Abstract
Purpose
Literature is scarce regarding cancer care utilization during the massive outbreak of coronavirus disease 2019 (COVID-19) in the Republic of Korea. We investigated functional impairments in mental health and their relationships with depression, anxiety regarding the viral epidemic, and disruptions in healthcare service utilization among cancer patients in the COVID-19 pandemic era.
Materials and Methods
We used an online survey with questions related to the disturbances faced by patients with cancer in utilizing healthcare services in the pandemic era. Current mental health status was assessed using the Work and Social Adjustment Scale (WSAS), Stress and Anxiety to Viral Epidemics-6 (SAVE-6) scale, Patient Health Questionnaire-9 (PHQ-9), Insomnia Severity Index (ISI), Brief Resilience Scale (BRS), Cancer-Related Dysfunctional Beliefs about Sleep Scale (C-DBS), and Fear of COVID-19 over Cancer (FCC).
Results
Among the 221 responders, 95 (43.0%) reported disruptions in healthcare service utilization during the COVID-19 pandemic. Logistic regression analysis revealed that functional impairment in the mental health of these patients was expected due to disruptions in healthcare service utilization, high levels of depression, anxiety regarding the viral epidemic, fear of COVID over cancer, and low resilience. Mediation analysis showed that patient resilience and cancer-related dysfunctional beliefs about sleep partially mediated the effects of viral anxiety on functional impairment.
Conclusion
In this pandemic era, patients with cancer experience depression, anxiety regarding the viral epidemic, and disruptions in healthcare service utilization, which may influence their functional impairments in mental health.
Keywords: COVID-19, Pandemics, Cancer care facilities, Anxiety, Depression
Introduction
Coronaviruses are RNA viruses that are known to infect various species of hosts including humans and mainly cause respiratory and gastrointestinal disorders. The 21st century saw two outbreaks of coronavirus infection caused by viral mutations; namely, severe acute respiratory syndrome and Middle East respiratory syndrome [1]. In December 2019, another novel coronavirus emerged in Wuhan, China, which was highly contagious and pathogenic, resulting in a cluster of pneumonia cases [2]. The disease caused by the virus was named coronavirus disease 2019 (COVID-19) and spread rapidly worldwide, leading to its declaration as a global pandemic by the World Health Organization (WHO). Although the WHO launched the “Solidarity” clinical trial to develop treatments and vaccines for COVID-19, research in this area has been challenging.
In the era of the COVID-19 pandemic, cancer care utilization is changing rapidly due to the shortage of medical personnel, hospital beds, and personal protective equipment (e.g., masks, gowns, and gloves). Moreover, both patients and medical staff need to ensure social distancing to prevent the spread of viral infection. For cancer patients, the direct consequences of treatment delay or non-adherence are later-stage diagnosis or stage shift, which are of utmost importance among clinician precautions [3]. These predicaments have emerged in the care of patients with cancer, resulting in the deterioration of cancer treatment while the benefit of cancer therapy is left as it was. Therefore, patients with cancer are experiencing high rates of psychiatric problems such as depression, anxiety, post-traumatic stress disorder, insomnia, and impulsivity [4].
The main strategies for cancer treatment should include the prevention of COVID-19. The risks and benefits of active interventions in the cancer population must be considered individually. Treatment modalities such as chemotherapy and elective surgery could be delayed in patients at low risk for disease progression. Minimizing the number of outpatient visits by utilizing telemedicine can help prevent potential viral exposure [5]. Recent articles suggest that the strategy of parsimonious radiation therapy such as short-course radiation therapy could be a reasonable clinical approach to alleviate the clinical burden and protect cancer patients at risk of viral infection [6,7]. Expert opinions from the Society of Surgical Oncology require clinicians to triage their cancer patients by medical urgency and defer surgery accordingly. Although there are some differences among cancer types and stages, cancer surgery could be deferred for at least 3 months or more, if possible. For instance, maximizing neoadjuvant chemotherapy is recommended as an alternative option for limiting surgical procedures [8].
In this context, we investigated the functional impairments in mental health and explored their relationships with depression, anxiety regarding the viral epidemic, and disruption in healthcare service utilization among cancer patients in this COVID-19 pandemic era.
Materials and Methods
1. Patients and study design
This online survey study was carried out between July 15 and August 15, 2020, at Asan Medical Center, Seoul, Korea. The survey contained questions on the disturbances experienced by patients with cancer in utilizing medical facilities in the pandemic era. Data on the subjects’ age, sex, marital status, cancer type, current treatment modalities, cancer stages according to the subjects’ knowledge, psychiatric history, and current psychiatric symptoms were also collected via the online survey. The responders were provided an e-gift coupon valued at approximately $3.
