Abstract
Numerous measures were implemented to contain the COVID‐19 pandemic. Adhering to these measures as well as getting vaccinated is associated with subjective costs and benefits. Since young people like university students largely feel less vulnerable to the virus, other costs and benefits than health might be more decisive for them. This article combines the results of a qualitative and a quantitative longitudinal study conducted with university students mainly living in Tyrol, Austria. The studies focused on the second wave of infections of the COVID‐19 pandemic. Health concerns, altruistic concerns, worrying about the economic consequences of the measures and reactance played an important role for students in deciding what measures to follow and their vaccination attitudes. The effects were partially mediated by understanding the measures' necessity. Qualitative results enabled further insights into thought processes during these decisions and revealed additional aspects, such as concerns about mental health consequences. This research suggests that students make their decisions about adherence and vaccinations based on a variety of aspects that they weigh against each other. Understanding the individual assessments of costs and benefits is crucial to promote both adherence to the measures against the COVID‐19 pandemic and vaccination readiness.
Keywords: adherence, compliance, COVID‐19, university students, vaccination attitudes
INTRODUCTION
Following the global spread of SARS‐CoV‐2 and the associated disease COVID‐19, measures were taken to contain its transmission. Non‐pharmaceutical interventions were implemented for this purpose, such as curfews, contact restrictions, social distancing and wearing of face masks. With the spread of new SARS‐CoV‐2 variants, maintaining these measures becomes even more crucial (Grubaugh et al., 2021). Successful implementation of such measures requires profound behavioural changes (van Bavel et al., 2020) that are largely based on voluntary adherence (Bodas & Peleg, 2020; Clark et al., 2020). Compared with compliance, adherence is based more strongly on communication, collaboration and common goals (Gould & Mitty, 2010). Both terms stem from the medical field with compliance indicating a patient–clinician relationship in which clinicians instruct patients how to contribute to the treatment procedure (Tilson, 2004). Adherence, contrarily, represents a more modern approach based on cooperation and equal footing in decision‐making processes. In this article, we use the term ‘adherence’ to emphasise the participants' active role when deciding to adhere to COVID‐19 measures.
Adherence to non‐pharmaceutical interventions can be influenced by several factors and trade‐offs between them (Moya et al., 2020; Teasdale et al., 2014; Wang et al., 2021). Interpreting a disease as a threat to one's health is a critical determinant of health behaviours (Ferrer & Klein, 2015), so health concerns—regarding oneself and others—are an important predictor for adherence (Smith et al., 2020; Wang et al., 2021). Additionally, a sense of social obligation (Wang et al., 2021; Williams et al., 2020) and empathy (Pfattheicher et al., 2020) are associated with increased adherence during the COVID‐19 pandemic. These factors promoting adherence are weighed against personal and societal costs by individuals (Moya et al., 2020; Wang et al., 2021). In qualitative surveys, the economic consequences of non‐pharmaceutical interventions are often mentioned as inhibiting adherence (Baum et al., 2009; Teasdale et al., 2014). In this sense, people show increased adherence when provided with financial compensation during quarantines and lockdowns (Bodas & Peleg, 2020; Wright et al., 2020), and financial losses are a negative predictor for individual adherence (Smith et al., 2020; Webster et al., 2020). As the crisis prolongs, some people additionally worry about their mental health when adhering to the measures that largely rely on contact restrictions. These mental health concerns are associated with decreased adherence (Smith et al., 2020). The measures cause disruptions in everyday life and conflicts between public interests and basic individual rights like freedom of movement (Baum et al., 2009). The crisis thereby causes a cooperative dilemma as some people bear higher costs while benefitting less from adhering (Moya et al., 2020). Furthermore, some measures, like wearing masks, are uncomfortable for the individual and therefore rejected (Teasdale et al., 2014). Individuals likely assess the risks of infection, both for themselves and others, and weigh the advantages and disadvantages of adherence.
Since the approval of the first vaccines against COVID‐19 at the end of 2020, vaccination readiness has been the second crucial factor in containing the spread of the virus. Similar to adherence, attitudes towards vaccination are more positive if health concerns are more intense (Brewer et al., 2007). People are more willing to get vaccinated when they feel vulnerable to the disease and expect the vaccine to protect them (Zampetakis & Melas, 2021). Although the primary reason for getting vaccinated is to protect oneself, altruistic motives are also relevant. This is especially true for people with little risk for a serious course of illness in case of infection (Vietri et al., 2012), like most young people when they get infected with SARS‐CoV‐2.
Another aspect that makes young people a relevant group during the COVID‐19 pandemic is that they are severely affected by the measures. University students are in a developmental stage marked by profound changes and variability (Arnett, 2000; Shanahan, 2000) that makes them particularly sensitive to societal problems. With most universities switching from in‐classroom teaching to distance learning and the prohibition of social gatherings, the students' everyday lives significantly changed. At the same time, media reports accuse them of behaving ruthlessly by not complying with the measures and thereby threatening the wellbeing and lives of elderly and vulnerable people, and in studies, younger age is associated with less adherence (Bodas & Peleg, 2020; Wang et al., 2021). Simultaneously, young people largely state that they worry about vulnerable people (Elmer et al., 2020; Son et al., 2020).
The present study
In this paper, we examine adherence and vaccination attitudes of university students and their perception on costs and benefits of these behaviours focusing on the second wave of SARS‐CoV‐2 infections. We hypothesised that concerns about COVID‐19, such as health concerns and altruistic concerns, are associated with increased adherence. We further hypothesised that the apprehension of negative economic or mental health effects and experiencing the measures as being highly disruptive for their everyday lives are associated with decreased adherence. Concerning vaccination attitudes, health and altruistic concerns were expected to be associated with more positive attitudes towards vaccination. Regarding the effects of the apprehension of the measures' economic and mental health consequences and reactance on vaccination attitudes, there were two potential directions. If people fear consequences and feel strongly restricted in their everyday lives, they should have more positive attitudes towards vaccination because of being more interested in the pandemic to end compared with people reporting fewer worries. However, low adherence could be a sign of generally rejecting all measures based on perceiving them as unnecessary or excessive. That way, reactance and the apprehension of consequences of the measures could be associated with less positive vaccination attitudes. We combined quantitative and qualitative data to comprehensively understand young adults' perceptions and assessments of the governmental measures to contain the pandemic. Additionally, we analysed changes in the course of the pandemic by comparing adherence during the first and second wave of SARS‐CoV‐2 infections.
METHOD
This article connects data from a quantitative and a qualitative study. They were merged in the analysis. The focus of this article lies on cross‐sectional data collected during the second wave of SARS‐CoV‐2 infections. Additionally, both studies had a longitudinal design, which allowed to compare adherence during the first and second wave of the pandemic.
