Abstract
Background
Lateral epicondylitis (LE) is a highly prevalent musculoskeletal disorder in workers, often associated with physically demanding work. Knowledge of work‐relatedness of LE is crucial to develop appropriate preventive measures. This study investigates the prospective association between work‐related physical risk factors and LE.
Methods
A systematic literature review was conducted in MedLine using PubMed from January 1, 2010 until February 16, 2021. Published reports were included if: (1) LE was clinically assessed, (2) exposure to work‐related physical risk factors was assessed, and (3) associations between LE and work‐related physical risk factors were reported in prospective studies. Quality of evidence was assessed using the Grading of Recommendations, Assessment, Development and Evaluation.
Results
In total, 318 workers with LE from a population of 5036 workers in five studies were included. Meta‐analyses revealed high‐quality evidence for associations between LE and a Strain Index (SI) score >5.1 (odds ratio [OR]: 1.75, 95% confidence interval (CI): 1.11–2.78) and moderate‐quality evidence for forearm rotation >4 h/day or forearm rotation ≥45° for ≥45% time (OR: 1.85, 95% CI: 1.10–3.10). Gripping, flexion and extension of the wrist, and repetitive movements showed no significant associations with LE.
Conclusion
High‐quality evidence was found indicating that a higher SI increased the risk of LE. Moderate‐quality evidence was found for an association between forearm rotation and LE. No associations were found between other physical risk factors and LE. Primary preventive interventions should focus on a reduction of the SI and of high forearm rotation in work.
Keywords: elbow tendinopathy, lateral epicondylitis, occupational disease, occupational exposures, occupational physician, physical risk factors, prevention, tennis elbow, workers' health
1. INTRODUCTION
Lateral epicondylitis (LE), also known as tennis elbow or lateral elbow tendinopathy, is an overuse injury of the short extensor of the wrist (extensor carpi radialis brevis), and a common cause of pain in the lateral side of the elbow. 1 , 2 The etiology of LE is not completely understood, but it is assumed that overuse leads to increased tenocyte proliferation and production of ground substance. 3
LE is most prevalent among people of working age between 20 and 65 years. 4 It is a frequently reported condition in several working populations, such as computer users, manufacturing workers, and service workers. 5 , 6 , 7 LE might become a chronic disorder, as, for example, a study of Nilson et al. showed that 54% and 55% of patients respectively still experienced pain and function loss after 2 years. 8 LE can result in loss of function, such as decreased handgrip strength. 9 As a result, LE can lead to the long‐term and frequent sick leave of workers, 10 and potential productivity loss. As recovery can take more than a year, 11 LE in workers puts a high burden on society. 12
While there are several treatment options for LE, such as corticosteroids injections and platelet‐rich plasma injections and surgery, 3 evidence on the effectiveness of these treatments is inconclusive. 3 As the majority of cases of LE are self‐limiting when the patient avoids aggravating activities, 3 , 13 the prevention of overuse that causes LE is crucial. Effective interventions to prevent work‐related LE should be based on evidence‐based risk factors. 14 This indicates that knowledge of the risk factors of LE is needed to implement appropriate preventive measures.
Recently, three systematic reviews addressed risk factors associated with LE. Sayampanathan et al. found that personal risk factors, such as female sex and having a smoking history, were associated with LE. 15 However, this study did not report on work‐related risk factors. The study of Curti et al. concluded that limited evidence was found for a causal relationship between occupational exposure to biomechanical risk factors and LE based on a qualitative best‐evidence data synthesis. 16 This review did not provide a meta‐analysis. Moreover, not only were prospective cohort studies included—one of the preferred designs in etiological studies—but case referent and cross‐sectional studies were, too. These same two limitations are applicable to the systematic review of Seidel et al., who wrote about work‐related physical risk factors. 17
Although psychosocial factors like low job control and low social support are associated with an increased risk of LE, 18 these factors are probably more so called distal factors and not directly affecting the onset of the tendinopathy. For instance, Keijsers et al. showed that there was limited and inconsistent evidence that psychological factors in work were a risk factor for LE. 3 In addition, a systematic review including prospective cohort studies, showed that psychosocial factors contributed to a much lesser extent in the onset of specific shoulder tendinitis when also correcting for biomechanical exposures. 19
Therefore, a systematic review including prospective cohort studies, assessing physical risk factors and clinically assessed LE, and meta‐analyses with evidence synthesis using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) framework 20 might shed better insight into the impact of work‐related risk factors on the onset or worsening of LE. The aim of the present systematic review is to investigate (1) which work‐related physical risk factors are prospectively associated with clinically diagnosed LE and (2) to what extent these risk factors are associated with the onset or worsening of LE.
2. METHODS
A systematic review including a meta‐analysis was performed based on the criteria of the PRISMA statement. 21 No review protocol was published.
2.1. Eligibility criteria
The following criteria for inclusion were used: the study was written in English, German, or Dutch; LE was clinically assessed; work‐related physical risk factors were described in terms of high and low physical exposure; study designs were prospective cohort studies; the association between LE and work‐related physical risk factors were described using effect estimates, or could be calculated from the data provided.
