Abstract
Benefits of physical activity (PA) in breast cancer survivors (BCS) are well established. However, programs to promote PA among BCS tailored to real-world contexts within low- to middle-income countries are limited. Cross-sector co-creation can be key to effective and scalable programs for BCS in these countries. This study aimed to evaluate the networking process to engage multisector stakeholders in the co-creation of a PA program for Colombian BCS called My Body. We employed a mixed-methods design including semistructured interviews, workshops and a social network analysis of centrality measures to assess stakeholders’ engagement, resources and skills enabling the collaborative work, challenges, outcomes and lessons learned. The descriptive analysis and the centrality measures of the network revealed that 19 cross-sector stakeholders engaged in the My Body collaborative network. Through ongoing communication and cooperation, My Body built relationships between the academic lead institutions (local and international), and local and national public, private and academic institutions working in public health, sports and recreation, social sciences and engineering fields. The outcomes included the co-creation of the community-based PA program for BCS, its implementation through cross-sector synergies, increased relationships and communications among stakeholders, and successful dissemination of evidence and project results to the collaboration partners and other relevant stakeholders and community members. The mixed-methods assessment enabled understanding of ways to advance cross-sector co-creation of health promotion programs. The findings can help to enable continued development of sustainable cross-sector co-creation processes aimed at advancing PA promotion.
Keywords: mixed-methods, cross-sector collaboration, physical activity, cancer, social network analysis
INTRODUCTION
Physical activity (PA) programs for breast cancer survivors (BCS) provide an opportunity to produce changes in health-related behaviors and improve self-care practices as preventive measures to reduce the risk of cancer recurrence and mortality, as well as the development of other noncommunicable diseases (Battaglini, 2014; Jankowski et al., 2014). Regular PA can be effective for health and functional outcomes enhancement, and can promote quality of life (Zhu et al., 2016; Covington et al., 2019). Despite the evidence that supports the benefits of PA in BCS (Battaglini, 2014; 2018 Physical Activity Guidelines Advisory Committee, 2018) and support for translating recommendations into strategies tailored to real-world settings, there currently is limited focus on such PA programs within low- to middle-income countries (LMIC) (Rositch et al., 2020). These countries are currently facing not only the increasing burden of providing timely diagnosis and treatment, but also the need for effective and feasible strategies to improve survivorship and quality of life among BCS (Lopez-Class et al., 2012; Johnson et al., 2018; Franco-Rocha et al., 2021).
The Colombian healthcare system provides ‘universal coverage’ through the mandatory national social insurance scheme. In theory, all services for cancer care (primary prevention, screening and early detection, diagnostic services, oncological treatments and palliative care) are available in the Colombian healthcare system, however, access is a challenge (Murillo et al., 2016). From the demand side, poverty, health literacy, beliefs and knowledge are barriers to cancer care. From the supply side, availability of services, fragmentation in services provision and the existence of administrative barriers hinder access to cancer care (de Vries et al., 2018; Franco-Rocha et al., 2021). In Colombia, 13 380 women are newly diagnosed with breast cancer annually, and the 5-year net survival for women diagnosed with this type of cancer is 72.15% (Allemani et al., 2018). Educational attainment, socioeconomic status and administrative barriers have been associated to breast cancer patients’ delays in access to treatment (de Vries et al., 2018). Additionally, survivors’ ongoing needs are a critical gap in Colombian governmental and research literature (Franco-Rocha et al., 2021). In fact, healthcare overall monitoring, oversight and research aimed at BCS health enhancement is weak and mainly limited to the clinical sphere. A medicalization focus has prevailed, downplaying nonpharmaceutical strategies, such as PA, that can mitigate physical, psychological and social health challenges associated with BC survivorship (Spector et al., 2012; Caperchione et al., 2016).
Coordination within and beyond the health sector is a priority for strengthening healthcare services for BCS in Colombia. To accomplish this, the Colombian Comprehensive Health Care Policy (Ministerio de Salud y Protección Social de Colombia, 2016b) proposed comprehensive healthcare pathways for (i) health promotion and maintenance, (ii) risk groups (such as cancer patients) and (iii) specific events (Ministerio de Salud y Protección Social de Colombia, 2016a). The implementation of these pathways is an ongoing process seeking the progressive development of interventions through the collaborative work of multiple actors, sectors and the community (Ministerio De Salud y Protección Social de Colombia, 2013b).
The implementation of community-wide programs has been highlighted as a key investment for increasing PA (International Society for Physical Activity and Health (ISPAH), 2020). However, there is limited evidence on the process of integrating PA interventions into practice especially from controlled research conditions into real-world community settings (Cooper et al., 2021). Previous studies in high-income countries (HIC) on the translation of evidence-based interventions to real-world settings have implemented innovative community-based programs to promote PA targeted to BCS’ needs and interests (Caperchione et al., 2019; Pullen et al., 2019). However, little is known about the implementation of evidence-based interventions in community settings in LMIC countries (Cooper et al., 2021). Therefore, it is necessary to systematically document and analyze which coordinated actions at multiple levels may encourage cross-sector cooperation to co-create multidisciplinary health-promoting programs in LMIC real-world settings (Frahsa et al., 2014; Hope Corbin et al., 2018; Leask et al., 2019).
Colombia has significant experience in developing community-wide publicly funded PA programs, which have shown promise to increase PA levels (Torres et al., 2016; Díaz del Castillo et al., 2017). The ‘Recreovía’ program, coordinated by Bogotá’s District Sports and Recreation Institute (IDRD, by its initials in Spanish), has offered free PA classes in public parks since 1995, increasing PA levels particularly among women by incorporating dance in guided sessions (Díaz del Castillo et al., 2017). For this reason, acknowledging the current constraints within the healthcare system to increase opportunities for BCS to be active, we proposed to leverage the experience of the Recreovía community-wide program and facilitate synergies between multisector stakeholders, to co-create a theory-driven, community-based group dance intervention to promote PA among BCS, delivered by Bogotá’s capital district government. Promoting multisectoral engagement has been reported as a relevant strategy to co-create evidence-based, context-specific, accessible and culturally appropriate health enhancing interventions in real-world settings, with potential to be translated into policy (Hämäläinen et al., 2016; Hope Corbin et al., 2018; Leask et al., 2019; Laird et al., 2020).
As stakeholders are urged to strengthen their collaborations and networks, the use of tools such as social network analysis (SNA) can provide a means of evaluating the composition and functioning of the networks (Haines et al., 2011). SNA has been used to plan and evaluate collaborative research in public health by analyzing the cooperation structure (Kothari et al., 2014). In the Colombian context, the Ciclovía (open-streets to promote PA) and the Recreovía programs are examples of multisectoral programs aimed at addressing public health problems which have been evaluated using SNA (Meisel et al., 2014; Jaramillo et al., 2020).
In this context, this research aimed to evaluate the networking process to co-create the My Body PA program by systematically (i) assessing stakeholders’ engagement in the cross-sector network; (ii) identifying resources and skills that facilitated the cross-sector collaboration; (iii) highlighting real-world challenges and outcomes of the co-creation and (iv) identifying lessons learned from the collaborative network.
METHODS
Study setting
The study was conducted in Bogotá, Colombia. In Colombia, comprehensive care and PA promotion have been on the public agenda for more than 10 years (Ministerio de Salud y Protección Social de Colombia, 2013a; 2018). Separate entities at the national and local levels coordinate services to cover the healthcare sector and the recreation, sports and leisure sector. While municipal efforts have, since 2008, aimed to foster cross-sector strategies to promote PA in clinical and community populations (Gaffney et al., 2019), no systematic processes have been employed to evaluate such efforts.
