Summary
Video‐assisted thoracoscopic surgery has become increasingly popular due to faster recovery times and reduced postoperative pain compared with thoracotomy. However, analgesic regimens for video‐assisted thoracoscopic surgery vary significantly. The goal of this systematic review was to evaluate the available literature and develop recommendations for optimal pain management after video‐assisted thoracoscopic surgery. A systematic review was undertaken using procedure‐specific postoperative pain management (PROSPECT) methodology. Randomised controlled trials published in the English language, between January 2010 and January 2021 assessing the effect of analgesic, anaesthetic or surgical interventions were identified. We retrieved 1070 studies of which 69 randomised controlled trials and two reviews met inclusion criteria. We recommend the administration of basic analgesia including paracetamol and non‐steroidal anti‐inflammatory drugs or cyclo‐oxygenase‐2‐specific inhibitors pre‐operatively or intra‐operatively and continued postoperatively. Intra‐operative intravenous dexmedetomidine infusion may be used, specifically when basic analgesia and regional analgesic techniques could not be given. In addition, a paravertebral block or erector spinae plane block is recommended as a first‐choice option. A serratus anterior plane block could also be administered as a second‐choice option. Opioids should be reserved as rescue analgesics in the postoperative period.
Keywords: analgesia, evidence‐based medicine, postoperative pain, systematic review, video‐assisted thoracoscopic surgery
Recommendations
Regional analgesic techniques such as paravertebral block and erector spinae plane block are recommended. Serratus anterior plane block can be used as a second choice.
Systemic analgesia should include paracetamol and non‐steroidal anti‐inflammatory drugs or cyclo‐oxygenase‐2‐specific inhibitors administered pre‐operatively or intra‐operatively and continued postoperatively.
Intra‐operative administration of intravenous dexmedetomidine is recommended when basic analgesics cannot be given.
Opioids should be used as rescue analgesics postoperatively.
Thoracic epidural analgesia is not recommended for postoperative analgesia.
Why was this guideline developed?
Video‐assisted thoracoscopic surgery (VATS), although less painful than thoracotomy, is associated with significant acute and chronic postoperative pain, negatively affecting recovery [1, 2]. This guideline aims to provide clinicians with an evidence‐based approach to pain management after pulmonary resection under VATS, and to improve postoperative pain relief.
What other guidelines are available on this topic?
In 2018, Piccioni et al. published an enhanced recovery after surgery programme for thoracic surgery [3]. Batchelor et al. also published guidelines for enhanced recovery after surgery for all types of thoracic surgical procedures [4].
How does this guideline differ from other guidelines?
The procedure‐specific postoperative pain management (PROSPECT) approach to developing guidelines is unique such that the available evidence is critically assessed for current clinical relevance. This approach reports true clinical effectiveness in the setting of a specific surgical procedure by balancing the invasiveness of the analgesic interventions and the degree of pain after surgery, as well as balancing efficacy and adverse effects. Compared with previous guidelines, PROSPECT guidelines focus on pain management in the specific setting of VATS.
Introduction
Video‐assisted thoracoscopic surgery is a minimally invasive procedure allowing the reduction of surgical stress and postoperative pain. Previous PROSPECT guidelines concerning pain after thoracotomy recommended using a regional analgesic technique such as a continuous paravertebral or thoracic epidural block [5]. As VATS is less painful, Bendixen et al. suggested using less invasive regional analgesic techniques or systemic analgesia [2]. However, patients can still experience severe pain after VATS [1]. In this setting, pain management is just as essential as it is for open surgery as it might reduce postoperative complications [2]. Systemic analgesia is evolving with multimodal analgesia using intravenous (i.v.) medications like lidocaine, α2‐adrenergic agonists or N‐methyl‐D‐aspartate (NMDA) antagonists. Several regional analgesic techniques have also been developed to manage thoracic postoperative pain such as the paravertebral block, the erector spinae plane (ESP) block and the serratus anterior plane block. There is consequently a need to determine the most appropriate analgesic technique(s) or protocol(s) to control pain after VATS.
The PROSPECT Working Group is a collaborative group of surgeons and anaesthetists working together to formulate procedure‐specific recommendations for pain management after common but potentially painful surgical procedures. The recommendations are based on a procedure‐specific systematic review of randomised controlled trials followed by Delphi rounds to formulate and agree recommendations. The methodology considers clinical practice, efficacy and adverse effects of analgesic techniques [6, 7].
In this study, we aimed to summarise the literature on pain control after VATS over the past 10 y and retrieved the evidence regarding pre‐, intra‐ and postoperative pain management strategies. The primary outcome included postoperative pain scores and opioid requirements. Other recovery outcomes, including postoperative nausea and vomiting and other adverse effects, were also assessed when reported and the limitations of the data were reviewed. The ultimate objective was to develop recommendations for pain management after VATS.
Methods
This review was performed in accordance with the PROSPECT methodology [6, 7, 8]. Specific to this study, the Embase; MEDLINE; PubMed; Cochrane Central Register of Controlled Trials; Cochrane Database of Abstracts of Reviews of Effects; and Cochrane Database of Systematic Reviews were searched for randomised controlled trials published between 01 January 2010 and 01 January 2021. We focused on this time period because VATS was uncommonly performed for lung resection in the preceding years, with thoracotomy being the standard of care at that time.
Search terms used were related to pain and interventions for VATS. These comprised ‘video‐assisted thoracoscopic surgery’ and/or ‘thoracoscopic’ and/or ‘video‐assisted wedge’ and/or ‘video‐assisted lobectomy’ and/or ‘pain’ and/or ‘analgesia’ and/or ‘anaesthesia’ and/or ‘anesthetic’ and/or ‘visual analogue’ and/or ‘vrs’ and/or ‘mcgill’ and/or ‘epidural’ and/or ‘neuraxial’ and/or ‘spinal’ and/or ‘paravertebral block’ and/or ‘erector spinae’ and/or ‘serratus block’ and/or ‘intercostal block’ and/or ‘suprascapular block’ and/or ‘intrathecal’ and/or ‘caudal’ and/or ‘intrapleural’ and/or ‘narcotic’ and/or ‘continuous intercostal nerve block’ and/or ‘combined epidural‐general’ and/or ‘combined regional‐general’ and/or ‘NMDA’ and/or ‘peripheral block’ and/or ‘infiltration’ or ‘instillation’ or ‘NSAID’ or ‘COX‐2’ or ‘paracetamol’ or ‘acetaminophen’ or ‘gabapentin’ or ‘pregabalin’ or ‘clonidine’ or ‘opioid’ or ‘ketamine’ or ‘corticosteroid’ or ‘dexamethasone’ or ‘magnesium’ or ‘lidocaine’ or ‘patient‐controlled analgesia’ or ‘PCA’ or ‘PEC block’ or ‘transcutaneous electrical nerve stimulation’ and/or ‘TENS’.
We included randomised controlled trials and systematic reviews published in English assessing pain management for patients undergoing VATS for lung resection. We excluded studies with patients who underwent a thoracotomy and studies in which more than 75% of the included patients underwent surgery for pneumothorax, as the peri‐operative pain profiles varied from VATS for lung resection. These studies were removed from analysis because pleural abrasion or resection prevents the use of some regional anaesthetic techniques such as paravertebral block. Pain control after pneumothorax surgery is an issue that is somewhat different from pain control after lung resection, and the aim of PROSPECT review being to provide clinicians appropriate recommendations applying specifically for dedicated surgical procedures.
Quality assessment, data extraction and data analysis adhered to the PROSPECT methodology [7]. The studies were required to measure pain intensity using a visual analogue scale (VAS) or a numeral rating scale (NRS). We defined a change of more than 10 on a scale of 0–100 as clinically relevant. We used the PROSPECT methodology previously described for the assessment of the study protocols and results [9]. A p value of <0.05 was considered to be statistically significant, and if two or more studies achieved a significant difference, we considered there to be enough data to recommend the treatment or the technique.
Recommendations were made according to the PROSPECT methodology [9]. Criteria for the assessment of the quality of eligible studies included allocation concealment (A, adequate; B, unclear; C, inadequate; D, not used), numerical (1–5) quality scoring system used by Jadad et al. to assess randomisation, blinding and flow of patients; follow‐up of more or less than 80% of the included patients; and whether the study met the requirements of the CONSORT 2010 statement. The suggested recommendations were sent to the PROSPECT Working Group for review and comments through a modified Delphi approach as previously described [9]. Once consensus was achieved, the lead authors drafted the final document, which was ultimately approved by the Working Group.
Results
A total of 69 randomised controlled trials were included in the final qualitative analysis (Fig. 1). These studies are listed in the online Supporting Information (Table S1) with their respective methodological quality scores. Online Supporting Information (Tables S2 and S3) describe the characteristics of included studies.
Figure 1.
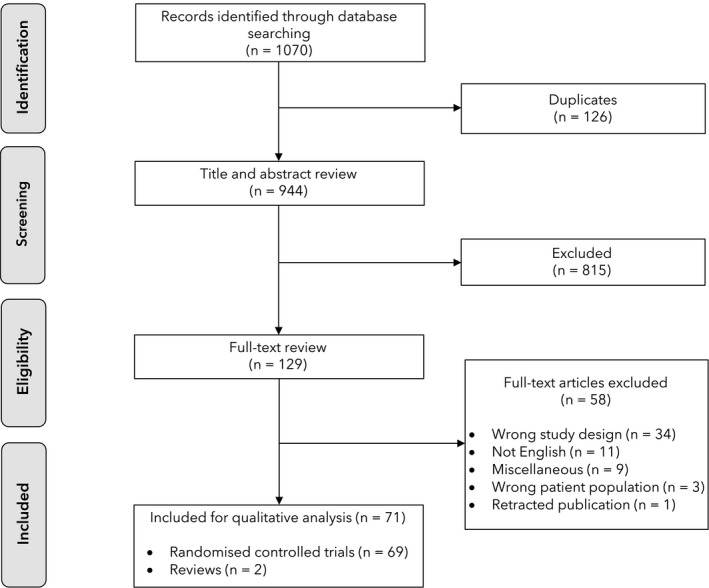
Flow diagram of studies identified, screened and included in this systematic review.
