Abstract
Background
African-Americans are underrepresented in mobile health intervention research studies which can perpetuate health inequities and the digital divide. A community-based, user-centered approach to designing mobile health interventions may increase their sociocultural relevance and effectiveness, especially with increased smartphone use during the coronavirus disease 2019 pandemic. We aimed to refine an existing mobile health intervention via a virtual focus group series.
Methods
African-American community members (n = 15) from churches in Minneapolis-St. Paul and Rochester, Minnesota were enrolled in a virtual (via videoconferencing), three-session focus group series over five months to refine a cardiovascular health-focused mobile health application (FAITH! [Fostering African-American Improvement in Total Health!] App). Participants accessed the app via their smartphones and received a Fitbit synced to the app. Participants engaged with multimedia cardiovascular health-focused education modules, a sharing board for social networking, and diet/physical activity self-monitoring. Participant feedback on app features prompted iterative revisions to the FAITH! App. Primary outcomes were app usability (assessed via Health Information Technology Usability Evaluation Scale range: 0–5) and user satisfaction.
Results
Participants (mean age [SD]: 56.9 [12.3] years, 86.7% female) attended a mean 2.8 focus groups (80% attended all sessions). The revised FAITH! App exceeded the goal Health Information Technology Usability Evaluation Scale score threshold of ≥4 (mean: 4.39, range: 3.20–4.95). Participants positively rated updated app content, visual appeal, and use of social incentives to maintain engagement. Increasing user control and refinement of the moderated sharing board were identified as areas for future improvement.
Conclusions
Community-partnered, virtual focus groups can optimize usability and increase participant satisfaction of mobile health lifestyle interventions that aim to promote cardiovascular health in African-Americans.
Keywords: Mobile health lifestyle intervention, African-Americans, user-centered design, cardiovascular health, community–academic partnership
Introduction
Existing cardiovascular health (CVH)-related disparities between White people and African-Americans (AAs) in the United States 1 have been exacerbated by the coronavirus disease 2019 (COVID-19) pandemic. 2 AAs and other communities of color account for a greater proportion of COVID-19-related mortality despite comprising a lower percentage of the US population compared to White people.3,4 This disproportionate COVID-19-associated mortality among AAs may be explained by long-standing structural, social, and health-related inequities. AAs have a greater burden of poorly controlled co-morbidities such as hypertension, diabetes, and obesity compared to White people that have been associated with higher risk of COVID-19-associated mortality.5,6
Now more than ever, there is a need to increase access to technology-based interventions to improve CVH in AAs. The COVID-19 pandemic necessitated a rapid transition to virtual and telehealth care models which magnified the digital divide between AAs and other racial/ethnic groups in the United States.7,8 A user-centered approach that accounts for technology usage patterns among AAs may be an avenue to design socioculturally relevant and effective interventions that reduce the digital divide. 9 AAs are more likely to rely solely on smartphones compared to White people in order to access the Internet, online social networking sites, and health information.10,11 Thus smartphone-based lifestyle interventions can be effective platforms to address these CVH disparities in AAs, but require the use of a community-engaged, and user-centered approach to develop successful interventions.9,12–14 There has been a lag in the widespread adoption of evidence-based, community-based participatory research (CBPR) approaches to build equitable community–academic partnerships with AA communities. These approaches have been shown to be effective in recruiting historically underrepresented and marginalized racial/ethnic minority groups into clinical research using culturally tailored recruitment strategies.15–17
Study objective and aims
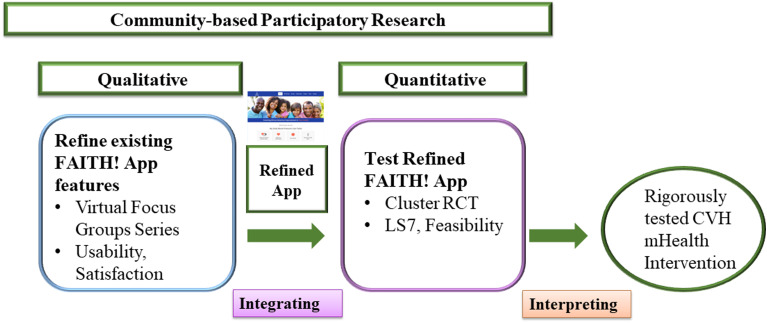
Funded by the American Heart Association (AHA) and the National Institutes of Health/National Institute on Minority Health and Health Disparities, this study applied a CBPR approach within the Fostering African-American Improvement in Total Health! (FAITH!) Trial to rigorously refine and test the feasibility and preliminary efficacy of our FAITH! App to improve CVH among AAs within a cluster, randomized controlled trial (RCT) with delayed intervention (Figure 1). The FAITH! App promotes the AHA Life's Simple 7 (LS7) by incorporating user-individualized and interpersonal features through multimedia education modules, tailored messaging, diet/physical activity (PA) self-monitoring, and social networking. The current study describes the process implemented to refine the FAITH! App through an innovative virtual focus group series. The aim of this study was to obtain participant feedback on refinements made to the FAITH! App after completion of a pilot study 13 and to identify further areas of improvement within the app prior to its use in a larger RCT.
Figure 1.
Fostering African-American Improvement in Total Health! (FAITH!) Trial overview: Exploratory sequential/participatory mixed-methods design.
The focus group series was transitioned from an anticipated in-person focus group to a virtual series due to the COVID-19 pandemic and social unrest related to the murder of Mr. George Floyd in the Minneapolis, MN metropolitan area during the recruitment phase for this study. Significant efforts were made to maintain fidelity of the aims of this study with the transition of this focus group series to a virtual platform.
Methods/Design
The study was reviewed and approved by the Mayo Clinic Institutional Review Board and registered (clinicaltrials.gov NCT03777709).
