Abstract
Adhering to a healthy diet plays an essential role in preventing many nutrition-related diseases, such as obesity, diabetes, high blood pressure, and other cardiovascular diseases. This study aimed to predict adherence to the prescribed diets using a hybrid model of artificial neural networks (ANNs) and the genetic algorithm (GA). In this study, 26 factors affecting diet adherence were modeled using ANN and GA(ANGA). A dataset of 1528 patients, including 1116 females and 412 males, referred to a private clinic was applied. SPSS Ver.25 and MATLAB toolbox 2017 were employed to make the model and analyze the data. The results showed that the accuracy of the proposed ANN and ANGA models for predicting diet adherence was 93.22% and 93.51%, respectively. Also, the Pearson coefficient showed a significant relationship among the factors. The developed model showed the proper performance for predicting adherence to the diet. Moreover, the most effective factors were selected using GA. Some important factors that affect diet adherence include the duration of the marriage, the reason for referring to the clinic, weight, body mass index (BMI), weight satisfaction, lunch and dinner times, and sleep time. Therefore, applying the proposed model can help dietitians identify people who need more support to adhere to the diet.
Subject terms: Health care, Nutrition, Information technology
Introduction
A healthy diet includes a variety of foods and beverages that assist a person in maintaining a healthy weight, being healthy, and preventing diseases1,2. Diet is also an important aspect of lifestyle and personal habits that affect body composition and weight, as well as the prevention of obesity3,4. To prevent the complications and consequences of poor nutrition, in addition to choosing a healthy diet, it is necessary to pay attention to its continuity and adherence3,4,6. The concept of “adherence to diet” expresses the patient's right to choose whether or not to follow dietary recommendations and indicates the extent to which the patient actively engages in diet and treatment5. Many factors, such as culture and available food resources in the community, play a role in whether or not people adopt healthy diets6. In addition, food prices might be one of the barriers to choosing and adhering to a balanced diet, particularly among people with low income7. Therefore, these factors may force people to have an unhealthy diet despite their desire8. For example, Naalweh et al. found that adherence to diet and regimen therapy was less than the desired level in patients with dialysis, so 45% of them had low and moderate adherence to the recommended diets9. In contrast, a Nigerian cross-sectional survey showed that 67.4 percent of diabetic patients followed the diets10. Although the Mediterranean diet is consistently suggested as a healthy diet11–14, Daniela et al. discovered that adherence to the diet was low (16.7% of the participants aged 6–16 years).
Numerous factors, such as behavioral characteristics and lifestyle, may play a role in adherence to a diet15. A few additional factors, including age, ethnicity, place of residence, education, occupation, and smoking, were also discussed by Hatthachote et al.16. A similar study conducted in China evaluated the same parameters17. Another study indicated that the factors influencing adherence to diet were age, gender, education, physician–patient relationship, and social support10. In addition, understanding the relationship between adherence to a diet and patient education was also emphasized9.
As mentioned above, numerous studies have been conducted on a diet to prevent diseases and the factors affecting diet adherence9,10,15–23. However, these studies did not note intelligent algorithms such as neural networks and genetic algorithms to determine the influential factors in diet adherence.
Artificial neural networks have been utilized as auxiliary and standard models in classification, pattern recognition, and disease prediction24. Neural networks are comprised of input layers (to receive data from the user), output layers (to generate the desired responses), and hidden layers (processing layers)25. For example, neural networks have been used to predict people's weight after dietary interventions and following dietary recommendations26. Furthermore, by using machine learning methods such as KNN (K-nearest neighbors algorithm), it is possible to improve people's eating habits and ultimately control chronic diseases related to eating habits27.
Additionally, a genetic algorithm (GA) is an optimization and feature selection technique that can be utilized to identify relevant and effective elements28. This method generates a set of random solutions (individuals), where each has a different set of attributes (chromosomes). According to the rules of genetics, crossover and mutation are formed in chromosomes to develop the second generation of individuals with more diversified characteristics than the first. This procedure continues until the algorithm's termination condition is identified and satisfied. For example, It is possible to provide a subset of suitable factors for predicting diseases and nutrition-related problems when dealing with large data sets such as diet data29.
The importance of this study was the use of artificial intelligence in modeling behavioral patterns that may be effective in following the diet. These patterns assist dietitians in guiding patients to achieve their goals. Therefore, the present study aimed to find suitable factors to predict diet adherence using intelligent algorithms.
Methods
In this applied study, ANN and GA were employed to predict adherence to the diet based on lifestyle factors. Although this was not an interventional or clinical trial study, all methods were carried out under the relevant guidelines and regulations and the study protocol with the reference number of IR.AJUMS.REC.1399.437 was approved by the Ethics Committee of Ahvaz University of Medical Science as well as all methods were performed in accordance with the relevant guidelines and regulations.
The data were gathered under confidentiality and privacy rules from 1528 records of a nutrition and diet therapy clinic in Ahvaz (a metropolis located in the southwest of Iran) between 2017 and 2019. Inclusion criteria comprised the record of people referred to the clinic to gain or lose weight. The records of patients with diabetes, endocrine problems, and pregnant women were excluded from the study. Criteria for adhering to the diet were considered as follows: 1. following at least three sessions of diet therapy. 2. Gaining or losing (based on the goal) 5% of the initial weight within six months30,31.
Twenty-six predictor variables were selected to apply in the model, including age (years), gender (male/female), education (illiterate, primary school, middle, and high education), occupation (government employed, employed in the private sector, housewife, non-employed, etc.), marital status (single/ married), duration of being married (1–5 years, 15–30 years, 30–45 years, 45–60 years, over 60 years), the reason of referring to the clinic (losing weight due to overweight or obesity, and gaining weight due to thin or very thin), clients’ body image (obese, overweight, fit, thin and very thin), Weight, height, BMI (< 18.5 underweight, 18.5–24.9 normal, 25–29.9 overweight, and > = 30 obese), smoking, history of previous diet, weight satisfaction, history of obesity in childhood, Physical activity, having breakfast, the meal that consumes the most food, wake up time in the morning, breakfast time, lunch time, dinner time, Eating speed, sleeping time ( at night), being invited to a restaurant and party in a month, family (mother, father, sister, and brother) history of diabetes.
