Abstract
Background: Our institution has been offering the General inpatient hospice (GIP) services within the premises of our hospital since 2013. Our previous data had suggested increased acceptance of hospice and GIP care with this model. We wanted to study the impact of the current COVID-19 pandemic, on utilization of Hospice with this model of care.
Objectives: Compare utilization of GIP at HUMC during the first COVID-19 surge, (3/1/2020–6/30/2020) to pre-COVID period (11/1/2019–2/29/2020).
Methods: Using a retrospective chart review was done for GIP admissions from 11/2019 to 6/2020 at Hackensack University Medical Center (HUMC), an academic hospital in New Jersey which was approved by HUMC institutional review board. Data was collected for demographics and comorbidities. Descriptive statistics were reported.
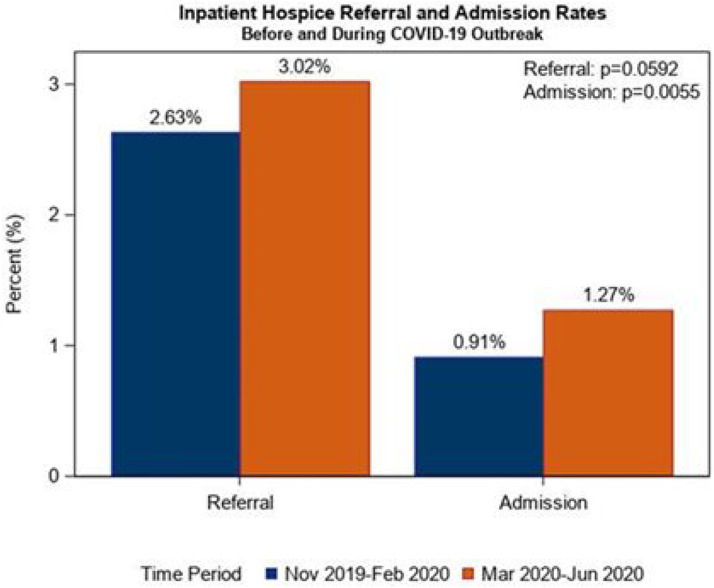
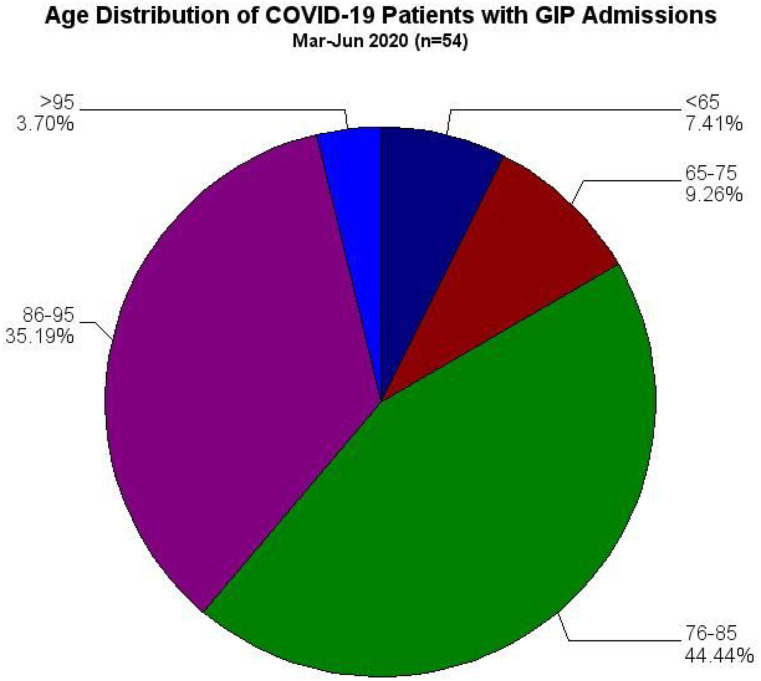
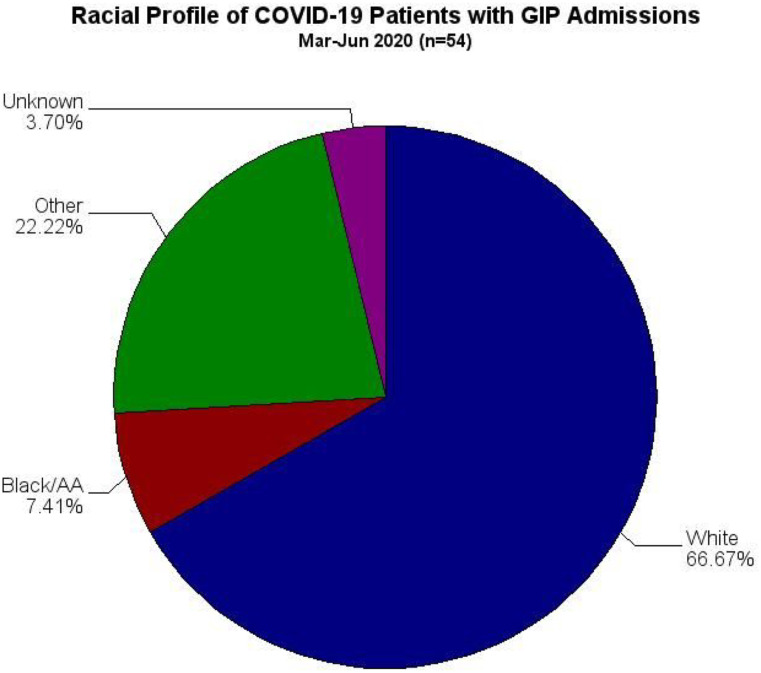
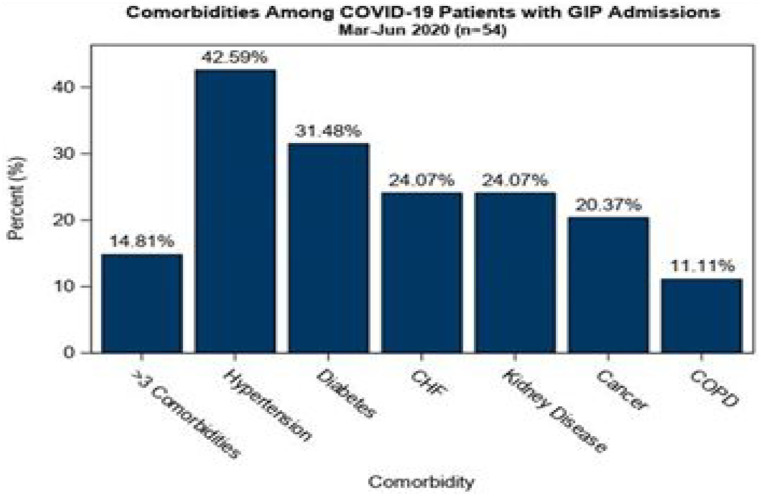
Results: The primary findings show increased hospice referrals during the study period (3.02%) compared to the pre-covid time period (2.63%), P = .0592. Furthermore, GIP admissions increased from 122/13 440 (.91%) in the pre-covid period to 146/11 480 (1.27%) during covid, P = .0055. There were 54 patients admitted to GIP with COVID-19. Descriptive statistics showed male and female distribution was almost equal (53.70% vs. 46.30%), and mean age of 82 years. In GIP patients with COVID-19, majority patients were white patients, (66.67%) age group of 76–95 years old and had < 3 comorbidities (85.19%), about half were with hypertension, next chronic condition was diabetes.
Conclusions: COVID-19 outbreak increased both hospice referral and admission in our model of care. Availability of GIP in the hospital setting may help acceptance and facilitation of these essential end-of-life care services.
Keywords: covid-19, hospice, inpatient hospice, the general inpatient hospice, bereavement, end-of-life care
Introduction and Background
Covid-19 which is caused by the SARS-COV-2 virus has resulted in a rapid global pandemic in 2020. In December 2019, cases of COVID-19 appeared in China. Subsequently, the disease spread, and on March 11, 2020, the World Health Organization declared COVID-19 a pandemic. First reported case in the USA was in Washington state in January 2020 after travel to China but community transmission was likely happening by the end of February 2020 per Center for Disease Control (CDC). As of the beginning of June 2021, USA had over 33.5 million cases and above 602 000 deaths per CDC.
