Abstract
Objective
This study reviewed the quantitative and qualitative evidence‐base for multi‐family therapy (MFT) for eating disorders regarding change in physical and psychological symptoms, broader individual and family factors, and the experience of treatment.
Method
A systematic scoping review was conducted. Four databases (PsycInfo, Medline, Embase, CENTRAL) and five grey literature databases were searched on 24th June 2021 for relevant peer‐reviewed journal articles, book chapters, and dissertations. No beginning time‐point was specified. Only papers that presented quantitative or qualitative data were included. No restrictions on age or diagnosis were imposed. Studies were first mapped by study design, participant age, and treatment setting, then narratively synthesized.
Results
Outcomes for 714 people who received MFT across 27 studies (one mixed‐method, 17 quantitative and nine qualitative) were synthesized. MFT is associated with improvements in eating disorder symptomatology and weight gain for those who are underweight. It is also associated with improvements in other individual and family factors including comorbidities, self‐esteem, quality of life, and some aspects of the experience of caregiving, although these findings are more mixed. MFT is generally experienced as both helpful and challenging due to the content addressed and intensive group process.
Discussion
MFT is associated with significant improvements in eating disorder symptoms across the lifespan and improvement in broader individual and family factors. The evidence base is small and studies are generally underpowered. Larger, higher‐quality studies are needed, as is research investigating the unique contribution of MFT on outcomes, given it is typically an adjunctive treatment.
Keywords: adolescent, adult, anorexia nervosa, bulimia nervosa, caregiver, child, eating disorders, family‐based treatment (FBT), Maudsley family therapy, multi‐family therapy (MFT), young adult
Resumen
Objetivo
Este estudio revisó la evidencia cuantitativa y cualitativa para la terapia multifamiliar (MFT, por sus siglas en inglés) para los trastornos de la conducta alimentaria con respecto al cambio en los síntomas físicos y psicológicos, los factores individuales y familiares más extensos, y la experiencia del tratamiento.
Método
Se realizó una revisión sistemática del alcance. Se realizaron búsquedas en cuatro bases de datos (PsycInfo, Medline, Embase, CENTRAL) y en cinco bases de datos de literatura gris el 24.06.2021 para obtener artículos relevantes de revistas revisadas por pares, capítulos de libros y disertaciones. No se especificó ningún punto de tiempo inicial. Sólo se incluyeron los artículos que presentaban datos cuantitativos o cualitativos. No se impusieron restricciones de edad o diagnóstico. Los estudios se mapearon primero por el diseño del estudio, la edad de los participantes y el entorno de tratamiento, y luego se sintetizaron narrativamente.
Resultados
Se sintetizaron los resultados de 714 pacientes que recibieron MFT en 27 estudios (un método mixto, 17 cuantitativos y nueve cualitativos). MFT se asocia con mejoras en la sintomatología del trastorno de la conducta alimentaria y el aumento de peso para aquellos que tienen bajo peso. También se asocia con mejoras en otros factores individuales y familiares, incluidas las comorbilidades, la autoestima, la calidad de vida y algunos aspectos de la experiencia del cuidador, aunque estos hallazgos son más mixtos. MFT generalmente se experimenta como útil y desafiante debido al contenido abordado y al proceso grupal intensivo.
Discusión
La MFT se asocia con mejoras significativas en los síntomas del trastorno de la conducta alimentaria a lo largo de la vida y una mejora en factores individuales y familiares más amplios. La base de evidencia es pequeña y los estudios generalmente tienen poco poder. Se necesitan estudios más grandes y de mayor calidad, al igual que la investigación que investiga la contribución única de la MFT en los resultados, dado que generalmente es un tratamiento complementario.
Palabras clave
terapia multifamiliar (MFT), terapia familiar de Maudsley, tratamiento basado en la familia (FBT), trastornos de la conducta alimentaria, anorexia nerviosa, bulimia nerviosa, niño, adolescente, adulto joven, adulto, cuidador
1. INTRODUCTION
Bringing families together to form multi‐family groups has been part of eating disorder treatment for decades (Gelin, Cook‐Darzens, & Hendrick, 2018). This emerged in the context of a longer tradition of multi‐family groups for people with schizophrenia (Laqueur, Laburt, & Morong, 1964; McFarlane, 2002), and more recent models for depression (Anderson et al., 1986; Lemmens, Eisler, Buysse, Heene, & Demyttenaere, 2009) and substance misuse (Kaufman & Kaufmann, 1977).
Early eating disorder multi‐family group work in the 1980s focused on young adults with anorexia nervosa (Slagerman & Yager, 1989) and bulimia nervosa (Wooley & Lewis, 1987). These early eating disorders focused multi‐family groups primarily targeted family relationships and improving patient support. In the 1990s, multi‐family group therapy (MFT) models began emerging for children and adolescents with eating disorders (Dare & Eisler, 2000; Scholz & Asen, 2001), which were theoretically rooted in the principles of eating disorder focused family therapy (Eisler, Simic, Blessitt, Dodge, & MCCAED Team, 2016).
This umbrella term, eating disorder‐focused family therapy, encompasses several, similar forms of evidence‐based family therapy for eating disorders, including Maudsley family therapy (Eisler et al., 2016) and family‐based treatment (Lock & Le Grange, 2012). While some differences exist, all eating disorder focused family therapies are phased, emphasize working with the family rather than treating the family, initially focus on symptom management with parents taking a central role supporting their child's eating, and broadens out to adolescent and family functioning once healthier food and eating practices are established and physical health has improved.
Different versions of MFT for anorexia nervosa and atypical anorexia nervosa (MFT‐AN) have now been manualized for children and adolescents (Simic, Baudinet, Blessitt, Wallis, & Eisler, 2021), as well as adults (Tantillo, McGraw, & Le Grange, 2020). Typically, MFT‐AN involves a group of up to eight families working together with at least two healthcare professionals. The group usually engages in a mixture of different types of activities, including small and large group discussions, nonverbal activities, and therapeutic games. This all occurs in various constellation, such as separate young person, sibling and parent groups, mixed groups, or pairs, etc. The group will usually also eat up to three meals together during each MFT day. MFT‐AN is now a recommended treatment for adolescents by several practice guidelines (Couturier et al., 2020; Heruc et al., 2020; NICE, 2017) and a specific version has recently been developed for adolescents with bulimia nervosa (MFT‐BN; Stewart et al., 2019).
Individual differences exist between MFT models (Gelin et al., 2018; Gelin, Cook‐Darzens, Simon, & Hendrick, 2016). Some offer three (Whitney et al., 2012) or five days (Knatz et al., 2015; Marzola et al., 2015; Wierenga et al., 2018) of MFT groups as a stand‐alone intervention. Others are much longer and offer 10 (Simic et al., 2021) or even 20 days or more (Gelin et al., 2016; Scholz, Rix, Scholz, Gantchev, & Thömke, 2005) of MFT groups spread across 12 months with reducing frequency. The number of families per group also varies, ranging from two (Whitney, Murphy, et al., 2012) to eight or nine (Simic et al., 2021). Similarly, MFT intensity is variable, with some meeting weekly/fortnightly for 1–2 hours (Gelin et al., 2016; Stewart et al., 2019) and others for several full consecutive days (Scholz et al., 2005).
All MFT models are designed to improve treatment outcomes by reducing perceived isolation and stigma, enhance family relationships and promote family skill building (Asen & Scholz, 2010; Dawson, Baudinet, Tay, & Wallis, 2018; Simic & Eisler, 2015). Some models also specifically aim to intensify treatment, particularly at the early stages (Simic & Eisler, 2015; Wierenga et al., 2018), which has been shown to be a critical time during treatment. Early eating disorder symptom change has been shown to be a robust predictor of end of treatment outcomes across diagnosis, age range, treatment type, and setting (Nazar et al., 2017; Vall & Wade, 2015); hence, the importance of a more intensive intervention, such as MFT, at this stage of treatment.
Given MFT can provide early, intensive support, that focuses on both patient and family factors, it has great potential to improve upon current treatment outcomes either as a stand‐alone or adjunctive intervention. Its use also fits with practice guidelines, which increasingly suggest involving family members in child, adolescent, and adult treatments (Fleming, Le Brocque, & Healy, 2020; Hilbert, Hoek, & Schmidt, 2017; National Institute for Health and Care Excellence (NICE), 2017; Treasure, Parker, Oyeleye, & Harrison, 2021).
Emerging evidence indicates that MFT is associated with improved physical health, a reduction in eating disorder symptoms and improvements in a range of other patient and family factors, such as self‐esteem, quality of life, and caregiver burden (Gelin et al., 2016). Results from the only outpatient randomized controlled trial (RCT) published indicate global outcomes at discharge from family therapy with adjunctive MFT are improved compared to family therapy alone for adolescents with anorexia nervosa (Eisler, Simic, Hodsoll, et al., 2016).
Yet, despite its promise, MFT remains relatively understudied. The heterogeneity of MFT models described and evaluated, as well as the relatively high resource cost and intensity required of some MFT models, makes it difficult to implement and evaluate. Furthermore, MFT is rarely a stand‐alone treatment and large variability exists between studies in the way MFT is delivered, including setting (inpatient, day program, outpatient), treatment duration, and treatment intensity (Gelin et al., 2018), making MFT‐specific findings difficult to generalize.
Given MFT is now widely used in clinical services internationally, a systematic scoping and synthesis of the available data is needed to determine the evidence base and identify gaps for future research. To better understand the impact of MFT on eating disorder treatment outcomes, this study aimed to systematically review and synthesize the available quantitative and qualitative findings. While a review has previously been completed of MFT for a range of psychiatric disorders (Gelin et al., 2018), including eating disorders, this was not exhaustive, missed some important papers (Jewell & Lemmens, 2018), and did not include qualitative data. Specifically, this review has three aims:
To review the impact of MFT on the physical and psychological symptoms of eating disorders.
To review the impact of MFT on families and caregivers.
To review the individual and family experience of receiving MFT.
2. METHOD
A systematic scoping review methodology (Peters et al., 2015) was used to explore the existing research into MFT for eating disorders across the age range. This was identified as the most appropriate methodology given the heterogeneity of existing research and the broad aims of this review. This allowed for more descriptive studies that included some outcome data to be included. Current scoping review guidelines (Peters et al., 2020) and Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) extension for scoping reviews guidance (Tricco et al., 2018) were used to conduct this review. The research was reviewed and approved by an institutional review board.
The methodology was initially developed by one author (JB) using the PICOS (population, intervention, comparison, outcome, study design) framework (Methley, Campbell, Chew‐Graham, McNally, & Cheraghi‐Sohi, 2014). Two authors (JB, LD) then independently executed the search strategy, study selection and data extraction. Disagreements were resolved by consensus discussions. Data were reviewed using a parallel‐results convergent synthesis design (Noyes et al., 2019), whereby quantitative and qualitative data were initially analyzed and presented separately; then, synthesized for interpretation of the findings. This was deemed the most appropriate method of initially scoping both the quantitative and qualitative data, as well as synthesizing all available data.
2.1. Eligibility criteria
Eligibility criteria for this review are presented in Table 1.
TABLE 1.
Systematic scoping review eligibility criteria
| Included | Excluded | |
|---|---|---|
| Publication type |
|
|
| Language |
|
|
| Study objectives |
|
|
| Methodology/design |
|
|
| Sample |
|
|
2.2. Search strategy
Four main databases (PsycInfo, Medline, Embase, CENTRAL) and five grey literature databases (Scopus, Web of Science, OpenGrey, ProQuest Dissertations and Theses Global, EThOS UK Theses) were searched using variations of the terms “eating disorder” and “multi‐family therapy” on 24th June 2021 (see Appendix S1 for exact search terms). References lists of identified articles were then reviewed as a final step for any additional, relevant papers that met the inclusion criteria.
2.3. Selection process
After completing the initial search, duplicates were deleted, and the remaining titles and abstracts were reviewed. Full‐text citations and reference lists for relevant articles were screened for eligibility before reaching consensus at the included papers in this synthesis (see Figure 1 for PRISMA flowchart). Zotero software was used in this process.
FIGURE 1.
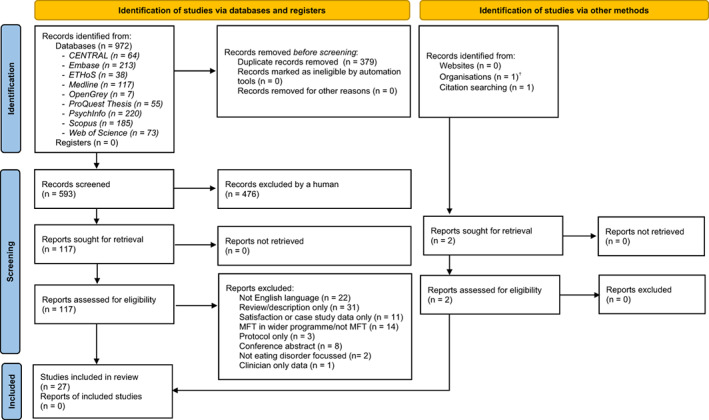
PRISMA flow diagram. †MSc dissertation identified by co‐author (IE) who supervised the work. From: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: 10.1136/bmj.n71. For more information, visit: http://www.prisma‐statement.org/
2.4. Data extraction, charting, and categorization
All included articles were grouped according to three main categories: type of data generated (quantitative or qualitative), participant age (young person [≤25 years] or adult [≥17 years]), and treatment setting (inpatient/day‐patient/residential or outpatient). Regarding the overlap in how young adults, aged 17–25 years, were categorized: if a program was predominantly child and adolescent focused but included young adults, it was categorized as “young person.” When the participant age range started at 17 years and extended beyond 25 years, this program was categorized as an adult program. No program was exclusively for young adults. Quantitative studies were further charted according to study design (RCT, non‐randomized comparison study, case series).
The data charting forms were developed by JB in consultation with LD to determine which variables to extract. For quantitative studies, data on change in eating disorder symptoms, physical health outcomes, comorbid individual and family factors, and general function data from baseline to discharge (and follow‐up if available) was extracted, as well as effect sizes. MFT program characteristics (intensity and duration) were also extracted. For qualitative data, themes, and sub‐themes were extracted. This was completed by both authors (JB and LD) via an iterative process in repeated consultation. Any missing data were explicitly reported, where applicable. This information was used to inform the narrative synthesis of eligible studies. In line with current scoping review guidance, risk of bias assessment was not completed (Munn et al., 2018; Peters et al., 2020).