The variables were considered based on the literature and were selected based on availability in the patients' records. The Data were extracted from a questionnaire with 26 multiple-choice and short answer questions that patients filled out at the time of admission. Therefore, each question was measured as a variable of the model.
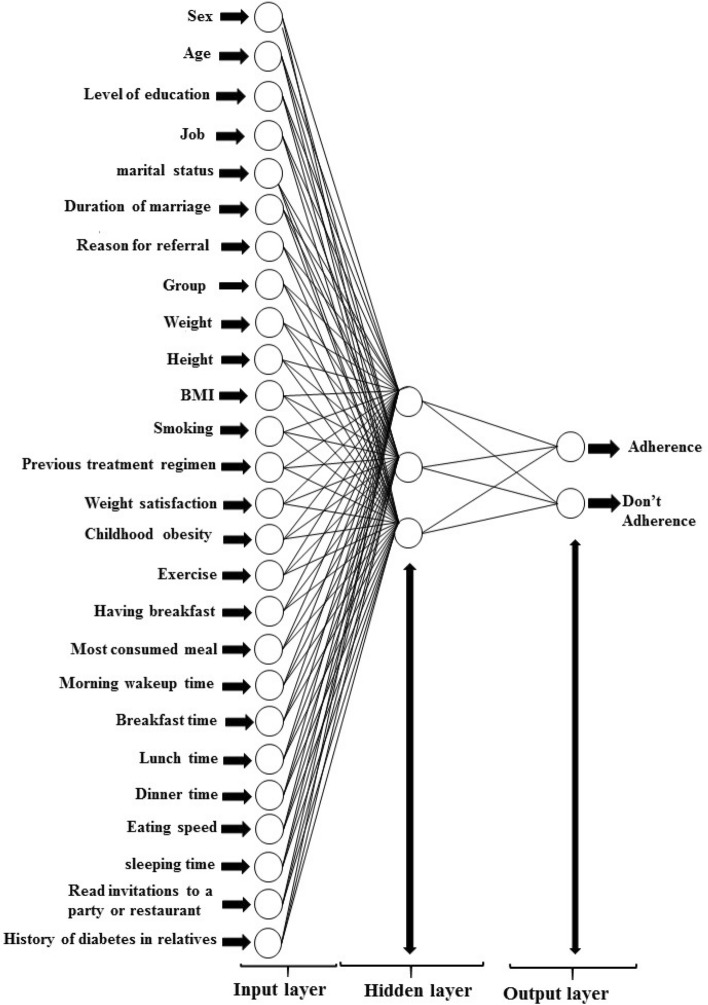
The current study used a feedforward net neural network of backpropagation as a classification algorithm of neural networks. After several experiments (it means several neural networks were performed to obtain the best results.), an optimized architecture including 26 input layers (number of variables of the study) and three hidden layers was generated. The number of hidden layers was usually determined based on the trial and error rule and the results’ accuracy. Therefore, the numerous hidden layers were selected, but the accuracy obtained from three hidden layers with [15 12 12] Neurons was the best. In addition, two output layers were selected based on the output results of the dependent variable. The output layers demonstrate if the individuals follow the diet or not. Therefore, the neural network model's accuracy can show the model's ability to predict diet adherence. It means that each patient, based on the questionnaire's response, was divided into one of two weight-changed and weight-not-changed groups by the model. The patients who gained the ideal weight and followed the diet belonged to the weight-changed group, and those who did not follow the diet and did not achieve the desired weight belonged to the weight-not-changed group. After entering the information of individuals in Matlab software, each group is assigned a number.
In this study, to continue the function training process, improve the results, and obtain optimal results in errors and weights, max_fail was considered zero. As a result, the data was divided into train and test data, with 85% and 15%, respectively. The model's sensitivity, specificity, and accuracy were calculated to measure the operating characteristics. Figure 1 depicts a sample of the neural network that was created. The trainbar (Bayesian regularization backpropagation) function was used to train the model, and the error was calculated using the Mean Squared Error (MSE) function. Also, the network was implemented using Matlab2017.
Figure 1.
Structure of the neural network for predicting diet adherence in the patients referring to the nutrition clinic.
The purpose of implementing the genetic algorithm in the study was to select a subset of the studied features with an unknown number of independent factors (26 in total) so that by choosing new factors, the MSE of the neural network is kept at a minimum, on the other hand, because the number of selected features affected the MSE, the number of selected features should also be minimized. Thus, the objective function was defined as Z = MSE + (1 + Brf). B is a coefficient of the number of selected features. The feature selection problem was coded using the Feature Selection function in conjunction with the neural network. The hybrid function was recalled as an input function of the GA to return the proper factor indices. With the selected factors as a new input in the neural network, the sensitivity, specificity, and accuracy of the neural network performance were calculated using confusion matrices compared to the neural network model with 26 inputs, which was used as a baseline. The flowchart (Fig. 2) depicts the procedure of GA implementation.
Figure 2.
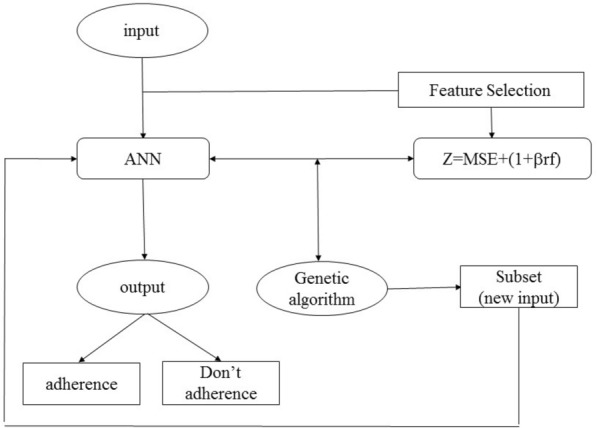
Implementation of GA for feature selection and developing proper factors for adherence to the diet.
