Abstract
Excision repair complementary complex 5 (ERCC5) is an important component in the repair pathway of platinum-induced damage. The current study evaluated the effect of ERCC5 variants (rs751402 and rs1047768) on the clinical outcome of platinum-based regimens in non-small cell lung cancer (NSCLC) patients. A prospective, cohort study was conducted on 57 newly diagnosed NSCLC Egyptian patients. Patients received either cisplatin or carboplatin-based chemotherapy. DNA was extracted and the variants were analyzed using real time PCR. This study found no significant difference between the studied variants and patients’ response to chemotherapy, progression-free survival (PFS) or overall survival (OS). However, a statistically significant association was found between the histologic subtypes and the studied variants (p = 0.028 and 0.018 for rs751402 and rs1047768, respectively). A statistically significant association was evident between the type of the allele present in the studied polymorphisms, p value = 0.000040. Moreover, the minor allele frequency (MAF) of the studied variants rs751402 and rs1047768 were similar to those of African and European populations, respectively. Results of this study have concluded that ERCC5 variants did not affect the clinical outcome of platinum-based chemotherapy in NSCLC. A significant coinheritance was found between the two variants of ERCC5. Moreover, the similarity between the MAF of the studied variants and the African or European population can guide future research when extrapolating data from African European populations to their Egyptian counterparts.
Keywords: ERCC5, Non-small cell lung cancer, Platinum, rs751402, rs1047768
Introduction
Lung cancer is the second most diagnosed cancer worldwide. It’s the leading cause of cancer-related death in men while in women, it represents the second cause of death after breast cancer [1] with a cumulative 5-year survival of 10–20% [2].
Histologically it’s divided into two subtypes non-small cell lung cancer (NSCLC) which represents about 85% and small cell lung cancer (SCLC) which represent 15% [3]. NSCLC is further subdivided into non- squamous carcinoma (including adenocarcinoma, large-cell carcinoma, other cell types) and squamous cell carcinoma [4, 5].
Unfortunately NSCLC patients are mostly diagnosed at advanced stages (stage 3 and 4) which leads to poor prognosis [6].
Before the era of targeted and immunotherapy, platinum-based chemotherapy was the standard of care for NSCLC patients with advanced or metastatic disease. It consists of cisplatin or carboplatin in addition to taxanes, gemcitabine, vinorelbine, etoposide or pemetrexed [7, 8].
Cisplatin and carboplatin are heavy metal complexes that damage DNA molecules by crosslinking with the purine bases on the DNA; producing adducts that eventually cause apoptosis [9]. Interestingly, patients with the same histological types of tumor and of the same stage respond differently to chemotherapy, suggesting that there might be other factors contribute to chemoresistance such as genetic variants of certain genes involved in the response to chemotherapy [10].
Different pathways exist to repair DNA damage induced by platinum agents such as base excision repair pathway (BER), double strand break repair (DSB), DNA mismatch repair, and most importantly nucleotide excision repair (NER) [8, 10, 11]. Consequently single nucleotide polymorphisms (SNPs) in DNA repair genes may play an important role in response to chemotherapy, chemotherapy toxicity as well as cancer survival [6, 8, 10, 12].
Nucleotide excision repair (NER) enzymes are one of the main pathways involved in the repair process of platinum DNA adducts. It involves coordination of many enzymes that restore the platinum-induced DNA damage as excision repair cross-complementing group 1 (ERCC1), excision repair cross-complementation group 2 (ERCC2), excision repair cross-complementation group 5 (ERCC5) [8, 11].
Excision Repair Complementary Complex 5 (ERCC5), also known as the xeroderma pigmentosum complementation group G (XPG) gene, located on chromosome 13, is an important component of NER [13]. It contains 15 exons which forms a structure specific endonuclease that recognizes and cleaves the platinum—DNA adduct at both the 3′ and 5′ ends [14, 15]. Hence, change in the activity or expression of ERCC5 might affect the platinum activity which in turn affect response to platinum chemotherapy.
Most of the published studies have focused on the relation between single nucleotide polymorphisms (SNPs) in ERCC5 and the risk of various types of cancer [14–18] as well as cancer prognosis [19–21] while few studies have addressed the association between XPG polymorphisms and chemotherapy outcome [22, 23] and most of them were done on Asian populations.
Thus the objective of this study was to evaluate the effect of polymorphism in the ERCC5/XPG (rs751402 and rs1047768) gene on the clinical outcome of platinum-based regimens used in the treatment of NSCLC in Egyptian patients.
Materials and methods
Design and settings
A prospective, cohort study was conducted on 57 histologically confirmed non-small cell lung cancer (NSCLC) Egyptian patients recruited from the department of clinical oncology, faculty of medicine, Ain Shams University. Patient recruitment started from March 2017 to January 2019.
Patients
Newly diagnosed histologically confirmed NSCLC patients receiving platinum-based chemotherapy with a performance status (PS) of 0–2 [24] and adequate bone marrow reserve were included in the study. Patients were excluded if they received previous chemotherapy or targeted therapy, had central nervous system metastases, inadequate liver, or kidney function, second primary malignancy, or were pregnant or lactating.
