Abstract
BACKGROUND
There are approximately 1 million adults in the United States with multiple sclerosis (MS). Persons with MS are interested in diet as a second-line therapy for improving MS symptoms and disease progression. Examination of desired resources regarding diet among persons with MS is necessary for supporting behavior change.
METHODS
Twenty-five adults with MS completed 1-on-1, online semistructured interviews. An inductive, 6-phase, semantic thematic analysis was applied to identify themes associated with participant preferences for dietary behavior change.
RESULTS
The research team crafted 4 key themes from the data that encompassed participants’ desired resources for dietary behavior change. Theme 1, MS-specific evidence, involved the need for clear information about the impact of diet regimens or specific foods on MS. Theme 2, dietary guidelines, was related to guidelines provided by a reliable source such as a registered dietitian. Theme 3, behavioral supports, underscored the need for support for behavior change, including accountability, self-monitoring, motivation, habituation, and incremental changes. Theme 4, diet resources, highlighted tangible resources for supporting dietary change, including recipes, food lists, meal services, or games.
CONCLUSIONS
This study provides a foundation for guiding dietary interventions for persons with MS that incorporates their needs and preferences and could improve their overall health. Such dietary change can be facilitated by theory-based behavioral interventions that incorporate behavior change techniques such as self-monitoring and goal setting for supporting behavior change.
Keywords: qualitative, multiple sclerosis, diet, wellness, behavior change
There are an estimated 1 million adults in the United States and 2.8 million adults globally with multiple sclerosis (MS),1,2 a disease of the central nervous system wherein immune-mediated inflammation causes demyelination and transection of axons and results in hallmark debilitating outcomes such as mobility impairment, cognitive dysfunction, and fatigue.3,4 The pro-inflammatory nature of MS has prompted interest in lifestyle approaches that may be anti-inflammatory as second-line therapies for managing disease manifestations, in conjunction with first-line pharmaceutical interventions such as disease-modifying therapies.5 A recent study indicated that persons with MS are interested in wellness approaches, particularly regarding diet, to manage the disease, and diet is the most frequently searched wellness strategy on the internet by persons with MS.6
The National Multiple Sclerosis Society (NMSS) recently convened a Wellness Research Working Group that reviewed the literature on diet in MS and provided guidance for further research.7 The NMSS Wellness Research Working Group concluded that the study of specific dietary regimens and how they affect MS symptoms and disease progression is in its infancy.7 Research regarding diet and MS has largely focused on inflammation, given the pathogenesis of MS, and examined the associations among saturated fatty acids, leptin, cytokines, and, more recently, dysbiosis of gut microbiota with MS manifestations.8 This evidence has generated increased research regarding the effects of specific diets, vitamins/minerals, essential fatty acids, and antioxidant supplements in MS.9 One ongoing quandary remains: there is currently no class I evidence from randomized controlled trials of the benefits of any specific diet in MS. The provision of a behavioral knowledge base that focuses on the dietary information needs and preferences of persons with MS is required before implementation of any dietary intervention and for the purposes of enhanced health and wellness and long-term adherence.
The tradition of qualitative research is an important approach to understand diet in MS. Qualitative methods gather first-hand, lived experiences and opinions such that interventions can be designed that more closely meet the needs, wants, and desires of persons with MS.10 A recent study explored perceptions about dietary information among persons newly diagnosed as having MS11 and added further support to the necessity to generate a focused line of research on diet. Study participants requested further research given the perceived incompatibility or lack of general dietary advice considering disease seriousness (their first theme) that can underpin participant-reported engagement in self-experimentation with dietary approaches for managing MS (their third theme).11 This is but 1 example demonstrating that a focus on diet is a key priority for persons with MS6 and that qualitative inquiry is a meaningful approach to capture the needs, wants, desires, opinions, fears, and experiences regarding diet among persons with MS. Previous qualitative research further highlights a current lack of resources for supporting changes in healthy eating behaviors.11–13 An in-depth understanding regarding desired resources for supporting future dietary change from a behavioral perspective would complement adjacent research examining biological changes and specific dietary regimens for improving outcomes among persons with MS.9,14
One primary research question put forth by the NMSS working group was, “What are the optimal ways to promote the adoption and maintenance of specific dietary regimens?”7 Qualitative inquiry is an ideal approach for providing a foundation that addresses this question because it allows a research team to identify barriers to and facilitators of adoption and maintenance of behavior change from the viewpoint of the target population. To that end, the present study adopted qualitative inquiry and examined the desired resources for supporting dietary changes in persons with MS. The overarching goal of this research involved the provision of guidelines for behavioral interventions promoting healthy eating based on the preferences of persons with MS.