Study overview
The overall FAITH! Trial design incorporates an exploratory sequential/participatory mixed-methods design approach 18 to accomplish its two specific aims (Figure 1). To refine the intervention through community input, we conducted an iterative, semi-structured focus group series comprised of AA community members affiliated with partnering AA churches. This work builds on formative evaluation results from in-person focus groups conducted following the FAITH! App pilot study 13 that assessed overall satisfaction and suggestions for improvement of the app. 14 Full details on the FAITH! App prototype features and user-centered19,20 and participatory design21,22 processes have been previously described in detail.9,23 Modifications to the existing FAITH! App prototype were completed based on the pilot study post-intervention focus groups findings, prior to start of the current study. The focus groups reported here were then convened to review the preliminary app revisions while providing an opportunity to further refine the app to bolster cultural relevance for the AA faith community and encourage optimal user engagement prior to use of the FAITH! App in the RCT. 24 The RCT results will be reported separately.
Utilization of behavioral theory to refine FAITH! App
The findings from the focus group sessions completed immediately after the pilot study13,14 provided the research team the opportunity to revise the app prior to the current study. These revisions were completed utilizing a theory-based approach. Participant feedback post-pilot study recommended the addition of prompts to encourage app use, and personalization based on individuals’ cardiovascular risk. The Precaution Adoption Process Model (PAPM) 24 informed the development of predetermined decision rule-based messages within the app to promote behavior change (e.g. healthy diet, regular PA) based on participant stage-of-change 25 and individual LS7 focus area (e.g. blood pressure, weight maintenance). These messages were delivered three to four times/week to participants within the app dashboard messaging inbox. For example, individuals categorized in the early stages-of-change (1–2) received messages aimed at increasing their awareness and readiness to act; while those in advanced stages-of-change (5–6) received messages centered on positive reinforcement and performance capacity-building. Additional reminders were delivered via the app dashboard to encourage consistent self-monitoring of diet and PA. 26 Post-pilot study feedback also highlighted the need for updates to app self-monitoring features. Guided by the Social Ecological Model (SEM),27,28 app self-monitoring features for diet and PA were further streamlined for ease of use and to increase participant self-efficacy and self-regulation. The principles of the SEM also guided the addition of education module content that discussed the unique stressors, social determinants of health (SDOH), and health disparities burdening AA communities and the need for health equity to ensure access to quality healthcare services to surpass these factors. Behavioral economics29–31 were utilized to incorporate social incentives within the app such as individual and interchurch competition for the highest daily fruit and vegetable intake and PA to motivate participant engagement. Table 1 outlines all revisions made to the FAITH! App prior to the current study.
Table 1.
Summary of FAITH! App modifications.
| Revisions made prior to current study | Refinements made during current study |
|---|---|
|
|
AA, African-American; FAITH!, Fostering African-American Improvement in Total Health!; LS7, Life's Simple 7; PA, physical activity; SDOH, social determinants of health.
Recruitment
Recruitment of participants for the focus group series started in April 2020. We set a goal to recruit 15 participants from AA churches in Rochester and Minneapolis–St Paul through church flyers, announcements, and advertisements, as well as referrals from established community partners (e.g. FAITH! community steering committee (CSC) members, FAITH! Program church liaisons. 32 Inclusion criteria were the following: AA race/ethnicity, age ≥18 years, basic Internet skills (e.g. navigating a web browser, ability to check email and search for information on the Internet, etc.), and active email address. Individuals expressing interest in participation to the study team were emailed an electronic screener to assess their eligibility and electronic health literacy (EHL) by the electronic health literacy scale [eHEALS].33,34 EHL is defined as an individual's ability to seek, find, understand, and appraise health information from electronic sources and apply these skills toward health issues. High EHL is defined as an eHEALS score ≥26 which has been previously validated in a similar AA population. 34 We sought to include individuals with a range of EHL levels to allow input from a broad literacy range.
Interested individuals deemed eligible completed electronic informed consent via a secure website. Prior to the first focus group, participants completed a baseline electronic survey capturing sociodemographics, mobile technology use, and electronic health information sources. Participants also received a personal PA monitor (Fitbit Versa 2) to sync with the FAITH! App. As an incentive for participation, a total of $100 by cash card ($50 at enrollment, $50 at completion) was provided to participants.
Data collection and outcomes
Focus group series
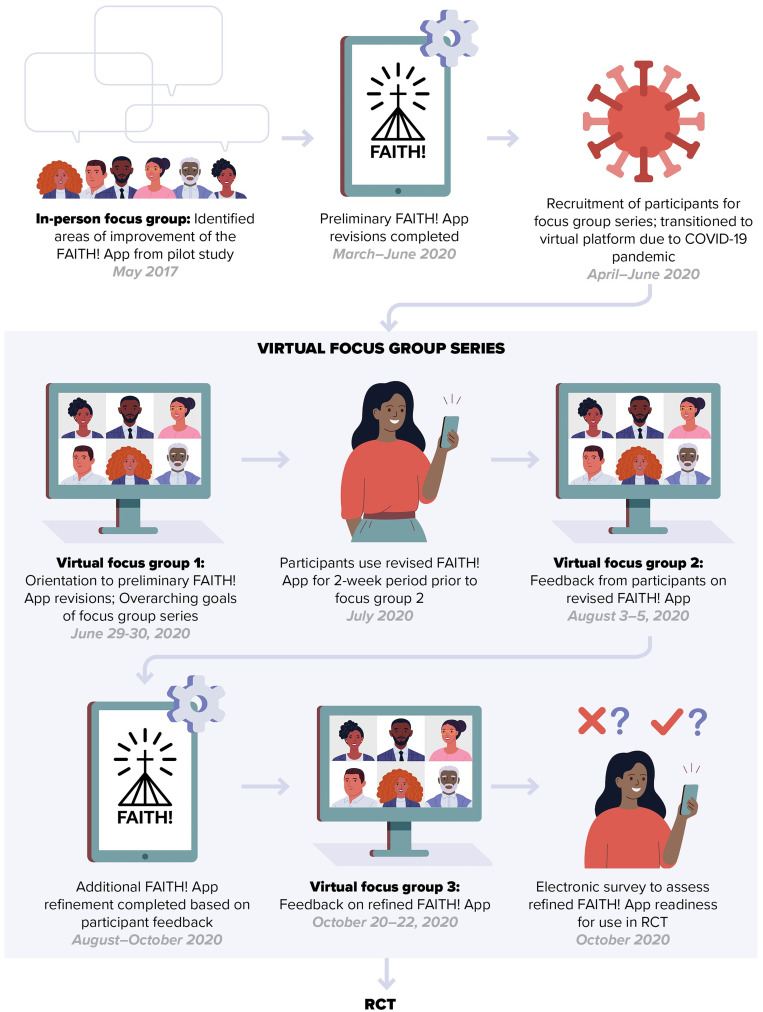
Three focus group sessions including an orientation session were convened over a five-month period (June–October 2020) via videoconferencing (Zoom). Following the orientation, participants were divided into groups of five and assigned to a focus group cluster that convened together for the remainder of the study. Thus, each focus group was a collection of three sessions that included five participants along with the moderators. See Figure 2 for an overview of the virtual focus group series.