2. Rating scales
(1) Stress and Anxiety to Viral Epidemics-6
The Stress and Anxiety to Viral Epidemics-6 (SAVE-6) is an anxiety subcategory of the SAVE-9 scale [9]. The SAVE-6 consists of six items scored on a five-point scale ranging from 0 (never) to 4 (always) based on responders’ self-evaluations. The cut-off score was 15 based on the least mild degree (≥ 5 points) on the General Anxiety Scale-7 (GAD-7) [10].
(2) Patient Health Questionnaire-9
The Patient Health Questionnaire-9 (PHQ-9) was developed to assess depressive symptoms. This self-administered scale consists of nine items scored on a three-point scale ranging from 0 (not at all) to 3 (nearly every day) [11]. The total score of the PHQ-9 ranges from 0 to 27, with a higher score indicating severe depressive symptoms. In this study, we defined a cut-off score of 10 for clinical depression.
(3) Insomnia Severity Index
The Insomnia Severity Index (ISI) includes seven self-reported questions that evaluate difficulty in falling asleep and staying asleep, problems with waking too early, sleep satisfaction, interference in daily functions and awareness of impairments due to sleep problems, and distress from sleep disturbance [12]. Each item is scored with points ranging between 0 (no problem) and 4 (very severe problem), with a total possible score of 28. A higher ISI score indicates greater insomnia severity while a score below 8 indicates no clinically significant insomnia or remission after insomnia treatment [13].
(4) Brief Resilience Scale
The Brief Resilience Scale (BRS) was developed to assess resilience, i.e., the ability to recover from stress [14]. It consists of six self-administered questionnaires, with point scores ranging from 1 to 5 for a total possible score of 30. The BRS score is calculated as the total sum divided by the total number of questions answered. We used the previously developed Korean version of the BRS.
(5) Cancer-Related Dysfunctional Beliefs about Sleep Scale
The Cancer-Related Dysfunctional Beliefs about Sleep Scale (C-DBS) is a two-item rating scale developed to evaluate dysfunctional beliefs about sleep in patients with cancer [15]. The two items are “My immune system will have serious problems if I don’t go to sleep at a certain time” (question 1, immune dysfunction) and “If I don’t sleep well at night, my cancer may recur or metastasize” (question 2, cancer recurrence). Each item is rated on a scale from 0 (strongly disagree) to 10 (strongly agree).
(6) Work and Social Adjustment Scale
The Work and Social Adjustment Scale (WSAS) is a self-reported five-item scale that evaluates impairment in daily functions caused by mental health problems. It assesses abilities in performing work, home management, interpersonal relationships, and leisure activities. Each item is scored between 0 (not at all) and 8 (very severely) [16]. Total WSAS scores above 10 and 21 indicate meaningful and severe functional impairments, respectively.
(7) Fear of COVID-19 over cancer
The question “Are you more afraid of coronavirus than cancer?” was designed for this study to assess the fear of COVID over cancer among patients with cancer. The patients were asked to answer this question using a number from 0 to 10, with a higher score indicating a higher fear of COVID-19 than cancer.
3. Statistical analysis
Statistical analyses were conducted using IBM SPSS Statistics for Windows ver. 21.0 (IBM Corp., Armonk, NY). Clinical characteristics were summarized as mean±standard deviation. The level of significance for all analyses was defined as two-tailed p-values < 0.05. We performed Student’s t tests for continuous variables and chi-squared tests for categorical variables for between-group analyses. Spearman correlation analysis was conducted to assess the relationships between clinical characteristics and mental health symptoms. Logistic regression analysis was performed to explore the expected factors related to patients’ functional impairment of mental health during the COVID-19 pandemic. Finally, to explore the mediating effect of resilience on the relationship of depression with functional impairment, the bootstrap method with 2,000 resamples was implemented.
Results
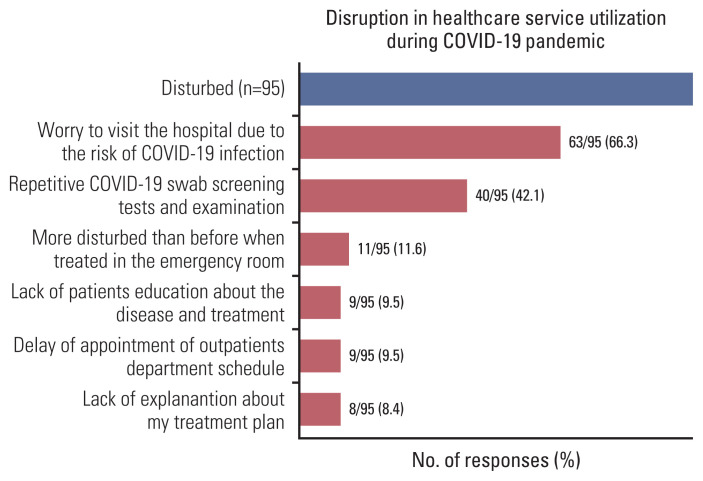
Among the 221 responders, 104 (47.1%) reported functional impairments in mental health (WSAS ≥ 11) and 95 (43.0%) reported having experienced disturbances in healthcare service utilization during the COVID-19 pandemic (Table 1, Fig. 1). The responders’ cancer types included breast (n=89, 40.3%), colorectal (n=23, 10.4%), gastro-esophageal (n=18, 8.1%), thoracic (n=15, 6.8%), pancreatobiliary (n=11, 5.0%), central nervous system, head and neck (n=10, 4.5%), hematologic (n=9, 4.1%), liver (n=8, 3.6%), genitourinary (n=11, 5.0%), gynecologic (n=6, 2.7%), thyroid (n=4, 1.8%), and others including double primary (n=17, 7.7%).