The data were analyzed using SPSS, Version 25. The percentage and frequency of all variables were obtained first in the study. Then the Pearson / Spearman coefficient was used to show an association between the variables. The significant level was determined to be 0.05. Finally, the sensitivity, specificity, and accuracy were calculated to measure the model's characteristics.
Results
Table 1 shows that the proportion of females to males was 2.7. Most participants who followed the diets were 20 to 35 years. The education level of most participants was higher than the diploma, and only 1% were illiterate. More than half of the participants were unemployed, mainly homemakers or students. According to BMI data, more than half of the individuals were obese. In total, only 40 individuals had a history of smoking. The percentage of dissatisfaction with weight in the participants was 97.3 vs. 2.7. Only one-third of them had a history of childhood obesity. The proportion of the physical activity vs. those with no physical activity was 14.2 to 85.8, and more than half of the individuals had lunch.
Table 1.
Basic characteristics of the prediction of continuity in referral to nutrition for diet follow-up Data presented by (number (%)).
| Variables | Adherence to diet (n, %) |
Do not adherence to diet (n, %) |
Total (n, %) |
|
|---|---|---|---|---|
| Sex (N = 1528) | Male | 217 (27.0) | 195(26.9) | 412(27.0) |
| Female | 586 (73.0) | 530(73.1) | 1116(73.0) | |
| Age (N = 1528) | 5–20 | 86(10.7) | 102(14.1) | 188(12.3) |
| 20–35 | 387(48.2) | 351(48.4) | 738(43.8) | |
| 35–50 | 232(28.9) | 212(29.2) | 444(29.1) | |
| 50–65 | 90(11.2) | 53(7.3) | 143(9.4) | |
| 65–80 | 8(1.0) | 7(1.0) | 15(1.0) | |
| Level of education (N = 1528) | Literacy | 1(0.1) | 1(0.1) | 2(1.0) |
| Elementary | 22(2.7) | 27(3.7) | 49(3.2) | |
| High school | 109(13.6) | 99(13.7) | 208(13.6) | |
| Diploma | 223(27.8) | 160(22.1) | 383(25.1) | |
| Associate degree | 52(6.5) | 43(5.9) | 95(6.2) | |
| Bachelor's degree and higher | 396(49.3) | 395(54.5) | 791(51.8) | |
| Job (N = 1528) | Government jobs | 144(17.9) | 134(18.5) | 278(18.2) |
| Private jobs | 104(13.0) | 101(13.9) | 205(13.4) | |
| Educational jobs | 50(6.2) | 59(8.1) | 109(7.1) | |
| Therapeutic occupations | 18(2.2) | 22(3.0) | 40(2.6) | |
| Unemployed | 487(60.6) | 409(56.4) | 896(58.6) | |
| Marital status(N = 1528) | Married | 502(62.5) | 438(60.4) | 940(61.5) |
| Single | 301(37.5) | 287(39.6) | 588(38.5) | |
| Duration of marriage (year) | 0 | 301(37.5) | 287(36.6) | 588(38.5) |
| 1–15 | 275(34.2) | 292(40.3) | 567(37.1) | |
| 15–30 | 155(19.3) | 92(12.7) | 247(16.2) | |
| 30–45 | 65(8.1) | 47(6.5) | 112(7.3) | |
| 45–60 | 7(0.9) | 7(1.0) | 14(0.9) | |
| Reason for referral (N = 1528) | Diet modification | 9(1.1) | 10(1.4) | 19(1.2) |
| Gaining weight | 30(3.7) | 98(13.5) | 128(8.4) | |
| Fitness | 1(0.1) | 16(2.2) | 17(1.1) | |
| Weight Loss | 756(94.1) | 487(67.2) | 1243(81.3) | |
| High weight | 7(0.9) | 114(14.7) | 121(7.9) | |
| Group (N = 1528) | ||||
| From the patients' point of view | Overweight | 426(53.1) | 382(52.7) | 808(52.9) |
| Obese | 332(43.1) | 221(30.5) | 553(36.2) | |
| Very thin | 11(1.4) | 33(4.6) | 44(2.9) | |
| Thin | 20(2.5) | 64(8.8) | 84(5.5) | |
| Fit | 14(1.7) | 25(3.4) | 39(2.6) | |
| Weight (kg) | 23–65 | 45(5.6) | 124(17.1) | 169(11.1) |
| 63–103 | 571(71.1) | 484(66.8) | 1055(69.0) | |
| 103–143 | 172(21.4) | 110(15.2) | 282(18.2) | |
| ≥ 143 | 15(1.9) | 7(1.0) | 22(1.4) | |
| Height (centimeter) | 124–144 | 4(0.5) | 8(1.1) | 12(0.8) |
| 144–164 | 406(50.6) | 375(51.7) | 781(51.1) | |
| 164–183 | 371(46.2) | 329(45.4) | 700(45.8) | |
| ≥ 183 | 22(2.7) | 13(1.8) | 35(2.3) | |
| Underweight | 19(2.4) | 48(6.6) | 67(4.4) | |
| Normal weight | 34(4.2) | 81(11.2) | 115(7.5) | |
| Overweight | 160(19.9) | 184(25.4) | 344(22.5) | |
| Obese | 590(73.5) | 412(56.8) | 1002(65.6) | |
| Smoking (N = 1528) | Yes | 16(2.0) | 24(3.3) | 40(2.6) |
| No | 787(98.0) | 701(96.7) | 1488(97.4) | |
| Previous treatment regimen | Yes | 414(51.6) | 379(52.3) | 793(51.9) |
| No | 389(48.4) | 346(47.7) | 735(48.1) | |
| Weight satisfaction | Yes | 13(1.6) | 28(3.9) | 41(2.7) |
