Abstract
Background
Self‐perceptions of ageing (SPA) is an important predictor for physical and mental health of older adults in successful ageing. SPA is mainly studied from negative or positive perspectives using variable‐centred methodologies. The aim of the current study was to explore distinct profiles of SPA among Chinese community‐dwelling older adults using a person‐centred method and validate the SPA profiles by examining associations with psychological outcomes.
Methods
Participants aged 65 and over were randomly divided into test and validation samples (n = 451, respectively). SPA was measured by the Brief Ageing Perceptions Questionnaire using latent profile analysis.
Results
Three SPA profiles were identified. One adaptive subgroup was designated as ‘Low ageing awareness and high positive control’ (LAPC, 84.7% and 75% in both samples, respectively). Two maladaptive SPA subgroups were designated as ‘Low positive consequences and control’ (LPCC, 3.9% and 8.2% in both samples, respectively), and ‘High ageing awareness and negative control’ (HANC, 11.4% and 16.8% in both samples, respectively). Similar to negative/positive SPA, the HANC and LAPC subgroups showed the highest and lowest levels of depressive symptoms and cognitive decline. Low cognitive function was found in the LPCC subgroup.
Conclusions
These findings highlight the heterogeneity of older adults' SPA. SPA profiles may aid community healthcare providers in China to identify individuals with high risk of maladaptive SPA and to tailor targeted interventions for psychological health in later life. Distinct SPA profiles require different interventions targeting negative or positive control or both aspects. More positive control strategies might be beneficial for cognitive functioning in older adults from the LPCC subgroup.
Keywords: cognitive function, depression, latent profile analysis, self‐perceptions of ageing
INTRODUCTION
As the global population is rapidly ageing, especially in China, it is critical for the entire society, community, and individuals to reduce negative stereotypes of ageing and develop more positive self‐perceptions of ageing (SPA) for healthy ageing. SPA encompasses a wide range of constructs such as older adults' attitudes toward their own ageing, subjective age, and even ageing identities. 1 It has been of great interest in healthy ageing research and has been broadly studied. Literature on SPA of older adults mainly focuses on assessment tools such as the Ageing Perceptions Questionnaire (APQ), 2 Brief Ageing Perceptions Questionnaire (B‐APQ), 3 or questionnaire on Awareness of Age‐Related Change (AARC), 4 risk and protective factors, 5 , 6 , 7 , 8 associations with health‐related‐behaviours, 9 and mortality, 10 , 11 as well as other physical and mental health outcomes. 12 , 13
Depression is one of the most important mental health concerns; approximately 22.3% of older adults in China have been reported as having depressive symptoms. 14 Several studies revealed that SPA directly or indirectly predicted the onset and persistence of depressive symptoms. 15 , 16 For example, the odds of belonging to the depressed ageing group rose by 17% because of a one‐unit increase in negative SPA. 17 Accordingly, SPA has been considered as an important target for reducing depressive symptoms among older adults.
Other than depression, SPA has also been a crucial factor affecting cognitive function of older adults. Levy and colleagues found that individuals in midlife with a negative attitude toward ageing had poorer cognitive functions, such as in visual memory, 38 years later. 18 Further, Stephan and colleagues reported that feeling older was a marker of older adults' subsequent cognitive impairment. 19 Robertson and colleagues emphasised that negative views of ageing predicted cognitive decline. Specifically, verbal fluency and memory declined in the older population after adjusting for other related factors over a 2‐year longitudinal study. 20 In contrast, Brown and colleagues demonstrated positive rather than negative SPA predicted cognitive functions. 21 More efforts are therefore needed to elucidate the relationship between SPA and cognitive functions.
The wide‐reaching implications of older adults' SPA for psychological, physical and even behavioural outcomes have been discussed using variable‐centred methods. For example, SPA has been divided into positive/negative or more/less favourable or gain/loss‐related SPA, favourable or unfavourable SPA based on cut‐off scores such as the total scores below or above the mean of SPA or attitudes toward ageing, 22 , 23 , 24 or even median score. 25 Furthermore, SPA has been also divided into quartiles such as low, low‐moderate, moderate‐high, and high, according to distributions of samples for detecting threshold effect on healthcare resources. 26 Huy and colleagues used factor and cluster analyses to identify the typology of older adults' views of ageing and found three different groups (‘fit and performance‐hungry’, ‘conventional’, and ‘easy‐going and committed’ groups) mainly based on healthy lifestyles. 27 None of those categories of SPA using variable‐centred strategies considered unobserved heterogeneity. Ageing is not homogeneous, 28 and older adults' SPA might not be a homogenous construct that the traditional variable‐centred approach has assumed, leading to a gap in understanding SPA categories.
To our knowledge, there are still no studies on heterogeneity of older adults' ageing perceptions. Person‐centred approaches such as latent class analysis (LCA) and latent profile analysis (LPA) might extend previous findings of SPA categories by considering homogeneity within a given subgroup and heterogeneity across different subgroups as well as measurement errors. 29 Whether there are some similar groups in both person‐centred and variable‐centred approaches or totally different subgroups using person‐centred analytic methods is still not known.
More studies are aware that SPA is a multidimensional and modifiable construct17, 30 Barker and colleagues used Leventhal's self‐regulation framework to define SPA as subjective perceptions and emotional reactions aroused by physical, psychological, and social threats to ageing. 2 Therefore, APQ, especially B‐APQ, was developed to assess multidimensional SPA, which includes five ageing perception‐related subscales. 3 ‘Timeline Chronic’ relates to ageing beliefs and constant awareness of ageing; ‘Consequences Positive’ refers to ongoing development; ‘Control Positive’ refers to an individual's ability to manage one's positive experience of ageing; ‘Consequences and Control Negative’ refers to an individual's inability to control the experience of ageing, resulting in physical decline and loss. ‘Emotional Representations’ relate to anxiety, worry, and depressive emotions about ageing.