2.2. Literature search
A literature search was conducted in MedLine using PubMed from January 2010 until February 16, 2021. Several terminologies of LE and work‐related physical risk factors were combined to generate the search strategy. References of included studies were screened for additional studies to include. Table 1 shows the complete search strategy in Medline using PubMed (Table 1).
Table 1.
Search strategy in medline using Pubmed, performed on February 16th 2021
| PubMed | |
|---|---|
| Tennis elbow | (("elbow tendinopathy"[Title/Abstract] OR ("tennis elbow"[MeSH Terms] OR "elbow tendinopathy"[MeSH Terms] OR "lateral epicondylitis"[Title/Abstract] OR "elbow injur*"[Title/Abstract] OR "tennis elbow"[Title/Abstract]) OR ("elbow"[MeSH Terms] OR "elbow joint"[MeSH Terms])) |
| Work‐related risk factors | ("occupational disease*"[MeSH Terms] OR "occupational disease*"[Title/Abstract] OR "risk factor*"[MeSH Terms] OR "risk factor*"[Title/Abstract] OR "work‐related"[Title/Abstract] OR ("causality"[MeSH Terms] OR “etiology"[Title/Abstract])) OR ("psychosocial load"[Title/Abstract] OR "physical load"[Title/Abstract] OR "occupational exposure*"[Title/Abstract] OR "occupational exposure*"[MeSH Terms]) |
2.3. Study selection
After duplicates were removed by SB, all studies were screened independently by at least two of the authors. First, studies were screened by title and abstract, and studies that did not meet the inclusion criteria were excluded. Second, all remaining studies were reviewed in full text and included if they met the inclusion criteria. Disagreements (19.5%) were resolved by discussion between two authors and a third reviewer made the final decision, if necessary.
2.4. Data collection
The following data were extracted from the included studies by SB: author, year of publication, country where the study was performed, study design, length of follow‐up, definition of work‐related physical risk factors, method of assessment of work‐related physical risk factors, study population, control group, case definition of LE, method of clinical assessment of LE, and (adjusted) risk estimate in odds ratio, hazard ratio, Incidence rate ratio or relative risk, including 95% confidence intervals (95% CI) and correction for confounders. All extracted data were checked by a second author FL.
2.5. Quality assessment
The methodological quality of the study and additional physical exposure assessment was independently rated by two authors (SB and FL). For the quality assessment of the study, the checklist from the systematic review of van der Molen et al. 19 was used. The checklist covers five topics, and 16 items in total. The five topics were (1) study population (e.g., if the study population was defined), (2) assessment of exposure (e.g., if the exposure was clearly defined), (3) assessment of outcome (e.g., if the outcome was defined), (4) study design and analysis (e.g., if inclusion and exclusion criteria were clearly defined), and (5) data analysis (e.g., if risk estimate was provided). An overview of the complete checklist is shown in Appendix 1. Possible decisions on the items were (1) positive, (2) negative, or (3) unclear. Methodological quality was considered as high when at least 11 of the 16 items were judged as positive.
To assess the quality of the physical exposure assessment and the clinical outcome assessment of LE, we used the scoring system of Sulsky et al. 22 For the assessment of the physical exposure, a maximum of five points could be obtained if the exposure had a direct measurement of the elbow strain described in specific quantitative data, (e.g., applied force measurements, load weight handled, time of holding a specific elbow posture, number of repetitions per time unit), four points if measurement of the elbow strain was indirect using qualitative specifications (e.g., high repetition, awkward posture, heavy load weight) that were additionally checked through video analysis. If the qualitative specifications were not additionally checked by video analysis, three points could be obtained, and two points if the intensity (e.g., how long, or how heavy was the load weight) of the qualitative specifications were not provided (e.g., flexion/extension of the wrist or dynamic movements). The study would score one point if only the type of work was reported (e.g., manual factory worker, neurosurgeon). For the assessment of the clinical outcome, a study could obtain a maximum of three points if the assessment of LE was diagnosed by a (para) medical expert, two points if a clinical questionnaire without a clinical diagnosis was conducted, and one point if the assessment of LE was self‐reported. The complete checklist is shown in Appendix 2.
2.6. Data analysis
A meta‐analysis was performed to assess whether work‐related physical risk factors were associated with LE. A prerequisite was that at least two categories of high versus low exposure were defined in the study for each work‐related physical risk factor. In addition, at least 10 cases of LE had to be present in the high and the low exposure category to be included in the meta‐analysis, otherwise we combined two or more exposure categories when available to meet this criterion. We calculated a pooled OR and 95% CI for each work‐related physical risk factor, using I 2 as a measure of consistency in a random effects model of Cochrane's Revman 5.4. The results are presented as forest plots. No additional analyses were performed.