| No | 790(98.4) | 697(96.1) | 1487(97.3) | |
| Childhood obesity | Yes | 196(24.4) | 169(23.3) | 365(23.9) |
| No | 607(75.6) | 556(76.7) | 1163(76.1) | |
| Exercise | Yes | 100(12.5) | 117(16.1) | 217(14.2) |
| No | 703(87.5) | 608(83.9) | 1311(85.8) | |
| Having breakfast | Some days | 279(34.7) | 286(39.4) | 565(37.0) |
| Most days | 143(17.8) | 141(19.4) | 284(18.6) | |
| Everyday | 381(47.4) | 297(41.0) | 678(44.4) | |
| Never | 0(0) | 1(0.1) | 1(0.1) | |
| Most consumed meal | Breakfast | 50(6.2) | 49(6.8) | 99(6.5) |
| Lunch | 571(71.1) | 464(64.0) | 1035(67.7) | |
| Dinner | 114(14.2) | 140(19.3) | 254(16.6) | |
| Breakfast and Lunch | 10(1.2) | 11(1.5) | 21(1.4) | |
| Breakfast and Dinner | 2(0.2) | 2(0.3) | 4(0.3) | |
| Lunch and Dinner | 41(5.1) | 46(6.3) | 87(5.7) | |
| All three meals | 15(1.9) | 12(1.7) | 27(1.8) | |
| None | 0(0) | 1(0.1) | 1(0.1) | |
| Morning wake-up time | 3–8 | 365(45.5) | 287(39.6) | 652(42.7) |
| 8–13 | 425(52.9) | 413(57.0) | 838(54.8) | |
| 13–18 | 13(1.6) | 25(3.4) | 38(2.5) | |
| Breakfast time | 0 | 86(10.7) | 90(12.4) | 176(11.5) |
| 5.30–10 | 476(59.3) | 370(51.0) | 846(55.4) | |
| 10–14.30 | 241(30.0) | 265(36.6) | 506(33.1) | |
| Lunchtime | 0 | 5(0.6) | 2(0.3) | 7(0.5) |
| 11–15 | 623(77.6) | 518(71.4) | 1141(74.1) | |
| 15–19 | 175(21.8) | 205(28.3) | 380(24.9) | |
| Dinner time | 0 | 62(7.7) | 17(2.3) | 79(5.2) |
| 16–22 | 448(55.8) | 359(49.5) | 807(52.8) | |
| 22–3 | 293(36.5) | 349(48.1) | 642(42.0) | |
| Eating speed | Slow | 70(8.7) | 78(10.8) | 148(9.7) |
| Medium | 439(54.7) | 418(57.7) | 857(56.1) | |
| Fast | 294(36.6) | 229(31.6) | 523(34.2) | |
| sleeping time | 21–1 | 337(42.0) | 269(37.1) | 606(39.7) |
| 1–5 | 459(57.2) | 446(61.5) | 905(59.2) | |
| ≥ 5 | 7(0.9) | 10(1.4) | 17(1.1) | |
| Read invitations to a party or restaurant | Unknown | 5(0.6) | 1(0.1) | 6(0.4) |
| Never | 115(14.3) | 86(11.9) | 201(13.2) | |
| Rarely | 22(2.7) | 21(2.9) | 43(2.8) | |
| Few | 498(62.0) | 435(60.0) | 933(61.1) | |
| Much | 146(18.2) | 163(22.5) | 309(20.2) | |
| Very much | 17(2.1) | 19(2.6) | 36(2.4) | |
| History of diabetes in relatives | Yes | 478(59.5) | 441(68.8) | 919(60.1) |
| No | 325(40.5) | 284(39.2) | 609(39.9) | |
Table 2 demonstrates a significant relationship between the studied factors and diet adherence.
Table 2.
Association of independent variables and dependent variables using Pearson / Spearman coefficient.
| Variables | Adherence to diet or not | |
|---|---|---|
| Pearson / Spearman correlation | Sig(2-tailed) | |
| Sex (N = 1528) | 0.001 | 0.955 |
| Age (N = 1528) | 0.064* | 0.013 |
| Level of education (N = 1528) | − 0.036 | 0.156 |
| Job (N = 1528) | 0.029 | 0.251 |
| marital status(N = 510) | 0.022 | 0.399 |
| Duration of marriage (year) | 0.061* | 0.018 |
| Reason for referral (N = 504) | 0.052* | 0.040 |
|
Group (N = 503) From the patients’ point of view |
− 0.125** | < 0.001 |
| Weight (kg) | 0.167** | < 0.001 |
| Height (centimeter) | 0.030 | 0.246 |
| BMI (N = 504) | 0.197** | < 0.001 |
| Smoking (N = 504) | 0.041 | 0.107 |
| Previous treatment regimen | 0.007 | 0.779 |
| Weight satisfaction | 0.069** | 0.007 |
| Childhood obesity | − 0.013 | 0.615 |
| Exercise | 0.053* | 0.039 |
| Having breakfast | 0.061* | 0.018 |
| Most consumed meal | − 0.041 | 0.111 |
| Morning wake up time | 0.071** | 0.005 |
| Breakfast time | − 0.038 | 0.136 |
| Lunchtime | − 0.077** | 0.002 |
| Dinner time | − 0.147** | < 0.001 |
| Eating speed | 0.057* | 0.025 |
| Sleeping time | − 0.053* | 0.039 |
| Read invitations to a party or restaurant | − 0.061* | 0.017 |
| History of diabetes in relatives | 0.013 | 0.604 |
*Correlation is significant at the 0.05 level (2-tailed).
**Correlation is significant at the 0.01 level (2-tailed).
The relationship among factors like age, duration of the marriage, the reason for referring to the nutrition clinic, physical activity, breakfast time, eating speed, sleeping time, being invited to parties and restaurants, and diet adherence was borderline statistically significant (p > 0.05).
Factors like group, weight, BMI, satisfaction, wake-up time, breakfast, lunch, and dinner time were strongly correlated with diet adherence (p > 0.01).