Paracetamol and NSAIDs
Jahangiri et al. [10] compared paracetamol with ketorolac administered after VATS and continued as a postoperative continuous infusion. They did not receive any additional baseline analgesia but had i.v. morphine as a rescue. No significant difference was documented between the ketorolac and paracetamol groups in pain scores; morphine consumption; and patient satisfaction. The volume of blood in thoracic drains was significantly higher in the ketorolac group (309 ml vs. 273 ml; p = 0.001) but the difference was not clinically relevant. There was no difference in other side‐effects.
Dastan et al. [11] compared three groups of patients receiving either morphine 20 mg, paracetamol 4 g or ketorolac 120 mg at the end of surgery and continued for the first day, with i.v. morphine 0.05–0.1 mg.kg‐1 used as rescue analgesia, with no multimodal analgesia provided. They found no difference in pain scores between the three groups. Mean (SD) VAS scores on coughing were significantly higher in the morphine group throughout the study period (3.5 (2.5) in the morphine group; 1.4 (1.4) in the ketorolac group; and 2.7 (2.6) in the paracetamol group). The number of patients who needed rescue mediation was higher in the paracetamol group; however, the mean dose of morphine given as rescue was comparable in the three groups. There was a clinically unimportant difference in the volume of blood loss between the groups (ketorolac 291 ml; paracetamol 250 ml; and morphine 169 ml).
Intravenous α2‐adrenergic agonists
Lee et al. compared i.v. dexmedetomidine 1 μg.kg‐1 vs. saline control 20 min before the end of surgery [12]. No basic analgesia (e.g. paracetamol, NSAIDs) was reported, but all patients received a loading dose of fentanyl 1 μg.kg‐1 followed by a continuous infusion of 0.4 μg.kg‐1.h‐1. Baseline quality of recovery (QoR)‐40 global and dimensional scores were comparable in the two groups. Pain NRS scores at rest and coughing and opioid consumption were significantly lower in the dexmedetomidine group compared with the control group (rescue fentanyl needed in 58% of patients in the dexmedetomidine group vs. 82% of patients in the control group) during the first 24 h. More patients were agitated on emergence from anaesthesia in the control group. Forced expiratory volume for 1 s (FEV1) was significantly greater in the dexmedetomidine group compared with the control group on the first and second days after surgery. Nausea and vomiting were more frequent in the control group, but there were no differences in the incidence of hypotension or bradycardia between the two groups.
Jannu et al. [13] also compared two groups of patients receiving either i.v. dexmedetomidine or saline. They started with a 1 μg.kg‐1‐loading dose of dexmedetomidine before induction followed by a 0.5 mg.kg‐1 infusion until 20 min before the end of surgery. All patients received i.v. paracetamol every 8 h for the first 72 h after surgery. Tramadol was used as rescue and there was no additional baseline analgesia. They documented a significant reduction in pain scores and rescue medication (72% of patients in the intervention group vs. 92% of patients in the control group) in the dexmedetomidine group during the first 24 h. Patients in the intervention group also had a better FEV1 and shorter hospital stay. Hypotension and bradycardia were not reported in this study.
Kweon et al. [14] compared a postoperative i.v. infusion of a low dose (0.15 µg.kg‐1.d‐1) of dexmedetomidine vs. saline. The use of basic analgesia (paracetamol, NSAIDs) was not reported. Patients in both groups had i.v. sufentanil patient‐controlled analgesia (PCA). Sufentanil requirement and pain scores at rest and on movement were lower in the dexmedetomidine group during the first 24 h. Postoperative nausea and vomiting were lower in the dexmedetomidine group. There was no difference between the two groups in the occurrence of bradycardia at 1 h, 4 h, 8 h and 24 h postoperatively. Mean arterial blood pressure was lower in the dexmedetomidine group at 8 h postoperatively but the difference was not clinically relevant.
Miao et al. [15] compared a loading dose of dexmedetomidine intra‐operatively followed by an i.v. dexmedetomidine PCA (0.1 µg. kg‐1.h‐1) vs. a loading dose of saline intra‐operatively followed by an i.v. sufentanil PCA. All patients had NSAIDs and an intercostal nerves block performed by the surgeon at the end of the surgical procedure. There was no significant difference between the two groups in pain scores or rescue analgesia. The incidence of nausea and vomiting was significantly lower in the dexmedetomidine group. A significant reduction in mean arterial blood pressures, heart rate and sufentanil consumption was observed within 48 h after surgery in the dexmedetomidine group compared with the sufentanil group.
Wang et al. [16] compared a loading dose of dexmedetomidine administered at the end of surgery plus dexmedetomidine PCA vs. a loading dose of saline followed by saline PCA. The use of basic analgesia (paracetamol and NSAIDs) was not reported, and oxycodone was provided to all patients. No additional baseline analgesia was used. Median VAS pain scores (2 in the dexmedetomidine group vs. 4 in the oxycodone group) and median oxycodone consumption (13 mg in the dexmedetomidine group vs. 16 mg in the saline group) were significantly lower in the dexmedetomidine group until 24 h after surgery, and nausea and vomiting were also lower. There was no difference between the two groups in the occurrence of bradycardia at different time‐points assessed.
We did not include any studies that assessed the use of clonidine in VATS.
Systemic opioid analgesia
Bai et al. [17] compared different opioids and modalities of administration. They compared three groups: i.v. morphine PCA without basal infusion; i.v. hydromorphone PCA with a basal infusion; or i.v. hydromorphone PCA without basal infusion. Basic analgesia (paracetamol and NSAIDs) was not reported. Surgeons performed intercostal nerves block in all patients. They found no difference in pain scores or patient satisfaction.
There was only one study comparing different opioids for postoperative pain control. However, morphine was commonly used as a rescue to treat postoperative pain using PCA and opioid (commonly morphine) consumption was used as an outcome in most studies. There was no study assessing anaesthesia with different opioids (remifentanil; sufentanil; fentanyl) or without opioids (opioid‐free anaesthesia).
Steroids
Bjerregaard et al. [18] compared high‐dose methylprednisolone (125 mg) before surgery with placebo. Baseline analgesia included paracetamol, ibuprofen and gabapentin, supplemented by paravertebral block and an intercostal nerves block, with morphine or a bolus of bupivacaine in the intercostal nerves block given as rescue. On the day of surgery, pain scores at rest and during mobilisation were significantly reduced in the methylprednisolone group (1.7 vs. 2.5) but not during arm abduction or coughing. Pain scores on the first and second days after surgery, and opioid consumption were comparable. Side‐effects were comparable in the two groups, except that patients in the methylprednisolone group needed more insulin for high blood glucose levels. Indeed, corticosteroid boluses lead to an increase in blood sugar levels. We do not know if this transient hyperglycaemia has any relevant clinical consequences. There were no included studies assessing dexamethasone in this setting.
N‐methyl‐D‐aspartate (NMDA) antagonists
We did not retrieve any studies assessing the use of ketamine in VATS. One study aiming to assess both dexmedetomidine and ketamine has been registered in cinicaltrials.gov (NCT03596424). Sohn et al. [19] studied the administration of an i.v. bolus of magnesium sulphate of 50 mg.kg‐1 for 10 min, followed by a continuous infusion of 50 mg.kg‐1.h‐1 during surgery after tracheal intubation, followed by a continuous infusion until the end of the surgery vs. a control group with saline. A fentanyl PCA associated with a basal i.v. infusion was started at the end of surgery. Basic analgesia (NSAIDs) was used at the discretion of the physicians incharge of the patients. The mean opioid demand was significantly lower in the magnesium sulphate group compared with the control group (35.1 mg vs. 44.7 mg at 24 h). Pain scores and rescue analgesics were comparable in both groups. Postoperative FEV1 and forced vital capacity were higher in the magnesium group when compared with the control group.
Gabapentinoids
Kim et al. [20] documented that a single administration of pregabalin before surgery decreased postoperative pain scores up to 24 h and the need for additional rescue analgesics without an increase in the incidence of side‐effects. Patients did not receive any additional baseline analgesia in this study.
Konstantatos et al. [21] reported that the administration of pregabalin before and for 5 days after surgery was associated with did not reduce pain scores or postoperative opioid consumption. All patients received paracetamol and port sites were infiltrated with a ropivacaine solution.
Homma et al. [22] administered pregabalin for 3 months from the second postoperative day. All patients received NSAIDs and had thoracic epidural analgesia for 2 days after surgery. The number of patients who experienced postoperative neuropathic pain was significantly lower in the pregabalin group compared with the control group (19.6% vs. 41.3%, respectively). However, the delay between surgery and the occurrence of postoperative neuropathic pain was comparable between groups.
Intravenous lidocaine
Slovack et al. [23] compared the administration of an i.v. lidocaine bolus after the induction of anaesthesia followed by continuous infusion until the end of surgery vs. placebo. Basic analgesia was not reported. They found no significant difference in pain scores and opioid consumption.
