Implication Statement
The “Teddy Bear Hospital Project” (TBHP) is a low cost, international initiative aimed at reducing children’s fears associated with healthcare visits by modelling these interactions using teddy bears. The University of Ottawa program had the additional objective of assessing whether TBHP increased pre-clerkship medical students’ comfort communicating medical concepts to children. Our student volunteers reported a statistically significant increase in their comfort communicating medical topics to young children and all volunteers would recommend TBHP to a colleague interested in pursuing family medicine or pediatrics. Our program could also be easily replicated by Pediatric Interest Groups at other Canadian medical schools.
Énoncé des implications de la recherche
Le «Teddy Bear Hospital Project» (TBHP) est une initiative internationale à faible coût visant à apaiser les craintes des enfants liées aux visites médicales en modélisant ces interactions à l’aide d’ourson en peluche. Le programme de l’Université d’Ottawa avait pour objectif supplémentaire de déterminer si le TBHP permettait aux étudiants du pré-externat de communiquer plus facilement des concepts médicaux aux enfants. Nos étudiants bénévoles ont signalé une augmentation statistiquement significative de leur aisance à communiquer des notions médicales à de jeunes enfants et tous les bénévoles recommanderaient le TBHP à des collègues intéressés par la médecine familiale ou la pédiatrie. Notre programme peut être facilement reproduit par les groupes d’intérêt en pédiatrie d’autres facultés de médecine au Canada.
Introduction
TBHP is an initiative that has been shown to reduce children’s fears associated with healthcare visits by having children model these interactions using their teddy bears.1,2 Previous qualitative studies suggest that TBHP increases volunteers’ comfort interacting with children, prepares children for uncomfortable procedures, and improves history-taking from pediatric patients.3,4 However, no study has demonstrated its effect on volunteers’ comfort communicating medical concepts to children, an important skill to acquire for students hoping to pursue a career with a large proportion of pediatric patients (i.e. family medicine or pediatrics).5 Medical students with limited prior experience with children are less comfortable interacting with children in a clinical context.6,7 Given there are limited opportunities to communicate directly with children in pre-clerkship curricula, we aimed to investigate whether: 1) the University of Ottawa’s (uOttawa) adaptation of the TBHP was effective in increasing pre-clerkship students’ comfort communicating medical topics to young children; 2) the program impacted students’ decision to pursue a career with a large proportion of pediatric patients, and 3) volunteers would recommend this experience to colleagues interested in pursuing a career with a pediatric focus.
Innovation
Our program was established by medical students through the Pediatric Interest Group at uOttawa in 2018, with the X-Ray & MRI station modeled after Western University’s previously existing program. During school visits, pre-clerkship volunteers entered kindergarten and first-grade classrooms as “Teddy Bear Doctors” and tended to the children’s “sick teddies.” There was mandatory training for volunteers consisting of a PowerPoint presentation with videos of mock classroom visits. During each session, children rotated through four 15-minute stations: immunization and handwashing; well-child visit; X-ray & MRI; and casting & bone health as depicted in Figure 1.8 The stations were designed with the following considerations in mind: interactivity, enjoyment, and notably common and/or anxiety-provoking interactions for children.8 In addition to helping alleviate children’s fears of visiting the doctor, TBHP also provided medical students the chance to interact with young children in a low-risk setting.9 Activities emphasized the importance of simple language, analogies, and interaction.10 An overview of stations can be found in Appendix A; links to training videos are found in Appendix B. Costs solely included a one-time purchase of re-usable supplies including pre-wrap medical tape for casting, needleless syringes for immunizations, and toy otoscopes. This project was exempt from ethics review by Children’s Hospital of Eastern Ontario Research Ethics Board.
Figure 1.