For the quantitative study, we conducted standardised online surveys and invited German‐speaking university students to participate. The study has a longitudinal design with multiple data collection points over the course of the COVID‐19 pandemic. Data collection coincided with waves of infections and tightening and lifting of lockdowns. The first survey took place between 20 and 30 April 2020. Between 23 November and 21 December 2020, another survey was conducted. Students for both data collection points were recruited via the mailing systems of two universities in Innsbruck, Austria, and an additional mailing list of students interested in participating in social surveys. The surveys were advertised by stating that the study aims at investigating university students' situation during the COVID‐19 crisis regarding their mental wellbeing as well as their opinions and attitudes concerning the crisis. The focus of this article is on the data collection in November and December 2020. The quantitative sample in this survey included 614 students with no missing data. Among these, 432 (70%) were female, 180 (29%) were male and two students did not identify with those categories. The mean age was 23.25 years (SD = 4.83). Most students lived in Austria (82%) and in Germany (10%). Of those 614 students, 101 had also participated in the first survey. Data of these students were used for additional longitudinal analysis comparing the first and second wave of the COVID‐19 pandemic.
The second study implemented a qualitative approach including written narratives (Atkinson, 1998). The first data collection phase took place between 1 and 7 April 2020. Social media and snowball systems were used to recruit participants enrolled at universities in Tyrol, Austria, and aged 18 years or older. The study was advertised as researching the impact of the pandemic on young adults in their educational phase and aiming at providing insights for developing interventions for future pandemics. The same students repeatedly participated in the study and wrote several narratives during the COVID‐19 crisis. In this article, we focused on written narrative data collected from 16 to 22 November 2020. A total of 67 university students participated, with 49 (73%) being female and 18 (27%) being male. For comparison of the first and second wave of the pandemic, narratives collected in November 2020 were contrasted with narratives in April 2020. Data collection was supported by student researchers who received extensive training in methods, standards of good scientific practice and research ethics. Information on counselling services was provided to counteract possible negative psychological impacts of the deep engagement with problems and difficulties during the COVID‐19 crisis.
The pandemic situation during the survey period
We focused on data collected during November and December 2020, as this time marks the ‘second wave’ of SARS‐CoV‐2 infections in Austria and neighbouring countries. The numbers of infections rose higher than during the first wave in spring 2020. Governments reacted by implementing strict measures like social distancing and curfews. Figure 1 presents the situation in Austria. We assumed that this period marked the optimal context to assess adherence to measures as students had gained ‘practical experience’ with the pandemic situation and measures were no longer new to them. Additionally, at the beginning of November, the first vaccine was announced to have the efficacy of over 90% in a Phase III trial (BioNTech, 2020), which gave the prospect to end the pandemic; however, it was approved in the European Union only after the data collection (European Medicines Agency, 2020). Using longitudinal analyses, we compared the results during this second wave of SARS‐CoV‐2 infections with data collected during the first wave of infections and the first lockdown in spring 2020. Both data collection points coincided with higher infection rates and restrictions in everyday life to detain the spread of the virus.
FIGURE 1.
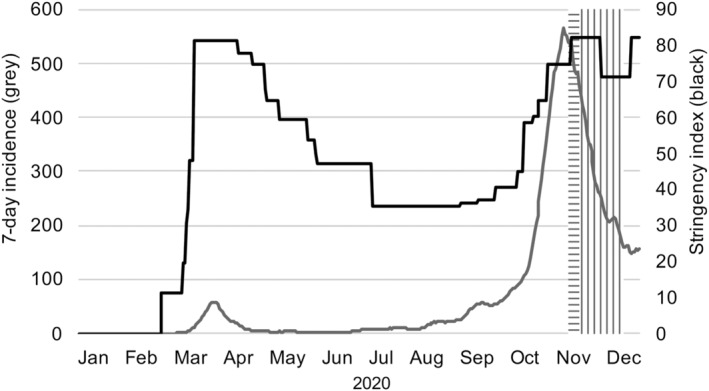
The pandemic situation in Austria during the survey period. Note: Horizontal stripes = qualitative data collection period; vertical stripes = quantitative data collection period. 7‐day incidence according to AGES (2021), stringency of measures according to the Oxford COVID‐19 government response tracker (Hale et al., 2021)
Quantitative measures
Attitudes towards COVID‐19 measures
At the beginning of data collection in April 2020, we developed four items to assess adherence to COVID‐19 measures. These items were rated on a five‐point Likert response format (1 [does not apply at all] to 5 [fully applies]) and used throughout the subsequent surveys. To allow a deeper analysis of adherence and its predictors, we included additional items for the data collection in November and December 2020, considering the aspects of following governmental rules and taking own precautions to prevent infection. We developed items based on media reports, official recommendations and the COSMO study (Betsch et al., 2020). Overall, 14 items were developed. Factor analysis yielded a three‐factorial structure of this questionnaire: (1) understanding of the measures (six items, Cronbach's α = .85, e.g. ‘I think the measures are appropriate.’), (2) self‐reliant adherence to the measures (five items, Cronbach's α = .77, e.g. ‘I am complying with the government's measures.’) and (3) attitudes towards vaccination against COVID‐19, including willingness to get vaccinated (three items, Cronbach's α = .85, e.g. ‘I think it is important that as many people as possible get vaccinated voluntarily.’). For the longitudinal comparison, we used the four items included in both surveys. Scales were constructed in accordance with the identified factors in the 14‐item scale. This resulted in a three‐item scale for understanding and one item indicating adherence. Attitudes towards vaccination were not measured in spring 2020 and were therefore not included in the longitudinal analysis.
Protection motivation
Two items asked whether participants adhered to protect themselves (‘I take measures mainly to protect myself.’) or others (‘I take measures mainly to protect others.’). These items were designed for this study and used repeatedly in the subsequent data collection points. They were rated on a five‐point Likert response format (1 [does not apply at all] to 5 [fully applies]).
Concerns regarding the crisis
Concerns regarding the crisis were assessed with 11 items, rated on a four‐point Likert response format (1 [I do not agree at all] to 4 [I agree completely]). Based on literature reviews, we included concerns regarding physical health, mental health, economy and disadvantaged groups. Factor analysis confirmed the following four factors: (1) health concerns (four items, Cronbach's α = .81, e.g. ‘I am worried that I might infect someone else.’), (2) altruistic concerns (two items, Cronbach's α = .84, e.g. ‘I am worried about socially disadvantaged people.’), (3) apprehension of economic consequences (three items, Cronbach's α = .60, e.g. ‘The crisis will make it difficult to find a job after graduating.’) and (4) apprehension of mental health consequences (two items, Cronbach's α = .71, e.g. ‘I am concerned about my mental health.’). Health concerns, apprehension of economic consequences and apprehension of mental health consequences each include concerns about the students themselves and about other people or the broader economy.
Reactance
Reactance was assessed with a four‐item scale from Betsch et al. (2020) using a five‐point Likert response format (1 [does not apply at all] to 5 [fully applies]; Cronbach's α = .87, e.g. ‘How much do you feel the measures restrict your freedom?’).
