Supplemental Digital Content is Available in the Text.
Key Words: Multifocal soft contact lenses, Myopia, Orthokeratology, Myopia control
Abstract
Objectives:
This randomized, single-blind, clinical trial compared the effectiveness of multifocal soft contact lenses (MFSCLs), orthokeratology contact lenses (Ortho-kCLs), and single vision spectacles (SVSs) for myopia control.
Methods:
Sixty-six eligible Chinese subjects, aged 7 to 15 years old with cycloplegic refraction measurements between −1.00 and −8.00 diopters (D), astigmatism not more than 1.00 D, and no history of myopia control treatment, were randomly assigned to wear MFSCLs, Ortho-kCLs, or SVSs for 1 year. For all three groups, baseline measurements of cycloplegic refraction, axial length (AL), and corneal endothelial cell density (CECD) were made. At the 6- and 12-month follow-up visits, changes in cycloplegic refraction, AL, and CECD were measured in the MFSCL and SVS groups. For the Ortho-kCL group, only changes in the AL were measured at 6 and 12 months, and CECD was measured at the 12-month follow-up visit.
Results:
After 1 year of lens wear, myopia progression of the SVS group, −0.938±0.117 D, was greater than that of the MFSCLs group, −0.591±0.106 D (P=0.032). Thus, MFSCLs reduced the rate of myopia progression by 37.0% compared with the SVSs. The AL elongations after 1 year were 0.30±0.03 mm for MFSCLs (P=0.027 vs SVSs), 0.31±0.04 mm for Ortho-kCLs (P=0.049 vs SVSs), and 0.41±0.04 mm for SVSs. Compared with the SVS group, the reduction in AL elongation was 26.8% and 24.4% in the MFSCL and Ortho-kCL groups, respectively. There were no significant differences in CECD among the three groups (P>0.05).
Conclusions:
Compared with SVSs, wearing MFSCLs and Ortho-kCLs significantly delayed myopia progression. MFSCLs and Ortho-kCLs are safe and promising methods of myopia control (chictr.org number, ChiCTR2100048452).
Myopia is one of the most common diseases, the prevalence of which is higher in East Asia than in western countries.1–3 In China, the myopia rate of high school students has reached 84%.4 It is estimated that there will be 4,758 million myopes by 2050, which is nearly double that in 2020.5 Myopia can cause many vision-threatening diseases, such as choroidal neovascularization, retinal detachment, glaucoma, cataract, maculopathy, and others.6–10 Therefore, it is crucial to take early measures to control the development of myopia in children and prevent the occurrence of partial or complete loss of vision. Besides behavior management, there are many ways to control the progression of myopia, such as rigid gas-permeable contact lenses, peripheral defocusing soft contact lenses such as multifocal soft contact lenses (MFSCLs), orthokeratology contact lenses (Ortho-kCLs), bifocal or multifocal spectacles, and antimuscarinic agents.11–14 Daily disposable MFSCLs not only avoid the inconvenience of wearing spectacles and the complexity of cleaning Ortho-kCLs but also minimize the adverse reactions that can occur with other treatments, even with the correct care and guidance.15–19
Many animal20,21 and human22 studies have confirmed that peripheral defocus can control eye growth. Ortho-kCLs and MFSCLs may reduce axial elongation by inducing peripheral myopia defocus.23,24 However, the relative effectiveness of MFSCLs on myopia control compared with Ortho-kCLs has not been determined. Therefore, the purpose of this randomized clinical trial was to determine if MFSCLs and Ortho-kCLs retard the progression of myopia in adolescents in comparison to single vision spectacles (SVSs). The effectiveness was evaluated by changes of cycloplegic refraction and axial length (AL) over a one-year study period.
METHODS
Study Design
This was a parallel, longitudinal, single-blind, randomized clinical trial conducted in two centers to investigate the change of cycloplegic refraction, AL, and corneal endothelial cell density (CECD) in myopic children wearing MFSCLs, Ortho-kCLs, or SVSs for 1 year. The protocol was conducted in conformance with the Declaration of Helsinki and approved before study initiation by the Institutional Review Boards of The First and The Fourth Affiliated Hospital, Zhejiang University School of Medicine. Written informed consents were obtained from both subjects and their parents before participation in the study, which was performed at the two hospitals.
An online resource was used to generate the random group allocation sequence. One investigator was unmasked for enrolling the participants, generating the random allocation sequence, grouping, lens fitting, clinical aftercare, evaluating lens condition, and recording data. The investigating optometrists, who underwent standardized training for making outcome measurements, were masked.
Participants
Children aged between 7 and 15 years who visited either of the two hospitals between January 1, 2019, and March 31, 2020, were recruited according to the study protocol. Inclusion criteria were cycloplegic refraction measurements between −8.00 diopters (D) and −1.00 D, astigmatism of ≤1.00 D, myopia progression of ≥0.75 D in the last year or≥0.50 D in the last 6 months, ability to complete a follow-up of at least 12 months, ability to understand the purpose of the trial, and voluntarily participate. Exclusion criteria were history of ocular injury, ocular surgery, tumor, or chronic ocular disease, contraindication and previous experience in contact lens wearing, other myopia treatment in the past, unwilling or unable to participate in follow-up visits on time, poor compliance with treatment, or suffering from chronic systemic disease. Recruited subjects from the two hospitals (n=40, n=41, respectively) were examined in each hospital and randomly assigned to the MFSCL, Ortho-kCL, or the SVS group. For this study, participants wearing the SVSs were designated as the control group, and those wearing the MFSCLs or the Ortho-kCLs were designated as the treatment groups.