Figure 2.
Visual summary of virtual focus group series. Prior to start of the current study, data collected from an in-person focus group was used to complete preliminary revisions of the FAITH! App. Focus groups were transitioned to a virtual platform due to the COVID-19 pandemic and consisted of three virtual sessions. The shaded panel highlights features of the virtual focus group series. Focus group 1 oriented participants to the FAITH! App, after which participants used the FAITH! App for 2 weeks prior to focus group 2. Using feedback from focus group 2, additional refinements were made to FAITH! App and were reviewed during focus group 3. Participants completed electronic surveys rating app usability and satisfaction at the end of the focus group series.
COVID-19, coronavirus disease 2019; FAITH!, Fostering African-American Improvement in Total Health!; RCT, randomized controlled trial.
During the virtual orientation session (focus group #1), participants received instructions on how to download the FAITH! App to their smartphones and general use of the core app features. Participants were asked to test the updated app prototype for a 2-week period prior to focus group #2 and continued to have access to the FAITH! App throughout the duration of the focus group series. Following the final focus group (focus group #3), participants completed a follow-up electronic survey capturing mobile technology use, and impressions on FAITH! App updates.
Each focus group session was led by a trained moderator, 60–90 minutes in duration, and was audio-recorded and transcribed. A co-moderator recorded field notes and managed the Zoom platform features (e.g. chat function, slide share). The discussion followed a semi-structured moderator guide, informed by preliminary studies and the Health Information Technology Usability Evaluation Model/Scale (Health-ITUEM 35 /Health-ITUES,36,37) on app prototype features, proposed revisions, and LS7 incorporation. To create the moderator guide, we developed open-ended questions to promote participant discussion regarding the FAITH! App refinements. These questions were developed using foundational principles in the literature on focus group data collection, 38 input from church partners, and based on the moderator guides utilized during the post-pilot study in-person focus groups. 14 The moderator guide consists of questions that gauge participants’ perceptions of the app (relevance and value of the app to participants), app usability (how the app fits into participants’ daily lives, circumstances of interaction), app satisfaction (sociocultural relevance of app, content of educational modules, use of tracking and sharing board features, ease of app navigation), and app sustainability (ability to maintain healthy lifestyle via app even during times of crisis such as the COVID-19 pandemic and social unrest) (see Supplemental material). The Health Information Technology Usability Evaluation Model (Health-ITUEM) and Health Information Technology Usability Evaluation Scale (Health-ITUES) are systematic rubrics for evaluating mobile health (mHealth) intervention usability, particularly for health-related apps. Questions were structured by category 39 and sessions integrated attentiveness to AA faith community cultural norms and values. 40 Using the most salient themes identified from focus groups, sequential revisions of the app prototype components were completed by the study team and software developers for review at subsequent focus groups.
Primary outcomes
App usability and user satisfaction
App usability was assessed via the Health-ITUES which participants completed following the final focus group. The Health-ITUES 36 consisted of 20 items rated on a 5-point Likert scale (1 = strongly disagree to 5 = strongly agree) with subscales assessing impact (3 items), perceived usefulness (9 items), ease of use (5 items), and user control (3 items). Items assessing impact evaluated the relevance of educational content and degree to which the app met community needs. Perceived usefulness gauged how well the app assisted participants to enact positive CVH behaviors. Perceived ease of use evaluated ease of app navigation. Lastly, user control items evaluated the clarity of messaging when troubleshooting within the app. We aimed to finalize the app and proceed to the RCT if the participant rating of the app readiness met a predetermined goal (mean overall Health-ITUES score of ≥4). If <4, an additional focus group would be convened to address the remaining usability/satisfaction needs. App user satisfaction was assessed with questions rating the specific app features/refinements (poor to excellent) including likes, dislikes, and perceived cultural appropriateness.
Data analysis
Sample characteristics from electronic surveys were summarized by descriptive statistics (frequencies/percentages and means/SDs). Immediately following each focus group, a summary analysis of discussion highlights was compiled by the moderator. 41 Subsequently, transcripts of each session were independently reviewed by two study team members (L.C.B., A.K.) for thematic analysis 42 and incorporated codes from the Health-ITUEM. 35 A third team member (L.E.B.) assisted to resolve discrepancies. Recurrent themes and most salient participant commentary were further summarized to inform sequential app refinement. Content analysis was facilitated by QSR NVivo software, v10 (Doncaster, Victoria, Australia).