Mean values were calculated for all scales with higher values implying greater approval. The surveys included additional scales not reported here, as they are not relevant for this article. Students further provided information on socio‐demographic data such as age and gender. Results from factor analyses, items and descriptive data are presented in Tables S1 and S2.
Qualitative narratives
For the qualitative study, written narratives were used as an effective method for exploring individual experiences with and reflections on complex processes of change (Carlsson et al., 2015; Laughland‐Booÿ et al., 2018; McAdams, 2001, 2011). At each data collection point, participants received a written storytelling prompt asking them to write the narrative, file it via word processing software and return the file when completed. The purpose of the storytelling prompt was to facilitate participants' engagement with the topic. Prompts included questions like ‘How do you evaluate your own behaviour during the curfew?’, ‘How do you evaluate the behaviour of others?’, and ‘What expectations do you have of yourself and others during the curfew?’. Basic socio‐demographic data were included in these files.
Data analysis
Statistical analysis of quantitative data was conducted using IBM SPSS Statistics, Version 26.0. Hierarchical linear regression analyses were computed to examine the effects of demographic data and protection motivations on attitudes towards COVID‐19 measures and the effects of concerns on protection motivations. Gender and age were entered into the models first. Two participants who did not identify as being male or female had to be excluded from these analyses due to the limited sample size. Mediation analyses were conducted using PROCESS, Version 3.5, (Hayes, 2018) with all COVID‐19 concerns added as covariates. Effects with p < .05 or 95% confidence intervals (CIs) of 5000 bootstrap samples not including zero were interpreted as significant. To complement the results with a longitudinal perspective, t‐tests for dependent samples were used to compare understanding, adherence and protection motivations during the first and the second wave of COVID‐19 infections.
For the analysis of written narratives, content analysis is a widely employed strategy (Vandebosch & Green, 2019). We used deductive category formation for qualitative data analyses (Mayring, 2000, 2014) supported by the software MaxQDA 2020 (VERBI Software, 2019). Categories for the deductive analysis were defined parallel to the quantitative study. Openness to widening and revising the categories allowed new insights from the qualitative study. The qualitative data material was screened for relevant text passages. These were categorised according to a predefined coding system, that is, every text passage referencing adherence was assigned the proficiency ‘high’, ‘medium’ or ‘low’. MaxQDA's cross‐tabulation function was used to relate and compare categories. Quotes that represented the opinions succinctly were chosen to illustrate the results. To secure the participants' anonymity, we use pseudonyms.
For the integration of quantitative and qualitative results, findings from each were cross‐checked and combined in the results section. Diverging findings are further elaborated.
RESULTS
The adherence score (M = 4.15, SD = 0.73) was higher than the understanding (M = 3.61, SD = 0.87) and the vaccination score (M = 3.27, SD = 1.22). In the narratives, students largely described high adherence and positive vaccination attitudes, as illustrated in Alexander's (22) comment:
In my circle of friends and acquaintances in Innsbruck, there is no one who thinks that the current set of measures is exaggerated or even unnecessary. There are also no vaccination opponents or people who believe in any conspiracy theories.
Still, students did not comply with the measures uncritically, but they did inquire their advantages and disadvantages as well as their appropriateness like Elisa (24) who noted: ‘I am sympathetic to the new stay at home orders, but I also question them critically’.
We observed moderate to strong positive correlations of understanding with adherence (r = .48, p < .001) and with vaccination attitudes (r = .53, p < .001). Further, adherence and vaccination attitudes were correlated positively (r = .29, p < .001). In the qualitative data, some students who reported adhering to the measures were optimistic that the vaccines might end the pandemic, such as Henry (24): ‘Honestly, I think it will all be over when there is a vaccine, and everyone gets a vaccination’. Conversely, others preferred sticking to non‐pharmaceutical interventions because they feared side effects and did not want to get vaccinated. These students criticised an easing of the measures, like Jasmin (26): ‘In general, people should make sure that they wash their hands regularly and do not get too close to others. Vaccination cannot replace everything’.
To assess the impact of demographic variables and underlying motivations on the three factors understanding, adherence and vaccination attitudes, regression analyses were run. Results are presented in Table 1 and described in the following paragraphs.
TABLE 1.
Hierarchical regression analyses predicting understanding, adherence, and vaccination attitudes
| Understanding | Adherence | Vaccination attitudes | ||||
|---|---|---|---|---|---|---|
| β | p | β | p | β | p | |
| Gender | .05 | .228 | −.16 | <.001 | .09 | .026 |
| Age | −.13 | .001 | −.00 | .985 | −.12 | .002 |
| R2 | .02 | .03 | .02 | |||
| ΔF | 5.78 | .003 | 7.80 | <.001 | 6.76 | .001 |
| Gender | .13 | <.001 | −.06 | .057 | .14 | <.001 |
| Age | −.11 | .001 | .03 | .349 | −.10 | .014 |
| Protecting self | .32 | <.001 | .30 | <.001 | .12 | .002 |
| Protecting others | .36 | <.001 | .45 | <.001 | .28 | <.001 |
| R 2 | .28 | .34 | .12 | |||
| ΔF | 107.41 | <.001 | 142.85 | <.001 | 33.27 | <.001 |
Note: N = 612; gender: 0 = female, 1 = male. Bold writing indicates significant effects after Bonferroni correction (p < .017).
Demographic data
In the quantitative data, younger students reported higher levels of understanding of the measures (β = −.13, p = .001) and more positive vaccination attitudes (β = −.12, p = .002). We could not reveal an effect of age on adherence. Female students reported higher levels of adherence (β = −.16, p < .001). This effect was nonsignificant after adding protection motivations into the model. However, in the full model, male students reported higher understanding (β = .13, p < .001) and more positive vaccination attitudes (β = .14, p < .001) compared to female students.
Protecting oneself and others
Wanting to protect oneself predicted understanding of the measures (β = .32, p < .001), adherence (β = .30, p < .001), and vaccination attitudes (β = .12. p = .002). Wanting to protect others was also associated with higher levels of all three factors (understanding β = .36; adherence β = .45; vaccination attitudes β = .28, all p < .001). Both types of protection motivations were correlated marginally (r S = .08, p = .040). Table 2 presents predictors of wanting to protect oneself or others. Older students were more motivated by protecting themselves (β = .13, p = .002) but less motivated by protecting others (β = −.16, p < .001) than were younger students. Women were more motivated by both protecting themselves (β = −.09, p = .021) and others (β = −.15, p < .001) but gender effects were nonsignificant after adding COVID‐19 concerns. Health concerns predicted both wanting to protect oneself (β = .23, p < .001) as well as others (β = .28, p < .001) with more health concerns being associated with increased protection motivations. Reactance, on the other hand, was associated with decreased adherence to protect oneself (β = −.29, p < .001) and others (β = −.15, p < .001). Altruistic concerns were associated with increased motivation to protect others (β = .13, p = .002) but not oneself. There were no effects of apprehension of economic or mental health consequences on the protection motivations.