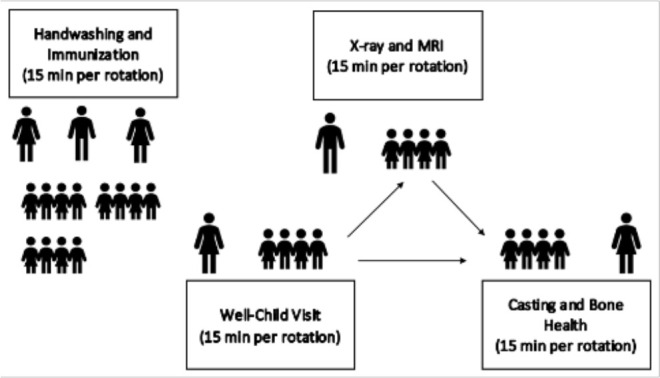
Ratio of child participants to facilitators for each station of the four stations.
Note that the first 15-minute station was Handwashing and Immunization, facilitated by all three volunteers to the complete group of students. After this point, students and volunteers split into three groups and rotated in 15-minute intervals between the three remaining stations (well-child visit; X-ray & MRI; and casting & bone health).
Outcomes
Volunteers completed a pre- and post-visit surveys to measure: (1) comfort communicating medical topics to children; (2) comfort interacting with children; (3) comfort interacting with children in a clinical setting; and (4) interest in pursuing a career with a large proportion of pediatric patients (i.e. family medicine/pediatrics) on a 9-point Likert scale with the following anchors: “Not comfortable at all,” “Neutral,” and “Very Comfortable.” Data from pre- and post-visit surveys were analyzed using paired t-tests.
In total, 36 volunteers assisted with 24 school visits completed between September 2019 and March 2020. Twenty-seven (75%, 27/36) volunteers completed both surveys. There was a statistically significant increase in volunteers’ comfort communicating medical topics to young children (p = 0.01); however, there was no statistically significant difference in volunteers’ interest in pursuing a career with a pediatric focus (p = 0.24). Additionally, 89% (24/27) of volunteers agreed that the teddy bear hospital experience improved their ability to communicate their medical knowledge to a young child and 100% (27/27) of volunteers reported that they would recommend TBHP to a colleague interested in pursuing family medicine or pediatrics.
The main limitation of this quality improvement study was the self-reported nature of the survey responses. This may have introduced bias as volunteers may have wanted to feel they benefited from the program after having invested time in it. It is important to consider that self-reported measures of comfort do not necessarily correlate with actual abilities. While our volunteers may feel more comfortable communicating medical topics to children, any improvement should this be objectively evaluated.
Next steps
Looking ahead, we plan to follow volunteers longitudinally during clerkship to determine if TBHP allowed for a smoother transition to the clinical setting through comparison of pre- and post-clerkship surveys. Another future goal is to explore whether returning volunteers show a significant improvement in their comfort levels after multiple TBHP visits.
Acknowledgements
Thank you to the Schulich School of Medicine & Dentistry at Western University and their Teddy Bear Hospital Interest Group Executives (Dr. Rachelle Beanlands, Dr. Jessica Empringham and Dr. Sasha Ayoubzadeh) for their materials and support in establishing the initiative as a part of the Pediatric Specialty Interest Group at uOttawa.
Appendix A. Brief overview of each station
- Immunization and Handwashing:
- Explains the purpose of vaccines to children in an accessible way, while also modelling a positive discussion about vaccines that they can then practice with their teddy. Children are asked to volunteer their favourite movies to explain that just like in the children’s favourite movies where there are both “heroes” and “villains”, our body contains both “good” and “bad” germs.
- Well-Child Visit:
- Familiarizes children with the common tools (i.e. otoscope, stethoscope) and procedures (i.e. auscultating, immunizing) they might encounter in primary care.
- X-ray and MRI:
- Familiarizes children with the process of getting an X-ray or MRI. Children look at X-ray images of fractured animal paws, tails and extremities, and work in pairs to identify the fracture by looking for “a zig-zag line”. Additionally, participants practice lying still for an MRI, while the MRI noises are played.