2.7. GRADE
We used the GRADE framework (Grading of Recommendations, Assessment, Development and Evaluation) 23 to assess the quality of evidence for the studies included in the meta‐analysis, and used the criteria of van der Molen et al. for the work‐relatedness of specific shoulder disorders as GRADE factors. 20 The quality of evidence was judged as: high, moderate, low, or very low. The starting point of evidence for each work‐related physical risk factor was high, as all included studies were prospective cohort studies seeking to confirm an independent association between risk factor and outcome. The quality of evidence was downgraded based on (1) study limitation (downgraded if a high risk of bias was present in the majority of included studies), (2) inconsistency (downgraded if I 2 was higher than 70%), (3) indirectness (downgraded if LE was not clinically diagnosed), (4) imprecision (downgraded if CI effect size was <1 and >2), and (5) publication bias (downgraded if publication bias was strongly suspected or unclear). The quality of evidence could be upgraded (if no downgrade was performed on these previous criteria), based on (1) effect size (upgraded if the OR [95% CI] of a risk factor was greater than 2.5) and (2) dose effect (upgraded if a dose effect is present in the majority of studies for that risk factor).
3. RESULTS
3.1. Study selection
The search resulted in 1042 studies. There were no duplicates. After initial screening of titles and abstracts, 29 studies remained for full text screening. In total, five studies fulfilled the inclusion criteria and were included, namely Descatha et al., 24 Fan and Bao et al., 25 Fan and Silverstein et al., 26 Garg et al., 27 and Herquelot et al. 28 (Figure 1).
Figure 1.
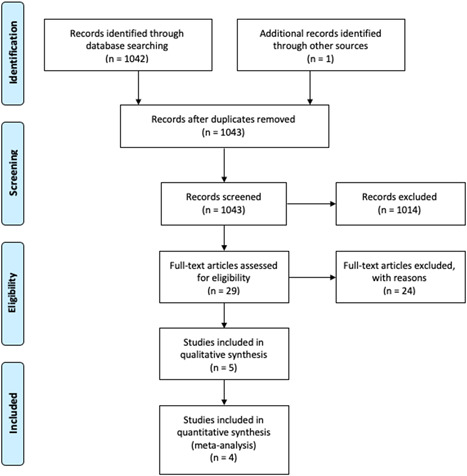
Flow diagram of included studies [Color figure can be viewed at wileyonlinelibrary.com]
3.2. Study characteristics
Of the included prospective cohort studies on work‐related physical risk factors and the incidence of LE, four studies were conducted in the United States 24 , 25 , 26 , 27 and one study was conducted in France. 28 Included workers were manufacturing workers, 24 , 25 , 26 , 27 construction, biotechnology, 24 and healthcare workers, 24 , 26 those in the service industry, 26 and workers in poultry processing. 27 The study of Herquelot et al. included skilled and unskilled blue collar workers, cleaning operatives, and healthcare assistants. 28 The total population of workers included in all studies in this review consisted of 5036 workers, of which two studies used the same population. 25 , 26 In total, 318 cases of LE were observed. LE was assessed by physical examination in all five studies. In the studies of Fan and Bao et al. and Fan and Silverstein et al., LE was diagnosed as pain in the lateral humeral epicondylar region on resisted wrist extension, or tenderness on palpation of the lateral epicondyle as occurring during physical examination. The physical examination was conducted by an occupational physician, a registered nurse, or a physical therapist, all blinded to self‐reported health status. 25 , 26 In the study of Garg et al., the physical examination investigated pain at or near the lateral epicondyle, pain upon palpation in one or more of six points when applying approximately 4 kg of force, and lateral epicondylar region pain upon either resisted wrist extension or third digit extension—all were used to diagnose LE. The physical examination was performed by a trained registered occupational therapist. 27 In the study of Herquelot et al. physical examinations were performed by occupational physicians using the methodology and clinical tests of the Saltsa consensus document of LE. 28 Finally, in the study of Descatha et al. a physical examination was conducted, however, the characteristics of the examiner were not mentioned. 24 (complete overview of data extraction is shown in Appendix 3).
Two studies assessed the association between the exposure of wrist flexion and extension 24 , 26 and LE. Two studies assessed both the exposure of forearm rotation 24 , 26 and of tasks including hand gripping and pinch grip force, and the incidence of LE. 24 , 26 Two studies assessed the association between repetitive tasks and the incidence of LE. 25 , 27 Finally, two studies assessed the association between a high score on the Strain Index (SI) and the incidence of LE. 25 , 27
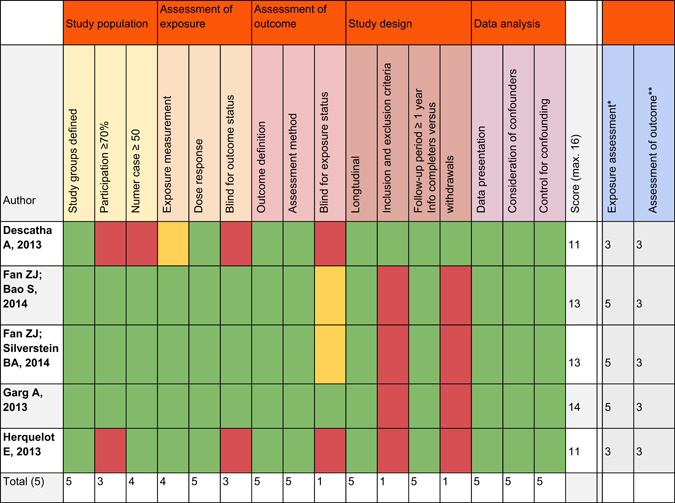
3.3. Quality of studies (methodological quality)
The quality score of the studies ranged from 11 to 14 points in total, indicating that all studies had a high methodological quality (Table 2). The initial agreement between the two raters was 81%. The study by Garg et al. had the highest quality score of 14 out of 16 points in total. 27 Inclusion and exclusion criteria and information about possible withdrawals were not reported by all studies, except for the study of Descatha et al. 24
Table 2.