Table 1.
Clinical characteristics of the study subjects (n=221)
| Variable | WSAS < 11 (n=117) | WSAS ≥ 11 (n=104) | p-value |
|---|---|---|---|
| Female sex | 84 (71.8) | 84 (80.8) | 0.10 |
| Age (yr) | 50.8±12.1 | 49.3±14.6 | 0.40 |
| Marital status, married | 99 (84.6) | 79 (76.0) | 0.10 |
| Duration of illness from cancer diagnosis (yr) | 3.5±3.7 | 3.0±3.3 | 0.34 |
| Cancer type | |||
| Breast | 47 (40.2) | 42 (40.4) | 0.42 |
| Gastro-intestinal and pancreato-biliary | 30 (25.6) | 22 (21.2) | |
| Other | 40 (34.2) | 40 (38.5) | |
| Cancer stage | |||
| 0, I, II, III | 72 (61.5) | 66 (63.5) | 0.17 |
| IV | 17 (14.5) | 21 (20.2) | |
| Unknown or non-TNM staging | 28 (23.9) | 17 (16.3) | |
| Cancer treatment | |||
| Systemic chemotherapy | 54 (46.2) | 45 (43.3) | 0.50 |
| Radiation therapy | 30 (25.6) | 39 (37.5) | 0.08 |
| Hormone therapy | 18 (15.4) | 20 (19.2) | 0.52 |
| Operation | |||
| Operation performed | 80 (68.4) | 73 (70.2) | 0.10 |
| Waiting for operation | 15 (12.8) | 8 (7.7) | |
| Inoperable | 1 (0.9) | 5 (4.8) | |
| Currently no treatment | 27 (23.1) | 23 (22.1) | 0.76 |
| Rating scale scores | |||
| Patient Health Questionnaire-9 | 4.9±4.7 | 10.3±5.2 | < 0.001 |
| Stress and Anxiety to Viral Epidemics-6 | 12.4±4.4 | 16.3±3.5 | < 0.001 |
| Insomnia Severity Index | 8.6±5.6 | 12.3±4.9 | < 0.001 |
| Brief Resilience Scale | 19.8±3.3 | 17.5±3.3 | < 0.001 |
| Cancer-related Dysfunctional Beliefs about Sleep | 12.0±5.4 | 14.2±4.7 | 0.01 |
| Are you more afraid of COVID-19 than cancer? | 2.7±2.9 | 4.2±3.5 | 0.01 |
| Do you think you are currently depressed or anxious, or do you need help for your mood state? (yes) | 19 (16.2) | 30 (28.8) | 0.03 |
| Have you experienced or been treated for either depression, anxiety, or insomnia? (yes) | 22 (18.8) | 24 (23.1) | 0.28 |
Values are presented as number (%) or mean±standard deviation. COVID-19, coronavirus disease 2019; WSAS, Work and Social Adjustment Scale.
Fig. 1.
Disruption in healthcare service utilization during the coronavirus disease 2019 (COVID-19) pandemic.
There were no significant differences in the proportions of cancer stages, cancer types, and cancer treatment between responders with (WSAS ≥ 11) and without functional impairment (WSAS < 11). The proportions of patients currently needed help for their mood state, and PHQ-9, SAVE-6, ISI, C-DBS, and Fear of COVID-19 over Cancer (FCC) scores were higher and the resilience was lower in the functional impairment group (Table 1).
1. Disruption in healthcare service utilization by cancer patients during the COVID-19 pandemic
Among the 95 patients who reported disruption of hospital utilization, the most common causes of disruption were “worried about visiting the hospital because of the risk of COVID-19 infection” (n=63, 66.3%), “repetitive COVID-19 swab screening tests and examination” (n=40, 42.1%), “more disturbed than before when treated in the emergency room” (n=11, 11.6%), “lack of patient education on the disease and treatment” (n=9, 9.5%), “delay in the outpatient department (OPD) schedule and treatment schedule” (n=9, 9.5%), and “lack of explanation about my treatment plan” (n=8, 8.4%) (Fig. 1).
