. The risk factors that we found to be associated with subsequent CACL injury among female athletes appear to be distinct from those associated with a first-time ACL injury. While there are many factors that contribute to the risk of suffering CACL injury, the factors examined in the present study can be easily and inexpensively assessed at the time of the first ACL injury. Identification of individuals at increased risk will allow clinicians to use targeted injury prevention programs.2,32,49 This is supported by a recent meta-analysis of meta-analyses that revealed that the use of injury prevention programs can reduce the risk of ACL trauma in female athletes by up to two-thirds.57 While more research with a larger sample size is necessary to further elucidate risk factors and more effectively detect at-risk individuals so injury prevention programs can be targeted toward them, this study demonstrates that there are distinct risk factors for CACL injury after an initial ACL injury.
CONCLUSION
This study of risk factors for noncontact CACL injury after a first-time noncontact ACL injury confirms that the risk factors for CACL injury are distinct from those for first-time ACL injury. A portion of these factors were modifiable (time spent participating in sport, potentially anterior knee stiffness with bracing), while others were nonmodifiable (younger age, increased hip anteversion).
Acknowledgments
One or more of the authors has declared the following potential conflict of interest or source of funding: Support for this investigation came from the National Institutes of Health (NIAMS R01 AR050421-08) and the Robert Larner M.D. College of Medicine. J.R.S. reports education payments from Prodigy Surgical Distribution (Arthrex) and compensation for services other than consulting from Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Footnotes
Investigation performed at Department of Orthopaedics & Rehabilitation, McClure Musculoskeletal Research Center, University of Vermont Larner College of Medicine, Burlington, Vermont, USA
REFERENCES
- 1.Ajuied A, Wong F, Smith C, et al. Anterior cruciate ligament injury and radiologic progression of knee osteoarthritis: a systematic review and meta-analysis. Am J Sports Med. 2014;42(9):2242–2252. [DOI] [PubMed] [Google Scholar]
- 2.Al Attar WS, Soomro N, Pappas E, Sinclair PJ, Sanders RH. Reply to Thorborg et al. : High risk of bias and low transparency in “How effective are F-MARC injury prevention programs for soccer players? A systematic review and meta-analysis”. Sports Med. 2016;46(2):295–296. [DOI] [PubMed] [Google Scholar]
- 3.Amraee D, Alizadeh MH, Minoonejhad H, Razi M, Amraee GH. Predictor factors for lower extremity malalignment and non-contact anterior cruciate ligament injuries in male athletes. Knee Surg Sports Traumatol Arthrosc. 2017;25(5):1625–1631. [DOI] [PubMed] [Google Scholar]
- 4.Beighton P, Solomon L, Soskolne CL. Articular mobility in an African population. Ann Rheum Dis. 1973;32(5):413–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beynnon BD, Hall JS, Sturnick DR, et al. Increased slope of the lateral tibial plateau subchondral bone is associated with greater risk of non-contact ACL injury in females but not in males: a prospective cohort study with a nested, matched case-control analysis. Am J Sports Med. 2014;42(5):1039–1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beynnon BD, Johnson RJ, Toyama H, Renstrom PA, Arms SW, Fischer RA. The relationship between anterior-posterior knee laxity and the structural properties of the patellar tendon graft. A study in canines. Am J Sports Med. 1994;22(6):812–820. [DOI] [PubMed] [Google Scholar]
- 7.Beynnon BD, Vacek PM, Newell MK, et al. The effects of level of competition, sport, and sex on the incidence of first-time noncontact anterior cruciate ligament injury. Am J Sports Med. 2014;42(8):1806–1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chung KS, Ha JK, Yeom CH, et al. Are muscle strength and function of the uninjured lower limb weakened after anterior cruciate ligament injury? Two-year follow-up after reconstruction. Am J Sports Med. 2015;43(12):3013–3021. [DOI] [PubMed] [Google Scholar]