METHODS
Design and Assumptions
This study was approved by the University of Alabama at Birmingham institutional review board. An inductive, exploratory qualitative design was used to explore desired dietary resources of persons with MS.15 This study was underpinned by an interpretative paradigm framed by ontological relativism and epistemological subjectivism. As such, we perceived reality as multiple and subjective, depending on each individual participant, and each participant’s “truth” or reality as unique to them but equally valid.16,17 We further perceived that the creation of knowledge was a cooperative effort between ourselves and the participants, and this knowledge creation was influenced by the experiential, historical, political, and cultural background of each individual’s lived experience. All members of the research team have previous experience designing and conducting qualitative studies that examine health behaviors in diverse samples of persons with disabilities, including MS. The first author (S.L.S.) previously conducted a qualitative study of exercise preferences among wheelchair users with MS that led to the development of a behavioral intervention. The second author (E.V.R.) is a leading expert in qualitative methods and disability studies who has led more than a dozen individual qualitative studies regarding physical activity and wellness in samples with MS, spinal cord injury, and other disabilities. The third author (R.W.M.) is a leading expert on wellness in persons with MS who has implemented qualitative methods in research for the past decade.
Participants
Participants were recruited using purposive sampling methods involving convenience and maximum variation strategies. Regarding convenience strategies, we contacted individuals who expressly desired information about future research conducted by the team. To honor this request, we used a maximum variation technique by designing a call-to-research flyer that was purposefully distributed among individuals with a wide range of clinical and demographic characteristics, such as MS type and duration, socioeconomic status, location, and race. The rationale for this approach was to capture as wide a range of opinions and desires for dietary resources as possible. The email invitation was distributed among 40 potential participants, and 26 expressed interest. The inclusion criteria were (1) age 18 years or older, (2) confirmed diagnosis of MS, and (3) willingness to take part in a recorded interview.
Procedure
Participants were emailed instructions for the online interview platform and an information sheet before the interview session that explicitly stated what was being asked. All interviews began with a discussion regarding the information sheet, and verbal informed consent was received before interviews began. Participants were further informed that they could terminate the interviews at any time and sit in a location of choice, thereby aligning with best practices for facilitating comfort and convenience.18
Data were collected through online, semistructured, 1-on-1 interviews via video teleconferencing software (Zoom; Zoom Video Communications Inc) licensed by the University of Alabama at Birmingham. This software was chosen given the higher levels of security afforded with university-sponsored accounts that require the use of waiting rooms and passwords for entering meeting rooms and an individual option for use of a camera. In addition, the software allows users to download recordings directly to a password-protected computer as opposed to the Kaltura Cloud. The research team examined previous literature regarding dietary behaviors in persons with MS and then created and refined an interview guide. Online interviews were chosen for numerous reasons. First, this allowed researchers to interview individuals from a wide geographic range, capturing not only those local to the research laboratory but also individuals from across the United States. This allows for a cultural snapshot of desired resources within this country. Second, online interviews are a preferred method of data collection among persons with MS because they can reduce the fatigue, pain, and stress associated with travel.17 Third, this method ensured the safety of both the researcher and the participant not only regarding travel but also because these interviews were conducted in April and May 2020, during COVID-19 restrictions.19
The semistructured approach was taken to allow participants freedom to discuss experiences and opinions important to them while allowing interviewers/researchers to ensure that areas of interest that spoke to the research questions (ie, desired resources for nutrition) were meaningfully captured.20 The interview began with general introductions (ie, grand tour) wherein researchers inquired about demographic and clinical characteristics. Participants were then asked about personal informational needs for dietary behavior change, for example, “What information do you want to know about nutrition and MS?” We further inquired about resources that participants would need to support changes in diet, for example, “What would help you incorporate nutrition into your management plan for MS?” and “How would you change your diet? What tools or resources?” The other questions asked are provided in APPENDIX S1, which is published in the online version of this article at ijmsc.org. The semistructured design allowed flexibility for participants when providing specific information regarding previous experiences with various diet regimens and future diet preferences and providing rich, in-depth data.
The first and second authors conducted the interviews, and they engaged in critical reflection after each interview was conducted. All the interviews were deidentified before transcription. Audio data were transcribed by a third-party transcription company (Rev.com).
Rigor
To ensure rigor and trustworthiness throughout the research process, we adopted a relativist approach, which stipulates that rather than a universal list of criteria applied to all research, there are nuances in research that must be appreciated and different standards of quality depending on the purpose, methods, and analysis of each approach.21 This approach to rigor aligned with our philosophical underpinnings regarding multiple subjective realities co-constructed between the participants and the researchers and allowed us to choose markers of quality that both aligned with the objectives for the research and ensured the scientific quality of the methods.22 We chose the evaluative markers of substantive contribution, rich rigor, critical friends, and naturalistic generalizations, which we selected from Tracy23 and the ongoing list from Smith and Caddick.24 We ensured substantive contribution by identifying gaps in participants’ knowledge regarding diet information and support among persons with MS. Enhancing knowledge about what persons with MS need and want regarding diet can inform future research and highlight ways to help improve wellness in this group. We sought rich rigor by using an appropriate sample, applying rigorous data collection and analysis methods, and using applicable theoretical constructs to support meaningful, important findings. Related to this, we used critical friends to help problematize conclusions and act as sounding boards to alternative ideas. In the context of this study, the first author led the data analysis effort and created initial codes and themes, which were critiqued by the second and third authors. Furthermore, the first, second, and third authors have complementary expertise in diet, qualitative methods, and MS, respectively, and were able to support each other throughout the process as well as challenge each other’s thinking. Finally, we aspired for naturalistic generalizability whereby the findings of this work may resonate with other readers who experience the same things (ie, persons with MS searching for diet information).25 We did this through rich descriptions and quotations from participants as well as deliberately choosing a sample from across the culturally diverse United States.