Results
Participant characteristics
A total of 15 participants (8, 53.3% from Rochester, MN area churches, 100% of recruitment goal) were recruited to participate in the focus groups series to review the refined FAITH! App. Participants had a mean age (SD) of 56.9 (12.3) years (range: 31–72) and were predominantly female (13, 86.7%). There was overall high EHL (mean: 28.5 (SD 2.5), range: 23–31, low EHL: 2/15 (13%)). On average participants attended a mean of 2.8 sessions (80% attended all sessions).
FAITH! App usability and satisfaction
Overall, participants favorably viewed the updates made to the app based on the focus groups 14 performed immediately after the end of the pilot study. 13 Table 1 summarizes the modifications made prior to and during the current study. After additional iterative revisions were made based on participant feedback, the refined FAITH! App exceeded the app usability Health-ITUES score threshold goal for approval to integrate the intervention into the planned RCT (mean: 4.39, range: 3.20–4.95). Table 2 summarizes the Health-ITUES overall and subscale scores after the focus group series. The following new app features/refinements received the highest satisfaction ratings (very good/excellent): diet and PA tracking log (73.3%) and education module icons (66.7%). The majority of the participants found the app culturally appropriate (good to excellent, 93.3%).
Table 2.
FAITH! App usability ratings after virtual focus group series (n = 15).
| Health-ITUES score | Mean (SD, Range) |
|---|---|
| Impact | 4.67 (0.40, 4.00–5.00) |
| Perceived Usefulness | 4.44 (0.53, 3.22–5.00) |
| Perceived Ease of Use | 4.44 (0.77, 2.20–5.00) |
| User Control | 3.87 (0.83, 2.00–5.00) |
| Mean | 4.39 (0.49, 3.20–4.95) |
| Overall App Rating (0 = Poor, 10 = Excellent) | 8.40 (1.45, 5.00–10.00) |
FAITH!, Fostering African-American Improvement in Total Health!; Health-ITUES, Health Information Technology Usability Evaluation Scale.
Synthesis of participant feedback and emergent themes
Table 3 summarizes emergent themes identified from the focus groups to inform app refinements. Further salient points and details from participants with illustrative quotes are described below as well.
Table 3.
Emergent themes from focus group series.
| Focus group dates | Emergent themes |
|---|---|
| Focus group 1: June 29-30, 2020 | Introduction to focus group series and updated FAITH! App |
| Focus group 2: August 3-5, 2020 | General perceptions of the FAITH! App
|
Using the FAITH! App in daily life and perception of transition to virtual focus group series (from in-person)
|
|
COVID-19 pandemic and utility of FAITH! App in incorporating healthy behaviors
|
|
Suggestions for FAITH! App refinement: visual and educational content, sharing board, tracking features
|
|
| Focus group 3: October 20-22, 2020 | Updated visual features
|
Updated testimonial videos
|
|
App engagement: moderated sharing board, interchurch competition, tailored messaging, and fitness videos
|
|
Future Recommendations
|
COVID-19, coronavirus disease 2019; FAITH!, Fostering African-American Improvement in Total Health!.
Focus group 2
General perceptions of the FAITH! App
Participants found the education modules to be informative, credible, and relevant to their health concerns.
“the content is so valuable…especially for our community. You’d be surprised what people just don’t know…about how their choices can impact their health and…what can make a difference for their health” [Focus group 2 participant, August 3, 2020]
COVID-19 pandemic and utility of FAITH! App in incorporating healthy behaviors
Participants found that use of the FAITH! App helped incorporate healthy behaviors into their daily lives and assisted them to make more mindful health choices during the pandemic. Several participants reported that increased time at home resulted in poorer diet quality and increased their sedentary behaviors.
“before the pandemic, I was extremely active…as a result of…the lockdown, I was having to find different ways to be active. And I was eating…not as healthy. But when we started the study again, it kind of reminded me…that I needed to be more conscious of everything that I ate and everything that I was doing…because of the app and being reminded of things that are really pertinent to your heart health, I think I'm more focused now, even in the midst of the pandemic” [Focus group 2 participant, August 5, 2020]
“Even though we’re in this pandemic, this app and this Fitbit still continues to motivate me to get my steps in…So it still makes me want to continue to move and do what I should be doing even with this pandemic” [Focus group 2 participant, August 4, 2020]
Suggestions for FAITH! App refinement
Feedback from focus group #2 suggested that improvement in visual features and the addition of fitness videos or live events could further enhance the user experience. This had not been highlighted in the prior in-person focus group series conducted immediately after the pilot study.
“Just visual, like visually, for me, the website looks a little bit outdated…and it doesn’t have enough color. …the testimonial videos also look older… just an enhancement in…the look of the technology…would also make someone like me want to utilize the app.” [Focus group 2 participant, August 3, 2020]
“the little pictures of the modules…they are simple. But…you could grab some more attention” [Focus group 2 participant, August 3, 2020]
“I definitely love the idea of adding some exercise videos…if you have something…that’s like 15–20 min long that people – which would be considered like a good exercise time, so if they like it, they could continue to keep going back to that” [Focus group 2 participant, August 3, 2020]
These suggested updates were incorporated into the app prior to the next focus group series. A series of fitness videos with a variety of activities including cardioaerobic, strength, and flexibility exercises to gospel and inspirational music was added to the FAITH! App (Figure 3).
Figure 3.
Screenshot of fitness video.
A moderated sharing board was also added to increase participation prior to focus group #3 in order to foster further discussion on self-efficacy, self-regulation, social support, and barriers/facilitators to a healthy lifestyle. This feature was also in alignment with the SEM to promote healthy behavior change.
Focus group 3
Updated visual features and testimonials
Participants found that updates of education module icons and visual elements within the app platform after focus group #2 increased appeal of the app and increased motivation for engagement. The sequence of the education modules was altered to prioritize information on PA and healthy eating early on in the CVH curriculum. Figure 4 shows before (4A) and after (4B) of the education module icons following the incorporation of participant feedback.