Apart from concise, theory‐based, and multidimensional features of B‐APQ, it is worth mentioning that the B‐APQ has some other advantages. First, a systematic review exploring measurement properties of all kinds of ageing stereotype questionnaires recently concluded that B‐APQ might be the most suitable assessment tool of SPA at present for its reasonable psychometric properties. 31 Second, B‐APQ, together with other similar short versions of APQ, have been widely used in multiple cultures such as Ireland, 3 Malaysia, 32 Turkey, 33 Iran, 34 and China. 35 For example, B‐APQ was used to examine the predictive roles of negative SPA on physical, psychological, and behavioural outcomes in Ireland where age stereotypes became more and more negative. 15 , 36 , 37 , 38 In Eastern Asian cultures under which older adults are highly respected and filial piety is advocated broadly, B‐APQ could be also used to measure ageing perceptions of older adults even with chronic diseases. 39 , 40 The reasons why these findings mentioned above could reflect SPA accurately might be related to the following two aspects. On the one hand, all items in B‐APQ were originally developed from community older adults' experiences and beliefs of ageing using a focus group method, including beliefs about awareness of ageing, beliefs about the impact and personal control of ageing, and emotional responses to ageing, thereby this measure could be considered as the holistic representation of beliefs about ageing. 2 On the other hand, similar to other measurement tools of SPA, 41 B‐APQ could capture the multidimensional nature of SPA and effectively predict health‐related outcomes but also capture malleable characteristics of SPA from a self‐regulatory lens.
Based on B‐APQ, the purpose of the current study was to explore SPA subgroups using LPA and examine the relationship between different SPA profiles and depression as well as cognitive functions, aiming at better understanding the heterogenous nature of SPA categories and providing targets for SPA interventions according to distinct characteristics of SPA subgroups. Taken together, we hypothesised that there would be multiple distinct subgroups of SPA that might not be limited to positive or negative SPA. Additionally, distinct SPA subgroups may be differentially linked to depressive symptoms and cognitive performance.
METHODS
Participants
All participants were community‐dwelling older adults aged 65 years and older recruited from a designated community healthcare centre for annual physical examination in Xinxiang, China. Participants included 917 older adults, and 15 participants were excluded from analysis because of missing data exceeding 20% of the total questionnaires. Questionnaire data were collected by trained interviewers face to face. Disabled older adults or those with severe hearing or visual impairments or with diagnosed dementia were excluded from the study. The present study was approved by the Institutional Review Boards and Ethics Committee of Xinxiang Medical University.
For better identifying the subgroups of SPA among community‐dwelling Chinese older adults, the remaining 902 participants were divided randomly into test and validation samples by SPSS random sampling. 42 Test samples were first used to explore the potential optimal number of SPA profiles and the identified solution was validated in the validation sample.
The 902 participants ranged in age from 65 to 95 (mean = 71.28 years, SD = 5.38). More older adults were female (n = 526, 58.3%) than male (n = 376, 41.7%). Test and validation samples (n = 451, respectively) did not differ significantly by age, gender, marital status, education, physical activity, smoking, drinking, healthy diet, and healthy lifestyles (Tables S1 and S2). Additionally, there were no significant differences between test and validation samples in terms of SPA, depressive symptoms, or cognitive function (Table S2).
MEASURES
Assessment of SPA
All participants finished a packet of questionnaires including the B‐APQ, which is a five‐point Likert scale and comprises 17 items indicating five ageing perception domains: Timeline‐Chronic (TC, e.g., ‘I always classify myself as old’), Consequences Positive (PS, e.g., ‘As I get older, I get wiser’), Control Positive (PC, e.g., ‘The quality of my relationships with others in later life depends on me’), Consequences and Control Negative (NC, e.g., ‘Getting older makes me less independent or slowing down with age is not something that I can control’), and Emotional Representations (ER, e.g., ‘I feel angry when I think about getting older’).
The items of the NC subscale were reverse‐coded. Thus, positive SPA is indicated by low levels of TC and ER and high levels of PS, PC, and NC. 3 In the present study, the internal consistencies of the B‐APQ and subscales were 0.718, 0.738, 0.665, 0.907, 0.738, and 0.608, respectively, which was comparable with previous studies. 21 , 32 Factor analysis confirmed the original factorial structure of B‐APQ in the present study: Chi‐square, 447.472; df, 109; root mean square error of approximation, 0.059; 90% CI, 0.053–0.064; comparative fit index, 0.934; Tucker–Lewis index, 0.918; standardised root mean square residual, 0.048. Scores in each subscale were standardised into Z scores for comparison with other studies and interpretation of the latent profiles.
Assessment of depression
The nine‐item Patient Health Questionnaire (PHQ‐9) was used to detect depressive symptoms over 2 weeks before the questionnaire was delivered. In the present study, the Cronbach's α coefficient was 0.707, which is acceptable. 43
Assessment of cognitive functions
The Chinese version of the Mini‐Mental State Examination (MMSE) was used to study cognitive functions in older adults. 44 This scale comprises 30 items and five subcategories, including orientation to time and place, language, mental arithmetic, immediate and short‐term auditory word memory, and visual construction. Total scores on the MMSE were analysed and the Cronbach's α was 0.804 in this study.
Assessment of sociodemographic characteristics
Demographic information and lifestyles were investigated including age, gender, marital status, education, physical activity, smoking, drinking, healthy diet, and healthy lifestyles. 45 Healthy lifestyles (from 0 = very unhealthy to 4 = very healthy) were calculated according to four scores consisting of healthy diet including vegetable and fruit intake (0 = not regularly, 1 = regularly), physical activity (0 = not regularly, 1 = regularly) and smoking (0 = regularly, 1 = not regularly) as well as drinking (0 = regularly, 1 = not regularly).
Statistical analyses
LPA was conducted to detect the most likely numbers of SPA classes based on the B‐APQ using Mplus 7.1. 46 Akaike information criterion (AIC), Bayesian information criterion (BIC), sample size‐adjusted Bayesian information criterion (aBIC), entropy, Lo–Mendell–Rubin adjusted likelihood ratio test (LMR), and the bootstrap likelihood ratio test (BLRT) were used to explore the optimal subgroups. Smaller values of AIC, BIC, and aBIC demonstrate better model fits. Entropy is used to determine the latent classification accuracy. A value of entropy exceeding 0.8 indicates a much better classification. Both LMR and BLRT indicate how well a k profile model surpasses a k‐1 profile model, and a significant P value indicates a k profile model is superior to the k‐1 profile. Posterior classification probabilities were also supplied in the study.