Sample Size
The sample size was calculated to determine if changes in spherical equivalent refraction (SER) or in AL in the MFSCL and Ortho-kCL groups progressed slower compared with the SVS group. The sample size estimation was based on the number of subjects needed to detect, with a power of 80% and an alpha level difference of 0.05, differences in axial elongation of at least 0.15 mm per year among the groups. For these calculations, we assumed a measurement SD of 0.15 mm.14,25 Based on the calculations, a minimum sample size of 19 was required for each group. Thus, the final sample size was sufficient to detect statistical differences in the measured parameters for each group.
Lenses
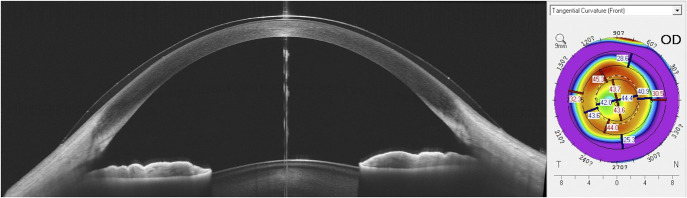
The BioThin (Bio Optic, Inc., Taiwan, China) MFSCLs used in this study used an aspheric design fitted by conics that allowed manipulation of the spherical aberration to modify the depth of focus. The lens material, ocufilcon D, was a copolymer of 2-hydroxyethylmethacrylate and methacrylic acid, cross-linked with ethylene glycol dimethacrylate, plus initiator. The water content was 55%, and the oxygen permeability DK was 20×10−11 (cm2/s) (ml O2/ml×mm Hg). The overall diameter was 14.20±0.20 mm (Fig. 1). The MFSCLs had a unique central back with a base curve radius ranging from 8.20 to 9.20 mm. The front surface had an aspherical design with two different optic zones. One of the zones was 7.52±0.20 mm in diameter, with a central apical zone of 2.50 mm, which provided the target refractive power for distance vision correction. The annular zone, with diameters ranging from 2.50 to 7.50 mm, was the treatment zone in which the power gradient from the target refractive power to the periphery of the lens was +6.0 D. This design corresponded to about 35 degrees of retinal eccentricity. Optical coherence tomography (OCT, VG200; SVision Imaging, Ltd, Luoyang, China) of an eye wearing an MFSCL showed the novel aspheric design as revealed in the corneal topography map illustrating the multifocal ring formed by the lens (Fig. 2).
FIG. 1.
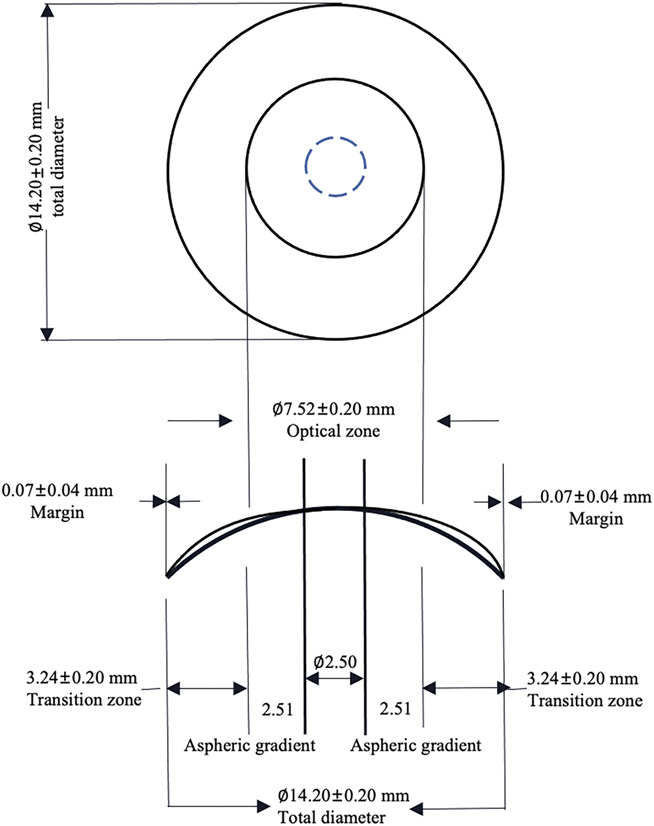
Design of the BioThin multifocal soft contact lens.
FIG. 2.
Optical coherence tomography and topography map of an eye wearing an MFSCL. The OCT image (left) shows the novel aspheric design of a −3.75 D lens. The corneal topography map (right) reveals the multifocal ring formed by the lens. OCT, optical coherence tomography; MFSCL, multifocal soft contact lens; D, diopter. OD, oculus dexter (right eye).