The study was approved by the Faculty of Pharmacy, Ain Shams University, Cairo, Egypt research ethics committee for experimental and clinical studies under number PHCL137. All the patients were required to give an informed consent for participation in the study without any obligations to withdraw from the study anytime. The study was conducted in accordance with the declaration of Helsinki as revised in 2013. The study was registered at clinical trial registry with Clinical trial.gov registration number: NCT03154242.
Methods
Treatment and clinical assessments
Patients received intravenous doses of gemcitabine 1200 mg/m2 on day 1 and 8 or etoposide 100 mg/m2 day on day 1,2 and 3 plus cisplatin 75 mg/m2 or gemcitabine 1000 mg/m2 on day 1 and 8 or Paclitaxel 175 mg/m2 plus carboplatin AUC 5 on day 1 every 21 days per cycle for a maximum of 6 cycles. Chemotherapy was given only if neutrophils ≥ 1.5 × 109/L, platelets ≥ 100 × 109/L, and haemoglobin ≥ 9.0 gm/dL. Patients with poor performance or documented renal impairment or hearing loss were started with carboplatin rather than cisplatin-based regimen. Patients were shifted to carboplatin-based regimen during the chemotherapy cycles if they developed toxicities or could not tolerate it during subsequent cycles. Patients who experienced grade 3 or 4 toxicity had a change in therapy either dose reduction, discontinuation, or pharmacologic intervention to prevent or treat the toxicity according to the regimen protocol.
At baseline, patients’ demographic and clinical data were assessed including complete history, physical examination, radiographic investigations as CT scan (chest and pelvi-abdomen). Moreover, laboratory analysis including complete blood count (CBC) and liver and kidney function tests were performed. Patient prognostic stage was assessed using TNM 7th edition [25]. All laboratory analyses were repeated every cycle and CBC was repeated before day 8 of chemotherapy. Tumor response was evaluated using the Response Evaluation Criteria in Solid Tumors (RECIST) Version 1.1 [26].
The primary outcome was the progression-free survival (PFS); defined as the time from start of chemotherapy to the day of documented disease progression or death. While the secondary outcomes were objective response rate (ORR), and overall survival (OS); defined as the time from start of chemotherapy to death from any cause. Each patient was followed up to 18 months. Patients who completed the follow-up period without disease progression or death were considered censored. Patients who did not complete the follow-up period were censored at the last follow-up visit.
Polymorphism selection
Data about the allelic frequencies of different genes in the Egyptian population is still lacking, and hence we hypothesized its similarity to the European and African population distribution based on its location with respect to Africa and Europe. The single nucleotide polymorphisms (SNPs) were selected according to an average minor allele frequency (MAF) of more than or equal to 25% with higher frequencies in European or African population.
Sample collection and genotyping
Two millilitres of venous blood were withdrawn from each patient into vacutainer tubes containing Ethylene diamine tetra acetic acid (EDTA). DNA was isolated with the QIAamp DNA blood Mini kit (QIAGEN®, Germany), according to the manufacturer’s instructions [27]. For Single nucleotide polymorphism (rs1047768 and rs751402) genotyping; Taqman® Single nucleotide polymorphism (SNP) genotyping assay (Applied Biosystems®) [28] and TaqMan Universal PCR Master Mix (Applied Biosystems®) was used. Real-time PCR using Rotor gene Q (QIAGEN®) was performed.
Statistical analysis
Statistical analysis was done by the statistical software package version 20 (SPSS Inc., Chicago, IL). Frequencies and percentages were used to summarize categorical data. For assessment of agreement of genotype frequencies with those expected under Hardy–Weinberg equilibrium standard chi-square test was performed. Each polymorphism was analysed using general genetic model (homozygous major allele versus heterozygous versus homozygous minor allele) and those who were found statistically significant were further analysed using the dominant model (homozygous major allele compared to others) and recessive model (homozygous minor allele compared to others).
Chi-square and fisher’s exact tests were used to test if there was an association between the investigated polymorphisms and different clinicopathological variables or ORR. OS and PFS were evaluated with the Kaplan–Meier method and groups were compared with the log-rank test. All reported values were 2-sided and p-values < 0.05 were considered significant.
Results
Baseline characteristics
Patients’ characteristics at baseline are shown in Table 1. The median age of patients was 55 years (range 33–80), males comprised 80.7% of patients and 9 patients had 1st degree family history of cancer. Non-smokers represented 22.8% of patients. The patients’ tumor histologic subtypes were as follows; 47.4% adenocarcinoma, 36.8% squamous, and 15.8% other subtypes as large-cell or not otherwise specified. On presentation, 47 patients (82.5%) had advanced stage (stage 3b and 4) while 10 patients (17.5%) had earlier stages for which 3 of them had undergone surgery. Four patients of the study cohort undergone radical radiotherapy.
Table 1.