- 9.Cloninger CR, Svrakic DM, Wetzel RD. The Temperament and Character Inventory (TCI): A Guide to Its Development and Use. St. Louis, MO: Center for Psychobiology of Personality, Washington University; 1994. [Google Scholar]
- 10.Faltstrom A, Hagglund M, Magnusson H, Forssblad M, Kvist J. Predictors for additional anterior cruciate ligament reconstruction: data from the Swedish national ACL register. Knee Surg Sports Traumatol Arthrosc. 2016;24(3):885–894. [DOI] [PubMed] [Google Scholar]
- 11.Fleming BC, Brattbakk B, Peura GD, Badger GJ, Beynnon BD. Measurement of anterior-posterior knee laxity: a comparison of three techniques. J Orthop Res. 2002;20(3):421–426. [DOI] [PubMed] [Google Scholar]
- 12.Flynn RK, Pedersen CL, Birmingham TB, Kirkley A, Jackowski D, Fowler PJ. The familial predisposition toward tearing the anterior cruciate ligament: a case control study. Am J Sports Med. 2005;33(1): 23–28. [DOI] [PubMed] [Google Scholar]
- 13.Gordon MD, Steiner ME. Anterior cruciate ligament injuries. In: Garrick JG, ed. Orthopaedic Knowledge Update Sports Medicine III. Rose-mont, IL: American Academy of Orthopaedic Surgeons; 2004:169. [Google Scholar]
- 14.Hasue M, Fujiwara M, Kikuchi S. A new method of quantitative measurement of abdominal and back muscle strength. Spine (Phila Pa 1976). 1980;5(2):143–148. [DOI] [PubMed] [Google Scholar]
- 15.Hewett TE, Myer GD, Ford KR. Anterior cruciate ligament injuries in female athletes: Part 1, mechanisms and risk factors. Am J Sports Med. 2006;34(2):299–311. [DOI] [PubMed] [Google Scholar]
- 16.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492–501. [DOI] [PubMed] [Google Scholar]
- 17.Hofbauer M, Thorhauer ED, Abebe E, Bey M, Tashman S. Altered tibiofemoral kinematics in the affected knee and compensatory changes in the contralateral knee after anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42(11):2715–2721. [DOI] [PubMed] [Google Scholar]
- 18.Imwalle LE, Myer GD, Ford KR, Hewett TE. Relationship between hip and knee kinematics in athletic women during cutting maneuvers: a possible link to noncontact anterior cruciate ligament injury and prevention. J Strength Cond Res. 2009;23(8):2223–2230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Johnston JT, Mandelbaum BR, Schub D, et al. Video analysis of anterior cruciate ligament tears in professional American football athletes. Am J Sports Med. 2018;46(4):862–868. [DOI] [PubMed] [Google Scholar]
- 20.Kaeding CC, Pedroza AD, Reinke EK, Huston LJ, Consortium M, Spindler KP. Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med. 2015;43(7):1583–1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kaneko M, Sakuraba K. Association between femoral anteversion and lower extremity posture upon single-leg landing: implications for anterior cruciate ligament injury. J Phys Ther Sci. 2013;25(10):1213–1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Levins JG, Argentieri EC, Sturnick DR, et al. Geometric characteristics of the knee are associated with a noncontact ACL injury to the contralateral knee after unilateral ACL injury in young female athletes. Am J Sports Med. 2017;45(14):3223–3232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Levins JG, Sturnick DR, Argentieri EC, et al. Geometric risk factors associated with noncontact anterior cruciate ligament graft rupture. Am J Sports Med. 2016;44(10):2537–2545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leys T, Salmon L, Waller A, Linklater J, Pinczewski L. Clinical results and risk factors for reinjury 15 years after anterior cruciate ligament reconstruction: a prospective study of hamstring and patellar tendon grafts. Am J Sports Med. 2012;40(3):595–605. [DOI] [PubMed] [Google Scholar]