Results quality assessment of the studies and of the physical exposure and clinical outcome lateral epicondylitis
|
3.4. Quality assessment of physical exposure and assessment of outcome
The quality of the physical exposure assessment in all five studies was high, namely six to eight points in total (Table 2, last two columns). Two studies used questionnaires to measure work‐related physical risk factors. 24 , 28 Three studies scored the maximum amount of five points. They used videotape analyses to measure the exposure of work‐related physical risk factors. 25 , 26 , 27 All studies scored the maximum number of points for the clinical assessment of LE, given this was an inclusion criterion in our review. 24 , 25 , 26 , 27 , 28 (Table 2, last two columns).
3.5. Meta‐analysis and GRADE
For the following five work‐related physical risk factors, a meta‐analysis and assessment of the GRADE criteria was performed: flexion and extension movements of the wrist, forearm rotation, (pinch) gripping, repetitive movements, and SI. Details of the assessment of the GRADE framework are presented in Table 4.
Table 4.
Grading of Recommendations Assessment Development and Evaluations (GRADE) framework for the work‐related physical risk factors for lateral epicondylitis
| Work‐related physical risk factor | Number of participants (number of Incident cases of LE) | Prospective cohort studies |
Phase of investigation 1=explorative ↓ 2/3=explanatory |
Study limitations risk of bias across studies↓ | Inconsistency (i 2 >70%)↓ |
Indirectness Diagnosis not clinically assessed↓ |
Imprecision CI effect size (<1 and >2) Yes↓ |
Publication bias strongly suspected Yes ↓ |
Effect size OR>2.5↑ |
Dose effect Majority of studies↑ |
Certainty |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Flexion/extension wrist 24 , 26 | 1452 (87) | 2/2 | 2 | 1/2↓ | 85%↓ | 0/2 | 1.61 [0.47 – 5.52] ↓ | Not detected | 1.61 | N.a. | Very low |
| Forearm rotation 24 , 26 | 1307 (80) | 2/2 | 2 | 1/2↓ | 14% | 0/2 | 1.85 [1.10 – 3.10] | Not detected | 1.85 | N.a. | Moderate |
| (Pinch) gripping 24 , 26 | 1264 (78) | 2/2 | 2 | 1/2↓ | 70%↓ | 0/2 | 0.96 [0.36 – 2.55] ↓ | Not detected | 0.96 | N.a. | Very low |
| Repetitive movements 25 , 27 | 1083 (93) | 2/2 | 2 | 0/2 | 0% | 0/2 | 0.71 [0.42 – 1.20] | Not detected | 0.71 | N.a. | High |
| Strain Index 25 , 27 | 1252 (113) | 2/2 | 2 | 0/2 | 0% | 0/2 | 1.75 [1.11 – 2.78] | Not detected | 1.75 | N.a. | High |
Abbreviations: CI, confidence interval; OR, odds ratio.
3.6. Flexion and extension of the wrist
The meta‐analyses showed, based on two studies, 24 , 26 that there was very low‐quality evidence that high exposure to flexion and extension movements of the wrist was not significantly associated with an increased risk of the onset of LE (OR: 1.61, 95% CI: 0.47–5.52) (Figure 2) (Table 4). High exposure to flexion was defined as bending more than 4 h a day, or wrist flexion and extension ≥15° for ≥40% time (Table 3).
Figure 2.
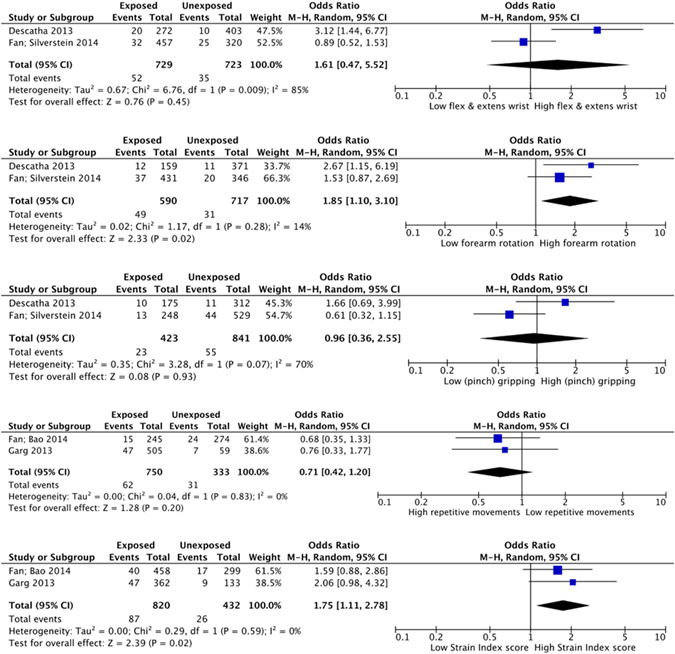
Forest plots of the five work‐related physical risk factors for developing lateral epicondylitis [Color figure can be viewed at wileyonlinelibrary.com]
Table 3.