SPSS 24.0 (IBM Corporation, Armonk, NY, USA) was used to compare the demographic characteristics, SPA subscale and related psychological outcomes in test and validation samples or results among three latent profiles through Chi‐square test, t‐test, non‐parametric test, or one‐way analysis of variance (ANOVA). To compare the differential magnitude of distinct profiles derived from LPA, independent t‐test and Cohen's d effect sizes were also used to depict the standardised magnitude difference of SPA for each subgroup. 47 The Block, Croon, and Hagenaars method (BCH) is strongly recommended to examine the relationships between latent profiles and psychological variables such as depressive symptoms and cognitive functions. 48
RESULTS
LPA for the test and validation sample
Test sample
Table 1 presents fit indices for 1–6 latent profile models. The lowest BIC value, significant BLRT, LMR, and entropy values closer to one have been considered as a way to yield the optimal number of profiles. 49 The smallest aBIC value was found for a six‐profile model but the LMR was not significant in both the five‐ and six‐profile models. Although a four‐profile model yielded slightly lower BIC values, the three‐profile model had the highest entropy value of 0.919, indicating accurate classifications in a three‐profile model. Hence, the three‐profile model was chosen and submitted for the following analysis.
Table 1.
Fit indices for six latent profiles in the test and validation sample
| Sample | Fit indices | Number of profiles | |||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | ||
| Test N = 451 | AIC | 6425.660 | 6229.403 | 6145.870 | 6077.449 | 6049.871 | 6028.613 |
| BIC | 6466.774 | 6295.187 | 6236.323 | 6192.570 | 6189.661 | 6193.072 | |
| aBIC | 6435.038 | 6244.409 | 6166.503 | 6103.709 | 6081.758 | 6066.127 | |
| Entropy | 0.891 | 0.919 | 0.762 | 0.801 | 0.796 | ||
| LMR | <0.001 | 0.098 | 0.027 | 0.150 | 0.543 | ||
| BLRT | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||
| Validation N = 451 | AIC | 6396.819 | 6270.138 | 6158.528 | 5995.104 | 5907.582 | 5474.675 |
| BIC | 6437.934 | 6335.921 | 6248.981 | 6110.225 | 6047.371 | 5639.133 | |
| aBIC | 6406.197 | 6285.143 | 6179.161 | 6021.363 | 5939.468 | 5512.188 | |
| Entropy | 0.532 | 0.862 | 0.942 | 0.934 | 0.947 | ||
| LMR | 0.019 | <0.001 | 0.346 | 0.066 | 0.061 | ||
| BLRT | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||
aBIC, sample size‐adjusted Bayesian information criterion; AIC, Akaike information criterion; BIC, Bayesian information criterion; BLRT, bootstrap likelihood ratio test; LMR, Lo–Mendell–Rubin adjusted likelihood ratio test
As shown in Figure 1, Class 1 was labelled ‘Low positive consequences and control’ subgroup (LPCC), containing 3.95% of the test sample, characterised by relatively low standardised mean scores on TC and ER and moderate scores on Consequences and Control Negative but the lowest standardised mean scores on Consequences Positive and Control Positive. Class 2 was labelled the ‘Low ageing awareness and high positive control’ subgroup (LAPC), comprising 84.7% of the test sample, and it had the highest standardised mean scores on Consequences Positive and Control Positive and highest standardised mean scores on Consequences and Control Negative (reverse‐coded) and low scores on ER. Class 3 was labelled the ‘High ageing awareness and negative control’ subgroup (HANC), consisting of 11.4% of the test sample, and had the highest standardised mean scores on TC and ER and the lowest scores on Consequences and Control Negative (reverse‐coded) together with a moderate level of Control Positive and Consequences Positive, suggesting that negative ageing awareness and maladaptive coping strategies might predominate in this subgroup.
Figure 1.
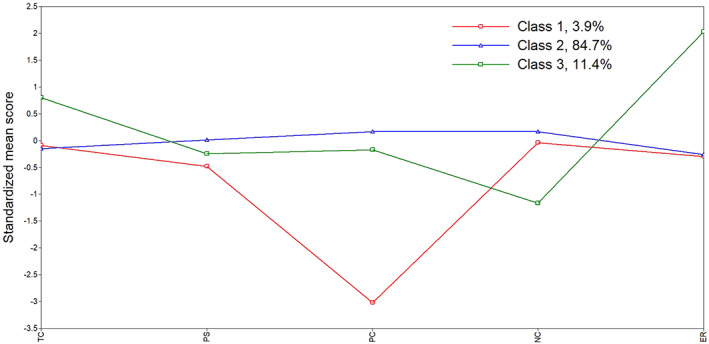
Plot of the standardised mean scores of self‐perceptions of ageing (SPA) across the three identified latent profiles in the test sample. TC, timeline‐chronic; PS, Consequences Positive; PC, Control Positive; NC, Consequences and Control Negative; ER, Emotional Representations.
Furthermore, Table 2 illustrates that the probabilities of LPCC, LAPC, and HANC were 93.2%, 97.2%, and 91.6%, respectively, suggesting good discriminability and accuracy of results with the three‐profile model in the test sample.
Table 2.
Average latent profile class probabilities for the most likely class membership (row) by latent class (column) in the test and validation samples
| Sample | Latent class | The most likely class membership | ||
|---|---|---|---|---|
| LPCC | LAPC | HANC | ||
| Test N = 451 | 1 | 0.932 | 0.052 | 0.016 |
| 2 | 0.007 | 0.972 | 0.021 | |
| 3 | 0.002 | 0.082 | 0.916 | |
| Validation N = 451 | 1 | 0.878 | 0.082 | 0.040 |
| 2 | 0.010 | 0.956 | 0.034 | |
| 3 | 0.006 | 0.101 | 0.893 | |
LPCC, low positive consequences and control subgroup; LAPC, low ageing awareness and high positive control subgroup; HANC, high ageing awareness and negative control subgroup.