Patient demographics, clinical and genotypic characteristics
| Characteristics | Category | n (%) |
|---|---|---|
| Gender | Female | 11 (19.3) |
| Male | 46 (80.7) | |
| Median age (range) | 55 (33–80) | |
| < 55 | 26 (45.6) | |
| ≥ 55 | 31 (54.4) | |
| Comorbidities | Hypertension | 10 (17.5) |
| Diabetes | 6 (10.5) | |
| Smoking | Ever smoker | 44 (77.2) |
| Non-smoker | 13 (22.8) | |
| Family history (first degree) | No | 48 (84.2) |
| Yes | 9 (15.8) | |
| NSCLC subtype | Adenocarcinoma | 27 (47.4) |
| Squamous cell carcinoma | 21 (36.8) | |
| Others | 9 (15.8) | |
| Performance status (PS)a | 0 | 3 (5.3) |
| 1 | 33 (57.9) | |
| 2 | 21 (36.8) | |
| Stageb | Early (≤ 3A) | 10 (17.5) |
| Late (3B and 4) | 47 (82.5) | |
| Other treatment modalities | Surgery | 3 (5.3) |
| Radical radiotherapy | 4 (7) | |
| Chemotherapy regimenc | Platinum/Gemcitabine | 51 (89.5) |
| Platinum/Etoposide | 5 (8.8) | |
| Platinum/Paclitaxel | 1 (1.8) | |
| Type of platinum | Cisplatin-based | 39 (68.4) |
| Carboplatin-based | 18 (31.6) | |
| Number of cycles | < 4 | 17 (29.8) |
| ≥ 4 | 40 (70.2) | |
| rs751402 | AA | 5 (8.8) |
| AG | 25 (43.9) | |
| GG | 27 (47.4) | |
| rs1047768 | CC | 15 (26.3) |
| CT | 32 (56.1) | |
| TT | 10 (17.5) |
aPerformance Status (PS) was assessed using Eastern Cooperative Oncology Group performance status (ECOG)
bStage was assessed using AJCC TNM 7th edition
cChoice was based mainly on the availability in the hospital
At the start of chemotherapy, Performance status (PS) included 57.9% of patients PS 1 and 36.8% PS 2. Most of the platinum-based chemotherapy (68.4%) was cisplatin-based and 89.5% of patients received gemcitabine as their second agent. Most of the patients completed 4 or more cycles of chemotherapy.
Genotype distribution and association between clinicopathologic variables and polymorphisms
Genotype frequencies of both ERCC5 rs751402 A > G and rs1047768 T > C are listed in Table 1 with minor alleles; A allele for rs751402 and T allele for rs1047768. Both frequencies are in concordance with those expected under Hardy–Weinberg equilibrium (p = 0.937 and p = 0.426, respectively).
On analysing the coinheritance between the genetic variants of the two variants as shown in Table 2, a statistically significant difference was found between them in every genetic model assessed (p = 0.00004, 0.000033, and 0.033 for general, dominant, and recessive models, respectively).
Table 2.
Analysis of the coinheritance between the genetic variants of ERCC5
| SNP | rs1047768 | p value | ||
|---|---|---|---|---|
| CC | CT | TT | ||
| rs751402 | ||||
| AA | 0 (0) | 2 (3.5) | 3 (5.3) | 0.000040a |
| AG | 1 (1.8) | 18 (31.6) | 6 (10.5) | 0.000033b |
| GG | 14 (24.6) | 12 (21.1) | 1 (1.8) | 0.033c |
ap value was computed by fisher’s exact test comparing rs751402 variants to rs1047768 variants, bold indicate statistical significance
bp value was computed by chi-square test comparing rs751402 in dominant model (GG vs AA + AG) and rs1047768 in dominant model (CC vs TT + CT), bold indicate statistical significance
cp value was computed by fisher’s exact test comparing rs751402 in recessive model (AA vs GG + AG) and rs1047768 in recessive model (TT vs CC + CT), bold indicate statistical significance
Moreover, a statistically significant difference was evident between the various histologic subtypes and both rs751402 and rs1047768 genetic variants in the general model (p = 0.028 and 0.018, respectively). On further analysis, the association was found in rs751402 dominant genetic model; homozygous major allele GG compared to those with heterozygous and homozygous minor allele (AG + AA). However, this association was not evident in the recessive model (homozygous minor allele AA compared to the others (AG + GG) with p = 0.017. On the contrary, for rs1047768 variants the statistically significant difference was found in the recessive model between homozygous minor allele TT compared to (CC + CT) but not in the dominant model (CC vs TT + CT) with p = 0.014 as shown in Table 3
Table 3.