Definition of the high versus low exposure groups as used in the meta‐analysis
| Work‐related physical risk factors | High exposure (n: lateral epicondylitis) | Low exposure (n: lateral epicondylitis) | OR | 95% CI |
|---|---|---|---|---|
| Flexion and extension wrist |
Bending: more than 4 h a day 24 (272:20) Wrist flexion/extension ≥15° for ≥40% time 26 (457:32) |
Bending: no or <1, 1–2, 2–4 h a day 24 (403:10) Wrist flexion/extension ≥15° for <40% time 26 (320:25) |
1.61 | 0.47–5.52 |
| Forearm rotation |
Rotating more than 4 h a day 24 (159:12) Forearm rotation ≥45° for ≥45% time 26 (431:37) |
Rotating no or <1 h a day 24 (371:11) Forearm rotation ≥45° for <45% time 26 (346:20) |
1.85 | 1.10–3.10 |
| (Pinch) gripping |
Gripping for more than 4 h a day 24 (175:10) Any pinch grip force 26 (248:13) |
No gripping 24 (312:11) No pinch grip 26 (529:44) |
0.96 | 0.36–2.55 |
| Repetitive movements |
>15 efforts per minute 25 (245:15) >15 efforts per minute 27 (505:47) |
<9 efforts per minute 25 (274:24) <9 efforts per minute 27 (59:7) |
0.71 | 0.42–1.20 |
| Strain Index |
SI ≥ 5 25 (458: 40) SI ≥ 6.1 27 (362:47) |
SI < 5 25 (299:17) SI < 6.1 27 (133:9) |
1.75 | 1.11–2.78 |
Abbreviations: CI, confidence interval; OR, odds ratio.
3.7. Forearm rotation
The meta‐analysis showed, based on two studies, 24 , 26 that there was moderate quality evidence that forearm rotation was significantly associated with an increased risk of the onset of LE (OR: 1.85, 95% CI: 1.10–3.10) (Figure 2) (Table 4). High exposure was defined as the forearm rotating more than 4 h a day, or forearm rotation ≥45° for ≥45% time (Table 3).
3.8. (Pinch) gripping
The meta‐analysis showed that based on two studies, 24 , 26 there was very low‐quality evidence that high exposure of (pinch) gripping was not significantly associated with increased risk of the onset of LE (OR: 0.96, 95% CI: 0.36–2.55 (Figure 2) (Table 4). High exposure was defined as gripping for more than 4 h a day or any pinch grip force (Table 3).
3.9. Repetitive movements
The meta‐analysis showed, based on two studies, 25 , 27 that there was high quality evidence that high exposure to repetitive movements was not significantly associated with LE (OR: 0.71, 95% CI: 0.42–1.20) (Figure 2) (Table 4). High exposure was defined as more than 15 efforts per minute (Table 3).
3.10. SI
The meta‐analysis showed, based on two studies, 25 , 27 that there was high‐quality evidence that a high score, according to the SI, was significantly associated with an increased risk of the onset of LE (OR: 1.75, 95% CI: 1.11–2.78) (Figure 2) (Table 4). High exposure was defined as a SI higher than 6.1 or SI higher than 5.0 (Table 3).
4. DISCUSSION
This review, including meta‐analyses, showed high‐quality evidence for a prospective association between a high score on the SI and LE, and moderate‐quality evidence for an association between high exposure to forearm rotation and LE among workers. No significant associations were found for high exposure to wrist flexion and extension, pinch‐ gripping, or repetitiveness of movements for an increased risk of LE.
Applying the Bradford Hill criteria for causation, 29 the risk estimates for the association between physical exposure and LE were substantial (strength of association) and present among large and various working populations (consistency) for clinically assessed LE (specificity). All studies were prospective (temporality) and two studies 25 , 27 showed biological gradients, namely the presence of a dose‐response relationship.
Although previous systematic reviews did find an effect for repetitiveness, 17 , 18 our meta‐analysis showed that repetitiveness was not significantly associated with LE. In our meta‐analysis of repetitiveness, we used results from the two studies using the SI, in which high exposure was defined as more than 15 efforts per minute, and low exposure less than nine efforts per minute. 25 , 27 A possible explanation is that data included under the category of low repetitiveness included tasks with heavy loads, which is more likely to lead to an increased risk of LE, and as a result, reduced the significance of association for high‐ versus low‐ repetitiveness of movement.