TABLE 2.
Hierarchical regression analyses predicting protection motivations
| Protecting self | Protecting others | |||
|---|---|---|---|---|
| β | p | β | p | |
| Gender | −.09 | .021 | −.15 | <.001 |
| Age | .13 | .002 | −.16 | <.001 |
| R 2 | .02 | .05 | ||
| ΔF | 7.13 | .001 | 16.55 | <.001 |
| Gender | −.06 | .095 | −.08 | .025 |
| Age | .14 | <.001 | −.09 | .013 |
| Health concerns | .23 | <.001 | .28 | <.001 |
| Altruistic concerns | −.03 | .505 | .13 | .002 |
| Economic consequences | .08 | .048 | −.06 | .163 |
| Mental health consequences | .02 | .678 | .09 | .028 |
| Reactance | −.29 | <.001 | −.15 | <.001 |
| R 2 | .19 | .23 | ||
| ΔF | 24.91 | <.001 | 27.39 | <.001 |
Note: N = 612; gender: 0 = female, 1 = male. Bold writing indicates significant effects after Bonferroni correction (p < .025).
In the qualitative data, several students mentioned groups they wanted to protect, such as Jasmin (26) who argued that she only does ‘what is necessary, hoping that the numbers will go down and [she] can protect [her] mother and other risk groups by doing so’. The qualitative data further revealed that even though self‐protection was not the main concern for most students, there were some with intense fears of infection who implemented rigorous measures to protect themselves:
At the beginning of October, we had a case of Corona in our group of friends and had to go into quarantine […] I was so afraid of catching it […] and developing long‐term effects [of the disease] that I practically forced my roommates and friends to barricade themselves in their rooms and keep their distance [...]. At least I'm doing a great job of sticking to the curfew, since I do not want to see anyone anyway. ( Helena, 21).
Given the moderate to strong correlation of understanding with adherence and vaccination attitudes, we assumed that understanding was a precondition for both and that the effects of other factors were mediated by understanding. This was partly confirmed by mediation analysis. The results are presented in Figure 2 and described in the following paragraphs.
FIGURE 2.
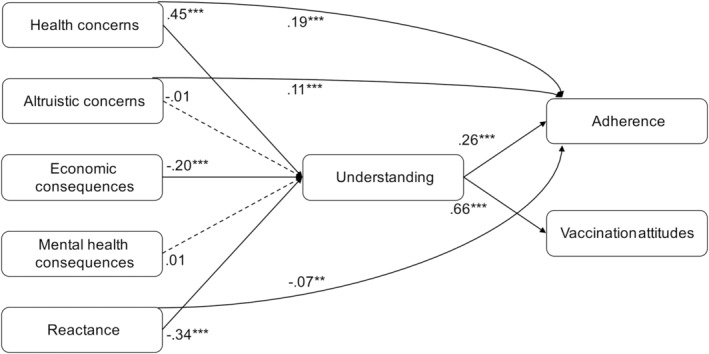
Mediation model of effects on adherence and vaccination attitudes mediated by understanding the measures' necessity. Note: N = 614. All coefficients are unstandardised. Solid lines indicate significant coefficients, dashed lines indicate non‐significant coefficients. **p < .01, ***p < .001
Health concerns
Health concerns had a positive indirect (b = 0.12, SE = 0.02 95% CI [0.07, 0.17]) and direct effect (b = 0.19, SE = 0.04, p < .001, 95% CI [0.10, 0.27]) on adherence, while there was only an indirect effect on vaccination attitudes (b = 0.30, SE = 0.04, 95% CI [0.21, 0.38]; direct effect b = 0.09, SE = 0.07, p = .192, 95% CI [−0.05, 0.24]).
The role of health concerns was emphasised by students explaining that thinking about the risks of infection motivates them to adhere. Most described that they wanted to avoid transmitting the virus to others, such as Juna (23) who ‘just couldn't reconcile it with [her] conscience if [she] infected [her parents]’. The narratives further demonstrated how students deliberately weighed the costs and benefits of vaccination for different groups depending on vulnerability. For example, although Alexander (22) was sceptic about the newly developed vaccine, he acknowledged the importance of getting vaccinated especially for groups vulnerable to the virus:
Of course, I have to admit that I too would have preferred another already better‐tested type of vaccine to win the race. [...] Nevertheless, I think that especially the vulnerable groups of people will be grateful to receive immunization through this vaccine.
Altruistic concerns
Altruistic concerns had a positive direct effect on adherence (b = 0.11, SE = 0.03, p < .001, 95% CI [0.04, 0.17]). There was no indirect effect on adherence mediated by understanding (b = −0.00, SE = 0.01, 95% CI [−0.03, 0.02]) and neither a direct (b = 0.05, SE = 0.05, p = .332, 95% CI [−0.06, 0.16]) nor an indirect effect (b = −0.01, SE = 0.02, 95% CI [−0.06, 0.04]) on vaccination attitudes.
In the qualitative data, an altruistic mindset was repeatedly mentioned as a reason for adherence, for example, by Emil (25): ‘In my opinion, anything else is simply selfish and negligent.’ Additionally, when thinking about the vaccine, global injustice was a concern for highly adherent students like Alexander (22): ‘Poorer countries, as so often, come in second.’
Apprehension of economic consequences
The effects of apprehension of economic consequences were mediated by understanding for adherence (indirect effect b = −0.05, SE = 0.01, 95% CI [−0.09, −0.02]; direct effect b = 0.05, SE = 0.04, p = .186, 95% CI [−0.03, 0.13]) as well as for vaccination attitudes (indirect effect b = −0.13, SE = 0.03, 95% CI [−0.20, −0.07]; direct effect b = −0.13, SE = 0.07, p = .054, 95% CI [−0.27, 0.01]).
Some of the students' narratives supported the finding of negative associations between economic concerns and adherence. Students were worried about the economic consequences of the crisis and criticised the measures as excessive:
The consequences will be felt for many years to come if the economy is not revived soon. I think it will have a bad impact on the future and job finding for many students. [...] I'm just annoyed by Austrian politics and regulations, which I find quite exaggerated. ( Emily, 23).
Nevertheless, several individuals mentioned economic consequences but decided to adhere to the measures because of their expected health benefits, such as Alexander (22): ‘Of course, it is safe to assume that this lockdown will greatly shake our country's economy, yet I believe that every human life that can be saved must be worth more than trying to save the economy’, or due to a feeling of social obligation, like Ella (22): ‘I expect the economy to take a big hit. I don't know exactly how that will affect my future. Nevertheless, I still dutifully follow the restrictions’.
Apprehension of mental health consequences
Apprehension of mental health consequences was not associated with adherence (direct effect b = 0.05, SE = 0.03, p = .077, 95% CI [−0.01, 0.12]; indirect effect b = 0.00, SE = 0.01, 95% CI [−0.02, 0.02]) and vaccination attitudes (direct effect b = 0.09, SE = 0.05, p = .068, 95% CI [−0.01, 0.20]; indirect effect b = 0.01, SE = 0.02, 95% CI [−0.04, 0.05]).