Transcutaneous electrical nerve stimulation (TENS)
Regarding the use of TENS, we found two studies with different results. Engen et al. [24] compared TENS plus opioid analgesia vs. opioid analgesia alone. Basic analgesia was not reported. No difference in analgesia or opioid consumption was observed.
Chen et al. [25] compared transcutaneous electrical acupuncture points stimulation vs. placebo TENS using very low amperage. Basic analgesia was not reported and no additional baseline was used. They found a reduction in mean VAS pain scores up to 48 h postoperatively (3.2 vs. 5.8, 2.9 vs. 6.0, 1.7 vs. 2.9 at 6 h, 24 h and 48 h in TENS and control groups, respectively), with reduced consumption of rescue morphine.
Regional analgesia
Paravertebral block
We included three studies assessing continuous paravertebral blocks with catheter placement performed intra‐operatively by surgeons. Giang et al. [26] compared this technique with i.v. morphine PCA and noted significantly lower pain scores only during the first 4 postoperative hours. Opioid consumption was higher in the PCA group. Baseline analgesia was not reported. There was no difference in side‐effects. Lee et al. [27] did a comparable study, with an i.v. fentanyl PCA. All patients received tramadol and paracetamol as basic analgesia. They also documented lower opioid consumption in the paravertebral group with no difference in pain scores between groups. There was a higher incidence of postoperative nausea and vomiting and discontinuation of i.v. fentanyl PCA in the PCA group. Wu et al. [28] compared paravertebral catheter to systemic analgesia with i.v. sufentanil PCA. All patients received systemic NSAIDs. Mean VAS was not significantly different between groups but morphine consumption was significantly higher in the sufentanil PCA group. There was significantly more postoperative nausea and vomiting and more rescue analgesia in the sufentanil PCA group.
Four studies focused on the paravertebral single‐shot technique. Zhang et al. [29] documented a lower VAS score on coughing and lower opioid consumption in the paravertebral single‐shot group (performed by the surgeon under direct vision) compared with local wound infiltration. All patients received NSAIDs and i.v. morphine PCA as a rescue. A recent study from Chu et al. [30] found lower pain scores and lower opioid consumption in the single‐shot paravertebral block group (performed by an anaesthetist) compared with the control group with no block. All patients received NSAIDs and i.v. sufentanil PCA as a rescue. Another study by Chu et al. [31] compared three different groups. The first group received a pre‐and postoperative paravertebral injection performed by the anaesthetist using ropivacaine 2 mg.ml‐1, the second group only received a postoperative injection and the third group had a sham block with saline. The basic analgesia protocol was not reported. No significant difference in pain scores was documented between the three groups. There was a significant decrease in opioid use in the pre‐ and postoperative group compared with the other groups. Kang et al. [32] examined the effect of ultrasound‐guided paravertebral blocks on rehabilitation using the decline rate of the six‐minute walking test (6MWT) on postoperative day 1 as the primary outcome. Basic analgesia use was not reported. There was a lower decline rate of 6MWT on postoperative days 1 and 2 in the paravertebral group compared with the control group. Postoperative analgesic consumption was also lower in the paravertebral group.
Hutchins et al. [33] compared continuous paravertebral block with ropivacaine 2 mg.ml‐1 infused at 10–14 ml.h‐1 through a catheter placed by the anaesthetist vs. single‐shot intercostal nerves block with ropivacaine 2.5–5.0 mg.ml‐1 performed by the surgeon. Basic and baseline analgesia were not reported. They found lower pain scores in the paravertebral catheter group but no difference in opioid use. Kadomatsu et al. [34] compared a continuous paravertebral vs. intercostal nerves block, with a catheter placed by a surgeon in both instances. Basic analgesia was provided with NSAIDs. They found no significant difference between the two groups.
Several studies assessed the addition of dexmedetomidine to paravertebral blocks. Xu et al. [35] looked at multilevel paravertebral blocks with ropivacaine plus dexmedetomidine vs. plain ropivacaine. Basic analgesia was provided with NSAIDs. They observed lower pain scores in the dexmedetomidine group but similar opioid consumption. Hong et al. [36] used a similarly designed protocol but with nefopam as baseline analgesia and NSAIDs as a rescue analgesia and found lower pain scores and reduced opioid consumption in the dexmedetomidine plus ropivacaine group. Abd‐Elshafy et al. [37] compared paravertebral block with bupivacaine 5 mg.ml‐1 plus dexmedetomidine vs. plain bupivacaine. They observed only a significant decrease in pain and only within the first 2 h. Opioid consumption was not reported. They found a reduction of chronic pain at 3 months but not at 6 months in the dexmedetomidine group as a secondary outcome.
Ding et al. [38] compared three groups: thoracic epidural plus a single dose of epidural morphine vs. single‐shot paravertebral vs. single‐shot paravertebral with dexmedetomidine. They found that patients in the dexmedetomidine paravertebral group and those in the thoracic epidural group had significantly lower pain scores.
Different modalities of administration of local anaesthetics by a paravertebral catheter have been studied. Taketa et al. [39] looked at programmed intermittent bolus vs. continuous infusion for postoperative analgesia. They failed to demonstrate a significant difference in analgesia, opioid consumption and postoperative nausea and vomiting. There were, however, a larger number of dermatomes anaesthetised in the programmed intermittent bolus group. Chen et al. [40] did a similar study with a smaller number of patients. They found lower pain scores at rest and with coughing in the programmed intermittent bolus group and also lower consumption of local anaesthetic.
Kamalanathan et al. [41] looked specifically at the timing of the block, either after incision or at the end of the procedure. Basic analgesia was supplied by NSAIDs and paracetamol. There was no significant difference between the two groups in terms of pain score and opioid consumption.
Kaya et al. [42] looked at multiple injections (five injections from T4 to T8) vs. a single injection at T6. Multiple injections were more painful and took longer to be performed but both the analgesic effect and opioid consumption were similar.
Regarding the combination of opioids with local anaesthetic for paravertebral block, we only found one study. Bauer et al. [43] compared continuous paravertebral block with ropivacaine plus sufentanil vs. ropivacaine alone. There was no significant difference between the two groups for pain scores and opioid consumption.
Taketa et al. [44] compared an intercostal approach vs. a paralaminar approach to paravertebral block. This study suggested that the paralaminar approach provided superior analgesia. In the paralaminar group the number of postoperative fentanyl rescue doses was lower than that intercostal group at 3 h, 6 h, 12 h and 24 h postoperatively.
Erector spinae plane block
We found two studies that compared single‐shot erector spinae plane (ESP) block performed with 20 ml bupivacaine 5 mg.ml‐1 vs. a control group with no block. Patients were administered NSAIDs for basic analgesia. Ciftci et al. [45] concluded that patients having ESP blocks had lower active and passive pain scores and lower opioid consumption during the first 24 h, as well as a lower incidence of postoperative nausea and vomiting. Liu et al. [46] also compared single‐shot ESP vs. no block. Results were similar, with lower pain scores and lower opioid consumption. A secondary outcome was a faster postoperative out‐of‐bed activity. No basic analgesia (paracetamol and NSAIDs) was reported.
Two other studies compared ESP block with ropivacaine vs. placebo block with saline. Yao et al. [47] found that ESP block with ropivacaine reduced pain scores at rest and during coughing for the first 8 h after surgery. Non‐steroidal anti‐inflammatory drugs were used as basic analgesia. Postoperative sufentanil utilisation was lower in the first 24 h; QoR‐40 scores were higher on the first and second postoperative days; patients were discharged earlier; and patient satisfaction was higher in the ESP block group than the sham group. Shim et al. [48] performed a similar study, but no basic analgesia was stated. They reported lower pain scores in the ESP block group in the first 6 h, but not after this time‐point. Rescue opioid use, however, was lower in the placebo group. As with Yao et al., length of stay was also significantly shorter in the ESP block group.
Two studies compared ESP with paravertebral blocks. Zhao et al. [49] compared single‐shot ESP block vs. single‐shot paravertebral block in patients receiving infusions of NSAIDs for basic analgesia. They found no significant difference in pain scores, quality of recovery or opioid consumption during the first 48 h. Taketa et al. [50] compared continuous ESP blocks with paravertebral blocks with no basic analgesia. They also found no difference in pain scores or opioid consumption during the first 48 h. Chen et al. [51] compared three groups: ESP block vs. paravertebral block vs. intercostal nerves block. There were no additional baseline and basic analgesia was not reported. They observed that opioid consumption and pain scores at rest and while coughing were significantly lower in the paravertebral block group compared with the ESP block and intercostal nerves block groups up to 8 h postoperatively. There was no significant difference in pain scores between ESP block and intercostal nerves block groups during the first 48 h. Turhan et al. [52] also compared ESP block, paravertebral block and intercostal nerves block. Patients all received basic analgesia with paracetamol and NSAIDs. Pain scores were lower in the paravertebral block group compared with the intercostal nerves block group and lower in the intercostal nerves block group compared with the ESP block group. Morphine consumption was lower in the intercostal nerves block and the paravertebral block groups compared with the ESP block group. There was no difference in morphine consumption between the paravertebral block and intercostal nerves block groups. There was no difference between the three groups in mobilisation times.
Gao et al. [53] studied three groups with different adjuvants combined with ropivacaine in ultrasound‐guided ESP block where NSAIDs were used as basic analgesia. The first group received plain ropivacaine, the second group had ropivacaine plus dexamethasone and the third group had ropivacaine plus dexmedetomidine. They reported that the dexmedetomidine group had reduced pain scores, lower need for rescue analgesia and shorter hospital stay compared with the other two groups.