Association between patients’ clinicopathological variables and genetic polymorphism of rs751402 and rs1047768 (n = 57)
| Variable n (%) | rs751402 n (%) |
p value | rs1047768 n (%) |
p value | ||||
|---|---|---|---|---|---|---|---|---|
| AA | AG | GG | CC | CT | TT | |||
| Gender | ||||||||
| Male | 0 (0) | 5 (8.8) | 6 (10.5) | 0.782b | 1 (1.8) | 7 (12.3) | 3 (5.3) | 0.376b |
| Female | 5 (8.8) | 20 (35.1) | 21 (36.8) | 14 (24.6) | 25 (43.9) | 7 (12.3) | ||
| Age | ||||||||
| < 55 | 1 (1.8) | 13 (22.8) | 12 (21.1) | 0.529b | 7 (12.3) | 15 (26.3) | 4 (7) | 0.926a |
| ≥ 55 | 4 (7) | 12 (21.1) | 15 (26.3) | 8 (10.4) | 17 (29.8) | 6 (10.5) | ||
| Smoking | ||||||||
| Non-smoker | 0 (0) | 6 (10.5) | 7 (12.3) | 0.717b | 2 (3.5) | 7 (12.3) | 4 (7) | 0.346b |
| Ever smoker | 5 (8.8) | 19 (33.3) | 20 (35.1) | 13 (22.8) | 25 (43.9) | 6 (10.5) | ||
| Family history | ||||||||
| No | 4 (7) | 23 (40.4) | 21 (36.8) | 0.337b | 13 (22.8) | 25 (43.9) | 10 (17.5) | 0.290b |
| Yes | 1 (1.8) | 2 (3.5) | 6 (10.5) | 2 (3.5) | 7 (12.3) | 0 (0) | ||
| Subtype | ||||||||
| Adeno | 3 (5.3) | 12 (21.1) | 12 (21.1) | 0.028b | 5 (8.8) | 19 (33.3) | 3 (5.3) | 0.018b |
| Squamous | 0 (0) | 7 (12.3) | 14 (24.6) | 0.017b* | 8 (14) | 11 (19.3) | 2 (3.5) | 0.297a* |
| Other | 2 (3.5) | 6 (10.5) | 1 (1.8) | 0.098b** | 2 (3.5) | 2 (3.5) | 5 (8.8) | 0.014b** |
| ECOG PS | ||||||||
| 0 | 0 (0) | 2 (3.5) | 1 (1.8) | 0.853b | 1 (1.8) | 2 (3.5) | 0 (0) | 0.788b |
| 1 | 4 (7) | 14 (24.6) | 15 (26.3) | 7 (12.3) | 20 (35.1) | 6 (10.5) | ||
| 2 | 1 (1.8) | 9 (15.8) | 11 (19.3) | 7 (12.3) | 10 (17.5) | 4 (7) | ||
| Stage† | ||||||||
| Early (≤ 3A) | 1 (1.8) | 5 (8.8) | 4 (7) | 0.882b | 3 (5.3) | 5 (8.8) | 2 (3.5) | 0.901b |
| Late (3B & 4) | 4 (7) | 20 (35.1) | 23 (40.4) | 12 (21.1) | 27 (47.4) | 8 (14) | ||
| Type of platinum | ||||||||
| Cisplatin | 5 (8.8) | 19 (33.3) | 15 (26.3) | 0.096b | 10 (17.5) | 23 (40.4) | 6 (10.5) | 0.797b |
| Carboplatin | 0 (0) | 6 (10.5) | 12 (21.1) | 5 (8.8) | 9 (15.8) | 4 (7) | ||
| No. of cycles | ||||||||
| < 4 | 2 (3.5) | 7 (12.3) | 8 (14) | 0.833b | 3 (5.3) | 10 (17.5) | 4 (7) | 0.487b |
| ≥ 4 | 3 (5.3) | 18 (31.6) | 19 (33.3) | 12 (21.1) | 22 (38.6) | 6 (10.5) | ||
ECOG PS Eastern Cooperative Oncology Group performance status
*p value obtained from analysis of dominant model (GG vs AA + AG) for rs751402 and (CC vs TT + CT) for rs1047768
**p value obtained from analysis of recessive model (AA vs GG + AG) for rs751402 and (TT vs CC + CT) for rs1047768
†Stage was assessed using AJCC TNM 7th edition
aChi-square test, two-sided p value < 0.05 is significant, b Fisher's exact test, two-sided p value < 0.05 is significant, bold indicates statistical significant
Response analysis
Among the studied patients, none achieved complete response (CR) while 6 patients (10.5%) had partial response (PR), 18 patients (31.6%) had stable disease (SD) and 23 patients (40.4%) had progressed disease (PD). Nine patients (15.8%) had not undergone response assessment; 3 patients (5.3%) of them due to receiving chemotherapy as neoadjuvant or adjuvant and 6 patients (10.5%) due to patient’s death or loss to follow-up before undergoing first CT scan during chemotherapy cycles.
No statistically significant difference was observed between genetic polymorphisms of ERCC5 rs751402 and rs1047768 and patients’ response to chemotherapy as shown in Table 4
Table 4.