- 25.Lohmander LS, Ostenberg A, Englund M, Roos H. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum. 2004;50(10):3145–3152. [DOI] [PubMed] [Google Scholar]
- 26.Maletis GB, Inacio MC, Funahashi TT. Risk factors associated with revision and contralateral anterior cruciate ligament reconstructions in the Kaiser Permanente ACLR registry. Am J Sports Med. 2015; 43(3):641–647. [DOI] [PubMed] [Google Scholar]
- 27.Markolf KL, Mensch JS, Amstutz HC. Stiffness and laxity of the knee—the contributions of the supporting structures. A quantitative in vitro study. J Bone Joint Surg Am. 1976;58(5):583–594. [PubMed] [Google Scholar]
- 28.McLean SG, Mallett KF, Arruda EM. Deconstructing the anterior cruciate ligament: what we know and do not know about function, material properties, and injury mechanics. J Biomech Eng. 2015; 137(2):020906. [DOI] [PubMed] [Google Scholar]
- 29.Montalvo AM, Schneider DK, Yut L, et al. “What’s my risk of sustaining an ACL injury while playing sports?” A systematic review with meta-analysis. Br J Sports Med. 2019;53:1003–1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nguyen AD, Shultz SJ, Schmitz RJ. Landing biomechanics in participants with different static lower extremity alignment profiles. J Athl Train. 2015;50(5):498–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nguyen AD, Shultz SJ, Schmitz RJ, Luecht RM, Perrin DH. A preliminary multifactorial approach describing the relationships among lower extremity alignment, hip muscle activation, and lower extremity joint excursion. J Athl Train. 2011;46(3):246–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Noyes FR, Barber-Westin SD. Neuromuscular retraining intervention programs: do they reduce noncontact anterior cruciate ligament injury rates in adolescent female athletes? Arthroscopy. 2014;30(2): 245–255. [DOI] [PubMed] [Google Scholar]
- 33.Oiestad BE, Holm I, Aune AK, et al. Knee function and prevalence of knee osteoarthritis after anterior cruciate ligament reconstruction: a prospective study with 10 to 15 years of follow-up. Am J Sports Med. 2010;38(11):2201–2210. [DOI] [PubMed] [Google Scholar]
- 34.Paterno MV, Kiefer AW, Bonnette S, et al. Prospectively identified deficits in sagittal plane hip-ankle coordination in female athletes who sustain a second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Clin Biomech (Bristol, Avon). 2015;30(10):1094–1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med. 2014;42(7):1567–1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968–1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Powers CM. The influence of abnormal hip mechanics on knee injury: a biomechanical perspective. J Orthop Sports Phys Ther. 2010; 40(2):42–45. [DOI] [PubMed] [Google Scholar]
- 38.Ramesh R, Von Arx O, Azzopardi T, Schranz PJ. The risk of anterior cruciate ligament rupture with generalised joint laxity. J Bone Joint Surg Br. 2005;87(6):800–803. [DOI] [PubMed] [Google Scholar]
- 39.Roberts D, Friden T, Stomberg A, Lindstrand A, Moritz U. Bilateral proprioceptive defects in patients with a unilateral anterior cruciate ligament reconstruction: a comparison between patients and healthy individuals. J Orthop Res. 2000;18(4):565–571. [DOI] [PubMed] [Google Scholar]
- 40.Roewer BD, Di Stasi SL, Snyder-Mackler L. Quadriceps strength and weight acceptance strategies continue to improve two years after anterior cruciate ligament reconstruction. J Biomech. 2011;44(10):1948–1953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ryman Augustsson S, Ageberg E. Weaker lower extremity muscle strength predicts traumatic knee injury in youth female but not male athletes. BMJ Open Sport Exerc Med. 2017;3(1):e000222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Salmon L, Russell V, Musgrove T, Pinczewski L, Refshauge K. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy. 2005;21(8): 948–957. [DOI] [PubMed] [Google Scholar]