3. RESULTS
3.1. Study selection and characteristics
Nine‐hundred‐and‐seventy‐two papers were initially identified through the systematic literature search. After duplicates were deleted and screening was performed according to the eligibility criteria (Table 1), a total of 27 articles were determined eligible for this review (see Figure 1 for PRISMA flowchart). The total sample reported on who received MFT is 714 (mean age = 18.7 years, range = 11–62, 97% female).
Outcomes from the 27 studies are synthesized below, comprising data generated from one mixed‐method, 17 quantitative, and nine qualitative studies. Three of the quantitative studies also included some qualitative feedback data; however, the data analysis methodology was not adequately reported on to reach the review inclusion criteria. As such, only the quantitative data from these studies are included in this review (Dimitropoulos, Farquhar, Freeman, Colton, & Olmsted, 2015; Mehl, Tomanová, Kuběna, & Papežová, 2013; Wierenga et al., 2018). The only included mixed‐method study was a doctoral dissertation (Salaminiou, 2005), of which most (but not all) of the outcome data were published in a peer‐review journal (Salaminiou, Campbell, Simic, Kuipers, & Eisler, 2017). Both the dissertation and article were identified by the search strategy and included in this review. Data reported in Salaminiou et al. (2017) are reported as such. All remaining quantitative and qualitative data are reported as Salaminiou (2005) henceforth.
Most studies were from Europe (n = 18, 67%) and had relatively small sample sizes. Nearly, a quarter of the quantitative studies had 30 participants or less (n = 6, 22%) and only two (7%) had a sample size greater than 100. Twenty‐three studies reported on MFT in an outpatient setting (17 young person, six adult) and four on a day‐ or inpatient setting (two young person, two adult). Seven studies compared MFT outcomes to another treatment (five young person, two adult). See Table 2 for a summary of included study characteristics. See Tables 3, 4 and 5 for a summary of the quantitative eating disorder outcomes, quantitative comorbid and family outcomes, and qualitative outcomes, respectively.
TABLE 2.
Methodologies of included studies
| Young person | Adult | ||||
|---|---|---|---|---|---|
| OP | I/DP | OP | I/DP | Total | |
| RCT | 1 | 1 | 0 | 1 | 3 |
| Non‐randomized comparison studies | 2 | 1 | 1 | 0 | 4 |
| Case series | 7 | 0 | 3 | 0 | 10 |
| Qualitative | 6 | 0 | 2 | 1 | 9 |
| Mixed‐method | 1 | 0 | 0 | 0 | 1 |
| Total | 17 | 2 | 6 | 2 | 27 |
Abbreviations: I/DP, inpatient or day‐patient; OP, outpatient; RCT, randomized controlled trial.
TABLE 3.
Summary of findings for changes in eating disorder symptoms and weight during MFT (n = 17)
| Author and place | Design | Mean age (SD, range) | Sample N (% female, race/ethnicity, SES) | Diagnosis | Setting | MFT model | #MFT sessions | Tx length | Baseline data (mean, SD) | End of treatment ED data (mean, SD) | ES | Dropout (n, %) and follow‐up data (time to FU, n, % of initial sample a ) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Young people—outpatient MFT | ||||||||||||
| RCTs | ||||||||||||
| Eisler, Simic, Hodsoll, et al. (2016) [UK] |
Multi‐Center RCT: FT‐AN (n = 82) vs. MFT + FT‐AN (n = 85) |
15.7 (1.7, 12–20) |
167 (F: 91%) (R/E: White 90%, other 4%, missing 6%) (SES: nr) |
AN (76%) EDNOS‐R (24%) |
Outpatient | Maudsley model (Simic et al., 2021) | 10 sessions | 12 months |
%mBMI: 77.6 (6.3) [MFT] 78.4 (5.8) [FT] |
%mBMI: 90.0 (9.1) [MFT] 87.8 (10.1) [FT] Time effect *** Treatment effect ns |
%mBMI: Time: nr Tx: z = .37 |
Dropout: 18 (11%) 9 (11%) [MFT] 9 (11%) [FT‐AN] FU: 6‐month [18 months post‐randomization] (n = 38–60, 22–34%) %mBMI: 90.6 (8.2) [MFT] 85.2 (10.2) [FT] Time effect *** a (ES nr) Treatment effect ** a (z = .68) EDE‐R: 1.4 (1.7) [MFT] 1.8 (1.4) [FT] Time effect *** a (ES nr) Treatment effect ns a (z = .26) Morgan Russel (good and intermediate) outcome: 78% [MFT] 57% [FT] Treatment effect ns |
|
EDE‐R: 2.7 (1.8) [MFT] 2.9 (1.7) [FT] |
EDE‐R: 1.8 (1.7) [MFT] 1.4 (1.5) [FT] Time effect *** Treatment effect ns |
EDE‐R: Time: nr Tx: z = .26 |
||||||||||
|
Morgan Russel outcome (good & intermediate): 8% [MFT] 10% [FT] |
Morgan Russel outcome (good and intermediate): 76% [MFT] 58% [FT] Treatment effect* |
|||||||||||
| Non‐randomized comparison studies | ||||||||||||
| Gabel et al. (2014) [Canada] |
Retrospective chart review comparison: TAU (n = 25) vs. TAU + MFT (n = 25) |
14.1 (2.0, 11–18) |
50 (F: 100%) (R/E: nr) (SES: nr) |
AN (100%) |
Specialist ED service (outpatient, day patient and inpatient) |
Maudsley model | nr | 12 months |
%IBW: 77.7 (nr) [MFT] 79.1 (nr) [TAU] |
%IBW: 99.6 (7.3) [MFT] 95.4 (6.8) [TAU] Time effect sig nr Treatment effect* |
nr |
Dropout: nr No FU |
|
EDE‐Q: 3.1 (1.8) [MFT] nr [TAU] |
EDE‐Q: 2.1 (1.4) [MFT]* nr [TAU] Time effect nr Treatment effect nr |
|||||||||||
| Marzola et al. (2015) [USA] |
30‐month follow up: Intensive FT (n = 20) vs. MFT (n = 54) |
14.7 (2.8, nr) |
74 (F: 92%) (R/E: Cauc. 92%, other nr) (SES: nr) |
AN (60%) EDNOS (40%) |
Outpatient | “Intensified FT‐AN” | 5 days [40 h] | 1 week |
%EBW: 86.4 (8.7) [total sample] ED measure: nr |
nr [follow‐up data only] | nr |
Tx dropout nr [loss to FU: 18 (20%) of eligible participants] FU: 30.9 (20.2, 4–83) month (n = 55–74, 60–80%) %EBW: 97.8 (10.1) [MFT] 102.2 (17.5) [I‐FT] Time effect*** a (d = 1.18) Treatment effect ns ED measure: nr |
| Case series | ||||||||||||
| Dennhag, Henje, & Nilsson, 2019 [Sweden] | Case series |
13.9 (1.1, 13–16) |
24 (F: 100%) (R/E: Cauc. 100%) (SES: 78.5% parents with uni. Degree/100% fathers and 60% mothers employed full‐time) |
AN (37.5%) EDNOS (62.5%) |
Outpatient (n = 7 commenced MFT while inpatient) | As per Wallin (2007) manual | 10.5 days | 1 year |
BMI: 17.9 (2.0) %EBW: 93.0 (3.7) EDE‐Q (G): 2.9 (1.6) |
BMI: 20.1 (2.2)*** %EBW: 101.3 (10.0)** EDE‐Q (G): 2.0 (1.9)* [Full remission: 10 (42%) c , No ED dx: 13 (54%)] |
d = 1.16 d = .72 d = .56 |
Dropout: nr No FU |
| Gelin, Fuso, Hendrick, Cook‐Darzens, and Simon (2015) [Belgium] | Case series |
16.0 (1.5, 11–19) |
82 (F: 98%) (R/E: nr) (SES: nr) |
AN‐R (84%) AN‐BP (11%) BN (5%) |
Outpatient | Influenced by Maudsley and Dresden models | 21 days | 11 months |
%EBW: 77.0 (9.8) EDI‐DT: 12.5 d (IQR: 5–18) |
%EBW: 86.8 (11.2)** EDI‐DT: 4.0 d (IQR: 1–11)** |
d = .93 r = .60 |
Dropout: 7 (9%) FU: 1‐year (n = 42, 51%) %EBW: “Continues to increase significantly” EDI: “Stabilize after treatment” [data not reported] |
| Hollesen, Clausen, and Rokkedal (2013) [Denmark] | Case series |
14.9 (1.1, 12–17) |
20 (F: 100%) (R/E: nr) (SES: nr) |
AN (40%) EDNOS‐R (60%) |
Outpatient | Influenced by Maudsley & Dresden models | 12 days | 1 year (range = 8.4–11.8 months) |
BMI: 16.2 (1.4) EDE‐R: 3.2 (1.2) EDI‐DT: 12.5 (5.7) |
BMI: 18.4 (1.4)** EDE‐R: 1.8 (1.6)** EDI‐DT: 6.1 (5.7)** [No ED dx: 13 (65%)] |
d = .63 d = 1.0 d = 1.13 |
Dropout: 1 (3%) No FU |
| Knatz et al. (2015) [USA] | Case series |
14.6 (2.9, nr) |
40 (F: nr) (R/E: Cauc. 90%, other nr) (SES: nr) |
nr | Outpatient | Influenced by Maudsley and Dresden models | 5 days [40 h] | 1 week |
BMI: 17.6 (2.1) ED measure nr |
BMI: 20.7 (2.1)** ED measure nr |
nr |
Dropout: nr No FU |
| Mehl et al. (2013) [Czech Republic] | Case series |
17.7 (2.5, 14–23) |
15 (F: nr) (R/E: nr) (SES: nr) |
nr | Outpatient | Maudsley model | 8 | 12 months |
BMI: 16.9 (1.5) ED measure nr |
BMI* (mean and SD nr) ED measure nr |
nr |
Dropout: 2 (13%) No FU |
| Salaminiou et al. (2017) [UK] | Case series |
15.4 (1.8, 11–18) |
30 (F: 90%) (R/E: nr) (SES: 50% UK class I/II, 50% class III/IV) e |
AN (90%) EDNOS‐R (10%) |
Outpatient | Maudsley model | 9–11 days | 9 months |
%mBMI: 75.8 (6.5) EDI‐2‐DT: 14.1 (7.1) |
%mBMI: 86.1 (8.7)*** EDI‐2‐DT: 9.6 (7.9)** |
d = 1.4 d = .6 |
Dropout: 2 (7%) No FU |
| Stewart et al., 2019 [UK] (study 1 data presented) | Case series |
15.6 (1.4, nr) |
50 (F: 98%) (R/E: nr) (SES: nr) |
BN (100%) | Outpatient | Maudsley model | 14 × 2 h Sessions | 4 months |
EDE‐Q (SC): 5.3 (1.0) Binge/wk: 7 b (range = 0–195) Purge/wk: 10 b (range = 0–195) Weight nr |
EDE‐Q (SC): 4.81*** Binge/wk: 5 d (range = 0–100)** Purge/wk: 3 d (range = 0–120)* Weight nr |
r = −.47 r = −.35
r = −.29 |
Dropout study 1: nr Dropout study 2: 2 (4%) [MFT] 18 (21%) [TAU‐no MFT] No FU |
| Young people—Inpatient MFT | ||||||||||||
| RCTs | ||||||||||||
| Geist, Heinmaa, Stephens, Davis, and Katzman (2000) [Canada] |
Single‐Center RCT: FT (n = 12) vs. Family group psychoed. (MFT, n = 13) |
14.3 (1.5, 12–17.3) |
25 (F: 100%) (R/E: nr) (SES: nr) |
AN‐R (76%) EDNOS‐R (24%) |
Inpatient [NB: All transitioned to outpatient setting during MFT] |
Psychoeducation groups | 8 × 90 m fortnightly sessions | 4 months |
%IBW: 77.2 (11.1) [MFT] 74.9 (9.2) [FT]
EDI‐2‐DT: 13.7 (6.2) 11.1 (5.8) [FT] |
%IBW: 96.3 (8.2) [MFT] 91.3 (7.3) [FT] Time effect *** Treatment effect ns EDI‐2‐DT: 13.3 (7.6) [MFT] 12.3 (7.5) [FT] Time effect ns Treatment effect ns |
“small to medium” |
Dropout: nr No FU [59% had concerns about being randomized to new treatment] |
| Non‐randomized comparison studies | ||||||||||||
| Depestele et al. (2017) [Belgium] |
Uncontrolled comparison: MFT (n = 62) vs. Parent group (n = 50) |
17.1 (2.2, 14–21) |
112 (F: 100%) (R/E: nr) (SES: nr) |
AN‐R (41%) AN‐BP (23%) BN (21%) EDNOS (14%) NSSI (62%) BP (53%) Non‐BP (46%) |
Inpatient |
Maudsley model (Eisler, 2005) NB: No siblings |
7 (2–3 h sessions) | 10 weeks +1 x 6‐month follow‐up session |
Weight: nr EDI‐DT: 35.4 (nr) [MFT] 34.0 (nr) [PG] |
Weight: nr EDI‐DT: 29.7 (nr) [MFT] 28.1 (nr) [PG] Time effect*** Treatment effect ns |
nr |
Dropout: 13 (12%) 7 (11%) families [MFT] 6 (12%) families [PG] FU: 1 MFT session at 6‐month described (no data reported) |
| Adult—outpatient MFT | ||||||||||||
| Case series | ||||||||||||
| Skarbø and Balmbra (2020) [Norway] | Case series |
21.3 (3.5, 17–30) |
68 (F: 100%) (R/E: nr) (SES: nr) |
AN (76.5%) BN (23.5%) |
Outpatient | Adapted from Maudsley and Toronto models | 13 days | 12 months |
BMI: 17.8 (2.1) [total sample] 16.6 (1.5) [underweight group only] |
BMI: 18.0 (2.0) [total sample] ns 17.4 (1.9)** [underweight group only] |
d = .1
d = .48 |
Dropout: 5 (7.4%) No FU |
| Tantillo, McGraw, Lavigne, Brasch, and Le Grange (2019) [USA] | Case series |
23 (3.6, 20–31) |
10 (F: 100%) (R/E: Cauc. 100%) (SES: nr) |
AN (40%) OSFED‐R (60%) |
Outpatient | Manualized R4R MFT Group (Tantillo et al., 2020) | 16 sessions | 26 weeks |
BMI: 20.7 (3.3) EDE (global): 2.8 (1.2) |
BMI: 21.2 (3.3) ns EDE (global): 1.8 (0.7)** |
d = .16 d = .75 |
Dropout: 0 (0%) FU: 6‐month (n, % nr) BMI: 21.5 (3.90) ns (d = .22) a EDE (global): 1.3 (0.6)** (d = 1.41) a |
| Wierenga et al. (2018) [USA] | Case series |
24.5 (8.8, nr) |
54 (F: 100%) (R/E: Cauc. 85%, other nr) (SES: nr) |
AN‐R (52%) AN‐BP (24%) EDNOS‐R (24%) |
Outpatient | Neurobiologically informed intensive FT‐AN | 5 days [40 h] | 5 days |
BMI: 18.1 (2.1) EDE‐Q (global): 3.5 (1.3) |
BMI: 18.3 (2.0)* EDE‐Q (global): 3.1 (1.5)* |