“I did notice the changes in the icons…the pictures were more appealing and kind of showed a little bit more information that would kind of catch the eye…something visually appealing that would encourage the learner and also help them to know what it is they were getting ready to learn about.” [Focus group 3 participant, October 20, 2020]
Figure 4.
Fostering African-American Improvement in Total Health! (FAITH!) App homepage education modules icons. (A) Preliminary prototype layout. (B) Refined layout.
Participants appreciated the use of images within the app that were representative of the AA community and responded positively to the efforts by researchers to enhance diversity within the testimonial videos by ensuring that participants from each church community were represented.
“I would definitely say that the testimonials…showed more representation from a couple more churches…and I also appreciated that the backgrounds were changed in those testimonial videos…and just helped it to be… more appealing and just a little bit more updated.” [Focus group 3 participant, October 20, 2020]
While testimonial videos were positively reviewed, participants suggested that shortening these videos, and ensuring that community members of all ages and body shapes with a balance of men and women would further improve inclusivity and uptake of the FAITH! App.
“make sure that you have a good age representation…young people, older people, in between, and…even weight representation” [Focus group 3 participant, October 20, 2020]
App engagement
With respect to engagement, utilization of a sharing board and tailored messaging facilitated increased and sustained engagement in healthy behaviors for participants.
“I like the sharing board, and I use it a lot…I enjoyed reporting and sharing my daily walks and the healthy food and meals that I was preparing…and it encouraged me to go out each day to walk and to share my experience and to take photos and post them” [Focus group 3 participant, October 22, 2020]
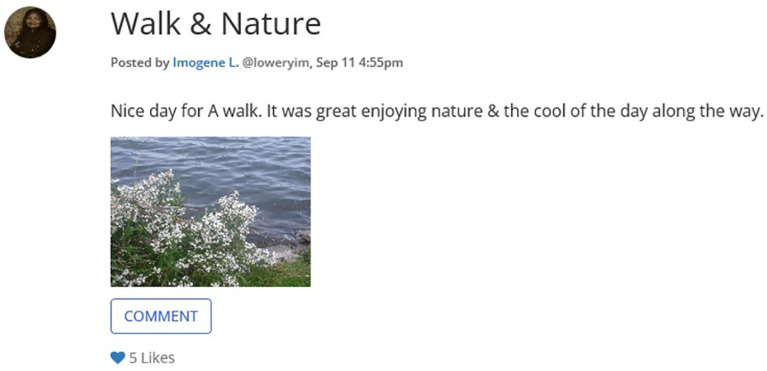
Of note, even participants who were less active on the sharing board seemed to gain benefit from posts by more active members with respect to managing the loss of motivation and maintaining healthy behaviors. See Figure 5 for example of a sharing board post.
“I was encouraged by the ones that did post…If a person wasn’t feeling really up to it, they shared that, and that helps me to understand that we are not 100% every day. So just that little encouragement, or I walked and I saw the beauty out in nature. I enjoyed reading that.” [Focus group 3 participant, October 21, 2020]
Figure 5.
Example post from the participant on sharing board.
Moderated sharing board posts did not seem to significantly increase participant-initiated posting activity within the sharing board; however, the posts provided participants with valuable information.
I like the posting…and it did allow me to look into it. But once again, I didn’t respond…but it gave me something to think about. [Focus group 3 participant, October 21, 2020]
The addition of the moderated sharing board in the latter half of the study may have contributed to the lack of benefit seen as some participants were not as clearly aware of this update and unaware of individuals who were moderators within the app. For future iterations of the app, participants suggested that moderators within the sharing board should be more clearly identified up-front within the sharing board.
“distinguishing themselves a little bit might have been a little bit more helpful to just recognize that they’re on there participating.” [Focus group 3 participant, October 22, 2020]
The use of social incentives at the collective (interchurch competition) and individual levels. Participants found the individual level and collective church level competitive elements to be motivating factors to maintain healthy behaviors to support their churches.
“the winning church of the week. I kind of looked forward to that…because I'm sort of a competitive person, and so it was good to see who was winning and who – it basically encouraged me to do even more.” [Focus group 3 participant, October 22, 2020]
Future recommendations
Additional recommendations at the end of focus group #3 primarily focused on increasing the customizability of app notifications and increasing the accessibility of app content on multiple devices. Participants expressed a desire to increase their ability to share content with household members and to increase ease of access into the app when receiving reminders.
“I don’t know if it’s possible as far as where the app is right now in development, but…another way that I think that you might be able to get some more engagement is…you’re looking at a notification…one tap or one swipe into an app to interact with the messaging that you’re receiving.” [Focus group 3 participant, October 20, 2022]
“in our house…we use a lot of active videos, especially now in the pandemic, to do exercises…We always like Chromecast them to the television or something…if there was some method possible for these videos to be cast to another device, like a larger screen or something, I think that would be awesome” [Focus group 3 participant, October 21, 2022]
Discussion
In this mixed-methods, CBPR study, we successfully recruited participants to a virtual focus group series to refine a CVH and wellness app for AAs for subsequent evaluation in a larger RCT. Despite the need for rapid transition to a virtual platform, the integrity of the study was not compromised as the focus groups had excellent participant retention and engagement. Through the virtual platform, participants provided valuable qualitative and quantitative feedback to enhance the FAITH! App. The refinement of the FAITH! App through this iterative approach resulted in favorable usability and satisfaction ratings and yielded a fully functional, culturally relevant app ready for testing in the RCT.