Multifocal soft contact lens fitting was performed after measurement of the visible iris diameter, corneal curvature, and subjective refraction in the uncorrected state. Adjustments to the final prescription were based on spherical overrefraction.
The dimensions of the Ortho-kCLs (Paragon CRT, Paragon, Gilbert, AZ) were calculated based on the manufacturer's protocols. The Ortho-kCLs were designed to have a congruent anterior and posterior surface, each consisting of a central zone, a mathematically designed sigmoidal corneal proximity “return zone,” a noncurved (tangent) landing zone, and a convex elliptical edge zone joining both surfaces.26
Single vision spectacle fitting was performed by subjective refraction. The lenses used in the SVS group were products of Zeiss (Carl Zeiss Jena GmbH, Jena, Germany). If the monocular best-corrected visual acuity (BCVA) was less than 20/20 or the residual SER was more than 0.50 D during a follow-up visit, the previous treatment prescription was updated according to the subject's conditions.
Study Procedures
Subjects in the MFSCL group were required to wear their lenses for 12 hr per day (8 am–8 pm) and then to wear their spectacles afterward. All subjects were required to wear the prescribed treatment every day. Subjects in the Ortho-kCL group were required to wear their lenses before going to bed until waking up the next morning, ensuring that they wore the lenses for at least 8 hr during sleep. The subjects in the SVS group were required to wear their spectacles beginning at 8 am every day until going to bed.
At the initial visit to establish baseline values, the eye examination included measurements of AL, corneal curvature, refraction, and CECD. All subjects then participated in follow-up visits at 6 and 12 months to reassess these parameters. For subjects in the Ortho-kCL group, the cycloplegic refraction measurements were taken only at baseline because cessation of wearing the Ortho-kCL for less than four weeks would cause the measurements to be inexact. Therefore, we did not take the measurements at the 6- and 12-month visits. And, CECD was measured at the baseline and 12-month visit. Clinical care was provided by a practitioner at the two hospitals throughout the study period.
AL measurements were performed by IOLMaster 700 (Carl Zeiss Jena GmbH). Corneal curvature (Pentacam HR; Oculus Optikgera¨te GmbH, Wetzlar, Germany) was measured in the Ortho-kCL and MFSCL groups. Cycloplegia was then induced with 1 to 2 drops of 1% cyclopentolate HCL (Alcon Laboratories, Fort Worth, TX) instilled every 5 min over a 15-min period. Cycloplegic refraction was performed 45 min later by autorefraction (Humphrey Autorefractor Keratometer HARK-599; Carl Zeiss Meditec AG, Jena, Germany). Corneal endothelial cell density was evaluated by a noncontact specular microscope (SP-3000 P; Topcon, Tokyo, Japan).
Statistical Analysis
There were no statistically significant differences between data from the two eyes of each subject, and only data of right eyes were included in the analyses. Statistical analysis (SPSS software ver. 26.0, SPSS, Inc., Chicago, IL) was performed by the principal investigator. The baseline characteristics, AL elongation, and changes in SER among the three groups were compared using analysis of variance. Repeated-measures analysis of variance tests were used to analyze the changes in AL, SER, and CECD during the study period. At different times, CECD within each of the three groups were compared by paired t test.
The intention-to-treat approach was used to analyze the data of subjects who dropped out. The missing data were handled by the generalized estimating equations of SPSS. Generalized estimating equations were used to determine the effect of different treatments on the changes of AL, SER, and CECD adjusted for some covariates with one within-subject factor (time), one between-subject factor (treatments), and the interactions. Covariates included gender, age, initial AL, and initial SER.
The treatment effects of Ortho-kCL and MFSCL on AL were calculated as follows12,25:
,
where ALe is axial length elongation.
The treatment effects on SER were also calculated by this formula.
RESULTS
Baseline Measurements
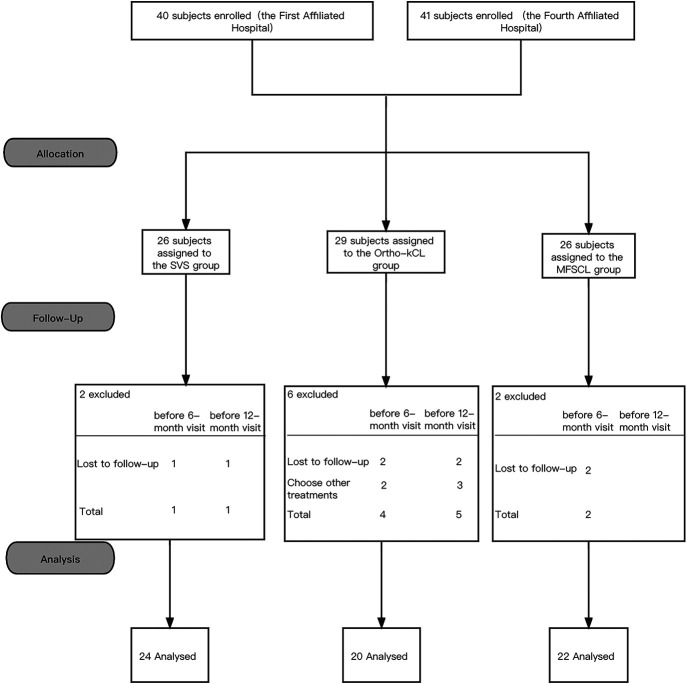
After recruitment and basic screening, 81 children from the two hospitals participated in the study and were assigned to either the MFSCL group (n=26), the Ortho-kCL group (n=29), or the SVS group (n=26). Finally, 66 subjects completed the one-year study (MFSCL, n=22; Ortho-kCL, n=20; SVS, n=24; Fig. 3).