Validation sample
Table 1 also shows the fit indices for the one‐ to six‐latent profile models. The five‐ and six‐profile model offered the lowest aBIC values and the higher entropy values, but the LMR was not significantly different from the four‐ to six‐profiles (P > 0.05). Compared with the two‐profile model, the three‐profile model had a slightly higher entropy of 0.862. The three‐profile model was therefore selected as the optimal solution. As shown in Figure 2, the same labels for each subgroup were used because of the very similar characteristics in both samples. Class 1 was labelled ‘Low positive consequences and control’ subgroup (LPCC), containing 8.2% of the validation sample. Class 2 was labelled ‘Low ageing awareness and high positive control’ subgroup (LAPC), comprising 75% of the validation sample. Class 3 was labelled the ‘High ageing awareness and negative control’ subgroup (HANC), consisting of 16.8% of the validation sample. The HANC subgroup was characterised by the highest mean scores on TC and the lowest scores on Consequences and Control Negative despite the highest score on Consequences Positive and moderate level on Control Positive. Table 2 also shows that the probabilities of LPCC, LAPC, and HANC were 87.8%, 95.6%, and 89.3%, respectively, suggesting results from LPA in the validation sample were accurate.
Figure 2.
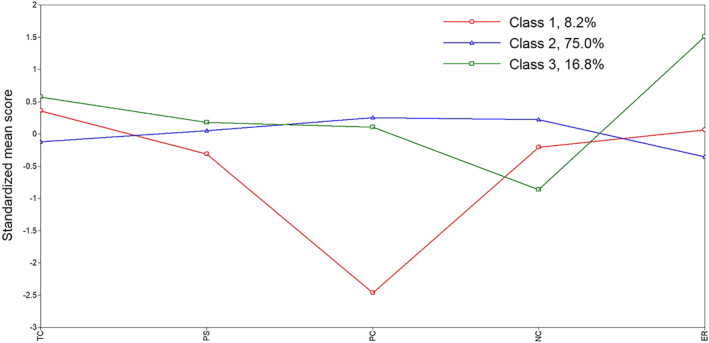
Plot of the standardised mean scores of self‐perceptions of ageing (SPA) across the three identified latent profiles in the validation sample. TC, timeline‐chronic; PS, Consequences Positive; PC, Control Positive; NC, Consequences and Control Negative; ER, Emotional Representations.
For comparisons of the five subscales across the three latent profiles, Table 3 displays mean, SD, and Cohen's d comparisons in the test and validation samples. Larger magnitudes of Cohen's d were found on the TC and Consequences and Control Negative subscales by pairwise comparisons of the LPCC subgroup and HANC subgroup in the test samples (1.203, 1.117) and by pairwise comparisons of the LPCC subgroup and LAPC subgroup in the validation samples (0.611, 1.142), respectively.
Table 3.
Mean, SD and Cohen's d of the three latent subgroups of self‐perceptions of ageing in the test and validation samples
| Sample | 1 LPCC | 2 LAPC | 3 HANC | d 2‐1 | d 3‐1 | d 3‐2 | |||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||||
| Test sample N = 451 | |||||||||
| TC | −0.190 | 0.956 | −0.138 | 1.000 | 0.818 | 0.700 | 0.053 | 1.203 | 1.107 |
| PS | −0.422 | 1.384 | −0.016 | 0.976 | −0.214 | 1.067 | 0.339 | 0.168 | 0.193 |
| PC | −3.193 | 0.794 | 0.155 | 0.732 | −0.184 | 0.964 | 4.384 | 3.407 | 0.396 |
| NC | −0.065 | 1.340 | 0.159 | 0.888 | −1.242 | 0.651 | 0.197 | 1.117 | 1.799 |
| ER | −0.026 | 0.965 | −0.252 | 0.689 | 2.179 | 0.738 | 0.269 | 2.567 | 3.405 |
| Validation sample N = 451 | |||||||||
| TC | 0.439 | 0.891 | −0.128 | 0.964 | 0.613 | 0.830 | 0.611 | 0.202 | 0.824 |
| PS | −0.285 | 0.942 | 0.054 | 0.960 | 0.148 | 1.089 | 0.356 | 0.425 | 0.009 |
| PC | −2.478 | 0.742 | 0.251 | 0.710 | 0.140 | 0.638 | 3.758 | 3.783 | 0.164 |
| NC | −0.219 | 1.142 | 0.219 | 0.905 | −0.945 | 0.886 | 1.142 | 0.710 | 1.299 |
| ER | 0.084 | 0.712 | −0.358 | 0.638 | 1.645 | 0.695 | 0.653 | 2.218 | 3.002 |
LPCC, low positive consequences and control subgroup; LAPC, low ageing awareness and high positive control subgroup; HANC, high ageing awareness and negative control subgroup; TC, timeline‐chronic; PS, Consequences Positive; PC, Control Positive; NC, Consequences and Control Negative; ER, Emotional Representations.
Comparison of demographic variables in each latent subgroup
For participants in the three‐class pattern of the test sample, there were no significant differences with respect to age, F (2) = 2.525, P = 0.082; or marital status, χ 2(6) = 2.105, P = 0.722; or education, χ 2(6) = 11.131, P = 0.083; or healthy lifestyles, χ 2(8) = 3.647, P = 0.731. LPCC had more females (75%) as compared with the other two subgroups (around 40%), χ 2(2) = 7.688, P = 0.021.
For participants in the three‐class pattern of the validation sample, there were no significant differences in age, F (2) = 1.962, p = 0.142; gender, χ 2(2) = 2.959, P = 0.228; or marital status, χ 2(6) = 10.498, P = 0.105; or smoking, χ 2(2) = 1.813, P = 0.404; or drinking, χ 2(2) = 2.944, P = 0.229; healthy diet, χ 2(2) = 1.409, P = 0.494; or healthy lifestyles, χ 2(6) = 8.124, P = 0.229. However, there were more participants with a college education (52%) and at least primary school education (4.1%) in LAPC than in other subgroups, χ 2(6) = 23.185, P = 0.001. More participants in LAPC also engaged in physical activity (90.1%) than the other two subgroups, χ 2(2) = 15.032, P = 0.001.