d = .10 d = .27 |
Dropout: 1 (2%) FU: >3‐month [EDE data mean = 142.2 (81.5) days / BMI data mean = 228.0 (177.7) days] (n = 28–39, 52–72%) BMI: 19.6 (2.0)*** (ƞ2 = .41) a EDE‐Q (global): 3.0 (1.5)** (ƞ2 = .24) a |
| Adult—Inpatient MFT | ||||||||||||
| RCTs | ||||||||||||
| Whitney, Murphy, et al. (2012) [UK] |
Single‐Center RCT: FT (n = 25) vs. 3‐day MFT (n = 23) |
43.5 [MFT] (14.8, nr) 47.9 [FT] (14.1, nr) |
48 (F: 98%) (R/E: nr) (SES: 2% post‐grad degree / 11% employed FT or PT) |
AN (100%) | Inpatient | Family day workshops (Treasure, Whitaker, Todd, & Whitney, 2011) |
3‐days [FT: 18 h (1–2 h per sessions)] |
3 days [FT: Weekly‐fortnightly] |
BMI: 13.2 (1.5) [MFT] 13.3 (1.6) [FT]
SEED‐AN: 2.6 (0.4) [MFT] 2.5 (0.5) [FT] |
BMI: 18.4 (1.8) [MFT] 17.6 (1.9) [FT] Time effect ns Treatment effect ns Interaction effect* SEED‐AN: 1.8 (0.9) [MFT] 2.0 (1.1) [FT] Time effect ns Treatment effect ns |
BMI: Time: nr Tx: z = .5
SEED‐AN: Time: nr Tx: z = .4 |
Dropout: 6 (12.5%) 3 (13%) [MFT] 3 (12%) [FT] NB: One MFT dropout moved to FT group FU: 3‐year (n = 29–44, 60–92%) BMI: 15.8 (2.6) [MFT] 16.8 (2.2) [FT] Time effect ns Treatment effect ns SEED‐AN: 1.9 (0.9) [MFT] 1.7 (0.7) [FT] Time effect sig nr Treatment effect sig nr |
| Non‐randomized comparison studies | ||||||||||||
| Dimitropoulos et al. (2015) [Canada] |
Uncontrolled comparison: FT (n = 17) vs. MFT (n = 28) |
26.2 (7.4, 18–57) |
45 (F: 100%) (R/E: nr) (SES: nr) |
AN‐R (44%) AN‐BP (56%) |
Inpatient (73%) & day program (27%) | Based in Cognitive‐Interpersonal Maintenance Model of AN (Schmidt and Treasure, 2006) c | 8 × 90 m, sessions | 8 weeks |
BMI: 15.7 (1.6) [total sample]
EDE‐Q (global): 4.1 (1.4) [total sample] |
BMI: 20.3 (1.4) [total sample] Time effect** Treatment effect ns EDE‐Q (global): 2.5 (1.2) [total sample] Time effect** Treatment effect ns |
BMI: Time: ƞ 2 = .88 Tx: nr EDE‐Q: Time: ƞ 2 = .74 Tx: nr |
Dropout: 8 (18%) 5 (17%) [MFT] 3 (18%) [FT] FU: 3‐month (weight and ED data nr, only family FU data) |
Abbreviations: ACT, acceptance and commitment therapy; AN, anorexia nervosa; AN‐rd, anorexia nervosa and related disorders; ARFID, avoidant/restrictive food intake disorder; Ax, assessment; BED, binge eating disorder; BMI, body mass index; BN, bulimia nervosa; BN‐rd, bulimia nervosa and related disorders; CBT, cognitive behavioral therapy; CRT, cognitive remediation therapy; DBT, dialectical behavior therapy; DP, day program; ED, eating disorder; ED‐Rs, restrictive eating disorders; EDNOS, eating disorder not otherwise specified; EDNOS‐R, eating disorder not otherwise specified characterised by restriction; EOT, end of treatment; FBT, family‐based treatment; FT‐AN, family therapy for anorexia nervosa; FU, follow up; IBW, ideal body weight; IOP, intensive outpatient program; IP, inpatient; MDT, multi‐disciplinary team; MI, motivational interviewing; OSFED, other specified feeding and eating disorder; OSFED‐R, other specified feeding and eating disorder characterized by restriction; PG, parent group; PHP, partial‐hospitalization program; PMM, predictors, moderators or mediators; RO DBT, radically open dialectical behavior therapy; SES, socioeconomic status; UFED, unspecified feeding and eating disorder.
Significant testing compares baseline to follow‐up period.
Median reported instead of mean. Full remission was defined as normal weight (≥95% of expected for sex, age, and height), Eating Disorder Examination Questionnaire (EDE‐Q) global score within 1 SD of norms, and absence of binge–purging behaviors. Partial remission was defined as weight ≥85% of expected or ≥95% but with elevated EDE‐Q global score and presence of binge–purging symptoms (<1/week).
Definition of full remission: at least 95%EBW and EDE global score within 1 SD of community norms (Lock, 2018).
Median reported instead of mean.
As per Classifications of Occupations 1980, Office of Population Censuses and Surveys, Her Majesty's Stationary Office, London.
*p < .05; **p < .01; ***p < .001.
TABLE 4.
Summary of the patient, caregiver, and family psycho‐social functioning factors assessed in quantitative studies
| Patient factors | Caregiver factors | Family factors | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Measure: baseline mean (SD) | EOT mean (SD) | Effect size | Measure: Baseline mean (SD) | EOT mean (SD) | Effect size | Measure: Baseline mean (SD) | EOT mean (SD) | Effect size | |
| Young person—outpatient MFT | |||||||||
| RCT | |||||||||
| Eisler, Simic, Hodsoll, et al. (2016) [UK] |
BDI: |
BDI: | ECI (negative): 85.6 (nr) | −15.81 a [MFT‐AN]** | z = −.52 | Nil | Nil | Nil | |
| 23.9 (14.3) [MFT] | −5.9 a (nr) [MFT‐AN]*** | z = .41 | −13.59 a [FT‐AN]** | z = −.45 | |||||
| 25.2 (14.4) [FT‐AN] | −8.8 a (nr) [FT‐AN]*** | z = −.62 | ECI (positive): 28.3 (nr) | 1.13 a [MFT‐AN] ns | z = .13 | ||||
| RSES: | RSES: | .42 a [FT‐AN] ns | z = .05 | ||||||
| 25.1 (6.6) [MFT] | −1.6 a (nr) [MFT‐AN] ns | z = −.24 | |||||||
| 26.3 (6.9) [FT‐AN] | −.5 a (nr) [FT‐AN] ns | z = −.08 | |||||||
| Non‐randomized comparison studies | |||||||||
| Gabel et al. (2014) [Canada] | CDI total: 64.8 (15.2) [MFT] | 52.9 (18.2) [MFT]* | nr | Nil | Nil | Nil | Nil | Nil | Nil |
| Marzola et al. (2015) [USA] | Nil | Nil | Nil | Nil | Nil | Nil | Nil | Nil | Nil |
| Case series | |||||||||
| Dennhag et al., 2019 [Sweden] | CGAS: 48.1 (7.3) | 61.7 (11.5)*** | d = .96 |
EDSIS total (m): 39.9 (12.0) EDSIS total (f): 34.1 (11.9) |
26.9 (15.9)***
23.9 (11.2)*** |
d = .92
d = .63 |
Nil | Nil | Nil |
| Gelin et al. (2015) [Belgium] | OQ‐45 total: 77.8 (27.3) | 46.4 (32.6)*** | r = .47 | Nil | Nil | Nil | Nil | Nil | Nil |
| Hollesen et al. (2013) [Denmark] |
IIP: means, SD nr SASB‐Intrex: means, SD nr |
“Less domineering” ns “Less vindictive”* “Less self‐blaming” ns “More controlling to mo.” ns “More submissive to mo.” ns “More emancipating to fa.” ns “Fa. more ignorant and distant” ns |
d = .41 d = .52 d = .52 d = .42 d = .51 d = .35 d = .27 |
Nil | Nil | Nil | Nil | Nil | Nil |
| Knatz et al. (2015) [USA] | Nil | Nil | Nil | Nil | Nil | Nil | Nil | Nil | Nil |
| Mehl et al. (2013) [Czech Republic] |
RSES b : 25.73 (4.20) SOS‐10 b : 25.73 (9.05) |
23.07 (3.75)** 35.13 (9.57)** |
nr η2 = .48 |
Nil | Nil | Nil | Nil | Nil | Nil |
| Salaminiou et al. (2017) [UK] |
BDI‐II: 27.8 (12.1) RSES: 18.4 (6.9) |
17.2 (14.6)** 24.5 (8.3)** |
d = .8 d = .8 |
BDI‐II (m): 13.9 (6.1) BDI‐II (f): 8.0 (5.6) |
9.7 (7.8)* 5.8 (5.6) ns |
d = .7 d = .4 |
Nil | Nil | Nil |
| Salaminiou (2005) [UK] | As above | As above | As above |
SCFI (mother to child) c ‐crit. comms. (m): 1.5 (1.9) ‐pos. rem. (m): .9 (1.1) EOI (m): 1.9 (1.3) ‐warmth (m): 2.0 (1.1) ‐hostility (m): .6 (1.1) SCFI (father to child) c ‐crit. comms. (f): 1.1 (1.5) ‐pos. rem. (f): .64 (.9) ‐EOI (f): 1.2 (1.0) ‐warmth (f): 2.0 (1.1) ‐hostility (f): .4 (.9) |
SCFI (mother to child) c ‐crit. comms. (m): .8 (1.4) ns ‐pos. rem. (m): 1.4 (1.5) ns ‐EOI (m): 1.6 (1.2) ns ‐warmth (m): 2.4 (1.2) ns ‐hostility (m): .2 (.8) ns SCFI (father to child) c ‐crit. Comms. (f): .6 (1.1)* ‐pos. rem. (f): 1.1 (1.1) ns ‐EOI (f): 1.1 (1.1) ns ‐warmth (f): 2.3 (1.3) ns ‐hostility (f): .2 (.7) ns |
nr |
SFI (px): 46.0 (12.9) SFI (m): 41.6 (9.9) SFI (f): 39.8 (10.1) |
47.6 (11.1) ns 43.6 (9.3) ns 40.4 (10.6) ns |
nr |
| Stewart et al., 2019 [UK] (study 1 data presented) |
RCADS (dep.): 73.5 (9.7) RCADS (anx.): 67.3 (11.0) DERS total: 139.5 (13.0) |
64.58 (13.23)* 60.26 (13.64)* 110.12 (29.51)** |
d = −.78 d = −.64 d = −.64 |
HADS (dep.): 6.2 (4.0) HADS (anx.): 9.4 (3.5) ECI‐neg.: 84.8 (25.1) |
4.68 (3.4)* 7.94 (4.4) ns 74.00 (30.9)* |
d = −.33 d = −.31 d = −.46 |
Nil | Nil | Nil |
| Young person— inpatient MFT | |||||||||
| RCTs | |||||||||
| Geist et al. (2000) [Canada] |
CDI: 14.0 (4.7) [MFT] 11.8 (6.6) [FT] BSI (px): 1.4 (.9) [MFT] 1.3 (.6) [FT] BSI (m): .6 (.5) [MFT] .7 (.8) [FT] BSI (f): .4 (.3) [MFT] .7 (.7) [FT] |
CDI: ns 15.4 (4.9) [MFT] ns 12.2 (7.4) [FT] BSI (px): ns 1.2 (.6) [MFT] 1.2 (.7) [FT] BSI (m): ns .6 (.5) [MFT] .6 (.5) [FT] BSI (f): ns .3 (.2) [MFT] .4 (.4) [FT] |
“small to medium” | Nil | Nil | Nil |
FAM‐III (px): 50.9 (10.8) [MFT] 48.3 (7.3) [FT] |
FAM‐III (px)* 55.8 (7.7) [MFT] 52.2 (8.5) [FT] (NB: Perceived family functioning worsened) |
“small to medium” |
| Non‐randomized comparison studies | |||||||||
| Depestele et al. (2017) [Belgium] |
SIQ‐TR: nr EDES: nr NSSI: 62% lifetime prevalence |
n/a | n/a |
ECI‐neg. (m): 93.9 (3.7) [MFT] 90.6 (4.2) [PG] ECI‐neg. (f): 72.7 (3.7) [MFT] 76.3 (4.6) [PG] ECI‐pos. (m): 29.7 (1.1) [MFT] 29.3 (1.2) [PG] ECI‐neg. (f): 24.2 (1.2) [MFT] 25.4 (1.5) [PG] |
ECI‐neg. (m):*** 79.1 (4.0) [MFT] 72.5 (4.7) [PG] ECI‐neg. (f):*** 60.6 (4.5) [MFT] 63.0 (5.3) [PG] ECI‐pos. (m): ns 28.7 (1.1) [MFT] 28.4 (1.3) [PG] ECI‐neg. (f): Ns 22.0 (1.3) [MFT] 26.9 (1.5) [PG] |
nr |
FAD‐GF (px): 2.1 (.1) [MFT] 2.1 (.1) [PG] FAD‐GF (m): 2.0 (.1) [MFT] 1.9 (.1) [PG] FAD‐GF (f): 2.0 (.1) [MFT] 2.0 (.1) [PG] |
FAD‐GF (px): ns 2.1 (.1) [MFT] 2.0 (.1) [PG] FAD‐GF (m): ns 1.9 (.1) [MFT] 2.1 (.1)[PG] FAD‐GF (f):* 1.9 (.1) [MFT] 1.8 (.1) [PG] |
nr |
| Adult—Outpatient MFT | |||||||||
| Case series | |||||||||
| Skarbø and Balmbra (2020) [Norway] | Nil | Nil | Nil | Nil | Nil | Nil | Nil | Nil | Nil |
| Tantillo et al. (2019) [USA] |
DERS‐LEA: 15.3 (5.2) DERS‐LAERS: 18.8 (6.9) |
12.9 (3.7)* 16.8 (2.3) ns |
d = .49 d = .32 |
Nil | Nil | Nil | Nil | Nil | Nil |
| Wierenga et al. (2018) [USA] |
STAI‐state: 56.2 (12.8) STAI‐trait: 55.3 (10.3) |
47.8 (12.3)*** 53.4 (10.0) ns |
d = .68 d = .19 |
Nil | Nil | Nil | FAD‐GF: 2.2 (.59) | 2.0 (.53)** | d = .36 |
| Adult—Inpatient MFT | |||||||||
| RCTs | |||||||||
| Whitney, Murphy, et al. (2012) [UK] d |
IIP: 122.5 (39.5) [MFT] 109.8 (30.9) [FT] |
IIP: ns 117.3 (47.8) [MFT] 110.9 (36.5) [FT] |
nr |
GHQ: 15.4 (5.9) [MFT] 16.6 (6.1) [FT] ECI‐neg.: 89.6 (30.9) [MFT] 74.7 (32.1) [FT] ECI‐pos.: 29.2 (9.6) [MFT] 25.4 (9.2) [FT] LEE: 72.2 (7.5) [MFT] 75.6 (9.9) [FT] |
GHQ:* 14.7 (7.4) [MFT] 15.2 (4.2) [FT] ECI‐neg.: ns 79.6 (38.1) [MFT] 65.5 (24.4) [FT] ECI‐pos.: ns 30.1 (8.0) [MFT] 25.4 (9.7) [FT] LEE:** 71.8 (8.0) [MFT] 72.9 (8.7) [FT] |
nr | Nil | Nil | Nil |
| Non‐randomized comparison studies | |||||||||
| Dimitropoulos et al. (2015) [Canada] |
DCCFS: 15.93 (3.14) [MFT] 14.94 (3.30) [FT] |
DCCFS: Ns 15.64 (3.02) [MFT] 15.46 (2.89) [FT] |
η 2 = .02 |
EDSIS total: 35.1 (15.1) [MFT] 35.1 (11.6) [FT] FQ‐crit.: 19.9 (4.7) [MFT] 16.8 (6.2) [FT] FQ‐EOI: 26.2 (4.4) [MFT] 27.1 (4.3) [FT] SPS total: 76.5 (9.4) [MFT] 78.2 (7.1) [FT] DCCFS: 14.3 (3.9) [MFT] 13.4 (2.6) [FT] BDI: 12.6 (9.8) [MFT] 10.5 (7.5) [FT] |
EDSIS total:** 22.3 (14.7) [MFT] 18.2 (10.1) [FT] FQ‐crit.:** 16.5 (4.7) [MFT] 15.1 (4.3) [FT] FQ‐EOI:** 24.0 (5.2) [MFT] 24.2 (4.4) [FT] SPS total: ns 78.4 (8.8) [MFT] 77.4 (6.3) [FT] DCCFS: Ns 14.8 (2.6) [MFT] 13.4 (2.7) [FT] BDI:** 8. (9.9) [MFT] 7.5 (7.5) [FT] |
η2 = .52
η 2 = .29
η2 = .45
η 2 = .02
η2 = <.01
η 2 = .25 |
Nil | Nil | Nil |
Note: When data for two treatment groups are reported (e.g., MFT and FT) significance values reported are for time effect, not treatment or interaction effect.