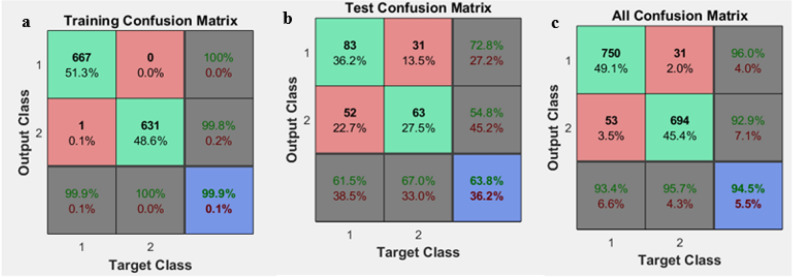
After 20 times of implementing the model, the average accuracy, sensitivity, and specificity are calculated based on the confusion matrix and compared with the hybrid neural network and GA model, where its results are given in Table 3. Also, Fig. 3 shows a snapshot of the confusion matrix obtained from the neural network implementation.
Table 3.
The results obtained from implementing the neural network before and after feature selection using GA.
| Model | Sensitivity (%) | Specificity (%) | Accuracy (%) | |
|---|---|---|---|---|
|
Before Applying GA |
ANN (train) | 99.39 | 99.57 | 99.47 |
| ANN (test) | 61.80 | 53.44 | 57.90 | |
| ANN (Total) | 93.82 | 92.60 | 93.22 | |
|
After Applying GA |
ANN (train) | 98.63 | 99.21 | 98.92 |
| ANN (test) | 61.39 | 56.09 | 59 | |
| ANN (Total) | 93.09 | 92.71 | 93.51 |
Figure 3.
An example of confusion matrices after network implementation in traing (a) test (b) and all confusion (c).
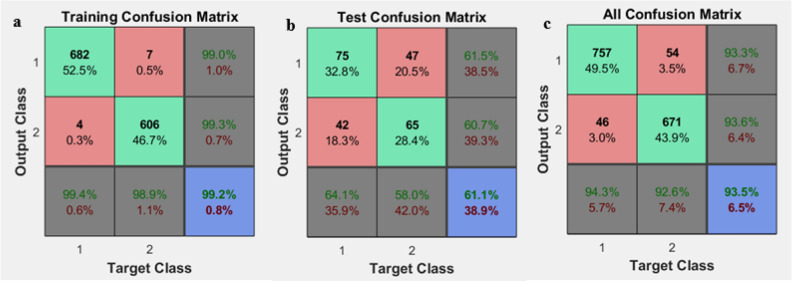
GA was implemented to select proper factors in diet adherence. Due to the importance of adjusting the beta coefficient in selecting appropriate factors, beta = 0.52 was obtained to determine the suitable variables. Also, in this method, the number of iterations was 50. In this method, the initial population was 30, crossover = 0.8, and the number of offspring in each generation was calculated using the following equation:
where, nc is the number of offspring in each generation, pc is the crossover percentage, and npop is the initial population. A comparable confusion matrix associated with sensitivity, specificity, and accuracy of the GA after integration with the neural network is shown in Fig. 4. In addition, a diagram of the GA's best accuracy in selecting the features affecting diet is shown in Fig. 5. The results of implementing GA showed that 15 relevant factors could be chosen to predict the continuity of the diet. The index number of these factors is shown in Fig. 6. The name of these factors is also given in Table 4.
Figure 4.
An example of confusion matrices after GA implementation in integration with ANN for selecting the effective factors. Training confusion (a). Test confusion (b) and all confusion (c).
Figure 5.
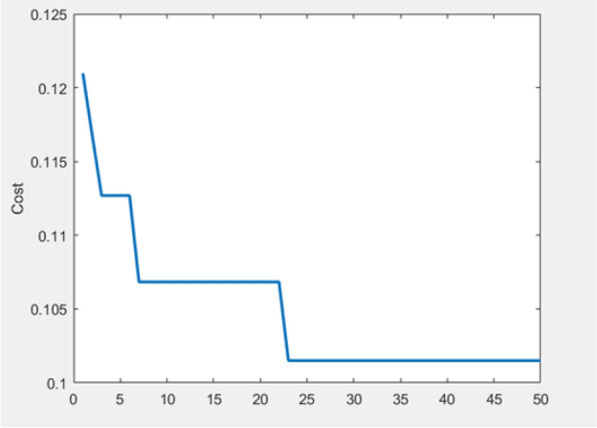
Accuracy of GA in selecting proper factors after 50 iterations.
Figure 6.
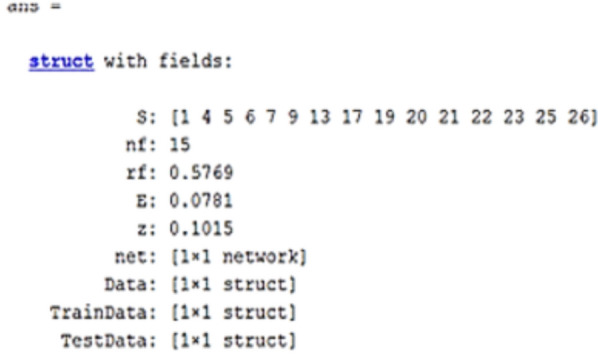
Result of implementing GA for selecting 15 effective factors in diet adherence.
Table 4.
The result of performing feature selection using a genetic algorithm.
| Age | 1 |
| Job | 4 |
| Marital status | 5 |
| Duration of marriage | 6 |
| Reason for referral | 7 |
| Weight | 9 |
| Previous treatment regimen | 13 |
| Having breakfast | 17 |
| Morning wake-up time | 19 |
| Breakfast time | 20 |
| Lunchtime | 21 |
| Dinner time | 22 |
| Sleeping time | 23 |
| Read invitations to a party or restaurant | 25 |
| History of diabetes in relatives | 26 |
Discussion
A healthy diet containing essential vitamins effectively preserves health and prevents diseases32. Also, avoiding high-risk factors like smoking and low physical activity26 might affect a healthy weight and life33. In addition, lifestyle changes might affect improper diet adoption34,35. The results showed that various factors affect diet adherence. For example, those who were overweight or underweight had a more regular continuation of their diet. Also, the study found that individuals who ate their lunch and dinner at the appropriate times of the day were more successful at sticking to their diet. Some studies showed that these factors could affect nutritional status. For example, Akbarzade et al. discovered that the volume and composition of the midday meal could impact obesity36. Therefore, having lunch at the wrong time will be a predisposing factor for obesity and overweight.