Our iterative process aligns well with recommended best practices for user-centered19,20 and participatory design21,22 approaches for refinement of mHealth lifestyle apps by utilizing both qualitative (focus group discussion) and quantitative (utilization of a validated instrument to assess app usability) methods. 43 Additionally, using a theoretical framework of behavioral change theory to underpin the app refinements allowed for the creation of enhanced refinements that increased participant satisfaction and motivation. In the MOYO study, researchers combined the health belief model and social cognitive theory with a CBPR approach to successfully design a CVH intervention for AA youth. 44 In their mHealth intervention to increase PA among AA women, Rodney and colleagues utilized social cognitive theory mediators to guide the data collection on the feasibility and acceptability of the intervention. Thus, our approach is in line with methods used in other mHealth usability studies for interventions among AAs12,44,45 and represents a model of a successful community–academic partnership. 17
There were several lessons learned (or recommendations) for other investigators interested in designing and refining mHealth interventions using a community-informed, user-centered process:
Use of social incentives at the individual and collective level may be effective tools to increase participant motivation and app engagement.
Updating app content and visual features may be useful to maintain app novelty for continued user engagement.
Factors that increase customizability and ease of use may further enhance user satisfaction.
Similar to our findings, an integrative review of user-centered mHealth apps, found evidence to suggest that gaming or competitive incentives are strong reinforcing factors for ongoing app use. 46 Furthermore, they reported that updating app content and visual elements within mHealth platforms may preserve novelty and sustain user engagement. 46 Newton and colleagues conducted a user feasibility study of a mHealth lifestyle app for AA men and concluded that dynamic informational content such as videos may prompt more engagement than static informational material as participants in their study had a low engagement with reading material provided through their lifestyle app. 45
Areas of future opportunity to improve the FAITH! App include increasing user customizability. At the end of the focus groups, participants expressed a strong preference for the mHealth intervention to be fully transitioned to a commercially available, native mobile app to further increase accessibility. Participants also recommended the incorporation of features to easily transmit app content to multiple devices to share with other members in their household/community. These themes suggest that participants would like to have more user control over the app. Degree of app customizability helps decrease user burden and has been shown to maintain user engagement 46 and satisfaction. 43
Lastly, the collaboration with community members in formative focus group evaluation of the FAITH! App strengthened existing relationships between researchers and participants. The FAITH! App gained further acceptability 47 within the community as it was designed for community members by community members and thus enhanced recruitment of AAs from these communities for the RCT. These are important steps toward moving the needle toward digital health equity for AAs.8,9
An unforeseen positive finding from this study was that participants found that the use of a culturally relevant mHealth lifestyle app assisted them in maintaining healthy behaviors during the COVID-19 pandemic. This was not objectively evaluated as it was beyond the scope of this study but was supportive of the value and relevance of our intervention during the current public health emergency. It is possible that concurrently conducting the virtual focus groups with access to the FAITH! App may have provided participants with additional support at a time when they are overwhelmed with multiple competing demands. The remarkably favorable feedback from participants suggests that a mHealth lifestyle app can be a potent tool to maintain CVH in times of crisis and warrants further evaluation.
Limitations
We acknowledge that our study has several limitations. Inherent to focus groups is the tendency toward participants providing socially desirable or acceptable opinions/responses within discussions. 48 We attempted to minimize this by emphasizing the importance to participants of providing feedback, whether positive or negative, on the FAITH! App components. It was reiterated at each focus group that all input would be reviewed by the study team. Further, some individuals in focus groups tend to have a dominant voice or are more vocal than others due to their comfortability with speaking in group settings. Interestingly, to our advantage, the Zoom platform facilitated contributions from all focus group participants to discussions as there were several modalities available for them to do so based on their comfort levels, preferences, and environmental settings. These included direct communication with video, audio only, and chat function features. In addition, it is acknowledged that individuals volunteering to participate in the study and those that elected to attend the actual focus group sessions may differ considerably from those who chose not to participate or not to remain as active in the series. However, another benefit to the virtual formatting was the allowance of flexibility of participants to attend the sessions within the comfort of their own homes (or preferred location) during times of social/physical distancing and mandated quarantines/shutdowns of the pandemic. This undoubtedly contributed to our excellent study participation and retention rates.
Moreover, our study was small scale. Nevertheless, since our study was qualitative in nature, the sample size fulfilled the need to garner valuable insights and feedback for further enhancement of the mHealth intervention for AAs as conducted with our prior studies.9,14,23 Another limitation is our convenience sample of AAs within faith communities in Minnesota which limits generalizability to other faith communities and AAs as a whole in other geographic areas. However, our study sample was comparable to and representative of the prioritized population of AAs within predominant AA church congregations planned for enrollment within the RCT to formally test the FAITH! App.
Conclusions
Using a formative virtual focus group process, we refined the FAITH! App intervention for application in a community-based RCT. Our approach to app refinement through a virtual focus group series during the COVID-19 pandemic contributes to the growing literature on user-centered approaches to develop and refine mHealth lifestyle interventions for AAs. Our formative process further highlights that the optimal design of mHealth interventions for racial/ethnic minority groups are potentially enhanced with a theory-based, community-engaged approach. Such approaches are crucial in the context of the pandemic to prevent the unintended magnification of the digital divide and to create effective technology-based interventions to achieve digital health equity and meet community needs.
Supplemental Material
Supplemental material, sj-docx-1-dhj-10.1177_20552076221110537 for Sign of the times: Community engagement to refine a cardiovascular mHealth intervention through a virtual focus group series during the COVID-19 Pandemic by LaPrincess C. Brewer, Jissy Cyriac, Ashok Kumbamu, Lora E. Burke, Sarah Jenkins, Sharonne N. Hayes, Clarence Jones, Lisa A. Cooper and Christi A. Patten in Digital Health
Acknowledgments
We are grateful to all of the focus group participants and participating churches for their commitment to the FAITH! initiative and using their voices to improve cardiovascular health in African-American communities. We would also like to thank Mr. Nic Breutzman for graciously providing his excellent graphic design expertise.