FIG. 3.
Flow diagram of study progression.
Among the three groups, there were no significant differences in age, initial SER, initial AL, or CECD (all P>0.05, Table 1). The mean initial SER in the MFSCL, Ortho-kCL, and SVS groups were −3.144±0.303, −2.659±0.208, −3.005±0.285 D, respectively. The mean initial AL in the MFSCL, Ortho-kCL, and SVS groups were 25.10±0.20, 24.85±0.14, and 24.96±0.20 mm, respectively. The mean initial CECD in the MFSCL, Ortho-kCL, and SVS groups were 3,045.25±82.51, 3,136.63±15.88, and 3,102.55±29.53 cells per square millimeter, respectively (Table 1). Of those who completed the study, there were more female patients than male patients in the MSFCL group than in the SVS group (P=0.019), but there were no other significant gender differences between the groups. The BCVA of the subjects receiving any of the three treatments was not less than 20/20.
TABLE 1.
Group Baseline Data
| Parameter | All | Completed | Discontinued | ||||||
| MFSCL (n=26) | Ortho-kCL (n=29) | SVS (n=26) | MFSCL (n=22) | Ortho-kCL (n=20) | SVS (n=24) | MFSCL (n=4) | Ortho-kCL (n=9) | SVS (n=2) | |
| Age (years) | 12.8±0.1 | 12.5±0.2 | 13.0±0.2 | 12.8±0.2 | 12.5±0.3 | 13.0±0.2 | 12.5±0.3 | 12.6±0.4 | 12.5±0.5 |
| Gender (F:M) | 14:12 (54% F) | 12:17 (41% F) | 8:18 (31% F) | 14:8 (64% F)a | 8:12 (40% F) | 7:17 (29% F) | 0:4 (0 of 4 F) | 4:5 (4 of 9 F) | 1:1 (1 of 2 F) |
| SER (D) | −3.144±0.303 | −2.659±0.208 | −3.005±0.285 | −3.233±0.326 | −2.681±0.279 | −3.031±0.306 | −2.656±0.880 | −2.611±0.270 | −2.688±0.688 |
| AL (mm) | 25.10±0.20 | 24.85±0.14 | 24.96±0.20 | 25.14±0.22 | 24.97±0.15 | 25.02±0.20 | 24.94±0.57 | 24.57±0.30 | 24.24±0.97 |
| CECD (cells/mm2) | 3,045.25±82.51 | 3,136.63±15.88 | 3,102.55±29.53 | 3,034.59±89.77 | 3,169.63±18.04 | 3,128.78±28.83 | 3,162.50±50.50 | 3,070.64±12.58 | 2,984.50±31.50 |
Continuous variables presented as mean±SDs.
AL, axial length; CECD, corneal endothelial cell density; D, diopter; F, female; MFSCL, multifocal soft contact lens; Ortho-kCL, orthokeratology contact lens; M, male; SER, spherical equivalent refraction; SVS, single vision spectacles.
MFSCL vs. SVS P=0.019.
Spherical Equivalent Refraction Changes
Repeated-measures analysis of variance showed that both treatments (P=0.039) and times (P<0.0001) had a significant effect on SER changes. At the 6-month follow-up visit, there were no differences in the changes of SER from the baseline values for the MFSCL (n=22) and SVS (n=24) groups (Table 2). However, at 12 months, the change in SER of the MFSCL group, −0.631±0.118 D, was smaller than that of the SVS group, −1.005±0.116 D (P=0.029, Table 2). Compared with the SVS group, the progression of myopia in the MFSCL group decreased by 37.2%.
TABLE 2.
Changes in SER, AL, and CECD
| Parameter | MFSCL (n=22) | Ortho-kCL (n=20) | SVS (n=24) |
| ΔSER (D) | |||
| 6 months | −0.489±0.093 | nd | −0.661±0.091 |
| 12 months | −0.631±0.118a | nd | −1.005±0.116 |
| ΔAL (mm) | |||
| 6 months | 0.13±0.02b | 0.18±0.03 | 0.22±0.02 |
| 12 months | 0.31±0.03c | 0.34±0.04d | 0.45±0.04 |
| ΔCECD (cells/mm2) | |||
| 6 months | 2,999.10±88.77 | nd | 3,079.63±55.96 |
| 12 months | 2,982.97±67.41 | 3,165.78±18.02 | 3,084.88±45.19 |
Values are mean±SDs.
MFSCL vs. SVS P=0.029.
MFSCL vs. SVS P=0.007.
MFSCL vs. SVS P=0.006.
Ortho-kCL vs. SVS P=0.043. All other comparisons were not statistically significant.