- 43.Schilaty ND, Nagelli C, Bates NA, et al. Incidence of second anterior cruciate ligament tears and identification of associated risk factors from 2001 to 2010 using a geographic database. Orthop J Sports Med. 2017;5(8):2325967117724196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schmitz RJ, Ficklin TK, Shimokochi Y, et al. Varus/valgus and internal/external torsional knee joint stiffness differs between sexes. Am J Sports Med. 2008;36(7):1380–1388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2009;37(2):246–251. [DOI] [PubMed] [Google Scholar]
- 46.Shultz SJ, Dudley WN, Kong Y. Identifying multiplanar knee laxity profiles and associated physical characteristics. J Athl Train. 2012;47(2):159–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shultz SJ, Nguyen AD, Levine BJ. The relationship between lower extremity alignment characteristics and anterior knee joint laxity. Sports Health. 2009;1(1):54–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shultz SJ, Nguyen AD, Windley TC, Kulas AS, Botic TL, Beynnon BD. Intratester and intertester reliability of clinical measures of lower extremity anatomic characteristics: implications for multicenter studies. Clin J Sport Med. 2006;16(2):155–161. [DOI] [PubMed] [Google Scholar]
- 49.Silvers-Granelli H, Mandelbaum B, Adeniji O, et al. Efficacy of the FIFA 111 injury prevention program in the collegiate male soccer player. Am J Sports Med. 2015;43(11):2628–2637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sturnick DR, Vacek PM, DeSarno MJ, et al. Combined anatomic factors predicting risk of anterior cruciate ligament injury for males and females. Am J Sports Med. 2015;43(4):839–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sturnick DR, Van Gorder R, Vacek PM, et al. Tibial articular cartilage and meniscus geometries combine to influence female risk of anterior cruciate ligament injury. J Orthop Res. 2014;32(11):1487–1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tourville TW, Smith HC, Shultz SJ, et al. Reliability of a new stabilized dynamometer system for the evaluation of hip strength. Sports Health. 2013;5(2):129–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Uhorchak JM, Scoville CR, Williams GN, Arciero RA, St Pierre P, Taylor DC. Risk factors associated with noncontact injury of the anterior cruciate ligament: a prospective four-year evaluation of 859 West Point cadets. Am J Sports Med. 2003;31(6):831–842. [DOI] [PubMed] [Google Scholar]
- 54.Urbach D, Nebelung W, Weiler HT, Awiszus F. Bilateral deficit of voluntary quadriceps muscle activation after unilateral ACL tear. Med Sci Sports Exerc. 1999;31(12):1691–1696. [DOI] [PubMed] [Google Scholar]
- 55.Vacek PM, Slauterbeck JR, Tourville TW, et al. Multivariate analysis of the risk factors for first-time noncontact ACL injury in high school and college athletes: a prospective cohort study with a nested, matched case-control analysis. Am J Sports Med. 2016;44(6):1492–1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wang HM, Shultz SJ, Schmitz RJ. Association of anterior cruciate ligament width with anterior knee laxity. J Athl Train. 2016;51(6):460–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Webster KE, Hewett TE. Meta-analysis of meta-analyses of anterior cruciate ligament injury reduction training programs. J Orthop Res. 2018;36(10):2696–2708. [DOI] [PubMed] [Google Scholar]
- 58.Whitney DC, Sturnick DR, Vacek PM, et al. Relationship between the risk of suffering a first-time noncontact ACL injury and geometry of the femoral notch and ACL: a prospective cohort study with a nested case-control analysis. Am J Sports Med. 2014;42(8):1796–1805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2016;44(7):1861–1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wright RW, Dunn WR, Amendola A, et al. Risk of tearing the intact anterior cruciate ligament in the contralateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction: a prospective MOON cohort study. Am J Sports Med. 2007;35(7):1131–1134. [DOI] [PubMed] [Google Scholar]