Serratus anterior plane block
Serratus anterior plane blocks can be performed by injecting local anaesthetic above the serratus anterior muscle, between it and the latissimus dorsi muscle (superficial serratus anterior plane block) or below the serratus muscle, between it and the intercostal muscles (deep serratus anterior plane block). Four studies compared the serratus anterior plane block vs. no block. Ökmen et al. [54] concluded that pain scores were lower in the deep serratus anterior plane block group, and patients used less tramadol as rescue medication in this group. Non‐steroidal anti‐inflammatory drugs were given in both groups as routine analgesia. Park et al. [55] found lower pain scores and opioid in the first 24 h in patients who received deep serratus anterior plane block compared with those who did not. Routine analgesia was used, with paracetamol and NSAIDs. Viti et al. [56] reported better pain control with deep serratus anterior plane blocks using baseline analgesia with tramadol and NSAIDs. Opioid consumption was not reported in this study. Semyonov et al. [57] documented lower pain scores in the first 8 h and significantly lower opioid consumption among patients who received serratus anterior plane block (either a deep or a superficial injection at the operator's discretion). Postoperative nausea and vomiting were lower in the serratus anterior plane block group. Paracetamol and NSAIDs were given to both groups as basic analgesia.
Kim et al. [58] used an intervention group with superficial serratus anterior plane block with ropivacaine vs. saline. They found that pain scores at rest were lower in the serratus anterior plane block group, with lower opioid consumption and less postoperative nausea and vomiting. Basic analgesia was applied with paracetamol, codeine and NSAIDs.
Chen et al. [59] allocated patients to one of two groups: superficial serratus anterior plane block or local anaesthetic infiltration before the surgical incision. They reported a difference in pain scores favouring the serratus anterior plane block group at 2 h and 8 h after surgery, but not later. During the first 8 h, opioid consumption in the serratus anterior plane block group was lower. No basic analgesia was reported in any group. Shang et al. [60] also compared superficial serratus anterior plane block vs. local anaesthetic infiltration of the surgical incision. Basic analgesia included NSAIDs. The estimated median time to the first VAS ≥4 was significantly longer in the serratus anterior plane block group. Kim et al. [61] compared deep serratus anterior plane block vs. intercostal nerves block but found no significant difference in both opioid consumption and pain scores. Paracetamol was used as basic analgesia. Lee et al. [62] also compared ultrasound‐guided superficial serratus anterior plane with intercostal nerves block performed by the surgeon (under direct vision). No basic analgesia was reported. They also found no significant difference in pain scores and postoperative analgesic consumption.
Li et al. [63] studied the use of different doses of dexmedetomidine (0.5 μg.kg‐1 or 1 μg.kg‐1) as an adjuvant to ropivacaine in superficial serratus anterior plane block. Basic analgesia was delivered with paracetamol and NSAIDs. They reported significant lower pain scores in the high‐dose dexmedetomidine group (1 μg.kg‐1), with reduced opioid consumption when compared with lower doses.
Comparisons were made between the serratus anterior plane block and the ESP block in three different studies. Ekinci et al. [64] found lower pain scores and lower opioid consumption in the ESP block group compared with deep serratus anterior plane block. Basic analgesia was provided with NSAIDs only. Gaballah et al. [65] performed a superficial serratus anterior plane block and found comparable results, but they used both NSAIDs and paracetamol as rescue medication. Finnerty et al. [66] found no difference between deep serratus anterior plane block and ESP block, both in analgesic effect and opioid consumption. Paracetamol and NSAIDs were given to both groups.
A systematic review and meta‐analysis by Zhang et al. [67] investigated whether peri‐operative ultrasound‐guided serratus anterior plane block combined with general anaesthesia is more effective and safer than systemic analgesia after VATS. They included three randomised controlled trials and one retrospective trial. They found that peri‐operative serratus anterior plane block reduced postoperative pain scores and analgesic consumption after general anaesthesia. Moreover, serratus anterior plane block provided better patient satisfaction. No significant difference was found in duration of surgery, time to chest tube removal, length of stay or side‐effects.
Thoracic epidural analgesia
Seven studies investigated the use of thoracic epidural analgesia for VATS. Zejun et al. [68] compared thoracic epidural analgesia with i.v. sufentanil PCA in patients receiving NSAIDs as basic analgesia. In the thoracic epidural group, a bolus of 5 ml ropivacaine 2.5 mg.ml‐1 solution was administered after catheter placement before surgery, followed by a 5 ml.h‐1 infusion of the same solution. Postoperatively, patients in the thoracic epidural group received ropivacaine 1.5 mg.ml‐1 and sufentanil 0.2 μg.ml‐1 at a rate of 5–10 ml.h‐1 with a bolus of 5 ml allowed every 40 min. They found superiority in pain control at rest and mobilisation in the thoracic epidural group. Epidural analgesia was also associated with a reduced incidence of nausea and vomiting and a shorter duration of postoperative ileus.
Tseng et al. [69] compared thoracic epidural vs. i.v. fentanyl PCA and low‐dose ketamine. Basic analgesia was provided by intercostal nerves block performed by surgeons. All patients received ketorolac. The authors did not find any difference in pain scores at rest and during mobilisation at 48 h. There was no difference in the occurrence of postoperative nausea and vomiting.
Three studies compared thoracic epidural analgesia with paravertebral block. Okajima et al. [70] compared thoracic epidural with paravertebral block catheter and found no difference in pain scores and opioid consumption. All patients received NSAIDs. There was more hypotension in patients who received thoracic epidural. Yeap et al. [71] compared thoracic epidural with paravertebral block delivered in two methods. In the thoracic epidural group, an infusion of bupivacaine 1.25 mg.ml‐1 with hydromorphone 0.05 mg.ml‐1 was commenced postoperatively. In one paravertebral group, a single shot of 30 ml of ropivacaine 5 mg.ml‐1 was injected through the catheter inserted before surgery. In the other paravertebral group, 10 ml.h‐1 of ropivacaine 2 mg.ml‐1 was administered continuously through the same catheter. Basic analgesia consisted of pre‐operative pregabalin and paracetamol followed by postoperative paracetamol. This study reported that thoracic epidural provided greater analgesia than both single‐shot and continuous infusion paravertebral blocks. There was also less opioid consumption in the thoracic epidural group compared with the paravertebral block group. There was no difference in the incidence of chronic pain at 6 months between the groups. Huang et al. [72] compared thoracic epidural vs. ultrasound‐guided continuous paravertebral block performed either by a parasagittal or a transverse approach. All patients received NSAIDs. Pain scores were lower in the thoracic epidural group and a larger sensory block extension was obtained. There was a high ratio of failure to identify the epidural space (14.6%) and hypotension in the thoracic epidural group and an even higher rate of failure of catheter placement in the parasagittal paravertebral group (27.1%).
A review by Harky et al. [73] sought to compare thoracic epidural and paravertebral blocks for analgesia and postoperative complications. They included three small‐randomised controlled trials and one small cohort study. From a pain perspective, there was no conclusive evidence to recommend either thoracic epidural or paravertebral block: one study by Kashiwagi et al. [74] demonstrated significantly lower levels of pain with thoracic epidural, one study by Kosinski et al. [75] showed better pain control with paravertebral block and the third study by Okajima et al. [70] found no difference between the two techniques. Paravertebral block was associated with lower rates of urinary retention and hypotension compared with thoracic epidural.
Hotta et al. [76] compared thoracic epidural with extrapleural blocks. Basic analgesia was provided with flurbiprofen. The authors found no significant difference in analgesic effect and opioid consumption.
Lee et al. [77] showed that the addition of magnesium 100 mg to an epidural injection of ropivacaine did not improve postoperative pain within the first 48 postoperative hours and did not reduce opioid consumption. The primary outcome, chronic postoperative pain, did not differ between the two groups.
Intercostal nerves block
Ahmed et al. [78] assessed the effect of single‐shot intercostal nerves block performed at the end of the surgical procedure by the anaesthetist vs. no block. They reported significantly lower pain scores in the intervention group, with less rescue analgesics required. Basic analgesia was not reported.
Zhang et al. [67] studied four different groups with different local anaesthetic mixtures used for intercostal nerves blocks: ropivacaine plus perineural dexamethasone; ropivacaine plus perineural dexmedetomidine; ropivacaine plus perineural dexmedetomidine and dexamethasone; and a control group of plain ropivacaine. The study concluded that the duration of analgesia was significantly longer in the dexamethasone and dexmedetomidine group compared with the other three groups. The duration of analgesia was significantly shorter in the control group compared with the other three groups. There was no difference between the dexmedetomidine and the dexamethasone group. Maher et al. [79] compared an intercostal nerves block with ropivacaine plus dexamethasone vs. plain ropivacaine. They reported a prolonged duration of analgesia in the intervention group, with lower pain scores and reduced opioid requirements at 24 h. Paracetamol was given in both groups.
Subpleural block with catheter
Ghee et al. [80] compared subpleural catheter with a bupivacaine infusion inserted intra‐operatively by the surgeon vs. intra‐operative infiltration of the incision site with bupivacaine. There was no difference in the analgesic effect. There was no significant difference in the two groups' usage of narcotics. Basic analgesia was achieved with paracetamol and NSAIDs.
Surgical site infiltration
Yang et al. [81] compared pre‐emptive bupivacaine injection around the surgical incision vs. no block. There was no basic analgesia reported. There was no difference in analgesic effect between groups and a higher need for rescue analgesia in the intervention group.