Response analysis of rs751402 and rs1047768 polymorphisms (n = 57)
| Response | Tumor responsea,b n (%) |
p valuec | Response categorya, b n (%) |
p valuec | |||
|---|---|---|---|---|---|---|---|
| PR | SD | PD | Responder (CR + PR) |
Non-responder (SD + PD) |
|||
| rs751402 | 0.369 | 0.217 | |||||
| AA | 1 (1.8) | 1 (1.8) | 3 (5.3) | 1 (1.8) | 4 (7) | ||
| AG | 4 (7) | 6 (10.5) | 10 (17.5) | 4 (7) | 16 (28) | ||
| GG | 1 (1.8) | 11 (19.3) | 11 (19.3) | 1 (1.8) | 22 (38.6) | ||
| rs1047768 | 0.574 | 1.00 | |||||
| CC | 2 (3.5) | 7 (12.3) | 4 (7) | 2 (3.5) | 11 (19.3) | ||
| CT | 3 (5.3) | 8 (14) | 15 (26.3) | 3 (5.3) | 23 (40.4) | ||
| TT | 1 (1.8) | 3 (5.3) | 5 (8.8) | 1 (1.8) | 8 (14) | ||
CR complete response, PD progressed disease, PR partial response, SD stable disease
aNine (15.8%) patients have not undergone response assessment
bResponse was assessed using RECIST 1.1
cFisher's exact test, two-sided p value < 0.05 is significant
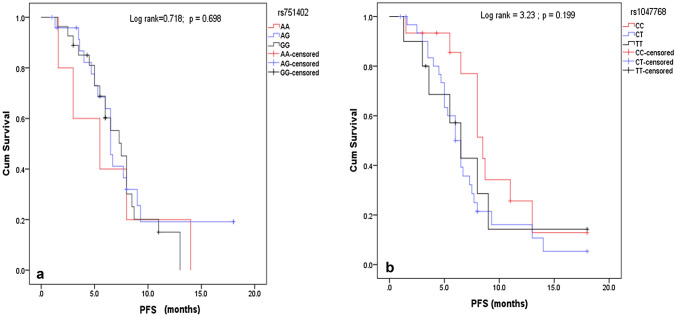
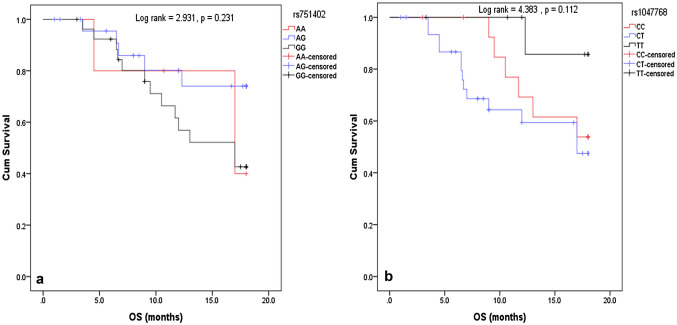
Survival analysis
Progression-free survival (PFS) at the end of the 18 months period, 43 patients (75.4%) had progressed, 3 patients had not shown any disease progression and 11 patients (19.3%) were lost to follow-up while for Overall survival (OS) 20 patients (35.1%) died, 22 patients (38.6%) completed the follow-up period, while 15 patients (26.3%) were lost to follow-up.
There was not any statistically significant difference between PFS or OS and each of rs751402 and rs1047768 polymorphisms as shown in Figs. 1 and 2
Fig. 1.
Kaplan Meier curve showing the effect of genetic variants on Progression-Free Survival (PFS). a Curve represents the relation between rs751402 variants (AA vs AG vs GG) and PFS. b Curve represents the relation between rs1047768 variants (CC vs CT vs TT) and PFS
Fig. 2.
Kaplan Meier curve showing the effect on Overall Survival (OS). a Curve represents the relation between rs751402 variants (AA vs AG vs GG) and OS. b Curve represents the relation between rs1047768 variants (CC vs CT vs TT) and OS
Discussion
Non-small cell lung cancer (NSCLC) is one of the leading causes of cancer-related deaths [1, 4]. Platinum-based chemotherapy is essential for treatment of NSCLC patients without driver mutations and for those who cannot afford the cost of targeted and immunotherapy [29]. Since the response to platinum-based regimens is variable therefore the need for identifying patients who would benefit more from chemotherapy is crucial.
Enzyme repair complementary complex 5 (ERCC5) is one of the key players for repairing platinum DNA adduct through the dual incision at both the 5’ and 3’ sides of the adduct which may lead to a decrease in platinum activity against cancer [30]. Hence, mutations in ERCC5 might enhance platinum effect on cancer cells. The current study is one of the few studies that addressed the relation between ERCC5 polymorphisms in rs751402 and rs1047768 and the outcome of platinum-based chemotherapy in terms of response and survival. Moreover, most of the published studies have focused on Asian populations rather than Caucasians.
The polymorphisms of rs751402 and rs1047768 both followed the Hardy–Weinberg distribution with a minor allele frequency (MAF) of 29.7% for the A allele in rs751402 which resembles the MAF of this allele in the African population (30–31%). While the T allele, which is the minor allele of rs1047768, showed a frequency of 41.8% which resembles the MAF of the same allele in the European population (41.2%) according to the alfa project from NCBI [31, 32]. Data regarding the allelic frequencies and ethnicity origin of the Egyptian population is still lacking, with a proposed heterogenous distribution from African–European ancestry. Hence, the results of the current study could pave the way when interpreting the scarce data addressing the Egyptian population. Moreover, it can guide future research when extrapolating data from African European populations to their Egyptian counterparts.