The meta‐analysis also showed significant associations between high exposure to forearm rotation, and an increased risk of LE. This finding is supported by results from cadaver studies showing that forearm pronation led to significantly higher bone‐to‐tendon contact, which is considered to be one of the causes of LE. 30
While no significant association for repetitiveness and LE was found, our meta‐analysis showed that a high score on the SI was significantly associated with LE, and the strength of evidence was the highest of all pooled estimates, according to the GRADE framework. The SI consists of three quantitative variables: (1) duration of exertion, (2) number of exertions, and (3) duration of a task per day, and three qualitative variables relying on an analysist's judgement: (1) intensity of exertion, (2) hand/wrist posture, and (3) speed of work. Based on given scores, each task is assigned a rating between one and five, in which one is assigned to the lowest‐scoring category and five to the highest‐scoring category of the variable. Finally, depending on the assigned rating of the task, each task is assigned to a unique multiplier, and the SI is calculated by multiplying these six multipliers. 31 As high exposure to wrist flexion and extension, repetitiveness, and (pinch) grip were not significantly associated with LE, the intensity and duration of exertion might be important determinants for risk of LE. Future research should investigate these different elements of SI and thresholds to determine the most appropriate risk factor for preventive interventions in the workplace. In addition, a revised SI has been developed in which categorical multipliers are replaced by continuous multipliers. Future studies investigating risk factors of LE might benefit from the use of this revised SI. 32
The study of Curti et al. also described a positive association between SI and LE. 16 In addition, Descatha et al. also performed a systematic review and meta‐analysis on work‐related physical risk factors for LE, including prospective cohort studies only, 7 and found a significant association for overall biomechanical exposure involving the wrist and/or elbow and risk of LE. Although our search was performed until 2021, we did not find any additional prospective cohort studies, but conducted meta‐analyses for five different biomechanical factors and assessed the strength of each meta‐analysis with GRADE.
4.1. Methodological considerations
Assuming that the onset of LE is caused by overuse, and an earlier study showed that the evidence on psychosocial risk factors for LE was limited, 3 we did not include psychosocial factors in our study. However, the role of psychosocial work‐related factors cannot be ruled out in the etiology of LE, 18 and should be taken into account in prevention and treatment.
The search for this systematic review was only conducted in the Medline database, using PubMed as a database that is more focused on clinically assessed conditions. However, since recommendations are to conduct a search in more than one database 33 this might be a limitation of the study. Nevertheless, to make sure we did not miss relevant articles, we also looked for additional studies in the references of the included studies. Moreover, as recently similar systematic reviews on risk factors for LE were published, we checked the references of these systematic review articles too, and found that all relevant studies were also shown in the results of our search in PubMed.
A strength of this review is that we included only prospective cohort studies, as they enable a better distinction between exposure and effect. 14 In addition, we performed a meta‐analysis and used the GRADE framework for assessment of the quality of evidence. 20
In this review, we only included studies with LE as clinical diagnosis, which is also considered a strength. However, clinical case definitions and physical examination differed between included studies, indicating a standardized or harmonized clinically method of diagnosing LE 34 is still lacking in prospective work‐related studies. Future studies on LE should preferably use harmonized case definitions. 35
Another strength of this review is the extensive assessment of the quality of evidence, including the assessments of physical exposure. 22 Using the scoring system of Sulsky, 22 it appeared that the majority of included studies used direct measurement of elbow strain with quantitative data, and therefore yielded the highest score for quality of assessment of physical exposure. However, Stock et al. showed that self‐reported questions on physical effort had good agreement for validity with reference methods. 36 This result shows that for some exposure variables, self‐reports are valid to assess physical demands at work.
A final limitation could be in the existance of three reviews within the last 10 years on this topic. However, we compared the outcomes of these reviews and further unraveled the separate contribution of each risk factor based on quantitative data.
4.2. Future research and practical implications
Exposures combining SI and forearm rotationshould be especially targeted at worksites to reduce the risk of LE. Working populations like neurosurgeons, 37 fruit‐tree farmers, 38 coalminers, 39 and nursery cooks 40 are all examples of jobs in which physical exposure plays an important factor, and therefore, are jobs with a high risk for LE. In contrast, workers in jobs which are characterized by predominantly low force repetitiveness without extreme forearm rotation appear less likely to be at risk for LE. As no new evidence has emerged since 2014, prospective cohort studies and preventive activities should particularly focus on factors arising from high SI and forearm rotation.
We conclude from this meta‐analysis that work‐related physical risk factors involving the wrist or elbow might be associated with LE. High‐quality evidence was found for significant associations between a high score on the SI and the risk of LE, and moderate‐quality evidence was found for high exposure to forearm rotation and LE. Furthermore, no significant associations were found for high exposure to wrist flexion and extension, repetitiveness of movements, and (pinch) grip in work. Occupational physicians should be aware of the possible work‐related physical risk factors for LE, and preventive measures should be focused on reducing exposure to high‐risk factors for LE, such as forearm rotation at work.
CONFLICTS OF INTEREST
The authors declare that there are no conflicts of interest.
DISCLOSURE BY AJIM EDITOR OF RECORD
John Meyer declares that he has no conflict of interest in the review and publication decision regarding this article.
AUTHOR CONTRIBUTIONS
Henk F. van der Molen and P. Paul F. M. Kuijer were involved in conception of the work. Henk F. van der Molen, P. Paul F. M. Kuijer, S. Fransje Bretschneider, Denise Eygendaal, and Felicia S. Los were involved in acquisition, analysis, and interpretation of the data, S. Fransje Bretschneider and Felicia S. Los made the draft, and P. Paul F. M. Kuijer, Henk F. van der Molen, and Denise Eygendaal revised the draft. All authors read and approved the final version to be published. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity are investigated or resolved.