Discussion
Using the PROSPECT approach, we advise the administration of a combination of paracetamol, NSAIDs or a COX‐2‐specific inhibitor, pre‐operatively or intra‐operatively, and continued in the postoperative period. The benefits of these basic analgesics are well described for other procedures [82, 83]. The benefit of the association of NSAIDs and paracetamol is not demonstrated in the setting of VATS but we consider that these are fundamental analgesics patients may receive and in addition it seems inconceivable that patients received only rescue analgesia in control groups when a new drug or analgesic technique is assessed [10, 11]. Further, although there is no study assessing the use of opioids on demand, the design of many studies highlights that patients need complementary on‐demand analgesia, commonly provided by an opioid, in addition to the study drug or technique.
Pre‐operative corticosteroids are routinely used in other surgical procedures for their anti‐emetic properties, ability to increase the duration of the analgesic effect of regional anaesthetic techniques and opioid‐sparing effect. However, there is limited procedure‐specific evidence for the use of corticosteroids in VATS. Therefore, pre‐operative administration of i.v. corticosteroids is not recommended due to the lack of specific evidence in the setting of VATS. However, this does not mean that it contra‐indicated considering the benefits previously reported [84].
We recommend intra‐operative use of i.v. dexmedetomidine because two studies documented that it reduces pain scores and opioid demand [12, 13]. Dexmedetomidine also decreased the incidence of postoperative agitation and cognitive dysfunction, and postoperative nausea and vomiting [12, 13, 14]. An improvement in lung function with an increase in FEV1 and vital capacity has also been demonstrated [12, 13]. Dexmedetomidine, which is an α2‐adrenergic agonist, may cause bradycardia and hypotension. In the studies reviewed, bradycardia and hypotension were observed at several time‐points but did not prove to be clinically relevant. However, patients with severe cardiac disease, conduction and/or rhythm disorders were excluded from these studies and dexmedetomidine should not be used in that cohort of patients. On the contrary, postoperative i.v. dexmedetomidine is not recommended due to conflicting evidence and heterogeneous protocols. Reported side‐effects (sedation; hypotension; bradycardia) were limited but could lead to serious complications without proper monitoring. We found no effect of dexmedetomidine administration on the incidence of chronic pain.
There are no studies comparing anaesthetic maintenance with or without opioid, and no study dedicated to ‘opioid‐free anaesthesia’ in VATS. Most studies used fentanyl or sufentanil for anaesthetic maintenance and rarely remifentanil. The benefits of remifentanil use (shorter acting opioid effects and possibly faster recovery) should be balanced against the possible side‐effects such as hyperalgesia. However, this should be formally studied in well‐designed trials.
Table 1 summarises the interventions that are not recommended for pain management in patients undergoing VATS.
Table 1.
Analgesic interventions that are not recommended for pain management in patients undergoing video‐assisted thoracoscopic surgery.
| Intervention | Reason for not recommending |
|---|---|
| Pre‐operative and intra‐operative | |
| Gabapentinoids | Inconsistent evidence |
| Corticosteroids | Lack of procedure‐specific evidence |
| Magnesium sulphate | Limited procedure‐specific evidence |
| Intravenous lidocaine | Lack of procedure‐specific evidence |
| Transcutaneous electrical nerve stimulation | Inconsistent and limited evidence |
| Wound infiltration | Limited procedure‐specific evidence |
| Intrapleural analgesia | Limited procedure‐specific evidence |
| Intercostal nerves block | Lack of procedure‐specific evidence |
| Thoracic epidural | Non‐inferiority of less invasive techniques with fewer side‐effects |
| Postoperative | |
| Gabapentinoids | Inconsistent evidence |
| Intravenous lidocaine | Lack of procedure‐specific evidence |
| Dexmedetomidine | Lack of procedure‐specific evidence |
| Transcutaneous electrical nerve stimulation | Inconsistent and limited evidence |
The addition of a regional analgesic technique as a component of multimodal analgesia is strongly recommended, as VATS is otherwise associated with severe postoperative pain. The PROSPECT Group previously recommended the use of paravertebral block for thoracotomy. Paravertebral block is still recommended for VATS due to its efficacy on pain control and limited side‐effects compared with thoracic epidurals. The use of a catheter instead of single‐shot analgesia prolongs the analgesic effect but we do not recommend intermittent bolus techniques compared with continuous infusions due to a lack of evidence [39, 40]. We also are unable to recommend a particular technique or approach to perform this block, although catheter placement by the surgeon under direct supervision is easy to perform [42]. A pre‐operative injection is also not recommended over postoperative injection due to the lack of evidence.
We also recommend ESP blocks as several studies have shown the efficacy of ESP block vs. sham block [47, 48]. Compared with paravertebral block, two studies have shown its non‐inferiority and ESP block should therefore be considered as an alternative. It could be more specifically indicated when the parietal pleural leaflet is damaged precluding the efficacy of a paravertebral block with a catheter.
The serratus anterior plane block is simple and quick to perform and side‐effects are limited. The studies retrieved considered a single injection and documented a benefit in terms of pain and opioid consumption compared with systemic basic analgesia or compared with infiltration of the incision site. Studies comparing the serratus anterior plane block with the ESP block are not demonstrative enough to conclude the superiority of the latter, but reported a higher consumption of morphine in the former [54, 55]. Therefore, serratus anterior plane block cannot be considered as first‐line treatment until its efficacy compared with the more established paravertebral and ESP blocks has been confirmed by other studies. In addition, the possibility of continuous catheter administration has not been evaluated. If used, either a deep or a superficial injection can be performed because there is currently no evidence of superiority of one over the other.
Although there are no specific studies dedicated to this point, the aforementioned chest wall fascial plane blocks can be performed at a thoracic level adapted to the location of the port sites, regardless of technique.
Unlike previous PROSPECT recommendations for post‐thoracotomy analgesia [5], we do not currently recommend thoracic epidural, even as a second‐line option for VATS. Even if this technique provides adequate pain management, it is a more invasive intervention than the peripheral nerve block techniques described above. It conveys the risks of hypotension, urinary retention and potential lower limb weakness, which can delay early rehabilitation and resumption of walking. In addition, there may be difficulties in inserting the catheter or drug injection errors with serious consequences. These complications make it inappropriate to use thoracic epidurals when there are other alternatives.
To prolong the duration and analgesic depth of regional anaesthetic techniques, several adjuvants have been administered in addition to local anaesthetic solutions. The addition of preservative‐free dexmedetomidine to local anaesthesia is recommended. It remains to be demonstrated that a comparable effect could be achieved with i.v. administration of dexmedetomidine making it more appropriate for clinical use.
The limitations of this review are those of the studies retrieved. Most studies had no systemic multimodal analgesic strategies reported. Paracetamol and NSAIDs were not used as standard analgesia in many of the randomised controlled trials. The sizes of control and intervention groups were commonly small and the studies were at a high risk of bias. There was significant heterogeneity between the studies regarding the methods of the study, the dosing regimens and administration. There was only qualitative assessment and no quantitative analyses conducted. The effect sizes were not highlighted and there was reliance on statistical significance of included studies.
There are further limitations regarding the outcomes of interest both in this current manuscript as well as those reported in included studies. In thoracic surgery, accelerated rehabilitation is important. Postoperative outcomes are influenced by the patient's ability to get out of bed and participate in physical respiratory therapy exercises. However, very few studies had a primary endpoint related to functional outcomes (e.g. time to resume walking; time to get out of bed; number of steps by day; pain scores during physiotherapy). Only a few studies looked at length of stay as secondary outcomes. Time in hospital and time to ambulation were rarely described. It is known that thoracic surgery is associated with chronic pain [85]. However, few studies included chronic pain as an outcome. Future studies, preferably with sufficient sample sizes and using standardised protocols, should be assessed to provide recommendations considering the safety profile of analgesic interventions.
In summary, this review has identified the agents and techniques that could be recommended for the management of pain after VATS (Table 2). Postoperative pain regarding video‐assisted thoracoscopy requires standardised pain management. A multimodal approach is recommended and should be adjusted for each individual and his comorbidities, weighing analgesic efficacy vs. potential risks. Regional anaesthetic techniques such as paravertebral block and ESP block should be strongly considered. Serratus anterior plane block can also be used to effectively reduce pain. In combination with paracetamol and NSAIDs, opioids should still be used as rescue treatment in patients with significant postoperative pain.
Table 2.
Overall recommendations for pain management in patients undergoing video‐assisted thoracoscopic surgery.
| Pre‐operative and intra‐operative |
| Paracetamol (Grade D) |
| NSAID (Grade D)/COX‐2‐specific inhibitor (Grade D) |
| Dexmedetomidine (excluding patient with severe cardiac disease or conduction and/or rhythm disorders) (Grade B) |
| Postoperative |
| Paracetamol (Grade D) |
| COX‐2‐specific inhibitor/NSAIDs (Grade D) |
| Opioid for rescue (Grade D) |
| Regional analgesia |
| Paravertebral block: single‐shot (Grade A); continuous (Grade A) |
| Erector spinae plane block: single‐shot (Grade A); continuous (Grade B) |
| Serratus anterior plane block: single‐shot (Grade A); continuous (Grade D) |
Supporting information
Table S1. Quality assessment and level of evidence assigned to the randomised trials included in the review for analgesia after video‐assisted thoracoscopic surgery.
Table S2. Summary of key results from studies evaluating systemic analgesics, systemic analgesic adjuncts and regional analgesia used to support the recommended interventions in patients after video‐assisted thoracoscopic surgery.