Although there was no association in the quantitative data, in their narratives, some students reported being more adherent to the measures because of mental health impairments they had experienced, like Pia (20) who was in quarantine and adhered to the measures to spare others the experience:
The second Corona wave also hit me, and I was in quarantine for 21 days. These 21 days were for me, psychologically, among the worst of my life. [...] This makes me even more cautious now. Because besides the physical discomfort of the pandemic, I do not wish these psychological discomforts on anyone. Therefore, I adhere to all measures and stay‐at‐home orders to avoid this.
Others expressed difficulties in adhering due to the mental health strains of contact restrictions and confinement:
I was afraid and even panicked a bit at times that the lockdown would be as bad for me again as the first one. […] I had been taking therapy sessions, everything was going well […]. And now I'm supposed to go back to ‘staring at the wall’ and negative vibes? ( Hannah, 22).
Reactance
Reactance had both a negative direct (b = −0.07, SE = 0.03, p = .010, 95% CI [−0.14, −0.01]) and a negative indirect effect (b = −0.09, SE = 0.02, 95% CI [−0.13, −0.05]) on adherence, whereas there was only an indirect (b = −0.23, SE = 0.03, 95% CI [−0.29, −0.16]) but no direct effect (b = −0.02, SE = 0.05, p = .741, 95% CI [−0.12, 0.08]) on vaccination attitudes.
In the narratives, there also was an association of reactance and acute anger with reduced adherence. Students who were angry and annoyed explained how they only complied with the measures as much as absolutely necessary. However, other students described their efforts to adhere for a common good despite being frustrated and not fully understanding the measures, such as Luisa (22) who stated she ‘can understand the frustration of many because some regulations really do not seem so comprehensible. […] Nevertheless [she expected herself] and others to comply well with the regulations now so that the situation will improve as soon as possible’. Others reported understanding the measures but feeling unable to restrict their everyday lives as much as demanded: ‘I understand the limitations very well, but I feel that in the long run, I am not able to maintain my close relationships in such a reduced way and from a distance.’ (Nora, 23).
Changes in the course of the crisis
The longitudinal data allowed placing the cross‐sectional results into a longitudinal context. The students who participated in the quantitative surveys both in spring and in winter 2020 (n = 101) reported decreased understanding of the measures during the second compared to the first lockdown (t[100] = 5.76, p < .001; first lockdown M = 3.80, SD = 0.85; second lockdown M = 3.26, SD = 0.88). However, there were no changes in self‐reported adherence to the governmental measures (t[100] = 1.90, p = .060) and no changes in protection motivations (protecting self t[100] = −0.63, p = .532; protecting others t[100] = 0.58, p = .561).
Qualitative data illustrated these changes in attitudes. During the first lockdown, there was a sense of acceptance of the novel situation and persevering through it. For example, Anna (23) claimed that it ‘is probably best in this situation that you accept the situation, you can't change it anyway’ and was adherent with all measures during the first lockdown. During the second lockdown, the mindset often was more critical towards the government‐imposed measures and students started to make more self‐reliant decisions independently of official regulations.
DISCUSSION
This article focused on university students' attitudes towards measures and vaccinations to contain the spread of COVID‐19. Overall, students reported consistently high levels of adherence to the measures in both qualitative and quantitative data. This result is in line with other studies conducted at the beginning of the pandemic (e.g. Williams et al., 2020). Quantitative outcomes further support previous studies showing higher adherence in women (Bodas & Peleg, 2020; Clark et al., 2020; Moussaoui et al., 2020; Smith et al., 2020). This effect can be attributed to higher motivations to protect both themselves and others in women. In contrast, male students reported a higher degree of understanding the measures' necessity and more positive attitudes towards vaccination after adding protection motivations. The result of more positive vaccination attitudes corroborates previous studies (Kittel et al., 2020; Zampetakis & Melas, 2021). The qualitative data show mixed reactions to the newly developed vaccines against COVID‐19. They gave hope and the strength to continue adhering to the non‐pharmaceutical measures to some. Others were worried about potential side effects or criticised that there was too much focus on vaccines and too little on continuing social distancing measures.
Focusing on costs and benefits
Our findings indicate that individuals weighed the costs and benefits of measures considering various aspects. They decided on their adherence based on that process. Even if the cost–benefit calculations were not always directly addressed in the narratives, students mentioned advantages and disadvantages of adherence and vaccinations and described their efforts to navigate these. They frequently acknowledged possible costs of adherence like economic or mental health impacts but nevertheless decided to accept them to achieve the benefits of fighting the pandemic. The repeatedly changing measures and newly developed vaccines made evaluating and comparing the presumed consequences necessary to form a well‐founded decision on adherence and vaccination readiness. Brief comparisons of students' opinions during the first and the second lockdown indicated that this weighing process became more important during the second lockdown. As the crisis prolonged, participants questioned the appropriateness of the measures more critically and made more self‐reliant decisions on their adherence.
During the second lockdown in winter 2020, health and altruistic concerns were associated with a higher level of adherence and more positive vaccination attitudes. The concerns were more strongly directed at others than the students themselves, which supports previous studies (Elmer et al., 2020; Son et al., 2020). Still, some individuals strongly worried about themselves and therefore adopted rigorous measures.
In the quantitative data, vaccination attitudes were predicted by both concerns about oneself and by concerns about others with larger effect sizes for wanting to protect others. Getting vaccinated to protect others stands in contrast to the uncertainty about the vaccines' ability to prevent the transmission of the virus above preventing the disease at the time of the survey (Mallapaty, 2021). Additionally, in preliminary results from surveys in Austria, vaccination attitudes were predicted more strongly by wanting to protect oneself rather than to protect others (Kittel et al., 2020). The difference to our findings might be caused by the fact that most students do not perceive themselves as vulnerable. Although the primary motive for getting vaccinated is of egoistic origin, people who are not vulnerable can be motivated by altruism (Vietri et al., 2012). This opens a potential approach to encourage young people to get vaccinated: If vaccines indeed can protect against passing on the virus to others, young people who do not feel like they need to get vaccinated to protect themselves might be willing to get a vaccine to protect those around them.
While health and altruistic concerns weighed in support of adhering to the measures, worrying about economic consequences and reactance were associated with reduced adherence and less positive vaccination attitudes in the quantitative data. This result seems problematic since low adherence and low vaccination readiness will extend the pandemic and therefore the necessity for measures (Bodas & Peleg, 2020). Low adherence might be understandable for people with high economic concerns and reactance, but negative vaccination attitudes are highly maladaptive because vaccines might be able to restrict the spread of the pandemic without causing further economic recessions. Students seem to be aware of this contradiction, as those who mentioned worries about economic consequences or felt severely restricted still frequently reported adhering to the measures in the qualitative data. We can therefore conclude that there is a difference in the effects of apprehension of economic consequences on a subjective individual level compared to the statistical level when a large number of students is questioned. While individuals did not perceive economic concerns impairing their adherence, there are statistically significant effects of apprehension of economic consequences on adherence and vaccination readiness.