Relationships between SPA profiles and psychological outcomes
As shown in Table 4, regression mixture modelling demonstrated there was no difference between the LAPC subgroup and LPCC subgroup, while the HANC subgroup significantly had the highest and lowest mean scores on depressive symptoms and cognitive functions, respectively, in the test samples. As shown in Table 4, in terms of depressive symptoms and cognitive function, similar results were confirmed when the LAPC and HANC subgroups were compared between the test and the validation samples. However, unlike results in the test sample, there was no difference regarding depressive symptoms between the LPCC and HANC subgroups but a significant difference was found between LPCC and LAPC subgroups according to cognitive function in the validation sample, suggesting psychological outcomes fluctuated in the LPCC profile, which was uneven in both test and validation samples. It was notable that standardised mean scores of cognitive functions were consistently low in LPCC in both samples, indicating self‐control might be important for maintaining healthy cognitive functions.
Table 4.
Standardised mean scores of PHQ‐9, MMSE across latent profiles on self‐perceptions of ageing in the test and validation samples
| Sample | 1 LPCC | 2 LAPC | 3 HANC | Chi‐square | |||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SE | Mean | SE | Mean | SE | l vs 2 | 1 vs 3 | 2 vs 3 | |
| Test sample N = 451 | |||||||||
| PHQ‐9 | −0.057 | 0.205 | −0.170 | 0.040 | 1.020 | 0.283 | 0.285 | 9.303** | 16.544** |
| MMSE | −0.096 | 0.188 | 0.053 | 0.049 | −0.352 | 0.187 | 0.582 | 0.923 | 4.198** |
| Validation sample N = 451 | |||||||||
| PHQ‐9 | 0.242 | 0.241 | −0.166 | 0.044 | 0.606 | 0.175 | 2.724 | 1.447 | 16.991** |
| MMSE | −0.447 | 0.262 | 0.149 | 0.046 | −0.474 | 0.195 | 4.895* | 0.007 | 8.954** |
* P < 0.05, ** P < 0.01. LPCC, low positive consequences and control subgroup; LAPC, low ageing awareness and high positive control subgroup; HANC, high ageing awareness and negative control subgroup; PHQ, 9‐item Patient Health Questionnaire; MMSE, Mini‐Mental State Examination.
DISCUSSIONS
The present study extends previous research by exploring heterogenous profiles of SPA using LPA based on B‐APQ. Three distinct subgroups of SPA, characterised by different beliefs about ageing, control types, and ageing‐related emotions, were found among community‐dwelling Chinese older adults, supporting the existence of heterogenous subgroups beyond negative/positive SPA under the self‐regulation framework. Specifically, the largest subgroup, LAPC, was the most adaptive subgroup, while the second largest subgroup, HANC, was the most maladaptive according to differential associations with depressive symptoms and cognitive function. Nevertheless, cognitive functions were below average level in a particular LPCC subgroup characterised by the lowest scores on Consequences and Control Positive, indicating that adopting positive ageing perceptions rather than reducing negative aspects of SPA might be more beneficial for prevention and interventions against cognitive decline. Accordingly, more attention should be paid to individuals in the LPCC subgroup beyond the most maladaptive HANC subgroup for maintaining mental health of older adults.
Latent subgroup of SPA
Although positive attitudes of Chinese people toward ageing have been challenged after rapid sociocultural transformation and modernisation, our results support that overwhelmingly the majority of older adults' views on their own ageing were positive. The largest LAPC subgroup was similar to the positive SPA group in a two‐factor construct. Specifically, the lowest scores on depressive symptoms and cognitive decline in the LAPC subgroup indicated an adaptive psychological status in the majority of Chinese community‐dwelling older adults. Results in the LAPC subgroup were consistent with prior findings that feeling not old was associated with fewer depressive symptoms in the Chinese urban sample. 50 The reason may be linked to a self‐protective or self‐enhancement strategy because individuals in the LAPC subgroup viewed ageing as a process of consistent personal ongoing development. 51 Another explanation might be attributed to feelings of autonomy in older adults who had fewer depressive symptoms. 52 They considered their lives are controllable and they might be involved in more physical activities to adjust to ageing. 22 The highest level of Consequence and Control Negative (reverse‐coded) in the LAPC subgroup not only indicated high autonomy but also contributed to good cognitive performance. 20 More importantly, results from the LAPC subgroup might further highlight the importance of the self‐regulatory theory of SPA in individual mental health. 1 Both increasing positive and reducing negative consequences and control seem to be equally important for maintaining mental health of older adults in the LAPC subgroup.
The second largest HANC subgroup accounted for an average 14% in both samples. Older adults in the HANC subgroup had the highest level of Chronic‐Timeline and ER beyond depressive symptoms, supporting the previously identified link between negative SPA and depression using the variable‐centred method. 16 , 50 Consistent ageing awareness or ageing beliefs were found to be maladaptive and associated with increased depressive symptoms. The underlying mechanisms might be attributed to three aspects, including physiological pathways, such as high level of stress‐related C‐reactive protein 53 and cortisol levels in urine, 23 a psychosocial pathway such as self‐efficacy,54 and even a behavioural pathway such as physical activity. 9 , 11 Furthermore, it is worth noting that maladaptive psychological outcomes in the HANC subgroup might be attributed to its strikingly low levels of Consequence and Control Negative (reverse‐coded), regardless of moderate to the highest level of Consequence and Control Positive. Accordingly, healthcare providers should be aware that reducing negative consequences and control prevailed over increasing positive aspects of SPA for interventions in the HANC subgroup.