Table S3. Summary of key results from studies evaluating systemic analgesics, systemic analgesic adjuncts and regional analgesia used to support interventions that are not recommended for analgesic benefit in patients having video‐assisted thoracoscopic surgery.
Acknowledgements
SF and JL contributed equally to this manuscript and share first authorship. PROSPECT is supported by an unrestricted grant from the European Society of Regional Anaesthesia and Pain Therapy (ESRA). In the past, PROSPECT has received unrestricted grants from Pfizer Inc. New York, NY, USA and Grunenthal, Aachen, Germany. GJ has received honoraria from Baxter and Pacira Pharmaceuticals. FB has received honoraria from Grunenthal, The Medicine Company, Abbott France and Nordic Pharma France. MVdV has received honoraria from Sintetica, Grunenthal, Vifor Pharma, MSD, Nordic Pharma, Janssen Pharmaceuticals, Heron Therapeutics and Aquettant. No other competing interests declared.
Appendix 1. PROSPECT Working Group
G. P. Joshi, E. Pogatzki‐Zahn, M. Van de Velde, S. Schug, H. Kehlet, F. Bonnet, N. Rawal, A. Delbos, P. Lavand’homme, H. Beloeil, J. Raeder, A. Sauter, E. Albrecht, P. Lirk, D. Lobo, S. Freys.
This article is accompanied by an editorial by Singh and Ramachandran, Anaesthesia, 2022; 77: 252–6.
See Appendix 1.
Contributor Information
M. Van de Velde, Email: marc.vandevelde@uzleuven.be, @MarcVandeVelde6.
the PROSPECT Working Group *of the European Society of Regional Anaesthesia and Pain Therapy:
G. P Joshi, E Pogatzki‐Zahn, M Van de Velde, S Schug, H Kehlet, F Bonnet, N Rawal, A Delbos, P Lavand’homme, H Beloeil, J Raeder, A Sauter, E Albrecht, P Lirk, D Lobo, and S Frey
References
- 1. Holbek BL, Horsleben Petersen R, Kehlet H, Hansen HJ. Fast‐track video‐assisted thoracoscopic surgery: future challenges. Scandinavian Cardiovascular Journal 2016; 50: 78–82. [DOI] [PubMed] [Google Scholar]
- 2. Bendixen M, Jørgensen OD, Kronborg C, Andersen C, Licht PB. Postoperative pain and quality of life after lobectomy via video‐assisted thoracoscopic surgery or anterolateral thoracotomy for early stage lung cancer: a randomised controlled trial. Lancet Oncology 2016; 17: 836–44. [DOI] [PubMed] [Google Scholar]
- 3. Piccioni F, Segat M, Falini S, et al. Enhanced recovery pathways in thoracic surgery from Italian VATS Group: perioperative analgesia protocols. Journal of Thoracic Disease 2018; 10: S555–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Batchelor TJP, Rasburn NJ, Abdelnour‐Berchtold E, et al. Guidelines for enhanced recovery after lung surgery: recommendations of the Enhanced Recovery After Surgery (ERAS®) Society and the European Society of Thoracic Surgeons (ESTS). European Journal of Cardio‐Thoracic Surgery 2019; 55: 91–115. [DOI] [PubMed] [Google Scholar]
- 5. Joshi GP, Bonnet F, Shah R, et al. A systematic review of randomized trials evaluating regional techniques for postthoracotomy analgesia. Anesthesia and Analgesia 2008; 107: 1026–40. [DOI] [PubMed] [Google Scholar]
- 6. Joshi GP, Schug SA, Kehlet H. Procedure‐specific pain management and outcome strategies. Best Practice and Research Clinical Anaesthesiology 2014; 28: 191–201. [DOI] [PubMed] [Google Scholar]
- 7. Joshi GP, Kehlet H, Beloeil H, et al. PROSPECT Working Group. Guidelines for perioperative pain management: need for re‐evaluation. British Journal of Anaesthesia 2017; 119: 703–6. [DOI] [PubMed] [Google Scholar]
- 8. Lee B, Schug SA, Joshi GP, et al. PROSPECT Working Group . Procedure‐specific pain management (PROSPECT) – an update. Best Practice and Research Clinical Anaesthesiology 2018; 32: 101–11. [DOI] [PubMed] [Google Scholar]
- 9. Joshi GP, Van de Velde M, Kehlet H, et al. PROSPECT Working Group Collaborators . Development of evidence‐based recommendations for procedure‐specific pain management: PROSPECT methodology. Anaesthesia 2019; 74: 1298–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jahangiri Fard A, Farzanegan B, Khalili A, et al. Paracetamol instead of ketorolac in post‐video‐assisted thoracic surgery pain management: a randomized trial. Anesthesiology and Pain Medicine 2016; 6: e39175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dastan F, Langari ZM, Salamzadeh J, Khalili A, Aqajani S, Jahangirifard A. A comparative study of the analgesic effects of intravenous ketorolac, paracetamol, and morphine in patients undergoing video‐assisted thoracoscopic surgery: a double‐blind, active‐controlled, randomized clinical trial. Annals of Cardiac Anaesthesia 2020; 23: 177–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lee SH, Lee CY, Lee JG, Kim N, Lee HM, Oh YJ. Intraoperative dexmedetomidine improves the quality of recovery and postoperative pulmonary function in patients undergoing video‐assisted thoracoscopic surgery. Medicine 2016; 95: e2854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Jannu V, Dhorigol MG. Effect of Intraoperative Dexmedetomidine on postoperative pain and pulmonary function following video‐assisted thoracoscopic surgery. Anesthesia: Essays and Researches 2020; 14: 68–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kweon D‐E, Koo Y, Lee S, Chung K, Ahn S, Park C. Postoperative infusion of a low dose of dexmedetomidine reduces intravenous consumption of sufentanil in patient‐controlled analgesia. Korean Journal of Anesthesiology 2018; 71: 226–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Miao Z, Wu P, Wang J, et al. Whole‐course application of dexmedetomidine combined with ketorolac in nonnarcotic postoperative analgesia for patients with lung cancer undergoing thoracoscopic surgery: a randomized control trial. Pain Physician 2020; 23: E185–93. [PubMed] [Google Scholar]
- 16. Wang X, Wang K, Wang B, et al. Effect of oxycodone combined with dexmedetomidine for intravenous patient‐controlled analgesia after video‐assisted thoracoscopic lobectomy. Journal of Cardiothoracic and Vascular Anesthesia 2016; 30: 1015–21. [DOI] [PubMed] [Google Scholar]
- 17. Bai Y, Sun K, Xing X, et al. Postoperative analgesic effect of hydromorphone in patients undergoing single‐port video‐assisted thoracoscopic surgery: a randomized controlled trial. Journal of Pain Research 2019; 12: 1091–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bjerregaard LS, Jensen PF, Bigler DR, et al. High‐dose methylprednisolone in video‐assisted thoracoscopic surgery lobectomy: a randomized controlled trial. European Journal of Cardio‐Thoracic Surgery 2018; 53: 209–15. [DOI] [PubMed] [Google Scholar]
- 19. Sohn H‐M, Jheon S‐H, Nam S, Do S‐H. Magnesium sulphate improves pulmonary function after video‐assisted thoracoscopic surgery: a randomised double‐blind placebo‐controlled study. European Journal of Anaesthesiology 2017; 34: 508–14. [DOI] [PubMed] [Google Scholar]
- 20. Kim JC, Byun S, Kim S, Lee S‐Y, Lee JH, Ahn S. Effect of preoperative pregabalin as an adjunct to a multimodal analgesic regimen in video‐assisted thoracoscopic surgery: a randomized controlled trial. Medicine 2017; 96: e8644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Konstantatos AH, Howard W, Story D, Mok LYH, Boyd D, Chan MTV. A randomised controlled trial of peri‐operative pregabalin vs. placebo for video‐assisted thoracoscopic surgery. Anaesthesia 2016; 71: 192–7. [DOI] [PubMed] [Google Scholar]
- 22. Homma T, Doki Y, Yamamoto Y, et al. Efficacy of 50 mg pregabalin for prevention of postoperative neuropathic pain after video‐assisted thoracoscopic surgery and thoracotomy: a 3‐month prospective randomized controlled trial. Journal of Thoracic Disease 2019; 11: 694–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Slovack M, Taylor B, Bryce R, Ong D. Does intravenous lidocaine infusion during video‐assisted thoracoscopic surgery reduce postoperative analgesia? A randomized controlled study. Canadian Journal of Anesthesia 2015; 62: 676–7. [DOI] [PubMed] [Google Scholar]
- 24. Engen DJ, Carns PE, Allen MS, et al. Evaluating efficacy and feasibility of transcutaneous electrical nerve stimulation for postoperative pain after video‐assisted thoracoscopic surgery: a randomized pilot trial. Complementary Therapies in Clinical Practice 2016; 23: 141–8. [DOI] [PubMed] [Google Scholar]
- 25. Chen J, Zhang Y, Li X, et al. Efficacy of transcutaneous electrical acupoint stimulation combined with general anesthesia for sedation and postoperative analgesia in minimally invasive lung cancer surgery: a randomized, double‐blind, placebo‐controlled trial. Thoracic Cancer 2020; 11: 928–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Giang NT, Van Nam N, Trung NN, et al. Patient‐controlled paravertebral analgesia for video‐assisted thoracoscopic surgery lobectomy. Local and Regional Anesthesia 2018; 11: 115–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lee CY, Narm KS, Lee JG, et al. A prospective randomized trial of continuous paravertebral infusion versus intravenous patient‐controlled analgesia after thoracoscopic lobectomy for lung cancer. Journal of Thoracic Disease 2018; 10: 3814–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wu Z, Fang S, Wang Q, Wu C, Zhan T, Wu M. Patient‐controlled paravertebral block for video‐assisted thoracic surgery: a randomized Trial. Annals of Thoracic Surgery 2018; 106: 888–94. [DOI] [PubMed] [Google Scholar]