On investigating the coinheritance between the studied polymorphisms, we found a statistically significant association in the general genetic model as well as the dominant and recessive models as shown in Table 2. These associations might be attributed to the effect of rs751402, located in the promotor region, on the rs1047768, located in the exon region, indicating that rs751402 variants might affect the type of the allele present on rs1047768. Similarly, Blomquist et al. in their study on normal bronchial epithelial cells found that the A allele on rs751402 was associated with higher expression of T allele on rs1047768 [33].
On studying the association between the clinicopathologic variables and rs751402 or rs1047768 genetic variants, no statistically significant difference was found apart from the histologic subtypes. Interestingly, there was a statistically significant association between the histologic subtypes and the studied genotypes in some of the genetic models. Regarding rs751402, a relation between the histologic subtypes and different genotypes was found in the general model and dominant model. This might indicate that the A allele (minor allele) was more expressed with specific histologic subtypes. On the other hand, for the rs1047768, the association was found in the general and recessive model representing a link with the C allele (major allele). Rulli et al. found a similar association between ERCC1 (rs11615) genetic variants and the histologic subtypes of NSCLC [34].
The current study did not report an association between any of the investigated SNPs and the platinum response. Similarly, other NSCLC patients of different ethnicities did not report an association [35, 36]. However, a metanalysis in NSCLC found that patients with C allele in rs1047768 were more platinum sensitive [37]. Similarly, He et al. in their study on Chinese population with NSCLC found that AA genotype of rs751402 had better platinum response than AG + GG genotypes specially in the squamous subtype [38]. The discrepancies between those studies and ours might be attributed to the racial differences between the two populations.
In accordance with what was found in other studies [22, 34], the current study showed no statistically significant difference between the different genotypes in both SNPs and neither PFS nor OS. On the contrary, these findings contradict what was found in a trial on NSCLC patients where the TT genotype of rs1047768 had statistically significant shorter PFS and OS compared to the CC genotype [39]. This difference in relation to our findings might be attributed to several factors including greater sample size and differences in the genetic makeup between the populations.
Conclusion and limitation
This study couldn’t find an association between the polymorphisms of ERCC5 rs751402 or rs1047768 and the outcome of platinum-based chemotherapy, however, it showed an association between rs751402 and rs1047768 genetic variants and the histologic subtypes of NSCLC. Moreover, a strong association was evident between the type of the allele present in the two selected SNPs. Precision medicine aims at targeting therapy, improving outcomes & subsequently reducing costs. Hence, identifying those variants that will affect and those that will not affect are both important in guiding therapy decisions. The coinheritance among the studied genetic variants might suggest a linkage disequilibrium among them which might pave the way for further research of finding tag SNPs that could predict response. The similarity between the MAF of the studied variants and the African or European population might shed the light on further understanding of the ethnicity of the Egyptian population. This study is limited by the small sample size and short follow-up period. Hence, larger studies with longer follow-up is needed to confirm the results of this study and to better elucidate the relationship between the two studied variants.
Author contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by ESA, AAN. The first draft of the manuscript was written by ESA and was revised by all authors. All authors read and approved the final manuscript.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Ethical approval
This observational study was approved by the Faculty of Pharmacy, Ain Shams University, Cairo, Egypt research ethics committee for experimental and clinical studies under number PHCL137. The study was conducted in accordance with the declaration of Helsinki as revised in 2013.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Esraa S. Abdalkhalek, Email: esraa.abdalkhalek@pharma.asu.edu.eg
Lamia M. El Wakeel, Email: lamia.elwakeel@pharma.asu.edu.eg.
Ahmed A. Nagy, Email: ahmedalynagy@yahoo.com
Nagwa A. Sabri, Email: Nagwa.sabri@pharma.asu.edu.eg
References
- 1.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Mattiuzzi C, Lippi G. Current cancer epidemiology. J Epidemiol Glob Health. 2019;9(4):217–222. doi: 10.2991/jegh.k.191008.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zappa C, Mousa SA. Non-small cell lung cancer: current treatment and future advances. Transl Lung Cancer Res. 2016;5(3):288–300. doi: 10.21037/tlcr.2016.06.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Duma N, Santana-Davila R, Molina JR. Non-small cell lung cancer: epidemiology, screening, diagnosis, and treatment. Mayo Clin Proc. 2019;94(8):1623–1640. doi: 10.1016/j.mayocp.2019.01.013. [DOI] [PubMed] [Google Scholar]
- 5.NCCN, Non-Small Cell Lung Cancer (Version 5.2021), 2021. https://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf. Accessed 8 Aug 2021.