Furthermore, among all subjects, 22 reported delays in their OPD or treatment schedules. Among them, 12 patients (54.5%) reported a delay in their OPD schedule, resulting in a delayed decision on their treatment plan. Four patients reported delays in their operation schedule, four patients reported delays in their chemotherapy plan, and one patient reported a delay in the radiation treatment plan. The periods of delay were 1 week (n=8, 36.4%), 2 weeks (n=7, 31.8%), and over 3 weeks (n=5, 22.7%). Nineteen patients (86.4%) reported fear of disease recurrence or progression because of the delayed schedule.
2. Functional impairments in the mental health of patients with cancer
Patient functional impairment, as measured by the WSAS, was significantly associated with high depression level, anxiety regarding the viral epidemic, insomnia, cancer-related dysfunctional beliefs to sleep, FCC, and low BRS (Table 2). Patient depressive symptoms, as measured by the PHQ-9, were significantly correlated with high anxiety response to COVID-19, insomnia symptoms, dysfunctional beliefs about sleep score, and low resilience (Table 2). High levels of anxiety response to COVID-19 were significantly correlated with insomnia symptoms, dysfunctional beliefs about sleep, fear of COVID-19 over cancer, and low resilience.
Table 2.
Spearman’s correlation coefficients for each variable
| Variable | Age | WSAS | PHQ-9 | SAVE-6 | ISI | BRS | C-DBS |
|---|---|---|---|---|---|---|---|
| Age | 1.000 | ||||||
| WSAS | −0.11 | 1.000 | |||||
| PHQ-9 | −0.08 | 0.54** | 1.000 | ||||
| SAVE-6 | −0.02 | 0.48** | 0.38** | 1.000 | |||
| ISI | −0.06 | 0.36** | 0.62** | 0.21** | 1.000 | ||
| BRS | 0.06 | −0.35** | −0.56** | −0.20** | −0.40** | 1.000 | |
| C-DBS | −0.06 | 0.31** | 0.36** | 0.32** | 0.33** | −0.25** | 1.000 |
| FCC | 0.11 | 0.19** | 0.08 | 0.17* | 0.06 | 0.01 | 0.03 |
BRS, Brief Resilience Scale; C-DBS, Cancer-Related Dysfunctional Beliefs about Sleep Scale; FCC, Fear of COVID-19 over Cancer; ISI, Insomnia Severity Index; PHQ-9, Patient Health Questionnaire-9; SAVE-6, Stress and Anxiety to Viral Epidemics-6 items; WSAS, Work and Social
Adjustment Scale.
p < 0.05,
p < 0.01.
Logistic regression analysis revealed that functional impairment in mental health of cancer patients was expected following disruption in healthcare service utilization (adjusted odds ratio [aOR], 2.54; 95% confidence interval [CI], 1.19 to 5.43), high depression level (aOR, 1.12; 95% CI, 1.02 to 1.23), anxiety regarding the viral epidemic (aOR, 1.21; 95% CI, 1.08 to 1.35), fear of COVID over cancer (aOR, 1.14; 95% CI, 1.01 to 1.28), and low resilience (aOR, 0.87; 95% CI, 0.76 to 1.00) (Table 3).
Table 3.
Logistic regression analysis to explore factors predicting functional impairment in the mental health of patients with cancer during COVID-19 pandemic
| Variable | cOR (95% CI) | p-value | aOR (95% CI) | p-value |
|---|---|---|---|---|
| Age | 0.99 (0.97–1.01) | 0.40 | 1.00 (0.97–1.03) | 0.98 |
| Duration of illness | 0.96 (0.89–1.04) | 0.34 | 0.98 (0.87–1.09) | 0.66 |
| Cancer stages | 1.35 (0.66–2.77) | 0.42 | 1.91 (0.68–5.35) | 0.22 |
| Currently need help for mood | 2.05 (1.07–3.92) | 0.03 | 0.48 (0.18–1.28) | 0.14 |
| Disruption in healthcare service utilization | 3.76 (2.14–6.59) | < 0.001 | 2.54 (1.19–5.43) | 0.02 |
| PHQ-9 | 1.23 (1.15–1.31) | < 0.001 | 1.12 (1.02–1.23) | 0.02 |
| SAVE-6 | 1.30 (1.19–1.42) | < 0.001 | 1.21 (1.08–1.35) | 0.001 |
| ISI | 1.14 (1.08–1.21) | < 0.001 | 1.05 (0.97–1.14) | 0.20 |
| BRS | 0.80 (0.72–0.88) | < 0.001 | 0.87 (0.76–1.00) | 0.04 |
| C-DBS | 1.09 (1.03–1.15) | 0.002 | 0.99 (0.92–1.08) | 0.88 |
| FCC | 1.15 (1.06–1.25) | 0.001 | 1.14 (1.01–1.28) | 0.04 |
aOR, adjusted odds ratio; BRS, Brief Resilience Scale; C-DBS, Cancer-related Dysfunctional Beliefs about Sleep Scale; CI, confidence interval; cOR, crude odds ratio; COVID-19, coronavirus disease 2019; FCC, Fear of COVID-19 over Cancer; ISI, Insomnia Severity Index; PHQ-9, Patient Health Questionnaire-9; SAVE-6, Stress and Anxiety to Viral Epidemics-6 items.