Footnotes
Contributorship: All authors participated intellectually or practically in this work including conception and design (Brewer, Kumbamu, Jenkins, Burke, Hayes, Patten, Cooper, and Jones), data analysis and data interpretation (Brewer, Jenkins, Cyriac, and Kumbamu), and drafting of the manuscript (Brewer, Cyriac, Jenkins, Burke, Hayes, Patten, Cooper, Kumbamu, and Jones).
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: The study was reviewed and approved by the Mayo Clinic Institutional Review Board (ID 18-006846).
Funding: This study was supported by the National Institutes of Health (NIH)/National Institute on Minority Health and Health Disparities (NIMHD) (Grant No. R21 MD013490-01), Clinical and Translational Science Awards (CTSA) (Grant No. UL1 TR000135) from the National Center for Advancing Translational Sciences (NCATS) to Mayo Clinic and the Mayo Clinic Center for Health Equity and Community Engagement in Research. Dr Brewer was supported by the American Heart Association-Amos Medical Faculty Development Program (Grant No. 19AMFDP35040005), NCATS (CTSA Grant No. KL2 TR002379), and the Centers for Disease Control and Prevention (CDC) (Grant No. CDC-DP18-1817) during the implementation of this work. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NCATS, NIH, or CDC. The funding bodies had no role in study design; in the collection, analysis, and interpretation of data; writing of the manuscript; and in the decision to submit the manuscript for publication.
Guarantor: LCB.
Informed consent: This study included human subjects and informed consent was obtained prior to study enrollment via electronic survey.
ORCID iDs: LaPrincess C. Brewer https://orcid.org/0000-0002-6468-9324
Jissy Cyriac https://orcid.org/0000-0001-6340-4254
Sharonne N. Hayes https://orcid.org/0000-0003-3129-362X
Trial registration: Not applicable, because this article does not contain any clinical trials.
Supplemental material: Supplementary material for this article is available online.
References
- 1.Pool LR, Ning H, Lloyd-Jones DM, et al. Trends in racial/ethnic disparities in cardiovascular health among US adults from 1999–2012. J Am Heart Assoc 2017; 6: 1–16. DOI: 10.1161/JAHA.117.006027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wadhera RK, Figueroa JF, Rodriguez F, et al. Racial and ethnic disparities in heart and cerebrovascular disease deaths during the COVID-19 pandemic in the United States. Circulation 2021; 143: 2346–2354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haynes N, Cooper LA, Albert MA, et al. At the heart of the matter: unmasking and addressing the toll of COVID-19 on diverse populations. Circulation 2020; 142: 105–107. [DOI] [PubMed] [Google Scholar]
- 4.Acosta AM, Garg S, Pham H, et al. Racial and ethnic disparities in rates of COVID-19-associated hospitalization, intensive care unit admission, and in-hospital death in the United States from March 2020 to February 2021. JAMA Netw Open 2021; 4: e2130479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ferdinand K, Batieste T, Fleurestil M. Contemporary and future concepts on hypertension in African Americans: COVID-19 and beyond. J Natl Med Assoc 2020; 112: 315–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ferdinand KC, Nasser SA. African-American COVID-19 mortality: a Sentinel event. J Am Coll Cardiol 2020; 75: 2746–2748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eberly LA, Khatana SAM, Nathan AS, et al. Telemedicine outpatient cardiovascular care during the COVID-19 pandemic: bridging or opening the digital divide? Circulation 2020; 142: 510–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shaw J, Brewer LC, Veinot T. Recommendations for health equity and virtual care arising from the COVID-19 pandemic: narrative review. JMIR Form Res 2021; 5: e23233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brewer LC, Fortuna KL, Jones C, et al. Back to the future: achieving health equity through health informatics and digital health. JMIR Mhealth Uhealth 2020; 8: e14512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Anderson C, Cohn S. Mobile technology and home broadband 2019. Washington, DC: Pew Research Center, June 13, 2019. [Google Scholar]
- 11.Smith A. African Americans and technology use. Washington, DC: Pew Research Center, January 6, 2014. [Google Scholar]
- 12.Joseph RP, Ainsworth BE, Hollingshead K, et al. Results of a culturally tailored smartphone-delivered physical activity intervention among midlife African American women: feasibility trial. JMIR Mhealth Uhealth 2021; 9: e27383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brewer LC, Hayes SN, Jenkins SM, et al. Improving cardiovascular health among African-Americans through Mobile health: the FAITH! App pilot study. J Gen Intern Med 2019; 34: 1376–1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brewer LC, Kumbamu A, Smith C, et al. A cardiovascular health and wellness mobile health intervention among Church-going African Americans: formative evaluation of the FAITH! App. JMIR Form Res 2020; 4: e21450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Prasanna A, Miller HN, Wu Y, et al. Recruitment of black adults into cardiovascular disease trials. J Am Heart Assoc 2021; 10: e021108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brewer LC, Pasha M, Seele P, et al. Overcoming historical barriers: enhancing positive perceptions of medical research among African Americans through a conference-based workshop. J Gen Intern Med 2021; 36: 2547–2554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wieland ML, Njeru JW, Alahdab F, et al. Community-engaged approaches for minority recruitment into clinical research: a scoping review of the literature. Mayo Clin Proc 2021; 96: 733–743. [DOI] [PubMed] [Google Scholar]
- 18.Fetters MD, Curry LA, Creswell JW. Achieving integration in mixed methods designs-principles and practices. Health Serv Res 2013; 48: 2134–2156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Norman DA, Draper SW. User centered system design: new perspectives on human-computer interaction. Hillsdale, NJ: Lawrence Earlbaum Associate, 1986. [Google Scholar]
- 20.Hermawati S, Lawson G. Managing obesity through mobile phone applications: a state-of-the-art review from a user-centred design perspective. Pers Ubiquitous Comput 2014; 18: 2003–2023. [Google Scholar]