Analysis
We conducted an inductive, semantic, thematic analysis to identify themes associated with participant preferences for dietary behavior change. Specifically, the methods were inductive wherein the themes were determined by the data and semantic wherein codes were applied based on the explicit, surface-level data. We followed the 6-phase guidance for thematic analysis outlined by Braun et al.26 Phase 1 involved the first and second authors becoming familiar with the data through conducting interviews and rereading transcripts. During this initial immersion phase, the first author submitted audio for transcription within 24 hours of an interview and read each transcript upon receipt from the transcription service. Both the first and second authors independently open coded all the data using Microsoft Word (Microsoft Corp) during phase 2 and noted resources needed and interest in future dietary behavior change. For phase 3, the first author proposed 4 themes that manifested from coding that were then reviewed by all the authors in phase 4. All discrepancies were addressed through debate and discussion among the research team. Phase 5 involved the final naming of the 4 themes and descriptions and an iterative review to ensure that they aligned with the data. Phase 6 was a comprehensive report and summary, included in the Results and Discussion sections that follow.
RESULTS
Participants and Interviews
Of the 26 individuals who expressed interest, 25 were screened for the inclusion criteria and provided informed consent. Participant characteristics are provided in TABLE 1. The mean (SD) participant age was 56.5 (8.7) years (range, 42–74 years), and most participants were female (n = 23) and self-identified as White (n = 24). Participants had a mean (SD) disease duration of 16.4 (8.6) years (range, 3–38 years). Twelve participants reported a diagnosis of relapsing-remitting MS and 12 participants reported a diagnosis of progressive MS (5 primary and 7 secondary); 1 participant did not report a clinical course.
TABLE 1.
Participant Demographic and Clinical Characteristics
| Participant No. | Sex | Age, y | Marital status | Race | Employment status | Time since MS diagnosis, y | MS type |
|---|---|---|---|---|---|---|---|
| 1 | M | 58 | Married | White | Retired | 13 | PPMS |
| 2 | F | 64 | Married | White | Retired | 38 | SPMS |
| 3 | F | 74 | Married | White | Retired | 15 | PPMS |
| 4 | F | 58 | Married | White | Retired | 10 | RRMS |
| 5 | F | 73 | Married | White | Retired | 20 | SPMS |
| 6 | F | 56 | Married | White | Retired/disability | 25 | RRMS |
| 7 | F | 46 | Single | White | Retired | 6 | RRMS |
| 8 | F | 55 | Married | White | Retired | 14 | RRMS |
| 9 | F | 67 | Partnership | White | Retired | 22 | SPMS |
| 10 | F | 51 | Married | White | Retired | 30 | PPMS |
| 11 | F | 60 | Married | White | Retired/disability | 22 | NR |
| 12 | F | 60 | Married | White | Retired | 12 | RRMS |
| 13 | M | 58 | Married | White | Retired | 18 | PPMS |
| 14 | M | 52 | Divorced | White | Disability | 8 | SPMS |
| 15 | F | 42 | Married | White | Employed part-time | 9 | RRMS |
| 16 | F | 48 | Married | Caribbean | Employed full-time | 3 | PPMS |
| 17 | F | 48 | Partnership | White | Retired/disability | 3 | RRMS |
| 18 | F | 50 | Partnership | White | Retired/disability | 19 | RRMS |
| 19 | F | 61 | Married | White | Employed full-time | 10 | RRMS |
| 20 | F | 63 | Married | White | Retired/disability | 24 | SPMS |
| 21 | F | 50 | Divorced | White | Retired/disability | 11 | RRMS |
| 22 | F | 53 | Married | White | Retired/disability | 26 | RRMS |
| 23 | F | 49 | Partnership | African American | Employed full-time | 13 | RRMS |
| 24 | F | 71 | Married | White | Retired | 14 | SPMS |
| 25 | F | 46 | Married | White | Retired/disability | 24 | SPMS |
MS, multiple sclerosis; PPMS, primary progressive MS; RRMS, relapsing-remitting MS; SPMS, secondary progressive MS.
The first author conducted 15 interviews and the second author conducted 10 interviews. Overall, 1328 total minutes of audio data were collected, with a mean (SD) interview length of 53 (9) minutes (range, 40–79 minutes).