My Body intervention
My Body was a theory-driven, community-based intervention to promote PA through dancing among BCS, delivered by a public entity using a ‘real-world’ community setting approach. The behavioral theories that informed the intervention were social cognitive and self-determination (Pudkasam et al., 2018; McEwan et al., 2020). The dance-based 8-week intervention included group-based sessions 3 times/week 45 min initially, followed by 5-min increases/week, until reaching 60 min by the week 5, plus 10-min warm-up and 10-min cool-down activities. PA intensity increases were determined using maximum heart rate (HR) based on reference equations for BCS and considering the relationship between expected exercise HR and tempo or speed of a given song (Karageorghis et al., 2011). Based on this, the playlist music was selected according to each song’s tempo (beats per minute) and expected exercise HR to maintain a comfortable level of exertion during the exercise (Yamashita et al., 2006), included culturally relevant rhythms. The researchers designed a psychoeducational booklet for BCS (validated with stakeholders) containing behavior change activities (e.g. personalized goal-setting, self-monitoring, overcoming PA barriers, decisional balance—weighing the pros and cons—of being active) (Pinto and Ciccolo, 2011; Grimmett et al., 2019). As will be described throughout this paper, the intervention components and delivery were agreed by members of the interdisciplinary research team, one BCS (who was from a local-private public health institution) and professionals in respiratory therapy, physical education, psychology, behavioral sciences, sports medicine and physiotherapy representing different public, private and academic institutions. During facilitated workshops, stakeholders reviewed the international evidence-based PA guidance for cancer survivors (Campbell et al., 2019; Schmitz et al., 2019), built consensus on the components for the dance-based protocol, and PA instructors, certified by the Recreovía program, were trained in behavior change premises by members of the research team, to deliver the behavior change strategies.
Complete findings from the quasi-experimental study conducted to assess the acceptability and preliminary effectiveness of My Body dance intervention are reported elsewhere (under review). Recruitment was conducted in collaboration with partner organizations. BCS were recruited through word of mouth, flyers and social media. Eligible women were BCS at least 6 months post completion of their treatment, more than 18 years of age, living in Bogotá, and willing to attend the program and its associated assessments at Universidad de los Andes. Participants were assessed by the project’s sports medicine physicians. The first half of the participants with physicians’ approval were allocated to the intervention group (N = 31), while the second half were allocated to the control group (N = 33). We found increases in average minutes of moderate-to-vigorous PA per day (intervention: +8.99 vs. control: −3.7 min; p = 0.01), and in ratings of motivation (p = 0.01). Through interviews, BCS reported satisfaction with the program (i.e. sessions, instructors, practicing PA with peers). Participants in the control group received the PA intervention at the end of the 8-week study period after completing the pre–post study assessments. These results indicated that My Body has potential to increase PA levels and motivation and to contribute to well-being.
Study design
Using a multidisciplinary approach, this study is based on actor-network theory, which posits that a public health intervention is a complex system mobilizing actors from various sectors (Bilodeau and Potvin, 2018). The connection of actors is a relational process that shapes—and is shaped by—networks (Bilodeau and Potvin, 2018). To better capture My Body’s complex system, this study employed a convergent mixed-methods approach (Pluye and Hong, 2014), integrating qualitative and quantitative data to systematically evaluate stakeholders’ networking. The qualitative component included data collected through interviews and workshops, and the quantitative component included SNA measures. Throughout the paper, we will use the term ‘stakeholder’ to refer to research, policy and practice actors from various sectors that have been part of the My Body network. ‘Cross-sector collaboration’ describes the partnership that results when individuals and institutions from different sectors come together to use their diverse perspectives and resources to jointly achieve a shared goal. ‘Sector’ refers to different economic entities (public, private and nonprofit, such as academia), different levels of decision-making (local, national and international) or different governmental or disciplinary fields (such as health, sports, education and transport) (Hämäläinen et al., 2016).
Ethical approval for this project was granted by the committee for ethics in research at Universidad de los Andes (ethical approval #949 2018).
Qualitative component
To document thoroughly every stage of the networking process, we employed an array of qualitative methodologies, including semistructured interviews and facilitated workshops (Supplementary Table S1; Tables 1 and 2). Purposive sampling methods were used to identify interviewees with expertise regarding PA promotion and the care of cancer patients. From September 2018 to August 2020, we used snowball sampling to contact local- and national-level healthcare and sports and recreation authorities, healthcare services providers, nongovernmental community organizations and academic researchers from different universities. First, we contacted policymakers with whom we had prior collaborative research experience to promote PA, enabled by the citizen science approach ‘Our Voice’ (Rubio et al., 2020, 2022). These stakeholders introduced us, in turn, to other relevant stakeholders. Two researchers (M.R. and D.M.) with training and experience in qualitative interviewing conducted the semistructured interviews. We conducted interviews until we reached thematic saturation or the point at which no new information emerged. Interviews were conducted in a quiet area in the interviewees’ workplace, with average duration of 35 min. The research team facilitated virtual or in-person workshops at stakeholders’ or Universidad de los Andes’ facilities:
Table 1:
Qualitative and quantitative measures to assess My Body network
| Dimension | Data source | Outcome measures |
|---|---|---|
|
Engagement
Cross-sector stakeholders contributing to synergies between research, policy and practice to advance the design, implementation, evaluation and dissemination of community-based PA promotion targeted to BCS |
Qualitative methods | Descriptive analysis of the context and the shared objectives that enabled cross-sector networking |
| Quantitative methods | Measurement of the cross-sectoral composition of the network: - Number of stakeholders (institutions) that participated in My Body network - Level of engagement according to two SNA centrality measures: degree and weighted degree |
|
|
Resources and skills
Institutional resources and individual skills relevant to advance collaborative work within the cross-sector network |
Qualitative methods | Descriptive analysis of reported resources and skills that facilitated the collaborative work and the implementation of the My Body program |
| Quantitative methods | Measurement of influential institutions that intermediated the information flows through the network (betweenness centrality measure) | |
| Challenges and outcomes of the collaborative network Stakeholders’ perceived setbacks challenging the collaboration and highlighted outcomes |
Qualitative methods | Descriptive analysis of the co-creation challenges and outcomes Descriptive analysis of stakeholders’ roles in the implementation of My Body program |
| Lessons learned Stakeholders’ perceived opportunities to improve and maintain the cross-sector network and My Body program |
Qualitative methods | Descriptive analysis of stakeholders’ evaluation of My Body program including lessons learned and policy recommendations |
| Quantitative methods | Descriptive analysis of network growth over time according to the institutions’ attributes |
Qualitative and quantitative measures to assess My Body network.