- BDI: Beck Depression Inventory (depression symptoms) (Beck, Steer, & Brown, 1996);
- BSI: Brief Symptom Inventory (psychological symptoms of psychiatric and medical patients) (Derogatis, 1992);
- CDI: Children's Depression Inventory (depression symptoms) (Kovacs, 1992);
- DCCFS: Devaluation of consumers and consumer families scales (perceived discrimination and stigma) (Struening et al., 2001);
- DERS: Difficulties in Emotion Regulation Scale (emotion regulation) (Gratz & Roemer, 2004);
- DERS‐LEA: Lack of Emotional Awareness subscale (ability to attend to and acknowledge emotions) (Gratz & Roemer, 2004);
- DERS‐LAERS: Limited Access to Emotion Regulation Strategies subscale (belief that one can access effective emotion regulation strategies) (Gratz & Roemer, 2004);
- EDSIS: The Eating Disorders Symptom Impact Scale (impact of caring for person with eating disorder) (Sepulveda, Whitney, Hankins, & Treasure, 2008);
- ECI: Experience of Caregiving Inventory (negative and positive aspects of caregiving) (Szmukler et al., 1996);
- FAD: Family Assessment Device‐general family functioning subscale (general family functioning) (Epstein et al., 1983);
- FQ: Family Questionnaire (expressed emotion‐criticism and emotional overinvolvement) (Wiedemann, Rayki, Feinstein, & Hahlweg, 2002);
- GHQ: General health Questionnaire (psychological morbidity and distress) (Goldberg & Williams, 1998);
- IIP: Inventory of Interpersonal Problems (self‐image and perception of interpersonal relations) (Horowitz, Rosenberg, Baer, Ureño, & Villaseñor, 1988);
- LEE: Level of Expressed Emotion (perceived expressed emotion of caregiver towards person with eating disorder) (Kazarian, Malla, Baker, & Cole, 1990);
- OQ‐45: Outcome questionnaire (quality of life) (Lambert et al., 1996);
- RCADS: Revised Child Anxiety and Depression Scale (depression and anxiety symptoms) (Chorpita, Yim, Moffitt, Umemoto, & Francis, 2000);
- RSES: Rosenberg self‐esteem scale (self‐esteem) (Rosenberg, 1965);
- SASB‐Intrex: Structural analysis of social behavior‐intrex (perceived interpersonal difficulties, incl. With parents) (Benjamin, 1974:197);
- SFI: self‐report family inventory‐health and competence scale (family functioning) (Beavers, Hampson, & Hulgus, 1985);
- SIQ‐TR: Self‐Injury Questionnaire‐Treatment Related (self‐harm) (Claes & Vandereycken, 2007);
- SOS‐10: Schwartz Outcome Scale, Czech version (quality of life) (Dragomirecka, Lenderking, Motlova, Goppoldova, & Šelepova, 2006);
- SPS: Social Provisions Scale (social support) (Cutrona & Russell, 1987);
- STAI: Spielberger State–Trait Anxiety Inventory (anxiety symptoms) (Spielberger, Gorsuch, & Lushene, 1970).
Abbreviations: EOT, end of treatment; f, father; FT, family therapy; m, mother; MFT, multi‐family therapy; nr, not reported; NSSI, nonsuicidal self‐injury; PG, parent group; px, patient.
Mean difference from baseline to EOT (12‐months) presented as means unavailable.
Measure translated into Czech.
Expressed emotion scores are from parent towards child.
Short‐term (3‐month) outcomes.
*p < .05; **p < .01; ***p < .001.
TABLE 5.
Summary of qualitative findings (n = 10)
| Author | Design | Mean age | Sample N (% female a , race/ethnicity a , SES) | Diagnosis | Setting | MFT model | #MFT days | Mean length (months) | Analysis methodology/notes | Themes and findings |
|---|---|---|---|---|---|---|---|---|---|---|
| Young person MFT | ||||||||||
| Baumas et al. (2021) [France] | YP and parent focus groups of MFT experience and change mechanisms | Px: 16.3 (2.5, 14–19) |
9 [from 4 families] ‐3 Px ‐4 mothers ‐2 fathers (F: 67%) (R/E: nr) (SES: nr) |
AN (100%) | Inpatient and Outpatient |
Blend of Cook‐Darzens (2007) and “Maudsley model” |
10 x 3 h sessions | 1 year | Thematic analysis |
Main themes (both groups)
Adolescent and parent group specific themes
Parent only group‐specific themes
|
| Duarte (2012) [UK] | Individual interviews and focus groups of YP and parent's experience of MFT for BN | Px: 15.8 (nr, 14–17) |
15 [from 9 families] ‐6 Px ‐8 parents ‐1 sibling (F: 100%) (R/E: White brit. 33%, Mixed race 11%, missing 56%) (SES: nr) |
BN (% nr) EDNOS‐BP (% nr) |
Outpatient | Maudsley model (Stewart et al. 2015) | 12 | 20 weeks | Thematic analysis of groups and individual interviews of YP and parents |
Themes
|
| Engman‐Bredvik, Carballeira Suarez, Levi, and Nilsson (2016) [Sweden] | Parent structured interviews on the experiences of MFT | [Px: 14.9 (nr, 12–17)] |
12 [from 6 families] ‐0 Px ‐6 mothers ‐6 fathers (F: 100%) (R/E: nr) (SES: nr) |
[YP: AN (100%)] | Inpatient and Outpatient | Wallin (2011) model | 10 days | 1 year | Empirical, psychological, phenomenological method (EPP) (Lundberg, et al., 2007) 1–2 months post‐EOT | Themes:
|
| Salaminiou (2005) [UK] | YP and parents interviews of the experience of MFT | nr (<18) |
34 [from 18 families] ‐16 Px ‐18 mothers ‐10 fathers (F: 94%) (R/E: nr) (SES: 50% UK social class I or II / 50% social class III or IV)^ |
AN (% nr) EDNOS‐R (% nr) |
Outpatient | Maudsley model | 9–11 days | 9 months | Content analysis of EOT interviews with researcher |
Themes
|
| ||||||||||
| ||||||||||
| ||||||||||
| Voriadaki et al. (2015) [UK] | YP and parent experience of MFT process during first 4‐days (focus groups, daily diary writing, rating scales) | nr (nr, 15–16) |
15 [from 6 families] ‐5 Px ‐6 mothers ‐4 fathers (F:100%) (R/E: White brit. 80%, Asian brit. 20%) (SES: 100% “social class II or III”)^ |
AN (100%) | Outpatient | Maudsley model | 10 (only experience of first 4 days reflected on) | 9 months | Interpretative phenomenological analysis using multiple data sources (focus groups, daily diary writing, rating scales) | Main themes for first 4 days of MFT:
|
| Wiseman, Ensoll, Russouw, and Butler (2019a) [UK] | Focus group and interviews: Caregiver and clinician experience of MFT | [Px: 14.6 (nr, 14–16)] |
4 [from 3 families] [family role nr] (F: 100%) (R/E: White brit. 100%) (SES: “Diverse”) [All YP (n = 5) declined to participate] |
[YP: AN (100%)] | Outpatient | Maudsley model | 9 days | 7 months | Thematic analysis (Braun & Clarke, 2006) | Main themes identified:
|
| Wiseman, Ensoll, Russouw, and Butler (2019b) [UK] | Focus groups and interviews: Caregiver and clinician perspective on how change occurs and how MFT adds to existing treatment pathways | [Px: 14.6 (nr, 14–16)] |
4 [from 5 families] ‐0 Px ‐2 fathers ‐1 mother ‐1 g.mother (F: 100%) (R/E: White brit. 100%) (SES: “Diverse”) [All YP (n = 5) declined to participate] |
[YP: AN (100%] | Outpatient | Maudsley model | 10 days | nr | Thematic analysis (Braun & Clarke, 2006) | Sub‐themes of main theme: Mechanisms of MFT for creating recovery‐focused change:
|
| Adult MFT | ||||||||||
| Brinchmann and Krvavac (2021) [Norway] | Patient and families' experience of MFT. Data collected from field observations in 2 MFT groups as well as qualitative group and individual interviews | Px: mean nr (nr, 18–22) |
48 b [from 12 families] ‐12 Px ‐12 “sets of parents” c ‐9 siblings ‐1 g.mother ‐2 partners] (F:100%) (R/E: nr) (SES: nr) |
AN (67%) BN (33%) | Inpatient and (mostly) outpatient | As per Skarbø and Balmbra (2020) | 6 x 2–3 day gatherings | 1 year | Grounded theory | Main categories:
|
| Tantillo, McGraw, Hauenstein, and Groth (2015) [USA] | Focus groups of patient and carer experience of recovery process and emo/beh/ improvement in MFT | Px: 23.4 (6.0, 20–34) |
17 [from 10 families] ‐5 Px ‐9 mothers ‐3 fathers (F: 80%) (R/E: Cauc. 82%, Asian Amer. 12%, Latino 6%) d (SES: 80% full time college, 20% working FT) d |
AN (% nr) EDNOS (% nr) | Outpatient | Relational/motivational MFT group | 8 sessions | 8 weeks | Content analysis | Themes identified:
|
| Whitney, Currin, Murray, and Treasure (2012)) [UK] | 60–90 m individual interviews investigating carers experience of FT (n = 10) or MFT (n = 11) |
[Px: 25 (9, 18–53)] Carers: 47 (13, 21–62) |
23 [from 15 families] ‐0 Px ‐17 parents ‐4 siblings ‐1 husband ‐1 daughter (F: nr) (R/E: nr) (SES: nr) |
[Px: AN (100%)] | Inpatient | Family day workshops (Treasure et al., 2011) | 3 days | 3 days | Interpretive phenomenological analysis (IPA) |
Main themes:
|
| ||||||||||
Abbreviations: AN, anorexia nervosa; BN bulimia nervosa; EDNOS, eating disorder not otherwise specified; EOT, end of treatment; FT, family therapy; MFT, multi‐family therapy; MFTG‐RM, Relational/motivational multi‐family therapy group; nr, not reported; px, patient; SES; socioeconomic status; YP, young person.
Patient data only.
Sample size reported is for all participants included in fieldwork and qualitative interviews.
Counted as n = 24 individuals in study total sample above (N = 48).
Data are for all participants in study (N = 17) as patient‐only data are not reported.