- Casting and Bone Health:
- Normalizes the process of getting a cast and discusses bone health. Children discuss why someone might need a cast and use casting pre-wrap material to cast their teddy’s paw. The volunteer also leads a discussion using images that reflect activities/foods that help maintain bone health.
Appendix B: Links to training materials
1. Volunteer Training PowerPoint: https://drive.google.com/file/d/109FGtndtKNmZxxJvEwI5dJR5_URtkTg-/view?usp=sharing
2. Volunteer Training Videos:
-
Teddy Bear Project - Part 1 (Introduction, Handwashing and Immunizations)
-
Teddy Bear Project - Part 2 (Well-Child Visit)
-
Teddy Bear Project - Part 3 (X-ray and MRI)
-
Teddy Bear Project - Part 4 (Casting and Bone Health)
3. Parent Letter with Program Explanation:
https://drive.google.com/file/d/1h1aFquN3cduZ0s_Pp2HMjI1bsqSsKsR0/view?usp=sharing
4. Station Resources for Volunteers:
- Immunizations & Handwashing:
- Casting & Bone Health:
5. French Resources:
https://drive.google.com/drive/folders/1zbxT1RfxImuRTA7bHbIWTdgNnJRBno7h?usp=sharing
Conflicts of Interest
The authors have received no financial support for the creation of this innovation and all authors have no conflicts of interest to disclose.
Authorship
Hannah Kis and Kaitlin Endres are co-first authors of this submission.
References
- 1.Bloch YH, Toker A. Doctor, is my teddy bear okay? The “teddy bear hospital” as a method to reduce children’s fear of hospitalization. Isr Med Assoc J. 2008;10(9):597–9. [PubMed] [Google Scholar]
- 2.Dalley JS, Creary PR, Durzi T, McMurtry CM. An interactive teddy bear clinic tour: teaching veterinary students how to interact with young children. J Vet Med Educ. 2017;44(2):302–15. 10.3138/jvme.1115-180R1 [DOI] [PubMed] [Google Scholar]
- 3.Husøy G. Teddy bear hospital — students’ learning in the field of practice with children. Nord J Nurs Res. 2013;33(1):51–5. 10.1177/010740831303300111 [DOI] [Google Scholar]
- 4.Nheu L, Uahwatanasakul W, Gray A. Medical students’ experience of a teddy bear hospital as part of a paediatric curriculum. Health Prof Edu. 2018;19(3):22–4. 10.11157/fohpe.v19i3.217 [DOI] [Google Scholar]
- 5.Whitt R, Toussaint G, Bruce SB, Borges NJ. Strengthening student communication through pediatric simulated patient encounters. J Educ Eval Health Prof. 2014;11:21. 10.3352/jeehp.2014.11.21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Soares N, Stratton T, Wilson J. Medical students’ comfort with children. Clin Teach. 2015;12(3):176-80. 10.1111/tct.12262 [DOI] [PubMed] [Google Scholar]
- 7.Teh JJ, Cheung KY, Patrick Y, Panahi M, Boyle R, Tudor-Williams G. Self-perceived confidence of medical students communicating with pediatric patients in a 7-week pediatric placement: A pilot survey. Adv Med Educ Pract. 2020;11:163-169. 10.2147/AMEP.S234856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beanlands R, Epringham J. Schulich. Medical school teddy bear hospital project interest group. [Telephone Interview, 18 June]. Ottawa; 2018. [Unpublished]. [Google Scholar]
- 9.Santen L, Feldman T. Teddy bear clinics: a huge community project. Am J Matern Child Nurs. 1994;19(2):102–6. 10.1097/00005721-199403000-00011 [DOI] [PubMed] [Google Scholar]
- 10.Kaufman J, Modak M, Moylan S. The teddy bear hospital in Australia. J Paediatr Child Health. 2012;48(6):541–2. 10.1111/j.1440-1754.2012.02482.x [DOI] [PubMed] [Google Scholar]