Table 2:
Stakeholders engaged in My Body cross-sector network
| Institution | Label | Level of decision-making | Sector | Governmental or disciplinary field | Description of the institution/role in My Body program | |
|---|---|---|---|---|---|---|
| 1 | Stanford University | International academic partner | International | Academia | Public Health; Social Sciences | One of the world’s leading research universities. Research and teaching stress interdisciplinary approaches to problem solving. Professors advised the design, implementation and analysis of the program and outcomes. |
| 2 | Universidad de los Andes | Leading institution | Local | Academia | Public Health/Social Sciences/Engineering | Colombian university contributing to the national and regional scientific and technological development. The research group of epidemiology of the school of medicine was the coordinating unit leading the design, implementation and evaluation of the program and outcomes. |
| 3 | Universidad Manuela Beltrán | Local-academic sports and recreation institution | Local | Academia | Sports and Recreation | University in Bogotá contributing to the national scientific development, with expertise in disciplinary fields such as health, physical education, physical therapy and sports. A professor from the sports and recreation field advised on the design and implementation of the PA program. |
| 4 | Universidad Libre | Local-academic sports and recreation institution | Local | Academia | Sports and Recreation | University in Bogotá contributing to the national scientific development, with expertise in disciplinary fields such as physical education and sports and recreation. A professor from the sports and recreation field advised on the design and implementation of the PA program. |
| 5 | Universidad Nacional de Colombia | National-academic public health institution | National | Academia | Public Health | Colombian university contributing to the national and regional scientific and technological development. Professors from public health advised on the design of the PA program and the dissemination of results. |
| 6 | Pontificia Universidad Javeriana | Local-academic public health institution | Local | Academia | Public Health | Colombian university contributing to the national and regional scientific and technological development. A physical education professor advised on the design of the PA program and the dissemination of results. |
| 7 | Universidad del Rosario | Local-academic public health institution | Local | Academia | Public Health | Colombian university contributing to the national and regional scientific and technological development. A physical education professor advised on the design of the project. |
| 8 | Instituto Distrital de Recreación y Deporte (IDRD) (District’s Institute for Recreation and Sports) | Local-public sports and recreation institution | Local | Public | Sports and Recreation | The governmental institution in charge of the promotion of recreation, PA, the good use of parks and sports in Bogotá. This entity coordinates the community-based PA program Recreovía. Representatives advised and assisted the design and implementation of the program. The institution provided the PA instructors and the facility for the delivery of the program. |
| 9 | Secretaría Distrital de Salud (District’s Health Department) | Local-public public health institution | Local | Public | Public Health | The governmental institution in charge of preventing disease and guaranteeing access to health services to all residents of Bogotá. Representatives advised and assisted the implementation of the program. A nutritionist delivered two nutrition workshops and supplied recipe books for BCS. |
| 10 | Secretaría Distrital de la Mujer (District’s Women Department) | Local-public public health institution | Local | Public | Public Health; Social Sciences | The governmental institution in charge of the public policy to protect women’s rights and promote gender equality. A representative advised on the design and dissemination of the program. |
| 11 | Ministerio de Salud y Protección Social (Ministry of Health and Social Security) | National-public public health institution | National | Public | Public Health | Directs and organizes the health system to guarantee access to health services and disease prevention programs throughout the country. Representatives advised on the design and dissemination of the program. |
| 12 | Instituto Nacional de Cancerología (National cancer institute) | National-public clinic and public health institution | National | Public | Clinic; Public Health | Entity of the national order, attached to the Ministry of Health and Social Protection, in charge of advising on cancer-related policies, research and practice. It is a teaching center and a hospital specialized in oncology care. A representative advised on the design of the program. |
| 13 | Hospital San Blas (San Blas Hospital) | Local-public clinic institution | Local | Public | Clinic | Public hospital that has diagnostic and therapeutic support units for all medical specialties. A representative advised on the design of the program. |
| 14 | Fundación SIMMON (SIMMON Foundation) | Local-private public health institution | Local | Private | Public Health | Community organization created to contribute to improving quality of life of cancer patients, their families and caregivers. Representatives engaged on the open call to recruit BCS and provided databases. |
| 15 | Fundación ANNAS (ANNAS Foundation) | National-private public health institution | National | Private | Public Health | Community organization committed to evidence dissemination and political incidence aimed at informing and promoting public policy to achieve the 2030 Sustainable Development Goals. A representative advised on the dissemination of the program outcomes. |
| 16 | Liga Contra el Cáncer de Bogotá (Bogotá’s League Against Cancer) | Local-private clinic institution | Local | Private | Clinic | Healthcare services provider and community organization contributing to education, prevention and early diagnosis and treatment of cancer. Representatives engaged on the open call to recruit BCS and provided databases. |
| 17 | Asociación Ámese (Ámese Foundation) | Local-private public health institution | Local | Private | Public Health | Community organization created to contribute to disseminating knowledge and self-care of the breast for an early diagnosis. Representatives engaged on the open call to recruit BCS and provided databases. |
| 18 | Hospital de San José (San José Hospital) | Local-academic clinic institution | Local | Academia | Clinic | Scientific and educational entity opened in 1925. The Hospital is a university institution that has diagnostic and therapeutic support units for all medical specialties. Sports medicine physicians screened the BCS to ensure they had the physical aptitude to participate in the intervention. |
| 19 | TransMilenio | Local-private transportation institution | Local | Private | Transportation | Manages the Integrated Public Transport System in Bogotá. Representatives attended some meetings during the design stage of the program. |
Stakeholders engaged in My Body cross-sector network.
The first phase included in-person interviews with 15 stakeholders that assessed local needs regarding PA promotion among BCS.
The second phase included three in-person workshops with total participation of 11 stakeholders with the purpose of finalizing intervention content and validating the design of the breast cancer-specific dance-based PA intervention.
The third phase included one in-person workshop (n = 8) and seven interviews (via telephone or through online platforms due to restrictions during COVID-19 pandemic) which evaluated the process, validated study findings and also discussed the maintenance of the collaborative network and the PA intervention as a community-based, publicly funded program.
All collected data were analyzed using thematic analysis (Catherine et al., 2000). The analytic categories were specific and relevant to each study phase (Supplementary Table S1). Data from the first phase were used to inform the design of My Body study, results from phase 2 are detailed in the co-created protocol. In this paper, we present findings from the third phase as the elements that in the end showed to be key for the co-creation of My Body. Iteration, which is defined as a cyclical process and key to learning in co-creation (Leask et al., 2019), was used throughout the analytical process to maintain methodological rigor. The transcripts from the data collected in the third phase were analyzed using categories that emerged from (i) the literature review process and (ii) through identifying iterative categories provided by the interviews. Four researchers (D.M., P.G., C.T. and M.D.) independently analyzed all transcripts using a matrix in Excel to systematically document the emergent themes related to the following categories: stakeholders’ engagement, challenges, resources and skills for collaborative work, outcomes and lessons learned. To identify the salient themes per category, the researchers discussed the findings in monthly meetings over 6 months following an iterative reflection process (Leask et al., 2019).
Quantitative component
We systematically monitored all study-related meetings to track the development of the collaborative network and conducted SNA to characterize the network composition, i.e. the number of engaged stakeholders, their institutional attributes and their relevance in the network according to the SNA centrality measures (Valente, 2012). The SNA methodology allowed us to map cross-sector stakeholders, characterize their attributes, model the interactions of the institutions and draw conclusions about the level and types of engagement determined by these interactions. First, we developed a tracking system tool in MS Excel to capture each meeting from 2017 to 2020. Data captured included the date, the attributes of participants (institutional affiliation; governmental or disciplinary field, including public health, sports and recreation, clinic, social sciences, transportation or engineering) and the attributes of the institutions (level of decision-making, i.e. local, national, international; type of sector, i.e. academy, public, private). Second, we modeled an undirected temporal network in which the nodes were the institutions, and their attributes were given by the attributes registered for each institution and of its affiliated participants. For example, if an institution included participants from the clinic and public health fields, the node was assigned with both values for the field attribute. The formation of an edge between two nodes was given based on the first time that two institutions met. Therefore, at a given point in time, the number of edges adjacent to each node (defined as ‘degree’ in SNA) corresponded to the number of institutions with which each institution had met up until that time point.
Also, each edge between two institutions has a weight that increases over time indicating the accumulated number of meetings between a given pair of institutions. The weighted degree was also calculated for each institution to measure the total number of meetings held with other institutions. This metric is represented by the sum of the edges’ weight adjacent to a given institution. We measured the change over time of the engagement of each institution in the network by using the degree and weighted degree measures (Pryke, 2005; Monaghan et al., 2017; Jasny et al., 2021) since these quantify the connectivity and participation of the institutions within the network. Betweenness centrality measures the extent to which a node lies on paths between other nodes, providing information about the influence institutions have over the flow of information among them. We analyzed the interactions defined by this network according to the level, sector and disciplinary field of each institution.
Data triangulation
We used a simultaneous bidirectional integration approach (Moseholm and Fetters, 2017) to triangulate the qualitative and quantitative results. Through an iterative process of revisiting the main findings, the researchers assessed through ongoing meetings the convergence of the datasets: (i) Qualitative results regarding each evaluated dimension (engagement, challenges, resources and skills, outcomes and lessons learned) and (ii) SNA results regarding the size, composition, interactions and changes over time of the network (Online resource 2). The final interpretation of triangulated results was written up as a manuscript and circulated to the research team to ensure an accurate version of events was documented.
RESULTS
The stakeholders that participated in phase 3 evaluating the co-creation process, included PA policymakers from the local- and national-level healthcare authorities (n = 2); and practitioners affiliated with multisectoral organizations that were involved in different roles for the implementation of My Body intervention (n = 5) (Online resource 1). We identified three salient themes per each dimension evaluated: engagement (i.e. ‘normative frameworks’, ‘political context’, ‘common goals’), challenges (‘safety concerns’, ‘administrative barriers’, ‘recruitment’), resources and skills (‘communication’, ‘cooperation’, ‘multidisciplinary approach’), lessons learned (‘windows of opportunity’, ‘communication’, ‘dissemination’).