- 29. Zhang X, Shu L, Lin C, et al. Comparison between intraoperative two‐space injection thoracic paravertebral block and wound infiltration as a component of multimodal analgesia for postoperative pain management after video‐assisted thoracoscopic lobectomy: a randomized controlled trial. Journal of Cardiothoracic and Vascular Anesthesia 2015; 29: 1550–6. [DOI] [PubMed] [Google Scholar]
- 30. Chu H, Dong H, Wang Y, Niu Z. Effects of ultrasound‐guided paravertebral block on MMP‐9 and postoperative pain in patients undergoing VATS lobectomy: a randomized, controlled clinical trial. BMC Anesthesiology 2020; 20: 59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Chu L, Zhang X, Lu Y, et al. Improved analgesic effect of paravertebral blocks before and after video‐assisted thoracic surgery: a prospective, double‐blinded, randomized controlled trial. Pain Research and Management 2019; 2019: 9158653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kang K, Meng X, Li B, et al. Effect of thoracic paravertebral nerve block on the early postoperative rehabilitation in patients undergoing thoracoscopic radical lung cancer surgery. World Journal of Surgical Oncology 2020; 18: 298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hutchins J, Sanchez J, Andrade R, Podgaetz E, Wang Q, Sikka R. Ultrasound‐guided paravertebral catheter versus intercostal blocks for postoperative pain control in video‐assisted thoracoscopic surgery: a prospective randomized trial. Journal of Cardiothoracic and Vascular Anesthesia 2017; 31: 458–63. [DOI] [PubMed] [Google Scholar]
- 34. Kadomatsu Y, Mori S, Ueno H, Uchiyama M, Wakai K. Comparison of the analgesic effects of modified continuous intercostal block and paravertebral block under surgeon’s direct vision after video‐assisted thoracic surgery: a randomized clinical trial. General Thoracic and Cardiovascular Surgery 2018; 66: 425–31. [DOI] [PubMed] [Google Scholar]
- 35. Xu J, Yang X, Hu X, Chen X, Zhang J, Wang Y. Multilevel thoracic paravertebral block using ropivacaine with/without dexmedetomidine in video‐assisted thoracoscopic surgery. Journal of Cardiothoracic and Vascular Anesthesia 2018; 32: 318–24. [DOI] [PubMed] [Google Scholar]
- 36. Hong B, Lim C, Kang H, et al. Thoracic paravertebral block with adjuvant dexmedetomidine in video‐assisted thoracoscopic surgery: a randomized, double‐blind study. Journal of Clinical Medicine 2019; 8: 352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Abd‐Elshafy SK, Abdallal F, Kamel EZ, et al. Paravertebral dexmedetomidine in video‐assisted thoracic surgeries for acute and chronic pain prevention. Pain Physician 2019; 22: 271–80. [PubMed] [Google Scholar]
- 38. Ding W, Chen Y, Li D, et al. Investigation of single‐dose thoracic paravertebral analgesia for postoperative pain control after thoracoscopic lobectomy – a randomized controlled trial. International Journal of Surgery 2018; 57: 8–14. [DOI] [PubMed] [Google Scholar]
- 39. Taketa Y, Irisawa Y, Fujitani T. Programmed intermittent bolus infusion versus continuous infusion of 0.2% levobupivacaine after ultrasound‐guided thoracic paravertebral block for video‐assisted thoracoscopic surgery: a randomised controlled trial. European Journal of Anaesthesiology 2019; 36: 272–8. [DOI] [PubMed] [Google Scholar]
- 40. Chen L, Wu Y, Cai Y, et al. Comparison of programmed intermittent bolus infusion and continuous infusion for postoperative patient‐controlled analgesia with thoracic paravertebral block catheter: a randomized, double‐blind, controlled trial. Regional Anesthesia and Pain Medicine 2019; 44: 240–5. [DOI] [PubMed] [Google Scholar]
- 41. Kamalanathan K, Knight T, Rasburn N, Joshi N, Molyneux M. Early versus late paravertebral block for analgesia in video‐assisted thoracoscopic lung resection. A double‐blind, randomized, placebo‐controlled trial. Journal of Cardiothoracic and Vascular Anesthesia 2019; 33: 453–9. [DOI] [PubMed] [Google Scholar]
- 42. Kaya FN, Turker G, Mogol EB, Bayraktar S. Thoracic paravertebral block for video‐assisted thoracoscopic surgery: single injection versus multiple injections. Journal of Cardiothoracic and Vascular Anesthesia 2012; 26: 90–4. [DOI] [PubMed] [Google Scholar]
- 43. Bauer C, Pavlakovic I, Mercier C, et al. Adding sufentanil to ropivacaine in continuous thoracic paravertebral block fails to improve analgesia after video‐assisted thoracic surgery: a randomised controlled trial. European Journal of Anaesthesiology 2018; 35: 766–73. [DOI] [PubMed] [Google Scholar]
- 44. Taketa Y, Irisawa Y, Fujitani T. Comparison of analgesic efficacy between two approaches of paravertebral block for thoracotomy: a randomised trial. Acta Anaesthesiologica Scandinavica 2018; 62: 1274–9. [DOI] [PubMed] [Google Scholar]
- 45. Ciftci B, Ekinci M, Celik EC, Tukac IC, Bayrak Y, Atalay YO. Efficacy of an ultrasound‐guided erector spinae plane block for postoperative analgesia management after video‐assisted thoracic surgery: a prospective randomized study. Journal of Cardiothoracic and Vascular Anesthesia 2020; 34: 444–9. [DOI] [PubMed] [Google Scholar]
- 46. Liu L, Ni X‐X, Zhang L‐W, Zhao K, Xie H, Zhu J. Effects of ultrasound‐guided erector spinae plane block on postoperative analgesia and plasma cytokine levels after uniportal VATS: a prospective randomized controlled trial. Journal of Anesthesia 2021; 35: 3–9. [DOI] [PubMed] [Google Scholar]
- 47. Yao Y, Fu S, Dai S, et al. Impact of ultrasound‐guided erector spinae plane block on postoperative quality of recovery in video‐assisted thoracic surgery: a prospective, randomized, controlled trial. Journal of Clinical Anesthesia 2020; 63: 109783. [DOI] [PubMed] [Google Scholar]
- 48. Shim J‐G, Ryu K‐H, Kim PO, et al. Evaluation of ultrasound‐guided erector spinae plane block for postoperative management of video‐assisted thoracoscopic surgery: a prospective, randomized, controlled clinical trial. Journal of Thoracic Disease 2020; 12: 4174–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Zhao H, Xin L, Feng Y. The effect of preoperative erector spinae plane vs. paravertebral blocks on patient‐controlled oxycodone consumption after video‐assisted thoracic surgery: a prospective randomized, blinded, non‐inferiority study. Journal of Clinical Anesthesia 2020; 62: 109737. [DOI] [PubMed] [Google Scholar]
- 50. Taketa Y, Irisawa Y, Fujitani T. Comparison of ultrasound‐guided erector spinae plane block and thoracic paravertebral block for postoperative analgesia after video‐assisted thoracic surgery: a randomized controlled non‐inferiority clinical trial. Regional Anesthesia and Pain Medicine 2020; 45: 10–5. [DOI] [PubMed] [Google Scholar]
- 51. Chen N, Qiao Q, Chen R, Xu Q, Zhang Y, Tian Y. The effect of ultrasound‐guided intercostal nerve block, single‐injection erector spinae plane block and multiple‐injection paravertebral block on postoperative analgesia in thoracoscopic surgery: a randomized, double‐blinded, clinical trial. Journal of Clinical Anesthesia 2020; 59: 106–11. [DOI] [PubMed] [Google Scholar]
- 52. Turhan Ö, Sivrikoz N, Sungur Z, Duman S, Özkan B, Şentürk M. Thoracic paravertebral block achieves better pain control than erector Spinae Plane Block and Intercostal Nerve Block in thoracoscopic surgery: a randomized study. Journal of Cardiothoracic and Vascular Anesthesia 2020; 35: 2920–7. [DOI] [PubMed] [Google Scholar]
- 53. Gao Z, Xiao Y, Wang Q, Li Y. Comparison of dexmedetomidine and dexamethasone as adjuvant for ropivacaine in ultrasound‐guided erector spinae plane block for video‐assisted thoracoscopic lobectomy surgery: a randomized, double‐blind, placebo‐controlled trial. Annals of Translational Medicine 2019; 7: 668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Ökmen K, Metin ÖB. Evaluation of the effect of serratus anterior plane block for pain treatment after video‐assisted thoracoscopic surgery. Anaesthesia, Critical Care and Pain Medicine 2018; 37: 349–53. [DOI] [PubMed] [Google Scholar]
- 55. Park MH, Kim JA, Ahn HJ, Yang MK, Son HJ, Seong BG. A randomised trial of serratus anterior plane block for analgesia after thoracoscopic surgery. Anaesthesia 2018; 73: 1260–4. [DOI] [PubMed] [Google Scholar]
- 56. Viti A, Bertoglio P, Zamperini M, et al. Serratus plane block for video‐assisted thoracoscopic surgery major lung resection: a randomized controlled trial. Interactive Cardiovascular and Thoracic Surgery 2020; 30: 366–72. [DOI] [PubMed] [Google Scholar]