- 6.Powrozek T, Mlak R, Krawczyk P, Homa I, Ciesielka M, Koziol P, Prendecka M, Milanowski J, Malecka-Massalska T. The relationship between polymorphisms of genes regulating DNA repair or cell division and the toxicity of platinum and vinorelbine chemotherapy in advanced NSCLC patients. Clin Transl Oncol. 2016;18(2):125–131. doi: 10.1007/s12094-015-1343-6. [DOI] [PubMed] [Google Scholar]
- 7.Rose MC, Kostyanovskaya E, Huang RS. Pharmacogenomics of cisplatin sensitivity in non-small cell lung cancer. Genom Proteom Bioinform. 2014;12(5):198–209. doi: 10.1016/j.gpb.2014.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Perez-Ramirez C, Canadas-Garre M, Molina MA, Robles AI, Faus-Dader MJ, Calleja-Hernandez MA. Contribution of genetic factors to platinum-based chemotherapy sensitivity and prognosis of non-small cell lung cancer. Mutat Res. 2017;771:32–58. doi: 10.1016/j.mrrev.2016.11.003. [DOI] [PubMed] [Google Scholar]
- 9.Dasari S, Tchounwou PB. Cisplatin in cancer therapy: molecular mechanisms of action. Eur J Pharmacol. 2014;740:364–378. doi: 10.1016/j.ejphar.2014.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zou HZ, Zhao YQ. XPG polymorphisms are associated with prognosis of advanced non-small cell lung cancer treated with platinum-based doublet chemotherapy. Genet Mol Res. 2015;14(1):500–506. doi: 10.4238/2015.January.26.3. [DOI] [PubMed] [Google Scholar]
- 11.Liu D, Wu J, Shi GY, Zhou HF, Yu Y. Role of XRCC1 and ERCC5 polymorphisms on clinical outcomes in advanced non-small cell lung cancer. Genet Mol Res. 2014;13(2):3100–3107. doi: 10.4238/2014.April.17.6. [DOI] [PubMed] [Google Scholar]
- 12.Sullivan I, Salazar J, Majem M, Pallares C, Del Rio E, Paez D, Baiget M, Barnadas A. Pharmacogenetics of the DNA repair pathways in advanced non-small cell lung cancer patients treated with platinum-based chemotherapy. Cancer Lett. 2014;353(2):160–166. doi: 10.1016/j.canlet.2014.07.023. [DOI] [PubMed] [Google Scholar]
- 13.Clarkson S. The XPG story. Biochimie. 2003;85(11):1113–21. [DOI] [PubMed]
- 14.Liu ZQ, Chen GG, Sun RL, Chen C, Lu MY, Guan LF, Chi XL, Jian YQ, Zhu X, Liu RQ, Cai BY, Chen FF, Liu B. XPG rs873601 G>A contributes to uterine leiomyoma susceptibility in a Southern Chinese population. 2018. Biosci Rep. 10.1042/BSR20181116. [DOI] [PMC free article] [PubMed]
- 15.Huang J, Liu X, Tang LL, Long JT, Zhu J, Hua RX, Li J. XPG gene polymorphisms and cancer susceptibility: evidence from 47 studies. Oncotarget. 2017;8(23):37263–37277. doi: 10.18632/oncotarget.16146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liang J, Xu YY, Zhang C, Xia QR. Association of XPG gene rs751402 polymorphism with gastric cancer risk: a meta-analysis in the Chinese population. Int J Biol Markers. 2018;33(2):174–179. doi: 10.5301/ijbm.5000313. [DOI] [PubMed] [Google Scholar]
- 17.Ma SH, Ling FH, Sun YX, Chen SF, Li Z. Investigation on the role of XPG gene polymorphisms in breast cancer risk in a Chinese population. Genet Mol Res. 2016 doi: 10.4238/gmr.15028066. [DOI] [PubMed] [Google Scholar]
- 18.Bhat GR, Sethi I, Bhat A, Verma S, Bakshi D, Sharma B, Nazir M, Dar KA, Abrol D, Shah R, Kumar R. Genetic evaluation of the variants using MassARRAY in non-small cell lung cancer among North Indians. Sci Rep. 2021;11(1):11291. doi: 10.1038/s41598-021-90742-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang XQ, Terry PD, Li Y, Zhang Y, Kou WJ, Wang MX. Association of XPG rs2094258 polymorphism with gastric cancer prognosis. World J Gastroenterol. 2019;25(34):5152–5161. doi: 10.3748/wjg.v25.i34.5152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li C, Yu X, Guo D, Liu G, Zhang K, Teng Q, Lin H. Association between common polymorphisms in ERCC gene and prognosis of osteosarcoma in patients treated with chemotherapy: a meta-analysis. Onco Targets Ther. 2018;11:3495–3504. doi: 10.2147/OTT.S158167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li YK, Xu Q, Sun LP, Gong YH, Jing JJ, Xing CZ, Yuan Y. Nucleotide excision repair pathway gene polymorphisms are associated with risk and prognosis of colorectal cancer. World J Gastroenterol. 2020;26(3):307–323. doi: 10.3748/wjg.v26.i3.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yuli Y, Zhe S, Xia W, Siqing L, Zhenxuan W, Yu-Hua Z, Bing S, Jun-Wei C. XPG is a novel biomarker of clinical outcome in advanced non-small-cell lung cancer. Pak J Med Sci. 2013;29(3):762–767. doi: 10.12669/pjms.293.3664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sun XH, Hou WG, Zhao HX, Zhao YL, Ma C, Liu Y. Single nucleotide polymorphisms in the NER pathway and clinical outcome of patients with bone malignant tumors. Asian Pac J Cancer Prev. 2013;14(3):2049–2052. doi: 10.7314/APJCP.2013.14.3.2049. [DOI] [PubMed] [Google Scholar]
- 24.Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, Carbone PP. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5(6):649–655. doi: 10.1097/00000421-198212000-00014. [DOI] [PubMed] [Google Scholar]
- 25.Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010;17(6):1471–1474. doi: 10.1245/s10434-010-0985-4. [DOI] [PubMed] [Google Scholar]
- 26.Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, Rubinstein L, Shankar L, Dodd L, Kaplan R, Lacombe D, Verweij J. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1) Eur J Cancer. 2009;45(2):228–247. doi: 10.1016/j.ejca.2008.10.026. [DOI] [PubMed] [Google Scholar]
- 27.QIAGEN. QIAamp DNA mini and blood mini handbook, QIAGEN; 2016.