3. Mediation effect of resilience on the relationship of depression with functional impairment
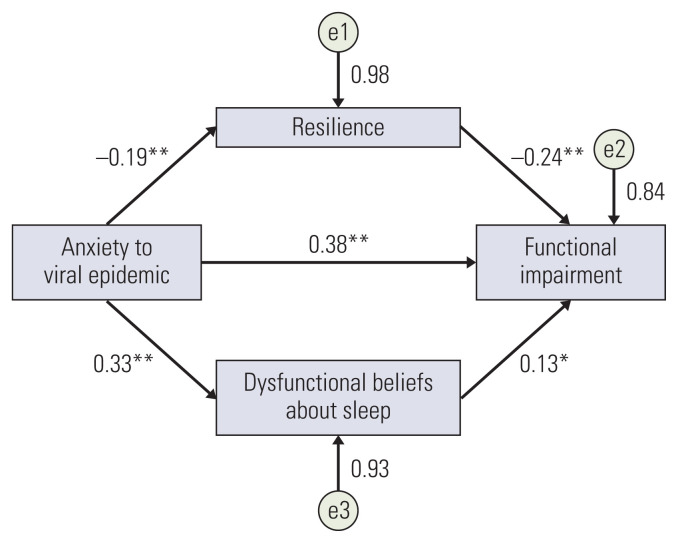
Mediation analysis showed that the complete pathway from anxiety regarding the viral epidemic (independent variable) to resilience and dysfunctional beliefs to sleep (mediator) to functional impairment of cancer patients (dependent variable) was significant (z=7.71, p < 0.001) (Table 4), indicating that resilience and cancer-related dysfunctional beliefs about sleep partially mediated the effects of anxiety regarding the viral epidemic on functional impairment (Fig. 2).
Table 4.
The results of direct, indirect, and total effects on mediation analysis
| Effect | Standardized estimator | S.E. | Z-value | p-value | 95% CI |
|---|---|---|---|---|---|
| Direct effect | |||||
| SAVE-6 → WSAS | 0.38 | 0.12 | 6.14 | < 0.001 | 0.12 to 0.52 |
| Indirect effect | |||||
| SAVE-6 → BRS → WSAS | 0.05 | 0.04 | 2.37 | 0.018 | 0.02 to 0.17 |
| SAVE-6 → C-DBS → WSAS | 0.04 | 0.04 | 1.96 | 0.05 | 0.001 to 0.17 |
| Component | |||||
| SAVE-6 → BRS | −0.19 | 0.05 | −4.07 | 0.004 | −0.25 to −0.05 |
| BRS → WSAS | −0.24 | 0.15 | −4.07 | < 0.001 | −0.90 to −0.32 |
| SAVE-6 → C-DBS | 0.33 | 0.07 | 5.16 | < 0.001 | 0.24 to 0.53 |
| C-DBS → WSAS | 0.13 | 0.10 | 2.12 | 0.03 | 0.02 to 0.42 |
| Total effect | |||||
| SAVE-6 → WSAS | 0.46 | 0.12 | 7.71 | < 0.001 | 0.70 to 1.17 |
BRS, Brief Resilience Scale; C-DBS, Cancer-related Dysfunctional Beliefs about Sleep Scale; CI, confidenceinterval; SAVE-6, Stress and Anxiety to Viral Epidemics-6 items; S.E., standard error; WSAS, Work and Social Adjustment Scale.
Fig. 2.
Mediation model showing that the effect of anxiety related to the viral epidemic (independent variable) on functional impairment (outcome) is mediated by resilience and dysfunctional beliefs about sleep (mediator). *p < 0.05, **p < 0.01.
Discussion
This study explored the disruptions experienced by patients with cancer in healthcare service utilization during the COVID-19 pandemic. Nearly half of the patients (43%) experienced disruptions. Moreover, the functional impairment in the mental health of patients with cancer was predicted by disruptions in healthcare service utilization, high depression level, anxiety regarding the viral epidemic, fear of COVID over cancer, and low resilience. Mediation analysis showed that patient resilience and cancer-related dysfunctional beliefs about sleep partially mediated the effects of anxiety regarding the viral epidemic on functional impairment.