- 57. Semyonov M, Fedorina E, Grinshpun J, et al. Ultrasound‐guided serratus anterior plane block for analgesia after thoracic surgery. Journal of Pain Research 2019; 12: 953–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Kim D‐H, Oh YJ, Lee JG, Ha D, Chang YJ, Kwak HJ. Efficacy of ultrasound‐guided serratus plane block on postoperative quality of recovery and analgesia after video‐assisted thoracic surgery: a randomized, triple‐blind, placebo‐controlled study. Anesthesia and Analgesia 2018; 126: 1353–61. [DOI] [PubMed] [Google Scholar]
- 59. Chen G, Li Y, Zhang Y, Fang X. Effects of serratus anterior plane block for postoperative analgesia after thoracoscopic surgery compared with local anesthetic infiltration: a randomized clinical trial. Journal of Pain Research 2019; 12: 2411–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Shang LH, Xiao ZN, Zhao YL, Long B. Analgesic effect of serratus anterior plane block after thoracoscopic surgery: a randomized controlled double‐blinded study. Therapeutics and Clinical Risk Management 2020; 16: 1257–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Kim S, Bae C‐M, Do YW, Moon S, Baek SI, Lee DH. Serratus anterior plane block and intercostal nerve block after thoracoscopic surgery. Thoracic and Cardiovascular Surgeon 2020; 69: 564–9. [DOI] [PubMed] [Google Scholar]
- 62. Lee J, Lee DH, Kim S. Serratus anterior plane block versus intercostal nerve block for postoperative analgesic effect after video‐assisted thoracoscopic lobectomy: a randomized prospective study. Medicine 2020; 99: e22102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Li X, Liu Y, Zhao J, Xiang Z, Ren C, Qiao K. The safety and efficacy of ultrasound‐guided serratus anterior plane block (SAPB) combined with dexmedetomidine for patients undergoing video‐assisted thoracic surgery (VATS): a randomized controlled trial. Journal of Pain Research 2020; 13: 1785–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Ekinci M, Ciftci B, Gölboyu BE, Demiraran Y, Bayrak Y, Tulgar S. A randomized trial to compare serratus anterior plane block and erector spinae plane block for pain management following thoracoscopic surgery. Pain Medicine 2020; 21: 1248–54. [DOI] [PubMed] [Google Scholar]
- 65. Gaballah KM, Soltan WA, Bahgat NM. Ultrasound‐guided serratus plane block versus erector spinae block for postoperative analgesia after video‐assisted thoracoscopy: a pilot randomized controlled trial. Journal of Cardiothoracic and Vascular Anesthesia 2019; 33: 1946–53. [DOI] [PubMed] [Google Scholar]
- 66. Finnerty DT, McMahon A, McNamara JR, Hartigan SD, Griffin M, Buggy DJ. Comparing erector spinae plane block with serratus anterior plane block for minimally invasive thoracic surgery: a randomised clinical trial. British Journal of Anaesthesia 2020; 125: 802–10. [DOI] [PubMed] [Google Scholar]
- 67. Zhang X, Zhang C, Zhou X, et al. Analgesic effectiveness of perioperative ultrasound‐guided serratus anterior plane block combined with general anesthesia in patients undergoing video‐assisted thoracoscopic surgery: a systematic review and meta‐analysis. Pain Medicine 2020; 21: 2412–2. [DOI] [PubMed] [Google Scholar]
- 68. Zejun N, Wei F, Lin L, He D, Haichen C. Improvement of recovery parameters using patient‐controlled epidural analgesia for video‐assisted thoracoscopic surgery lobectomy in enhanced recovery after surgery: a prospective, randomized single center study. Thoracic Cancer 2018; 9: 1174–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Tseng W‐C, Lin W‐L, Lai H‐C, Huang T‐W, Chen P‐H, Wu Z‐F. Fentanyl‐based intravenous patient‐controlled analgesia with low dose of ketamine is not inferior to thoracic epidural analgesia for acute post‐thoracotomy pain following video‐assisted thoracic surgery: a randomized controlled study. Medicine 2019; 98: e16403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Okajima H, Tanaka O, Ushio M, et al. Ultrasound‐guided continuous thoracic paravertebral block provides comparable analgesia and fewer episodes of hypotension than continuous epidural block after lung surgery. Journal of Anesthesia 2015; 29: 373–8. [DOI] [PubMed] [Google Scholar]
- 71. Yeap YL, Wolfe JW, Backfish‐White KM, et al. Randomized prospective study evaluating single‐injection paravertebral block, paravertebral catheter, and thoracic epidural catheter for postoperative regional analgesia after video‐assisted thoracoscopic surgery. Journal of Cardiothoracic and Vascular Anesthesia 2020; 34: 1870–6. [DOI] [PubMed] [Google Scholar]
- 72. Huang Q‐W, Li J‐B, Huang Y, Zhang W‐Q, Lu Z‐W. A comparison of analgesia after a thoracoscopic lung cancer operation with a sustained epidural block and a sustained paravertebral block: a randomized controlled study. Advances in Therapy 2020; 37: 4000–14. [DOI] [PubMed] [Google Scholar]
- 73. Harky A, Clarke CG, Kar A, Bashir M. Epidural analgesia versus paravertebral block in video‐assisted thoracoscopic surgery. Interactive Cardiovascular and Thoracic Surgery 2019; 28: 404–6. [DOI] [PubMed] [Google Scholar]
- 74. Kashiwagi Y, Iida T, Kunisawa T, Iwasaki H. Efficacy of ultrasound‐guided thoracic paravertebral block compared with the epidural analgesia in patients undergoing video‐assisted thoracoscopic surgery. Japanese Journal of Anesthesiology 2015; 64: 1010–4. [PubMed] [Google Scholar]
- 75. Kosinski S, Fryzlewicz E, Wilkojc M, Cmiel A, Zielinski M. Comparison of continuous epidural block and continuous paravertebral block in postoperative analgesia after video‐assisted thoracoscopic surgery lobectomy: a randomised, non‐inferiority trial. Anaesthesiology Intensive Therapy 2016; 48: 280–7. [DOI] [PubMed] [Google Scholar]
- 76. Hotta K, Endo T, Taira K, et al. Comparison of the analgesic effects of continuous extrapleural block and continuous epidural block after video‐assisted thoracoscopic surgery. Journal of Cardiothoracic and Vascular Anesthesia 2011; 25: 1009–13. [DOI] [PubMed] [Google Scholar]
- 77. Lee J‐H, Yang W‐D, Han S‐Y, et al. Effect of epidural magnesium on the incidence of chronic postoperative pain after video‐assisted thoracic surgery. Journal of Cardiothoracic and Vascular Anesthesia 2012; 26: 1055–9. [DOI] [PubMed] [Google Scholar]
- 78. Ahmed Z, Samad K, Ullah H. Role of intercostal nerve block in reducing postoperative pain following video‐assisted thoracoscopy: a randomized controlled trial. Saudi Journal of Anaesthesia 2017; 11: 54–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Maher DP, Serna‐Gallegos D, Mardirosian R, et al. The combination of IV and perineural dexamethasone prolongs the analgesic duration of intercostal nerve blocks compared with iv dexamethasone alone. Pain Medicine 2017; 18: 1152–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Ghee CD, Fortes DL, Liu C, Khandhar SJ. A randomized controlled trial of continuous subpleural bupivacaine after thoracoscopic surgery. Seminars in Thoracic and Cardiovascular Surgery 2018; 30: 240–9. [DOI] [PubMed] [Google Scholar]
- 81. Yang HC, Lee J‐Y, Ahn S, et al. Pain control of thoracoscopic major pulmonary resection: is pre‐emptive local bupivacaine injection able to replace the intravenous patient controlled analgesia? Journal of Thoracic Disease 2015; 7: 1960–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Ong CKS, Seymour RA, Lirk P, Merry AF. Combining paracetamol (acetaminophen) with nonsteroidal antiinflammatory drugs: a qualitative systematic review of analgesic efficacy for acute postoperative pain. Anesthesia and Analgesia 2010; 110: 1170–9. [DOI] [PubMed] [Google Scholar]
- 83. Martinez V, Beloeil H, Marret E, Fletcher D, Ravaud P, Trinquart L. Non‐opioid analgesics in adults after major surgery: systematic review with network meta‐analysis of randomized trials. British Journal of Anaesthesia 2017; 118: 22–31. [DOI] [PubMed] [Google Scholar]
- 84. Apfel CC, Korttila K, Abdalla M, et al. A factorial trial of six interventions for the prevention of postoperative nausea and vomiting. New England Journal of Medicine 2004; 350: 2441–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Bayman EO, Parekh KR, Keech J, Selte A, Brennan TJ. A prospective study of chronic pain after thoracic surgery. Anesthesiology 2017; 126: 938–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Quality assessment and level of evidence assigned to the randomised trials included in the review for analgesia after video‐assisted thoracoscopic surgery.
Table S2. Summary of key results from studies evaluating systemic analgesics, systemic analgesic adjuncts and regional analgesia used to support the recommended interventions in patients after video‐assisted thoracoscopic surgery.
Table S3. Summary of key results from studies evaluating systemic analgesics, systemic analgesic adjuncts and regional analgesia used to support interventions that are not recommended for analgesic benefit in patients having video‐assisted thoracoscopic surgery.