3.2. Narrative synthesis
3.2.1. MFT models: Population, setting, intensity, and duration
There was substantial variability in the different types of MFT models described (see Tables 2 and 4). However, when studies were clustered according to age, diagnosis, and setting, more homogeneity emerged. One commonality between most studies was that MFT was an adjunctive treatment. Apart from a stand‐alone 5‐day MFT program described in three studies, all from the same center, MFT was always offered in combination with another form of outpatient treatment (e.g., single‐family therapy) or as part of an inpatient admission.
Outpatient MFT‐AN typically lasted 9–12 months and included between 8 and 21 days of MFT treatment. The only exceptions were the three studies from the same center that offered the stand‐alone 5‐day MFT‐AN model (Knatz et al., 2015; Marzola et al., 2015; Wierenga et al., 2018). Almost all were influenced by the Maudsley Hospital (Simic & Eisler, 2015) and/or Dresden (Scholz & Asen, 2001) models. Outcomes for MFT‐BN were only described in two studies from the same child and adolescent service, which lasted four months (Duarte, 2012; Stewart et al., 2019). Inpatient MFT models for young people were briefer, ranging from 2 (Depestele et al., 2017) to 4 months (Geist et al., 2000). During the latter program, all participants were discharged to outpatient treatment during the course of MFT (Geist et al., 2000).
Adult MFT models were generally much more varied compared to those described for young people. Outpatient adult MFT included a stand‐alone 5‐day model (Wierenga et al., 2018), a 26‐week model (Tantillo et al., 2019), and a 12‐month model (Skarbø & Balmbra, 2020), with the latter specifically targeting a mixed‐diagnostic group of adults with “severe eating disorders.” Two studies described MFT as part of inpatient or day‐patient treatment. One program described was a very brief (3‐day) MFT workshop (Whitney, Currin, et al., 2012; Whitney, Murphy, et al., 2012). The other used an 8‐week program that was offered to those on the inpatient and day‐patient units (Dimitropoulos et al., 2015). Brief MFT was considered more cost effective than family therapy on an adult inpatient unit in one study (Whitney, Murphy, et al., 2012). There were no specific MFT‐BN program for adults identified by the search strategy.
3.2.2. Outcomes: Quantitative results
Randomized controlled trials
Three studies used an RCT design, all of which compared MFT to a version of single‐family therapy (see Table 2). One investigated MFT‐AN for young people in an outpatient setting (Eisler, Simic, Hodsoll, et al., 2016), one for MFT for young people on an inpatient unit (Geist et al., 2000), and one for adult inpatient MFT (Whitney, Murphy, et al., 2012). See Table 2 for details.
The largest study (N = 167), and only multi‐center trial identified by the search strategy, randomized young people (age range = 12–20) to 12 months of outpatient FT‐AN alone or FT‐AN plus 10 days of MFT‐AN (Eisler, Simic, Hodsoll, et al., 2016). No significant differences between groups at baseline were observed. Regardless of the treatment arm, significant improvements in global outcomes, weight, eating disorder psychopathology, and mood, as well as the negative aspects of caregiving were reported. Participants randomized to receive MFT‐AN also had better global outcomes at end of treatment, using the Morgan Russel outcome criteria (Russell, Szmukler, Dare, & Eisler, 1987), compared to those who received FT‐AN alone. Seventy‐six percent had a Good or Intermediate outcome in the MFT group compared to 58% in the FT‐AN group (Eisler, Simic, Hodsoll, et al., 2016). This difference was no longer statistically significant at 6‐month follow‐up (18‐months post randomization); however, the MFT group continued to have significantly higher %mBMI (MFT‐AN group = 91% vs. FT‐AN group = 85%, respectively). Self‐report self‐esteem did not change between baseline and end of treatment in either study arm, although the authors note that baseline scores were within the normal range, suggesting a ceiling effect (Eisler, Simic, Hodsoll, et al., 2016).
The remaining two RCTs identified were both much smaller and conducted on inpatient units. Geist et al. (2000) randomized adolescents (N = 25) to receive either single‐family therapy or MFT as part of their inpatient treatment package. No baseline differences between the groups were reported. Treatment in both arms was associated with physical health and eating disorder symptom improvement; however, no differences were reported in weight, eating disorder symptoms, or family functioning outcomes between the two treatments (Geist et al., 2000). Contrary to findings from the Eisler, Simic, Hodsoll, et al. (2016) RCT, no changes in symptoms of depression or severity of general psychopathology were reported (Geist et al., 2000). Notably, self‐report family functioning significantly deteriorated in both treatments, indicating an acknowledgement of more family psychopathology at the end of treatment.
On an adult inpatient unit, Whitney, Murphy, et al. (2012) randomized participants (N = 48) to either 18 hours of weekly/fortnightly single‐family therapy or a 3‐day MFT intervention during their admission. They reported a significant treatment by time interaction effect. Post hoc comparisons showed that participants who received MFT had higher BMI at 6‐month follow‐up, but lower BMI at 36‐month follow‐up. However, these did not reach statistical significance. Across both treatments, a significant reduction in expressed emotion and improvement in caregiver general wellbeing was also observed; however, neither the negative nor positive aspects of caregiving significantly changed. Furthermore, no differences between the treatments were reported on any other individual or family outcome measure at short (3‐month) and long (3‐year) term follow‐up, potentially emphasizing the general benefits of family involvement, rather than any MFT‐specific benefits.
Non‐randomized comparison studies
Two outpatient (both young person) and two inpatient studies (one young person, one adult) compared outcomes following MFT to another type of treatment using a non‐randomized design (see Table 2 for details).
In a retrospective chart review of treatment response in a specialist child and adolescent service (N = 50), Gabel et al. (2014) compared those who received MFT as part of their treatment package with age‐matched controls who received treatment as usual, defined as medical monitoring, nutrition therapy including meal plans, pharmacological treatment as required, psychoeducation, individual, and/or mental health therapy. Those who received MFT in addition to treatment as usual had significantly higher mean weight after 12 months than those who only had treatment as usual (99.6%IBW vs. 95.4%IBW, respectively). Outcomes for the sub‐group who received MFT showed significant improvements in eating disorder and depression symptoms, although these changes were not compared to the control group outcomes. There were no differences between the two groups at baseline.
Marzola et al. (2015) also conducted a retrospective chart review. They compared outcomes at follow‐up for two different 5‐day versions of intensive outpatient family therapy for young people; intensive single‐family, and MFT. End‐of‐treatment (5 days) outcomes were not compared; however, each is associated with eating disorder symptom improvements and reported separately elsewhere (Knatz et al., 2015; Rockwell, Boutelle, Trunko, Jacobs, & Kaye, 2011). At follow‐up (mean = 30.9 months, SD = 20.2) both treatments continue to be associated with improvements, although no differences between groups with respect to %mBMI, global outcomes and need for higher levels of care (inpatient or residential) are reported (Marzola et al., 2015). Of note, the MFT group were significantly younger (16.4 vs 19.2 years), had a shorter time to follow‐up (22.5 vs. 53.4 months), and more were undergoing treatment at follow‐up (58% vs. 32%), making comparisons tentative.
In the inpatient context, the benefits of MFT over other types of intervention are less clear. Depestele et al. (2017) compared adjunctive MFT with or without young person involvement (i.e., MFT vs. parent groups). Treatment allocation was not randomized and was dependent on the time of admission to the unit with the type of intervention offered switching every 6 months. At end of treatment, both groups reported a significant improvement in eating disorder symptoms and some aspects of family functioning, although no differences were reported according to treatment type. Specifically, fathers reported improved general functioning and young people reported improved problem solving, whereas mothers reported decreased problem solving on the Dutch version of the Family Assessment Device (FAD) (Epstein, Baldwin, & Bishop, 1983; Wenniger, Hageman, & Arrindell, 1993). No differences in behavioral control, affective involvement, or affective responsiveness were reported after MFT (Depestele et al., 2017). At baseline, the groups did not differ with regard to eating disorder symptoms or other family factors, although the MFT group was significantly older (17.4 vs. 16.6 year) and fewer reported engaging in non‐suicidal self‐injury (51.6 vs 74.0%). These differences were controlled for in analyses.
Using an uncontrolled pilot study design (N = 45), Dimitropoulos et al. (2015) compared 8 weeks of either single‐family therapy or MFT for adults receiving day‐ or inpatient treatment. Treatment was assigned non‐randomly based on MFT availability, which was offered four times per year, and no baseline differences in patient or family characteristics were observed between the two treatment groups. At the end of treatment, Dimitropoulos et al. (2015) reported that a range of individual (BMI, eating disorder symptoms, perceived stigma) and caregiver factors (perceived burden, expressed emotion, and caregiver symptoms of depression) all significantly improved. These changes were either maintained (caregiver burden) or continued to improve (expressed emotion and caregiver depressive symptoms) at a 3‐month follow‐up. Nevertheless, the level of perceived social support and impact of stigma for caregivers did not change across treatment or follow‐up period (Dimitropoulos et al., 2015). Furthermore, no differences between interventions were reported on any individual (BMI and eating disorder psychopathology) or caregiver factors (perceived burden, expressed emotion, perceived social supports, and stigma) (Dimitropoulos et al., 2015).
Case series
Physical health and eating disorder symptomatology
MFT‐AN was associated with significant improvements in weight, regardless of age or treatment setting (see Table 2). Only one study did not report a significant improvement in weight during MFT; however, participants in this study started treatment within the healthy range (mean BMI = 20.7, SD = 3.3), which was maintained during treatment (Tantillo et al., 2019). Significant improvements were also reported in eating disorder psychopathology, including binge‐purge symptoms, by every study that measured it, irrespective of age, setting or instrument used (see Table 2).
Comorbid symptomatology
Outpatient MFT‐AN for young people was associated with a significant reduction in symptoms of depression from baseline to discharge (Salaminiou et al., 2017). Salaminiou et al. (2017) reported that symptoms of depression reduced from just below the “severely depressed” range to within the “mild” range after 6 months of MFT‐AN. Similarly, self‐report symptoms of both depression and anxiety significantly reduced during outpatient MFT‐BN, although, parent reports of their child's symptoms did not reveal significant changes (Stewart et al., 2019).
The only adult MFT case series to investigate comorbid symptoms found that state, but not trait, anxiety reduced during a 5‐day MFT week (Wierenga et al., 2018). Change in symptoms of depression was not investigated in any adult MFT study in this review.
Broader individual functioning and well‐being
Several studies assessed broader symptoms of general well‐being in addition to eating disorder symptom change (see Table 3). Outpatient MFT‐AN for young people was associated with significant improvements in quality of life (Gelin et al., 2015; Mehl et al., 2013), self‐perception and self‐image (Hollesen et al., 2013), and self‐esteem (Mehl et al., 2013; Salaminiou et al., 2017). MFT‐BN for adolescents was associated with significant improvements in emotion regulation capacity (Stewart et al., 2019).
Regarding MFT for adults, at the end of treatment, patients reported significant improvements in emotional awareness but no change in emotion regulation strategies (Tantillo et al., 2019). In the inpatient context, difficulties with interpersonal functioning did not change from baseline to short‐ and long‐term follow‐up (Whitney, Murphy, et al., 2012).
Family functioning
In outpatient MFT‐AN for young people, Salaminiou (2005) found that family functioning did not change during 6 months of MFT, although the author noted that mean scores at baseline were mid‐ranged, indicating adequate family functioning. For adults who attend a 5‐day MFT, a significant improvement in general family functioning was reported (Wierenga et al., 2018). See Table 3 for further details.
Parent and caregiver factors
Outpatient MFT‐AN for young people was associated with a range of caregiver/parent improvements. By the end of treatment, caregiver burden and most negative impacts of the illness significantly reduced in one study (Dennhag et al., 2019). Perceived caregiver isolation was the only aspect that did not change during MFT (Dennhag et al., 2019). In another study, parental mood improved (Salaminiou et al., 2017). This improvement was significant for mothers, but not fathers, however, baseline maternal and paternal scores were within the normal range, suggesting a floor effect (Salaminiou et al., 2017). In the same study, adjusted regression analysis revealed change in parental depressive symptoms across treatment was not associated with young person percentage median Body Mass Index (%mBMI) outcome at end of treatment (Salaminiou, 2005). Following outpatient MFT‐BN, caregiver burden and parental mood also significantly improved in one study, although level of anxiety did not (Stewart et al., 2019).
The impact of MFT on expressed emotion (critical comments, positive remarks emotional overinvolvement, warmth, and hostility) is mixed. Paternal critical comments significantly reduced from baseline to 6 months in one study (Salaminiou, 2005); however, all other aspects of maternal and paternal expressed emotion towards the child did not change during 6 months of treatment. Salaminiou (2005) also measured level of expressed emotion between parents, as one marker of how well the parental dyad was functioning. Again, no change was observed, except for warmth from mothers towards fathers, which significantly increased (Salaminiou, 2005). Furthermore, adjusted regression analysis revealed that a reduction in paternal criticism and an increase in emotional overinvolvement during MFT‐AN was associated with improved young person %mBMI at end of treatment in the same study (Salaminiou, 2005).
Dennhag et al. (2019) also explored whether baseline and change in caregiver factors during MFT were associated with young person outcomes. At baseline, maternal level of guilt was associated with poorer end‐of‐treatment eating disorder symptom outcomes. Furthermore, increased paternal social isolation and perceived burden of dysregulated behaviors was also associated with poorer physical health outcomes for the young person at end of treatment (Dennhag et al., 2019). Regarding parental change over treatment and its association with outcome, regardless of role in the family, decreases in parental perceived isolation was associated with improved young person physical health and general functioning at end of treatment (Dennhag et al., 2019).
Outcomes at follow‐up
Follow‐up data are reported in three adult MFT case series. They indicate that end‐of‐treatment improvements are generally maintained or improved upon at follow‐up. Wierenga et al. (2018) reported that weight continued to significantly increase, with mean BMI within the healthy range (mean = 19.6, SD = 2.0), and eating disorder symptom improvement was maintained at follow‐up from their stand‐alone 5‐day MFT program (mean duration to follow‐up = 4.7–7.6 months [varies depending on measure]). Similarly, Tantillo et al. (2019) found that participants maintained their weight and eating disorder symptoms continued to improve at 6‐month follow‐up from their 26‐week program (see Table 2 for further details). In addition, emotion regulation capacity was either maintained or continued to improve during the follow‐up period (Tantillo et al., 2019). One case series with young people reported that weight continued to significantly improve, while the quality of life and eating disorder symptoms stabilized at 1‐year follow up; however, no data were reported (Gelin et al., 2015).