Engagement
Both qualitative and quantitative findings indicate that the engagement in the collaborative network allowed building meaningful relationships. Through the interviews, the stakeholders indicated that the main factor supporting the favorable context to engage in the collaborative network was the existing normative framework from the local- and national-level government for PA-supportive strategies. In the last decade, the normative framework endorsing cross-sector partnerships to promote PA among different populations, such as BCS, has grown. The stakeholders noted, however, that despite this normative context, there was a gap in the translation of policy to real-world settings. Focusing on BCS-specific needs, they identified the scarcity of comprehensive health-promoting programs for cancer survivors, particularly integrating exercise prescription and practice into clinical care, and the lack of a healthcare mechanism to follow up BCS upon finalizing cancer treatment in order to identify those at higher risk (due to comorbidities, age, socioeconomic status) as well as facilitate referrals to appropriate community-facing PA programs.
Additionally, stakeholders underscored the political context as a determinant of the cross-sector collaboration. On the one side, they perceived that the current mayor’s administration (2016–2019) focus was on infrastructure for public spaces and government branding, rather than financing the strengthening of health-related programs. However, the subsequent mayor’s administration (2020–2023) has encouraged the strengthening of community-based health-promoting programs focused on prioritized populations such as women BCS. On the other side, stakeholders stressed that citizens’ distrust toward the governmental sector and negative perceptions of the quality of the healthcare system affects uptake of community-based PA programs in Bogotá.
Underscoring these contextual facts, the stakeholders saw My Body as an opportunity to engage in collaborative work with cross-sector peers who shared common goals. The reported shared objectives were to (i) increase the quality of life of BCS, particularly underserved individuals; (ii) identify opportunities and roles in different sectors to encourage better institutional practices aimed at optimizing the use of resources (human, economic, logistics) for PA promotion; (iii) promote a holistic perspective within each institutional setting to leverage multisectoral partnerships and policy impacts and (iv) follow the global, national and local agendas aimed at preventing noncommunicable diseases from a comprehensive, intersectoral perspective.
One stakeholder stated: ‘I had never worked in a successful intersectoral program like this (…) [The study showed the importance of research]—something that is not a high priority at this time among governmental institutions’ (Interviewee 2).
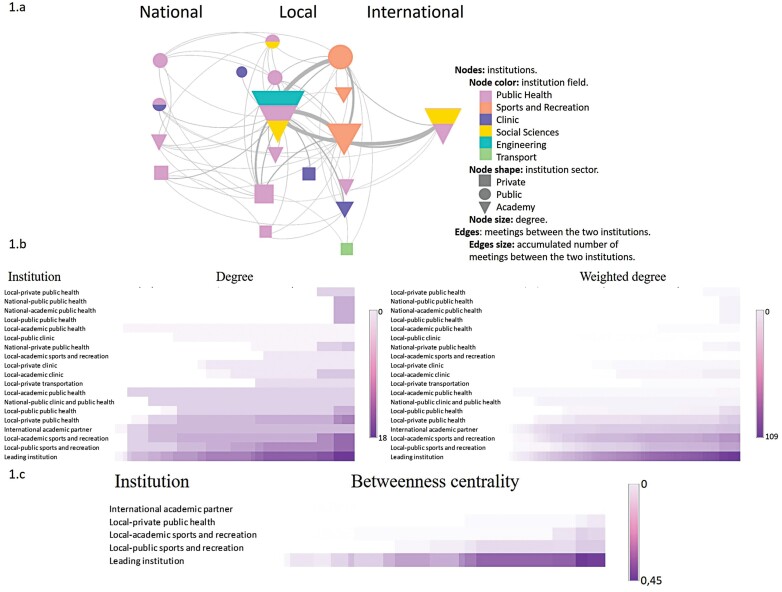
In accordance, findings from the SNA revealed the multisectoral composition of the collaborative network. Of the 19 institutions participating, 36.8% represented the academic, 31.6% the public and 31.6% the private sectors. The three main governmental or disciplinary fields of the stakeholders who most often participated in the network included public health (52.5%), clinical (17%) and sports and recreation (13%). The network started in October 2017 with a single edge (connection) between the two leading academic institutions: Stanford University (international) and Universidad de los Andes (local), and by March 2020, ended with 60 edges connecting the 19 institutions (Figure 1a, Online resource 3). Regarding the number of connections among institutions, the node degree ranged between 0 and 18, and the average degree was 6.31. This suggests that the institutional disconnection initially identified by the stakeholders was reduced with the collaborative network. Figure 1a shows the final iteration of the network and illustrates stakeholders’ main attributes (level, sector, governmental/disciplinary field).
Fig. 1:
My Body network. (a) My Body’s aggregated collaborative network on the final date. Nodes: institutions. Edges: meetings attended by two institutions. Edge size: weight according to the accumulated number of meetings between two institutions over time. Node color: governmental or disciplinary field. Node shape: institution sector. Node size: degree. Nodes sorted by their decision-making level. (b) Degree and weighted degree of the stakeholders engaged in My Body’s collaborative network. Axis X: institutions. Axis Y: time. Color: degree and weighted degree. Degree: number of institutions with which each institution met. Weighted degree: accumulated number of meetings. (c) Betweenness centrality in institutions with a value greater than zero: influential stakeholders intermediating the information flows through My Body’s collaborative network.
Over time, the institutions that participated in more meetings were the two academic leading institutions and one public, one private and third academic institution, all working at the local level in the public health and sports/recreation fields. These five institutions had the highest degree (i.e. had the most meetings with a greater number of institutions) and weighted degree (i.e. had the most accumulated number of meetings) (Figure 1b). Importantly, they all represent diverse disciplinary fields covering public health, sports and recreation, social sciences and engineering.
Additionally, the network’s changes over time (Figure 1a) indicated that institutions engaged differently in the collaborative work across the various stages of the project. The five central institutions began to participate in meetings within 6 months after the first meeting (2017). In the second and third years (2018 and 2019), public health and clinical institutions joined the network, with the second semester of that year—the implementation stage—having the most meetings, and respectively, the highest increase in the weighted degree (i.e. accumulated number of meetings). In the last year (2020), the meetings with the public sector were more frequent.
Finally, the SNA showed that the leading institution consistently played a central role in the network, having the highest degree linking stakeholders from different levels. This is consistent with the information identified by stakeholders during the interviews. However, if we were to remove the leading institution from the network, 88.8% of the stakeholders would remain connected (16 of 18 stakeholders without the leading institution) due to the collaborative work. In other words, the leading institution connected the network, but the collaborative work connected the other institutions to one another as well, establishing local clusters that could have future collaborations in absence of the leading institution.
Challenges
Stakeholders perceived two aspects that were challenging with respect to co-creation: (i) the limited participation of physicians and (ii) administrative barriers within clinical settings for reaching BCS. Both might have been related to patient safety concerns regarding the delivery of a PA intervention within the clinical care setting. Stakeholders acknowledged that there is a long way to go to transform perceived risks that some healthcare professionals have toward PA in cancer patients and, therefore, integrate exercise prescription and practice into the clinical care of BCS.
Key resources and skills
Stakeholders identified as enablers of the multisectoral co-creation process: (i) communication; (ii) cooperation and (iii) the multidisciplinary approach of My Body study.
Communication
Stakeholders reported that communication was of critical importance to facilitate the collaboration, underscoring the role of the project manager in ensuring that each stakeholder’s interests were incorporated. The main communication channel was e-mail. The project manager from the lead institution reported periodically via e-mail on each completed milestone and challenge of the study inviting stakeholders’ reaction and comments. This fluid communication allowed identifying the best possible contributions from each stakeholder considering expertise, available resources and experience. This led to definition of roles and cooperation on tasks related to program adoption, implementation and dissemination. The ongoing communication was also useful for acknowledging how each stakeholder cooperated in the network.
The betweenness centrality results obtained from the SNA (Figure 1c) indicated that the three institutions that were more influential for communicating information through the network were the leading institution and the local public and academic institutions working in the sports and recreation field.