A recent study on the impact of COVID-19 on oncological care showed that 30% of cancer patients reported a conversion of oncological treatment from hospital visits to mobile consultation [17]. The most frequently adjusted treatments were chemotherapy and immunotherapy. More than half of patients with cancer who experienced treatment delays or discontinuation reported feeling concerned about these changes [18]. Thus, the COVID-19 pandemic may have resulted in variable outcomes between patients with cancer and without cancer. Even after adjusting for age, sex, and comorbidities, cancer was associated with an increased risk of death and/or admission to the intensive care unit, with an odds ratio of 5.4 [19]. Therefore, oncologists must weigh the benefit of cancer treatment against the risk of morbidity from COVID-19. Clinicians should strive to avoid limitations in evidence-based cancer care when the risks from COVID-19 are outweighed by the treatment benefits [20]. In this context, Hanna et al. [21] proposed a framework for prioritizing the use of radiotherapy and systemic treatments during the COVID-19 pandemic. This framework was conceptual rather than prescriptive and should be understood considering the capacity of locoregional health systems and the epidemic situation [21].
Although the present study was conducted in a single hospital in Korea, 43% of patients reported disruptions in healthcare service utilization during the COVID-19 pandemic. The most common causes of disruption were “risk of COVID-19 infection” and “repetitive COVID-19 swab screening tests” rather than delay or disturbance in clinical practice. Surprisingly, the clinic and therapeutic schedules were not significantly delayed. This finding might be due to the relatively smaller number of confirmed cases in Korea compared to those in other countries or that the hospitals in Korea rapidly developed prevention plans. Furthermore, in this study, cancer diagnosis, treatment type, and cancer stage were not significantly associated with the patients’ daily mental function. However, depression, anxiety regarding the viral epidemic, insomnia, and resilience were associated with mental functional impairment in patients with cancer. Approximately 40% of responders reported depression and anxiety and only 22.2% reported feeling a need for help regarding their mood state. From the perspective of cancer patients, compared to the healthy population, the COVID-19 pandemic has additional impacts; thus, it is critical to be aware of the emotional state and actively intervene to improve these symptoms in patients with cancer during the COVID-19 pandemic era.
High levels of worry about COVID-19 infection prevented patients from visiting the hospital. A study in the US showed that adults were more likely to have both anxiety and depression during the COVID-19 pandemic than during the first half of 2019. Interestingly, anxiety symptoms were more pronounced than depressive symptoms [22]. Moreover, high levels of worry were related to both anxiety and depressive symptoms. In this context, the SAVE-6, which assesses anxiety responses to the COVID-19 pandemic, might be a useful screening tool to detect mental health problems. Recent efforts have been made to evaluate psychological distress, including various anxiety symptoms triggered by COVID-19 [23,24]. Careful clinical attention is required as anxiety, especially in combination with growing resignation, could lead to dire consequences such as suicidal ideation or suicide risk [25]. As mentioned earlier, disruptions in healthcare service utilization among patients with cancer might be explained by the SAVE-6 score. Maringe et al. [17] reported a significantly increased avoidable death rate and years of life lost among patients with cancer in the United Kingdom during the pandemic period, which was attributed to detrimental changes in cancer treatment patterns that induced anxiety and subjective disturbance in these patients. Since the development and distribution of COVID-19 vaccines are not finalized, it is crucial to ensure personal hygiene, active communication between patients with cancer and medical staff, proper prioritization and transfer of patients with cancer as needed, as well as reducing anxiety to reasonably manage patients with cancer in the COVID-19 pandemic era [26].
In this study, the functional impairments in the mental health of patients with cancer were also predicted by the high levels of depression, anxiety, and fear of COVID over cancer and low resilience. Since the WSAS, which indicates functional impairment, includes assessments of leisure activities and interpersonal relationships, patients who are anxious about the viral epidemic might be withdrawn and isolated from social activities; therefore, their daily mental function might be impaired. These findings are consistent with those of previous studies reporting that anxiety, fear, and depression could be problematic during times of infectious epidemic crisis [27]. Previous research indicated significant relationships among anxiety, depression, and insomnia over time and affecting each other bidirectionally. Furthermore, high C-DBS scores were associated with high anxiety levels in this and a previous study [28]. Moreover, it is known that resilience and dysfunctional belief about sleep among cancer patients mediated the relationship of anxiety regarding the viral epidemic with the functional impairment of mental health; however, that the cancer-related dysfunctional beliefs about sleep mediate the influence of anxiety to viral epidemic on functional impairment in COVID-19 has not been reported previously. Nevertheless, resilience is an important factor associated with enhancing the quality of life of patients with cancer [29]. The cancer-related dysfunctional beliefs about sleep consisted of two items of “cancer recurrence” and “immune function” [15]. Cancer patients are anxious that their immune function might be disrupted if they do not sleep well. In the context of the COVID-19 pandemic, patients with cancer panic that they are at risk for COVID-19 since they belong to a high-risk group. High prevalence of depression, stress, anxiety, and insomnia during the COVID-19 pandemic was reported among cancer patients [30]. Stress or anxiety can induce sleep problems during the pandemic, which might influence their dysfunctional beliefs about sleep and ultimately affect the mental function of patients with cancer.