- 21.Kushniruk A, Nøhr C. Participatory design, user involvement and health IT evaluation. Stud Health Technol Inform 2016; 222: 139–151. [PubMed] [Google Scholar]
- 22.Pilemalm S, Timpka T. Third generation participatory design in health informatics--making user participation applicable to large-scale information system projects. J Biomed Inform 2008; 41: 327–339. [DOI] [PubMed] [Google Scholar]
- 23.Brewer LC, Hayes SN, Caron AR, et al. Promoting cardiovascular health and wellness among African-Americans: community participatory approach to design an innovative mobile-health intervention. PLoS One 2019; 14: e0218724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Brewer LC, Jenkins S, Hayes SN, et al. Community-based, cluster-randomized pilot trial of a cardiovascular mHealth intervention: Rationale, design, and baseline findings of the FAITH! Trial. Am Heart J. 2022 May;247:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weinstein ND. The precaution adoption process. Health Psychol 1988; 7: 355–386. [DOI] [PubMed] [Google Scholar]
- 26.Lemacks J, Wells BA, Ilich JZ, et al. Interventions for improving nutrition and physical activity behaviors in adult African American populations: a systematic review, January 2000 through December 2011. Prev Chronic Dis 2013; 10: E99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Coughlin SS, Smith SA. Community-Based participatory research to promote healthy diet and nutrition and prevent and control obesity among African-Americans: a literature review. J Racial Ethn Health Disparities 2017; 4: 259–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McKenzie JF, Neiger BL, Thackeray R. Planning, implementing, and evaluating health promotion programs : a primer. 7th ed. Boston, MA: Pearson, 2017. [Google Scholar]
- 29.Asch DA, Rosin R. Engineering social incentives for health. N Engl J Med 2016; 375: 2511–2513. [DOI] [PubMed] [Google Scholar]
- 30.Rogers T, Milkman KL, Volpp KG. Commitment devices: using initiatives to change behavior. JAMA 2014; 311: 2065–2066. [DOI] [PubMed] [Google Scholar]
- 31.Patel MS, Benjamin EJ, Volpp KG, et al. Effect of a game-based intervention designed to enhance social incentives to increase physical activity among families: the BE FIT randomized clinical trial. JAMA Intern Med 2017; 177 (11): 1586–1593. DOI: 10.1001/jamainternmed.2017.3458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Manjunath C, Ifelayo O, Jones C, et al. Addressing cardiovascular health disparities in Minnesota: establishment of a community steering committee by FAITH! (Fostering African-American improvement in total health). Int J Environ Res Public Health 2019; 16: 1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Norman CD, Skinner HA. ehealth literacy: essential skills for consumer health in a networked world. J Med Internet Res 2006; 8: e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Richtering SS, Hyun K, Neubeck L, et al. ehealth literacy: predictors in a population with moderate-to-high cardiovascular risk. JMIR Hum Factors 2017; 4: e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brown W, III, Yen PY, Rojas M, et al. Assessment of the Health IT Usability Evaluation mModel (health-ITUEM) for evaluating mobile health (mHealth) technology. J Biomed Inform 2013; 46: 1080–1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schnall R, Cho H, Liu J. Health Information Technology Usability Evaluation Scale (Health-ITUES) for usability assessment of Mobile health technology: validation study. JMIR Mhealth Uhealth 2018; 6: e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yen PY, Wantland D, Bakken S. Development of a customizable health IT usability evaluation scale. AMIA Annu Symp Proc 2010; 2010: 917–921. [PMC free article] [PubMed] [Google Scholar]
- 38.Krueger RA, Casey MA. Focus Groups A Practical Guide for Applied Research. Fourth Edition. Thousand Oaks, CA: SAGE; 2009. [Google Scholar]
- 39.Morgan D, Krueger R, King J. Focus group kit. Thousand Oaks, CA: Sage Publications, 1998. [Google Scholar]
- 40.Patton MQ. Qualitative research and evaluation methods. Thousand Oaks, CA: Sage Publications, 2015. [Google Scholar]
- 41.Beebe J. Rapid assessment process. New York, NY: Altamira, 2001. [Google Scholar]
- 42.Bradley EH, Curry LA, Devers KJ. Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health Serv Res 2007; 42: 1758–1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Molina-Recio G, Molina-Luque R, Jimenez-Garcia AM, et al. Proposal for the user-centered design approach for health apps based on successful experiences: integrative review. JMIR Mhealth Uhealth 2020; 8: e14376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Taylor HA, Jr., Francis S, Evans CR, et al. Preventing cardiovascular disease among urban African Americans with a Mobile Health App (the MOYO App): protocol for a usability study. JMIR Res Protoc 2020; 9: e16699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Newton RL , Jr., Carter L, St Romain J, et al. Development of a mobile phone app to maintain physical activity in African American men: MobileMen. Mhealth 2019; 5: 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Birkhoff SD, Smeltzer SC. Perceptions of smartphone user-centered Mobile Health Tracking Apps across various chronic illness populations: an integrative review. J Nurs Scholarsh 2017; 49: 371–378. [DOI] [PubMed] [Google Scholar]
- 47.Sieck CJ, Rastetter M, Hefner JL, et al. The five A's of access for TechQuity. J Health Care Poor Underserved 2021; 32: 290–299. [Google Scholar]
- 48.Wilkinson S. Analysing interaction in focus groups. In: Drew P, Raymond G, Weinberg D. (eds) Talk and interaction in social research methods. London, UK: Sage Publications Ltd, 2006, pp.50–62. 10.4135/9781849209991. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-dhj-10.1177_20552076221110537 for Sign of the times: Community engagement to refine a cardiovascular mHealth intervention through a virtual focus group series during the COVID-19 Pandemic by LaPrincess C. Brewer, Jissy Cyriac, Ashok Kumbamu, Lora E. Burke, Sarah Jenkins, Sharonne N. Hayes, Clarence Jones, Lisa A. Cooper and Christi A. Patten in Digital Health