The COVID-19 pandemic reached the U.S. state of New Jersey with the first confirmed case occurring in Bergen County on March 2, 2020 and testing positive for COVID-19 on March 4, 2020.1
As the disease continued to progress, a large number of patients were getting admitted in the first wave, a significant number of them were in critical condition, with poor prognosis. Many patients had substantial symptoms and palliative needs. With lack of any specific treatment options at the beginning of the pandemic, a high volume of patients needed end-of-life care quickly.
Multiple studies have highlighted the urgent need for an integrated Palliative care approach for COVID-19 patients to meet the end-of-life needs.2,3 But it remains unknown whether the COVID-19 pandemic has had an impact on General inpatient hospice (GIP) utilization, there are not many published articles or data around this.4,5
Hospice is a specialized program that provides care to patients who have a terminal illness and life expectancy of 6 months or less. Hospice programs not only provide support to patients’ families while patients are alive but also up to 12 months after a patient has expired. It addresses: physical, psycho-social, emotional, and spiritual needs. It provides services to the patient, caregiver, and family necessary for the palliation and management of the terminal illness and related conditions. The hospice philosophy emphasizes: optimizing comfort, well-being, dignity, and quality of life with focus on caring, not curing. It provides bereavement support to the families and caregivers up to 12 months after the death of the patient. The General inpatient hospice is a specialized part, which focuses on more intensive management of uncontrolled symptoms. This service is provided in either hospice facility or any other acute or subacute facility with 24 hours registered nurse available.
Hackensack University Medical Center (HUMC) has had an inpatient hospice service since 2013. Hospice referral and admissions between pre GIP period versus GIP period showed a statistically significant reduction on the time when hospice referral was placed since the day of admission to hospital. Mean number of days of admission till referral placed with no inpatient hospice was 9.35 days, and with inpatient GIP beds it was 7.51 days.6
Utilization of hospice and GIP during COVID-19 as well as referral pattern has not been well studied.
This highly infectious virus has significantly impacted end-of-life care and urgency for multiple symptom control as hospices respond to the challenging needs of COVID-19 patients and their families.
Our goal was to look at how COVID-19 has impacted referral and admission to GIP during the first surge of the pandemic.
Methods
A retrospective chart review was conducted at Hackensack University Medical Center, a 775 bedded academic center in New Jersey, USA. Records were reviewed between November 1, 2019 and June 30, 2020. The data collection included the total number of hospitalizations, hospice referrals, and hospice admissions during this period. In addition, demographic information was collected for age, sex, and race for patients diagnosed with COVID-19 who were admitted to hospice. Comorbidity information was also collected. Comorbidities were identified via ICD-10 codes (Supplementary Table 1). The time period between November 1, 2019 and February 29, 2020 was considered the pre-COVID time period while March 1, 2020 to June 30, 2020 was considered the COVID time period.
Statistical Method
Descriptive statistics are presented as either n (%) or mean (SD). Hospice referral and admission rates were calculated with the total number of hospitalizations during that time period as the denominator. To assess whether hospice referral and admission rates differed prior to and during the COVID-19 pandemic, the differences in proportions were calculated along with 95% confidence intervals and chi-square tests were performed. All analyses were performed in SAS version 9.4. A P-value less than .05 was considered statistically significant.
Results
Compared to the pre-COVID time period, both GIP referrals and admissions increased during the first wave of the COVID-19 pandemic (Figure 1). Referrals increased from 2.63% to 3.02% (difference = .39% [−.02%, .81%], P = .0592) and admissions from .91% to 1.27% (difference = .36% [.10%, .62%], P = .0055).
Figure 1.
Frequency of inpatient hospice referrals and admissions before and during the COVID-19 pandemic out of total hospitalizations.
There were 13 440 and 11 480 hospitalizations in pre-COVID and during COVID-19, respectively. Hospice referrals and admissions were 353 and 122 in the pre-COVID period and 347 and 146, respectively, during the first COVID surge.