While possible mental health consequences did not have statistically significant effects in the quantitative data, they played a meaningful part in the decision‐making process of individual students in the qualitative data. Some expressed additional difficulties in adhering to the measures because of strains on their mental health. Others claimed that the mental health toll of the pandemic motivated them to adhere to the measures. Therefore, mental health concerns seemed to have diverse effects depending on individual factors.
The role of understanding of the measures
Understanding the measures' necessity was a mediator for the effects of most of the above‐mentioned factors in the quantitative data. People who felt they understood the governmental measures were more adherent to them and had more positive vaccination attitudes. It can be assumed that this understanding was based on considering the health of oneself and close ones as threatened. In contrast, fear of economic consequences and reactance were associated with decreased understanding. These worries and perceptions might therefore be a symptom of a general scepticism towards how the pandemic is managed – and if COVID‐19 is ‘threatening enough’ to justify the measures.
Nevertheless, several students mentioned scepticism towards the governmental measures while adhering to them. This finding may be caused by several factors. Some students thought that the reinforcement of the measures took place too late or that the measures were not fully sensible and not strict enough. Especially those who had health concerns might therefore have perceived the necessity of adopting own precautions. Additionally, the effect of altruistic concerns on adherence was independent of understanding. This suggests that adherence based on feeling socially responsible is not necessarily based on an understanding of the measures. The non‐altruistic course of action of many governments during the pandemic might further contribute to the missing link between altruistic concerns and understanding of governmental measures.
Implications
The study results have several implications for public health communication and policies. Because most effects were mediated by understanding of the measures, promoting recognition of the measures' necessity comprises a crucial factor in promoting adherence and vaccination readiness. One way to achieve this is the involvement of the public in the decision‐making process. Involving persons of diverse backgrounds in focus groups and discussions can support transparency and trust and thereby improve adherence (Baum et al., 2009). Additionally, these discussions can help to predict problems some social groups might experience when adhering to the measures and facilitate avoiding barriers. Besides including the public in the decision‐making process, established strategies and rules should be communicated by trusted messengers (Baum et al., 2009; van Bavel et al., 2020). This approach is not only advisable for supporting non‐pharmaceutical interventions but has also been promoted for communication about vaccines given the increasing mistrust in their safety and necessity (Larson et al., 2011). The recommendations can therefore be applied to the COVID‐19 vaccines as well. Furthermore, transparent communication and involvement of the public may decrease concerns about economic consequences. People felt societal problems like a looming economic crisis are ignored at the dawn of the pandemic (Codagnone et al., 2020). To avoid this impression, it is important to communicate how and when tightening and alleviating the measures are planned and in what way novel information is considered (Habersaat et al., 2020). If the population's concerns about the measures' economic consequences are ignored, it might lead to a general rejection of all measures taken to contain the spread of SARS‐CoV‐2. This rejection affects even the measures that do not harm the economy, like vaccines, and might therefore prolong the pandemic.
Strengths and limitations
This study is not without limitations. First, only German‐speaking university students were included in the study. Results can therefore not be generalised to other nations, occupational groups and age groups nor to young people in general. We additionally used a convenience sample, which further reduces generalizability. Second, we did not use an objective measure of adherence and vaccination readiness but self‐evaluation. Although self‐reports of adherence reflect real behaviour to a certain degree (Gollwitzer et al., 2020), they likely are biased by social expectations (Bughin et al., 2020). Additionally, we did not distinguish between different kinds of behaviours although not all behaviours to contain the spread of SARS‐CoV‐2 are adopted to the same extent (Moussaoui et al., 2020). Third, the cross‐sectional data do not allow to draw causal conclusions. However, although a bidirectional effect or the role of third variables cannot be precluded, effects purely in the direction from adherence and vaccination attitudes to concerns are theoretically improbable.
Nevertheless, the combination of qualitative and quantitative data offers the possibility of directly comparing effects on an individual and a group level including several hundreds of students. While the qualitative data allowed assessing individuals' subjective reflections on their attitudes and their behaviour, the quantitative data investigated effects on a more abstract level of the student population. The combination allowed more comprehensive insights into decision‐making processes during the COVID‐19 pandemic. Most findings were supported by both methods, but we also observed unique results. For example, there were effects of apprehension of economic consequences on students' behaviour in the quantitative data that they did not seem to be aware of themselves. Additionally, the consideration of mental health effects and their consequences for adherence as well as few students intensely fearing the virus only surfaced in the qualitative data.
CONCLUSION
University students comprise a relevant group to consider when studying adherence and vaccination readiness during the COVID‐19 crisis. They largely feel less vulnerable to the virus but still can potentially spread it to vulnerable groups or fall ill themselves. By combining qualitative and quantitative data, we demonstrated that students weighed the costs and benefits of adhering to non‐pharmaceutical measures and getting vaccinated. They considered health and altruistic concerns as well as possible economic consequences and reactance. Understanding the measures' necessity played an essential role in this process but decreased during the pandemic. We suggest adopting more participative procedures when deciding on public health measures. An appropriate and balanced communication about the measures and their costs and benefits is necessary to enhance university students' understanding, adherence, and vaccination readiness.
ETHICAL STATEMENT
Both studies were approved by the Review Board for Ethical Questions of the University of Innsbruck. They were conducted in accordance with all requirements of the ethical principles of good scientific practice and with the guidelines of the Declaration of Helsinki. Study participants provided informed consent before the start of data collection and could withdraw their participation at any time.
CONFLICT OF INTEREST
The authors declare that there are no financial or nonfinancial competing interests that might be perceived to influence the interpretation of this article.
FUNDING INFORMATION
This work was supported by funding from Förderkreis 1669 of the University of Innsbruck (grant no. 329327); and by the University of Innsbruck doctoral scholarship (grant no. 2020/1/Geo‐12).
Supporting information
Table S1: Factor analysis for attitudes towards the COVID‐19 measures providing a three‐factor solution (‘understanding’, ‘adherence’, and ‘vaccination attitudes’)
Table S2: Factor analysis for concerns and apprehension of consequences providing a four‐factor solution (‘health concerns’, ‘economic consequences’, ‘altruistic concerns’, and ‘mental health consequences’)
Kulcar, V. , Straganz, C. , Kreh, A. , Siller, H. , File, N. , Canazei, M. , Bork‐Hüffer, T. , & Juen, B. (2022). University students' adherence and vaccination attitudes during the COVID‐19 pandemic: Focusing on costs and benefits. Applied Psychology: Health and Well‐Being, 14(2), 572–590. 10.1111/aphw.12320
Funding information University of Innsbruck, Grant/Award Numbers: 329327, 2020/1/Geo‐12
DATA AVAILABILITY STATEMENT
The quantitative data are openly available on Zenodo online (https://doi.org/10.5281/zenodo.4651503). The qualitative data are available from the authors upon reasonable request. The data are not publicly available due to their containing information that could compromise the privacy of research participants.