Cooperation
Committed to the missions of reaching underserved populations and building capacity for PA promotion, the network cooperated to overcome the challenges by mobilizing resources within each partnered institution. Specifically, representatives from local-academic institutions working in the public health and sports and recreation fields engaged as advisors mainly during the intervention design and data analysis phases. The local-private institutions working either in the public health or clinical fields facilitated the recruitment of BCS by providing databases to contact them. We signed agreements to access their databases and co-created an open call to BCS. Also, sports physicians from a local-private clinical institution who were willing to promote safe PA in clinical and community settings engaged in the network to screen the physical ability of the BCS participants. The representatives from the local public sports and recreation institution provided their specialized knowledge on community-based logistics and operational resources, including PA instructors and an adequate space in which to deliver the sessions. Moreover, the local public health institution facilitated the nutrition component of the program by delivering workshops to BCS on healthy nutrition and recipe books. The national public health institution contributed to disseminate the intervention results by inviting relevant national stakeholders to the dissemination events.
Multidisciplinary approach
Tailoring the group dance-based PA protocol for BCS was possible due to the workshops that enabled input from several disciplines. The workshops served to review the international evidence-based PA guidance for cancer survivors (Campbell et al., 2019; Schmitz et al., 2019), and build consensus on the components for the My Body intervention (e.g. frequency and length of sessions, progressive moderate PA intensity increases, theory-based activities to foster behavior change). This contributed to BCS safety during the PA program, while also preserving the feasibility of the theory-driven PA intervention in a real-world setting.
Stakeholders perceived that flexibility and receptivity toward academic research were essential to exchange ideas on how to create and implement a comprehensive intervention for BCS and perform in a functional network. The interest in or experience with academic research on the part of some stakeholders, specifically, representatives from the public local institutions working in the sports and recreation and public health fields, was valuable. Despite not having directly used their research skills, they performed as disseminators of the intervention results and of the relevance of research itself. Also, they highlighted the value of the qualitative component of the project, as they perceived it to be innovative to the evidence-based translational purpose, as well as relevant for replication within their institutions.
Outcomes
Among the achieved outcomes of the collaborative work that stakeholders underscored were: (i) the co-creation of the PA protocol tailored to BCS; (ii) the successful implementation of the My Body intervention; (iii) the positive relationships among institutions and (iv) the dissemination of evidence to continue advancing PA promotion through cross-sector collaboration.
Lessons learned from co-creating My Body
Overall, My Body was evaluated as an intervention that enabled cross-sector cooperation. In general, stakeholders underscored three lessons learned through the experience: (i) Cross-sector collaboration may open windows of opportunity to prioritize topics and allocate resources accordingly; (ii) to continue advancing multisectoral communication, it is necessary to maintain open communication channels and (iii) it is necessary to continue to develop strategies for disseminating results to make visible the valuable outcomes that can come from such cross-sector collaborations.
Engaging in the network was perceived by stakeholders as a window of opportunity to (i) position PA and cancer care as a continuum beyond treatment and as relevant topics within their institutions, (ii) advocate for comprehensive multidisciplinary work approaches and (iii) use research to improve decision-making in public health. Likewise, the political context is by itself a window of opportunity to advance cross-sector health-promoting interventions with gender and community-based foci. This can be done through enacting the Comprehensive Health Care Policy and Routes (PAIS and RIAS, for its Spanish acronym (Ministerio de Salud y Protección Social de Colombia, 2018).
From the interviewees’ perspectives, the best way to nurture the cross-sector network is maintaining the communication channels that were built within My Body. The stakeholders proposed to create a cross-sector advisory board to follow up and advise on PA promotion, integrating both scientific and real-world perspectives. According to the stakeholders, through establishing dialogues with different sectors, the leading institution enabled policymakers’ networking, something that was not common in this policy setting. The facilitated workshops allowed them to listen to different initiatives that were being implemented in the institutions, which contributed to mending the existing multisectoral disconnections to advance joint interventions. They mentioned the positive role of the My Body project manager, an anthropologist, who was able to employ interdisciplinary theoretical and methodological frameworks that helped in the elicitation of cross-sector dialogues.
Interviewees also remarked on the relevance of continuing the dissemination of My Body results to (i) acknowledge institutional synergies and outcomes, (ii) incentivize further collaborative research and practice efforts, (iii) reach healthcare service providers and insurers at the regional level and (iv) link more institutions with the collaborative network, including the Ministries of Sports, Transport, Education, and the Pan American Health Organization.
The network’s changes over time captured through the SNA (Figure 1a) showed the increased engagement by public institutions during the dissemination stage. It is important as a reflection of the increasing opportunities to scale up the results and encouraging the replication of this type of PA intervention in other locales. In fact, in August 2020 the representative from Bogotá’s public health authority orchestrated a co-created webinar to disseminate My Body results. He underscored the potential of the collaborative network to advance research and policy evaluation to a broad audience of policymakers from the local and national levels. Additionally, the Ministry of Health launched on October 2021 the first co-created product of the cross-sector PA advisory board that emerged after My Body program (Ministerio de Salud de Colombia, 2021). Moreover, the representatives from the public sector highlighted the opportunity to participate in a broader, international research network that can help to leverage PA promotion programs in Latin American contexts by disseminating promising pilots.
Finally, the BCS who participated in My Body were successful in filing a right to petition to the Bogotá mayor’s office to maintain the PA program. This reflected the acceptability and potential scalability of My Body. The stakeholders recommended that the intervention be tailored through virtual technologies in consideration of the COVID-19 context. In fact, since the beginning of the COVID-19 lock-down, the public local sports institution has offered PA sessions through Facebook live streaming platforms. Regarding recommendations for future projects, interviewees suggested expanding the number of participating BCS to the national level and for patients with other types of cancers. One stakeholder suggested implementing a similar PA program at incarceration settings.
DISCUSSION
My Body is the first study to co-create a theory-driven community-based PA program for BCS in Colombia through engaging cross-sector stakeholders and capitalizing on existing local resources. Using a mixed-methods approach, we documented the networking and co-creation process to implement the PA program in Bogotá’s context. Findings from the interviews and the SNA showed the cross-sectoral nature of the My Body network and revealed increased communication as the key resource to advance collaborative work. The engagement was facilitated by the stakeholders’ shared goals, normative frameworks and the political context. The main outcomes were the successful co-creation and uptake of the PA program for BCS, and the relationships among stakeholders, which addressed institutional disconnection related to this area. Implementing the SNA allowed us to track the network evolution and visualize the complexity of the cross-sector system, which through the co-creation of the My Body program improved synergies between research, policy and practice.
Regarding enablers of the cross-sector collaboration, our findings are consistent with previous studies that have evaluated collaborative research experiences among PA programs in LMIC (Paez et al., 2015), PA programs targeted to vulnerable prioritized populations in HIC (16,22) and PA programs for BCS in HIC (Basen-Engquist et al., 2017). My Body followed the recommendations presented in the most recent studies exploring PA promotion for BCS (Piacentine et al., 2018; McNeely et al., 2019) and other public health interventions (Pinto and Ciccolo, 2011; McEwan et al., 2020) that proposed to include stakeholders from the beginning and identify common goals to ensure better results for program implementation. My Body’s participatory approach was evaluated by stakeholders as relevant. In addition, as endorsed in other studies (Pryke, 2005; Frahsa et al., 2014), the project manager played the mediator and leadership role, which was critical for enabling communication flow in the network. Consistent with international recommendations (Rositch et al., 2020), the employed dissemination strategies strengthened the collaborative network. Stakeholders expressed that this made them feel an active part of the process and opened windows of opportunity for maintaining the network and PA program.
Our findings regarding the challenges are consistent with previous studies conducted in LMIC to evaluate community-based PA programs (Frahsa et al., 2014; Paez et al., 2015; Grimmett et al., 2019), studies conducted in HIC evaluating PA programs targeted to low-income populations (Bilodeau and Potvin, 2018; Hope Corbin et al., 2018), and PA interventions for BCS in HIC (Caperchione et al., 2016; Glasgow et al., 2019; Pullen et al., 2019). Those studies, as well as My Body, identified institutional isolation, inadequate public infrastructure and lack of communication channels between different public institutions working on similar projects or topics.