This study had several limitations. First, although this study included more than 10 types of cancer, breast cancer accounted for 40% of the study sample; thus, selection bias is possible. Second, information on cancer stages/types was gathered from patients’ self-report and not by chart review; thus, there was a possibility that inaccurate information was reported. Third, owing to the cross-sectional study design, it was difficult to compare the mental status of patients with cancer before and after the COVID-19 pandemic. Fourth, in the pandemic era, while about one-tenth of the patients reported delays in their treatment schedules, most of their schedules were rearranged within 2 weeks. The delay was shorter than expected, possibly because of the relatively small number of patients with COVID-19 in the Republic of Korea compared to that in other countries. Although this study was conducted in a high-volume tertiary medical center that partially represents the nationwide medical condition, it is difficult to generalize our results. Further studies are needed to estimate the effect of disturbances in various medical environments.
In conclusion, in this pandemic era, about half of the cancer patients experienced functional impairment due to emotional problems as well as disruptions in healthcare service utilization. These disturbances and functional impairment were strongly associated with anxiety and depression levels. Since the daily mental function and emotional problems affect the cancer patients’ progress, the psychological demands of patients in both acute stage of the disease and with stable status should be addressed to relieve their concerns. Thus, the care system should be managed to help cancer patients during the pandemic era.
Footnotes
Ethical Statement
The study protocol was approved by the Institutional Review Board, which waived the requirement for written informed consent (2020-1055).
Author Contributions
Conceived and designed the analysis: Ahn MH, Son KY, Kim JE, Kim HJ, Yoo SM, Kim SH, Kwon MJ, Koh SJ, Seo S, Chung S.
Collected the data: Kim SH, Kwon MJ, Seo S, Chung S.
Contributed data or analysis tools: Kim K, Lee J, Kim SH, Kwon MJ, Kim HJ, Koh SJ, Seo S, Chung S.
Performed the analysis: Kim K, Kim H, Lee J, Cho IK, Kim HJ, Seo S, Chung S.
Wrote the paper: Kim K, Kim H, Lee J, Cho IK, Ahn MH, Son KY, Kim JE, Kim HJ, Yoo SM, Kim HJ, Koh SJ, Seo S, Chung S.
Conflicts of Interest
Conflict of interest relevant to this article was not reported.
References
- 1.Cui J, Li F, Shi ZL. Origin and evolution of pathogenic corona-viruses. Nat Rev Microbiol. 2019;17:181–92. doi: 10.1038/s41579-018-0118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chan JF, Yuan S, Kok KH, To KK, Chu H, Yang J, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395:514–23. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carlos RC, Lowry KP, Sadigh G. The coronavirus disease 2019 (COVID-19) pandemic: a patient-centered model of systemic shock and cancer care adherence. J Am Coll Radiol. 2020;17:927–30. doi: 10.1016/j.jacr.2020.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kang L, Li Y, Hu S, Chen M, Yang C, Yang BX, et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. 2020;7:e14. doi: 10.1016/S2215-0366(20)30047-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Al-Shamsi HO, Alhazzani W, Alhuraiji A, Coomes EA, Chemaly RF, Almuhanna M, et al. A practical approach to the management of cancer patients during the novel coronavirus disease 2019 (COVID-19) pandemic: an international collaborative group. Oncologist. 2020;25:e936–45. doi: 10.1634/theoncologist.2020-0213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Braunstein LZ, Gillespie EF, Hong L, Xu A, Bakhoum SF, Cuaron J, et al. Breast radiation therapy under COVID-19 pandemic resource constraints: approaches to defer or shorten treatment from a comprehensive cancer center in the United States. Adv Radiat Oncol. 2020;5:582–8. doi: 10.1016/j.adro.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Romesser PB, Wu AJ, Cercek A, Smith JJ, Weiser M, Saltz L, et al. Management of locally advanced rectal cancer during the COVID-19 pandemic: a necessary paradigm change at memorial sloan kettering cancer center. Adv Radiat Oncol. 2020;5:687–9. doi: 10.1016/j.adro.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bartlett DL, Howe JR, Chang G, Crago A, Hogg M, Karakousis G, et al. Management of cancer surgery cases during the COVID-19 pandemic: considerations. Ann Surg Oncol. 