Themes
From the data, 4 key themes were crafted that encompassed participants’ overall desired resources for dietary behavior change: (1) MS-specific evidence, (2) dietary guidelines, (3) behavioral supports, and (4) diet resources. FIGURE 1 provides a detailed representation of the 4 key themes and codes.
FIGURE 1.
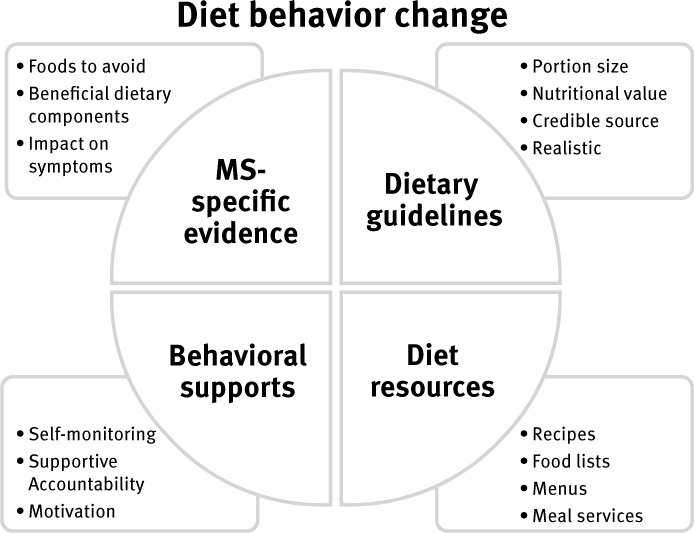
Study Themes Outlining Resources for Dietary Behavior Change
Theme 1: MS-Specific Evidence
Participants reported a desire for clear, MS-specific evidence regarding the impact of diet regimens or specific foods on MS. Participants referenced symptoms that might be linked with MS-specific evidence for diet and food consumption. For example, participant 22 mentioned inflammation and fatigue with diet: “I wanted to know what increases inflammation and what reduces it and what keeps my energy up. I saw a study where intermittent fasting, like you fast a day then you eat the next day, is supposed to help with some kind of inflammation. And wanted to pick the doctor’s brain. But yeah, that’s basically it nutrition-wise, what’s going to make me feel like I want to get out of bed and do things and not take 3 naps a day.” Further participants stated that a lack of evidence regarding diet and health undermined the possibilities of engaging in effective dietary behavior change. For example, participant 2 said, “It’s not as big a factor because I haven’t read anything that says ‘You should eat this’ or ‘Don’t eat that.’ But thus far, no one has tied anything dietary to what’s good for you or bad for you in terms of my health.” Participant 4 shared this concern regarding the lack of MS-specific evidence but went further to state a desire and need for published media to disseminate dietary information: “I would just want to, what we’re were talking about earlier, just more specifics on what to eat, what not to eat. Different things that would help us as far as diet and nutrition. Like I said, I’m a sponge, so I love to read, and I love to read helpful...I like to read things that will help me, I like to learn, so anything that would be published would be good.” Of note, however, participant 5 reported experiencing issues regarding conflicting dietary evidence through disseminated information: “Yeah, that’s the problem because one day coffee’s good for you, and the next day coffee’s bad for you. Then they go back, ‘Well it’s good for you.’ There’s too many different opinions about what is good for you and what is bad for you.” Overall, there was a general call among participants for evidence from credible, widely available resources regarding diet and foods specific to managing MS.
Theme 2: Dietary Guidelines
Participants expressed a critical need for dietary guidelines from a reliable source such as a registered dietitian. Participant 11 directly mentioned a desire for guidelines: “I would kind of like to have better guidelines and more things spelled out for what we need to eat or things to avoid.” One of the primary foci of such guidelines was portion sizes. For example, participant 19 stated, “Probably basic information, portion sizes. Sometimes it’s hard for me, I know with my age and my height and my activity level, I probably should be eating about 1100 calories a day. That’s not a lot. What foods should I put that in so that I’ve not gobbled up all my calorie content in breakfast and lunch, stuff like that.” Participant 20 took this 1 step further and proposed a need for guidance regarding protein: “Another question I had is: how much protein am I supposed to eat?” Participants expressed an additional need for guidelines designed by reliable sources. For example, participant 15 said, “I have found people respond best if you, whatever body of authority guidelines, and then they say, “Eat this. Do this.” I find people respond more to that. Or at least I have over the years, right? Yes. So I’d like the National MS Society or whoever university guidelines.” The overarching suggestion from participants was dietary guidelines that would promote healthy eating and were disseminated via credible sources.