Supporting information
Supporting information.
Supporting information.
Supporting information.
ACKNOWLEDGMENT
Grant sponsor: the Ministry of Social Affairs and Employment, the Netherlands. Grant number: 5100‐26151
Bretschneider SF, Los FS, Eygendaal D, Kuijer PPFM, Molen HF. Work‐relatedness of lateral epicondylitis: Systematic review including meta‐analysis and GRADE work‐relatedness of lateral epicondylitis. Am J Ind Med. 2022;65:41‐50. 10.1002/ajim.23303
S. Fransje Bretschneider and Felicia. S. Los shared first authorship.
DATA AVAILABILITY STATEMENT
The data that supports the findings of this study are available in the supplementary material of this article
REFERENCES
- 1. Shiri R, Viikari‐Juntura E, Varonen H, Heliövaara M. Prevalence and determinants of lateral and medial epicondylitis: a population study. Am J Epidemiol. 2006;164(11):1065‐1074. [DOI] [PubMed] [Google Scholar]
- 2. Roquelaure Y, Ha C, Leclerc A, et al. Epidemiologic surveillance of upper‐extremity musculoskeletal disorders in the working population. Arthritis Rheum. 2006;55(5):765‐778. [DOI] [PubMed] [Google Scholar]
- 3. Keijsers R, de Vos RJ, Kuijer PPF, van den Bekerom MP, van der Woude HJ, Eygendaal D. Tennis elbow. Shoulder Elbow. 2019;11(5):384‐392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sanders TL Jr., Maradit Kremers H, Bryan AJ, Ransom JE, Smith J, Morrey BF. The epidemiology and health care burden of tennis elbow: a population‐based study. Am J Sports Med. 2015;43(5):1066‐1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. da Costa JT, Baptista JS, Vaz M. Incidence and prevalence of upper‐limb work related musculoskeletal disorders: a systematic review. Work. 2015;51(4):635‐644. [DOI] [PubMed] [Google Scholar]
- 6. van der Molen HF, Hulshof CT, Kuijer PPF. How to improve the assessment of the impact of occupational diseases at a national level? The Netherlands as an example. Occup Environ Med. 2019;76(1):30‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Descatha A, Albo F, Leclerc A, et al. Lateral epicondylitis and physical exposure at work? A review of prospective studies and meta‐analysis. Arthritis Care Res (Hoboken). 2016;68(11):1681‐1687. [DOI] [PubMed] [Google Scholar]
- 8. Nilsson P, Baigi A, Swärd L, Möller M, Månsson J. Lateral epicondylalgia: a structured programme better than corticosteroids and NSAID. Scand J Occup Ther. 2012;19(5):404‐410. [DOI] [PubMed] [Google Scholar]
- 9. Dilek B, Batmaz I, Sarıyıldız MA, et al. Kinesio taping in patients with lateral epicondylitis. J Back Musculoskelet Rehabil. 2016;29(4):853‐858. [DOI] [PubMed] [Google Scholar]
- 10. Walker‐Bone K, Palmer KT, Reading I, Coggon D, Cooper C. Occupation and epicondylitis: a population‐based study. Rheumatology (Oxford). 2012;51(2):305‐310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bot SD, van der Waal JM, Terwee CB, van der Windt DA, Bouter LM, Dekker J. Course and prognosis of elbow complaints: a cohort study in general practice. Ann Rheum Dis. 2005;64(9):1331‐1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Degen RM, Conti MS, Camp CL, Altchek DW, Dines JS, Werner BC. Epidemiology and disease burden of lateral epicondylitis in the USA: analysis of 85,318 patients. HSS J. 2018;14(1):9‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bisset L, Coombes B, Vicenzino B. Tennis elbow. BMJ Clin Evid. 2011;2011:2011. [PMC free article] [PubMed] [Google Scholar]
- 14. van der Beek AJ, Dennerlein JT, Huysmans MA, et al. A research framework for the development and implementation of interventions preventing work‐related musculoskeletal disorders. Scand J Work Environ Health. 2017;43(6):526‐539. [DOI] [PubMed] [Google Scholar]
- 15. Sayampanathan AA, Basha M, Mitra AK. Risk factors of lateral epicondylitis: a meta‐analysis. Surgeon. 2020;18(2):122‐128. [DOI] [PubMed] [Google Scholar]
- 16. Curti S, Mattioli S, Bonfiglioli R, Farioli A, Violante FS. Elbow tendinopathy and occupational biomechanical overload: a systematic review with best‐evidence synthesis. J Occup Health. 2021;63(1):e12186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Seidel DH, Ditchen DM, Hoehne‐Hückstädt UM, Rieger MA, Steinhilber B. Quantitative measures of physical risk factors associated with work‐related musculoskeletal disorders of the elbow: a systematic review. Int J Environ Res Public Health. 2019;16(1):130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. van Rijn RM, Huisstede BM, Koes BW, Burdorf A. Associations between work‐related factors and specific disorders at the elbow: a systematic literature review. Rheumatology (Oxford). 2009;48(5):528‐536. [DOI] [PubMed] [Google Scholar]