REFERENCES
- AGES . (2021). COVID‐19 dashboard: Datenbestand des epidemiologischen meldesystems. https://covid19-dashboard.ages.at/
- Arnett, J. J. (2000). Emerging adulthood: A theory of development from the late teens through the twenties. American Psychologist, 55(5), 469–480. 10.1037//0003-066X.55.5.469 [DOI] [PubMed] [Google Scholar]
- Atkinson, R. (1998). The life story interview. Sage. 10.4135/9781412986205 [DOI] [Google Scholar]
- Baum, N. M. , Jacobson, P. D. , & Goold, S. D. (2009). ‘Listen to the people’: Public deliberation about social distancing measures in a pandemic. The American Journal of Bioethics, 9(11), 4–14. 10.1080/15265160903197531 [DOI] [PubMed] [Google Scholar]
- Betsch, C. , Wieler, L. H. , Habersaat, K. , & COSMO group . (2020). Rapid, flexible, cost‐effective monitoring tool for behavioural insights related to COVID‐19 across countries. The Lancet, 395(10232), 1255–1256. 10.1016/S0140-6736(20)30729-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- BioNTech . (2020). Pfizer and BioNTech announce vaccine candidate against COVID‐19 achieved success in first interim analysis from phase 3 study [press release]. New York. https://investors.biontech.de/news-releases/news-release-details/pfizer-and-biontech-announce-vaccine-candidate-against-covid-19
- Bodas, M. , & Peleg, K. (2020). Income assurances are a crucial factor in determining public compliance with self‐isolation regulations during the COVID‐19 outbreak: Cohort study in Israel. Israel Journal Health Policy Research, 9(1), 54. 10.1186/s13584-020-00418-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer, N. T. , Chapman, G. B. , Gibbons, F. X. , Gerrard, M. , McCaul, K. D. , & Weinstein, N. D. (2007). Meta‐analysis of the relationship between risk perception and health behavior: The example of vaccination. Health Psychology, 26(2), 136–145. 10.1037/0278-6133.26.2.136 [DOI] [PubMed] [Google Scholar]
- Bughin, J. R. , Cincera, M. , Reykowska, D. , Żyszkiewicz, M. , & Ohme, R . (2020). Perceptive risk clusters of European citizens and NPI compliance in face of the COVID‐19 pandemics (iCite Working Paper 2020‐042). International Centre for Innovation Technology and Education; Solvay Brussels School; Université libre de Bruxelles. 10.2139/ssrn.3749926 [DOI]
- Carlsson, J. , Wängqvist, M. , & Frisén, A. (2015). Identity development in the late twenties: A never‐ending story. Developmental Psychology, 51(3), 334–345. 10.1037/a0038745 [DOI] [PubMed] [Google Scholar]
- Clark, C. , Davila, A. , Regis, M. , & Kraus, S. (2020). Predictors of COVID‐19 voluntary compliance behaviors: An international investigation. Global Transitions, 2, 76–82. 10.1016/j.glt.2020.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Codagnone, C. , Bogliacino, F. , Gómez, C. , Charris, R. , Montealegre, F. , Liva, G. , Lupiáñez‐Villanueva, F. , Folkvord, F. , & Veltri, G. A. (2020). Assessing concerns for the economic consequence of the COVID‐19 response and mental health problems associated with economic vulnerability and negative economic shock in Italy, Spain, and the United Kingdom. PLoS ONE, 15(10), e0240876. 10.1371/journal.pone.0240876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elmer, T. , Mepham, K. , & Stadtfeld, C. (2020). Students under lockdown: Comparisons of students' social networks and mental health before and during the COVID‐19 crisis in Switzerland. PLoS ONE, 15(7), e0236337. 10.1371/journal.pone.0236337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- European Medicines Agency . (2020). EMA recommends first COVID‐19 vaccine for authorization in the EU [press release]. https://www.ema.europa.eu/en/news/ema-recommends-first-covid-19-vaccine-authorisation-eu
- Ferrer, R. , & Klein, W. M. (2015). Risk perceptions and health behavior. Current Opinion in Psychology, 5, 85–89. 10.1016/j.copsyc.2015.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gollwitzer, A. , Martel, C. , Marshall, J. , Höhs, J. M. , & Bargh, J. A. (2020). Connecting self‐reported social distancing to real‐world behavior. PsyArXiv.. 10.31234/osf.io/kvnwp [DOI] [Google Scholar]
- Gould, E. , & Mitty, E. (2010). Medication adherence is a partnership, medication compliance is not. Geriatric Nursing, 31(4), 290–298. 10.1016/j.gerinurse.2010.05.004 [DOI] [PubMed] [Google Scholar]
- Grubaugh, N. D. , Hodcroft, E. B. , Fauver, J. R. , Phelan, A. L. , & Cevik, M. (2021). Public health actions to control new SARS‐CoV‐2 variants. Cell, 184(5), 1127–1132. 10.1016/j.cell.2021.01.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Habersaat, K. B. , Betsch, C. , Danchin, M. , Sunstein, C. R. , Böhm, R. , Falk, A. , Brewer, N. T. , Omer, S. B. , Scherzer, M. , Sah, S. , Fischer, E. F. , Scheel, A. E. , Fancourt, D. , Kitayama, S. , Dubé, E. , Leask, J. , Dutta, M. , MacDonald, N. E. , Temkina, A. , … Butler, R. (2020). Ten considerations for effectively managing the COVID‐19 transition. Nature Human Behaviour, 4(7), 677–687. 10.1038/s41562-020-0906-x [DOI] [PubMed] [Google Scholar]
- Hale, T. , Angrist, N. , Goldszmidt, R. , Kira, B. , Petherick, A. , Phillips, T. , Webster, S. , Cameron‐Blake, E. , Hallas, L. , Majumdat, S. , & Tatlow, H. (2021). A global panel database of pandemic policies (Oxford COVID‐19 government response tracker). Nature Human Behaviour, 5, 529–538. 10.1038/s41562-021-01079-8 [DOI] [PubMed] [Google Scholar]
- Hayes, A. F. (2018). Introduction to mediation, moderation, and conditional process analysis: A regression‐based approach (2nd ed.). Guilford Press. [Google Scholar]
- Kittel, B. , Paul, K. T. , Kieslich, K. , & Resch, T. (2020). Die impfbereitschaft der österreichischen bevölkerung im Dezember 2020. Corona‐Blog. Universität Wien. https://viecer.univie.ac.at/corona-blog/corona-blog-beitraege/blog93/
- Larson, H. J. , Cooper, L. Z. , Eskola, J. , Katz, S. L. , & Ratzan, S. (2011). Addressing the vaccine confidence gap. The Lancet, 378(9790), 526–535. 10.1016/S0140-6736(11)60678-8 [DOI] [PubMed] [Google Scholar]
- Laughland‐Booÿ, J. , Skrbiš, Z. , & Newcombe, P. (2018). Identity and intimacy: A longitudinal qualitative study of young Australians. Journal of Adolescent Research, 33(6), 725–751. 10.1177/0743558416684959 [DOI] [Google Scholar]