Some participants expressed a need for guidelines but were uncertain about whether these were achievable and would be aligned with personal preferences. For example, participant 9 stated, “I’ll just eat the best way I can and still be happy. There’s no way I’m going to eat a plant-based diet. There’s no way I’m going to eat just fruits and vegetables. I’m never going to be a vegan. To say, oh yeah send me a piece of paper that says eat 3 or 4 vegetables a day, I’m not going to do that. I mean, I’ll be right up front with that.” Participant 15 provided further insights regarding the presentation and specificity of guidelines that can address resistance: “Five fruits a day or whatever. Not even servings. Forget that because they don’t get what a serving really is. You should eat 5 fruits a day. You should eat 3 vegetables. Very specific, but none of those words because people just turn off. They’ll tune out.” In addition, guidelines need to be readily available, as expressed by participant 11: “I don’t want to have to do the research looking for things, going to different sites, trying to find something then just finding generic information. I want more specific guidelines.” Overall, participants provided insights to help guide the presentation of dietary guidelines that could be integral for promoting uptake of the desired MS-specific diet, outlined in theme 1.
Theme 3: Behavioral Supports
Participants highlighted behavioral supports as a primary resource that would promote dietary behavior change. Behavioral supports involve constructs and strategies that directly support modification of behavior, including strategies such as motivation, self-monitoring, habituation, incremental changes, and accountability. Motivation was a primary subtheme reported by participants; for example, participant 16 said, “I noticed if you don’t have that hope or desire, you can have all the resources in the world and nothing is going to change.” Participant 8 highlighted that motivation varies among individuals, “Yeah. It’s hard to figure out what motivates, I guess everyone motivates differently.” Therefore, identifying approaches for enhancing motivation may be a primary consideration for understanding adoption and maintenance of dietary behavior change.
Several participants underscored the utility of self-monitoring for dietary behavior change using mobile applications such as MyFitnessPal, which can aid in raising awareness regarding diet composition. Participant 2 specifically referenced experience with self-monitoring: “Well it’s like with MyFitnessPal, diet is what you put into the diary. And nutrition is actually the nutrition button that you can look at and see what you’re getting. And I’ll stop a second here, but going back to MyFitnessPal, it can really open peoples’ eyes. Oh my goodness.” An additional behavioral component of interest among participants was habituation. Participant 1 reflected on experience with dietary behavior change and habituation: “I think it helped to break the habits because that’s the one thing that you’re struggling with. People get habitually...I don’t know. Whatever it is that they’re used to having all the time and they habituate that and so they need to break that habit.”
Participant 4 mentioned a focus on incremental, realistic changes: “If it was an easy change and something that I could incorporate without an awful lot of trouble, yes. If it’s a major change, I doubt that I would do it.” This collectively suggests that self-monitoring and realistic goals that align with individual habits and routines may be primary considerations to support dietary behavior change.
Participants expressed a need for supportive accountability to adopt dietary behavior change. Participant 7 was interested in peer-facilitated supportive accountability: “So you could go onto it, like fitness buddies, people with MS, and then see if you could find a match that you could support each other with as far as fitness goes and healthy eating and encourage it. There’s no such thing for MS, and I would love to see something like that, especially for those of us that live alone.” Participant 22 mentioned an interest in support that was not authoritative: “I mean support would be good. Dictating, I’d be like yeah, bye-bye.” Some participants had the opportunity to meet with a registered dietitian or nutritionist and had positive experiences. For example, participant 24 said, “Prior to moving to [excluded], my primary care physician asked if I wanted to meet with a nutritionist before moving. And so she introduced it to me, to MyFitnessPal, and I found it so easy to use that I did it for a while.” Overall, participants had an interest in various options for accountability facilitated by peers or health care practitioners in a supportive and nonjudgmental manner.
Theme 4: Diet Resources
Participants identified a need for tangible resources for dietary behavior change, including recipes, food lists, menus, food preparation services, meal services, and technology-based knowledge translation. For example, participant 4 provided comprehensive insights that encompassed how these resources would complement each other: “I like to see recipes. Lists of good foods, lists of foods that are not, to stay away from, different meal plans, suggestions, but I like easy, so recipes that might be easier than...I don’t want something that has 15 items in it of food. I’d rather have something that would be easy to prepare, but good for you. Maybe different suggested menus.”
Participant 10 aligned the utility for a small set of recipes and menus for individuals with MS who experience brain fog: “Look, this is what you shouldn’t be eating anymore because it’s a fog mind issue. Let’s find you 2 weeks of meals that work for you, so you have 2 weeks, you’re only cooking 1 meal twice in a month, so you can plan ahead, you can get it done. You know it’s good every time, and that’s what she did for me and that helped so much, so much, because now I have made the meals.” Participant 20 reiterated a need for recipes that included a reasonable number of items and suggested resources be widely available online: “Probably something online that could be printed off or saved or pulled back up that would be quick and easy tips or recipes. But then I looked at 1 recipe that looked really good until I saw it had 16 ingredients.” Therefore, participants were keenly interested in meal preparation resources that ensured variety, but with a reasonable number of ingredients, and that could be feasibly implemented.