Non‐completion rates (all study designs)
MFT non‐completion, also referred to as dropout, is typically reported to be low and is an often‐stated benefit of the treatment (Gelin et al., 2018). Twelve of the 17 quantitative studies reported dropout rates, which ranged from 0% to 17%. Six of these studies reported dropout rates below 10% (see Table 3 for details). Data are presented here synthesized, rather than by study design, to provide a better overview of all available data.
3.2.3. Experience of MFT: Qualitative data
Qualitative data are reported in 10 studies: seven reporting on the experience of MFT for young people and their family members, and three on MFT for adults and their family members. Most commonly, data were generated from individual or focus group interviews and responses analyzed using thematic or content analysis. See Table 3 for further details. The total sample reported on consisted of 47 people with eating disorders (30 young people and 17 adults) and 140 caregivers (120 parents, 14 siblings, three partners, two grandparents, and one adult patient's child). Several papers also reported on clinician experience of MFT (Brinchmann et al., 2019; Wierenga et al., 2018; Wiseman et al., 2019a, 2019b), which is not reported here as it is beyond the scope of this review. Of note, the majority of qualitative data are generated from the family and caregiver perspective. Only six studies (four young persons, two adults) included patients in their sample, and two studies, which appear to use the same sample, noted that they attempted to recruit young people but all declined (Wiseman et al., 2019a, 2019b).
Qualitative studies were initially reviewed separately according to MFT target population (young person or adult) and setting (outpatient or day/inpatient) and were intended to be presented separately. However, due to large overlap in participants' experiences, the data are synthesized and presented together.
Across all studies, there was a common finding that MFT is experienced as both helpful and challenging with similar experiences described for adults and young people for both MFT‐AN and MFT‐BN. From data generated through observation, interviews and focus groups collected during and after treatment, there was a sense by most participants that MFT helped the family to view the eating disorder symptoms in new ways (Baumas et al., 2021; Duarte, 2012; Salaminiou, 2005; Voriadaki, Simic, Espie, & Eisler, 2015), take on new perspectives (Duarte, 2012; Engman‐Bredvik et al., 2016; Tantillo et al., 2015;Whitney, Currin, et al., 2012; Wiseman et al., 2019b), gain new skills (Duarte, 2012; Tantillo et al., 2015) and feel more empowerment (Engman‐Bredvik et al., 2016; Salaminiou, 2005). Together, this helped people, particularly parents/caregivers, feel less guilty, scared, and anxious (Whitney, Currin, et al., 2012) and feel more confident (Whitney, Currin, et al., 2012; Wiseman et al., 2019b). In two studies, adult patients and carers noted that MFT helped them to open up and share their experiences (Berit Støre Brinchmann & Krvavac, 2021; Tantillo et al., 2019).
A common theme across several studies was that MFT led to a shift in the quality of family connection and dynamics (Baumas et al., 2021; Berit Støre Brinchmann & Krvavac, 2021; Duarte, 2012; Tantillo et al., 2015; Wiseman et al., 2019b). Commonly, parents/caregivers felt MFT provided a new support network that helped people in all family roles feel less alone and isolated (Duarte, 2012; Engman‐Bredvik et al., 2016; Salaminiou, 2005; Tantillo et al., 2015; Wiseman et al., 2019b), which was also echoed by some patients, albeit fewer (Duarte, 2012; Salaminiou, 2005). There was value placed on being able to observe and learn from other families who had similar experiences (Duarte, 2012; Whitney, Currin, et al., 2012; Wiseman et al., 2019b). In one study, participants struggled to differentiate the contribution that MFT made to their overall treatment compared to other elements of their treatment program (Baumas et al., 2021).
The challenging aspects of MFT were multifaceted. There were concerns by some about the potential for unhelpful comparisons to be made, the fact that individual family needs could not always be addressed, and that it was difficult at times to manage disparities regarding the different rates of recovery for each person in the group (Baumas et al., 2021). Of note, comparisons were also sometimes seen as helpful as they helped people feel validated and less isolated (Voriadaki et al., 2015).
A minority of parents/caregivers mentioned concerns that the group may set recovery backwards or that the patients may share unhelpful eating disorder “tricks” (Baumas et al., 2021; Salaminiou, 2005). The intensity of the group was also mentioned by some participants as both helpful and exhausting (Voriadaki et al., 2015; Whitney, Currin, et al., 2012; Wiseman et al., 2019b).
To understand changes in the patient experience during MFT, Voriadaki et al. (2015) collected data at different time points over four consecutive MFT days. They found that participants tended to move from anxiety and apprehension about attending, to noticing similarities and then feeling more settled. This helped people to become more aware of the illness and the role in it played in their relationships. By the end of the 4 days, the focus was shifted towards future coping and reflecting on progress. This matches data reported by Wiseman et al. (2019a) who specifically investigated the way family members perceived change to occur in MFT. No young people consented to participate in this study; however, parents perceived the treatment mechanisms to include the increased intensity, the experience of being with other families, family bonding, shifting of guilt and blame, improved parental confidence, and understanding the illness differently (Wiseman et al., 2019a).
3.2.4. Meta‐synthesis
Taken together, MFT is both perceived as helpful and leads to a wide range of improvements. It is also associated with several challenges for different participants at different time points. The benefits regarding eating disorder symptoms and other individual and family factors are reported by most, more so by family members than patients, and are reflected in robust quantitative and qualitative findings of eating disorder symptoms and physical health improvements by the end of treatment and often at follow‐up.
As might be expected of any eating disorder treatment, MFT is also challenging, which is reflected in the more mixed family and caregiver quantitative and qualitative data. There are difficulties associated with the group process, such as concerns about the comparison that comes from being in a group, the intensity of MFT, and the realization of needing to try new things. However, these were balanced by a reduction in perceived isolation and support from the group. The low dropout rate further supports that the group process is engaging and acceptable.
The work required of participants during MFT coupled with the increased support afforded by coming together does yield rewards. Eating disorder symptoms and physical health do consistently improve, but the difficulty and anxiety associated with reaching these changes are clearly reflected in the experiences, and more mixed quantitative findings, particularly regarding family factors. Nevertheless, while qualitative data suggest a key benefit of MFT is a reduction in isolation and an increase in solidarity, this may not generalize beyond the MFT group itself. Quantitative findings from one study indicate that self‐report perceived social supports, isolation, and stigma more broadly do not significantly change during MFT.
One notable finding is that MFT can be described by the patient as more helpful for other family members, yet improvements are more consistently observed for the patient themselves. This fits with findings from one study, in which the majority of parents reported that the benefits of MFT for the patient came indirectly via themselves as parents (Salaminiou, 2005). This perceived disparity in helpfulness may also reflect the stage of recovery of participants at the time of data collection (typically during or at the end of treatment). What is perceived as unhelpful or challenging in the moment may be perceived as helpful and needed with hindsight. Salaminiou (2005) found that participants experienced some exercises to be both difficult and helpful, and vice versa, bringing into question the usefulness of the dichotomous helpful/unhelpful divide when discussing MFT (and potentially other psychological treatments). Furthermore, there was relatively good agreement between participants regarding which MFT activities were perceived as helpful, yet little agreement on what was perceived as unhelpful. This further highlights how specific and idiosyncratic unhelpful aspects may be to each individual.
This disparity also underscores the important role that family members have in the recovery process and MFT's capacity to support the entire system, not just the patient. It emphasizes the need for MFT (and potentially other interventions) to continue to include and support family members, given their own levels of need and the mixed outcomes for parents/caregivers specifically. Of note, there are no data comparing the experience of MFT to the experience of other treatments, making it difficult to determine whether these processes are unique to MFT or common across all eating disorder interventions that involve family members. Qualitative data collected at different time points are also needed to understand whether the patient perspective shifts at longer follow‐up.
4. DISCUSSION
MFT has been used in clinical practice for decades (Gelin et al., 2018; Gelin et al., 2016) and practice guidelines often recommend including and supporting family members in eating disorder treatments (Hay et al., 2014; Hilbert et al., 2017; NICE, 2017). The current review highlights that MFT is associated with improvements in a range of individual and family factors. However, the evidence base is relatively small, with most studies underpowered and large heterogeneity in the MFT models tested.
Regarding the first aim of this study, it can be concluded that MFT is associated with physical and psychological improvement for people with eating disorders, across the age range, treatment setting, and diagnoses. This was almost unanimously reported across all studies, often with medium and large effect sizes. However, with the exception of a stand‐alone 5‐day model, all other MFT models were adjunctive treatments. As such, the unique benefits of MFT cannot be ascertained from the available data.
When MFT outcomes are compared to other types of treatment, the findings are mixed. There is evidence from two studies that 12 months of MFT alongside single‐family therapy or treatment as usual may lead to better global outcomes and higher weight at follow‐up for young people in an outpatient setting. This finding was reported in the largest study and only outpatient RCT that was identified in this review, meaning more weight could arguably be given to this finding. However, most other studies that included a comparison group found outcomes following MFT were equivalent to other treatments, both in outpatient and inpatient settings and across the age range. Furthermore, outcomes following intensive versions of family therapy have similar outcomes, regardless of whether it is provided in the single‐ or multi‐family format. One potential benefit of MFT was its cost‐effectiveness as an adjunctive adult inpatient treatment, although more data is needed here to form any firm conclusions.
Regarding the impact of MFT on individual and family/caregiver factors, the data highlights a range of benefits for all involved. For the patient, it is associated with improvements in symptoms of depression and anxiety, self‐esteem, quality of life, and facets of emotion regulation capacity. However, MFT does not seem to be associated with improvements in perceived interpersonal problems or stigma.
Family members also report improvements in their own symptoms of depression, improvements in the negative aspects of caregiving, general well‐being, and some changes in level of expressed emotion, although these data are mixed. This fits with evidence that not all aspects of expressed emotion may be as relevant for adolescents as they are with adults. A recent review found that parental emotional overinvolvement with adolescents was not associated with problematic symptoms or behaviors across a range of mental health diagnoses, and may even have some benefits (Rienecke, 2020). No changes were reported in the positive experiences of caregiving, level of caregiver anxiety, or perceived stigma and social supports. Data regarding changes in general family functioning are more mixed with some studies reporting improvements, others no change, and one a deterioration in functioning.
These findings match the data on the experience of MFT well. These data show that MFT is generally valued, albeit with a fair degree of variability. Benefits are reported by most, especially the increase in perceived support by being in a group with people who have had similar experiences. The process can be exhausting and anxiety provoking, as might be expected of any psychological treatment, and may be part of what makes the treatment effective. Some participants raised concerns about the inevitable comparison that comes from being in a group and the realization of needing to try new things. However, available data on the process of change during MFT suggests these anxieties are alleviated quickly and by the third MFT day participants are more settled and perceived support from the group has increased. Given the experience of MFT can be intense and anxiety provoking, it is unsurprising that some aspects of caregiving and family functioning remain unchanged. Whether MFT experiences and learning lay a foundation for future benefits is yet to be determined and no data are available to report on this.
Despite the many benefits of MFT, the current review highlights some key areas for future research. Generally, the included studies were uncontrolled with small sample sizes, meaning most are likely underpowered. Even the RCTs tended to be small, with two of the three identified in this review having sample sizes of less than 50 participants. Furthermore, given most MFT models were adjunctive, the specific contribution and cost‐effectiveness of adding MFT to other treatments remain unclear. Future studies are needed that examine the unique contribution made by MFT, both regarding outcomes and the experience of treatment, and whether the additional resources required of families and services are worth the benefit.
4.1. Limitations
There are several important limitations to this review. First, only English language studies were reviewed, and the publication type was limited to peer‐reviewed journal articles, book chapters, and dissertations (not conference abstracts). Furthermore, this is not an exhaustive review of MFT treatment models. Many theoretical and descriptive papers exist outlining MFT models that vary from those described here, without reporting any data or methodology for data collection.
Regarding the papers reviewed, the most notable are the small sample sizes and uncontrolled nature of study methodologies. Even though three RCTs were identified, two had sample sizes below 50. Similarly, sample sizes for qualitative studies were also often small, with the voice of the person with the eating disorder limited or missing. Furthermore, there was a lack of diversity across the studies. The sample reported on was predominantly white and female with very little socioeconomic data reported. This makes interpretation of the data and conclusions from this review very tentative.
Finally, it is very hard to determine treatment response for people with bulimia nervosa and other eating disorder presentations. There was no data for adult MFT‐BN and very limited data for young people. MFT‐BN findings are very preliminary.
5. CONCLUSIONS
The current review suggests MFT is an effective treatment for anorexia nervosa and leads to improvements in individual, as well as some caregiver and family factors. The most robust finding is for young people seen in an outpatient setting. When added to single‐family therapy, MFT may enhance outcomes compared to single‐family therapy alone, although replication studies are needed. Several benefits afforded by MFT appear unique to the multi‐family context; however, the impact of these benefits (e.g., increased support) cannot be determined from the current review. When compared to other types of treatment, MFT is generally non‐inferior, although it is typically an adjunctive treatment, making it difficult to determine its value alone. Future studies are needed that specifically investigate the unique contribution and cost‐effectiveness of MFT compared to other treatments. The evidence base also needs strengthening with higher quality studies with larger sample sizes and more diverse eating disorder presentations. Study designs that consider patient and family preferences, and previous treatment history are also needed, as well as clearer indication criteria for MFT and extended guidelines for the use of MFT in stepped care approaches.
CONFLICT OF INTEREST
Ulrike Schmidt is supported by a National Institute of Health Research (NIHR) Senior Investigator Award. She receives salary support from the NIHR Mental Health Biomedical Research Center (BRC) at the South London and Maudsley NHS Foundation Trust and King's College London (KCL).