Approximately 6% of individuals on average labelled in the LPCC subgroup were characterised by the lowest levels of Consequences and Control Positive, confirming the hypothesis that differential subgroups exist apart from positive and negative SPA. 43 One underlying reason for the LPCC subgroup finding might be their expression of Consequences and Control Positive, such as, ‘whether I continue living life to the full depends on me’, which have been demonstrated as largely concentrating on gains in personal growth and self‐realisation rather than solely positive control strategies. 2 Some older adults might be hesitant to express growth because traditional Chinese culture is somewhat introverted and conservative in a collectivism cultural context. This explanation warrants further investigations. The varied depressive symptoms in the LPCC subgroup might be linked to differential magnitude of the effect size on TC between the LPCC and other subgroups, suggesting ageing awareness might be an important intervention target for treating depressive symptoms in this subgroup.
Relationships between different SPA profiles and cognitive functions
Feeling older or negative SPA is associated with cognitive decline, 19 , 20 while a positive SPA benefits older adults even with dementia. 55 Consistent with prior findings, individuals in the LAPC subgroup as opposed to their counterparts in the HANC subgroup believed they could control themselves, and use more cognitive strategies to maintain cognitive performance as they aged. 56 Regarding cognitive functioning, although differential statistical significances were found between the LPCC subgroup and LAPC subgroup in test and validation samples, cognitive functioning in the LPCC subgroup were consistent and lower than the average level in both the test and validation samples. Debates about the effects of different dimensions of the SPA on the impacts of cognitive function are ongoing. 19 , 20 , 21 Given individuals who had the lowest scores on Consequence and Control Positive in the LPCC subgroup also had low cognitive functioning, our results supported that positive rather than negative control of SPA might be more important for maintaining cognitive functions, indicating targeted interventions toward ageing attitudes in the LPCC subgroup.
The current study contributes to the existing literature by providing a novel perspective to advance our understanding of SPA categories. The study is also the first known study to explore the latent SPA profiles using LPA among older adults and illuminate the heterogeneous subgroups of SPA beyond traditional positive and negative SPA. Distinct SPA profiles among community‐dwelling Chinese older adults and their associations with mental health underscore the importance of taking a person‐centred approach to study of SPA in further research, given the rate of population ageing is extremely rapid and mental health problems might become a huge challenge in China. Our findings will benefit the design of targeted interventions for community‐dwelling Chinese older adults based on distinct profiles to improve mental health of older adults.
Limitations and future directions
First, the present study used convenience sampling that may limit the generalisability of our results to Chinese community‐dwelling older adults in urban areas. Findings should be re‐examined in Chinese rural areas and in other cultural settings because negative attitudes toward ageing are ubiquitous. Second, a cross‐sectional study design was unable to delineate causal relationships of different latent SPA profiles with emotional or cognitive outcomes. Further longitudinal research, therefore, is needed to better understand whether the identified three potent SPA profiles in older adults change over time and if psychological consequences vary after interventions.
From a cultural lens, the present findings might be unique, based on the samples from Henan Province which represents the traditional central plains culture of China, advocating filial piety, so that the majority of participants hold positive SPA. Small numbers of individuals within the LPCC subgroup disagreed with expressions in items of the Control Positive subscale such as ‘social life, relationships and living life to the full depends on me’ because these might not be encouraged in an Asian cultural context. 57 Individuals from cultures with high self‐expression reported more positive views toward new learning, which promotes better cognitive functioning. 58 In part, it is therefore understandable why older adults within the LPCC subgroup exhibited relatively high cognitive decline compared with counterparts in the LAPC subgroup.
It is necessary to examine in additional studies whether the robust three‐classification is still suitable in older adults aged 60–65 years or younger ones, such as using latent transition analysis and latent class growth modelling to better understand the dynamic characteristics of SPA profiles, in order to provide preventive strategies for inappropriate ageing perceptions.
In conclusion, three distinct profiles beyond the positive/negative SPA classification among Chinese community‐dwelling older adults can advance theoretical and methodological knowledge of SPA classification and further expand the self‐regulation framework of SPA. The majority of Chinese community‐dwelling older individuals hold adaptive SPA. Community health service providers should distinguish older adults with maladaptive SPA as target populations and adapt differential interventional strategies, either reducing feelings of negative control of ageing or improving positive control and consequently to maintain positive mental health among older adults.
Supporting information
Table S1 Comparison of demographic characteristics between the test and validation samples.
Table S2 Comparison of age, self‐perceptions of ageing (SPA) and psychological characteristics between the test and validation samples.
ACKNOWLEDGEMENTS
The author(s) disclosed receipt of the following financial support for the research, authorship, and /or publication of this article: This study was supported by the Project of Humanities and Social Sciences in Henan Province, Grant 2020‐ZZJH‐374, and The Key Scientific Research Projects in Colleges and Universities of Henan under Grant 21A310013.