Some participants were interested in meal services, such as participant 2: “I’m probably more into you can have someone cooking and pay for the food service. And I’d probably look pretty heavy into that. Somebody or hire a chef or something. Or not, I would do that, but hire a meal person like Jenny Craig.” Participant 23 expressed an interest in prepared meals but noted issues with them aligning with dietary needs: “Well, I tried to do one of the meal planning things, where they would just prepare the meals for you. You just go pick up. I tried to do that. But they did a lot of tomato-based things. So it’s kind of every, pretty much all of their meals, or a lot of their meals were tomato-based. So I couldn’t eat them. I try to limit my pork and beef intake, so it just kind of made it really challenging to do. So I thought that was a waste of my money.”
Importantly, cost is a significant barrier for many individuals with MS, as highlighted by participant 15: “So money is a barrier.” Symptoms can be an additional barrier for food preparation. Participant 17 mentioned issues with vertigo and using knives: “Struggling with my vertigo lately, and so I shouldn’t use knives when I’m struggling with my vertigo.” Collectively, there is a growing industry in prepared meals in the general population that may be a resource leveraged by individuals with MS.
Participants mentioned delivery of resources via the internet, such as recipes. One unique idea was presented by participant 8 regarding gamifying knowledge translation: “And then I just thought of something weird, but people like to play games and maybe there’s some kind of game that could be developed so they could learn about nutrition.” Such innovative approaches for disseminating information can be incorporated into future nutrition programs and resources.
DISCUSSION
To our knowledge, this is the first study using qualitative methods to examine resources and preferences for dietary change in persons with MS. This study was motivated and informed by seminal and guiding papers on the topic as well as a strong interest in diet among persons with MS.6,7 Participants expressed a pressing need for a foundation regarding the impact of diet on MS and guidelines for optimal diet for persons with MS. In addition, desired resources for initiating diet in MS aligned with previous qualitative inquiry, particularly the need for autonomous approaches that allow for individualization and self-experimentation.11 The findings from this study are summarized in FIGURE 1 and provide a roadmap regarding necessary steps for adopting dietary behavior change as a second-line therapy among persons with MS.
The 4 themes identified in this study align with social cognitive theory (SCT) behavior change principles. Indeed, SCT posits that knowledge regarding benefits and health risks is a precursor of health behavior change (ie, theme 1: MS-specific evidence).27 Outcome expectations for health behavior change are critical in persons with MS, and findings from this study highlight a need for evidence regarding the impact of diet on debilitating MS symptoms. Relatedly, participants expressed a need for dietary guidelines for persons with MS (theme 2) that can guide goal setting, self-monitoring, and action planning. There are physical activity guidelines for persons with MS,28 and, therefore, dietary guidelines for persons with MS that are based on evidence regarding the impact of diet on MS may be appropriate. Participants expressed a need for behavioral supports and strategies for dietary behavior change after the establishment of evidence and dietary guidelines. Participants highlighted several components that align with SCT behavior change principles, including motivation, goal setting, self-monitoring, and supportive accountability (theme 3: behavioral supports).27 Tangible resources such as recipes, food lists, menus, food preparation services, and meal services were also identified as tools necessary to support dietary behavior change. Taken together, behavioral supports and diet resources can be skillfully delivered via theory-based behavioral interventions to support dietary change. These theory-based behavioral interventions are distinct from randomized controlled trials testing different dietary recommendations or prescriptions because the underlying challenges associated with dietary behavior change must be addressed using a strong behavioral medicine evidence base.
The internet has been identified as a primary source of information provision among persons with MS, and study participants expressed an interest in internet resources; therefore, this is a ripe opportunity for dissemination of evidence-based internet resources to support dietary behavior change.29 Such resources could be delivered through the NMSS website, which is often one of the first places persons with MS seek information regarding second-line therapies.7,30 In addition, diet resources could be delivered by neurologists or health care providers given recent evidence establishing that neurologists are a preferred source of information among persons with MS.31 However, a recent qualitative study illuminated barriers to dietary behavior change cited by neurologists that included juggling conflicting diet evidence and acknowledging the risks and benefits of diet.31 The authors of that study concluded that neurologists might meet the current needs of patients by promoting the benefits of national dietary guidelines, such as the Dietary Guidelines for Americans in the United States, and being prepared to explain the potential risks of specific diets.31,32 Another recent study highlighted that persons with MS are skeptical about the appropriateness of national dietary guidelines and want specific dietary guidelines for MS, which might lead to resistance or skepticism in discussions with neurologists or other health care providers.13 Therefore, we assert that the use of national dietary guidelines can provide a temporary solution, and this study provides guidance for areas of future research that build on a strong theoretical foundation. Such studies would investigate diet in MS, provide clear guidelines for persons with MS, and create programs that include behavioral supports and resources that support dietary behavior change.