Supporting information
Appendix S1: Supporting Information
Baudinet, J. , Eisler, I. , Dawson, L. , Simic, M. , & Schmidt, U. (2021). Multi‐family therapy for eating disorders: A systematic scoping review of the quantitative and qualitative findings. International Journal of Eating Disorders, 54(12), 2095–2120. 10.1002/eat.23616
Action Editor: Kelly Klump
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study
REFERENCES
- Anderson, C. M. , Griffin, S. , Rossi, A. , Pagonis, I. , Holder, D. P. , & Treiber, R. (1986). A comparative study of the impact of education vs. process groups for families of patients with affective disorders. Family Process, 25(2), 185–205. 10.1111/j.1545-5300.1986.00185.x [DOI] [PubMed] [Google Scholar]
- Asen, E. , & Scholz, M. (2010). Multi‐family therapy: Concepts and techniques. London/New York: Routledge. [Google Scholar]
- Baumas, V. , Zebdi, R. , Julien‐Sweerts, S. , Carrot, B. , Godart, N. , Minier, L. , & Rigal, N. (2021). Patients and Parents' experience of multi‐family therapy for anorexia nervosa: A pilot study. Frontiers in Psychology, 12. 10.3389/fpsyg.2021.584565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beavers, W. R. , Hampson, R. B. , & Hulgus, Y. F. (1985). Commentary: The Beavers systems approach to family assessment. Family Process, 24(3), 398–405. 10.1111/j.1545-5300.1985.00398.x [DOI] [Google Scholar]
- Beck, A. T. , Steer, R. A. , & Brown, G. K. (1996). Manual for the Beck depression inventory‐II. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Benjamin, L. S. (1974). Structural analysis of social behavior (SASB). Psychological Review, 81, 392–425. [Google Scholar]
- Braun, V. , & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- Brinchmann, B. S. , & Krvavac, S. (2021). “Breaking down the wall” patients' and families' experience of multifamily therapy for young adult women with severe eating disorders. Journal of Eating Disorders, 9(1), 56. 10.1186/s40337-021-00412-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brinchmann, B. S. , Moe, C. , Valvik, M. E. , Balmbra, S. , Lyngmo, S. , & Skarbo, T. (2019). An Aristotelian view of therapists' practice in multifamily therapy for young adults with severe eating disorders. Nursing Ethics, 26(4), 1149–1159. 10.1177/0969733017739780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chorpita, B. F. , Yim, L. , Moffitt, C. , Umemoto, L. A. , & Francis, S. E. (2000). Assessment of symptoms of DSM‐IV anxiety and depression in children: A revised child anxiety and depression scale. Behaviour Research and Therapy, 38(8), 835–855. 10.1016/S0005-7967(99)00130-8 [DOI] [PubMed] [Google Scholar]
- Claes, L. , & Vandereycken, W. (2007). Self‐injurious behavior: Differential diagnosis and functional differentiation. Comprehensive Psychiatry, 48(2), 137–144. 10.1016/j.comppsych.2006.10.009 [DOI] [PubMed] [Google Scholar]
- Cook‐Darzens, S. (2007). Thérapies multifamiliales. Toulouse: Érès. Cairn.info. https://www.cairn.info/therapies-multifamiliales-9782749207094.htm
- Couturier, J. , Isserlin, L. , Norris, M. , Spettigue, W. , Brouwers, M. , Kimber, M. , … Pilon, D. (2020). Canadian practice guidelines for the treatment of children and adolescents with eating disorders. Journal of Eating Disorders, 8(1), 4. 10.1186/s40337-020-0277-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutrona, C. E. , & Russell, D. W. (1987). The provisions of social relationships and adaptation to stress. Advances in Personal Relationships, 1, 37–67. [Google Scholar]
- Dare, C. , & Eisler, I. (2000). A multi‐family group day treatment programme for adolescent eating disorder. European Eating Disorders Review, 8(1), 4–18. [DOI] [Google Scholar]
- Dawson, L. , Baudinet, J. , Tay, E. , & Wallis, A. (2018). Creating community—The introduction of multi‐family therapy for eating disorders in Australia. Australian and New Zealand Journal of Family Therapy, 39(3), 283–293. 10.1002/anzf.1324 [DOI] [Google Scholar]
- Dennhag, I. , Henje, E. , & Nilsson, K. (2019). Parental caregiver burden and recovery of adolescent anorexia nervosa after multi‐family therapy. Eating Disorders, 9315161, 1–17. 10.1080/10640266.2019.1678980 [DOI] [PubMed] [Google Scholar]
- Depestele, L. , Claes, L. , Dierckx, E. , Colman, R. , Schoevaerts, K. , & Lemmens, G. M. D. (2017). An adjunctive multi‐family group intervention with or without patient participation during an inpatient treatment for adolescents with an eating disorder: A pilot study. European Eating Disorders Review, 25(6), 570–578. 10.1002/erv.2556 [DOI] [PubMed] [Google Scholar]
- Derogatis, L. R. (1992). The brief symptom inventory (BSI): Administration, scoring and procedures: Manual II. Clinical Psychometric Research: Baltimore. [Google Scholar]
- Dimitropoulos, G. , Farquhar, J. C. , Freeman, V. E. , Colton, P. A. , & Olmsted, M. P. (2015). Pilot study comparing multi‐family therapy to single family therapy for adults with anorexia nervosa in an intensive eating disorder program: Multi‐family therapy for anorexia nervosa. European Eating Disorders Review, 23(4), 294–303. 10.1002/erv.2359 [DOI] [PubMed] [Google Scholar]
- Dragomirecka, E. , Lenderking, W. R. , Motlova, L. , Goppoldova, E. , & Šelepova, P. (2006). A brief mental health outcomes measure: Translation and validation of the Czech version of the Schwartz outcomes Scale‐10. Quality of Life Research, 15(2), 307–312. 10.1007/s11136-005-1389-y [DOI] [PubMed] [Google Scholar]
- Duarte, A. E. (2012). The experiences of adolescents and their parents/carers with a multi‐family therapy Programme for bulimia nervosa. MSc Dissertation . London, UK: King's College London. [Google Scholar]
- Eisler, I. (2005). The empirical and theoretical base of family therapy and multiple family day therapy for adolescent anorexia nervosa. Journal of Family Therapy, 27(2), 104–131. 10.1111/j.1467-6427.2005.00303.x [DOI] [Google Scholar]
- Eisler, I. , Simic, M. , Blessitt, E. , Dodge, L. , & MCCAED Team . (2016). Maudsley Service Manual for Child and Adolescent Eating Disorders . https://mccaed.slam.nhs.uk/wp-content/uploads/2019/11/Maudsley-Service-Manual-for-Child-and-Adolescent-Eating-Disorders-July-2016.pdf
- Eisler, I. , Simic, M. , Hodsoll, J. , Asen, E. , Berelowitz, M. , Connan, F. , … Landau, S. (2016). A pragmatic randomised multi‐Centre trial of multifamily and single family therapy for adolescent anorexia nervosa. BMC Psychiatry, 16(1), 422. 10.1186/s12888-016-1129-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engman‐Bredvik, S. , Carballeira Suarez, N. , Levi, R. , & Nilsson, K. (2016). Multi‐family therapy in anorexia nervosa—A qualitative study of parental experiences. Eating Disorders, 24(2), 186–197. 10.1080/10640266.2015.1034053 [DOI] [PubMed] [Google Scholar]
- Epstein, N. B. , Baldwin, L. M. , & Bishop, D. S. (1983). The McMasters family assessment device. Journal of Marital and Family Therapy, 9(2), 171–180. 10.1111/j.1752-0606.1983.tb01497.x [DOI] [Google Scholar]
- Fleming, C. , Le Brocque, R. , & Healy, K. (2020). How are families included in the treatment of adults affected by eating disorders? A scoping review. International Journal of Eating Disorders, 54, 244–279. 10.1002/eat.23441 [DOI] [PubMed] [Google Scholar]
- Gabel, K. , Pinhas, L. , Eisler, I. , Katzman, D. , & Heinmaa, M. (2014). The effect of multiple family therapy on weight gain in adolescents with anorexia nervosa: pilot data. Journal of the Canadian Academy of Child and Adolescent Psychiatry, 23(3), 196–199. [PMC free article] [PubMed] [Google Scholar]
- Geist, R. , Heinmaa, M. , Stephens, D. , Davis, R. , & Katzman, D. (2000). Comparison of family therapy and family group psychoeducation in adolescents with anorexia nervosa. Canadian Journal of Psychiatry, 45(2), 173–178. 10.1177/070674370004500208 [DOI] [PubMed] [Google Scholar]
- Gelin, Z. , Cook‐Darzens, S. , & Hendrick, S. (2018). The evidence base for multiple family therapy in psychiatric disorders: A review (part 1). Journal of Family Therapy, 40(3), 302–325. 10.1111/1467-6427.12178 [DOI] [Google Scholar]
- Gelin, Z. , Cook‐Darzens, S. , Simon, Y. , & Hendrick, S. (2016). Two models of multiple family therapy in the treatment of adolescent anorexia nervosa: A systematic review. Eating and Weight Disorders—Studies on Anorexia, Bulimia and Obesity, 21(1), 19–30. 10.1007/s40519-015-0207-y [DOI] [PubMed] [Google Scholar]
- Gelin, Z. , Fuso, S. , Hendrick, S. , Cook‐Darzens, S. , & Simon, Y. (2015). The effects of a multiple family therapy on adolescents with eating disorders: An outcome study. Family Process, 54(1), 160–172. 10.1111/famp.12103 [DOI] [PubMed] [Google Scholar]
- Goldberg, D. P. , & Williams, P. (1998). A User's guide to the general health questionnaire. Windsor: nferNelson., 1, 1–129. [Google Scholar]
- Gratz, K. L. , & Roemer, L. (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 14, 41–54. [Google Scholar]
- Hay, P. , Chinn, D. , Forbes, D. , Madden, S. , Newton, R. , Sugenor, L. , … Ward, W. (2014). Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for the treatment of eating disorders. Australian & New Zealand Journal of Psychiatry, 48(11), 977–1008. 10.1177/0004867414555814 [DOI] [PubMed] [Google Scholar]
- Heruc, G. , Hurst, K. , Casey, A. , Fleming, K. , Freeman, J. , Fursland, A. , … Wade, T. (2020). ANZAED eating disorder treatment principles and general clinical practice and training standards. Journal of Eating Disorders, 8(1), 63. 10.1186/s40337-020-00341-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilbert, A. , Hoek, H. W. , & Schmidt, R. (2017). Evidence‐based clinical guidelines for eating disorders: International comparison. Current Opinion in Psychiatry, 30(6), 423–437. 10.1097/YCO.0000000000000360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollesen, A. , Clausen, L. , & Rokkedal, K. (2013). Multiple family therapy for adolescents with anorexia nervosa: A pilot study of eating disorder symptoms and interpersonal functioning: Outcome of multiple family therapy. Journal of Family Therapy, 35, 53–67. 10.1111/1467-6427.12000 [DOI] [Google Scholar]
- Horowitz, L. M. , Rosenberg, S. E. , Baer, B. A. , Ureño, G. , & Villaseñor, V. S. (1988). Inventory of interpersonal problems: Psychometric properties and clinical applications. Journal of Consulting and Clinical Psychology, 56(6), 885–892. 10.1037/0022-006X.56.6.885 [DOI] [PubMed] [Google Scholar]
- Jewell, T. , & Lemmens, G. (2018). Multiple family therapy: Forever promising? Commentary on Gelin et al. (2018) and Cook‐Darzens et al. (2018), the evidence base for multiple family therapy in psychiatric and non‐psychiatric conditions: A review (parts 1 and 2). Journal of Family Therapy, 40(3), 344–348. 10.1111/1467-6427.12231 [DOI] [Google Scholar]
- Kaufman, E. , & Kaufmann, P. (1977). Multiple family therapy: A new direction in the treatment of drug abusers. The American Journal of Drug and Alcohol Abuse, 4(4), 467–478. 10.3109/00952997709007004 [DOI] [PubMed] [Google Scholar]
- Kazarian, S. S. , Malla, A. K. , Baker, B. , & Cole, J. D. (1990). Comparisons of two expressed emotion scales with the Camberwell family interview. Journal of Clinical Psychology, 46(3), 306–309. [DOI] [PubMed] [Google Scholar]
- Kinston, W. , & Loader, P. (1984). Eliciting whole‐family interaction with a standardized clinical interview. Journal of Family Therapy, 6(3), 347–363. 10.1046/j.1467-6427.1984.00655.x [DOI] [Google Scholar]
- Kinston, W. , & Loader, P. (1986). Preliminary psychometric evaluation of a standardized clinical family interview. Journal of Family Therapy, 8(4), 351–369. 10.1046/j..1986.00731.x [DOI] [Google Scholar]
- Knatz, S. , Murray, S. B. , Matheson, B. , Boutelle, K. N. , Rockwell, R. , Eisler, I. , & Kaye, W. H. (2015). A brief, intensive application of multi‐family‐based treatment for eating disorders. Eating Disorders, 23(4), 315–324. 10.1080/10640266.2015.1042318 [DOI] [PubMed] [Google Scholar]
- Kovacs, M. (1992). The Children's depression inventory (CDI). Toronto: Multi‐Health Systems. [Google Scholar]
- Lambert, M. J. , Burlingame, G. M. , Umphress, V. , Hansen, N. B. , Vermeersch, D. A. , Clouse, G. C. , & Yanchar, S. C. (1996). The reliability and validity of the outcome questionnaire. Clinical Psychology & Psychotherapy, 3(4), 249–258. [DOI] [Google Scholar]
- Laqueur, H. P. , Laburt, H. A. , & Morong, E. (1964). Multiple family therapy. Current Psychiatric Therapies, 4, 150–154. [PubMed] [Google Scholar]
- Lemmens, G. M. D. , Eisler, I. , Buysse, A. , Heene, E. , & Demyttenaere, K. (2009). The effects on mood of adjunctive single‐family and multi‐family group therapy in the treatment of hospitalized patients with major depression a 15‐month follow‐up study. Psychotherapy and Psychosomatics, 78(2), 98–105. 10.1159/000201935 [DOI] [PubMed] [Google Scholar]
- Lock, J. , & Le Grange, D. (2012). Treatment manual for anorexia nervosa: A family‐based approach (2nd ed.). New York: Guilford Press. [Google Scholar]