The My Body program adds to the existing literature by underscoring facilitators that had not been reported in other studies. First, prior positive research experiences on the part of some stakeholders were fundamental to activate cooperation in the implementation of My Body. This study also allowed stakeholders to comply with their institutional guidelines and goals while participating. The establishment of collaborative relationships was evaluated as efficient because each actor could share power in the network—as suggested by Bilodeau and Potvin (Bilodeau and Potvin, 2018)—through sharing their capabilities and knowledge. Finally, belonging to a multidisciplinary network that could generate impact at the local, national and transnational levels was a facilitator for sustaining the commitment during project implementation.
Social network research in the health literature has focused typically on academic networks by assessing dynamics of interdisciplinary collaboration among scholars who work on interventions to improve population health (e.g. co-authorship, scientific productivity, meetings) (Luo et al., 2014; Luke et al., 2015). Some SNA has been used to evaluate collaborative research in public health by analyzing the cooperation structure and central participants, and identifying gaps (Kothari et al., 2014). Regarding breast cancer or cancer in general, a small literature has noted SNA’s potential for capturing the relationships surrounding cancer patients or survivors (Jones et al., 2018) and the relevance of fostering adequate social support among BCS (Michael et al., 2002). Our study findings underscore SNA as a powerful tool to track the composition and evolution of cross-sector partnerships and stakeholder perceptions, including both quantitative and qualitative methods.
This study has limitations. Although we found successful engagement of multisectoral stakeholders in a community-based program to promote PA among BCS in a LMIC, the findings represent the local context in Bogotá and may not fully generalize to other contexts. For future projects, the co-creation process could include other relevant stakeholders, such as private healthcare providers that did not engage in our network, given that the study was not implemented within clinical settings. It could be key approaching more skeptical stakeholders to join the collaborative network in future opportunities. Similarly, future studies should aim to include larger and more diverse samples.
This study has some policy implications for PA interventions aimed at populations with chronic diseases, specifically for BCS in LMIC, Latin America and Colombia. First, research activities can be useful to boost networking among cross-sector stakeholders. Second, My Body showed that cross-sector and multidisciplinary work enables the creation of context-specific health-promoting programs that can be feasible and culturally appropriate. Third, our study results showed that it is essential to demystify the risk perceptions that exist around PA in cancer patients as well as stakeholders, and help them to adequately weigh risks and benefits. The healthcare services providers should train health professionals on the benefits of regular PA so they can help BCS choose safe and enjoyable PA. Fourth, it is important that the national healthcare system applies a comprehensive approach in the cancer continuum of care, for instance, by implementing a monitoring system to track BCS upon finalizing treatment. Finally, strategic dissemination of My Body outcomes can encourage institutional practices to optimize the use of cross-sector resources and apply the policy guidelines to promote PA among BCS. The networking strategies used in My Body could be replicated in other low- to middle-income settings to benefit populations through cross-sector community-based programs.
Supplementary Material
Acknowledgments
We are grateful to the stakeholders for their engagement in this research. We are deeply indebted to Oscar Rubiano, Luis Fernando Alarcón, Adriana Garzón, Catalina Abaúnza, Sonia Arias and Patricia Vásquez, for their generous engagement and contributions. We are grateful to Paula Guevara, Carlos M. Mejía-Arbeláez and Catalina Trillos for their assistance with study procedures.
Contributor Information
María Alejandra Rubio, Department of Public Health, School of Medicine, Universidad de los Andes, Carrera 1 #18ª-12, Bogotá, Colombia.
Daniela Mosquera, Department of Public Health, School of Medicine, Universidad de los Andes, Carrera 1 #18ª-12, Bogotá, Colombia.
Martha Blanco, Department of Industrial Engineering, School of Engineering, Universidad de los Andes, Carrera 1 #18ª-12, Bogotá, Colombia.
Felipe Montes, Department of Industrial Engineering, School of Engineering, Universidad de los Andes, Carrera 1 #18ª-12, Bogotá, Colombia.
Carolyn Finck, Department of Psychology, Universidad de los Andes, Carrera 1 #18ª-12, Bogotá, Colombia.
Martin Duval, Department of Public Health, School of Medicine, Universidad de los Andes, Carrera 1 #18ª-12, Bogotá, Colombia.
Catalina Trillos, Department of Public Health, School of Medicine, Universidad de los Andes, Carrera 1 #18ª-12, Bogotá, Colombia.
Ana María Jaramillo, Department of Industrial Engineering, School of Engineering, Universidad de los Andes, Carrera 1 #18ª-12, Bogotá, Colombia.
Lisa G Rosas, Department of Epidemiology and Population Health, Stanford University School Medicine, Stanford, CA 94305, USA; Division of Primary Care and Population Health, Department of Medicine, Stanford University School of Medicine, Stanford, CA 94305, USA.
Abby C King, Department of Epidemiology and Population Health, Stanford University School Medicine, Stanford, CA 94305, USA; Stanford Prevention Research Center, Department of Medicine, Stanford University School of Medicine, Stanford, CA 94305, USA.
Olga L Sarmiento, Department of Public Health, School of Medicine, Universidad de los Andes, Carrera 1 #18ª-12, Bogotá, Colombia.
Funding
This work was supported by the National Institutes of Health (Award 5P20CA217199) and CRDF Global (Agreements OISE-19-66198-1). The founding sources did not have involvement in the study design, collection, analysis, interpretation of data, writing of the article or submission.
Authors’ Contribution
María Alejandra Rubio: conceptualization, methodology, formal analysis, writing—original draft, project administration. Daniela Mosquera: methodology, formal analysis, writing—original draft. Martha Blanco: methodology, formal analysis, writing—original draft. Felipe Montes: methodology, validation, data curation. Carolyn Finck: validation, writing—review and editing, funding acquisition. Martin Duval: formal analysis. Catalina Trillos: formal analysis. Ana María Jaramillo: methodology, visualization, writing—review and editing. Lisa G. Rosas: methodology, writing—review and editing, funding acquisition. Abby C. King: writing—review and editing, supervision, funding acquisition. Olga L. Sarmiento: conceptualization, methodology, writing review and editing, supervision, funding acquisition.
Ethical Approval
The study was approved by the Ethics Committee from the Universidad de los Andes in Bogotá, Colombia (Minutes no. 964 of 2018).
Conflict of Interest
The authors declare that they have no conflict of interest.