The present study is not without limitations. Online interviews were necessary given COVID-19 restrictions; however, this method reduces the interviewer’s ability to discern nonverbal cues, which can provide rich information. The research team used convenience sampling methods, and this yielded a sample that was diverse in terms of geographic area, sex, and disability status; however, the age range of participants was 42 to 74 years, and further research is warranted among younger adults with MS. In addition, the time since MS diagnosis ranged from 3 to 38 years, and, given a growing interest in behavior change immediately after diagnosis, focal inquiry regarding dietary behavior change preferences is warranted among those recently diagnosed. The current paucity of evidence regarding diet in MS presents a challenge to providing clear recommendations for neurologists and other health care providers based on the results of the present study; however, a leading group of experts in wellness research for persons with MS provided some guidance for the promotion of a healthy diet, such as a focus on consumption of whole foods and attention to food labels.33
We conclude that diet is consistently a second-line therapy of interest among persons with MS that requires further research regarding biological mechanisms in conjunction with the establishment of guidelines and the creation of tangible resources. These resources might be ideally delivered via behavioral interventions that address motivation and implement evidence-based behavior change techniques such as self-monitoring and goal setting. Collectively, the findings from the present study provide a foundation to guide future research in dietary interventions for persons with MS that incorporates their needs and preferences and could potentially improve their overall health and quality of life.
PRACTICE POINTS
» Persons with multiple sclerosis (MS) often inquire about diet as an adjuvant therapy for managing MS and desire clear information regarding the impact of specific regimens or courses of action on disease course.
» Persons with MS desire evidence-based dietary guidelines to support dietary behavior change that can be facilitated through MS clinicians such as registered dietitians.
» Behavioral interventions for supporting dietary change in MS can include behavioral supports and resources such as recipes, menus, and food lists to help support well-being in persons with MS.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank the participants in this study for their time and the insights that made this research possible.
Funding Statement
FUNDING/SUPPORT: This work was supported, in part, by the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health (grant F32HD101214) and the Healthy Aging through LifesTyle (HALT) Research Center, which was supported by the National Multiple Sclerosis Society (grant 000518032).
Footnotes
FINANCIAL DISCLOSURES: The authors declare no conflicts of interest.
DISCLAIMER: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
REFERENCES
- 1.GBD 2016 Neurology Collaborators Global, regional, and national burden of multiple sclerosis 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol . 2019;18(5):459–480. doi: 10.1016/S1474-4422(18)30499-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Walton C, King R, Rechtman L et al. Rising prevalence of multiple sclerosis worldwide: insights from the Atlas of MS. Mult Scler . 2020;26(14):1816–1821. doi: 10.1177/1352458520970841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dendrou CA, Fugger L, Friese MA. Immunopathology of multiple sclerosis. Nat Rev Immunol. 2015;15(9):545–558. doi: 10.1038/nri3871. [DOI] [PubMed] [Google Scholar]
- 4.Kister I, Bacon TE, Chamot E et al. Natural history of multiple sclerosis symptoms. Int J MS Care . 2013;15(3):146–158. doi: 10.7224/1537-2073.2012-053. Published correction appears in Int J MS Care 2014;16(4):170. doi:10.7224/1537-2073.2012-053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moss BP, Rensel MR, Hersh CM. Wellness and the role of comorbidities in multiple sclerosis. Neurotherapeutics . 2017;14(4):999–1017. doi: 10.1007/s13311-017-0563-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dunn M, Bhargava P, Kalb R. Your patients with multiple sclerosis have set wellness as a high priority-and the National Multiple Sclerosis Society is responding. US Neurol . 2015;11(2):80–86. doi: 10.17925/USN.2015.11.02.80. [DOI] [Google Scholar]
- 7.Motl RW, Mowry EM, Ehde DM et al. Wellness and multiple sclerosis: the National MS Society establishes a Wellness Research Working Group and research priorities. Mult Scler . 2018;24(3):262–267. doi: 10.1177/1352458516687404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Esposito S, Bonavita S, Sparaco M, Gallo A, Tedeschi G. The role of diet in multiple sclerosis: a review. Nutr Neurosci . 2018;21(6):377–390. doi: 10.1080/1028415X.2017.1303016. [DOI] [PubMed] [Google Scholar]