There were 54 patients with COVID-19 diagnosis who were admitted to inpatient hospice between March 1, 2020 and June 30, 2020. Figures 2 and 3 describes the demographic characteristics of the study population. Comorbidities were common in this patient population shown in Figure 4. Number of Comorbidities ≤3 was 85.19% and >3 was 14.81%, Hypertension was seen in 42.59%, Diabetes in 31.48%, CHF in 24.07%, Kidney Disease in 24.07%, Cancer in 20.37%, and COPD in 11.11%. About half of those patients had Hypertension (42.59%) and the next most common was diabetes (31.48%) while 14.81% of patients had more than three comorbidities of interest. About three fourths of patients had either hypertension or diabetes.
Figure 2.
Age distribution of COVID-19 patients admitted to General inpatient hospice between March 1, 2020 and June 30, 2020.
Figure 3.
Racial distribution of COVID-19 patients admitted to General inpatient hospice between March 1, 2020 and June 1, 2020.
Figure 4.
Comorbidities among COVID-19 patients admitted to General inpatient hospice between March 1, 2020 and June 30, 2020.
Discussion
Hospice is an important aspect of care during the end of life, where the goal is comfort. Multiple studies have shown certain patterns of hospice acceptance as per race and ethnicity. When looking at our institution, with offering inpatient hospice care on the premises, we had already seen a trend in increased acceptance of hospice care for symptoms management6 even prior to COVID-19 pandemic. During COVID-19 surge, we saw the numbers show further increase.
When we looked at our data, we continued to see increased acceptance of hospice care for appropriate patients during the pandemic. It could be secondary to the already established strong inpatient hospice program within the walls of the hospital. We already had a well-functioning GIP model 3 years prior to the pandemic, allowing us to provide end-of-life care in any bed across our acute care setting. Our observation has been that this eased families’ concern about moving their loved ones when there were significant needs for symptom control. Rather than moving patients to hospice beds, we have been bringing our hospice team to the patient bedside. This is also allowing the same staff, who had been involved in that patient’s care for a prolonged period of time in a significant number of cases to be able to continue care as team members as patients transition to comfort care. This again may help minimize concerns for the family members and patients.
The established GIP provided a great resource to be able to provide comfort care during this pandemic. Our institution provided care to a significant number of COVID positive patients early on and we continue to provide care to significant numbers of COVID-19 patients to date. The on premises GIP care model allowed us to offer hospice care at any bed including intensive care, thereby minimizing the additional burdens during these unprecedented times for the staff. We were able to direct our resources appropriately. Since the staff was already trained with this model of care in the pre-pandemic time, there was no additional learning required when the need for comfort care increased significantly.
Our ongoing experiences definitely make a strong case for integrating end-of-life care models in the acute care setting, to facilitate comfort care transitions and it may help families make these complex decisions. Even though it is a single center experience, we are seeing the continual trend for the past 5 years and a significant increase during the COVID-19 pandemic.
Our sample size does highlight racial differences, with low acceptance of hospice in Black and other populations. This has also been highlighted in previous studies as well.7,8 We do need to continue our efforts for community education. This will allow us to provide comfort care and quality death to more people with diverse backgrounds needing end-of-life care.
COVID has brought forward various gaps in care, especially around access to palliative care and goals of care conversation. Some studies have shown that COVID-19 did not have any impact on the acceptance of hospice care for clinically appropriate individuals.4
Covid-19 also brought dying alone to the forefront. Since families had restricted access during this pandemic, many families did not have an opportunity to be there for their loved ones during these critical times. It also led to not getting closure with the loss of a loved one. We have seen multiple media pieces around this. Our institution did allow visitation for one family member for the GIP patients. This was an additional benefit for the families of patients who were enrolled in the hospice program. The access to bereavement after the death of the patient, an important benefit of enrolling in the hospice program, was much more valuable during these unprecedented times of the pandemic. Social isolation has been a significant effect of the pandemic. This psychosocial support has been crucial for the families and caregivers in dealing with the loss of their loved ones.