Δ, change; AL, axial length; CECD, corneal endothelial cell density; nd, not done; Ortho-kCL, orthokeratology contact lens; MFSCL, multifocal soft contact lens; SER, spherical equivalent refraction; SVS, single vision spectacles.
After adjustment of the model, different treatments (P=0.033) and times (P<0.0001) were significantly associated with the magnitude of SER progression. The mean change of SER in the MFSCL group (n=26), −0.591±0.106 D, was smaller than in the SVS group (n=26), −0.938±0.117 D (P=0.032, see Table, Supplemental Digital Content 1, http://links.lww.com/ICL/A213). Thus, the progression of myopia in the MFSCL group decreased by 37.0% when compared with the SVS group.
Axial Length Changes
Repeated-measures analysis of variance showed that the treatments had a significant effect on axial elongation (P=0.014). At 6 months, the AL elongation of the MFSCL group (n=22), 0.13±0.02 mm, was significantly slower than that of the SVS group (n=24) (P=0.007, Table 2). In contrast, AL elongation of the Ortho-kCL group (n=20) was 0.18±0.03 mm, which was not significantly different from the SVS group. At 12 months, the AL elongation of the MFSCL group and Ortho-kCL group were 0.31±0.03 and 0.34±0.04 mm, respectively, both of which were less than the 0.45±0.04 mm (P=0.006 and P=0.043, Table 2) in the SVS group. Compared with the SVS group, axial elongation was reduced by 31.1% in the MFSCL group and 24.4% in the Ortho-kCL group.
The model-adjusted changes of AL were 0.30±0.03, 0.31±0.04, and 0.41±0.04 mm for the MFSCL (n=26), Ortho-kCL (n=29), and SVS (n=26) treatments, respectively. Different treatments (P=0.024) and times (P<0.0001) were significantly associated with the magnitude of axial elongation. Compared with the SVS group, the reduction in AL elongation was 26.8% and 24.4% in the MFSCL group and Ortho-kCL group, respectively (P=0.027, P=0.049, respectively, see Table, Supplemental Digital Content 1, http://links.lww.com/ICL/A213). The adjusted changes in the two treatment groups were not significantly different from one another (P=0.528). After controlling for covariates, there were no significant changes in the effects of the different treatments compared with the unadjusted means.
Corneal Endothelial Cell Density
The baseline CECD for the MFSCL group (n=22) was 3,034.59±89.77 cells per square millimeter (Table 1), and there were no significant changes at six or 12 months (P=0.969, P=0.072, respectively, Table 2). The CECD of 16 subjects in the Ortho-kCL group (n=20) were tested during the follow-up period between 11 and 17 months after study initiation (13.38±1.67 months). The baseline CECD for the Ortho-kCL group was 3,169.63±18.04 cells per square millimeter, and there were no significant changes at 12 months (P=0.51, Table 2). At baseline, the SVS (n=24) CECD was 3,128.78±28.83 cells per square millimeter (Table 1), and there were no significant changes at six or 12 months (P=0.118, P=0.050, respectively, Table 2).
After adjustment of the model, CECD in three groups did not change over time to a statistically significant degree. The CECD at 12 months were 2,898.60±60.45, 3,134.07±15.64, and 3,067.64±34.82 cells per square millimeter in the MFSCL (n=26), Ortho-kCL (n=29), and SVS (n=26) groups, respectively, and there were no significant differences among the three groups in any of the periods (P>0.05, see Table, Supplemental Digital Content 1, http://links.lww.com/ICL/A213).
DISCUSSION
It is commonly thought that the occurrence and progression of myopia are caused by peripheral hyperopic defocus.27 In animal models28 and in humans,29 the progression of myopia is influenced by the visual input at the retina. Many studies have shown that increasing the peripheral myopic defocus slows the progression of myopia.12,23,30,31 These results are consistent with our present findings. Although our results did not reach the expected difference of 0.15 mm, which did not seem to have clinical meaningfulness but were truly significantly slower than the SVS group. The 0.1-mm AL reduction corresponds to the 0.30 D SER decrease per year, which still plays an important role in the long run of myopia control.
Although the design, defocus amount, and size of the central distance zone of the MFSCLs used here are different from other MSFCLs, the effectiveness in myopia and axial elongation control were consistent with those reported for other similar lenses, for example, 25% to 51%12,23,30,32 and 0.06 to 0.15 mm/year.12,23,25,30 The defocus amount of the MFSCLs in our study was+6.00 D, compared with the +2.00 D reported by Anstice et al.,32 the +1.00 D at the 2-mm semichord reported by Sankaridurg et al.,23 and the +2.50 D reported by Lam et al.12 These factors will affect the ability of MFSCLs to control myopia progression; therefore, it is important to continue exploring the optimal defocus amount and the correction area of MFSCLs to achieve the best myopia control.