Disclosure: The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
REFERENCES
- 1. Hausknecht S, Low LF, O'Loughlin K et al. Older adults' self‐perceptions of aging and being older: a scoping review. Gerontologist 2019; 60(7):e524–e534. [DOI] [PubMed] [Google Scholar]
- 2. Barker M, O'Hanlon A, McGee HM et al. Cross‐sectional validation of the Aging Perceptions Questionnaire: a multidimensional instrument for assessing self‐perceptions of aging. BMC Geriatr 2007; 7: 9–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sexton E, King‐Kallimanis BL, Morgan K, McGee H. Development of the brief ageing perceptions questionnaire (B‐APQ): a confirmatory factor analysis approach to item reduction. BMC Geriatr 2014; 14: 44–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Brothers A, Gabrian M, Wahl H‐W, Diehl M. A new multidimensional questionnaire to assess awareness of age‐related change (AARC). Gerontologist 2019; 59: e141–e151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. English AN, Bellingtier JA, Neupert SD. It's "the Joneses": the influence of objective and subjective socioeconomic status on subjective perceptions of aging. Eur J Ageing 2019; 16: 121–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pan Y, Chan SHW, Xu Y, Yeung KC. Determinants of life satisfaction and self‐perception of ageing among elderly people in China: an exploratory study in comparison between physical and social functioning. Arch Gerontol Geriatr 2019; 84: 103910. [DOI] [PubMed] [Google Scholar]
- 7. Sargent‐Co KA, Anstey KJ, Luszcz MA. Change in health and self‐perceptions of aging over 16 years: the role of psychological resources. Health Psychol 2012; 31: 423–432. [DOI] [PubMed] [Google Scholar]
- 8. Wurm S, Wiest M, Wolff JK, Beyer AK, Spuling SM. Changes in views on aging in later adulthood: the role of cardiovascular events. Eur J Ageing 2020; 17: 457–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Klusmann V, Sproesser G, Wolff JK, Renner B. Positive self‐perceptions of aging promote healthy eating behavior across the life span via social‐cognitive processes. J Gerontol B Psychol Sci Soc Sci 2019; 74: 735–744. [DOI] [PubMed] [Google Scholar]
- 10. Levy BR, Slade MD, Kunkel SR, Kasl SV. Longevity increased by positive self‐perceptions of aging. J Pers Soc Psychol 2002; 83: 261–270. [DOI] [PubMed] [Google Scholar]
- 11. Zhang X, Kamin ST, Liu S, Fung HH, Lang FR. Negative self‐perception of aging and mortality in very old Chinese adults: the mediation role of healthy lifestyle. J Gerontol B Psychol Sci Soc Sci 2020; 75: 1001–1009. [DOI] [PubMed] [Google Scholar]
- 12. Brothers A, Kornadt AE, Nehrkorn‐Bailey A, Wahl HW, Diehl M. The effects of age stereotypes on physical and mental health are mediated by self‐perceptions of aging. J Gerontol B Psychol Sci Soc Sci 2021; 76: 845–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tovel H, Carmel S, Raveis VH. Relationships among self‐perception of aging, physical functioning, and self‐efficacy in late life. J Gerontol B Psychol Sci Soc Sci 2019; 74: 212–221. [DOI] [PubMed] [Google Scholar]
- 14. Wen Y, Liu C, Liao J, Yin Y, Wu D. Incidence and risk factors of depressive symptoms in 4 years of follow‐up among mid‐aged and elderly community‐dwelling Chinese adults: findings from the China Health and Retirement Longitudinal Study. BMJ Open 2019; 9: e029529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Freeman AT, Santini ZI, Tyrovolas S, Rummel‐Kluge C, Haro JM, Koyanagi A. Negative perceptions of ageing predict the onset and persistence of depression and anxiety: findings from a prospective analysis of the Irish Longitudinal Study on Ageing (TILDA). J Affect Disord 2016; 199: 132–138. [DOI] [PubMed] [Google Scholar]
- 16. Gum AM, Ayalon L. Self‐perceptions of aging mediate the longitudinal relationship of hopelessness and depressive symptoms. Int J Geriatr Psychiatry 2018; 33: 591–597. [DOI] [PubMed] [Google Scholar]
- 17. Luo MS, Li LW. Are self‐perceptions of aging associated with health trajectories among middle‐aged and older adults? Gerontologist 2020; 60: 841–850. [DOI] [PubMed] [Google Scholar]
- 18. Levy BR, Zonderman AB, Slade MD, Ferrucci L. Memory shaped by age stereotypes over time. J Gerontol B Psychol Sci Soc Sci 2012; 67: 432–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Stephan Y, Sutin AR, Luchetti M et al. Feeling older and the development of cognitive impairment and dementia. J Gerontol B Psychol Sci Soc Sci 2017; 72: 966–973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Robertson DA, King‐Kallimanis B, Kenny RA. Negative perceptions of aging predict longitudinal decline in cognitive function. Psychol Aging 2016; 31: 71–81. [DOI] [PubMed] [Google Scholar]
- 21. Brown KE, Kim J, Stewart T, Fulton E, McCarrey AC. Positive, but not negative, self‐perceptions of aging predict cognitive function among older adults. Int J Aging Hum Dev 2020; 93(1):543–561. [DOI] [PubMed] [Google Scholar]
- 22. Xiao L, Yang H, Du W et al. Subjective age and depressive symptoms among Chinese older adults: a moderated mediation model of perceived control and self‐perceptions of aging. Psychiatry Res 2019; 271: 114–120. [DOI] [PubMed] [Google Scholar]
- 23. Levy BR, Moffat S, Resnick SM, Slade MD, Ferrucci L. Buffer against cumulative stress: positive age self‐stereotypes predict lower cortisol across 30years. GeroPsych 2016; 9(3):141–146. [Google Scholar]
- 24. Marquet M, Boutaayamou M, Schwartz C et al. Does negative information about aging influence older adults' physical performance and subjective age? Arch Gerontol Geriatr 2018; 78: 181–189. [DOI] [PubMed] [Google Scholar]
- 25. Schroyen S, Letenneur L, Missotten P et al. Impact of self‐perception of aging on mortality of older patients in oncology. Cancer Med 2020; 9: 2283–2289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sun JK, Smith J. Self‐perceptions of aging and perceived barriers to care: reasons for health care delay. Gerontologist 2017; 57: S216–S226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Huy C, Schneider S, Thiel A. Perceptions of aging and health behavior: determinants of a healthy diet in an older German population. J Nutr Health Aging 2010; 14: 381–385. [DOI] [PubMed] [Google Scholar]
- 28. Kotter‐Grühn D, Kornadt AE, Stephan Y. Looking beyond chronological age: current knowledge and future directions in the study of subjective age. Gerontology 2015; 62: 86–93. [DOI] [PubMed] [Google Scholar]