- Lock, J. (2018). Family therapy for eating disorders in youth. Current Opinion in Psychiatry, 31(6), 431–435. 10.1097/yco.0000000000000451 [DOI] [PubMed] [Google Scholar]
- Marzola, E. , Knatz, S. , Murray, S. B. , Rockwell, R. , Boutelle, K. , Eisler, I. , & Kaye, W. H. (2015). Short‐term intensive family therapy for adolescent eating disorders: 30‐month outcome: Short‐term intensive family therapy. European Eating Disorders Review, 23(3), 210–218. 10.1002/erv.2353 [DOI] [PubMed] [Google Scholar]
- McFarlane, W. R. (2002). Multifamily groups in the treatment of severe psychiatric disorders. New York & London: Guilford Press. [Google Scholar]
- Mehl, A. , Tomanová, J. , Kuběna, A. , & Papežová, H. (2013). Adapting multi‐family therapy to families who care for a loved one with an eating disorder in The Czech Republic combined with a follow‐up pilot study of efficacy: Multifamily therapy and eating disorders in Czech Republic. Journal of Family Therapy, 35, 82–101. 10.1111/j.1467-6427.2011.00579.x [DOI] [Google Scholar]
- Methley, A. M. , Campbell, S. , Chew‐Graham, C. , McNally, R. , & Cheraghi‐Sohi, S. (2014). PICO, PICOS and SPIDER: A comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Services Research, 14, 579. 10.1186/s12913-014-0579-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munn, Z. , Peters, M. D. J. , Stern, C. , Tufanaru, C. , McArthur, A. , & Aromataris, E. (2018). Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Medical Research Methodology, 18(1), 143. 10.1186/s12874-018-0611-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence (NICE) . (2017). Eating Disorders (NICE Guideline ng69 : https://www.nice.org.uk/guidance/ng69 [PubMed]
- Nazar, B. P. , Gregor, L. K. , Albano, G. , Marchica, A. , Coco, G. L. , Cardi, V. , & Treasure, J. (2017). Early response to treatment in eating disorders: A systematic review and a diagnostic test accuracy meta‐analysis: Early response to eating disorder treatment. European Eating Disorders Review, 25(2), 67–79. 10.1002/erv.2495 [DOI] [PubMed] [Google Scholar]
- Noyes, J. , Booth, A. , Moore, G. , Flemming, K. , Tunçalp, Ö. , & Shakibazadeh, E. (2019). Synthesising quantitative and qualitative evidence to inform guidelines on complex interventions: Clarifying the purposes, designs and outlining some methods. BMJ Global Health, 4(Suppl 1), e000893. 10.1136/bmjgh-2018-000893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters, M. D. J. , Godfrey, C. M. , Khalil, H. , McInerney, P. , Parker, D. , & Soares, C. B. (2015). Guidance for conducting systematic scoping reviews. International Journal of Evidence‐Based Healthcare, 13(3), 141–146. 10.1097/XEB.0000000000000050 [DOI] [PubMed] [Google Scholar]
- Peters, M. D. J. , Godfrey, C. M. , McInerney, P. , Munn, Z. , Tricco, A. C. , & Khalil, A. C. (2020). Chapter 11: Scoping reviews (2020 version). In Aromataris E. & Munn Z. (Eds.), JBI manual for evidence synthesis. JBI . https://doi.org/10.46658/JBIMES-20-12 [Google Scholar]
- Rienecke, R. D. (2020). Emotional Overinvolvement with adolescents: A problematic construct? Current Treatment Options in Psychiatry, 7(2), 162–185. 10.1007/s40501-020-00205-z [DOI] [Google Scholar]
- Rockwell, R. E. , Boutelle, K. , Trunko, M. E. , Jacobs, M. J. , & Kaye, W. H. (2011). An innovative short‐term, intensive, family‐based treatment for adolescent anorexia nervosa: Case series: Anorexia nervosa family therapy. European Eating Disorders Review, 19(4), 362–367. 10.1002/erv.1094 [DOI] [PubMed] [Google Scholar]
- Rosenberg, M. (1965). Society and the adolescent self‐image. Princeton, NJ: Princeton University Press. [Google Scholar]
- Russell, G. F. M. , Szmukler, G. I. , Dare, C. , & Eisler, I. (1987). An evaluation of family therapy in anorexia nervosa and bulimia nervosa. Archives of General Psychiatry, 44(12), 1047–1056. 10.1001/archpsyc.1987.01800240021004 [DOI] [PubMed] [Google Scholar]
- Salaminiou, E. (2005). Families in multiple family therapy for adolescent anorexia nervosa: Response to treatment experience and family and individual change (Ph.D., University of London, King's College). University of London, King's College, London, UK. ProQuest Dissertations & Theses Global (301637040). https://search.proquest.com/docview/301637040?accountid=11862
- Salaminiou, E. , Campbell, M. , Simic, M. , Kuipers, E. , & Eisler, I. (2017). Intensive multi‐family therapy for adolescent anorexia nervosa: An open study of 30 families: Multi‐family therapy for adolescent anorexia nervosa. Journal of Family Therapy, 39(4), 498–513. 10.1111/1467-6427.12075 [DOI] [Google Scholar]
- Schmidt, U. , & Treasure, J. (2006). Anorexia nervosa: Valued and visible. A cognitive‐interpersonal maintenance model and its implications for research and practice. British Journal of Clinical Psychology, 45(3), 343–366. 10.1348/014466505x53902 [DOI] [PubMed] [Google Scholar]
- Scholz, M. , Rix, M. , Scholz, K. , Gantchev, K. , & Thömke, V. (2005). Multiple family therapy for anorexia nervosa: Concepts, experiences and results. Journal of Family Therapy, 27(2), 132–141. 10.1111/j.1467-6427.2005.00304.x [DOI] [Google Scholar]
- Scholz, M. , & Asen, E. (2001). Multiple family therapy with eating disordered adolescents: Concepts and preliminary results. European Eating Disorders Review, 9(1), 33–42. 10.1002/erv.364 [DOI] [Google Scholar]
- Sepulveda, A. R. , Whitney, J. , Hankins, M. , & Treasure, J. (2008). Development and validation of an eating disorders symptom impact scale (EDSIS) for carers of people with eating disorders. Health and Quality of Life Outcomes, 6(1), 28. 10.1186/1477-7525-6-28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simic, M. , Baudinet, J. , Blessitt, E. , Wallis, A. , & Eisler, I. (2021). Multi‐family therapy for anorexia nervosa: A treatment manual (1st ed.). London, UK: Routledge. 10.4324/9781003038764 [DOI] [Google Scholar]
- Simic, M. , & Eisler, I. (2015). Multi‐family therapy. In Loeb K. L., Le Grange D., & Lock J. (Eds.), Family therapy for adolescent eating and weight disorders (1st ed., pp. 110–138). New York: Imprint Routledge. [Google Scholar]
- Skarbø, T. , & Balmbra, S. M. (2020). Establishment of a multifamily therapy (MFT) service for young adults with a severe eating disorder—Experience from 11 MFT groups, and from designing and implementing the model. Journal of Eating Disorders, 8(101610672), 9. 10.1186/s40337-020-0285-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slagerman, M. , & Yager, J. (1989). Multiple family group treatment for eating disorders: A short term program. Psychiatric Medicine, 7(4), 269–283. [PubMed] [Google Scholar]
- Spielberger, C. , Gorsuch, R. , & Lushene, R. (1970). STAI manual for the state trait anxiety inventory. Palo Alto, CA: Consulting Psychologists Press. [Google Scholar]
- Stewart, C. S. , Baudinet, J. , Hall, R. , Fiska, M. , Pretorius, N. , Voulgari, S. , … Simic, M. (2019). Multi‐family therapy for bulimia nervosa in adolescence: A pilot study in a community eating disorder service. Eating Disorders, 9315161, 1–17. 10.1080/10640266.2019.1656461 [DOI] [PubMed] [Google Scholar]
- Stewart, C. , Voulgari, S. , Eisler, I. , Hunt, K. , & Simic, M. (2015). Multi‐family therapy for bulimia nervosa in adolescence. Eating Disorders, 23(4), 345–355. 10.1080/10640266.2015.1044348 [DOI] [PubMed] [Google Scholar]
- Struening, E. L. , Perlick, D. A. , Link, B. G. , Hellman, F. , Herman, D. , & Sirey, J. A. (2001). Stigma as a barrier to recovery: The extent to which caregivers believe Most people devalue consumers and their families. Psychiatric Services, 52(12), 1633–1638. 10.1176/appi.ps.52.12.1633 [DOI] [PubMed] [Google Scholar]
- Szmukler, G. I. , Burgess, P. , Herrman, H. , Benson, A. , Colusa, S. , & Bloch, S. (1996). Caring for relatives with serious mental illness: The development of the experience of caregiving inventory. Social Psychiatry and Psychiatric Epidemiology, 31(3–4), 137–148. 10.1007/BF00785760 [DOI] [PubMed] [Google Scholar]
- Tantillo, M. , McGraw, J. S. , Hauenstein, E. J. , & Groth, S. W. (2015). Partnering with patients and families to develop an innovative multifamily therapy group treatment for adults with anorexia nervosa. Advances in Eating Disorders, 3(3), 269–287. 10.1080/21662630.2015.1048478 [DOI] [Google Scholar]
- Tantillo, M. , McGraw, J. S. , Lavigne, H. M. , Brasch, J. , & Le Grange, D. (2019). A pilot study of multifamily therapy group for young adults with anorexia nervosa: Reconnecting for recovery. The International Journal of Eating Disorders, 52(8), 950–955. 10.1002/eat.23097 [DOI] [PubMed] [Google Scholar]
- Tantillo, M. , McGraw, J. S. , & Le Grange, D. (2020). Multifamily therapy Group for Young Adults with anorexia nervosa: Reconnecting for recovery (1st ed.). London, UK: Routledge. [DOI] [PubMed] [Google Scholar]
- Treasure, J. , Parker, S. , Oyeleye, O. , & Harrison, A. (2021). The value of including families in the treatment of anorexia nervosa. European Eating Disorders Review, 29(3), 393–401. 10.1002/erv.2816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treasure, J. , Whitaker, W. , Todd, G. , & Whitney, J. (2011). A description of multiple family workshops for carers of people with anorexia nervosa. European Eating Disorders Review, 20(1), e17–e22. 10.1002/erv.1075 [DOI] [PubMed] [Google Scholar]
- Tricco, A. C. , Lillie, E. , Zarin, W. , O'Brien, K. K. , Colquhoun, H. , Levac, D. , … Straus, S. E. (2018). PRISMA extension for scoping reviews (PRISMA‐ScR): Checklist and explanation. Annals of Internal Medicine, 169(7), 467–473. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- Vall, E. , & Wade, T. D. (2015). Predictors of treatment outcome in individuals with eating disorders: A systematic review and meta‐analysis: Predictors of treatment outcomes in individuals with eating disorders. International Journal of Eating Disorders, 48(7), 946–971. 10.1002/eat.22411 [DOI] [PubMed] [Google Scholar]
- Voriadaki, T. , Simic, M. , Espie, J. , & Eisler, I. (2015). Intensive multi‐family therapy for adolescent anorexia nervosa: Adolescents' and parents' day‐to‐day experiences: Day‐to‐day experience in MFT for anorexia nervosa. Journal of Family Therapy, 37(1), 5–23. 10.1111/1467-6427.12067 [DOI] [Google Scholar]
- Wallin, U. (2007). Multi‐family therapy with anorexia nervosa. A treatment manual. Lund: Lund University. [Google Scholar]
- Wallin, U. (2011). Multifamiljeterapi vid anorexia nervosa [multifamily therapy of anorexia nervosa]. Lund, Sweden: Behandlingsmanual. [Google Scholar]
- Wenniger, W. F. M. D. B. , Hageman, W. J. J. M. , & Arrindell, W. A. (1993). Cross‐national validity of dimensions of family functioning: First experiences with the Dutch version of the McMaster family assessment device (FAD). Personality and Individual Differences, 14(6), 769–781. 10.1016/0191-8869(93)90090-P [DOI] [Google Scholar]
- Whitney, J. , Currin, L. , Murray, J. , & Treasure, J. (2012). Family work in anorexia nervosa: A qualitative study of Carers' experiences of two methods of family intervention. European Eating Disorders Review, 20(2), 132–141. 10.1002/erv.1077 [DOI] [PubMed] [Google Scholar]
- Whitney, J. , Murphy, T. , Landau, S. , Gavan, K. , Todd, G. , Whitaker, W. , & Treasure, J. (2012). A practical comparison of two types of family intervention: An exploratory RCT of family day workshops and individual family work as a supplement to inpatient Care for Adults with anorexia nervosa. European Eating Disorders Review, 20(2), 142–150. 10.1002/erv.1076 [DOI] [PubMed] [Google Scholar]
- Wiedemann, G. , Rayki, O. , Feinstein, E. , & Hahlweg, K. (2002). The family questionnaire: Development and validation of a new self‐report scale for assessing expressed emotion. Psychiatry Research, 109(3), 265–279. 10.1016/S0165-1781(02)00023-9 [DOI] [PubMed] [Google Scholar]
- Wierenga, C. E. , Hill, L. , Knatz Peck, S. , McCray, J. , Greathouse, L. , Peterson, D. , … Kaye, W. H. (2018). The acceptability, feasibility, and possible benefits of a neurobiologically‐informed 5‐day multifamily treatment for adults with anorexia nervosa. The International Journal of Eating Disorders, 51(8), 863–869. 10.1002/eat.22876 [DOI] [PubMed] [Google Scholar]
- Wiseman, H. , Ensoll, S. , Russouw, L. , & Butler, C. (2019a). Implementing multi‐family therapy within a community eating disorder Service for Children and Young People. Journal of Systemic Therapies, 38(3), 50–66. 10.1521/jsyt.2019.38.3.50 [DOI] [Google Scholar]
- Wiseman, H. , Ensoll, S. , Russouw, L. , & Butler, C. (2019b). Multi‐family therapy for young people with anorexia nervosa: Clinicians' and carers' perspectives on systemic changes. Journal of Systemic Therapies, 38(3), 67–83. 10.1521/jsyt.2019.38.3.67 [DOI] [Google Scholar]
- Wooley, S. C. , & Lewis, K. G. (1987). Multi‐family therapy within an intensive treatment program for bulimia. Harkaway (Ed.) In J., Eating Disorders: The family therapy collections, 20, (pp. 12–24). Rockville: Aspen Publishers. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1: Supporting Information
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study