- 28.Applied Biosystems, TaqMan SNP genotyping assays protocol 2010.
- 29.Rottenberg S, Disler C, Perego P. The rediscovery of platinum-based cancer therapy. Nat Rev Cancer. 2021;21(1):37–50. doi: 10.1038/s41568-020-00308-y. [DOI] [PubMed] [Google Scholar]
- 30.Malik SS, Mubarik S, Masood N, Khadim MT. An insight into clinical outcome of XPG polymorphisms in breast cancer. Mol Biol Rep. 2018;45(6):2369–2375. doi: 10.1007/s11033-018-4401-7. [DOI] [PubMed] [Google Scholar]
- 31.dbSNP. Reference SNP (rs) report; 2021. https://www.ncbi.nlm.nih.gov/snp/rs1047768?vertical_tab=true#frequency_tab. Accessed 21 Sept 2021.
- 32.dpSNP, Reference SNP (rs) report; 2021. https://www.ncbi.nlm.nih.gov/snp/rs751402?vertical_tab=true#frequency_tab. Accessed 21 Sept 2021.
- 33.Blomquist TM, Crawford EL, Willey JC. Cis-acting genetic variation at an E2F1/YY1 response site and putative p53 site is associated with altered allele-specific expression of ERCC5 (XPG) transcript in normal human bronchial epithelium. Carcinogenesis. 2010;31(7):1242–1250. doi: 10.1093/carcin/bgq057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rulli E, Marabese M, Piva S, Bonomi L, Caiola E, Ganzinelli M. DNA repair gene polymorphisms in non-small-cell lung cancer patients treated with first-line platinum-containing chemotherapy. Tumori J. 2016;102(4):367–375. doi: 10.5301/tj.5000526. [DOI] [PubMed] [Google Scholar]
- 35.Rulli E, Guffanti F, Caiola E, Ganzinelli M, Damia G, Garassino MC, Piva S, Ceppi L, Broggini M, Marabese M. The 5'UTR variant of ERCC5 fails to influence outcomes in ovarian and lung cancer patients undergoing treatment with platinum-based drugs. Sci Rep. 2016;6:39217. doi: 10.1038/srep39217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sullivan I, Salazar J, Majem M, Pallarés C, Del Río E, Páez D, Baiget M, Barnadas A. Pharmacogenetics of the DNA repair pathways in advanced non-small cell lung cancer patients treated with platinum-based chemotherapy. Cancer Lett. 2014;353(2):160–166. doi: 10.1016/j.canlet.2014.07.023. [DOI] [PubMed] [Google Scholar]
- 37.Xu M, Liu Y, Li D, Wang X, Liang S, Zhang G, Yang X. Chinese C allele carriers of the ERCC5 rs1047768 polymorphism are more sensitive to platinum-based chemotherapy: a meta-analysis. Oncotarget. 2018;9(1):1248–1256. doi: 10.18632/oncotarget.18981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.He C, Duan Z, Li P, Xu Q, Yuan Y. Role of ERCC5 promoter polymorphisms in response to platinum-based chemotherapy in patients with advanced non-small-cell lung cancer. Anticancer Drugs. 2013;24(3):300–305. doi: 10.1097/CAD.0b013e32835bd6ce. [DOI] [PubMed] [Google Scholar]
- 39.Zhang T, Sun J, Lv M, Zhang L, Wang X, Ren JC, Wang B. XPG is predictive gene of clinical outcome in advanced non-small-cell lung cancer with platinum drug therapy. Asian Pac J Cancer Prev. 2013;14(2):701–705. doi: 10.7314/APJCP.2013.14.2.701. [DOI] [PubMed] [Google Scholar]