Furthermore, this study showed that adherence to the diet was almost equally low in both sexes, and people with a high school diploma and associated degree were more likely to adhere to the diet. Similarly, the study conducted by Morge et al. discovered that females and adults with higher education levels showed better adherence to self-care behaviors such as nutrition, exercise, and other activities10. In addition, the results showed that being employed could be a factor in predicting diet adherence. These results were expected because employed people have a more adjusted daily schedule than non-employed people.
Although a study in Spain showed that physical activity was effective in following the Mediterranean diet37, the results showed that most participants did not report exercise and physical activity. It may be due to the coronavirus and the lockdown38. Moreover, in line with the results of the present study, some studies showed that weight satisfaction39 was a significant factor in people's adherence to a diet and that individuals who were dissatisfied with their weight followed a healthier diet40. For instance, according to a study conducted in Georgia, body satisfaction was found to have a relationship with diet adherence. This was especially true in adolescent girls with inflammatory bowel disease, where body dissatisfaction was higher and diet adherence was lower41. In addition, the results showed that the participants who received many invitations to restaurants were less likely to follow their diet. This may be due to high-calorie, and unhealthy foods served in restaurants.
Furthermore, the results revealed that having a regular life plan, such as waking up in the morning at the appropriate time, going to bed at the proper time, and eating breakfast properly, were effective variables in adhering to the diet. The results of the GA model also indicated a significant relationship between the factors and adherence to the diet. To the best of our knowledge, most studies related to diet adherence have focused on the effects of lifestyle on obesity and overweight35,42,43. However, no study has been observed on diet adherence using intelligent methods. Although intelligent approaches such as neural networks and genetic algorithms have been utilized in many studies, no evidence has been found about diet adherence. Like the present study's intelligent method, Eduardo et al. applied an intelligent model using the MLP neural network to predict the duration and dietary changes. They implemented the model on a dataset of 105 different diets44. Although the present study showed that several factors could play a role in diet adherence, it did not define a suitable way to measure the degree of adherence to a proper diet. However, a study showed that awareness of a healthy diet did not improve adherence to the diet45.
There were several limitations in this study. First, Due to the lack of a standard, the data were collected only from the patient records of a diet clinic instead of several clinics. Second, comparing the model's accuracy with other studies was impossible since similar studies were not found. Third, whereas this study was limited to the factors obtained from the patient record, in addition to the 26 behavioral factors applied, perhaps other factors were not included in the model. Fifth, although different types of neural networks such as CNN have been used in android based applications, which have provided advice about measuring food calories46, a study that uses intelligent methods to predict adherence to diet has not been found.
Conclusion
The results showed that diet adherence was significantly associated with various factors such as lifestyle, waking up early in the morning, and eating breakfast, lunch, and dinner at appropriate times. This study also showed that the proposed model using artificial neural networks had reasonable accuracy for predicting diet adherence. Also, using GA and integrating it with the neural network can increase the model's accuracy.
Applying this model can help dietitians identify patients with a low chance of diet adherence. They can employ appropriate methods such as supportive methods, for example, social networking46, to increase the likelihood of diet adherence and improve the effectiveness of the diet. In addition, further studies are needed to determine other factors that may affect diet adherence and provide a more comprehensive model.
Supplementary Information
Acknowledgements
This research was approved by Nutrition and Metabolic Diseases Research Center, Clinical Sciences Research Institute, Ahvaz Jundishapur University of Medical Sciences (AJUMS), Ahvaz, Iran, as a master's thesis (Hediye Mousavi) with no. NRC-9902.
Author contributions
Authors’ contributions: A.H. and H.M. conceived of the idea. M.K. and A.J. developed and designed the study. H.M. and M.K. performed the experiments and collected data. A.H. and A.J. analyzed the data. M.K. verified the results. All authors discussed the results. H.M. wrote the first draft with contributions from A.H., and All authors reviewed and commented on the manuscript, as well as all are responsible for the content of the manuscript.
Data availability
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-022-16680-8.