2020;27:1717–20. doi: 10.1245/s10434-020-08461-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chung S, Kim HJ, Ahn MH, Yeo S, Lee J, Kim K, et al. Development of the stress and anxiety to viral epidemics-9 (SAVE-9) scale for assessing work-related stress and anxiety in the healthcare workers in response to viral epidemics. J Korean Med Sci. 2021 Dec 06;36(47):e319. doi: 10.3346/jkms.2021.36.e319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chung S, Ahn MH, Lee S, Kang S, Suh S, Shin YW. The Stress and Anxiety to Viral Epidemics-6 Items (SAVE-6) Scale: a new instrument for assessing the anxiety response of general population to the viral epidemic during the COVID-19 pandemic. Front Psychol. 2021;12 doi: 10.3389/fpsyg.2021.669606. 669606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bastien CH, Vallieres A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 13.Morin CM, Vallieres A, Guay B, Ivers H, Savard J, Merette C, et al. Cognitive behavioral therapy, singly and combined with medication, for persistent insomnia: a randomized controlled trial. JAMA. 2009;301:2005–15. doi: 10.1001/jama.2009.682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. 2008;15:194–200. doi: 10.1080/10705500802222972. [DOI] [PubMed] [Google Scholar]
- 15.Chung S, Youn S, Choi B. Assessment of cancer-related dysfunctional beliefs about sleep for evaluating sleep disturbance in cancer patients. Sleep Med Res. 2017;8:98–101. [Google Scholar]
- 16.Mundt JC, Marks IM, Shear MK, Greist JH. The Work and Social Adjustment Scale: a simple measure of impairment in functioning. Br J Psychiatry. 2002;180:461–4. doi: 10.1192/bjp.180.5.461. [DOI] [PubMed] [Google Scholar]
- 17.Maringe C, Spicer J, Morris M, Purushotham A, Nolte E, Sullivan R, et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol. 2020;21:1023–34. doi: 10.1016/S1470-2045(20)30388-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.de Joode K, Dumoulin DW, Engelen V, Bloemendal HJ, Verheij M, van Laarhoven HWM, et al. Impact of the coronavirus disease 2019 pandemic on cancer treatment: the patients’ perspective. Eur J Cancer. 2020;136:132–9. doi: 10.1016/j.ejca.2020.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liang W, Guan W, Chen R, Wang W, Li J, Xu K, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21:335–7. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spicer J, Chamberlain C, Papa S. Provision of cancer care during the COVID-19 pandemic. Nat Rev Clin Oncol. 2020;17:329–31. doi: 10.1038/s41571-020-0370-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hanna TP, Evans GA, Booth CM. Cancer, COVID-19 and the precautionary principle: prioritizing treatment during a global pandemic. Nat Rev Clin Oncol. 2020;17:268–70. doi: 10.1038/s41571-020-0362-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Twenge JM, Joiner TE. U.S. Census Bureau-assessed prevalence of anxiety and depressive symptoms in 2019 and during the 2020 COVID-19 pandemic. Depress Anxiety. 2020;37:954–6. doi: 10.1002/da.23077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Taylor S, Landry CA, Paluszek MM, Fergus TA, McKay D, Asmundson GJ. Development and initial validation of the COVID Stress Scales. J Anxiety Disord. 2020;72:102232. doi: 10.1016/j.janxdis.2020.102232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 scale: development and initial validation. Int J Ment Health Addict. 2022;20:1537–45. doi: 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stanley IH, Boffa JW, Rogers ML, Hom MA, Albanese BJ, Chu C, et al. Anxiety sensitivity and suicidal ideation/suicide risk: a meta-analysis. J Consult Clin Psychol. 2018;86:946–60. doi: 10.1037/ccp0000342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.European Society for Medical Oncology. Cancer treatment management during the COVID-19 pandemic [Internet] Lugano: European Society for Medical Oncology; c2020. [cited 2020 Dec 3]. Available from: https://www.esmo.org/guidelines/cancer-patient-management-during-the-covid-19-pandemic . [Google Scholar]
- 27.Serrano-Ripoll MJ, Meneses-Echavez JF, Ricci-Cabello I, Fraile-Navarro D, Fiol-deRoque MA, Pastor-Moreno G, et al. Impact of viral epidemic outbreaks on mental health of health-care workers: a rapid systematic review and meta-analysis. J Affect Disord. 2020;277:347–57. doi: 10.1016/j.jad.2020.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yeo S, Yi K, Kim C, Lee J, Youn S, Suh S, et al. Cancer-related dysfunctional beliefs about sleep may influence insomnia of cancer patients regardless of depressive symptoms. Sleep Med Res. 2019;10:31–5. [Google Scholar]
- 29.Celik GK, Cakir H, Kut E. Mediating role of social support in resilience and quality of life in patients with breast cancer: structural equation model analysis. Asia Pac J Oncol Nurs. 2021;8:86–93. doi: 10.4103/apjon.apjon_44_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Juanjuan L, Santa-Maria CA, Hongfang F, Lingcheng W, Pengcheng Z, Yuanbing X, et al. Patient-reported outcomes of patients with breast cancer during the COVID-19 outbreak in the epicenter of China: a cross-sectional survey study. Clin Breast Cancer. 2020;20:e651–62. doi: 10.1016/j.clbc.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]