- 19. van der Molen HF, Foresti C, Daams JG, Frings‐Dresen MHW, Kuijer P. Work‐related risk factors for specific shoulder disorders: a systematic review and meta‐analysis. Occup Environ Med. 2017;74(10):745‐755. [DOI] [PubMed] [Google Scholar]
- 20. Guyatt GH, Oxman AD, Schünemann HJ, Tugwell P, Knottnerus A. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol. 2011;64(4):380‐382. [DOI] [PubMed] [Google Scholar]
- 21. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. BMJ. 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sulsky SI, Carlton L, Bochmann F, et al. Epidemiological evidence for work load as a risk factor for osteoarthritis of the hip: a systematic review. PLOS One. 2012;7(2):e31521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Huguet A, Hayden JA, Stinson J, et al. Judging the quality of evidence in reviews of prognostic factor research: adapting the GRADE framework. Syst Rev. 2013;2:71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Descatha A, Dale AM, Jaegers L, Herquelot E, Evanoff B. Self‐reported physical exposure association with medial and lateral epicondylitis incidence in a large longitudinal study. Occup Environ Med. 2013;70(9):670‐673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Fan ZJ, Bao S, Silverstein BA, Howard NL, Smith CK, Bonauto DK. Predicting work‐related incidence of lateral and medial epicondylitis using the strain index. Am J Ind Med. 2014;57(12):1319‐1330. [DOI] [PubMed] [Google Scholar]
- 26. Fan ZJ, Silverstein BA, Bao S, Bonauto DK, Howard NL, Smith CK. The association between combination of hand force and forearm posture and incidence of lateral epicondylitis in a working population. Hum Factors. 2014;56(1):151‐165. [DOI] [PubMed] [Google Scholar]
- 27. Garg A, Kapellusch JM, Hegmann KT, et al. The strain index and TLV for HAL: risk of lateral epicondylitis in a prospective cohort. Am J Ind Med. 2014;57(3):286‐302. [DOI] [PubMed] [Google Scholar]
- 28. Herquelot E, Guéguen A, Roquelaure Y, et al. Work‐related risk factors for incidence of lateral epicondylitis in a large working population. Scand J Work Environ Health. 2013;39(6):578‐588. [DOI] [PubMed] [Google Scholar]
- 29. Hill AB. The environment and disease: association or causation? Proc R Soc Med. 1965;58(5):295‐300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Tanaka Y, Aoki M, Izumi T, Wada T, Fujimiya M, Yamashita T. Effect of elbow and forearm position on contact pressure between the extensor origin and the lateral side of the capitellum. J Hand Surg Am. 2011;36(1):81‐88. [DOI] [PubMed] [Google Scholar]
- 31. Moore JS, Garg A. The Strain Index: a proposed method to analyze jobs for risk of distal upper extremity disorders. Am Ind Hyg Assoc J. 1995;56(5):443‐458. [DOI] [PubMed] [Google Scholar]
- 32. Garg A, Moore JS, Kapellusch JM. The Revised Strain Index: an improved upper extremity exposure assessment model. Ergonomics. 2017;60(7):912‐922. [DOI] [PubMed] [Google Scholar]
- 33. Bramer WM, Rethlefsen ML, Kleijnen J, Franco OH. Optimal database combinations for literature searches in systematic reviews: a prospective exploratory study. Syst Rev. 2017;6(1):245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Vaquero‐Picado A, Barco R, Antuña SA. Lateral epicondylitis of the elbow. EFORT Open Rev. 2016;1(11):391‐397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. van der Molen HF, Visser S, Alfonso JH, et al. Diagnostic criteria for musculoskeletal disorders for use in occupational healthcare or research: a scoping review of consensus‐ and synthesised‐based case definitions. BMC Musculoskelet Disord. 2021;22(1):169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Stock SR, Fernandes R, Delisle A, Vézina N. Reproducibility and validity of workers' self‐reports of physical work demands. Scand J Work Environ Health. 2005;31(6):409‐437. [DOI] [PubMed] [Google Scholar]
- 37. Polat O, Tuncer C, Kati YA, Uckun OM, Er U. Investigation of lateral epicondylitis in neurosurgeons. Turk Neurosurg. 2019;29(3):414‐419. [DOI] [PubMed] [Google Scholar]
- 38. Kim M, Yoo JI, Kim MJ, Na JB, Lee SI, Park KS. Prevalence of upper extremity musculoskeletal diseases and disability among fruit tree farmers in Korea: cross‐sectional study. Yonsei Med J. 2019;60(9):870‐875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Özdolap S, Emre U, Karamercan A, Sarikaya S, Köktürk F. Upper limb tendinitis and entrapment neuropathy in coal miners. Am J Ind Med. 2013;56(5):569‐575. [DOI] [PubMed] [Google Scholar]
- 40. Ono Y, Nakamura R, Shimaoka M, et al. Epicondylitis among cooks in nursery schools. Occup Environ Med. 1998;55(3):172‐179. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Supporting information.
Supporting information.
Data Availability Statement
The data that supports the findings of this study are available in the supplementary material of this article