As children age, the rate of axial elongation slows, and the therapeutic effect of controlling myopia will become less evident.33 Thus, in older children, the treatment effect, measured as a percentage change, may be similar to that in younger children. However, the impact in terms of slowing myopia progression and inhibiting associated vision-threatening diseases may be less obvious because axial growth in older children is generally less than that in younger ones. In the present study, the AL elongation in the MFSCL group was smaller at the first 6-month visit than at the 12-month visit. The effect on myopia control by MFSCLs was also more significant during the first 6 months. However, 6 months may not be enough time to fully manifest the above changes. Therefore, for periods greater than 6 months, the influence of age on myopia control should be considered along with any therapeutic effects when deciding on the best course of treatment. Activities such as increased outdoor time34 and decreased near work35 are considered to reduce the development of myopia. Although the durations of these activities were not strictly regulated during the first and second 6 months of our study, they could have contributed to the differences in myopia progression associated with the three treatment groups during the two periods. Future studies should consider these variables as covariates and explore the effect of different optical treatments such as the lenses used in this study.
In our study, there was no difference in the reduction in AL elongation between the MFSCL and Ortho-kCL groups (P=0.528). However, the treatment effect on AL elongation, 26.8% for the MFSCLs, was superior to 24.4% for Ortho-kCLs. This seems to contradict the conclusion from Pauné et al., who reported that MFSCLs were less effective in controlling myopia progression than were Ortho-kCLs25 (27% and 38%, resp.). Pauné et al. also reported that compared with subjects wearing spectacles, Ortho-kCLs reduced SER progression by 67%, whereas soft radial refractive gradient contact lenses reduced it by only 43%. However, the subjects in that study did not stop wearing the Ortho-kCLs when the SER measurements were made. Thus, the Ortho-kCL effect on SER was not washed out, making the corneal central epithelium thinner and the midperipheral stroma thicker,36 which likely affected the results; therefore, it was not appropriate to compare the changes of refractive error under these circumstances.14 Axial elongation can serve as a good indicator of myopia progression where refractive state cannot be measured independently when wearing Ortho-kCL.37 Additionally, although we did not measure the amount of corneal central epithelium flattening or the anterior chamber depth changes after wearing Ortho-kCLs, Ortho-kCLs can flatten the central cornea epithelium by 19.0±2.6 μm,36 which will affect the AL measurement, that is, the distance from the anterior cornea to retinal pigment epithelium. The flattening effect of the Ortho-kCLs31,36,38 could result in an overestimate of myopia control. This calls into question the conclusion of Pauné et al.25 that the myopia control effect of Ortho-kCLs is better than that of MFSCLs. Additionally, the initial myopia of MFSCL was greater than that of the Ortho-kCL group, although the difference was not significant. This indicates that the initial rate of myopia progression was greater in the MFSCL group than in the Ortho-kCL group. However, the axial elongation was slower in MFSCL group compared with the Ortho-kCL group. Given the above reasons, the real myopia control effect of Ortho-kCL may not be as good as that of MFSCL.
In the present study, we speculate that MFSCLs are more effective in controlling myopia progression because the multifocal ring formed by the lens is stable, whereas the multifocal ring formed by Ortho-kCLs is unstable and irregular as a result of eye movements and sleep duration at night. Additionally, the MFSCLs are comfortable and easy to care for, and they are easy to wear during the day so that children will want to wear them every day. In the MFSCL group, 84.6% completed the 1-year study. In contrast, only 69.0% of the Ortho-kCL group completed it. Thus, the compliance of MFSCL wear by the myopic children in this study was high, which probably improves the opportunity for myopia control. Finally, another likely reason for the greater effectiveness of MFSCLs over Ortho-kCLs in controlling myopia is the power gradient. The power changes to +6.00 D in the treatment zone may provide more sustained myopically defocused images to the retina, even during near work, than the +2.00 D add power. Thus, we speculate that, in fact, the myopia control effect of this MFSCL is better than that of the Ortho-kCLs used in this study.
After 1 year, there was no difference in CECD among the three groups, which is consistent with the absence of reports concerning endothelial cell damage caused by the wearing of MFSCLs by children. Alterations in the morphology of corneal endothelial cells and reductions in CECD have been reported in adult wearers who wore hydrogel contact lenses for more than 5 years.39 Therefore, further investigation of possible changes in the CECD after long-term wearing of MFSCLs is necessary.
A potential limitation of this study is that there were slight differences in the baseline genders among the three groups. The effect of gender on the progression of myopia is inconclusive.34,40 A second potential limitation of the study is associated with our inability to measure the refraction of the Ortho-kCL group at the 6- and 12-month visits for reasons described above and discussed below. Therefore, we cannot say that, based on the changes in SER, the MFSCLs were more effective in controlling myopia than the Ortho-kCLs. However, the development of myopia is strongly associated with the AL elongation that occurs during juvenile and adolescent development. Clearly, the MFSCLs were more effective in controlling the AL elongation than were the Ortho-kCLs. Therefore, our inability to directly measure the SER changes in the Ortho-kCL group does not diminish our hypothesis that the MFSCLs were more effective than the Ortho-kCLs in controlling the development of myopia through reduction in the rate of axial elongation. A third limitation of our study is that our research cycle of 1 year is relatively short, and longer clinical studies should be performed. A fourth limitation is that our sample size was relatively small. Larger sample size studies are needed to compare the myopia control effect of MFSCLs with Ortho-kCLs in the future.