References
- 1.Nelson ME, Hamm MW, Hu FB, Abrams SA, Griffin TS. Alignment of healthy dietary patterns and environmental sustainability: A systematic review. Adv. Nutr. (Bethesda, Md). 2016;7(6):1005–1025. doi: 10.3945/an.116.012567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Force UPST. Behavioral counseling interventions to promote a healthy diet and physical activity for cardiovascular disease prevention in adults with cardiovascular risk factors: US preventive services task force recommendation statement. JAMA. 2020;324(20):2069–2075. doi: 10.1001/jama.2020.21749. [DOI] [PubMed] [Google Scholar]
- 3.Sarkhosh-Khorasani S, Mozaffari-Khosravi H, Mirzaei M, Nadjarzadeh A, Hosseinzadeh M. Empirically derived dietary patterns and obesity among Iranian adults: Yazd health study-TAMYZ and Shahedieh cohort study. Food Sci. Nutr. 2020;8(5):2478–2489. doi: 10.1002/fsn3.1538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sarkhosh-Khorasani, S., Mozaffari-Khosravi, H., Mirzaei, M., Nadjarzadeh, A., Hosseinzadeh, M. Dietary approach to stop hypertension and obesity among Iranian adults: Yazd health study-TAMYZ and Shahedieh Cohort 1–21 (2021). [DOI] [PMC free article] [PubMed]
- 5.Desroches S, Lapointe A, Ratté S, Gravel K, Légaré F, Turcotte S. Interventions to enhance adherence to dietary advice for preventing and managing chronic diseases in adults. Cochrane Database Syst. Rev. 2013;2:1–134. doi: 10.1002/14651858.CD008722.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kanerva N, Harald K, Männistö S, Kaartinen NE, Maukonen M, Haukkala A, et al. Adherence to the healthy Nordic diet is associated with weight change during 7 years of follow-up. Br. J. Nutr. 2018;120(1):101–110. doi: 10.1017/S0007114518001344. [DOI] [PubMed] [Google Scholar]
- 7.Pastor R, Pinilla N, Tur JA. The economic cost of diet and its association with adherence to the mediterranean diet in a cohort of Spanish primary schoolchildren. Int. J. Environ. Res. Public Health. 2021;18(3):1282–1292. doi: 10.3390/ijerph18031282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tong TY, Imamura F, Monsivais P, Brage S, Griffin SJ, Wareham NJ, et al. Dietary cost associated with adherence to the Mediterranean diet, and its variation by socio-economic factors in the UK Fenland Study. Br. J. Nutr. 2018;119(6):685–694. doi: 10.1017/S0007114517003993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Naalweh KS, Barakat MA, Sweileh MW, Al-Jabi SW, Sweileh WM, Zyoud Se H. Treatment adherence and perception in patients on maintenance hemodialysis: A cross—sectional study from Palestine. BMC Nephrol. 2017;18(1):1–9. doi: 10.1186/s12882-017-0598-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mogre V, Abanga ZO, Tzelepis F, Johnson NA, Paul C. Adherence to and factors associated with self-care behaviours in type 2 diabetes patients in Ghana. BMC Endocr. Disord. 2017;17(1):1–8. doi: 10.1186/s12902-017-0169-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Godos J, Ferri R, Caraci F, Cosentino FII, Castellano S, Galvano F, et al. Adherence to the mediterranean diet is associated with better sleep quality in Italian adults. Nutrients. 2019;11(5):1–15. doi: 10.3390/nu11050976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Garcia-Mantrana I, Selma-Royo M, Alcantara C, Collado MC. Shifts on gut microbiota associated to mediterranean diet adherence and specific dietary intakes on general adult population. Front. Microbiol. 2018;9(890):1–11. doi: 10.3389/fmicb.2018.00890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arcila-Agudelo AM, Ferrer-Svoboda C, Torres-Fernàndez T, Farran-Codina A. Determinants of adherence to healthy eating patterns in a population of children and adolescents: Evidence on the mediterranean diet in the city of Mataró (Catalonia, Spain) Nutrients. 2019;11(4):1–13. doi: 10.3390/nu11040854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Agnoli C, Sieri S, Ricceri F, Giraudo MT, Masala G, Assedi M, et al. Adherence to a Mediterranean diet and long-term changes in weight and waist circumference in the EPIC-Italy cohort. Nutr. Diabetes. 2018;8(1):1–10. doi: 10.1038/s41387-018-0023-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cavaliere A, De Marchi E, Banterle A. Exploring the adherence to the mediterranean diet and its relationship with individual lifestyle: The role of healthy behaviors, pro-environmental behaviors, income, and education. Nutrients. 2018;10(2):141. doi: 10.3390/nu10020141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hatthachote P, Rangsin R, Mungthin M, Sakboonyarat B. Trends in the Prevalence of obesity among young Thai men and associated factors: from 2009 to 2016. Mil. Med. Res. 2019;6(1):1–8. doi: 10.18502/rmm.v6i1.3919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.He Y, Pan A, Wang Y, Yang Y, Xu J, Zhang Y, et al. Prevalence of overweight and obesity in 158 million men aged 15–49 years in rural China from 2010 to 2014. Sci. Rep. 2017;7(1):1–10. doi: 10.1038/s41598-016-0028-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saber SS, Hassan MT, Ismael SA. Dietary habits among type 2 diabetic patients in Erbil City. J. Kurd. Board Med. Spec. 2020;6(1):43–49. [Google Scholar]
- 19.Nouri M, Tarighat-Esfanjani A, Ghazizahedi S. The relationships between dietary patterns and energy and nutrient intakes and body mass index in Iranian adults. J. Health. 2017;8(1):85–101. [Google Scholar]
- 20.Mohebbi B, Tafaghodi B, Sadeghi R, Tol A, Yekanenejad M. Factors predicting nutritional knowledge, illness perceptions, and dietary adherence among hypertensive middle-aged women: Application of transtheoretical model. J. Educ. Health Promot. 2021;10(1):1–7. doi: 10.4103/jehp.jehp_1343_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mohammed MA, Sharew NT. Adherence to dietary recommendation and associated factors among diabetic patients in Ethiopian teaching hospitals. Pan. Afr. Med. J. 2019;33(260):1–11. doi: 10.11604/pamj.2019.33.260.14463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kroeger CM, Trepanowski JF, Klempel MC, Barnosky A, Bhutani S, Gabel K, et al. Eating behavior traits of successful weight losers during 12 months of alternate-day fasting: An exploratory analysis of a randomized controlled trial. Nutr. Health. 2018;24(1):5–10. doi: 10.1177/0260106017753487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim B-Y, Choi D-H, Jung C-H, Kang S-K, Mok J-O, Kim C-H. Obesity and physical activity. J. Obes. Metab. Syndr. 2017;26(1):15–22. doi: 10.7570/jomes.2017.26.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Abiodun OI, Jantan A, Omolara AE, Dada KV, Mohamed NA, Arshad H. State-of-the-art in artificial neural network applications: A survey. Heliyon. 2018;4(11):1–41. doi: 10.1016/j.heliyon.2018.e00938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nasser IM, Abu-Naser SS. Predicting tumor category using artificial neural networks. Int. J. Acad. Health Med. Res. (IJAHMR) 2019;3(2):1–7. [Google Scholar]
- 26.Babajide, O., Hissam, T., Anna, P., Anatoliy, G., Astrup, A., Alfredo Martinez, J., & Sørensen, T. I. A machine learning approach to short-term body weight prediction in a dietary intervention program. In International Conference on Computational Science 441-455 (Springer, Cham, 2020).