Limitations of our study are
1. It is a single center study that would need to be confirmed on a larger scale.
2. We did not explore demographics for non-COVID patients who accepted hospice during this period. So we do not know if the rate of these comorbidities and these demographics differ between COVID and non-COVID patients.
3. We also cannot answer the question “were COVID patients younger than non-COVID patients admitted to hospice during the same time period.”
Conclusion
COVID-19 outbreak increased hospice utilization at our institution where we offer GIP care in the same setting as our acute care. In GIP COVID-19 admissions, there were more white patients, in the age group of 76–95 years old. We observed a high prevalence of hypertension and diabetes in our admitted COVID-19 patients which is consistent with the existing literature. It was interesting to see that patients with more than 3 comorbidities were only 14.81%. Our study, though a single center study, did suggest that hypertension and diabetes show increased association with mortality in patients with COVID-19. Larger, multicenter studies are needed to confirm the association.
Supplemental Material
Supplemental Material, sj-pdf-1-ajh-10.1177_10499091211064833 for Impact of COVID-19 Pandemic on Utilization of the Inpatient Hospice Services (General Inpatient Hospice) by Arunima Sarkar, Manisha Parulekar and Angeline Sanders in American Journal of Hospice and Palliative Medicine®
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplemental Material: Supplemental material for this article is available online.
ORCID iD
Arunima Sarkar https://orcid.org/0000-0003-3107-0776
References
- 1.Author Anonymous. nj.com/coronavirus/2020/03-coronavirus-in-new-jersey-a-timeline-of-the-outbreak.html
- 2.Fadul N, Elsayem AF, Bruera E. Integration of palliative care into COVID-19 pandemic planning. BMJ Support Palliat Care. 2021;11(1):40-44. doi: 10.1136/bmjspcare-2020-002 [DOI] [PubMed] [Google Scholar]
- 3.Etkind SN, Bone AE, Lovell N, et al. The role and response of palliative care and hospice services in epidemics and pandemics: a rapid review to inform practice during the COVID-19 pandemic. J Pain Symptom Manag. 2020;60:e31-e40. doi: 10.1016/j.jpainsymman.2020.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chou Y-C, Yen Y-F, Feng R-C, et al. Impact of the COVID-19 pandemic on the utilization of hospice care services: a cohort study in Taiwan. J Pain Symptom Manage. 2020;60:e1-e6. doi: 10.1016/j.jpainsymman.2020.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sarkar A, Parulekar M, Sanders. How comorbidity and COVID-19 outbreak affected hospice referral and inpatient hospice admission. Presented at AGS21 (American Geriatric society annual meeting 2021, virtual meeting due to pandemic), March 29, 2021, New York, NY. Abstract Number A352. https://meeting.americangeriatrics.org/sites/default/files/inline-files/2021%20JAGS%20Abstract%20Supplement.pdf [Google Scholar]
- 6.Acevedo E, Sarkar A, Parulekar M, Rogers C. In House General Inpatient Hospice (GIP) care model and its impact on referral and acceptance of hospice presented at AGS19. Annual American Geriatric Society meeting 2019, May 2-4, 2019, Portland, OR. Abstract number A187. https://agsjournals.onlinelibrary.wiley.com/toc/15325415/2019/67/S1 [Google Scholar]
- 7.Rizzuto J, Aldridge MD. Racial disparities in hospice outcomes: a race or hospice-level effect? J Am Geriatr Soc. 2018;66(2):407-413. doi: 10.1111/jgs.15228. Published in final edited form as:Published online 2017 Dec 18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ornstein KA, RothRoth DL, Huang J, et al. Evaluation of racial disparities in hospice use and end-of-life treatment intensity in the REGARDS cohort. JAMA Network Open. 2020;3(8):e2014639. doi: 10.1001/jamanetworkopen.2020.14639. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-pdf-1-ajh-10.1177_10499091211064833 for Impact of COVID-19 Pandemic on Utilization of the Inpatient Hospice Services (General Inpatient Hospice) by Arunima Sarkar, Manisha Parulekar and Angeline Sanders in American Journal of Hospice and Palliative Medicine®