In conclusion, MFSCLs worn for 1 year by 7- to 15-year-old myopic Chinese children significantly slowed the progression of myopia by 37.0% and inhibited axial elongation by 26.8% compared with control subjects wearing SVSs. For the same period, Ortho-kCLs also significantly inhibited axial elongation by 24.4%. Therefore, MFSCL and Ortho-kCL wear are promising treatments in controlling myopia progression.
Supplementary Material
ACKNOWLEDGMENTS
The authors express their gratitude to Jianbing Wang, associate professor from the School of public health, Zhejiang University School of Medicine, for statistical consultation in this work. The authors also express their gratitude to Britt Bromberg, PhD, Xenofile Editing (https://xenofileediting.com/), for providing editing services for this manuscript.
Footnotes
The authors have no conflicts of interest to disclose.
This project is supported by the Science and Technology program of Jinhua Science and Technology Bureau (Grant No. 20203017).
Design of the study (C.D., Z.H.); Conduct of the study, data collection, analysis and interpretation (C.D., J.F., Z.H., M.Z., Y.L., Q.W., X.C.); Manuscript preparation and review (C.D., J.F., Z.H., W.X.).
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.eyeandcontactlensjournal.com).
Statement about conformity: The Institutional Review Board for Human Research of The First Affiliated and The Fourth Affiliated Hospital, Zhejiang University School of Medicine.
Contributor Information
Jianxia Fang, Email: 22018493@zju.edu.cn.
Zhu Huang, Email: flycatty@zju.edu.cn.
Yan Long, Email: 1507153@zju.edu.cn.
Miaomiao Zhu, Email: drzmm@zju.edu.cn.
Qin Wu, Email: 32085961@qq.com.
Xiaojun Chen, Email: xjchen_6@126.com.
Wei Xv, Email: xuwei_mm@163.com.
REFERENCES
- 1.Tay SA, Farzavandi S, Tan D. Interventions to reduce myopia progression in children. Strabismus 2017;25:23–32. [DOI] [PubMed] [Google Scholar]
- 2.Baird PN, Saw SM, Lanca C, et al. Myopia. Nat Rev Dis Primers 2020;6:99. [DOI] [PubMed] [Google Scholar]
- 3.Lin Z, Vasudevan B, Gao T, et al. Refractive change and incidence of myopia among rural Chinese children: The Handan Offspring Myopia Study. Br J Ophthalmol 2021;630:1–5. [DOI] [PubMed] [Google Scholar]
- 4.Wu PC, Huang HM, Yu HJ, et al. Epidemiology of myopia. Asia Pac J Ophthalmol 2016;5:386–393. [DOI] [PubMed] [Google Scholar]
- 5.Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology 2016;123:1036–1042. [DOI] [PubMed] [Google Scholar]
- 6.Ng DSC, Lai TYY, Cheung CMG, et al. Anti-vascular endothelial growth factor therapy for myopic choroidal neovascularization. Asia Pac J Ophthalmol 2017;6:554–560. [DOI] [PubMed] [Google Scholar]
- 7.Lakawicz JM, Bottega WJ, Fine HF, et al. On the mechanics of myopia and its influence on retinal detachment. Biomech Model Mechanobiol 2020;19:603–620. [DOI] [PubMed] [Google Scholar]
- 8.Perera SA, Aung T. Myopia and glaucoma. Myopia Anim Model Clin Trials 2010;51:150–165. [Google Scholar]
- 9.Brown NA, Hill AR. Cataract: The relation between myopia and cataract morphology. Br J Ophthalmol 1987;71:405–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ruiz-Medrano J, Montero JA, Flores-Moreno I, et al. Myopic maculopathy: current status and proposal for a new classification and grading system (ATN). Prog Retin Eye Res 2019;69;80–115. [DOI] [PubMed] [Google Scholar]
- 11.Walline JJ. Myopia control: A review. Eye Contact Lens 2016;42:3–8. [DOI] [PubMed] [Google Scholar]
- 12.Lam CS, Tang WC, Tse DY, et al. Defocus Incorporated Soft Contact (DISC) lens slows myopia progression in Hong Kong Chinese schoolchildren: A 2-year randomised clinical trial. Br J Ophthalmol 2014;98:40–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhu Q, Liu Y, Tighe S, et al. Retardation of myopia progression by multifocal soft contact lenses. Int J Med Sci 2019;16:198–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huang J, Wen D, Wang Q, et al. Efficacy comparison of 16 interventions for myopia control in children: A network meta-analysis. Ophthalmology 2016;123:697–708. [DOI] [PubMed] [Google Scholar]
- 15.Hutchinson K, Apel A. Infectious keratitis in orthokeratology. Clin Exp Ophthalmol 2002;30:49–51. [DOI] [PubMed] [Google Scholar]
- 16.Young AL, Leung AT, Cheung EY, et al. Orthokeratology lens-related Pseudomonas aeruginosa infectious keratitis. Cornea 2003;22:265–266. [DOI] [PubMed] [Google Scholar]
- 17.Chia A, Chua WH, Cheung YB, et al. Atropine for the treatment of childhood myopia: Safety and efficacy of 0.5%, 0.1%, and 0.01% doses (atropine for the treatment of myopia 2). Ophthalmology 2012;119:347–354. [DOI] [PubMed] [Google Scholar]