- Mallapaty, S. (2021). Can COVID vaccines stop transmission? Scientists race to find answers. Nature, 10. 10.1038/d41586-021-00450-z [DOI] [PubMed] [Google Scholar]
- Mayring, P. (2000). Qualitative content analysis. Qualitative Social Research, 1(2), 1–10. 10.17169/fqs-1.2.1089 [DOI] [Google Scholar]
- Mayring, P. (2014). Qualitative content analysis: Theoretical foundation, basic procedures, and software solution. Klagenfurt. https://nbn-resolving.org/urn:nbn:de:0168-ssoar-395173
- McAdams, D. P. (2001). The psychology of life stories. Review of General Psychology, 5(2), 100–122. 10.1037/1089-2680.5.2.100 [DOI] [Google Scholar]
- McAdams, D. P. (2011). Narrative identity. In Schwartz S. J., Luyckx K., & Vignoles V. L. (Eds.), Handbook of identity theory and research (pp. 99–115). Springer. 10.1007/978-1-4419-7988-9 [DOI] [Google Scholar]
- Moussaoui, L. S. , Ofosu, N. D. , & Desrichard, O. (2020). Social psychological correlates of protective behaviours in the COVID‐19 outbreak: Evidence and recommendations from a nationally representative sample. Applied Psychology. Health and Well‐Being, 12(4), 1183–1204. 10.1111/aphw.12235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moya, C. , Peniche, P. C. C. , Kline, M. A. , & Smaldino, P. E. (2020). Dynamics of behavior change in the COVID world. American Journal of Human Biology, 32(5), e23485. 10.1002/ajhb.23485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfattheicher, S. , Nockur, L. , Böhm, R. , Sassenrath, C. , & Petersen, M. B. (2020). The emotional path to action: Empathy promotes physical distancing and wearing of face masks during the COVID‐19 pandemic. Psychological Science, 31(11), 1363–1373. 10.1177/0956797620964422 [DOI] [PubMed] [Google Scholar]
- Shanahan, M. J. (2000). Pathways to adulthood in changing societies: Variability and mechanisms in life course perspective. Annual Review of Sociology, 26(1), 667–692. 10.1146/annurev.soc.26.1.667 [DOI] [Google Scholar]
- Smith, L. E. , Amlȏt, R. , Lambert, H. , Oliver, I. , Robin, C. , Yardley, L. , & Rubin, G. J. (2020). Factors associated with adherence to self‐isolation and lockdown measures in the UK: A cross‐sectional survey. Public Health, 187, 41–52. 10.1016/j.puhe.2020.07.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Son, C. , Hegde, S. , Smith, A. , Wang, X. , & Sasangohar, F. (2020). Effects of COVID‐19 on college students' mental health in the United States: Interview survey study. Journal of Medical Internet Research, 22(9), e21279. 10.2196/21279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teasdale, E. , Santer, M. , Geraghty, A. W. A. , Little, P. , & Yardley, L. (2014). Public perceptions of non‐pharmaceutical interventions for reducing transmission of respiratory infection: Systematic review and synthesis of qualitative studies. BMC Public Health, 14, 589. 10.1186/1471-2458-14-589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tilson, H. H. (2004). Adherence or compliance? Changes in terminology. The Annals of Pharmacotherapy, 38(1), 161–162. 10.1345/aph.1D207 [DOI] [PubMed] [Google Scholar]
- van Bavel, J. J. , Baicker, K. , Boggio, P. S. , Capraro, V. , Cichocka, A. , Cikara, M. , Crockett, M. J. , Crum, A. J. , Douglas, K. M. , Druckman, J. N. , Drury, J. , Dube, O. , Ellemers, N. , Finkel, E. J. , Fowler, J. H. , Gelfand, M. , Han, S. , Haslam, S. A. , Jetten, J. , … Willer, R. (2020). Using social and behavioural science to support COVID‐19 pandemic response. Nature Human Behaviour, 4(5), 460–471. 10.1038/s41562-020-0884-z [DOI] [PubMed] [Google Scholar]
- Vandebosch, H. , & Green, L. (2019). Narratives in research and interventions on cyberbullying among young people. Springer International Publishing. 10.1007/978-3-030-04960-7 [DOI] [Google Scholar]
- VERBI Software . (2019). MAXQDA 2020 [computer software]. : VERBI Software. [Google Scholar]
- Vietri, J. T. , Li, M. , Galvani, A. P. , & Chapman, G. B. (2012). Vaccinating to help ourselves and others. Medical Decision Making, 32(3), 447–458. 10.1177/0272989X11427762 [DOI] [PubMed] [Google Scholar]
- Wang, D. , Marmo‐Roman, S. , Krase, K. , & Phanord, L. (2021). Compliance with preventative measures during the COVID‐19 pandemic in the USA and Canada: Results from an online survey. Social Work in Health Care, 60(1), 240–255. 10.1080/00981389.2020.1871157 [DOI] [PubMed] [Google Scholar]
- Webster, R. K. , Brooks, S. K. , Smith, L. E. , Woodland, L. , Wessely, S. , & Rubin, G. J. (2020). How to improve adherence with quarantine: Rapid review of the evidence. Public Health, 182, 163–169. 10.1016/j.puhe.2020.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams, S. N. , Armitage, C. J. , Tampe, T. , & Dienes, K. (2020). Public perceptions and experiences of social distancing and social isolation during the COVID‐19 pandemic: A UK‐based focus group study. BMJ Open, 10(7), e039334. 10.1136/bmjopen-2020-039334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright, A. L. , Sonin, K. , Driscoll, J. , & Wilson, J. (2020). Poverty and economic dislocation reduce compliance with COVID‐19 shelter‐in‐place protocols. Journal of Economic Behavior & Organization, 180, 544–554. 10.1016/j.jebo.2020.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zampetakis, L. A. , & Melas, C. (2021). The health belief model predicts vaccination intentions against COVID‐19: A survey experiment approach. Applied Psychology. Health and Well‐Being, 13(2), 469–484. 10.1111/aphw.12262 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1: Factor analysis for attitudes towards the COVID‐19 measures providing a three‐factor solution (‘understanding’, ‘adherence’, and ‘vaccination attitudes’)
Table S2: Factor analysis for concerns and apprehension of consequences providing a four‐factor solution (‘health concerns’, ‘economic consequences’, ‘altruistic concerns’, and ‘mental health consequences’)
Data Availability Statement
The quantitative data are openly available on Zenodo online (https://doi.org/10.5281/zenodo.4651503). The qualitative data are available from the authors upon reasonable request. The data are not publicly available due to their containing information that could compromise the privacy of research participants.