REFERENCES
- Allemani, C., Matsuda, T., Di Carlo, V., Harewood, R., Matz, M., Nikšić, M.et al. (2018) Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet, 391, 1023–1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basen-Engquist, K., Alfano, C. M., Maitin-Shepard, M., Thomson, C. A., Schmitz, K. H., Pinto, B. M.et al. (2017) Agenda for translating physical activity, nutrition, and weight management interventions for cancer survivors into clinical and community practice. Obesity, 25, S9–S22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Battaglini, C. L. (2014) Twenty-five years of research on the effects of exercise training in breast cancer survivors: a systematic review of the literature. World Journal of Clinical Oncology, 5, 177–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bilodeau, A. and Potvin, L. (2018) Unpacking complexity in public health interventions with the Actor-Network Theory. Health Promotion International, 33, 173–181. doi: 10.1093/heapro/daw062 [DOI] [PubMed] [Google Scholar]
- Campbell, K. L., Winters-Stone, K. M., Patel, A. V., Gerber, L. H., Matthews, C. E., May, A. M.et al. (2019) An executive summary of reports from an international multidisciplinary roundtable on exercise and cancer: evidence, guidelines, and implementation. Rehabilitation Oncology, 37, 144–152. doi: 10.1097/01.REO.0000000000000186 [DOI] [Google Scholar]
- Caperchione, C. M., Sabiston, C. M., Clark, M. I., Bottorff, J. L., Toxopeus, R., Campbell, K. L.et al. (2016) Innovative approach for increasing physical activity among breast cancer survivors: protocol for Project MOVE, a quasi-experimental study. BMJ Open, 6, e012533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caperchione, C. M., Sabiston, C. M., Stolp, S., Bottorff, J. L., Campbell, K. L., Eves, N. D.et al. (2019) A preliminary trial examining a “real world” approach for increasing physical activity among breast cancer survivors: findings from project MOVE. BMC Cancer, 19, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catherine, P., Sue, Z. and Nicholas, M. (2000) Qualitative research in health care: analysing qualitative data. BMJ, 320, 114–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper, J., Murphy, J., Woods, C., Van Nassau, F., McGrath, A., Callaghan, D.et al. (2021) Barriers and facilitators to implementing community-based physical activity interventions: a qualitative systematic review. The International Journal of Behavioral Nutrition and Physical Activity, 18, 118. doi: 10.1186/s12966-021-01177-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Covington, K. R., Hidde, M. C., Pergolotti, M. and Leach, H. J. (2019) Community-based exercise programs for cancer survivors: a scoping review of practice-based evidence. Supportive Care in Cancer, 27, 4435–4450. [DOI] [PubMed] [Google Scholar]
- de Vries, E., Buitrago, G., Quitian, H., Wiesner, C. and Castillo, J. S. (2018) Access to cancer care in Colombia, a middle-income country with universal health coverage. Journal of Cancer Policy, 15, Part B, 104–112. doi: 10.1016/j.jcpo.2018.01.003 [DOI] [Google Scholar]
- Díaz del Castillo, A., González, S. A., Ríos, A. P., Páez, D. C., Torres, A., Díaz, M. P.et al. (2017) Start small, dream big: experiences of physical activity in public spaces in Colombia. Preventive Medicine, 103, S41–S50. [DOI] [PubMed] [Google Scholar]
- Frahsa, A., Rütten, A., Roeger, U., Abu-Omar, K. and Schow, D. (2014) Enabling the powerful? Participatory action research with local policymakers and professionals for physical activity promotion with women in difficult life situations. Health Promotion International, 29, 171–184. [DOI] [PubMed] [Google Scholar]
- Franco-Rocha, O. Y., Carillo-Gonzalez, G. M., Garcia, A. and Henneghan, A. (2021) Cancer survivorship care in Colombia: review and implications for health policy. Hispanic Health Care International, 20, 66–74. doi: 10.1177/15404153211001578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaffney, L. K., Lozano, O. D., Almanza, A., Ruiz, N., Mantero, A. and Stoutenberg, M. (2019) The implementation of a National Physical Activity Intervention in Colombia. Journal of Physical Activity and Health, 16, 430–436. doi: 10.1123/jpah.2018-0183 [DOI] [PubMed] [Google Scholar]
- Glasgow, R. E., Harden, S. M., Gaglio, B., Rabin, B., Smith, M. L., Porter, G. C.et al. (2019) RE-AIM planning and evaluation framework: adapting to new science and practice with a 20-year review. Frontiers in Public Health, 7, 1–9. doi: 10.3389/fpubh.2019.00064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimmett, C., Corbett, T., Brunet, J., Shepherd, J., Pinto, B. M., May, C. R.et al. (2019) Systematic review and meta-analysis of maintenance of physical activity behaviour change in cancer survivors. International Journal of Behavioral Nutrition and Physical Activity, 16, 1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haines, V. A., Godley, J. and Hawe, P. (2011) Understanding interdisciplinary collaborations as social networks. American Journal of Community Psychology, 47, 1–11. doi: 10.1007/s10464-010-9374-1 [DOI] [PubMed] [Google Scholar]
- Hämäläinen, R. M., Aro, A. R., Lau, C. J., Rus, D., Cori, L. and Syed, A. M. (2016) Cross-sector cooperation in health-enhancing physical activity policymaking: more potential than achievements? Health Research Policy and Systems, 14, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hope Corbin, J., Jones, J. and Barry, M. M. (2018) What makes intersectoral partnerships for health promotion work? A review of the international literature. Health Promotion International, 33, 4–26. doi: 10.1093/heapro/daw061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Society for Physical Activity and Health (ISPAH). (2020) Las Ocho Inversiones de la ISPAH para Mejorar la Actividad Física.www.ISPAH.org/Resources (last accessed 28 June 2022).
- Jankowski, C. M., Ory, M. G., Friedman, D. B., Dwyer, A., Birken, S. A. and Risendal, B. (2014) Searching for maintenance in exercise interventions for cancer survivors. Journal of Cancer Survivorship, 8, 697–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaramillo, A. M., Montes, F., Sarmiento, O. L., Ríos, A. P., Rosas, L. G., Hunter, R. F.et al. (2020) Social cohesion emerging from a community-based physical activity program: a temporal network analysis. Network Science, 9, 35–48. doi: 10.1017/nws.2020.31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jasny, L., Sayles, J., Hamilton, M., Roldan Gomez, L., Jacobs, D., Prell, C.et al. (2021) Participant engagement in environmentally focused social network research. Social Networks, 66, 125–138. [Google Scholar]
- Johnson, C. M., Molina, Y., Blas, M., Erickson, M., Bayer, A., Gutierrez, M. C.et al. (2018) “The disease is mine, the body is mine, I decide”: individual, interpersonal, and institutional barriers and facilitators among survivors of women’s cancers in Andean countries. Health Care for Women International, 39, 522–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones, E. C., Storksdieck, M. and Rangel, M. L. (2018) How social networks may influence cancer patients’ situated identity and illness-related behaviors. Frontiers in Public Health, 6. doi: 10.3389/fpubh.2018.00240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karageorghis, C. I., Jones, L., Priest, D. L., Akers, R. I., Clarke, A., Perry, J. M.et al. (2011) Revisiting the relationship between exercise heart rate and music tempo preference. Research Quarterly for Exercise and Sport, 82, 274–284. [DOI] [PubMed] [Google Scholar]
- Kothari, A., Hamel, N., MacDonald, J. A., Meyer, M., Cohen, B. and Bonnenfant, D. (2014) Exploring community collaborations: social network analysis as a reflective tool for public health. Systemic Practice and Action Research, 27, 123–137. [Google Scholar]
- Laird, Y., Manner, J., Baldwin, L., Hunter, R., McAteer, J., Rodgers, S.et al. (2020) Stakeholders’ experiences of the public health research process: time to change the system? Health Research Policy and Systems, 18, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leask, C., Sandlund, M., Skelton, D., Altenburg, T., Cardon, G., Chin A Paw, M.et al. (2019) Principles and recommendations for the application and reporting of participatory methodologies in the development and evaluation of public health interventions. Research Involvement and Engagement, 5, 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez-Class, M., Gomez-Duarte, J., Graves, K. and Ashing-Giwa, K. T. (2012) A contextual approach to understanding breast cancer survivorship among Latinas. Psycho-Oncology, 21, 115–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luke, D. A., Carothers, B. J., Dhand, A., Bell, R. A., Moreland-Russell, S., Sarli, C. C.et al. (2015) Breaking down silos: mapping growth of cross-disciplinary collaboration in a translational science initiative. Clinical and Translational Science, 8, 143–149. doi: 10.1111/cts.12248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo, J., Pelfrey, C. and Zhang, G.-Q. (2014) Visualizing and evaluating the growth of multi-institutional collaboration based on research network analysis. AMIA Joint Summits on Translational Science Proceedings, 2014, 60–66. [PMC free article] [PubMed] [Google Scholar]
- McEwan, D., Rhodes, R. E. and Beauchamp, M. R. (2020) What happens when the party is over? Sustaining physical activity behaviors after intervention cessation. Behavioral Medicine, 48, 1–9. doi: 10.1080/08964289.2020.1750335 [DOI] [PubMed] [Google Scholar]
- McNeely, M. L., Sellar, C., Williamson, T., Shea-Budgell, M., Joy, A. A., Lau, H. Y.et al. (2019) Community-based exercise for health promotion and secondary cancer prevention in Canada: protocol for a hybrid effectiveness-implementation study. BMJ Open, 9, e029975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meisel, J. D., Sarmiento, O. L., Montes, F., Martinez, E. O., Lemoine, P. D., Valdivia, J. A.et al. (2014) Network analysis of bogotá’s ciclovía recreativa, a self-organized multisectorial community program to promote physical activity in a middle-income country. American Journal of Health Promotion, 28, e127–e136. doi: 10.4278/ajhp.120912-QUAN-443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michael, Y. L., Berkman, L. F., Colditz, G. A., Holmes, M. D. and Kawachi, I. (2002) Social networks and health-related quality of life in breast cancer survivors: a prospective study. Journal of Psychosomatic Research, 52, 285–293. [DOI] [PubMed] [Google Scholar]
- Ministerio de Salud de Colombia. (2021) Directrices para la promoción y consejeria de actividad física y ejercicio por personal de talento humano en salud.https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/VS/PP/ENT/directrices-promocion-consejeria-af-ths.pdf (last accessed 28 June 2022).