- 29. Berlin KS, Williams NA, Parra GR. An introduction to latent variable mixture modeling: overview and cross‐sectional latent class and latent profile analyses. J Pediatr Psychol 2014; 39: 174–187. [DOI] [PubMed] [Google Scholar]
- 30. Jung S, Cham H, Siedlecki KL, Jopp DS. Measurement invariance and developmental trajectories of multidimensional self‐perceptions of aging in middle‐aged and older adults. J Gerontol B Psychol Sci Soc Sci 2021; 76: 483–495. [DOI] [PubMed] [Google Scholar]
- 31. Burton AE, Dean SE, Demeyin W, Reeves J. Questionnaire measures of self‐directed ageing stereotype in older adults: a systematic review of measurement properties. Eur J Ageing 2020; 18(1):117–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Jaafar MH, Villiers‐Tuthill A, Sim SH, Lim MA, Morgan K. Validation of the brief ageing perceptions questionnaire (B‐APQ) in Malaysia. Aging Ment Health 2020; 24: 620–626. [DOI] [PubMed] [Google Scholar]
- 33. Slotman A, Cramm JM, Nieboer AP. Validation of the Aging Perceptions Questionnaire Short on a sample of community‐dwelling Turkish elderly migrants. Health Qual Life Outcomes 2017; 15: 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Sadegh Moghadam L, Foroughan M, Mohammadi Shahboulaghi F, Ahmadi F, Sajjadi M, Farhadi A. Validity and reliability of the Persian version of the brief aging perceptions questionnaire in Iranian older adults. Clin Interv Aging 2016; 11: 507–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Chen X, Hu Y, Zhu D, Li J, Zhou L. Chinese version of the aging perceptions questionnaire (C‐APQ): assessment of reliability and validity. Aging Ment Health 2016; 20: 567–574. [DOI] [PubMed] [Google Scholar]
- 36. Robertson DA, Savva GM, King‐Kallimanis BL, Kenny RA. Negative perceptions of aging and decline in walking speed: a self‐fulfilling prophecy. PLoS One 2015; 10: e0123260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ng R, Allore H, Trentalange M et al. Increasing negativity of age stereotypes across 200 years: evidence from a database of 400 million words. PLoS One 2015; 10: e0117086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Villiers‐Tuthill A, Copley A, McGee H, Morgan K. The relationship of tobacco and alcohol use with ageing self‐perceptions in older people in Ireland. BMC Public Health 2016; 16: 627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Gu R, Zhang D, Jin X et al. The self‐perceptions of aging were an important factor associated with the quality of life in Chinese elderly with hypertension. Psychogeriatrics 2019; 19: 391–398. [DOI] [PubMed] [Google Scholar]
- 40. Wang YR, Lee HF, Chen CM. Validating a brief aging perception questionnaire (B‐APQ) for older persons with chronic disease in Taiwan. Aging Ment Health 2021; 25: 1143–1150. [DOI] [PubMed] [Google Scholar]
- 41. Boeder J, Tse DCK. Measuring self‐perceptions of aging: differences between measures when predicting health outcomes. J Gerontol B Psychol Sci Soc Sci 2021; 76: 825–835. [DOI] [PubMed] [Google Scholar]
- 42. Gu J, Karl A, Baer R, Strauss C, Barnhofer T, Crane C. Latent profile analysis of the five facet mindfulness questionnaire in a sample with a history of recurrent depression. Assessment 2020; 27: 149–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Turner SG, Hooker K, Geldhof GJ. Self‐perceptions of aging: factorial structure and invariance by gender. Gerontologist 2021; 61: 425–429. [DOI] [PubMed] [Google Scholar]
- 44. Li H, Jia J, Yang Z. Mini‐mental state examination in elderly Chinese: a population‐based normative study. J Alzheimers Dis 2016; 53: 487–496. [DOI] [PubMed] [Google Scholar]
- 45. Hou Y, Wu Q, Zhang D, Jin X, Wu W, Wang X. The differences in self‐perceptions of aging, health‐related quality of life and their association between urban and rural Chinese older hypertensive patients. Health Qual Life Outcomes 2020; 18: 154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Muthén LK, Muthén BO. Mplus User's Guide, 7th edn. Los Angeles, CA: Muthén & Muthén, 1998. ‐2012. [Google Scholar]
- 47. Muller K. Statistical power analysis for the behavioral sciences. Dent Tech 1989; 31(4):499–500. [Google Scholar]
- 48. Dziak JJ, Bray BC, Zhang J, Zhang M, Lanza ST. Comparing the performance of improved classify‐analyze approaches for distal outcomes in latent profile analysis. Methodology (Gott) 2016; 12: 107–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Equ Modeling 2007; 14(4):535–569. [Google Scholar]
- 50. Liang K. The cross‐domain correlates of subjective age in Chinese oldest‐old. Aging Ment Health 2014; 18: 217–224. [DOI] [PubMed] [Google Scholar]
- 51. Liang K. Differential associations between subjective age and depressive symptoms among urban and rural Chinese older adults. Aging Ment Health 2020; 24: 1271–1277. [DOI] [PubMed] [Google Scholar]
- 52. Paque K, Goossens K, Elseviers M, van Bogaert P, Dilles T. Autonomy and social functioning of recently admitted nursing home residents. Aging Ment Health 2017; 21: 910–916. [DOI] [PubMed] [Google Scholar]
- 53. Stephan Y, Sutin AR, Terracciano A. Younger subjective age is associated with lower C‐reactive protein among older adults. Brain Behav Immun 2015; 43: 33–36. [DOI] [PubMed] [Google Scholar]
- 54. Dutt AJ, Wahl HW. Future time perspective and general self‐efficacy mediate the association between awareness of age‐related losses and depressive symptoms. Eur J Ageing 2019; 16: 227–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Sabatini S, Ukoumunne OC, Martyr A et al. Relationship between self‐perceptions of aging and 'living well' among people with mild‐to‐moderate dementia: findings from the ideal programme. Arch Gerontol Geriatr 2021; 94: 104328. [DOI] [PubMed] [Google Scholar]
- 56. Neupert SD, Allaire JC. I think I can, I think I can: examining the within‐person coupling of control beliefs and cognition in older adults. Psychol Aging 2012; 27: 742–749. [DOI] [PubMed] [Google Scholar]
- 57. Kim HS, Sherman DK. "Express yourself": culture and the effect of self‐expression on choice. J Pers Soc Psychol 2007; 92: 1–11. [DOI] [PubMed] [Google Scholar]
- 58. Löckenhoff CE, De Fruyt F, Terracciano A et al. Perceptions of aging across 26 cultures and their culture‐level associates. Psychol Aging 2009; 24: 941–954. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Comparison of demographic characteristics between the test and validation samples.
Table S2 Comparison of age, self‐perceptions of ageing (SPA) and psychological characteristics between the test and validation samples.