- 27.Baek J-W, Kim J-C, Chun J, Chung K. Hybrid clustering based health decision-making for improving dietary habits. Technol. Health Care. 2019;27(5):459–472. doi: 10.3233/THC-191730. [DOI] [PubMed] [Google Scholar]
- 28.Aalaei S, Shahraki H, Rowhanimanesh A, Eslami S. Feature selection using genetic algorithm for breast cancer diagnosis: Experiment on three different datasets. Iran. J. Basic Med. Sci. 2016;19(5):476–482. [PMC free article] [PubMed] [Google Scholar]
- 29.Morgenstern JD, Rosella LC, Costa AP, de Souza RJ, Anderson LN. Perspective: Big data and machine learning could help advance nutritional epidemiology. Adv. Nutr. 2021;12(3):621–631. doi: 10.1093/advances/nmaa183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Painter SL, Ahmed R, Kushner RF, Hill JO, Lindquist R, Brunning S, et al. Expert coaching in weight loss: Retrospective analysis. J. Med. Internet Res. 2018;20(3):1–12. doi: 10.2196/jmir.9738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Carney D, Schultz S, Lim J, Walters W. Successful medical weight loss in a community setting. J. Obes. Weight Loss Ther. 2015;5(1):1–10. doi: 10.4172/2165-7904.1000248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Akbarzade Z, Amini MR, Djafari F, Yarizadeh H, Mohtashaminia F, Majdi M, et al. Association of nutrient patterns with metabolic syndrome and its components in Iranian adults. Clin. Nutr. Res. 2020;9(4):318. doi: 10.7762/cnr.2020.9.4.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bertoni N, de Almeida LM, Szklo M, Figueiredo VC, Szklo AS. Assessing the relationship between smoking and abdominal obesity in a national survey of adolescents in Brazil. Prev. Med. 2018;111:1–5. doi: 10.1016/j.ypmed.2018.02.017. [DOI] [PubMed] [Google Scholar]
- 34.Lv J, Yu C, Guo Y, Bian Z, Yang L, Chen Y, et al. Adherence to Healthy lifestyle and cardiovascular diseases in the Chinese population. J. Am. Coll. Cardiol. 2017;69(9):1116–1125. doi: 10.1016/j.jacc.2016.11.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kopp W. How western diet and lifestyle drive the pandemic of obesity and civilization diseases. Diabetes, Metab. Syndr. Obes.: Targ. Ther. 2019;12:2221–2236. doi: 10.2147/DMSO.S216791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Akbarzade Z, Djafarian K, Saeidifard NN, Majd SA, Garousi N, Samadi F, Shab-Bidar S. The association between lunch composition and obesity in Iranian adults. Br. J. Nutr. 2021;127(10):1517–1527. doi: 10.1017/S0007114521002543. [DOI] [PubMed] [Google Scholar]
- 37.Zaragoza-Martí A, Ferrer-Cascales R, Hurtado-Sánchez JA, Laguna-Pérez A, Cabañero-Martínez MJ. Relationship between adherence to the Mediterranean diet and health-related quality of life and life satisfaction among older adults. J. Nutr. Health Aging. 2018;22(1):89–96. doi: 10.1007/s12603-017-0923-2. [DOI] [PubMed] [Google Scholar]
- 38.Lukács A. The impact of physical activity on psychological well-being and perceived health status during coronavirus pandemic in university students. J. King Saud Univ.-Sci. 2021;33(6):101531. doi: 10.1016/j.jksus.2021.101531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Xu F, Cohen SA, Greaney ML, Greene GW. The association between US adolescents’ weight status, weight perception, weight satisfaction, and their physical activity and dietary behaviors. Int. J. Environ. Res. Public Health. 2018;15(9):1931. doi: 10.3390/ijerph15091931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bahreynian M, Qorbani M, Motlagh ME, Heshmat R, Ardalan G, Kelishadi R. Association of perceived weight status versus body mass index on adherence to weight-modifying plan among Iranian children and adolescents: The CASPIAN-IV study. Indian Pediatr. 2015;52(10):857–863. doi: 10.1007/s13312-015-0732-9. [DOI] [PubMed] [Google Scholar]
- 41.Vlahou CH, Cohen LL, Woods AM, Lewis JD, Gold BD. Age and body satisfaction predict diet adherence in adolescents with inflammatory bowel disease. J. Clin. Psychol. Med. Settings. 2008;15(4):278–286. doi: 10.1007/s10880-008-9125-8. [DOI] [PubMed] [Google Scholar]
- 42.Shamsi SA, Salehzadeh M, Ghavami H, Asl RG, Vatani KK. Impact of lifestyle interventions on reducing dietary sodium intake and blood pressure in patients with hypertension: A randomized controlled trial. Turk. Kardiyol Dern. Ars. 2021;49(2):143–150. doi: 10.5543/tkda.2021.81669. [DOI] [PubMed] [Google Scholar]
- 43.Bondyra-Wiśniewska B, Myszkowska-Ryciak J, Harton A. Impact of lifestyle intervention programs for children and adolescents with overweight or obesity on body weight and selected cardiometabolic factors—A systematic review. Int. J. Environ. Res. Public Health. 2021;18(4):1–25. doi: 10.3390/ijerph18042061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brugnago EL, Hild TA, Weingärtner D, Beims MW. Classification strategies in machine learning techniques predicting regime changes and durations in the Lorenz system. Chaos: Interdiscip. J. Nonlinear Sci. 2020;30(5):1–7. doi: 10.1063/5.0003892. [DOI] [PubMed] [Google Scholar]
- 45.Sajwani RA, Shoukat S, Raza R, Shiekh MM, Rashid Q, Siddique MS, et al. Knowledge and practice of healthy lifestyle and dietary habits in medical and non-medical students of Karachi, Pakistan. J. Pak. Med. Assoc. 2009;59(9):650. [PubMed] [Google Scholar]
- 46.Tahmasebi R, Karandish M, Hadianfard AM. The effect of integrating online social networks into routine diet therapy on session follow-up in overweight and obese adults: a randomized controlled trial. Health Manag. Inf. Sci. 2021;8(4):235–241. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are included in this published article and its supplementary information files.