- 9.Sand IK. The role of diet in multiple sclerosis: mechanistic connections and current evidence. Curr Nutr Rep . 2018;7(3):150–160. doi: 10.1007/s13668-018-0236-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pathak V, Jena B, Kalra S. Qualitative research. Perspect Clin Res . 2013;4(3):192. doi: 10.4103/2229-3485.115389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Russell RD, Black LJ, Sherriff JL, Begley A. Dietary responses to a multiple sclerosis diagnosis: a qualitative study. Eur J Clin Nutr . 2019;73(4):601–608. doi: 10.1038/s41430-018-0252-5. [DOI] [PubMed] [Google Scholar]
- 12.Plow M, Finlayson M. A qualitative study of nutritional behaviors in adults with multiple sclerosis. J Neurosci Nurs . 2012;44(6):337–350. doi: 10.1097/JNN.0b013e3182682f9b. [DOI] [PubMed] [Google Scholar]
- 13.Russell RD, Black LJ, Begley A. Navigating dietary advice for multiple sclerosis. Health Expect . 2021;24(3):853–862. doi: 10.1111/hex.13226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wahls TL, Chenard CA, Snetselaar LG. Review of two popular eating plans within the multiple sclerosis community: low saturated fat and modified Paleolithic. Nutrients . 2019;11(2):352. doi: 10.3390/nu11020352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thomas DR. A general inductive approach for analyzing qualitative evaluation data. Am J Eval . 2006;27(2):237–246. doi: 10.1177/1098214005283748. [DOI] [Google Scholar]
- 16.Denzin NK, Lincoln YS. The Sage Handbook of Qualitative Research . 5th ed. Sage Publications; 2011. [Google Scholar]
- 17.Sparkes AC, Smith B. Qualitative Research Methods in Sport Exercise and Health From Process to Product . 1st ed. Routledge; 2013. [Google Scholar]
- 18.Sedgwick M, Spiers J. The use of videoconferencing as a medium for the qualitative interview. Int J Qual Methods . 2009;8(1):1–11. doi: 10.1177/160940690900800101. [DOI] [Google Scholar]
- 19.Synnot A, Hill S, Summers M, Taylor M. Comparing face-to-face and online qualitative research with people with multiple sclerosis. Qual Health Res . 2014;24(3):431–438. doi: 10.1177/1049732314523840. [DOI] [PubMed] [Google Scholar]
- 20.Smith B, Sparkes AC. Routledge Handbook of Qualitative Research in Sport and Exercise . 1st ed. Taylor & Francis; 2016. [Google Scholar]
- 21.Smith B, McGannon KR. Developing rigor in qualitative research: problems and opportunities within sport and exercise psychology. Int Rev Sport Exerc Psychol . 2018;11(1):101–121. doi: 10.1080/1750984X.2017.1317357. [DOI] [Google Scholar]
- 22.Burke S. Routledge Handbook of Qualitative Research in Sport and Exercise . 1st ed. Taylor & Francis; 2016. Rethinking ‘validity’ and ‘trustworthiness’ in qualitative inquiry: how might we judge the quality of qualitative research in sport and exercise sciences? pp. 352–362. [Google Scholar]
- 23.Tracy SJ. Qualitative quality: eight “big-tent” criteria for excellent qualitative research. Qual Inq . 2010;16(10):837–851. doi: 10.1177/1077800410383121. [DOI] [Google Scholar]
- 24.Smith B, Caddick N. Qualitative methods in sport: a concise overview for guiding social scientific sport research. Asia Pac J Sport Soc Sci . 2012;1(1):60–73. doi: 10.1080/21640599.2012.701373. [DOI] [Google Scholar]
- 25.Smith B. Generalizability in qualitative research: misunderstandings, opportunities and recommendations for the sport and exercise sciences. Qual Res Sport Exerc Health . 2018;10(1):137–149. doi: 10.1080/2159676X.2017.1393221. [DOI] [Google Scholar]
- 26.Braun V, Clarke V, Weate P. Routledge Handbook of Qualitative Research in Sport and Exercise . 1st ed. Taylor & Francis; 2016. Using thematic analysis in sport and exercise research; pp. 191–205. [Google Scholar]
- 27.Bandura A. Health promotion by social cognitive means. Health Educ Behav . 2004;31(2):143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 28.Latimer-Cheung AE, Ginis KAM, Hicks AL et al. Development of evidence-informed physical activity guidelines for adults with multiple sclerosis. Arch Phys Med Rehabil . 2013;94(9):1829–1836. doi: 10.1016/j.apmr.2013.05.015. [DOI] [PubMed] [Google Scholar]
- 29.Lejbkowicz I, Paperna T, Stein N, Dishon S, Miller A. Internet usage by patients with multiple sclerosis: implications to participatory medicine and personalized healthcare. Mult Scler Int . 2010;2010:640749. doi: 10.1155/2010/640749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marrie RA, Salter AR, Tyry T, Fox RJ, Cutter GR. Preferred sources of health information in persons with multiple sclerosis: degree of trust and information sought. J Med Internet Res . 2013;15(4):e67. doi: 10.2196/jmir.2466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Russell RD, Black LJ, Begley A. The unresolved role of the neurologist in providing dietary advice to people with multiple sclerosis. Mult Scler Relat Disord . 2020;44:102304. doi: 10.1016/j.msard.2020.102304. [DOI] [PubMed] [Google Scholar]
- 32.US Department of Agriculture and US Department of Health and Human Services Dietary Guidelines for Americans . 7th ed. US Government Printing Office; 2010. Dec, 2010. [Google Scholar]
- 33.Motl R, Ehde D, Shinto L, Fernhall B, LaRocca N, Zackowski K. Health behaviors, wellness, and multiple sclerosis amid COVID-19. Arch Phys Med Rehabil . 2020;101(10):1839–1841. doi: 10.1016/j.apmr.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