- 18.Jones LW, Hodes DT. Possible allergic reactions to cyclopentolate hydrochloride: Case reports with literature review of uses and adverse reactions. Ophthalmic Physiol Opt 1991;11:16–21. [PubMed] [Google Scholar]
- 19.Kwon S, Cotter S, Chu R. Safety and efficacy of 2% pirenzepine ophthalmic gel in children with myopia: Year two. Optom Vis Sci 2001;78:144. [Google Scholar]
- 20.Schaeffel F, Glasser A, Howland HC. Accommodation, refractive error and eye growth in chickens. Vis Res 1988;28:639–657. [DOI] [PubMed] [Google Scholar]
- 21.Wallman J, Wildsoet C, Xu A, et al. Moving the retina: Choroidal modulation of refractive state. Vis Res 1995;35:37–50. [DOI] [PubMed] [Google Scholar]
- 22.Read SA, Collins MJ, Sander BP. Human optical axial length and defocus. Invest Ophthalmol Vis Sci 2010;51:6262–6269. [DOI] [PubMed] [Google Scholar]
- 23.Sankaridurg P, Holden B, Smith E, et al. Decrease in rate of myopia progression with a contact lens designed to reduce relative peripheral hyperopia: One-year results. Invest Ophthalmol Vis Sci 2011;52:9362–9367. [DOI] [PubMed] [Google Scholar]
- 24.Cho P, Cheung SW. Retardation of myopia in orthokeratology (romio) study: A 2-year randomized clinical trial. Invest Ophthalmol Vis Sci 2012;53:7077–7085. [DOI] [PubMed] [Google Scholar]
- 25.Pauné J, Morales H, Armengol J, et al. Myopia control with a novel peripheral gradient soft lens and orthokeratology: A 2-year clinical trial. Biomed Res Int 2015;2015:507572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Marcotte-Collard R, Simard P, Michaud L. Analysis of two orthokeratology lens designs and comparison of their optical effects on the Cornea. Eye Contact Lens 2018;44:322–329. [DOI] [PubMed] [Google Scholar]
- 27.Yamaguchi T, Ohnuma K, Konomi K, et al. Peripheral optical quality and myopia progression in children. Graefes Arch Clin Exp Ophthalmol 2013;251:2451–2461. [DOI] [PubMed] [Google Scholar]
- 28.Schaeffel F, Feldkaemper M. Animal models in myopia research. Clin Exp Optom 2015;98:507–517. [DOI] [PubMed] [Google Scholar]
- 29.Wildsoet CF. Active emmetropization--evidence for its existence and ramifications for clinical practice. Ophthalmic Physiol Opt 1997;17:279–290. [PubMed] [Google Scholar]
- 30.Walline JJ, Greiner KL, McVey ME, et al. Multifocal contact lens myopia control. Optom Vis Sci 2013;90:1207–1214. [DOI] [PubMed] [Google Scholar]
- 31.Swarbrick HA, Alharbi A, Watt K, et al. Myopia control during orthokeratology lens wear in children using a novel study design. Ophthalmology 2015;122:620–630. [DOI] [PubMed] [Google Scholar]
- 32.Anstice NS, Phillips JR. Effect of dual-focus soft contact lens wear on axial myopia progression in children. Ophthalmology 2011;118:1152–1161. [DOI] [PubMed] [Google Scholar]
- 33.Hyman L, Gwiazda J, Hussein M, et al. Relationship of age, sex, and ethnicity with myopia progression and axial elongation in the correction of myopia evaluation trial. Arch Ophthalmol 2005;123:977–987. [DOI] [PubMed] [Google Scholar]
- 34.Guo Y, Liu LJ, Tang P, et al. Outdoor activity and myopia progression in 4-year follow-up of Chinese primary school children: The Beijing Children Eye Study. PLoS One 2017;12:e0175921–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wong CW, Tsai A, Jonas JB, et al. Digital screen time during the COVID-19 pandemic: Risk for a further myopia boom? Am J Ophthalmol 2021;223:333–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Alharbi A, Swarbrick HA. The effects of overnight orthokeratology lens wear on corneal thickness. Invest Ophthalmol Vis Sci 2003;44:2518–2523. [DOI] [PubMed] [Google Scholar]
- 37.Hou W, Norton TT, Hyman L, et al. Axial elongation in myopic children and its association with myopia progression in the correction of myopia evaluation trial. Eye Contact Lens 2018;44:248–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lau JK, Wan K, Cheung SW, et al. Weekly changes in axial length and choroidal thickness in children during and following orthokeratology treatment with different compression factors. Transl Vis Sci Technol 2019;8:9–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mohd-Ali B, Chen LY. The morphology of corneal endothelial cells in long term soft contact lens wearers in Kuala Lumpur. Contact Lens Anterior Eye 2021;44:72–75. [DOI] [PubMed] [Google Scholar]
- 40.Öner V, Bulut A, Oruç Y, et al. Influence of indoor and outdoor activities on progression of myopia during puberty. Int Ophthalmol 2016;36:121–125. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.