- Ministerio de Salud y Protección Social de Colombia. (2013a) Resolución 1841 de 2013 Por la cual se adopta el Plan Decenal de Salud Pública 2012-2021.https://www.suin-juriscol.gov.co/viewDocument.asp?ruta=Resolucion/30031789 (last accessed 28 June 2022).
- Ministerio de Salud y Protección Social de Colombia. (2013b) Resolución 3202 de 2016 Por la cual se adopta el Manual Metodológico para la elaboración e implementación de las Rutas Integrales de Atención en Salud — RIAS. https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/DE/DIJ/resolucion-3202-de-2016.pdf (last accessed 28 June 2022).
- Ministerio de Salud y Protección Social de Colombia. (2016a) Política de Atención Integral en Salud.https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/DE/modelo-pais-2016.pdf. Repositorio Institucional Digital Minsalud; (last accessed 28 June 2022). [Google Scholar]
- Ministerio de Salud y Protección Social de Colombia. (2016b) Resolución 429 de 2016 Por medio de la cual se adopta la Política de Atención Integral en Salud.https://www.minsalud.gov.co/Normatividad_Nuevo/Resoluci%C3%B3n%200429%20de%202016.pdf (last accessed 28 June 2022).
- Ministerio de Salud y Protección Social de Colombia. (2018) Resolución 3280 de 2018 Por medio de la cual se adoptan los lineamientos técnicos y operativos de la Ruta Integral de Atención para la Promoción y Mantenimiento de la Salud.https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/DE/DIJ/resolucion-3280-de-2018.pdf (last accessed 28 June 2022).
- Monaghan, S., Lavelle, J. and Gunnigle, P. (2017) Mapping networks: exploring the utility of social network analysis in management research and practice. Journal of Business Research, 76, 136–144. [Google Scholar]
- Moseholm, E. and Fetters, M. D. (2017) Conceptual models to guide integration during analysis in convergent mixed methods studies. Methodological Innovations, 10, 205979911770311. [Google Scholar]
- Murillo, R., Díaz, S., Perry, F., Poveda, C., Piñeros, M., Sánchez, O.et al. (2016) Increased breast cancer screening and downstaging in Colombian women: a randomized trial of opportunistic breast-screening. International Journal of Cancer, 138, 705–713. doi: 10.1002/ijc.29801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paez, D. C., Reis, R. S., Parra, D. C., Hoehner, C. M., Sarmiento, O. L., Barros, M.et al. (2015) Bridging the gap between research and practice: an assessment of external validity of community-based physical activity programs in Bogotá, Colombia, and Recife, Brazil. Translational Behavioral Medicine, 5, 1–11. doi: 10.1007/s13142-014-0275-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piacentine, L. B., Robinson, K. M., Waltke, L. J., Tjoe, J. A. and Ng, A. V. (2018) Promoting team-based exercise among African American breast cancer survivors. Western Journal of Nursing Research, 40, 1885–1902. [DOI] [PubMed] [Google Scholar]
- Pinto, B. M. and Ciccolo, J. T. (2011) Physical activity motivation and cancer survivorship. Recent Results in Cancer Research, 186, 367–387. [DOI] [PubMed] [Google Scholar]
- Pluye, P. and Hong, Q. N. (2014) Combining the power of stories and the power of numbers: mixed methods research and mixed studies reviews. Annual Review of Public Health, 35, 29–45. [DOI] [PubMed] [Google Scholar]
- Pryke, S. D. (2005) Towards a social network theory of project governance. Construction Management and Economics, 23, 927–939. [Google Scholar]
- Pudkasam, S., Polman, R., Pitcher, M., Fisher, M., Chinlumprasert, N., Stojanovska, L.et al. (2018) Physical activity and breast cancer survivors: importance of adherence, motivational interviewing and psychological health. Maturitas, 116, 66–72. [DOI] [PubMed] [Google Scholar]
- Pullen, T., Bottorff, J. L., Sabiston, C. M., Campbell, K. L., Eves, N. D., Ellard, S. L.et al. (2019) Utilizing RE-AIM to examine the translational potential of Project MOVE, a novel intervention for increasing physical activity levels in breast cancer survivors. Translational Behavioral Medicine, 9, 646–655. [DOI] [PubMed] [Google Scholar]
- 2018 Physical Activity Guidelines Advisory Committee. (2018). 2018 Physical Activity Guidelines Advisory Committee Scientific Report. U.S. Department of Health and Human Services, Washington, DC. doi: 10.1111/j.1753-4887.2008.00136.x. [DOI] [Google Scholar]
- Rositch, A. F., Unger-Saldaña, K., DeBoer, R. J., Ng’ang’a, A. and Weiner, B. J. (2020) The role of dissemination and implementation science in global breast cancer control programs: frameworks, methods, and examples. Cancer, 126(S10), 2394–2404. [DOI] [PubMed] [Google Scholar]
- Rubio, M. A., Guevara-Aladino, P., Urbano, M., Cabas, S., Mejia-Arbelaez, C., Rodriguez Espinosa, P.et al. (2022) Innovative participatory evaluation methodologies to assess and sustain multilevel impacts of two community-based physical activity programs for women in Colombia. BMC Public Health, 22, 771. doi: 10.1186/s12889-022-13180-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubio, M. A., Triana, C., King, A. C., Rosas, L. G., Banchoff, A. W., Rubiano, O.et al. (2020) Engaging citizen scientists to build healthy park environments in Colombia. Health Promotion International, 35, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmitz, K. H., Campbell, A. M., Stuiver, M. M., Pinto, B. M., Schwartz, A. L., Morris, G. S.et al. (2019) Exercise is medicine in oncology: engaging clinicians to help patients move through cancer. CA: A Cancer Journal for Clinicians, 69, 468–484. doi: 10.3322/caac.21579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spector, D., Battaglini, C., Alsobrooks, A., Owen, J. and Groff, D. (2012) Do breast cancer survivors increase their physical activity and enhance their health-related quality of life after attending community-based wellness workshops? Journal of Cancer Education, 27, 353–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torres, A., Díaz, M. P., Hayat, M. J., Lyn, R., Pratt, M., Salvo, D.et al. (2016) Assessing the effect of physical activity classes in public spaces on leisure-time physical activity: “Al Ritmo de las Comunidades” A natural experiment in Bogota, Colombia. Preventive Medicine, 103S, S51–S58. doi: 10.1016/j.ypmed.2016.11.005 [DOI] [PubMed] [Google Scholar]
- Valente, T. W. (2012) Network interventions. Science, 336, 49–53. [DOI] [PubMed] [Google Scholar]
- Yamashita, S., Iwai, K., Akimoto, T., Sugawara, J. and Kono, I. (2006). Effects of music during exercise on RPE, heart rate and the autonomic nervous system. The Journal of Sports Medicine and Physical Fitness, 46, 425–430. [PubMed] [Google Scholar]
- Zhu, G., Zhang, X., Wang, Y., Xiong, H., Zhao, Y. and Sun, F. (2016) Effects of exercise intervention in breast cancer survivors: a meta-analysis of 33 randomized controlled trails. OncoTargets and Therapy, 2016, 2153–2168. doi: 10.2147/OTT.S97864 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.